- 1Department of Physical Therapy and Health Rehabilitation, College of Applied Medical Sciences, Majmaah University, Majmaah, Saudi Arabia
- 2Department of Family and Community Medicine, College of Medicine, Majmaah University, Majmaah, Saudi Arabia
- 3College of Nursing, Majmaah University, Majmaah, Saudi Arabia
- 4Department of Medical Specialities, College of Medicine, Majmaah University, Majmaah, Saudi Arabia
- 5Alartawya General Hospital, Al Artawiyah, Saudi Arabia
- 6Health and Basic Sciences Research Center, Majmaah University, Majmaah, Saudi Arabia
- 7Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
- 8School of Psychology, Sports and Sensory Sciences, Anglia Ruskin University, Cambridge, United Kingdom
- 9Nursing Technician, King Khaled Majmaah Hospital, Majmaah, Saudi Arabia
- 10Informed Decision Making, Riyadh, Saudi Arabia
- 11Sharik Association for Research and Studies, Riyadh, Saudi Arabia
Introduction: This study aims to assess the level of mental health literacy (MHL) among healthcare providers working in different healthcare settings in Saudi Arabia and to examine how socio-demographic factors such as gender, education, age, and personal exposure to mental health conditions associate with MHL.
Methods: This is a cross-sectional study that used a computer-assisted telephone interview. The study followed a previously validated methodology, ensuring consistency and comparability for future studies. Interviewers were trained to adhere to the interview guidelines and data collection that were streamlined using the ZDataCloud system. Participants aged 18 years and above and from 13 administrative different regions in Saudi Arabia were included and informed consent was obtained verbally from all participants. Data collection included healthcare worker demographics, mental health history, and familiarity with mental health issues. The Arabic MHL scale was used to assess participants’ knowledge and understanding of mental health disorders. MHL scale has been validated in the population in Saudi Arabia, demonstrating strong reliability and validity.
Results: The study revealed that female healthcare providers had significantly higher MHL scores in mental health recognition (females = 8.7 ± 1.2, males = 7.2 ± 1.5; p < 0.001) and attitudes (females = 9.3 ± 1.1, males = 7.8 ± 1.4; p < 0.001) compared to males. Healthcare providers with a Bachelor’s degree or higher exhibited higher score in mental health recognition (8.9 ± 1.3 vs. 7.1 ± 1.6; p < 0.001) and information-seeking (8.4 ± 1.4 vs. 7.2 ± 1.5; p = 0.003) compared to lower level of education. Younger participants (20–29 years old) showed more positive attitudes (p = 0.011), while those exposed to mental illness (p = 0.001) and higher-income earners (p = 0.040) demonstrated higher overall MHL.
Conclusion: Significant association between MHL domains and sociodemographic factors among healthcare providers in Saudi Arabia, highlighting the need for targeted interventions to improve MHL across among different healthcare groups.
Introduction
Jorm et al. (1) first proposed the term “Mental Health Literacy,” as defined by them, it refers to “knowledge and beliefs about mental disorders which aid their recognition, management or prevention” (2). Mental Health Literacy (MHL) is a more comprehensive term that defines the awareness, understanding and perceptions of mental health-related disorders (3). MHL is thought to be pivotal in raising awareness, treating and preventing potential mental health disorders (3). Basically, MHL involves being able to recognize specific mental illnesses, know where and how to access mental health information, and understand risk factors and causes that commonly associated with various mental health disorders.
This study is theoretically grounded in the MHL model by Jorm et al., supported by the Health Belief Model (HBM), which together provide a lens for evaluating healthcare workers’ perceptions and readiness to engage with mental health issues. Evaluating MHL in various age and professional groups offers insight into current awareness levels and is essential for developing targeted, evidence-based interventions.
Evaluating MHL in different age groups offers the benefit of providing a broad characteristics regarding the current mental health context, which can assist in framing health-related policies and planning targeted mental health interventions (4). Specifically, such point-in-time assessments such as baseline MHL testing in adult population could be used for evaluating future medical/non-medical interventions (5). MHL is also critical among healthcare workforce as greater MHL among healthcare workers may greatly enhance individuals with mental health conditions broadening their access to high quality mental health care interventions (6). In general, most individuals experience some forms of mental illness symptoms between the ages of 14 and 24 years, and many of these individuals may seek medical services (7). Several tools have been developed to assess MHL, with most of these tools targeting different dimensions of mental health knowledge and/or attitudes (8, 9). These tools include disorder-specific tools that mainly focused on specific health conditions such as depression and/or anxiety (9). MHL’s tools allow clinicians to gain more detailed information about awareness level among the public and understanding specific mental health conditions (10). For instance, tools for depression or anxiety not only aimed to identify symptoms but also attitudes that are essential clinical components for health professionals to provide better treatment. Evaluating MHL across broader cross-sections of society will provide a clearer indication of the knowledge held by different population groups and also offers the added benefit of identifying systemic barriers to accessing mental health care (11).
In the Saudi Arabian context, research focusing on the general population’s MHL exists but there is a significant gap concerning healthcare providers. Given that these professionals are at the forefront of mental health care, understanding their MHL is crucial. This study specifically examines physicians, nurses, and allied healthcare professionals to assess their baseline MHL using the validated MHL Scale developed by O’Connor and Casey (12), a 35-item instrument known for its reliability and internal consistency (12–14). Previous research has explored Mental Health Literacy (MHL) within the general population (15); however, this paper uniquely focuses on MHL among healthcare providers, a topic that has not been previously published.
Findings from this research can inform mental health policies, improve workforce training programs, and identify systemic barriers to accessing care. The study hypothesizes that MHL levels vary across healthcare provider categories, with physicians likely to demonstrate higher scores than nurses and allied health professionals. Understanding these variations will allow for more strategic planning and resource allocation to bridge the mental health service gap. The current study aimed to assess the level of MHL among healthcare providers who work currently in Saudi Arabia and to examine how socio-demographic factors such as gender, education, age, and personal exposure to mental health conditions associate with MHL.
Materials and methods
Study design
This is a cross-sectional study that included healthcare providers working in Saudi Arabia. The data were conducted through computer-assisted telephone interviews and last for 8 min in 2023. The current study followed the same method that was previously validated and published to ensuring consistency and comparability for future studies (4, 12–14). This methodology offers a robust framework for evaluating MHL among healthcare workers in Saudi Arabia, setting a stage for comparison such as baseline vs. future outcome data. Prior to data collection, all interviewers were trained in conducting telephone surveys by taking extensive training sessions to familiarize themselves with the interview guidelines. These training sessions ensured that all interviewers adhered to the consistent standards when interacting with participants through phone calls. Data collection was streamlined using the ZDataCloud system (a research data governance and quality system), which facilitated the governance and organization of collected data. This system enabled the efficient collection of data while minimizing errors and ensuring data integrity throughout data collection (16). Prior to study beginning, an ethical approval for this study was obtained by Sharik Association for Research ethics committee (Approval no. 2023–8).
Participants and recruitment
This study conducted a secondary data analysis using data from the Saudi Mental Health Literacy (MHL) database. The analysis included only healthcare providers working in Saudi Arabia who were 18 years or older. Each participant was asked about their employment in the healthcare sector, and only those who affirmed their involvement had their data included in this study.
Participants were selected using a systematic random sampling method across all 13 administrative regions of Saudi Arabia, utilizing the ZDataCloud data governance and collection system. ZDataCloud is an advanced research data management platform designed to ensure high-quality data collection, adherence to scientific sampling methodologies, and automated validation processes. The system integrates eligibility verification, real-time monitoring, and compliance enforcement to maintain data integrity. Notably, the dataset exhibited no missing information, as ZDataCloud requires participants to complete all questions before submission, ensuring data completeness and accuracy.
The recruitment process involved contacting potential individuals via telephone list, with each participant receiving a maximum of three attempts to respond. If a participant did not respond after the third attempt, another individual with a similar demographic profile, such as age, gender, and location, was contacted. Informed consent was obtained verbally from all participants after they were informed about the purpose of the study, the type of data being collected, and their right to withdraw from the study at any time.
The verbal consent process, approved by the Sharik Association for Health Research, was documented in the data collection system.
Data collection
Data were collected using the ZDataCloud system, an advanced data collection platform designed to reduce sampling bias through automated processes, which allowed for real-time monitoring of participant eligibility and controlled the sample size within each dataset, and post-collection data integrity checks were performed, and no issues were found, confirming the accuracy of the data. The study focused on multiple variables, including healthcare worker demographics, mental health history, and familiarity with mental health issues. MHL scale was utilized to assess participants’ knowledge and understanding of mental health disorders (4). The MHL scale consists of 35 items that participants rated on a 4-point Likert scale (ranging from “Very unlikely” to “Very likely”). For example, one item asked participants to rate the likelihood that a person exhibits certain anxiety-related behaviors might have social phobia, while another item assessed attitudes toward seeing/seeking a mental health professional.
The MHL scale scores range from 35 to 160, with higher scores indicating MHL. The scale has been validated in the Saudi population, demonstrating strong reliability and validity (4).The psychometric properties of the MHL scale in Saudi Arabia, including its internal consistency has been previously published, reinforcing its suitability for the current study.
Statistical analysis
Data were entered in an Excel sheet and our statistical analyses were performed using the SPSS (V-28). Categorical variables were expressed as frequencies and percentages. Matrix data were presented as means, standard deviations, medians and percentiles. Relationship between MHL scores of different components and socio-demographic factors, history of mental health diagnosis, living with a person diagnosed with mental health and Friend with a person diagnosed with mental health were tested using t-tests or ANOVA tests based on the number of categories for our independent variables. The statistical significance level (p-value) was set a priori as less than 0.05.
Results
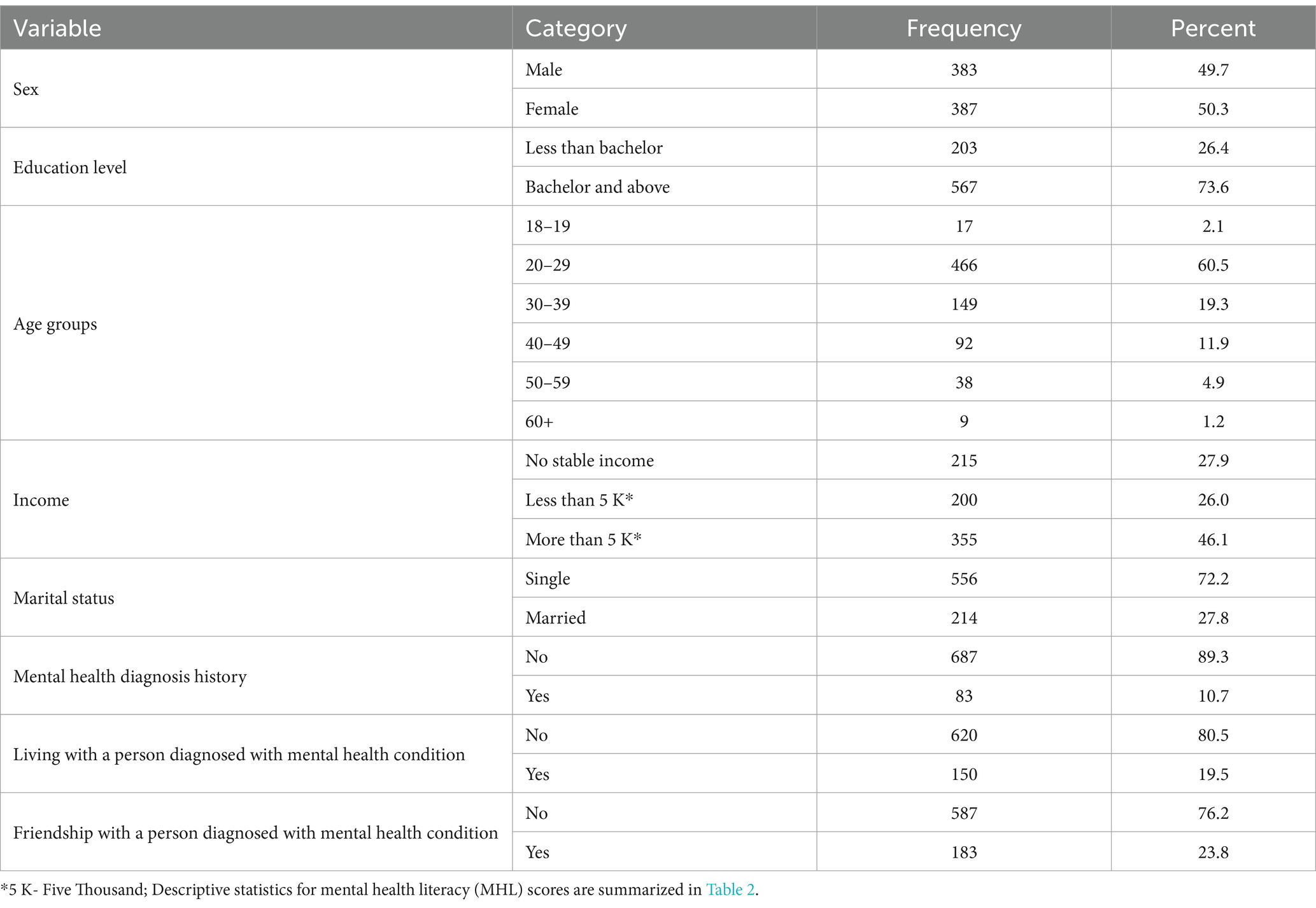
Table 1 presents the demographic characteristics of the study participants. Our sample was nearly evenly divided between males (49.7%) and females (50.3%). A significant majority (73.6%) of our sample held a Bachelor’s degree or higher, while 26.4% of them had less than a Bachelor’s education. The largest age group was 20–29 years (60.5%), followed by 30–39 years (19.3%). Regarding monthly income, 46.1% of participants reported earning more than 5 K (5,000 Saudi Riyals), while 27.9% had no stable monthly income. Most of our participants were singles (72.2%), and the majority had no history of mental health diagnoses (89.3%). Additionally, 19.5% of our participants reported living with someone diagnosed with a mental health condition, and 23.8% indicated having a friend with mental health disorders.
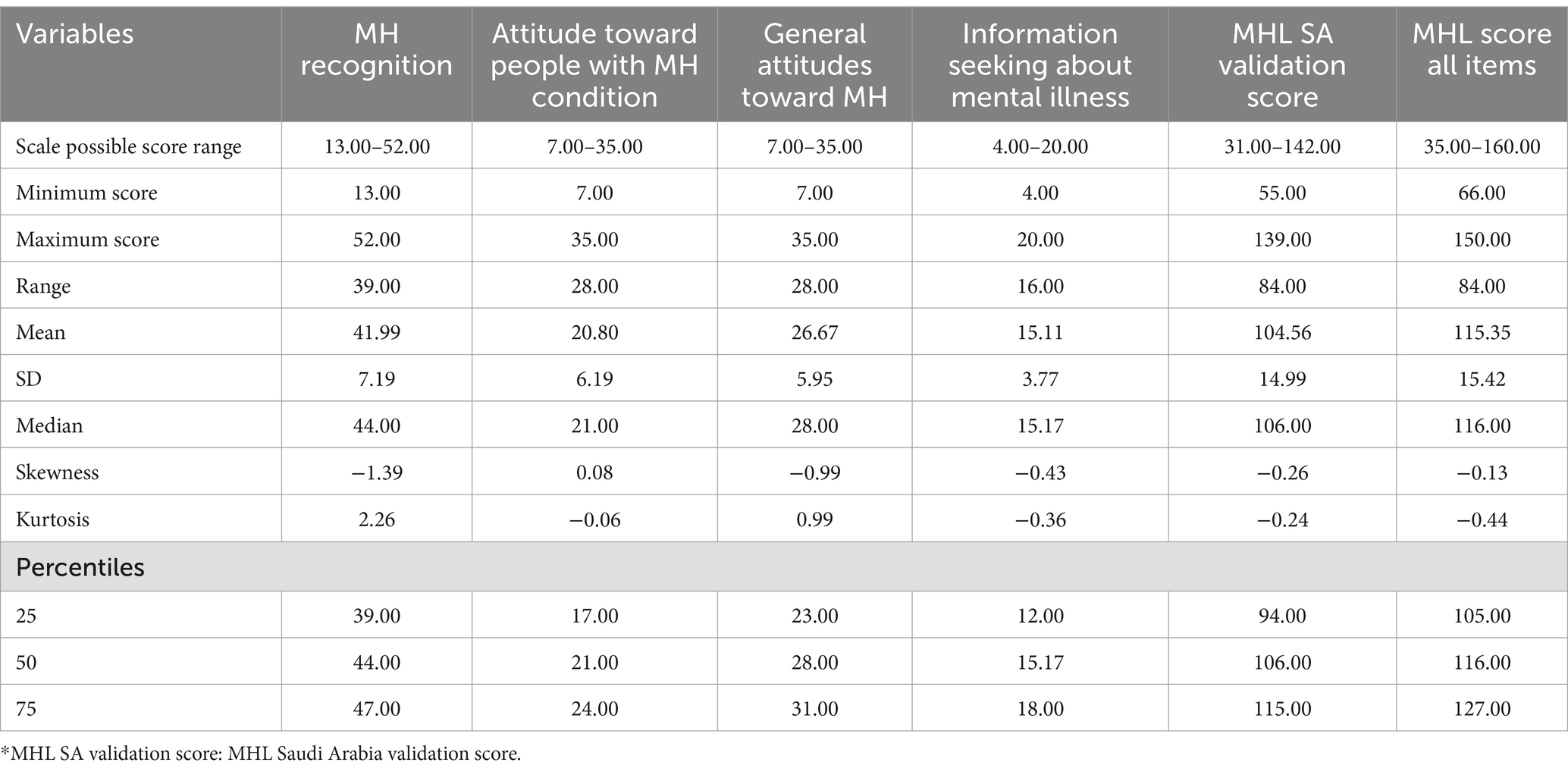
Table 2 presents descriptive statistics for Mental Health Literacy (MHL) scores among health care providers in Saudi Arabia. The results show that the average overall MHL score (all items) was 115.35 (SD = 15.42), with scores ranging from 66.00 to 150.00. Among the subscales, “mental health recognition” had the highest mean score (M = 41.99, SD = 7.19), indicating relatively strong ability to identify mental health conditions. In contrast, “attitude toward people with mental health conditions” had the lowest mean (M = 20.80, SD = 6.19), reflecting potential areas for improvement in stigma-related attitudes. The distributions for most subscales were slightly negatively skewed, suggesting a tendency toward higher scores within the sample. These findings highlight both strengths and gaps in MHL among healthcare providers, emphasizing the need for targeted interventions to address attitudinal barriers.
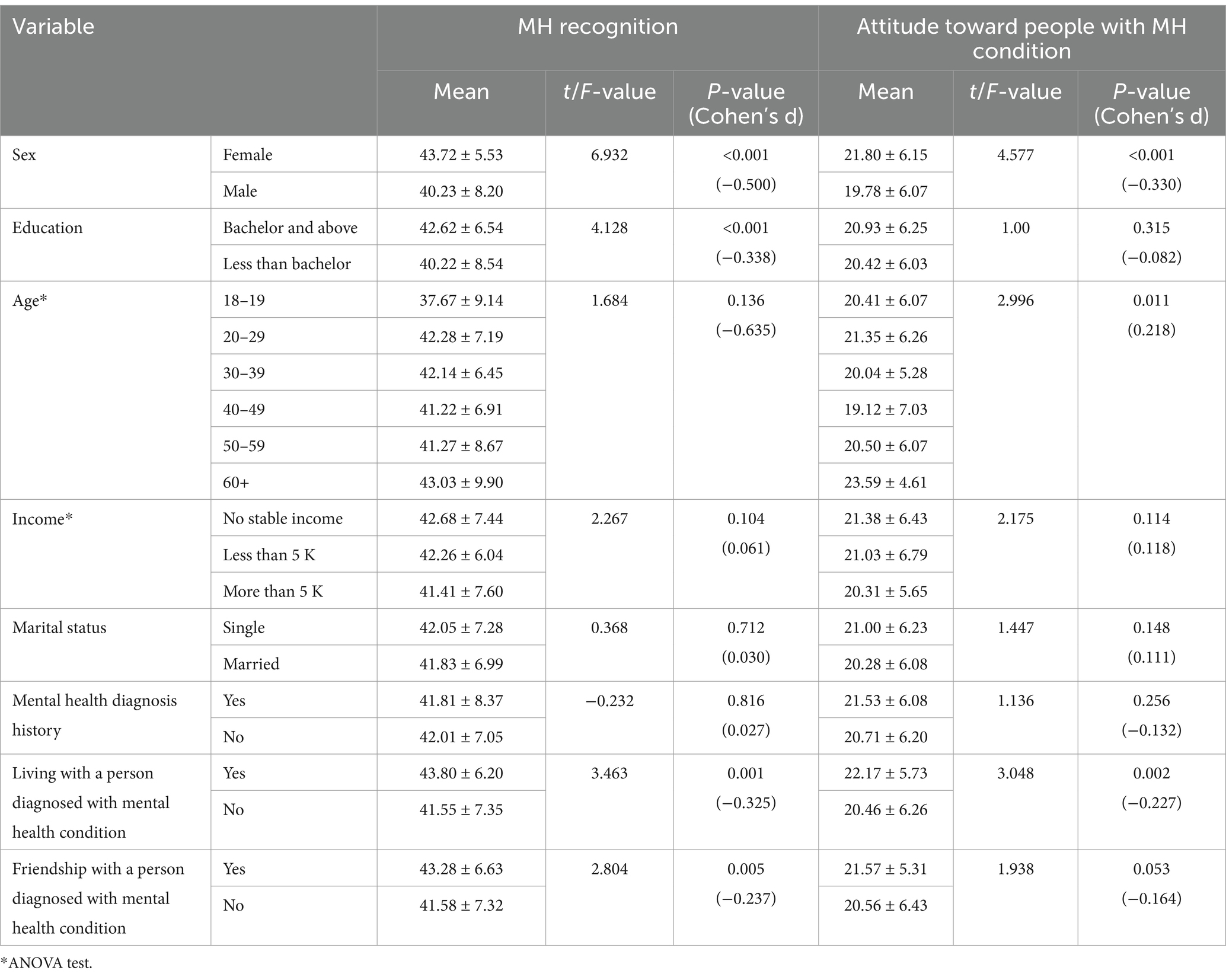
Table 3 explores the associations between MHL scores and socio-demographic characteristics. Female participants’ scores were significantly higher in both mental health recognition (p < 0.001) and attitudes toward people with mental health conditions (p < 0.001) compared to males. Those with a Bachelor’s degree or higher also exhibited significantly higher mental health recognition scores (p < 0.001). Although no significant differences were observed in mental health recognition scores across age groups, participants aged 20–29 years old displayed significantly more positive attitudes toward people with mental health conditions (p = 0.011). Additionally, participants living with someone diagnosed with a mental health condition had significantly higher scores in both mental health recognition (p = 0.001) and attitudes (p = 0.002).
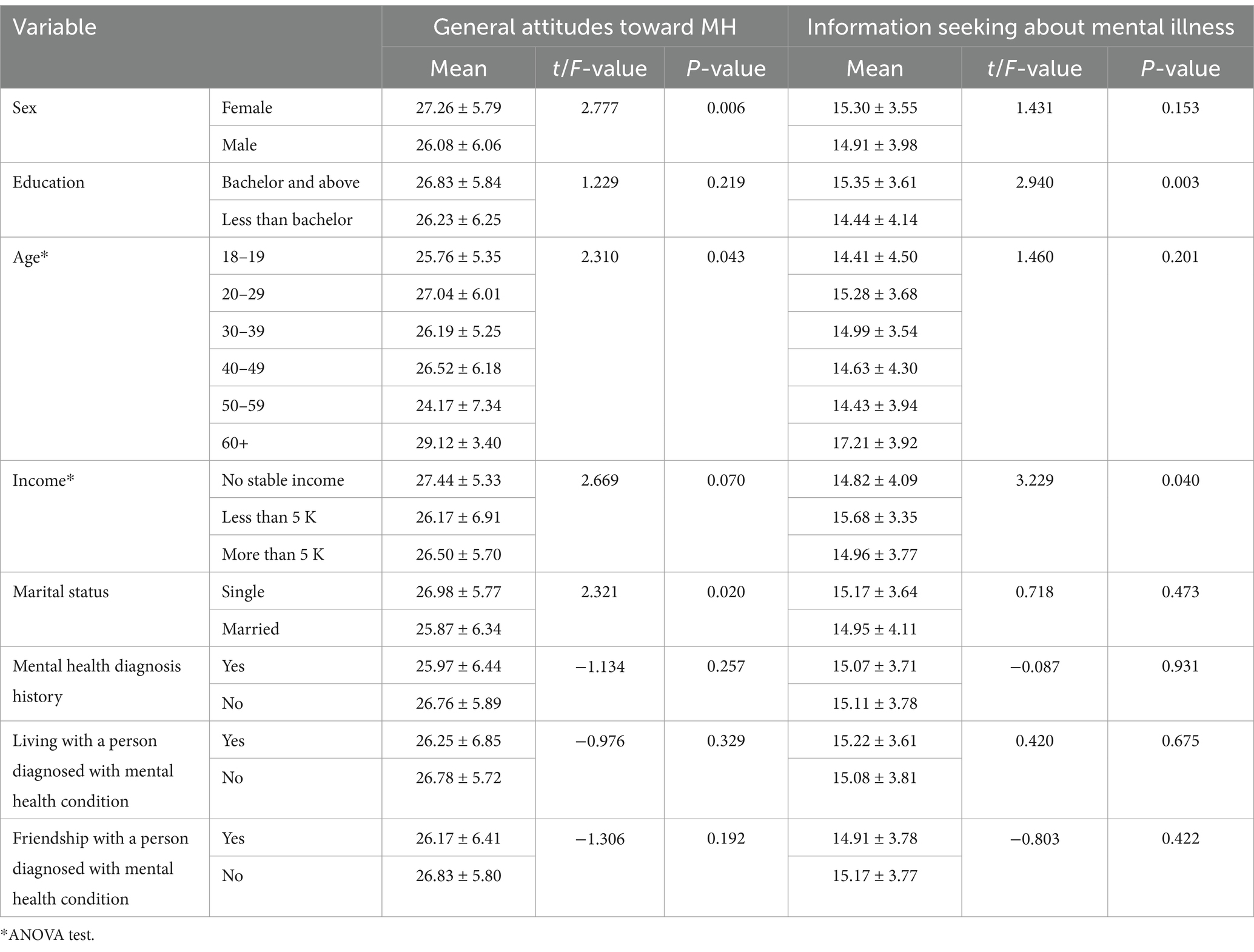
Table 4 analyzed the association between MHL scores and general attitudes toward mental health, as well as information-seeking behavior. Female participants exhibited significantly more positive general attitudes toward mental health (p = 0.006) than males. Participants with a Bachelor’s degree or higher were more likely to engage in information-seeking about mental illness (p = 0.003) than those who had educated less than a bachelor degree. Significant differences were also observed in the general attitudes and information-seeking behaviors across age and income groups, with older individuals and those with a stable income showing more positive attitudes and greater information-seeking behaviors (p = 0.043 and p = 0.040, respectively) than younger individuals and unstable income individuals.
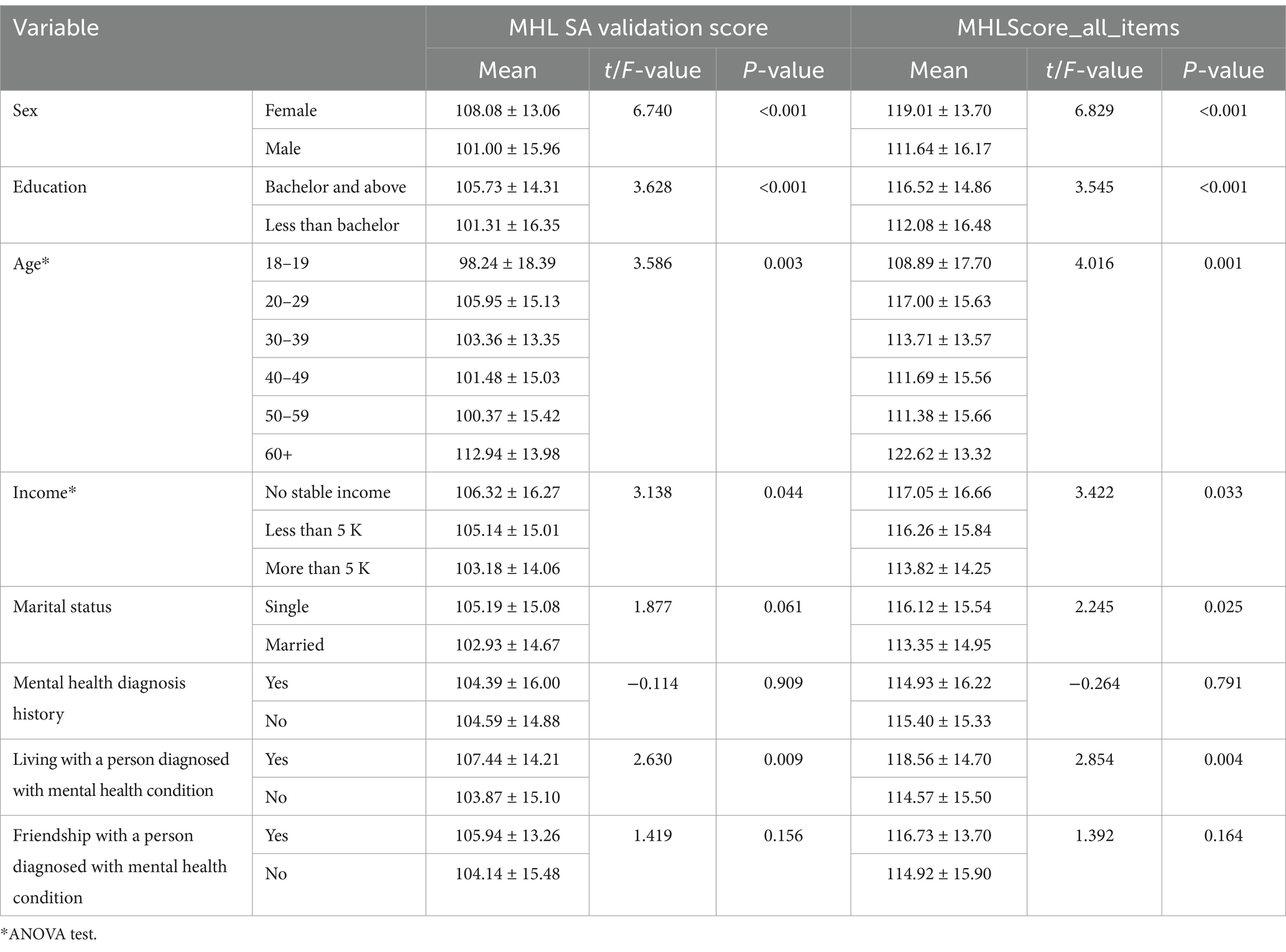
Table 5 evaluated the overall MHL scores in relation to socio-demographic variables. Female participants demonstrated significantly higher scores on both the MHL validation scale and the overall MHL score (p < 0.001) than males. Similarly, participants with a Bachelor’s degree or higher had significantly higher MHL scores across both metrics (p < 0.001) than those who had educated less than bachelor degree. Those living with someone diagnosed with a mental health condition also exhibited significantly higher scores on both the MHL validation and overall scales (p = 0.009 and p = 0.004, respectively) than those without living with someone diagnosed with a mental health condition. Age and income were also significantly positively associated with MHL scores, further emphasizing the role of socio-demographic factors in shaping mental health literacy.
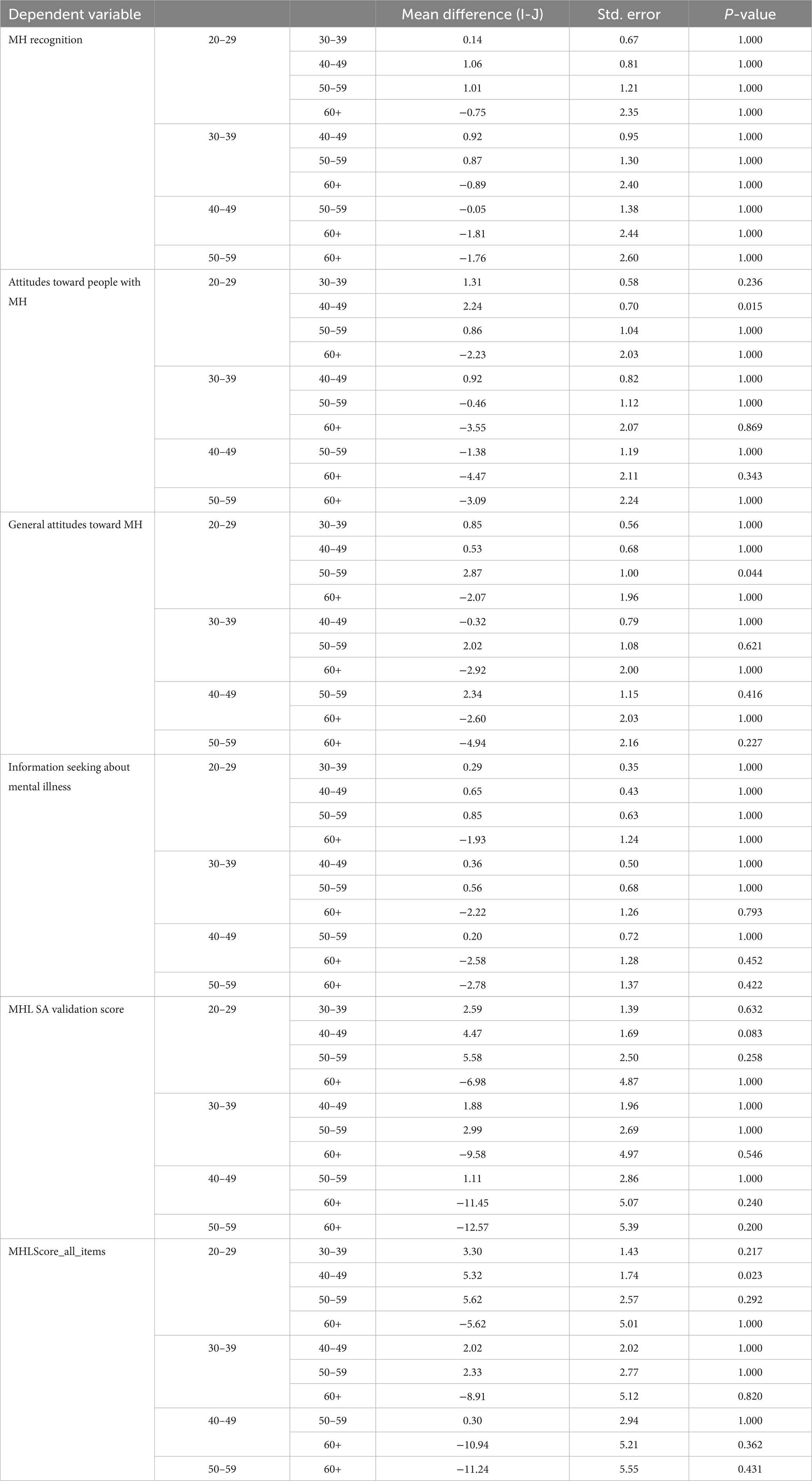
The post-hoc analysis using Bonferroni correction revealed no statistically significant differences in mental health (MH) recognition, attitudes toward people with MH, general attitudes toward MH, or information-seeking behavior across different age groups, with the exception of two comparisons. Participants aged 20–29 demonstrated significantly more positive attitudes toward people with mental health issues compared to those aged 40–49 (p = 0.015), and those aged 20–29 also showed significantly more favorable general attitudes toward MH than those aged 50–59 (p = 0.044). These findings suggest that younger age groups may hold more positive views and attitudes related to mental health compared to some older cohorts (Table 6).
Discussion
This study examined Mental Health Literacy (MHL) among healthcare providers working in diverse clinical settings in Saudi Arabia, analyzing how socio-demographic and experiential factors influence MHL levels. Significant associations were found between MHL and gender, education level, income, and personal exposure to mental health conditions. Although age did not demonstrate a strong statistical correlation with MHL, certain patterns were observed.
When disaggregated by professional role, physicians showed comparatively higher MHL scores than nurses and allied health professionals, particularly in domains of disorder recognition and information-seeking behavior. This aligns with Kutcher et al. (2) and O’Connor and Casey (12), who emphasized that greater medical training correlates with higher MHL. However, consistent with Elyamani and Hammoud (17), even formally educated professionals (especially junior staff and nurses) in the Arab Gulf context sometimes exhibit negative attitudes and limited practical competence in managing mental illness. This underscores the need for ongoing professional development beyond initial education.
Healthcare setting and professional role likely play an important role in shaping MHL, although due to sample limitations, comparisons across public vs. private institutions could not be fully explored. Future studies should incorporate this stratification to uncover setting-specific disparities.
Age-related findings revealed a nuanced pattern. Older healthcare professionals (60 + years) scored higher in some MHL domains, likely due to prolonged professional exposure. This partially contrasts Wei et al. (9), who found younger adults to be more knowledgeable due to recent academic exposure and digital literacy. Our findings suggest that while younger individuals may benefit from formal education, practical, on-the-job exposure among older professionals may compensate for a lack of recent training. Effect sizes, while modest, indicate a meaningful trend worth further exploration.
Female participants scored significantly higher than males in domains related to attitudes and help-seeking, aligning with O’Connor and Casey (12) and broader health literature that highlights greater empathy and proactive mental health engagement among women. While the effect size was moderate (Cohen’s d ≈ 0.4), it signals the need for gender-targeted mental health training initiatives, particularly for male healthcare workers, who may under-identify psychiatric symptoms and delay patient referrals.
Education level and income also emerged as significant predictors. Higher educational attainment was associated with better MHL, particularly in symptom recognition and treatment awareness, reinforcing the findings of Kutcher et al. (2). However, this relationship is not linear nor uniform, as illustrated in Elyamani and Hammoud (17) and Marangu et al. (18), who found low MHL even among academically trained professionals in resource-constrained or underserved contexts. Thus, formal qualifications alone may be insufficient without active professional reinforcement, clinical exposure, and training.
Personal exposure to mental illness, whether through patients, family, or personal experience, strongly influenced MHL. This is consistent with Morgan et al. (19), who highlighted the role of familiarity in reducing stigma. Yet, as shown by Oztas and Aydoğan (20), exposure outside structured mental health units may still result in suboptimal literacy unless supported by formal guidance and clinical supervision.
Cultural and systemic influences in Saudi Arabia must also be acknowledged. Despite growing national attention to mental health, cultural stigma, reliance on family-based care, and the limited integration of mental health into primary care continue to act as barriers. Religious beliefs and societal norms may influence provider attitudes, shaping their willingness or confidence in addressing psychiatric disorders.
While the findings are robust, the study is subject to limitations. Self-reported responses may introduce social desirability bias, and the cross-sectional design limits causal inference. Moreover, confounding variables such as specialty area, years of clinical experience, prior mental health training, or type of institution (public vs. private) were not fully controlled. Future research should incorporate multivariate regression models to isolate independent predictors of MHL.
Future directions
To build upon these findings, the following areas are recommended for further investigation:
1. Multivariable analyses that control for confounders such as clinical experience and workplace mental health training.
2. Longitudinal studies to assess whether MHL improves over time with targeted education.
3. Evaluation of differences in MHL across healthcare settings (urban vs. rural, public vs. private).
4. Development and validation of Saudi Arabia–specific MHL interventions that are culturally and linguistically appropriate.
5. Implementation of interventional studies to assess the impact of structured MHL training on clinical decision-making and patient outcomes.
Conclusion
The study showed significant associations between MHL and socio-demographic factors among healthcare providers in Saudi Arabia, emphasizing the need for targeted interventions to improve MHL across different groups. One of the steps toward improving health care would be to improve MHL among healthcare workers, which in turn could help advance mental health services—a focus area for Saudi Arabia. In order to achieve this, targeted programs for MHL need to be designed and implemented specifically catered toward male healthcare workers, lower educated, and lower monthly income groups.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Sharik Association for Research ethics committee (Approval no. 2023–8). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NZA: Conceptualization, Investigation, Project administration, Resources, Supervision, Validation, Writing – review & editing. RS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Writing – original draft, Writing – review & editing. MA: Conceptualization, Data curation, Writing – review & editing. BA: Conceptualization, Data curation, Supervision, Visualization, Writing – review & editing. TA: Conceptualization, Investigation, Resources, Visualization, Writing – review & editing. IA: Data curation, Supervision, Writing – review & editing. SB: Conceptualization, Methodology, Writing – review & editing. SA: Software, Writing – review & editing. KA: Conceptualization, Investigation, Writing – review & editing. NAA: Formal analysis, Project administration, Software, Writing – review & editing. NB: Conceptualization, Data curation, Formal analysis, Investigation, Software, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors extend the appreciation to the Deanship of Postgraduate Studies and Scientific Research at Majmaah University for funding this study with project no R-2025-1736. Also, author extends the appreciation to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R539), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Acknowledgments
The authors extend the appreciation to the Deanship of Postgraduate Studies and Scientific Research at Majmaah University for funding this study with project no R-2025-1736. Also, author extends the appreciation to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R539), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia Lastly, we would like to acknowledge National Center for Mental Health Promotion for their enablement to complete this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Reavley, NJ, and Jorm, AF. Recognition of mental disorders and beliefs about treatment and outcome: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. (2011) 45:947–56. doi: 10.3109/00048674.2011.621060
2. Kutcher, S, Wei, Y, and Coniglio, C. Mental health literacy: past, present, and future. Can J Psychiatry. (2016) 61:154–8. doi: 10.1177/0706743715616609
3. Coughlan, EC, Heyland, LK, Sheaves, A, Parlee, M, Wiley, C, Page, D, et al. Characteristics of mental health literacy measurement in youth: a scoping review of school-based surveys. Discov Ment Health. (2024) 4:24. doi: 10.1007/s44192-024-00079-0
4. ElKhalil, R, AlMekkawi, M, O'Connor, M, Sherif, M, Masuadi, E, Ahmed, LA, et al. Measurement properties of the mental health literacy scale (MHLS) validation studies: a systematic review protocol. BMJ Open. (2024) 14:e081394. doi: 10.1136/bmjopen-2023-081394
5. Krokos, O, Brandhorst, I, Seizer, L, Gawrilow, C, and Löchner, J. Improving mental health by improving the mental health literacy? Study protocol for a randomised controlled evaluation of an e-mental health application as a preventive intervention for adolescents and young adults. Internet Interv. (2024) 36:100733. doi: 10.1016/j.invent.2024.100733
6. Chao, HJ, Lien, YJ, Kao, YC, Tasi, IC, Lin, HS, and Lien, YY. Mental health literacy in healthcare students: an expansion of the mental health literacy scale. Int J Environ Res Public Health. (2020) 17:948. doi: 10.3390/ijerph17030948
7. Mental health disorders in adolescents. Committee opinion no. 705: mental health disorders in adolescents. Obstet Gynecol. (2017) 130:e32–41. doi: 10.1097/AOG.0000000000002160
8. Campos, L, Dias, P, Costa, M, Rabin, L, Miles, R, Lestari, S, et al. Mental health literacy questionnaire-short version for adults (MHLq-SVa): validation study in China, India, Indonesia, Portugal, Thailand, and the United States. BMC Psychiatry. (2022) 22:713. doi: 10.1186/s12888-022-04308-0
9. Wei, Y, McGrath, PJ, Hayden, J, and Kutcher, S. Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry. (2016) 16:1–6. doi: 10.1186/s12888-016-1012-5
10. Nejatian, M, Tehrani, H, Momeniyan, V, and Jafari, A. A modified version of the mental health literacy scale (MHLS) in Iranian people. BMC Psychiatry. (2021) 21:53. doi: 10.1186/s12888-021-03050-3
11. Renwick, L, Pedley, R, Johnson, I, Bell, V, Lovell, K, Bee, P, et al. Mental health literacy in children and adolescents in low-and middle-income countries: a mixed studies systematic review and narrative synthesis. Eur Child Adolesc Psychiatry. (2024) 33:961–85. doi: 10.1007/s00787-022-01997-6
12. O’Connor, M, and Casey, L. The mental health literacy scale (MHLS): a new scale-based measure of mental health literacy. Psychiatry Res. (2015) 229:511–6. doi: 10.1016/j.psychres.2015.05.064
13. Balula Chaves, C, Sequeira, C, Carvalho Duarte, J, Nelas, P, Gonçalves, A, and Santos, E. Mental health literacy: a systematic review of the measurement instruments. Rev INFAD Psicol. (2022) 3:181–94. doi: 10.17060/ijodaep.2021.n2.v3.2285
14. Montagni, I, and González Caballero, JL. Validation of the mental health literacy scale in French university students. Behav Sci. (2022) 12:259. doi: 10.3390/bs12080259
15. BinDhim, NF, Althumiri, NA, Ad-Dab'bagh, Y, Alqahtani, MMJ, Alshayea, AK, Al-Luhaidan, SM, et al. Exploring mental health literacy and its associated factors: a National Cross-Sectional Study in Saudi Arabia, 2023. Risk Manag Healthc Policy. (2024) 17:355–63. doi: 10.2147/RMHP.S442425
16. ZDataCloud: research data governance and quality system (2023). Available online at: https://zdatacloud.com (Accessed March 10, 2023).
17. Elyamani, R, and Hammoud, H. Mental health literacy of healthcare providers in Arab gulf countries: a systematic review. J Prim Care Community Health. (2020) 11:2150132720972271. doi: 10.1177/2150132720972271
18. Marangu, E, Mansouri, F, Sands, N, Ndetei, D, Muriithi, P, Wynter, K, et al. Assessing mental health literacy of primary health care workers in Kenya: a cross-sectional survey. Int J Ment Heal Syst. (2021) 15:55. doi: 10.1186/s13033-021-00481-z
19. Morgan, AJ, Reavley, NJ, Ross, A, Too, LS, and Jorm, AF. Interventions to reduce stigma towards people with severe mental illness: systematic review and meta-analysis. J Psychiatr Res. (2018) 103:120–33. doi: 10.1016/j.jpsychires.2018.05.017
Keywords: sociodemographic, literacy tool, Saudi Arabia, mental health, mental literacy
Citation: Alrashdi NZ, Shaik RA, Ahmad MS, Alrasheadi BA, Alotaibi TH, Alrashedy IZ, Bajuaifer S, Ahmad S, Alrashidi KA, Althumiri NA and BinDhim NF (2025) Exploring mental health literacy and its associated factors among health care providers: a National Cross-Sectional Study in Saudi Arabia. Front. Public Health. 13:1564013. doi: 10.3389/fpubh.2025.1564013
Edited by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaReviewed by:
Dushad Ram, Shaqra University, Saudi ArabiaShashank Saurabh Sinha, King George’s Medical University, India
Sujata Sethi, Pandit Bhagwat Dayal Sharma University of Health Sciences, India
Copyright © 2025 Alrashdi, Shaik, Ahmad, Alrasheadi, Alotaibi, Alrashedy, Bajuaifer, Ahmad, Alrashidi, Althumiri and BinDhim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Riyaz Ahamed Shaik, ci5zaGFpa0BtdS5lZHUuc2E=
 Naif Z. Alrashdi1,6
Naif Z. Alrashdi1,6 Riyaz Ahamed Shaik
Riyaz Ahamed Shaik Mohammad Shakil Ahmad
Mohammad Shakil Ahmad Bader A. Alrasheadi
Bader A. Alrasheadi Nora A. Althumiri
Nora A. Althumiri Nasser F. BinDhim
Nasser F. BinDhim