- 1Division of Medical Research, Faculty of Medicine and Health Sciences, SRM Medical College Hospital and Research Centre, SRM Institute of Science and Technology, Kattankulathur, India
- 2Department of Community Medicine, Faculty of Medicine and Health Sciences, SRM Medical College Hospital and Research Centre, SRM Institute of Science and Technology, Kattankulathur, India
Introduction: India faces a growing burden of non-communicable diseases (NCDs), particularly diabetes, cardiovascular conditions, and cancer, straining the healthcare system. Given the urgent need for prevention and management, a systematic review and meta-analysis (SRMA) of health-seeking behaviors for NCDs is essential to guide targeted interventions to improve health outcomes.
Methods: The SRMA protocol was registered in PROSPERO (CRD42023476381) and conducted adhering to the Preferred Reporting Items of Systematic reviews and Meta-Analysis (PRISMA) 2020 guidelines. PubMed-Medline and Scopus databases were searched from inception to October 27, 2023. Eligible studies focused on adults (>18 years) with NCDs covered under the National Programme for prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and stroke (NPCDCS). Data extraction and risk of bias assessment were conducted using predefined criteria. Meta-analysis of quantitative data was performed using DerSimonian and Laird random-effect model.
Results: From 2,917 identified studies, 64 were included in the SRMA, with 40 suitable for meta-analysis. The meta-analysis revealed that 72.72% (95% CI 59.48–85.97%, I2 = 99.97%) of individuals sought treatment for existing health conditions, with 73.09% (95% CI 54.01–92.16%, I2 = 99.18%) preferring allopathy, compared to 8.89% (95% CI 5.56–12.22%, I2 = 86.73%) preferring Alternative medicine with a significant heterogeneity. Major barriers to seeking treatment included illness not considered serious [0.4785 (95% CI 0.4556–0.5013)] and financial constraints [0.3263 (95% CI 0.1457–0.5069)], with delays in cancer treatment attributed to lack of disease awareness [0.5091 (95% CI 0.0294–0.9888)] and painlessness [0.4502 (95% CI 0.3312–0.5692)]. Private healthcare facilities (51.26, 95% CI 42.85–59.67%) were preferred over government facilities (33.78, 95% CI 28.10–39.45%).
Conclusion: This SRMA provide a comprehensive overview of health-seeking behavior for NCDs in India. The findings underscore the complex interplay of socioeconomic, cultural, and systemic factors influencing healthcare access and outcomes. Targeted interventions addressing barriers identified in this review are imperative for improving public health and reducing the burden of NCDs in India.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42023476381.
Introduction
India is experiencing a rising burden of non-communicable diseases (NCDs) in the recent decades along with unfinished agenda of infectious diseases with a non-communicable sequelae (1, 2). Among the major NCDs, cardiovascular disease and stroke account for the significant reduction in the number of productive years and increased premature deaths (3). According to the study report of the India State-Level Disease Burden Initiative which is supported by Indian Council of Medical Research (ICMR), a 23.9% increase in the proportions of deaths due to NCDs from 1990 to 2016 was recorded (4). Additionally, a 3.7% increase in Disability associated life years (DALYs) was observed for the cardiovascular diseases during the same period (4).
The increasing burden of NCDs, places a significant strain on the healthcare system, highlighting the need for niche specific prevention and management strategies. The National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) implemented in India since 2010 is the flagship national program for prevention and control of major NCDs (5). Recognizing health as a fundamental right and understanding the health-seeking behavior among a population is pivotal not only for strengthening niche specific public health surveillance systems, thereby enhancing the health outcomes (6).
Health-seeking behavior encompasses a broad spectrum of choices and actions taken by individuals to enhance, sustain, or ameliorate their health status. Over the years, several studies have examined the health seeking behavior and the barriers to affordability and accessibility of healthcare among the Indian population (7–10). We believe, to the best of our knowledge this Systematic Review and Meta-analysis (SRMA) is a pioneering effort to explore the patterns and processes associated with the health-seeking behavior of the Indian populace. To this end we have conducted a SRMA of studies focusing on the health-seeking behaviors of individuals afflicted with NCDs across the Indian subcontinent. The primary objective of this systematic review and meta-analysis is to synthesize available evidence on the patterns and determinants of health-seeking behavior among individuals with non-communicable diseases (NCDS) in India. Specifically, this review aims to (i) Estimate the prevalence of individuals with NCDs seeking treatment in various settings across India. (ii) Examine the patterns of healthcare utilization, particularly the preference between public and private healthcare providers. (iii) Assess the preferred system of medicine, including the choice between allopathic and AYUSH-based treatments. (iv) Identify and analyse factors associated with health-seeking behavior, such as age, gender, education, socioeconomic status, place of residence, and awareness of disease. (v) Explore the reasons for not seeking treatment and delay in seeking treatment among individuals diagnosed with or exhibiting symptoms of NCDs. Findings of this SRMA will hopefully form the foundation for targeted interventions aimed at improving health outcomes and strengthening public health programs across the Indian subcontinent.
Methods
Search strategy and selection criteria
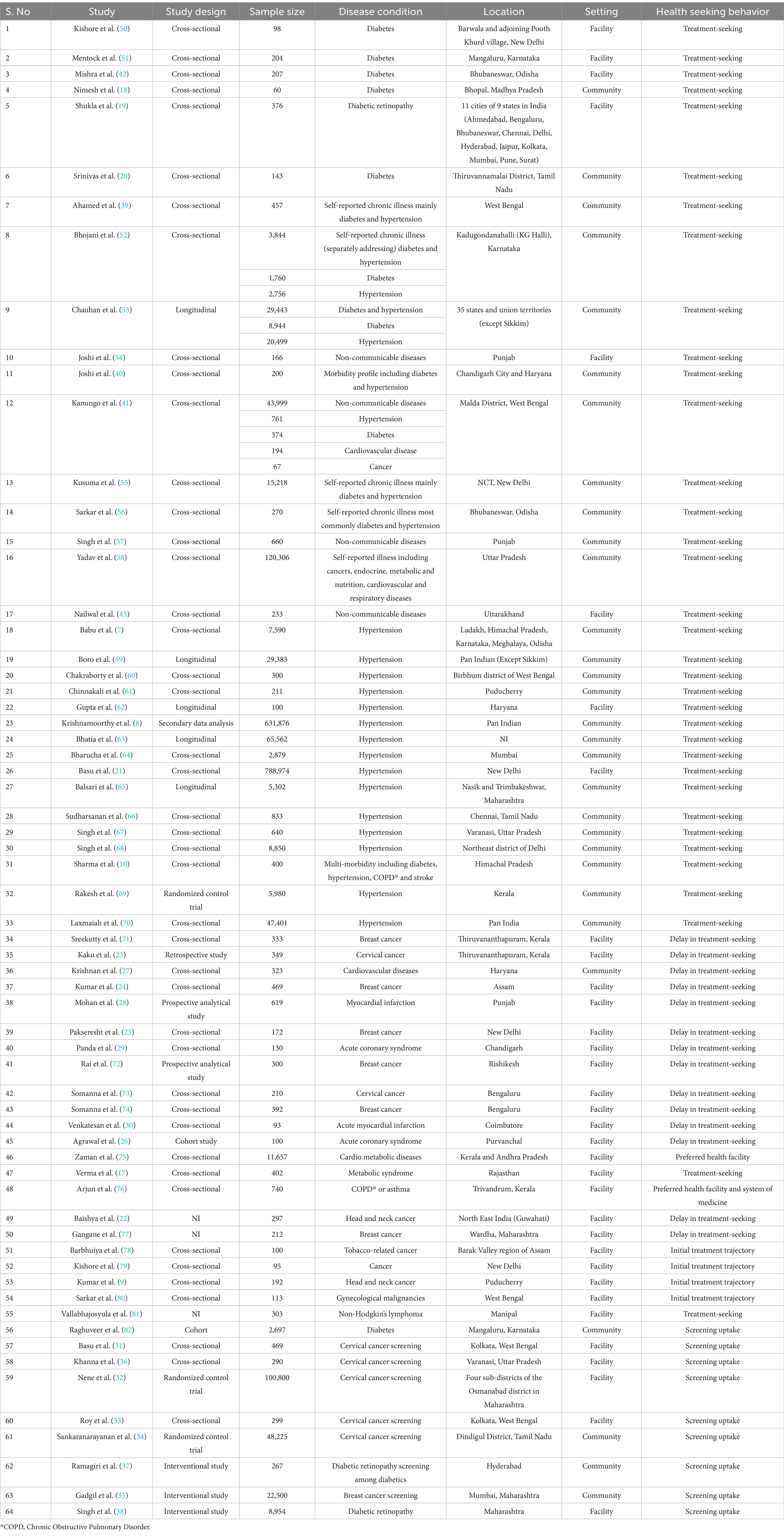
The SRMA protocol was registered in PROSPERO (CRD42023476381) and conducted adhering to the Preferred Reporting Items of Systematic reviews and Meta-Analysis (PRISMA) 2020 guidelines (11). We searched PubMed-Medline and Scopus databases for studies related to health-seeking behavior for NCDs in India from its inception till October 27, 2023. The search terms were identified based on the PEO approach, i.e., P (Population)- Human participants of any age, E (Exposure) -Non-communicable diseases, O (Outcome)- Health-seeking behaviors and S (Settings)- India. Both free text words and MESH terms were wherever necessary. A sensitivity and precision maximizing strategy was adopted to identify relevant studies. The detailed search strategy is presented in Supplementary Tables S1, S2. Inclusion criteria comprises of studies on adults (>18 years) exposed to NCDs under NPCDCS, included diabetes and its complications, hypertension, cardiovascular diseases, stroke, cancer, metabolic associated fatty liver, and chronic obstructive pulmonary disease. Studies assessing health-seeking behaviors, such as seeking treatment, type of healthcare facility visited, lifestyle modifications, and preventive screenings, were included. Studies on communicable diseases, other NCDs (mental health problems, neurodegenerative diseases, orthopedic disorders, and autoimmune diseases), qualitative studies on health-seeking behaviors, and HPV vaccine acceptability studies were excluded. Two reviewers (MH and DN) independently assessed the title, and abstract (TiAb) of the studies based on the eligibility criteria using Rayyan, a web-based tool designed to facilitate systematic review screening. Although Rayyan offers artificial intelligence (AI)-assisted features to expedite the screening process, these features were not utilized in this review. All screening decisions were made manually by the reviewers to ensure methodological rigor and consistency (12). Full text of the studies which passed the TiAb screening were reviewed. Any discrepancies in the decision (inclusion or exclusion) were solved by mutual consensus (Table 1).
Data analysis
Data was extracted independently by two authors (HM & DN) in a data extraction form created in MS Excel 2013. From the included studies, general study information, design, sample size, location, population demographics, disease prevalence, treatment-seeking behavior, reasons for not seeking treatment, preferred health facility and system of medicine and factors associated with the health seeking behavior were extracted. Risk of bias assessment was conducted independently by two reviewers (RRL and SPJ) using Appraisal tool for Cross-Sectional Studies (AXIS) tool for all the included studies. The AXIS tool consists of 20 items that cover key domains such as the clarity of study aims, appropriateness of study design, justification of sample size, definition and selection of the target population, measurement validity and reliability, risk of non-response bias, description and appropriateness of statistical methods, ethical approval, and funding declarations, as well as clarity and transparency of results and conclusions. Each item is evaluated with one of the following responses: Yes, No, or Do not know, providing a structured and comprehensive framework for critical appraisal of the studies’ methodological quality (13).
Meta-analysis of proportions was performed using the DerSimonian and Laird random-effect model (14). The random-effects model was chosen because it assumes that the true effect sizes may vary between studies due to differences in study populations, settings, or methodologies. This model accounts for both within-study variance and between-study heterogeneity, making it more appropriate for combining results from observational studies. Visual assessment of the forest plots, the Cochran-Q test, and I-squared (I2) statistics were used to assess heterogeneity among the included studies. The I2 value greater than 25% or the Cochrane- Q less than 0.1 was considered to be the indicator of heterogeneity between the included studies. The source of heterogeneity was further investigated by the sub-group analysis. Publication bias was assessed using Funnel plot or Eggers test (15). Meta-analysis was performed using Stata version 18 SE (16). Two-sided p < 0.05 was considered to be statistically significant except for the heterogeneity test, wherein p < 0.10 was considered significant. Studies which did not provide sufficient data for meta-analysis were synthesized qualitatively/narratively.
Results
A systematic search of PubMed and Scopus databases retrieved a total of 2,917 studies. After removing 92 duplicates, 2,825 studies were screened by title and abstract. From these, 205 studies were considered relevant for full-text retrieval. Despite efforts to contact corresponding authors, the full text of 39 studies could not be obtained. Out of the 166 studies assessed for full-text eligibility, 64 met the inclusion criteria and were included in the SRMA. The remaining 102 studies were excluded due to wrong exposure, outcome, study design, publication type, or setting, with list of reasons for exclusion and studies for exclusion provided in Supplementary Table S3. Of the 64 included studies, only 39 reported quantitative data suitable for meta-analysis. The results of the literature search, screening, and study selection process are documented in the PRISMA flowchart (Figure 1).
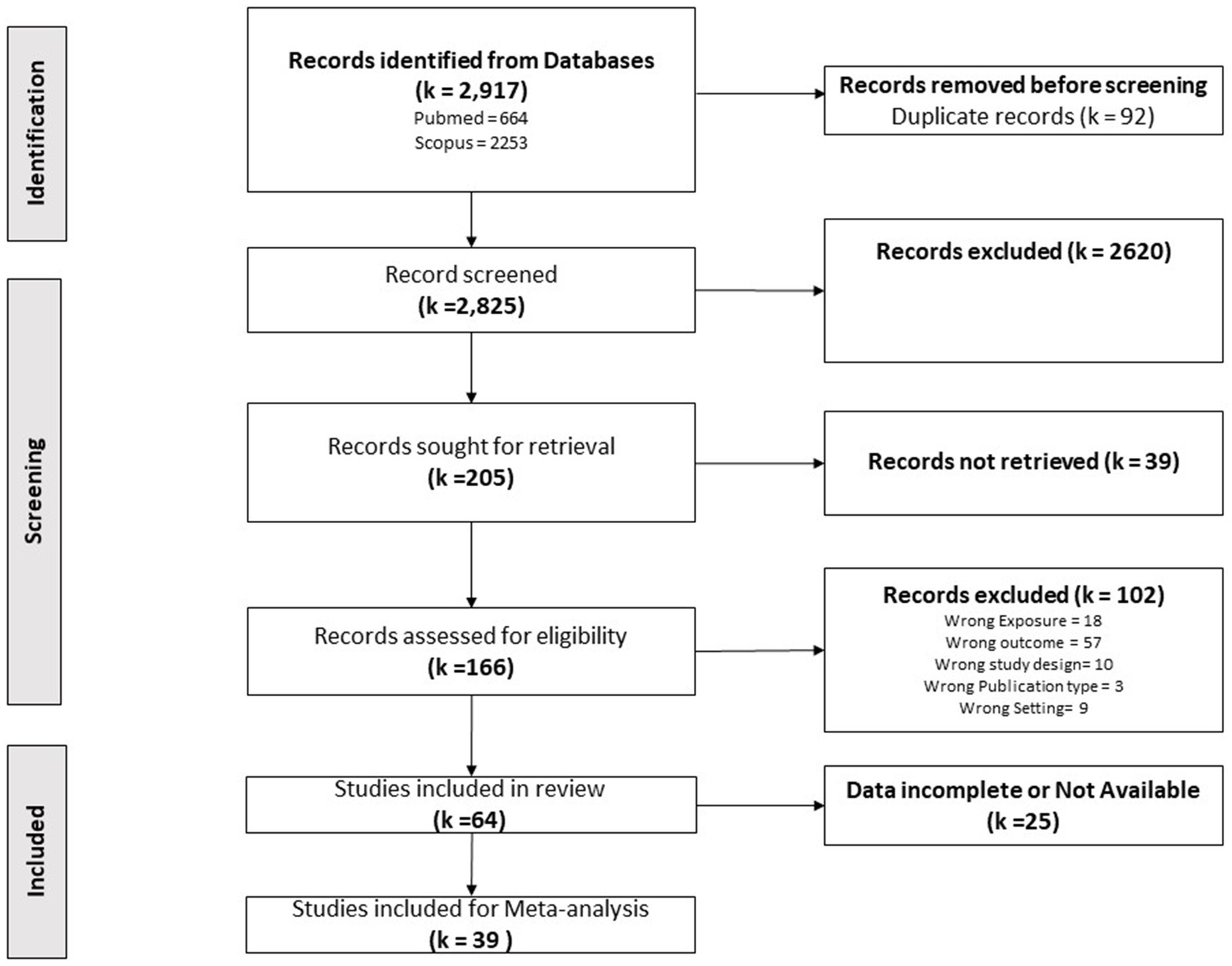
Figure 1. Study selection. PRISMA flow chart showing the total number studies identified in search, duplicates removed, studies excluded and included for the review.
Among the 64 included studies for SRMA, 36 studies were focussed on treatment-seeking for major NCDs including hypertension (16 studies), diabetes (six studies), cardiovascular disease (two studies) and Chronic Obstructive Pulmonary Disease (one study). Eleven studies were conducted within the general population, investigating the prevalence of Non-Communicable Diseases (NCDs), notably diabetes and hypertension, along with the health-seeking behaviors associated with them. Further, 14 studies addressed either presentation/treatment delays in individuals with cancer and acute cardiac conditions. Presentation delay refers to the time taken to seek formal consultation after the appearance of first symptoms, while treatment delay pertains to the time taken to initiate the appropriate treatment after diagnosis. Lastly, eight studies examined the screening uptake/willingness to undergo screening as a health-seeking behavior.
Qualitative synthesis
Eight out of the 36 studies on treatment-seeking for major NCDs, lacked quantitative data and hence, were included only for the systematic review. As per Verma et al. (17), 30% had good knowledge regarding CVD risk factors while only 9% engaged in implementing lifestyle measures. Inconsistent healthcare seeking behavior was reported among diabetic patients by Nimesh et al. (18) influenced by combination of factors including lack of improvement, affordability, accessibility, and healthcare personnel’s professional conduct. Shukla et al. (19) reported that the scale of city, type of the healthcare facility and education level had a statutory impact on health outcomes of patients afflicted with diabetic retinopathy.
Moreover, Srinivas et al. (20) reported that the noncompliance rate were extremely high among diabetic patients (57%), which was augmented by poor access to healthcare systems. Basu et al. (21) found out that treatment-seeking behaviors were absent among economically marginalized groups including rural dwellers and women. They reported 36.4% of individuals were hypertensive, while 48.5% were unaware about their condition (21).
Nine out of the 14 studies focussing on delay in treatment-seeking for cancer or acute cardiac conditions lacked sufficient quantitative data for meta-analysis and hence, were considered only for the systematic review. Health literacy and healthcare access were identified as potential strategies to mitigate delays and enhance health outcomes in four studies (22–25). Five studies focussed on presentation/treatment delays for acute cardiac conditions and stroke, highlighting the need for improving access to primary, secondary and tertiary health care facilities (26–30).
Eight studies described screening uptake out of which only six studies focussed on cancer and the remaining two focussed on diabetic retinopathy. None of the above mentioned studies provided consistent data to be included for meta-analysis, thereby limiting their inclusion only for systematic review. Studies focussing on Cancer screening revealed the influence of sociocultural barriers and demographic factors in screening uptake (31, 32). Additionally, low Pap test utilization was also reported among women which highlighted the need for effective cervical cancer screening strategies (33). Sankaranarayanan et al. (34) and Gadgil et al. (35) demonstrated the effectiveness of community-level screening strategies for cervical and breast cancer screening. Khanna et al. (36) stressed on the gap between awareness and actual participation in cervical cancer screening among community healthcare workers. Diabetic retinopathy screening studies emphasized that sustained use of health literacy videos as well as proximity to the healthcare facilities increased the screening uptake (37, 38).
Quantitative synthesis (meta-analysis with subgroup analyses)
Among the total number of included studies, only 39 provided quantitative data, which were subjected to meta-analysis. These articles focused on the health seeking behaviors which included the proportion of individuals seeking treatment for an existing health condition, the preference for government versus private healthcare facilities, the choice between allopathy and alternative medicine, the proportion of individuals not seeking treatment for varied reasons, the proportion of individuals experiencing delays in seeking treatment and the reasons behind treatment delays were pooled in the meta-analysis.
Prevalence of individuals with NCDs seeking treatment
Among the studies included, data regarding seeking treatment for existing disease conditions were reported in 20 studies. The meta-analysis of the proportion of individuals seeking treatment revealed a pooled proportion of 0.7272 (95% CI 0.5948–0.8597), with a significant heterogeneity (I2 = 99.97%) (Figure 2). To investigate the source of this heterogeneity, subgroup analyses were conducted based on disease conditions, age of the study population, study location (urban/rural/tribal), and study setting (community/facility) (Supplementary Figures S1–S4).
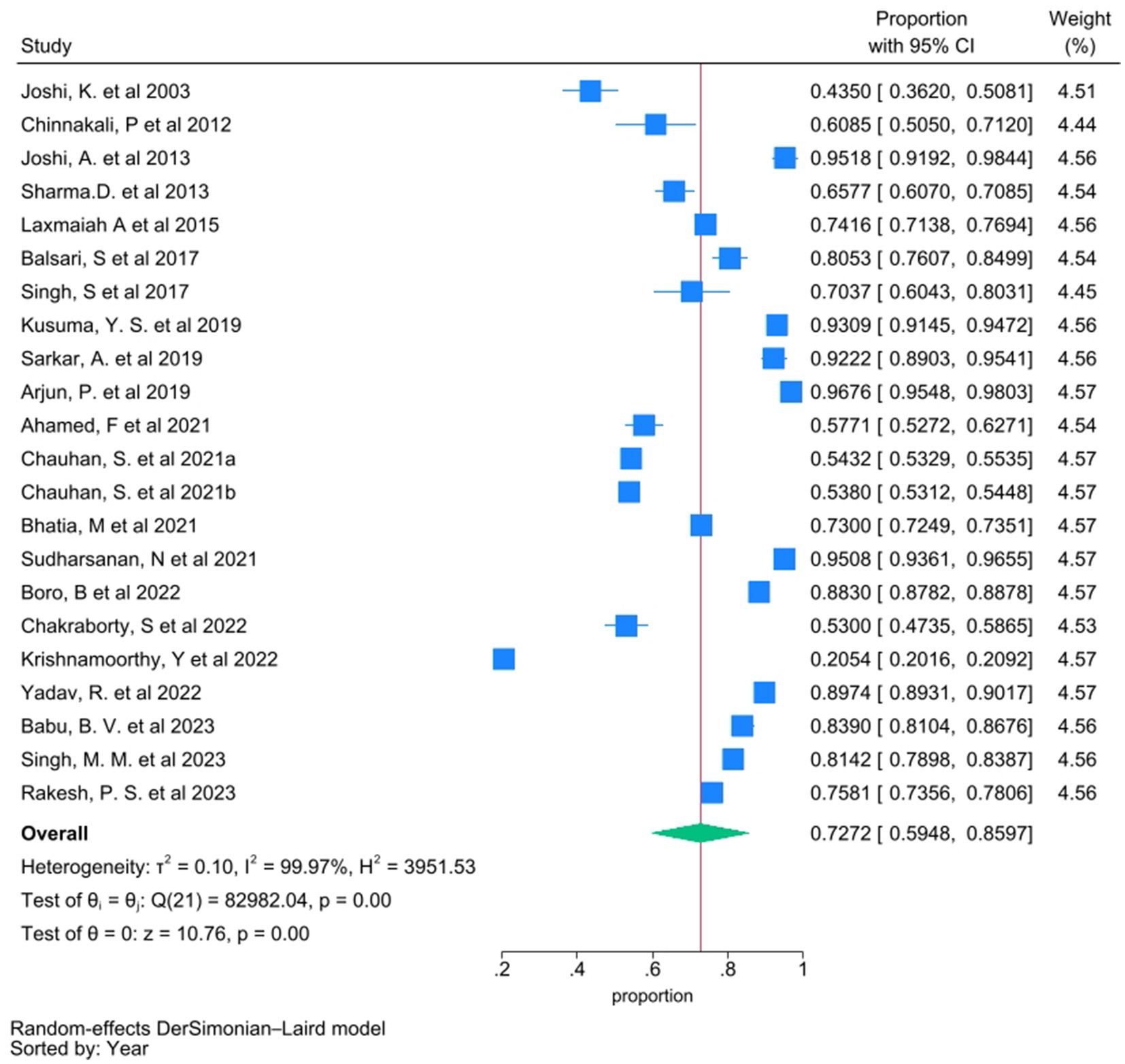
Figure 2. Forest plot showing pooled proportion of individuals who sought treatment for their existing disease condition. Proportion from individual studies was calculated by dividing the number of individuals who sought treatment with total number of individuals who had NCD/were aware of their disease condition, and synthesized by meta-analysis using random effect Dersimonian Laid model. Chauhan, S. et al. 2021a and Chauhan, S. et al. 2021b are same study with “a” indicating diabetic group and “b” indicating hypertensive group.
Patterns of healthcare utilization
Twenty studies examined the preferred type of health facilities for treatment, including government/public health facilities, private healthcare facilities, and unqualified practitioners. These studies reported the proportion of individuals seeking treatment from public or private facilities, either among those with the disease (prevalence) or those who sought treatment, which are presented as sub-groups in the forest plot analysis. The pooled proportion of individuals seeking treatment from government health facilities was 0.3378 (95% CI 0.2810–0.3945), with substantial heterogeneity (I2 = 99.42%) (Figure 3). The pooled proportion for the individual seeking care from private health facilities was 0.5126 (95% CI 0.4285–0.5967), also with substantial heterogeneity (I2 = 99.64%) (Figure 4).
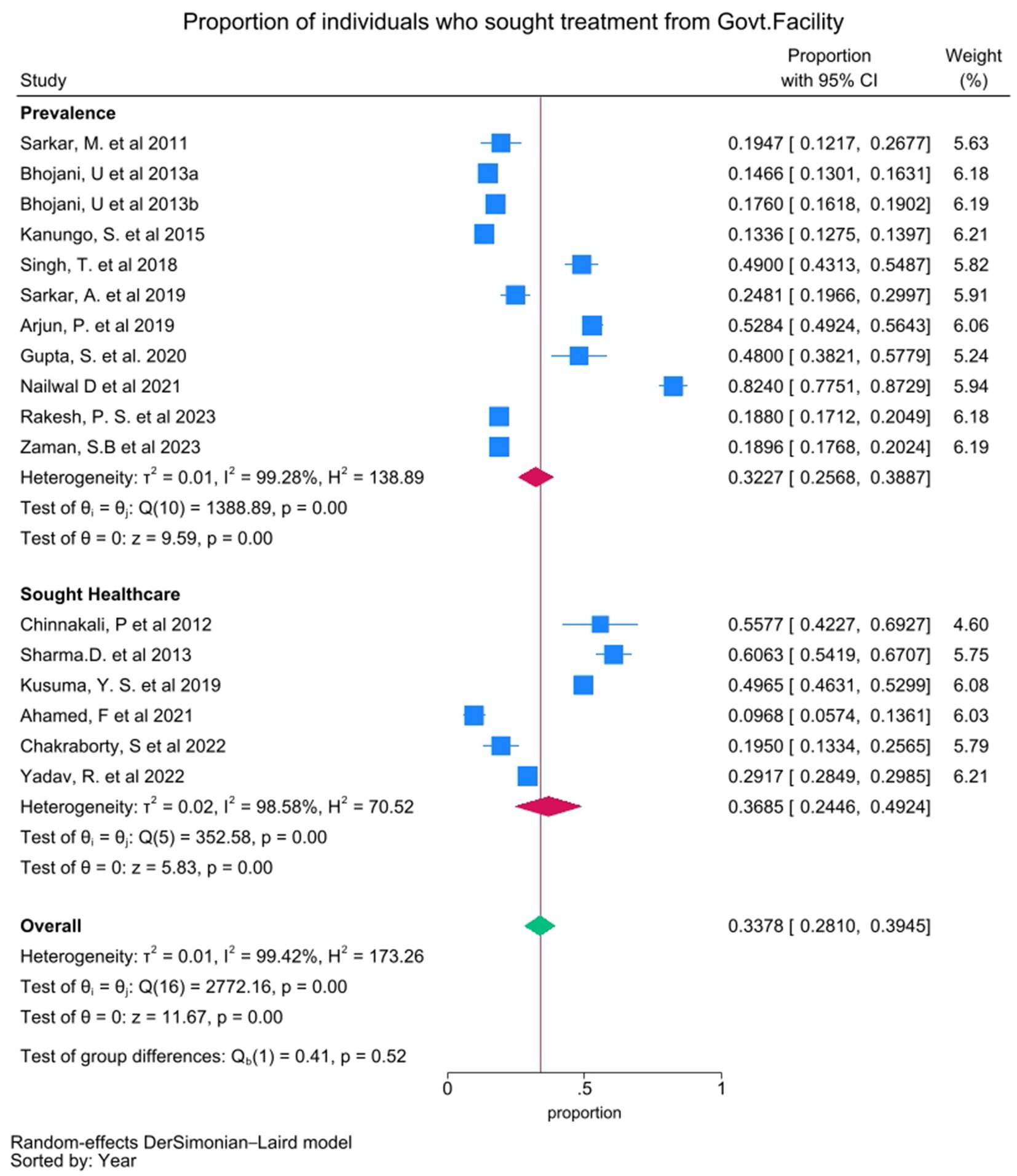
Figure 3. Forest plot showing pooled proportion of individuals who sought treatment from Government healthcare facilities. Proportion from individual studies was calculated by dividing the number of individuals who sought treatment from Government healthcare facilities with total number of individuals had NCD/sought treatment for NCD (presented as sub-groups), and synthesized by meta-analysis using random effect Dersimonian Laid model. Bhojani, U. et al. 2013a and Bhojani, U. et al. 2013b are same study with “a” indicating diabetic group and “b” indicating hypertensive group.
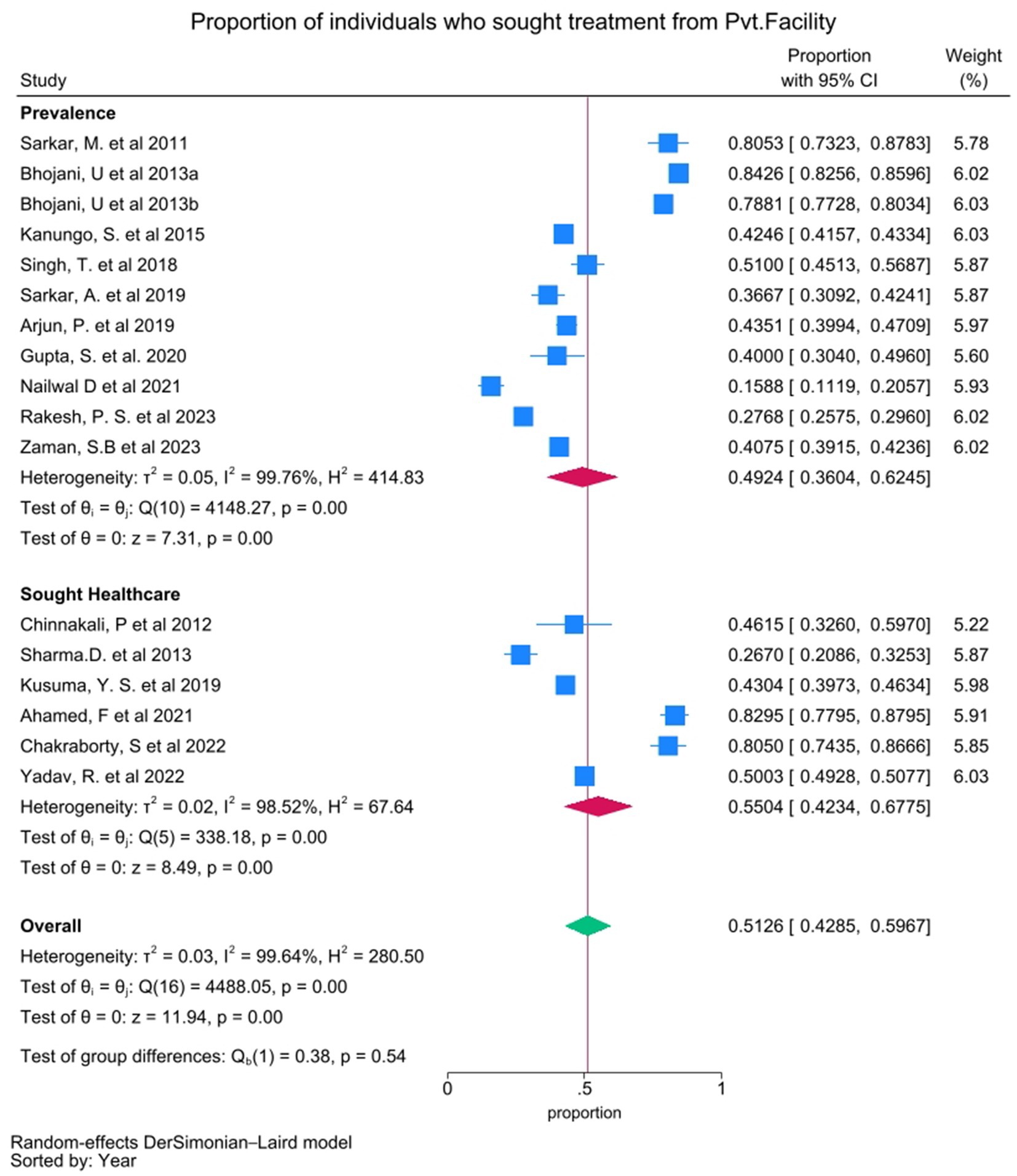
Figure 4. Forest plot showing pooled proportion of individuals who sought treatment from Private healthcare facilities. Proportion from individual studies was calculated by dividing the number of individuals who sought treatment from Private healthcare facilities with total number of individuals had NCD/sought treatment for NCD (presented as sub-groups), and synthesized by meta-analysis using random effect Dersimonian Laid model. Bhojani, U. et al. 2013a and Bhojani, U. et al. 2013b are same study with “a” indicating diabetic group and “b” indicating hypertensive group.
Preferred system of medicine
The choice between allopathic and alternative medicine was another frequently reported health-seeking behavior in the literature (10, 39–43). Our meta-analysis revealed that 73.09% (95% CI 54.01–92.16%, I2 = 99.18%) of individuals preferred allopathy, while 8.89% (95% CI 5.56 to 12.22%, I2 = 86.73%) opted for alternative medicine as their treatment choice for existing conditions, though there was substantial heterogeneity in the findings (Supplementary Figures S5, S6).
Reasons for not seeking treatment
Among the studies included for the meta-analysis, only a few studies stated the reasons for not seeking treatment. The most common reason for not seeking treatment was that the “illness was not considered to be serious.” The pooled proportion of individuals who cited this reason was 0.4785 (95% CI 0.4556–0.5013), based on data from four studies (Supplementary Figure S7). Financial constraints were the next major reason for not seeking treatment. The pooled proportion from four studies was 0.3263 (95% CI 0.1457–0.5069) (Supplementary Figure S8). Inaccessibility to healthcare facilities was another frequent reason, with a pooled proportion of 0.1329 (95% CI 0.0236–0.2422, I2 = 96.27%), based on five studies (Supplementary Figure S9). A smaller proportion of individuals reported lack of relief from treatment along with lack of trust in hospitals as the fundamental reason for not opting treatment (Supplementary Figures S10, S11). Other reasons included lack of family support, relying on faith for a cure, non-compliance with treatment, such as side effects of medications or improvement without treatment were not included in the meta-analysis due to insufficient data.
Reasons for delays in seeking treatment
Delays in seeking treatment were reported in 14 studies. Of these, four studies focused on acute cardiac conditions, while 10 studies examined various types of cancer, including breast cancer, cervical cancer and head and neck cancer. For studies focused on cancer, the average time taken between the onset of symptoms and the first hospital visit ranged from 11 to 180 days.
Some studies have reported data about the choice of initial treatment trajectory as a plausible cause of delay before reaching the actual cancer care providers (CCPs). A meta-analysis of this data revealed that while 54.62% (95% CI 38.4–70.84%) of patients consulted an allopathic physician only 21.22% (95% CI 7.38–35.05%) approached alternative medicine practitioners. Approximately 12.47% (95% CI 9.99–14.95%) visited primary health centers (PHCs) while a miniscule number of 7.28% (95% CI 2.76–11.8%) patients consulted unqualified treatment providers (including quacks and faith healers) before reaching the CCPs (Supplementary Figures S12–S15).
The most common reason for the presentation delay was a lack of disease awareness, as reported in five studies. The pooled proportion of individuals who delayed seeking treatment due to lack of knowledge about their disease was 0.5091 (95% CI 0.0294 to 0.9888), though with very high heterogeneity (I2 = 99.89%) (Supplementary Figure S16). The second major reason for delay was the absence of pain, particularly in the case of a lump, as reported in four studies. The pooled proportion was 0.4502 (95% CI 0.3312–0.5692), with substantial heterogeneity (I2 = 91.4%) (Supplementary Figure S17). Financial constraints were cited as a reason for delay in four studies, with a pooled proportion of 0.1472 (95% CI 0.0222–0.2721) (Supplementary Figure S18). Other reasons for delay included fear of diagnosis and prioritizing family responsibilities over personal health (Supplementary Figures S19, S20).
Assessment of publication bias and risk of bias
The funnel plots showed symmetry and Egger’s test indicated p = 1, suggesting no publication bias among the studies (Supplementary Figures S21–S23). ROB assessment revealed low risk of bias for the questions on study aim, design, target population, sample frame, outcome measurement tools, non-responders, risk factor and outcome variable measurement, statistical significance, reproducibility of methods, description of basic data, analyses description in methods, justification of discussion and conclusion, ethical approval and informed consent. However, high risk of bias was observed in terms of sample size justification (56%), selection bias (17%), outcome variables measured (64%), basic data description (47%), concerns about non-response bias (33%), description of non-responders (38%), consistency in results (83%), limitation (81%), funding sources or conflicts of interest (56%) (Supplementary Figures S24–S28).
Discussion
We conducted a SRMA to assess the health seeking behavior and its determinants in the Indian population who were afflicted with NCDs covered under the NPCDCS program. Specifically, we focused on attributes including treatment-seeking behavior, screening uptake as well as the presentation and treatment delay.
Our meta-analysis of 22 studies revealed that 72.72% (Figure 1) of individuals in India sought treatment for existing health conditions, which is significantly higher than the global average of 56% (95% CI: 44–68) (44). Even within the global estimate, the highest treatment-seeking rate was reported in an Indian study to be 91% (45). Thus higher treatment seeking rate in India could be attributed to several factors, including increasing awareness of NCDs, improved accessibility of healthcare services and expanding coverage through schemes like Ayushman Bharat (46). However, we also observed significant heterogeneity in our findings. Sub-group analysis showed variations in treatment-seeking patterns based on disease condition, age, study locations and settings. The majority of the included studies focused on hypertensive patients, with a treatment-seeking rate of 71.87%. A single study on COPD reported the highest treatment-seeking rate at 96.76%, while a study on diabetes showed a lower rate of 54.32%, possibly due to perceived severity (Supplementary Figure S1). This also highlights a dearth of studies on COPD and diabetes. Studies covering all ages reported the highest treatment-seeking rate at 93.17%, while a single study analyzing National Family Health Survey-4 data involving young adults with hypertension (<45 years) reported the lowest rate at 20.54% highlighting the need for age-specific strategies (Supplementary Figure S2).
Sub-groups based on studies conducted on populace residing in urban and rural areas, revealed higher treatment-seeking behavior in urban areas (84.82%) as compared to rural areas (68.04%) (Supplementary Figure S3) highlighting the disparities in healthcare access and utilization between these settings. According to Banerjee (47), education and the economic status were observed to be the major factors for the variances in the disease prevalence between the urban and rural milieus. Thus to overcome these disparities the demand is to develop nuanced niche specific surveillance strategies to promote health literacy and improve health outcomes in rural regions of the Indian sub-continent.
In contrast to the rural settings, health seeking behavior for hypertension among tribal population was observed to be higher (79.02%) (Supplementary Figure S3) among the individuals who are aware of their disease condition. However, disease awareness seems to be very poor in this population. Therefore, screening for hypertension in tribal populations is crucial to alleviate the burden of hypertension associated complications in these marginalized and under-served populations.
Facility-level studies showed higher treatment-seeking rates (96.55%) compared to community based studies (70.39%) (Supplementary Figure S4) whose discrepancy could be attributed to a selection bias, as individuals visiting a facility were more likely to be on treatment for their disease conditions. Therefore, community based studies maybe more reliable for assessing the health seeking behavior since they use a more representative sample of the population.
Our analyses revealed that private healthcare facilities were preferred in comparison to the government healthcare facilities (51.26% vs. 33.78%) (Figure 3). This disparity in preference of healthcare facilities underscores the need for community empowering ‘bottoms-up’ policies along with the strengthening of the public health infrastructure to alleviate the extant disparities with respect to accessibility and quality. Our results indicated a higher preference for the allopathic system of medicine (73.09%) compared to the alternative systems (8.89%) (Supplementary Figures S5, S6), based on the available studies. The reported results might have been influenced as most of the included studies were conducted in facilities delivering allopathic treatment. Additional investigations regarding AYUSH utilization in NCD management become essential to understand its role in India’s diverse healthcare environment. “Illness not considered to be serious” was the predominant reported reason (47.85%) for not seeking healthcare which was followed by “financial constraints” (32.63%), “non-accessibility” to healthcare facilities (13.29%), “no cure” perception (5.92%), and “distrust in hospitals” (2.95%) (Supplementary Figures S7–S11) which necessitates promotion of affordable and accessible healthcare facilities across 806 districts (and counting) of the Indian sub-continent to improve the health outcomes.
Regarding cancer as well as acute cardiac conditions, 14 studies reported presentation/treatment delay along with “Lack of awareness” (50.91%) as the major factor contributing to poor health outcomes. This forms the rationale for enhancing health literacy among the populace regarding the risk factors of various health conditions. Other factors cited were “painlessness” of cancer lumps (45.02%) followed by “fear of diagnosis” (5.84%) and “family priorities” (5.81%). Taken together, these factors indicate the confluence of misconceptions, psychosocial, and cultural barriers as taboos which hinder an individual from seeking the appropriate treatment options. Pro-active community engagement activities enmeshed with health literacy and health support campaigns are expected to significantly alleviate such barriers thereby improving timely access to affordable healthcare options.
Our SRMA highlighted certain evidence gaps toward understanding of health-seeking behavior for NCDs in the Indian sub-continent. There is a lack of broad representation of data at the pan-Indian level with majority of studies being restricted to geographically delimited areas. Additionally, current literature primarily studies healthcare-seeking behavior toward government and private providers yet overlooks the influence of unlicensed practitioners. In many rural regions without adequate healthcare facilities, people continue to seek treatment from unqualified practitioners. This should be one focus area of future research in order to comprehend the influence of such practices on health-seeking behavior. Structuring of inclusive community empowering ‘bottoms-up’ policies, along with automated allocation of the clinical resources is essential in a populace endowed with wide variation in genetic base inhabiting landscapes with unique geological relief structures contributing to segregated socio-cultural norms and practices. Furthermore, implementation of nuanced multifaceted approaches, such as Artificial Intelligence (AI)-enabled large-scale surveillance systems for now-casting and forecasting primary data, use of iterative and integrated dashboards with heuristic capabilities would be pivotal to address the diverse healthcare needs of the Indian populace (48). Establishment of Community Advisory Boards (CABs) in low- and middle-income countries, including India (49) are expected to be culturally sensitive and context specific promoting comprehensive health equality among the general populace. This in turn would construe as the platform toward the alignment with the United Nations charter of Sustainable Development Goals (SDGs).
Our study has several strengths. To the best of our knowledge, this is a pioneering effort in assessing the health-seeking behavior among the Indian population afflicted with NCDs across unique geological relief structures contributing to segregated socio-cultural norms and practices. We included a wide spectrum of NCDs to understand the intricate complexities of the health-seeking behavior comprehensively. Our study also has certain limitations. The inclusion of only quantitative studies depicting the patterns and processes associated with the health-seeking behavior of the Indian population might limit the scope of our understanding of the subtle variances in the health seeking behavior. Future research incorporating qualitative methodologies is needed to prefer a more comprehensive understanding of health-seeking behavior among the Indian populace.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. DN: Data curation, Writing – original draft. RR: Formal analysis, Writing – review & editing. SJ: Formal analysis, Writing – review & editing. VA: Writing – review & editing. RJ: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1580824/full#supplementary-material
References
1. Anjana, RM, Unnikrishnan, R, Deepa, M, Pradeepa, R, Tandon, N, das, AK, et al. Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17). Lancet Diabetes Endocrinol. (2023) 11:474–89. doi: 10.1016/S2213-8587(23)00119-5
2. GBD 2019 Child and Adolescent Communicable Disease Collaborators. The unfinished agenda of communicable diseases among children and adolescents before the COVID-19 pandemic, 1990-2019: a systematic analysis of the global burden of Disease study 2019. Lancet. (2023) 402:313–35. doi: 10.1016/S0140-6736(23)00860-7
3. Budreviciute, A, Damiati, S, Sabir, DK, onder, K, Schuller-Goetzburg, P, Plakys, G, et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. (2020) 8:574111. doi: 10.3389/fpubh.2020.574111
4. India State-Level Disease Burden Initiative Diabetes C. The increasing burden of diabetes and variations among the states of India: the global burden of Disease study 1990-2016. Lancet Glob Health. (2018) 6:e1352–62. doi: 10.1016/S2214-109X(18)30387-5
5. NPCDCS. National PROGRAMME for prevention & control of CANCER, diabetes, cardiovascular diseases & stroke (NPCDCS). (2010). Available online at: https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604 (Accessed July 25, 2024).
6. Century. IoMUCoAtHotPits. Understanding population health and its determinants. Washington, DC: National Academies Press (US) (2002).
7. Babu, BV, Hazarika, CR, Raina, SK, Masoodi, SR, Basappa, YC, Thomas, N, et al. Hypertension prevalence, awareness, treatment, control and risk factors in tribal population of India: a multi-centric cross-sectional study. J Racial Ethn Health Disparities. (2023) 11:3678–89. doi: 10.1007/s40615-023-01817-w
8. Krishnamoorthy, Y, Rajaa, S, Sulgante, S, Chinnakali, P, Jaswal, N, and Goel, S. Prevalence of hypertension and determinants of treatment-seeking behaviour among adolescents and young adults in India: an analysis of NFHS-4. J Public Health (Oxf). (2023) 45:e48–56. doi: 10.1093/pubmed/fdac006
9. Kumar, A, Sahu, SK, Karunanithi, G, and Laksham, KB. Treatment seeking behavior, treatment cost and quality of life of head and neck Cancer patients: a cross-sectional analytical study from South India. Asian Pac J Cancer Prev. (2021) 22:3023–30. doi: 10.31557/APJCP.2021.22.9.3023
10. Sharma, D, Mazta, SR, and Parashar, A. Morbidity pattern and health-seeking behavior of aged population residing in Shimla Hills of North India: a cross-sectional study. J Family Med Prim Care. (2013) 2:188–93. doi: 10.4103/2249-4863.117421
11. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
12. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
13. Downes, MJ, Brennan, ML, Williams, HC, and Dean, RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. (2016) 6:e011458. doi: 10.1136/bmjopen-2016-011458
14. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
15. Egger, M, Davey Smith, G, Schneider, M, and Minder, C. Bias in Meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
17. Verma, A, Mehta, S, Mehta, A, and Patyal, A. Knowledge, attitude and practices toward health behavior and cardiovascular disease risk factors among the patients of metabolic syndrome in a teaching hospital in India. J Family Med Prim Care. (2019) 8:178–83. doi: 10.4103/jfmpc.jfmpc_257_18
18. Nimesh, VV, Halder, A, Mitra, A, Kumar, S, Joshi, A, Joshi, R, et al. Patterns of healthcare seeking behavior among persons with diabetes in Central India: a mixed method study. J Family Med Prim Care. (2019) 8:677–83. doi: 10.4103/jfmpc.jfmpc_433_18
19. Shukla, R, Gudlavalleti, MV, Bandyopadhyay, S, Anchala, R, Gudlavalleti, AS, Jotheeswaran, AT, et al. Perception of care and barriers to treatment in individuals with diabetic retinopathy in India: 11-city 9-state study. Indian J Endocrinol Metab. (2016) 20:S33–41. doi: 10.4103/2230-8210.179772
20. Srinivas, G, Suresh, E, Jagadeesan, M, Amalraj, E, and Datta, M. Treatment-seeking behavior and compliance of diabetic patients in a rural area of South India. Ann N Y Acad Sci. (2002) 958:420–4. doi: 10.1111/j.1749-6632.2002.tb03017.x
21. Basu, S, Malik, M, Anand, T, and Singh, A. Hypertension control Cascade and regional performance in India: a repeated cross-sectional analysis (2015-2021). Cureus. (2023) 15:e35449. doi: 10.7759/cureus.35449
22. Baishya, N, Das, AK, Krishnatreya, M, Das, A, Das, K, Kataki, AC, et al. A pilot study on factors associated with presentation delay in patients affected with head and neck cancers. Asian Pac J Cancer Prev. (2015) 16:4715–8. doi: 10.7314/APJCP.2015.16.11.4715
23. Kaku, M, Mathew, A, and Rajan, B. Impact of socio-economic factors in delayed reporting and late-stage presentation among patients with cervix cancer in a major cancer hospital in South India. Asian Pac J Cancer Prev. (2008) 9:589–94.
24. Kumar, A, Bhagabaty, SM, Tripathy, JP, Selvaraj, K, Purkayastha, J, and Singh, R. Delays in diagnosis and treatment of breast Cancer and the pathways of care: a mixed methods study from a tertiary Cancer Centre in North East India. Asian Pac J Cancer Prev. (2019) 20:3711–21. doi: 10.31557/APJCP.2019.20.12.3711
25. Pakseresht, S, Ingle, GK, Garg, S, and Sarafraz, N. Stage at diagnosis and delay in seeking medical care among women with breast cancer, Delhi, India. Iran Red Crescent Med J. (2014) 16:e14490. doi: 10.5812/ircmj.14490
26. Agrawal, V, Lohiya, BV, Sihag, BK, and Prajapati, R. Clinical profile with angiographic correlation in Naïve acute coronary syndrome. J Clin Diagn Res. (2016) 10:OC10–4. doi: 10.7860/JCDR/2016/21166.8519
27. Krishnan, A, Asadullah, M, Kumar, R, Amarchand, R, Bhatia, R, and Roy, A. Prevalence and determinants of delays in care among premature deaths due to acute cardiac conditions and stroke in residents of a district in India. Lancet Reg Health Southeast Asia. (2023) 15:100222. doi: 10.1016/j.lansea.2023.100222
28. Mohan, B, Bansal, R, Dogra, N, Sharma, S, Chopra, A, Varma, S, et al. Factors influencing prehospital delay in patients presenting with ST-elevation myocardial infarction and the impact of prehospital electrocardiogram. Indian Heart J. (2018) 70:S194–8. doi: 10.1016/j.ihj.2018.10.395
29. Panda, P, Singh, NV, Kaur, N, Kaur, P, Kaur, A, Aujla, HK, et al. Delay in seeking medical treatment among patients with acute coronary syndrome. Cureus. (2021) 13:e17369. doi: 10.7759/cureus.17369
30. Venkatesan, VCK, and Madhavi, SR SK, P K. A study to explore the factors related to treatment seeking delay among adults diagnosed with acute myocardial infarction at KMCH, Coimbatore. Indian Heart J. (2018) 70:793–801. doi: 10.1016/j.ihj.2018.01.007
31. Basu, P, Sarkar, S, Mukherjee, S, Ghoshal, M, Mittal, S, Biswas, S, et al. Women's perceptions and social barriers determine compliance to cervical screening: results from a population based study in India. Cancer Detect Prev. (2006) 30:369–74. doi: 10.1016/j.cdp.2006.07.004
32. Nene, B, Jayant, K, Arrossi, S, Shastri, S, Budukh, A, Hingmire, S, et al. Determinants of womens participation in cervical cancer screening trial, Maharashtra, India. Bull World Health Organ. (2007) 85:264–72. doi: 10.2471/BLT.06.031195
33. Roy, B, and Tang, TS. Cervical cancer screening in Kolkata, India: beliefs and predictors of cervical cancer screening among women attending a women's health clinic in Kolkata, India. J Cancer Educ. (2008) 23:253–9. doi: 10.1080/08858190802189105
34. Sankaranarayanan, R, Rajkumar, R, Arrossi, S, Theresa, R, Esmy, PO, Mahé, C, et al. Determinants of participation of women in a cervical cancer visual screening trial in rural South India. Cancer Detect Prev. (2003) 27:457–65. doi: 10.1016/j.cdp.2003.09.006
35. Gadgil, A, Sauvaget, CA-O, Roy, N, Muwonge, R, Lucas, E, and Sankaranarayanan, R. Setting up a breast cancer awareness project in Mumbai: methodology, experiences and challenges. J Cancer Educ. (2020) 35:579–88. doi: 10.1007/s13187-019-01500-x
36. Khanna, D, Khargekar, N, and Budukh, A. Knowledge, attitude, and practice about cervical cancer and its screening among community healthcare workers of Varanasi district, Uttar Pradesh, India. J Family Med Prim Care. (2019) 8:1715–9. doi: 10.4103/jfmpc.jfmpc_143_19
37. Ramagiri, R, Kannuri, NK, Lewis, MG, Murthy, GVS, and Gilbert, C. Evaluation of whether health education using video technology increases the uptake of screening for diabetic retinopathy among individuals with diabetes in a slum population in Hyderabad (2020) 68:S37–41. doi: 10.4103/ijo.IJO_2028_19
38. Singh, S, Shukla, AK, Sheikh, A, Gupta, G, and More, A. Effect of health education and screening location on compliance with diabetic retinopathy screening in a rural population in Maharashtra. Indian J Ophthalmol. (2020) 68:S47–51. doi: 10.4103/ijo.IJO_1976_19
39. Ahamed, F, Ghosh, T, Kaur, A, and Debnath, A. Prevalence of chronic morbidities and healthcare seeking behavior among urban community dwelling elderly population residing in Kalyani municipality area of West Bengal, India. J Family Med Prim Care. (2021) 10:4193–9. doi: 10.4103/jfmpc.jfmpc_893_21
40. Joshi, K, Kumar, R, and Avasthi, A. Morbidity profile and its relationship with disability and psychological distress among elderly people in northern India. Int J Epidemiol. (2003) 32:978–87. doi: 10.1093/ije/dyg204
41. Kanungo, S, Bhowmik, K, Mahapatra, T, Mahapatra, S, Bhadra, UK, and Sarkar, K. Perceived morbidity, healthcare-seeking behavior and their determinants in a poor-resource setting: observation from India. PLoS One. (2015) 10:e0125865. doi: 10.1371/journal.pone.0125865
42. Mishra, A, Pradhan, SK, Sahoo, BK, Das, A, Singh, AK, and Parida, SP. Assessment of medication adherence and associated factors among patients with diabetes attending a non-communicable Disease Clinic in a Community Health Centre in eastern India. Cureus. (2023) 15:e43779. doi: 10.7759/cureus.43779
43. Nailwal, D, VR, B, and Gupta, A. Patterns and predictors of complementary and alternative medicine use in people presenting with the non-communicable disease in an urban health facility, North India. J Public Health Res. (2021) 10:2109. doi: 10.4081/jphr.2021.2109
44. Anagaw, TF, Melaku Mazengia, E, Bogale, EK, Talie Fenta, E, Eshetu, HB, Kebede, N, et al. Health-seeking behavior among non-communicable disease patients globally, systematic review and meta-analysis. SAGE Open Med. (2023) 11:20503121231215236. doi: 10.1177/20503121231215236
45. John, BMU, Babu, A, Jiji, A, Babu, A, Joshy, A, and Athira, PR. Risk factors and health-seeking behaviours in non-communicable diseases among a community sample of women. Geriatr Educ Med Sci. (2022) 9:47–52. doi: 10.18231/j.agems.2022.011
46. Grewal, H, Sharma, P, Dhillon, G, Munjal, RS, Verma, RK, and Kashyap, R. Universal health care system in India: an in-depth examination of the Ayushman Bharat initiative. Cureus. (2023) 15:e40733. doi: 10.7759/cureus.40733
47. Banerjee, S. Determinants of rural-urban differential in healthcare utilization among the elderly population in India. BMC Public Health. (2021) 21:939. doi: 10.1186/s12889-021-10773-1
48. Ranjan, P, Nandi, D, Kaur, KN, Rajiv, R, Shrivastav, KD, Ghosh, A, et al. An indigenous computational platform for Nowcasting and forecasting non-linear spread of COVID-19 across the Indian sub-continent: a geo-temporal visualization of data. Proc Comput Sci. (2024) 235:496–505. doi: 10.1016/j.procs.2024.04.049
49. Zhao, Y, Fitzpatrick, T, Wan, B, Day, S, Mathews, A, and Tucker, JD. Forming and implementing community advisory boards in low- and middle-income countries: a scoping review. BMC Med Ethics. (2019) 20:73. doi: 10.1186/s12910-019-0409-3
50. Kishore, J, Kohli, C, Gupta, N, Kumar, N, and Sharma, PK. Awareness, practices and treatment seeking behavior of type 2 diabetes mellitus patients in Delhi. Ann Med Health Sci Res. (2015) 5:266–73. doi: 10.4103/2141-9248.160184
51. Mentock, SM, Ng, VY, Narayana, R, Ullal, H, Kumari, S, Badiger, S, et al. Treatment-seeking behavior and obstacles to treatment compliance in diabetic patients in Mangaluru, India. Diab Metab Syndr. (2017) 11:S617–22. doi: 10.1016/j.dsx.2017.04.014
52. Bhojani, U, Beerenahalli, TS, Devadasan, R, Munegowda, CM, Devadasan, N, Criel, B, et al. No longer diseases of the wealthy: prevalence and health-seeking for self-reported chronic conditions among urban poor in southern India. BMC Health Serv Res. (2013) 13:306. doi: 10.1186/1472-6963-13-306
53. Chauhan, S, Gupte, SS, Kumar, S, and Patel, R. Urban-rural differential in diabetes and hypertension among elderly in India: a study of prevalence, factors, and treatment-seeking. Diabetes Metab Syndr. (2021) 15:102201. doi: 10.1016/j.dsx.2021.102201
54. Joshi, A, Mohan, K, Grin, G, and Perin, DM. Burden of healthcare utilization and out-of-pocket costs among individuals with NCDs in an Indian setting. J Community Health. (2013) 38:320–7. doi: 10.1007/s10900-012-9617-1
55. Kusuma, YS, and Babu, BV. The costs of seeking healthcare: illness, treatment seeking and out of pocket expenditures among the urban poor in Delhi, India. Health Soc Care Community. (2019) 27:1401–20. doi: 10.1111/hsc.12792
56. Sarkar, A, Mohapatra, I, Rout, RN, and Thakur, B. Morbidity pattern and healthcare seeking behavior among the elderly in an urban settlement of Bhubaneswar, Odisha. J Family Med Prim Care. (2019) 8:944–9. doi: 10.4103/jfmpc.jfmpc_8_19
57. Singh, T, Bhatnagar, N, Singh, G, Kaur, M, Kaur, S, Thaware, P, et al. Health-care utilization and expenditure patterns in the rural areas of Punjab, India. J Family Med Prim Care. (2018) 7:39–44. doi: 10.4103/jfmpc.jfmpc_291_17
58. Yadav, R, Zaman, K, Mishra, A, Reddy, MM, Shankar, P, Yadav, P, et al. Health seeking behaviour and healthcare utilization in a rural cohort of North India. Healthcare (Basel). (2022) 10:757. doi: 10.3390/healthcare10050757
59. Boro, B, and Banerjee, S. Decomposing the rural-urban gap in the prevalence of undiagnosed, untreated and under-treated hypertension among older adults in India. BMC Public Health. (2022) 22:1310. doi: 10.1186/s12889-022-13664-1
60. Chakraborty, S, Rai, RK, Biswas, AK, Barik, A, Gurung, P, and Praveen, D. Health care seeking behaviour and financial protection of patients with hypertension: a cross-sectional study in rural West Bengal, India. PLoS One. (2022) 17:e0264314. doi: 10.1371/journal.pone.0264314
61. Chinnakali, P, Mohan, B, Upadhyay, RP, Singh, AK, Srivastava, R, and Yadav, K. Hypertension in the elderly: prevalence and health seeking behavior. N Am J Med Sci. (2012) 4:558–62. doi: 10.4103/1947-2714.103314
62. Gupta, S, Virk, A, Mittal, A, and Agarwal, BK. Patterns and determinants of healthcare-seeking behavior among hypertensive patients in a rural population of North India: a mixed-method study. J Family Med Prim Care. (2020) 9:2830–6. doi: 10.4103/jfmpc.jfmpc_200_20
63. Bhatia, M, Kumar, M, Dixit, P, and Dwivedi, LK. Diagnosis and treatment of hypertension among people aged 45 years and over in India: a sub-national analysis of the variation in performance of Indian states. Front Public Health. (2021) 9:766458. doi: 10.3389/fpubh.2021.766458
64. Bharucha, NE, and Kuruvilla, T. Hypertension in the Parsi community of Bombay: a study on prevalence, awareness and compliance to treatment. BMC Public Health. (2003) 3:1. doi: 10.1186/1471-2458-3-1
65. Balsari, S, Vemulapalli, P, Gofine, M, Oswal, K, Merchant, R, Saunik, S, et al. A retrospective analysis of hypertension screening at a mass gathering in India: implications for non-communicable disease control strategies. J Hum Hypertens. (2017) 31:750–3. doi: 10.1038/jhh.2017.54
66. Sudharsanan, N, Ali, MK, and McConnell, M. Hypertension knowledge and treatment initiation, adherence, and discontinuation among adults in Chennai, India: a cross-sectional study. BMJ Open. (2021) 11:e040252. doi: 10.1136/bmjopen-2020-040252
67. Singh, S, Shankar, R, and Singh, GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int J Hypertens. (2017) 2017:1–10. doi: 10.1155/2017/5491838
68. Singh, MM, Basu, S, Lalwani, H, Rao, S, Maheshwari, V, Garg, S, et al. Hypertension care cascade in an urban resettlement colony and slum in Delhi, India: a cross-sectional survey. BMC Public Health. (2023) 23:2116. doi: 10.1186/s12889-023-17021-8
69. Rakesh, PS, Renjini, BA, Mohandas, S, Menon, J, Numpelil, M, Sreedevi, A, et al. Hypertension in urban slums of southern India: burden, awareness, health seeking, control and risk factor profile. Indian Heart J. (2023) 75:258–62. doi: 10.1016/j.ihj.2023.06.004
70. Laxmaiah, A, Meshram, II, Arlappa, N, Balakrishna, N, Rao, KM, Reddy, CG, et al. Socio-economic & demographic determinants of hypertension & knowledge, practices & risk behaviour of tribals in India. Indian J Med Res. (2015) 141:697–708. doi: 10.4103/0971-5916.159592
71. Sreekutty, SJ, Rohini, AM, Thajudheen, RB, and Elavally, S. Determinants of patient delay among women with carcinoma breast. Asian Pac J Cancer Prev. (2023) 24:3109–15. doi: 10.31557/APJCP.2023.24.9.3109
72. Rai, A, Sharda, P, Aggarwal, P, and Ravi, B. Study of diagnostic delay among symptomatic breast Cancer patients in northern India: a mixed-methods analysis from a dedicated breast Cancer Centre. Asian Pac J Cancer Prev. (2022) 23:893–904. doi: 10.31557/APJCP.2022.23.3.893
73. Somanna, SN, Murthy, SN, Chaluvarayaswamy, R, and Malila, N. Time from self-detection of symptoms to seeking definitive care among cervical Cancer patients. Asian Pac J Cancer Prev. (2020) 21:3301–7. doi: 10.31557/APJCP.2020.21.11.3301
74. Somanna, SN, Nandagudi Srinivasa, M, Chaluvarayaswamy, R, and Malila, N. Time interval between self-detection of symptoms to treatment of breast Cancer. Asian Pac J Cancer Prev. (2020) 21:169–74. doi: 10.31557/APJCP.2020.21.1.169
75. Zaman, SA-O, Evans, RA-O, Chow, CK, Joshi, R, Thankappan, KR, Oldenburg, B, et al. Morbidity and utilisation of healthcare services among people with cardiometabolic disease in three diverse regions of rural India. Chronic Illn. (2023) 19:873–88. doi: 10.1177/17423953231153550
76. Arjun, P, Nair, S, Jilisha, G, Anand, J, Babu, V, Moosan, H, et al. Assessing health-seeking behavior among asthma and COPD patients in urban South India. J Family Med Prim Care. (2019) 8:2714–9. doi: 10.4103/jfmpc.jfmpc_485_19
77. Gangane, N, Anshu, MS, Ng, N, Hurtig, AK, and San, SM. Prevalence and risk factors for patient delay among women with breast Cancer in rural India. Asia Pac J Public Health. (2016) 28:72–82. doi: 10.1177/1010539515620630
78. Barbhuiya, F. Treatment trajectory of tobacco-related cancer patients: a study in Assam, India. Cancer Epidemiol. (2019) 63:101614. doi: 10.1016/j.canep.2019.101614
79. Kishore, J, Ahmad, I, Kaur, R, and Mohanta, PK. Beliefs and perceptions about cancers among patients attending radiotherapy OPD in Delhi, India. Asian Pac J Cancer Prev. (2008) 9:155–8.
80. Sarkar, M, Konar, H, and Raut, DK. Knowledge and health care-seeking behavior in relation to gynecological malignancies in India: a study of the patients with gynecological malignancies in a tertiary care hospital of Kolkata. J Cancer Educ. (2011) 26:348–54. doi: 10.1007/s13187-010-0168-9
81. Vallabhajosyula, S, Baijal, G, Vadhiraja, BM, Fernandes, DJ, and Vidyasagar, MS. Non-Hodgkin's lymphoma: is India ready to incorporate recent advances in day to day practice? J Cancer Res Ther. (2010) 6:36–40. doi: 10.4103/0973-1482.63571
Keywords: health-seeking behavior, healthcare access, non-communicable diseases, NPCDCS, India, systematic review, meta-analysis
Citation: Haridoss M, Nandi D, Rajesh Lenin R, John SP, Anantharaman VV and Janardhanan R (2025) Health-seeking behavior and its determinants for non-communicable diseases in India - a systematic review and meta-analysis. Front. Public Health. 13:1580824. doi: 10.3389/fpubh.2025.1580824
Edited by:
Maryam Khazaee-Pool, Mazandaran University of Medical Sciences, IranReviewed by:
Samson Malwa Haumba, Georgetown University Medical Center, United StatesAbhishek Tiwari, Motilal Nehru Medical College, India
Copyright © 2025 Haridoss, Nandi, Rajesh Lenin, John, Anantharaman and Janardhanan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madhumitha Haridoss, bWFkaHVtaWhAc3JtaXN0LmVkdS5pbg==; Rajiv Janardhanan, cmFqaXZqQHNybWlzdC5lZHUuaW4=
 Madhumitha Haridoss
Madhumitha Haridoss Dhruva Nandi
Dhruva Nandi Raji Rajesh Lenin
Raji Rajesh Lenin Shiny P. John1
Shiny P. John1 Rajiv Janardhanan
Rajiv Janardhanan