- 1Key Laboratory of Geriatric Long-term Care (Naval Medical University), Ministry of Education, Shanghai, China
- 2Department of Nursing, Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 3Department of Nursing Clinical Nursing Teaching and Research, Naval Medical University, Shanghai, China
Aim: To examine and synthesize qualitative data regarding the experiences of stroke survivors who underwent rehabilitation using virtual reality (VR).
Methods: We critically appraised the included study using the Joanna Briggs Institute Critical Assessment Checklist for Qualitative Research. Relevant qualitative studies were searched in PubMed, EMBASE, CINAHL, Web of Science, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Database, China Science and Technology Journal Database, and China Biomedical Literature Database from inception to December 2024. Two researchers independently extracted and analysed the data and integrated the results using a pooled meta-aggregation approach.
Results: Sixteen studies (n = 145 stroke survivors) were included. A total of 5 meta-themes, 12 categories, and 38 research results were extracted. The meta-themes included perceived benefits, facilitating factors of using VR, and hindering factors of using VR, changes in the physical and mental health following VR rehabilitation, and suggestions and expectations for VR rehabilitation.
Conclusion: Stroke survivors perceived the benefits and barriers of using VR-based rehabilitation (VRBR); therefore, it is a complex perceptual change for them. They require emotional support from family and peers, professional support from healthcare professionals, and financial support from the government. Moreover, rehabilitation motivation is an important factor that influences utilization. Updating VRBR content and functionality is essential to improve user experience.
Systematic review registration: PROSPERO CRD42024504700, https://www.crd.york.ac.uk/PROSPERO/search.
1 Introduction
Stroke, a leading cause of death and disability (1), incurs a global cost estimated at over US$721 billion, which is 0.66% of the global GDP (2). Rehabilitation therapy effectively reduces disability in stroke survivors (3). In China alone, approximately 25 million stroke survivors required rehabilitation therapy in 2019 (4). Traditional rehabilitation treatments include physical therapy (5), speech therapy (6) and occupational therapy (7). New assistive technologies for rehabilitation therapy, such as virtual reality (VR), rehabilitation robots, and remote rehabilitation technology (8), are valued for their convenience and task-oriented training. VR combines computer graphics technology and related equipment, providing immersive and interactive virtual environments for patients and obtaining real-time feedback on their performance through multiple senses (9). Virtual reality-based rehabilitation (VRBR) can be tailored to a patient’s needs and is a personalized and progressive rehabilitation method (10). Currently, numerous quantitative studies have confirmed the effectiveness of VRBR on the upper limb (11), lower limb (12), and cognitive functions (13) of stroke survivors. However, qualitative research is needed to explore the motivation for rehabilitation, as well as facilitators and barriers to using VRBR. Qualitative meta-synthesis combines qualitative findings from disparate investigations (14) and meta-synthesis of existing qualitative studies, improving the generalization and resonance of the results. This study aimed to systematically evaluate the experiences and needs of individuals who survived a stroke when using VRBR to exercise upper limb, lower limb, balance, walking, and cognitive functions. This meta-synthesis of qualitative studies will propose specific strategies to improve VRBR interventions, providing a reference for future research on VRBR for stroke survivors.
2 Literature review
Previous studies have shown that although stroke patients have no preference for user interfaces (15), interesting and immersive virtual reality scenarios not only appeal to young stroke patients, but also have the potential to maintain stroke patients’ motivation for rehabilitation (16). In addition, virtual reality-based rehabilitation therapy has been experienced better in patients with other diseases. For instance, breast cancer patients had high levels of acceptance and satisfaction with VRBR interventions and are willing to recommend this approach to their peers (17). Finally, three key concepts mentioned in this study are explained here to the reader. VRBR is an innovative therapeutic approach utilizing virtual reality technology, which integrates motor learning, neuroplasticity, and ecological systems theory to deliver a dynamic, patient-centered, and task-oriented rehabilitation program (e.g., for stroke survivors) (10). Virtual reality-based rehabilitation (VRBR) employs immersive, task-specific virtual environments to promote motor learning and neuroplasticity through adaptive training paradigms, real-time biofeedback, and ecologically valid simulations that enhance skill transfer to daily living while maintaining patient engagement and personalized therapeutic challenge (18). Rehabilitation motivation refers to the psychological need for individuals to engage in exercise and therapy for rehabilitation (19). Social support in rehabilitation is defined as a comprehensive system of external factors, including family members, friends, healthcare professionals, and government financial support, that help individuals cope with illness or injury and promote their psychological and physical well-being (20).
3 Methods
3.1 Reporting guidelines
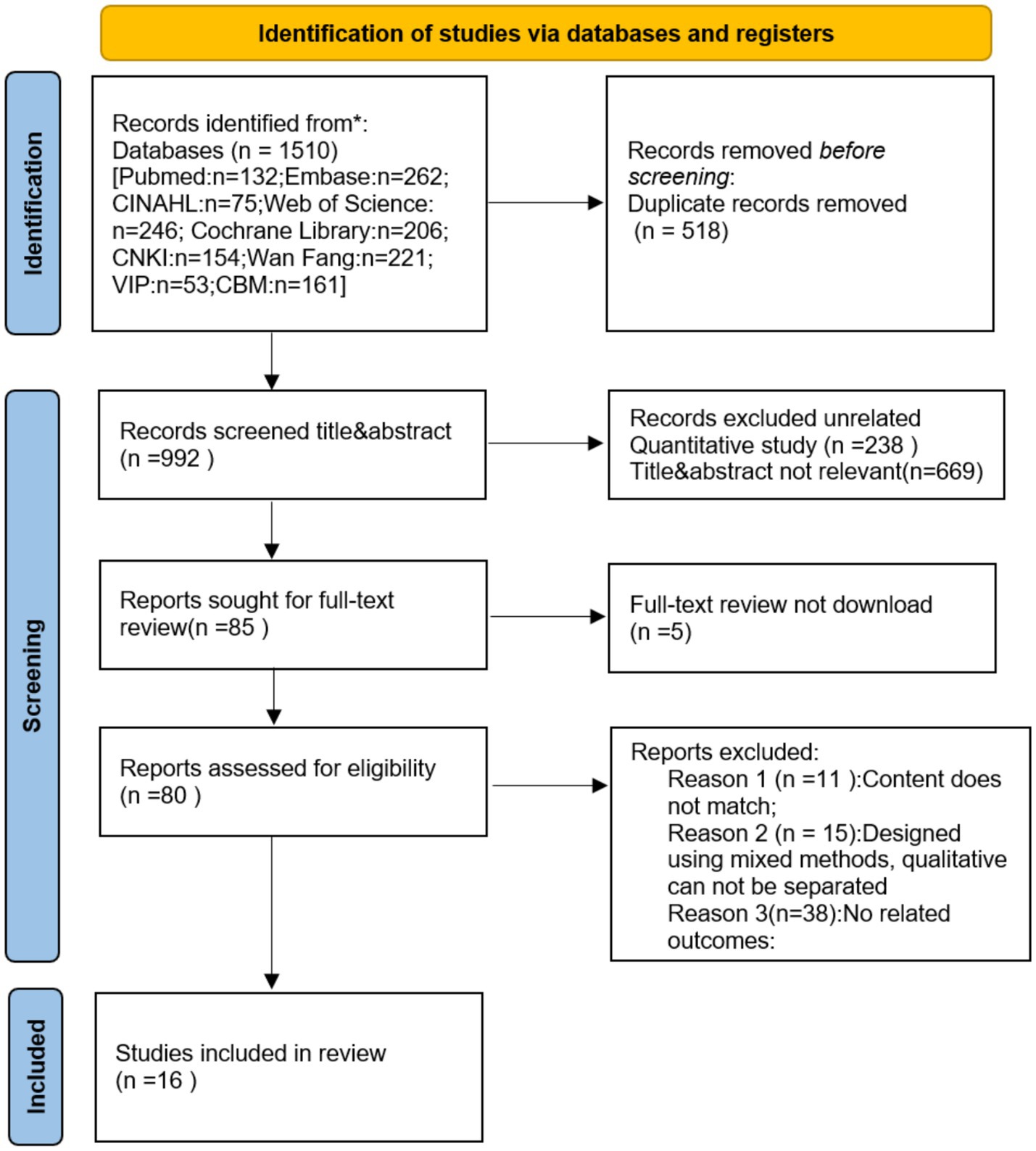
This study was conformed to the ENTREQ (Enhancing Transparency in Reporting the Synthesis of Qualitative Research) statement, which can improve the transparency of qualitative research synthesis reports (21). The search results were tracked and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) standards (22).
3.2 Inclusion and exclusion criteria
The inclusion criteria for the literature were determined according to the PICoS principles (23). Inclusion criteria: (a) study population (P): individuals who survived a stroke (age ≥18 years; non-acute phase); (b) phenomenon of interest (I): attitudes, experiences, and expectations of VRBR; (c) context (Co): experiences with VRBR in the hospital, community, or home; (d) study design (S): qualitative research, including phenomenological studies, descriptive qualitative research, rooted theory, ethnography.
Exclusion criteria: (a) duplicate publications (retaining only the one with the most information); (b) literature for which full text was not available, or data were incomplete; (c) literature not in Chinese or English; and (d) literature designed using mixed methods and qualitative data that cannot be separated.
3.3 Data sources and search strategy
PubMed, Embase, CINAHL, Web of Science, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Database, China Science and Technology Journal Database, and China Biomedical Literature Database were searched using a computer, and the retrieval time limit was from inception to December 2024. The words are retrieved in the following form: stroke (stroke*, cerebrovascular*, accident*, cerebral infarction*, cerebral haemorrhage*, apoplexy*, or poststroke*), virtual reality rehabilitation (virtual reality*, exergames*, gaming*, serious games*, motion-sensing games*, or interactive games*, virtual therapy*,or virtual rehabilitation*), qualitative (qualitative*, interview*, attitude*, experience*, phenomenology*, qualitative research*, qualitative thematic analysis*, semi-structured*). Additionally, we traced the reference lists of the included studies to identify potentially eligible studies.
3.4 Literature selection
The literature was imported into EndnoteX9.1, and duplicates were removed. The literature was independently screened by two researchers trained in evidence-based nursing, who cross-checked the extracted information. In cases of disagreement, a third researcher was consulted to assist in the judgment process. The extracts included authors, year, country, methodology, data collection, data analysis, study population, phenomena of interest, and main results.
3.5 Literature quality assessment
According to the Australian Joanna Briggs Institute Center for Evidence-Based Health Care’s (2016) quality assessment criteria for qualitative research, two researchers independently evaluated the methodology of the included literature. The assessment consisted of 10 elements, each rated as “yes,” “no,” “unclear,” or “not applicable.” The quality of the included literature was categorized into three grades: A (met all evaluation indicators), B (partially met), and C (did not meet). Studies with grade C were excluded. When disagreements occurred, the two researchers made decisions based on mutual agreement. If necessary, a third researcher included the literature.
3.6 Data analysis
In this study, the results were integrated using the meta-aggregation approach (23), which requires a three-step approach: (1) extracting all findings from the included studies with an accompanying illustration and an allocated level of plausibility for each finding; (2) grouping findings into categories, with at least two findings per category; and (3) synthesizing one or more findings from at least two categories. The results were thoroughly understood and meticulously analysed multiple times by two researchers to ensure accuracy and depth of interpretation. They grouped similar results into new categories, which were summarized into meta-themes.
3.7 Meta-theme results quality evaluation
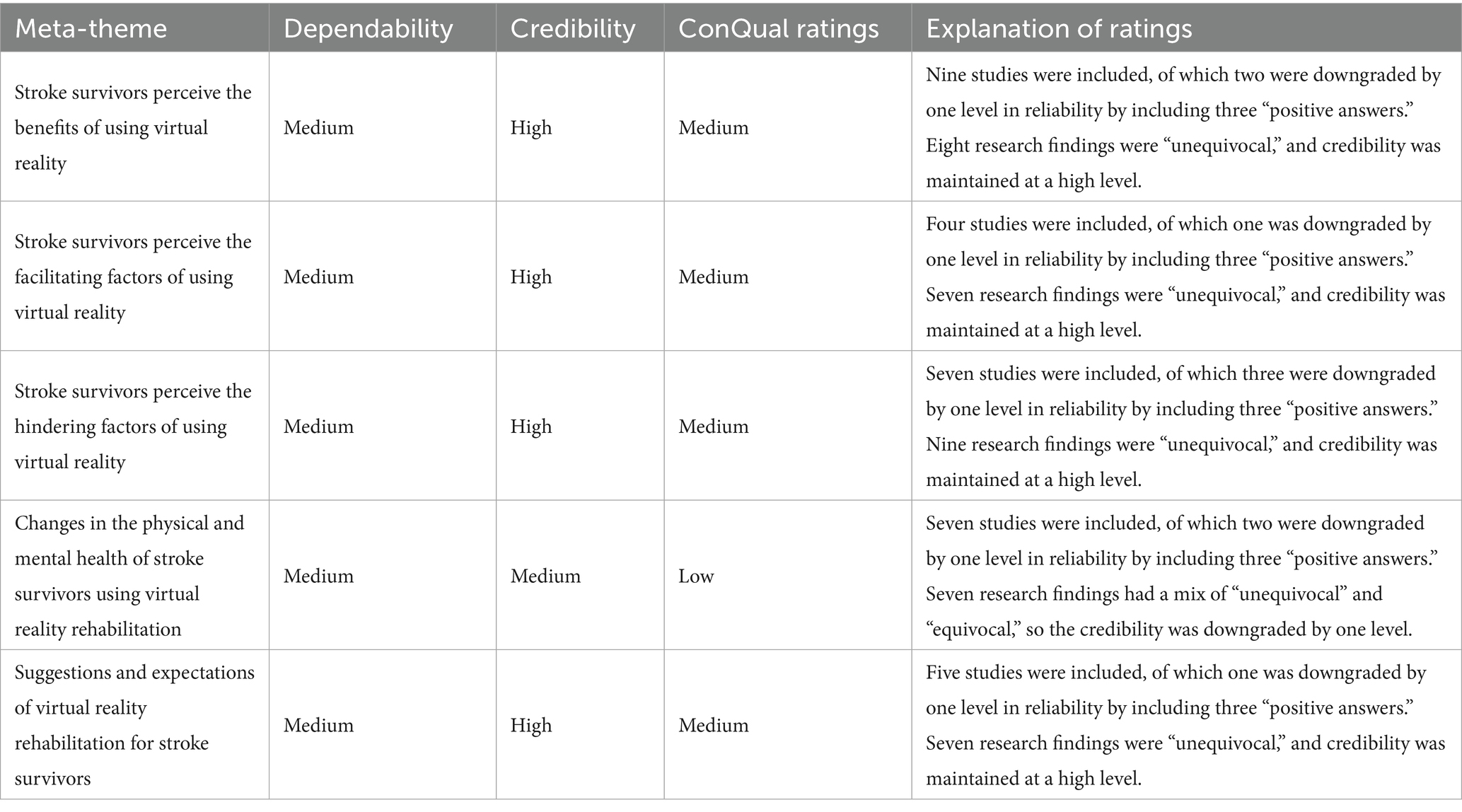
The meta-theme results were rated for quality (high, medium, low, and very low) according to the Qualitative Research Integration Evidence Assessment Tool (confidence in the qualitative evidence, ConQual) (24) constructed by the JBI Center for Evidence-Based Health Care. Ratings began at “high” and were downgraded based on reliability and trustworthiness. Dependability was determined using five questions from the JBI Quality Evaluation Criteria for Qualitative Research, which mainly evaluated the quality of the original studies included in the meta-analysis. A result of 4–5 positive answers indicated “not downgraded,” 2–3 positive answers indicated “downgraded 1,” and 0–1 positive answer indicated “downgraded 2.” Credibility was examined for consistency between the integrated results (i.e., the authors’ interpretations) and the supporting data. The findings were rated on three levels: unequivocal, equivocal, and unsupported. “No downgrade” if the integrated evidence is all from unequivocal results; ‘downgrade 2’ if the integrated evidence is all from equivocal results; and ‘downgrade 4’ if the integrated evidence is all from unsupported results”.
4 Results
4.1 Results of the literature search
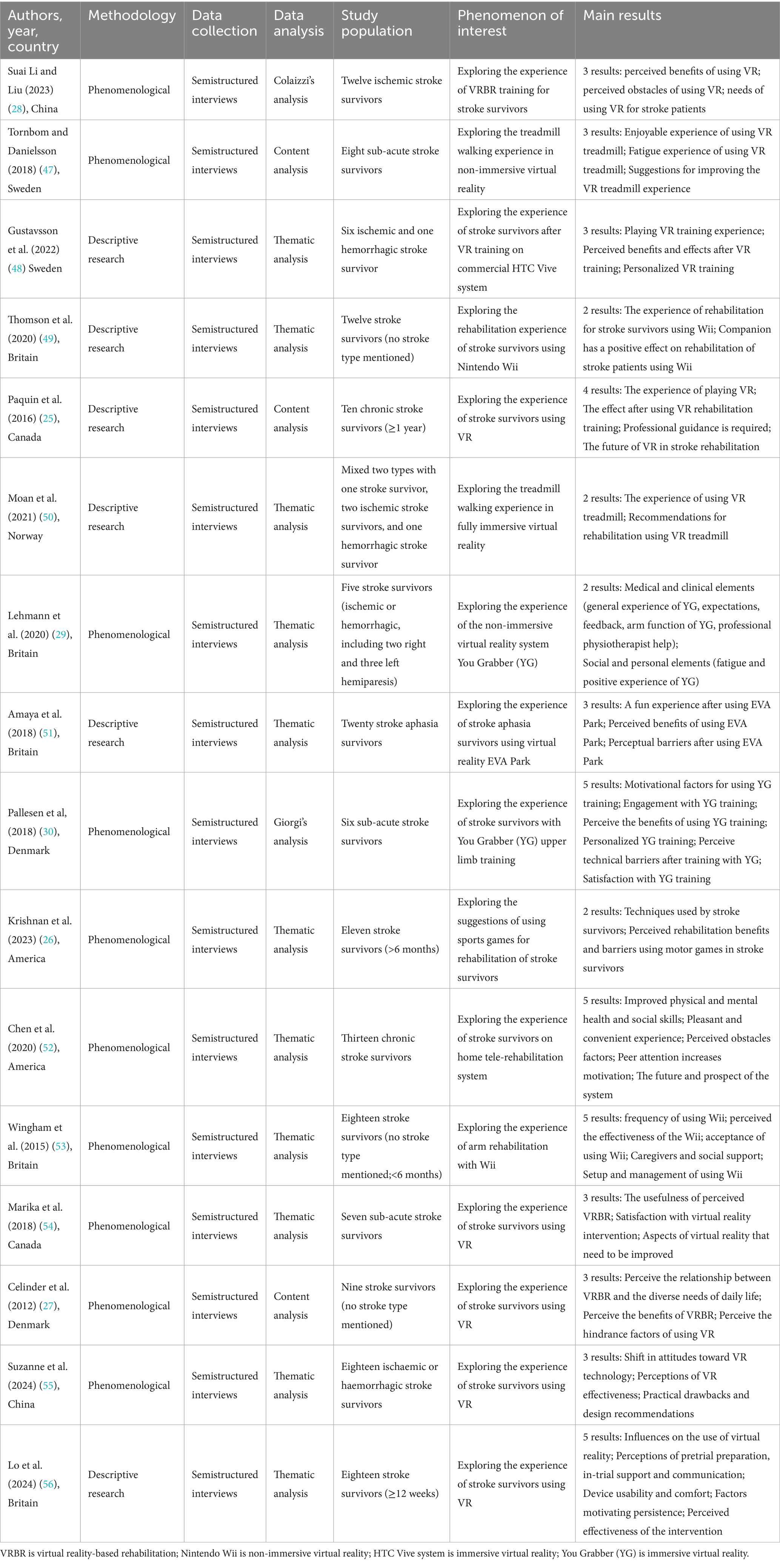
Our researchers initially examined 1,510 articles in the literature, ultimately retaining 16 literature. A detailed flowchart of the literature review is shown in Figure 1. Table 1 summarizes the features of the included studies.
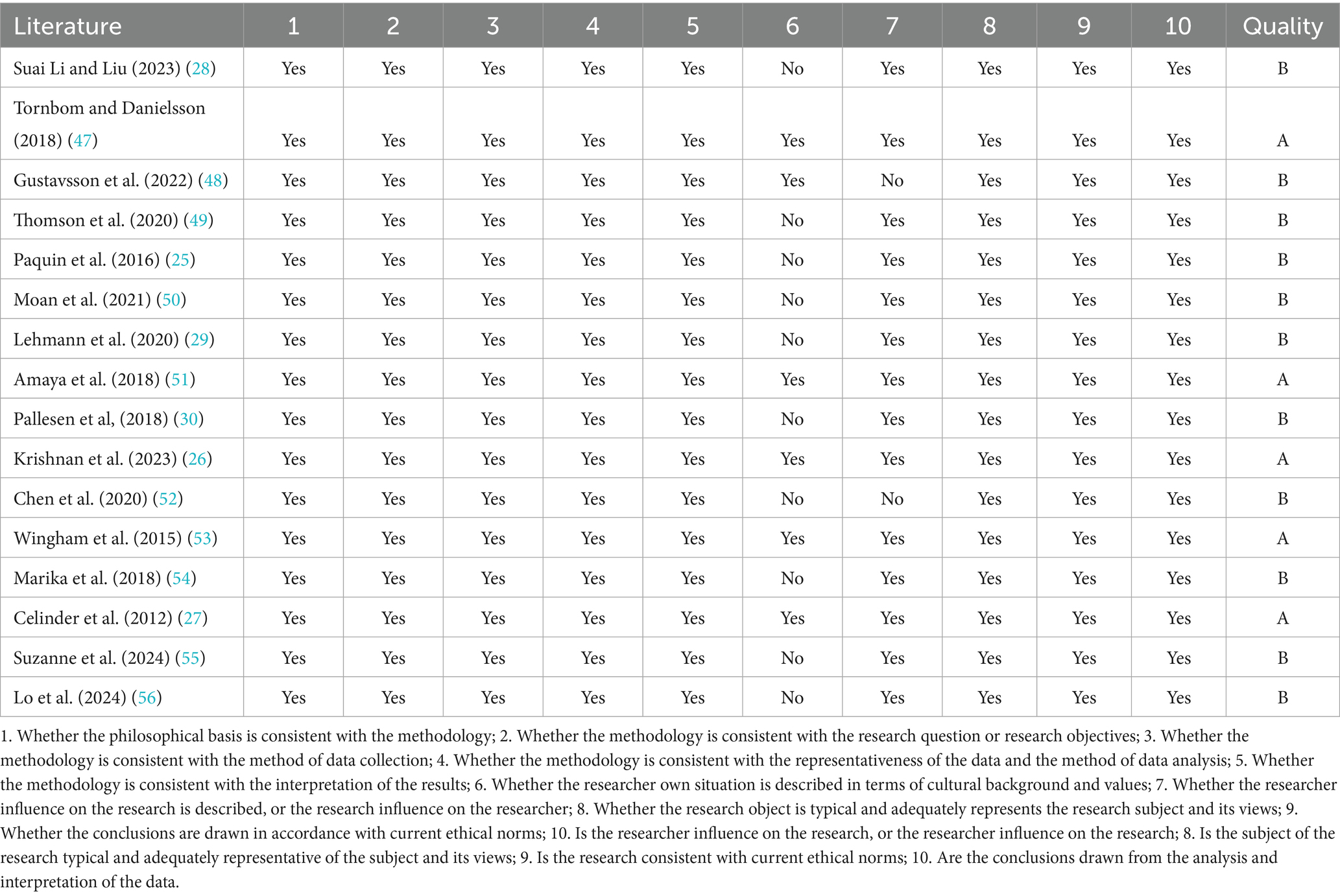
4.2 Quality assessment of included studies
Among the 16 included studies, 5 had a quality rating of A, and 11 had a rating of B (see Table 2). Among them, item 6 (whether the researcher own situation is described in terms of cultural background and values) of 10 included studies were evaluated as “no.” Item 7 (whether the researcher influence on the research is described, or the research influence on the researcher) of 2 included studies were evaluated as “no,” the remaining entries were evaluated as ‘yes’.
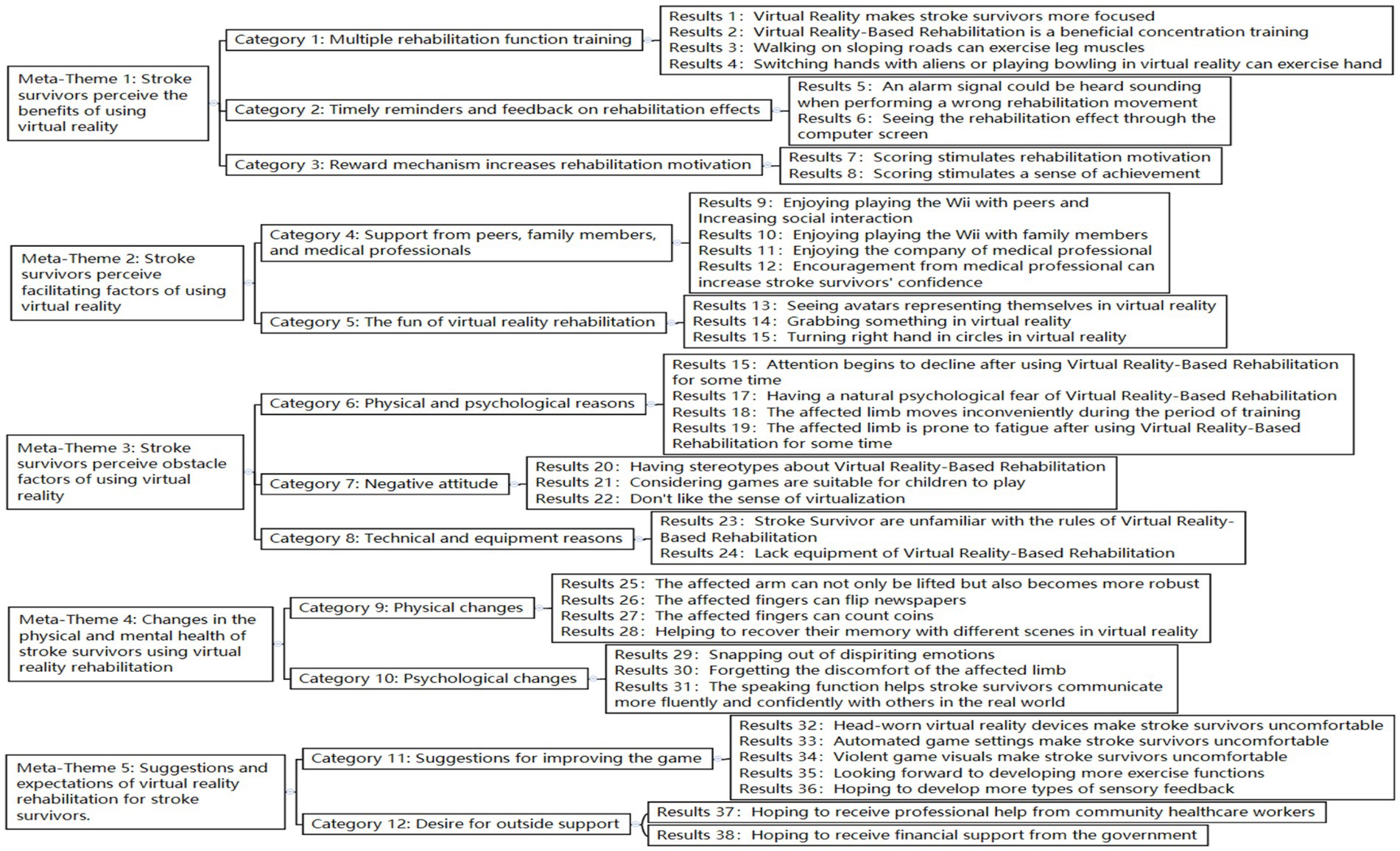
4.3 Meta-synthesis
Two researchers interpreted the 16 literature, extracting 38 research findings. Similar results were summarized into 12 new categories, and a comprehensive summary of the five meta-themes was obtained. A detailed generalization and integration of the results are shown in Figure 2.
4.3.1 Meta-theme 1: stroke survivors perceive the benefits of using VR
4.3.1.1 Category 1: diversification of rehabilitation function training
VRBR includes various rehabilitation function training (e.g., concentration training, walking on sloping roads to exercise leg muscles, and stroke survivors switching hands with aliens or using their hands to play bowling in a virtual environment) (10, 18, 21, 22, 25, 26). VR games require focused attention, which is “entirely different than being at the rehabilitation centre” (22). One stroke survivor mentioned, “It’s training in concentration and very beneficial “(25). Others consider walking in VR an effective muscle workout, stating, “Suddenly, there’s a small decline that can tense your muscles differently” (18). In addition to exercising the legs, VRBR involves hand exercises. Aliens in VR could “keep the hand moving” (25) for stroke survivors, and “that game seemed to work” (25). Playing bowling in VR requires “a proper push down” (27) of the hand.
4.3.1.2 Category 2: timely reminders and feedback on rehabilitation effects
In addition to the mentioned rehabilitation training, timely reminders in VR are very useful, and feedback on rehabilitation effects helps stroke survivors correct their rehabilitation movement (10, 23). One participant noted, “When you make a mistake, you can hear the alarm signal, you register it” (23). Another stroke survivor stated, “I think VR rehabilitation is excellent; it can show the rehabilitation effect through a computer screen. I just did the right actions” (10).
4.3.1.3 Category 3: reward mechanism increases rehabilitation motivation
Stroke survivors reported that their motivation and sense of achievement increased as their VR scores increased (19, 26, 28). As one person expressed, “You get motivated to go down there” because “beating your record and getting more and more points” can “motivate you for the next session” (26). Seeing points “went from 3,000 to 30,000” is “some sort of enjoyment in that “(19).
4.3.2 Meta-theme 2: stroke survivors perceive facilitating factors of using VR
4.3.2.1 Category 4: support from peers, family members, and medical professionals
Stroke survivors expressed that playing Wii with family members or peers enhances social interaction, encourages medical professionals to answer questions promptly, and increases their confidence (10, 20, 21). One stroke survivor stated, “Sometimes I play with my niece’s son; we play ten-pin bowling. My niece’s daughter will say, it is my shot; it is my shot. My family has all been in and tried it” (20). Another stroke survivor expressed, “I’ve got friends that will play with the Wii. You could spend all night playing” (20). Playing Wii can “lift the mood and give people something to talk about” (20). Additionally, stroke survivors need the support and encouragement of medical professionals. As stroke survivors mentioned, “during the process of recovery, I want doctors and nurses to be with me at all times, and when I have questions, they can answer them promptly” (10). Medical professionals “kept motivating me to keep going. The encouragement was always encouragement” (21).
4.3.2.2 Category 5: the fun of VR rehabilitation
Stroke survivors reported that seeing avatars representing themselves and performing movements such as grabbing something or turning their right hand in circles were novel and exciting (10, 21, 23). One survivor stated, “When participating in the training project ‘Digital Grid’, I could see a virtual animated character representing myself on the screen, which was very interesting” (10). Another expressed, “For me, to work my hands, my right hand, in circles and stuff, that was entertaining for me” (21). With the help of VR, stroke survivors can “grab something and see it working, although the hand is not open,” which is “interesting” (29).
4.3.3 Meta-theme 3: stroke survivors perceive hindering factors of using VR
4.3.3.1 Category 6: physical and psychological reasons
Stroke survivors reported that decreased attention, natural psychological fear, and affected limbs prevented them from using VR for rehabilitation (10, 19, 23). One stroke survivor expressed, “After a while, you notice your concentration is lessening, then you make more mistakes; this can be seen clearly” (23). The affected limb was prone to fatigue after using VRBR. One stroke survivor stated, “I get tired very quickly and feel tired in the whole body” (19). The affected limbs of stroke survivors can move inconveniently during training. Another stroke survivor said, “I find it inconvenient because, at the moment, I can only walk forward, not backward yet” (10). Moreover, the problems of stroke survivors who cannot walk or stand have been resolved, but they “still have a sense of fear during the VR rehabilitation process” (10).
4.3.3.2 Category 7: negative attitude
Some stroke survivors had stereotypes about rehabilitation games in VR, viewing them as suitable for only children, while others disliked the virtual experience (20, 27, 28). One survivor stated, “At first, I thought, oh God no, I mean it’s, how ashamed am I going to use it? I mean it is for children. That’s what I thought, oh gosh, it’s for, it’s a game, it’s something for kids” (20). Another said, “I do not think you can get that [the effect of walking up a hill] with VR or AR” (27). Stroke survivors are more willing to interact with the natural world; one mentioned, “Doing my dusting and polishing and things like that, I am, probably look around now and see a cobweb is giving me more satisfaction than sitting down playing that [Wii]” (28).
4.3.3.3 Category 8: technical and equipment reasons
Unfamiliarity with rehabilitation rules and insufficient equipment have limited the use of VR rehabilitation among stroke survivors (28, 30). In the beginning, the stroke survivor expressed, “I found it hard to figure out what it was that gave points the rules of the game? Uh! What is it that gives points, what is it I have to go after” (25). This confusion renders their use more challenging. Another important reason was that stroke survivors found that “after being discharged from the hospital, they still want to continue receiving rehabilitation training, unlike traditional rehabilitation that can be done anytime, anywhere, VR rehabilitation requires hardware facilities” (10).
4.3.4 Meta-theme 4: changes in the physical and mental health of stroke survivors using VR rehabilitation
4.3.4.1 Category 9: physical changes
Stroke survivors reported substantial physical improvements (e.g., the ability to lift the affected arm and increased strength, and the affected fingers can flip newspapers or count coins, helping recover their memory of different scenes in VR) (18, 19, 21, 29). As the stroke survivor expressed, “The more I trained, the pain went away, and now I can lie on this side—I can turn” (19). Another stroke survivor stated, My arm started getting stronger. I could reach more, you know, and I practiced it. I started reaching the refrigerator with my right hand and doorknobs (29). Moreover, affected fingers can flip newspapers or count coins. One stroke survivor said, “Well, I can turn a page in the newspaper, you know, with my left hand if I have to. I even handle small coins when I pick them for parking. I pulled them out and counted them. I separate them with my left hand” (21). Additionally, different scenes in VR may help stroke survivors to recover their memories. As one stroke survivor said, “It is easier to bring your memory back for a person who has had a stroke. You know, some people used to go to the sea, while others liked to sit in the forests. This helps them to return to their memories” (18).
4.3.5 Category 10: psychological changes
Stroke survivors reported that they experienced many psychological changes (such as overcoming dispiriting emotions and forgetting the discomfort of the affected limb), and the speaking function helped stroke survivors communicate more fluently and confidently with others in the real world (24, 25, 28). As the stroke survivor expressed, “I was feeling emotional after the…stroke, um, because I was not well enough to do anything round the house… but that [the Wii] just perked me up and made me feel useful” (28). Another stroke survivor mentioned, “I felt, especially at the start, discomfort about that (points to her arm). I do not want to say actual pain but discomfort in that bad arm. So, it has helped me forget discomfort and train” (25). Another said, “I’m more fluent and more confident in outside situations” (24). Additionally, another stroke survivor expressed, “I’m not afraid now of saying what I want to say, so the words come out. Thus, confidence is returned. Cos before I was full of it, but now, after the stroke, it all disappeared” (24).
4.3.6 Meta-theme 5: suggestions and expectations for VR rehabilitation from stroke survivors
4.3.6.1 Category 11: suggestions for improving the game
Head-worn VR devices, automated game settings, and violent game visuals made stroke survivors uncomfortable. They expressed a desire for more exercise options and varied sensory feedback (18, 19, 23, 28). Stroke survivors wanted to wear VR devices in a more comfortable position because one stroke survivor stated, “I would like to have the screen dark and just listen to the sounds, but I get a headache from this headband” (18). Stroke survivors disliked the automated game settings or violent game visuals in VR. A stroke survivor expressed, “Sometimes the Wii would decide that you were going into the sand or going out, and there’s nothing you can do about it” (28). Another stated, “Once, one had a bow, and then you were supposed to shoot those; it’s not allowed really, to shoot someone to death” (18). They proposed improvements in VRBR. As one stroke survivor mentioned, “I would have wanted to put it in more sense! You can have a fan that blows and breezes little over your face as you walk and smell if you go past a lilac hedge, that would have been lovely” (18). Another stroke survivor said, “So in a sense, I was hoping it offers new exercise options, and in my opinion, that is the case” (23).
4.3.6.2 Category 12: desire for outside support
Stroke survivors expressed a desire for guidance on the standard rehabilitation programs from community healthcare workers. As one stroke survivor mentioned, “I was a person who was intent on getting better, and I investigated the internet, did all of these searches, to try and find different ways I could get better. I did not learn about the standard rehabilitation program until approximately 1 year after my stroke. And to me, that’s lost time” (21). Additionally, some stroke survivors discontinued their internet connections because of financial constraints. As one stroke survivor mentioned, “I have a computer, but I gave up my internet for financial reasons” (26). They hope to receive financial support from the government.
4.4 ConQual quality evaluation of meta-theme results
Of the 38 extracted research findings, 31 were considered “equivocal.” Among the 14 included studies, 3 assessed the dependability of the three positive responses (Table 3).
5 Discussion
This review provides qualitative evidence of stroke survivors’ experiences with VR rehabilitation, focusing on their needs and perspectives.
5.1 The use of VRBR is a complex perceptual change for stroke survivors
This review revealed that some stroke survivors reported improved physical, cognitive, speech, and psychological health through functional exercise with VRBR. This finding aligns with Blazquez-Gonzalez’s study, which indicated that VR could improve depression symptoms in stroke survivors (31), and Demeco’s study, which demonstrated that fully immersive VR improves upper limb flexibility, gait performance, and dynamic balance (32). However, negative attitudes and psychological fear hindered stroke survivors who used VRBR. The underlying causes of this complex perceptual variation may be related to individual differences in stroke survivors (e.g., personality, hobbies, culture, stroke type and location, and other factors). Sports games, such as bowling, are included in the VRBR content; this review found that stroke survivors who enjoyed sports quickly adapted to the intensity of rehabilitation. Stroke survivors may be more receptive to using VRBR in familiar environments, such as at home with family and friends. Some stroke survivors have stereotyped the use of the VRBR, believing that its games are intended for children.
5.2 The effect of rehabilitation motivation on the use of VRBR
Motivation is a critical component of a successful rehabilitation program (33). Several factors may influence the use of VRBR among stroke survivors. For example, reward strategies may encourage participation, as many stroke survivors reported that increasing grades motivated them. However, poor upper limb motor function may hinder stroke survivors’ motivation to participate in rehabilitation (34). Additionally, marital intimacy (35) affects the rehabilitation motivation of stroke survivors. Maintaining a strong motivation for rehabilitation improves stroke survivors’ activities of daily living (36), enhancing their quality of life and well-being. Therefore, several potentially relevant factors should be considered when engaging stroke survivors in functional exercises using a VRBR to stimulate motivation and adherence.
5.3 External support and assistance are important in the success of using VRBR
This review found that family members, peers, healthcare professionals, and government financial support are important external factors in using VRBR by stroke survivors. Family members and friends offer strong emotional support by accompanying stroke survivors during VRBR sessions. This companionship may increase interpersonal interactions and help restore social connections for stroke survivors. However, the extent and nature of this support may vary depending on cultural norms and healthcare system structures. In regions with limited healthcare resources, informal caregivers often play a central role, whereas in systems with well-established rehabilitation infrastructures, formal healthcare professionals tend to be the primary providers of support (37). Stroke survivors view expert guidance and encouragement from healthcare professionals as key forces in sustaining VRBR use. Studies have shown that music can ameliorate subjective anxiety caused by VR (38), suggesting that integrating calming elements such as music into VR sessions could improve user experience, particularly when fear or discomfort arises.
5.4 Optimize VRBR’S content settings and function modes and improve user experience
This review found that violent game visuals, uncomfortable head-worn VR devices, and complex rehabilitation rules are unsuitable for stroke survivors. This finding is similar to Sandra’s study in which a few older adults actively chose violent game visuals (39). Simplicity and ease of understanding are critical factors in older adults’ willingness to use new technology (40). Existing VR rehabilitation content settings and functions may not meet the needs of stroke survivors. Feasibility testing of sports games helps develop more features to meet user needs (41). Feasibility tests can be required the joint engagement of patients with post-stroke aphasia, healthy volunteers, healthcare professionals, and VR experts (42). Therefore, it is recommended that stroke survivors participate in feasibility tests to optimize the content settings and functional modes of VRBR.
6 Implications for research and practice
Currently, personalized exergames for in-home rehabilitation after stroke are already in the pilot phase (43). To enhance the usability and acceptance of VRBR systems, future development should incorporate participatory design methods, where stroke survivors are actively involved in co-designing interfaces, interactions, and content. This approach ensures that VRBR platforms align with users’ physical abilities, cognitive capacities, and emotional needs, thereby increasing engagement and adherence. At the same time, technology developers should optimize the VRBR support system (e.g., enriched content and improved functionality) and develop more comfortable virtual training equipment. Reward strategies have been identified as an effective way to increase rehabilitation motivation (44). In the future studies, healthcare professionals and rehabilitation therapists should conduct longitudinal trials of the effectiveness of VRBR interventions tailored based on meta-synthesis findings. Such trials could assess outcomes including motor recovery, psychological well-being, and reintegration into daily living over extended follow-up periods. Lin et al. (45) suggests that stroke survivors have numerous unmet needs when transitioning from hospitalization to the community or home. Thus, healthcare professional should actively promote the integration of VRBR into the community and at home to create a continuum of care. Healthcare professionals and rehabilitation therapists should continue exploring the relationship between reward mechanisms, motivation, and long-term adherence. Finally, stroke survivors should receive high attention from relevant government departments (46). Policymakers should prioritize improving accessibility to VR technology, especially in under-resourced settings, and strategies may include subsidizing VR equipment.
7 Limitations
Our meta-synthesis of qualitative studies has certain limitations. Nine studies had a quality rating of B, and one equivocal research finding was identified in 38 research findings. Three included studies had a dependability assessment of three positive responses, which may have created a risk of bias and weakened the overall confidence in our meta-synthesis results. It is important to acknowledge that most of the studies reviewed were conducted in high-income countries, which may limit the generalizability of the findings to other contexts. Beyond these methodological issues, VR-based rehabilitation itself presents broader challenges, such as accessibility barriers (e.g., limited availability of VR systems in clinical or home settings), challenges in aging-friendly design, high costs of VR equipment and treatment (10) and varying levels of technological literacy among stroke survivors, which may hinder widespread adoption and effectiveness.
8 Conclusion
VRBR is a complex perceptual change for stroke survivors that requires external support and assistance. Moreover, rehabilitation motivation is an important factor that influences utilization. The VRBR content settings and function modes must be updated to improve user experience.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
JC: Writing – original draft, Writing – review & editing. BL: Data curation, Writing – original draft. MS: Writing – review & editing. QW: Methodology, Supervision, Writing – review & editing. LZ: Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Social Science Foundation of China Major Project: Disability Prevention Strategies and Applied Research in the Context of Population Aging (21&ZD188).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Collaborators, G.B.D.S . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2. Feigin, VL, Brainin, M, Norrving, B, Martins, S, Sacco, RL, Hacke, W, et al. World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke. (2022) 17:18–29. doi: 10.1177/17474930211065917
3. Liu, K, Yin, M, and Cai, Z. Research and application advances in rehabilitation assessment of stroke. J Zhejiang Univ Sci B. (2022) 23:625–41. doi: 10.1631/jzus.B2100999
4. Zhao, P, and Sun, H. Evaluating the rehabilitation needs of stroke patients in China: a trend analysis from 1990 to 2019. Brain Behav. (2025) 15:e70389. doi: 10.1002/brb3.70389
5. Huang, J, Ji, JR, Liang, C, Zhang, YZ, Sun, HC, Yan, YH, et al. Effects of physical therapy-based rehabilitation on recovery of upper limb motor function after stroke in adults: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med. (2022) 11:521–31. doi: 10.21037/apm-21-3710
6. Zumbansen, A, Kneifel, H, Lazzouni, L, Ophey, A, Black, SE, Chen, JL, et al. Differential effects of speech and language therapy and rTMS in chronic versus subacute post-stroke aphasia: results of the NORTHSTAR-CA trial. Neurorehabil Neural Repair. (2022) 36:306–16. doi: 10.1177/15459683211065448
7. Un, KK, Sue, KT, and Won, OH. The effect of convergency: using digital contents action observation educations and task-oriented occupational therapy on activity of daily living and upper extremity function in patients with stroke. J Digit Converg. (2015) 13:445–52. doi: 10.14400/jdc.2015.13.7.445
8. LinMeng, D, and HonghongLiu, YQ. Research progress on new technologies for stroke rehabilitation treatment. Chin J Contemp Neurol Neurosurg. (2017) 17:171–5. doi: 10.3969/j.issn.1672-6731.2017.03.003
9. Bargeri, S, Scalea, S, Agosta, F, Banfi, G, Corbetta, D, Filippi, M, et al. Effectiveness and safety of virtual reality rehabilitation after stroke: an overview of systematic reviews. EClinicalMedicine. (2023) 64:102220. doi: 10.1016/j.eclinm.2023.102220
10. Aderinto, N, Olatunji, G, Abdulbasit, MO, Edun, M, Aboderin, G, and Egbunu, E. Exploring the efficacy of virtual reality-based rehabilitation in stroke: a narrative review of current evidence. Ann Med. (2023) 55:2285907. doi: 10.1080/07853890.2023.2285907
11. Chen, J, Or, CK, and Chen, T. Effectiveness of using virtual reality-supported exercise therapy for upper extremity motor rehabilitation in patients with stroke: systematic review and Meta-analysis of randomized controlled trials. J Med Internet Res. (2022) 24:e24111. doi: 10.2196/24111
12. Kim, M, and Kaneko, F. Virtual reality-based gait rehabilitation intervention for stroke individuals: a scoping review. J Exerc Rehabil. (2023) 19:95–104. doi: 10.12965/jer.2346114.057
13. Chen, X, Liu, F, Lin, S, Yu, L, and Lin, R. Effects of virtual reality rehabilitation training on cognitive function and activities of daily living of patients with poststroke cognitive impairment: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2022) 103:1422–35. doi: 10.1016/j.apmr.2022.03.012
14. Finfgeld-Connett, D . Generalizability and transferability of meta-synthesis research findings. J Adv Nurs. (2010) 66:246–54. doi: 10.1111/j.1365-2648.2009.05250.x
15. Spreij, LA, Visser-Meily, JMA, Sibbel, J, Gosselt, IK, and Nijboer, TCW. Feasibility and user-experience of virtual reality in neuropsychological assessment following stroke. Neuropsychol Rehabil. (2022) 32:499–519. doi: 10.1080/09602011.2020.1831935
16. Isbel, S, Holloway, H, Greber, C, Nguyen, K, Frost, J, Pearce, C, et al. Virtual reality after stroke: identifying important characteristics when designing experiences to improve engagement in upper limb rehabilitation. Digit Health. (2024) 10:20552076241251634. doi: 10.1177/20552076241251634
17. Zhou, Z, Li, J, Wang, H, Luan, Z, du, S, Wu, N, et al. Experience of using a virtual reality rehabilitation management platform for breast cancer patients: a qualitative study. Support Care Cancer. (2023) 31:307. doi: 10.1007/s00520-023-07765-9
18. de Rooij, IJM, van de Port, IGL, Visser-Meily, JMA, and Meijer, JWG. Virtual reality gait training versus non-virtual reality gait training for improving participation in subacute stroke survivors: study protocol of the ViRTAS randomized controlled trial. Trials. (2019) 20:89. doi: 10.1186/s13063-018-3165-7
19. Oh, SY, Hwang, SY, Chung, ML, and Lennie, TA. A prediction model of rehabilitation motivation in middle-aged survivors of stroke in rehabilitation facilities in Korea. J Cardiovasc Nurs. (2020) 35:475–82. doi: 10.1097/JCN.0000000000000656
20. Chronister, JA, Johnson, EK, and Berven, NL. Measuring social support in rehabilitation. Disabil Rehabil. (2006) 28:75–84. doi: 10.1080/09638280500163695
21. AFK, T, McInnes, E, Oliver, S, and Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. (2012) 27:181. doi: 10.1186/1471-2288-12-181
22. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89. doi: 10.1016/j.jclinepi.2021.03.001
23. Lockwood, C, Munn, Z, and Porritt, K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. (2015) 13:179–87. doi: 10.1097/XEB.0000000000000062
24. Munn, Z, Porritt, K, Lockwood, C, Aromataris, E, and Pearson, A. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol. (2014) 14:108. doi: 10.1186/1471-2288-14-108
25. Paquin, K, Crawley, J, Harris, JE, and Horton, S. Survivors of chronic stroke – participant evaluations of commercial gaming for rehabilitation. Disabil Rehabil. (2016) 38:2144–52. doi: 10.3109/09638288.2015.1114155
26. Krishnan, S, Mandala, MA, Wolf, SL, Howard, A, and Kesar, TM. Perceptions of stroke survivors regarding factors affecting adoption of technology and exergames for rehabilitation. PM and R. (2023) 15:1403–10. doi: 10.1002/pmrj.12963
27. Celinder, D, and Peoples, H. Stroke patients' experiences with Wii sports® during inpatient rehabilitation. Scand J Occup Ther. (2012) 19:457–63. doi: 10.3109/11038128.2012.655307
28. Suai Li, XZ, and Liu, M. Virtual reality rehabilitation experience in patients with motor dysfunction after ischemic stroke. Chin Nurs Manag. (2023) 23:744–8. doi: 10.3969/j.issn.1672-1756.2023.05.021
29. Lehmann, I, Baer, G, and Schuster-Amft, C. Experience of an upper limb training program with a non-immersive virtual reality system in patients after stroke: a qualitative study. Physiotherapy. (2020) 107:317–26. doi: 10.1016/j.physio.2017.03.001
30. Pallesen, H, Andersen, MB, Hansen, GM, Lundquist, CB, and Brunner, I. Patients' and health professionals' experiences of using virtual reality Technology for Upper Limb Training after stroke: a qualitative substudy. Rehabil Res Pract. (2018) 2018:1–11. doi: 10.1155/2018/4318678
31. Blazquez-Gonzalez, P, Mirón-González, R, Lendínez-Mesa, A, Moro-Tejedor, MN, Cobo-Sánchez, JL, Mancebo-Salas, N, et al. Efficacy of the therapeutic use of video games on the depressive state of stroke patients: protocol for systematic review and meta-analysis. PLoS One. (2022) 17:e0275740. doi: 10.1371/journal.pone.0275740
32. Demeco, A, Zola, L, Frizziero, A, Martini, C, Palumbo, A, Foresti, R, et al. Immersive virtual reality in post-stroke rehabilitation: a systematic review. Sensors (Basel). (2023) 23:1712. doi: 10.3390/s23031712
33. Dias, P, Silva, R, Amorim, P, Lains, J, Roque, E, Pereira, ISF, et al. Using virtual reality to increase motivation in Poststroke rehabilitation. IEEE Comput Graph Appl. (2019) 39:64–70. doi: 10.1109/MCG.2018.2875630
34. Li, W, Zhu, G, Lu, Y, Wu, J, Fu, Z, Tang, J, et al. The relationship between rehabilitation motivation and upper limb motor function in stroke patients. Front Neurol. (2024) 15:1390811. doi: 10.3389/fneur.2024.1390811
35. Moon, KJ, Chung, ML, and Hwang, SY. The perceived marital intimacy of spouses directly influences the rehabilitation motivation of hospitalized stroke survivors. Clin Nurs Res. (2021) 30:502–10. doi: 10.1177/1054773820924573
36. Ishida, S, Harashima, H, Miyano, S, and Kawama, K. Effect of rehabilitation motivation on improving activities of daily living in subacute stroke patients. J Stroke Cerebrovasc Dis. (2023) 32:107385. doi: 10.1016/j.jstrokecerebrovasdis.2023.107385
37. Singh, H, Fakembe, SP, Brown, RK, Cameron, JI, Nelson, MLA, Kokorelias, KM, et al. Stroke experiences and unmet needs of individuals of African descent living in high-income economy countries: a qualitative Meta-synthesis. J Racial Ethn Health Disparities. (2024) 11:2608–26. doi: 10.1007/s40615-023-01725-z
38. Seinfeld, S, Bergstrom, I, Pomes, A, Arroyo-Palacios, J, Vico, F, Slater, M, et al. Influence of music on anxiety induced by fear of heights in virtual reality. Front Psychol. (2015) 6:1969. doi: 10.3389/fpsyg.2015.01969
39. McKay, SM, and Maki, BE. Attitudes of older adults toward shooter video games: an initial study to select an acceptable game for training visual processing. Geron. (2010) 9:5–17. doi: 10.4017/gt.2010.09.01.001.00
40. Chandrasekaran, R, Katthula, V, and Moustakas, E. Too old for technology? Use of wearable healthcare devices by older adults and their willingness to share health data with providers. Health Informatics J. (2021) 27:14604582211058073. doi: 10.1177/14604582211058073
41. Villada Castillo, JF, Montoya Vega, MF, Muñoz Cardona, JE, Lopez, D, Quiñones, L, Henao Gallo, OA, et al. Design of Virtual Reality Exergames for upper limb stroke rehabilitation following iterative design methods: usability study. JMIR Serious Games. (2024) 12:e48900. doi: 10.2196/48900
42. Bu, X, Ng, PHF, Tong, Y, Chen, PQ, Fan, R, Tang, Q, et al. A Mobile-based virtual reality speech rehabilitation app for patients with aphasia after stroke: development and pilot usability study. JMIR Serious Games. (2022) 10:e30196. doi: 10.2196/30196
43. Desai, K, Prabhakaran, B, Ifejika, N, and Annaswamy, TM. Personalized 3D exergames for in-home rehabilitation after stroke: a pilot study. Disabil Rehabil Assist Technol. (2023) 18:704–13. doi: 10.1080/17483107.2021.1913518
44. Zhou, P, Li, W, Zhao, J, Chen, S, Chen, Y, Shen, X, et al. Modulated effectiveness of rehabilitation motivation by reward strategies combined with tDCS in stroke: study protocol for a randomized controlled trial. Front Neurol. (2023) 14:1200741. doi: 10.3389/fneur.2023.1200741
45. Lin, S, Wang, C, Wang, Q, Xie, S, Tu, Q, Zhang, H, et al. The experience of stroke survivors and caregivers during hospital-to-home transitional care: a qualitative longitudinal study. Int J Nurs Stud. (2022) 130:104213. doi: 10.1016/j.ijnurstu.2022.104213
46. Ahmad Ainuddin, H, Romli, MH, Hamid, TA, SF Salim, M, and Mackenzie, L. An exploratory qualitative study with older Malaysian stroke survivors, caregivers, and healthcare practitioners about falls and rehabilitation for falls after stroke. Front Public Health. (2021) 9:611814. doi: 10.3389/fpubh.2021.611814
47. Tornbom, K, and Danielsson, A. Experiences of treadmill walking with non-immersive virtual reality after stroke or acquired brain injury - A qualitative study. PLOS ONE, (2018). 13.
48. Gustavsson, M, Kjörk, EK, Erhardsson, M, and Murphy, MA. Virtual reality gaming in rehabilitation after stroke - user experiences and perceptions. Disabil Rehabil (2022) 44, 6759–6765.
49. Thomson, K , Pollock, A, Bugge, C, and Brady, MC. Commercial gaming devices for stroke upper limb rehabilitation: The stroke survivor experience. J Rehabil Assist Technol Eng. (2020) 7:2055668320915381. doi: 10.1177/2055668320915381
50. Moan, ME, Vonstad, EK, Su, X, Vereijken, B, Solbjør, M, and Skjæret-Maroni, N. Experiences of Stroke Survivors and Clinicians With a Fully Immersive Virtual Reality Treadmill Exergame for Stroke Rehabilitation: A Qualitative Pilot Study. Frontiers in Aging Neurosci. (2021). 13:735251. doi: 10.3389/fnagi.2021.735251
51. Amaya, A, Woolf, C, and Devane, N, Galliers, J, and Talbot, R, Wilson, S, et al. Receiving aphasia intervention in a virtual environment: the participants’ perspective. Aphasiology (2018). 32:538–558.
52. Chen, Y , Chen, Y , Zheng, K, Dodakian, K, See, J, Zhou, R, et al. A qualitative study on user acceptance of a home-based stroke telerehabilitation system. TOPICS IN STROKE REHABILITATION, 2020. 27:81–92. doi: 10.1080/10749357.2019.1683792
53. Wingham, J , Adie, K, and Turner, D, Schofield, C , Pritchard, C . Participant and caregiver experience of the Nintendo Wii Sports™ after stroke: qualitative study of the trial of Wii™ in stroke (TWIST). Clin Rehabil. (2015) 29:295‐305. doi: 10.1177/0269215514542638
54. Demers, M , Chan Chun Kong D, Levin MF. Feasibility of incorporating functionally relevant virtual rehabilitation in sub-acute stroke care: perception of patients and clinicians Disabil Rehabil Assist Technol. (2019). 14:361–367. doi: 10.1080/17483107.2018.1449019
55. Kilbride, C, Butcher, T, Warland, A, Ryan, J, Scott, DJM, Cassidy, E, et al. Rehabilitation via HOMe-Based gaming exercise for the Upper limb post Stroke (RHOMBUS): a qualitative analysis of participants\u0027 experience. BMJ Open. (2024) 14:e075821. doi: 10.1136/bmjopen-2023-075821
Keywords: stroke, virtual reality, rehabilitation, experience, meta-synthesis
Citation: Cai J, Liu B, Song M, Wang Q and Zhou L (2025) Virtual reality-based rehabilitation experience of stroke survivors: a meta-synthesis of qualitative studies. Front. Public Health. 13:1566813. doi: 10.3389/fpubh.2025.1566813
Edited by:
Hasheem Mannan, University College Dublin, IrelandReviewed by:
Latha S., SRM Institute of Science and Technology, IndiaJoão José Rolo Longo, Polytechnic Institute of Lusophony, Portugal
Kholidil Amin, Diponegoro University, Indonesia
Copyright © 2025 Cai, Liu, Song, Wang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lanshu Zhou, emhvdWxhbnNodUBob3RtYWlsLmNvbQ==
 Jingyi Cai
Jingyi Cai Beixue Liu1,3
Beixue Liu1,3 Lanshu Zhou
Lanshu Zhou