- Department of Psychiatry, Minhang District Mental Health Center, Shanghai, China
Objective: This study aimed to investigate the factors influencing depression and anxiety in individuals with schizophrenia during the COVID-19 pandemic, with the goal of providing evidence to support strategies for improving emotional disturbances during the pandemic.
Methods: A cross-sectional study was conducted among 159 outpatients with schizophrenia between January and June 2023. Data were collected using a self-developed sociodemographic questionnaire, the Chinese version of the Illness Perception Questionnaire-Revised (IPQ-R), the Patient Health Questionnaire-9 (PHQ-9), and the 7-item Generalized Anxiety Disorder scale (GAD-7). Regression analysis was performed using SPSS version 27.0 to identify the factors associated with depression and anxiety.
Results: Timeline cyclical and treatment control were significant predictors of depression among individuals with schizophrenia (R2 = 0.160, p < 0.01). Additionally, timeline cyclical and the presence of chronic comorbidities significantly predicted anxiety (R2 = 0.217, p < 0.01).
Conclusion: Illness perception concerning COVID-19 significantly influenced the severity of depression and anxiety in individuals with schizophrenia. Addressing these perceptions serves as an essential component of interventions aimed at improving mental health outcomes during the pandemic.
1 Introduction
In January 2020, the outbreak of coronavirus disease 2019 (COVID-19) rapidly evolved into a global pandemic. During the COVID-19 pandemic, a significant increase on COVID-anxiety syndrome (1, 2), loneliness (3), distress (4), and a significant decrease on well-being (5) has been observed. This includes the issue of a significant increase in the prevalence of depression and anxiety among individuals with schizophrenia. A large-scale survey conducted in China reported that all community-dwelling individuals with schizophrenia experienced varying degrees of depression and anxiety during the pandemic (6). Among these individuals, 34.9% exhibited moderate to severe depression, while 16.9% experienced moderate to severe anxiety. Another study found that the prevalence of depression rose by 42.9%, and the prevalence of anxiety increased by 10.2% during the pandemic (7).
Illness perception refers to the process by which both patients and those without medical conditions, interpret and analyze symptoms or diseases based on their prior knowledge and experiences (8). This concept is rooted in the Self-Regulation Model (SRM), which posits that patients adopt coping strategies and assess their effectiveness based on their cognitive and emotional representations of the disease (9). Information derived from these assessments is subsequently used to modify future coping behaviors (10). In 1996, Weinman et al. developed the Illness Perception Questionnaire (IPQ) based on the foundational structure of the SRM (11). This questionnaire was later revised by Moss-Morris et al. to create the Illness Perception Questionnaire-Revised (IPQ-R), which demonstrated improved reliability and validity (12–15).
Additionally, Chinese researchers validated the reliability and validity of the Chinese version of the IPQ-R in studies involving patients with stroke, breast cancer, and obstructive sleep apnea syndrome (OSAS) (16–18).
Patients exhibiting depression-associated characteristics—such as reduced energy levels, impaired attention, and heightened feelings of despair—are less likely to adhere to recommended preventive measures during the COVID-19 pandemic (19). This nonadherence exacerbates their condition, potentially leading to a vicious cycle of worsening mental health. Several studies demonstrated a significant association between illness perception and severity of depression and anxiety (20–22). Based on the hypotheses derived from the Self-Regulation Model, a mediational model has been proposed in which coping mediates the effect of illness perception on health outcomes, including psychological distress (23). Moreover, many studies have verified this mediation process (20, 22, 24), among which a study even applied meta-analytic path analyses to corroborate this model (24), so it is concluded that illness perception and symptoms of depression and anxiety are associated through the mediation of coping. However, there is a lack of research examining the relationship between illness perception of COVID-19 and the presence of depressive and anxiety symptoms in individuals with schizophrenia.
The present study aims to examine this relationship, with the goal of identifying strategies to improve negative emotional responses and providing guidance on improving the psychological well-being of individuals with schizophrenia during the pandemic.
2 Participants and methods
2.1 Participants
Individuals with schizophrenia who sought care at the Minhang Mental Health Center in Shanghai between January and June 2023 were recruited using convenience sampling. The inclusion criteria were as follows: (1) a diagnosis of schizophrenia based on the criteria outlined in the tenth edition of the International Classification of Diseases (ICD-10), (2) an age range between 18 and 65 years, (3) completion of at least a primary level of education, and (4) a Positive and Negative Syndrome Scale (PANSS) score of ≤ 5 points for delusion, hallucinatory behaviors, exaggeration, suspiciousness/paranoia, and unusual thought content, with a PANSS score of ≤ 4 points for conceptual disorganization.
Exclusion criteria were: (1) a history of substance abuse or other mental disorders within the past 6 months, (2) a diagnosis of serious physical illnesses such as chronic obstructive pulmonary disease (COPD) or coronary heart disease (CHD), and (3) communication or reading disorders.
Informed consent was obtained from all participants. Based on these criteria, a total of 159 participants were enrolled in the study.
2.2 Evaluation tools
A cross-sectional survey method was used in this study, by having multiple questionnaires, including a self-developed sociodemographic questionnaire, the Chinese version of the IPQ-R, the Patient Health Questionnaire-9 (PHQ-9), and the 7-item Generalized Anxiety Disorder scale (GAD-7).
The Chinese version of the IPQ-R was used to assess the illness perception of COVID-19 by the participants. The IPQ-R consists of three sections. For this study, only the illness representation (IR) dimension, which includes 38 items from the second section, was selected to evaluate cognitive and emotional representations of COVID-19. This dimension is divided into seven subscales, and the definition of each is as follows. Timeline refers to the patient’s perceptions of the likely duration of illness, categorized as acute/chronic, and the predictability and variability of illness, categorized as cyclical; consequences are the patient’s beliefs regarding the illness severity and the likely influence on individual social and psychological functioning; personal control reflects the patient’s belief about the ability of taking measures to personally control the illness and self-efficacy; treatment control is the patient’s belief about the degree to which his or her condition is amenable to cure; illness coherence refers to the extent of patients’ understanding of their illness; and emotional representations are the patient’s general mood in response to the illness. Each item is rated on a five-point Likert-type scale (1 = strongly disagree, 5 = strongly agree). The item responses are summed to obtain the IPQ-R subscale scores.
The questionnaire used in this study was adapted to align culturally with the Chinese context and demonstrated higher reliability and validity than the original version when applied to outpatient populations in general hospitals (25). In this study, the Cronbach’s α coefficient for the IR dimension was 0.8, while the coefficients for the seven subscales ranged from 0.61 to 0.87.
In this study, the PHQ-9 and GAD-7 were used to assess depression and anxiety, respectively. The PHQ-9 is a self-assessment tool comprising of nine items designed to evaluate depressive symptoms over the preceding 2 weeks. Each item is scored on a scale from 0 to 3, with higher scores indicating greater severity of depression.
The GAD-7 is a self-administered scale consisting of seven items, intended to screen for and assess the severity of anxiety symptoms in the past 2 weeks. Similar to the PHQ-9, each item on the GAD-7 is scored from 0 to 3, with higher scores reflecting more severe anxiety symptoms.
In this study, the PHQ-9 demonstrated a Cronbach’s α coefficient of 0.880, while the GAD-7 exhibited 0.922.
2.3 Research process
The study was carried out in the Outpatient Department of Minhang Mental Health Center in Shanghai. One-on-one interviews were conducted with all participants. Initially, psychiatric symptoms were assessed using the PANSS. Participants who met the inclusion criteria were then instructed to independently complete the remaining questionnaires. During this process, explanations were provided by the research team only when participants sought clarification regarding specific items.
Informed consent was obtained from all participants prior to their inclusion in the study. The research protocol was reviewed and approved by the hospital’s Ethics Committee (Approval No.: LW202205).
2.4 Statistical analysis
Data analysis was conducted using SPSS for Windows, version 27.0 (SPSS 27.0). The internal consistency reliability of the Chinese versions of the IPQ-R, PHQ-9, and GAD-7 were assessed.
The normality of all data was evaluated using the Shapiro–Wilk test. Data following a normal distribution were expressed as mean ± standard deviation (−x ± s), analyzed using Pearson correlation, and compared between groups using the t-test or among groups using one-way analysis of variance (ANOVA). Data not following a normal distribution were expressed as the median (interquartile range), analyzed using Spearman correlation, and compared between groups using the Mann–Whitney U test or among groups using the Kruskal-Wallis H test.
Multiple linear regression analysis was used to examine predictive relationships between variables. A significance level of p < 0.05 was considered statistically significant.
3 Results
3.1 Description of the sample
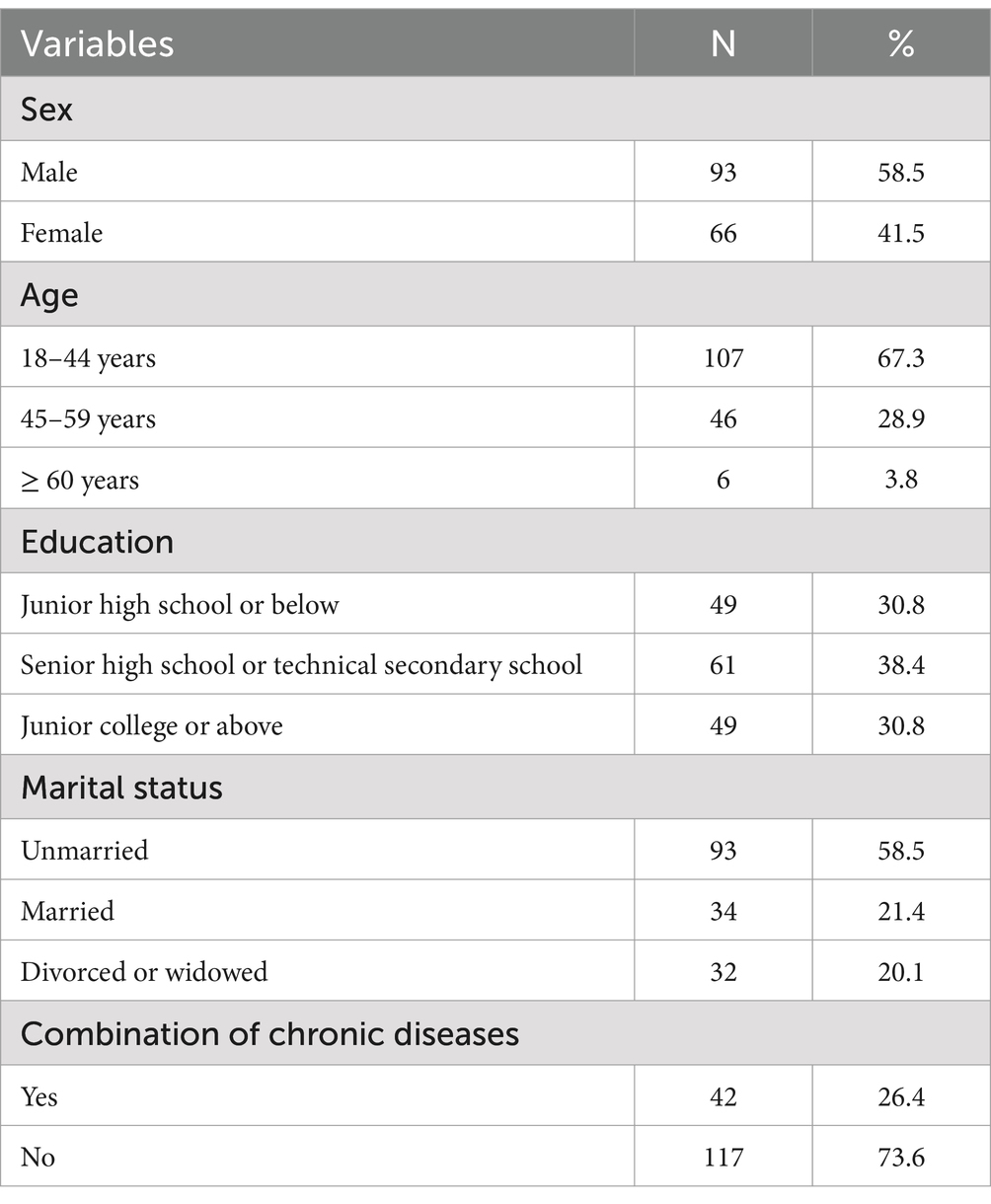
Among the 159 participants included in the final sample, 58.5% were male, 67.3% were classified as young adults, 69.2% had an educational qualification of senior high school or higher, and 58.5% were unmarried. Only a small proportion of participants reported having chronic diseases. No significant differences were observed in demographic variables—such as age, education, occupation, and marital status—between those included in the sample and individuals who were excluded. Detailed demographic data are presented in Table 1.
3.2 Illness perception of COVID-19
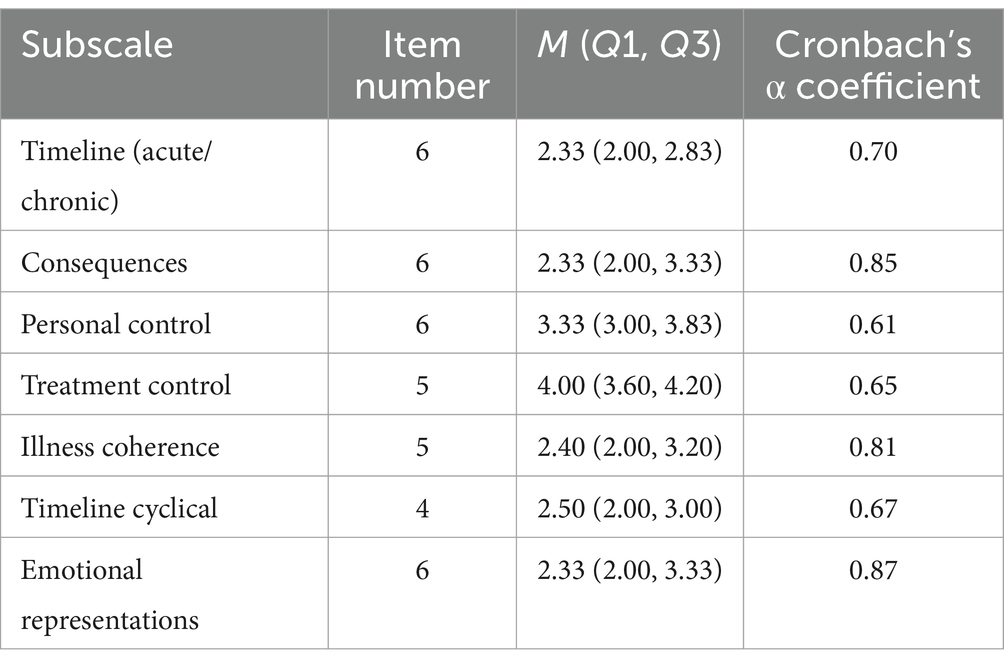
The quartile and Cronbach’s α coefficients for each subscale in the IR dimension are presented in Table 2. The results indicated that participants generally perceived the course of COVID-19 to be short and not likely to result in severe negative consequences. Most participants believed that personal efforts and medical treatment could improve their condition to some extent. Additionally, they reported a good level of understanding of the illness. Although many participants acknowledged the possibility of recurrence, they did not exhibit significant negative emotional responses when confronted with COVID-19. The Cronbach’s α coefficients for all subscales were within the ideal range.
3.3 Correlation analysis between depression, anxiety and illness perception
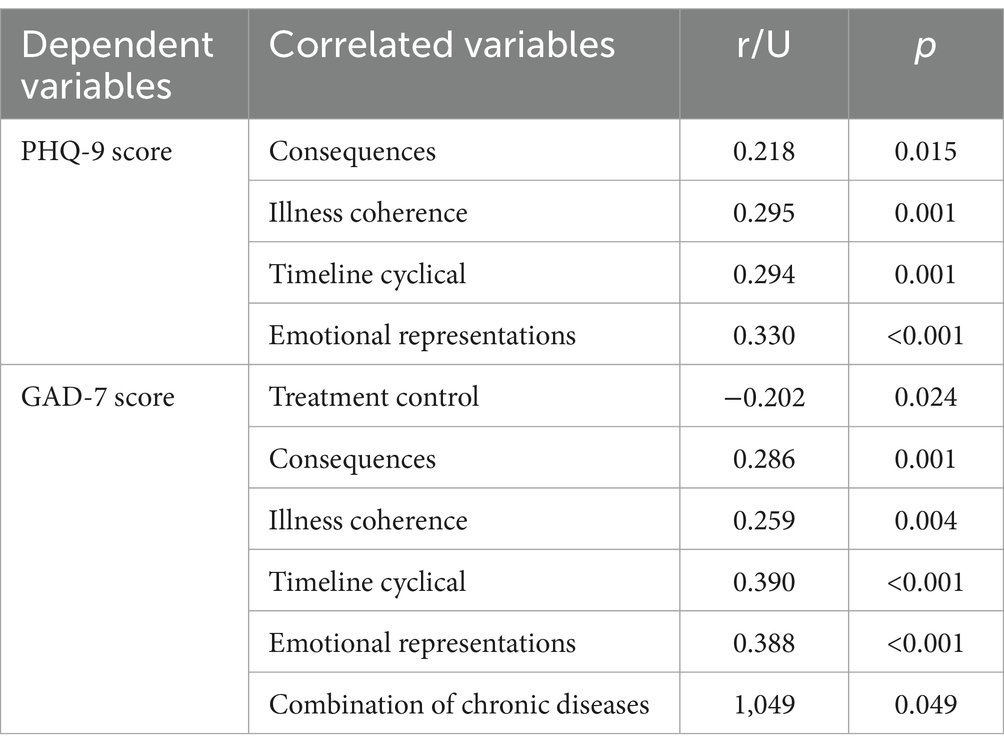
The PHQ-9 score demonstrated a positive correlation with several domains of the IPQ-R, including consequences, illness coherence, timeline cyclical, and emotional representations (p < 0.05). Conversely, a negative correlation was observed between the PHQ-9 score and treatment control (p < 0.05). The GAD-7 score was positively correlated with the same IPQ-R domains—consequences, illness coherence, timeline cyclical, and emotional representations (p < 0.05).
Additionally, a significant correlation was found between the combination of chronic diseases and the GAD-7 score (p < 0.05), indicating that individuals with chronic diseases were more susceptible to anxiety. Further details are provided in Table 3.
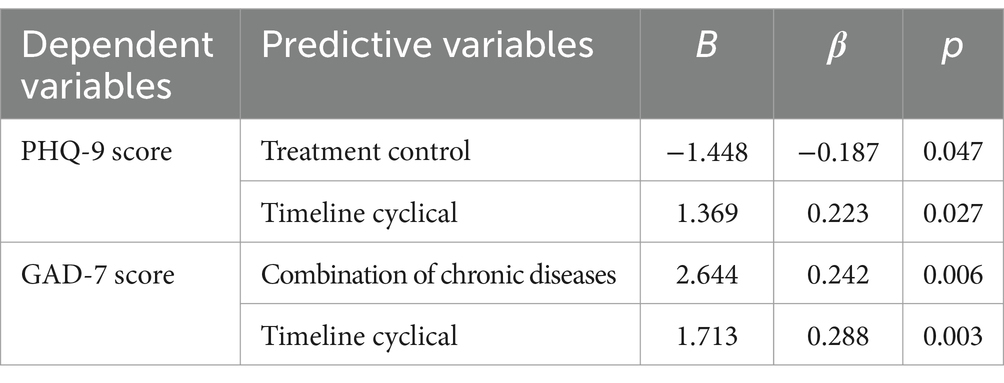
3.4 Linear regression analysis of depression and anxiety
Linear regression analysis was conducted using the PHQ-9 and GAD-7 scores as dependent variables. Independent variables that revealed significant correlations with depression and anxiety in the univariate analysis were included in the model. The results indicated that the illness perception domains of timeline cyclical and treatment control were significant predictors of depression in individuals with schizophrenia during the COVID-19 pandemic (R2 = 0.160, p < 0.01). Specifically, timeline cyclical was identified as a risk factor for depression (p < 0.05), while treatment control served as a protective factor (p < 0.05).
For anxiety, timeline cyclical and the combination of chronic diseases were significant predictors (R2 = 0.217, p < 0.01). Both predictors were identified as risk factors for anxiety (p < 0.01). Further details are provided in Table 4.
4 Discussion
COVID-19 continues to circulate globally, exhibiting recurrent fluctuations approximately every 6 months. In China, it has transitioned into a periodically prevalent respiratory disease, with a proportion of cases developing severe symptoms. Individuals with mental health conditions, including those with schizophrenia, have been shown to have an elevated mortality risk from infectious diseases (26). Adherence to recommended preventive measures is often challenging for individuals with schizophrenia due to the influence of psychiatric symptoms.
Depression and anxiety are key factors influencing the likelihood of an individual adhering to COVID-19 preventive measures (19, 27). Therefore, understanding the factors contributing to depression and anxiety in individuals with schizophrenia during the pandemic is crucial for improving adherence to preventive measures during outbreaks of infectious diseases.
The study findings indicate that participants were less likely to develop depression if they believed that current treatments could effectively control COVID-19 infection. However, those who perceived COVID-19 as a recurring condition demonstrated a higher risk of developing depression and anxiety. These results align with the theoretical framework of the Self-Regulation Model (SRM), which emphasizes the key role of cognitive and emotional representations in the self-regulation of health problems. This model posits that these representations influence both mental health and overall quality of life.
The negative correlation between treatment control and depression has been supported by several studies (28–31). One study on the general population’s perception of COVID-19, which utilized the same assessment tool as in this study, further reinforced this relationship (29). The study found that greater confidence in the efficacy of current treatments served as a protective factor against depression, as indicated by the negative correlation between treatment control and depressive symptoms. Enhancing public awareness of the effectiveness of available treatments during the pandemic may strengthen the confidence of individuals and improve mental health outcomes based on these findings.
Although few studies have examined the relationship between the timeline cyclical dimension of illness perception and depression or anxiety, the available evidence supports the results of this study. For instance, a validation study of the IPQ-R among Chinese patients with nasopharyngeal cancer demonstrated a significant positive correlation between the perception of cyclical symptoms and anxiety (31). Similarly, research on the relationship between illness perception, depression, and physical activity levels found that timeline cyclical was a predictive risk factor of depression (21). Another study involving patients with chronic rheumatic diseases, though not focused on the direct relationship between illness perception and depression or anxiety, revealed that timeline cyclical significantly contributed to negative emotional states (22). Furthermore, this study highlighted a statistically significant mediating effect of rumination on the relationship between timeline cyclical and negative emotions.
Given that rumination can be seen in some patients with schizophrenia, it is hypothesized that the schizophrenia patients who believe COVID-19 is likely to recur may engage in repeated, passive contemplation of the pain associated with the disease. This may increase their susceptibility to depression and anxiety.
Patients with schizophrenia are a mentally vulnerable population during the COVID-19 pandemic. They showed higher levels of loneliness and depression compared with the general population (32), and depression is in turn a strong predictor of poorer outcomes in schizophrenia (33). According to this study, illness perception concerning COVID-19 significantly influences the severity of depression and anxiety in individuals with schizophrenia. Additionally, illness perception is largely a subjective experience and is amenable to modification (34). So our study suggest that clinicians could contribute to alleviating depression and thereby improve their outcomes during a pandemic by routinely assessing and challenging nonadaptive illness perceptions.
This study has several limitations. First, as a preliminary exploratory survey, it did not establish causal relationships between variables. It is possible that depression and anxiety may influence illness perception rather than the other way around. Second, although the included participants were in a stable condition, their cognitive functioning and perceptions may still have been affected by their illness. Additionally, the limited sample size of the study and the constraints of the study site and time frame may have introduced biases into the findings.
To improve the understanding of this topic, future research should adopt a longitudinal design involving larger, multi-center sample groups. Including a control group without schizophrenia would also provide for more comprehensive insights into the relationship between illness perception and depression/anxiety.
5 Conclusion
In conclusion, the perception of illness related to COVID-19 serves as a significant predictor of the emotional state of individuals with schizophrenia. Integrating interventions aimed at addressing and correcting negative illness perceptions into routine health education for this population may help modify maladaptive beliefs, thereby alleviating symptoms of depression and anxiety. This approach enhances adherence to recommended preventive measures during the pandemic, ultimately supporting better mental and physical health outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of Minhang District Mental Health Center (Approval No.: LW202205). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MZ: Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. Y-FD: Conceptualization, Data curation, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. (1) Minhang District Health Commission Research project, with funding number: 2022 MW25 and (2) Minhang District Medical System University Science Construction Project (2025–2027), with funding number: 2025MWFC08.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
IPQ, Illness Perception Questionnaire; IPQ-R, Illness Perception Questionnaire-Revised; PHQ-9, Patient Health Questionnaire-9; GAD-7, 7-item Generalized Anxiety Disorder; COVID-19, Coronavirus Disease 2019; SRM, Self-Regulation Model; ICD-10, the tenth edition of the international classification of diseases; PANSS, Positive and Negative Syndrome Scale; IR, illness representations; SPSS 27.0, SPSS for windows version 27.0.
References
1. Mansueto, G, Palmieri, S, Marino, C, Caselli, G, Sassaroli, S, Ruggiero, GM, et al. The Italian COVID-19 anxiety syndrome scale: investigation of the COVID-19 anxiety syndrome and its association with psychological symptoms in an Italian population. Clin Psychol Psychother. (2022) 29:1972–90. doi: 10.1002/cpp.2767
2. Alhakami, A, Salem, V, Alateeq, D, Nikčević, AV, Marci, T, Palmieri, S, et al. The Arab COVID-19 anxiety syndrome scale (C-19ASS): COVID-19 anxiety syndrome and psychological symptoms in the Saudi Arabian population. Clin Psychol Psychother. (2023) 30:1083–94. doi: 10.1002/cpp.2860
3. Mansueto, G, Lopes, FL, Grassi, L, and Cosci, F. Impact of COVID-19 outbreak on Italian healthcare workers versus general population: results from an online survey. Clin Psychol Psychother. (2021) 28:1334–45. doi: 10.1002/cpp.2644
4. Brailovskaia, J, Cosci, F, Mansueto, G, Miragall, M, Herrero, R, Baños, RM, et al. The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: an investigation in Germany, Italy, Russia, and Spain. Psychiatry Res. (2021) 295:113596. doi: 10.1016/j.psychres.2020.113596
5. Fisicaro, F, Lanza, G, Concerto, C, Rodolico, A, di Napoli, M, Mansueto, G, et al. COVID-19 and mental health: a "pandemic within a pandemic". Adv Exp Med Biol. (2024) 1458:1–18. doi: 10.1007/978-3-031-61943-4_1
6. Chen, S, Sun, X, Zhu, Q, Zhao, Y, Tang, J, and Song, H. Factors influencing the level of depression and anxiety of community-dwelling patients with schizophrenia in China during the COVID-19 pandemic. Int J Environ Res Public Health. (2023) 20:4376. doi: 10.3390/ijerph20054376
7. Cheng, X, Huang, X, Wu, X, and Lin, S. Impact of the COVID-19 pandemic on lifestyle and mental state in patients with schizophrenia: a retrospective study. Medicine. (2023) 102:e32830. doi: 10.1097/MD.0000000000032830
8. Weinman, J, and Petrie, KJ. Illness perceptions: a new paradigm for psychosomatics? J Psychosom Res. (1997) 42:113–6. doi: 10.1016/S0022-3999(96)00294-2
9. Leventhal, H, Phillips, LA, and Burns, E. The common-sense model of self-regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. (2016) 39:935–46. doi: 10.1007/s10865-016-9782-2
10. Leventhal, H., Nerenz, D.R., and Purse, J., Illness Representations and Coping With Health Threats. (1984):219–252.
11. Weinman, J, Petrie, KJ, Moss-morris, R, and Horne, R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. (1996) 11:431–45.
12. Brzoska, P, Yilmaz-Aslan, Y, Sultanoglu, E, Sultanoglu, B, and Razum, O. The factor structure of the Turkish version of the revised illness perception questionnaire (IPQ-R) in patients with diabetes and cardiovascular disease. BMC Public Health. (2012) 12:852. doi: 10.1186/1471-2458-12-852
13. Ashley, L, Smith, AB, Keding, A, Jones, H, Velikova, G, and Wright, P. Psychometric evaluation of the revised illness perception questionnaire (IPQ-R) in cancer patients: confirmatory factor analysis and Rasch analysis. J Psychosom Res. (2013) 75:556–62. doi: 10.1016/j.jpsychores.2013.08.005
14. Kim, Y, Evangelista, LS, Phillips, LR, Pavlish, C, and Kopple, JD. Racial/ethnic differences in illness, perceptions in minority patients undergoing maintenance hemodialysis. Nephrol Nurs J. (2012) 39:39–48. doi: 10.1016/j.colegn.2011.12.003
15. Moss-Morris, R, Weinman, J, Petrie, K, Horne, R, Cameron, L, and Buick, D. The revised illness perception questionnaire (IPQ-R). Psychol Health. (2002) 17:1–16. doi: 10.1080/08870440290001494
16. Huang, W, Zhang, L, and Yan, J. Psychometric evaluation of the Chinese version of the revised illness perception questionnaire for breast cancer-related lymphedema. Eur J Cancer Care (Engl). (2019) 28:e12900. doi: 10.1111/ecc.12900
17. Liu, Y, Wei, M, Guo, L, Guo, Y, Zhu, Y, and He, Y. Association between illness perception and health behaviour among stroke patients: the mediation effect of coping style. J Adv Nurs. (2021) 77:2307–18. doi: 10.1111/jan.14761
18. Yu, Y, Wu, AMS, Wing, YK, Chan, JWY, Lau, MMC, and Lau, JTF. Validation of the revised illness perception questionnaire of obstructive sleep apnea among elderly Chinese in the general population. Sleep Breath. (2023) 27:337–44. doi: 10.1007/s11325-022-02598-y
19. Yuan, J, Cao, B, Zhang, C, Chan, PSF, Xin, M, Fang, Y, et al. Changes in compliance with personal preventive measures and mental health status among Chinese factory workers during the COVID-19 pandemic: an observational prospective cohort study. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.831456
20. Marcil, MJ, Houchi, C, Nadarajah, K, Khairy, P, Mageau, GA, Marin, MF, et al. The influence of illness perception and coping on anxiety in adults with congenital heart disease. JACC Adv. (2023) 2:100425. doi: 10.1016/j.jacadv.2023.100425
21. Nah, R, Robertson, N, Niyi-Odumosu, FA, Clarke, AL, Bishop, NC, and Smith, AC. Relationships between illness representations, physical activity and depression in chronic kidney disease. J Ren Care. (2019) 45:74–82. doi: 10.1111/jorc.12274
22. Lu, Y, Jin, X, Feng, LW, Tang, CSK, Neo, M, and Ho, RC. Effects of illness perception on negative emotions and fatigue in chronic rheumatic diseases: rumination as a possible mediator. World J Clin Cases. (2022) 10:12515–31. doi: 10.12998/wjcc.v10.i34.12515
23. Hagger, MS, and Orbell, S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. (2003) 18:141–84. doi: 10.1080/088704403100081321
24. Hagger, MS, Koch, S, Chatzisarantis, NLD, and Orbell, S. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol Bull. (2017) 143:1117–54. doi: 10.1037/bul0000118
25. Xong, NN. Cross-culture adaptation,validity and reliability of the Chinese version of the illness perception questionnaire-revised(IPQ-R) among outpatients. Chin Ment Health J. (2018) 32:713–9. doi: 10.3969/j.issn.1000-6729.2018.09.001
26. Maguire, PA, Reay, RE, and Looi, JCL. Nothing to sneeze at - uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australas Psychiatry. (2019) 27:171–8. doi: 10.1177/1039856218815748
27. van den Broek-Altenburg, E, and Atherly, A. Adherence to COVID-19 policy measures: behavioral insights from the Netherlands and Belgium. PLoS One. (2021) 16:e0250302. doi: 10.1371/journal.pone.0250302
28. Feng, C, Yu, B, Fu, Y, Reinhardt, JD, and Yang, S. Relationships of illness perceptions with depression and anxiety in people who live with HIV/AIDS in a high-prevalence ethnic autonomous region of Sichuan. China Aids Behav. (2022) 26:3783–93. doi: 10.1007/s10461-022-03707-4
29. Skapinakis, P, Bellos, S, Oikonomou, A, Dimitriadis, G, Gkikas, P, Perdikari, E, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress Res Treat. (2020) 2020:1–11. doi: 10.1155/2020/3158954
30. Maltinsky, W, Henton, S, Spaltro, G, Fowler, S, Chaudhuri, R, Higgs, C, et al. Illness perceptions, symptom severity and psychosocial outcomes in adults with dysfunctional breathing. J Asthma. (2024) 62:226–35. doi: 10.1080/02770903.2024.2397656
31. Cai, Y, Zhang, Y, Cao, W, Guo, VY, Deng, Y, Luo, L, et al. Preliminary validation of the revised illness perception questionnaire for patients with nasopharyngeal carcinoma in China. Health. (2023) 11:2469. doi: 10.3390/healthcare11182469
32. Lee, YR, Chung, YC, Kim, JJ, Kang, SH, Lee, BJ, Lee, SH, et al. Effects of COVID-19-related stress and fear on depression in schizophrenia patients and the general population. Schizophrenia (Heidelb). (2022) 8:15. doi: 10.1038/s41537-022-00213-3
33. Upthegrove, R, Marwaha, S, and Birchwood, M. Depression and schizophrenia: cause, consequence, or trans-diagnostic issue? Schizophr Bull. (2017) 43:240–4. doi: 10.1093/schbul/sbw097
Keywords: illness perception, depression, anxiety, COVID-19, schizophrenia
Citation: Zhang M and Deng Y-F (2025) Influence of illness perception on depression and anxiety in individuals with schizophrenia during the COVID-19 pandemic. Front. Public Health. 13:1583630. doi: 10.3389/fpubh.2025.1583630
Edited by:
Giovanni Mansueto, University of Florence, ItalyReviewed by:
Humbelina Robles Ortega, University of Granada, SpainSara Palmieri, Università di Sigmund Freud Milano, Italy
Lucia Salatini, Sigmund Freud University Vienna, Austria
Copyright © 2025 Zhang and Deng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan-Feng Deng, ZGVueWFuZmVuZ2dyZXRAMTYzLmNvbQ==
 Meng Zhang
Meng Zhang Yan-Feng Deng
Yan-Feng Deng