- 1Department of Cardiology, The Shapingba Hospital, Chongqing University (People’s Hospital of Shapingba District), Chongqing, China
- 2College of Traditional Chinese Medicine, Chongqing Medical University, Chongqing, China
- 3College of Pediatric, Chongqing Medical University, Chongqing, China
- 4The Second Clinical College, Chongqing Medical University, Chongqing, China
- 5Department of Basic Courses, Chongqing Medical and Pharmaceutical College, Chongqing, China
Objectives: This study aimed to assess the current situation and influencing factors of life satisfaction among Chinese older adults with hypertension and to identify its key factors.
Methods: In this study, 4,197 hypertensive patients were selected from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) database for inclusion in the analysis. A multivariate logistic regression model was used to analyze the influencing factors of life satisfaction in hypertensive patients, and the random forest was further used to rank the importance of the significant influencing factors.
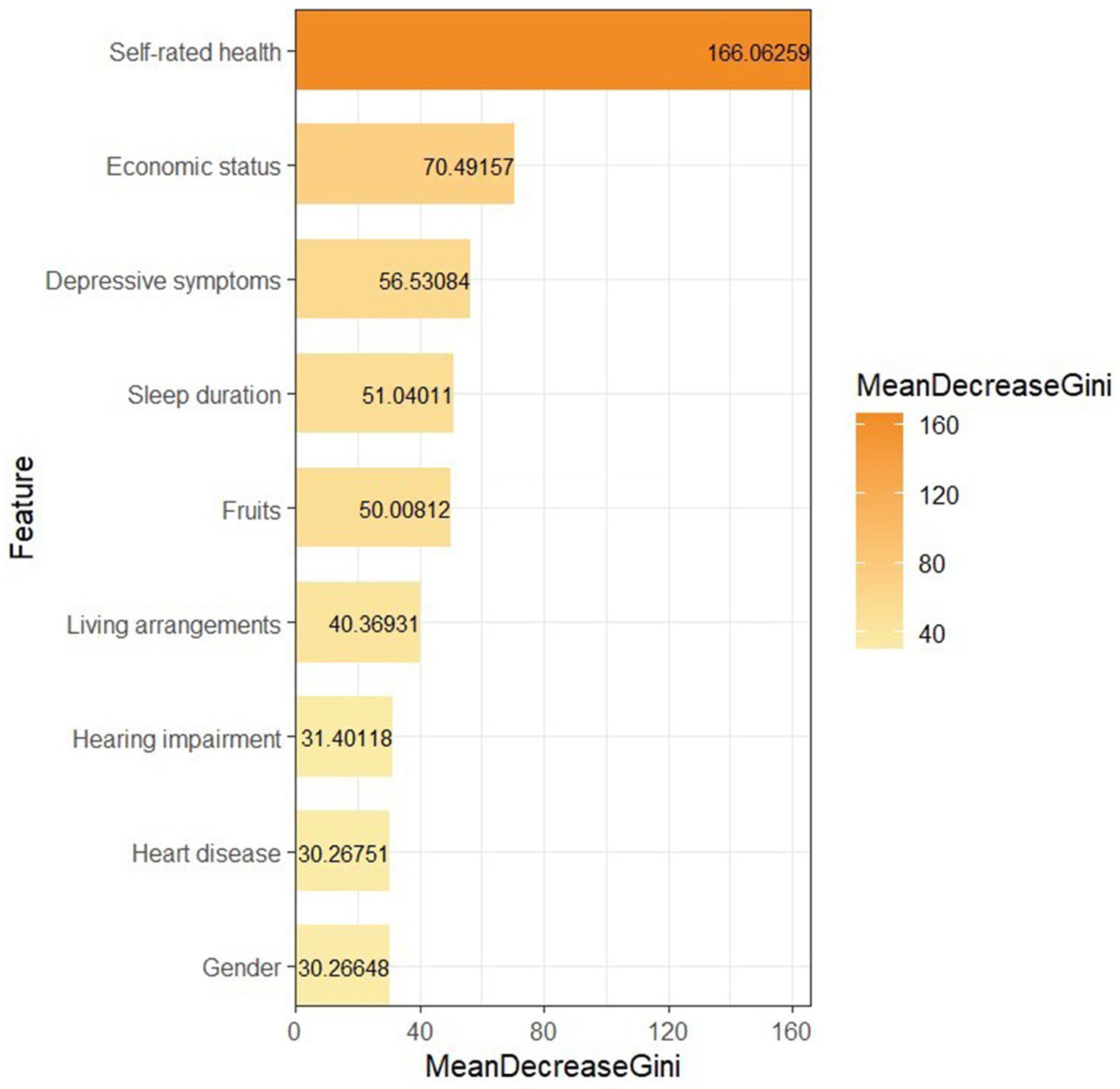
Results: Overall, 29.52% of hypertensive patients reported dissatisfaction with their lives. The life satisfaction of these patients was influenced by a combination of factors. According to the results of the random forest, the variables that significantly influenced life satisfaction, in descending order of importance, are self-rated health, economic status, depressive symptoms, sleep duration, fruits, living arrangements, hearing impairment, heart disease, and gender.
Conclusion: Our research indicates that currently, people with hypertension experience a high level of dissatisfaction with their lives, making it necessary to take preventive and intervention measures from multiple aspects.
1 Introduction
Population aging has inevitably become a major issue commonly faced across the globe (1). Studies have shown that the aging level in China has ranked among the upper-middle tier globally, with unprecedented speed and scale (2).
The aging population presents a heavy burden of diseases. Among these, hypertension, being the most common cardiovascular disease, occupies an important position (3). Currently, there are more than 1 billion adults with hypertension worldwide (4), and it is estimated that the global prevalence will reach 1.5 billion by 2025 (5). According to the results released in the Annual Report on National Center for Cardiovascular Diseases (6), the prevalence of hypertension among adults in China had reached as high as 31.6%. Although hypertension is one of the most preventable cardiovascular diseases and a key manageable risk factor for mortality (7), the World Health Organization (WHO) estimates that in 2019, more than half of all cardiovascular-related deaths could still be attributed to uncontrolled hypertension. Among people aged 30–79 with hypertension, only 21% have their blood pressure under control (8). Hypertension can lead to functional or organic damage to organs such as the heart, brain, and kidneys, leading to various chronic diseases like stroke, coronary heart disease, heart failure, cognitive impairment, and chronic kidney disease (9–12). All of these health issues are related to lower life satisfaction (LS) for patients (13, 14). This suggests that further understanding of the epidemiological trends and clinical features of low LS in hypertensive patients will help to improve the quality of their lives by early identification of those at high risk for low LS.
LS is defined as an individual’s subjective perception and feelings about their current state of life or overall quality of life (15, 16). It can influence an individual’s emotional experience and lifestyle, which, in turn, affects the overall atmosphere and the development of society. Numerous previous studies have reported various factors that influence the LS of older adults. For example, research conducted by Li et al. (17) found that financial pressure, depressive symptoms, filial piety, and access to medical services were significantly related to the LS of older adults. Other studies have also emphasized the significant impact of social activities (e.g., social isolation and basic community services) (18, 19) and lifestyles (e.g., exercise, diet, and sleep) (20, 21) on their LS. It is undeniable that these meaningful studies have all made important contributions to improving the LS of older adults. However, the applicability of these research conclusions to the population of older adults with hypertension in China remains to be further discussed. In addition, previous studies mainly relied on traditional logistic regression model for their research. As a machine learning algorithm, random forest (RF) is an excellent clinical research tool due to its strong classification capability and straightforward learning mechanism. In recent years, the RF algorithm has been widely used in the medical field for disease diagnosis and classification (22), clinical outcome prediction (23), and estimating the importance of exposure to risk factors (24).
In summary, this study aimed to use the cross-sectional data published by the Chinese Longitudinal Healthy Longevity Survey (CLHLS) in 2018 to analyze the influencing factors of LS in older adults with hypertension in China from the three dimensions of sociodemographic characteristics, health status, and lifestyles, and further rank the importance of these factors using the RF algorithm. The results of the study are of great reference value for intervening and improving the LS of older adults with hypertension and promoting their overall mental health.
2 Materials and methods
2.1 Data source
The data in this study came from CLHLS, and all data and questionnaire contents can be downloaded by registering on their official website.1 CLHLS is a national longitudinal survey project organized by the Center for Healthy Aging and Development/National School of Development of Peking University. It targeted older adults aged 65 and above and their children aged 35–64 and adopted the multi-stage whole cluster random sampling method to randomly select 631 cities and counties in 23 provinces in China, with samples covering about 85% of China’s population (25). It collected data on various aspects of the participants’ socioeconomic background, family structure, health status, and lifestyles with a high degree of reliability and representativeness. The baseline survey of the project started in 1998, and follow-up visits were conducted every 3–4 years after this. The project has provided a large amount of scientific evidence for geriatric health research, policy formulation, and social services. The CLHLS study received ethical approval from the Peking University Institutional Review Board (IRB00001052-13074), and each subject or their legal representative signed a written informed consent form.
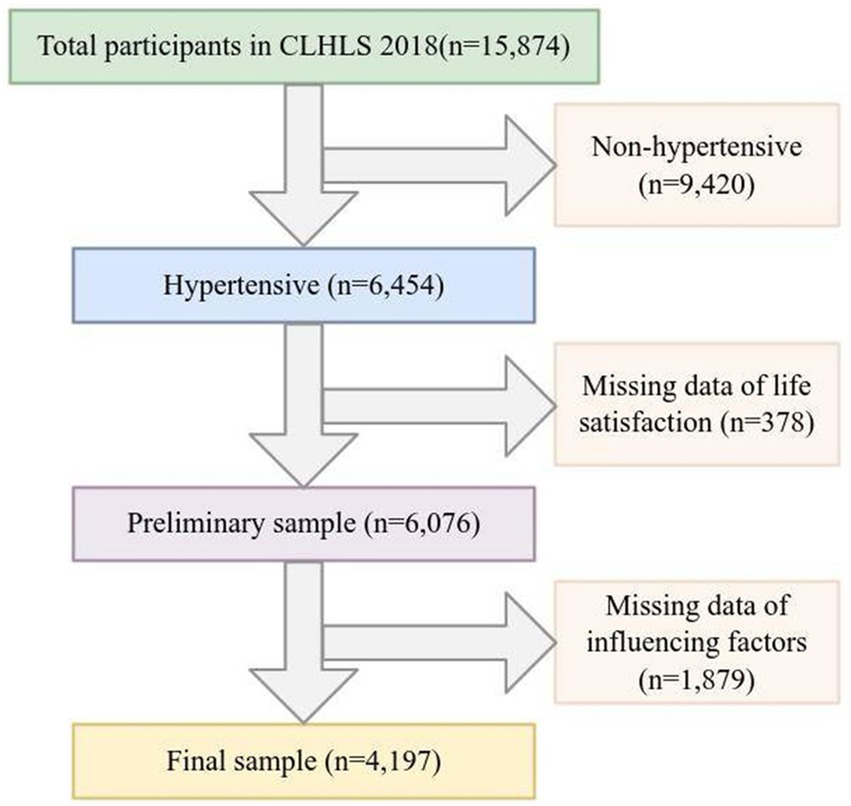
This study used survey data released by CLHLS in 2018 for analysis. The selection of the study sample was based on the question in the questionnaire: “Have you been diagnosed with hypertension by a doctor?” (26). Participants who answered “yes” were defined as hypertensive patients and further included in our follow-up study. In addition, after excluding samples with missing influencing factors and LS, 4,197 participants were included in the statistical analysis as valid samples. The detailed sample screening process is shown in Figure 1.
The minimum sample size required for the study was determined according to the formula for calculating sample size in cross-sectional studies:
(1) N denotes the sample size required for the study. (2) p denotes the prevalence of life dissatisfaction among Chinese older adults. (3) q = (1-p). (4) Zα/2 was set to 1. 96, and α was set to 0.05 for the two-sided test. (5) δ denotes the permissible error, calculated as 0.1p. According to the results of a previous study, the prevalence of life dissatisfaction among stroke patients in China was 16.9% (27). It was calculated that at least 1,889 participants were needed in this study to achieve the required sample size. Both stroke and hypertension are cardiovascular diseases that pose a high risk to Chinese older adults’ health. Therefore, we believe that there is a certain degree of reliability in our use of the reported rate of life dissatisfaction among stroke patients to estimate the prevalence of life dissatisfaction among hypertensive patients in this study.
2.2 Independent variable
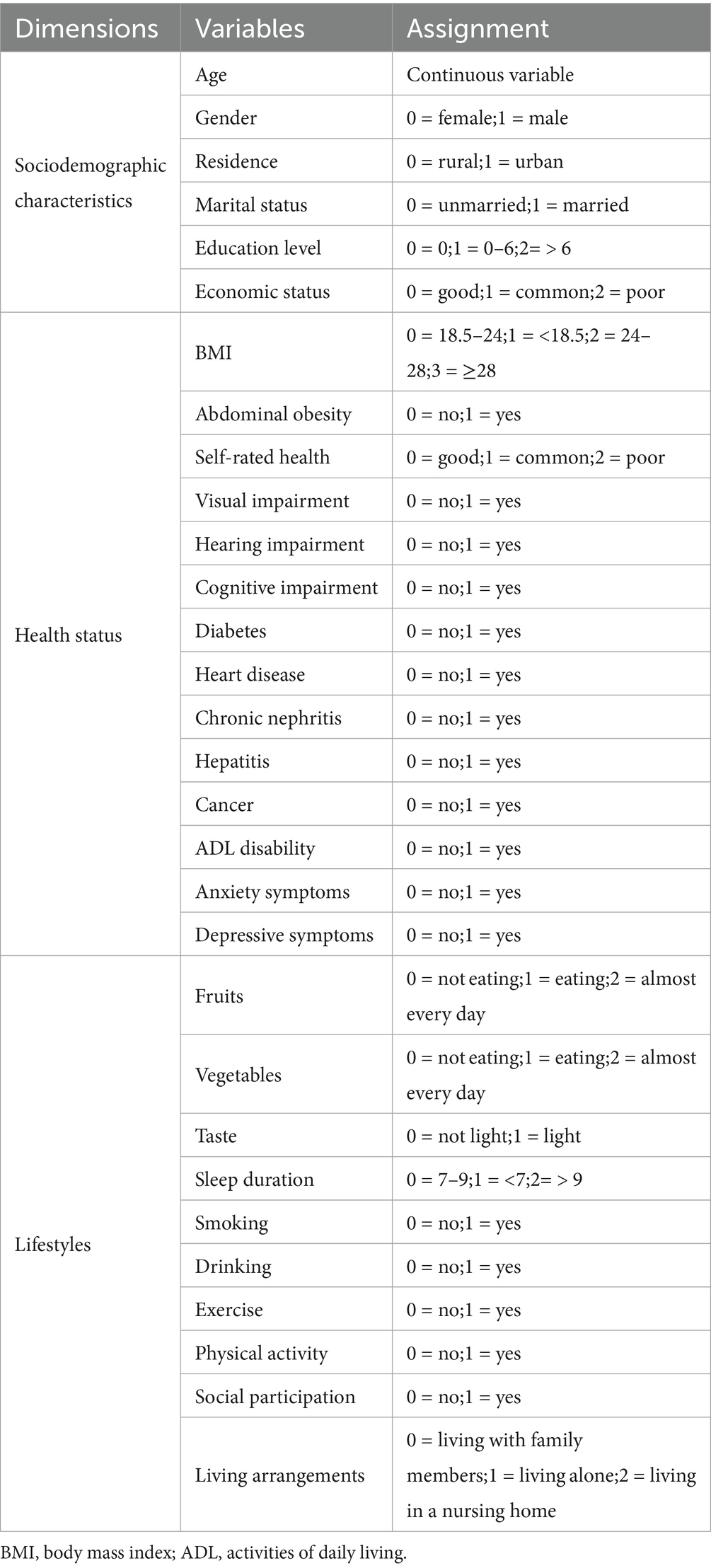
Based on previous research results and the availability of the CLHLS database (28), we considered 30 influencing factors from three dimensions: sociodemographic characteristics, health status, and lifestyles. Specifically, basic demographic characteristics include age, gender, residence, marital status, education level, and economic status. Health status includes body mass index (BMI), abdominal obesity, self-rated health, visual impairment, hearing impairment, cognitive impairment, diabetes, heart disease, chronic nephritis, hepatitis, cancer, activities of daily living (ADL) disability, anxiety, and depressive symptoms. Lifestyles include fruits, vegetables, taste, sleep duration, smoking, drinking, exercise, physical activity, social participation, and living arrangements. Detailed information on the assignment of all variables is provided in Table 1. For some influencing factors with complex measurement methods, the details are as follows:
Through the formula BMI = weight (kg)/[height (m)]2 to calculate BMI to define body obesity, BMI < 18.5 was defined as underweight, 18.5 ≤ BMI < 24 was normal, 24 ≤ BMI < 28 was overweight, and BMI ≥ 28 was obesity. According to previous studies, men with a waist circumference of >85 cm and women with a waist circumference of >80 cm were defined as having abdominal obesity (29). The investigator shone a flashlight at the circle on the eye chart, and the participants were asked to answer whether they could see the circles and distinguish the direction of the notches. There were four options: (1) can see and distinguish. (2) can see but cannot distinguish. (3) cannot see clearly. (4) Blind. If respondents chose (2)–(4), they were assessed as visual impairment (24). Cognitive impairment was assessed by the Mini-Mental State Examination (MMSE) (30). Specifically, the scale consists of 24 questions with a total score ranging from 0 to 30, with higher scores indicating better cognitive functioning. The MMSE cut-off values are set at 16/17 for illiterate individuals, 19/20 for individuals with 1–6 years of education, and 23/24 for individuals with 7 or more years of education. After adjusting for education level, a MMSE score below the cut-off value was defined as cognitive impairment (31). The Katz Activities of Daily Living scale was used to evaluate the ADL for older adults. It includes bathing, dressing, feeding, going to the toilet, moving from bed to chair, and controlling urination and defecation. Failure to independently complete any of those was considered an ADL disability (32). Anxiety symptoms were assessed using the 7-item Generalized Anxiety Disorder (GAD-7) scale, which consists of 7 items and has a total score range of 0 to 21. A higher score indicates more severe anxiety symptoms. Individuals with a GAD-7 score >5 were classified as having anxiety symptoms (33). The 10-item Center for Epidemiological Studies Depression (CESD-10) scale was used to assess depressive symptoms in older adults. The scale consists of 10 items, with a total score ranging from 0 to 30. Individuals with a depression score of ≥10 were defined as having depressive symptoms (34). Respondents were asked whether they were involved in social activities, and their responses were classified as “yes” or “no.” Social participation was defined as the presence or absence of such participation (35).
2.3 Life satisfaction
LS was assessed by the question, “How satisfied are you with your life as a whole now?” (27). The answers included five options: (1) Very satisfied. (2) Satisfied. (3) Average. (4) Dissatisfied. (5) Very dissatisfied. (1), (2), and (3) were combined as satisfied as the more positive responses to LS, and the more negative responses (4) and (5) were combined as dissatisfied. LS represents an individual’s evaluation of the overall state and quality of life, and it has been widely used currently (15, 27).
2.4 Statistical analysis
Kolmogorov–Smirnov test was used to assess the normality of continuous variables. When p > 0.05, the distribution of continuous variables was considered to conform to a normal distribution. Bartlett test was used to assess the homogeneity of variance of continuous variables. When p > 0.05, it was considered to satisfy the homogeneity of variance. Continuous variables that conformed to normality were described by mean and standard deviation (M ± SD), and categorical variables were expressed as frequencies and percentages [n(%)]. After testing for normalcy and variance homogeneity, two independent sample t-tests were used to compare the differences in continuous variables between different levels of LS. The Chi-square test was used to compare the differences in categorical variables between different levels of LS. A multivariate logistic regression model was used to analyze the relationship between each variable and LS. We report the odds ratio (OR) value and 95% confidence interval (CI) for all variables. To further determine the importance of factors influencing the LS of hypertensive patients, we included the variables that were significant (p < 0.05) in the logistic regression analysis into the RF and ranked the importance of the variables based on the decrease in the Gini coefficient. All data analyses were completed based on the software R 4.3.0, and variables with p values <0.05 (two-sided) were considered to indicate a statistically significant difference.
2.5 Random forest
RF is a machine-learning method based on classification trees. It is mainly used for classification and regression tasks, which improves the accuracy and stability of predictions by constructing multiple decision trees and integrating the prediction results (36). The basic principle is to use Bootstrap sampling to generate multiple training subsets, each of which independently trains a decision tree, while randomly selecting some features at each node split to increase the diversity of the model. Algorithmically, the RF derives the final prediction by classifying or regressing the prediction results of each decision tree. This method can effectively handle non-linear problems and is resistant to overfitting, as well as being able to handle large numbers of features and data. The model has strong generalization capabilities, and its prediction results are generally superior to other machine algorithms (37).
3 Results
3.1 Results of univariate analysis
3.1.1 Sociodemographic characteristics and life satisfaction of hypertensive patients
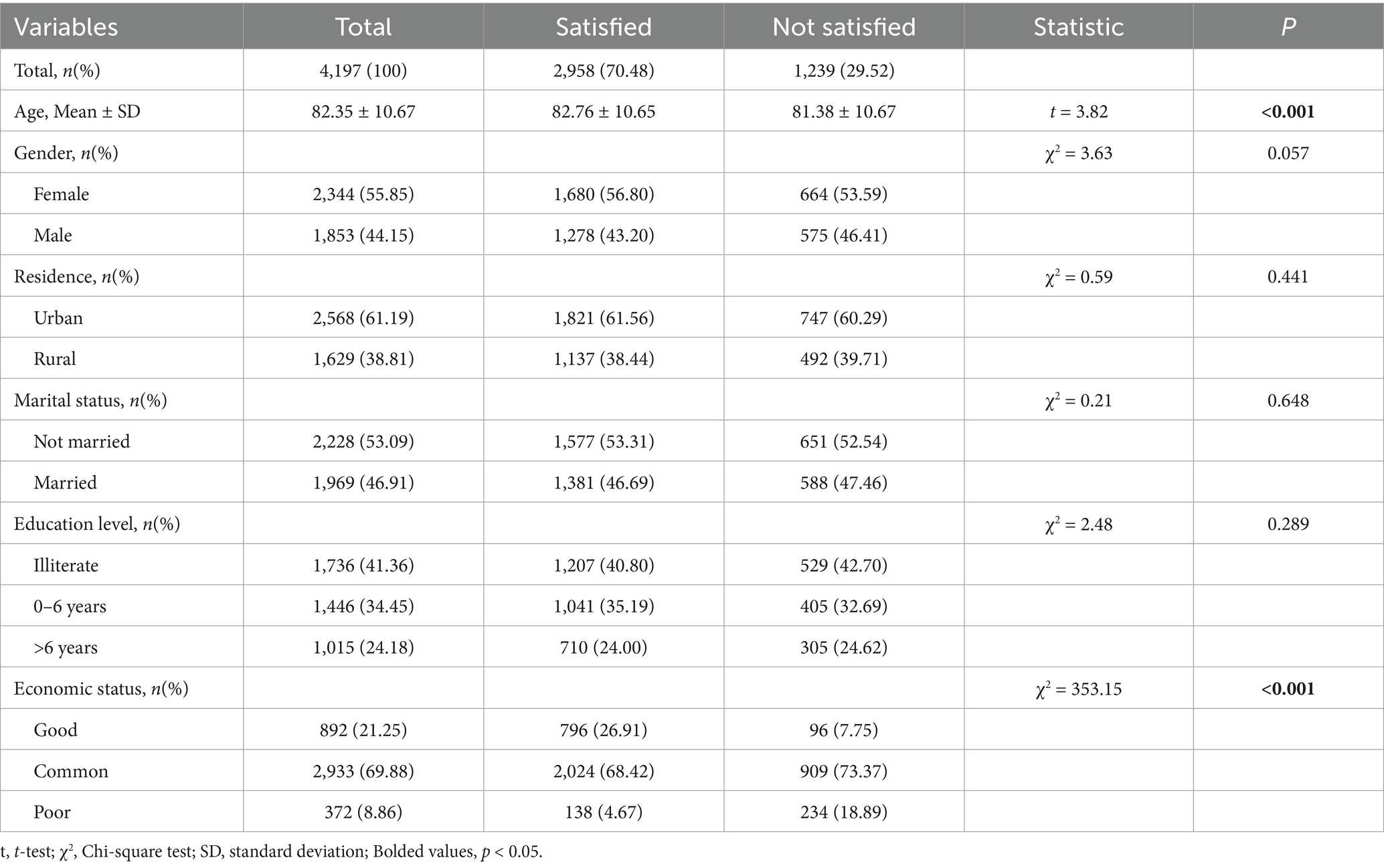
Table 2 shows the descriptive results of the sociodemographic characteristics of hypertensive patients and the results of the univariate analysis of their relationship with LS. Of the 4,197 participants, 2,958 (70.48%) reported being satisfied with their current living situation. The average age of the participants was 82.35 ± 10.67, of which 55.85% were female, 61.19% lived in urban areas, and 53.09% were unmarried. Only 27.18% of the participants had received more than 6 years of education. Most of the participants had a common level of economic status (69.88%). T-test and chi-square test showed that age and economic status differed significantly (p < 0.05) between different LS levels of hypertensive patients.
3.1.2 Health status and life satisfaction of hypertensive patients
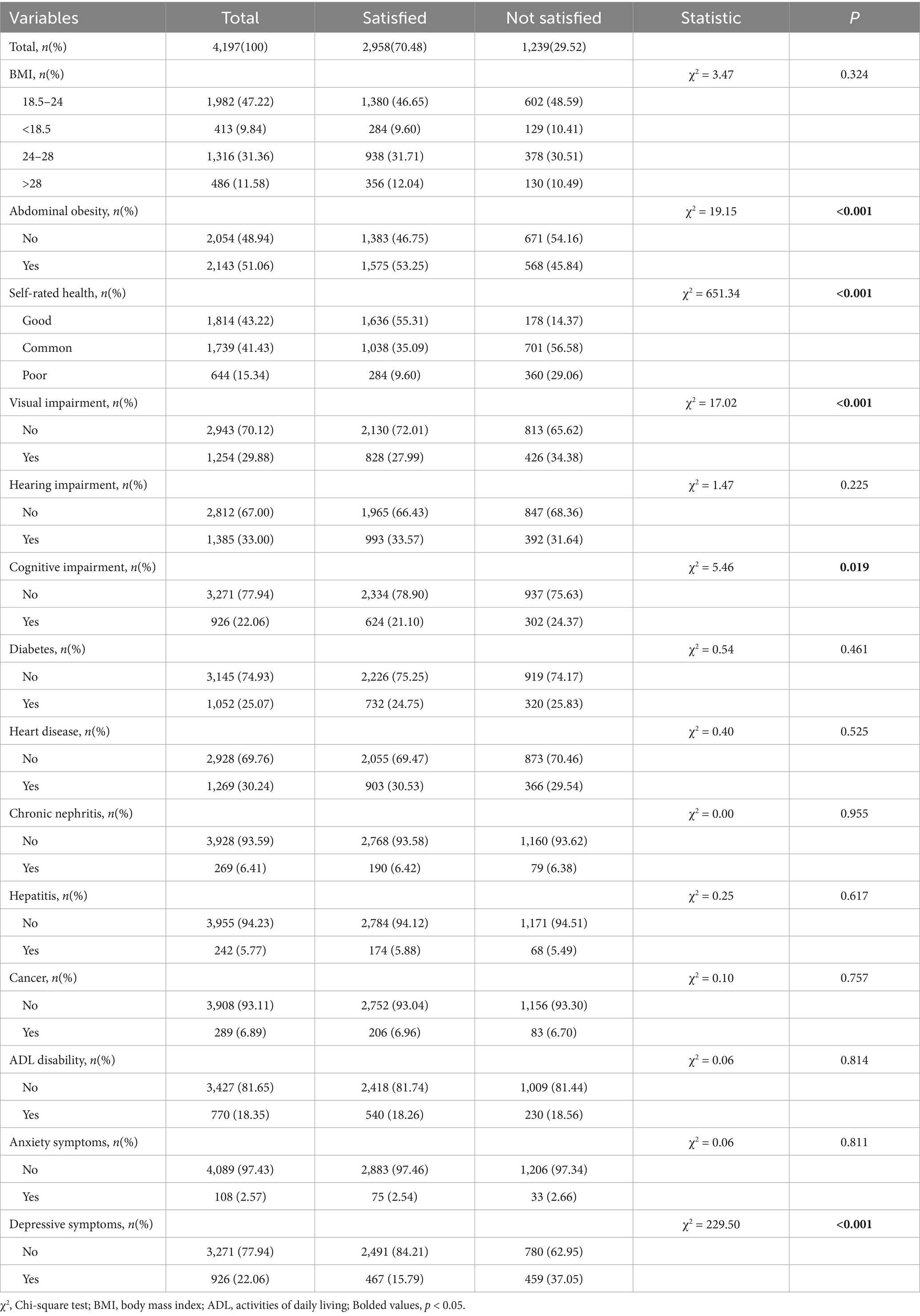
The results of the descriptive analysis of the health status of hypertensive patients and the univariate analysis of their relationships with LS are shown in Table 3. Less than half of the participants (47.22%) had a BMI within the normal range. Among participants, abdominal obesity prevalence reached 51.06%, whereas 43.22% considered their health status to be good. Among all participants, 29.88% had visual impairment, 33% had hearing impairment, and 22.06% had cognitive impairment. Most participants were free of diabetes, heart disease, chronic nephritis, hepatitis, cancer, and ADL disability (74.93, 69.76, 93.59, 94.23, 93.11, and 81.65%) and had no depressive and anxiety symptoms (97.43, 77.94%). The results of the chi-square test showed that abdominal obesity, self-rated health, visual impairment, cognitive impairment, and depressive symptoms were significantly different among hypertensive patients with different levels of LS (p < 0.05).
3.1.3 Lifestyles and life satisfaction of hypertensive patients
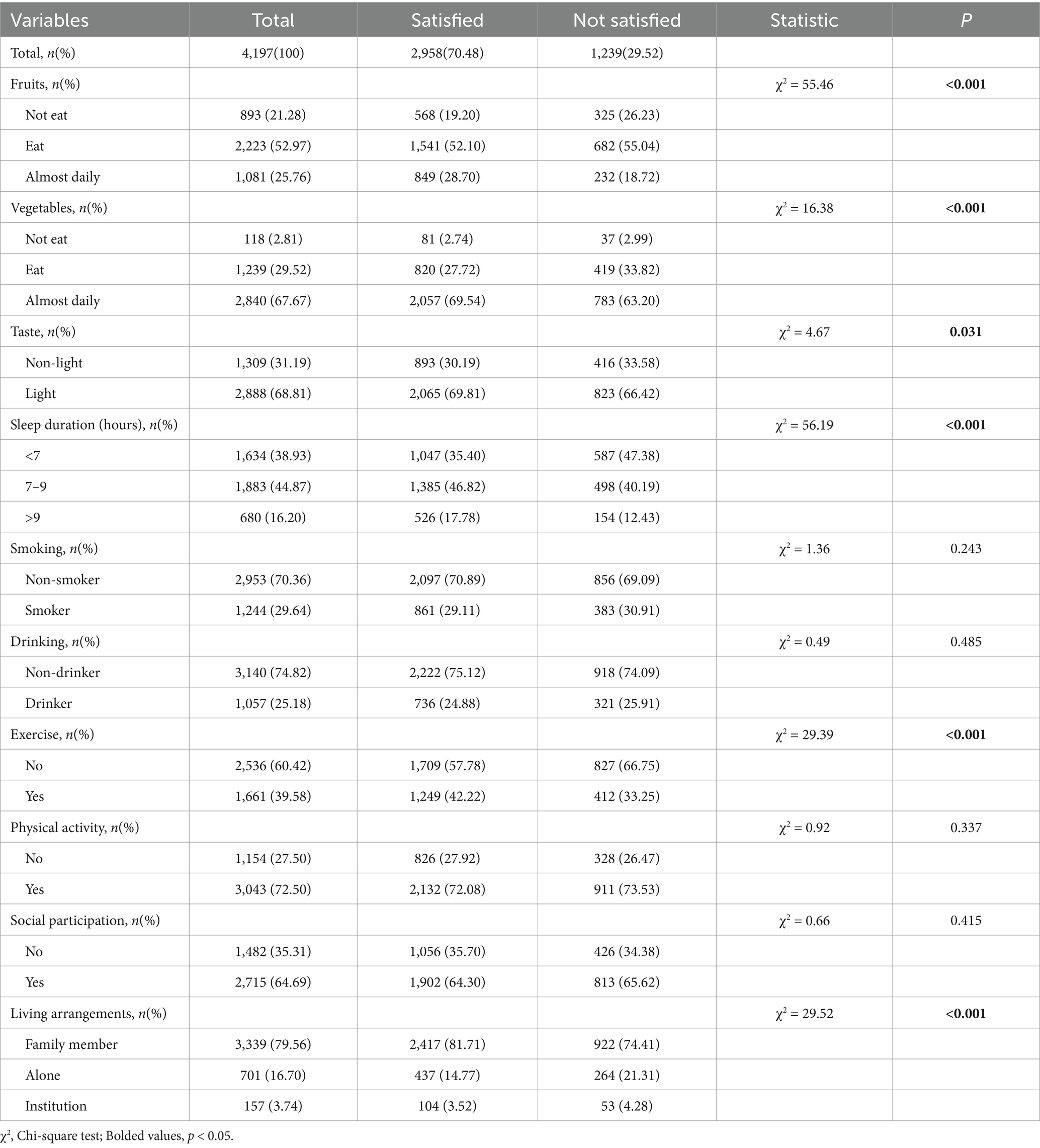
Table 4 shows the descriptive results of the lifestyle of hypertensive patients and the results of univariate analysis of their relationship with LS. Only a few participants did not eat fruits and vegetables (21.28, 2.81%). Among participants, 68.81% had a light taste, and 38.93% did not sleep for more than 7 h a day. The majority of the participants reported no smoking and drinking habits (70.36, 29.64%). Of all participants, only 39.58% had exercise habits, 72.50% performed physical activities, and 64.69% had social participation. Most participants lived with family members (79.56%), while only 16.70% lived alone. The results of the chi-square test showed that there were significant differences (p < 0.05) between the different LS levels of hypertensive patients in terms of fruits, vegetables, taste, sleep duration, exercise, and living arrangements.
3.2 Results of multivariable analysis
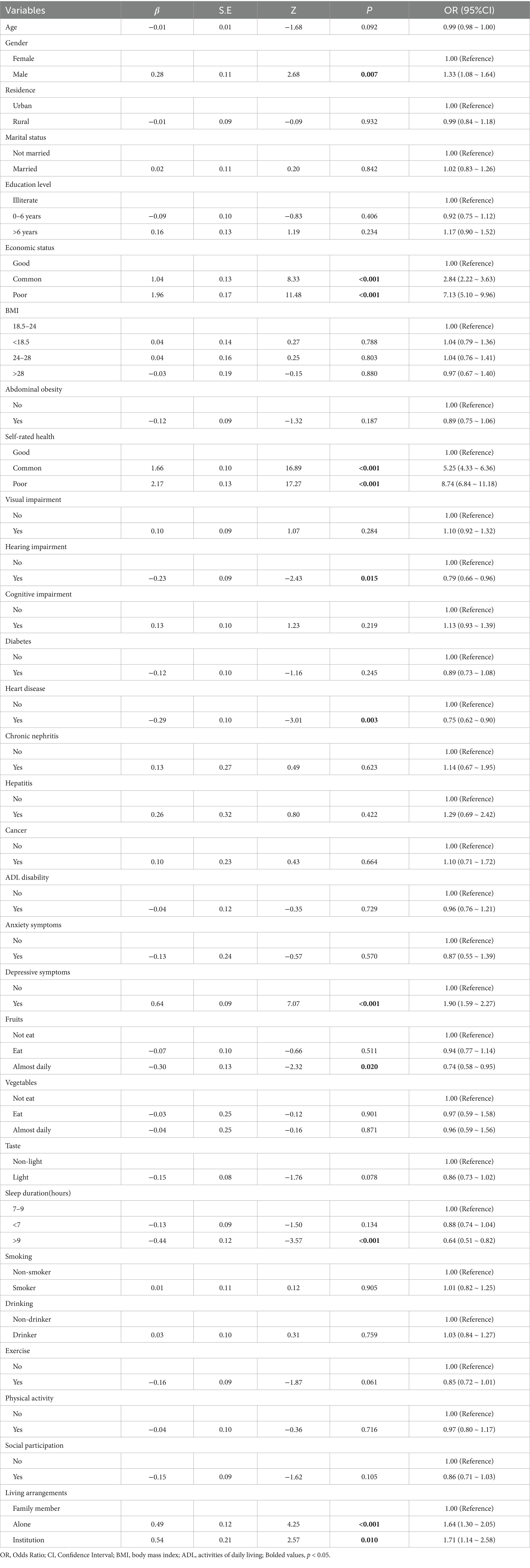
Table 5 shows the results of multifactorial analysis of LS of hypertensive patients. Regression analysis showed that gender, economic status, self-rated health, hearing impairment, heart disease, depressive symptoms, fruits, sleep duration, and living arrangements were independent factors influencing the LS of hypertensive patients (p < 0.05). Compared with females, males had a higher risk of poor LS (OR = 1.33, 95% CI: 1.08 ~ 1.64). Patients with poor economic status had a 7.13-fold higher risk of reporting low LS than those with good economic status (OR = 7.13, 95% CI: 5.10 ~ 9.96). Patients with poor self-rated health were 8.74 times more likely to report low LS than those with good self-rated health (OR = 8.74, 95% CI: 6.84 ~ 11.18). Hypertensive patients who had hearing impairment had higher LS than those with normal hearing (OR = 0.79, 95% CI: 0.66 ~ 0.96). Hypertensive patients with heart disease reported a 25% lower risk of low LS compared to those without heart disease (OR = 0.75, 95% CI:0.62 ~ 0.90), while patients with depressive symptoms reported a 90% increased risk of low LS compared to those who did not show depressive symptoms (OR = 1.90, 95% CI:1.59 ~ 2.27). Patients who ate fruit almost daily and slept more than 9 h were more likely to report high LS (OR = 0.74, 95% CI:0.58 ~ 0.95; OR = 0.64, 95% CI: 0.51 ~ 0.82). Compared with patients living with family members, those living in institutions or living alone had lower LS (OR = 1.71, 95% CI: 1.14 ~ 2.58; OR = 1.64, 95% CI:1.30 ~ 2.05).
3.3 Results of random forest
To further assess the relative importance of the influencing factors, we included the significant influencing variables obtained from the multivariate analysis into the RF and sorted them from high to low according to MeanDecreaseGini. The results are shown in Figure 2 (where the parameters of the RF are ntree = 500 and mtry = 3). The influencing factors were, in descending order, self-rated health, economic status, depressive symptoms, sleep duration, fruits, living arrangements, hearing impairment, heart disease, and gender.
4 Discussion
Using the nationally representative dataset, this study analyzed the prevalence and influencing factors of life dissatisfaction among Chinese older adults with hypertension and developed the RF to rank the importance of these factors. Overall, among all participants, 29.52% of hypertensive patients reported being dissatisfied with their lives. The study showed that the LS of hypertensive patients is influenced by variables in multiple dimensions. The final RF results showed that the key factors influencing the LS of hypertensive patients were, in order of importance, self-rated health, economic status, depressive symptoms, sleep duration, fruits, living arrangements, hearing impairment, heart disease, and gender.
Similar to the result of another study (38), the better the self-rated health, the higher the LS of the older adults. Self-rated health can be understood as a brief statement about how different aspects of health are combined within an individual’s perception (39). Due to its inclusiveness and non-definitive nature, it has been widely used as one of the most commonly used indicators of health status in various studies (40–42). Recent research has shown that subjective attitude towards health status can indirectly reflect an individual’s satisfaction with their current life (43). For hypertensive patients, the better their self-rated health, the higher their satisfaction with their health, and the less subjectively disturbed by the disease than those with poor self-rated health. As a result, they tend to have a better psychological state and a positive attitude towards life, so they are able to optimistically face the adverse effects of hypertension and other complications in their lives.
Our study found that there is a significant correlation between the economic situation and LS of hypertensive patients, which is consistent with the results of a previous study (44). Hypertension is a chronic disease that requires long-term treatment and control. Patients with hypertension need to take medication continuously, purchase medical devices, and undergo regular medical examinations. At the same time, they also need lifestyle adjustments such as a healthy diet and regular exercise. Financial support plays a significant role in all of these aspects. Poor economic status may mean that patients have limited access to high-quality medical services and daily care, which in turn leads to physical backwardness and psychological impairment in older adults. Some of the medical expenses that are necessary for hypertension will further increase the financial burden on poor people, thus reducing their LS.
The study also demonstrated a significant correlation between depressive symptoms and low LS in older adults with hypertension, which is also supported by a previous study (45). Depression is a psychological state of sadness, helplessness, and melancholy, with mood changes and somatic symptoms being its most common manifestations (46). Patients with depressive symptoms often lack positive emotions, lose enthusiasm and interest in life, and therefore have a reduced perception of well-being, showing a decrease in LS. At the same time, depression can be accompanied by sleep disorders and loss of appetite, which exacerbate physical fatigue and lead to a decline in functions such as the digestive and immune systems. A prolonged depressive state can cause serious damage to mental health and various bodily functions, thereby increasing the risk of developing various chronic diseases. A recent study provides preclinical evidence that lycopene may serve as a potential antidepressant, which provides an effective way to develop novel antidepressant therapies and improve the prognosis and LS of hypertensive patients (47).
In our study, patients with long sleep duration were more likely to report high LS, which may resonate with previous studies (48, 49). As one of the response indicators of sleep quality, there is a strong bidirectional relationship between sleep duration and LS (50). Studies have shown that adequate sleep helps to restore body functions and maintain metabolism, thus promoting the improvement of overall health (51, 52). For hypertensive patients, an appropriate amount of sleep can reduce their risk of secondary cardiovascular and cerebrovascular diseases and other age-related diseases, helping them control blood pressure and improve their prognosis (53). Sleep quality is also closely related to the gut microbiota. Gut microbes have been demonstrated to regulate blood pressure through immune, neural, and endocrine mechanisms (54, 55). Longer sleep durations provide optimal conditions for these microbes to influence bodily functions, which, to some extent, alleviates the disease burden of hypertensive patients. Meanwhile, adequate sleep also facilitates the regulation of some mood-related hormones (51), thereby alleviating negative emotions such as anger, anxiety, and tension and promoting mental health. Additionally, sleep can relieve physical and mental fatigue and increase an individual’s vitality. These conclusions all suggest that a longer sleep duration can significantly improve the LS of hypertensive patients. A recent study by Rachmawati et al. (56) demonstrated a significant improvement in sleep quality through hyperbaric oxygen therapy. This suggests a viable approach for managing blood pressure and preventing low life satisfaction in patients with hypertension.
We found that patients who ate fruit every day had a higher level of LS. Fruit intake is an important part of a healthy lifestyle. Numerous studies have shown that fruit has an undeniable effect on promoting physical health (57–60). Fruits are rich in a variety of vitamins, minerals, and other essential nutrients for the body, which can fight oxidation, promote digestion, and lower cholesterol, thereby helping hypertensive patients control blood pressure and prevent the occurrence of other chronic cardiovascular diseases (61). At the same time, eating fruits can also promote the improvement of mental health, which is also related to the large amount of vitamin B, vitamin C, antioxidants, carotenoids, and other substances in fruits (62). These substances may relieve stress, anxiety, tension, and depression by lowering the level of stress hormones in the body so as to promote the level of mental health of individuals (57, 62). Therefore, fruit plays a significant role in regulating blood pressure and enhancing overall life satisfaction. It is worth noting that the mechanism and effect of fruit on blood pressure regulation can vary depending on the type of fruit. Flavonoid-rich fruits such as citrus can inhibit the activity of angiotensin-converting enzyme (ACE) and improve vascular endothelial function (63, 64). They can also help regulate gut microbiota, contributing to blood pressure regulation. Berry fruits are rich in anthocyanins, which can activate endothelial nitric oxide synthase (eNOS) to promote vasodilation. They can also change the diversity and composition of gut microorganisms, promote the production of short-chain fatty acids (SCFAs), and thus exert a blood pressure-lowering effect (65, 66). In addition to the above mechanisms, fruits rich in dietary fiber, such as drupes, can improve the elasticity of blood vessel walls, thereby reducing blood vessel resistance and improving insulin sensitivity (67, 68). Moreover, the timing of fruit intake also has a different effect on blood pressure regulation. Eating fruit before meals can help hypertensive patients take better advantage of the satiating effects of dietary fiber, leading to reduced salt and fat intake. This can help them lose weight and protect cardiovascular function, which are all crucial measures to control blood pressure (69).
In addition to the above-mentioned key factors, there are a number of other factors that also played an important role in our study. For example, our study proved that participants living with their families have higher LS. This is similar to previous research (70). We speculate that the possible reason may be influenced by the Chinese family culture of filial piety and love for older adults. Family members can provide emotional support for older adults with hypertension, helping them to actively cope with difficulties and challenges in life through companionship, encouragement, and comfort. They may do so by taking care of their diets and daily lives and accompanying them to participate in social activities such as walking, fitness, and gatherings, which not only provides them with more opportunities to exercise but also makes them feel cared for and warmed up, thereby reducing feelings of loneliness and anxiety.
Hearing impairment is defined as a decrease in hearing thresholds at different frequencies, unilaterally or bilaterally (71). It has a huge negative impact on daily life. However, our study found that respondents with hearing impairment had higher LS, which is inconsistent with previous research results (72, 73). We speculate that although people with hearing impairment often feel inadequate in daily life and social interactions due to difficulties in speech recognition and output, to some extent, such impairments can help them isolate themselves from the interference of unpleasant sounds and improve their concentration. At the same time, they also enjoy higher social welfare and subsidies and more social care. These factors may lead to higher LS.
Similarly, we found that respondents with heart disease were more likely to report satisfaction with life, which may be related to a range of secondary effects of the disease. While heart disease places a heavy burden on the health of patients, it also increases their appreciation of healthy living. They tend to adopt more meticulous daily care and a more cautious lifestyle, such as careful regulation of diet and maintenance of calmness, as well as intentional avoidance of unhealthy lifestyles, which to some extent improves their physical and mental health. In addition, the care and support of society may also give them a greater sense of well-being and belonging.
Additionally, we found that gender also has a large impact on LS. Current studies are divided on this view (74, 75). In our study, male older adults with hypertension had lower LS than females. The reason may be related to the feudal social culture of “male goes out to work while female looks after the house” in the old society. In family life, the male’s role as a “pillar” usually leads them to bear heavier financial responsibilities and face greater mental pressure. After falling ill, their physical function declines, their sense of social value and self-esteem decreases, while psychological pressure further increases, which in turn leads to a decline in LS.
5 Limitation
Undeniably, there are still some limitations in our study that should be acknowledged. First, this study is a cross-sectional study based on the CLHLS database, making it impossible to establish the in-depth causal relationship between these influencing factors and LS. Second, most of the data for the variables came from self-reported questions, and we have to consider the impact of recall bias and subjective factors of the participants on the authenticity of the data. In addition, due to the limitations of the survey content of the database, many variables that may be important were not included in this study. For example, the intake of some medications also has a direct effect on blood pressure, which may in turn affect LS of hypertensive patients, such as those associated with thyroid disorders (76, 77). Further consideration of rich variables and diversity of measurement indicators is worth undertaking in future research.
6 Conclusion
In summary, this study used cross-sectional data published by CLHLS 2018 to analyze the influencing factors of LS in older adults with hypertension in China from three aspects: sociodemographic characteristics, health status, and lifestyles. The RF was used further to rank the importance of each significant influencing factor. These findings are of great guiding significance for the prevention and intervention of life dissatisfaction among older adults with hypertension. We advocate that policymakers and relevant health practitioners should focus on hypertensive patients with poor self-rated health, poor economic status, depressive symptoms, short sleep duration, no fruit consumption, living alone or in an institution, hearing impairment, and heart disease, and female hypertensive patients when formulating policies and providing clinical care.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YW: Conceptualization, Formal analysis, Methodology, Writing – review & editing. ZC: Investigation, Validation, Visualization, Writing – original draft. HF: Software, Validation, Visualization, Writing – original draft. SC: Data curation, Formal analysis, Visualization, Writing – original draft. XW: Software, Writing – original draft. TN: Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank the Chinese Longitudinal Healthy Longevity Survey (CLHLS) research and all participant involved in this study for their contribution sincerely.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Jakovljevic, M. Population ageing alongside health care spending growth. Srp Arh Celok Lek. (2017) 145:534–9. doi: 10.2298/sarh160906113j
2. Zhang, X, Huang, J, and Luo, Y. The effect of the universal two-child policy on medical insurance funds with a rapidly ageing population: evidence from China's urban and rural Residents' medical insurance. BMC Public Health. (2021) 21:1444. doi: 10.1186/s12889-021-11367-7
3. Kulkarni, S, Glover, M, Kapil, V, Abrams, SML, Partridge, S, McCormack, T, et al. Management of Hypertensive Crisis: British and Irish hypertension society position document. J Hum Hypertens. (2023) 37:863–79. doi: 10.1038/s41371-022-00776-9
4. Jain, V, Al Rifai, M, Khan, SU, Kalra, A, Rodriguez, F, Samad, Z, et al. Association between social vulnerability index and cardiovascular disease: a behavioral risk factor surveillance system study. J Am Heart Assoc. (2022) 11:e024414. doi: 10.1161/jaha.121.024414
5. Kearney, PM, Whelton, M, Reynolds, K, Muntner, P, Whelton, PK, and He, J. Global burden of hypertension: analysis of worldwide data. Lancet. (2005) 365:217–23. doi: 10.1016/s0140-6736(05)17741-1
6. National Center for Cardiovascular Diseases. China Cardiovascular Health and Disease Report 2023. (2023). p. 4.
7. James, PA, Oparil, S, Carter, BL, Cushman, WC, Dennison-Himmelfarb, C, Handler, J, et al. 2014 evidence-based guideline for the Management of High Blood Pressure in adults: report from the panel members appointed to the eighth joint National Committee (Jnc 8). JAMA. (2014) 311:507–20. doi: 10.1001/jama.2013.284427
8. Kario, K, Okura, A, Hoshide, S, and Mogi, M. The who global report 2023 on hypertension warning the emerging hypertension burden in globe and its treatment strategy. Hypertens Res. (2024) 47:1099–102. doi: 10.1038/s41440-024-01622-w
9. Manosroi, W, and Williams, GH. Genetics of human primary hypertension: focus on hormonal mechanisms. Endocr Rev. (2019) 40:825–56. doi: 10.1210/er.2018-00071
10. Doyle, AE. Hypertension and vascular disease. Am J Hypertens. (1991) 4:103s–6s. doi: 10.1093/ajh/4.2.103s
11. Santisteban, MM, Iadecola, C, and Carnevale, D. Hypertension, neurovascular dysfunction, and cognitive impairment. Hypertension. (2023) 80:22–34. doi: 10.1161/hypertensionaha.122.18085
12. Rayamajhi, S, Wang, L, Dhaka, P, Atti, V, Ling, X, and Wang, D. Hypertension and kidney disease: effect of intensive blood pressure intervention. J Hypertens. (2018) 36:e289. doi: 10.1097/01.hjh.0000539842.15933.af
13. Lv, R, Yang, L, Li, J, Wei, X, Ren, Y, Wang, W, et al. Relationship between social participation and life satisfaction in community-dwelling older adults: multiple mediating roles of depression and cognitive function. Arch Gerontol Geriatr. (2024) 117:105233. doi: 10.1016/j.archger.2023.105233
14. Rosella, LC, Fu, L, Buajitti, E, and Goel, V. Death and chronic disease risk associated with poor life satisfaction: a population-based cohort study. Am J Epidemiol. (2019) 188:323–31. doi: 10.1093/aje/kwy245
15. Boccaccio, DE, Cenzer, I, and Covinsky, KE. Life satisfaction among older adults with impairment in activities of daily living. Age Ageing. (2021) 50:2047–54. doi: 10.1093/ageing/afab172
16. Wu, W, Shang, Y, Calderón-Larrañaga, A, Rizzuto, D, Saadeh, M, Dove, A, et al. Association of Life Satisfaction with disability-free survival: role of chronic diseases and healthy lifestyle. Age Ageing. (2021) 50:1657–65. doi: 10.1093/ageing/afab086
17. Li, C, Chi, I, Zhang, X, Cheng, Z, Zhang, L, and Chen, G. Urban and rural factors associated with life satisfaction among older Chinese adults. Aging Ment Health. (2015) 19:947–54. doi: 10.1080/13607863.2014.977767
18. Jiang, C, Chow, JC, Zhou, L, Song, H, and Shi, J. Community support, social isolation and older Adults' life satisfaction: evidence from a National Survey in China. Aging Ment Health. (2024) 28:849–57. doi: 10.1080/13607863.2023.2277871
19. Song, H, and Li, Z. Community-based service, psychological resilience and life satisfaction among Chinese older adults: a longitudinal study. Geriatr Nurs. (2023) 54:148–54. doi: 10.1016/j.gerinurse.2023.09.004
20. Wang, RS, Huang, YN, Wahlqvist, ML, Wan, TTH, Tung, TH, and Wang, BL. The combination of physical activity with fruit and vegetable intake associated with life satisfaction among middle-aged and older adults: a 16-year population-based cohort study. BMC Geriatr. (2024) 24:41. doi: 10.1186/s12877-023-04563-0
21. Zhu, W, Wang, Y, Tang, J, and Wang, F. Sleep quality as a mediator between family function and life satisfaction among Chinese older adults in nursing home. BMC Geriatr. (2024) 24:379. doi: 10.1186/s12877-024-04996-1
22. Wang, S, Wang, Y, Wang, D, Yin, Y, Wang, Y, and Jin, Y. An improved random Forest-based rule extraction method for breast Cancer diagnosis. Appl Soft Comput. (2020) 86:105941. doi: 10.1016/j.asoc.2019.105941
23. Guo, L, Wang, Z, Du, Y, Mao, J, Zhang, J, Yu, Z, et al. Random-Forest algorithm based biomarkers in predicting prognosis in the patients with hepatocellular carcinoma. Cancer Cell Int. (2020) 20:251. doi: 10.1186/s12935-020-01274-z
24. Liu, Y, Xu, Y, Yang, X, Miao, G, Wu, Y, and Yang, S. The prevalence of anxiety and its key influencing factors among the elderly in China. Front Psych. (2023) 14:1038049. doi: 10.3389/fpsyt.2023.1038049
25. Aihemaitijiang, S, Zhang, L, Ye, C, Halimulati, M, Huang, X, Wang, R, et al. Long-term high dietary diversity maintains good physical function in Chinese elderly: a cohort study based on Clhls from 2011 to 2018. Nutrients. (2022) 14:730. doi: 10.3390/nu14091730
26. Zhai, X, Zhou, Z, Liu, G, Lu, J, Zhao, Y, Cao, D, et al. Catastrophic health expenditure of households with hypertension: a comparative study in China. Front Public Health. (2023) 11:1176170. doi: 10.3389/fpubh.2023.1176170
27. Liu, Y, Liu, J, Zhou, S, Xu, X, Cheng, Y, Yi, Y, et al. Life satisfaction and its influencing factors of middle-aged and elderly stroke patients in China: a National Cross-Sectional Survey. BMJ Open. (2022) 12:e059663. doi: 10.1136/bmjopen-2021-059663
28. Kim, ES, Delaney, SW, Tay, L, Chen, Y, Diener, ED, and Vanderweele, TJ. Life satisfaction and subsequent physical, behavioral, and psychosocial health in older adults. Milbank Q. (2021) 99:209–39. doi: 10.1111/1468-0009.12497
29. Liu, Z, Yang, H, Chen, S, Cai, J, and Huang, Z. The association between body mass index, waist circumference, waist-hip ratio and cognitive disorder in older adults. J Public Health (Oxf). (2019) 41:305–12. doi: 10.1093/pubmed/fdy121
30. Hu, Y, Peng, W, Ren, R, Wang, Y, and Wang, G. Sarcopenia and mild cognitive impairment among elderly adults: the first longitudinal evidence from Charls. J Cachexia Sarcopenia Muscle. (2022) 13:2944–52. doi: 10.1002/jcsm.13081
31. Li, H, Jia, J, and Yang, Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/jad-160119
32. Gong, J, Wang, G, Wang, Y, Chen, X, Chen, Y, Meng, Q, et al. Nowcasting and forecasting the care needs of the older population in China: analysis of data from the China health and retirement longitudinal study (Charls). Lancet Public Health. (2022) 7:e1005–13. doi: 10.1016/s2468-2667(22)00203-1
33. Löwe, B, Decker, O, Müller, S, Brähler, E, Schellberg, D, Herzog, W, et al. Validation and standardization of the generalized anxiety disorder screener (gad-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
34. Li, H, Zheng, D, Li, Z, Wu, Z, Feng, W, Cao, X, et al. Association of Depressive Symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Netw Open. (2019) 2:e1916591. doi: 10.1001/jamanetworkopen.2019.16591
35. Sun, J, and Lyu, S. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. (2020) 274:399–404. doi: 10.1016/j.jad.2020.05.091
36. Hu, J, and Szymczak, S. A review on longitudinal data analysis with random Forest. Brief Bioinform. (2023) 24:bbad002. doi: 10.1093/bib/bbad002
37. Deo, RC. Machine learning in medicine. Circulation. (2015) 132:1920–30. doi: 10.1161/circulationaha.115.001593
38. Iadecola, C, and Gottesman, RF. Neurovascular and cognitive dysfunction in hypertension. Circ Res. (2019) 124:1025–44. doi: 10.1161/circresaha.118.313260
39. Jylhä, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. (2009) 69:307–16. doi: 10.1016/j.socscimed.2009.05.013
40. Au, N, and Johnston, DW. Self-assessed health: what does it mean and what does it Hide? Soc Sci Med. (2014) 121:21–8. doi: 10.1016/j.socscimed.2014.10.007
41. Cislaghi, B, and Cislaghi, C. Self-rated health as a valid Indicator for health-equity analyses: evidence from the Italian health interview survey. BMC Public Health. (2019) 19:533. doi: 10.1186/s12889-019-6839-5
42. Wu, S, Wang, R, Zhao, Y, Ma, X, Wu, M, Yan, X, et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. (2013) 13:320. doi: 10.1186/1471-2458-13-320
43. Rubin, S, and Tomaszewski, M. Self-rated health in hypertension: navigating the complexities of cardiovascular risk prediction. J Hypertens. (2024) 42:1521–2. doi: 10.1097/hjh.0000000000003785
44. Chen, C, Song, J, Xu, X, Zhou, L, Wang, Y, and Chen, H. Analysis of influencing factors of economic burden and medical service utilization of diabetic patients in China. PLoS One. (2020) 15:e0239844. doi: 10.1371/journal.pone.0239844
45. Lee, SW, Choi, JS, and Lee, M. Life satisfaction and depression in the oldest old: a longitudinal study. Int J Aging Hum Dev. (2020) 91:37–59. doi: 10.1177/0091415019843448
46. Alexopoulos, GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/s0140-6736(05)66665-2
47. Xu, H, Wang, Y, Geng, D, Chen, F, Chen, Y, Niwenahisemo, LC, et al. Lycopene alleviates depression-like behavior in chronic social defeat stress-induced mice by promoting synaptic plasticity via the Bdnf-Trkb pathway. Food Sci Nutr. (2025) 13:e70003. doi: 10.1002/fsn3.70003
48. Pagan, R. Sleep duration, life satisfaction and disability. Disabil Health J. (2017) 10:334–43. doi: 10.1016/j.dhjo.2016.10.005
49. Cao, Y, Yang, Z, Yu, Y, and Huang, X. Physical activity, sleep quality and life satisfaction in adolescents: a cross-sectional survey study. Front Public Health. (2022) 10:1010194. doi: 10.3389/fpubh.2022.1010194
50. Zhu, C, Zhou, L, Zhang, X, and Walsh, CA. Reciprocal effects between sleep quality and life satisfaction in older adults: the mediating role of health status. Healthcare (Basel). (2023) 11:912. doi: 10.3390/healthcare11131912
51. Zhi, TF, Sun, XM, Li, SJ, Wang, QS, Cai, J, Li, LZ, et al. Associations of sleep duration and sleep quality with life satisfaction in elderly Chinese: the mediating role of depression. Arch Gerontol Geriatr. (2016) 65:211–7. doi: 10.1016/j.archger.2016.03.023
52. Shin, JE, and Kim, JK. How a good sleep predicts life satisfaction: the role of zero-sum beliefs about happiness. Front Psychol. (2018) 9:1589. doi: 10.3389/fpsyg.2018.01589
53. Korostovtseva, L, Bochkarev, M, and Sviryaev, Y. Sleep and cardiovascular risk. Sleep Med Clin. (2021) 16:485–97. doi: 10.1016/j.jsmc.2021.05.001
54. O'Donnell, JA, Zheng, T, Meric, G, and Marques, FZ. The gut microbiome and hypertension. Nat Rev Nephrol. (2023) 19:153–67. doi: 10.1038/s41581-022-00654-0
55. Hossain, MI, Islam, R, Islam Mimi, S, Ahmed Jewel, Z, and Ali, HU. Gut microbiota gut microbiota: succinct overview of impacts on human physique and current research status with future aspects. Int J Adv Life Sci Res. (2020) 3:1–10. doi: 10.31632/ijalsr.20.v03i02.001
56. Rachmawati, DS, Chabibah, N, and Mayasari, AC. Hyperbaric oxygen therapy on Elderly’s sleep quality: a pre experimental study. Int J Adv Life Sci Res. (2025) 8:154–60. doi: 10.31632/ijalsr.2025.v08i01.014
57. Slavin, JL, and Lloyd, B. Health benefits of fruits and vegetables. Adv Nutr. (2012) 3:506–16. doi: 10.3945/an.112.002154
58. Liu, RH. Health-promoting components of fruits and vegetables in the diet. Adv Nutr. (2013) 4:384s–92s. doi: 10.3945/an.112.003517
59. Dreher, ML. Whole fruits and fruit Fiber emerging health effects. Nutrients. (2018) 10:833. doi: 10.3390/nu10121833
60. Głąbska, D, Guzek, D, Groele, B, and Gutkowska, K. Fruit and vegetable intake and mental health in adults: a systematic review. Nutrients. (2020) 12:115. doi: 10.3390/nu12010115
61. Wang, Y, Gallegos, JL, Haskell-Ramsay, C, and Lodge, JK. Correction to: effects of chronic consumption of specific fruit (berries, Citrus and cherries) on Cvd risk factors: a systematic review and Meta-analysis of randomised controlled trials. Eur J Nutr. (2021) 60:641–2. doi: 10.1007/s00394-020-02456-1
62. Rooney, C, McKinley, MC, and Woodside, JV. The potential role of fruit and vegetables in aspects of psychological well-being: a review of the literature and future directions. Proc Nutr Soc. (2013) 72:420–32. doi: 10.1017/s0029665113003388
63. Lee, S, Youn, K, Lim, G, Lee, J, and Jun, M. In silico docking and in vitro approaches towards Bace1 and Cholinesterases inhibitory effect of Citrus flavanones. Molecules. (2018) 23:509. doi: 10.3390/molecules23071509
64. Alam, MA, Subhan, N, Rahman, MM, Uddin, SJ, Reza, HM, and Sarker, SD. Effect of Citrus flavonoids, Naringin and Naringenin, on metabolic syndrome and their mechanisms of action. Adv Nutr. (2014) 5:404–17. doi: 10.3945/an.113.005603
65. Bell, DR, and Gochenaur, K. Direct vasoactive and Vasoprotective properties of anthocyanin-rich extracts. J Appl Physiol. (1985) (2006) 100:1164–70. doi: 10.1152/japplphysiol.00626.2005
66. Si, X, Bi, J, Chen, Q, Cui, H, Bao, Y, Tian, J, et al. Effect of blueberry anthocyanin-rich extracts on peripheral and hippocampal antioxidant defensiveness: the analysis of the serum fatty acid species and gut microbiota profile. J Agric Food Chem. (2021) 69:3658–66. doi: 10.1021/acs.jafc.0c07637
67. Reynolds, AN, Akerman, A, Kumar, S, Diep Pham, HT, Coffey, S, and Mann, J. Dietary fibre in hypertension and cardiovascular disease management: systematic review and Meta-analyses. BMC Med. (2022) 20:139. doi: 10.1186/s12916-022-02328-x
68. Reynolds, AN, Akerman, AP, and Mann, J. Dietary fibre and whole grains in diabetes management: systematic review and Meta-analyses. PLoS Med. (2020) 17:e1003053. doi: 10.1371/journal.pmed.1003053
69. Appel, LJ, Brands, MW, Daniels, SR, Karanja, N, Elmer, PJ, and Sacks, FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. (2006) 47:296–308. doi: 10.1161/01.Hyp.0000202568.01167.B6
70. Preetz, R. Dissolution of non-cohabiting relationships and changes in life satisfaction and mental health. Front Psychol. (2022) 13:812831. doi: 10.3389/fpsyg.2022.812831
71. Resmerita, I, Cozma, RS, Popescu, R, Radulescu, LM, Panzaru, MC, Butnariu, LI, et al. Genetics of hearing impairment in north-eastern Romania-a cost-effective improved diagnosis and literature review. Genes. (2020) 11:506. doi: 10.3390/genes11121506
72. Ohlenforst, B, Zekveld, AA, Jansma, EP, Wang, Y, Naylor, G, Lorens, A, et al. Effects of hearing impairment and hearing aid amplification on listening effort: a systematic review. Ear Hear. (2017) 38:267–81. doi: 10.1097/aud.0000000000000396
73. Rong, H, Lai, X, Jing, R, Wang, X, Fang, H, and Mahmoudi, E. Association of Sensory Impairments with cognitive decline and depression among older adults in China. JAMA Netw Open. (2020) 3:e2014186. doi: 10.1001/jamanetworkopen.2020.14186
74. Joshanloo, M, and Jovanović, V. The relationship between gender and life satisfaction: analysis across demographic groups and global regions. Arch Womens Ment Health. (2020) 23:331–8. doi: 10.1007/s00737-019-00998-w
75. Calasanti, T, Carr, D, Homan, P, and Coan, V. Gender disparities in life satisfaction after retirement: the roles of leisure, family, and finances. Gerontologist. (2021) 61:1277–86. doi: 10.1093/geront/gnab015
76. Berta, E, Lengyel, I, Halmi, S, Zrínyi, M, Erdei, A, Harangi, M, et al. Hypertension in thyroid disorders. Front Endocrinol. (2019) 10:482. doi: 10.3389/fendo.2019.00482
Keywords: hypertension, life satisfaction, older adults, CLHLS, Cross-Sectional Survey
Citation: Wang Y, Chen Z, Fan H, Cao S, Wang X and Niu T (2025) Key influencing factors analysis on life satisfaction among Chinese older adults with hypertension: a National Cross-Sectional Survey. Front. Public Health. 13:1569935. doi: 10.3389/fpubh.2025.1569935
Edited by:
Adalberto Vieyra, Federal University of Rio de Janeiro, BrazilReviewed by:
Michael Wiblishauser, University of Houston Victoria, United StatesSandeep Poddar, Lincoln University College, Malaysia
Copyright © 2025 Wang, Chen, Fan, Cao, Wang and Niu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tengfei Niu, bml1dGVuZ2ZlaTE5ODYwMzI4QDEyNi5jb20=
 Yazhu Wang
Yazhu Wang Ziyi Chen
Ziyi Chen Heqian Fan
Heqian Fan Shiwei Cao
Shiwei Cao Xiaoyu Wang
Xiaoyu Wang Tengfei Niu
Tengfei Niu