- 1School of Nursing and Midwifery, Debre Berhan University, Debre Berhan, Ethiopia
- 2School of Computing, Mathematics and Engineering, Charles Sturt University, Wagga Wagga, NSW, Australia
Malnutrition, encompassing both underweight and obesity, poses a significant public health challenge for women worldwide, spanning across developed and developing nations. Sub-Saharan Africa (SSA) bears a notably high burden of underweight, despite recent years have seen a noticeable increase in obesity rates. Lactating women are especially vulnerable to malnutrition. This analytic review aimed to compile current knowledge on the spatial distribution, prevalence, and contributing factors of malnutrition among lactating mothers in Sub-Saharan Africa, highlighting research gaps. This review systematically searched previous primary studies and reports from databases including PubMed, MEDLINE, PsycINFO, Web of Science, HINARI, EMBASE, African Journal of Online (AJOL), Scopus and Google Scholar. Various significant findings were synthesized in textual descriptions, figures and tables. The prevalence of underweight among lactating women in sub-Saharan Africa exhibits considerable disparity, spanning from 5.6 to 54.8%. However, there was no comprehensive summarized evidence for this issue in the region. Additionally, our findings emphasize a deficiency in comprehending the geographic distribution and factors influencing malnutrition among lactating women in sub-Saharan Africa. The burden of overweight in SSA was 15.9% among reproductive women; this burden is going to be increased. However, there were no studies conducted among the most vulnerable women, lactating women. Similarly, despite the spatial distribution of obesity/overweight among reproductive omen in SSA was known, there were no evidences for lactating women who have high risk for malnutrition as pregnant women. Hence, conducting population-wide, representative, and comprehensive research utilizing Demographic Health Survey data from countries in sub-Saharan Africa is imperative to fully comprehend the extent of the problem and effectively address the burden of malnutrition in this vulnerable population. Additionally, identifying hotspot areas of malnutrition specifically among lactating women within sub-Saharan Africa through spatial distribution analysis is essential for allocating resources appropriately, addressing a critical concern in the region and helps to reduce morbidity and mortality.
1 Introduction
Malnutrition entails an imbalance between nutrient intake and the essential nutrients required for optimal health and bodily function. It can classified as undernutrition, overnutrition, or micronutrient deficiencies (1). The scope of this review addressed only the burden, spatial distribution and factors associated with underweight and obesity/overweight among lactating women. Underweight is delineated by a body mass index (BMI) of below 18.5 kg/m2, while obesity is identified as a BMI exceeding 30 kg/m2 (2) and if BMI is between 25 and 29.9 kg/m2 it is called overweight. According to prevailing literature in nutrition and women’s health, malnutrition can occur across the life course of women, including adolescence, pregnancy, lactation, and postmenopausal stages, each presenting unique nutritional challenges and health implications (3).
Globally, in 2022, approximately 390 million reproductive women were underweight, while 2.5 billion were deemed overweight and890 million suffered from obesity (4). Underweight in mothers who breastfeed is a serious problem worldwide, especially in developing nations. Research indicates that a significant percentage of lactating mothers are underweight, with prevalence rates in Africa ranging from 1.25 to 30% (5). Malnutrition among lactating mothers poses significant health risks not only to mothers themselves but also to their infants, contributing to intergenerational cycles of undernutrition and poor health outcomes (6). Therefore, this review addressed a critical area of concern within public health and maternal-child nutrition.
Studies have documented regional disparities in malnutrition prevalence. Additionally, research has identified a range of determinants, including socioeconomic factors, cultural practices, and access to healthcare, influencing nutritional outcomes among lactating mothers (7).
However, the extent of evidences about the spatial distribution, burden and factors associated with underweight, obesity and overweight among lactating women at SSA level was unknown. Therefore, this study aimed to extensively review the current evidences on this area and show research gaps which need future investigation.
2 Methodology
In this review, peer-reviewed articles, academic dissertations, and reports that described malnutrition among lactating mothers in SSA were searched, reviewed and included. Furthermore, it encompassed observational studies, systematic reviews, and meta-analyses written in English. Lastly, interventional studies were also considered to see programs effectiveness.
A comprehensive exploration spanned various databases, including PubMed, MEDLINE, PsycINFO, HINARI, EMBASE, African Journal of Online (AJOL), Scopus, Web of Science, Google Scholar, and Google. Our search strategy involved a combination of pertinent keywords and Medical Subject Headings (MeSH terms) pertaining to malnutrition, lactating women, and SSA. Identified articles were sifted for determinants according to specified terms. Additionally, primary article references were scrutinized. Statistical analysis was done using Stata version 16 software.
Lastly, the general topic of this research project gyrated around understanding the complex dynamics of malnutrition (underweight, obesity and overweight) among lactating women in SSA who breastfeed their under 2 years child Therefore, studies which conducted to see the spatial distributions, burden and determinants that influence the nutritional status in this population were considered.
3 Review results
Double burden of malnutrition (DBM) refers to the simultaneous presence of both undernutrition and overweight or obesity within individuals, households, and populations (8). DBM poses a momentous public health dare in low-and middle-income countries (LMICs) found in Asia (9) and Africa (10).
As shown in Figure 1, the African region is the most affected (11). In Africa, the DBM among children and women of reproductive age has been extensively studied, with numerous comprehensive and summarized pieces of evidence available (10, 12–21).

Figure 1. The global burden of malnutrition reported by a study conducted by Alem et al. (11).
However, the extent of evidence available on the malnutrition burden among lactating women was limited. Consequently, the subsequent sections review critically the exact of knowledge on spatial distribution, burden and factors associated with underweight and obesity/overweight among lactating women in SSA.
3.1 Spatial distributions of underweight and obesity
Spatial distribution is the arrangement or pattern of objects in physical space and the study of the relationships between them. It is one of the fundamental concepts in geography, urban planning, ecology, health, and other fields (22). By analyzing spatial distribution, researchers can gain insights into processes such as diffusion, migration, urbanization, and resource allocation (23, 24). Population distribution is primarily influenced by a multitude of factors. These include climate, landforms, topography, cultural and political considerations (25).
An analysis using data from the 2016 Ethiopian DHS focused on the geographic distribution of underweight among women of reproductive age identified regions with high burden; Amhara, Tigray, Gambella, and Afar regions (26). Another spatial study conducted among reproductive women in Ethiopia also identified hotspot regions; Tigray, Afar and Amhara (27). Besides, a study conducted in Ethiopia among women also indicated notable hotspot areas in the Eastern and northeastern part of the country (28).
Geospatial research among reproductive-age women in SSA identified significant regions where overweight/obesity and anemia co-occur (29). Several hotspot regions of co-existence were found in Nigeria, South Africa, Mali Cameroon, Mauritania, Tanzania, Liberia and Benin. Conversely, cold spot areas were observed in Burundi, Ethiopia, Guinea, Uganda, Sierra Leone, Madagascar and Rwanda (29). Another study done in Ghana mapped the distribution of undernutrition among non-pregnant women, highlighting clusters in the western Northern region and hotspots of overweight/obesity in several other areas (30).
A nationwide study conducted using data from the Nigerian DHS also examined the spatial distribution of obesity/overweight. It revealed significant variation across ethnic groups and states of residence, with the highest prevalence observed in Cross River State, in southeastern Nigeria, and the lowest in Osun State, situated in southwestern Nigeria (31). All the above studies were conducted among reproductive age women and we did not found any summarized evidence about the spatial distributions of malnutrition among lactating women in SSA. Therefore, a population based geospatial study among lactating women should be conducted using the national DHS data to identify the hotspot countries in the SSA.
3.2 Prevalence of underweight among lactating women in SSA
Globally, statistics reveal that approximately 13% of women are underweight. This prevalence is significantly higher in economically disadvantaged nations, with rates ranging from 20 to 25% for underweight (32–34). Pregnant and lactating women are more vulnerable than others (35). The global burden of undernutrition among lactating women is a substantial public health concern, particularly in low-and middle-income countries (LMICs). Recent estimates from the World Health Organization (WHO) indicate that about 22% of lactating women worldwide are affected by undernutrition (36). In SSA countries, this problem presents a grave concern. Consequently, the region grapples with alarmingly high morbidity and mortality rates (37), exacerbated by its susceptibility to both natural and manmade disasters, precipitating socio-economic adversities (5, 38).
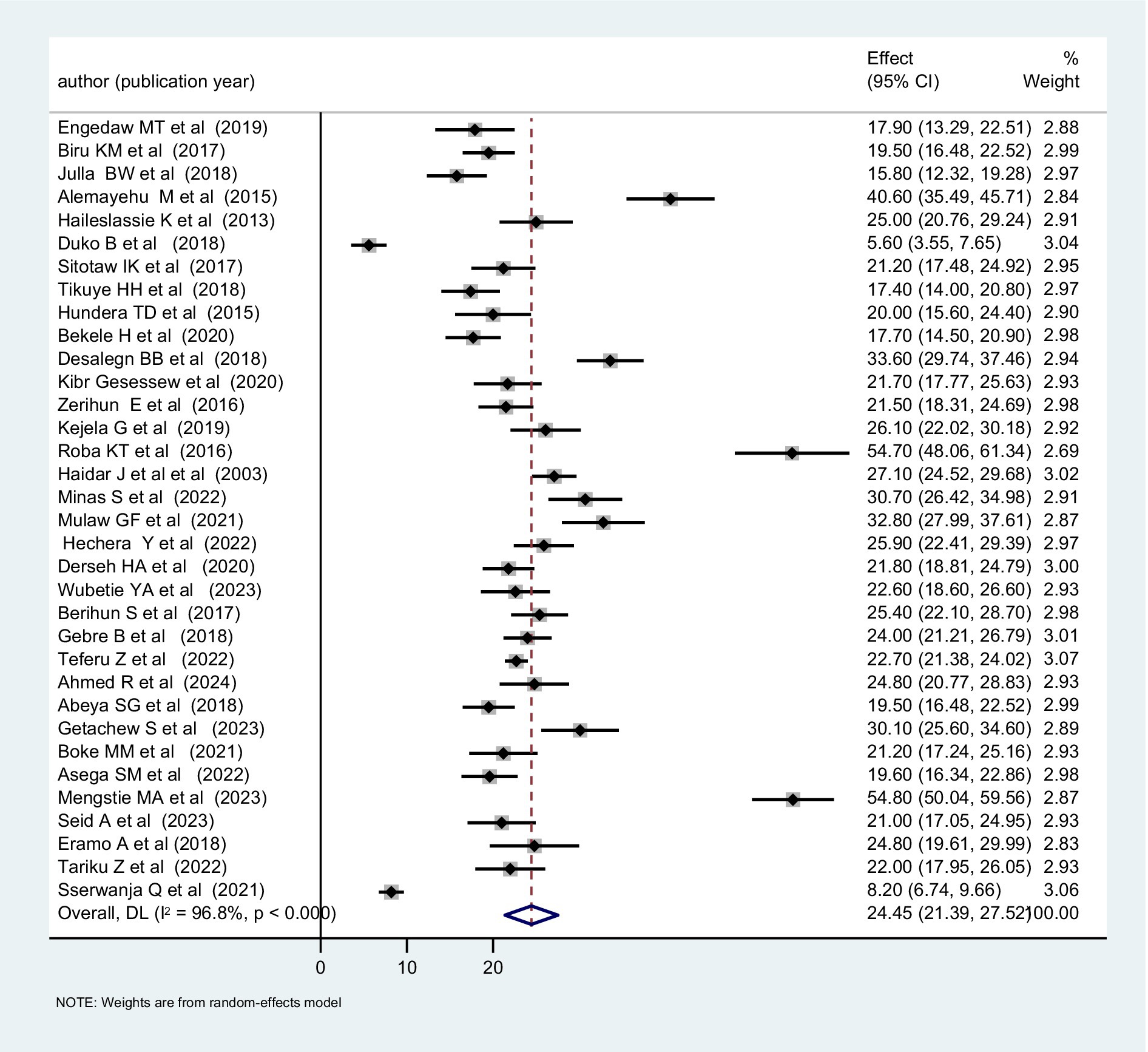
The occurrence of undernutrition among lactating women shows considerable variation across different regions and countries, with Sub-Saharan Africa (SSA) shouldering a disproportionate share of the burden. In this region, the prevalence of chronic undernutrition ranges from 10 to 20%, while acute undernutrition ranges from 20 to 25% (39). We analyzed primary studies conducted in Sub-Saharan Africa. Most of these studies were conducted since 2015 and reported a prevalence of undernutrition between 20 and 30% (Figure 2). The combined prevalence was 24.45% (Figure 3).
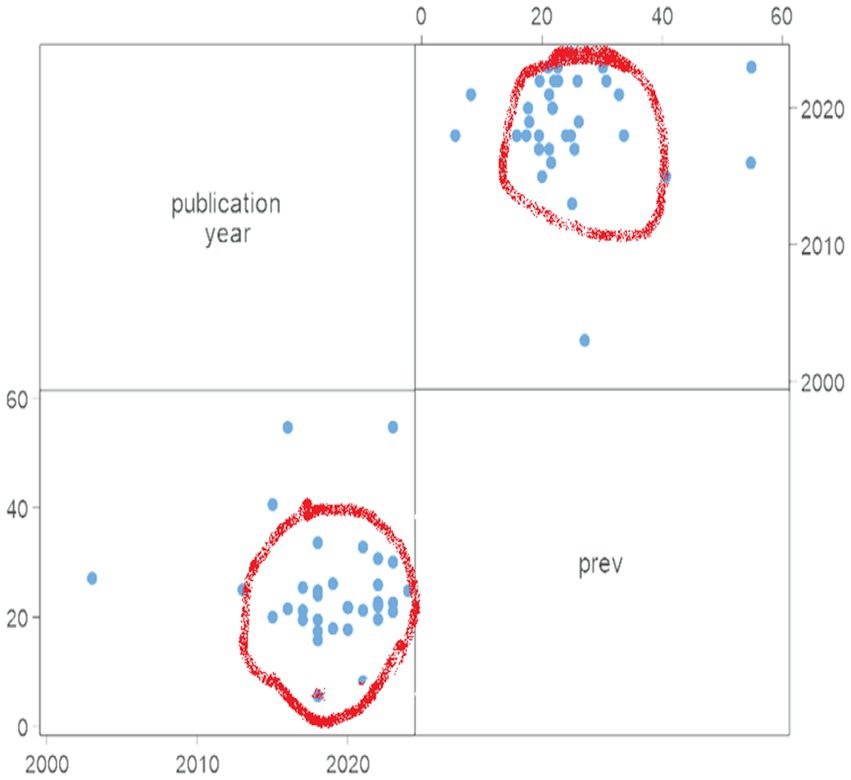
Figure 2. Characteristics of studies conducted in SSA to assess the undernutrition burden among lactating women: reported prevalence and publication year, 2024.
A study conducted in Uganda using DHS data evaluated the extent of undernutrition among lactating women and revealed that 8.2% of lactating women were underweight (40). Moreover, in Ethiopia, there are over 30 studies have been conducted to gage the extent of undernutrition among lactating women and the prevalence has been found to vary considerably, ranging from 5.6 to 54.8% (41, 42) (Table 1). Another systematic review conducted in Ethiopian also reported a pooled prevalence of underweight of 23.84% (43).

Table 1. Studies reported the burden and factors influencing underweight among lactating women in Sub-Saharan Africa, 2024.
However, most of the included studies were conducted in Ethiopia. There wasn’t evidence in the other countries found in SSA and the current combined prevalence could not show the burden in SSA. Therefore, to determine the burden of undernutrition in SSA, a meta-analysis should be conducted using the national DHS data of the member countries since studies included in this study only might not be representative.
3.3 Factors influencing underweight in lactating women
Factors contributing to undernutrition among lactating women are multifaceted and include socio-economic disparities, inadequate dietary intake, food insecurity, limited access to maternal healthcare services, and cultural practices (44, 45). Moreover, environmental factors such as climate change and natural disasters exacerbate food insecurity and further compound the risk of undernutrition among vulnerable populations (36).
A mini-review conducted in Ethiopia identified place of delivery, dietary diversity, income, food security, nutritional education programs, and antenatal care as determinants of undernutrition (46). Educational status emerged as a substantial factor for underweight among lactating women in a meta-analysis coxswained in Ethiopia (43).
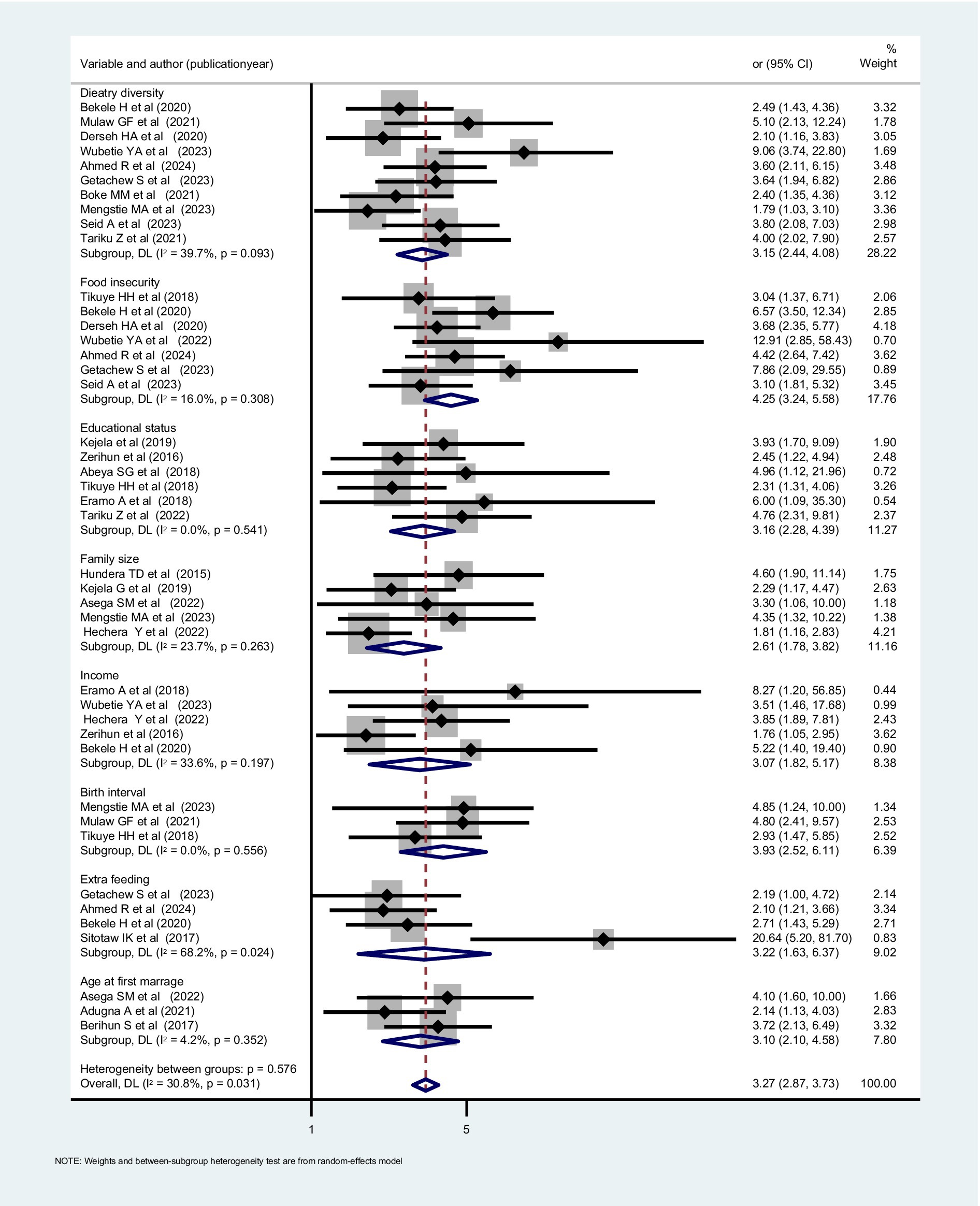
To reveal determinants that affect nutrition during lactation, different studies conducted in SSA were searched, and many factors that are described in the above paragraphs were scrutinized and included. In summary, the determinants are individual and community-level determinants (Table 1). In our review, the most frequently cited determinants included age at first marriage, dietary diversity score, educational status, family size, food insecurity, income, additional meals, and birth interval (Figure 4).
However, the factors mentioned above are identified from primary local studies, implying they may not fully capture the determinants of undernutrition in SSA. Almost all of the factors are reported from one nation, Ethiopia. Therefore, it is crucial to analyze individual and community-level determinants using comprehensive and representative population-based DHS data of SSA countries. This analysis should employ a multi-level approach, as it is a robust method for understanding the complex and interconnected determinants of undernutrition in SSA (47).
3.4 Prevalence and determinants of obesity among lactating women
A study conducted in 32 Sub-Saharan African countries, utilizing DHS data, revealed a pooled obesity prevalence of 6.6% among women. The lowest rate was observed in Madagascar, at 1.1%, while the highest was recorded in Lesotho, at 15.8%. Also, residency and wealth index are reported as determinants for obesity (48).
Another study using DHS data from 24 African countries found increasing obesity rates among urban women of reproductive age. Significant increases were observed across all countries, with notable trends in 17 nations. In Ghana, obesity rates boosted from 1993 to 2014, while Egypt recorded the highest commonness at 39% in 2014. Obesity rates doubled in Burkina Faso, Niger, Benin, Rwanda, Kenya, Ivory Coast, and Uganda and tripled in Malawi, Tanzania, Zambia, and Mali. Conversely, Madagascar and Ethiopia had the lowest obesity prevalence, ranging from 1 to 4% (49).
Furthermore, a separate study conducted in Tanzania documented the obesity prevalence among women, which stood at 9.1% in 2004. This prevalence has shown a consistent and gradual increase over time. Additionally, the study identified age, parity, and socioeconomic status as key determinants of obesity (50).
While studies have explored obesity among women in SSA, the lack of research on the prevalence and determinants of obesity specifically among lactating women in the region is a significant gap. Understanding and addressing obesity among lactating women in SSA, influenced by cultural perceptions, limited access to healthcare resources, and insufficient research focus, could have a profound impact. It has not received the same level of research attention as in other parts of the world (51).
Closing the gap in understanding and addressing obesity among lactating women in SSA requires interdisciplinary efforts involving healthcare professionals, policymakers, researchers, and community stakeholders. This includes promoting culturally sensitive healthcare practices, improving access to healthcare services, prioritizing maternal health and nutrition research, and implementing evidence-based interventions to support healthy weight management during the postpartum period. Furthermore, longitudinal large-scale studies should be conducted to assess the prevalence and determinants of obesity among lactating women in SSA. Addressing these factors can help mitigate the impact of obesity on maternal and child health outcomes in Africa.
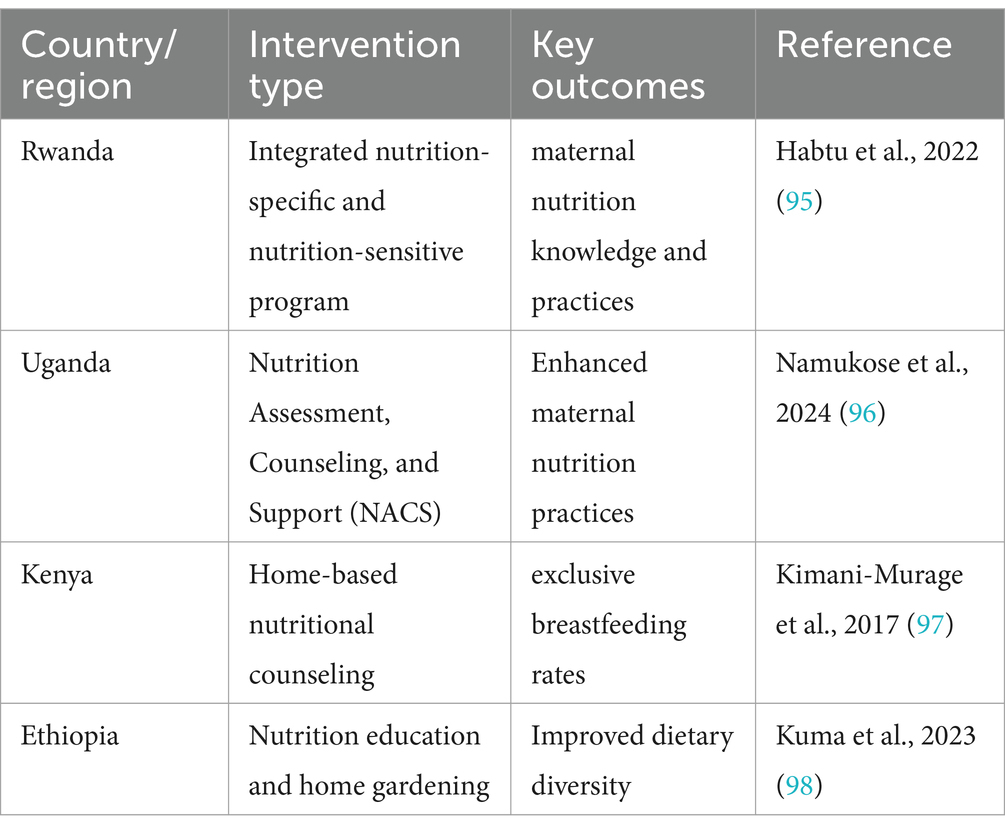
3.5 Interventional studies conducted in SSA
There were not many interventional studies in sub-Saharan Africa (SSA) that explicitly target obesity, overweight, and underweight among lactating women. Nonetheless, a number of observational studies provide light on the dietary difficulties this demographic faces and offer possible solutions.
According to a Ghanaian study, shorter risks of maternal obesity were linked to longer breastfeeding durations. The odds of being obese were significantly lower for women who breastfed for more than 18 months than for those who did not (52).
The results of observational research indicate that encouraging prolonged breastfeeding may help lower mother obesity, despite the paucity of direct interventional studies. Additionally, resolving the double burden of malnutrition among lactating women in SSA may require addressing socioeconomic variables at the individual and societal levels. There were studies conducted to the rural urban inequality of this problem among lactating women.
There were an additional interventional studies conducted in SSA which displayed on Table 2.
4 Discussion
This analytic review paper has aimed to assess the existing knowledge and identify research gaps on the spatial distributions, burden and factors of malnutrition among lactating women in SSA. Even though some studies have been conducted among reproductive-age women at the national level to describe the spatial distribution of malnutrition, no representative research has been conducted focusing on lactating women in SSA. However, investigating the spatial distribution of malnutrition helps to design new interventions and allocate resources, especially for Africa, where the malnutrition burden is high (53). This might be because the region is highly burdened with many communicable and non-communicable diseases. As a result, the concern given to lactating women has become less (54–56).
Although the exact pooled magnitude of underweight among lactating women in SSA remains unknown and most of the included studies were conducted in one country, based on our review, it spans a broad range of 5.6 to 54.8% and the pooled prevalence was 24.45%. This range and pooled prevalence notably exceeds the prevalence reported globally and in studies conducted in developed countries (57). The disparity in prevalence could be attributed to several factors unique to SSA, including disparities in healthcare service quality, lower utilization rates of antenatal and postnatal care, and limited access to nutritional counseling and education compared to developed countries (58, 59).
This review highlights numerous determinants identified by primary studies in SSA, encompassing individual and community-level factors. However, the meta-analysis-based review fails to identify the most pertinent and high-level determinants and their effects. Additionally, the extracted determinants are often sourced from local studies conducted in one country that may not represent broader populations. A population-based multinational study utilizing multilevel analysis of DHS data across SSA countries is warranted to address this gap.
Moreover, our literature review encompasses studies examining the prevalence and factors influencing obesity among women in SSA, revealing a range of 1.1 to 39%. This prevalence is comparable to that observed in high-income countries (60–62), presenting a significant concern and contributing to the DBM in the region. So far, no specific studies have been conducted among lactating women in sub-Saharan Africa. This could be because poverty, food insecurity, and undernutrition provide significant economic obstacles. These significant matters take precedence over obesity treatment, which is frequently perceived as a problem connected to income.
The burden of malnutrition in SSA has been well studied. However, the magnitude was high even compared to other developing countries in Asia, like Bangladesh (wasting of 10%) (63). This could be because a large number of Africans live below the poverty line, there is high food insecurity, and there is conflict in the region.
Despite this was review, it had limitations. Firstly, studies included in this review were mostly from one country which raises generalizability issue.
5 Conclusion
This study revealed the absence of evidences on the spatial distribution, burden and factors affecting underweight, obesity and overweight among lactating women in SSA. Moreover, this literature review underscores the critical need for focused attention on malnutrition (underweight and overweight/obesity) among lactating women in SSA. Despite the absence of representative studies in this vulnerable group, our findings reveal a wide prevalence range of underweight and obesity, indicative of significant challenges.
Factors contributing to this include healthcare disparities, limited access to nutritional resources, and the broader burden of disease in the region. Addressing these issues requires a multifaceted approach, including population-based multinational studies and utilization of data from sources like the DHS. Furthermore, the underexplored prevalence of obesity among lactating women underscores the urgent need for further research. This research is crucial to thoroughly understanding the extent of this issue and effectively addressing the problem in this vulnerable population. Identifying hotspot areas of malnutrition specifically among lactating women within sub-Saharan Africa through spatial distribution analysis is essential for allocating resources appropriately, addressing a critical concern in the region and helps to reduce morbidity and mortality. Therefore, to fill this gap studies using representative datasets like DHS data at SSA level is essential and future researchers should also give focus to lactating women nutrition since they are more vulnerable.
Author contributions
BG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMI, Body Mass Index; DBM, Double Burden of Malnutrition; DHS, Demographic and Health Surveys; SSA, Sub-Sahara Africa; WHO, World Health Organization.
References
1. Musimenta, N, and Onyango, R. Factors associated with malnutrition occurrence among children under 5 years in KIHENDA village HOIMA district. A cross-sectional study. SJ Pediatrics and Child Health Africa. (2024) 1:9. doi: 10.51168/yfancr93
2. Organization, W.H. Global nutrition monitoring framework: Operational guidance for tracking progress in meeting targets for 2025. WHO (2017).
3. Saunders, J, and Smith, T. Malnutrition: causes and consequences. Clin Med (Lond). (2010) 10:624–7. doi: 10.7861/clinmedicine.10-6-624
4. Organization, W.H. Global status report on noncommunicable diseases 2014. Geneva, Switzerland: World Health Organization (2014).
5. Lartey, A. Maternal and child nutrition in sub-Saharan Africa: challenges and interventions. Proc Nutr Soc. (2008) 67:105–8. doi: 10.1017/S0029665108006083
6. Black, RE, Allen, LH, Bhutta, ZA, Caulfield, LE, de Onis, M, Ezzati, M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
7. Girma, W., and Genebo, T., Determinants of nutritional status of women and children in Ethiopia. Calverton, Maryland, USA: ORC Macro (2002).
8. Organization, W.H. The double burden of malnutrition: Policy brief. Geneva, Switzerland: World Health Organization (2016).
9. Hossain, MI, Rahman, A, Uddin, MSG, and Zinia, FA. Double burden of malnutrition among women of reproductive age in Bangladesh: a comparative study of classical and Bayesian logistic regression approach. Food Sci Nutr. (2023) 11:1785–96. doi: 10.1002/fsn3.3209
10. Seifu, BL, Mare, KU, Legesse, BT, and Tebeje, TM. Double burden of malnutrition and associated factors among women of reproductive age in sub-Saharan Africa: a multilevel multinomial logistic regression analysis. BMJ Open. (2024) 14:e073447. doi: 10.1136/bmjopen-2023-073447
11. Alem, AZ, Yeshaw, Y, Liyew, AM, Tessema, ZT, Worku, MG, Tesema, GA, et al. Double burden of malnutrition and its associated factors among women in low and middle income countries: findings from 52 nationally representative data. BMC Public Health. (2023) 23:1479. doi: 10.1186/s12889-023-16045-4
12. Akombi, BJ, Chitekwe, S, Sahle, BW, and Renzaho, AMN. Estimating the double burden of malnutrition among 595,975 children in 65 low-and middle-income countries: a Meta-analysis of demographic and health surveys. Int J Environ Res Public Health. (2019) 16:2886. doi: 10.3390/ijerph16162886
13. Amugsi, DA, Dimbuene, ZT, and Kyobutungi, C. Correlates of the double burden of malnutrition among women: an analysis of cross sectional survey data from sub-Saharan Africa. BMJ Open. (2019) 9:e029545. doi: 10.1136/bmjopen-2019-029545
14. Nyanhanda, T, Mwanri, L, and Mude, W. Double burden of malnutrition: a population level comparative cross-sectional study across three sub-Saharan African countries-Malawi, Namibia and Zimbabwe. Int J Environ Res Public Health. (2023) 20:5860. doi: 10.3390/ijerph20105860
15. Okyere, J, Budu, E, Aboagye, RG, Seidu, AA, Ahinkorah, BO, and Yaya, S. Socioeconomic determinants of the double burden of malnutrition among women of reproductive age in sub-Saharan Africa: a cross-sectional study. Health Sci Rep. (2024) 7:e2071. doi: 10.1002/hsr2.2071
16. Alaba, OA, Chiwire, P, Siya, A, Saliu, OA, Nhakaniso, K, Nzeribe, E, et al. Socio-economic inequalities in the double burden of malnutrition among under-five children: evidence from 10 selected sub-Saharan African countries. Int J Environ Res Public Health. (2023) 20:5489. doi: 10.3390/ijerph20085489
17. Christian, AK, and Dake, FA. Profiling household double and triple burden of malnutrition in sub-Saharan Africa: prevalence and influencing household factors. Public Health Nutr. (2022) 25:1563–76. doi: 10.1017/S1368980021001750
18. Harper, A, Goudge, J, Chirwa, E, Rothberg, A, Sambu, W, and Mall, S. Dietary diversity, food insecurity and the double burden of malnutrition among children, adolescents and adults in South Africa: findings from a national survey. Front Public Health. (2022) 10:948090. doi: 10.3389/fpubh.2022.948090
19. Steyn, NP, and Nel, JH. Prevalence and determinants of the double burden of malnutrition with a focus on concurrent stunting and overweight/obesity in children and adolescents. Curr Nutr Rep. (2022) 11:437–56. doi: 10.1007/s13668-022-00417-0
20. Were, JM, Stranges, S, and Creed, IF. Fertility is a key predictor of the double burden of malnutrition among women of child-bearing age in sub-Saharan Africa. J Glob Health. (2020) 10:020423. doi: 10.7189/jogh.10.020423
21. Were, JM, Stranges, S, Wilk, P, Ali, S, Sharma, I, Vargas-Gonzalez, JC, et al. The double burden of malnutrition among women of reproductive age and preschool children in low-and middle-income countries: a scoping review and thematic analysis of literature. Nutrition. (2023) 111:112053. doi: 10.1016/j.nut.2023.112053
22. Rahman, A, and Harding, A. Small area estimation and microsimulation modeling. London, England and Wales: Chapman and Hall/CRC (2016).
23. Fabro, AYR. Spatial distribution of nitrate health risk associated with groundwater use as drinking water in Merida. Mexico Applied Geography. (2015) 65:49–57. doi: 10.1016/j.apgeog.2015.10.004
24. Rahman, A, Harding, A, Tanton, R, and Liu, S. Simulating the characteristics of populations at the small area level: new validation techniques for a spatial microsimulation model in Australia. Computational Statistics & Data Analysis. (2013) 57:149–65. doi: 10.1016/j.csda.2012.06.018
25. Murigi, MW. Factors influencing spatial distribution of small and medium size enterprises within Nairobi County, Kenya. Nairobi, Kenya: University of Nairobi (2016).
26. Tusa, BS, Weldesenbet, AB, and Kebede, SA. Spatial distribution and associated factors of underweight in Ethiopia: an analysis of Ethiopian demographic and health survey, 2016. PLoS One. (2020) 15:e0242744. doi: 10.1371/journal.pone.0242744
27. Kassie Tesema, A, Liyew, AM, Alem, AZ, Yeshaw, Y, Tesema, GA, and Teshale, AB. Spatial distribution and determinants of undernutrition among reproductive age women of Ethiopia: a multilevel analysis. PLoS One. (2021) 16:e0257664. doi: 10.1371/journal.pone.0257664
28. Kibret, KT, Chojenta, C, D'Arcy, E, and Loxton, D. Spatial distribution and determinant factors of anaemia among women of reproductive age in Ethiopia: a multilevel and spatial analysis. BMJ Open. (2019) 9:e027276. doi: 10.1136/bmjopen-2018-027276
29. Getnet, M, Sisay, WS, and Alem, AZ. Spatial distribution and associated factors of co-occurrence of overweight/obesity and Anemia among women in the reproductive age in sub-Saharan Africa: a multilevel analysis, DHS 2016-2021. PLoS One. (2024) 19:e0299519. doi: 10.1371/journal.pone.0299519
30. Nyarko, SH, Bitew, F, and Amu, H. Spatial and temporal inequalities in undernutrition among non-pregnant women in Ghana: a multilevel analysis. Spatial Demography. (2022) 10:193–207. doi: 10.1007/s40980-020-00074-3
31. Kandala, N-B, and Stranges, S. Geographic variation of overweight and obesity among women in Nigeria: a case for nutritional transition in sub-Saharan Africa. PLoS One. (2014) 9:e101103. doi: 10.1371/journal.pone.0101103
32. Organization, W.H. The state of food security and nutrition in the world 2019: safeguarding against economic slowdowns and downturns, vol. 2019. Rome: FAO (2019).
33. Kennedy, E, Tessema, M, Hailu, T, Zerfu, D, Belay, A, Ayana, G, et al. Multisector nutrition program governance and implementation in Ethiopia: opportunities and challenges. Food Nutr Bull. (2015) 36:534–48. doi: 10.1177/0379572115611768
34. Organization, W.H. Nutrition of women in the preconception period, during pregnancy and the breastfeeding period. Provisional Agenda Item. (2012) 13:A65.
35. Desalegn, BB, Lambert, C, Riedel, S, Negese, T, and Biesalski, HK. Ethiopian orthodox fasting and lactating mothers: longitudinal study on dietary pattern and nutritional status in rural Tigray, Ethiopia. Int J Environ Res Public Health. (2018) 15:1767. doi: 10.3390/ijerph15081767
36. Canton, H. Food and agriculture organization of the United Nations—FAO In: The Europa directory of international organizations 2021. edited by Europa Publications London, England and Wales: Routledge (2021). 297–305.
37. Rahman, A. Geospatial, socioeconomic, demographic and health determinants of childhood mortality in Bangladesh. Demography India: Population Society Econ Environ Interactions. (2019) 48:74–85.
38. Lindsay, K, Gibney, E, and McAuliffe, F. Maternal nutrition among women from sub-Saharan Africa, with a focus on Nigeria, and potential implications for pregnancy outcomes among immigrant populations in developed countries. J Hum Nutr Diet. (2012) 25:534–46. doi: 10.1111/j.1365-277X.2012.01253.x
39. Tikuye, HH, Gebremedhin, S, Mesfin, A, and Whiting, S. Prevalence and factors associated with undernutrition among exclusively breastfeeding women in Arba Minch Zuria District, southern Ethiopia: a cross-sectional community-based study. Ethiop J Health Sci. (2019) 29:913–922. doi: 10.4314/ejhs.v29i1.13
40. Sserwanja, Q, Kawuki, J, Mutisya, LM, Musaba, MW, Kagwisagye, M, Kato, IA, et al. Underweight and associated factors among lactating women in Uganda: evidence from the Uganda demographic health survey 2016. Health Sci Reports. (2021) 4:e356. doi: 10.1002/hsr2.356
41. Duko, B, Gebrie, M, and Hailu, D. Factors associated with nutritional status among lactating mothers at Shashemene Woreda, west Arsi zone, Oromia, Ethiopia: a comparative cross-sectional study. Int J Nutrition Metabolism. (2018) 10:37–46. doi: 10.5897/IJNAM2018.0243
42. Roba, KT. Anemia and undernutrition among children aged 6–23 months in two agroecological zones of rural Ethiopia. Pediatric Health, Med Therapeutics. (2016) 7:131–40. doi: 10.2147/PHMT.S109574
43. Girma, B, Nigussie, J, Molla, A, and Mareg, M. Under-nutrition and associated factors among lactating mothers in Ethiopia: a systematic review and Meta-analysis. Matern Child Health J. (2022) 26:2210–20. doi: 10.1007/s10995-022-03467-6
44. Nguyen, PH, Scott, S, Avula, R, Tran, LM, and Menon, P. Trends and drivers of change in the prevalence of anaemia among 1 million women and children in India, 2006 to 2016. BMJ Glob Health. (2018) 3:e001010. doi: 10.1136/bmjgh-2018-001010
45. Black, RE, Victora, CG, Walker, SP, Bhutta, ZA, Christian, P, de Onis, M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
46. Sserwanja, Q, and Kawuki, J. Prevalence of underweight and associated factors among lactating women in Ethiopia: a mini-review. J Adv Med Med Res. (2020) 32:1–9. doi: 10.9734/jammr/2020/v32i830459
47. Rahman, A. Estimating small area health-related characteristics of populations: a methodological review. Geospatial. Health. (2017) 12:3–14. doi: 10.4081/gh.2017.495
48. Neupane, S, KC, P, and Doku, DT. Overweight and obesity among women: analysis of demographic and health survey data from 32 sub-Saharan African countries. BMC Public Health. (2015) 16:1–9. doi: 10.1186/s12889-016-2698-5
49. Amugsi, DA, Dimbuene, ZT, Mberu, B, Muthuri, S, and Ezeh, AC. Prevalence and time trends in overweight and obesity among urban women: an analysis of demographic and health surveys data from 24 African countries, 1991–2014. BMJ Open. (2017) 7:e017344. doi: 10.1136/bmjopen-2017-017344
50. Villamor, E, Msamanga, G, Urassa, W, Petraro, P, Spiegelman, D, Hunter, DJ, et al. Trends in obesity, underweight, and wasting among women attending prenatal clinics in urban Tanzania, 1995–2004. Am J Clin Nutr. (2006) 83:1387–94. doi: 10.1093/ajcn/83.6.1387
51. Hu, FB. Overweight and obesity in women: health risks and consequences. J Women's Health. (2003) 12:163–72. doi: 10.1089/154099903321576565
52. Tuoyire, DA, and Tampah-Naah, AM. Association of breastfeeding duration with overweight and obesity among women in Ghana. Front Global Women's Health. (2024) 5:1251849. doi: 10.3389/fgwh.2024.1251849
53. Nel, JH, and Steyn, NP. The nutrition transition and the double burden of malnutrition in sub-Saharan African countries: how do these countries compare with the recommended lancet commission global diet? Int J Environ Res Public Health. (2022) 19:16791. doi: 10.3390/ijerph192416791
54. Gouda, HN, Charlson, F, Sorsdahl, K, Ahmadzada, S, Ferrari, AJ, Erskine, H, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the global burden of disease study 2017. Lancet Glob Health. (2019) 7:e1375–87. doi: 10.1016/S2214-109X(19)30374-2
55. Bigna, JJ, and Noubiap, JJ. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob Health. (2019) 7:e1295–6. doi: 10.1016/S2214-109X(19)30370-5
56. Akinwusi, PO. Communicable disease-related sudden death in the 21st century in Nigeria. Infection Drug Resistance. (2013) 6:125–32. doi: 10.2147/IDR.S47959
57. Shrimpton, R, and Rokx, C. The double burden of malnutrition. A review of global evidence. Washington, DC: World Bank (2012).
58. Eshetu, HB, Aragaw, FM, Negash, WD, Belachew, TB, Asmamaw, DB, Tareke, AA, et al. Assessing postnatal care for newborns in sub-Saharan Africa: a multinational analysis. PLoS One. (2024) 19:e0298459. doi: 10.1371/journal.pone.0298459
59. Alemayehu, M, Medhanyie, AA, and Mulugeta, A. A review of evidence on barriers to and facilitators of the utilization of reproductive, maternal and neonatal health services among pastoralist communities in sub-Saharan Africa. Ethiop J Heal Dev. (2018) 1021–6790.
60. McPherson, K. Reducing the global prevalence of overweight and obesity. Lancet. (2014) 384:728–30. doi: 10.1016/S0140-6736(14)60767-4
61. Swinburn, B, Hovmand, P, Waterlander, W, and Allender, S. The global syndemic of obesity, undernutrition, and climate change. Clin Obesity Adults Children. (2022):409–27. doi: 10.1002/9781119695257.ch31
62. Abarca-Gómez, L, Abdeen, ZA, Hamid, ZA, Abu-Rmeileh, NM, Acosta-Cazares, B, Acuin, C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
63. Rahman, A, Chowdhury, S, and Hossain, D. Acute malnutrition in Bangladeshi children: levels and determinants. Asia Pac J Public Health. (2009) 21:294–302. doi: 10.1177/1010539509335399
64. Engidaw, MT. Chronic energy deficiency and its associated factors among lactating women in Debre Tabor general hospital, northcentral Ethiopia. J Family Med Health Care. (2019) 5:1–7. doi: 10.11648/j.jfmhc.20190501.11
65. Julla, BW, Haile, A, Ayana, G, Eshetu, S, Kuche, D, and Asefa, T. Chronic energy deficiency and associated factors among lactating mothers (15-49 years old) in Offa Woreda, Wolayita zone, SNNPRs. Ethiopia World Scientific Res. (2018) 5:13–23. doi: 10.20448/journal.510.2018.51.13.23
66. Alemayehu, M, Argaw, A, and Mariam, AG. Factors associated with malnutrition among lactating women in subsistence farming households from Dedo and Seqa-Chekorsa districts, Jimma zone, 2014. Develop Country Stud. (2015) 5:117–8.
67. Haileslassie, K, Mulugeta, A, and Girma, M. Feeding practices, nutritional status and associated factors of lactating women in Samre Woreda, south eastern zone of Tigray. Ethiopia Nutrition J. (2013) 12:1–11. doi: 10.1186/1475-2891-12-28
68. Sitotaw, IK, Hailesslasie, K, and Adama, Y. Comparison of nutritional status and associated factors of lactating women between lowland and highland communities of district Raya, Alamata, southern Tigiray. BMC Nutrit. (2017) 3:1–12. doi: 10.1186/s40795-017-0179-6
69. Biru, K, Jima, A, and Abeya, S. Prevalence of chronic energy malnutrition and maternal health service utilizations among lactating mothers. Eastern Ethiopia: Walsh Medical Media (2017).
70. Hundera, TD. Nutritional status and associated factors among lactating mothers in Nekemte referral hospital and health centers. Ethiopia Int J Nutr Food Sci. (2015) 4:216–22.
71. Bekele, H, Jima, GH, and Regesu, AH. Undernutrition and associated factors among lactating women: community-based cross-sectional study in Moyale District, Borena zone, Southern Ethiopia. Advan Public Heal. (2020) 2020:1–10. doi: 10.1155/2020/4367145
72. Gesessew, K. Nutritional status and associated drivers of food choice among lactating women in Debre Birhan town, North Shoa zone, Amhara region, Ethiopia: a community based cross-sectional study. Int J Nutrition Metabolism. (2020) 12:16–24. doi: 10.5897/IJNAM2020.0268
73. Zerihun, E, Egata, G, and Mesfin, F. Under nutrition and its associated factors among lactating mothers in rural ambo district, west Shewa zone, Oromia region, Ethiopia. East African J Health Biomed Sci. (2016) 1:39–48.
74. Kejela, G., Under nutrition and associated factors among lactating mothers in southern Ethiopia: Institution based cross-sectional study. (2019).
75. Roba, KT, O'Connor, TP, Belachew, T, and O'Brien, NM. Seasonal variation in nutritional status and anemia among lactating mothers in two agro-ecological zones of rural Ethiopia: a longitudinal study. Nutrition. (2015) 31:1213–8. doi: 10.1016/j.nut.2015.03.007
76. Haidar, J, Muroki, NM, Omwega, AM, and Ayana, G. Malnutrition and iron deficiency anaemia in lactating women in urban slum communities from Addis Ababa, Ethiopia. East Afr Med J. (2003) 80:191–4. doi: 10.4314/eamj.v80i4.8640
77. Minas, S, Ayele, BH, Sisay, M, and Fage, SG. Undernutrition among khat-chewer and non-chewer lactating women in chiro district, eastern Ethiopia: comparative cross-sectional study. SAGE Open Med. (2022) 10:20503121221100143. doi: 10.1177/20503121221100143
78. Mulaw, GF, Mare, KU, and Anbesu, EW. Nearly one-third of lactating mothers are suffering from undernutrition in pastoral community, Afar region, Ethiopia: community-based cross-sectional study. PLoS One. (2021) 16:e0254075. doi: 10.1371/journal.pone.0254075
79. Hechera, Y, and Dona, A. Prevalence of undernutrition and its associated factors among lactating women in the Shebedino District, Sidama regional state, Ethiopia. Inquiry: J Health Care Organization, Provision, and Financing. (2022) 59:00469580221087883. doi: 10.1177/00469580221087883
80. Almaw Derseh, H, Zeleke, LB, Endalifer, ML, Muhammad, EA, and Derso, T. Undernutrition and associated factors among lactating mothers in Dega Damot Woreda, Northwest Ethiopia. J Nutrition Metabolism. (2020) 2020:4627278. doi: 10.1155/2020/4627278
81. Wubetie, BY, and Mekonen, TK. Undernutrition and associated factors among lactating mothers in rural Yilmana Densa District, Northwest Ethiopia: a community-based cross-sectional study. Food Sci Nutr. (2023) 11:1383–93. doi: 10.1002/fsn3.3176
82. Berihun, S, Kassa, GM, and Teshome, M. Factors associated with underweight among lactating women in Womberma woreda, Northwest Ethiopia; a cross-sectional study. BMC Nutrit. (2017) 3:1–7.
83. Gebre, B, Biadgilign, S, Taddese, Z, Legesse, T, and Letebo, M. Determinants of malnutrition among pregnant and lactating women under humanitarian setting in Ethiopia. BMC Nutrit. (2018) 4:1–8. doi: 10.1186/s40795-018-0222-2
84. Teferu, Z, Tekalegn, Y, Sahiledengle, B, Zenbaba, D, Desta, F, Seyoum, K, et al. Individual and community-level determinants of underweight among lactating mothers in Ethiopia: a multilevel analysis. PLoS One. (2022) 17:e0267821. doi: 10.1371/journal.pone.0267821
85. Ahmed, R, Ejeta Chibsa, S, Hussen, MA, Bayisa, K, Tefera Kefeni, B, Gezimu, W, et al. Undernutrition among exclusive breastfeeding mothers and its associated factors in Southwest Ethiopia: a community-based study. Women Health. (2024) 20:17455057241231478. doi: 10.1177/17455057241231478
86. Adugna, A., and Degu, A., Predictors of underweight among lactating mothers in Dangila District, North West Ethiopia. (2021).
87. Abeya, S, Biru, K, and Jima, A. Factors associated with underweight among lactating mothers in Adama district, Oromia region, Ethiopia. J Orthop Bone Res. (2018) 1:101.
88. Getachew, S, Belayneh, F, Lejore, E, Ayele, A, and Belayneh, T. Malnutrition and associated factors among lactating women in Dale District, Sidama, Ethiopia. J Health, Med Nurs. (2023) 9:64–78. doi: 10.47604/jhmn.1989
89. Boke, MM, Yesuf, A, and Gutema, BT. Prevalence of undernutrition and associated factors among lactating mothers of Angecha District, Kembata Tembaro zone, southern Ethiopia. J Nutrition Metabolism. (2021) 2021:1–8. doi: 10.1155/2021/6691982
90. Sewalem, M.A., Assesment of Nutritional Status and Associated Factors Among Lactating Mothers in Burie Town, North West Ethiopa. (2022).
91. Mengstie, MA, Worke, MD, Belay, Y, Chekol Abebe, E, Asmamaw Dejenie, T, Abdu Seid, M, et al. Undernutrition and associated factors among internally displaced lactating mothers in Sekota camps, northern Ethiopia: a cross-sectional study. Front Nutr. (2023) 10:1108233. doi: 10.3389/fnut.2023.1108233
92. Seid, A, and Cherie, HA. Dietary diversity, nutritional status and associated factors among lactating mothers visiting government health facilities at Dessie town, Amhara region, Ethiopia. PLoS One. (2022) 17:e0263957. doi: 10.1371/journal.pone.0263957
93. Eramo, A. Determinants of underweight among lactating mothers in Anlemo woreda, Hadiya Zone, Southern Ethiopia. Addis Ababa, Ethiopia: Addis Ababa University (2018).
94. Tariku, Z, Tefera, B, Samuel, S, Derese, T, Markos, M, Dessu, S, et al. Nutritional status and associated factors among lactating women in Dire Dawa. Ethiopia J Obstet Gynaecol Res. (2022) 48:1183–92. doi: 10.1111/jog.15198
95. Subandoro, A.W., Holschneider, S., and Ruel-Bergeron, J., Operationalizing multisectoral nutrition programs to accelerate progress: A nutrition governance perspective. World Bank Group (2021).
96. Namukose, S, Maina, GW, Kiwanuka, SN, and Makumbi, FE. Effect of nutrition assessment, counselling and support integration on mother-infant nutritional status, practices and health in Tororo and Butaleja districts, Uganda: a comparative non-equivalent quasi-experimental study. J Health Popul Nutr. (2024) 43:84. doi: 10.1186/s41043-024-00559-7
97. Kimani-Murage, EW, Griffiths, PL, Wekesah, FM, Wanjohi, M, Muhia, N, Muriuki, P, et al. Effectiveness of home-based nutritional counselling and support on exclusive breastfeeding in urban poor settings in Nairobi: a cluster randomized controlled trial. Glob Health. (2017) 13:1–16. doi: 10.1186/s12992-017-0314-9
Keywords: sub-Saharan Africa, lactating mothers, spatial distribution analysis, underweight, overweight/obesity
Citation: Girma B and Rahman A (2025) Malnutrition among lactating women in sub-Saharan Africa: an analytic review of spatial distribution, burden and determinants. Front. Public Health. 13:1564581. doi: 10.3389/fpubh.2025.1564581
Edited by:
Margarida Liz Martins, Coimbra School of Health Technology, PortugalReviewed by:
Masresha Leta, Haramaya University, EthiopiaGayathri Abeywickrama, University of Winchester, United Kingdom
Copyright © 2025 Girma and Rahman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bekahegn Girma, YmVrYWhlZ25nQGR1LmVkdS5ldA==
 Bekahegn Girma
Bekahegn Girma Azizur Rahman
Azizur Rahman