- 1School of Sports Leisure, Shandong Sport University, Jinan, China
- 2Department of Physical Education and Arts, Bengbu Medical University, Bengbu, China
- 3Department of Physical Education, Anhui Finance and Economics University, Bengbu, China
Background: Anomalies in basal metabolic rate (BMR) among middle-aged and older populations can lead to various metabolism-related diseases, presenting a significant global public health challenge. The association and mechanism between sleep duration and BMR remain unclear. This study aimed to investigate the mediating role of handgrip strength in the relationship between sleep duration and BMR.
Methods: The study utilized data from the 2015 China Health and Retirement Longitudinal Study (CHARLS), comprising 10,161 participants aged 45 and older. The mediating effect of handgrip strength on the relationship between sleep duration and BMR was analyzed using linear regression model and bootstrap method.
Results: After controlling for confounding variables, a positive correlation was observed between sleep duration and BMR, with standardized regression coefficients (β) of 1.65, 95% confidence interval (CI) ranging from 0.63 to 2.70, and a significance level of p = 0.002. Grip strength was positively correlated with BMR, β was 4.63, 95% CI: 4.34 to 5.91, p < 0.001. Handgrip strength mediates 22.42% of the total effect linking sleep duration to BMR. The mediating effect was 0.37, 95% CI: 0.07–0.67.
Conclusion: The study identified significant positive correlations between sleep duration and BMR, as well as handgrip strength and BMR, with handgrip strength mediating the relationship between sleep duration and BMR.
1 Introduction
The global discussion often focuses on population aging. The World Health Organization (WHO) anticipates a seven- to eight-fold rise in the older population in developing nations. By 2025, China’s population aged 60 and above is expected to exceed 300 million (1). Basal metabolic rate (BMR) is the minimum energy required to maintain essential physiological functions at rest (2). Factors such as age, sex, body weight, body composition, and ambient temperature affect BMR (3), which tends to be lower in middle-aged and older individuals (4). Abnormal BMR can negatively impact health, increasing vulnerability to infectious diseases, metabolic disorders, cancer, and affecting weight management success (3, 5–7). Individuals with atypical BMR may experience reduced productivity, negatively affecting labor efficiency and economic output, which increases the economic burden (8, 9). Additionally, they may encounter stigmatization and mental health issues, leading to discrimination or social isolation (10, 11). Thus, implementing preventive measures and early interventions is crucial to mitigate the effects of abnormal BMR in middle-aged and older populations.
Sleep duration is crucial for the health of middle-aged and older individuals (12), influenced by genetic, environmental, and physiological factors, such as inflammation (13, 14), which may also affect BMR abnormalities. Research indicates a significant link between sleep duration and BMR. sleep restriction lowers resting metabolic rate, a component of BMR (15). A meta-analysis suggests that both short and long sleep durations may increase the risk of metabolic syndrome, implying a link between sleep length and metabolic health, with sleep potentially affecting BMR through metabolic syndrome components (16). However, another study found that short sleep duration does not significantly impact total daily energy expenditure, including BMR (17). Thus, the precise relationship between sleep duration and BMR, along with the underlying mechanisms, requires further investigation.
Handgrip strength is a recognized indicator of physical performance and a predictor of health outcomes (18). It is strongly associated with sleep duration and mortality risk (19, 20). Previous research indicates that poor sleep quality and short sleep duration correlate with reduced muscle strength, including handgrip strength, in older adults (21), emphasizing the role of sleep in preserving muscle mass and function. Additionally, another study explored the relationship between sleep duration and handgrip strength, indicating that insufficient sleep could lead to a decline in muscle strength over time (22). Research indicates that reduced grip strength is linked to higher comorbidity risk, especially in older women, highlighting the importance of maintaining muscle strength for metabolic health and a healthy BMR (23). This relationship persists across different populations and remains significant after adjusting for confounders (24, 25). Insufficient sleep may lead to a decrease in handgrip strength, thereby reducing BMR. However, the role of handgrip strength in the mediating relationship between sleep duration and BMR remains unclear. Consequently, we undertook a nationally representative cross-sectional analysis utilizing data from the China Health and Retirement Longitudinal Study (CHARLS) database. The objective of this research was to investigate the relationships between sleep duration, handgrip strength, and BMR within Chinese middle-aged and older adults examines whether handgrip strength mediates this relationship.
2 Materials and methods
2.1 Study design and participants
This study utilized a cross-sectional design, drawing upon data from the CHARLS. Which is a national longitudinal survey aimed at Chinese residents aged 45 and above, meticulously designed to produce a high-quality, representative, and publicly accessible micro-database. This database offers extensive information on middle-aged and older individuals. Participants were chosen from 28 Chinese provinces using a multi-stage probability proportional to size sampling technique. Comprehensive details regarding CHARLS have been previously documented (26). The CHARLS Dataset can be downloaded from its official website. Participants provided written informed consent and the study was ethically approved by Peking University’s Biomedical Ethics Review Board (IRB00001052-11015).
This study analyzed baseline data from 21,095 participants collected in 2015. Initially, 1,280 participants under the age of 45 were excluded. Subsequently, 8,992 individuals without BMR data, 383 without sleep duration data, and 115 without grip strength data were also excluded. Additionally, 164 participants were excluded due to missing covariate data. Supplementary Table 1 displays the traits of the participants who were excluded. Consequently, the final sample comprised 10,161 participants. Figure 1 presents a flowchart detailing the exclusion criteria.
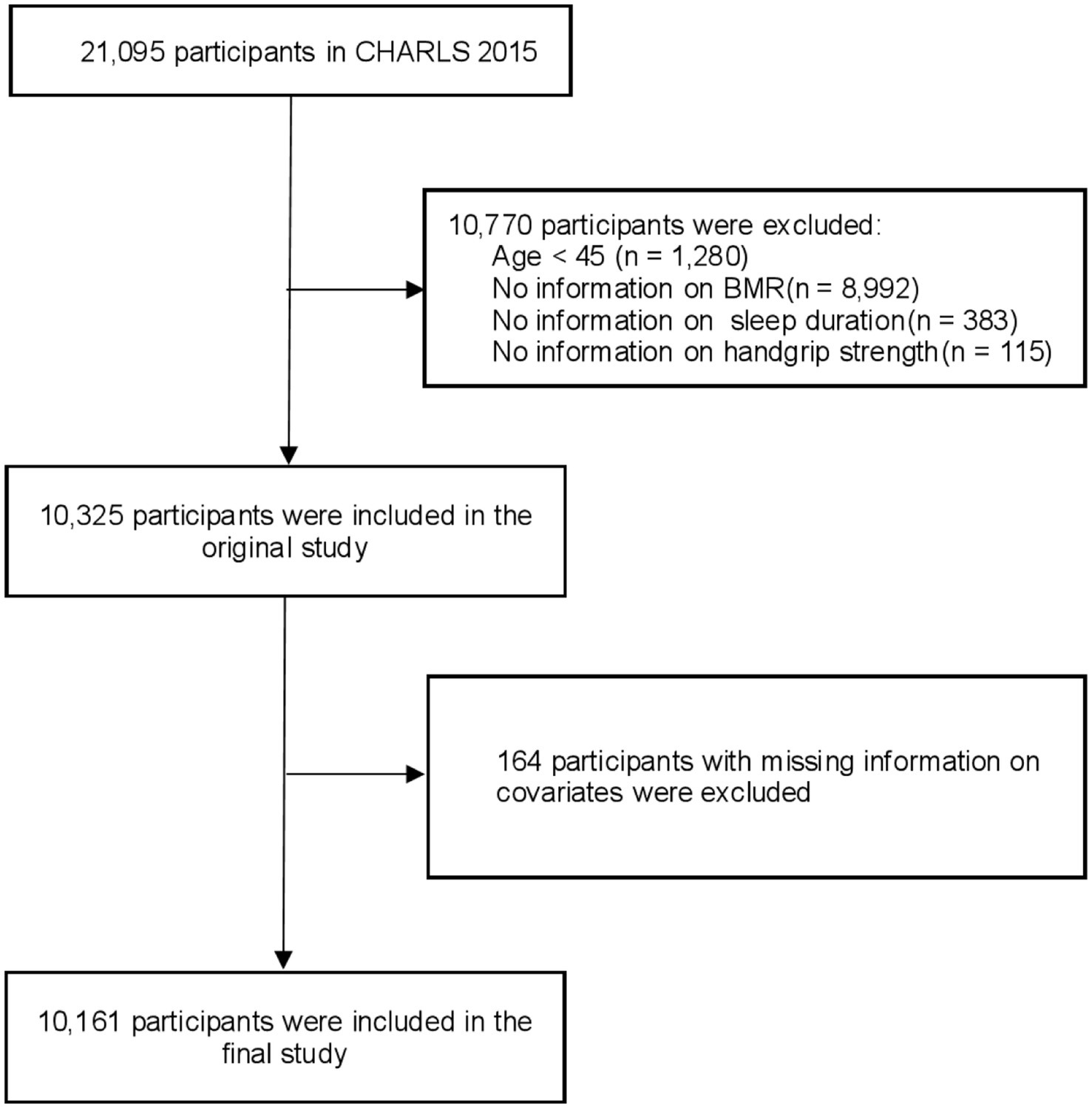
Figure 1. Flowchart of the participants selection process. CHARLS, China health and retirement longitudinal study, BMR, Basal metabolic rate.
2.2 Assessments
2.2.1 Sleep duration
Sleep duration was evaluated with the question: “Over the past month, how many hours of actual sleep did you obtain at night on average?” This aimed to determine the average sleep hours, accounting for both workdays and days off. This methodology enables a systematic analysis of sleep patterns in relation to health outcomes (27).
2.2.2 Handgrip strength
Handgrip strength was evaluated at baseline using a hydraulic handgrip dynamometer. Each participant’s hands were measured twice on both the left and right sides. For statistical analysis, the highest value among the four measurements was utilized as a continuous variable (28, 29).
2.2.3 Basal metabolic rate
BMR was calculated using the Mifflin St Jeor method (30). The Mifflin-St Jeor equations estimate BMR as follows: for males, BMR = 10 × weight (kg) + 6.25 × height (cm) − 5 × age (years) + 5; for females, BMR = 10 × weight (kg) + 6.25 × height (cm) − 5 × age (years) − 161.
2.2.4 Control variables
Building upon existing literature and clinical evidence (31, 32), this study incorporated sociodemographic characteristics, lifestyle habits, personal health status as covariates. Sociodemographic characteristics variables encompass age, gender, Education levels, marital status, and usual residence. Gender was defined as male or female. Educational attainment was categorized into three levels: “illiteracy,” “primary or middle school,” and “high school and above. “Marital status was classified as “married” for individuals cohabitating with a spouse, and “unmarried” for those who were separated, divorced, widowed, or single. Residence was dichotomized into rural or urban categories. Lifestyle habits encompassed smoking and drinking status, each classified as “yes” or “no.” The personal health status encompassed body mass index (BMI) and drinking status14 self-reported non-communicable conditions, 14 self-reported non-communicable conditions included hypertension, dyslipidemia, diabetes, cancer, chronic pulmonary disease, liver disease, myocardial infarction, cerebrovascular accident, renal disease, asthma, psychiatric disorders, gastrointestinal disease, cognitive disorders, and arthritis. Additionally, BMI was classified into categories: underweight, normal weight, Overweight, and Obesity.
2.3 Statistical analysis
This study conducted all analyses using R version 4.3.3. Sample characteristics were summarized using means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. A Shapiro–Wilk test was employed to assess the normality of the continuous variables’ distribution Initially, Spearman’s correlation was employed to assess the relationships among the primary variables. A multiple linear regression examined the associations between sleep duration, handgrip strength, and BMR, with the standardized regression coefficients (β) and 95% confidence interval (95% CI) serving to quantify the strength of these associations (33). Four adjusting progressive models were applied: an unadjusted model, Model 1 (adjusted for age, sex, educational level, and marital status), Model 2 (Model 1 plus adjustments for smoking status and drinking status), and Model 3 (adjusted for all covariates). Subsequently, using the adjustment variables from Model 3, restricted cubic spline (RCS) fitting was utilized to investigate potential nonlinear associations between sleep duration and BMR, as well as between the handgrip strength and BMR. nflection points (IP) and likelihood ratio tests (LRT) were employed to evaluate the threshold effects of sleep duration on BMR. Finally, we intend to further investigate the role of handgrip strength in this association. To this end, we developed a mediation effect model to assess the mediating role of handgrip strength in the pathway of association between sleep duration and BMR. The mediating effect’s significance was assessed through a bootstrap resampling method with 1,000 resamples (34). Statistical significance determined at a two-tailed p-value of less than 0.05.
3 Result
3.1 Baseline characteristics of the study participants
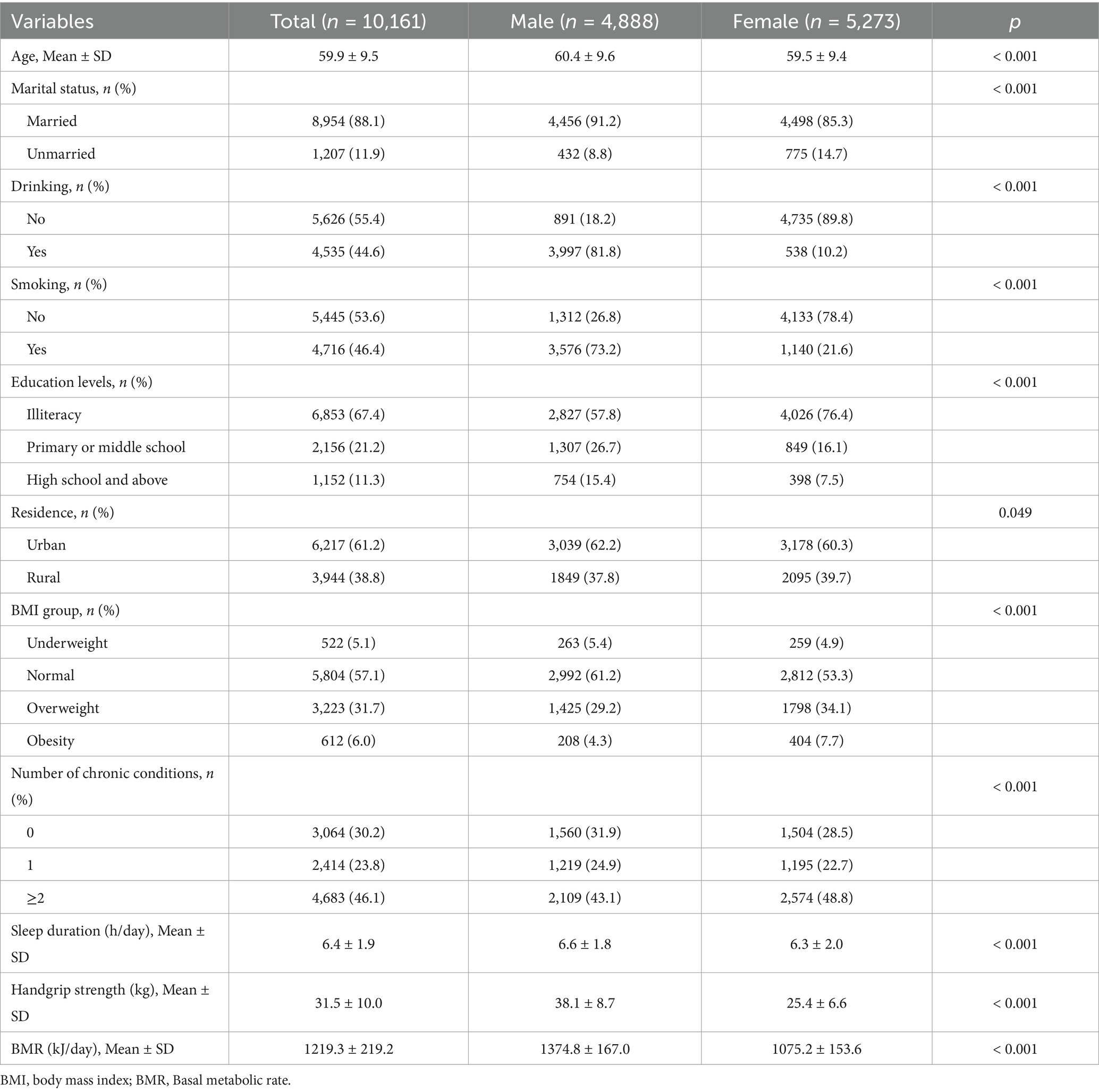
Participants were divided into male and female groups, with their characteristics detailed in Table 1. The study included 10,161 participants (mean age = 66.6 years, SD = 5.3), consisting of 4,888 men (mean age = 60.4 years, SD = 9.6) and 5,273 women (mean age = 59.5 years, SD = 9.4). The male cohort exhibited significantly higher marriage rates and educational attainment (p < 0.001). A significant percentage (61.2%) of middle-aged and older participants lived in urban regions. Significant differences in alcohol consumption, smoking habits, chronic medical conditions prevalence, and BMI were found between male and female groups (p < 0.001). Men averaged 6.6 h of sleep per day (SD = 1.8), while women averaged 6.3 h (SD = 2.0), with a statistically significant difference (p < 0.001). Mean grip strength was recorded at 38.1 kg (SD = 8.7) for men and 25.4 kg (SD = 6.6) for women (p < 0.001). The study found a significant difference in mean BMR between men (1,374.8 kJ/day, SD = 167) and women (1,075.2 kJ/day, SD = 153.6) with p < 0.001.
3.2 The relationship between important variables
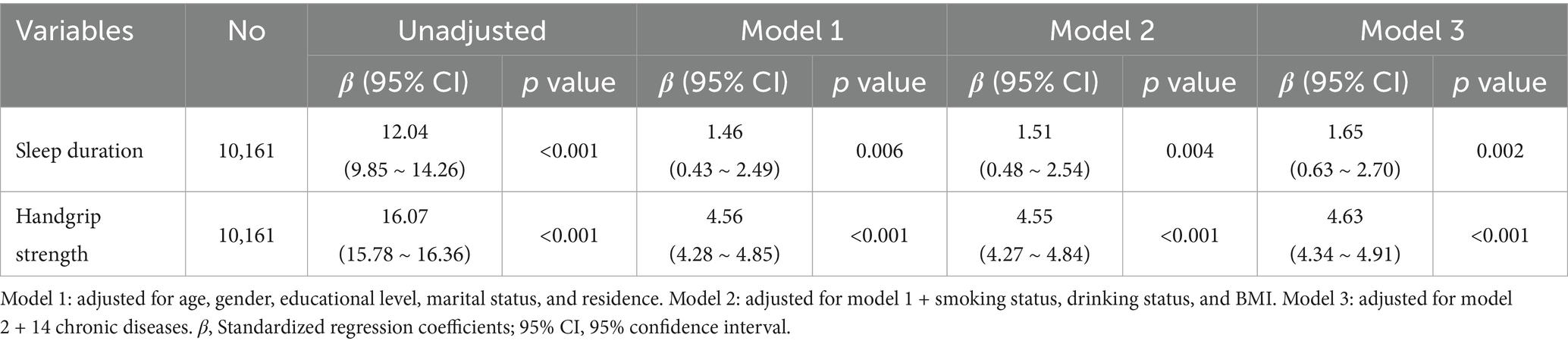
Table 2 presents the relationships between sleep duration, handgrip strength, and BMR. The research assessed the link between sleep duration and BMR among 10,161 participants. In the unadjusted model, the association between sleep duration and BMR showed a significant positive relationship, with a β of 12.04 (95% CI: 9.85–14.26, p < 0.001). In model 1, β was 1.46, 95% CI: (0.43–2.49); p = 0.006. In model 2, β = 1.51, 95% CI: (0.48–2.54); p = 0.004. In model 3, β was 1.65, 95% CI: (0.63–2.70); p = 0.002. This suggested that controlling for related factors did not significantly change the positive association between sleep duration and BMR. Handgrip strength was significantly associated with BMR in the unadjusted model (β = 16.07, 95% CI: 15.78.16.36, p < 0.001). In model 1, β was 4.56, 95% CI: (4.28–4.85); p < 0.001. In model 2, β was 4.55, 95% CI: (4.27–4.84); p < 0.001. In model 3, β was 4.63, 95% CI: (4.34–4.91); p < 0.001. The positive correlation between handgrip strength and BMR persisted significantly after controlling for relevant variables. In summary, both sleep duration and grip strength were significantly and positively associated with BMR. After accounting for various confounders, the effects of sleep duration and grip strength on BMR remained statistically significant and robust, despite variations in magnitude.
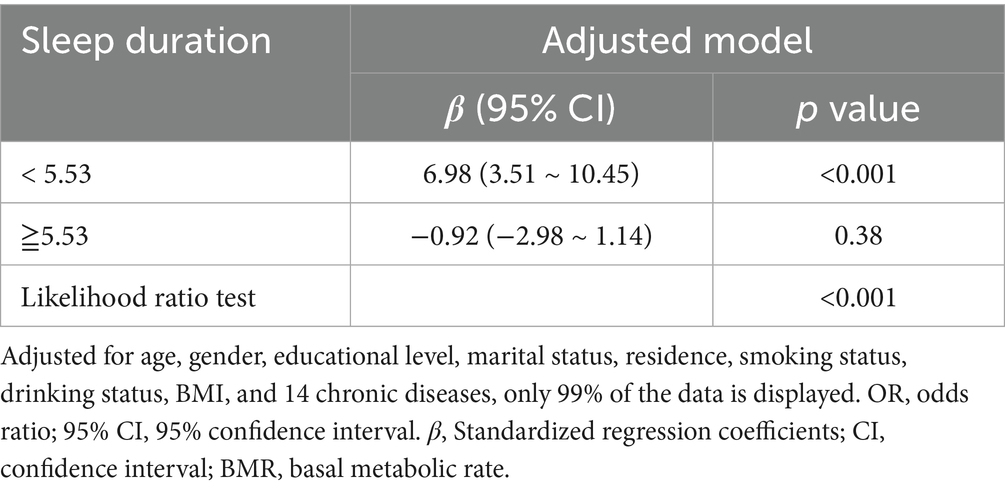
The RCS regression analysis indicated a nonlinear relationship between sleep duration and BMR, with a significant nonlinearity (p = 0.006; see Figure 2A). But, Figure 2B illustrates that no non-linear relationship exists between grip strength and BMR. In the threshold analysis, the association of participants with sleep duration < 5.53 and BMR, β was 6.94 (95% CI: 3.48–10.40, p < 0.001) (Table 3). For sleep durations of 5.53 h or more, the link between sleep duration and BMR lacked statistical significance (95% CI: −2.96 - 0.95, p = 0.33).
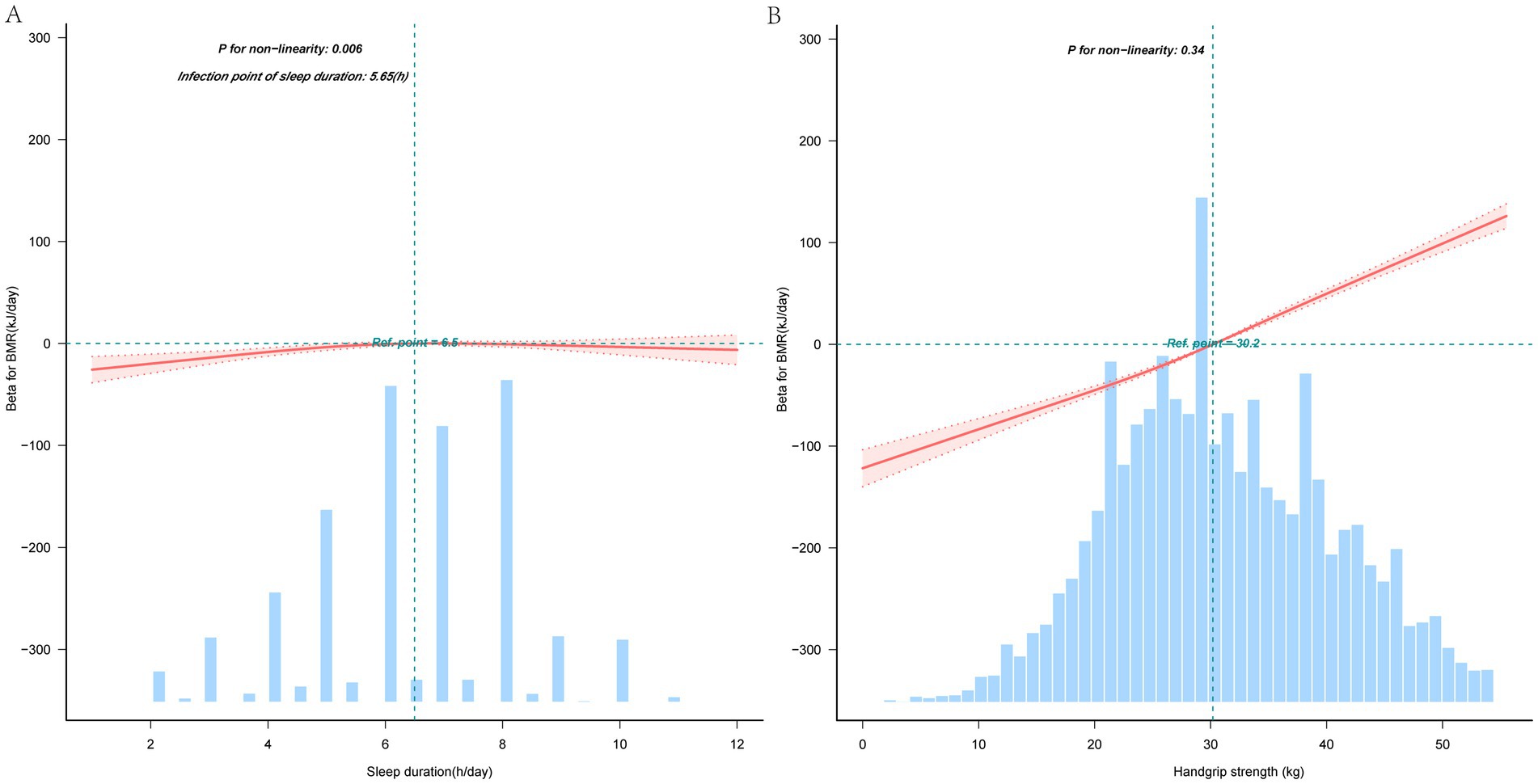
Figure 2. Nonlinear associations of sleep duration with basal metabolic rate (A), nonlinear associations of handgrip strength with basal metabolic rate (B). Solid and dashed lines represent the predicted value and 99% CI, respectively. The reference line (blue dot-dashed line) represents the median. Adjusted for age, gender, educational level, marital status, residence, smoking status, drinking status, BMI, and 14 chronic diseases, only 99% of the data is displayed. BMR, Basal metabolic rate.
3.3 Handgrip strength mediated the association between sleep duration and BMR
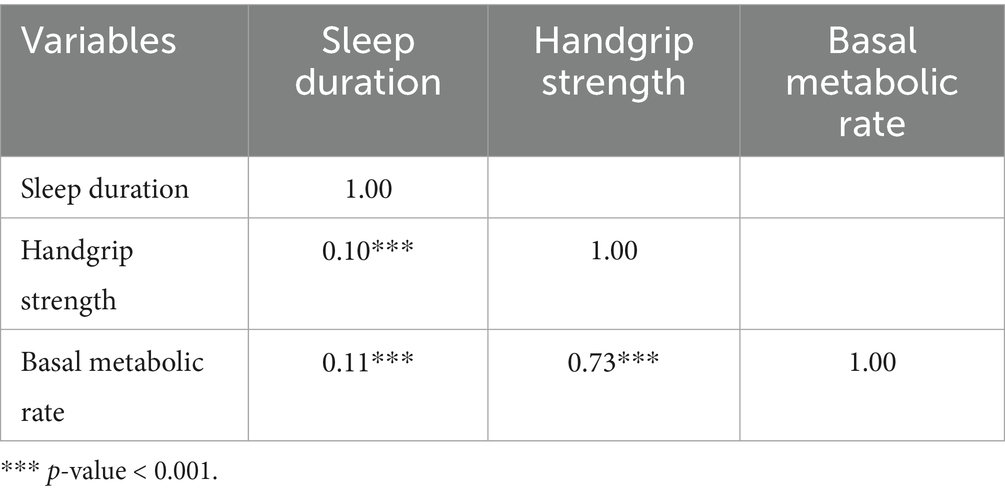
Table 4 shows the relationship between sleep duration, handgrip strength, and BMR. The study found a positive correlation between sleep duration and BMR (r = 0.11, p < 0.001). In addition, sleep duration was positively correlated with handgrip strength (r = 0.10, p < 0.001), and handgrip strength was positively correlated with BMR (r = 0.73, p < 0.001). By bootstrap analysis, the total effect of sleep duration on BMR was determined as 1.65, p = 0.002. Handgrip strength played a may mediate role between sleep duration and BMR, the size of the mediating effect was 0.37, 95% CI (0.07–0.67), accounting for 22.42% of the total effect of sleep duration on BMR, and the may mediate pathway is shown in Figure 3.
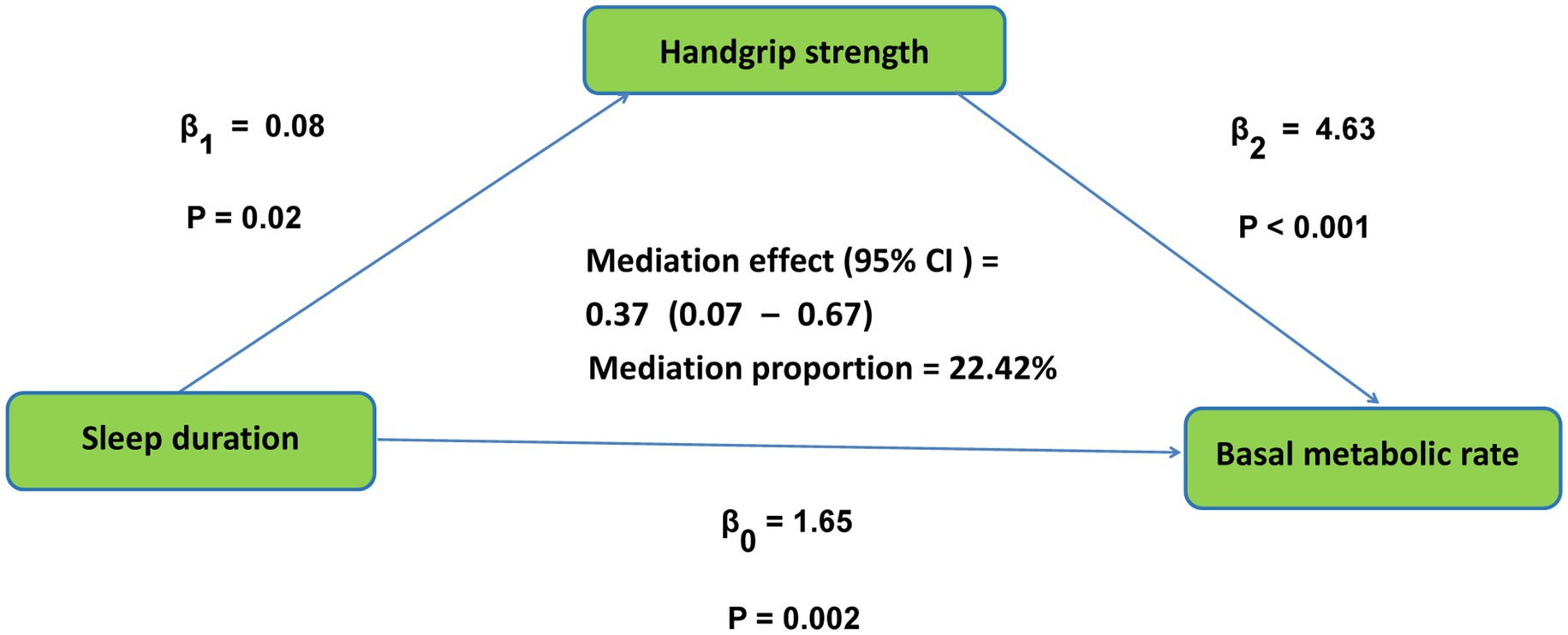
Figure 3. The conceptional framework of the mediation models. β0 was the total effect of sleep duration on basal metabolic rate; β1 represents the effect of sleep duration on handgrip strength; β2 represents the effect of handgrip strength on basal metabolic rate. The mediation effect was computed as the product of “β1” and “β2”(β1 × β2), and the mediation proportion was calculated as the ratio of the mediation effect product to total effects [(β1 × β2)/β0].
4 Discussion
This study is the first to explore how handgrip strength mediates the relationship between sleep duration and BMR in a cohort of middle-aged and older Chinese adults. The findings revealed a significant association between sleep duration and BMR. Furthermore, handgrip strength was found to partially may mediate this relationship, thereby supporting our initial hypothesis.
Research indicates a significant relationship between sleep duration and BMR, with studies highlighting the complex roles between sleep and metabolic processes. A study examined the impact of short sleep duration on energy metabolism, revealing that although it does not significantly alter total daily energy expenditure, it may influence specific components like resting metabolic rate and substrate utilization (17). This indicates that sleep duration could potentially affect BMR, given that RMR is a part of BMR. Furthermore, research on calorie restriction-like effects of resveratrol supplementation in obese humans demonstrated that resveratrol significantly reduced sleeping and resting metabolic rates, indicating that interventions affecting metabolic rate can be influenced by sleep-related factors (33). This study underscores the potential for sleep duration to modulate metabolic processes, including BMR. Finally, a study found that both long or short sleep duration were associated with increased risk of metabolic syndrome, which includes components such as altered glucose metabolism and obesity, both of which affect BMR (35). These studies show that sleep duration is closely connected to BMR and overall metabolic health, emphasizing the need for sufficient, quality sleep to maintain energy balance and metabolic function.
Sleep duration and handgrip strength have also been linked in multiple studies, underscoring the complex roles between sleep and physical health. One study examined the relationship between sleep duration and handgrip strength and found that both short and long sleep duration were associated with decreased handgrip strength, suggesting that optimal sleep duration is critical for maintaining muscle health (36). Similarly, another study found that sleep duration and quality were associated with muscle function, including handgrip strength, in older adults. Poor sleep quality and efficiency lead to decreased handgrip strength, highlighting the importance of good sleep hygiene for muscle maintenance (21). In addition, studies have shown that sleep duration affects metabolic and hormonal processes critical for muscle maintenance. Irregular sleep patterns can lead to hormonal imbalances that can affect muscle strength and recovery, including handgrip strength (37).
Handgrip strength, a measure of muscle strength, has proven significant association with BMR in older adults. For instance, a study conducted on older Koreans found a positive association between handgrip strength and BMR. The research indicated that higher handgrip strength was correlated with an increased BMR, suggesting that muscle strength exercises could be beneficial for regulating BMR in the older population (38). Meanwhile, another Korean study highlighted the relationship between handgrip strength and demographic factors, showing that handgrip strength was positively correlated with weight and height, which are key determinants of BMR (39). Additionally, the relationship between handgrip strength and physical performance has been explored in various populations. For instance, a study on older adults with type 2 diabetes found that handgrip strength relative to waist circumference was a strong predictor of mobility, which is closely linked to metabolic rate and energy expenditure (40). This underscores the potential of grip strength as an indicator of metabolic efficiency. Moreover, handgrip strength has been associated with cardiovascular health, which can influence metabolic rate. A study from the Korean Genome and Epidemiology Study found that handgrip strength was inversely related to arterial stiffness, a factor that can affect cardiovascular efficiency and, consequently, BMR (41). In summary, handgrip strength is a valuable measure that is associated with BMR through its links to muscle mass, physical performance, cardiovascular health, and overall metabolic efficiency.
Addressing poor sleep quality, low handgrip strength, and abnormal basal metabolic rate in middle-aged and older individuals necessitates a comprehensive strategy focusing on lifestyle modifications, physical activity, and nutritional interventions. Firstly, improving sleep quality is crucial as it is linked to various health outcomes. Exercise training programs moderately improve sleep quality in middle-aged and older adults. Programs involving moderate-intensity aerobic or high-intensity resistance exercises can decrease sleep latency and medication usage (42). Furthermore, music therapy, particularly listening to sedative music for a minimum of 4 weeks, enhances sleep quality in older adults (43). Regular physical activity also positively impacts handgrip strength, an indicator of overall health and mortality risk. Maintaining a healthy diet is crucial, as it correlates with increased muscle mass in older men (44). Additionally, interval walking training is a beneficial exercise that enhances physical fitness and may improve BMR in older adults (45, 46). Nutrition is vital in managing BMR. A balanced diet that includes adequate protein intake is essential for muscle maintenance and repair, which in turn supports a higher metabolic rate.
This study possesses several limitations. First, the self-reported sleep duration data may be subject to recall bias. Second, patients with missing data on the collected variables were excluded, which led to inevitable selective bias. Third, the cross-sectional study design imposes limitations on understanding the causality of the mediated moderation effect model. Thus, future research should employ a longitudinal study design to verify the causal direction of our mediated moderation model. Fourth, the study did not assess the severity and duration of grip strength loss, highlighting the need for further research. Fifth, our findings may have limited generalizability, because our study included only Chinese adults aged 45 years and above, this limitation may limit the relevance of our results to other ethnicities or global populations. Sixth, BMR is not measured directly but estimated using the Mifflin-St Jeor equation. Although the accuracy of this method is slightly higher compared with other methods, it is necessary to further study the directly measured BMR level.
5 Conclusion
The study found significant positive correlations between sleep duration and BMR, and between handgrip strength and BMR. Handgrip strength serves as a mediator between sleep duration and BMR. These findings are crucial for clinical practice and public health strategies aimed at preventing and managing BMR abnormalities in middle-aged and older adults.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/ participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
XS: Data curation, Project administration, Visualization, Writing – original draft, Writing – review & editing. CL: Formal analysis, Funding acquisition, Writing – original draft. HD: Supervision, Visualization, Writing – review & editing. HZ: Conceptualization, Methodology, Writing – review & editing. NB: Conceptualization, Methodology, Writing – original draft. XZ: Conceptualization, Funding acquisition, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Philosophy and Social Sciences Foundation of the Anhui Higher Education Institutions of China (2024AH052821 and 2024AH052823).
Acknowledgments
We express our gratitude to the China Center for Economic Research and the National School of Development at Peking University for their provision of the data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1567396/full#supplementary-material
References
1. Xia, C, Hu, S, Xu, X, Zhao, X, Qiao, Y, Broutet, N, et al. Projections up to 2100 and a budget optimisation strategy towards cervical cancer elimination in China: a modelling study. Lancet Public Health. (2019) 4:e462–72. doi: 10.1016/S2468-2667(19)30162-8
2. Naya, DE, Naya, H, and White, CR. On the interplay among ambient temperature, basal metabolic rate, and body mass. Am Nat. (2018) 192:518–24. doi: 10.1086/698372
3. Caudwell, P, Finlayson, G, Gibbons, C, Hopkins, M, King, N, Näslund, E, et al. Resting metabolic rate is associated with hunger, self-determined meal size, and daily energy intake and may represent a marker for appetite. Am J Clin Nutr. (2013) 97:7–14. doi: 10.3945/ajcn.111.029975
4. Miller, IM, Rytgaard, H, Mogensen, UB, Miller, E, Ring, HC, Ellervik, C, et al. Body composition and basal metabolic rate in hidradenitis Suppurativa: a Danish population-based and hospital-based cross-sectional study. J Eur Acad Dermatol Venereol. (2016) 30:980–8. doi: 10.1111/jdv.13522
5. Baranova, A, Song, Y, Cao, H, and Zhang, F. Causal associations between basal metabolic rate and COVID-19. Diabetes. (2023) 72:149–54. doi: 10.2337/db22-0610
6. Anthanont, P, and Jensen, MD. Does basal metabolic rate predict weight gain? Am J Clin Nutr. (2016) 104:959–63. doi: 10.3945/ajcn.116.134965
7. Kliemann, N, Murphy, N, Viallon, V, Freisling, H, Tsilidis, KK, Rinaldi, S, et al. Predicted basal metabolic rate and cancer risk in the European prospective investigation into Cancer and nutrition. Int J Cancer. (2020) 147:648–61. doi: 10.1002/ijc.32753
8. Cottrell, RC. Sugar: an excess of anything can harm. Nature. (2012) 483:158. doi: 10.1038/483158d
9. Bodenstein, L. CT risks dwarfed by diagnostic benefits. Science. (2011) 332:1032–3. doi: 10.1126/science.332.6033.1032-b
10. Arnold, MH, and Kerridge, I. Rejecting reality and substituting one?'s own; why bioethics should be concerned with medically unexplained symptoms. Am J Bioeth. (2018) 18:26–8. doi: 10.1080/15265161.2018.1445315
11. O'Leary, D. Why bioethics should be concerned with medically unexplained symptoms. Am J Bioeth. (2018) 18:6–15. doi: 10.1080/15265161.2018.1445312
12. Mesas, AE, Lopez-Garcia, E, Leon-Munoz, LM, Guallar-Castillon, P, and Rodriguez-Artalejo, F. Sleep duration and mortality according to health status in older adults. J Am Geriatr Soc. (2010) 58:1870–7. doi: 10.1111/j.1532-5415.2010.03071.x
13. Touchette, E, Dionne, G, Forget-Dubois, N, Petit, D, Pérusse, D, Falissard, B, et al. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics. (2013) 131:e1874–80. doi: 10.1542/peds.2012-2284
14. Wirth, MD, Jessup, A, Turner-McGrievy, G, Shivappa, N, Hurley, TG, and Hebert, JR. Changes in dietary inflammatory potential predict changes in sleep quality metrics, but not sleep duration. Sleep. (2020) 43:93. doi: 10.1093/sleep/zsaa093
15. Spaeth, AM, Dinges, DF, and Goel, N. Resting metabolic rate varies by race and by sleep duration. Obesity (Silver Spring). (2015) 23:2349–56. doi: 10.1002/oby.21198
16. Iftikhar, IH, Donley, MA, Mindel, J, Pleister, A, Soriano, S, and Magalang, UJ. Sleep duration and metabolic syndrome. An updated dose-risk meta-analysis. Ann Am Thorac Soc. (2015) 12:1364–72. doi: 10.1513/AnnalsATS.201504-190OC
17. Klingenberg, L, Sjodin, A, Holmback, U, Astrup, A, and Chaput, JP. Short sleep duration and its association with energy metabolism. Obes Rev. (2012) 13:565–77. doi: 10.1111/j.1467-789X.2012.00991.x
18. Cooper, R, Kuh, D, Cooper, C, Gale, CR, Lawlor, DA, Matthews, F, et al. Objective measures of physical capability and subsequent health: a systematic review. Age Ageing. (2011) 40:14–23. doi: 10.1093/ageing/afq117
19. Ma, Y, Liang, L, Zheng, F, Shi, L, Zhong, B, and Xie, W. Association between sleep duration and cognitive decline. JAMA Netw Open. (2020) 3:e2013573. doi: 10.1001/jamanetworkopen.2020.13573
20. Leong, DP, Teo, KK, Rangarajan, S, Lopez-Jaramillo, P, Orlandini, A, Seron, P, et al. Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. (2015) 386:266–73. doi: 10.1016/S0140-6736(14)62000-6
21. Buchmann, N, Spira, D, Norman, K, Demuth, I, Eckardt, R, and Steinhagen-Thiessen, E. Sleep, muscle mass and muscle function in older people. Dtsch Arztebl Int. (2016) 113:253–60. doi: 10.3238/arztebl.2016.0253
22. Peterson, MD, Collins, S, Meier, HCS, Brahmsteadt, A, and Faul, JD. Grip strength is inversely associated with DNA methylation age acceleration. J Cachexia Sarcopenia Muscle. (2023) 14:108–15. doi: 10.1002/jcsm.13110
23. Volaklis, KA, Halle, M, Thorand, B, Peters, A, Ladwig, KH, Schulz, H, et al. Handgrip strength is inversely and independently associated with multimorbidity among older women: results from the KORA-age study. Eur J Intern Med. (2016) 31:35–40. doi: 10.1016/j.ejim.2016.04.001
24. Kim, Y, White, T, Wijndaele, K, Westgate, K, Sharp, SJ, Helge, JW, et al. The combination of cardiorespiratory fitness and muscle strength, and mortality risk. Eur J Epidemiol. (2018) 33:953–64. doi: 10.1007/s10654-018-0384-x
25. Ho, FKW, Celis-Morales, CA, Petermann-Rocha, F, Sillars, A, Welsh, P, Welsh, C, et al. The association of grip strength with health outcomes does not differ if grip strength is used in absolute or relative terms: a prospective cohort study. Age Ageing. (2019) 48:684–91. doi: 10.1093/ageing/afz068
26. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
27. Hirshkowitz, M, Whiton, K, Albert, SM, Alessi, C, Bruni, O, DonCarlos, L, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1:40–3. doi: 10.1016/j.sleh.2014.12.010
28. Liu, Y, Chang, Q, Xia, Y, and Zhao, Y. Longitudinal associations between household solid fuel use and handgrip strength in middle-aged and older Chinese individuals: the China health and retirement longitudinal study. Front Public Health. (2022) 10:881759. doi: 10.3389/fpubh.2022.881759
29. Yu, B, Steptoe, A, Niu, K, and Jia, X. Social isolation and loneliness as risk factors for grip strength decline among older women and men in China. J Am Med Dir Assoc. (2020) 21:1926–30. doi: 10.1016/j.jamda.2020.06.029
30. Tian, S. Superiority of new predictive equation for resting energy expenditure should be reconsidered. Clin Nutr. (2018) 37:1084. doi: 10.1016/j.clnu.2018.01.043
31. Ruan, Y, Guo, Y, Kowal, P, Lu, Y, Liu, C, Sun, S, et al. Association between anemia and frailty in 13,175 community-dwelling adults aged 50 years and older in China. BMC Geriatr. (2019) 19:327. doi: 10.1186/s12877-019-1342-5
32. Bu, F, Deng, XH, Zhan, NN, Cheng, H, Wang, ZL, Tang, L, et al. Development and validation of a risk prediction model for frailty in patients with diabetes. BMC Geriatr. (2023) 23:172. doi: 10.1186/s12877-023-03823-3
34. Baron, RM, and Kenny, DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
35. Timmers, S, Konings, E, Bilet, L, Houtkooper, RH, van de Weijer, T, Goossens, GH, et al. Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell Metab. (2011) 14:612–22. doi: 10.1016/j.cmet.2011.10.002
36. Arora, T, Jiang, CQ, Thomas, GN, Lam, KBH, Zhang, WS, Cheng, KK, et al. Self-reported long total sleep duration is associated with metabolic syndrome: the Guangzhou biobank cohort study. Diabetes Care. (2011) 34:2317–9. doi: 10.2337/dc11-0647
37. Chen, R, Chen, Q, Lu, G, Zhang, M, Yang, H, Qi, K, et al. Sleep duration and depressive symptoms in Chinese middle-aged and older adults: the moderating effects of grip strength. J Affect Disord. (2023) 339:348–54. doi: 10.1016/j.jad.2023.07.059
38. Brady, EM, Bodicoat, DH, Hall, AP, Khunti, K, Yates, T, Edwardson, C, et al. Sleep duration, obesity and insulin resistance in a multi-ethnic UK population at high risk of diabetes. Diabetes Res Clin Pract. (2018) 139:195–202. doi: 10.1016/j.diabres.2018.03.010
39. Oh, SK, Son, DH, Kwon, YJ, Lee, HS, and Lee, JW. Association between basal metabolic rate and handgrip strength in older Koreans. Int J Environ Res Public Health. (2019) 16:4377. doi: 10.3390/ijerph16224377
40. Lim, SH, Kim, YH, and Lee, JS. Normative data on grip strength in a population-based study with adjusting confounding factors: sixth Korea National Health and nutrition examination survey (2014-2015). Int J Environ Res Public Health. (2019) 16:2235. doi: 10.3390/ijerph16122235
41. Kis, OS, Buch, A, Eldor, R, and Moran, DS. Hand grip strength relative to waist circumference as a means to identify men and women possessing intact mobility in a cohort of older adults with type 2 diabetes. Biomedicines. (2023) 11:352. doi: 10.3390/biomedicines11020352
42. Kim, W, Kim, SH, Choi, CU, Lee, SK, Kang, DO, Choi, JY, et al. Role of arterial stiffness in the association between hand grip strength and cardiovascular events: the Korean genome and epidemiology study. J Hypertens. (2021) 39:1203–9. doi: 10.1097/HJH.0000000000002753
43. Yang, PY, Ho, KH, Chen, HC, and Chien, MY. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother. (2012) 58:157–63. doi: 10.1016/S1836-9553(12)70106-6
44. Chen, CT, Tung, HH, Fang, CJ, Wang, JL, Ko, NY, Chang, YJ, et al. Effect of music therapy on improving sleep quality in older adults: A systematic review and meta-analysis. J Am Geriatr Soc. (2021) 69:1925–32. doi: 10.1111/jgs.17149
45. Jung, M, Park, S, Kim, H, and Kwon, O. Association of Diet Quality with low muscle mass-function in Korean elderly. Int J Environ Res Public Health. (2019) 16:2733. doi: 10.3390/ijerph16152733
Keywords: sleep duration, basal metabolic rate, handgrip strength, middle-aged and older adults, CHARLS
Citation: Sun X, Li C, Ding H, Zhou H, Bai N and Zhao X (2025) The mediating effect of handgrip strength on the association between sleep duration and basal metabolic rate in middle-aged and older adults: evidence from the China health and retirement longitudinal study. Front. Public Health. 13:1567396. doi: 10.3389/fpubh.2025.1567396
Edited by:
Ricardo Aurélio Carvalho Sampaio, Federal University of Sergipe, BrazilReviewed by:
Yingyun Gong, Nanjing Medical University, ChinaPriscila Yukari Sewo Sampaio, Federal University of Sergipe, Brazil
Copyright © 2025 Sun, Li, Ding, Zhou, Bai and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaojiang Zhao, emhhb3hpYW9qaWFuZzIwMTBAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Xinxiang Sun1†
Xinxiang Sun1† Xiaojiang Zhao
Xiaojiang Zhao