- 1Department of Cardiothoracic Surgery, Singapore General Hospital, Singapore, Singapore
- 2Department of General Surgery, Singapore General Hospital, Singapore, Singapore
- 3International Eye Cataract Retina Center, Mount Elizabeth Medical Center and Farrer Park Medical Center, Singapore, Singapore
- 4Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 5Department of Ophthalmology and Visual Sciences, Khoo Teck Puat Hospital, Singapore, Singapore
Introduction
The global prevalence of myopia has been increasing in the last few decades and is projected to reach 50% by the year 2050 in the absence of effective intervention measures (1). Each additional diopter (D) of myopia is associated with increased risk of ocular pathologies such as open-angle glaucoma (20%), posterior subcapsular cataract (21%), retinal detachment (30%), and myopic maculopathy (58%) (2). Hence, there is a pressing need to control myopia progression to reduce the burden of its associated sight-threatening complications.
Preventive strategies for childhood myopia progression
Until now, the prevention of childhood myopia has been largely focused on secondary prevention, i.e., reducing the severity of the condition for those who already have myopia. Various pharmacologic and optical interventions are currently in use to retard myopia progression (3, 4).
Studies such as the landmark Atropine for the Treatment Of Myopia 2 (ATOM2) (5) and Low-concentration Atropine for Myopia Progression (LAMP) (6) trials in East Asia have provided robust evidence for the effect of atropine on myopia control. The prevailing theory on the mechanism of action is on atropine modulating muscarinic receptors in ocular tissues during development (7). This effect is dose-dependent: the weighted mean differences (WMD) in refraction and axial elongation per year was 0.73 D and −0.26 mm for high-concentration (0.5%−1%) atropine, 0.65 D and −0.37 mm for moderate concentration (0.1%−0.25%), and 0.35 D and −0.11 mm for low-concentration (0.005%−0.05%) (8).
Interestingly, the Atropine for the Treatment Of childhood Myopia in India (I-ATOM) trial on 100 Indian children with mild to moderate myopia found that topical 0.01% atropine reduced refraction progression but had no significant effect on axial elongation (9). The Pediatric Eye Disease Investigator Group (PEDIG) trial on 187 American children with low to moderate myopia found that nightly topical 0.01% atropine did not slow myopia progression or axial elongation after 2 years compared with placebo (10). Change in spherical equivalent refraction (SER) were −0.82 D (atropine) and −0.80 D (placebo; adjusted difference −0.02D; 95% CI, −0.19 to +0.15 D; p = 0.83) and axial length (AL) were 0.44 mm (atropine) and 0.45 mm (placebo; adjusted difference −0.002 mm; 95% CI, −0.106 to 0.102 mm). It is worth noting that only a small proportion of participants (11%) in this trial were of East Asian descent, suggesting genetic and cultural or environmental influences on myopia progression.
Balancing effectiveness and potential side effects, topical atropine 0.05% has been deemed to be the optimal concentration for myopia control (8). The commonly reported side effects include photophobia and mild blurry near vision due to pupil dilation and reduced accommodation (11). Most children adapt well over time, and the side effects are reversible upon cessation of treatment (12).
Optical interventions with lenses designed for peripheral myopic defocus have been proven to be effective in signaling the eye to slow down its growth, resulting in slower myopia progression (13). For example, orthokeratology uses myopic shift and peripheral retinal defocus (14) in addition to reshaping the cornea temporarily to achieve good unaided vision during lens-free periods in the daytime (15). Spectacle lenses with highly aspherical lenslets (HAL) (16) and Defocus Incorporated Multiple Segments (DIMS) (17) provide refractive correction for distance vision and peripheral myopic defocus simultaneously by converging some incoming light rays in front of the retina. Cylindrical Annular Refractive Elements (CARE) lenses represent the latest addition to this new generation of myopia control spectacle lenses (18).
Primary prevention of childhood myopia
Primary prevention of childhood myopia focuses on children who do not yet have myopia (19). Premyopia, as defined by the International Myopia Institute, is a refractive state between +0.75 and −0.50 D in children with risk factors such as increased AL, myopic parents, or environmental influences (20). While no strict age cutoff is given, children are considered at higher risk if their refractive error is < +0.75 D at age 6, ≤ +0.50 D at ages 7–8, and ≤ +0.25 D at ages 9–10 (21). Current practices rely solely on behavioral modification to delay the onset of myopia in premyopes but we posit that in high risk groups, supplementing this with prophylactic treatment using pharmacologic and/or optical interventions may increase the efficacy of myopia control.
Behavioral modification
Outdoor time and sunlight exposure have been hypothesized to prevent myopia development by stimulating light-sensitive dopamine release in the retina (22). Dopamine inhibits ocular axial elongation, the anatomical basis of myopia development (22). This relationship has been proven in several studies (23–25), including a 3-year cluster-randomized trial in Guangzhou, China, which demonstrated a 9.1% absolute reduction in myopia incidence and 23% relative reduction over 3 years with 40 min of outdoor activity added per school day (39.5% incidence in control group vs. 30.4% in intervention group, p < 0.001) (24). Reduction of near work and longer viewing distances also exert a protective effect against myopia onset by reducing variation in accommodative demand and promote more uniform levels of retinal focus (25–27).
Prophylactic treatment of childhood myopia
Treating myopia before its onset in premyopes can potentially further reduce the risk of myopia-associated morbidities than current preventive strategies. Among the modalities, low-concentration atropine is currently the most evidence-supported intervention.
Pharmacologic intervention
Using topical low-concentration atropine in premyopes is a novel primary prevention strategy (28). A recent meta-analysis of three randomized controlled trials (RCT) and one non-RCT involving a total of 644 premyopic children aged 4–12 years highlighted its effectiveness in reducing rapid myopic shift (≥0.5 D/year, p < 0.04) and myopia incidence (p = 0.03) with 12–24 months of use as compared to placebo (Table 1) (28).
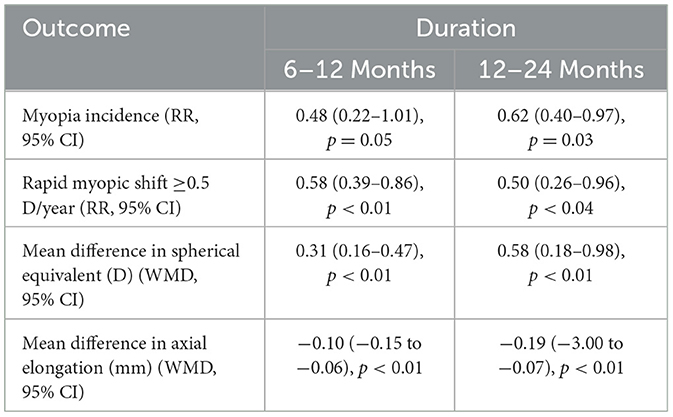
Table 1. Summary of results from a meta-analysis of three randomized controlled trials (RCT) and one non-RCT on the effectiveness of low-concentration atropine vs. placebo in reducing myopia incidence, rapid myopia shift, refraction (spherical equivalent, D) and axial elongation (mm) in premyopic children (28).
Optical intervention
Evidence is now emerging that lenses with HAL and DIMS may be useful in treating premyopes. A RCT with 108 low-hyperopic (0 to +2.00 D) Chinese children aged 6–9.9 years demonstrated significantly slower axial elongation (p < 0.001) with HAL lenses (0.11 mm; interquartile range [IQR]: 0.05–0.17 mm) compared to single vision lenses (0.27 mm; 0.21–0.33 mm) (29). A dose-response relationship was observed, with >30 h of wear per week proving efficacious (29). DIMS lenses were also shown to stabilize progression in SER (+0.04 D) and axial elongation (+0.06 mm) over 3 months of usage of ≥10 h/day in a pilot study involving 24 premyopic Taiwanese children aged 5–6 (30). Comparatively, mean axial elongation in a 6-year-old Chinese population was 0.58 mm/year (99% confidence interval [CI] 0.56–0.59 mm/year) in myopes and at 0.65 mm/year (99% CI 0.62–0.67 mm/year) in incident myopes (31). Over 9 months of DIMS lenses use, the average cycloplegic SER remained stable with a yearly change of +0.06 D compared to −0.15 D in a control group (32). There are currently no published studies specifically evaluating the use of orthokeratology lenses in premyopic children.
A game changer?
We are excited by the findings of these recent studies and believe that the prophylactic treatment of childhood myopia could be a game-changer in combating the scourge of myopia. Myopia control interventions employed in myopic children typically reduces axial elongation by < 0.4mm compared with control groups within a 2-year study period (29). In contrast, delaying myopia onset from age 9–10 is estimated to reduce axial elongation into adulthood by around 0.5 mm, suggesting that preventing or delaying onset may have a greater long-term impact (29).
Challenges in starting prophylactic treatment of myopia
Currently, topical low-concentration atropine therapy and optical interventions for prophylactic myopia treatment are not yet part of routine clinical practice (33, 34). One possible concern is the main side effect of atropine use—photophobia, although low atropine concentrations do not significantly affect vision-related quality of life (p > 0.05) (35). Simple measures such as wearing sunglasses outdoors, using photochromic lenses (36), or administering atropine eye drops at bedtime can ameliorate this symptom.
Wearing myopia control spectacles can lead to concerns about appearance, discomfort, and inconvenience—such as slipping, fogging, or pressure on the nose bridge during daily activities and sports (37). Seventeen per cent of premyopic children reported inconvenience to their daily activities at home and 8.3% had eye strain using DIMS lenses, although the frequency and severity of the complaints were mild (30). These factors can make optical interventions challenging to adopt in premyopic children who have good unaided vision.
There is currently a gap in public awareness about pharmacologic and optical intervention for primary myopia prevention, with few seeking treatment at a premyopic stage as vision is not problematic yet (38). Additionally, starting prophylactic myopia treatment may lead to greater financial burden as treatment, follow-up and opportunity costs start accumulating at a younger age (39, 40).
Despite these caveats, prophylactic treatment appears to be a promising novel strategy to delay the onset of myopia. Combined with secondary prevention, they aim to ultimately reduce the prevalence of high myopia and its associated sight-threatening complications.
Further research
Further studies on different topical atropine concentrations for primary myopia prevention can guide clinicians on the optimal concentration in this population. Investigating synergistic treatment such as low-concentration atropine and myopia control spectacle lenses can aid in proposing solutions for children intolerant to higher doses. Lastly, by developing multifactorial risk scores for premyopia for patient selection and better public education, we can hopefully see a large benefit in this new approach to preventing myopia-related complications and improving long-term outcomes.
Conclusions
Primary prevention of myopia with topical low-concentration atropine has recently been proven effective in delaying myopia incidence by reducing rapid myopic shift in SER and axial elongation. While we await future research to shed more light on prophylactic interventions, current evidence suggests that incorporating prophylactic treatment of myopia in premyopic children into current myopia control strategies could potentially be a game changer in combating the scourge of myopia.
Author contributions
DMXL: Writing – original draft, Writing – review & editing. JTWAE: Writing – original draft, Writing – review & editing. KGAE: Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
2. Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI. The risks and benefits of myopia control. Ophthalmology. (2021) 128:1561–79. doi: 10.1016/j.ophtha.2021.04.032
3. Zhu Z, Chen Y, Tan Z, Xiong R, McGuinness MB, Müller A. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. (2023) 107:160–6. doi: 10.1136/bjophthalmol-2021-319306
4. Chen KS, Au Eong JTW, Au Eong KG. Changing paradigm in the management of childhood myopia. Eye Lond Engl. (2024) 38:1027–8. doi: 10.1038/s41433-023-02831-2
5. Chia A, Lu QS. Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 001% eyedrops. Ophthalmology. (2016) 123:391–9. doi: 10.1016/j.ophtha.2015.07.004
6. Yam JC Li FF, Zhang X, Tang SM, Yip BHK, Kam KW, et al. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: phase 2 report. Ophthalmology. (2020) 127:910–9. doi: 10.1016/j.ophtha.2019.12.011
7. Upadhyay A, Beuerman RW. Biological mechanisms of atropine control of myopia. Eye Contact Lens. (2020) 46:129–35. doi: 10.1097/ICL.0000000000000677
8. Hou P, Wu D, Nie Y, Wei H, Liu L, Yang G. Comparison of the efficacy and safety of different doses of atropine for myopic control in children: a meta-analysis. Front Pharmacol. (2023) 14:1227787. doi: 10.3389/fphar.2023.1227787
9. Saxena R, Dhiman R, Gupta V, Kumar P, Matalia J, Roy L, et al. Atropine for the treatment of childhood myopia in India: multicentric randomized trial. Ophthalmology. (2021) 128:1367–9. doi: 10.1016/j.ophtha.2021.01.026
10. Repka MX, Weise KK, Chandler DL, Wu R, Melia BM, Manny RE, et al. Low-dose 001% atropine eye drops vs. placebo for myopia control: a randomized clinical trial. JAMA Ophthalmol. (2023) 141:756–65. doi: 10.1001/jamaophthalmol.2023.2855
11. Gong Q, Janowski M, Luo M, Wei H, Chen B, Yang G, et al. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. (2017) 135:624–30. doi: 10.1001/jamaophthalmol.2017.1091
12. Pérez-Flores I, Macías-Murelaga B, Barrio-Barrio J. A multicenter Spanish study of atropine 001% in childhood myopia progression. Sci Rep. (2021) 11:21748. doi: 10.1038/s41598-021-00923-1
13. Ma JX, Tian SW, Liu QP. Effectiveness of peripheral defocus spectacle lenses in myopia control: a meta-analysis and systematic review. Int J Ophthalmol. (2022) 15:1699–706. doi: 10.18240/ijo.2022.10.20
14. Berntsen DA, Barr CD, Mutti DO, Zadnik K. Peripheral defocus and myopia progression in myopic children randomly assigned to wear single vision and progressive addition lenses. Investig Opthalmology Vis Sci. (2013) 54:5761. doi: 10.1167/iovs.13-11904
15. Guan M, Zhao W, Geng Y, Zhang Y, Ma J, Chen Z, et al. Changes in axial length after orthokeratology lens treatment for myopia: a meta-analysis. Int Ophthalmol. (2020) 40:255–65. doi: 10.1007/s10792-019-01167-9
16. Bao J, Yang A, Huang Y, Li X, Pan Y, Ding C, et al. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br J Ophthalmol. (2022) 106:1171. doi: 10.1136/bjophthalmol-2020-318367
17. Lam CSY, Tang WC, Tse DYY, Lee RPK, Chun RKM, Hasegawa K, et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. (2020) 104:363–8. doi: 10.1136/bjophthalmol-2018-313739
18. Chen X, Wu M, Yu C, Ohlendorf A, Rifai K, Boeck-Maier C, et al. Slowing myopia progression with cylindrical annular refractive elements (CARE) spectacle lenses-Year 1 results from a 2-year prospective, multi-centre trial. Acta Ophthalmol. (2024). Available online at: https://onlinelibrary.wiley.com/doi/10.1111/aos.16795 (Accessed June 9, 2025).
19. Saw SM, Matsumura S, Hoang QV. Prevention and management of myopia and myopic pathology. Invest Ophthalmol Vis Sci. (2019) 60:488–99. doi: 10.1167/iovs.18-25221
20. Flitcroft DI, He M, Jonas JB, Jong M, Naidoo K, Ohno-Matsui K, et al. IMI – defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. (2019) 60:M20–30. doi: 10.1167/iovs.18-25957
21. Zadnik K, Sinnott LT, Cotter SA, Jones-Jordan LA, Kleinstein RN, Manny RE, et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. (2015) 133:683–9. doi: 10.1001/jamaophthalmol.2015.0471
22. Jan C, Li L, Keay L, Stafford RS, Congdon N, Morgan I. Prevention of myopia, China. Bull World Health Organ. (2020) 98:435–7. doi: 10.2471/BLT.19.240903
23. Deng L, Pang Y. Effect of outdoor activities in myopia control: meta-analysis of clinical studies. Optom Vis Sci Off Publ Am Acad Optom. (2019) 96:276–82. doi: 10.1097/OPX.0000000000001357
24. He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. (2015) 314:1142–8. doi: 10.1001/jama.2015.10803
25. Biswas S, El Kareh A, Qureshi M, Lee DMX, Sun CH, Lam JSH, et al. The influence of the environment and lifestyle on myopia. J Physiol Anthropol. (2024) 43:7. doi: 10.1186/s40101-024-00354-7
26. Flitcroft DI, Harb EN, Wildsoet CF. The spatial frequency content of urban and indoor environments as a potential risk factor for myopia development. Invest Ophthalmol Vis Sci. (2020) 61:42. doi: 10.1167/iovs.61.11.42
27. Au Eong JTW, Tsai JHJ, Crosby NJ, Au Eong KG. Childhood myopia and the coronavirus disease 2019 pandemic: lessons for future pandemics. Taiwan J Ophthalmol. (2024) 14:284–5. doi: 10.4103/tjo.TJO-D-24-00010
28. Lee SH, Tseng BY, Wang JH, Chiu CJ. Efficacy and safety of low-dose atropine on myopia prevention in premyopic children: systematic review and meta-analysis. J Clin Med. (2024) 13:1506. doi: 10.3390/jcm13051506
29. Zhang Z, Zeng L, Gu D, Wang B, Kang P, Watt K, et al. Spectacle lenses with highly aspherical lenslets for slowing axial elongation and refractive change in low-hyperopic Chinese children: a randomized controlled trial. Am J Ophthalmol. (2025) 269:60–8. doi: 10.1016/j.ajo.2024.08.020
30. Yang HY, Tsai DC, Yang YC, Wang CY. Preliminary results and adaptability to the defocus incorporated multiple segments spectacle lenses among pre-myopic children of preschool age. Hoyavision. Available online at: https://www.hoyavision.com/globalassets/__regional-assets/global/imc-2024/abstracts/preliminary-results-pdims-in-pre-myopic-taiwanese-children.pdf (Accessed April 19, 2025).
31. Naduvilath T, He X, Xu X, Sankaridurg P. Normative data for axial elongation in Asian children. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. (2023) 43:1160–8. doi: 10.1111/opo.13159
32. Yang HY, Tsai DC. Efficacy of defocus incorporated multiple segments (DIMS) lenses in retarding myopic shifts among pre-myopic preschoolers: nine-month results of a pilot study (2025). Available online at: https://www.hoyavision.com/globalassets/__regional-assets/global/arvo-2025/yang-et-al.-effectiveness-of-dims-in-pre-myopic-children-arvo-2025-abstract.pdf (Accessed June 9, 2025).
33. Chen YX, Liao CM, Tan Z, He MG. Who needs myopia control? Int J Ophthalmol. (2021) 14:1297–301. doi: 10.18240/ijo.2021.09.01
34. Cooper J, Tkatchenko AV. A review of current concepts of the etiology and treatment of myopia. Eye Contact Lens. (2018) 44:231–47. doi: 10.1097/ICL.0000000000000499
35. Yam JC, Zhang XJ, Zhang Y, Yip BHK, Tang F, Wong ES, et al. Effect of low-concentration atropine eyedrops vs. placebo on myopia incidence in children: the LAMP2 randomized clinical trial. JAMA. (2023) 329:472–81. doi: 10.1001/jama.2022.24162
36. Wu PC, Kuo HK. Effect of photochromic spectacles on visual symptoms and contrast sensitivity of myopic schoolchildren treated with low concentration atropine. Invest Ophthalmol Vis Sci. (2016) 57:2484. Available online at: https://iovs.arvojournals.org/article.aspx?articleid=2560920 (Accessed June 9, 2025).
37. Killeen OJ, Cho J, Raven SA, Wang GM, Mubeen A, Kim L, et al. A qualitative assessment of the experiences with eye health and barriers to eyeglasses among US Youth. Optom Vis Sci. (2023) 100:255–60. doi: 10.1097/OPX.0000000000002003
38. Ortiz-Peregrina S, Solano-Molina S, Martino F, Castro-Torres JJ, Jiménez JR. Parental awareness of the implications of myopia and strategies to control its progression: a survey-based study. Ophthalmic Physiol Opt. (2023) 43:1145–59. doi: 10.1111/opo.13190
39. Agyekum S, Chan PP, Adjei PE, Zhang Y, Huo Z, Yip BHK, et al. Cost-effectiveness analysis of myopia progression interventions in children. JAMA Netw Open. (2023) 6:e2340986. doi: 10.1001/jamanetworkopen.2023.40986
Keywords: myopia, premyopia, low-concentration atropine, low-dose atropine, highly aspherical lenslets, defocus incorporated multiple segments
Citation: Lee DMX, Au Eong JTW and Au Eong KG (2025) Prophylactic treatment of childhood myopia: a game-changer in combating the scourge of myopia? Front. Public Health 13:1556199. doi: 10.3389/fpubh.2025.1556199
Received: 06 January 2025; Accepted: 16 June 2025;
Published: 14 July 2025.
Edited by:
Rohit Saxena, All India Institute of Medical Sciences, IndiaReviewed by:
Vinay Gupta, All India Institute of Medical Sciences, IndiaCopyright © 2025 Lee, Au Eong and Au Eong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kah-Guan Au Eong, YXVlb25na2FoZ3VhbkBnbWFpbC5jb20=
 Deborah M. X. Lee
Deborah M. X. Lee Jonathan T. W. Au Eong
Jonathan T. W. Au Eong Kah-Guan Au Eong
Kah-Guan Au Eong