- 1Department of Epidemiology and Biostatistics, Addis Continental Institute of Public Health, Addis Ababa, Ethiopia
- 2Division of Biology and Medicine, Warren Alpert Medical School of Brown University, Providence, RI, United States
- 3Department of Pediatrics, Brigham and Women’s Hospital, Boston, MA, United States
- 4Harvard Medical School, Boston, MA, United States
- 5Department of Reproductive Health and Population, Addis Continental Institute of Public Health, Addis Ababa, Ethiopia
- 6Department of Global Health and Health Policy, Addis Continental Institute of Public Health, Addis Ababa, Ethiopia
- 7Department of Nutrition and Behavioural Sciences, Addis Continental Institute of Public Health, Addis Ababa, Ethiopia
- 8Addis Continental Institute of Public Health, Bahir Dar, Ethiopia
- 9Addis Continental Institute of Public Health, Addis Ababa, Ethiopia
- 10Addis Ababa University College of Health Science, Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia
- 11Department of Human Development, Teachers College, Columbia University, New York, NY, United States
- 12Boston Children’s Hospital, Boston, MA, United States
- 13Department of Child and Adolescent Psychiatry, New York University Grossman School of Medicine, New York, NY, United States
- 14Center for Neonatal Research, Children’s Hospital of Orange County, California, CA, United States
Background: Magnetic resonance imaging (MRI) and electroencephalography (EEG) are valuable tools for studying neuroanatomical and electrophysiological features of early brain development. Studies implementing neuroimaging tools in low- and middle-income countries are still rare, and there is limited data on the acceptability of such tools among rural communities. The present study explores the perceptions, feasibility, and acceptability of introducing MRI and EEG for child development research in the rural Amhara region of Ethiopia.
Methods: A total of 40 in-depth interviews were conducted among community members (n = 24) and clinicians (n = 16). A semi-structured interview included four themes: (1) Baseline imaging knowledge, (2) Perceptions of MRI and EEG, (3) Facilitators and barriers to acceptability of MRI and EEG, and (4) Recommendations to improve MRI and EEG uptake. Interviews were conducted in Amharic, the local language. All interviews were transcribed verbatim to Amharic, translated into English, and double-coded. We used thematic analysis to organize data according to predefined and emerging themes.
Results: Knowledge of MRI and EEG was limited, and none of the community members had previous experiences with either technology. Broadly, participants responded positively to our introductory videos showing MRI and EEG acquisition and expressed high levels of acceptability. However, participants reported concerns about possible harms related to radiation, electrical shock, and injury from MRI/EEG procedures. Those with lesser education were identified to be less accepting of MRI/EEG. In addition, several mothers expressed that consent from their husbands was necessary for their child’s participation in neurodevelopmental research. Potential logistical barriers identified included transportation challenges to the neuroimaging study sites, especially for rural-dwelling families. Creating awareness, using explanatory videos, and engaging community members and clinicians were recommended to facilitate acceptance of EEG and MRI.
Conclusion: In this formative study, MRI and EEG were viewed as acceptable methods for assessing child neurodevelopment in rural areas of Ethiopia. Community members’ and clinicians’ views were impacted largely by social, religious, educational, and logistical aspects. Concerns related to MRI radiation, electrical shock, and injuries from EEG can be addressed through awareness creation and education. Engaging community leaders and healthcare providers is key to improving acceptability.
Introduction
In low-and middle-income countries (LMICs), approximately 250 million children under 5 years of age are at risk of not achieving their full developmental potential and failing to meet expected cognitive or socio-developmental milestones (1, 2). This increased risk of developmental delay in low-income settings can affect human capital and productivity into adulthood (3). A majority of developmental delays among children in LMICs remain unidentified, precluding children from accessing necessary health services and early developmental interventions (1). Magnetic resonance imaging (MRI) and electroencephalography (EEG) can help characterize the anatomy and function of the developing brain and aid in the early identification of infants at risk for developmental delays (4, 5). These techniques are generally non-invasive, safe, and well-tolerated in children in Western contexts (5–8). However, neurodevelopmental studies implementing well-established neuroimaging techniques such as MRI and EEG have been largely restricted to high-income countries (1, 8). Historically, the use of neuroimaging methods has been limited by cost factors and the lack of access/availability in developing countries (4). Recent developments of cost-effective and portable neuroimaging devices, such as point-of-care MRI systems and portable EEG devices, are poised to benefit research in LMICs by providing a cost-effective method for assessing neurodevelopment (6–9). Thus, implementing low-cost and accessible imaging devices will aid in characterizing neurodevelopmental trajectories and identifying potential delays and may allow for early diagnosis and intervention, ultimately improving developmental outcomes (6).
The lack of familiarity with neuroimaging modalities such as MRI or EEG may lead to difficulty in implementing these neuroimaging methods in rural LMICs due to a lack of community acceptability. A study in India that examined the acceptability and feasibility of administering EEG in rural communities showed initial parental hesitancy to consent due to concern that the device could harm their children (9). Other studies in LMICs emphasized the importance of working with parents and local community members to gain acceptance when implementing novel imaging devices (10). As cultural values can influence how new technologies are understood and adopted, it is important to explore local communities’ perspectives, levels of awareness, and acceptability before introducing new technologies to ensure community buy-in and engagement. Prior to the introduction of MRI and EEG technology for a research study in a rural community in Amhara, Ethiopia (NCT06296238), we conducted a qualitative study to explore the feasibility and acceptability of neuroimaging techniques (MRI and EEG) for assessing child neurodevelopment among community members and clinicians.
Materials and methods
We conducted semi-structured, in-depth interviews (IDI) between September and October 2022 to inform the introduction of MRI and EEG in Amhara, Ethiopia, and the development of educational materials for the Impact of Maternal Antenatal Nutrition and Infection Treatment Interventions on Longitudinal Infant Development and Growth (“LIDG”) longitudinal child follow-up study in rural Ethiopia (NCT06296238) (11). The LIDG study follows infants born to mothers enrolled in the Enhancing Nutrition and Antenatal Infection Treatment (“ENAT”) cluster randomized trial (ISRCTN15116516) (12). The LIDG study aims to examine the effects of prenatal nutrition and infection management interventions on offspring’s long-term growth and neurodevelopmental outcomes.
Study site
This formative study was conducted in four selected health centers involved in the ENAT study in the West Gojjam and South Gondar zones (12), and two health centers and a comprehensive referral hospital in Bahir Dar, the regional capital of the Amhara region. The comprehensive referral hospital provides imaging services that include both MRI and EEG.
Study design, participants, and sampling procedures
This study used a qualitative approach to assess MRI and EEG knowledge, perceptions, and acceptability with key informant interviews. We used a purposive sampling procedure to identify study participants. Among community members, we interviewed two mothers who had children two years or younger at each health center. We also interviewed other community members, including fathers, religious leaders, women development armies, and community administrators. Among clinicians, we interviewed health center directors, nurses, and health officers working at the pediatric outpatient department at each health center, as well as radiography technologists, pediatricians, and EEG nurses at the referral hospital. To be eligible, clinicians needed to have more than 2 years of experience working in the study area, and be currently providing child health services to communities of the selected health center, be the director of the health center, or have previous imaging experience (for hospital staff). This purposive selection of participants enabled us to gather detailed information about the feasibility and acceptability of the new technologies in rural areas. The information obtained from the IDIs helped develop a community-guided and acceptable strategy for introducing neurodevelopmental assessments, including MRI and EEG, in the rural population of Amhara.
Participant recruitment
Written informed consent was obtained for all study participants. For those with limited literacy, a witness who was either a family member (if in attendance) or study staff read the consent form, and participants provided thumbprints to consent to their participation. We based our sample size on the principle of saturation (13). Drawing on our previous experience in this study area and population, we anticipate that a sample size of 10–15 participants per group will be sufficient to achieve both code and meaning saturation, allowing for a thorough exploration and characterization of key issues and themes (13–17).
Data collection
A semi-structured interview guide was developed based on existing literature to capture the main themes related to community awareness, perceptions, and acceptability of MRI and EEG in research assessing child development. Clinicians were also interviewed about their prior experiences and the feasibility of implementing MRI and EEG at the health centers and the hospital. The interview guides were developed in English and translated into Amharic, the local language of the study area. Interviews were conducted face-to-face by research staff who had master’s level training in public health as well as relevant experience in qualitative data collection techniques, analysis, and write-up. Research staff were paired when conducting interviews. All IDIs took place on the premises of the selected health facilities in a private location and focused on 4 main themes. The first theme was regarding participants’ prior experience with imaging. Participants then watched a five-minute introductory video, after which they were interviewed about their perceptions of MRI and EEG (Theme 2) and the facilitators and barriers influencing their acceptability of these technologies (Theme 3). The introductory video described the benefits, potential harms, and procedures of the Hyperfine MRI machine and EEG device used for the study. The fourth theme focused on participant, recommendations to improve the uptake of MRI and EEG within their community. To minimize the burden, clinicians were interviewed at a convenient time when the patient load was lighter. With the participant’s permission, the interviews were recorded using digital audio recorders along with interview notes. The interviews took an average of 45 minutes.
Data analysis
The interviews were transcribed verbatim in Amharic and translated into English for analysis. Data were analyzed using thematic analysis (18). Four themes were pre-defined based on specific questions developed a priori to examine the (1) baseline imaging knowledge, (2) perceptions of MRI and EEG (3) facilitators and barriers to acceptability of MRI and EEG, as well as (4) recommendations to improve MRI and EEG uptake. In the familiarization phase, three independent researchers (FW, KY, and TC) reviewed all full-text translations and identified codes line by line using both inductive and deductive approaches. All translations were double-coded. Microsoft Excel was used for coding, grouping themes and categories within our larger topic areas, and conducting synthesis. The results of this initial coding process were compared and agreement was reached on the overall thematic framework. Illustrative quotations were integrated with the narrative description of the study findings.
Ethical considerations
The study was approved by the institutional review boards of Addis Continental Institute of Public Health (Addis Ababa, Ethiopia) (ACIPH/IRB/002/2022) and Massachusetts General Brigham (Boston, Massachusetts, United States) (2023P000461). Support letters were obtained from Amhara Public Health Institute (Bahir Dar, Amhara, Ethiopia), and permission was obtained from the zonal health departments, health centers, and the referral hospital. We obtained informed written consent from all the participants after providing detailed information on the purpose of the study. Participant responses, recordings, and data were kept anonymous and no names were recorded. Participants were not compensated and did not directly benefit from study participation. Participants were not directly informed of the study results, but the findings were presented at each of the study health centers.
Results
Participant characteristics
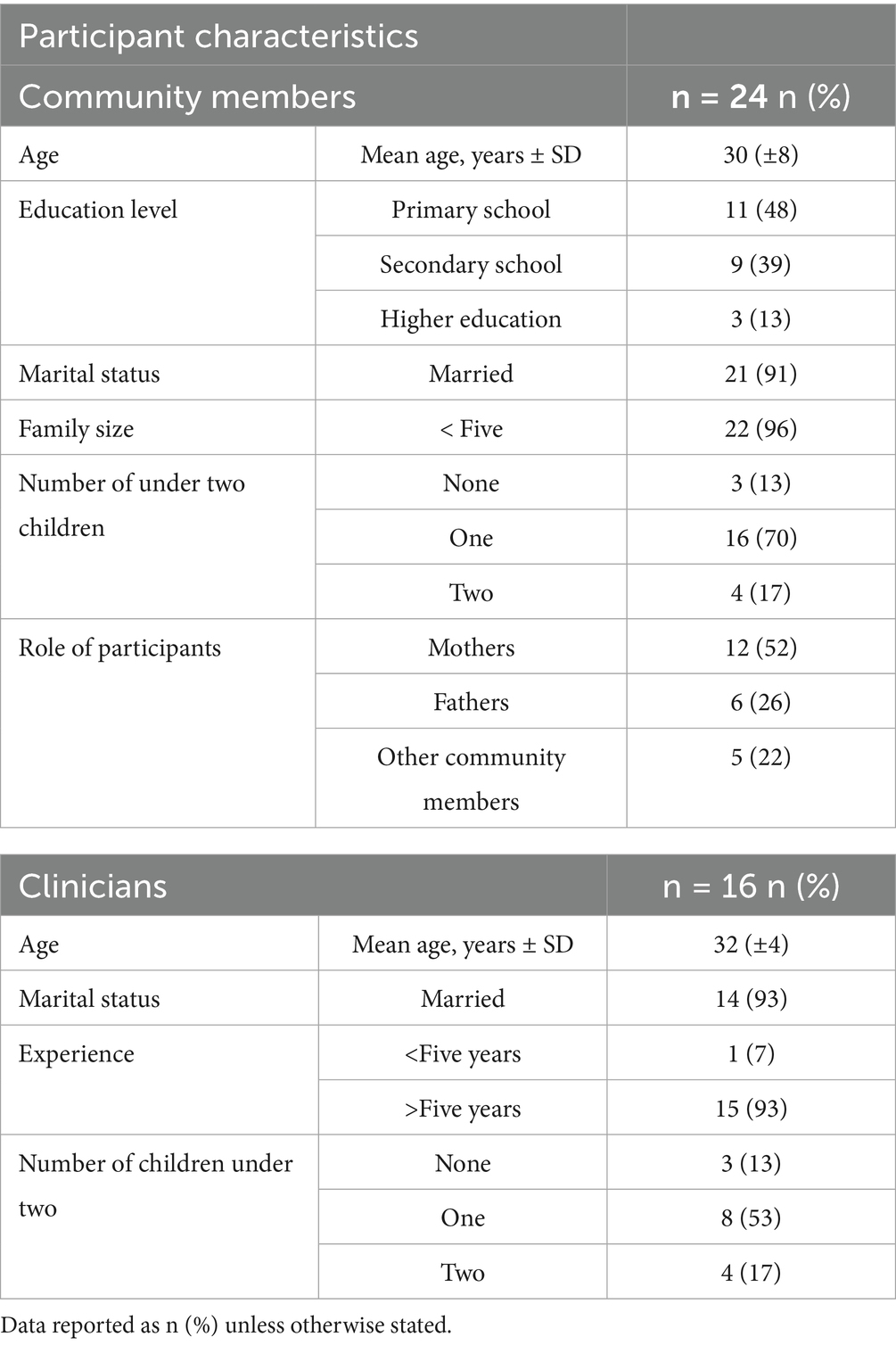
Our study sample (Table 1) included 24 community members (12 mothers, 6 fathers, and 6 community representatives) and 16 clinicians (two health officers, nine nurses, one EEG nurse, and two radiography technologists). Approximately 50% of the community members had completed primary education. Most clinicians had more than five years of professional experience, which may have helped them gain a deeper perspective on neuroimaging technologies.
Themes and subthemes
Theme 1: Baseline imaging knowledge
All community members had some prior familiarity with medical imaging, primarily X-ray and ultrasonography. CT scanning and MRI were mentioned by only four participants, all of whom had higher levels of education or resided in the regional capital with higher likelihood of being exposed to media advertisements and other sources of information (e.g., the Internet, social media). The primary sources of imaging knowledge were self-experience and from other individuals such as family members. All mothers mentioned having an ultrasound during prenatal care at nearby health facilities. Additionally, three community members mentioned personally having had an X-ray. The other community members noted that they were exposed to information related to X-rays and ultrasounds during their visits to the health centers. Whereas no community members were familiar with EEG, MRI was mentioned by two mothers and one community member, all of whom were residing in Bahir Dar.
Clinicians who work at the health centers had heard about MRI and EEG during their clinical training. However, none had observed the procedures or were aware of their availability within Ethiopia. The hospital radiography technicians had experience conducting other imaging techniques (e.g. CT, X-ray), but not MRI. Except for one nurse, all other clinicians were new to EEG procedure being conducted either at a health center or hospital.
Theme 2: Perceptions of MRI and EEG
After watching the introductory video, community members and clinicians were asked about their perceptions of MRI and EEG. Community members and clinicians had positive attitudes toward both of these neuroimaging methods for clinical and research use. Additionally, they expressed positive feelings and perceived neuroimaging as potentially helpful for monitoring children’s growth and development. Clinicians perceived the Hyperfine MRI as safe for infants and children given the very low magnetic field and low sound intensity, and were pleased about the young age of infant scanning allowed. Clinicians also perceived the EEG to be easier than the MRI since it would be conducted while children are awake and sitting on their mother’s lap, which was believed to minimize anxiety in the mothers. However, some concerns and misconceptions were also raised regarding the safety of MRI and EEG. In particular, community members and health center clinicians were concerned about potential exposure to radiation and risk for epilepsy with having an MRI, as well as possible electric shock for EEG. For MRI, concerns were raised about possible adverse outcomes if the baby woke up during the MRI procedure, and whether the mother would be accompanying the child during the scan. For EEG, the concerns were related to whether the cap would be worn for a long duration. Another concern shared was the treatment and management plan if any abnormalities were detected during the scans. The perceptions and concerns of community members and clinicians about MRI and EEG after the are summarized below in Table 2, along with representative quotes.
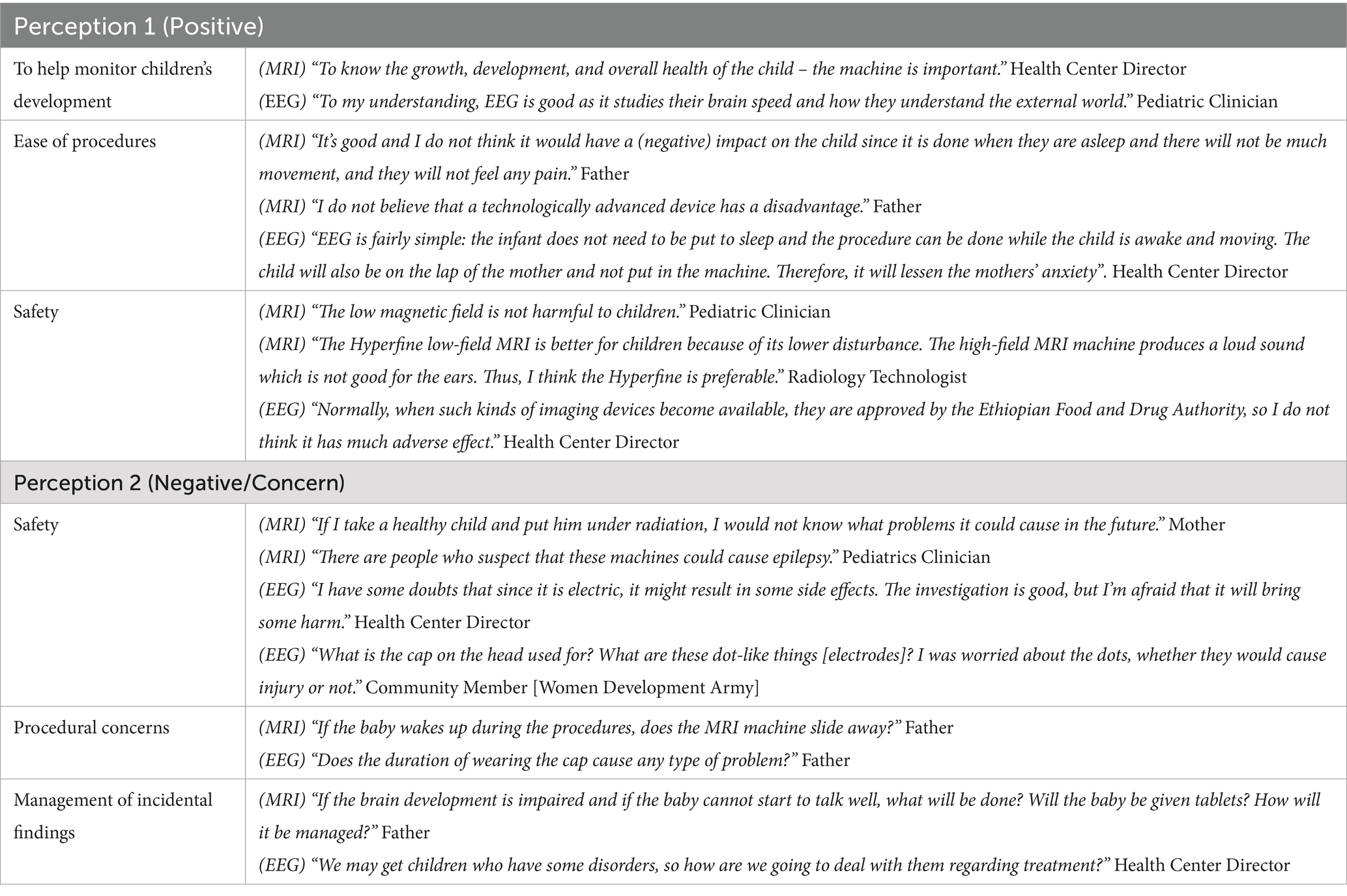
Table 2. Representative quotes regarding perceptions of MRI and EEG from community members and clinicians.
Theme 3: Facilitators and barriers to acceptability of MRI and EEG
A majority of participants felt that MRI and EEG procedures would be acceptable for children and families in the community. During interviews, participants were prompted on factors that may influence the acceptability of MRI and EEG use for research on healthy children in their community. Several participants reported that individuals with lower education may be less accepting of MRI and EEG due to a limited understanding of the procedures. By contrast, several clinicians suggested that those with lower education would be more trusting of recommendations from their clinicians and thus more accepting of MRI and EEG, whereas those with higher education may be more likely to challenge the use of MRI and EEG on their healthy children for research purposes. Logistical factors, including lack of transportation and job demands, especially among rural-dwelling families, were identified as possible barriers to acceptability. Several participants also reported that mothers may require permission from their husbands prior to their children undergoing MRI or EEG. Finally, religion may also influence the acceptability of MRI and EEG among community members. Those who are religious may be less accepting of MRI and EEG due to beliefs that their child’s development is determined by God and additional investigations may not be necessary. However, religious leaders may play a role in encouraging community members, which may aid in improving the uptake of MRI and EEG. Representative quotes summarizing identified barriers and facilitators of acceptability are shown in Table 3.
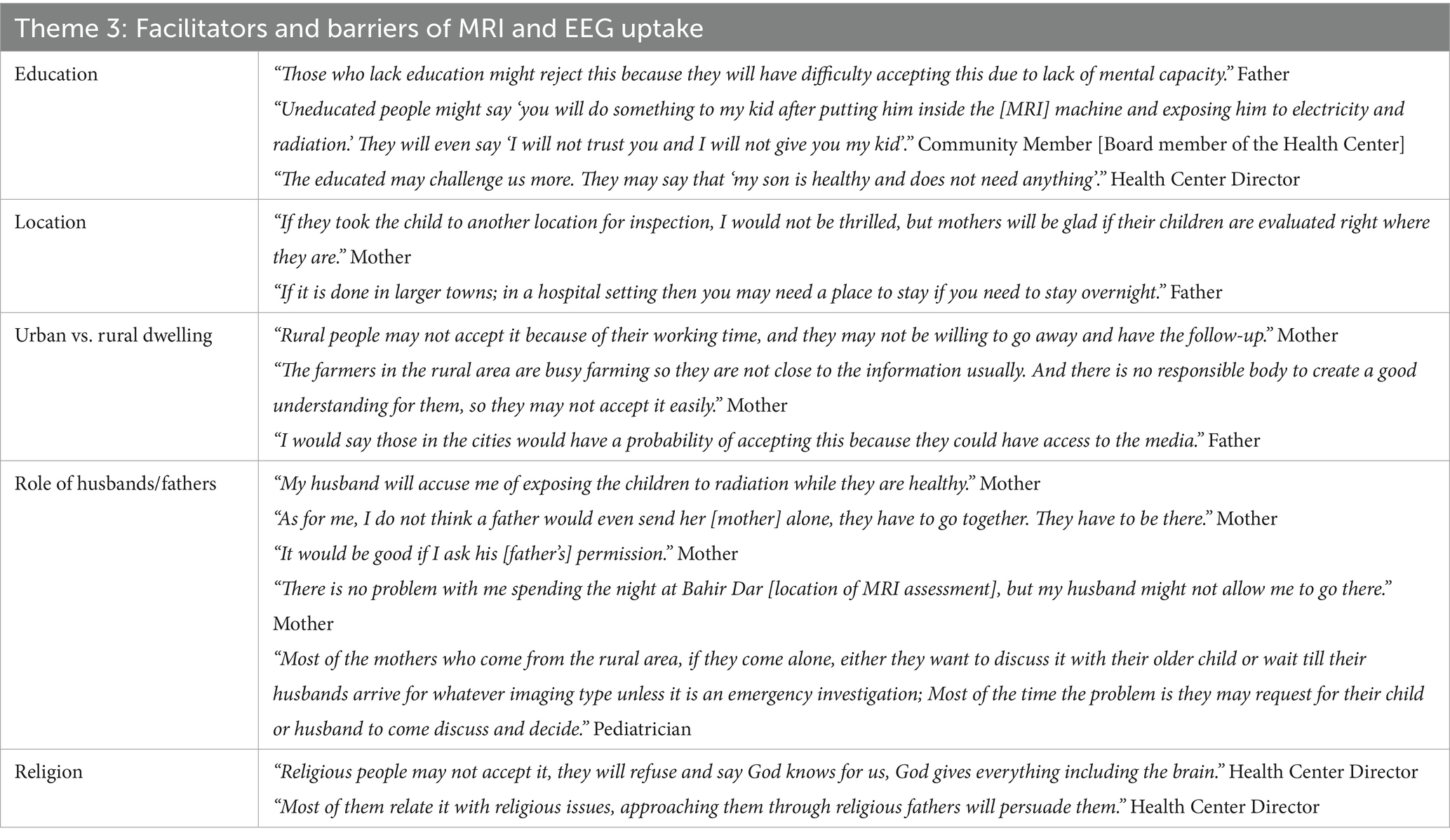
Table 3. Representative quotes summarizing facilitators and barriers to acceptability of MRI and EEG.
Theme 4: Recommendation to improve MRI and EEG uptake
Participants made numerous recommendations to facilitate the community’s acceptance of MRI and EEG, revolving mainly around broadening the introductory video, community mobilization activities, and engaging clinicians and community leaders.
• Introductory video: Develop a comprehensive video that includes the purpose, benefits, potential risks, and side effects of MRI and EEG procedures for the child, as well as the process for result notification and follow-up care. Clear, contextually relevant examples tailored to the community’s level of understanding can improve comprehension and facilitate acceptance by the community.
• Awareness creation activities: Organizing health education sessions at the health center or community gatherings to educate the community using multiple approaches such as presentations, or the distribution of informational flyers, can facilitate community education. Additionally, broader dissemination of the information through local broadcasting channels may help to reach a broader population and create awareness.
• Engagement of community leaders: Engaging key figures in the community, including local administration and religious leaders, would enhance acceptability.
• Engaging clinicians: The community demonstrated a high level of trust in clinicians and it was noted that their participation in educational sessions would improve acceptance of the procedures.
• Logistics: Facilitation of transportation and lodging arrangements to address the needs of the family was mentioned as important to enable participation
Discussion
This paper discusses the findings from a formative study conducted as part of the LIDG infant follow-up study to examine the first-time implementation of MRI and EEG for research in rural Ethiopia (11). Community members and clinicians had positive perceptions and high levels of acceptability, driven by a desire to learn about a child’s development. The main concerns were related to possible harms from radiation from MRI, and electrical shock and injuries from EEG. Creating community awareness will help address these concerns. Additionally, the engagement of key community members and healthcare providers would be important for improving the acceptance of these new technologies in rural areas.
Our study showed that community members were familiar with the two commonly used imaging devices, ultrasound and X-ray, but not MRI and EEG. Similar to previous studies, knowledge of ultrasound was mainly related to familiarity, as community members – especially women – mentioned prenatal care as the main source of knowledge for an ultrasound (19). Understanding previous knowledge of imaging (ultrasound and X-ray) gained through different sources helped establish a baseline for introducing new technologies in rural areas. This existing knowledge can be leveraged to build trust and address concerns about more advanced imaging through targeted educational efforts, using ultrasound and X-ray as a relatable reference to improve acceptability.
The present study highlights positive perceptions of neuroimaging research for assessing child growth and development among community members and clinicians. A similar qualitative research found that parents viewed neuroimaging positively if it centered on medical benefits and comfort (20). Despite broadly positive responses, interviews revealed possible therapeutic misconceptions, where participants mistake participation in research using MRI and EEG as clinical care. Findings emphasize previous recommendations to establish clear guidelines to address potential misconceptions by offering participants opportunities to ask questions, communicating the broader purpose of research, and emphasizing that participation in research does not substitute clinical care or confer any direct benefits (21).
The concerns and misunderstandings raised were related to the safety of the machines and fear of possible adverse effects on their children’s health. The Healthy Brain and Child Development study revealed that, even though parents were familiar with MRI, their knowledge about the safety of the procedure was minimal, with only half of the participants understanding MRI was safe for babies (22). Misperceptions that MRI would expose their children to harmful radiation were also reported in a study conducted in Nepal, where 85.5% of the study participants perceived that MRI uses harmful ionizing radiation like radiography and CT scanning (22, 23). Such misperceptions likely stemmed from the study participants’ medical imaging knowledge being limited to general imaging tools such as X-ray which are known to present risks of radiation. A study that assessed children’s and parents’ perception of MRI after examination also noted that parents felt anxious because of the limited information they received beforehand (24). Therefore, providing detailed and accurate information about the safety of MRI and EEG may help minimize these concerns (24, 25).
Several factors were identified as possible barriers to MRI and EEG. Most participants believed that those with lower education are less likely to accept MRI and EEG due to limited understanding and awareness of neuroimaging procedures. However, clinicians involved in the present study expressed that those with lower education may be more likely to trust recommendations provided by medical professionals. Together, these findings support conclusions from previous work on the importance of participant education regarding the procedures, as well as community sensitization and strengthening of local partnerships via the engagement of key community representatives to create greater awareness of MRI and EEG (21). Consistent with previous reports examining EEG acceptability in India, logistical factors such as lack of transportation may serve as a barrier to participation, particularly for families in rural areas (1). Further, communities in the rural areas are largely composed of farmers, and demands of these professions may prohibit attendance to MRI or EEG research visits. Additionally, approval from husbands was brought up as a critical factor for mothers’ ability to consent to their child’s participation in MRI and EEG. Relative to individualistic cultures in Western study settings, it is common practice for husbands to make healthcare decisions in the family-oriented cultures that are predominant in LMICs.
Engaging local stakeholders, doing formative work, and designing studies based on the formative work are crucial to understand community acceptability of MRI and EEG. Based on the findings of this formative study, we refined educational materials and the consenting protocol before study initiation. Specifically, existing introductory videos included additional comprehensive information regarding the safety of MRI and EEG on children. Additional descriptions of the misconceptions related to procedural safety were also included in the video. Leveraging these recommendations during the study, consent rates for MRI/EEG were high (>80%) for the LIDG infant follow-up study (11).
A key strength of this study is the inclusion of a diverse group of community members, including fathers, who are historically underrepresented in child development literature; community influencers, such as religious leaders; and clinicians who play essential roles in rural Ethiopian communities. This allowed us to capture detailed, personal perceptions and diverse perspectives, providing a deeper understanding of the acceptability and feasibility of MRI and EEG in rural areas. Limitations of the study include possible self-report bias. Participants may have overstated or understated their views about neuroimaging technologies due to social desirability.
Conclusion
In conclusion, our study highlighted the overall acceptability and positive perception of MRI and EEG for neurodevelopmental assessment in children in rural Ethiopian communities. The perception and acceptability of MRI and EEG among community members and clinicians were influenced by various social, religious, educational, and logistical factors. While most participants expressed positive views of MRI and EEG, concerns about possible harms and side effects–including MRI radiation, electric shock from EEG, and discomfort from EEG caps–were notable. Addressing these concerns with targeted awareness-creation and educational activities is important. It is recommended that future neuroimaging research in LMIC prioritize engaging community leaders and healthcare providers to build trust and enhance the acceptability of these technologies in similar settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Boards of Addis Continental Institute of Public Health (Addis Ababa, Ethiopia) (ACIPH/IRB/002/2022) and Massachusetts General Brigham (Boston, Massachusetts, United States) (2023P000461). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FW: Data curation, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. TC: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. KY: Data curation, Formal analysis, Supervision, Writing – original draft, Writing – review & editing. KN: Writing – review & editing. NF: Writing – review & editing. WT: Supervision, Writing – review & editing. BA: Supervision, Writing – review & editing. SM: Data curation, Writing – review & editing. GA: Writing – review & editing. AT: Writing – review & editing. ST-R: Writing – review & editing. SJ: Writing – review & editing. MT: Writing – review & editing. TI: Writing – review & editing. CN: Writing – review & editing. AW: Writing – review & editing. AL: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing. YB: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Institute of Child Health and Development (R01HD106106 and R01HD1067475) and the Bill and Melinda Gates Foundation (INV-045894).
Acknowledgments
We sincerely thank the study participants for their willingness to participate in this study. We also thank Aditi Luitel for her support of the data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lockwood Estrin, G, Bhavnani, S, Goodwin, A, Arora, R, Divan, G, Haartsen, R, et al. From the lab to the field: acceptability of using electroencephalography with Indian preschool children. Wellcome Open Res. (2023) 7:99. doi: 10.12688/wellcomeopenres.17334.2
2. Lu, C, Black, MM, and Richter, LM. Risk of poor development in young children in low-income and middle-income countries: an estimation and analysis at the global, regional, and country level. Lancet Glob Health. (2016) 4:e916–22. doi: 10.1016/S2214-109X(16)30266-2
3. Gil, JD, Ewerling, F, Ferreira, LZ, and Barros, AJ. Early childhood suspected developmental delay in 63 low-and middle-income countries: large within-and between-country inequalities documented using national health surveys. J Glob Health. (2020) 10:010427. doi: 10.7189/jogh.10.010427
4. Galler, JR, Bringas-Vega, ML, Tang, Q, Rabinowitz, AG, Musa, KI, Chai, WJ, et al. Neurodevelopmental effects of childhood malnutrition: a neuroimaging perspective. Neuroimage. (2021) 231:117828. doi: 10.1016/j.neuroimage.2021.117828
5. Momen, AA, Jelodar, G, and Dehdashti, H. Brain magnetic resonance imaging findings in developmentally delayed children. Int J Pediatr. (2011) 2011:386984:1–4. doi: 10.1155/2011/386984
6. Deoni, SCL, Medeiros, P, Deoni, AT, Burton, P, Beauchemin, J, D’Sa, V, et al. Development of a mobile low-field MRI scanner. Sci Rep. (2022) 12:5690. doi: 10.1038/s41598-022-09760-2
7. Bhavnani, S, Lockwood Estrin, G, Haartsen, R, Jensen, SKG, Gliga, T, Patel, V, et al. EEG signatures of cognitive and social development of preschool children–a systematic review. PLoS One. (2021) 16:e0247223. doi: 10.1371/journal.pone.0247223
8. Wedderburn, CJ, Subramoney, S, Yeung, S, Fouche, JP, Joshi, SH, Narr, KL, et al. Neuroimaging young children and associations with neurocognitive development in a south African birth cohort study. Neuroimage. (2020) 219:116846. doi: 10.1016/j.neuroimage.2020.116846
9. Bhavnani, S, Parameshwaran, D, Sharma, KK, Mukherjee, D, Divan, G, Patel, V, et al. The acceptability, feasibility, and utility of portable electroencephalography to study resting-state neurophysiology in rural communities. Front Hum Neurosci. (2022) 16:802764. doi: 10.3389/fnhum.2022.802764
10. Katus, L, Hayes, NJ, Mason, L, Blasi, A, McCann, S, Darboe, MK, et al. Implementing neuroimaging and eye tracking methods to assess neurocognitive development of young infants in low-and middle-income countries. Gates Open Res. (2019) 3:1113. doi: 10.12688/gatesopenres.12951.2
11. Workneh, F, Chin, TI, Yibeltal, K, Fasil, N, North, K, Jensen, SKG, et al. Impact of maternal antenatal nutrition and infection treatment interventions on longitudinal infant development and growth in rural Ethiopia: protocol of the LIDG child follow-up study. BMJ Paediatr Open. (2024) 8:e002840. doi: 10.1136/bmjpo-2024-002840
12. Lee, AC, Abate, FW, Mullany, LC, Baye, E, Berhane, YY, Derebe, MM, et al. Enhancing nutrition and antenatal infection treatment (ENAT) study: protocol of a pragmatic clinical effectiveness study to improve birth outcomes in Ethiopia. BMJ Paediatr Open. (2022) 6:e001327. doi: 10.1136/bmjpo-2021-001327
13. Hennink, M, and Kaiser, BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. (2022) 292:114523. doi: 10.1016/j.socscimed.2021.114523
14. Ahmed, SK. Sample size for saturation in qualitative research: debates, definitions, and strategies. J Med Surg Public Health. (2025) 5:100171. doi: 10.1016/j.glmedi.2024.100171
15. Guest, G, Bunce, A, and Johnson, L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. (2006) 18:59–82. doi: 10.1177/1525822X05279903
16. Hennink, MM, Kaiser, BN, and Marconi, VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. (2017) 27:591–608. doi: 10.1177/1049732316665344
17. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
18. Gale, NK, Heath, G, Cameron, E, Rashid, S, and Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. doi: 10.1186/1471-2288-13-117
19. Ginsburg, AS, Liddy, Z, Khazaneh, PT, May, S, and Pervaiz, F. A survey of barriers and facilitators to ultrasound use in low-and middle-income countries. Sci Rep. (2023) 13:3322. doi: 10.1038/s41598-023-30454-w
20. Neuroimaging of Young Children: Parents’ Perceptions and Influence on Language. Available from: https://www.researchgate.net/publication/383272032_
21. Shen, FX, Wolf, SM, Bhavnani, S, Deoni, S, Elison, JT, Fair, D, et al. Emerging ethical issues raised by highly portable MRI research in remote and resource-limited international settings. Neuroimage. (2021) 238:118210. doi: 10.1016/j.neuroimage.2021.118210
22. Kohlasch, KL, Cioffredi, LA, Lenninger, C, Stewart, E, Vatalaro, T, Garavan, H, et al. Factors associated with parent views about participation in infant MRI research provide guidance for the design of the healthy brain and child development (HBCD) study. Dev Cogn Neurosci. (2021) 50:100986. doi: 10.1016/j.dcn.2021.100986
23. Assessment of Patients’ Knowledge, Perception and Safety Regarding MRI Scan. Available online at: https://www.researchgate.net/publication/343992819.Citedon (Accessed November 30, 2024).
24. Edwinson Månsson, M, and Gårdling, J. Children’s and parent’s perceptions of a magnetic resonance imaging examination. J Radiol Nurs. (2014) 33:30–4. doi: 10.1016/j.jradnu.2013.11.006
Keywords: magnetic resonance imaging, electroencephalogram, acceptability, feasibility, rural, Ethiopia
Citation: Workneh F, Chin TI, Yibeltal K, North K, Fasil N, Tarekegn W, Abate BH, Mulugeta S, Asmamaw G, Teklehaimanot A, Troller-Renfree SV, Jensen SKG, Thomason ME, Inder T, Nelson CA, Worku A, Lee ACC and Berhane Y (2025) Feasibility and acceptability of magnetic resonance imaging and electroencephalography for child neurodevelopmental research in rural Ethiopia. Front. Public Health. 13:1551982. doi: 10.3389/fpubh.2025.1551982
Edited by:
Sairam Geethanath, Johns Hopkins University, United StatesReviewed by:
Johnes Obungoloch, Mbarara University of Science and Technology, UgandaJon-Fredrik Nielsen, University of Michigan, United States
Copyright © 2025 Workneh, Chin, Yibeltal, North, Fasil, Tarekegn, Abate, Mulugeta, Asmamaw, Teklehaimanot, Troller-Renfree, Jensen, Thomason, Inder, Nelson, Worku, Lee and Berhane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Firehiwot Workneh, ZmlyZWhpd290d29ya25laEBhZGRpc2NvbnRpbmVudGFsLmVkdS5ldA==; ZmlyZWhpd290d2FjaXBoQGdtYWlsLmNvbQ==
†These authors share first authorship
‡These authors share senior authorship
 Firehiwot Workneh
Firehiwot Workneh Theresa I. Chin
Theresa I. Chin Kalkidan Yibeltal5
Kalkidan Yibeltal5 Nebiyou Fasil
Nebiyou Fasil Charles A. Nelson
Charles A. Nelson