- Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden
Introduction: Attitudes towards vaccination are influenced by a broad range of factors, yet little is known about the drivers shaping adolescents’ vaccination beliefs. The aim of this study was to qualitatively explore the factors influencing adolescents’ individual decision-making towards COVID-19 vaccination.
Methods: A systematic review was conducted using Medline, Web of Science, Sociological Abstracts, and Publicly Available Content Database. Studies on attitudes, beliefs, and perceptions of adolescents regarding COVID-19 vaccines were included. The JBI Critical Appraisal Checklist was used for quality assessment, followed by thematic synthesis of the included studies.
Results: In total, 13 studies were included, revealing 5 key themes: (1) Limited vaccine literacy influences adolescents’ attitudes towards COVID-19 vaccines; (2) Family, peers, and community strongly influence adolescents’ COVID-19 vaccine decision-making; (3) Different levels of trust in vaccine providers and governments influence adolescents’ attitudes towards COVID-19 vaccines; (4) Desire to go back to normality influences adolescents’ COVID-19 vaccine attitudes towards vaccine acceptancy; (5) Autonomy influences adolescents’ COVID-19 vaccine decision-making.
Discussion: The review findings suggest that vaccine acceptance among adolescents could be improved through tailored and accessible vaccine literacy messaging, addressing structural mistrust, and empowering adolescents to make autonomous health decisions that take into account diverse contexts and populations.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024512197, identifier CRD42024512197.
Background
Vaccination is a cornerstone of public health and among the most cost-effective public health interventions available today (1, 2). Vaccination is the act of introducing a vaccine to acquire protection by stimulating the body’s natural defences against germs and diseases (3–5). The importance of vaccination was demonstrated recently by the critical role vaccines played in mitigating the COVID-19 pandemic. During this time, the COVID-19 Vaccines Global Access (COVAX) initiative expedited vaccine development while upholding rigorous standards for safety, efficacy, and ethical integrity (6, 7). As a result, COVID-19 vaccines saved approximately 14.4 million lives worldwide in 2021, contributing to a 63% reduction in global COVID-19-related deaths in the first year of vaccination (8, 9). Despite these achievements, a recent systematic review from 2023 estimated a global COVID-19 vaccine hesitancy rate of 29.72%, largely driven by low confidence and high levels of complacency (10).
Vaccine hesitancy is not a new phenomenon (11). It has been recognized by the World Health Organisation (WHO) as one of the top 10 threats to global public health (12). The Strategic Advisory Group of Experts on Immunization (SAGE) defines vaccine hesitancy as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services” (13), encompassing a continuum of attitudes (13, 14). Vaccine hesitancy has been described as a complex phenomenon, varying by time, place, and vaccine. It is influenced by factors such as complacency, convenience, and confidence, known as the WHO’s ‘3Cs’ model (13). An important aspect of vaccine confidence is trust, which is based on relationships between individuals or between individuals and a system, where one party willingly assumes a position of vulnerability, relying on the competence and good intentions of the other in order to simplify decision-making (15).
Additionally, vaccine hesitancy must be understood within its social, historical, and political context. In each setting, public health policies, healthcare workers’ (HCWs) recommendations, and media communication intersect to influence attitudes, with the level of trust playing an important role in this dynamic (14). For COVID-19 vaccines, primary global drivers of hesitancy have included a low perceived risk of infection and severity, limited institutional trust, and concerns regarding vaccine safety (16, 17). However, in different population subgroups, there are specific determinants that affect hesitancy.
Adolescents are a particularly important, yet understudied, subgroup for vaccination efforts, with distinct characteristics that set them apart from other age groups (18). For the purpose of this research, we have defined adolescence as individuals from ages 10 to 19 in the phase between childhood and adulthood, based on the WHO definition (19–21). Adolescence is a transitional phase, especially for decisional rights (22). Within this age range, individuals gain both legal autonomy and capacity for informed consent, but the exact age of consent varies by country (19, 21). This leads to a new navigation of the balance between authority figures’ influence and individual autonomy in informed health-related decision-making (23). The process of decision-making involves evaluating outcome alternatives through analysing gathered information and further selecting a course of action (24, 25). Yet, even in instances with legal consent, adolescents’ decision-making regarding vaccination often involves parents and HCWs.
Parental and HCW hesitancy, rooted in concerns about vaccine safety and related misinformation, institutional mistrust, and perceived rights infringements, especially regarding COVID-19, can lead to lower vaccination rates among adolescents (23, 26–32). In addition, a quantitative review on adolescent vaccine hesitancy identified individual key barriers to vaccination, such as low awareness, perceived low efficacy, and safety concerns, while facilitators included knowledge, perceived efficacy, information access through family and school, and autonomy in decision-making (18).
Given the public health importance of vaccination and risks posed by new variants and outbreaks, this study aims to enhance understanding of the factors influencing adolescents’ attitudes towards COVID-19 vaccination by synthesising qualitative studies on the topic. By exploring the nuanced factors influencing their perceptions, our findings can provide valuable insights to help develop tools to adequately measure and monitor adolescent vaccine confidence and identify strategies to address adolescents’ vaccine hesitancy.
Methods
The systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols 2015 (PRISMA-P 2015) guidelines (33). The guiding research question is ‘What are the factors, as described by adolescents, that influence their individual decision-making about COVID-19 vaccination?’. The PEO (Population, Exposure, and Outcome) tool was used in order to focus on the systematic analysis of qualitative research, in which associations between exposure and health outcomes are explored and can further guide health policies (34, 35). Then the research question was developed based on (P) Adolescents aged 10–17 years-old; (E) Factors such as adolescents’ knowledge, perceptions, and views about vaccination and COVID-19 vaccines; (O) Attitudes towards COVID-19 vaccines and vaccination decision-making (36).
The systematic review study protocol is registered in PROSPERO with the identification number CRD42024512197 (37). The original research question submitted in the PROSPERO protocol was: ‘What is the available evidence on adolescents’ perspectives, views, and attitudes about vaccines and vaccination in relation to this population’s COVID-19 vaccine hesitancy status?’ However, during the review, it was revised to better focus on the specific factors and attitudes influencing adolescents’ decisions, ensuring a more targeted and relevant analysis. To ensure comprehensive reporting, the authors followed both the PRISMA-P framework for review reporting (33) and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) checklists (38).
Data sources and searches
The last search was performed on 23 February 2024 in the following databases: Medline, Web of Science, Sociological Abstracts and Publicly Available Content Database (in collaboration with librarians at the Karolinska Institutet University Library). The search strategy was first developed in Medline (Ovid). For each search concept, Medical Subject Headings and free text terms were identified in Medline. The search was then translated, in part using Polyglot Search Translator (39), to efficiently translate search strategies across multiple databases, converting search strategies from Ovid MEDLINE into formats compatible with databases such as Cochrane Library, Embase (via Elsevier and Ovid), Web of Science, and others. Key terms for the search included vaccine, immunization, attitude, belief, trust, adolescent, young adult, and youth. No language restriction was applied, and articles older than 2020 were not reviewed. This decision was taken considering that COVID-19 emerged on the global scene in late December 2019. Thus, a comprehensive understanding of disease characteristics, burden, knowledge, and vaccine availability was not available prior to 2020.
De-duplication was done using the method described by Bramer et al. (40). One final, extra step was added to compare DOIs. A manual snowball search was applied to check references and citations of eligible studies from the database searches. The full search strategies for all databases are available in Appendix 1.
Study selection
NMC and EG independently screened the articles by reviewing titles and abstracts, followed by full-text assessments, based on the established inclusion and exclusion criteria. The inclusion criteria were: (1) qualitative or mixed-methods studies; (2) studies in English, Portuguese or Swedish; (3) study participants—adolescents aged 10 to 17 years old (studies that presented data from younger or older individuals were also included as long as the data extracted could be identified as from a person within 10 to 17 years old and/or the majority of subjects were within 10–19); (4) studies focusing on vaccine hesitancy, acceptance, and/or refusal of adolescents regarding COVID-19 vaccines and vaccination; and (5) studies focusing on knowledge, beliefs, views, perceptions and attitudes of adolescents regarding COVID-19 vaccines and vaccination. The exclusion criteria were: (1) studies focusing on parents and/or guardians’ knowledge, beliefs, views, perceptions, and attitudes regarding vaccination for their children; (2) studies focusing on adolescents’ knowledge, attitudes, and perceptions about general vaccination or other non-COVID-19 vaccines; and (3) studies focusing on HCWs’ knowledge, attitudes, and perceptions about COVID-19 vaccine hesitancy in adolescents. The process of revision and selection of articles was performed with the assistance of the Rayyan.ai tool (41). Conflicts were resolved among the team.
Data extraction
Data were extracted by NMC according to a predetermined excel data extraction table, including title, authors, year of publication, aim/objective, country, data collection period, study design, data collection method, sample size/participants characteristics, full results section (themes identified, codes identified, and quotes used). The extracted data were then reviewed by EG.
Quality assessment
Assessment of risk of bias on the included articles was performed by NMC and EG utilizing the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Qualitative Research (42). This tool was used to evaluate qualitative studies in a well-structured manner, allowing for a systematic and transparent assessment.
Data synthesis
A qualitative synthesis strategy was used to systematically evaluate and synthesize the results of the included qualitative or mixed-method studies (43). The process of qualitative synthesis included an analysis using summarization, descriptive statistics, and thematic synthesis of the selected articles. Prior to synthesis, a standardized data extraction sheet was developed that included: title, authors, year of publication, aim/objective, country, data collection period, study design, data collection method, sample size/participants characteristics, results—themes identified, codes identified, quotes used.
The extracted qualitative results were interpreted and integrated to identify recurring patterns and generate themes. An inductive thematic synthesis was performed by NMC in accordance with Thomas and Harden’s qualitative synthesis strategy, which is a strategy that was developed to address research questions related to the acceptability of interventions (43, 44). The analysis strategy evaluates barriers and facilitators of interventions; thus, it was used here to understand adolescents’ perceptions of vaccination. This synthesis helped us draw broader conclusions and gain a deeper understanding of adolescents’ experiences and expressed needs. An initial inductive line-by-line coding of the primary study findings was conducted, followed by organizing these codes into descriptive themes, which led to the development of analytical themes. To assist in the coding process, Atlas.ti software and Excel were utilized (45). In the final stages of coding, regular discussions of the themes among NMC, EG and SHvW were performed.
Ethical considerations
This study is an evaluation of published, publicly accessible studies and hence, no formal ethical approval was required according to the Swedish Ethics regulations.
Results
A total of 6,575 records were initially identified and out of the 4,051 records screened after deduplication, 13 studies (46–58) were eligible for inclusion. The study selection process is illustrated in the PRISMA 2020 flowchart in Figure 1.
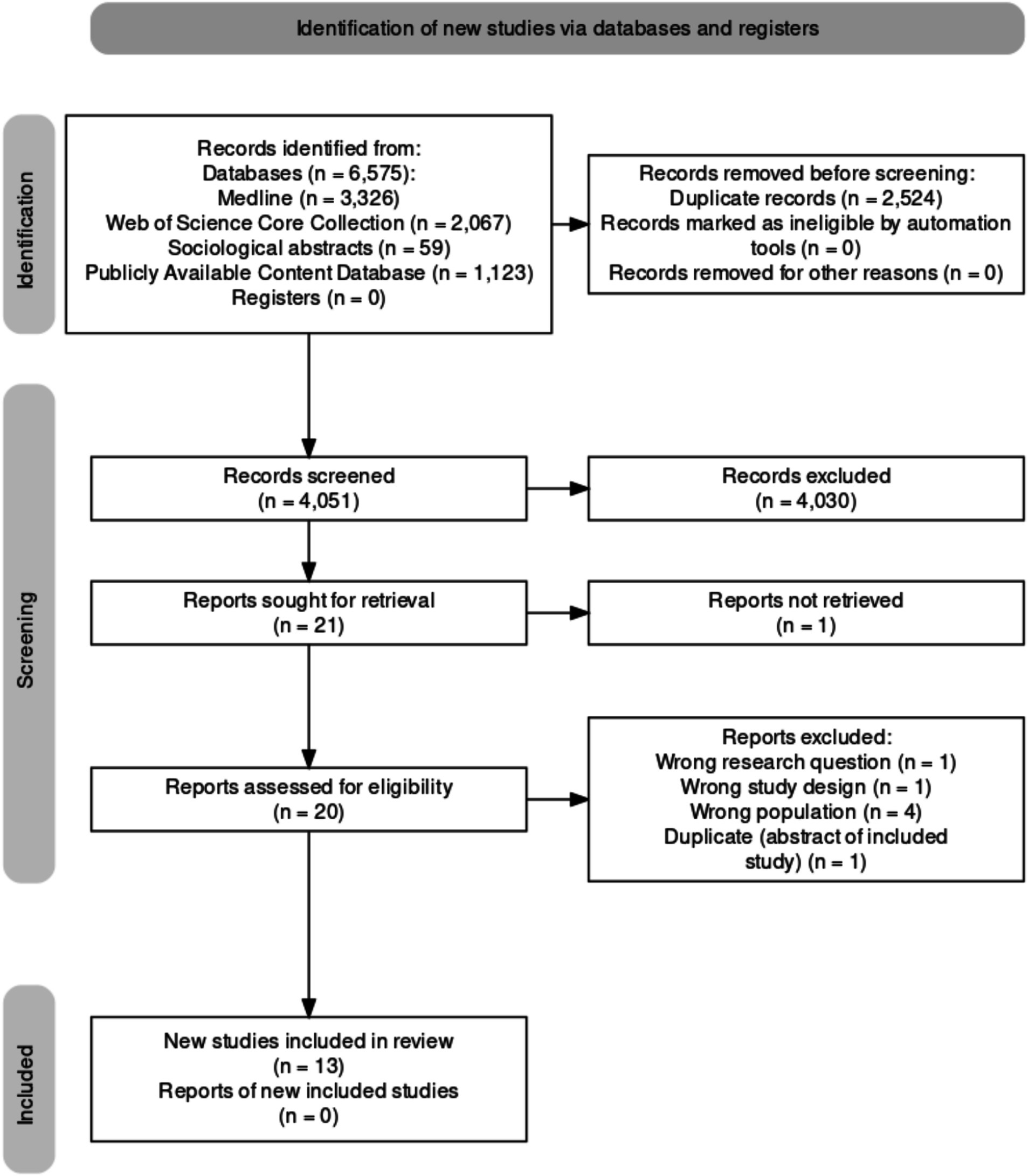
Figure 1. PRISMA 2020 flowchart of study selection process (71).
Characteristics of the included studies
Nine of the thirteen studies utilized interviews as their primary data collection method (47–49, 51–53, 55–57), two conducted focus groups (50, 54), and two used open-ended responses for qualitative analysis (46, 58). The studies represented a range of countries: six from the United States (US) (51, 54, 56–58), two from Canada (48, 49), and one each from South Africa (55), Ethiopia (53), Uganda (47), England (52), Sweden (46), Brazil (50), China (50), the Democratic Republic of Congo (50), Indonesia (50), Belgium (50), and Malawi (50). Additionally, seven studies focused on adolescent populations from vulnerable backgrounds (47–49, 51, 54, 57, 58), such as those experiencing homelessness, refugee status, or belonging to historically marginalized communities. The articles are all summarized in Table 1.
Findings from thematic synthesis
After data extraction and thematic synthesis, five overarching themes were generated: (1) Limited vaccine literacy influences adolescents’ attitudes towards COVID-19 vaccines; (2) Family, peers, and community strongly influence adolescents’ COVID-19 vaccine decision-making; (3) Different levels of trust in vaccine providers and governments influence adolescents’ attitudes towards COVID-19 vaccines; (4) Desire to go back to normality influences adolescents’ COVID-19 vaccine attitudes towards vaccine acceptancy; (5) Autonomy influences adolescents’ COVID-19 vaccine decision-making. These themes and their related categories are summarized in Appendix 3, with exemplifying quotes.
Theme 1: Limited vaccine literacy influences adolescents’ attitudes towards COVID-19 vaccines
This theme explores how adolescents’ vaccine literacy further influences their COVID-19 vaccine decisions. Some contradictions regarding vaccination attitudes were present in the studies, however, most studies associated low vaccine literacy with hesitancy or refusal, which was largely represented by low vaccine confidence (55). Low confidence was expressed by many adolescents through concerns about vaccine safety, citing fears of pain from vaccination, needles, unknown long-term side effects, and potential health impacts. Misinformation, mostly through social media platforms, further influences vaccine mistrust through peer criticism or conspiracy beliefs. Rapid vaccine development fuelled these doubts, as reflected in statements like: “Madam, I do not think it is really reliable because they found the vaccine already in one year … there is also a discussion that there may be other substances in the vaccine so that the world population cannot increase or that women cannot get pregnant– Female Belgian adolescent” (50). Associated with misinformation, some adolescents from marginalized communities acknowledged that standard public health messaging did not reflect their concerns or realities. Thus, they expressed a need for more relatable, tailored public health messages that resonated with their unique experiences and backgrounds.
Conversely, low vaccine literacy sometimes maintained high confidence, inspired by optimism about vaccine benefits (55, 56), e.g., “[…] I think it will help and cure a lot of people who had COVID-19, and people will be happy to have the vaccine” (55).
Theme 2: Family, peers, and community strongly influence adolescents’ COVID-19 vaccine decision-making
The role of family, peers, and community surfaced as a powerful influence on adolescents’ decision-making. Depending on the degree of trust and proximity, many adolescents tended to adopt the attitudes of trusted family members, which seemed to be particularly strong if these members were vaccine-acceptant HCWs, as exemplified in the quote below: “Me seeing…my grandmother [changed my mind about the vaccine], she works at a nursing home. She was around numerous patients who had COVID. She was in contact with them and everything, but by her havin’ two of the vaccine shots, she had not caught COVID yet – 15-year-old female living in rural Alabama” (51). In this case, acceptability was driven by trust in the family member and health outcome after vaccination. Similarly, community norms also significantly influenced attitudes: in China, collective community endorsement of vaccination motivated acceptance, while in other areas, such as parts of Malawi and the DRC, the absence of visible vaccination role models fuelled hesitancy, as reflected in the following statement: “If I’m told to take the vaccine, I will not take it because… I have not seen anyone get vaccinated, and I would not like to be the first one to be vaccinated” (50).
Theme 3: Different levels of trust in vaccine providers and governments influence adolescents’ attitudes towards COVID-19 vaccines
Adolescents’ confidence in COVID-19 vaccines is strongly shaped by the degree of trust in government and health institutions. Mistrust, particularly among marginalized groups, drives hesitancy, as explained from a rural Black youth in the US, “…[my friends] just do not trust the government or the systems, and the fact that they think that [the vaccine is] gonna be chipped” (51). 2SLGBTQ + (Two-Spirit, lesbian, gay, bisexual, transgender, queer (or questioning)) youth also voiced mistrust, often rooted in negative healthcare experiences (49). However, some indicated that trusted HCWs – particularly those with positive connections to the adolescents—could improve vaccine acceptance, as one adolescent explained, “Trust the advice of medical professionals because they know more than you do” (56).
Theme 4: Desire to go back to normality influences adolescents’ COVID-19 vaccine attitudes towards vaccine acceptance
Adolescents expressed a strong wish to regain a sense of “pre-pandemic normalcy,” motivated by both personal desires and altruistic concerns. Individual reasons for getting vaccinated were often cited, such as “I want to do a sport and it takes your two doses…for sure I’m going to do it because it’s my sport and well I love it” (48). Social mandates and vaccine passports further incentivised adolescents to get vaccinated, seeing it as a way to engage in social activities (48). These motivations were often linked more to individualist needs than community protection.
At the same time, however, many did see vaccination as a way to protect and bring stability to their families and communities. For example, one adolescent remarked, “When you are in a position when it [COVID-19] does not affect you, it would be selfish not to think of other people who you might pass it on to who it would affect” (52). Many also expressed empathetic attitudes in relation to older adult’s wellbeing, as in “I think a vaccine against COVID-19 is good because it protects us from getting sick, which leads to society being able to open up and older people do not need to live as isolated as they are now, barely able to go out and with lots of restrictions they have to follow so they do not risk getting sick” (46). Additional motivations were related to family welfare and opportunities to return to school (57).
Theme 5: Autonomy influences adolescents’ COVID-19 vaccine decision-making
Across the literature, adolescents consistently expressed a desire for autonomy in making their own vaccination decisions, both in relation to public health policies and parental authority. In Balma’s research, homeless adolescents experienced their autonomy as limited by institutional policies in health and housing settings (54). Similarly, adolescents from an ethnically diverse underserved community in Canada reported: “It’s like really shitty, sorry, but it’s really shitty because I think it’s really unfair, because it’s your body, your choice, and if you do not want to get the vaccine, that’s your choice, and I do not understand why you should lose your everyday privileges just because you did not get one dose or two” (48). Furthermore, adolescents experienced varying autonomy levels regarding parental influence. In the case of HCW parents, a physician’s child felt compelled to state, “My dad was probably gonna make me do it… I’d agreed with him,” while a nurse’s child felt fully autonomous, saying, “I would probably put it at 100% my own decision” (56). In some instances, adolescents even challenged their family members’ opinions, as in the following example in a Brazilian context: “Then she [grandmother] thinks she is not going to get the vaccine, and I say ‘where is your sister to take care of you?’ Because her sister keeps putting in her head that this vaccine is from the devil, that it’s this, that it’s that. Then I said, ‘well, now you call your sister to take care of you, because you do not listen to us” (50). This illustrates the adolescents’ ability to self-govern and act according to their own values.
Quality assessment
The quality of each included study was assessed using the JBI Critical Appraisal Checklist for Qualitative Research, as summarized in Appendix 2. Among the thirteen studies, nine were rated as medium methodological quality (46, 47, 49–52, 54, 56, 58), three as high quality (48, 55, 57) and one as low quality (53). However, none were excluded due to quality. Notably, eleven studies (46, 47, 49–54, 56–58) did not position the researcher culturally or theoretically, nor did they acknowledge the reciprocal influence between the researcher and the research. Additionally, Balma et al. cited that they did not require IRB ethical approval, but did obtain consent when conducting the interviews (54).
Discussion
This study systematically reviewed qualitative research to explore factors influencing COVID-19 vaccine decision-making and hesitancy among adolescents. Thirteen articles were analysed, revealing five key themes about the role of vaccine literacy, the influence of personal relationships, the impact of levels of trust, the desire to return to normalcy, and the adolescents’ feelings of autonomy on vaccine decision making.
First, our study illustrated the complex relationship between vaccine literacy and vaccine decision-making. One finding that there is a direct relationship between low literacy and low confidence aligns with existing literature and often arises from a lack of understanding, insufficient information, or spread of misinformation (59, 60). However, we also found that the inverse could be true. A study suggested that vaccine-literate people can also refuse vaccines due to not knowing how to interpret received messages from an overload of information (61). Similarly, so-called “vaccine enquirers” refers to individuals with high vaccine literacy, who after receiving informed research make deliberate vaccination choices within the continuum of vaccination attitudes. This distinction emphasizes their confidence and agency in decision-making, suggesting that public health narratives could shift to avoid vaccine-related stigma by recognizing this empowered approach (62). However, we also observed an inverse relationship between low vaccine literacy and high confidence, which might be attributable more to external influences than low knowledge itself. Thus, the relationship between vaccine literacy and adolescent vaccine decision-making is not always straightforward.
To address barriers relating to vaccine literacy and misinformation, the adolescents voiced a need for tailored vaccine messaging. The typical information received was often not well understood or not clearly provided (13, 63). Particularly among adolescents in vulnerable situations, there was a sense that existing vaccine messages did not align with their experiences or livelihood. This suggests that improving vaccine messaging clarity and accessibility could enhance vaccine literacy and foster informed decision-making. Additionally, it is crucial to ensure that credible, trusted sources are accessible to adolescents to counter false narratives effectively.
Notably, in our study, the low levels of vaccine confidence in vulnerable groups extend beyond information and seemed to be deeply rooted in government or health systems mistrust. This mistrust often stemmed from a history of marginalization and experience of mistreatment by health systems and governments. This finding was also present in systematic reviews of vaccine hesitancy among vulnerable groups (64), the general population (16, 17, 65) and during pandemics (66). Addressing these deep-seated structural inequalities and general mistrust could help replace hesitant attitudes with greater confidence. One potential solution is to harness the existing trust in healthcare workers who are considered trustworthy providers of both vaccines and information. Other common and trusted sources of information include the community and family, who could also be avenues for improving adolescent vaccine confidence.
Confidence also includes trust in the effectiveness and safety of the vaccines themselves. Fears around safety and long-term effects of COVID-19 vaccines were highlighted by adolescents in this study. This anxiety about long-term consequences might reflect broader vaccine hesitancy trends, particularly in relation to newer vaccines, as low confidence is not prevalent in all vaccine types (67). These concerns are often driven by factors such as misinformation and a lack of institutional trust. Additionally, fear surrounding more immediate concerns of vaccination, such as the perceived pain associated with the injection and fear of needles, were also consistently reported in other studies (18, 67). This highlights the need for strategies that not only build trust in vaccine safety but also take into consideration procedural fears, especially among younger populations.
This review, similar to prior evidence, also identified complacency in vaccination relating to low perceived risk for severe illness among adolescents (66, 67). It should be noted though, that in other diseases, such as hepatitis B, low perceived risk seemed to reflect the adolescent’s lack of understanding of disease transmission (67). This low perceived risk may stem from misinformation and a lack of trust in public health authorities among disadvantaged groups, while in more advantaged groups, it may reflect a sense of superiority toward public health agencies (68). Contrary to the cited complacency, other studies in the review showed that a vaccination driver is an altruistic desire to protect others, such as their family or the community. In addition to that, the desire to go back to a sense of pre-pandemic normalcy, influenced by both individualistic and collective motives, was another motivation for vaccination. This desire was found to be common among the general population during other pandemic studies (66, 69). Therefore, both individual risk perceptions and collective motivations may be key to addressing vaccine-hesitant attitudes.
Finally, at an individual level, adolescents showcased a desire to make autonomous health-related choices, echoing findings of previous general vaccine studies (18, 67). However, their autonomy was often limited by local legislation and parental authority, which frequently overruled adolescents’ choices, particularly in certain contexts. An additional barrier might also be HCWs’ hesitancy to vaccinate adolescents without parental approval, even in situations where legislation allowed for self-consent (67). As a result, factors such as legislation, parental authority, HCWs’ practices, and broader contextual influences all played a significant role in shaping adolescents’ autonomy in vaccine decision-making.
It is essential to recognize that all these factors must be considered within the context of different settings and the diverse socioeconomic backgrounds of adolescents. Context plays a critical role in shaping perceptions, as it is closely linked to specific policies and mandates, levels of institutional trust, and the degree of autonomy individuals have in making health decisions. Socioeconomic factors such as education and income can significantly impact access to vaccination services and information, while cultural beliefs further shape attitudes toward vaccination (18). Additionally, individual perception of health status, particularly in the presence of pre-existing conditions, influences vaccine perceptions, often affecting the perceived risks and benefits of immunization (70). Given the complexity of these factors, future research should explore adolescent attitudes toward vaccination across various sociocultural and economic contexts. Comparative studies across different regions and policy environments could provide valuable insights into how institutional trust, autonomy, and socioeconomic disparities shape vaccine decision-making.
Institutional trust emerged as a key factor influencing nearly all dimensions of vaccination decision-making among adolescents. Therefore, policymakers should not only ensure that vaccine-related information is accessible and relevant to adolescents but also foster open and transparent dialogue to build trust in government institutions and healthcare professionals (50). Empowering adolescents to make informed decisions about their health, will not only enhance trust but also contribute to a more resilient and health-conscious generation.
Limitations
This study had several limitations that should be considered. Firstly, the included studies had varying aims, research questions, data collection instruments, and interview guides, introducing heterogeneity in the findings. While this diversity may make it challenging to draw entirely consistent conclusions, it also provides a more comprehensive understanding of the topic by capturing different perspectives and offering a richer, more nuanced picture of vaccine uptake. Moreover, weaker or moderate-quality studies were included, potentially skewing results and compromising reliability. However, given our objective to capture all relevant insights, we chose to include these studies while acknowledging their quality. This approach ensured that we did not overlook valuable perspectives that could contribute to a broader understanding of adolescent vaccine hesitancy. Another key limitation was the variability in contextual factors, as vaccine availability varied across different countries and the timing of the studies. More favourable findings regarding vaccine uptake may have been observed in regions where vaccines were readily available, alongside visible reductions in COVID-19-related deaths. Additionally, local laws, cultural norms, and societal contexts differ between countries, limiting the generalizability of our results across settings. Nonetheless, our aim was to provide a broad synthesis of the evidence, and by including studies from diverse contexts, we ensured that the review captured a wide range of experiences and decision-making processes, making the findings more globally relevant.
Conclusion
This systematic review highlights the complex and interconnected factors influencing COVID-19 vaccine decision-making among adolescents. The findings demonstrate that adolescents’ vaccine confidence is multifaceted, shaped not only by their own understanding of vaccines but also by the attitudes of trusted social networks and institutions. Misinformation and mistrust, particularly among vulnerable groups, continue to be significant barriers to vaccine acceptance. In contrast, trusted HCWs and family and community members, along with the longing for a return to normal life, were crucial in promoting positive vaccination attitudes. In addition, autonomy was found to be important for adolescents. Therefore, these findings suggest that enhancing vaccine literacy through tailored, accessible messaging, addressing structural mistrust, and empowering adolescents to make autonomous health decisions are critical for improving vaccine acceptance. Future public health strategies should consider these nuanced influences in diverse contexts to effectively engage adolescents.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. ST: Writing – original draft, Writing – review & editing. EG: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. SH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by FORTE, the Swedish Research Council for Health, Working Life, and Welfare with grant number [2021-01299]. Open access funding is provided by Karolinska Institutet.
Acknowledgments
We would like to thank the Karolinska Institute librarian, Narcisa Hannerz, for her invaluable contribution during the search process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1563677/full#supplementary-material
References
1. European Commission. Vaccination overview. Available online at: https://health.ec.europa.eu/vaccination/overview_en (Accessed December 10, 2024).
2. World Health Organization. Vaccines and immunization; (2023). Available online at: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (Accessed March 4, 2024).
3. Center for disease control. Vaccines & immunizations. Explaining how vaccines work; (2024). Available online at: https://www.cdc.gov/vaccines/basics/explaining-how-vaccines-work.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fvaccines%2Fhcp%2Fconversations%2Funderstanding-vacc-work.html (Accessed March 24, 2025).
4. World Health Organization. Vaccines and immunization: what is vaccination? (2024). Available online at: https://www.who.int/news-room/questions-and-answers/item/vaccines-and-immunization-what-is-vaccination (Accessed March 4, 2024).
5. Center for Disease Control. Vaccines & immunizations. Vaccine basics; (2024). Available online at: https://www.cdc.gov/vaccines/basics/index.html (Accessed March 4, 2024).
6. WHO. COVAX. Available online at: https://www.who.int/initiatives/act-accelerator/covax (Accessed March 5, 2024).
7. John Hopkins Coronavirus Resource Center. Vaccine Research & Development. Available online at: https://coronavirus.jhu.edu/vaccines/timeline (Accessed March 5, 2024).
8. WHO. Vaccines and immunization: vaccine safety; (2023). Available online at: https://www.who.int/news-room/questions-and-answers/item/vaccines-and-immunization-vaccine-safety (Accessed October 21, 2024)
9. Mellis, C. Lives saved by COVID-19 vaccines. J Paediatr Child Health. (2022) 58:2129. doi: 10.1111/jpc.16213
10. Pourrazavi, S, Fathifar, Z, Sharma, M, and Allahverdipour, H. COVID-19 vaccine hesitancy: a systematic review of cognitive determinants. Health Promot Perspect. (2023) 13:21–35. doi: 10.34172/hpp.2023.03
11. Barrett, JS, Yang, SY, Muralidharan, K, Javes, V, Oladuja, K, Castelli, MS, et al. Considerations for addressing anti-vaccination campaigns: how did we get here and what can we do about it? Clin Transl Sci. (2022) 15:1380–6. doi: 10.1111/cts.13273
12. WHO. Ten threats to global health in 2019. Available online at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (Accessed October 21, 2024)
13. MacDonald, NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
14. Dubé, E, Laberge, C, Guay, M, Bramadat, P, Roy, R, and Bettinger, JA. Vaccine hesitancy. Hum Vaccin Immunother. (2013) 9:1763–73. doi: 10.4161/hv.24657
15. Larson, HJ, Clarke, RM, Jarrett, C, Eckersberger, E, Levine, Z, Schulz, WS, et al. Measuring trust in vaccination: a systematic review. Hum Vaccin Immunother. (2018) 14:1599–609. doi: 10.1080/21645515.2018.1459252
16. Romate, J, Rajkumar, E, Gopi, A, Abraham, J, Rages, J, Lakshmi, R, et al. What contributes to COVID-19 vaccine hesitancy? A systematic review of the psychological factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel). (2022) 10:1–21. doi: 10.3390/vaccines10111777
17. Pires, C. Global predictors of COVID-19 vaccine hesitancy: a systematic review. Vaccines (Basel). (2022) 10:1–39. doi: 10.3390/vaccines10081349
18. Cadeddu, C, Castagna, C, Sapienza, M, Lanza, T, Messina, R, Chiavarini, M, et al. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: a systematic review. Hum Vaccin Immunother. (2021) 17:4470–86. doi: 10.1080/21645515.2021.1961466
19. European Union Agency for Fundamental Rights. Consenting to medical treatment without parental consent; (2017) Available online at: https://fra.europa.eu/en/publication/2017/mapping-minimum-age-requirements-concerning-rights-child-eu/consenting-medical-treatment-without-parental-consent (Accessed March 24, 2025)
20. World Health Organization. Adolesc Health; (2025). Available online at: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (Accessed March 24, 2025).
22. WHO. Adolescent health. Available online at: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (Accessed March 24, 2025).
23. McGrew, S, and Taylor, HA. Adolescents, parents, and Covid-19 vaccination — who should decide? N Engl J Med. (2022) 386:e2. doi: 10.1056/NEJMp2116771
24. UMass Dartmouth. Decision-making process. Available online at: https://www.umassd.edu/fycm/decision-making/process/ (Accessed March 24, 2025).
25. Attwood, DA, Deeb, JM, and Danz-Reece, ME. Personal factors In: Ergonomic Solutions for the Process Industries. Elsevier: Gulf Professional Publishing. (2004). 29–63.
26. Peterson, CJ, Lee, B, and Nugent, K. COVID-19 vaccination hesitancy among healthcare workers—a review. Vaccines (Basel). (2022) 10:1–30. doi: 10.3390/vaccines10060948
27. English, A, and Middleman, AB. Adolescents, young adults, and vaccine hesitancy: who and what drives the decision to vaccinate? Pediatr Clin N Am. (2023) 70:283–95. doi: 10.1016/j.pcl.2022.11.006
28. White, J, Grabowski, M, Rositch, A, Gravitt, P, Quinn, T, Tobian, A, et al. Trends in adolescent human papillomavirus vaccination and parental hesitancy in the United States. J Infect Dis. (2023) 228:615–26. doi: 10.1093/infdis/jiad055
29. Obohwemu, K, Christie-de Jong, F, and Ling, J. Parental childhood vaccine hesitancy and predicting uptake of vaccinations: a systematic review. Prim Health Care Res Dev. (2022) 23:1–14. doi: 10.1017/S1463423622000512
30. Olick, R, Yang, Y, and Shaw, J. Adolescent consent to COVID-19 vaccination: the need for law reform. Public Health Rep. (2021) 137:163–7. doi: 10.1177/00333549211048784
31. Lin, C, Mullen, J, Smith, D, Kotarba, M, Kaplan, S, and Tu, P. Healthcare providers’ vaccine perceptions, hesitancy, and recommendation to patients: a systematic review. Vaccines (Basel). (2021) 9:713. doi: 10.3390/vaccines9070713
32. Cella, P, Voglino, G, Barberis, I, Alagna, E, Alessandroni, C, Cuda, A, et al. Resources for assessing parents’ vaccine hesitancy: a systematic review of the literature. J Prev Med Hyg. (2020) 61:E340–73. doi: 10.15167/2421-4248/jpmh2020.61.3.1448
33. Moher, D, Shamseer, L, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
34. Elsevier. Elsevier Blog. Clinical questions: PICO and PEO research. Available online at: https://scientific-publishing.webshop.elsevier.com/research-process/clinical-questions-pico-and-peo-research/ (Accessed March 24, 2025).
35. Hosseini, MS, Jahanshahlou, F, Akbarzadeh, MA, Zarei, M, and Vaez-Gharamaleki, Y. Formulating research questions for evidence-based studies. J Med Surg Public Health. (2024) 2:100046. doi: 10.1016/j.glmedi.2023.100046
36. Moola, S, Munn, Z, Sears, K, Sfetcu, R, Currie, M, Lisy, K, et al. Conducting systematic reviews of association (etiology): the Joanna Briggs Institute’s approach. JBI Evid Implement. (2015) 13:163–9. doi: 10.1097/XEB.0000000000000064
37. Herzig Van Wees, S, Gobbo, E, and Moreira De Cunha, N. COVID-19 vaccine hesitancy among adolescents: a qualitative synthesis of systematically reviewed studies; (2024). Available online at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42024512197 (Accessed April 22, 2024).
38. Tong, A, Flemming, K, McInnes, E, Oliver, S, and Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. (2012) 12:181. doi: 10.1186/1471-2288-12-181
39. Clark, JM, Sanders, S, Carter, M, Honeyman, D, Cleo, G, Auld, Y, et al. Improving the translation of search strategies using the polyglot search translator: a randomized controlled trial. J Med Libr Assoc. (2020) 108:195. doi: 10.5195/jmla.2020.834
40. Bramer, WM, Giustini, D, de Jonge, GB, Holland, L, and Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. (2016) 104:240–3. doi: 10.3163/1536-5050.104.3.014
41. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
42. Aromataris, E, Lockwood, C, Porritt, K, Pilla, B, and Jordan, Z, editors. JBI manual for evidence synthesis. JBI; (2024); Available online at: https://synthesismanual.jbi.global (Accessed May 2, 2024).
43. Barnett-Page, E, and Thomas, J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. (2009) 9:1–11. doi: 10.1186/1471-2288-9-59
44. Thomas, J, and Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:45. doi: 10.1186/1471-2288-8-45
45. ATLAS.ti. Scientific software development GmbH. Available online at: https://atlasti.com/ (Accessed October 21, 2024)
46. Nilsson, S, Mattson, J, Berghammer, M, Brorsson, AL, Forsner, M, Nolbris, M, et al. To be or not to be vaccinated against COVID-19 – the adolescents’ perspective – a mixed-methods study in Sweden. Vaccine X. (2021) 9:100117. doi: 10.1016/j.jvacx.2021.100117
47. Logie, CH, Okumu, M, Berry, I, McAlpine, A, Musoke, DK, Hakiza, R, et al. Multi-method findings on COVID-19 vaccine acceptability among urban refugee adolescents and youth in Kampala, Uganda. Glob Public Health. (2023) 18:1–14. doi: 10.1080/17441692.2023.2185800
48. McKinnon, B, Abalovi, K, Fortin, G, Parvez, M, Dalal, S, Bouabid, R, et al. Perspectives on COVID-19 vaccination and vaccine passports in a diverse urban adolescent population: a youth participatory mixed methods study. J Adolesc Health. (2023) 73:527–35. doi: 10.1016/j.jadohealth.2023.04.013
49. Abramovich, A, Pang, N, Kunasekaran, S, Moss, A, Kiran, T, and Pinto, AD. Examining COVID-19 vaccine uptake and attitudes among 2SLGBTQ+ youth experiencing homelessness. BMC Public Health. (2022) 22:122. doi: 10.1186/s12889-022-12537-x
50. Ramaiya, A, Mmari, K, Luiza Borges, A, Cabral, C, Mafuta, E, Lulebo, A, et al. Family, community, institutional and policy factors on COVID-19 vaccine perceptions among urban poor adolescents in seven countries: qualitative cross-site analysis. medRxiv. (2023). Available online at: http://medrxiv.org/content/early/2023/11/06/2023.11.03.23298048.abstract
51. Budhwani, H, Maycock, T, Murrell, W, and Simpson, T. COVID-19 vaccine sentiments among African American or black adolescents in rural Alabama. J Adolesc Health. (2021) 69:1041–3. doi: 10.1016/j.jadohealth.2021.09.010
52. Fisher, H, Lambert, H, Hickman, M, Yardley, L, and Audrey, S. Experiences of the coronavirus disease-19 (COVID-19) pandemic from the perspectives of young people: rapid qualitative study. Public Health Pract. (2021) 2:100162. doi: 10.1016/j.puhip.2021.100162
53. Alemu, D, Diribsa, T, and Debelew, G. COVID-19 vaccine hesitancy and its associated factors among adolescents. Patient Prefer Adherence. (2023) 17:1271–80. doi: 10.2147/PPA.S400972
54. Balma, B, Vasilakos, L, Osman, I, Elgonda, A, and Gewirtz O’Brien, JR. COVID-19 vaccine attitudes among youth experiencing homelessness: a qualitative analysis with opportunities for action. BMC Public Health. (2023) 23:1672. doi: 10.1186/s12889-023-16413-0
55. Groenewald, C, Isaacs, D, and Maluleka, M. “It doesn’t cure, but it protects”: COVID-19 vaccines through the eyes of children and their parents. Vaccines (Basel). (2023) 11:1305. doi: 10.3390/vaccines11081305
56. Mansfield, LN, Choi, K, Delgado, JR, Macias, M, Munoz-Plaza, C, Lewin, B, et al. Decision-making about COVID-19 vaccines among health care workers and their adolescent children. West J Nurs Res. (2023) 45:665–73. doi: 10.1177/01939459231170981
57. Garcia, J, Vargas, N, de la Torre, C, Magana Alvarez, M, and Clark, JL. Engaging Latino families about COVID-19 vaccines: a qualitative study conducted in Oregon, USA. Health Educ Behav. (2021) 48:747–57. doi: 10.1177/10901981211045937
58. Persaud, Y, Mandrell, BN, Sharma, A, Carroll, Y, Irvine, M, Olufadi, Y, et al. Attitudes toward COVID-19 vaccine among pediatric patients with sickle cell disease and their caregivers. Pediatr Blood Cancer. (2023) 70:e30274. doi: 10.1002/pbc.30274
59. Humer, E, Jesser, A, Plener, P, Probst, T, and Pieh, C. Education level and COVID-19 vaccination willingness in adolescents. Eur Child Adolesc Psychiatry. (2021) 32:537–9. doi: 10.1007/s00787-021-01878-4
60. Engelbrecht, M, Kigozi, G, and Heunis, C. Factors associated with limited vaccine literacy: lessons learnt from COVID-19. Vaccines (Basel). (2022) 10:1–14. doi: 10.3390/vaccines10060865
61. Biasio, L. Vaccine literacy is undervalued. Hum Vaccin Immunother. (2019) 15:2552–3. doi: 10.1080/21645515.2019.1609850
62. Herzig van Wees, S, and Ström, M. “Your child will have a bird brain!”: vaccination choices and stigma among vaccine enquirers in Sweden: a qualitative study. Soc Sci Med. (2024) 349:116893. doi: 10.1016/j.socscimed.2024.116893
63. Biasio, L, Zanobini, P, Lorini, C, Monaci, P, Fanfani, A, Gallinoro, V, et al. COVID-19 vaccine literacy: a scoping review. Hum Vaccin Immunother. (2023) 19:2176083. doi: 10.1080/21645515.2023.2176083
64. Hussain, B, Latif, A, Timmons, S, Nkhoma, K, and Nellums, L. Overcoming COVID-19 vaccine hesitancy among ethnic minorities: a systematic review of UK studies. Vaccine. (2022) 40:3413–32. doi: 10.1016/j.vaccine.2022.04.030
65. Yasmin, F, Najeeb, H, Moeed, A, Naeem, U, Asghar, MS, Chughtai, N, et al. COVID-19 vaccine hesitancy in the United States: a systematic review. Front Public Health. (2021):9. doi: 10.3389/fpubh.2021.770985
66. Truong, J, Bakshi, S, Wasim, A, Ahmad, M, and Majid, U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot Int. (2021) 37:1–13. doi: 10.1093/heapro/daab105
67. Mitchell, H, Lim, R, Gill, PK, Dhanoa, J, Dubé, È, and Bettinger, JA. What do adolescents think about vaccines? Systematic review of qualitative studies. PLOS Global Public Health. (2022) 2:e0001109. doi: 10.1371/journal.pgph.0001109
68. Vlasak, D, Dinero, RE, and Roitman, NA. Vaccine hesitancy at both ends of the socioeconomic spectrum: a new paradigm for understanding the role of systemic inequity. J Public Health Emerg. (2023) 7:1–7. doi: 10.21037/jphe-23-81
69. Schmid, P, Rauber, D, Betsch, C, Lidolt, G, and Denker, ML. Barriers of influenza vaccination intention and behavior – a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. (2017) 12:1–46. doi: 10.1371/journal.pone.0170550
70. Blahut, R, Flint, A, Orlando, E, DesChatelets, J, and Khowaja, A. A scoping review on the decision-making dynamics for accepting or refusing the COVID-19 vaccination among adolescent and youth populations. BMC Public Health. (2023) 23:1–9. doi: 10.1186/s12889-023-15717-5
Keywords: COVID-19, COVID-19 vaccines, vaccination hesitancy, adolescent, systematic review, qualitative synthesis
Citation: Moreira da Cunha N, Tzirita S, Gobbo E and Herzig van Wees S (2025) Factors influencing adolescents’ decision-making about COVID-19 vaccination: a systematic review with qualitative synthesis. Front. Public Health. 13:1563677. doi: 10.3389/fpubh.2025.1563677
Edited by:
Zephanie Tyack, Queensland University of Technology, AustraliaReviewed by:
Alessandra Naghettini, Universidade Federal de Goiás, BrazilZhaohui Su, Southeast University, China
Copyright © 2025 Moreira da Cunha, Tzirita, Gobbo and Herzig van Wees. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisa Gobbo, ZWxpc2EuZ29iYm9Aa2kuc2U=
 Nayara Moreira da Cunha
Nayara Moreira da Cunha Sofia Tzirita
Sofia Tzirita Elisa Gobbo
Elisa Gobbo Sibylle Herzig van Wees
Sibylle Herzig van Wees