- Department of Psychiatry, The First Hospital of Hebei Medical University, Shijiazhuang, Hebei, China
Objective: To investigate the incidence and influencing factors of non-suicidal self-injury (NSSI) among middle school students in a city within Hebei Province.
Methods: A total of 11,321 students from grades one to three from two middle schools in Dingzhou, Hebei Province, were randomly selected. Socio-demographic data, mental disorders, coping styles, and experiences of childhood abuse were collected.
Results: 10,982 students finally included in the statistical analysis. We found that the detection rate of NSSI in the past year was 11.6%. Comparatively, the NSSI group and the non-NSSI group revealed significant discrepancies in coping styles, childhood abuse, and mental disorders. Factors protective against NSSI included living with parents, a problem-oriented coping style, and a preference for participating in extracurricular activities (OR = 0.729, 0.966, 0.815). NSSI's risk factors included frequent parental quarrels, interpersonal tension and sensitivity, depression, emotion-oriented coping styles, and childhood emotional abuse (OR = 1.322, 1.045, 1.141, 1.023, 1.137).
Conclusion: The detection rate of NSSI within the past year in the city of Hebei stands at 11.6%. Considering the recognized risk and protective factors for NSSI, the possibility of NSSI may be decreased through the promotion of a harmonious home environment, encouraging positive emotional interaction, and the facilitation of greater involvement in extracurricular activities.
Background
Non-suicidal self-injury (NSSI) refers to the deliberate, self-inflicted harm to one's own body without suicidal intent (1). Common forms of this behavior include scratching, beating, and burning oneself (2). NSSI is prevalently seen during adolescence, especially among female adolescents. Research indicates that the incidence of NSSI among international adolescents is 17.2% (3), while the detection rate among Chinese middle school students is 22.37% (4). Many studies have shown that NSSI occurs much earlier than attempted suicide and it is a strong predictor of attempted suicide or suicidal behavior (5, 6). The relationship between NSSI characteristics (such as cutting, burning, etc.) or high-frequency NSSI behaviors and suicide attempts is inseparable (6). These factors can significantly shorten the time from NSSI to attempted suicide. This finding is more obvious among girls and adolescents with depressive symptoms (5). The escalating issue of adolescent mental health problems is becoming a significant public health concern. NSSI not only directly endangers the physical health of teenagers and aggravates their emotional problems, but also may increase the risk of teenagers dropping out of school or even committing suicide (7). Recognizing NSSI behavior in adolescents and implementing intervention strategies for risk factors could potentially reduce the frequency of harmful outcomes, such as suicidal behaviors.
Prior research has demonstrated that NSSI in adolescents is associated with numerous factors. A troubled parent-child relationship is linked closely to NSSI. This relationship includes factors such as domestic violence or abuse, parental divorce or separation, limited parent-child contact, and a lack of family support, all of which are critical risk factors for NSSI (8, 9). Family factors play an important role in the early stage of teenagers' psychological development. Family also plays an important role in cultivating teenagers' social skills and emotional development, and these factors have a significant impact on NSSI (10). Xue et al. (9) found in their research that high family function is a strong protective factor for NSSI. Effective family communication can effectively prevent the occurrence of NSSI. On the contrary, dysfunctional families can increase the risk of NSSI by 21% (10). Additionally, strained interpersonal relationships, adverse childhood experiences, and symptoms of anxiety and depression can independently forecast the incidence of NSSI among adolescents (1, 2).
Wang et al. (11) discovered that adolescents who suffered childhood abuse were more likely to display NSSI behaviors compared to their healthier counterparts. Childhood abuse is an independent risk factor for NSSI in adolescents with a depressive disorder, with emotional abuse and emotional neglect being particularly impactful (1). Adverse childhood experiences can inflict short-term psychological and physical harm on individuals, and these effects can persist throughout their lifetimes (12). Prolonged adverse events during adolescence may trigger deviations in the developmental trajectory, impacting cognitive function development and personality trait formation (13), which subsequently increases the risk of NSSI in adolescents.
Coping style refers to the varying cognitive and behavioral efforts individuals employ to manage internal or external demands that exceed their capacities (14). Depending on their distinct functions and expression modes, coping styles can be categorized into problem-oriented and emotion-oriented styles. Prior research has indicated that emotion-oriented coping styles, typified by patience and evasion, can lead adolescents to choose damaging behaviors such as self-harm to evade reality (15). The act of self-harm might, in itself, represent a maladaptive coping style (16)—an improperly regulated method of dealing with negative emotions when more effective strategies are absent (17).
With the rise in detection rates of NSSI among adolescents, increased attention has been given by parents, medical professionals, and schools. However, there is a lack of large-sample screenings focusing on NSSI detection rates and influential factors among middle school students in Hebei Province. Consequently, this study aimed to estimate the NSSI detection rate among middle school students in Hebei Province via large-sample screening and to explore the impacts of mental disorders, coping styles, and childhood abuse on NSSI. The results of this study can provide a theoretical framework for preventing NSSI among adolescents.
Methods
This study conducted a random selection of two middle schools in Dingzhou City, Hebei Province, and administered screenings to all students in these schools from May 2024 to June 2024. A total of 11,321 students were screened, but 52 of them declined to participate. We collected a total of 11,269 questionnaires, producing a recovery rate of 97.5%. After dismissing 287 invalid questionnaires, we included 10,982 valid questionnaires in the final statistical analysis.
The screening tool for this study is the information network evaluation system, designed by the Hebei Mental Health Technology Innovation Center. Students were required to complete the questionnaire by inputting their account number and password on the website. Upon logging in, students needed to provide informed consent before proceeding with the scale. If they disagreed, they would be considered to have withdrawn from participation in the screening.
In this study, a custom-made general information questionnaire was used to gather data on the subjects' gender, age, grade, parents' education level, whether they live with their parents, the frequency of their parents quarreling, and their regular participation in extracurricular activities.
Ottawa self-injury inventory (OSI)
The OSI is employed to determine if the subject had engaged in NSSI within the past year, as well as the frequency, intent, location, and methods of NSSI implementation (18). This scale has commendable reliability and validity in evaluating the NSSI of adolescents (19). This study adopted the Chinese revised version of OSI, and the Cronbach's was 0.849.
Coping style scale for middle school students (CSS)
CSS is used to assess how subjects typically respond to difficulties or challenges (20). It is divided into two subscales: one is the problem-oriented response subscale, and the other is the emotion-oriented response subscale. In this study, the Cronbach's α of this scale was 0.784.
Mental health scale for middle school students (MSSMHS)
MSSMHS is used to gauge the comprehensive mental health level of middle school students (21). In this study, the Cronbach's α was 0.966.
Childhood trauma questionnaire short form (CTQ-SF)
CTQ-SF, a self-assessment tool, is used to evaluate experiences of abuse (22). It is one of the most frequently utilized instruments to measure childhood abuse and neglect. This scale has commendable reliability and validity in evaluating the childhood abuse of adolescents (23). In this study, the Cronbach's α was 0.717.
The investigators included staff from the Mental Health Center of the First Hospital of Hebei Medical University and high school teachers from the schools involved in the screening. The investigators received uniform training before the screening, with uniform guidelines in place to ensure consistency in the screening results. During the screening process, students were instructed to think independently and fill out the Symptom Self-Assessment Scale according to the provided guidance. Upon completion, the students clicked the submit button. After the screening, the completed scales submitted by the students were reviewed, and questionnaires with obvious errors or incomplete answers were discarded.
The statistical analysis was conducted using SPSS 25.0 software. The Chi-square test was employed for the comparison of categorized data, while the two-independent sample t-test was applied for the comparison of continuous variables. To analyze the influencing factors of NSSI, logistic regression analysis was utilized, with a P value of < 0.05 indicating statistical significance.
This study received approval from the Clinical Research Ethics Committee at the First Hospital of Hebei Medical University [Approval number: (2024) Research Review No. (091)].The authors confirm that all research was performed in accordance with relevant guidelines/regulations.
Consent statement: Verbal and written consent was obtained from adolescent and parents/caregivers.
Results
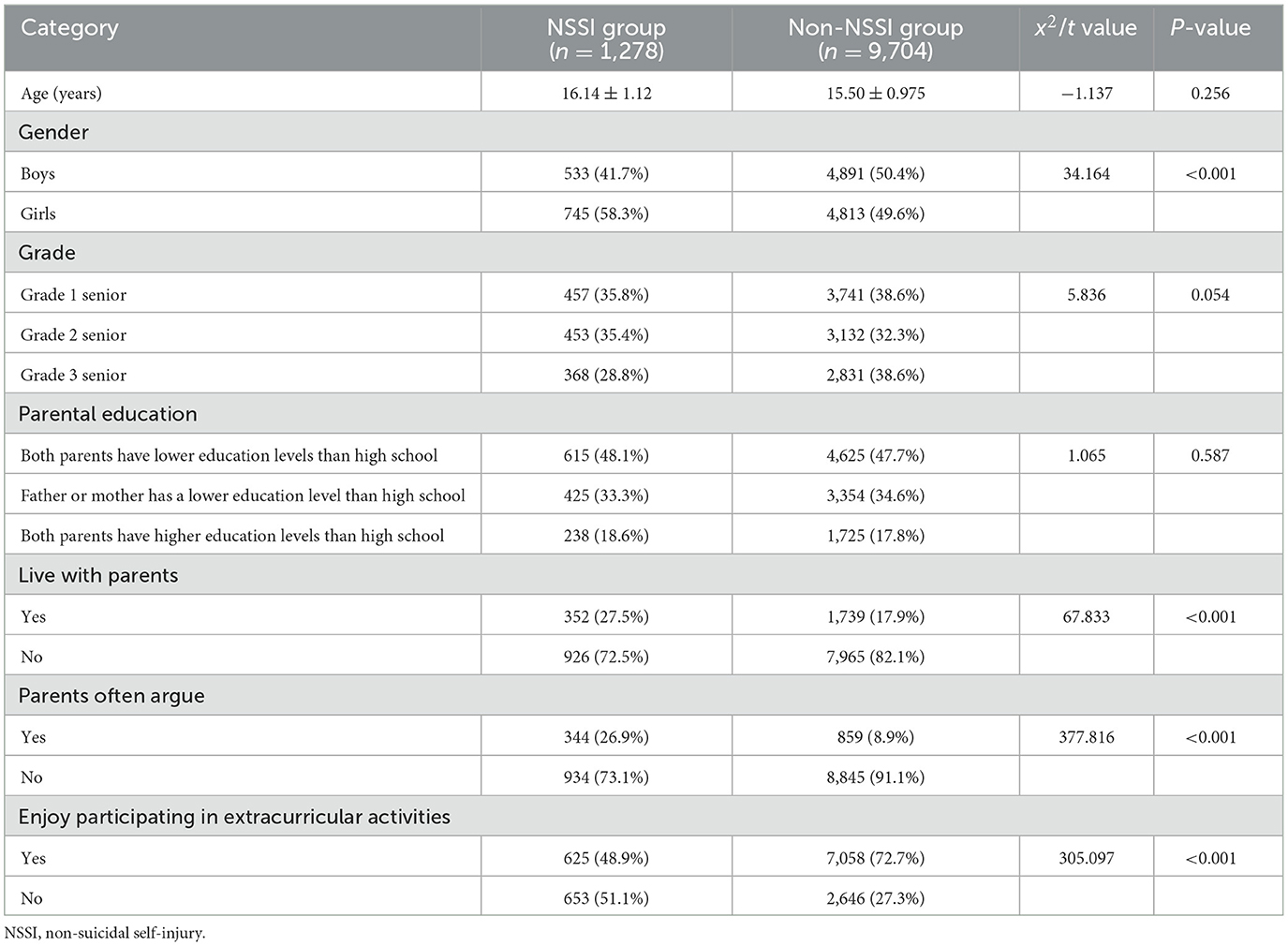
A total of 11,321 middle school students were screened in this study. Among them, 52 did not sign the informed consent form and did not participate in the screening. 287 questionnaires with incomplete data were excluded, and finally 10,982 people were included in the statistical analysis. According to OSI, if one subject showed any of the self-harm patterns once or more, it is determined to have NSSI behavior (24). Students screened out with NSSI behaviors were classified as the NSSI group (n = 1,278), and the remaining students were classified as the non-NSSI group (n = 9,704). It was found that the detection rate of NSSI in the past year was 11.6%. The average age of the NSSI group was 16.14 years old, and that of the non-NSSI group was 15.50 years old. Among the adolescents with NSSI, there were 745 girls and 533 boys. The number of girls was significantly higher than that of boys (χ2 = 34.164, P < 0.001) (Table 1).
Female adolescents primarily self-injured through scratches/abrasions and bites/pinches, while male adolescents' primary methods were scratches/bruises and blows, mainly focusing on arms, fingers/hands, and wrists. The main motivators behind NSSI were to release unbearable tension, discharge anger, alleviate sadness, and self-punishment. A statistical comparison revealed significant differences between the NSSI and the non-NSSI groups in terms of factors such as living with parents, frequency of parents' arguments, and affinity toward extracurricular activities (P < 0.001). However, there were no significant disparities regarding age, grade, and parental education levels between the two groups (Table 1).
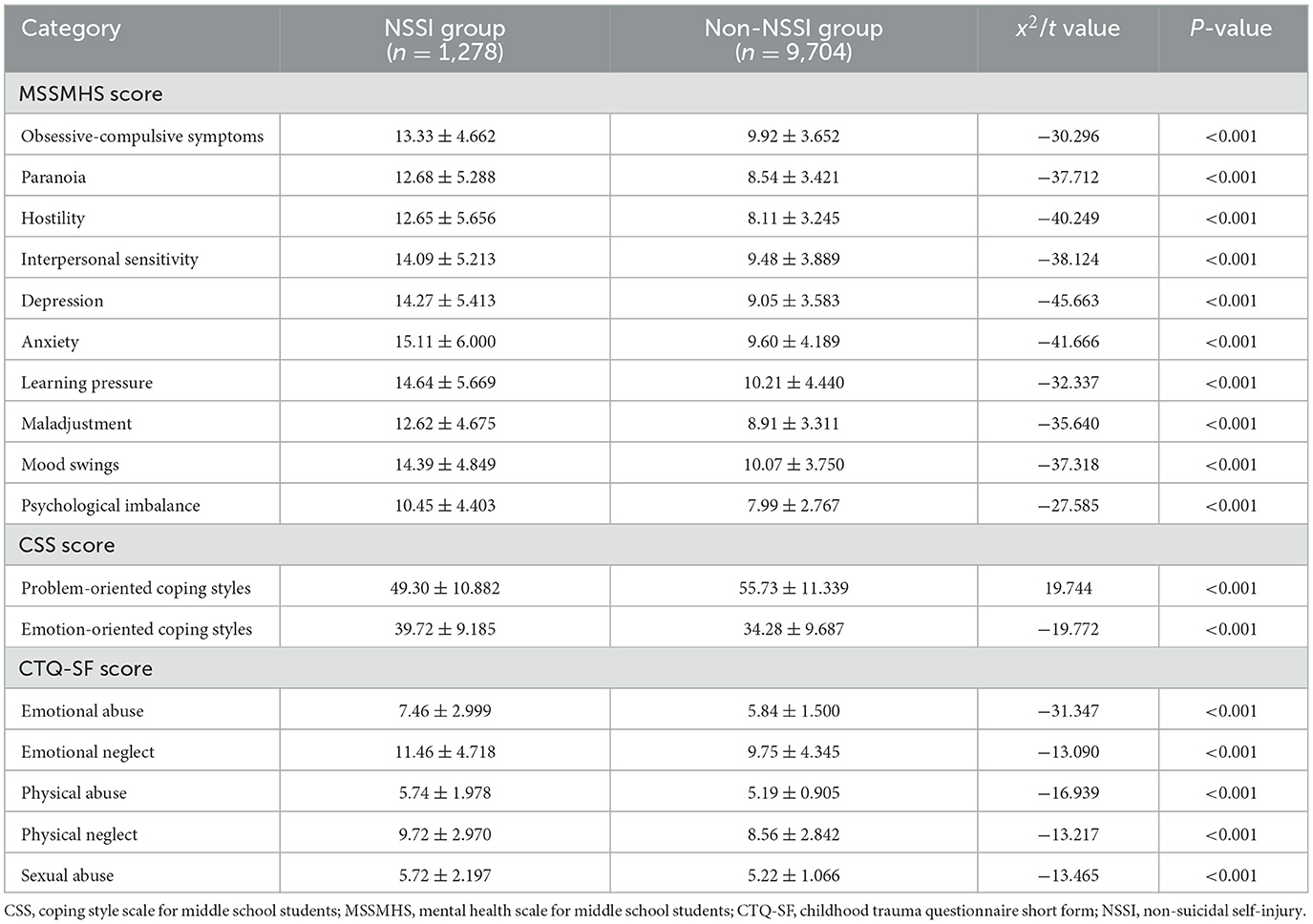
As delineated in Table 2, notable differences were evident in coping styles, instances of childhood abuse, and prevalence of mental disorders between the two groups (P < 0.001). Students within the NSSI group, notably middle school students, appeared more inclined toward experiencing interpersonal difficulties, symptoms of anxiety and depression, increased academic stress, and a preference for emotionally charged coping mechanisms. These students in the NSSI group have been subjected to a greater number of adverse childhood experiences, including emotional neglect, emotional abuse, physical neglect, physical abuse, or sexual abuse.
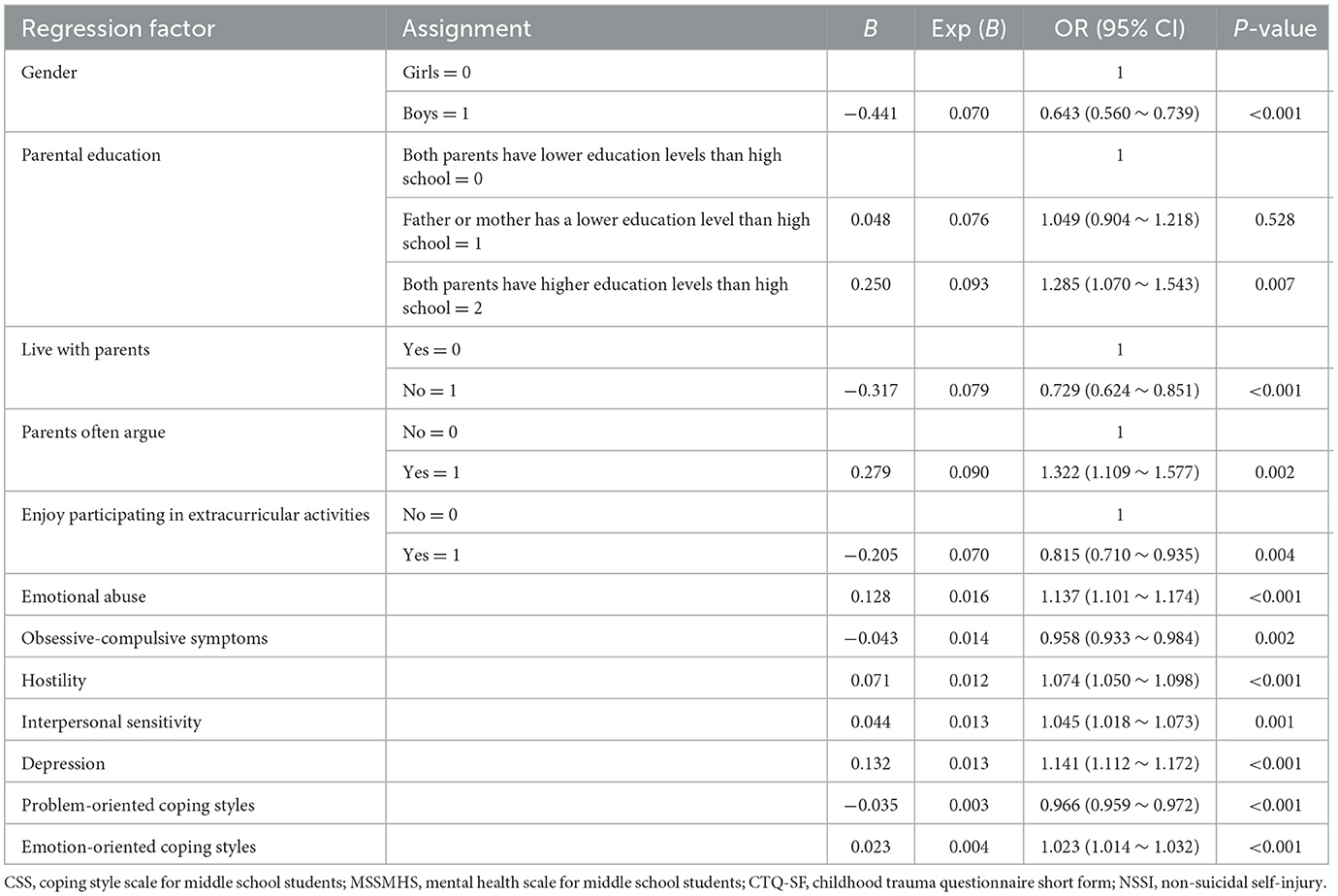
NSSI was selected as the dependent variable, with potential influencing factors acting as independent variables in the logistic regression analysis. Using the Forward: Logistic Regression method, we found that factors such as gender, interpersonal sensitivity, depression, coping style, and emotional abuse were linked to the occurrence of NSSI. The occurrence of NSSI in middle school students from families with dysfunctional parents was 1.322 times higher than those from families with harmonious relationships (OR = 1.322, 95% CI: 1.109–1.577). Students engaging in extracurricular activities exhibited less NSSI behavior (OR = 0.815, 95% CI: 0.710–0.935). The likelihood of NSSI occurrence was 0.271 times lower in students living with parents compared to those without (OR = 0.729, 95% CI: 0.624–0.851), signifying that living with parents can act as a protective factor against NSSI. Problem-oriented coping styles served as protective factors for NSSI, while emotion-oriented coping styles posed as risk factors (Table 3).
Discussion
Our study found that the detection rate of NSSI among middle school students in Hebei was 11.6% in the past year. The prevalence of NSSI in developing countries ranged from 11.5% to 33.8%, according to a retrospective study (25). In our study, the detection rate of NSSI was close to the lowest value, which may be influenced by the regional economic development level, related psychological education activities, and curriculum proliferation. In addition, cultural differences, including the importance of family and community, and views on NSSI, may also be the reasons for the different NSSI survey results in different countries (24). Due to cultural differences, in China, NSSI is often regarded as a “cowardly” behavior that cannot be understood by parents or classmates, which may affect their willingness to report NSSI and result in a lower detection rate than other studies. Some studies have used different scale assessment tools to evaluate NSSI behaviors, which may also lead to different examination rates (3). Of course, the two middle schools involved in this screening employ psychological teachers who regularly disseminate relevant psychological knowledge to students, alleviate students' negative emotions, and may consequently reduce the occurrence of adverse events.
This screening discovered that the majority of adolescents with NSSI were female, making up 58.3% of cases, a finding consistent with those of Andrews et al. (26). It could be that girls are more sensitive to negative emotions when confronted with stressors such as peer relationships, making them more likely to adopt negative coping styles. As a result, they may resort to NSSI as a means to alleviate their negative emotions (27). Some studies have also found that girls are highly correlated with “typically” feminine characteristics such as anxiety, depression, eating disorders, negative self-image, oversensitivity, which makes them more sensitive to emotional changes and more susceptible to negative emotions, thereby increasing the risk of developing NSSI (28).
This study discovered that adolescents who did not reside with their parents and had discordant family relationships were more prone to develop NSSI. A harmonious family environment plays a significant role in adolescent growth and development. Poor family interaction skills and a lack of positive emotional interchange amongst family members might create an unhealthy growth setting for adolescents. In strained family relationships, teenagers often resort to extreme measures such as self-harm to alleviate their inner negative emotions (29, 30). However, our study indicated that an increase in extracurricular activities might reduce such self-harming behaviors. This may be due to the release of beta-endorphins and a subsequent increase in endogenous opioid levels when participating in extracurricular activities, thereby reducing the inclination to self-harm (31, 32). Increasing outdoor activities for teenagers can help enhance interpersonal interaction, improve self-awareness and coping skills, thereby having a positive effect on their academic performance, health and behavior (33). Hence, enhancing students' extracurricular activities and balancing work and rest might decrease the incidence of NSSI in adolescents.
In our study, we found that emotional abuse was an independent risk factor for NSSI. This is in line with the findings of Xie et al. (7), who also reported that emotional abuse had the strongest association with NSSI. Childhood abuse can adversely impact an individual's attitudes and self-perceptions, as well as their outlook on life events and the future. These negative effects are often manifested in the form of exacerbated depressive symptoms and personality deficiencies (34). Moreover, childhood abuse may escalate the incidence of self-harming and suicidal behaviors—a harmful emotional coping mechanism that may persist into adolescence (7, 35).
This study revealed that the total score and dimension scores of the MSSMHS scale within the NSSI group were considerably higher than those in the non-NSSI group. Depression, hostility, subpar interpersonal relationships, and sensitivity can be potential risk factors for NSSI. Baetens et al. (36) discovered that positive interactions and increased peer contact may serve as protective factors against NSSI. On the other hand, poor interpersonal relationships, frequent disputes with classmates, and a lack of close friendships might heighten the risk of self-injury (37). A depressive mood can foresee the incidence of NSSI, and a significant amount of empirical literature has demonstrated that mood disorders and NSSI often transpire together (38). Compared to adolescents without NSSI, those with NSSI showed increased levels of anxiety and depression severity (39).
Adolescent behavior patterns may be influenced by different coping styles. This study found significant differences in problem-oriented and emotion-oriented coping styles between adolescents in the NSSI group and those without NSSI. The NSSI group scored higher on emotion-oriented coping styles than the non-NSSI group, while scoring lower on problem-oriented coping styles. This aligns with the findings of Jin et al. When adolescents encounter negative life events, emotion-oriented coping styles can often incite NSSI, with such self-harming behaviors frequently resulting from failures in emotional regulation (16, 20, 40). OR for emotion-oriented coping styles is minimal, but we should consider the practical significance of this factor.
This study has certain limitations. Firstly, this study is a cross-sectional study and cannot accurately explain the complex causal relationship between the research factors and NSSI. In the future, it is considered to add longitudinal studies to explore this topic. Secondly, the CTQ used in this study assesses the past experiences of the subjects and may have a certain degree of recall bias. Thirdly, the research was limited to Dingzhou City. Future research needs to expand the scale of the investigation to increase the universality of the research results.
Conclusion
To sum up, the detection rate of NSSI within the past year in the city of Hebei stands at 11.6%, with a higher rate among girls than boys. Childhood trauma, emotional abuse, interpersonal relationship problems, depression and emotion-oriented coping styles are risk factors for NSSI, while problem-oriented coping styles are protective factors. Students with NSSI are more likely to be exposed to interpersonal relationship and study pressure problems. Considering the recognized risk and protective factors for NSSI, the possibility of NSSI may be decreased through the promotion of a harmonious home environment, encouraging positive emotional interaction, and the facilitation of greater involvement in extracurricular activities. Carrying out targeted extracurricular activities or family counseling programs, regularly holding parent-child activities, establishing a supportive school and family environment, and forming stable and close teacher-student or parent-child relationships can help build teenagers' sense of belonging to school and family, thereby enhancing their mental health. In conclusion, adolescent NSSI should receive extensive attention from all. Early identification of related risk factors and timely intervention may reduce the risk of NSSI.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Clinical Research Ethics Committee of the First Hospital of Hebei Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
YLiu: Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. NL: Formal analysis, Visualization, Writing – original draft, Writing – review & editing. YLi: Resources, Supervision, Visualization, Writing – review & editing. MW: Methodology, Supervision, Visualization, Writing – review & editing. YW: Formal analysis, Investigation, Writing – review & editing. YC: Data curation, Investigation, Writing – review & editing. LH: Investigation, Writing – review & editing. JL: Investigation, Writing – review & editing. WL: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing. MG: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Medical Science Research Project of Hebei, No. 20230167. The funding was used for labor expenses during screening.
Acknowledgments
Thanks to the teachers of Dingzhou No. 1 Middle School and Dingzhou Middle School for actively organizing students to participate in the screening.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shao C, Wang X, Ma Q, Zhao Y, Yun X. Analysis of risk factors of non-suicidal self-harm behavior in adolescents with depression. Ann Palliat Med. (2021) 10:9607–13. doi: 10.21037/apm-21-1951
2. Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, Dickson JM. A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord. (2018) 227:759–69. doi: 10.1016/j.jad.2017.11.073
3. Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. (2014) 44:273–303. doi: 10.1111/sltb.12070
4. Lang J, Yao Y. Prevalence of nonsuicidal self-injury in Chinese middle school and high school students: a meta-analysis. Medicine. (2018) 97:e12916. doi: 10.1097/MD.0000000000012916
5. Griep SK, MacKinnon DF. Does nonsuicidal self-injury predict later suicidal attempts? A review of studies. Arch Suicide Res. (2022) 26:428–46. doi: 10.1080/13811118.2020.1822244
6. Poudel A, Lamichhane A, Magar KR, Khanal GP. Non suicidal self injury and suicidal behavior among adolescents: co-occurrence and associated risk factors. BMC Psychiatry. (2022) 22:96. doi: 10.1186/s12888-022-03763-z
7. Xie X, Li Y, Liu J, Zhang L, Sun T, Zhang C, et al. The relationship between childhood maltreatment and non-suicidal self-injury in adolescents with depressive disorders. Psychiatry Res. (2024) 331:115638. doi: 10.1016/j.psychres.2023.115638
8. Fasolato R, Raffagnato A, Miscioscia M, Gatta M. Non-suicidal self-injury in inpatient and outpatient adolescents: disentangling psychopathology and interactive family dynamics. Front Psychiatry. (2024) 15:1483745. doi: 10.3389/fpsyt.2024.1483745
9. Xue J, Yan F, Hu T, He W. Family functioning and NSSI urges among Chinese adolescents: a three-wave chain multiple mediation model. J Youth Adolesc. (2025) 54:1128–39. doi: 10.1007/s10964-024-02119-y
10. Zhou SC, Zhou Z, Tang Q, Yu P, Zou H, Liu Q, et al. Prediction of non-suicidal self-injury in adolescents at the family level using regression methods and machine learning. J Affect Disord. (2024) 352:67–75. doi: 10.1016/j.jad.2024.02.039
11. Wang YJ, Li X, Ng CH, Xu DW, Hu S, Yuan TF. Risk factors for non-suicidal self-injury (NSSI) in adolescents: a meta-analysis. EClinicalMedicine. (2022) 46:101350. doi: 10.1016/j.eclinm.2022.101350
12. Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. (2019) 4:e517–28. doi: 10.1016/S2468-2667(19)30145-8
13. Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, et al. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bull World Health Organ. (2014) 92:641–55. doi: 10.2471/BLT.13.129247
14. Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Annu Rev Psychol. (1993) 44:1–21. doi: 10.1146/annurev.ps.44.020193.000245
15. Portzky G, De Wilde EJ, van Heeringen K. Deliberate self-harm in young people: differences in prevalence and risk factors between the Netherlands and Belgium. Eur Child Adolesc Psychiatry. (2008) 17:179–86. doi: 10.1007/s00787-007-0652-x
16. Castro K, Kirchner T. Coping and psychopathological profile in nonsuicidal self-injurious Chilean adolescents. J Clin Psychol. (2018) 74:147–60. doi: 10.1002/jclp.22493
17. Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol. (2005) 114:140–6. doi: 10.1037/0021-843X.114.1.140
18. Yu L, Zhao J, Zhao T, Xiao Y, Ou Q, He J, et al. Multicenter analysis on the non-suicidal self-injury behaviors and related influencing factors-a case study of left-behind children in northeastern Sichuan. J Affect Disord. (2023) 320:161–8. doi: 10.1016/j.jad.2022.09.081
19. Brown JT, Volk F, Gearhart GL. A psychometric analysis of the Ottawa self-injury inventory-f. J Am Coll Health. (2018) 66:23–31. doi: 10.1080/07448481.2017.1366496
20. Zhou J, Zhang J, Huang Y, Zhao J, Xiao Y, Zhang S, et al. Associations between coping styles, gender, their interaction and non-suicidal self-injury among middle school students in rural west China: a multicentre cross-sectional study. Front Psychiatry. (2022) 13:861917. doi: 10.3389/fpsyt.2022.861917
21. Li Y, Wang Z, You W, Liu X. Core self-evaluation, mental health and mobile phone dependence in Chinese high school students: why should we care. Ital J Pediatr. (2022) 48:28. doi: 10.1186/s13052-022-01217-6
22. Xu H, Li M, Cai J, Yuan Y, He L, Liu J, et al. Comparison of ACE-IQ and CTQ-SF for child maltreatment assessment: reliability, prevalence, and risk prediction. Child Abuse Negl. (2023) 146:106529. doi: 10.1016/j.chiabu.2023.106529
23. Aloba O, Opakunle T, Ogunrinu O. Childhood trauma questionnaire-short form (CTQ-SF): dimensionality, validity, reliability and gender invariance among Nigerian adolescents. Child Abuse Negl. (2020) 101:104357. doi: 10.1016/j.chiabu.2020.104357
24. Thai TT, Jones MK, Nguyen TP, Pham TV, Bui HHT, Kim LX, et al. The prevalence, correlates and functions of non-suicidal self-injury in Vietnamese adolescents. Psychol Res Behav Manag. (2021) 14:1915–27. doi: 10.2147/PRBM.S339168
25. Mannekote Thippaiah S, Shankarapura Nanjappa M, Gude JG, Voyiaziakis E, Patwa S, Birur B, et al. Non-suicidal self-injury in developing countries: a review. Int J Soc Psychiatry. (2021) 67:472–82. doi: 10.1177/0020764020943627
26. Andrews T, Martin G, Hasking P, Page A. Predictors of onset for non-suicidal self-injury within a school-based sample of adolescents. Prev Sci. (2014) 15:850–9. doi: 10.1007/s11121-013-0412-8
27. Sun XJ, Niu GF, You ZQ, Zhou ZK, Tang Y. Gender, negative life events and coping on different stages of depression severity: a cross-sectional study among Chinese university students. J Affect Disord. (2017) 209:177–81. doi: 10.1016/j.jad.2016.11.025
28. Son Y, Kim S, Lee JS. Self-injurious behavior in community youth. Int J Environ Res Public Health. (2021) 18:1955. doi: 10.3390/ijerph18041955
29. Nemati H, Sahebihagh MH, Mahmoodi M, Ghiasi A, Ebrahimi H, Barzanjeh Atri S, et al. Non-suicidal self-injury and its relationship with family psychological function and perceived social support among Iranian high school students. J Res Health Sci. (2020) 20:e00469. doi: 10.34172/jrhs.2020.04
30. Liang K, Zhao L, Lei Y, Zou K, Ji S, Wang R, et al. Nonsuicidal self-injury behaviour in a city of China and its association with family environment, media use and psychopathology. Compr Psychiatry. (2022) 115:152311. doi: 10.1016/j.comppsych.2022.152311
31. Jarvi SM, Hearon BA, Batejan KL, Gironde S, Björgvinsson T. Relations between past-week physical activity and recent nonsuicidal self-injury in treatment-seeking psychiatric adults. J Clin Psychol. (2017) 73:479–88. doi: 10.1002/jclp.22342
32. Bresin K, Gordon KH. Endogenous opioids and nonsuicidal self-injury: a mechanism of affect regulation. Neurosci Biobehav Rev. (2013) 37:374–83. doi: 10.1016/j.neubiorev.2013.01.020
33. O'Flaherty M, Baxter J, Campbell A. Do extracurricular activities contribute to better adolescent outcomes? A fixed-effects panel data approach. J Adolesc. (2022) 94:855–66. doi: 10.1002/jad.12069
34. Forsberg A, Nilsson M, Jakobsson S, Lennerling A, Kisch A. Fear of graft rejection 1–5 years after lung transplantation–a nationwide cohort study. Nurs Open. (2018) 5:484–90. doi: 10.1002/nop2.184
35. Brown RC, Heines S, Witt A, Braehler E, Fegert JM, Harsch D, et al. The impact of child maltreatment on non-suicidal self-injury: data from a representative sample of the general population. BMC Psychiatry. (2018) 18:181. doi: 10.1186/s12888-018-1754-3
36. Baetens I, Claes L, Muehlenkamp J, Grietens H, Onghena P. Non-suicidal and suicidal self-injurious behavior among Flemish adolescents: a web-survey. Arch Suicide Res. (2011) 15:56–67. doi: 10.1080/13811118.2011.540467
37. Baetens I, Greene D, Van Hove L, Van Leeuwen K, Wiersema JR, Desoete A, et al. Predictors and consequences of non-suicidal self-injury in relation to life, peer, and school factors. J Adolesc. (2021):100–8. doi: 10.1016/j.adolescence.2021.06.005
38. Raffagnato A, Iannattone S, Fasolato R, Parolin E, Ravaglia B, Biscalchin G, et al. A pre-adolescent and adolescent clinical sample study about suicidal ideation, suicide attempt, and self-harming. Eur J Investig Health Psychol Educ. (2022) 12:1441–62. doi: 10.3390/ejihpe12100100
39. Raffagnato A, Iannattone S, Fasolato R, Rossaro MP, Spoto A, Gatta M. Psycho-behavioral profiles of pediatric inpatients with past and recent onset of nonsuicidal self-injury: a cluster analysis approach. J Clin Med. (2022) 11:4602. doi: 10.3390/jcm11154602
Keywords: non-suicidal self-injury, middle school student, influenced factor, investigation, China
Citation: Liu Y, Li N, Li Y, Wang M, Wang Y, Chen Y, Hang L, Ling J, Lu W and Gao M (2025) An investigation into non-suicidal self-injury and its influencing factors among middle school students in a city in Hebei province. Front. Public Health 13:1564746. doi: 10.3389/fpubh.2025.1564746
Received: 22 January 2025; Accepted: 30 June 2025;
Published: 17 July 2025.
Edited by:
Padmavati Ramachandran, Schizophrenia Research Foundation, IndiaReviewed by:
Michela Gatta, University of Padua, ItalyShuang-Jiang Zhou, Peking University HuiLongGuan Clinical Medical School, China
Copyright © 2025 Liu, Li, Li, Wang, Wang, Chen, Hang, Ling, Lu and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Minglong Gao, NTc4MDA5NjJAaGVibXUuZWR1LmNu; Wenting Lu, d2VudGluZzUyM0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
 Yanan Liu†
Yanan Liu† Wenting Lu
Wenting Lu Minglong Gao
Minglong Gao