- 1World Health Organization Regional Office for Africa, Brazzaville, Republic of Congo
- 2Geomatys, Montpellier, France
- 3New York University School of Global Public Health, New York, NY, United States
- 4Scientific Computing Program - Oswaldo Cruz Foundation, FIOCRUZ, Rio de Janeiro, Brazil
- 5Centre for Health Services Studies (CHSS), University of Kent, Canterbury, United Kingdom
- 6World Health Organization Country Office, Abuja, Nigeria
- 7World Health Organization Country Office, Asmara, Eritrea
- 8World Health Organization Country Office, Harare, Zimbabwe
- 9UNICEF Headquarters, Nairobi, Kenya
During a public health emergency, early implementation of response activities is crucial for saving lives and protecting livelihoods. The COVID-19 pandemic, declared by the World Health Organization (WHO) on March 11, 2020, posed a global public health crisis that required timely decision-making despite limited data and capacity. In this context, WHO’s Regional Office for Africa (AFRO) developed the Situations of Concern (SOC) classification system to assess and monitor epidemiological risk across its 47 Member States. We conducted a retrospective analysis to evaluate the performance and operational utility of the SOC system. Using weekly country-level COVID-19 surveillance data, we found that the system demonstrated strong alignment with epidemic wave patterns, with a sensitivity of 83% and specificity of 88%. SOC classifications supported timely operational decision-making in over 70% of documented support instances. Effective management of limited resources through SOC assessments also helped ensure fair distribution of support across communities. Our findings suggest that adaptable classification systems like SOC can provide effective decision-support under conditions of limited data availability, improving outbreak preparedness and response in resource-constrained settings.
Introduction
The COVID-19 pandemic, caused by the sudden emergence of SARS-CoV-2 from an animal reservoir (1), posed unprecedented challenges for modern health emergency response systems worldwide (2). At the onset of the pandemic, with response systems still being established and the potential impact of the virus largely unknown, countries implemented sweeping measures such as travel bans and the interruption of major societal functions. These actions, while necessary to curb transmission, led to significant economic and social disruptions (3–5). In addition to these technical interventions, many countries emphasized behavioral non-pharmaceutical interventions (NPIs)—such as mask-wearing, hand hygiene, and physical distancing—sometimes referred to as “behavioral vaccines” (6). These practices played a vital role in reducing transmission regardless of geographic or socioeconomic context. In the World Health Organization (WHO) African Region (AFR), where many Member States (MS) had limited preparedness capacities, reliance on such blanket measures was pronounced. In contrast, countries with more advanced capacities were able to lift restrictions earlier, leveraging strategies such as widespread testing to limit viral spread (7–9).
Decisions regarding when and how to act, as well as how to allocate limited resources, were critical in containing SARS-CoV-2 transmission. By 2021, the second year of the pandemic, most AFR Member States had emerged from initial lockdowns. However, new waves of COVID-19 driven by variants with distinct transmissibility and severity profiles began affecting populations at different times (10). One of the core responsibilities of the WHO Regional Offices during the pandemic was to rapidly assess the needs of Member States, make evidence-based recommendations for response activities, and support these efforts through resource mobilization. Although individual countries maintained their own monitoring and evaluation systems for national and sub-national operations, these systems varied widely in their objectives, data quality, and ability to account for unique local contexts. Crucially, no unified system existed to enable cross-country assessment of the pandemic’s impact within a region while accounting for such variations. This gap highlighted the need for a regional operational classification system capable of informing decisions about scaling response activities up or down in line with each country’s changing epidemiological landscape. While a global system was under development by a WHO Headquarters team in Geneva to coordinate efforts across all six regions (11), the Regional Office for Africa (AFRO) developed an interim system tailored to the immediate needs and specific contexts of its 47 Member States.
In June 2021, the Incident Management Support Team (IMST) for the AFR Regional COVID-19 response introduced a set of indicators using basic epidemiological data from Member States to track the pandemic’s trajectory. These indicators, collectively termed Situations of Concern (SOC), enabled systematic classification of Member States into epidemic categories (“low incidence,” “very high incidence,” “alert,” and “resurgence”) based on national disease burden and public health impact. Classification assignments were informed by criteria such as recent trends in new cases and deaths, incidence per capita, COVID-19 test positivity rates, and vaccination coverage. These indicators were assessed weekly to categorize each Member State, providing a foundation for operational decision-making regarding resource allocation.
Following the emergence of the SARS-CoV-2 Omicron variant and subsequent changes in transmission dynamics, the SOC indicator criteria were adjusted in September 2022 (12). These adjustments allowed the system to remain relevant and operationally useful, and several Member States adopted the SOC classification for subnational early warning and decision-making. At the global level, the classifications informed international efforts to monitor and prioritize epidemic situations across WHO regions (11).
Retrospective evaluations of decision-support systems are essential to assess their real-world impact, identify opportunities for improvement, and inform the design of future outbreak preparedness tools (13). Although future pandemics may differ from COVID-19, many of the systemic, logistical, and information-related challenges observed are likely to recur, particularly in resource-constrained settings (14).
This study retrospectively reviews the implementation of the WHO AFR’s SOC indicator-based decision-making system. It evaluates the system’s utility as an early warning and decision-making tool and its effectiveness in raising timely alerts about concerning epidemic situations across WHO AFR Member States. Conducting this retrospective analysis provides a critical opportunity to learn from past experience. Understanding the strengths and limitations of the SOC classification during the COVID-19 pandemic can inform the design of future surveillance systems and decision-making tools—especially in regions with limited resources and high epidemiological uncertainty.
Methods
Study design
This study utilized a retrospective analysis to assess the operational utility of the Situation of Concern (SOC) classification system in predicting and signaling observed COVID-19 trends across WHO African Region Member States. The analysis period covered the period from Epidemiological Week (EW) 23 of 2021 (June 7, 2021) to EW 6 of 2023 (February 6, 2023), corresponding to the timeframe during which the SOC classifications were implemented and used to guide operational decisions.
Participants
Inclusion criteria
All 47 Member States within the WHO African Region (15) were eligible for inclusion in the analysis. These Member States submitted COVID-19 surveillance data to the WHO Regional Office for Africa in compliance with the International Health Regulations (2005) (16). Each Member State served as an individual unit for SOC classification and epidemic wave assessment.
Procedure
Definitions
Confirmed COVID-19 cases were defined as individuals testing positive for SARS-CoV-2 by polymerase chain reaction (PCR) or antigen rapid diagnostic test (AgRDT), meeting either probable or suspected case definitions per WHO guidelines, or as an asymptomatic contact of a probable or confirmed case with a positive test result (17). COVID-19 deaths were defined as fatalities attributable to a clinically compatible illness in probable or confirmed COVID-19 cases, excluding deaths caused by unrelated factors (17).
National epidemic waves were identified retrospectively by examining weekly incidence trends. A COVID-19 epidemic “wave” was defined as a period of sustained and significant week-on-week increases in new cases, followed by a decline until weekly incidence returned to pre-wave levels. Wave events were characterized by two milestones. The “start” week was the epidemiological week when cases began rising, and the “peak” week was the week with the highest incidence, signifying the highest transmission period of SARS-CoV-2. For irregular data reporting, a 3-week moving average of incidence rates was used to determine peaks.
Data source
Primary epidemiological data on confirmed COVID-19 cases, deaths, testing rates, and vaccination coverage were obtained from Member State submissions to WHO’s Regional Office for Africa and published on the WHO’s global COVID-19 dashboard (18), in compliance with International Health Regulations (2005) (16). The data were aggregated by epidemiological week (Monday through Sunday) according to international standards of epidemiological data reporting (19).
COVID-19 Situation of Concern (SOC) classification
SOC classifications were assigned weekly to Member States based on the defined criteria. Initially, three criteria were used:
(i) A 20% or more increase in the weekly incidence or mortality over two consecutive weeks (or over four consecutive weeks for irregular reporting).
(ii) A 30% or more increase in weekly incidence compared to the previous peak and.
(iii) A weekly incidence ratio of 500 or more cases per 100,000 population.
A Member State was classified as being in “Resurgence” for the week under review if it met the first two criteria. For those classified as “Alert,” at least one of the first two criteria had to be met. Member States meeting only the third criterion were categorized as having “Very High Incidence.” If none of the criteria were met, the Member State was classified as “Low Incidence,” even if no new cases were reported. In cases where sufficient data were unavailable by the evaluation date, the existing classification was retained.
In September 2022, WHO AFRO began revising the methodology for the SOC classification in response to the unprecedented surge in COVID-19 cases and the altered transmission dynamics associated with the emergence of the Omicron variant. This period was marked by very high transmission rates and incidence levels, coupled with relatively lower mortality compared to earlier phases of the pandemic. During this transitional phase, Alert classifications were issued for suspected new epidemic events based on contextual assessments and patterns observed during pre-Omicron waves, even when official criteria were not met. However, Resurgence classifications were used less frequently due to uncertainty and challenges in maintaining consistent messaging while the criteria were under review.
By Epidemiological Week 1 of 2023, the following revised criteria were officially adopted for SOC classifications:
(i) A 20% or more increase in transmission indicators such as per-capita incidence ratio or test positivity rate (TPR).
(ii) A 20% or more increase in severity indicators such as new hospital admissions or mortality.
An “Alert (Rising) Concern” classification was issued when one of the two parameters increased over a two-week period. “Resurgence Concern” was assigned if one parameter increased over a three-week period. “Critical Concern” classification was designated if both parameters increased over a three-week period. An additional phase was introduced to the classification to account for an “Alert (Reduced) Concern,” to classify Member States showing a decline in either parameter over a two-week period. If none of the parameters were met, the Member State was classified as being of “No or Low concern” (Figure 1).
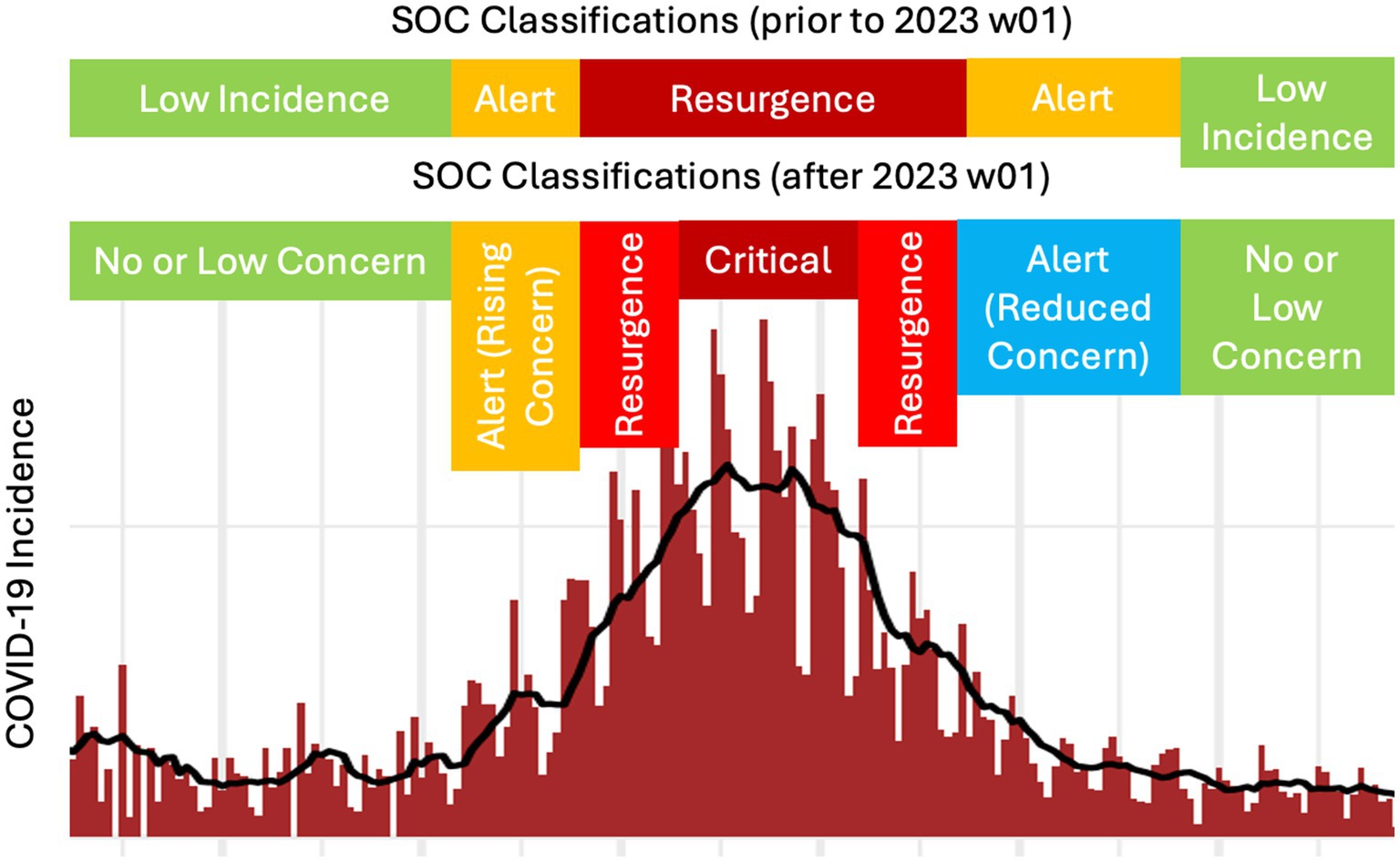
Figure 1. COVID-19 epidemic Situation of Concern (SOC) alert classifications as they relate to observed case incidence (here, shown for daily timesteps).
Data analysis
Calculation of epidemic indicators
The percentage change in incidence and mortality were computed as the week-on-week percentage difference in confirmed COVID-19 cases and deaths, respectively, (20). The test positivity rate was calculated as the proportion of positive tests among all SARS-CoV-2 tests conducted (21). The per-capita incidence ratio was expressed as the number of new cases per million population of the Member State (22). The vaccination coverage was calculated as the proportion of individuals who received at least one dose of a COVID-19 vaccine, using UN population estimates as the denominator (23, 24). Data analysis was conducted using R (version 4.0.3) (25).
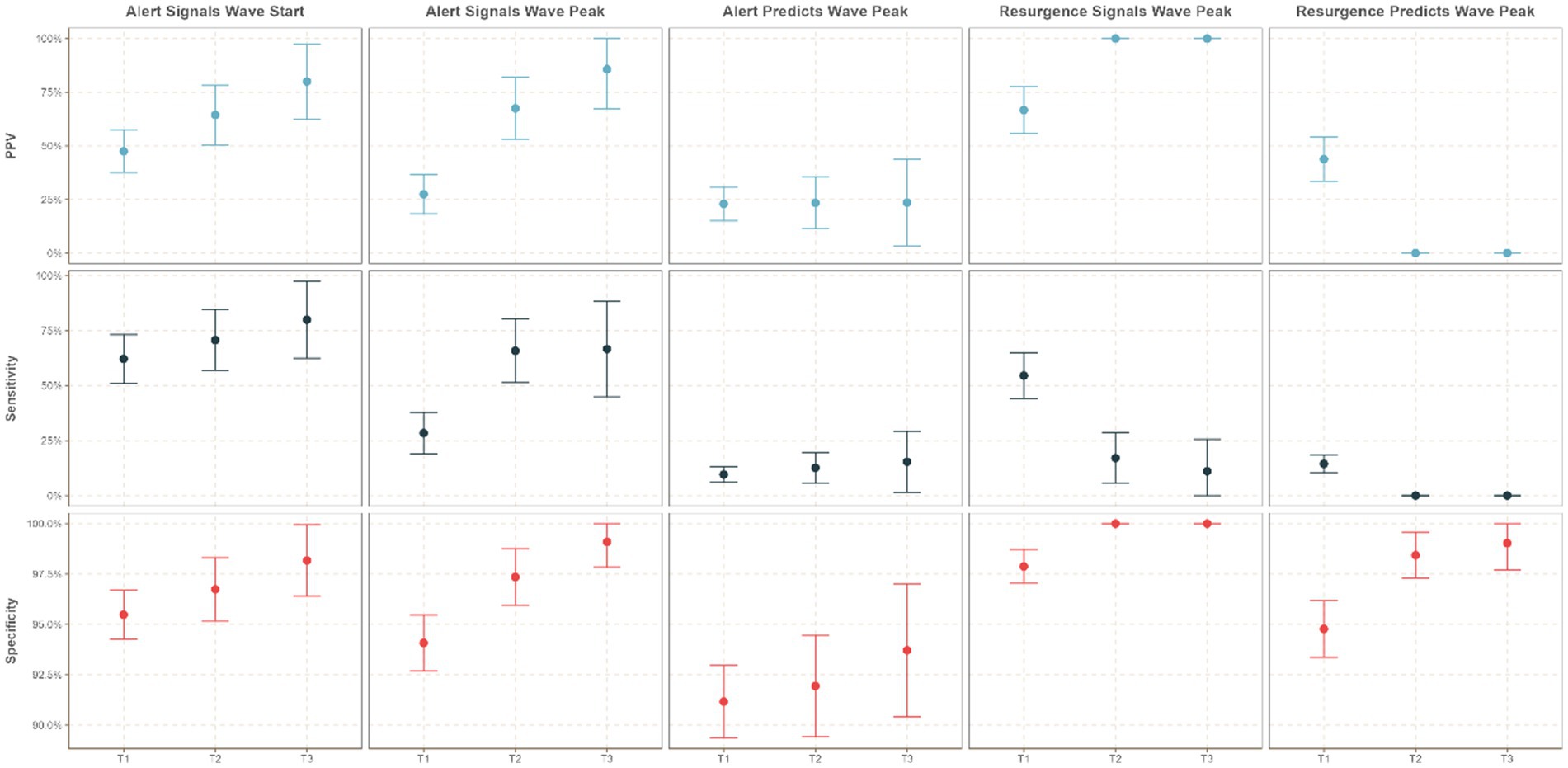
Evaluation of the operational utility of the SOC classification
The operational utility of the SOC classification system was evaluated based on five hypotheses focusing on the ability of Alert and Resurgence classifications to signal or predict the growing or re-emerging burden of COVID-19. The analyses assessed:
(1) The capacity of Alert or Resurgence classifications to signal the occurrence of an epidemic wave. This hypothesis addresses the specific purpose for which the SOC classification system was designed. The following hypotheses test for additional utility of the system by addressing timeliness and adaptability of the classifications.
(2) The ability of Alert classification to signal the start of a wave.
(3) The ability of Alert classification to predict or signal the peak of a wave.
(4) The ability of Resurgence classification to predict or signal the peak of a wave.
(5) The impact of Omicron-driven changes on classification utility, tested by evaluating performance pre- and post-criteria adjustments.
The term predict refers to instances where an SOC classification (Alert or Resurgence) was issued at least 2 weeks prior to the event of interest, providing early notice. In contrast, signal refers to SOC classifications issued within 2–3 weeks of the event, indicating an imminent or ongoing situation. Both measures were designed to evaluate how effectively the SOC indicators could guide preparedness and resource allocation within the WHO African region.
The evaluation of operational capacity began with an analysis of the ability of SOC classifications to signal the occurrence of a COVID-19 wave. This involved examining the success of issuing an Alert or Resurgence classification during periods extending from 3 weeks before the start of a wave to 3 weeks after its end. Recorded weekly SOC classifications were cross tabulated with documented epidemic wave events to compute performance metrics, including sensitivity, specificity, and positive predictive value (PPV).
The operational utility of the SOC classifications in predicting and signaling the start and peak of COVID-19 waves in a timely manner were then evaluated. Predictive ability was evaluated by determining whether an Alert or Resurgence classification was issued at least 2 weeks prior to the wave’s peak. For signaling ability, performance metrics (sensitivity, specificity, PPV) were calculated for Alert classifications issued within 3 weeks before or after the start of the wave; and for Alert or Resurgence classification issued within 2 weeks before or after the peak of the wave. Instances where no Alert or Resurgence classification was issued during the specified epidemic event periods represented false negatives (FNs), while false positives (FPs) referred to cases where an Alert or Resurgence classification was issued outside of these periods. FN and FP classifications were based on the hypotheses under evaluation and did not necessarily indicate errors in classification. In instances where epidemic events occurred in close succession, a single classification could align with the detection window of one wave while falling outside the window for another. To prevent counting a single alert as both a true and false positive, we conservatively classified such cases as true positives. This approach acknowledges the alert’s relevance in signaling ongoing or imminent transmission.
Time-stratified analysis
To assess the impact of the September 2022 adjustments on the operational utility of the SOC indicators in the context of the Omicron variant’s emergence, the study period was segmented into three distinct time strata:
• T1: Epidemiological Week (EW) 23 of 2021 to EW 7 of 2022, representing the period prior to the Omicron-driven changes in COVID-19 dynamics.
• T2: EW 8 of 2022 to EW 35 of 2022, corresponding to the Omicron surge period during which no adjustments were made to the SOC system.
• T3: EW 36 of 2022 to EW 6 of 2023, encompassing the period after the modified SOC criteria were introduced in response to the Omicron variant (Figure 2).
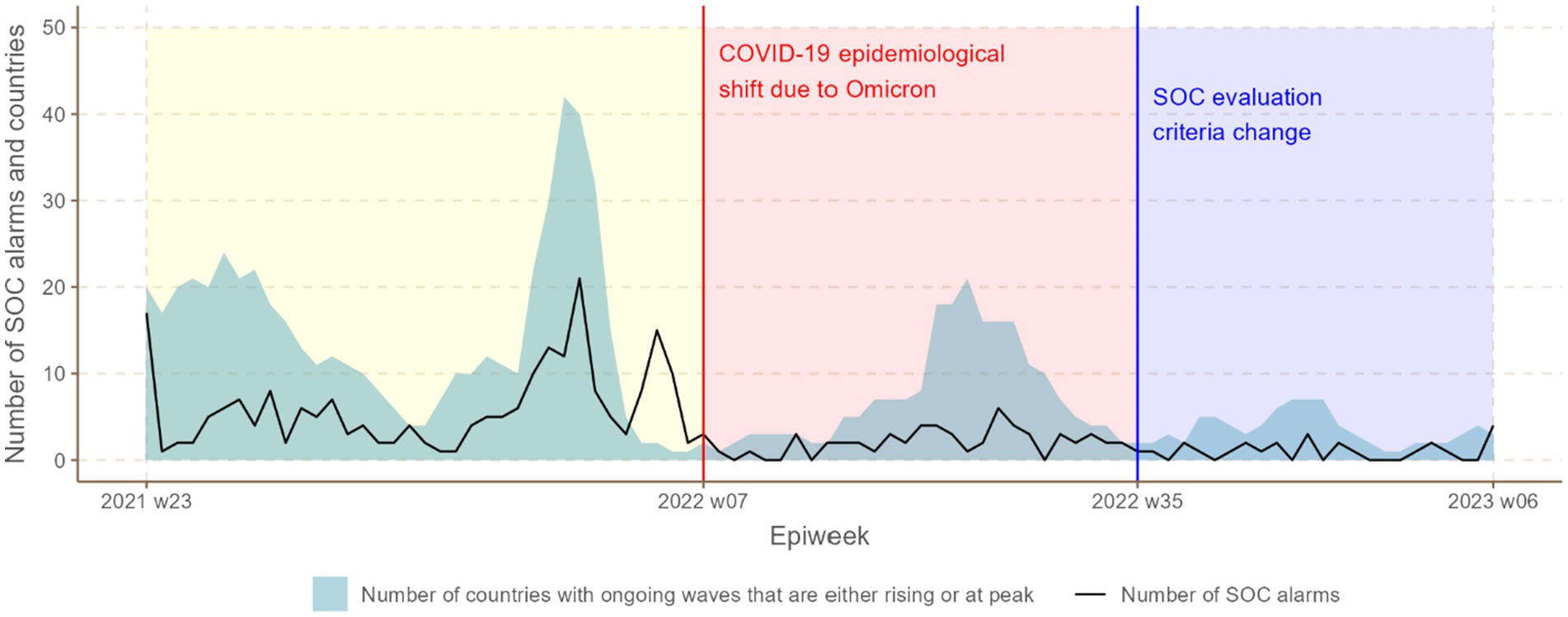
Figure 2. Temporal trends in number of SOC epidemic concern classifications (Alert or Resurgence classification) and epidemic waves over time stratified by time period during the COVID-19 pandemic.
The SOC classifications were reassessed for each period using the same analytical methods as the main analysis. Performance metrics, including sensitivity, specificity, and positive predictive value (PPV), were calculated and compared across the three time periods to assess differences in the system’s ability to predict and signal epidemic events. For this time-stratified analysis, the Critical Concern classification was categorized as a Resurgence classification, while only the Alert (Rising Concern) classification was considered as an Alert classification. The Alert (Declining Concern) classification was excluded from predictive and signaling performance analyses to maintain focus on rising epidemic trends.
Results
Descriptive analysis
Over the 88 epidemiological weeks analyzed, the WHO African Region recorded 146 national COVID-19 epidemic waves across its 47 Member States, as depicted in Figure 2. During this period, WHO AFRO issued 98 Resurgence and 204 Alert classifications, illustrated in Figures 2, 3. The relationship between national COVID-19 waves and SOC epidemic concern classifications is detailed in Figure 4 further shows the distribution of SOC classifications in relation to the start and peak of COVID-19 epidemic waves.
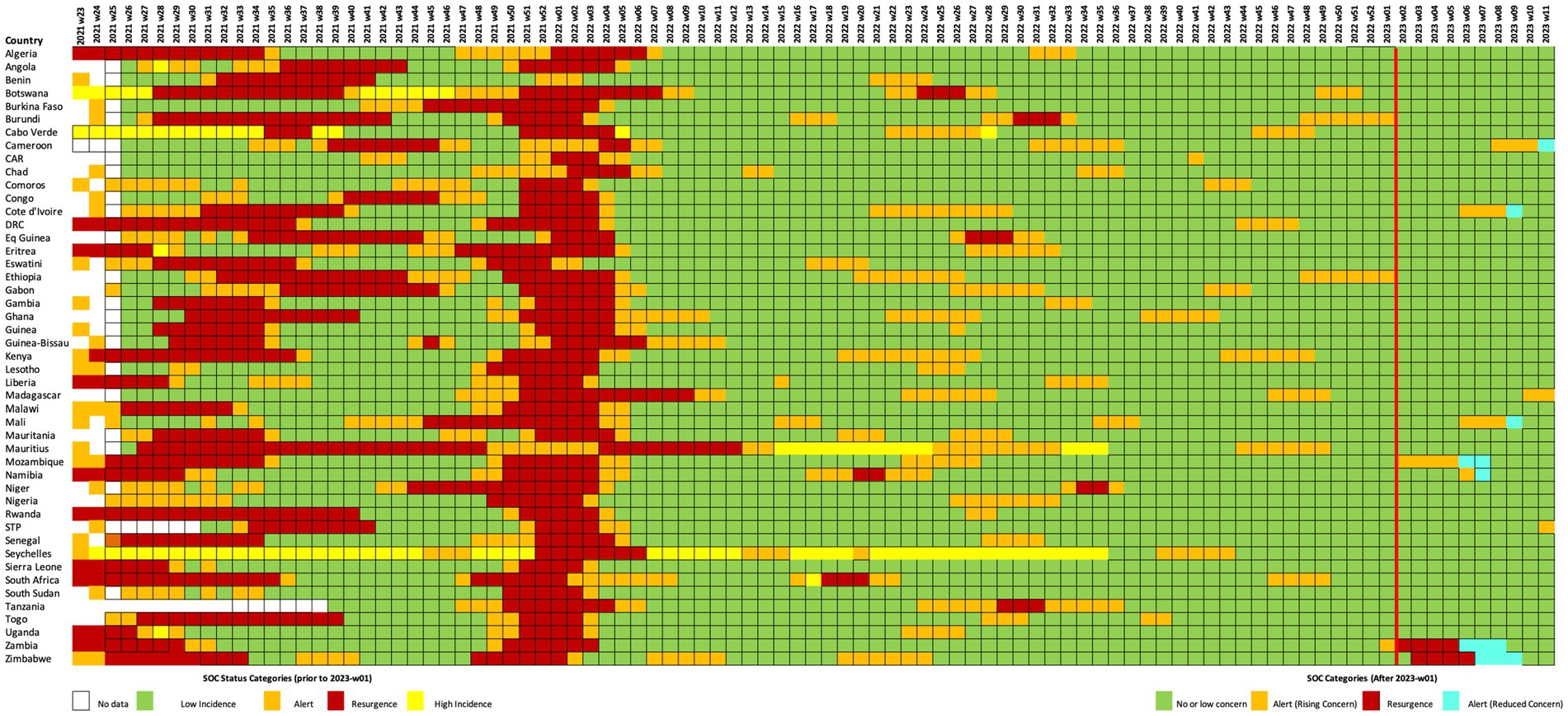
Figure 3. Weekly SOC classification of Member States from epidemiological week 23-2021 to week 11-2023. The red vertical line signifies when SOC criteria were revised to adapt to the shift in epidemiological characteristics provoked by emergence of the Omicron variant. The following colors signify the SOC classification in place for each week: Green = no or low concern, Yellow = Very High Incidence, Orange = Alert (rising or reduced concern, prior to revised SOC criteria; rising concern following revised SOC criteria), Red = Resurgence, and Blue = Alert (Reduced Concern), White = No classification.
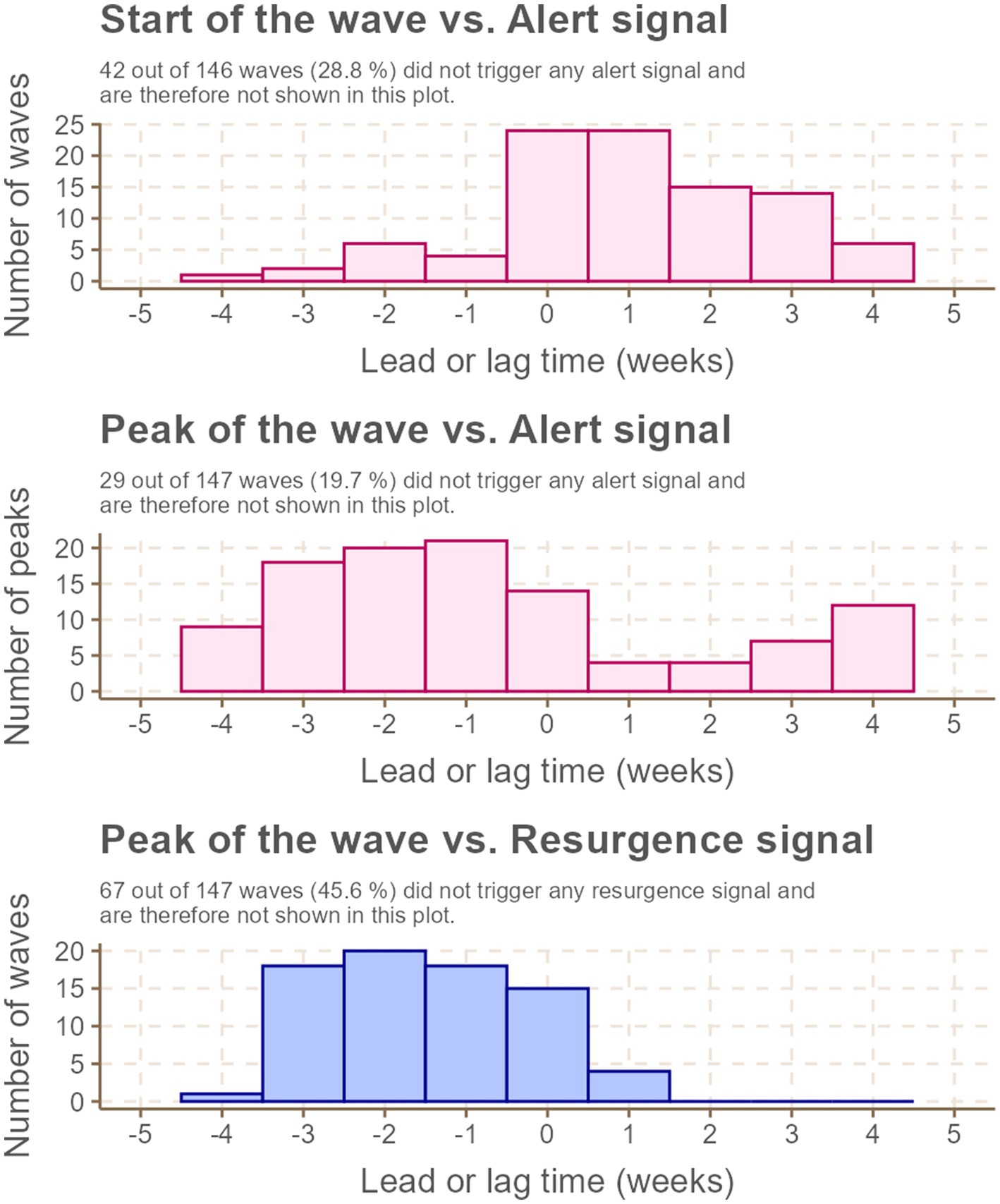
Figure 4. Lead (negative) and lag (positive) times (in weeks) for issuance of SOC Alert and Resurgence classifications compared to epidemic events (start or peak of national COVID-19 epidemic waves).
Among the 146 COVID-19 waves observed during the study period, over half were associated with a Resurgence classification issued within 5 weeks before or after the wave’s start, and more than 70% were linked to an Alert classification issued within the same time frame. Of these waves, 26.0% had an Alert classification issued either prior to or during their start week, with a median lead or lag time of 0 weeks (interquartile range [IQR]: 0–2 weeks of lag). Regarding wave peaks, 56.5% had an Alert classification issued either preceding or concurrent with the peak, with a median lead time of 2 weeks (IQR: 1–3 weeks). Similarly, 51.0% of peaks were preceded or simultaneously accompanied by a Resurgence classification, also with a median lead time of 2 weeks (IQR: 1–3 weeks).
Operational utility of the SOC classifications
Table 1 provides an overview of the operational utility of SOC Resurgence and Alert classifications in predicting and signaling national COVID-19 epidemic events. Overall, the SOC classifications demonstrated high specificity and low sensitivity for predicting epidemic events. Their performance was notably stronger in signaling epidemic events, as reflected by higher sensitivity and positive predictive value (PPV) metrics (Table 1).
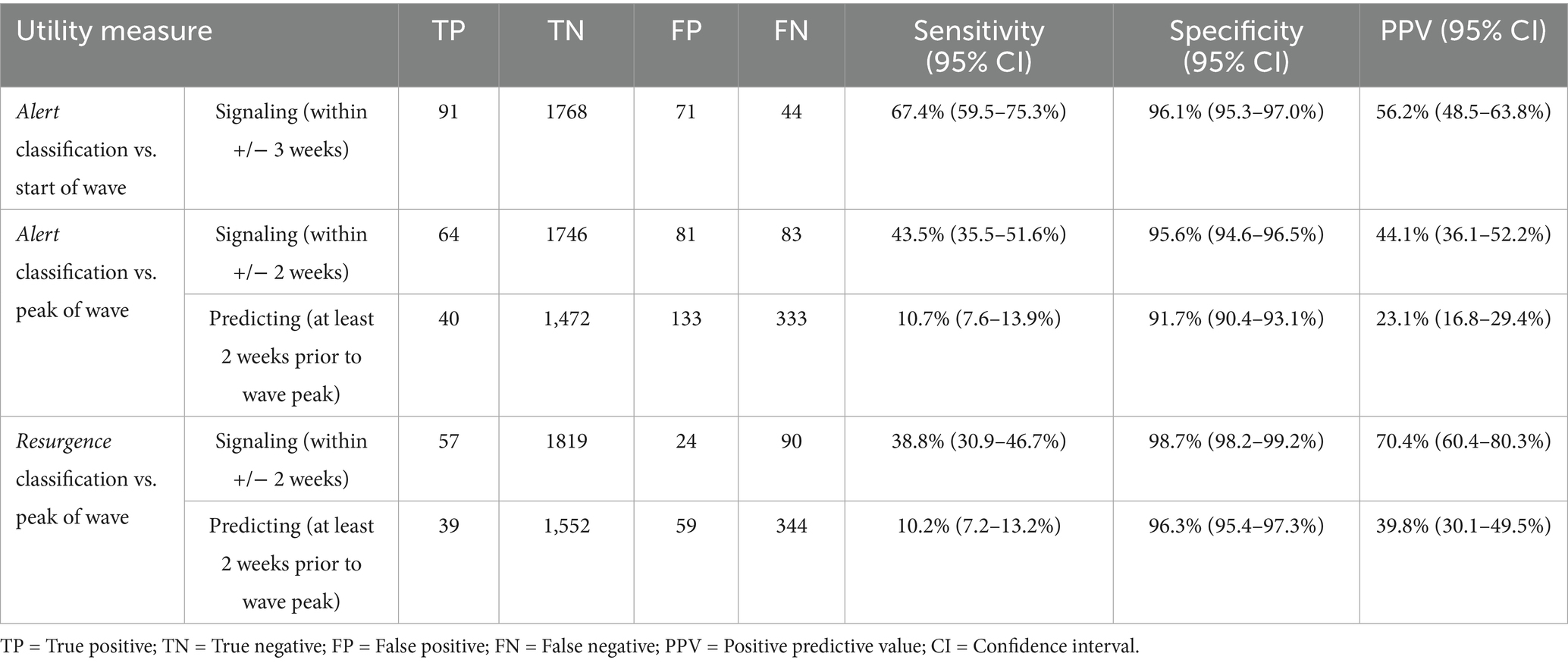
Table 1. Summary of operational utility of the SOC classifications in comparison to the COVID-19 epidemic events (start and peak of national waves).
More than 90% of the SOC classifications effectively signaled or predicted one of the two epidemic events (start or peak of a wave). Specifically, 67.4% of waves were signaled by epidemic concern classifications within 3 weeks of their start. However, the classifications exhibited comparatively lower effectiveness in signaling or predicting wave peaks (Table 1).
Time-stratified analysis
Figure 5 highlights changes in the operational utility of SOC indicators across three defined time strata.
The emergence of the Omicron variant during T2 significantly impacted the performance of the Resurgence classification, particularly in predicting and signaling wave peaks. During T2, the sensitivity of Resurgence classifications to predict wave peaks dropped to 0% (95% CI: 0–0%) with a PPV of 0% (95% CI: 0–0%), compared to T1, where sensitivity was 14.4% (95% CI: 10.3–18.6%) and PPV was 43.8% (95% CI: 33.5–54.1%). Similarly, the sensitivity of Resurgence classifications to signal wave peaks declined to 17.1% (95% CI: 5.6–28.6%) during T2, with a PPV of 100% (95% CI: 100–100%), compared to T1’s sensitivity of 54.5% (95% CI: 44.1–64.9%) and PPV of 66.7% (95% CI: 55.8–77.6%).
Despite the modifications to SOC classification criteria during T3, the sensitivity of the Resurgence classification did not improve. However, the two resurgence events that occurred during T3—in Zambia and Zimbabwe—were accurately captured using the revised SOC methodology.
In contrast, the operational utility of the Alert classification demonstrated resilience during the emergence of Omicron and showed notable improvement over time, particularly in signaling the start and peak of epidemic waves. During T2, the sensitivity of Alert classifications to signal the start of a wave increased to 70.7% (95% CI: 56.8–84.7%) with a PPV of 64.4% (95% CI: 50.5–78.4%), compared to T1’s sensitivity of 62.2% (95% CI: 51.1–73.2%) and PPV of 47% (95% CI: 37.5–57.4%). Similarly, the sensitivity of Alert classifications to signal wave peaks improved to 65.9% (95% CI: 51.3–80.4%) during T2, with a PPV of 67.5% (95% CI: 53.0–82.0%), compared to T1’s sensitivity of 28.4% (95% CI: 19.0–37.8%) and PPV of 27.5% (95% CI: 18.3–36.6%).
During T3, the Alert classification’s ability to signal epidemic events showed significant enhancement. The sensitivity to signal the start of waves within 3 weeks before or after increased to 80% (95% CI: 62.5–97.5%), with a PPV of 80% (95% CI: 62.5–97.5%). Additionally, the sensitivity to signal wave peaks within 3 weeks before or after rose to 67% (95% CI: 44.9–88.4%), with a PPV of 85.7% (95% CI: 67.4–100.0%). The sensitivity of Alert classifications to predict wave peaks within 3 weeks before or after also improved during T3, reaching 15.4% (95% CI: 1.5–29.3%), with a PPV of 23.5% (95% CI: 3.4–43.7%).
Discussion
This study aimed to assess the implementation, operational utility, strengths, and limitations of the COVID-19 Situations of Concern (SOC) classification system in the WHO African Region. Our findings provide clear evidence on the system’s overall performance in signaling epidemic waves and guiding resource allocation, while also highlighting challenges related to data quality and contextual variability. The impact of evolving epidemiological dynamics, notably the Omicron variant surge, and subsequent system adaptations were critically evaluated. The following sections elaborate on these key themes, beginning with an overview of the SOC system’s performance.
Overall performance of the SOC classification system
The SOC classification system was designed to inform decisions that support the adequate mobilization and distribution of resources to various Member States by the WHO Africa Regional Office during the acute phase of the COVID-19 pandemic. This approach aligns with evidence from the African Region showing that real-time situational analysis and early warning mechanisms were critical in shaping timely and effective COVID-19 responses (26). A retrospective review of the system’s predictive ability and operational utility revealed high specificity but low sensitivity in forecasting the start and peak of epidemic waves of COVID-19 in the African region. While both the Resurgence and Alert signals displayed specificity above 90%, the Alert signal exhibited the highest sensitivity in predicting the peak of the COVID-19 wave following the re-adjustment of SOC criteria and classifications after the emergence of the SARS CoV-2 Omicron variant.
Challenges and contextual factors
The low sensitivity primarily stemmed from the inherent limitations of the SOC indicator criteria, which relied on the assessment of epidemiological developments in preceding weeks, often complicated by delayed and incomplete reporting. While the definition of an “epidemic wave” can vary across settings and remains a subject of debate in the scientific literature (27), our use of the term was operationally defined to support the structured application and evaluation of the SOC classification system within the WHO African Region. Consequently, as illustrated in Figure 3, most signals (52.6%) were issued with a median lag of 1 week (IQR: 0–3 weeks). In some instances, delays in reporting from Member States to the regional office exacerbated the problem of extended lags. For example, notable missed events in Chad and Lesotho underscored the critical reliance of the methodology on prompt data reporting. Delays in reporting from these countries led to delayed signals issued after peak periods, highlighting the imperative for enhanced data transmission mechanisms and a more robust review process to mitigate such occurrences.
Additionally, systematic delays observed in countries like Cameroon underscored the importance of integrating contextual information with epidemiological data for a comprehensive assessment of the epidemic situation. Contextual factors such as health worker strikes, exemplified by those in Equatorial Guinea, could significantly influence the interpretation of data and the classification of signals. As highlighted in the outbreak analytics literature, the integration of contextual information with quantitative signals enhances situational awareness and supports more nuanced public health decision-making (28). In countries like Cameroon, contextual nuances such as regional conflicts or resource constraints were critical in maintaining or issuing alerts despite apparent epidemiological improvements. These factors emphasize the necessity for a flexible system that considers real-time operational contexts alongside raw epidemiological data.
Importantly, every week, the WHO AFRO IMST was informed of where data reporting was delayed, allowing the identification of countries needing support despite an absence of an epidemic concern classification. This proactive approach was crucial, as the global situation classification system developed by WHO headquarters often down-classified countries without consulting the regional office, overlooking nuanced local realities.
Impact of the omicron variant and system adaptations
As anticipated, the predictive performance of both Resurgence and Alert signals declined during the period (T2) heavily impacted by the Omicron variant. However, subsequent adjustments to the SOC classification criteria managed to restore and, in some cases, enhance its compromised performance. These adjustments underscore the significance of operational agility in fast-evolving health emergency response systems, necessitating adaptive strategies to uphold effectiveness amidst dynamic challenges.
One of the major adaptations was the addition of the “Alert (Reduced) Concern” classification. This category allowed limited resources to be redirected without giving a false signal of “low or no risk.” It also clarified the need to continue some reduced non-pharmaceutical interventions (NPIs) and vaccination campaigns.
However, one major drawback of the SOC indicators was their inability to capture nuanced variations in health systems capacity and the actual impact of epidemiological situations across countries, particularly during prolonged waves with high peaks such as those due to Omicron variants. While the criteria demonstrated reasonable effectiveness in categorizing countries based on their needs to receive support, the indicators had an inherent bias toward prioritizing countries with stronger health systems and better coordination in response activities that supported timely data reporting to the regional office. Conversely, in countries with relatively small populations, certain criteria proved insufficient in accurately reflecting changes in the epidemiological landscape over time.
A notable example is Seychelles, an island nation with an estimated population of less than 100,000 people. Throughout the study period, Seychelles consistently remained in the “Very High Incidence” category for most weeks, as its incidence rate exceeded 500 cases per 100,000 people. However, this classification was predominantly influenced by Seychelles’ proactive approach to detecting COVID-19 cases and its small population size, which posed challenges to achieving lower incidence rates. This misclassification created political tensions due to the negative economic and social impacts of what was actually a highly effective response to the epidemic. A similar, though less pronounced, issue was observed in Mauritius, but not in Sao Tome and Principe or Comoros, all of which are relatively small island countries. Differences in COVID-19 testing and case management capacity, sociodemographic characteristics influencing disease dynamics, vaccination rates, and the implementation of NPIs contributed to these variations (29).
A key limitation of this analysis is the lack of a retrospective sensitivity assessment examining the impact of changes in SOC classification criteria over time, particularly the fixed threshold of >500 cases per 100,000 population. Given that the epidemiological context and data availability evolved during the pandemic, it is possible that earlier or alternative thresholds may have yielded different performance outcomes. A formal comparison of historical data against alternative thresholds and indicator combinations could provide useful insights into the robustness and adaptability of the SOC approach. This type of retrospective modeling would help to inform optimal threshold setting in future applications of the system.
Another limitation of this analysis is the variability in country-level data completeness and timeliness, which likely influenced the performance of the SOC system. Countries with irregular reporting patterns—due to technical challenges, personnel turnover, or shifting priorities—were more prone to mismatches between alerts and on-the-ground epidemic trends. These mismatches typically manifested as delays in alert issuance or missed signals. In contrast, countries with consistent and timely data reporting yielded more reliable alert classification. While a formal exclusion-based sensitivity analysis was not feasible due to the dynamic and continuously updated nature of the database, we recognize that performance metrics are partially contingent on data quality. Similar challenges in timeliness and data completeness have been documented in other settings (30), highlighting the critical role of reliable reporting and the need to invest in robust data systems to ensure the effectiveness of real-time surveillance tools, particularly in resource-constrained settings.
Implications and recommendations for future surveillance
In summary, implementing SOC indicators during the COVID-19 pandemic has yielded several key insights. Firstly, to effectively support resource allocation within constraints, operational systems must comprehensively capture the myriad factors contributing to countries’ successful pandemic responses. This necessitates a holistic approach that goes beyond basic epidemiological data to include factors such as testing rates, health systems capacity, and data reporting capacity. Secondly, as the pandemic transitioned from emergency to routine surveillance, a sustainable, long-term strategy for assessing ongoing epidemic situations became critical. While the SOC indicators were effective in identifying countries requiring emergency support during the global crisis, adapting the methodology and criteria for unique local contexts is essential, particularly with the shift toward sub-national surveillance. This shift underscores the need for real-time epidemiological tools that are adaptable to evolving surveillance contexts, particularly at subnational levels (31). Continuous and timely updating of classification criteria to reflect changing epidemiological realities and pressures on surveillance and case management capacities is paramount.
Moreover, the SOC tool has demonstrated the pivotal importance of enhancing data quality, flow, and surveillance capacity across countries. For any regional assessment to adequately prioritize countries in need, collective motivation among countries to enhance surveillance practices is indispensable. Lastly, evaluation studies assessing the impact of such tools on public health outcomes, including morbidity and mortality, are crucial for advocating their continued utility. By demonstrating the tangible benefits of SOC classifications, policymakers and stakeholders can make informed decisions regarding their integration into ongoing pandemic response efforts and future public health strategies.
Conclusion
This retrospective analysis of the implementation of the SOC indicator-based operational decision-making system during the COVID-19 pandemic demonstrates its valuable role in supporting timely decision-making and resource allocation across the WHO African Region during the pandemic. Despite inherent challenges such as data delays and evolving epidemiological dynamics, it showed high specificity and reasonable operational utility, particularly after adapting to the Omicron variant context. By addressing its limitations and incorporating contextual adaptations, the system holds promise for enhancing epidemic intelligence and support data-driven responses in both national and sub-national settings, especially in resource-limited environments.
Author contributions
OO: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. JA: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. SK: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. MD: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. MM: Data curation, Methodology, Writing – original draft, Writing – review & editing. DaC: Investigation, Software, Validation, Writing – original draft, Writing – review & editing. LB: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. TB: Supervision, Writing – original draft, Writing – review & editing. BO: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. AF: Supervision, Writing – original draft, Writing – review & editing. JB-T: Methodology, Supervision, Writing – original draft, Writing – review & editing. GW: Data curation, Writing – original draft, Writing – review & editing. FMb: Methodology, Writing – original draft, Writing – review & editing. CO: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. FMu: Investigation, Writing – original draft, Writing – review & editing. KL: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. EE: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. TK: Investigation, Methodology, Writing – original draft, Writing – review & editing. RK: Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. PA: Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing. NG: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. BH: Formal analysis, Validation, Writing – original draft, Writing – review & editing. SW: Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. JO: Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. EK: Formal analysis, Supervision, Validation, Writing – original draft, Writing – review & editing. DiC: Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. FB: Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing. AG: Funding acquisition, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the WHO AFRO COVID-19 Incident Management Team. The WHO Regional Office for Africa also supported the reported activities. The funders had no role in study design, data collection and analysis, publication decisions, or manuscript preparation.
Acknowledgments
We would like to express our sincere gratitude to the stakeholders across the WHO African Region, including WHO Member States and WHO Country Offices, for their invaluable contributions to this study. Their insights played a crucial role in facilitating the retrospective analysis. We also wish to thank our colleagues at WHO AFRO for their constructive feedback and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer PR declared a shared affiliation with the author(s) DC to the handling editor at the time of review.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lytras, S, Xia, W, Hughes, J, Jiang, X, and Robertson, DL. The animal origin of SARS-CoV-2. Science. (2021) 373:968–70. doi: 10.1126/science.abh0117
2. World Health Organization. (2020). Statement on the second meeting of the international health regulations (2005) emergency committee regarding the outbreak of novel coronavirus (2019-nCoV). Available online at:https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
3. Cronin, CJ, and Evans, WN. Total shutdowns, targeted restrictions, or individual responsibility: how to promote social distancing in the COVID-19 era? J Health Econ. (2021) 79:102497. doi: 10.1016/j.jhealeco.2021.102497
4. Verschuur, J, Koks, EE, and Hall, JW. Global economic impacts of COVID-19 lockdown measures stand out in high-frequency shipping data. PLoS One. (2021) 16:e0248818. doi: 10.1371/journal.pone.0248818
5. Panchal, U, Salazar de Pablo, G, Franco, M, Moreno, C, Parellada, M, Arango, C, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. (2023) 32:1151–77. doi: 10.1007/s00787-021-01856-w
6. Bish, A, and Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. (2010) 15:797–824. doi: 10.1348/135910710X485826
7. Haider, N, Osman, AY, Gadzekpo, A, Akipede, GO, Asogun, D, Ansumana, R, et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob Health. (2020) 5:e003319. doi: 10.1136/bmjgh-2020-003319
8. Verani, A, Clodfelter, C, Menon, AN, Chevinsky, J, Victory, K, and Hakim, A. Social distancing policies in 22 African countries during the COVID-19 pandemic: a desk review. Pan Afr Med J. (2020) 37, 5–6. doi: 10.11604/pamj.supp.2020.37.1.27026
9. James, A, Dalal, J, Kousi, T, Vivacqua, D, Câmara, DCP, dos Reis, IC, et al. An in-depth statistical analysis of the COVID-19 pandemic’s initial spread in the WHO African region. BMJ Glob Health. (2022) 7:e007295. doi: 10.1136/bmjgh-2021-007295
10. Thakur, V, Bhola, S, Thakur, P, Patel, SKS, Kulshrestha, S, Ratho, RK, et al. Waves and variants of SARS-CoV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection. (2021) 50:309–25. doi: 10.1007/s15010-021-01734-2
11. McMenamin, M, Kolmer, J, Djordjevic, I, Campbell, F, Laurenson-Schafer, H, Abbate, JL, et al. WHO global situational alert system: a mixed methods multistage approach to identify country-level COVID-19 alerts. BMJ Glob Health. (2023) 8:e012241. doi: 10.1136/bmjgh-2023-012241
12. Iuliano, AD, Brunkard, JM, Boehmer, TK, Peterson, E, Adjei, S, Binder, AM, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020–January 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:146–52. doi: 10.15585/mmwr.mm7104e4
13. Príncipe, AS, and Filho, ASN. Decision support frameworks in public health emergencies: a systematic review of dynamic models in complex contexts. Int J Disaster Risk Reduct. (2023) 85:103579. doi: 10.3390/ijerph20176685
14. Moon, S, Sridhar, D, Pate, MA, Jha, AK, Clinton, C, Delaunay, S, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. Lancet. (2015) 386:2204–21. doi: 10.1016/S0140-6736(15)00946-0
15. World Health Organization. WHO African region: member states. (2021). Available online at: https://www.afro.who.int/countries
16. World Health Organization (2008) International health regulations (2005) (2nd ed.) Available online at:https://www.who.int/publications/i/item/9789241580496
17. World Health Organization (2022) WHO COVID-19 case definition Available online at:https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2022.1
18. World Health Organization. WHO COVID-19 dashboard (2019). Available online at: https://data.who.int/dashboards/covid19/cases?n=c
19. Pan American Health Organization. Norms and standards in epidemiology: guidelines for epidemiological surveillance. Epidemiol Bull. (1999) 20:11–3.
20. Chintalapudi, N, Battineni, G, and Amenta, F. Sentimental analysis of COVID-19 tweets using deep learning models. Infect Disease Rep. (2021) 13:329–39. doi: 10.3390/idr13020032
21. Rothman, KJ, and Greenland, S. Modern epidemiology. 2nd ed. Philadelphia, PA, USA: Lippincott-Raven Publishers. (1998).
22. McDonald, HI, Tessier, E, White, JM, Woodruff, M, Knowles, C, Bates, C, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. (2020) 25:2000848. doi: 10.2807/1560-7917.ES.2020.25.19.2000848
23. United Nations, Department of Economic and Social Affairs, Population Division (2019) World population prospects 2019: Highlights (ST/ESA/SER.A/423). Available online at:https://population.un.org/wpp/assets/Files/WPP2019_Highlights.pdf
24. R Core Team. R: A language and environment for statistical computing R Foundation for Statistical Computing. Vienna, Austria (2020).
25. Nkengasong, J, Ndembi, N, Tshangela, A, and Raji, T. COVID-19 vaccines: how to ensure Africa has access. Nature. (2020) 586:197–9. doi: 10.1038/d41586-020-02774-8
26. Taboada, M, González, M, Alvarez, A, Eiras, M, Costa, J, Álvarez, J, et al. First, second and third wave of COVID-19. What have we changed in the ICU management of these patients? J Infect. (2021) 82:e14–5. doi: 10.1016/j.jinf.2021.03.027
27. Polonsky, JA, Baidjoe, A, Kamvar, ZN, Cori, A, Durski, K, Edmunds, WJ, et al. Outbreak analytics: a developing data science for informing the response to emerging pathogens. Philos Trans R Soc Lond Ser B Biol Sci. (2019) 374:20180276. doi: 10.1098/rstb.2018.0276
28. Kousi, T, Vivacqua, D, Dalal, J, James, A, Câmara, DCP, Botero Mesa, S, et al. COVID-19 pandemic in Africa’s island nations during the first 9 months: a descriptive study of variation in patterns of infection, severe disease, and response measures. BMJ Glob Health. (2022) 7:e006821. doi: 10.1136/bmjgh-2021-006821
29. Reijn, E, Swaan, CM, Kretzschmar, MEE, and van Steenbergen, JE. Analysis of timeliness of infectious disease reporting in the Netherlands. BMC Public Health. (2011) 11:409. doi: 10.1186/1471-2458-11-409
30. Abat, C, Chaudet, H, Colson, P, Rolain, JM, Bassene, H, Diallo, A, et al. Real-time epidemiology: a better approach for the surveillance of emerging diseases. Front Public Health. (2016) 4:45. doi: 10.3389/fpubh.2016.00045
Keywords: COVID-19, epidemic, SAR-CoV-2, Situation of Concern, WHO African region
Citation: Ogundiran O, Abbate JL, Kim S, Diallo MSK, Muteba M, Camara DCP, Bianchi L, Balde T, Oyugi B, Fortin A, Baykika-Tusiime J, Williams GS, Mboussou F, Okot C, Mutoka Banza F, Laundry K, Ejiofor EN, Kanyowa TM, Kamara R, Atuhebwe P, Gumede N, Herring BL, Woldetsadik S, Okeibunor J, Koua E, Chamla D, Braka F and Gueye AS (2025) Assessing the utility of the COVID-19 epidemic Situations of Concern classification system in guiding operational responses to the pandemic in the WHO African region: retrospective analysis. Front. Public Health. 13:1562525. doi: 10.3389/fpubh.2025.1562525
Edited by:
Zisis Kozlakidis, International Agency for Research on Cancer (IARC), FranceReviewed by:
Marco Tagliabue, Oslo Metropolitan University, NorwayPablo Ivan Pereira Ramos, Gonçalo Moniz Institute (IGM), Brazil
Copyright © 2025 Ogundiran, Abbate, Kim, Diallo, Muteba, Camara, Bianchi, Balde, Oyugi, Fortin, Baykika-Tusiime, Williams, Mboussou, Okot, Mutoka Banza, Laundry, Ejiofor, Kanyowa, Kamara, Atuhebwe, Gumede, Herring, Woldetsadik, Okeibunor, Koua, Chamla, Braka and Gueye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph Okeibunor, b2tlaWJ1bm9yakB3aG8uaW50
 Opeayo Ogundiran
Opeayo Ogundiran Jessica L. Abbate
Jessica L. Abbate Sooyoung Kim
Sooyoung Kim Mamadou Saliou Kalifa Diallo1
Mamadou Saliou Kalifa Diallo1 Daniel Cardoso Portela Camara
Daniel Cardoso Portela Camara Thierno Balde
Thierno Balde Boniface Oyugi
Boniface Oyugi Ann Fortin
Ann Fortin Jayne Baykika-Tusiime
Jayne Baykika-Tusiime George Sie Williams
George Sie Williams Freddy Mutoka Banza
Freddy Mutoka Banza Kabego Laundry
Kabego Laundry Ephraim Nonso Ejiofor
Ephraim Nonso Ejiofor Trevor M. Kanyowa
Trevor M. Kanyowa Rashidatu Kamara
Rashidatu Kamara Nicksy Gumede
Nicksy Gumede Solomon Woldetsadik
Solomon Woldetsadik Joseph Okeibunor
Joseph Okeibunor Dick Chamla
Dick Chamla