- 1Department of General Surgery, The University of Jordan, Amman, Jordan
- 2School of Medicine, The University of Jordan, Amman, Jordan
Introduction: Waterpipe smoking has gained popularity globally, often perceived as a safer alternative to cigarettes, particularly among young adults. This study aimed to assess the prevalence, socio-demographic effects, knowledge, attitudes, and behaviors toward waterpipe tobacco smoking (WTS) among healthcare students in Jordan.
Methods: Using a quantitative cross-sectional design, data was collected from August 2022 to February 2023 through a structured, anonymous online survey. Out of 2003 responses, 1988 met the inclusion criteria.
Results: The prevalence of waterpipe tobacco smoking was 46.3%, predominantly among males (59.6%). Univariate analysis linked WTS with age, gender, year of study, father’s education, and cigarette smoking. Logistic regression showed higher WTS odds in males and cigarette smokers. Waterpipe tobacco smokers viewed WTS as less addictive than cigarettes.
Discussion: High WTS prevalence among healthcare students suggests societal acceptance and misinformation-driven use, despite awareness of health risks. Comprehensive studies and educational interventions are recommended.
1 Introduction
Hookah, Narghile, Shisha, and Hubble bubble, these are all common names used worldwide to describe waterpipe tobacco smoking (WTS), a method of tobacco consumption which originated in India and the Middle East in the 16th century. It was developed by physician Hakim Abul Fath as an allegedly safer alternative to smoking, as it involves the passage of the smoke through water prior to its inhalation which was believed to filter out toxins reducing its harm and addiction (1). However, current research refutes his claims, with various studies linking WTS to numerous health risks such as periodontitis, cardiovascular diseases, metabolic disorders, respiratory illnesses, pregnancy complications, and various cancers (2–4). Additionally, studies indicated up to a tenfold increase in carbon monoxide inhalation due to the long duration of WTS smoking sessions, exposing users to higher level of carcinogens and heavy metals (5, 6).
Despite these risks, this practice has gained popularity worldwide, transcending cultural boundaries to become prevalent in several regions such as Europe, North Africa, and the United States (7). For instance, a study conducted among university students from four major public universities in the Western Cape, across all faculties found that 63% of them had smoked a waterpipe at least once in their lives (8). Similarly, data from the 2011 National Youth Tobacco Survey (NYTS) found that 7.3% of adolescents in the United States reported WTS at least once in their lifetime (9). Additionally, WTS was recorded with a prevalence of 4.8% among international medical students in Germany and Hungary (10). However, despite its growing popularity, the persistent misconception of WTS being a safer alternative continues to drive its use, highlighting the need for better public awareness of its health consequences.
A study completed in King Saud University in 2019 reported several common reasons behind WTS among university students including passing time (45.2%), relieving stress (33.3%), and the availability of various flavors of tobacco which attracts individuals with various taste preferences (11). Another study showed that the increase in WTS prevalence can be attributed to various factors like its easy acceptability, as it is commonly enjoyed in cafes and lounges among friends (7). It is increasing prevalence may be largely attributed to its social allure, as it is often viewed as communal activity (5, 6). Jordan, located in the northern part of the Arabian Peninsula, has a diverse population consisting of both urban and rural communities, with a total population of around 11 million people (12). Its population has a slightly higher proportion of males compared to females, with males comprising 52.9% of the country’s demographic (13). Additionally, Jordan has one of the youngest demographics with 63% of its inhabitants under the age of 30 (14).
Despite the country’s ongoing efforts to reduce tobacco consumption, Jordan has one of the highest rates of tobacco use in the region including cigarettes, waterpipes, cigars and pipes, with a prevalence of 32.3% (15). The country ranks second globally for tobacco smoking among adult males (70.2%), with a notable prevalence of 23.3% among the youth (16, 17). Cigarette smoking is the most prevalent form of tobacco use, accounting for 93.0% of tobacco use, and WTS is the second most common form, representing 8.6% of the cases (15). A recent study in Jordan reported that 41.3% of urban Jordanians over the age of 18 engaged in WTS (18). WTS has experienced a notable rise in several countries in the Middle East such that Turkey recorded 32.7% among university students,29.5% in Lebanon, 51.5% in United Arab Emirates, and Saudi Arabia witnessed an increase from 36.6% in 2010 to 46.6% in 2019 (19). However, Jordan stands out with a particularly high prevalence among its university students, where approximately 56% have used waterpipes (20). This high level of tobacco use has led the United Nations to declare the rising tobacco epidemic in Jordan as a public health emergency.
These findings extend to healthcare students as well, making it crucial to study the underlying reasons as this demographic tends to have a critical role in promoting public health and modeling healthy behavior in their respective community (2). In a study targeting university students in Jordan, students from medical faculties demonstrated more knowledge and awareness about the risks and harmful effects of WTS in comparison to their non-medical peers (3). Despite this awareness, many healthcare students still choose to engage in this activity.
Thus, gaining a comprehensive understanding of the reasoning behind their behavior can provide an insight into potential gaps in medical education and challenges faced by this specific population. This study aims to investigate the prevalence, associated factors, and knowledge of WTS in healthcare students in Jordan.
2 Methodology
2.1 Study design
This study took place at the healthcare faculties of the University of Jordan (UJ), Jordan’s largest and oldest university, located in the capital city Amman (21). Its central location makes it an attraction to students from various backgrounds across Jordan, with an enrollment of over 38,418 students as of 2023 (22). It comprises six medical faculties, holding the highest number of healthcare students among all other institutions in Jordan (23). This study utilized a quantitative cross-sectional design to investigate the prevalence and associated factors of WTS among healthcare students in the country. The cross-sectional nature of our study enabled us to study multiple outcomes within a single time frame.
2.2 Sampling technique
A random probability sampling method was implemented to select a sample from the total population of 11,323 healthcare students currently enrolled in healthcare specialties like medical laboratory sciences, rehabilitation, medicine, dentistry, pharmacy, and nursing programs at the University of Jordan (22). The use of this method ensured a sample that is representative of the broader student population, enhancing the generalizability and statistical validity of our findings. It also contributed to reducing researcher bias, consequently increasing the reliability of our study.
2.3 Data collection
The data was collected between August 2022 and February 2023 via a structured, anonymous, self-administered online survey developed using Google forms. This instrument was developed and validated based on The Grounded Psychometric Development and Initial Validation of the Health Literacy Questionnaire (HLQ), as well as three other published studies: Measuring Waterpipe Tobacco Smoking in Survey Research by Erin L. Sutfin, Characteristics, Reasons, Behavior, and Knowledge Toward Waterpipe Smoking in Saudi Arabia by Elluru Venkatesh, and the Global Adult Tobacco Survey (GATS)—2020.It was then modified and adapted to suit the purpose of our study (24–27). The privacy provided by this method of data collection ensured that students felt comfortable disclosing their smoking habits, reducing potential social desirability bias.
The survey consisted of 42 questions, defining WTS as “a form of tobacco consumption that utilizes a single or multi-stemmed instrument to smoke flavored or non-flavored tobacco, where smoke is designed to pass through water or other liquid before reaching the smoker” (28). It covered questions on demographics, behavior, perception, and knowledge of water pipe smoking as well as comparative views with cigarette smoking. For this research, 42 questions were analyzed, and their outcomes were examined thoroughly.
Out of the 2003 responses received, 1988 were included in the final analysis as they fulfilled the inclusion criteria which includes consent and being a healthcare student at the University of Jordan. When analyzing the grade point average (GPA) with WTS, only 1,542 responses were used as 446 responses were excluded due to incomplete responses. Among the 1988 participants, 920 were WT smokers, however, when asked to provide complete details regarding their WTS habits, only 249 provided complete details. The remaining 671 incomplete responses were excluded during the analysis of tendencies, behaviors, beliefs, knowledge and perceptions of WT smokers.
2.4 Data analysis
This data was analyzed using IBM SPSS Statistics version 27.0.1. Categorical variables were presented as numbers and percentages, and continuous variables as mean and standard deviation. Univariate analysis was performed to assess associated factors with waterpipe smoking, using independent-sample t-test for continuous variables and Chi-square test for categorical variables. Any p value < 0.05 was considered to be significant. Post-hoc analysis was utilized with p-value set according to the Bonferroni adjustment (29). Binary logistic regression was then carried out to analyze the predictive variables associated with waterpipe smoking. A goodness-of-fit test was carried out through Hosmer-Lemeshow test, indicating the model as a good fit with a p-value higher than 0.05 (p = 0.955). The logistic regression test was carried out with the exclusion of GPA due to incomplete responses.
Behavior, perception and knowledge were assessed using a Likert scale of 3 levels (Disagree, Neutral, Agree). The analysis of knowledge and perception’s association with waterpipe smoking was assessed using Chi-square tests.
2.5 Ethical considerations
This study received approval from the Institutional Review Board (IRB) of the Ministry of Health (MOH). Additionally, participants were informed of the purpose of the study and were asked to sign their informed consent prior to their participation. They were assured of the confidentiality and anonymity of their responses, as well as their right to withdraw at any time.
3 Results
3.1 Participant characteristics
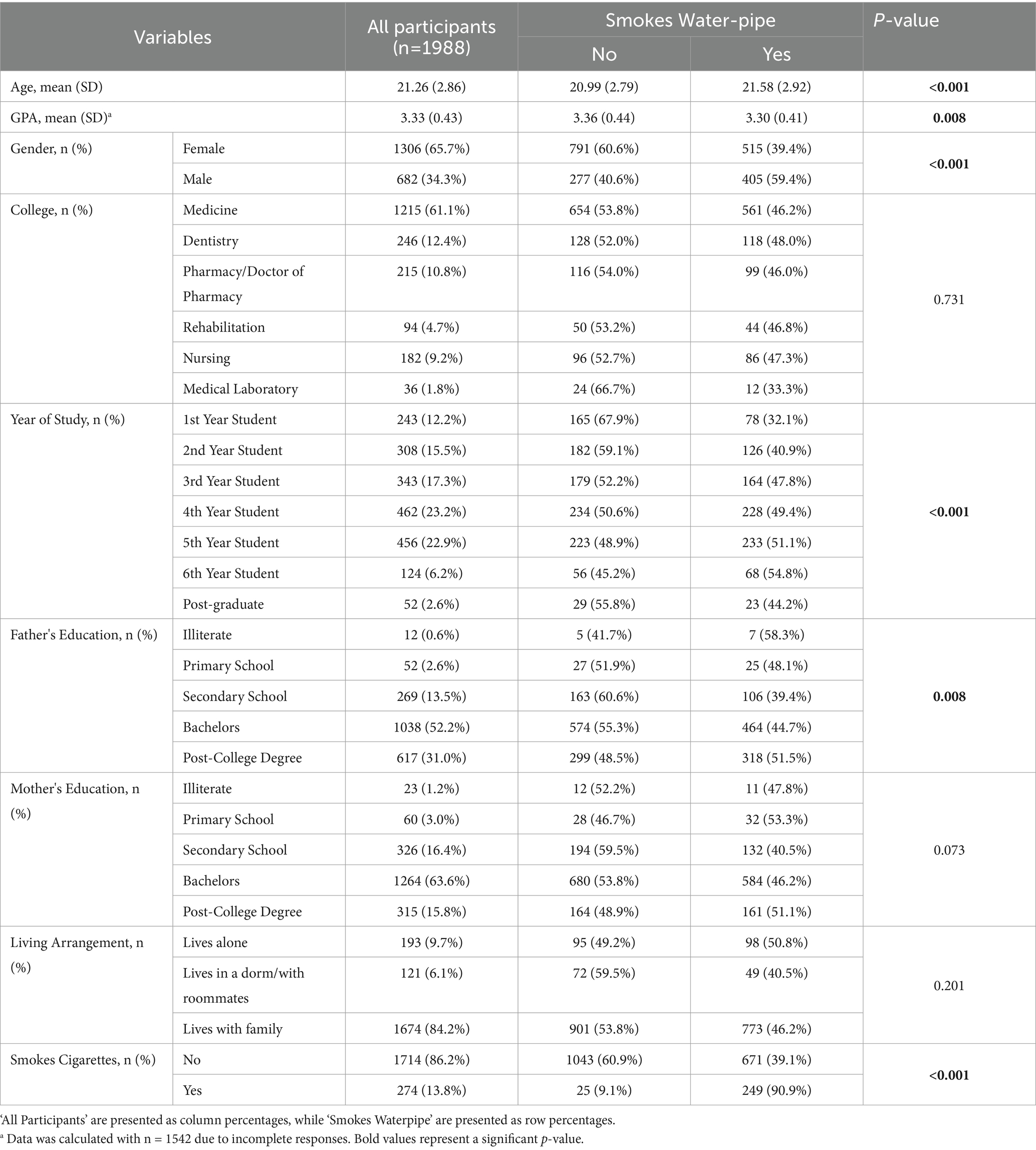
The total number of respondents in this study was 1988. Over half of the participants (65.7%) were female. Two-thirds of the participants were enrolled in medicine (61.1%). The majority of students were fourth and fifth-year students (23.2 and 22.9%, respectively) as medicine in Jordan is a six-year degree. Both father’s and mother’s education of the participants were mainly bachelor’s degrees (52.2 and 63.6%, respectively). The mean age of our sample was 21.26 years (SD = 2.86), as post-graduate students in the healthcare field enrolled in further programs (internship, residency, fellowship, masters, etc.) were included in our sample. GPAs were averaged at 3.33/ 4.0 (SD = 0.43). Out of our sample, 13.8% (n = 274) reported smoking cigarettes (Table 1).
3.2 The association between demographic factors and water-pipe tobacco smoking
Out of our participants, 920 (46.3%), answered ‘Yes’ to WTS. We found that 59.6% of males and 39.4% of females were self-reported WT smokers. Dentistry students had the highest percentage of WT smokers (48.0%), while medical laboratory students had the lowest (33.3%). The average age of WT smokers was higher than non-smokers (μ = 21.58, SD = 2.92 vs. μ = 20.99, SD = 2.79, respectively). The average GPA of WT smokers was lower than non-smokers (μ = 3.30, SD = 0.41 vs. μ = 3.36, SD = 0.44). Sixth-year students had the highest percentage of WT smokers (54.8%), while first-year students had the lowest (32.1%). Students with illiterate fathers or mothers holding a primary school diploma had the highest percentage of WT smokers (58.3 and 53.3%, respectively). Of students who lived alone, 50.8% were WT smokers. As for participants who answered ‘No’ for cigarette smoking, 39.1% reported as WT smokers, whereas almost all (90.88%) cigarette smokers were WT smokers (Table 1).
An independent-samples t-test revealed statistical significance in mean age (t (1986) = 4.592, p = <0.001, 95% CI [0.337, 0.839]) and GPA (t (1540) = −2.655, p = 0.008, 95% CI [−0.10025, −0.01506]) between WT smokers and non-smokers. Chi-square test also showed statistical significance for gender X2 (1, N = 1988) = 71.731, p < 0.001, year of study X2 (6, N = 1988) = 33.303, p < 0.001, father’s education X2 (4, N = 1988) = 13.789, p = 0.008, and cigarette smoking X2 (1, N = 1988) = 254.253, p < 0.001 between WT smokers and non-smokers. Post-hoc analysis comparing z-scores of two proportions with Bonferroni adjustment was carried out. The proportion of first-year student non-smokers was statistically higher than that of WT smokers (p < 0.001). Post-hoc analysis also revealed statistical significance of WT smokers with fathers of higher studies education (p = 0.01).
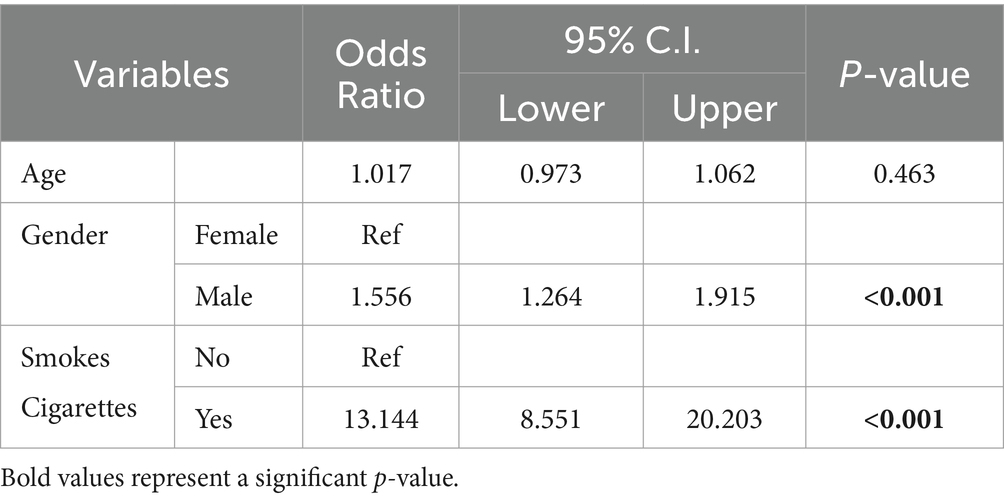
Binary logistic regression showed that gender and cigarette smoking were significantly associated with WTS while age, year of study and father’s education were not. GPA was not included in the model due to missing values. According to the model, the odds of males to WT smoke were 1.56 times higher of those of females. Cigarette smokers’ odds of WTS were 13.14 times higher than those who do not smoke cigarettes (Table 2).
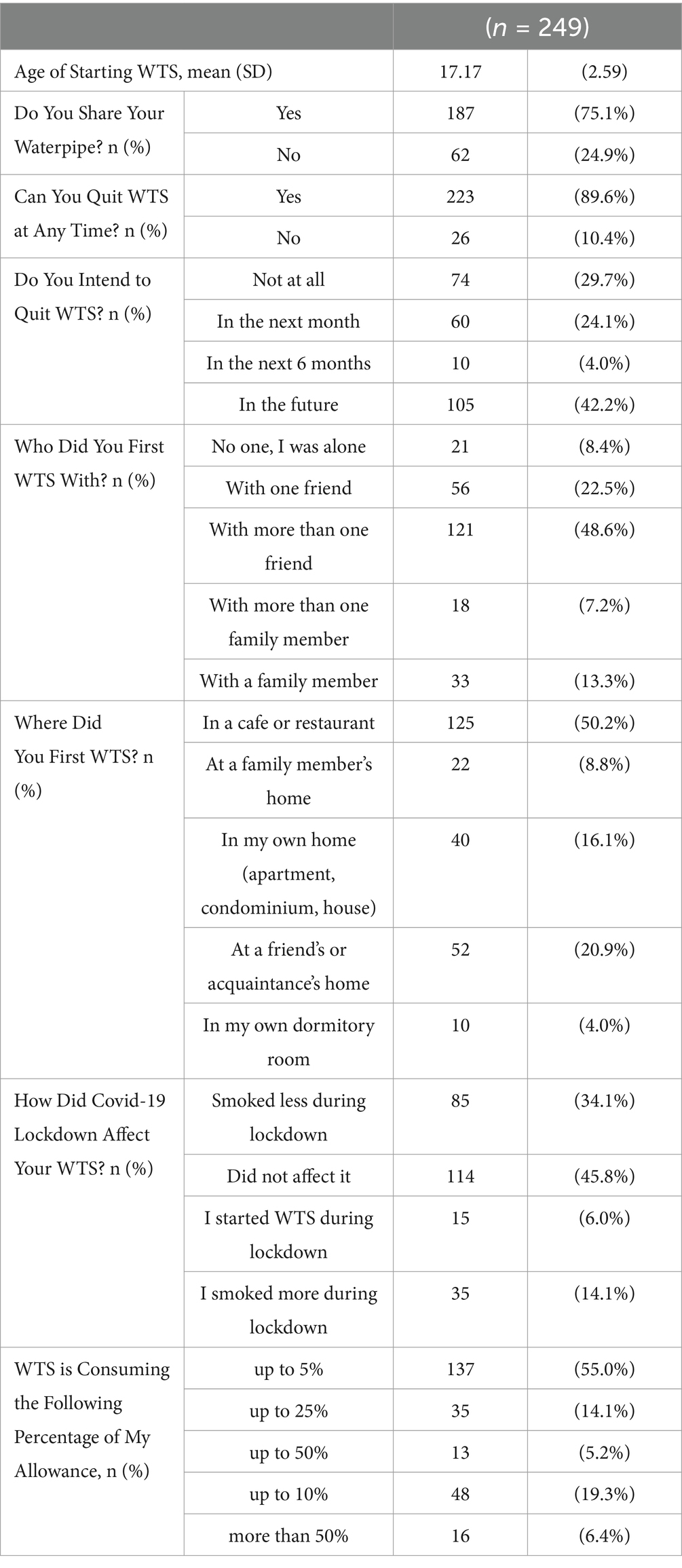
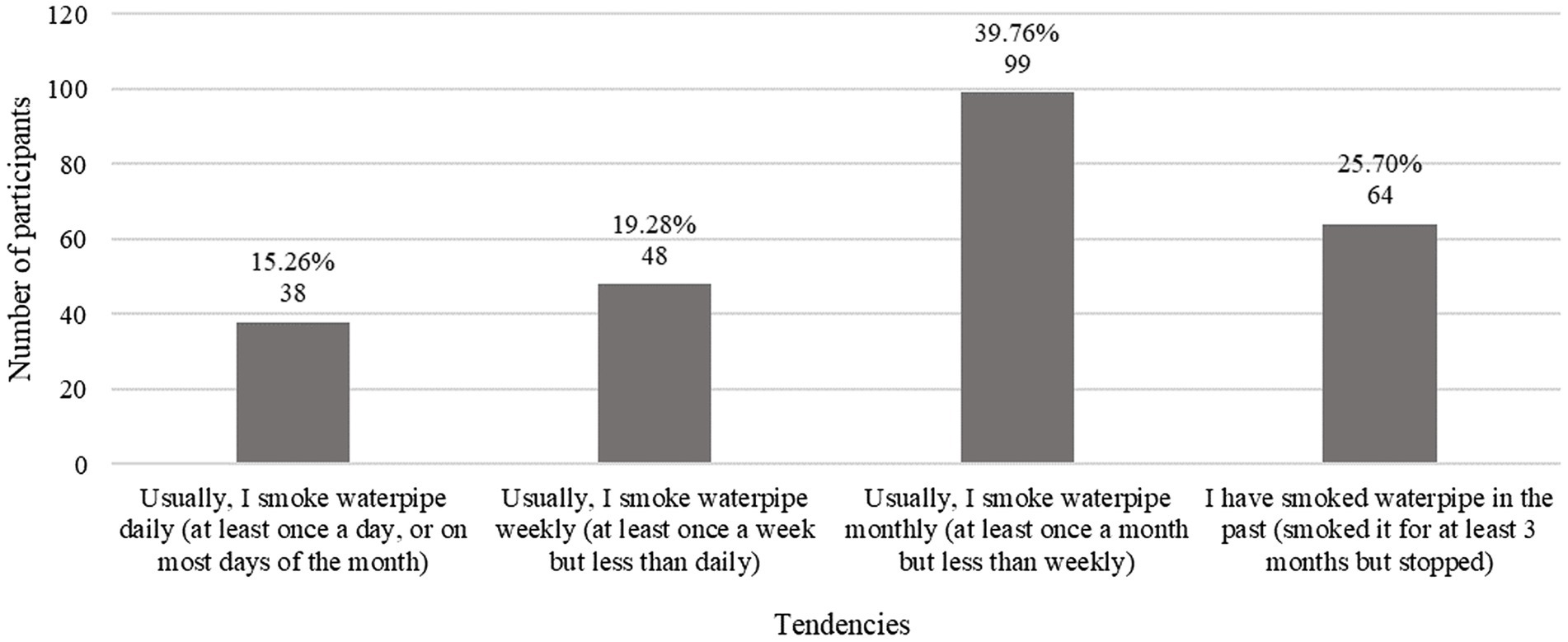
Of the 920 participants who reported WTS, 249 submitted complete responses surrounding their WTS details. The mean age of starting WTS was approximately 17.17 (SD = 2.59; Table 3). More than a third (39.76%, n = 99) of WTS participants reported smoking monthly (Figure 1).
Almost all (89.6%) of WT smokers believed they could quit WTS at any time, however 29.7% answered that they do not intend on quitting and 42.2% said they would quit in the foreseeable future. Almost half (48.6%) of WT smokers had their first WTS experience with more than one friend, and 50.2% first WT smoked at cafes or restaurants. Around three-quarters of the WT smoker participants (75.1%) have shared their waterpipe. More than half (55.2%) reported that WTS consumed only up to 5% of their allowance. When asked about the effect of Covid-19 lockdown on their WTS habits, 45.8% of WT smokers said it had no effect at all (Table 3).
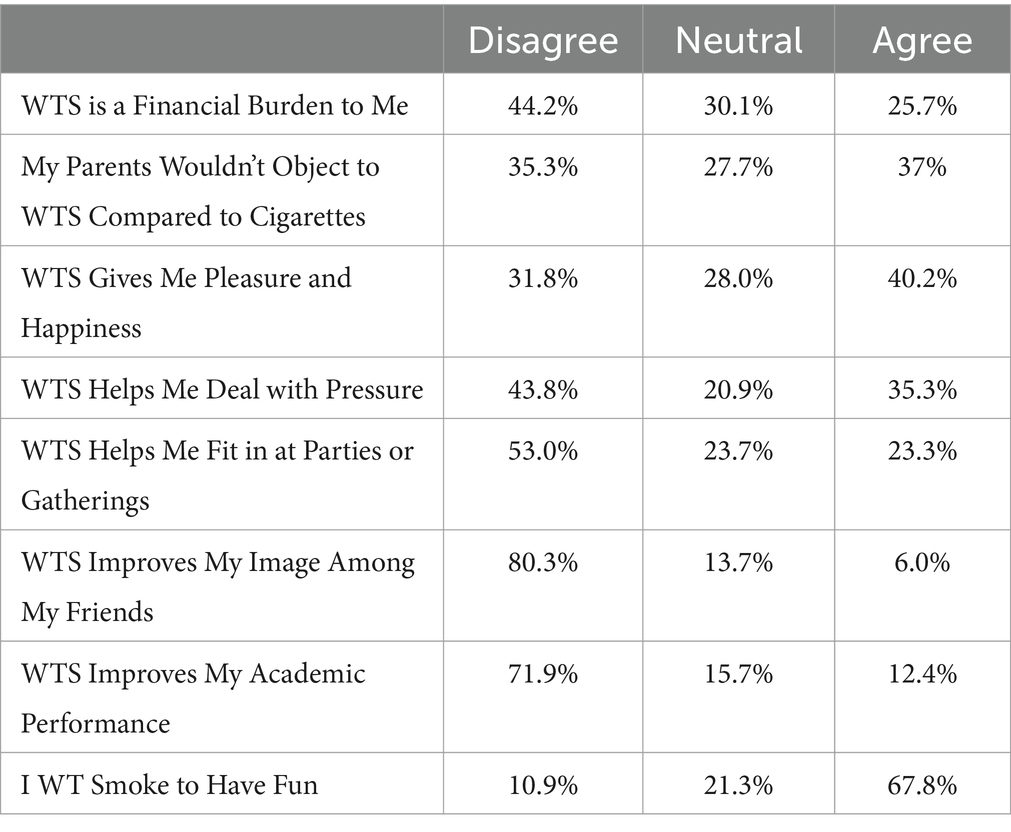
Almost half (44.2%) of our WT smoker participants disagreed with WTS being a financial burden. Additionally, 35.3% agreed with sentiment that their parents would object to WTS compared to cigarette smoking, and 27.7% felt neutral about it. WTS gives happiness to around 40.2% of smokers, while 31.8% disagreed with the statement. Almost half (43.8%) disagreed about WTS helping them deal with pressure, as well as helping them fit in at parties or gatherings (53.0%). A large percentage (80.3%) of WT smokers reported that WTS does not improve their image among their friends. Around three-quarters (71.9%) believed that WTS does not improve their academic performance. Lastly, more than two-thirds (67.8%) WT smoke to simply have fun (Table 4).
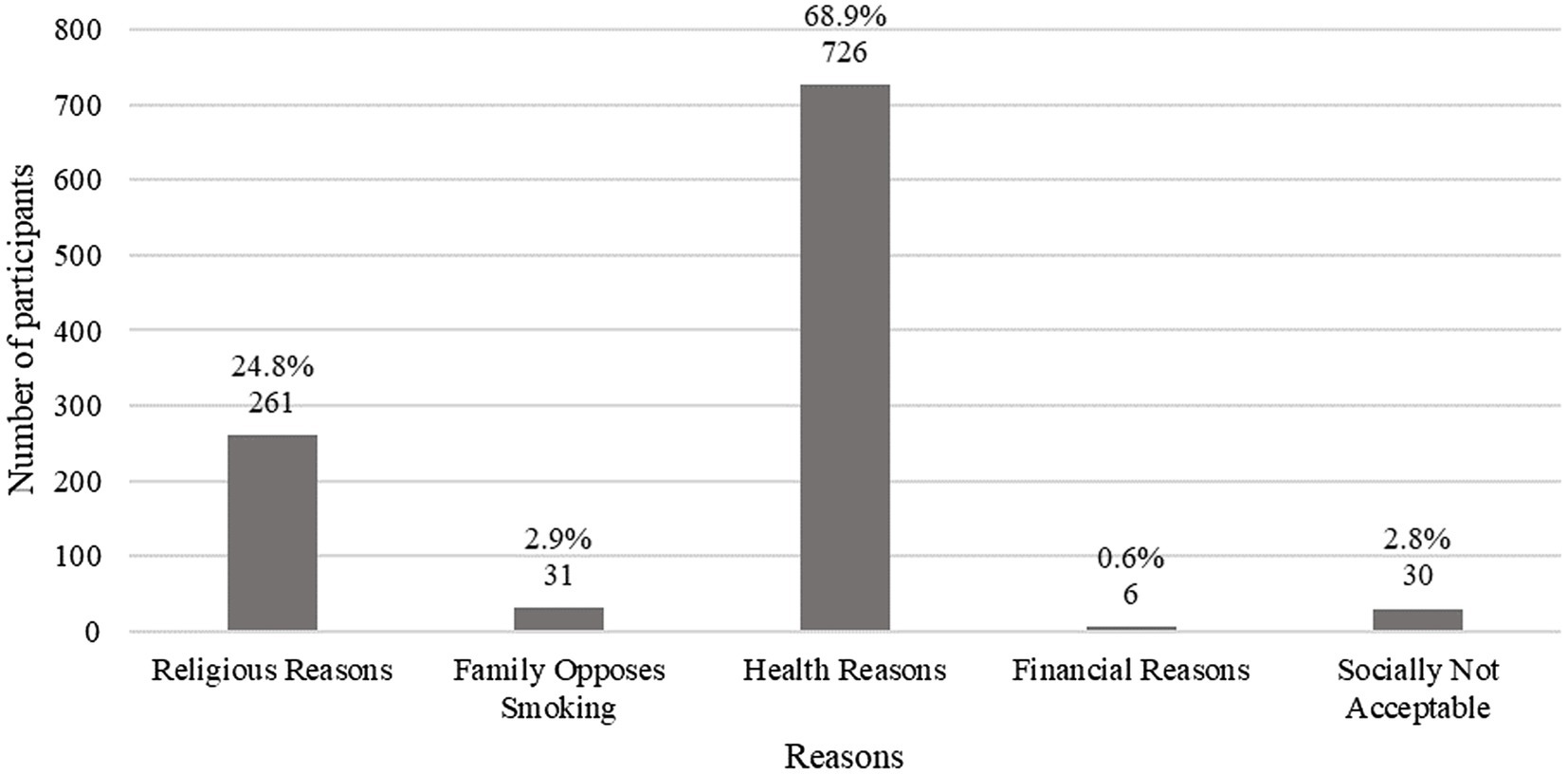
Of the 1988 participants, 1,068 (53.7%) answered ‘No’ to ever WTS. Over two-thirds (68.88%, n = 726) of non-smokers chose health as a reason for abstaining from WTS, with religious reasons following at 24.76% (n = 261; Figure 2).
3.3 Knowledge and perception of participants regarding WTS
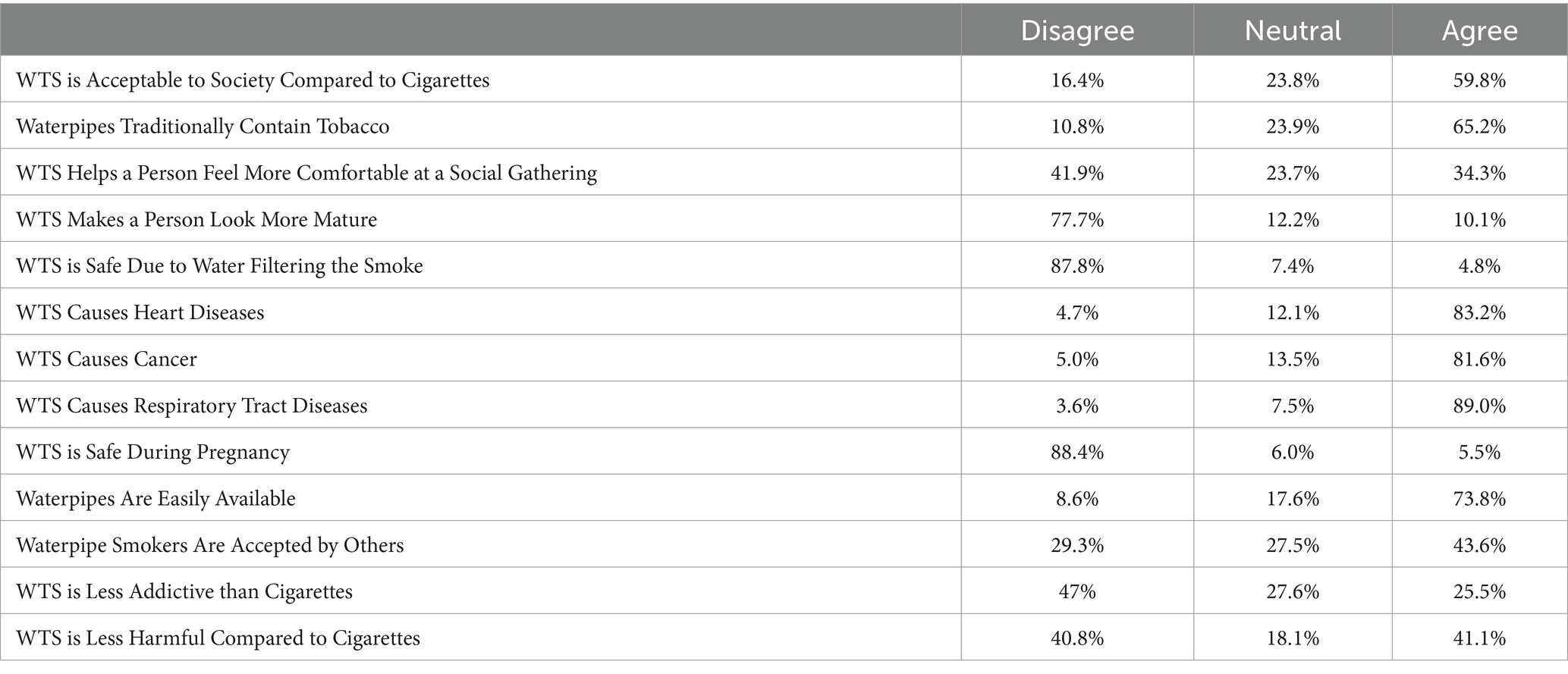
Of our 1988 participants, 59.8% believe that WTS is acceptable to society compared to cigarette smoking. When asked if WTS contains tobacco, 65.2% agreed while the rest disagreed or were neutral regarding the statement. Moreover, 41.9% disagree that WTS helps a person feel more comfortable at a social gathering and 23.7% took a neutral stance. More than three-quarters (77.7%) disagreed with the idea of WTS making a person look more mature. Almost all participants (87.8%) do not believe that WTS is safe due to the water filtering the smoke. Of our participants, 83.2% agreed that WTS causes cardiac diseases, 81.6% agreed that it causes cancer, and 89.0% agreed that it causes respiratory difficulties. As for safety of WTS during pregnancy, 88.4% disagreed. When asked if WTS was easily accessible, 73.8% agreed. Almost half (43.2%) agreed that WTS is accepted by others, while 29.3% disagreed. Almost half (47.0%) of our participants disagreed with the statement that WTS is less addictive that cigarette smoking. Although 41.1% believe it is less harmful than cigarettes, 40.8% disagreed (Table 5).
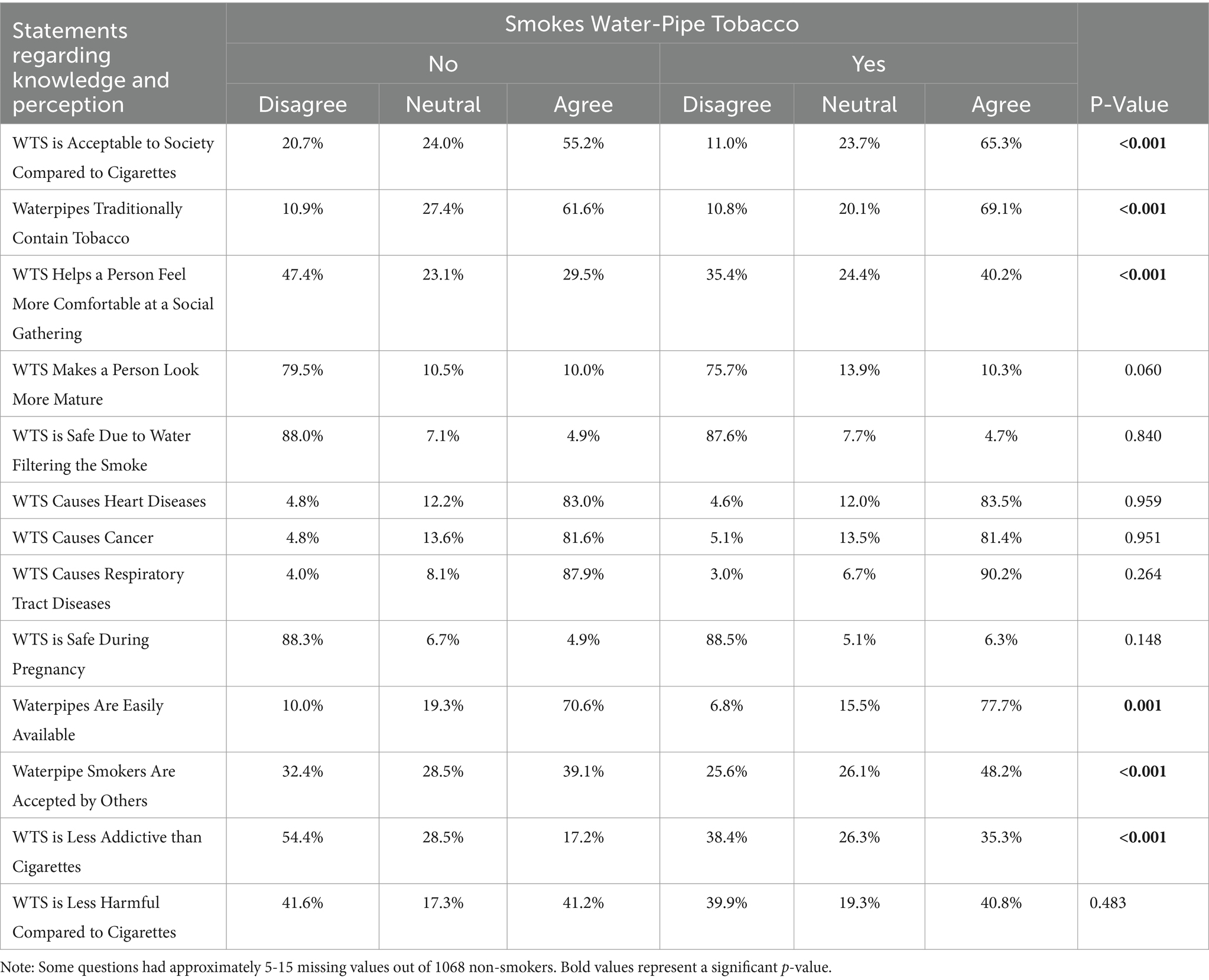
Chi-square tests revealed statistical difference between WT smokers and non-smoker’s knowledge and perception regarding: WTS acceptability in society (p < 0.001), WTS containing tobacco (p < 0.001), helping a person feel more comfortable at a social gathering (p < 0.001), availability of WTS (p = 0.001), acceptability by others (p < 0.001), and lower addiction than cigarettes (p < 0.001; Table 6).
4 Discussion
Our study examined the prevalence of WTS among healthcare students in Jordan, including demographics, knowledge, attitudes, and behaviors. The findings revealed a high prevalence of WTS at 46.3%, which surpasses the prevalence of cigarette smoking (13.2%). This observation indicates a greater tendency toward WTS compared to cigarettes, thus, highlighting an increased shift in popularity and acceptance toward it among healthcare students. Unlike similar studies conducted in other regions, there is a lack of research that examines WTS prevalence among healthcare students in Jordan, making direct comparisons difficult. However, two other studies reported comparable findings among healthcare students; a WTS prevalence of 37 and 48.9% in Southeastern US and Saudi Arabia, respectively (2, 30).
Age and gender were significantly associated with WTS in our study, with the majority of WT smokers being male (59.6%), despite our sample being predominantly female (65.7%). Similarly, another study with a female dominant sample found that mostly male students WT smoke. The study suggested that social and cultural norms in countries like Saudi Arabia and some Mediterranean countries may discourage female smoking as it is not seen as a socially acceptable behavior (31). This could also explain the results of our study conducted in Jordan. Furthermore, the findings align with Daradka’s study, which also noted the impact of age (32). This may be due to having expanded social networks and increased participation in social events as individuals grow older, as well as greater access to venues offering WTS. In contrast, another study found no significant association of age and gender with waterpipe smoking (19).
Most of our sample of WT smokers stated no significant change in their smoking frequency during Covid-19. This may be due to the participants adhering to a fixed smoking routine that is not affected by the lockdown routine. The finding contradicts that of a study done in Arab countries in 2022, where WTS was significantly higher in Jordan during Covid-19 compared to the WTS levels before the pandemic (33).
Parents’ educational background was observed to play a role as well, with higher levels of paternal education being associated with a higher prevalence. This might be explained by the fact that parents with a higher educational level tend to earn a higher income, enabling their children to afford WTS habits easily. Additionally, the academic year and performance of individuals also contributed significantly, with lower GPAs and higher academic years being associated with higher prevalence. This aligns with Jawad’s study, which found that fifth-year students were more likely to engage in WTS (34). The association between low GPAs and increased prevalence of WTS may be attributed to general unhealthy lifestyle habits that students adopt to manage academic pressure and emotional distress.
A significant correlation was identified between cigarette smoking and WTS, with 90.88% of our cigarette smokers tending to engage in WTS. Another study on Jordanian adults found that participants who smoked cigarettes within the past 30 days were almost 2.69 times more likely to use WTS (35). Similar studies conducted in the US and Lebanon among university students also found cigarette smoking to be a strong predictor of WTS use (36, 37). This may be due to their misconception that other forms of smoking have a lower risk compared to cigarette smoking. Most of our WT smokers reported smoking monthly and 89.6% believed that they can quit at any time, due to possibly considering WTS to be a social activity rather than a habitual act. An intent to quit was noted in 42.2% of the smokers versus 29.7% which stated no intention of quitting. Similar results were seen in a study conducted in Jordan on dental students, where the proportion of WT smokers who had an intent to quit was 42.0% (38). Understanding this perceived sense of self-control over smoking tendencies is crucial to help develop appropriate and effective cessation programs.
As for the non-WT smokers, most cited health reasons, followed by religious reasons as primary motivations for their abstinence. To our knowledge, no previous articles have reviewed motivators for abstaining from WTS, however our findings were similar to those of abstaining from cigarette smoking. For instance, a study conducted among medical students in King Fahad medical city identified these same motives (health and religion) as important markers for not initiating cigarette smoking or giving up on smoking (39).
In addition, most of our waterpipe smokers stated that they only smoke for fun. However, when asked whether it provided them with a sense of happiness and pleasure, the responses were equally divided between agreement and disagreement. This suggests that there may be other underlying reasons behind their decision to WT smoke, and according to our findings, the strong social aspect of WTS might be the motivator. Similar studies have highlighted other reasons beyond fun and enjoyment as motivators for WTS such as peer pressure, relieving social anxiety, for experience and out of curiosity (40).
The majority of our WT smokers stated that they frequently participated in the social aspect of waterpipe sharing. Nearly half of the WT smokers disclosed that they originally initiated this habit with family or friends in public settings like cafes or restaurants and the majority stated that they frequently participated in the social aspect of waterpipe sharing. This finding is consistent with studies that have correlated increased accessibility of waterpipes in cafes and restaurants with higher prevalence rates, as well as studies that have observed its role as a tool for socializing in some communities (19, 41). Contrary to expectations, our sample demonstrated that although WTS was perceived as more socially acceptable than cigarette smoking (59.8%), most participants agreed that it did not make them feel more comfortable at social gatherings.
We observed a disparity between knowledge and behavior among our sample, prompting the need to develop strategies to address these misconceptions urgently. Despite a significant awareness among our population regarding the adverse aspects of WTS such as its tobacco content, addictiveness, and associated health risks like cardiac diseases, cancers, respiratory difficulties, and pregnancy complications, the prevalence of WTS remained to be considerably high. Additionally, responses were varied regarding whether WTS is less harmful than cigarette smoking. These findings align with previous studies that noted students’ general awareness of these risks may not necessarily influence their decision to continue using WTS (3). Regarding the students’ level of knowledge, some studies agreed with our findings while others disagreed (3, 40). This might be due to varying levels of public health among different populations and a lack of unified and effective global efforts to create public awareness which reach their intended populations. As for the evident disparity between understanding the risks but still smoking, there might be an element of optimism bias; where a person thinks they are invulnerable, and a negative event will happen to others but not them. Additionally, students who WTS should be guided to smoking cessation clinics more often, and there is a need for positive role models and continuous educational efforts for them (3, 40).
Our findings highlight the influence of actual experience on the levels of knowledge and perception of WTS. Significant differences were observed between WT smokers and non-smokers in their perception of the acceptability of WTS compared to cigarettes, awareness of the tobacco content in waterpipes, social acceptability, and availability. Additionally, more WT smokers tended to believe that WTS brought them comfort at social gatherings, whereas most non-WT smokers disagreed. Furthermore, non-WT smokers disagreed with WTS being less addictive than cigarette smoking, while WT smokers were evenly split between agreement and disagreement. This contrasts with a study that found that university students who WT smoke perceived WTS as less addictive. This suggests that healthcare students may have a lower level of misinformation compared to other university students (40).
Based on our findings, several actions are needed to reduce waterpipe smoking (WTS) among healthcare students at the University of Jordan and address the underlying causes and behaviors. Smoking cessation programs should target both cigarette and waterpipe smoking, given the direct relationship between the two, with 90.88% of cigarette smokers also engaging in WTS. These programs must focus on combating the belief that WTS is a harmless social activity, while promoting healthy stress-coping strategies and offering a support network for students. In addition, the study highlights the significance of religious and health motivations for non-smokers. Since religion plays a pivotal role in Jordan, religious leaders could be key in promoting anti-smoking messages. Collaborations between religious leaders and universities to host seminars on the religious stance against smoking and its health consequences could align religious values with healthier lifestyle choices. Furthermore, stronger regulations are needed to limit WTS in public spaces. This includes banning its use in settings like cafes and restaurants and enforcing existing laws that prohibit underage purchasing and smoking, with clear and strict penalties for violations. By implementing these strategies, WTS prevalence could be reduced and a healthier environment could be provided for students.
A limitation to this paper is its exclusive focus on healthcare students at the University of Jordan, which might limit its generalizability to students from other universities. However, the effect of this limitation is alleviated, due to utilizing a large sample size from Jordan’s largest university, which holds the highest number of healthcare students. Additionally, the cross-sectional nature of our study limits our ability to establish causality as there may be still some residual confounding factors despite our efforts to control them. In addition to that, our choice of data collection method does not account for recall bias.
To the best of our knowledge, this study is one of the few recent papers exploring WTS among Jordanian healthcare students specifically, as most studies have shifted their focus to e-cigarettes. Despite the growing popularity of e-cigarettes, WTS prevalence continues to rise, which highlights the importance of research and continuous efforts to combat this increase.
A longitudinal study that follows WT smokers, tracking the changes in their behavior over time, and evaluating the long-term effects of cessation programs and educational campaigns is recommended to gain further insight into the factors affecting WTS tendencies in this crucial group, due to their vital societal role and the extensive healthcare-related responsibilities.
5 Conclusion
Our findings indicate that the recorded high prevalence of WTS among healthcare students presents a public health concern that is primarily influenced by societal acceptance and misinformation despite the students’ awareness of the associated health risks. Future comprehensive studies on the impact of social approval are suggested. The social nature of WTS introduces significant public health concerns regarding second-hand smoke exposure. In order to develop effective cessation programs, governments must take action to address the persistence of misinformation, as well as work on reducing the accessibility of waterpipes, and banning WTS in public and social venues.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This retrospective study was approved by Jordan University Hospital Institutional Review Board and all procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and the principles of the World Medical Association Declaration of Helsinki. The requirement for informed consent was waived for this study owing to its retrospective nature by the Jordan University Hospital Institutional Review Board.
Author contributions
AB: Conceptualization, Project administration, Resources, Supervision, Visualization, Writing – review & editing. SM: Conceptualization, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. MS: Conceptualization, Resources, Supervision, Writing – review & editing. FB: Writing – original draft, Writing – review & editing, Formal analysis, Project administration, Visualization. SO: Writing – original draft. EZ: Methodology, Writing – original draft. NA: Data curation, Investigation, Methodology, Writing – original draft. RR: Data curation, Investigation, Methodology, Writing – original draft. FB-K: Data curation, Investigation, Methodology, Writing – original draft. MO: Data curation, Investigation, Methodology, Writing – original draft. LA: Data curation, Investigation, Methodology, Writing – original draft. RA: Conceptualization, Resources, Supervision, Writing – review & editing. RA-T: Conceptualization, Formal analysis, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kadhum, M, Sweidan, A, Jaffery, AE, Al-Saadi, A, and Madden, B. A review of the health effects of smoking shisha. Clinical Medicine, (2015) 15:263–6. doi: 10.7861/clinmedicine.15-3-263
2. Alqahtani, MM, Goodfellow, LT, Zimmerman, RD, and Zavorsky, GS. Waterpipe smoking in health-care students: prevalence, knowledge, attitudes, and motives. Respir Care. (2019) 64:321–7. doi: 10.4187/respcare.06263
3. Al-Sawalha, NA, Almomani, BA, Al-Shatnawi, SF, and Almomani, BN. Attitudes and knowledge of the harmful effects of Waterpipe tobacco smoking among university students: a study from Jordan. Environ Sci Pollut Res. (2021) 28:43725–31. doi: 10.1007/s11356-021-13888-5
4. Mariam, Z, Abdelalim, B, and Ghallaba, N. The effect of waterpipe smoking on periodontal health among a sample of adult Egyptian patients: a hospital based cross-sectional study. Advanced Dent J. (2023) 5:98–109. doi: 10.21608/adjc.2023.181538.1217
5. Aslam, HM, Saleem, S, German, S, and Qureshi, WA. Harmful effects of shisha: literature review. Int Arch Med. (2014) 7:7. doi: 10.1186/1755-7682-7-16
6. Von Rappard, J, Schönenberger, M, and Bärlocher, L. Carbon monoxide poisoning following use of a water pipe/hookah. Dtsch Arztebl Int. (2014) 111:674–9. doi: 10.3238/arztebl.2014.0674
7. Muzammil, AAD, Al Rethaiaa, A, Al Mutairi, A, Al Rashidi, T, Al Rasheedi, H, et al. Prevalence and perception of shisha smoking among university students: a cross-sectional study. J Int Soc Prev Community Dent. (2019) 9:275–81. doi: 10.4103/jispcd.JISPCD_407_18
8. Kruger, L, Van Walbeek, C, and Vellios, N. Waterpipe and cigarette smoking among university students in the Western cape. South Africa Am J Health Behav. (2016) 40:416–26. doi: 10.5993/AJHB.40.4.3
9. Amrock, SM, Gordon, T, Zelikoff, JT, and Weitzman, M. Hookah use among adolescents in the United States: results of a national survey. Nicotine Tob Res. (2014) 16:231–7. doi: 10.1093/ntr/ntt160
10. Balogh, E, Faubl, N, Riemenschneider, H, Balázs, P, Bergmann, A, Cseh, K, et al. Cigarette, waterpipe and e-cigarette use among an international sample of medical students. Cross-sectional multicenter study in Germany and Hungary. BMC Public Health. (2018) 18:591. doi: 10.1186/s12889-018-5494-6
11. Amin, H, Alomair, A, Alhammad, A, Altwijri, F, Altaweel, A, and Alandejani, T. Tobacco consumption and environmental exposure among healthcare students in King Saud University in Riyadh. J Family Med Prim Care. (2020) 9:657–63. doi: 10.4103/jfmpc.jfmpc_1217_19
12. World Bank . Jordan world bank. (2023). Available online at: https://data.worldbank.org/country/jordan (Accessed September 13, 2024).
13. Department of Statistics Jordan . (2023). Jordanian Women: Facts and Figures, Available online at: https://dosweb.dos.gov.jo/ar/المرأة-الأردنية-حقائق-وأرقام/ (Accessed September 13, 2024).
14. UNICEF . Youth in Jordan. (2019). Available online at: https://www.unicef.org/jordan/youth (Accessed September 13, 2024).
15. Jaghbir, M, Shreif, S, and Ahram, M. Pattern of cigarette and waterpipe smoking in the adult population of Jordan (2014).
16. Bellizzi, S, AlResheidat, Z, and Boukerdenna, H. COVID-19 as a game changer for National Tobacco Policies: the experience of Jordan. Nicotine Tob Res. (2022) 24:1319–20. doi: 10.1093/ntr/ntac022
17. Arrazola, RA, Ahluwalia, IB, Pun, E, de Quevedo, Garcia I, Babb, S, Armour, BS, et al. Morbidity and mortality weekly report current tobacco smoking and desire to quit smoking among students aged 13-15 years-global youth tobacco survey, 61 Countries, 2012–2015. (2017).
18. Alkouri, O, Khader, Y, and Al-Bashaireh, AM. Prevalence of cigarettes and Waterpipe smoking among Jordanians, refugees, and migrants in Jordan and its associated factors: a secondary data analysis. Int J Environ Res Public Health. (2023) 20:20. doi: 10.3390/ijerph20010082
19. Al-Jayyousi, GF, Kurdi, R, Islam, N, Alhussaini, NWZ, Awada, S, and Abdul, RH. Factors affecting Waterpipe tobacco smoking among university students in Qatar. Subst Use Misuse. (2022) 57:392–401. doi: 10.1080/10826084.2021.2012695
20. Khabour, OF, Alzoubi, KH, Eissenberg, T, Mehrotra, P, Azab, M, Carroll, MV, et al. Waterpipe tobacco and cigarette smoking among university students in Jordan. Int J Tuberculosis Lung Dis. (2012) 16:986–92. doi: 10.5588/ijtld.11.0764
21. The University of Jordan . About UJ. (2024). Available online at: https://www.ju.edu.jo/Pages/AboutUJ.aspx (Accessed September 26, 2024).
22. Jordanian Ministry of Higher Education and Scientific Research . Available online at: https://www.admhec.gov.jo/mjr2017/UnivMajorCapacity.aspx (Accessed October 11, 2024).
23. The University of Jordan . University of Jordan schools (2024). Available online at: https://www.ju.edu.jo/Pages/Academics.aspx (Accessed September 26, 2024).
24. Osborne, RH, Batterham, RW, Elsworth, GR, Hawkins, M, and Buchbinder, R. The grounded psychometric development and initial validation of the health literacy questionnaire (HLQ). BMC Public Health. (2013) 13:658. doi: 10.1186/1471-2458-13-658
25. Sutfin, EL, McKelvey, K, Soule, E, Glasser, A, Kim, H, Wiseman, KD, et al. Measuring waterpipe tobacco smoking in survey research. Tob Control. (2019), 29:593–600. doi: 10.1136/tobaccocontrol-2019-055000
26. Venkatesh, E, Al Jemal, MY, and Al Samani, AS. Characteristics, reasons, behavior and knowledge towards waterpipe smoking in Saudi Arabia. Int J Adolesc Med Health. (2017) 32. doi: 10.1515/ijamh-2017-0090
28. World Health Organization . Why is waterpipe tobacco smoking becoming more popular, especially among young people? (2015).
29. Beasley, TM, and Schumacker, RE. Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. J Exp Educ. (1995) 64:79–93. doi: 10.1080/00220973.1995.9943797
30. Awan, KH, Alrshedan, A, Al Kahtani, M, and Patil, S. Waterpipe smoking among health sciences university students: knowledge, attitude and patterns of use. Saudi Dent J. (2016) 28:189–93. doi: 10.1016/j.sdentj.2016.05.001
31. MagdaAM, M, Youssef, HAM, Mawajdeh, A, Nabeel, AA, and Ayasreh, IRA. Awareness, attitude and practice of smoking among medical sciences& non-medical sciences students at Taif University: comparative study. Int J Sci Res (IJSR). (2015) 4:255–64.
32. Daradka, H, Khabour, O, Alzoubi, K, Nakkash, R, and Eissenberg, T. Tobacco and waterpipe use among university students in Saudi Arabia: impact of tobacco sales ban. East Mediterr Health J. (2019) 25:111–8. doi: 10.26719/emhj.18.021
33. Al Sabbah, H, Assaf, E, Taha, Z, Qasrawi, R, Cheikh Ismail, L, Al Dhaheri, A, et al. Impact of COVID-19 lockdown on smoking (waterpipe and cigarette) and participants’ BMI across various sociodemographic groups in Arab countries in the Mediterranean region. Tob Induc Dis. (2022) 20:98–16. doi: 10.18332/tid/155007
34. Jawad, M, Lee, JT, and Millett, C. Waterpipe tobacco smoking prevalence and correlates in 25 eastern Mediterranean and eastern European countries: cross-sectional analysis of the global youth tobacco survey. Nicotine Tob Res. (2016) 18:395–402. doi: 10.1093/ntr/ntv101
35. Abughosh, S, Yang, M, Wu, I, Hawari, F, Peters, R, and Essien, E. Waterpipe smoking among Jordanian adults: predictors and correlates. J Behav Health. (2012) 1:7. doi: 10.5455/jbh.20120313034424
36. Eissenberg, T, Ward, KD, Smith-Simone, S, and Maziak, W. Waterpipe tobacco smoking on a U.S. college campus: prevalence and correlates. J Adolesc Health. (2008) 42:526–9. doi: 10.1016/j.jadohealth.2007.10.004
37. Jradi, H, Wewers, ME, Pirie, PP, Binkley, PF, and Ferketich, AK. Cigarette and waterpipe smoking associated knowledge and behaviour among medical students in Lebanon. East Mediterr Health J. (2013) 19:861–8. doi: 10.26719/2013.19.10.861
38. Obeidat, SR, Alzoubi, KH, Mahasneh, AM, Bibars, ARM, Khader, YS, et al. Prevalence, social acceptance, and awareness of waterpipe smoking among dental university students: a cross sectional survey conducted in Jordan. BMC Res Notes. (2014) 7:832. doi: 10.1186/1756-0500-7-832
39. Al-Kaabba, A, Saeed, A, Abdalla, A, Hassan, H, and Mustafa, A. Prevalence and associated factors of cigarette smoking among medical students at king Fahad Medical City in Riyadh of Saudi Arabia. J Fam Community Med. (2011) 18:8–12. doi: 10.4103/1319-1683.78631
40. Arshad, A, Matharoo, J, Arshad, E, Sadhra, SS, Norton-Wangford, R, and Jawad, M. Knowledge, attitudes, and perceptions towards waterpipe tobacco smoking amongst college or university students: a systematic review. BMC Public Health. (2019) 19:439. doi: 10.1186/s12889-019-6680-x
Keywords: waterpipe tobacco smoking (WTS), healthcare students, prevalence, misinformation, societal acceptance, health risks
Citation: Bani Hani A, Mansour S, Al Smady MM, Bani Hani F, Obeidat SM, Zahran EA, Awamleh N, Rayyan R, Bani-Khaled FT, Odeh M, Alshdaifat LT, Addasi R and Al-Taher R (2025) Waterpipe tobacco smoking in healthcare students in the University of Jordan. Front. Public Health. 13:1576868. doi: 10.3389/fpubh.2025.1576868
Edited by:
Mona Mohamed Aboelkhair Alsadek Radwan, Medicine Faculty, EgyptReviewed by:
Kamal Eldeirawi, University of Illinois Chicago, United StatesAbdul Salam Nazmi, National University of Science and Technology (Muscat), Oman
Copyright © 2025 Bani Hani, Mansour, Al Smady, Bani Hani, Obeidat, Zahran, Awamleh, Rayyan, Bani-Khaled, Odeh, Alshdaifat, Addasi and Al-Taher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farah Bani Hani, YmFuaWhhbmlmYXJhaDNAZ21haWwuY29t
 Amjad Bani Hani
Amjad Bani Hani Shahd Mansour
Shahd Mansour Moaath M. Al Smady1
Moaath M. Al Smady1 Seba Mohanned Obeidat
Seba Mohanned Obeidat Eman Ahmed Zahran
Eman Ahmed Zahran Farah T. Bani-Khaled
Farah T. Bani-Khaled Mahmoud Odeh
Mahmoud Odeh Raed Al-Taher
Raed Al-Taher