- 1Department of Cardiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Nursing, Shandong First Medical University, Taian, China
- 3School of Nursing, Health Science Center, Xian Jiaotong University, Xi'an, China
Objective: This study aimed to comprehensively evaluate the eHealth literacy of patients with cardiovascular diseases and uncover the associated influencing factors. The findings are intended to lay a solid foundation for formulating targeted strategies to enhance the health literacy of this patient population.
Methods: Between October 2023 and June 2024, a purposive sampling approach was employed to recruit patients with cardiovascular diseases visiting the cardiology department of a tertiary hospital in Shandong Province. The eHealth Literacy Scale (eHEALS) was utilized to assess the eHealth literacy levels of the participants. Based on the assessment results, the subjects were classified into qualified and unqualified groups. Subsequently, logistic regression analysis was conducted to identify the influencing factors underlying eHealth literacy.
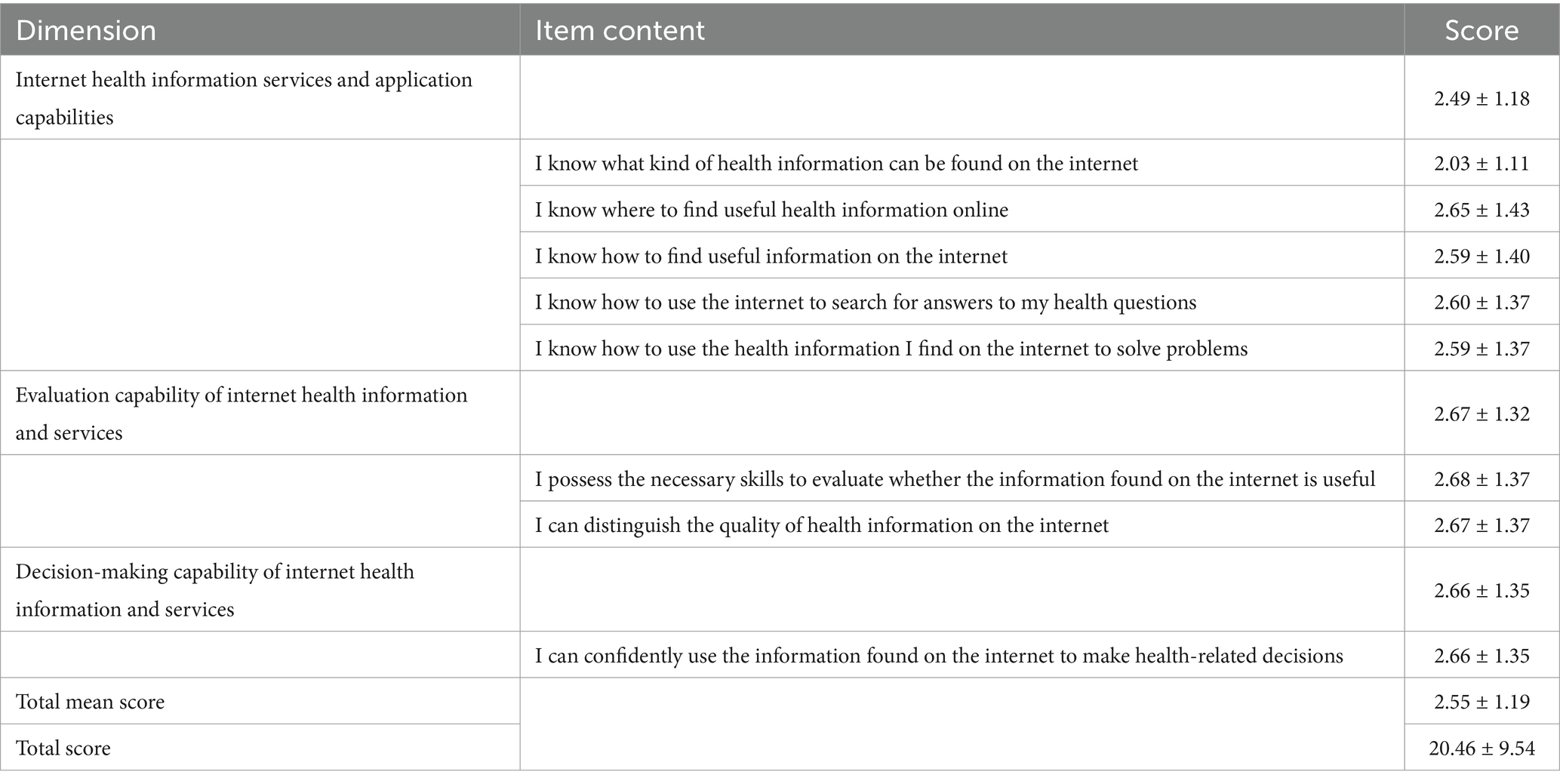
Results: The eHealth literacy score among cardiovascular disease patients was 20.46 ± 9.54, with a passing rate of 38.6%. The overall mean score across all items was 2.5 ± 1.19. Specifically, for the sub-domains of internet health information service capabilities and application abilities, evaluation capabilities of internet health information and services, and decision - making capabilities of internet health information and services, the mean scores were 2.49 ± 1.18, 2.67 ± 1.32, and 2.66 ± 1.35, respectively. Findings from binary logistic regression analysis suggest that education level, sleep quality, residing in close proximity to a medical institution (distance < 5 km), prior utilization of medical information websites or search engines, as well as the interaction between proactive health awareness and utilization of medical information websites or search engines, were all influencing factors for the qualification of e - health literacy (p < 0.05). These results underscore the complex interplay of multiple factors in determining patients’ eHealth literacy levels, which has important implications for the design and implementation of effective health information dissemination and patient education strategies in the digital age.
Conclusion: Our findings reveal that the eHealth literacy among cardiovascular disease (CVD) patients remains at a relatively low level. This situation underscores the urgent need for interventions aimed at enhancing patients’ proactive health awareness and delivering targeted eHealth training programs. Specifically, such initiatives should be designed to enable patients to accurately access, comprehensively understand, critically evaluate, and effectively apply health information in the digital realm. By doing so, we can empower CVD patients to better manage their health in the context of the digital age, ultimately leading to an improvement in their eHealth literacy levels. These efforts are not only crucial for individual patient care but also have broader implications for optimizing health outcomes at a population level.
1 Introduction
Chronic non-communicable diseases (NCDs), encompassing cardiovascular and cerebrovascular diseases, respiratory diseases, diabetes, malignant tumors, and mental health disorders, are a global health challenge of increasing significance (1). As per the “World Health Statistics 2021” report, chronic diseases account for 71.93% of all deaths, topping the list of mortality causes (2).
In China, among the older adult population aged 70 and above, cardiovascular and cerebrovascular diseases stand out as the leading contributor to disability-adjusted life years (39.11%), as indicated by relevant prevalence statistics (3). Cardiovascular diseases are characterized by an insidious onset, a protracted course, and a high recurrence rate, resulting in substantial disability and mortality. This not only places a heavy psychological burden on patients but also exacts a significant economic toll.
Given these circumstances, it is of utmost importance to implement appropriate strategies. These strategies should aim to assist chronic disease patients in accessing disease related information, effectively managing their conditions, and making well - informed health decisions. By doing so, we can potentially decelerate the progression of chronic diseases, thus improving patients’ quality of life and alleviating the burden on healthcare systems.
In the era of seamless integration between the internet and the healthcare domain, intelligent and digital technologies have emerged as pivotal pillars in chronic disease prevention (4). A plethora of information platforms now offer eHealth resources tailored for patients grappling with chronic cardiovascular diseases. The capacity of patients to actively seek, critically evaluate, comprehensively understand, and effectively apply these resources is encapsulated within the concept of eHealth literacy (5).
Accumulating evidence has firmly established a positive association between eHealth literacy and health - promoting behaviors (6–8). Given this connection, accurately gauging patients’ eHealth literacy levels and ensuring the targeted dissemination of eHealth resources assume paramount importance.
In recent years, research endeavors into eHealth literacy in the context of chronic diseases have witnessed a steady upsurge, covering a wide spectrum of themes (9). Nevertheless, the body of literature specifically dedicated to exploring eHealth literacy in cardiovascular diseases and other distinct chronic conditions remains relatively scarce.
Against this backdrop, the present study endeavors to employ a survey-based approach to evaluate the eHealth literacy levels of cardiovascular disease patients. Through this investigation, we aim to dissect the influencing factors and subsequently formulate evidence - based strategies to enhance eHealth literacy, thereby fostering better health outcomes for this patient population.
Prior studies have established the importance of eHealth literacy in chronic disease management (10–12). However, limited research focuses on cardiovascular patients, particularly in China. Additionally, existing literature lacks consensus on the key sociodemographic predictors of eHealth literacy in this population. Therefore, this study addresses the following research questions: (1) What is the current level of eHealth literacy among cardiovascular disease patients? (2) Which sociodemographic and clinical factors significantly influence eHealth literacy levels?
The aim of this study is to assess eHealth literacy levels among cardiovascular disease patients and identify key determinants, providing evidence for targeted health communication strategies.
2 Materials and methods
2.1 Research subjects
We employed purposive sampling to recruit study participants. Cardiovascular disease patients who visited the cardiology department of a tertiary hospital in Shandong Province between January 2023 and August 2023 were selected. The inclusion criteria were as follows: (1) aged 18 years or older; (2) with a confirmed diagnosis of cardiovascular disease, including hypertension (ICD-10: I10-I15), coronary artery disease (I20-I25), heart failure (I50), and arrhythmias (I44-I49), as documented in their medical records. (3) having clear consciousness and the capacity to accurately comprehend the questionnaire content; and (4) providing voluntary consent to participate in the survey.
2.2 Methods
A purposive sampling strategy was employed between October 2023 and June 2024 at a tertiary hospital in Shandong Province. Eligible patients were approached during routine outpatient visits or post-hospitalization follow-ups. Research assistants explained the study purpose and obtained written informed consent.
A total of 720 questionnaires were distributed to cardiovascular patients, and 616 valid responses were retrieved, yielding an effective response rate of 85.5%. To minimize selection bias, recruitment was conducted across both urban and rural clinics, and all eligible individuals within the study period were invited unless they declined participation. Questionnaires were deemed invalid and excluded if they met any of the following criteria: (1) Missing values in ≥20% of eHEALS items; (2) Implausible responses (e.g., identical answers for all Likert-scale questions); (3) Completion time <5 min (determined via pilot testing as insufficient for thoughtful responses). Among 720 distributed questionnaires, 104 were excluded based on these criteria, yielding 616 valid responses for analysis.
A self-developed eHealth literacy survey questionnaire for cardiovascular disease patients was utilized. This questionnaire is composed of two principal components. The first part is designed to gather general information, encompassing patients’ age, gender, place of residence, educational attainment, marital status, and other fundamental demographic details. The second part is written by scholars including Norman, C. D (5), titled The eHealth Literacy Scale (eHEALS), which assesses competencies in searching, evaluating, and applying online health information. This scale predominantly comprises 8 items, each employing a five-point Likert scale. The response options are “strongly agree,” “agree,” “neutral,” “disagree,” and “strongly disagree”, which are assigned scores of 5, 4, 3, 2, and 1 point, respectively. Higher aggregate scores signify greater eHealth literacy levels. A score of 24 or above is defined as the threshold for adequate eHealth literacy, enabling the categorization of patients into groups with adequate and inadequate eHealth literacy (13).
The translated eHEALS has been rigorously validated, demonstrating good reliability and validity (14). In this study, the questionnaire exhibited a Cronbach’s α coefficient of 0.895. All surveyors received standardized training from the research team. They meticulously explained the study’s objectives, significance, and completion guidelines to the patients. The survey was administered via an online questionnaire platform. After securing patients’ informed consent, they were directed to scan a QR code to complete the data collection online, ensuring a seamless and efficient data - gathering process.
2.3 Statistical analyses
All statistical analyses were carried out using SPSS software, version 26.0. For measurement data, descriptive statistics were presented as the mean ± standard deviation. The t-test was employed to assess differences between groups. Categorical variables were expressed as percentages, and group differences were evaluated using the chi - square test. To establish statistical significance, logistic regression analysis was performed, with statistical significance set at a threshold of p < 0.05.
3 Results
3.1 Results of general information
A total of 720 questionnaires were disseminated. Following data screening and the exclusion of invalid data, 616 valid questionnaires were retained, resulting in an effective recovery rate of 85.5%. Among the 616 patients with cardiovascular disease, 274 (44.5%) were aged over 50 years. The sample consisted of 381 males (61.9%) and 235 females (38.1%). A total of 315 patients (51.1%) had a high school education or lower. The majority of patients (272, 44.2%) resided in urban areas. The monthly income of most patients fell within the range of 2000–5,000 yuan (243, 39.4%). The distance from their residences to the medical institutions they frequently visited was mainly 2–5 kilometers (205, 33.3%). Further details of the general data are presented in Table 1.
3.2 eHealth literacy scores among cardiovascular disease patients
The eHealth literacy scores of cardiovascular disease patients averaged 20.46 ± 9.54, with a passing rate of 38.6%. The mean score across all items was 2.55 ± 1.19. Specifically, for the items related to the capability of accessing and applying internet health information, evaluating internet health information and services, and making decisions based on such information and services, the mean scores were 2.49 ± 1.18, 2.67 ± 1.32, and 2.66 ± 1.35, respectively. Among individual items, the statement “I possess the necessary skills to evaluate whether the information found on the internet is useful” received the highest score, while “I know what kind of health information can be found on the internet” had the lowest score. Further details are presented in Table 2.
3.3 Binary logistic analysis of factors influencing eHealth literacy in cardiovascular disease
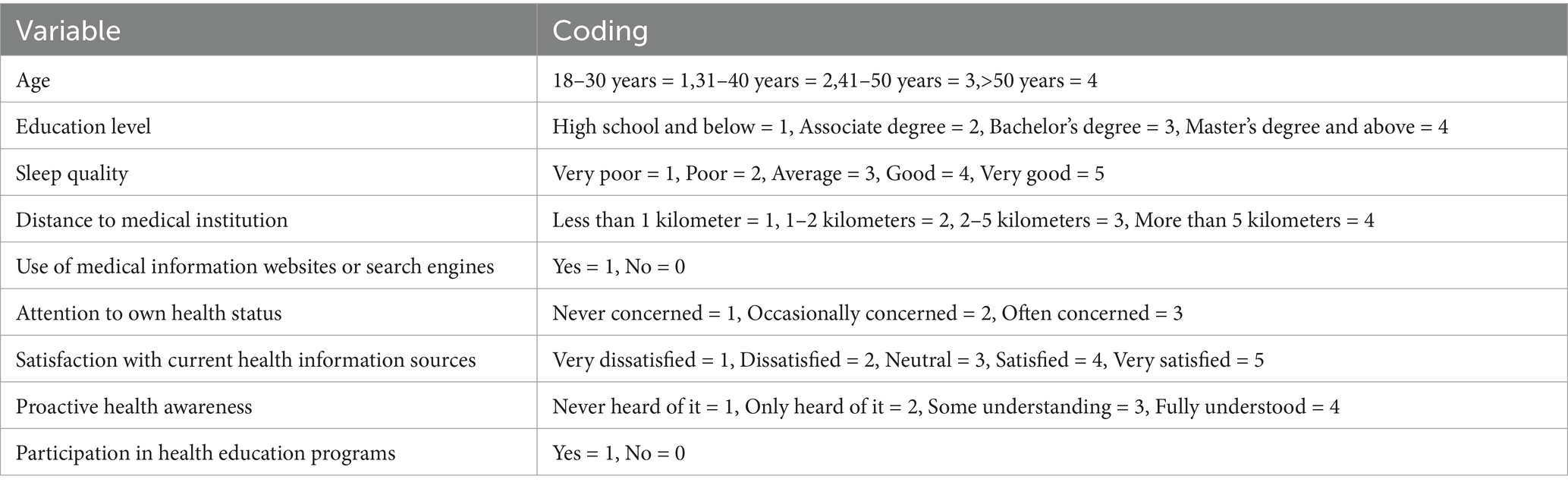
We employed eHealth literacy qualification as the dependent variable (coded as: unqualified = 0, qualified = 1). Binary logistic regression analysis was then performed, with the factors identified as significant in the univariate analysis serving as independent variables. The detailed coding of these variables is provided in Table 3.
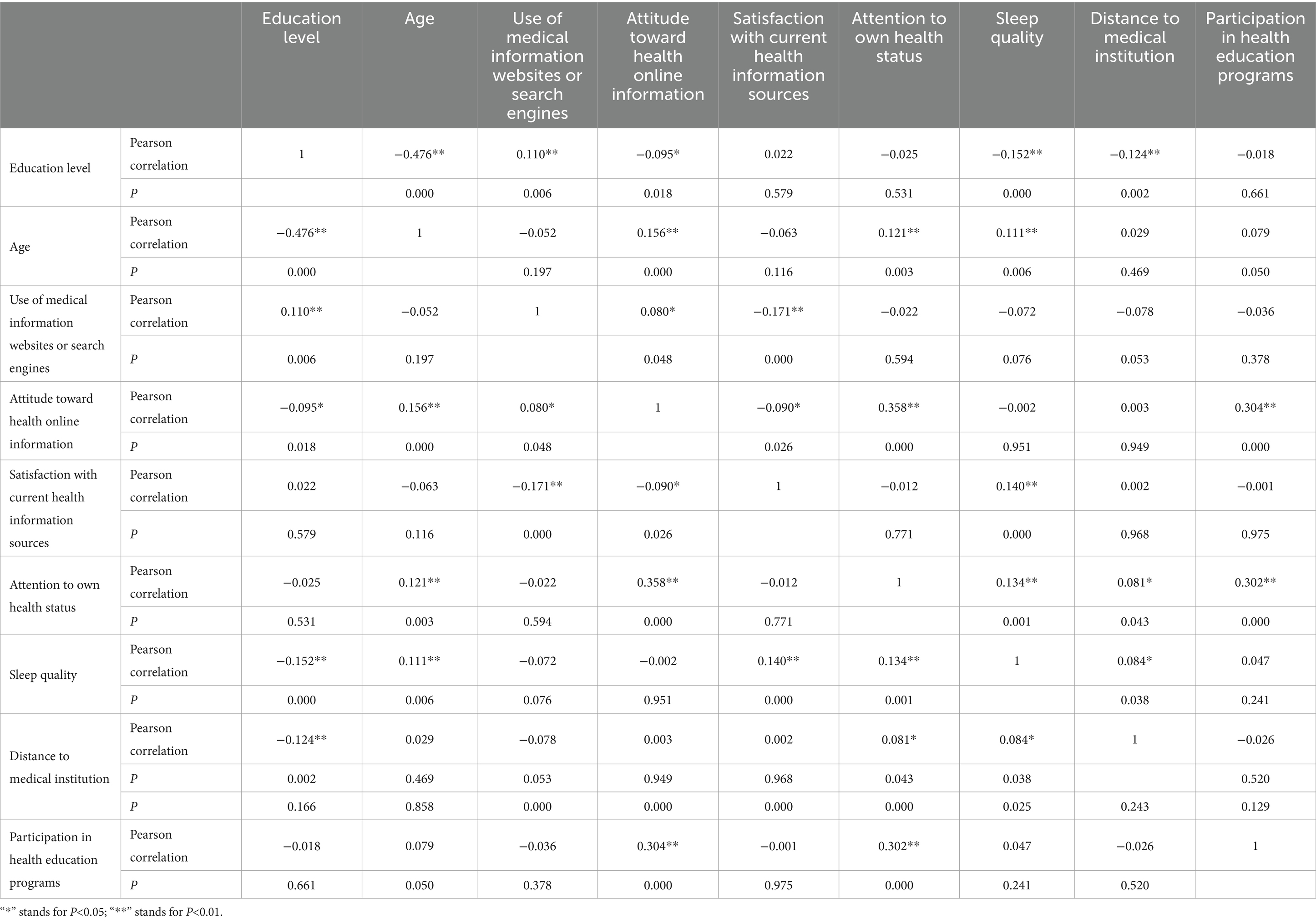
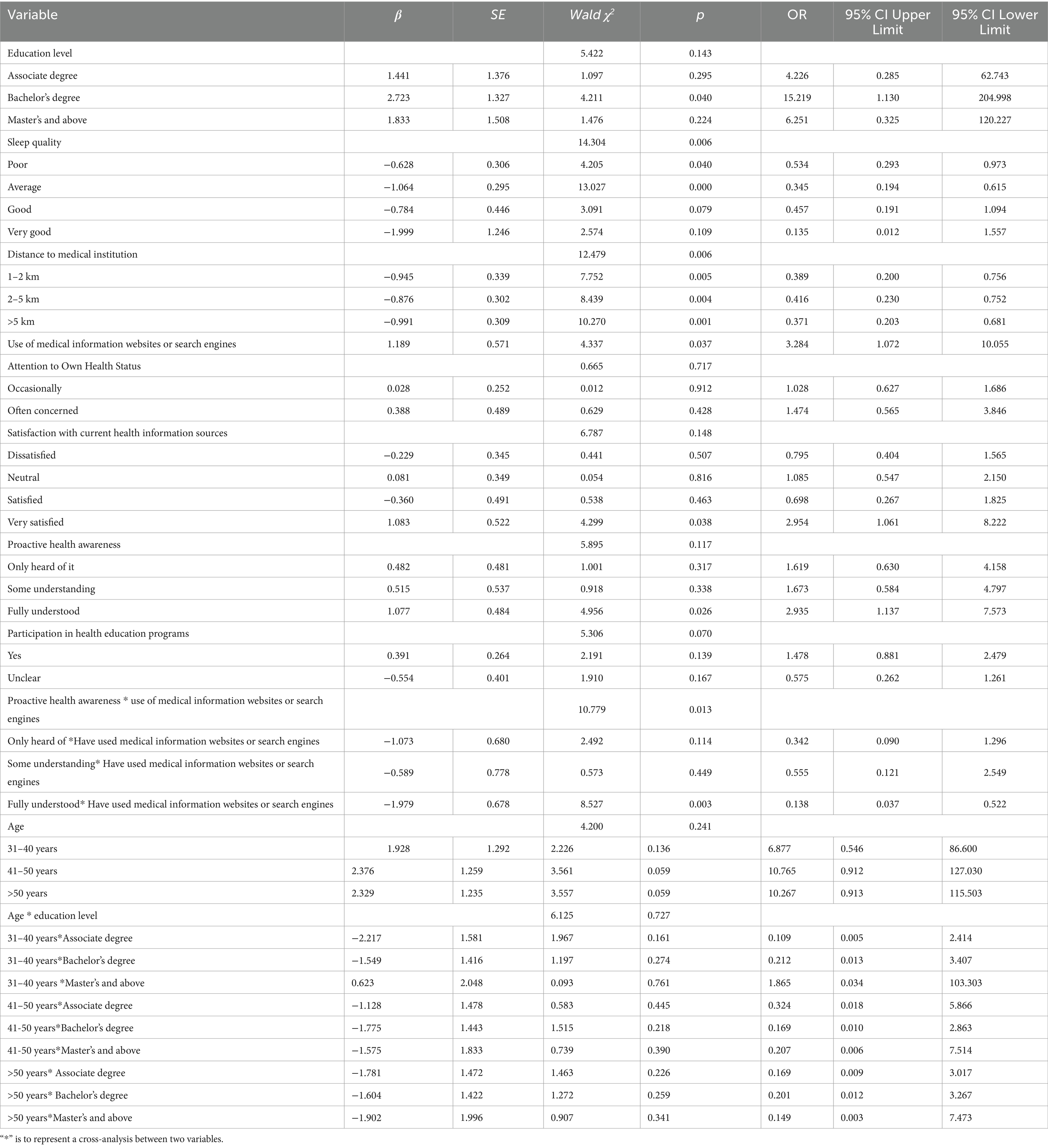
Pearson correlation analysis was conducted to assess multicollinearity. The results revealed that all correlation coefficients between variables were below 0.8, indicating no high linear associations among the variables, thus allowing for further analysis. The results of the Pearson correlation analysis are presented in Table 4.The findings of the binary logistic analysis revealed that several factors were associated with eHealth literacy qualification among cardiovascular disease patients. Specifically, education level, sleep quality, residing in close proximity to a medical institution (distance < 5 km), prior utilization of medical information websites or search engines, as well as the interaction between proactive health awareness and utilization of medical information websites or search engines were all important determinants (p < 0.05).The results of this analysis are presented in Table 5.
4 Discussion
4.1 Current status of eHealth literacy among cardiovascular disease patients
The survey findings reveal that the eHealth literacy score of cardiovascular disease patients is 20.46 ± 9.54. This value is lower than that of the general health check-up population (15), hospitalized patients with chronic kidney disease (16), hospitalized respiratory disease patients (17), and cancer patients (13). Nevertheless, it is marginally higher than the eHealth literacy score of the older adult. These results imply that there exists substantial potential for improving the eHealth literacy levels among cardiovascular disease patients.
Previous research has demonstrated that, both globally and domestically, the eHealth literacy levels of chronic disease patients are generally suboptimal (18–21), aligning with the outcomes of our study. This underscores the pressing necessity to enhance eHealth literacy among chronic disease patients, particularly in the face of an aging demographic and the accelerating pace of digitalization.
Notably, the dimension of “internet health information services and application capabilities” received the lowest score. This suggests that cardiovascular disease patients lack clarity regarding the utilization of the internet for acquiring health knowledge and information.
The relatively low eHealth literacy among cardiovascular disease patients may be attributed to the fact that a substantial proportion of them are middle - aged and older adult individuals. These patients typically have less frequent exposure to electronic devices, which in turn restricts their capabilities in accessing, evaluating, and applying online health information (22).
Healthcare professionals play a pivotal role in addressing this issue. They can assist patients by disseminating reliable online health knowledge resources, fostering an environment that encourages patients to engage in active learning, and promoting shared decision - making processes. This approach enables patients to make well - informed health - related decisions.
Notwithstanding the extensive presence of online health information, its complexity and variable quality pose significant challenges. Even younger demographics may encounter difficulties in discerning the quality of such information. This complexity can impede patients from making accurate health decisions based on online resources (23).
Consequently, healthcare professionals are urged to offer comprehensive training in eHealth. This includes curating a list of reliable health information websites, designing professional information - sharing platforms tailored to patients’ needs, and recommending trustworthy eHealth products and wearable devices (24–26). Such initiatives would empower patients to access, comprehend, evaluate, and apply relevant health information more effectively, ultimately leading to an improvement in their overall health status.
4.2 Analysis of factors influencing eHealth literacy among cardiovascular disease patients
The survey findings reveal that education level, sleep quality, proximity to medical institutions, utilization of medical information websites or search engines are determinants of eHealth literacy attainment in cardiovascular disease patients.
Using high school education or below as the reference group, individuals with undergraduate-level educational attainment demonstrated 15.219 times higher odds of achieving adequate eHealth literacy (OR: 15.219, 95% CI: 1.130–204.998). This aligns with previous research showing education level strongly predicts digital health competency through enhanced information processing and critical thinking skills (27). Therefore, health education interventions should particularly target less-educated populations through: (1) Developing tiered education programs using visual aids and simplified language for low-literacy groups; (2) Implementing community-based digital navigation services to bridge the “last mile” of health information access; (3) Creating hospital-community linkage mechanisms for sustained health education support.
The e-health literacy among the general population with relatively poor sleep quality is 0.534 (95% CI: 0.293, 0.973) and 0.345 times (95% CI: 0.194, 0.615) for those with very poor sleep quality. This is consistent with the results of previous studies, person with higher eHealth literacy are more likely to seek health information online, which may trigger excess searches online (28). Excessive internet use directly reduces netizens’ sleep duration and quality, leading to poor sleep.
The distances from medical institutions to home of 1–2, 2–5, and over 5 kilometers are 0.756 times (95% CI: 0.389–0.200), 0.416 (95% CI: 0.230–0.752), and 0.371 times (95% CI: 0.203–0.681) respectively, compared to the group whose distance from home is less than 1 kilometer. And contrary to initial hypotheses, administrative geographic labels (urban/town/rural) showed no direct association with eHealth literacy (p = 0.719). This finding challenges the utility of broad rural–urban dichotomies in digital health research. Instead, functional access barriers—proximity to medical institutions and community health education availability—emerged as stronger predictors, suggesting that physical and informational accessibility, rather than residency classification, may better explain disparities.
Patients residing in closer proximity to medical institutions, benefit from better access to comprehensive medical services (29). This likely leads to a greater emphasis on personal health, contributing to a higher perceived level of health literacy. This observation implies that health and wellness authorities should optimize the distribution of medical resources to narrow the urban - rural divide and safeguard patients’ equitable access to healthcare services (30, 31). And policymakers should prioritize expanding telehealth infrastructure and community-based training in underserved areas, regardless of administrative boundaries.
Some patients with high active health and more engine use have a low level of e-health literacy, which may be related to distrust of content in the network. Most patients who have previously utilized medical search engines demonstrate proficiency in acquiring health information online. They are more likely to be skilled in exploring diverse information - gathering strategies (32). Those who used such websites or search engines were 3.284 times more likely to be e-health literacy eligible than those who did not. Moreover, they tend to be more satisfied with their current health information sources, which is associated with a higher perceived eHealth literacy. This highlights the necessity for eHealth knowledge dissemination initiatives, such as health knowledge seminars and online health education campaigns. These efforts should promote reliable sources of cardiovascular health information, including search engines and specialized information portals (33).
Previous studies have demonstrated an inverse correlation between age and eHealth literacy, with younger populations exhibiting superior capabilities in health information seeking, evaluation, and application due to earlier exposure and adaptability to digital tools (34). Furthermore, aging-related cognitive decline diminishes older adults’ capacity to process electronic health information, compounded by distinct health needs and insufficient adaptability to eHealth technologies, collectively contributing to lower eHealth literacy levels in older adult populations (35). Occupation has conventionally been identified as a determinant of eHealth literacy, with technology-intensive professionals (e.g., education, healthcare, IT) demonstrating enhanced literacy levels attributable to higher socioeconomic status and routine digital tool utilization (36).
Notwithstanding theoretical expectations regarding the substantial influence of age and occupation on eHealth literacy, our regression analysis revealed no statistically significant associations for either variable. This discrepancy may stem from age-related sampling bias, as 44.5% of participants exceeded 50 years old. The restricted variability in eHealth literacy within this subgroup, potentially attributable to comparable digital health technology exposure and skill levels, might have attenuated the independent age effect. Additionally, age might exert indirect effects on eHealth literacy through mediating variables such as educational attainment and prior utilization of medical search engines, thereby diminishing its direct explanatory power. The occupational variable’s significance could be obscured by interaction bias with age, given the potential overrepresentation of older participants in low-digital-literacy occupations (e.g., retirees, traditional industry workers), consequently weakening the overall occupational effect magnitude.
Although the eHEALS scale effectively measures general eHealth literacy, it does not assess patients’ ability to use emerging tools such as mobile health apps or wearable devices. Future interventions could combine targeted educational materials with innovative case management via remote monitoring technologies. For example, integrating wearable device data into patient portals may facilitate personalized feedback and improve health outcomes. Based on our findings, critical next steps include: (1) Developing pilot training programs to test the efficacy of curated eHealth resources; (2) Designing longitudinal studies to evaluate the impact of wearable device integration on disease management; (3) Collaborating with technology developers to create patient-centered eHealth tools with simplified interfaces.
This study has several limitations. First, the purposive sampling from a single tertiary hospital limits generalizability, as participants may represent a more medically engaged subgroup compared to the broader CVD population. Second, the online data collection methodology likely excluded individuals with lower digital literacy or limited internet access, potentially inflating eHealth literacy estimates. While this approach ensured standardized administration, it introduces selection bias that future studies could mitigate through mixed-methods designs combining online and community-based recruitment. Finally, this study is limited by the potential age distribution bias in the sample (44.5% aged over 50 years), which may obscure the genuine effects of age and occupational characteristics. Future research will employ stratified sampling to balance age and occupational distributions while expanding the young population sample to enhance statistical power. Additionally, the current investigation inadequately explores potential mediating pathways through which age influences eHealth literacy. Subsequent studies should quantify age-related indirect effects using structural equation modeling to elucidate comprehensive causal mechanisms.
Data availability statement
The datasets presented in this article are not readily available because the policies and confidentiality agreements adhered to in our laboratory, we regretfully cannot furnish the raw data. Requests to access the datasets should be directed to WW, MTQ3MDc4NzI5QHFxLmNvbQ==.
Ethics statement
The studies involving humans were approved by Shandong Provincial Hospital Ethics Committee on Biomedical Research Involving Human Subjects. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
WW: Investigation, Resources, Supervision, Writing – review & editing. MJ: Formal analysis, Investigation, Writing – original draft. XZhao: Formal analysis, Supervision, Writing – original draft. CC: Investigation, Methodology, Writing – original draft. WJ: Project administration, Supervision, Writing – review & editing. XZhan: Formal analysis, Methodology, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the following funding sources: Shandong Province Social Science Planning Research Project (22CGLJ36), Shandong Province Social Science Planning and Research Special Project (21CSDJ60), and Shandong Province Medical and Health Science and Technology Project (202303010274).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhang, AY, and Kong, LZ. The epidemic situation and prevention countermeasures of chronic diseases. Chin J Pre Contr Chron Dis. (2005) 1:1–3. doi: 10.3969/j.issn.1671-3141.2020.54.193
2. Machado, DB, Pescarini, JM, Ramos, D, Teixeira, R, Lozano, R, Pereira, VOM, et al. Monitoring the progress of health-related sustainable development goals (SDGs) in Brazilian states using the global burden of disease indicators. Popul Health Metrics. (2020) 18:7. doi: 10.1186/s12963-020-00207-2
3. Wang, LM, Chen, ZH, Zhang, M, Zhao, ZP, Huang, ZJ, Zhang, X, et al. Prevalence and disease burden of chronic diseases among the elderly in China. Chin J Epidemiol. (2019) 40:277–83. doi: 10.3760/cma.j.issn.0254-6450.2019.03.005
4. Wu, SY, Cai, YY, Xu, XY, Zheng, KC, and Li, HY. Challenges and opportunities of "medical-prevention" integration for common chronic diseases in China. Chin J Public Health. (2019) 35:1289–92. doi: 10.11847/zgggws1126005
5. Norman, CD, and Skinner, HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e27. doi: 10.2196/jmir.8.4.e27
6. Choi, NG, and Dinitto, DM. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. (2013) 15:e93. doi: 10.2196/jmir.2645
7. Dai, CH, Wang, X, Zeng, XM, Xu, PX, and Feng, JG. Correlation analysis of eHealth literacy and health behaviors among. Prac J Cardiac Cerebral Pneumal Vascular Dis. (2020) 28:57–61. doi: 10.3969/j.issn.1008-5971.2020.06.011
8. Li, SJ, Cui, GH, Yin, YT, Wang, SY, Liu, XY, and Chen, L. Health-promoting behaviors mediate the relationship between eHealth literacy and health-related quality of life among Chinese older adults: a cross-sectional study. Quality of life research: an international journal of quality of life aspects of treatment. Qual Life Res. (2021) 30:2235–43. doi: 10.1007/s11136-021-02797-2
9. Chen, XY, Wang, YB, and Duan, HM. Topic mining and analysis of chronic disease health literacy based on LDA topic model. Chin J Nurs. (2022) 28:2111–5. doi: 10.3760/cma.j.cn115682-20211105-04992
10. Verweel, L, Newman, A, Michaelchuk, W, Packham, T, Goldstein, R, and Brooks, D. The effect of digital interventions on related health literacy and skills for individuals living with chronic diseases: a systematic review and meta-analysis. Int J Med Inform. (2023) 177:105114. doi: 10.1016/j.ijmedinf.2023.105114
11. Dawson, J, Lambert, K, Campbell, KL, and Kelly, JT. Incorporating digital platforms into nutritional care in chronic kidney disease. Semin Dial. (2024) 37:350–9. doi: 10.1111/sdi.12998
12. Lim, DSC, Kwok, B, Williams, P, and Koczwara, B. The impact of digital technology on self-Management in Cancer: systematic review. JMIR Cancer. (2023) 9:e45145. doi: 10.2196/45145
13. Kang, DQ, Lu, YH, and Wang, Y. Investigation on the current status and influencing factors of eHealth literacy among tumor patients. Chin J Nurs. (2020) 26:2998–3004. doi: 10.3760/cma.j.cn115682-20200407-02535
14. Chen, J, Zheng, Z, Zhao, J, and Ou, MX. Psychometric evaluation of the Chinese version of the eHealth literacy scale. Chin J Nurs. (2019) 25:2783–7. doi: 10.3760/cma.j.issn.1674-2907.2019.22.003
15. Wu, SZ, Gao, D, and Wang, D. Current status and influencing factors of eHealth literacy among people undergoing health check-ups. J Pract Med. (2022) 38:1141–6. doi: 10.3969/j.issn.1006-5725.2022.09.018
16. Liu, YX, Zhao, X, Duan, DF, Ma, DY, and Wen, Y. Current status and influencing factors of eHealth literacy among hospitalized patients with chronic kidney disease. Chin J Nurs. (2022) 28:4484–9. doi: 10.3760/cma.j.cn115682-20211231-05935
17. Chen, J, Zheng, Z, Han, YM, and Zhang, BW. Survey and analysis of eHealth literacy among inpatients with respiratory diseases in a tertiary hospital in Beijing. Chin J Nurs. (2019) 25:3129–33. doi: 10.3760/cma.j.issn.1674-2907.2019.24.021
18. Shiferaw, KB, Tilahun, BC, Endehabtu, BF, Gullslett, MK, and Mengiste, SA. E-health literacy and associated factors among chronic patients in a low-income country: a cross-sectional survey. BMC Med Inform Decis Mak. (2020) 20:181. doi: 10.1186/s12911-020-01202-1
19. Hoogland, AI, Mansfield, J, Lafranchise, EA, Bulls, HW, Johnstone, PA, and Jim, HSL. eHealth literacy in older adults with cancer. J Geriatr Oncol. (2020) 11:1020–2. doi: 10.1016/j.jgo.2019.12.015
20. Lee, WL, Lim, ZJ, Tang, LY, Yahya, NA, Varathan, KD, and Ludin, SM. Patients’ technology readiness and eHealth literacy: implications for adoption and deployment of eHealth in the COVID-19 era and beyond. Comput Inform Nurs. (2021) 40:244–50. doi: 10.1097/CIN.0000000000000854
21. Cui, GH, Li, SJ, Yin, YT, Chen, LJ, Li, JQ, Liang, FY, et al. The relationshipamong social capital, eHealth literacy and health behaviours in Chinese elderly people: a cross-sectional study. BMC Public Health. (2021) 21:45. doi: 10.1186/s12889-020-10037-4
22. Nahm, ES, Zhu, S, Bellantoni, M, Keldsen, L, Russomanno, V, Rietschel, M, et al. The effects of a theory-based patient portal e-learning program for older adults with chronic illnesses. Telemed J E Health. (2019) 25:940–51. doi: 10.1089/tmj.2018.0184
23. Oh, SS, Kim, K-A, Kim, M, Oh, J, Chu, SH, and Choi, J. Measurement of digital literacy among older adults: systematic review. J Med Internet Res. (2021) 23:e26145. doi: 10.2196/30828
24. Baker, DW, Dewalt, DA, Schillinger, D, Hawk, V, Ruo, B, DomingoK, B, et al. The effect of progressive, reinforcing telephone education and counseling versus brief educational intervention on knowledge, self-carebehaviors and heart failure symptoms. J Card Fail. (2011) 17:789–96. doi: 10.1016/j.cardfail.2011.06.374
25. Yanicelli, LM, Goy, CB, González, VDC, Palacios, GN, Martínez, EC, and Herrera, MC. Non-invasive home telemonitoring system for heart failure patients: a randomized clinical trial. J Telemed Telecare. (2021) 27:553–61. doi: 10.1177/1357633X19899261
26. Melholt, C, Joensson, K, Spindler, H, Tracey, A, Thorup, C, Kringelholt, R, et al. Cardiac patients’ experiences with a telerehabilitation web portal: implications for eHealth literacy. Patient Educ Couns. (2018) 101:854–61. doi: 10.1016/j.pec.2017.12.017
27. Wubante, SM, Tegegne, MD, Melaku, MS, Kalayou, MH, Tarekegn, YA, Tsega, SS, et al. eHealth literacy and its associated factors in Ethiopia: systematic review and meta-analysis. PLoS One. (2023) 18:e0282195. doi: 10.1371/journal.pone.0282195
28. Zhu, X, Zheng, T, Ding, L, and Zhang, X. Exploring associations between eHealth literacy, cyberchondria, online health information seeking and sleep quality among university students: a cross-section study. Heliyon. (2023) 9:e17521. doi: 10.1016/j.heliyon.2023.e17521
29. Dong, X, and Wang, Y. The geography of healthcare: mapping patient flow and medical resource allocation in China. Econ Hum Biol. (2024) 55:101431. doi: 10.1016/j.ehb.2024.101431
30. Zhang, QQ, Jin, H, Shi, XX, and Yu, DH. Implementation status of proactive health in China and suggestions for implementation strategies by responsibleentities. Chin Gen Pract. (2022) 25:3932. doi: 10.12114/j.issn.1007-9572.2022.0419
31. Eiland, L, and Drincic, A. Far apart, but close at heart: the importance of understanding patient barriers to telehealth and potential solutions. Circulation. (2022) 146:147–9. doi: 10.1161/CIRCULATIONAHA.121.057576
32. Cajita, MI, Hodgson, NA, Budhathoki, C, and Han, HR. Intention to use mHealth in older adults with heart failure. J Cardiovasc Nurs. (2017) 32:E1–7. doi: 10.1097/JCN.0000000000000401
33. Jones, J, Cassie, S, Thompson, M, Atherton, I, and Leslie, SJ. Delivering healthcare information via the internet: cardiac patients’ access, usage, perceptions of usefulness, and web site content preferences. Telemed J E Health. (2014) 20:223–8. doi: 10.1089/tmj.2013.0182
34. Abrha, S, Abamecha, F, Amdisa, D, Tewolde, D, and Regasa, Z. Electronic health literacy and its associated factors among university students using social network sites (SNSs) in a resource-limited setting, 2022: cross-sectional study. BMC Public Health. (2024) 24:3444. doi: 10.1186/s12889-024-21022-6
35. Jiang, X, Wang, L, Leng, Y, Xie, R, Li, C, Nie, Z, et al. The level of electronic health literacy among older adults: a systematic review and meta-analysis. Arch Public Health. (2024) 82:204. doi: 10.1186/s13690-024-01428-9
Keywords: cardiovascular disease, health literacy, eHealth literacy, health education, influencing factors
Citation: Wang W, Jiao M, Zhao X, Chen C, Jiang W and Zhang X (2025) Assessment of eHealth literacy among cardiovascular disease patients and analysis of influencing factors. Front. Public Health. 13:1587163. doi: 10.3389/fpubh.2025.1587163
Edited by:
Jordi Piera-Jiménez, Catalan Health Service, SpainReviewed by:
Isaac Cano, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), SpainRojan Gümüş, Dicle University, Türkiye
Marina Ramiro Pareta, Digitalization for the Sustainability of the Healthcare System (DS3) research group, Spain
Copyright © 2025 Wang, Jiao, Zhao, Chen, Jiang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoman Zhang, MTAyNjAzNDE0OEBxcS5jb20=; Wenhui Jiang, amlhbmd3ZW5odWlAbWFpbC54anR1LmVkdS5jbg==
 Wei Wang
Wei Wang Mengfan Jiao2
Mengfan Jiao2 Wenhui Jiang
Wenhui Jiang