- 1School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 2JSI Research and Training Institute, Inc., Addis Ababa, Ethiopia
Introduction: Infection accounts for about half of all neonatal deaths and it contributes to 37% of neonatal deaths in Sub-Saharan Africa where there is low health facility readiness and the quality of service given at health facilities is low. In this study, we assessed the influence of health posts’ readiness on the care-seeking behavior of mothers of sick young children.
Method: This study analyzed data from a community-based implementation survey conducted by JSI in the two districts of Ethiopia from April 2021 to July 2022. In this study, we enrolled 4,262 and 4,081 mothers with children < 15 months at the baseline and end-line surveys, respectively, of which 508 and 359 infants were diagnosed for illness at 66 and 64 health posts at the baseline and end-line surveys. We used the Service Availability and Readiness Assessment tool to compute the facility readiness score. We used independent sample t-test and logistic regression to see the contributions of facility readiness for care-seeking practices of mothers. AOR at 95% CI and p-value < 0.05 is used to declare a statistically significant association between variables and to control the confounding.
Results: In the end-line survey about 359 sick young infants were identified. And in the baseline survey, 508 young infants were ill. Most of 88.0% sick young infants sought care in the end line compared to 57.3% at the baseline (p < 0.001). The overall summated mean facility readiness score was 69.6%, equivalent to 49.0% of the standardized mean score. This study also highlights rich households (AOR = 2.02; 95% CI: 1.1–3.9), reaching out to health posts (HPs) equipped with materials and supplies (AOR = 1.52; 95% CI: 1.2–1.9), and ANC use (AOR = 2.35; 95%CI: 1.2–4.7) were positively associated with care seeking practice compared to their counterparts.
Conclusion: The study reveals a moderate level of health post-readiness that needs improvement. Health posts readiness, ANC use, parity, and wealth status influenced the care-seeking behavior of mothers for their sick children.
Introduction
Achieving adequate facility readiness to provide specific child health services especially at a population level is a complex process (1). But in concept it can be improved in terms of structural dimensions of quality; which is fulfilling important resources for the betterment of the process and outcome dimensions of quality (2). Facility readiness is an important first step to provide high quality services (3).
Through substantial investments in health facilities, Ethiopia has achieved prominent progress over the last decade in preventing child mortality and morbidity. Sick children benefit from high-impact interventions like integrated community case management (iCCM). However, neonatal mortality is still high (4). This is attributing to poor quality of services and low facility readiness. Lower level health facilities are positioned to improve access to quality child health services but the capacity and the readiness is often low (1).
Infection accounts for about half of all neonatal deaths in countries with the highest neonatal mortality rates. According to the World Health Organization (WHO), more than 2.5 million newborns died worldwide in 2017 due to infections, and there were 1.3–3.9 million cases of neonatal sepsis worldwide in 2018 (5). Infection was identified as a leading cause of mortality in sub-Saharan Africa, contributing to 37% of the 2.1 million neonatal deaths (6). Ethiopia ranks among the top 10 countries in neonatal mortality, with over 100,000 newborn deaths each year. The neonatal mortality rate (NMR) in Ethiopia was 30 deaths per 1,000 live births with no significant decline over the last decade (7, 8).
World Health Organization recommends a simplified regimen (injectable and oral antibiotics) for community-based management of newborns with possible serious bacterial infection (PSBI) when referral to a hospital is not possible (9), which in principle is an effective strategy to treat PSBIs at the community level that leads to high service coverage and a lower case fatality rate (10–14).
However, the coverage of sick newborn care is low due to multiple factors. Among them are a low supply of essential drugs, suboptimal supportive supervision, and poor referral links (15, 16). According to one study, inadequate care is attributed to 60% of disease-related deaths. Moreover, the use of health services has been more influenced by the quality of care (17).
According to the findings of the Lancet Commission for high-quality health, poor-quality service is the cause of 61% of neonatal fatalities (18); and 1.7 million newborn lives could be saved each year by investing in access to quality care for every newborn, everywhere (19).
Implementation of integrated community case management (iCCM) of common childhood illnesses improved the uptake of care for sick young infants (SYIs) aged 0–59 days by improving access and creating demand. However, evidence showed that iCCM programs that are implemented in different settings are usually of low quality and lack standardization in terms of the availability of important resources, including competent service providers (20, 21). In other words the iCCM programs, which have intensive training, supervision, fulfilling equipment, and supply support, provide better quality care (20, 21). Care-seeking for sick and young infants (SYI) from health posts increased significantly in the context of iCCM. However, many reasons exist for not seeking care at health facilities, including lower-level ones such as health posts. Considering the disease as not severe (56.2%), financial constraints (28.6%), being busy to visit health facilities (6.0%), the health facility being closed while visited (3.2%), transportation problems (2.7%), and underestimating the service quality at the nearby health facility (2.2%) are among the prominent reasons for the decline to get care at health facilities (22).
Health facility readiness measures quality in health facilities through interactions of different domains that could assist in visualizing the capacity of health facilities to provide appropriate care and services if different interventions such as iCCM are in place. Neonatal survival remains a primary concern for mothers, and facility readiness plays a critical role in influencing care-seeking behaviors, underpinning maternal confidence in the quality of services available. Consequently, readiness is a key determinant of maternal perceptions of care quality and functions as a pivotal enabler in the complex decision-making process regarding whether, when, and where to seek care. Enhancing facility readiness has the potential to substantially increase maternal health service utilization by fostering trust, alleviating concerns, and improving both perceived and actual service quality (23). A study in low- and middle-income countries indicates higher readiness of health facilities is associated with a higher quality of care for sick children; for every 10% point increase in readiness score, quality increased by about 1% (24). However, health facility readiness at the community level care across the available evidences was inadequate for the management of sick children (25). Not only low facility readiness reported but also, the influence of health facility readiness on mothers’ care-seeking practices for their sick children is not known, especially in the iCCM context; While many strategies including iCCM have been developed to enhance healthcare access for underserved populations at the community level, they often do so with limited emphasis on quality, particularly in terms of facility readiness. Therefore, in this study, we assessed the influence of health posts’ readiness on maternal care-seeking practices for their sick young infants in the context of iCCM in Ethiopia.
Methods
Context
Ethiopia is organized into 12 regional states and two autonomous city administrations, further divided into zones, districts (woredas), and villages (Kebeles which are the lowest administrative units). On the other hand, the healthcare system operates at three levels: primary, secondary, and tertiary. The primary level, consisting of health posts (HPs), health centers (HCs), and primary hospitals, provides community-based services close to residents. Each Kebele has at least one HP staffed by two female health extension workers (HEWs)—low-level healthcare workers with 10-month training mainly on disease prevention and cure to selected diseases. The secondary and tertiary levels focus on curative services and serve as referral centers. This study used data obtained from primary-level health facilities as part of implementation research under the JSI project, conducted between November 2020 and June 2022 in collaboration with woreda health offices and health centers in Lume and Dembecha werdas. The study aimed to improve the care-seeking behavior of mothers for their sick children and the community-level health services through the national iCCM strategy the details of which can be found in previously published works (26, 27). The iCCM is designed to enhance the care-seeking behavior of mothers for their sick children and to improve community-level health services; by linking women to the primary level health facilities. Key implementation strategies included on-site coaching and training for HEWs, facilitated referrals between health posts and health centers, strengthening supply chains, integrating PSBI treatment, and promoting early maternal and newborn care through pregnancy identification, home visits, delivery notifications, and postnatal care visits.
The study was conducted in two woredas (where the JSI project implementation site), in Ethiopia: Dembecha in the Amhara region and Lume in the Oromia region. Dembecha, located 349 km northwest of Addis Ababa, has a population of 129,260, with 13.9% living in urban areas. It includes 31 rural Kebeles, 31 HPs, and 6 HCs. Lume, situated 64 km east of Addis Ababa, has a population of 117,080, with 33.06% urban residents. It comprises 35 rural Kebeles, 35 HPs, and 7 HCs. For the study, 11 health centers and all 66 health posts across both districts were utilized (28),
Data
This study analyzed data obtained from a population-based cross-sectional study involving before and after implementation interviews without a control arm representing the two woredas from two regions of Ethiopia; collected by JSI from 18 April-24 May 2021 for baseline, and from 06 June-09 July 2022 for the end line. The data collection includes household surveys and HP observation assessments. In the household surveys, interviews were done among mothers who had live births within the previous 2–14 months. We used the baseline and end-line data to see the changes in the numbers of sick children who needed treatment and sought care from their mothers for their sickness. The end-line data constituted facility-level and individual-level factors that affect the care-seeking practice of mothers for their sick young infants.
Sampling and data collection
The sample size for all objectives of the project is calculated considering the following assumptions: 95% Confidence level (Zα/2 = 1.96), design effect (D = 1.5), and power of 80%, the proportion (p) 56% of sick children sought medical care (29), and the odds of care seeking among mothers who attended antenatal care (AOR = 1.68, 95% CI: 1.59–1.77); which gives the calculated sample size of 395 sick young infant cases that need care.
The survey used a two-stage stratified cluster sampling method, stratified by administrative regions and woredas. Interviews were conducted with all mothers whose children were under 15 months old. All households with children less than 15 months were recruited and eligible mothers were included in the study. Accordingly, 4,081 mothers with infants 2–14 months were identified and interviewed in the end line survey and 4,262 were in the baseline. Among all interviewed mothers during the end-line survey 359 mothers with sick young infants were identified and interviewed. For the health facility assessment, 11 HC and 64 HPs were included. Data were gathered through face-to-face interviews with mothers. During the interview, household and sociodemographic characteristics of mothers, awareness, and access to health services, and experiences of mothers related to the use of maternal health services were collected. The questionnaire used for the interview was translated into local languages (Amharic and Afan-Oromo).
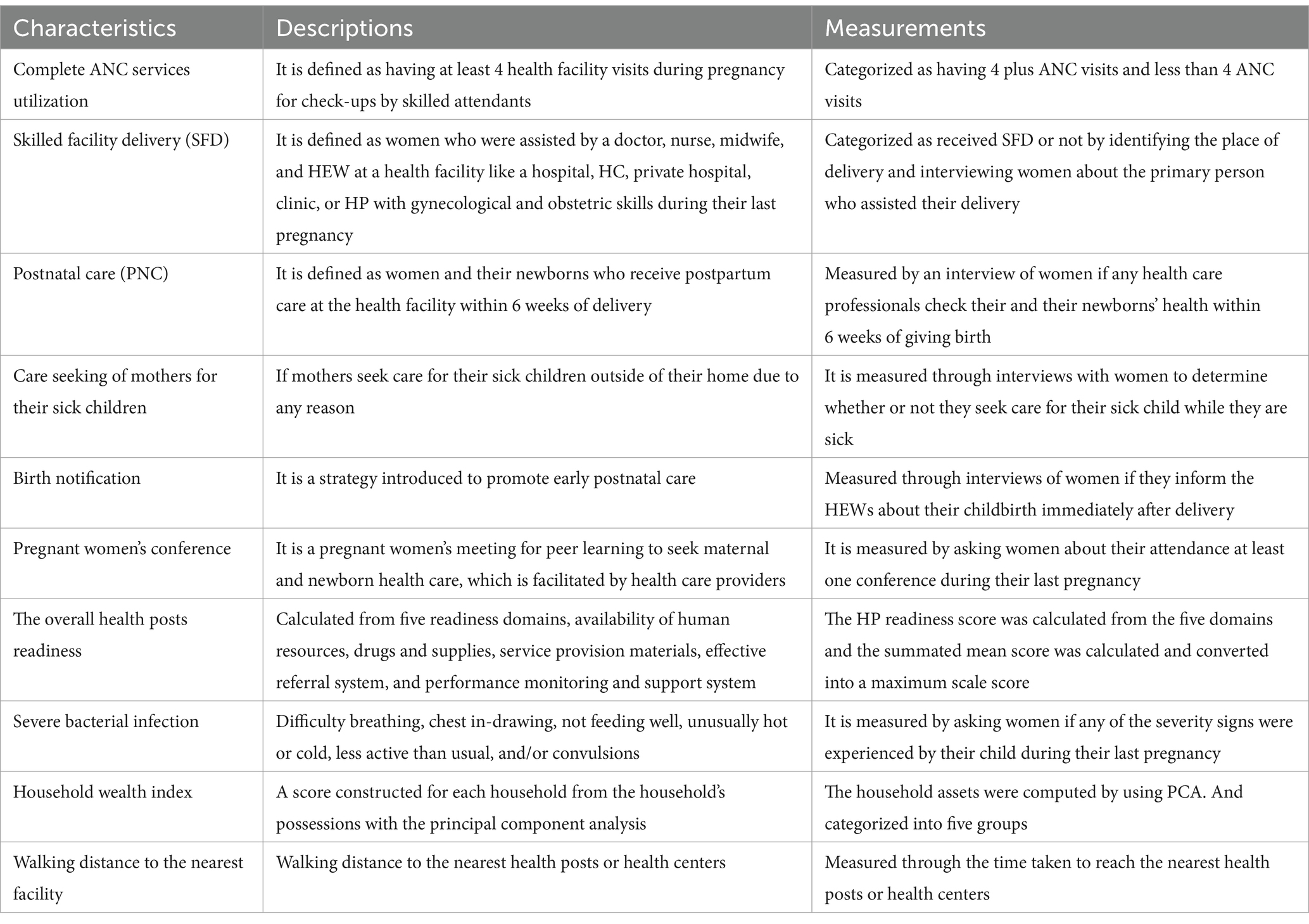
Measurements
To measure the care-seeking practice of mothers, interviews with mothers were about whether or not they sought care for their sick child outside of their home while the child was sick. To assess health posts’ readiness for the prevention and management of sick children, a review of the activity and observation checklists were adapted from the WHO Service Availability and Readiness Assessment (SARA) tool (30). The level of readiness was rated based on all questions asked and/or observed. The preparedness of facilities was measured in five domains including the availability of an adequate number of competent healthcare providers (i.e., healthcare providers who take trainings on iCCM and CBNC for management of sick children at the lower level health facilities, the availability of drugs, availability of equipment and supplies, availability of an effective referral system, and the availability of performance monitoring and support system were considered). One of the important approaches for implementing the iCCM strategy is to provide care or arrange referral to higher-level care as soon as possible during labor and PNC periods.
The level of facility readiness for the management of sick children was measured with the mean availability of tracer items across the five domains of readiness by assigning equal weight to each of the items. The overall service readiness score was calculated by computing the scores of the five domains; that provided the summated mean scores. Then to make our measurements comparable with other studies measured with different scales we calculated the maximum scale score. The wealth statuses of mothers were measured using the principal component analysis (PCA) and the other independent variables were measured by an interview of women for the presence or absence of each characteristic (Table 1).
Data analysis
To create a more complete dataset, we combined the facility-level data with the individual-level data using the unique identification given to each health facility. For this study, the mothers’ care-seeking practice for their sick children was taken as the dependent variable, and facility readiness is an independent variable measured using healthcare workers’ competence, drug availability, service provision material availability, the presence of an effective referral system, and the existence of performance monitoring and support system. Moreover, sociodemographic characteristics (maternal age, maternal education, paternal education, and marital status, sex of the child, gravidity, and parity), household wealth status, ANC follow-up, SBA/SFD use, and PNC use were considered confounding variables.
The wealth index of the household was determined using PCA. The level of health facility readiness was determined by calculating the proportions of the availability of tracer items for the five domains. The tracer items were coded as 1 if the item is available and 0 if not available. The item reliability was checked by calculating Chronbach’s alpha and the internal consistency of the tracer item for each domain was found to be in the acceptable range. We computed the readiness score by assigning equal weight for each of the tracer items for each domain. The overall readiness score was calculated from the five domains as a summated mean score. Then the summated mean score was standardized to the maximum scale score [i.e., converting summated scores (total of individual item scores)] into a standardized percentage to compare the results with others measured on different scales.
We did an independent sample t-test with a 95% CI and p-value < 0.05 to see the change in the care-seeking practice of mothers for their sick young infants during the implementation periods. To see the contributions of facility readiness and controlling confounding, we fitted a logistic regression. The crude odds ratios (COR) were calculated to select the candidate variables for multivariable analysis. Variables with a p < 0.25 for the COR were considered as candidates for multivariable regression analysis. In multivariable analysis, maximum likelihood estimation techniques were used. For the final model, multivariable logistic regression analysis with log link estimation techniques was done to identify the independent predictors of the care-seeking practice of mothers for their SYIs and to see the contributions of facility readiness for the care-seeking practice of mothers for their SYIs. The respective AOR at p < 0.05 and 95% confidence intervals were used to declare variables that have a statistically significant association.
Ethical approval
Ethical clearance was obtained from the Ethiopian Public Health Association (EPHA) Research Ethics Review Committee (Reference #: EPHA/OG/166/21 dated April 16, 2021) and renewed for the end-line survey (Reference #: EPHA/OG/781/22 dated April 18, 2022). Informed consent was obtained from all participants after providing them with comprehensive information about the research to ensure they fully understood the study. The consent form was approved by the IRB, and voluntary participation was ensured throughout the study. All participants were informed about the study’s purpose, benefits, and potential risks, and they were made aware of their right to opt out to answer any questions. When a respondent agreed to participate after reviewing the consent information, the interviewer documented consent by marking the questionnaire and providing a digital signature below the consent statement. Interviews proceeded only after consent was given and properly documented. For the facility assessment permission letters were obtained from the Woreda health offices. The researchers ensured that all information obtained from participants was kept confidential and private to respect their privacy and maintain the integrity of the study. All respondent identifiers were kept confidential, and data were anonymous. The authors confirm that all methods were performed in accordance with the relevant guidelines and regulations such as the Declaration of Helsinki and the Ethiopian National Research Ethics Review Guideline.
Results
Socio-demographic characteristics
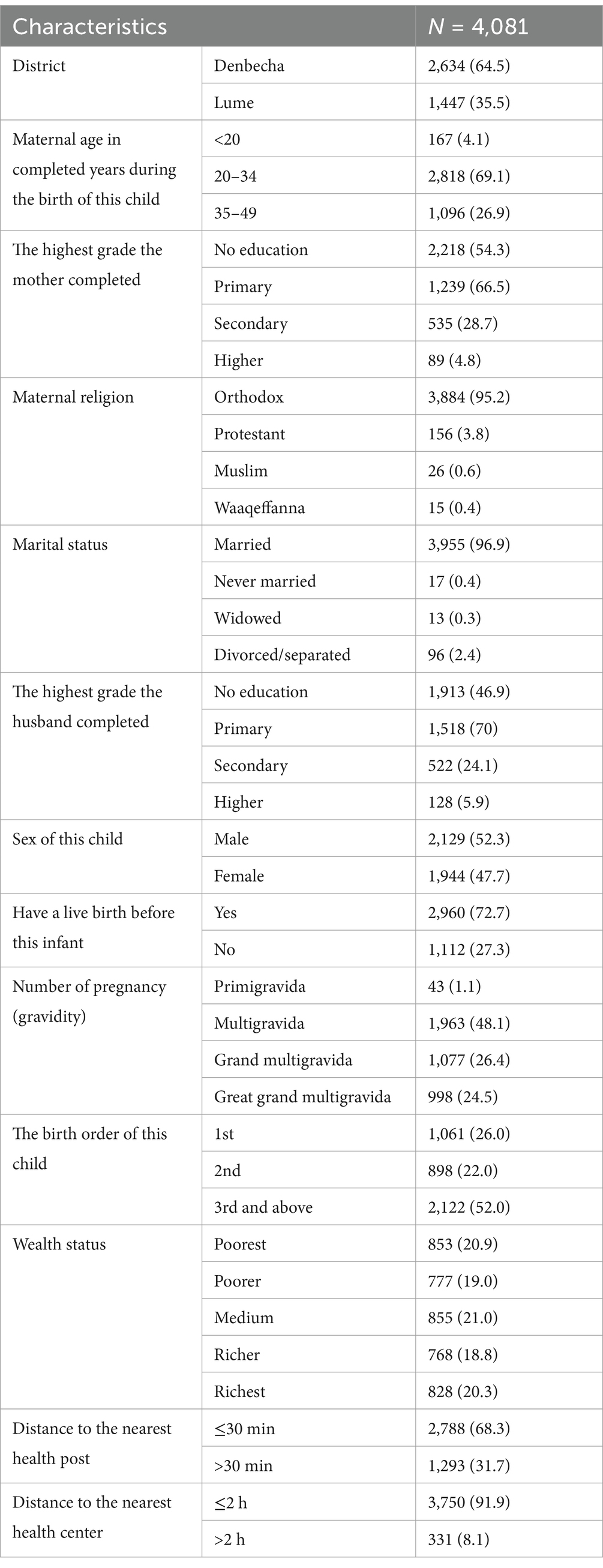
In the household survey, More than two-thirds of the respondents were 20–34 years old. About 1,518 (70%), had primary education, about 2,788 (68.3%) of them lived less than 30 min walking distance to the nearest health post, and 3,750 (91.9%) of them lived less than 2 h walking distance to the nearest health center Among the 64 HPs, 85.9% of them have trained HEWs, 59.4% of HPs have two or more HEWs, and 40.6% of them have only one HEW during the facility visit (Table 2).
Facility readiness
Availability of adequate numbers and competent healthcare providers
The mean readiness score for the availability of adequate numbers and competent healthcare providers was 74.6%(95%CI: 73.8–80.4). About 40.6% of HPs have less than the mean healthcare providers readiness score, and about 59.4% of HPs have more than the mean readiness score. In this regard, all HPs have HEW, 59.4% of HPs had more than one HEW who was working in each HP, and 40.6% of HPs had only one HEW. About 85.9% of HPs had at least one trained HEW (i.e., HEWs who gets special trainings about iCCM) for the management of sick children at the lower level health facilities (Table 3).
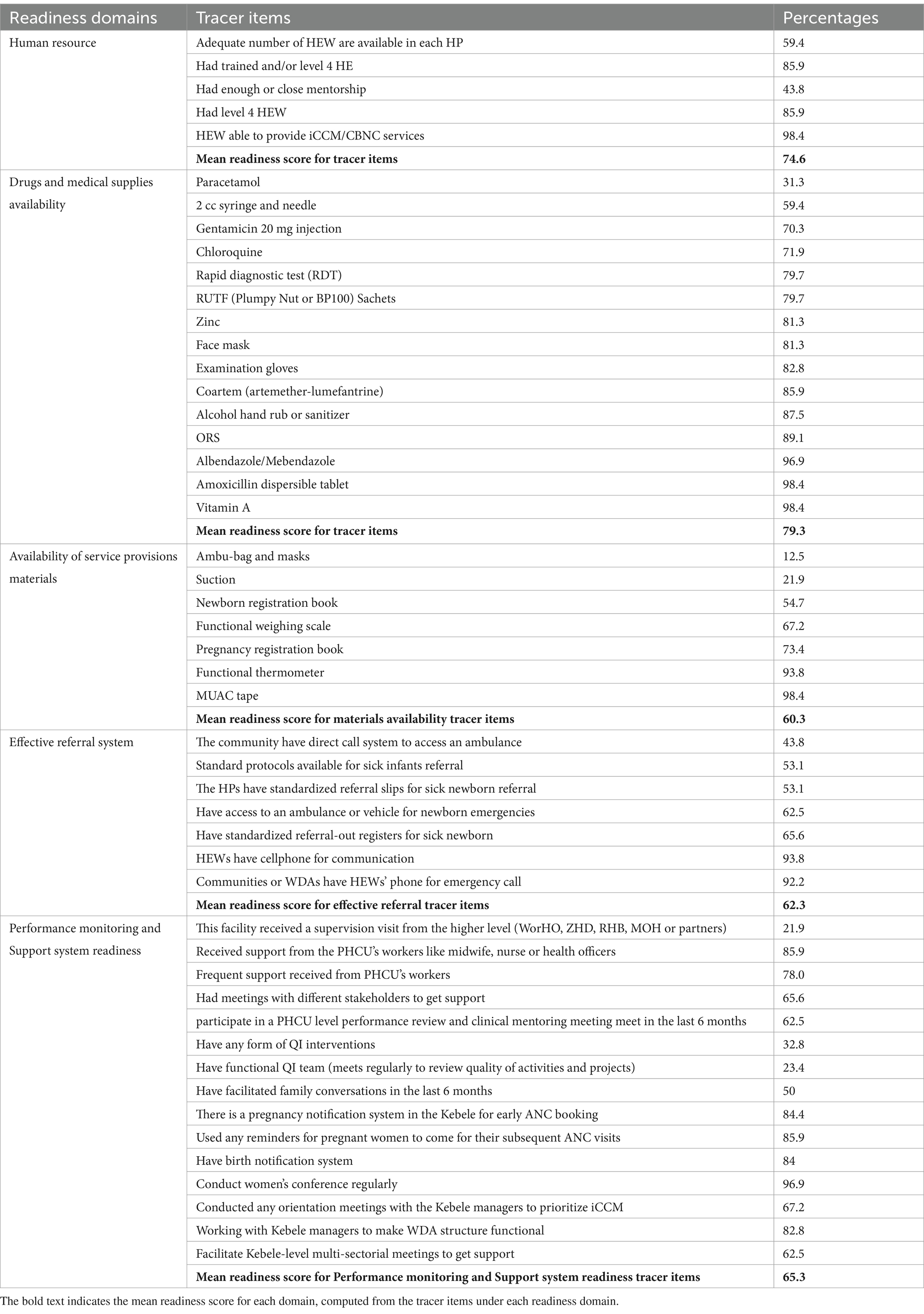
Table 3. Health posts readiness domains and tracer items for management of sick children in Denbecha and Lume districts, Ethiopia, June 2022.
Drugs and medical supplies availability
Health posts readiness for the management of sick children in terms of the availability of drugs and medical supplies was 79.3% (95%CI: 78.7–83.2%). About 28 (43.8%) of HPs have less than the mean readiness score, and 36 (56.3%) of HPs have a readiness score greater than the mean. Amoxicillin was available in 63 (98.4%) of HPs, Gentamicin (20 mg injection) was available in 45 (70.3%) of HPs, and Albendazole or Mebendazole was available in 62 (96.9%) of HPs. Whereas Paracetamol was available in only 31.3% of HPs (Table 3).
Availability of materials/equipment to provide healthcare service
Health posts readiness for the management of sick children in terms of the availability of materials used to provide healthcare was 60.3% (95%CI: 55–65.4%). Most health posts (98.4%) have functional thermometry, and the middle Upper Arm Circumference (MUAC) measurement apparatus is available in 93.8% of health posts. All HPs have an iCCM and/or Community-Based Newborn Care (CBNC) Chart booklet; 76.6% of HPs have functional blood pressure measuring apparatus. Whereas only 21.9 Health posts have suction and only 12.5% of HPs have Ambu bags and masks (Table 3).
Effective referral
Health posts’ readiness for the management of sick children in terms of the availability of an effective referral system was 62.3% (95%CI: 56.7–68.1). About 39.1% of HPs have a lower mean readiness score, and 60.9% of HPs have a greater mean readiness score. In 93.8% of HPs HEWs have cellphones and 92.2% of them give their phone numbers to the women development arms (WDAs), or the pregnant women for emergency calls. About 62.5% of HPs have access to an ambulance or another vehicle for newborns, and 65.6% of HPs have a functioning cellular telephone or a private cellular phone that is supported by the HC/district health office to facilitate the referral. About half of 53.1% of HPs have standard protocols for sick newborns’ referral (for whom, when, and where to refer) (Table 3).
Performance monitoring and support system readiness
Health posts readiness for the management of sick children with regards to performance monitoring and support system was 65.3% (95%CI: 60.3–71.3). About 85.9% of HPs had received integrated supervision from midwives, nurses, or health officers including the iCCM program for the management of SYIs. However, only 21.9% of HPs received supervisory visits from higher-level officials (district health office, zonal health department, regional health bureau, ministry of health, or partners). In 96.9% of HPs, HEWs conduct women’s conferences regularly, and in 84.4% of HPs, there was a pregnancy notification system. Whereas only 32.8% of HPs have quality improvement interventions and 67.2% of HPs conducted orientation meetings with the Kebele managers to prioritize iCCM. However, only 32.8% of HPs have any form of quality improvement (QI) interventions, and 23.4% have functional QI teams (Table 3).
Overall health facility readiness
The highest readiness score were 79.3%, the lowest readiness score were 60.3% and the overall summated mean score was 69.6% (95%CI: 66.2–72.8). However, as it is standardized using the maximum scale score it was only 49.0%. Among the five domains, the availability of drugs and medical supplies has the relatively highest readiness score (79.3%). Whereas, effective referral system and availability of service provisions materials domains had the lowest scores with 60.3 and 62.3%, respectively (Figure 1).
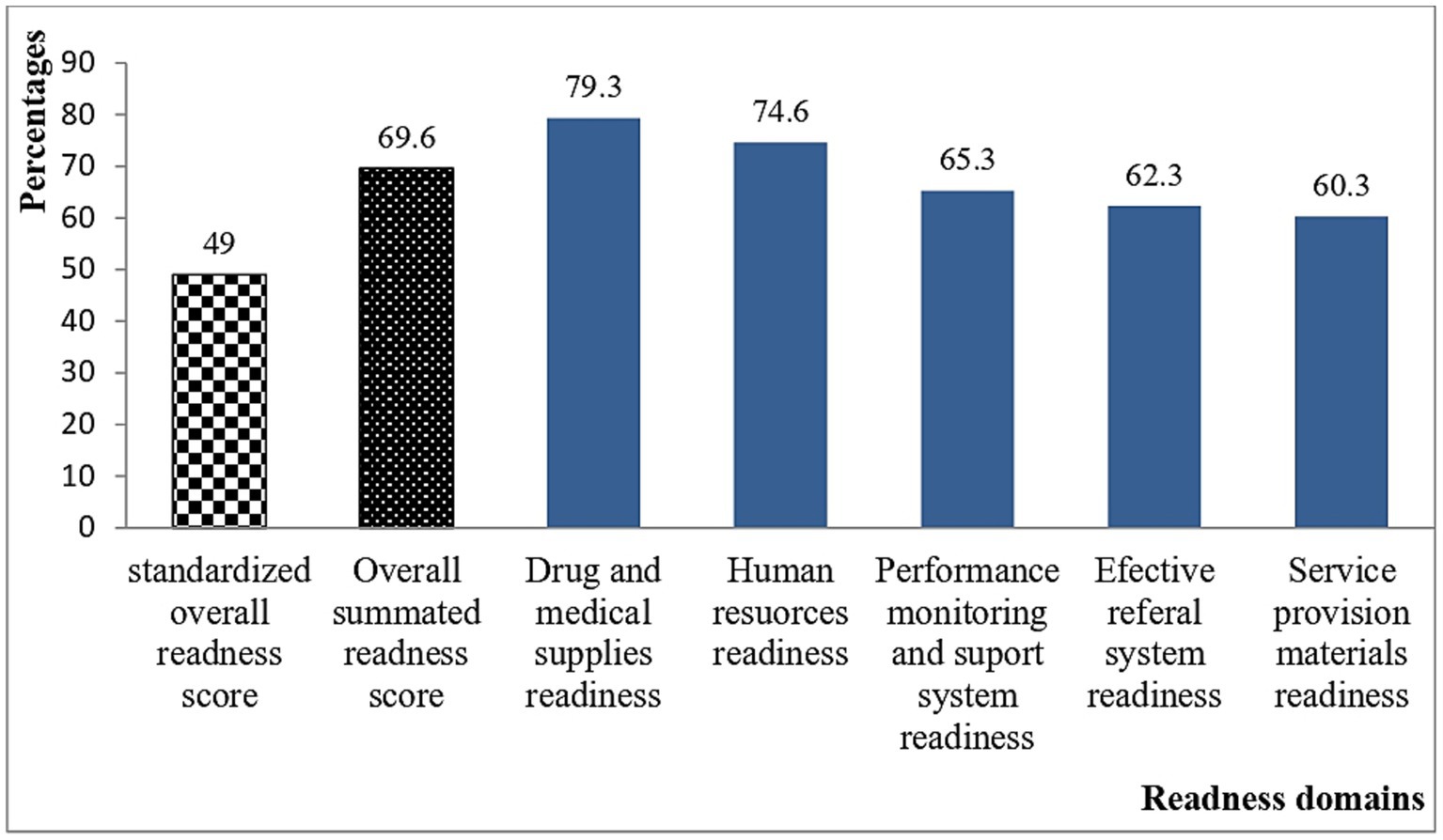
Figure 1. The overall health posts readiness score measured in six domains in Denbecha and Lume districts, Ethiopia: June, 2022.
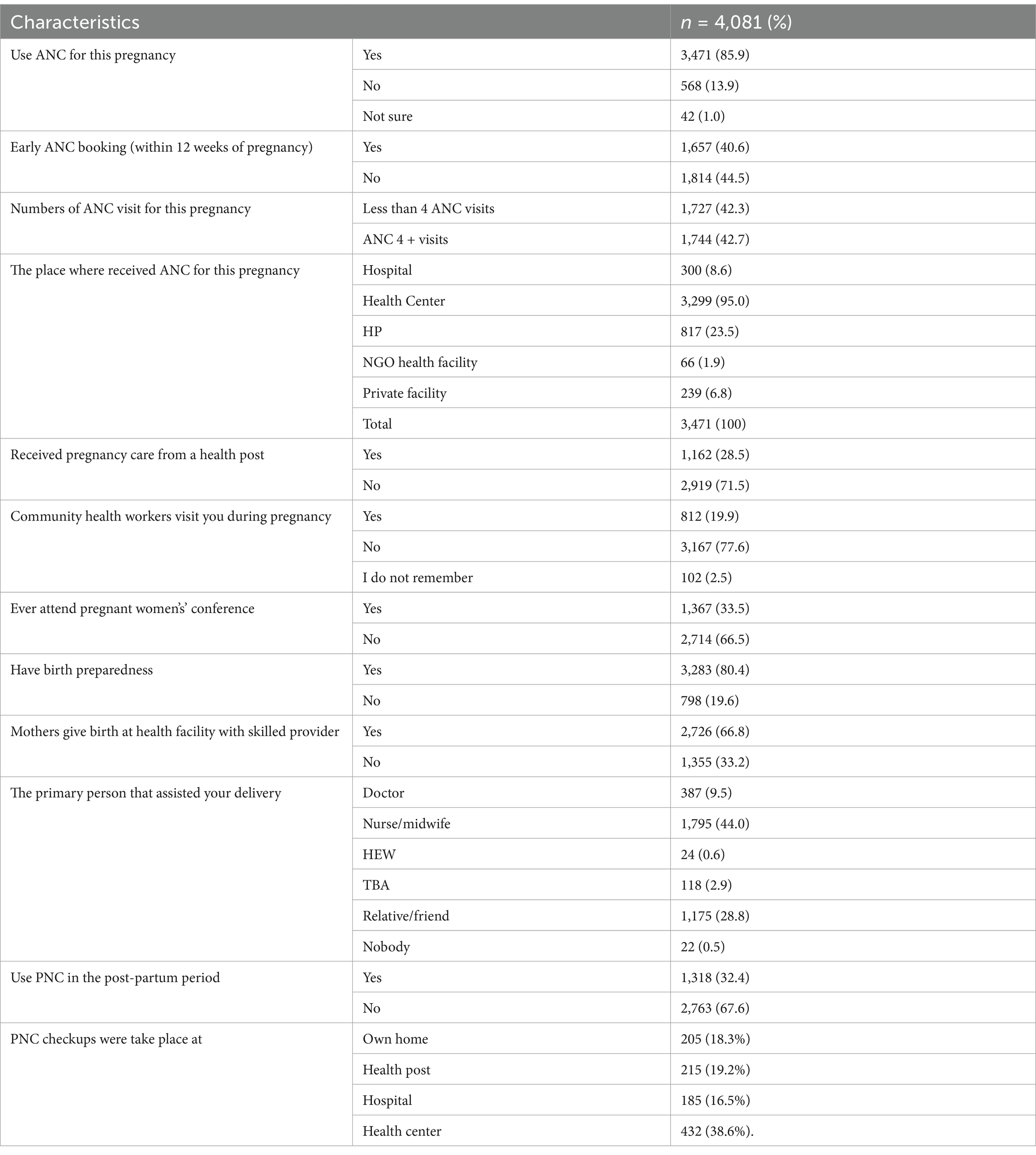
Maternal health service utilization
Most mothers 3,471 (85.5%) had ANC follow-up visits at a health facility. Among them, nearly half, 1,657 (47.7%) of mothers initiated early ANC within 12 weeks of pregnancy, and 1,744 (50.2%) had ANC4 + visits. Two-thirds of mothers, 2,726 (66.8%), gave birth in health facilities with a skilled provider. About 1,795 (44.0%) of them were assisted by midwives and nurses, 387 (9.5%) by doctors, and 24 (0.59%) by HEWs. However, a significant number, 1,175 (28.8%), of deliveries were assisted by nonprofessional relatives and friends. About 1,318 (32.4%) of mothers had at least one PNC visit; 1,120 (27.5%) did PNC visits for their third child and 995 (24.4%) had PNC for themselves. About 650 (15.9%) of mothers read or discussed about family health card (FHC) and only 298 (7.3%) of mothers had FHC. One-third, 1,367 (33.5%), of mothers attended pregnant women’s conferences (Table 4).
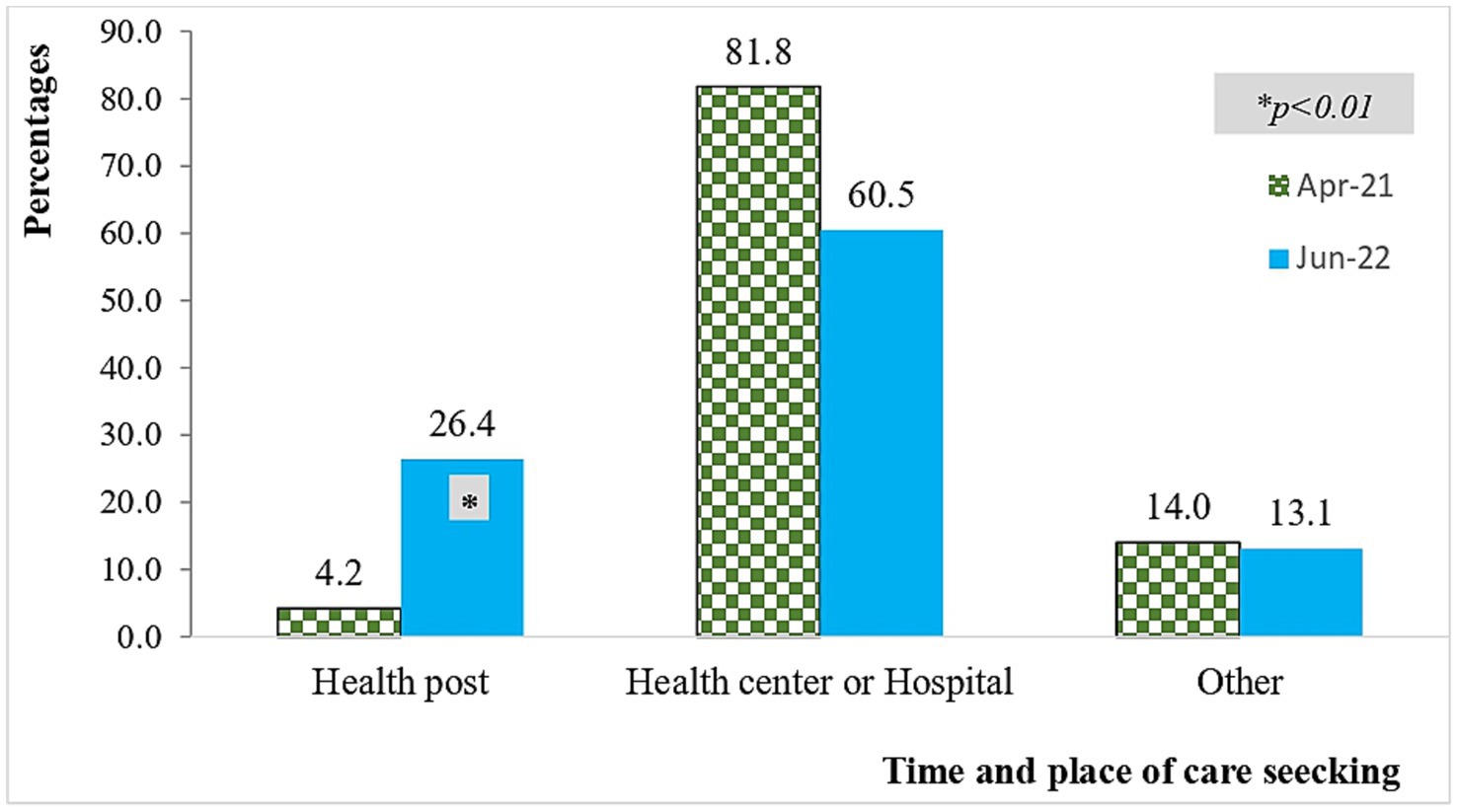
Changes in mothers’ care-seeking practice at health posts for their sick children
Approximately 26.4% of mothers sought care for severe infections at health posts (HPs) during the end-line study, representing a significant increase from the baseline figure of 4.2%. About 459 children were sick of whom 359 (78.2%) were young infants in the end-line survey. About 316 (88.0%) mothers with sick infants sought care in the end line survey compared with only 291 (57.3%) who did it in the base line survey. About 45.6% of SYI cases received care at health centers and 23.4% received care at health posts in the end line survey where as 69.8% of SYI cases received care at the health centers and 4.5% received care at health posts in the baseline survey indicating a significantly higher change in care seeking at health posts in the end line survey (Figure 2).
Data from the facility records also showed that, many sick children visited HPs and received appropriate treatment at the health post level. About 955 pneumonia cases were correctly evaluated in the last 8 months (from November 2021 to May 2022). From diagnosed children with pneumonia, about 912 (91.6%) of sick children were properly treated (i.e., took the correct dose of medication, adhered to the schedule, and followed the recommended duration of treatment) among cases seen in the last 8 months. Moreover, from 45 very severe diseases (VSD), 39 (86.7%) were correctly treated (i.e., take the correct dose of medication, adhere to the schedule, and follow the recommended duration of treatment) within the last 8 months from November 2021 to May 2022 (Figure 2).
The correlation between health posts readiness and care-seeking practice of mothers for their sick children
In bi-variable analysis, maternal age during the birth of the index child, district type, maternal education, religion, wealth status, parity, walking distance to the nearest health post, distance to the nearest health center, ANC use, PNC use, pregnant women’s conference attendance, health facility readiness in terms of human resources, drug availability, service provision material availability, support system readiness, performance monitoring readiness, and effective referral availability readiness were associated with the healthcare seeking of mothers for their sick children, at a p-value of < 0.25. On the other hand, wealth status, district type, parity, distance to the nearest HP, ANC use, health facility readiness in terms of service provision material availability, effective referral system availably, performance monitoring system readiness, and support system readiness had a statistically significant association with the healthcare seeking practice of mother for their young infants in multivariable analysis at a p-value of < 0.05 and 95% CI. The odds of healthcare seeking among mothers for their sick children in Lume district were 87% times lower than that of Denbecha district mothers to seek healthcare for children (AOR = 0.13: 95%CI; 0.1–0.3), and the odds of healthcare seeking among grand multipara mothers were 73% lower than primi-para women (AOR = 0.27: 95%CI; 0.1–0.7). The odds of care seeking for sick children among mothers who are members of rich households were 2.02 times higher compared to those living in poor households (AOR = 2.02: 95%CI; 1.1–3.9). The odds of care seeking for sick children among mothers who used ANC were 2.76 times higher compared to those who did not have ANC visits (AOR = 2.76: 95%CI; 1.3–5.7). The odds of healthcare seeking for sick children among mothers who had PNC visits were 41% lower than those who did not have PNC visits (AOR = 0.59 95%CI: 0.36–0.96). For every one-unit increase in the readiness score with the availability of materials and medical supplies, the odds of health-seeking care among mothers increased by 52% (AOR = 1.52: 95%CI; 1.2–1.9). Whereas, for every one-unit increase in the readiness score with the availability of an effective referral system, the odds of healthcare-seeking for sick children decreased by 19% (AOR = 0.81: 95%CI; 0.7–0.97). And for every one-unit increase in human resource readiness score the care-seeking practice of mothers decreased by 28% (AOR = 0.72 95%CI: 0.54–0.96) (Table 5).
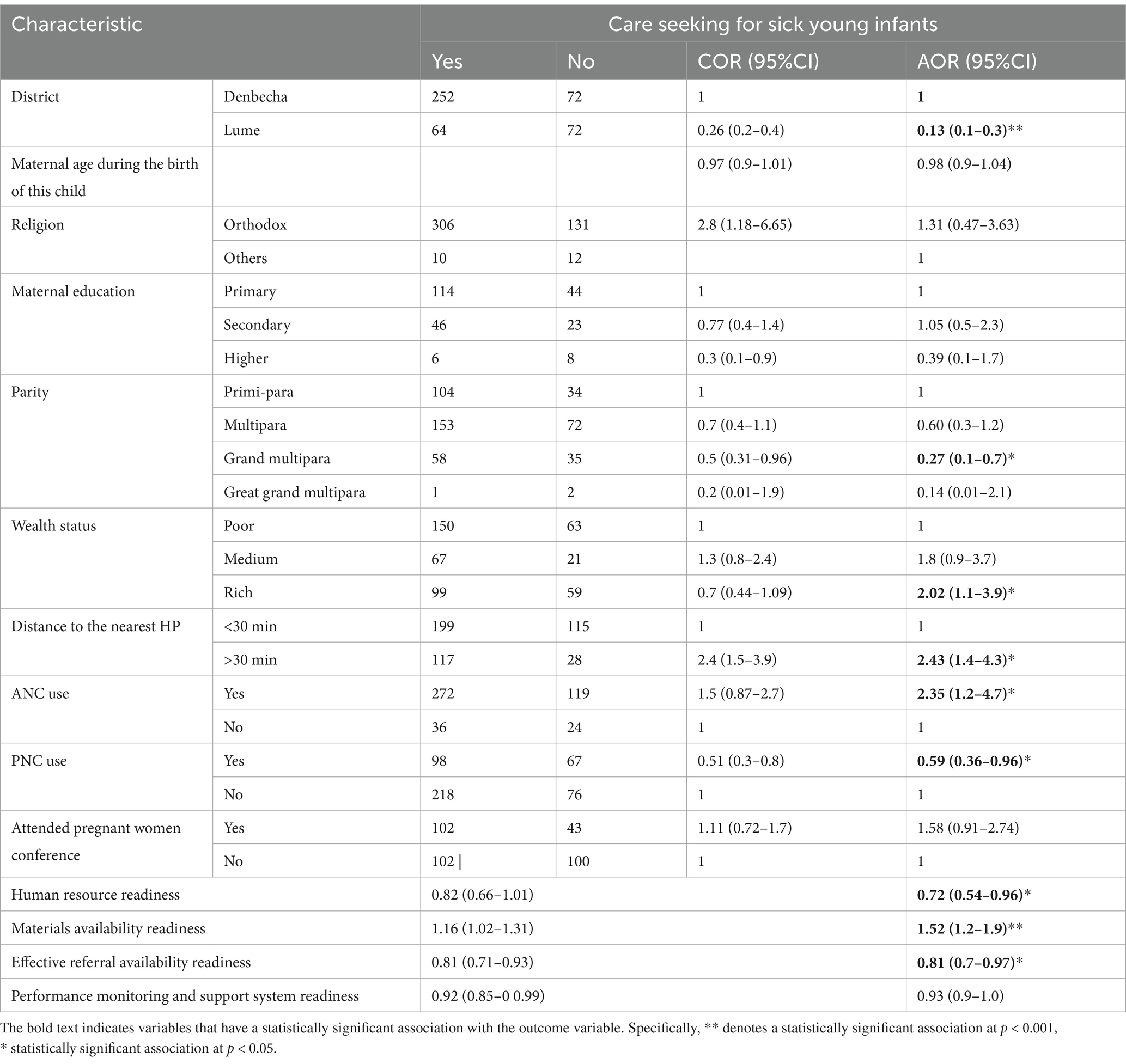
Table 5. Factors associated with the healthcare-seeking practice of mothers for their sick children in Denbecha and Lume districts Ethiopia 2022.
Discussion
This study identified the suboptimal readiness of health posts in Ethiopia to provide adequate care for sick children. Mothers’ care-seeking behavior for SYIs was significantly influenced by factors such as the material readiness of health facilities, ANC use, parity, wealth status, administrative woreda, and walking distance to health facilities. In contrast, PNC use, human resource readiness, and the availability of effective referral systems were found to be negatively associated with care-seeking behavior. The readiness of health posts influence mothers’ care-seeking practices for their sick children. The findings of this study highlight a significant improvement in mothers’ care-seeking practices, increasing from 57.3% at baseline to 88.0% at the end-line survey (p < 0.001), reflecting changes over the implementation period. These findings are higher than those of a previous study in Bangladesh, where most mothers only brought their children to the hospital lately after the child developed danger signs, severe forms of the disease, or associated complications (31). This might be attributed to the readiness of health posts, improved availability of drugs and medical supplies, and improved mothers’ care-seeking practices at the community level in Ethiopia. Health facility readiness influences mothers’ care-seeking behavior to offer essential child health treatments is a complex process. Essential child health care requires skilled healthcare professionals who can provide the necessary services in an environment with adequate infrastructure, medications, supplies, and equipment. Facility readiness on its own is insufficient for providing high-quality services (3); however, it is an important first step (1).
Subsequently, in this study, we found suboptimal level of overall readiness score, indicating an important snapshot of how prepared healthcare facilities are to manage sick children. Our study shows lower readiness scores compared to previous studies conducted in India (1). It is also lower than a study done in Timor, the readiness score increased from 44 to 89% after the implementation of health improvement projects at health posts, health centers, and hospitals (32). The gap may be due to differences in socio-economic status about healthcare infrastructure and resource availability. And, the implementation strategies in our context more focus on the accessibility of important drugs than on improving the overall quality dimensions. Our study is similar to studies conducted in Nepal, where the mean readiness score was 52.1%, and only 50% of facilities were ready to offer sick child care (33). It may be because in Nepal, many sick children have access to hospital care, and they ignore the fulfillment of supplies at the community level.
In this study, we identified a moderate level (74.6%) of HP readiness about the availability of adequate numbers and competent healthcare providers. This is better than a study done in Kenya that demonstrated providers at PHC units, lacked effective specialized knowledge and/or basic skills for the management of sick children (34). However, it is lower than the study done in Bangladesh, where all service providers received at least a 5-day training session on the infection management guidelines, and 63–97.7% of providers were able to classify PSBI (35). In our study, about 40.6% of HPs have only one HEW, and only 59.4% of HPs have more than one HEW in each HP. This is against the Ethiopian Health Extension Program (HEP); the implementation guidelines stipulate a staffing pattern of two HEWs for each HP (36).
Our study also identified a moderate level of 79.3% of HP readiness concerning the availability of drugs and supplies. Which is higher than the study done in Malawi (37) and India where essential drugs and supplies readiness scores increased from 52to 73% after the implementation of the intervention (1). Even though our study focused on primary health care units at the community level, it had the same result with Malawi that included all health facilities from the lower to the referral levels. This may be due to the implementation strategies that improved the facility readiness at the community level better than the hospital level readiness. This study is also higher than a nationwide service availability and readiness assessment done in Ethiopia (38). This may be due to the interventions in our study had improved the facility’s readiness (27).
A relatively lower readiness score was observed with the availability of service provision materials 60.3% and effective referral system 62.3% compared to all HP readiness domains. The readiness of HPs to successfully refer clients to the right services determines the life of the child. Delays in referral determine the life and death of the newborn because time is crucial for them. Poor referral systems due to the scarcity of resources, including healthcare providers, and a lack of communication technologies result in ineffective referral communications between facilities (39). Moreover, the receiving facility is expected to anticipate the arrival, provide care and follow-up for the patient, and send back the referral form and feedback to the initiating facility to confirm or disprove the appropriateness of the referral (39). This is similar to another nationwide service availability and readiness assessment done in Ethiopia, which shows the mean availability of tracer items for service provision materials was 63% and even lower at the health post level, which is 57% (38).
The performance monitoring and support system, a readiness score of 65.3% in this study indicates moderate readiness, suggesting that while some elements of a sound performance monitoring and support system are in place, there is room for improvement. This may involve the need for more consistent monitoring and support or enhanced training for staff involved in performance monitoring and supportive supervision. In more developed healthcare systems, performance monitoring systems generally have higher readiness scores and contribute to improved health outcomes within the context of shared responsibility and accountability for achieving desired results (40). The gap in this regard may be due to limited access to technology, insufficient training, and a lack of standardized monitoring practices are there.
This study analyzed the factors affecting mothers’ care-seeking practices for their sick children outside the home. The results indicate that after controlling for confounding variables, wealth status, maternal parity, district type, distance to the nearest healthcare facility, antenatal care utilization, healthcare provider readiness with available materials and medical supplies, an effective referral system, a strong support system, and a performance monitoring system are predictors of mothers’ care-seeking practices for their children.
Our analysis indicates a significant positive association between the health posts readiness and care-seeking practice of mothers for their sick children after controlling confounding variables. For every one-unit increase in the readiness score with availability of materials and medical supplies, the odds of seeking care among mothers increase by 52 %. This is similar to other studies done in Malawi: that highlight better facility quality is positively associated with the utilization of sick child healthcare services (37). This suggests improving the availability of medical supplies and materials in health facilities could substantially enhance the likelihood of care-seeking. When health facilities are well-prepared with essential materials and medical supplies, mothers are more likely to seek care for their children. This study remarks that an increase in the readiness score of HPs reflects how well-prepared they are to provide appropriate care, and increases the likelihood of mothers seeking care.
Whereas, against previous studies (15, 41); facility readiness with human resources and referral system were negatively associated with care care-seeking practice of mothers outside their homes. This may be due to mothers feeling more confident in the referral system, ensuring quick access to support and the appropriate level of care if needed. However, the particular intervention reduces the need to seek healthcare outside their home for every sickness. It also minimizes the need for mothers to travel long distances for care, as they can trust the local support system and monitoring system. Another reason could be cultural and social considerations. In some contexts, strong community support systems align with cultural preferences for seeking care within the community. Mothers may prefer staying at home due to these cultural and social factors (15). Another possible explanation is that unlike other studies the data collection period, which occurred between 2021 and 2022, coincided with the peak of the COVID-19 pandemic. During this time, mothers were advised to stay at home unless they faced serious medical conditions.
The odds of care seeking among women who were from rich wealth status were 2.02 times higher compared with poor families. This is in line with a study done in Nigeria (42). However, it contrasts to the findings of a study done in southern Ethiopia (43). The disagreement might be explained by the fact that our study encourages every woman to seek care at all health facilities; whereas the previous study aimed to serve the poorest households at the health post and household levels to increase service access to richer families who can access health services at higher level health facilities. In our study, ANC utilization was associated with the care-seeking practice of mothers for their children. The result is consistent with a previous study done in northwest Ethiopia (44). This highlights that ANC visits provide opportunities for mothers to meet healthcare providers, and receive important information from healthcare providers about newborn danger signs and the need for child health care. In this study, grand multipara women were 73% less likely to seek care for their sick child compared to primi-para women. This might be explained by the fact that multi-Para women have experience and can identify critical illnesses that require treatment: whereas first-time mothers are more likely to be younger, which may make them more cautious and inclined to seek medical help (45).
Limitations of the study
Despite its strength, this study has a limitation that the readers should consider; the basic amenities under the general service readiness items were not included in the health posts readiness assessment. And the study could have been more informative if it had been supplemented by a qualitative study.
Conclusion
In this study a suboptimal level of HP preparedness highlights the need for continued efforts to improve service provision materials availability, effective referral system, performance monitoring and support system, and continuous tanning and development of health workers for the management of sick children at the community level, particularly in under-resourced areas. Health post readiness significantly influences the healthcare-seeking practice of mothers for their sick children. The readiness of HPs, particularly in terms of materials and medical supplies, is a major factor in determining the care-seeking behavior of mothers for their sick children outside their homes. Moreover, ANC use, parity and wealth status, and distance to the health facility are significantly associated with the healthcare-seeking practice of mothers for their sick children.
Data availability statement
The datasets used in this study are included in the manuscript and can be obtained from the principal investigator upon reasonable request.
Ethics statement
Ethical clearance was obtained from the Ethiopian Public Health Association (EPHA) Research Ethics Review Committee (Reference #: EPHA/OG/166/21 dated April 16, 2021) and renewed for the end-line survey (Reference #: EPHA/OG/781/22 dated April 18, 2022). Informed consent was obtained from all participants after providing them with comprehensive information about the research to ensure they fully understood the study. The consent form was approved by the IRB, and voluntary participation was ensured throughout the study. All participants were informed about the study’s purpose, benefits, and potential risks, and they were made aware of their right to opt out or decline to answer any questions. When a respondent agreed to participate after reviewing the consent information, the interviewer documented consent by marking the questionnaire and providing a digital signature below the consent statement. Interviews proceeded only after consent was given and properly documented. The researchers ensured that all information obtained from participants was kept confidential and private to respect their privacy and maintain the integrity of the study. All respondent identifiers were kept confidential, and data were anonymous. The authors confirm that all methods were performed in accordance with the relevant guidelines and regulations such as Declaration of Helsinki and the Ethiopian National Research Ethics Review Guideline. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
WNM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. GT: Conceptualization, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WM: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are sincerely thankful to JSI for sharing their datasets for this study. We would also like to acknowledge and thank study participants and data collectors for their time and dedication during the study.
Conflict of interest
GT was employed by JSI Research and Training Institute, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
aIRR, Adjusted incidence rate ratio; ANC, Ante natal care; EPHA, Ethiopian Public Health Association; HEW, Health extension worker; HP, Health post; iCCM, Integrated community case management of childhood illnesses and newborn care; JSI, JSI Research and Training Institute Inc.; PNC, Post natal care; PPC, Peripartum care; SARA, Service availability and readiness assessment; SBAs, Skilled birth attendants; SFD, Skilled facility delivery; WDA, Women development army; WHO, World Health Organization.
References
1. Pelly, L, Srivastava, K, Singh, D, Anis, P, Mhadeshwar, VB, Kumar, R, et al. Readiness to provide child health services in rural Uttar Pradesh, India: mapping, monitoring and ongoing supportive supervision. BMC Health Serv Res. (2021) 21:1–11. doi: 10.1186/s12913-021-06909-z
2. Donabedian, A. The quality of care: how can it be assessed? JAMA. (1988) 260:1743–8. doi: 10.1001/jama.1988.03410120089033
3. Pandya, H, Slemming, W, and Saloojee, H. Health system factors affecting implementation of integrated management of childhood illness (IMCI): qualitative insights from a south African province. Health Policy Plan. (2018) 33:171–82. doi: 10.1093/heapol/czx154
4. Usman, AK, Wolka, E, Tadesse, Y, Tariku, A, Yeshidinber, A, Teklu, AM, et al. Health system readiness to support facilities for care of preterm, low birth weight, and sick newborns in Ethiopia: a qualitative assessment. BMC Health Serv Res. (2019) 19:860. doi: 10.1186/s12913-019-4672-2
5. Cassini, A, Allegranzi, B, Fleischmann-Struzek, C, Kortz, T, Markwart, R, Saito, H, et al. Global report on the epidemiology and burden on sepsis: current evidence, identifying gaps and future directions. Global report on the epidemiology and burden on sepsis: current evidence, identifying gaps and future directions. (2020).
6. Ahmed, I, Ali, SM, Amenga-Etego, S, Ariff, S, Bahl, R, Baqui, AH, et al. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in South Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health. (2018) 6:e1297–308. doi: 10.1016/S2214-109X(18)30385-1
7. EPHI I. Ethiopia mini demographic and health survey 2019: key indicators. Rockville, Maryland: EPHI and ICF (2019).
8. CSA I. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016. CSA and ICF Ethiopia: Addis Ababa, Rockville, MD (2016).
9. World Health Organization Guideline: managing possible serious bacterial infection in young infants when referral is not feasible (2015).
10. Berhane, M, Girma, T, Tesfaye, W, Jibat, N, Abera, M, Abrahim, S, et al. Implementation research on management of sick young infants with possible serious bacterial infection when referral is not possible in Jimma zone, Ethiopia: challenges and solutions. PLoS One. (2021) 16:e0255210. doi: 10.1371/journal.pone.0255210
11. Leul, A, Hailu, T, Abraham, L, Bayray, A, Terefe, W, Godefay, H, et al. Innovative approach for potential scale-up to jump-start simplified management of sick young infants with possible serious bacterial infection when a referral is not feasible: findings from implementation research. PLoS One. (2021) 16:e0244192. doi: 10.1371/journal.pone.0244192
12. Awasthi, S, Kesarwani, N, Verma, RK, Agarwal, GG, Tewari, LS, Mishra, RK, et al. Identification and management of young infants with possible serious bacterial infection where referral was not feasible in rural Lucknow district of Uttar Pradesh, India: an implementation research. PLoS One. (2020) 15:e0234212. doi: 10.1371/journal.pone.0234212
13. Guenther, T, Mopiwa, G, Nsona, H, Qazi, S, Makuluni, R, Fundani, CB, et al. Feasibility of implementing the World Health Organization case management guideline for possible serious bacterial infection among young infants in Ntcheu district, Malawi. PLoS One. (2020) 15:e0229248. doi: 10.1371/journal.pone.0229248
14. Wammanda, RD, Adamu, SA, Joshua, HD, Nisar, YB, Qazi, SA, Aboubaker, S, et al. Implementation of the WHO guideline on treatment of young infants with signs of possible serious bacterial infection when hospital referral is not feasible in rural Zaria, Nigeria: challenges and solutions. PLoS One. (2020) 15:e0228718. doi: 10.1371/journal.pone.0228718
15. Tareke, KG, Lemu, YK, and Feyissa, GT. Exploration of facilitators of and barriers to the community-based service utilization for newborn possible serious bacterial infection management in Debre Libanos District, Ethiopia: descriptive qualitative study. BMC Pediatr. (2020) 20:1–14. doi: 10.1186/s12887-020-02211-9
16. Gebretsadik, A, Melaku, N, and Haji, Y. Community acceptance and utilization of maternal and community-based neonatal care services provided by health extension workers in rural Sidama zone: barriers and enablers: a qualitative study. Pediatr Health Med Therapeut. (2020) 11:203–17. doi: 10.2147/PHMT.S254409
17. Kruk, ME, Gage, AD, Arsenault, C, Jordan, K, Leslie, HH, Roder-DeWan, S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. (2018) 6:e1196–252. doi: 10.1016/S2214-109X(18)30386-3
18. Kruk, ME, Gage, AD, Joseph, NT, Danaei, G, García-Saisó, S, and Salomon, JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. Lancet. (2018) 392:2203–12. doi: 10.1016/S0140-6736(18)31668-4
19. World Health Organization and the United Nations Children's Fund (UNICEF). Every newborn progress report 2019. Report. (2020).
20. Bosch–Capblanch, X, and Marceau, C. Training, supervision and quality of care in selected integrated community case management (iCCM) programmes: a scoping review of programmatic evidence. J Glob Health. (2014) 4:020403. doi: 10.7189/jogh.04.020403
21. World Health Organization Institutionalizing integrated community case management (iCCM) to end preventable child deaths: a technical consultation and country action planning, 22–26 July 2019, Addis Ababa (2020).
22. Gebremedhin, S, Astatkie, A, Amin, HM, Teshome, A, and Gebremariam, A. Changes in care-seeking for common childhood illnesses in the context of integrated community case management (iCCM) program implementation in Benishangul Gumuz region of Ethiopia. PLoS One. (2020) 15:e0242451. doi: 10.1371/journal.pone.0242451
23. Wanduru, P, Hanson, C, Waiswa, P, Kakooza-Mwesige, A, and Alvesson, HM. Mothers’ perceptions and experiences of caring for sick newborns in newborn care units in public hospitals in eastern Uganda: a qualitative study. Reprod Health. (2023) 20:106. doi: 10.1186/s12978-023-01649-1
24. Carter, ED, Sheffel, A, Requejo, J, Kosek, M, Campbell, H, Eisele, T, et al. Association between sick child facility readiness and quality of care at the individual and facility level in five low-and middle-income countries. BMC Health Serv Res. (2024) 24:1400. doi: 10.1186/s12913-024-11772-9
25. Namazzi, G, Hildenwall, H, Ndeezi, G, Mubiri, P, Nalwadda, C, Kakooza-Mwesige, A, et al. Health facility readiness to care for high risk newborn babies for early childhood development in eastern Uganda. BMC Health Serv Res. (2022) 22:306. doi: 10.1186/s12913-022-07693-0
26. Tiruneh, GT, Nigatu, TG, Magge, H, and Hirschhorn, LR. Using the implementation research logic model to design and implement community-based management of possible serious bacterial infection during COVID-19 pandemic in Ethiopia. BMC Health Serv Res. (2022) 22:1515. doi: 10.1186/s12913-022-08945-9
27. Tiruneh, GT, Fesseha, N, Emaway, D, Betemariam, W, Nigatu, TG, Magge, H, et al. Effect of community-based newborn care implementation strategies on access to and effective coverage of possible serious bacterial infection (PSBI) treatment for sick young infants during COVID-19 pandemic. PLoS One. (2024) 19:e0300880. doi: 10.1371/journal.pone.0300880
29. Tiruneh, GT, Hirschhorn, LR, Fesseha, N, Emaway, D, Eifler, K, and Betemariam, W. Care-seeking behaviours of mothers and associated factors for possible serious bacterial infection in young infants during COVID-19 pandemic in Ethiopia: mixed-methods formative research. BMJ Open. (2023) 13:e073118. doi: 10.1136/bmjopen-2023-073118
30. Organization WH. Service availability and readiness assessment (SARA). Geneva: World Health Organization (2015).
31. Ferdous, F, Farzana, DF, Ahmed, S, Das, SK, Malek, MA, Das, J, et al. Mothers’ perception and healthcare seeking behavior of pneumonia children in rural Bangladesh. ISRN Family Med. (2014) 2014:690315. doi: 10.1155/2014/690315
32. USAID (2013). The facility readiness format: improving service delivery at health posts, health centers, and hospitals.
33. Acharya, K, Subedi, D, and Acharya, P. Health facility readiness to provide integrated family planning, maternal and child health (FPMCH) services in Nepal: evidence from the comprehensive health facility survey. PLoS One. (2022) 17:e0264417. doi: 10.1371/journal.pone.0264417
34. Mbugua, S, Gitaka, J, Gitau, T, Odwe, G, Mwaura, P, Liambila, W, et al. Family and provider perceptions of quality of care in the management of sick young infants in primary healthcare settings in four counties of Kenya. BMJ Open Quality. (2021) 10:e001125. doi: 10.1136/bmjoq-2020-001125
35. Applegate, JA, Ahmed, S, Harrison, M, Callaghan-Koru, J, Mousumi, M, Begum, N, et al. Provider performance and facility readiness for managing infections in young infants in primary care facilities in rural Bangladesh. PLoS One. (2020) 15:e0229988. doi: 10.1371/journal.pone.0229988
36. Teklehaimanot, A, Kitaw, Y, Girma, S, Seyoum, A, Desta, H, and Ye-Ebiyo, Y. Study of the working conditions of health extension workers in Ethiopia. Ethiop J Health Dev. (2007) 21:249–250.
37. Liu, L, Leslie, HH, Joshua, M, and Kruk, ME. Exploring the association between sick child healthcare utilisation and health facility quality in Malawi: a cross-sectional study. BMJ Open. (2019) 9:e029631. doi: 10.1136/bmjopen-2019-029631
38. Institute EPH (2017). Ethiopia service availability and readiness assessment 2016 summary report.
39. Teklu, AM, Litch, JA, Tesfahun, A, Wolka, E, Tuamay, BD, Gidey, H, et al. Referral systems for preterm, low birth weight, and sick newborns in Ethiopia: a qualitative assessment. BMC Pediatr. (2020) 20:1–12. doi: 10.1186/s12887-020-02311-6
40. Weissman, EM (1997). Using performance monitoring to improve community health: conceptual framework and community experience. Nairobi, Kenya: African Field Epidemiology Network (AFENET) in collaboration with Pan African Medical Journal (PAMJ) Group.
41. Ibikunle, OO, Afape, AO, Bakare, CA, Ipinnimo, TM, Ibirongbe, DO, Ajidahun, EO, et al. Effect of integrated supportive supervision on availability of resources for health care service delivery and uptake of services in Ekiti state, Southwest Nigeria, evidence from the saving one million lives program for result supported facilities. Pan Afr Med J. (2024) 47:45. doi: 10.11604/pamj.2024.47.45.34291
42. Agunwa, C, Obi, I, Ndu, A, Omotowo, I, Idoko, C, Umeobieri, A, et al. Determinants of patterns of maternal and child health service utilization in a rural community in south eastern Nigeria. BMC Health Serv Res. (2017) 17:715. doi: 10.1186/s12913-017-2653-x
43. Gebremedhin, T, Atnafu, A, and Dellie, E. Community-based newborn care utilisation and associated factors in Geze Gofa rural district, South Ethiopia: a community-based cross-sectional study. BMJ Open. (2020) 10:e037792. doi: 10.1136/bmjopen-2020-037792
44. Bogale, TN, Worku, AG, Yalew, AW, Bikis, GA, and Tigabu Kebede, Z. Mothers treatment seeking intention for neonatal danger signs in Northwest Ethiopia: a structural equation modeling. PLoS One. (2018) 13:e0209959. doi: 10.1371/journal.pone.0209959
Keywords: health post readiness, sick children, community level care, iCCM context, care seeking
Citation: Mekonnen WN, Tiruneh GT, Birhane A and Mekonnen W (2025) Health post readiness and its influence on mothers’ care-seeking practice for their sick children in Ethiopia. Front. Public Health. 13:1569970. doi: 10.3389/fpubh.2025.1569970
Edited by:
Tafadzwa Dzinamarira, ICAP in Zimbabwe, ZimbabweReviewed by:
Udochisom Anaba, Tulane University School of Public Health and Tropical Medicine, United StatesAbdi Geda Gedefa, Mattu University, Ethiopia
Efa Ambaw Bogino, Wolaita Sodo University, Ethiopia
Copyright © 2025 Mekonnen, Tiruneh, Birhane and Mekonnen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wassie Negash Mekonnen, d2Fzc2llbmVnYXNoaEBnbWFpbC5jb20=
 Wassie Negash Mekonnen
Wassie Negash Mekonnen Gizachew Tadele Tiruneh
Gizachew Tadele Tiruneh Adugnaw Birhane
Adugnaw Birhane Wubegzier Mekonnen
Wubegzier Mekonnen