- 1Wuhan Centre for Disease Prevention and Control, Wuhan, China
- 2Maternal and Child Health Hospital of Hongshan District, Wuhan, China
- 3School of Public Health, Wuhan University of Science and Technology, Wuhan, China
Aim: This study aimed to investigate hypertension-associated disparities in health-related physical fitness (HRPF) among community-dwelling older adults in Wuhan.
Methods: This cross-sectional study employed multi-stage stratified random sampling: random selection of 7 districts from Wuhan’s 17 administrative districts and 3–5 communities per district. A total of 801 eligible adults aged ≥65 years were recruited (after exclusions). The sample size was determined using 2015 municipal census data (α = 0.05, power = 90%). Assessments included verification of hypertension and demographic questionnaires, as well as seven standardized HRPF tests across four domains. The data were analyzed using SPSS 13.0, which involved calculating descriptive statistics (means ± SDs, 95% CIs) and performing between-group comparisons (χ2 tests and ANOVA).
Results: Hypertensive participants (n = 291) demonstrated impaired dynamic balance: they had reduced One-Leg Balance (OLB) time (3.38 ± 3.30 s vs. 3.98 ± 3.81 s; p = 0.02). Decreased aerobic endurance: fewer 2-min step repetitions (65.62 ± 29.17 vs. 70.13 ± 26.71; p = 0.033). However, they showed enhanced shoulder flexibility: greater back scratch reach (−14.11 ± 12.36 cm vs. -10.47 ± 11.15 cm; p < 0.001).
Conclusion: Hypertension is associated with domain-specific HRPF impairments, particularly in balance and aerobic endurance. Targeted exercise interventions that prioritize these domains may mitigate functional decline and reduce cardiovascular burden in aging populations.
1 Introduction
China has become an aging society, with 164.5 million citizens aged 65 and above (1). Hypertension is a prevalent condition among the older population in China, affecting 60.56% of individuals aged 65 years and older (2, 3). The burden of hypertension and its complications imposes significant economic and health costs not only on affected individuals but also on their families and society at large (4). Consequently, addressing population aging and reducing hypertension are critical public health priorities in China.
Among diverse strategies for hypertension prevention, physical activity constitutes a core intervention approach. Regular physical activity generally helps prevent hypertension by improving large artery structure and peripheral circulatory function (5). Aerobic exercise modulates hypertension through various pathways, including improvements in insulin sensitivity, regulation of autonomic nervous system function, and reduction of oxidative stress (6, 7). Resistance training primarily influences vasoconstriction regulation (8). These differential mechanisms yield varying clinical effects on blood pressure (9, 10). Therefore, it is essential to establish objective indices for assessing physical activity capacity to optimize outcomes in hypertension prevention.
Health-related physical fitness (HRPF) refers to an individual’s capacity to maintain sufficient energy for daily activities (including occupational and cognitive tasks) without undue fatigue (11, 12). Evidence suggests that exercise modalities have differential effects on HRPF components (13). HRPF includes four core dimensions: muscular strength, aerobic endurance, flexibility, and balance, collectively reflecting integrated physiological function (14–16). Existing literature predominantly indicates that inadequate HRPF is associated with the development of hypertension in older populations (14, 16–18). However, the findings are not studied as a composite whole; research typically focuses on individual dimensions. For instance, studies have shown that good flexibility, muscle strength, or aerobic endurance alone can each reduce the incidence of hypertension (19–21). Conversely, multidimensional studies indicate that compared with aerobic endurance, the effect of muscle strength on hypertension is negligible (19). Conversely, research on children and adolescents is more extensive (19, 22, 23). Overall, existing research lacks a focus on the older population, while HRPF studies have typically been confined to a single dimension (14, 24, 25). We therefore hypothesize that hypertensive older adults in Wuhan exhibit significant HRPF disparities across all domains compared to normotensive peers. To address these gaps, this study aims to examine hypertension-HRPF relationships across all HRPF dimensions.
2 Materials and methods
2.1 Study design and participants
This cross-sectional study was conducted by the Disease Burden Innovation Research Department at the Wuhan Center for Disease Control and Prevention.
A stratified multistage random sampling design was implemented across Wuhan’s 17 administrative districts. Firstly, seven districts were systematically selected using a random sampling. Secondly, randomly select 3–5 communities per district (a total of 28 communities). Finally, we employed random sampling to enroll adults aged ≥65 years from community registries, targeting 300 participants per district (each community 60–100 subjects, initial N = 2,100). Inclusion criteria: community-dwelling adults aged ≥65 years; provision of written informed consent. Exclusion criteria: any of the following conditions: age <65 years; advanced cardiovascular disease, neuromuscular disorders (e.g., Parkinson’s disease, amyotrophic lateral sclerosis), acute hospitalization (current or within 3 months prior to assessment); cognitive impairment affecting consent capacity.
Field assessments were completed, resulting in 2,150 evaluations across all sites. After database construction and quality control, 54 ineligible samples were excluded, yielding a final analytical sample of 2,096 participants. Subsequently, 1,295 participants were excluded due to non-hypertensive comorbidities affecting fitness outcome (metabolic disorders, type 2 diabetes, dyslipidemia requiring medication, renal impairment, neuromuscular conditions, Parkinson’s disease). The final analytical sample included 801 community-dwelling older adults with isolated hypertension or normotension.
Hypertension was defined as meeting any one of the following criteria: either self-reported physician-diagnosed hypertension by certified healthcare institutions; or current use of antihypertensive medication (self-reported with verification of medication names); or objectively measured elevated blood pressure: Systolic BP ≥ 140 mmHg and/or Diastolic BP ≥ 90 mmHg (based on the average of three seated measurements using calibrated sphygmomanometers after 5-min rest).
2.2 General characteristics assessment
General characteristics were assessed using an investigator-developed questionnaire that captured key domains, including demographics (age, sex, marital status, and education level). It also included clinical history of physician-diagnosed chronic conditions (hypertension, diabetes mellitus, stroke, cardiovascular disease, and hyperlipidemia), and addressed lifestyle factors such as physical activity levels and smoking status (current/former/never). To ensure questionnaire quality, the project team implemented standardized investigator training and used uniform procedures and operational protocols for administering surveys to older participants.
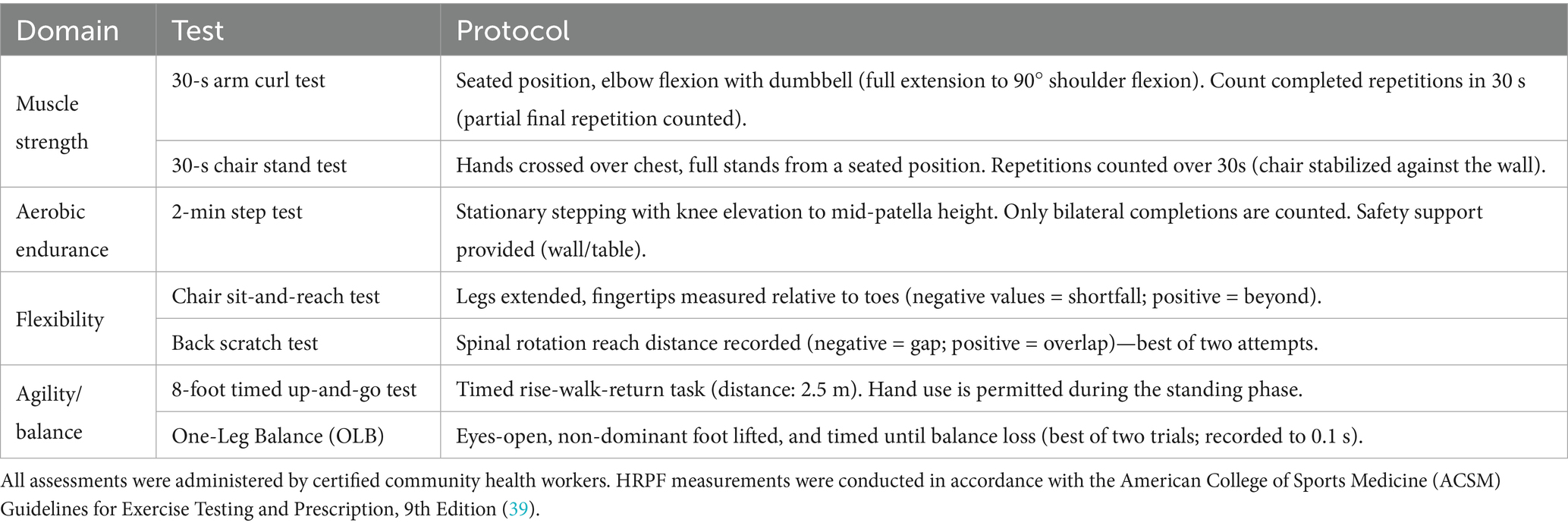
2.3 HRPF assessment
Seven validated tests were administered to assess four domains of HRPF, following standardized protocols with prioritization of safety (Table 1). Participants were instructed to perform at their natural pace without exertion; incomplete tests were documented without penalty. Each test included 1–2 practice trials before formal recording. Measurement instruments include timing devices: digital stopwatches (mobile phone applications permitted); distance measurement: graduated tape measure (precision: 0.1 cm). Equipment includes: an adjustable-height chair (seat height of 43 cm, backrest secured against the wall); dumbbells (3.6 kg for males, 2.25 kg for females); cones for marker placement; a calibrated sphygmomanometer and weight scale; blood pressure measurement instruments were provisioned by community health centers serving each residential area. The equipment inventory comprised both mercury sphygmomanometers and oscillometric devices across communities. Though heterogeneous in manufacturers and models, all devices underwent rigorous calibration traceable to national metrology institutes.
2.4 Statistical analysis
Data were analyzed using SPSS 13.0 (IBM Corp), and normality was assessed using the Kolmogorov–Smirnov test. For descriptive statistics, categorical variables are represented as frequencies and percentages, while continuous variables are expressed as mean ± standard deviation (SD) if normally distributed, or as the median and interquartile range if non-normally distributed. Between-group comparisons were conducted using Pearson’s chi-squared test for categorical variables and one-way ANOVA for normally distributed continuous variables. Statistical significance was defined as a two-tailed p-value of less than 0.05 (p < 0.05) (see Tables 2, 3).
3 Result
3.1 General characteristics of participants with hypertension and without hypertension
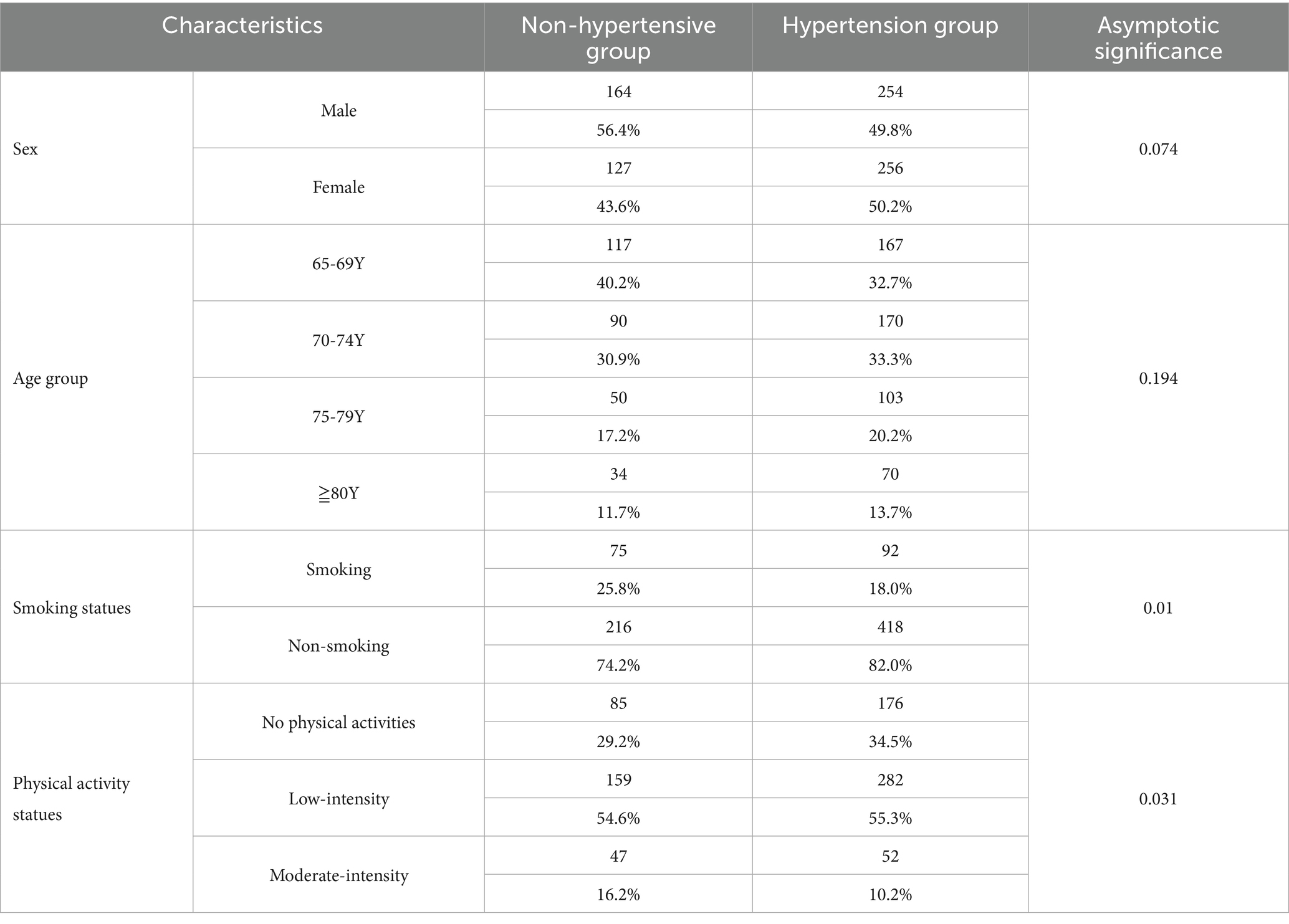
The analytical sample included 801 community-dwelling older adults (418 males and 383 females), derived from 2096 screened participants after excluding 1,295 individuals with diabetes or comorbidities that could influence HRPF. Participants were stratified into two groups: the hypertensive group (n = 291), which included individuals with hypertension but no other chronic conditions (50.2% female, average age of 73.01 years); the non-hypertensive group (n = 510) included normotensive individuals without chronic conditions (43.6% female, average age of 72.15 years). No significant age difference was observed between the groups (p = 0.074). Hypertension prevalence showed no significant variation across 5-year age strata (65–69, 70–74, 75–79, ≥80 years). Smoking behavior differed significantly (p = 0.01), with lower current smoking prevalence in hypertensive (18.0%) versus non-hypertensive participants (25.8%). Physical activity patterns revealed significant disparities (p = 0.031). Hypertensive participants reported higher rates of physical inactivity (34.5% vs. 29.2%), lower engagement in moderate-intensity exercise (10.2% vs. 16.2%), and comparable participation in low-intensity activity (55.3% vs. 54.6%).
3.2 Comparison of HRPF between hypertension and non-hypertensive groups
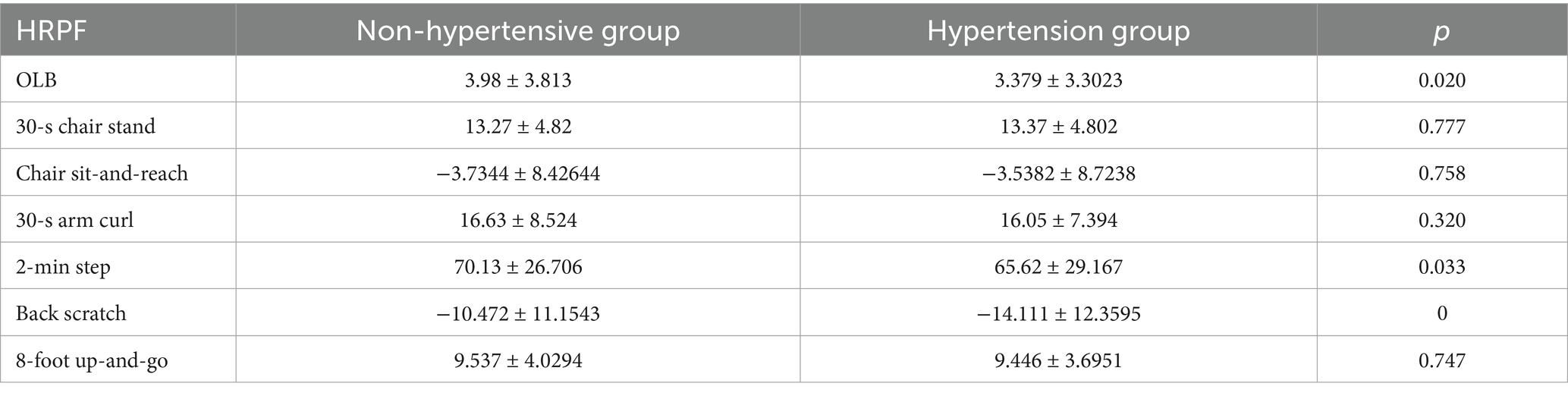
Significant between-group differences emerged in three of seven HRPF measures after comprehensive assessment. Hypertensive participants demonstrated reduced balance capacity with OLB time (3.38 ± 3.30 s vs. 3.98 ± 3.81 s; p = 0.02); impaired aerobic endurance with poor performance in the 2-min step test (65.62 ± 29.17 vs. 70.13 ± 26.71; p = 0.033); enhanced shoulder flexibility with greater reach in the back scratch test (−14.11 ± 12.36 cm vs-10.47 ± 11.15 cm; p < 0.001).
No significant differences were observed in: lower-body strength (30-s chair stand: 13.37 ± 4.80 vs. 13.27 ± 4.82; p = 0.777); hamstring flexibility (chair sit-and-reach: −3.54 ± 8.72 cm vs. -3.73 ± 8.43 cm; p = 0.758); upper-body strength (30-s arm curl: 16.05 ± 7.39 vs. 16.63 ± 8.52; p = 0.320); mobility (8-foot up-and-go: 9.45 ± 3.70 s vs. 9.54 ± 4.03 s; p = 0.747).
4 Discussion
This large-scale cross-sectional study examined hypertension-related disparities in HRPF among community-dwelling older adults in Wuhan. Our key findings reveal complex relationships between hypertension status and functional capacity, with implications for the development of targeted interventions.
Consistent with global trends, we observed no significant differences in hypertension prevalence across age groups, marital status, or education levels (1). However, hypertensive participants demonstrated significantly lower smoking rates (18.0% vs. 25.8%; p = 0.01), aligning with evidence that a hypertension diagnosis motivates smoking cessation (26). This behavioral shift may stem from heightened health awareness, as hypertensive smokers face elevated risks of malignant hypertension and accelerated atherosclerosis (27). Notably, both groups exhibited higher smoking rates than European and African cohorts, suggesting region-specific public health challenges (26, 28). Beside these, hypertensive older adults showed significantly higher inactivity rates (34.5% vs. 29.2%) and lower moderate-intensity exercise participation (10.2% vs. 16.2%). This activity profile may directly contribute to the observed HRPF deficits.
Within the specific HRPF domain, our study identified three significant differences. Hypertensive participants demonstrated significantly shorter OLB times (p = 0.020) and reduced performance on the 2-min step test (p = 0.033), indicating impaired balance and diminished aerobic endurance. Conversely, enhanced back scratch reach (p < 0.001) reflected superior flexibility in the hypertensive group. The aerobic endurance deficit likely indicates impaired oxygen delivery due to vascular endothelial dysfunction. Disrupted nitric oxide (NO) bioavailability, the principal endothelium-derived relaxing factor (EDRF) that mediates vascular smooth muscle relaxation, elevates peripheral resistance, and reduces skeletal muscle perfusion (29–31). Research in both humans and rodents has demonstrated that elevated nitric oxide levels improve endothelium-dependent vasodilation (32, 33). In patients with essential hypertension, the impairment of endothelial function and regulation of vascular tone results in increased peripheral vascular resistance and inadequate modulation of oxygen delivery to skeletal muscle, thereby affecting muscle function. Muscular function impairment may also help explain the impaired balance capacity in the hypertensive group (30).
Our study also demonstrated better flexibility in the hypertensive group. This finding contrasts with an earlier report that found a persistent inverse association between greater flexibility and lower hypertension incidence after controlling for confounders (34). While this observed flexibility advantage needs further investigation, it may indicate compensatory adaptation to balance limitations. Additionally, the potential confounding influence of sex cannot be excluded, particularly given the overrepresentation of females (who typically exhibit enhanced flexibility) in the hypertensive group (35).
Our results reinforce specific HRPF indexes associated with hypertension (17, 18, 36). Targeted exercise interventions should focus on aerobic training to improve endothelial function and oxygen delivery (37). Such interventions may reduce the increased frailty risk observed in hypertensive older adults (38).
5 Conclusion
This cross-sectional study demonstrated significant disparities in HRPF between hypertensive and non-hypertensive community-dwelling older adults in Wuhan. Key findings indicate that hypertensive older adults exhibit impaired functional capacities. Accelerated age-related decline is characterized by faster deterioration in aerobic endurance, flexibility, and dynamic balance compared to non-hypertensive peers. Activity pattern differences include higher rates of physical inactivity (34.5% vs. 29.2%) and lower engagement in moderate-intensity exercise.
These functional limitations likely originate from hypertension-associated vascular pathophysiology and suboptimal activity profiles. Implementing targeted exercise interventions, particularly combining aerobic training with balance-challenging components, may mitigate functional decline, reduce cardiovascular risk, and alleviate the growing disease burden affecting both families and society.
6 Limitations
This study has several limitations. Design limitations include the cross-sectional methodology, which precludes causal inference between HRPF and the development of hypertension. Unmeasured confounders, such as potential influencing factors (e.g., sex-specific fitness patterns, nutritional status, and medication adherence), were not fully evaluated. Activity assessment, including physical activity levels, depended on self-report without accelerometer validation. Future research should address these issues through prospective cohort studies with serial HRPF measurements. Furthermore, mechanistic investigations of hypertension-related neuromuscular decline and randomized controlled trials testing tailored exercise regimens for hypertensive older adults are recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was reviewed and approved by the Ethics Committee of Wuhan Center for Disease Control and Prevention (approval number: NO. WHCDCIRB-K-2021058). Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required for participation in this study in accordance with the national legislation and the institutional requirements.
Author contributions
WL: Data curation, Formal analysis, Funding acquisition, Investigation, Software, Writing – original draft, Writing – review & editing. XC: Data curation, Investigation, Writing – review & editing, Writing – original draft. JW: Data curation, Investigation, Writing – review & editing. SK: Data curation, Investigation, Software, Writing – review & editing. WZ: Data curation, Investigation, Writing – review & editing. MY: Formal analysis, Supervision, Writing – review & editing. YG: Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Wuhan Science and Technology Bureau’s Knowledge Innovation Special Project (Nos. 2022020801020594 and 2023020201010205) and Wuhan Municipal Health Commission (No. WZ21B03).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fang, EF, Xie, C, Schenkel, JA, Wu, C, Long, Q, Cui, H, et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. (2020) 64:101174. doi: 10.1016/j.arr.2020.101174
2. Chaoyang, Z, Gang, Z, Juan, D, and Jie, G. Prevalence, awareness and control rates of hypertension among elderly aged ≥65 years in Wuhan. Chin J Hypertens. (2014) 22:5.
3. Zhang, W, Yan, Y, Liu, X, Zhou, X, and Guo, Y. Impact of hypertension, diabetes, hyperlipidemia and their comorbidities on cognitive function in elderly. Chin Prev Med. (2021) 22:411–7. doi: 10.16506/j.1009-6639.2021.06.003
4. Qiu, Y, Ma, J, Zhu, J, Liu, Y, Ren, W, Zhang, S, et al. Deaths and disability-adjusted life years of hypertension in China, South Korea, and Japan: a trend over the past 29 years. Front Cardiovasc Med. (2023) 10:1080682. doi: 10.3389/fcvm.2023.1080682
5. De Ciuceis, C, Rizzoni, D, and Palatini, P. Microcirculation and physical exercise in hypertension. Hypertension. (2023) 80:730–9. doi: 10.1161/HYPERTENSIONAHA.122.19465
6. Moraes-Silva, IC, Mostarda, C, Moreira, ED, Silva, KA, dos Santos, F, de Angelis, K, et al. Preventive role of exercise training in autonomic, hemodynamic, and metabolic parameters in rats under high risk of metabolic syndrome development. J Appl Physiol. (2013) 114:786–91. doi: 10.1152/japplphysiol.00586.2012
7. Korsager Larsen, M, and Matchkov, VV. Hypertension and physical exercise: the role of oxidative stress. Medicina (Kaunas). (2016) 52:19–27. doi: 10.1016/j.medici.2016.01.005
8. Araujo, AJ, Santos, AC, Souza, KD, Aires, MB, Santana-Filho, VJ, Fioretto, ET, et al. Resistance training controls arterial blood pressure in rats with L-NAME-induced hypertension. Arq Bras Cardiol. (2013) 100:339–46.
9. Rossi, AM, Moullec, G, Lavoie, KL, Gour-Provencal, G, and Bacon, SL. The evolution of a Canadian hypertension education program recommendation: the impact of resistance training on resting blood pressure in adults as an example. Can J Cardiol. (2013) 29:622–7. doi: 10.1016/j.cjca.2013.02.010
10. Börjesson, M, Onerup, A, Lundqvist, S, and Dahlöf, B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. (2016) 50:356–61. doi: 10.1136/bjsports-2015-095786
11. Boutcher, YN, and Boutcher, SH. Exercise intensity and hypertension: what's new? J Hum Hypertens. (2017) 31:157–64. doi: 10.1038/jhh.2016.62
12. Tremblay, MS, Colley, RC, Saunders, TJ, Healy, GN, and Owen, N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. (2010) 35:725–40. doi: 10.1139/H10-079
13. Dong, B, Beauchamp, M, and Hao, Q. Exercise for sarcopenia in older people: a systematic review and network meta-analysis. J Cachexia Sarcopenia Muscle. (2023) 14:1199–211. doi: 10.1002/jcsm.13225
14. Yumei, L, Zuoliang, W, Yunhong, W, Yaoxiu, C, and Enping, L. Health-related physical fitness and chronic diseases analysis in active elderly adults. Chin J Geriatr. (2015) 34:561–4. doi: 10.3760/cma.j.issn.0254-9026.2015.05.028
15. Rikli, RE, and Jones, CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. (2013) 53:255–67. doi: 10.1093/geront/gns071
16. Ho, CC, Lee, PF, Chen, HL, Tseng, CY, Hsieh, XY, and Chiu, CH. Poor health-related physical fitness performance increases the overweight and obesity risk in older adults from Taiwan. BMC Geriatr. (2021) 21:170. doi: 10.1186/s12877-021-02112-1
17. Navarrete-Villanueva, D, Gómez-Cabello, A, Marín-Puyalto, J, Moreno, LA, Vicente-Rodríguez, G, and Casajús, JA. Frailty and physical fitness in elderly people: a systematic review and meta-analysis. Sports Med. (2021) 51:143–60. doi: 10.1007/s40279-020-01361-1
18. Faselis, C, Doumas, M, Kokkinos, JP, Panagiotakos, D, Kheirbek, R, Sheriff, HM, et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension. (2012) 60:333–8. doi: 10.1161/HYPERTENSIONAHA.112.196493
19. Crump, C, Sundquist, J, Winkleby, MA, and Sundquist, K. Interactive effects of physical fitness and body mass index on the risk of hypertension. JAMA Intern Med. (2016) 176:210–6. doi: 10.1001/jamainternmed.2015.7444
20. Nishiwaki, M, Kurobe, K, Kiuchi, A, Nakamura, T, and Matsumoto, N. Sex differences in flexibility-arterial stiffness relationship and its application for diagnosis of arterial stiffening: a cross-sectional observational study. PLoS One. (2014) 9:e113646. doi: 10.1371/journal.pone.0113646
21. Luo, JH, Zhang, TM, Yang, LL, Cai, YY, and Yang, Y. Association between relative muscle strength and hypertension in middle-aged and older Chinese adults. BMC Public Health. (2023) 23:2087. doi: 10.1186/s12889-023-17007-6
22. Ortega, FB, Ruiz, JR, Castillo, MJ, and Sjostrom, M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. (2008) 32:1–11. doi: 10.1038/sj.ijo.0803774
23. Agostinis-Sobrinho, C, Ruiz, JR, Moreira, C, Lopes, L, Ramírez-Vélez, R, García-Hermoso, A, et al. Changes in muscular fitness and its association with blood pressure in adolescents. Eur J Pediatr. (2018) 177:1101–9. doi: 10.1007/s00431-018-3164-4
24. Leong, DP, Teo, KK, Rangarajan, S, Lopez-Jaramillo, P, Avezum, A Jr, Orlandini, A, et al. Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. (2015) 386:266–73. doi: 10.1016/S0140-6736(14)62000-6
25. Cohen, DD, Gómez-Arbeláez, D, Camacho, PA, Pinzon, S, Hormiga, C, Trejos-Suarez, J, et al. Low muscle strength is associated with metabolic risk factors in Colombian children: the ACFIES study. PLoS One. (2014) 9:e93150. doi: 10.1371/journal.pone.0093150
26. Bager, JE, Mourtzinis, G, Andersson, T, Nåtman, J, Rosengren, A, Björck, S, et al. Trends in blood pressure, blood lipids, and smoking from 259 753 patients with hypertension in a Swedish primary care register: results from QregPV. Eur J Prev Cardiol. (2022) 29:158–66. doi: 10.1093/eurjpc/zwab087
27. Virdis, A, Giannarelli, C, Neves, MF, Taddei, S, and Ghiadoni, L. Cigarette smoking and hypertension. Curr Pharm Des. (2010) 16:2518–25. doi: 10.2174/138161210792062920
28. Noubiap, JJ, Nansseu, JR, Endomba, FT, Ngouo, A, Nkeck, JR, Nyaga, UF, et al. Active smoking among people with diabetes mellitus or hypertension in Africa: a systematic review and meta-analysis. Sci Rep. (2019) 9:588. doi: 10.1038/s41598-018-37858-z
29. Caspersen, CJ, Powell, KE, and Christenson, GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. (1985) 100:126–31.
30. Nyberg, M, Gliemann, L, and Hellsten, Y. Vascular function in health, hypertension, and diabetes: effect of physical activity on skeletal muscle microcirculation. Scand J Med Sci Sports. (2015) 25:60–73. doi: 10.1111/sms.12591
31. Das, S, and Kumar, KN. Nitric oxide: its identity and role in blood pressure control. Life Sci. (1995) 57:1547–56. doi: 10.1016/0024-3205(95)02130-b
32. Hotta, K, Behnke, BJ, Arjmandi, B, Ghosh, P, Chen, B, Brooks, R, et al. Daily muscle stretching enhances blood flow, endothelial function, capillarity, vascular volume and connectivity in aged skeletal muscle. J Physiol. (2018) 596:1903–17. doi: 10.1113/JP275459
33. Bisconti, AV, Cè, E, Longo, S, Venturelli, M, Coratella, G, Limonta, E, et al. Evidence for improved systemic and local vascular function after long-term passive static stretching training of the musculoskeletal system. J Physiol. (2020) 598:3645–66. doi: 10.1113/JP279866
34. Gando, Y, Sawada, SS, Momma, H, Kawakami, R, Miyachi, M, Lee, IM, et al. Body flexibility and incident hypertension: the Niigata wellness study. Scand J Med Sci Sports. (2021) 31:702–9. doi: 10.1111/sms.13867
35. Araújo, CGS, de Souza E Silva, CG, Kunutsor, SK, Franklin, BA, Laukkanen, JA, Myers, J, et al. Reduced body flexibility is associated with poor survival in middle-aged men and women: a prospective cohort study. Scand J Med Sci Sports. (2024) 34:e14708. doi: 10.1111/sms.14708
36. Lopez-Jaramillo, P, Lopez-Lopez, JP, Tole, MC, and Cohen, DD. Muscular strength in risk factors for cardiovascular disease and mortality: a narrative review. Anatol J Cardiol. (2022) 26:598–607. doi: 10.5152/AnatolJCardiol.2022.1586
37. Kim, YH, Jeong, MK, Park, H, and Park, SK. Effects of regular taekwondo intervention on health-related physical fitness, cardiovascular disease risk factors and epicardial adipose tissue in elderly women with hypertension. Int J Environ Res Public Health. (2021) 18:2935. doi: 10.3390/ijerph18062935
38. Yang, Y, Xu, H, Liu, X, Li, J, Liew, Z, Liu, X, et al. Joint association of smoking and physical activity with mortality in elderly hypertensive patients: a Chinese population-based cohort study in 2007-2018. Front Public Health. (2022) 10:1005260. doi: 10.3389/fpubh.2022.1005260
39. Thompson, PD, Arena, R, Riebe, D, and Pescatello, LSAmerican College of Sports Medicine. ACSM'S new preparticipation health screening recommendations from ACSM'S guidelines for exercise testing and prescription, ninth edition. Curr Sports Med Rep. (2013) 12:215–7. doi: 10.1249/JSR.0b013e31829a68cf
Keywords: hypertension, health related physical fitness, aging population, cross-sectional study, Wuhan
Citation: Luo W, Chen X, Wang J, Ke S, Zhang W, Yang M and Guo Y (2025) The relationship between hypertension and health-related physical fitness in older adult residences in Wuhan: a cross-sectional study. Front. Public Health. 13:1555638. doi: 10.3389/fpubh.2025.1555638
Edited by:
Giuseppe Caminiti, Università telematica San Raffaele, ItalyCopyright © 2025 Luo, Chen, Wang, Ke, Zhang, Yang and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Guo, Z3VveWFuODEwMUBmb3htYWlsLmNvbQ==; Mei Yang, eWFuZ21laTg4QHd1c3QuZWR1LmNu
 Wen Luo
Wen Luo Xi Chen1
Xi Chen1 Mei Yang
Mei Yang Yan Guo
Yan Guo