- 1Center for Stress-Related Disease Control and Prevention, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 2Department of Respiratory Medicine, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 3Department of Work Systems and Health, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 4Department of Occupational Health Practice and Management, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 5Department of Mental Health, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 6Disaster Occupational Health Center, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 7Department of Environmental Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 8Department of Preventive Medicine and Community Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
- 9Department of Environmental Epidemiology, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Fukuoka, Japan
Objective: Research has not fully determined the impact of the infection control practices adopted in workplaces during the COVID-19 pandemic on employees’ feelings of loneliness. This study aimed to clarify the relationship between these control measures and employees’ loneliness during the COVID-19 pandemic, including their relationship with perceived organizational support (POS).
Methods: A prospective cohort study was conducted via an internet-based questionnaire. Of the 27,036 responses, data from 10,562 were analyzed. Workplace infection control practices were divided into four groups based on the number of practices adopted by participants. The odds ratios (ORs) of loneliness associated with each workplace infection control practice were calculated using multilevel logistic regression analysis.
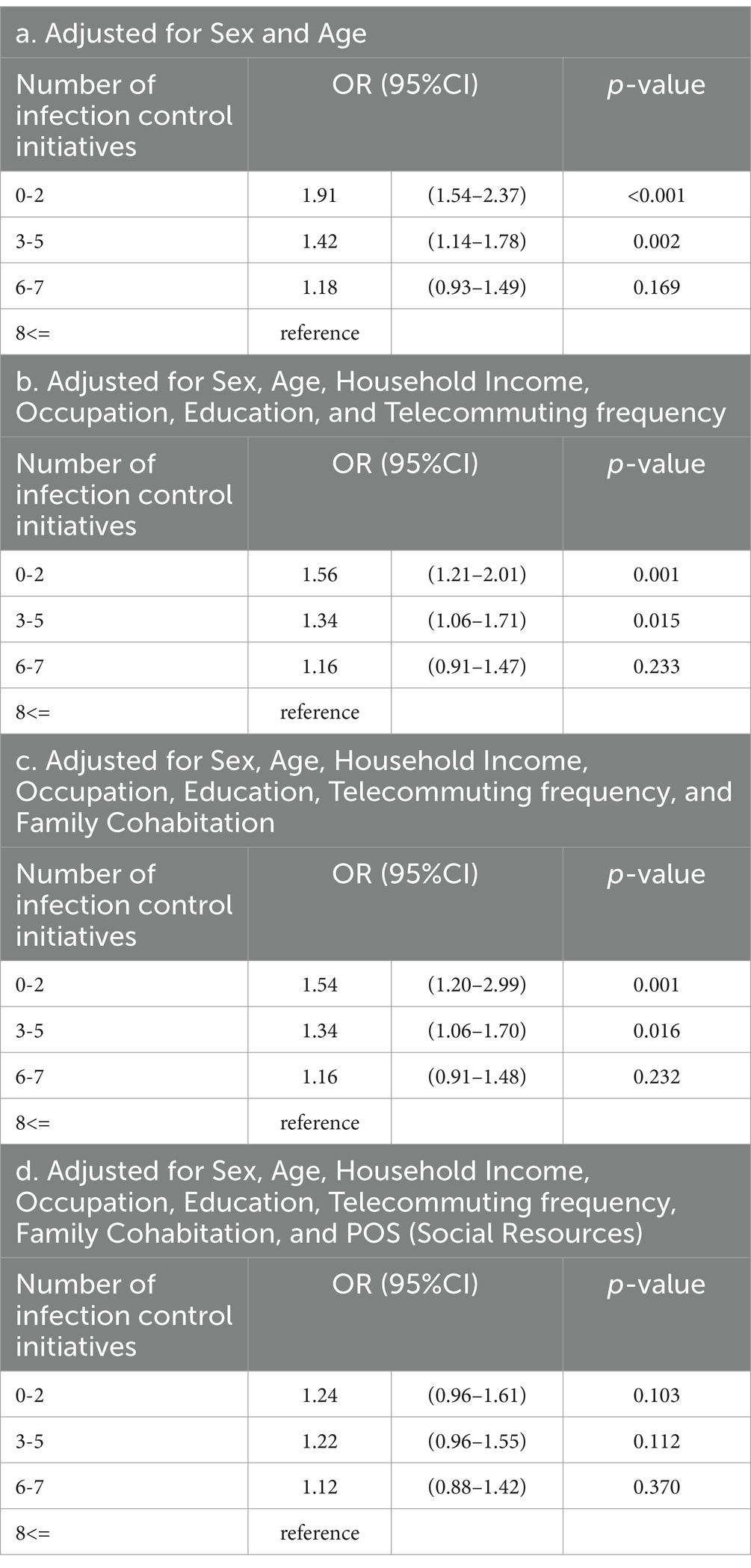
Results: Among the participants, 22.1, 23.6, 22.2, and 32.1% worked at companies that implemented 0–2, 3–5, 6–7, and 8 or more infection control practices, respectively. Loneliness was reported by 6.3% of the participants. After adjustments for sex and age, the OR of the group with the fewest infection control practices was 1.91 (95% CI: 1.54–2.37, p < 0.001) compared with the group with the most practices adopted. Adjusting the model for household income, education, occupation, telecommuting frequency, and family cohabitation decreased the OR for the group with the fewest infection control practices adopted to 1.54 (95% CI: 1.20–2.99, p = 0.001). After adjustments for either POS, these associations became non-significant.
Discussion: Proactive infection control practices at work were positively associated with workers’ experiences of loneliness. Conversely, loneliness owing to fewer infection control practices was attenuated after adjusting for POS.
1 Introduction
The practices implemented in 2020 in response to the COVID-19 pandemic caused considerable changes, curtailing or reducing social activities in people’s everyday lives and work environments. Many countries have implemented strategies to mitigate the risk of the 3 Cs: crowded areas, close-contact environments, and closed spaces. The restriction of social interactions, called lockdowns, was also implemented in some countries. In Japan, the government temporarily enacted a state of emergency and recommended the preventive measures for the 3 Cs (1). For example, individuals were advised to avoid going out for meals, drinks, and shopping, and to work from home by telecommuting and teleworking.
Workplace infection control was a major initiative for COVID-19 infection control during the early months of the pandemic. At work, individuals interact in closed spaces for relatively long periods. This leads to the spread of virus owing to the strong infectivity and airborne transmission routes of COVID-19. In Japan, the following practices were recommended and implemented in many workplaces, in accordance with the Guide to Countermeasures for COVID-19 for the Workplace (2): voluntarily restricting or reducing business travel, visitors, and in-person company meetings; encouraging limitations on social events and dinners; enforcing mandatory mask-wearing during work hours; installing partitions and reconsidering office layouts; recommending daily temperature checks and teleworking; and banning eating at desks.
During the COVID-19 pandemic, the infection control practices implemented in workplaces had diverse impacts on mental health, leading to a deterioration of conditions such as depression, anxiety, and insomnia (3, 4). Additionally, loneliness emerged as a significant social issue (5). Loneliness frequently signifies a sense of societal and community isolation (6) and is linked to not only psychological distress but also depression, anxiety, sleep disorders, and other psychiatric disorders (7–9). Loneliness leads to increased morbidity of psychiatric disorders and risk of mortality, including suicide (10, 11). Maintaining physical distance from others and reducing opportunities for communication among workers negatively affected their feelings of loneliness. Research has shown that the number of individuals feeling lonely rose during the COVID-19 pandemic, compared with the period before COVID-19 (12, 13). The proportion of individuals who reported experiencing loneliness varied, with rates ranging between 20 and 55.2% (6, 10, 14–16) in different countries, and reported as 41.4% (17) in Japan.
However, the influence of workplace infection control practices against COVID-19 on loneliness remains unclear. Generally, these practices may have had a negative impact on workers’ mental health and performance because many of them required physical distancing from others and reduced communication opportunities (18). Meanwhile, the implementation of appropriate infection control practices in the workplace may have been positively perceived by employees as an organizational attitude that represents the employer’s concern for the health and safety of employees, thus increasing employees’ perceived organizational support (POS). POS is defined as the general perception of the extent to which an organization values the contributions of its employees and cares about their well-being (19, 20). It represents two logically distinct aspects of the organization’s positive evaluation of one’s contribution and the organization’s consideration for one’s well-being (21). A negative relationship between POS and loneliness at work has been reported (22). We hypothesized that workers’ loneliness increased as more infection control practices were implemented in the workplace. However, positive infection control practices in the workplace may have also increased workers’ POS and moderated their loneliness and its negative effect on their mental health. As such, we examined the relationship between employees’ loneliness and workplace infection control practices, including the relationship with POS.
2 Methods
2.1 Subjects
We conducted a prospective cohort investigation via an online survey. The initial survey was conducted in December 2020, followed by a subsequent survey in December 2021. This research was a component of the the Collaborative Online Research on the Novel-coronavirus and Work (CORoNaWork) project and received approval from the Ethics Committee of the University of Occupational and Environmental Health, Japan (reference number R2-079 and R3-006). All participants in the study were requested to fill out online questionnaires both at the initial phase and during the follow-up. They were informed about the study’s objectives and gave their informed consent. The survey was conducted by Cross Marketing Inc., based in Tokyo, Japan, which has a pool of 4.7 million pre-registered monitors. An initial email was sent to 60,531 men and women aged 20–65 years, and 55,045 responded to the initial screening questions. A total of 33,087 responses fulfilled the inclusion criteria (related to the respondent’s age, sex, region of residence, and employee status), whereas 6,051 were excluded as invalid responses. We set the following exclusion criteria: extremely brief response time (<6 min), unusually low body weight (<30 kg) or height (<140 cm), inconsistent answers to similar queries (such as marital status or region of residence), and incorrect answers to questions specifically designed to identify invalid responses. Among the 27,036 individuals eligible at baseline, 11,622 who felt lonely at baseline were excluded; of the remaining 15,414 eligible for follow-up, 10,770 (69.9%) were enrolled in the follow-up study. Following the exclusion of 208 individuals who were not employed at the time of follow-up, a total of 10,562 individuals were finally included in the analysis. Figure 1 illustrates the selection process. This paper was prepared in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (23).

Figure 1. Flowchart of the sample selection procedure in this study. The following exclusion criteria were set: extremely brief response time (<6 min), unusually low body weight (<30 kg) or height (<140 cm), inconsistent answers to similar queries (such as marital status or region of residence), and incorrect answers to questions specifically designed to identify invalid responses.
2.2 Assessment of workplace infection control practices
We identified 10 specific practices related to workplace infection prevention: limiting or refraining from business trips and visitors; reducing or requesting limits on attendees at social events and dinners; decreasing or limiting in-person internal meetings; enforcing mandatory mask-wearing during work hours; installing partitions and modifying workplace layouts; recommending daily temperature checks at home; promoting telecommuting; forbidding eating at desks; and advising employees to stay home when feeling unwell. The respondents answered “yes” or “no” according to their experiences. We categorized the respondents into four groups based on the number of practices to which they answered “yes”: 0–2, 3–5, 6–7, and 8 or more items.
2.3 Assessment of loneliness
We used the University of California, Los Angeles Loneliness Scale (24), and participants were categorized as lonely when they answered “always” to any of following questions: “Do you feel like you do not socialize with others?”; “Do you feel left out from others?”; and “Do you feel isolated from others?”.
2.4 Assessment of POS
The assessment of POS was conducted by asking respondents how strongly they agreed with the statement: “Your organization assists its staff in achieving equilibrium between dynamic, efficient work and a lifestyle that promotes health.” This statement was focused on the organizational support for employees’ health and work-life balance. Answers were given on a four-point scale: strongly agree, agree, disagree, and completely disagree. The responses were then categorized into four levels of perceived support: very high (4 points), high (3 points), low (2 points), and very low (1 point).
2.5 Other covariates
Potential confounders included the respondent’s occupation (deskwork, interpersonal, or manual), educational attainment (middle school, high school, or university degree and above), workplace size (<10, 10–49, 50–99, 100–999, or >1,000 employees), household income, living arrangement (with/without family member/s), and number of individuals working at home (at least 4 days per week, at least 2 days per week, at least 1 day per week, at least 1 day per month, and almost never). Participants answered “yes” or “no” to the following inquiry: “Do you feel lonely?”.
2.6 Statistical analysis
We calculated the odds ratios (ORs) of loneliness associated with each workplace infection control practice using multilevel logistic regression nested by region of residence. We progressively added subjective ratings of sex, age, education, occupation, household income, family cohabitation, POS, and friendships to the model as adjustment factors. A p value less than 0.05 was considered statistically significant. All the data analyses in the study were conducted using Stata17 (Stata, College Station, TX, United States).
3 Results
Table 1 lists the fundamental characteristics of the participants, categorized into four groups based on the number of infection control practices adopted in their workplaces. Notably, small companies with fewer than 10 employees accounted for more than half of those that tended to have few infection control measures (0–2). The number of infection control practices in the workplace tended to increase with company size.
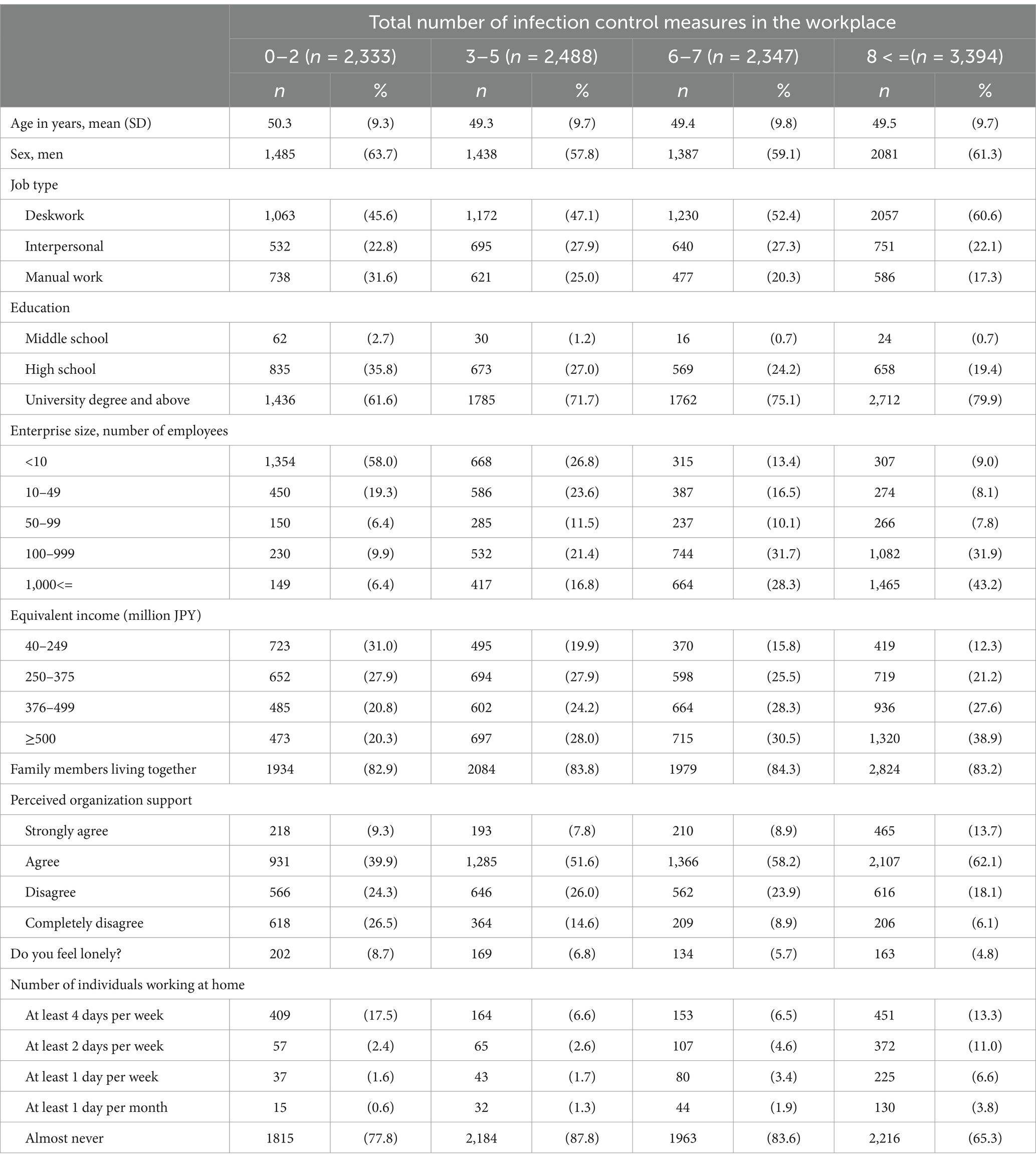
Table 1. Characteristics of participants according to the number of infection control practices implemented in their workplace.
Table 2 presents the number and rate of infection control practices in the workplace. “Mandatory mask-wearing during work hours” and “reducing or requesting limits on attendees at social events and dinners” tended to be the most common practices adopted in companies that implemented few and many practices, respectively. Meanwhile, “forbidding eating at desks” was rarely reported.
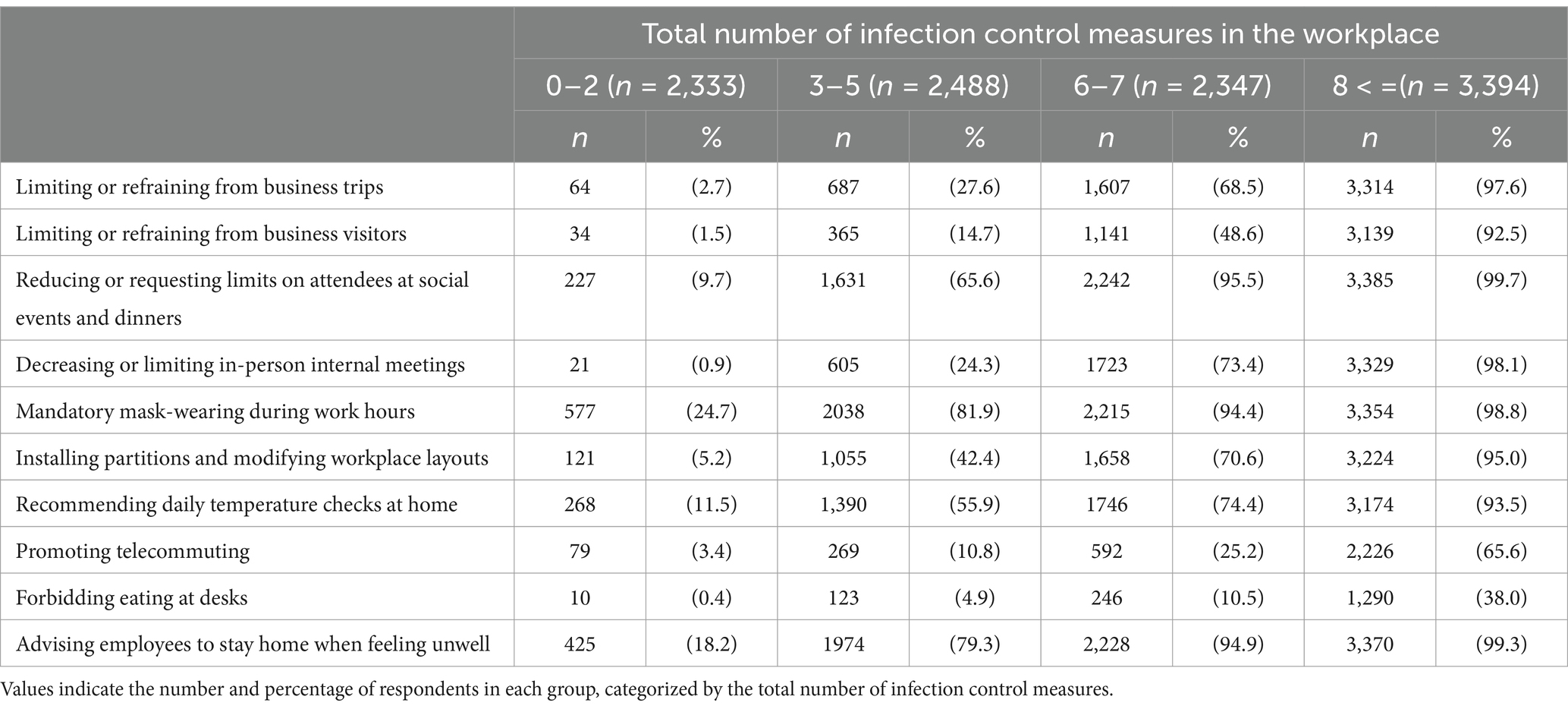
Table 2. Adoption of infection control practices in each respondent grouped by total number of infection control measures implemented.
Multivariable adjusted ORs for age and sex of individuals experiencing “loneliness” for the number of infection control practices at work are shown in Table 3a. Compared with the group with the highest number of infection control practices at work (8 or more), the ORs for loneliness increased in the groups with fewer infection control practices. The group with the fewest measures (0–2) had significantly higher ORs (1.91, 95% CI: 1.54–2.37, p < 0.001) in the age- and sex-adjusted model (Table 3a). When the model was adjusted for household income, occupation, education, and telecommuting frequency (Table 3b), the ORs in the group with the fewest measures (0–2) significantly decreased to 1.56 (95% CI: 1.21–2.01, p = 0.001), further decreasing to 1.54 (95% CI: 1.20–2.99, p = 0.001) in the model adjusted for family cohabitation (Table 3c). After the model was further adjusted by adding “POS” (Table 3d), the number of workplace infection control practices and feelings of loneliness no longer showed a significant association.
4 Discussion
We evaluated the relationship between the number of workplace infection control practices and loneliness during the COVID-19 pandemic, and found that fewer infection control practices in the workplace were associated with more workers feeling lonely. This association was attenuated by employees’ POS. Notably, our results contradicted our initial hypothesis. Infection control practices during the COVID-19 pandemic have been reported to be associated with increased loneliness because of the reduced social involvement (14). Many of the workplace infection control practices that we examined in this study focused on avoiding interaction and contact with other people; therefore, we speculated that workers’ loneliness would increase. However, our findings showed that more positive and appropriate infection control practices in the workplace made workers feel less lonely.
We analyzed the underlying reasons for these unexpected associations. First, continuing to work in a facility that had difficulty implementing infection control practices during a rapid increase in COVID-19 cases could have led to an increased fear of infection risk and related events, such as hospital admission and death from COVID-19, which might have led to isolation from society and loneliness. Fear and anxiety related to COVID-19 have been reported to negatively affect people’s mental status (25). However, in line with our current findings, a prior report indicated that the implementation of workplace infection prevention and control practices during the early months of the COVID-19 pandemic and the increase in the number of infection prevention and control practices were positively related to improvements in the work engagement and mental health of employees (26). In addition, a study conducted among community residents reported an association between preventive behaviors against COVID-19 and decreased loneliness (17).
Second, some organizations may not have been interested in infection control even during the peak of the COVID-19 pandemic in 2020. These companies may not only have inadequate management systems for health and safety and for infection control but also little interest in the welfare and well-being of their workers. Working in such establishments may have increased feelings of isolation owing to insufficient support from the company and a lack of solidarity in the workplace. Indeed, a lack of social support leads to deterioration in workers’ mental health (27), while their loneliness decreases with higher perceived social support (28).
Third, our initial hypothesis may have ignored many other possible confounding factors related to infection control and work-related loneliness. The confounders were divided into individual and workplace/company types. Individual-level confounders included differences in individuals’ family relationships, economic status, education, and telecommuting frequency. However, our results revealed that the presence or absence of a family member living with the respondent did not show an association between infection control and loneliness (Tables 3b,c). Thus, feelings of loneliness while living with family members depended on how an individual felt, which might not be reflected in the differences between the presence or absence of family members. Although this study was unable to assess the association between intrafamily relationships and loneliness, our previous study reported that those who spent more time with their families were less likely to feel lonely during the COVID-19 pandemic (29). These relationships may need to be evaluated in the future. Nonetheless, the results regarding the differences between confounding factors and pathways must be interpreted with caution. Conversely, workplace-level confounders included workplace size and type, attitudes toward health and safety initiatives, and health culture. We adjusted for company size and type, but the effects of these factors were small. Further investigation is required to elucidate whether these factors are confounders or underlying mechanisms.
The results show that positive infection control in the workplace is associated with improvement in POS, which reduces loneliness. Before we conducted our study, we believed that workplace infection control could lead to increased risks of loneliness and isolation by reducing opportunities for interaction and communication among workers—our results demonstrated the opposite. POS for infection prevention during the COVID-19 pandemic has been reported to improve work engagement (30). Moreover, given that adjusting for POS lowered the loneliness reported by those working at companies that implemented few infection control practices, we speculated that POS had a positive relationship on workers and contributed to a reduction in loneliness. Alternatively, if workers do not feel supported by the organization because of inadequate implementation of infection control practices, then POS may not be a confounder but rather a mechanism.
Our results indicate that aggressive infection control practices based on precautionary principles have a favorable connection to workers’ feelings of loneliness. Many workplace infection control practices against the spread of COVID-19 were not necessarily evidence-based or empirically implemented based on precautionary principles for public health, and the negative effects of infection control measures, such as isolation, could be greater than the benefits of infection control. Exploring the effectiveness of workplace infection control practices against COVID-19 remains necessary. However, our results emphasized the socio-psychological benefits of the positive implementation of infection control practices in the workplace.
Our study has several limitations. First, workplace infection control was self-reported. However, to our knowledge, no established evaluation method exists other than self-report. We assumed that the estimated chances of misunderstanding by the respondents were low because infection control measures in the workplace were widely described in the guidelines of Japanese workplaces/companies. It is also possible that loneliness might have increased with lower perceived appropriateness, as the adequacy and effectiveness of infection control was not assessed for workers in this study, thus warranting further investigation. Second, the survey on workplace infection control practices was evaluated only at baseline, and it was unclear how the observation timing affected the results of the relationship between infection control measures in the workplace and loneliness. Many companies may have increased the number of their infection control practices as the COVID-19 pandemic lingered, and longer periods of infection control may be considered to have more psychological impact than shorter periods. Notably, these possible misclassifications may have underestimated the original association; therefore, our arguments were not affected by this issue. Third, in this study, the association between the level of infection control measures in the workplace and loneliness was evaluated rather than those between each infection control measure and loneliness. Thus, future studies should examine the latter association. In addition, loneliness may increase with lower perceived appropriateness, as the adequacy and effectiveness of infection control was not assessed for workers in this study. There remains a possibility that unmeasured confounders, such as hobbies, availability of pets, and religion, may have been associated with our results, although we adjusted for several potential confounders. Therefore, further investigation may be needed. Finally, we assessed loneliness using simple self-report items from the University of California, Los Angeles Loneliness Scale. Additionally, POS was also evaluated by a single question; although the measurement validity was untested, the same indicator was previously used (30).
In conclusion, workers experienced less loneliness at workplaces with active infection control practices. This association can be related to human relationships and POS, which can be involved as both confounders or contributing elements in the relationship between the number of infection control practices and loneliness in the workplace.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This research was received approval from the Ethics Committee of the University of Occupational and Environmental Health, Japan (reference number R2-079 and R3-006). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MF: Conceptualization, Writing – original draft. SN: Conceptualization, Writing – original draft. RM: Writing – review & editing. KO: Writing – review & editing. AH: Writing – review & editing. ST: Funding acquisition, Project administration, Writing – review & editing. MT: Funding acquisition, Project administration, Writing – review & editing. KY: Conceptualization, Writing – review & editing. SM: Funding acquisition, Project administration, Writing – review & editing. YF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was partly supported and funded by research grants from the University of Occupational and Environmental Health, Japan; Japanese Ministry of Health, Labour and Welfare (H30-josei-ippan-002, H30-roudou-ippan-007, 19JA1004, 20JA1006, 210,301–1, and 20HB1004); Anshin Zaidan, the Collabo-Health Study Group, Hitachi Systems, Ltd., and scholarship donations from Chugai Pharmaceutical Co., Ltd. These funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Available online at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00094.html (Accessed Dec 13, 2023).
2. Available online at: https://www.sanei.or.jp/files/topics/covid/COVID-19guide221227koukai.pdf (Accessed Dec 13, 2023).
3. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
4. Kim, HH, and Laurence, J. COVID-19 restrictions and mental distress among American adults: evidence from Corona impact survey (W1 and W2). J Public Health. (2020) 42:704–11. doi: 10.1093/pubmed/fdaa148
5. Gloster, AT, Lamnisos, D, Lubenko, J, Presti, G, Squatrito, V, Constantinou, M, et al. Impact of COVID-19 pandemic on mental health: an international study. PLoS One. (2020) 15:e0244809. doi: 10.1371/journal.pone.0244809
6. Banerjee, D, and Rai, M. Social isolation in COVID-19: the impact of loneliness. Int J Soc Psychiatry. (2020) 66:525–7. doi: 10.1177/0020764020922269
7. Cacioppo, JT, Hawkley, LC, Berntson, GG, Ernst, JM, Gibbs, AC, Stickgold, R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol Sci. (2002) 13:384–7. doi: 10.1111/1467-9280.00469
8. Jackson, J, and Cochran, SD. Loneliness and psychological distress. J Psychol. (1991) 125:257–62. doi: 10.1080/00223980.1991.10543289
9. Santini, ZI, Jose, PE, York Cornwell, E, Koyanagi, A, Nielsen, L, Hinrichsen, C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. (2020) 5:e62–70. doi: 10.1016/S2468-2667(19)30230-0
10. Kan, Z, Søegaard, EGI, Siqveland, J, Hussain, A, Hanssen-Bauer, K, Jensen, P, et al. Coping, social support and loneliness during the COVID-19 pandemic and their effect on depression and anxiety: Patients' experiences in community mental health centers in Norway. Healthcare. (2022) 10:875. doi: 10.3390/healthcare10050875
11. Leigh-Hunt, N, Bagguley, D, Bash, K, Turner, V, Turnbull, S, Valtorta, N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
12. Ernst, M, Niederer, D, Werner, AM, Czaja, SJ, Mikton, C, Ong, AD, et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am Psychol. (2022) 77:660–77. doi: 10.1037/amp0001005
13. Su, Y, Rao, W, Li, M, Caron, G, D'Arcy, C, and Meng, X. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int Psychogeriatr. (2023) 35:229–41. doi: 10.1017/S1041610222000199
14. Benke, C, Autenrieth, LK, Asselmann, E, and Pané-Farré, CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
15. Giorgi, G, Lecca, LI, Alessio, F, Finstad, GL, Bondanini, G, Lulli, LG, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. (2020) 17:7857. doi: 10.3390/ijerph17217857
16. Kirkland, SA, Griffith, LE, Oz, UE, Thompson, M, Wister, A, Kadowaki, L, et al. Increased prevalence of loneliness and associated risk factors during the COVID-19 pandemic: findings from the Canadian longitudinal study on aging (CLSA). BMC Public Health. (2023) 23:872. doi: 10.1186/s12889-023-15807-4
17. Stickley, A, Matsubayashi, T, and Ueda, M. Loneliness and COVID-19 preventive behaviours among Japanese adults. J Public Health. (2021) 43:53–60. doi: 10.1093/pubmed/fdaa151
18. Pai, N, and Vella, SL. COVID-19 and loneliness: a rapid systematic review. Aust N Z J Psychiatry. (2021) 55:1144–56. doi: 10.1177/00048674211031489
19. Eisenberger, R, Huntington, R, Hutchison, S, and Sowa, D. Perceived organizational support. J Appl Psychol. (1986) 71:500–7. doi: 10.1037/0021-9010.71.3.500
20. Eisenberger, R, and Stinglhamber, F. Perceived organizational support: Fostering enthusiastic and productive employees. Washington, DC: American Psychological Association Books. (2011) 25–60.
21. Kobayashi, Y, Nagata, T, Fujino, Y, Hino, A, Tateishi, S, Ogami, A, et al. Association between perceived organizational support and COVID-19 vaccination intention: a cross-sectional study. J Occup Health. (2021) 63:e12308. doi: 10.1002/1348-9585.12308
22. Tian, G, Liu, T, and Yang, R. Workplace loneliness mediates the relationship between perceived organizational support and job performance: differing by extraversion. Front Psychol. (2023) 14:1058513. doi: 10.3389/fpsyg.2023.1058513
23. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
24. University of California, Los Angeles Loneliness Scale. Availabled online at: https://fetzer.org/sites/default/files/images/stories/pdf/selfmeasures/Self_Measures_for_Loneliness_and_Interpersonal_Problems_UCLA_LONELINESS.pdf (Accessed May 20, 2024).
25. Eguchi, H, Hino, A, Inoue, A, Tsuji, M, Tateishi, S, Ando, H, et al. Effect of anxiety about COVID-19 infection in the workplace on the association between job demands and psychological distress. Front Public Health. (2021) 9:722071. doi: 10.3389/fpubh.2021.722071
26. Ikegami, K, Ando, H, Fujino, Y, Eguchi, H, Muramatsu, K, Nagata, T, et al. Workplace infection prevention control measures and work engagement during the COVID-19 pandemic among Japanese workers: a prospective cohort study. J Occup Health. (2022) 64:e12350. doi: 10.1002/1348-9585.12350
27. Kikunaga, K, Nakata, A, Kuwamura, M, Odagami, K, Mafune, K, Ando, H, et al. Psychological distress, Japanese teleworkers, and supervisor support during COVID-19. J Occup Environ Med. (2023) 65:e68–73. doi: 10.1097/JOM.0000000000002756
28. Groarke, JM, Berry, E, Graham-Wisener, L, McKenna-Plumley, PE, McGlinchey, E, and Armour, C. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 psychological wellbeing study. PLoS One. (2020) 15:e0239698. doi: 10.1371/journal.pone.0239698
29. Fujii, R, Konno, Y, Tateishi, S, Hino, A, Tsuji, M, Ikegami, K, et al. Association between time spent with family and loneliness among Japanese workers during the COVID-19 pandemic: a cross-sectional study. Front Psych. (2021) 12:786400. doi: 10.3389/fpsyt.2021.786400
30. Odagami, K, Nagata, T, Mafune, K, Ando, H, Tateishi, S, Kuwamura, M, et al. Association between perceived organizational support for infection prevention and work engagement during the COVID-19 pandemic among Japanese workers: a prospective cohort study. Int J Environ Res Public Health. (2022) 19:16142. doi: 10.3390/ijerph192316142
Keywords: COVID-19, Japan, loneliness, occupational health, perceived organizational support
Citation: Funada M, Noguchi S, Matsugaki R, Odagami K, Hino A, Tateishi S, Tsuji M, Yatera K, Matsuda S and Fujino Y (2025) Association of workplace infection control and perceived organizational support on worker loneliness during the COVID-19 pandemic. Front. Public Health. 13:1558282. doi: 10.3389/fpubh.2025.1558282
Edited by:
Wenjie Duan, East China University of Science and Technology, ChinaReviewed by:
Lambert Zixin Li, Stanford University, United StatesSatoru Kanamori, Teikyo University, Japan
Copyright © 2025 Funada, Noguchi, Matsugaki, Odagami, Hino, Tateishi, Tsuji, Yatera, Matsuda and Fujino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yoshihisa Fujino, emVucUBtZWQudW9laC11LmFjLmpw
 Midori Funada
Midori Funada Shingo Noguchi2
Shingo Noguchi2 Ryutaro Matsugaki
Ryutaro Matsugaki Kiminori Odagami
Kiminori Odagami Ayako Hino
Ayako Hino Seiichiro Tateishi
Seiichiro Tateishi Kazuhiro Yatera
Kazuhiro Yatera Yoshihisa Fujino
Yoshihisa Fujino