- 1College of Public Health Sciences, Chulalongkorn University, Bangkok, Thailand
- 2Boromarajonani College of Nursing Chiang Mai, Faculty of Nursing, Praboromarajchanok Institute, Chiang Mai, Thailand
- 3Department of Mental Health, Prasrimahabhodi Hospital, Ubon Ratchathani, Thailand
- 4School of Nursing, Johns Hopkins University, Baltimore, MD, United States
Background: The differential effects of the COVID-19 pandemic across various regions and demographic groups underscore the importance of comprehending the role of social determinants of health (SDOH) in shaping mental health disparities. This research seeks to investigate the influence of both individual-level and provincial-level factors on stress experienced by the Thai general population during the second wave of the pandemic. By incorporating the SDOH conceptual framework within a multi-level modeling approach. The focus is on understanding the impact of these factors on mental health concerns, which have significantly increased due to the pandemic.
Methods: This study is a secondary data analysis of data collected between December 17, 2020, and February 23, 2021, from the Department of Mental Health, Ministry of Public Health, Thailand. Data for the provincial-level including COVID-19 zone and population density, with 258,830 participants nested within the 77 provinces. Stress was measured with 5-item of Srithanya stress test (ST-5). Multilevel analysis was carried out in HLM 8.2 software.
Results: The study found that individual-level factors including male respondents, unemployed, financial hardship, chronic underlying diseases, having older and/or children in family, and having bedridden patients in family tended to report higher stress scores. While, older age respondents, contracted with COVID-19 infection in self and/or family, and having greater resilience showed the lower stress scores. After adjustment for individual-level factors, the respondents who lived in higher and strict control area, and higher population density reported higher stress scores.
Conclusion: Individual and provincial factors appear to influence elevated stress levels. Our research indicates that the government should establish effective resilience promotion programs to mitigate the impact of stress on severe physical and psychological illnesses. Implementing these measures will improve the mental health and well-being of the general population and enhance the country’s preparedness for future pandemics or emerging outbreaks.
1 Introduction
COVID-19 was declared a global pandemic in March 2020 (1, 2), with Thailand facing its first wave through superspreading events in nightclubs and boxing stadiums (3). A more severe second wave occurred between mid-December 2020 and late February 2021, driven by outbreaks among migrant workers and illegal border crossings. This wave saw a sevenfold increase in cases compared to the first (4). Beyond its physical impact, the pandemic significantly threatened global mental health. Evidence indicates a substantial increase in stress-related mental health issues among both the general population and vulnerable groups (5–7), leading to various physical and mental health concerns (8).
The social determinants of health (SDOH) encompass the wide range of conditions in which people are born, grow, work, live, and age, influenced by broader systemic factors such as policies, cultural norms, and economic structures that shape daily life (9). These determinants include socioeconomic status, education, physical environment, employment, social support networks, and access to healthcare, all of which interact to influence health outcomes across populations (10). The impact of SDOH is far-reaching, affecting both communicable diseases, such as those that spread from person to person, and non-communicable diseases, including chronic conditions like diabetes and heart disease. These factors do not operate in isolation; rather, they interact with one another in complex ways that can either support or hinder overall health and well-being. In the context of the COVID-19 pandemic, SDOH has played a significant role in determining how different populations are affected, with individuals in crowded living conditions, with limited access to healthcare, or in jobs that do not allow for remote work experiencing heightened stress levels and adverse health outcomes. This underscores the critical importance of considering SDOH in understanding health disparities and the varying impacts of global health crises on stress levels among different population segments.
In Thailand, investigating the role of SDOH is particularly crucial due to the country’s diverse socio-economic landscape, marked by significant inequalities in access to healthcare, economic resources, and living conditions. The uneven impact of the COVID-19 pandemic across diverse regions and demographic groups emphasizes the necessity of a more thorough examination of the ways in which social determinants shape mental health disparities. Given the stark differences between urban and rural areas and the economic challenges faced by vulnerable populations, a focused examination of SDOH can inform targeted public health interventions that address these disparities effectively.
A multilevel approach to understanding the effects of SDOH on stress during the COVID-19 pandemic provides a comprehensive analysis by considering both individual and provincial-level factors. At the individual level, sociodemographic characteristics such as age, gender, employment status, and chronic illness have been linked to increasing stress during the pandemic (11–14). Financial difficulties are particularly significant, leading to reduced access to healthcare, poorer living conditions, and heightened mental health challenges, aligning with the CSDH’s focus on the economic determinants (15). Chronic diseases further exacerbate mental health issues by reflecting both long-term health status and healthcare accessibility (16). Households with vulnerable members, such as children, the older adults, or those with severe illnesses, face additional stress due to income loss, caregiving responsibilities, and healthcare access challenges (17–19). Resilience, defined as the ability to positively adapt to life’s challenges, has proven to be a crucial factor in alleviating the negative impacts of the pandemic on stress levels (20, 21).
At the provincial level, two key factors—population density and COVID-19 zone classification—emerge as significant in the context of the COVID-19 pandemic. Living in crowded spaces or areas with high population density heightens the risk of COVID-19 infection, leading to increased stress levels (22). The COVID-19 zone classification, implemented by the Thai government, reflects the local epidemiological situation and determines the level of public health measures in each area. The Center for COVID-19 Situation Administration (CCSA) raised the level of preventive measures from surveillance areas to maximum and strict control areas based on the increasing number of new cases during the second wave (23). These zone-based measures, including school closures, business suspensions, and movement restrictions, can significantly impact stress levels among the population (4, 23, 24).
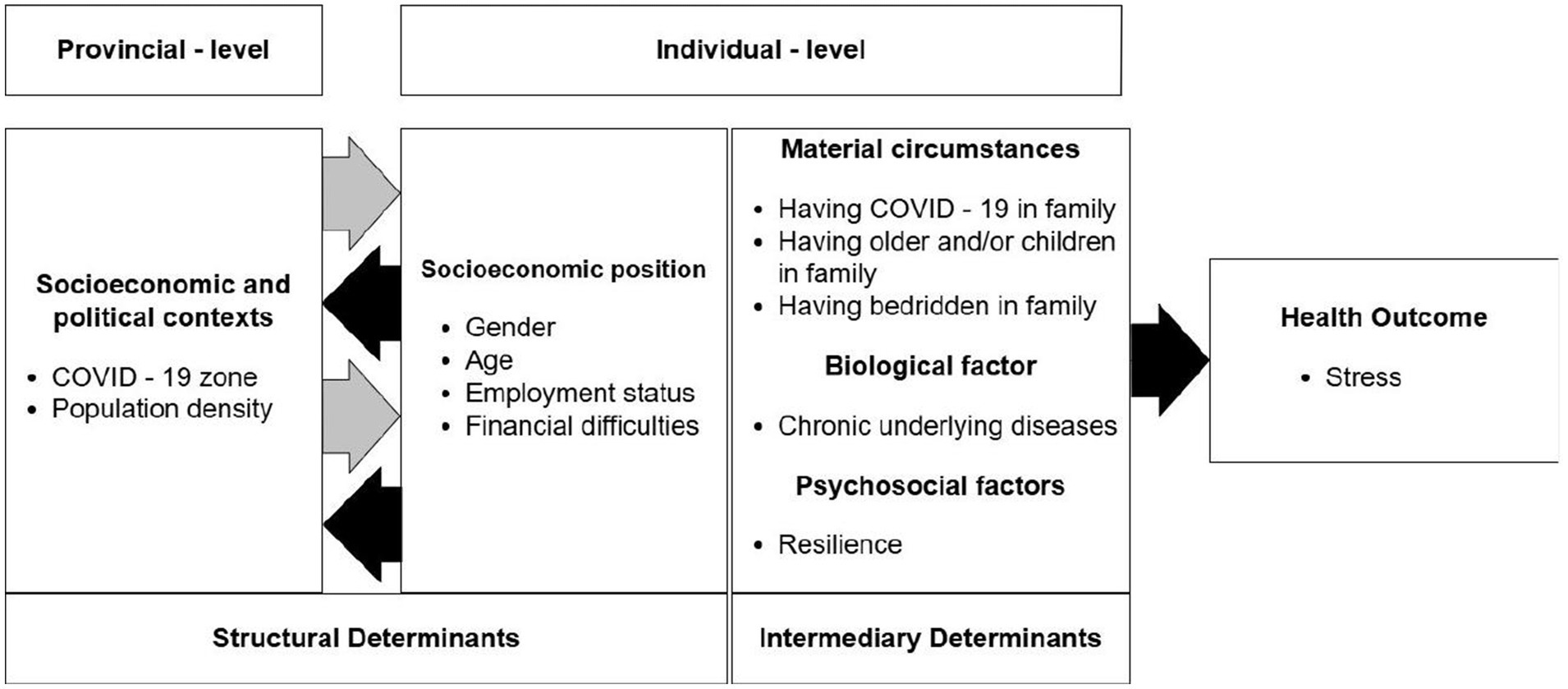
Guided by the World Health Organization (WHO)’s SDOH conceptual framework and integrating it into a multi-level model, our conceptual framework (Figure 1) demonstrates how stress is influenced at two distinct levels—individual and provincial. At the individual level, stress is shaped by a combination of both structural and intermediary determinants. These include socio-economic factors such as age, gender, employment status, and income, which define an individual’s position in society. Additionally, material circumstances like having COVID-19 in the family, caring for older adults or children, and managing bedridden family members are crucial intermediary determinants that directly impact daily life and elevate stress levels. Biological factors, such as chronic underlying diseases, further exacerbate stress by reflecting long-term health vulnerabilities. Psychosocial factors, particularly resilience—the ability to adapt positively to life’s challenges—serve as a critical buffer against stress.
At the provincial level, structural determinants such as COVID-19 zone classification and population density are significant factors that influence stress. These broader socioeconomic and political contexts shape the environment in which individuals live, determining the level of public health measures and the extent of pandemic-related challenges they face. The interaction between these individual and provincial factors ultimately culminates in the overall stress experienced by individuals. By integrating both levels of determinants within this multilevel framework, the model provides a comprehensive understanding of how various factors contribute to stress during the COVID-19 pandemic, emphasizing the complex interplay between individual circumstances and broader structural influences.
This study aims to investigate the influence of both individual-level and provincial-level factors on stress among the Thai general population during the second wave of the COVID-19 pandemic. By integrating the SDOH conceptual framework into a multi-level model approach, the research analyzes the impact of both individual factors, like sociodemographic and chronic illness, and provincial factors, such as population density and COVID-19 zone classification. The objective is to identify key determinants of stress across various regions and groups, offering insights that can inform targeted public health strategies to mitigate mental health disparities during this and future crises.
2 Methods
2.1 Study population and data source
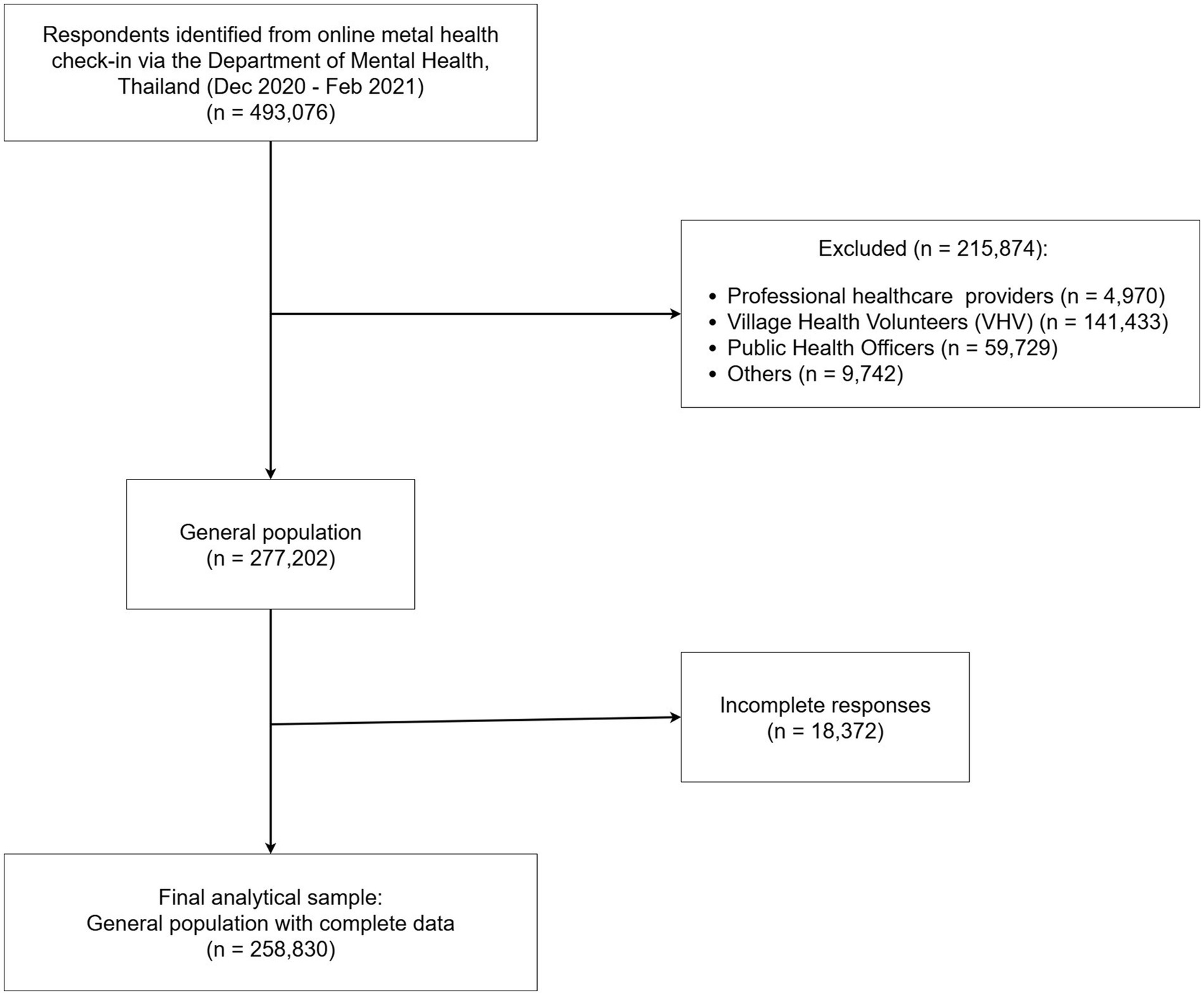
This study analyzed data collected through an online mental health check-in via the Department of Mental Health, Ministry of Public Health of Thailand website during the second wave of COVID-19 in Thailand between December, 2020 and February, 2021. The dataset initially included 493,076 respondents. After excluding 215,874 individuals who were healthcare professionals or volunteers, and 18,372 who did not provide complete information, the final sample comprised 258,830 individuals from the general population (Figure 2). Provincial-level data on COVID-19 surveillance and control areas were provided by the Center for COVID-19 Situation Administration (CCSA) (23) and population density (people/km2) data were obtained from the Official Statistics Registration Systems, Department of Provincial Administration of Thailand (25).
2.2 Study variables
2.2.1 Outcome variable
Stress was evaluated using the Srithanya Stress Test (ST-5), an established and broadly recognized tool endorsed by the Department of Mental Health, Ministry of Public Health of Thailand, for measuring stress levels within the Thai population. The ST-5 consists of 5 items that evaluate stress-related symptoms, including sleep problems, loss of concentration, irritability, boredom, and anti-social behavior (26). Each item is evaluated using a 4-point Likert scale: 0 for “Hardly ever or Never” (<1 times/week), 1 for “Sometimes” (1–2 times/week), 2 for “Usually” (3–4 times/week), and 3 for “Always” (5–7 times/week).” The total ST-5 scores span from 0 to 15, with higher scores reflecting a greater frequency or intensity of stress (27).
2.2.2 Individual-level variables
Individual demographic characteristics (e.g., gender, age, employment status, financial hardship, chronic underlying disease, and the presence of vulnerable family members) and resilience were included in the analysis. Resilience was measured using a 3-items scale. Respondents were asked about their ability to overcome obstacles and problems in life, to encourage themselves and feel supported by close relationships, and to manage their own problems and stress over the past 2 weeks. Responses were rated on a 10-point Likert scale, ranging from 1 (less confident) to 10 (very confident). The total resilience score could range from 3 to 30, with higher scores indicating a greater level of resilience (28).
2.2.3 Provincial-level variables
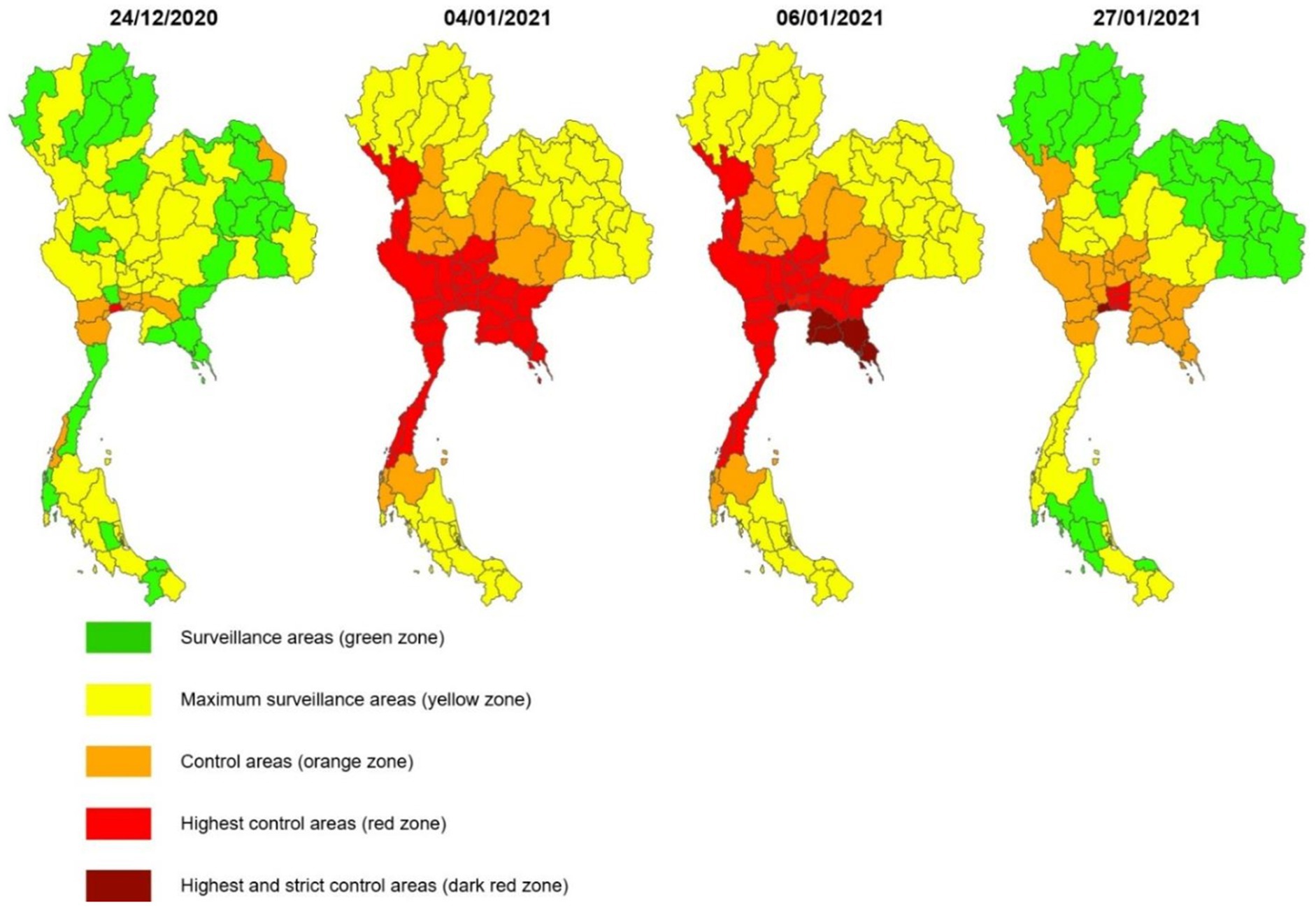
Population density (measured in people per square kilometer) and COVID-19 risk zones were treated as continuous variables across all 77 provinces in Thailand. The classification of COVID-19 zones followed official guidelines from the Center for COVID-19 Situation Administration (CCSA), which were based on the weekly incidence of newly reported cases per 100,000 population and the scope and intensity of locally implemented public health restriction measures at the local level. Five zone levels were designated: dark red (more than 15 cases or a super-spreader event with over 50 cases), red (5–15 cases or a test positivity rate below 5%), orange (1–5 cases or positivity rate under 2%), yellow (fewer than 1 case and no new cases reported in the preceding 7 days) (Figure 3), and green (no new infections for at least 28 consecutive days) (Figure 3). These classifications guided the implementation of localized restrictions, including curfews, suspension of alcohol sales and domestic travel, and closures of schools, restaurants, markets, entertainment venues, personal care businesses (such as spas, salons, and massage parlors), fitness centers, and other non-essential services (4, 8, 23). Population density data (people/km2) were obtained from the Official Statistics Registration Systems, Department of Provincial Administration of Thailand (25).
2.3 Statistical analysis
To evaluate model assumptions, a Q–Q plot of the residuals was inspected, revealing an approximately linear trend. This pattern supports the assumption of normality, indicating that the residuals were reasonably normally distributed. Regarding the independence of residuals at both levels, the observed variation in level-1 residuals across level-2 units justified the use of a multilevel modeling approach and suggested that the assumption of residual independence was adequately satisfied.
In this study, we utilized the Srithanya stress scale (ST-5) as the dependent variable, with scores ranging from 0 to 15. We investigated the factors influencing stress scores among the general population during the COVID-19 pandemic using a multilevel approach. The model incorporated two levels: the individual level (first level) nested within provinces (second level). This hierarchical structure allowed us to examine both individual-level and province-level factors contributing to stress scores, accounting for the potential clustering effect within provinces. The analysis was conducted using HLM 8.2 software.
The general form of the multilevel linear regression model is expressed as:
In this model, i and j denote individual and province subscripts, respectively. represents individual-level variables (e.g., gender, age, employment status), while represents province-level variables (e.g., COVID-19 surveillance and control area, population density). The terms and are residual errors at the province and individual levels, respectively. We assumed zero expectations for and in this model.
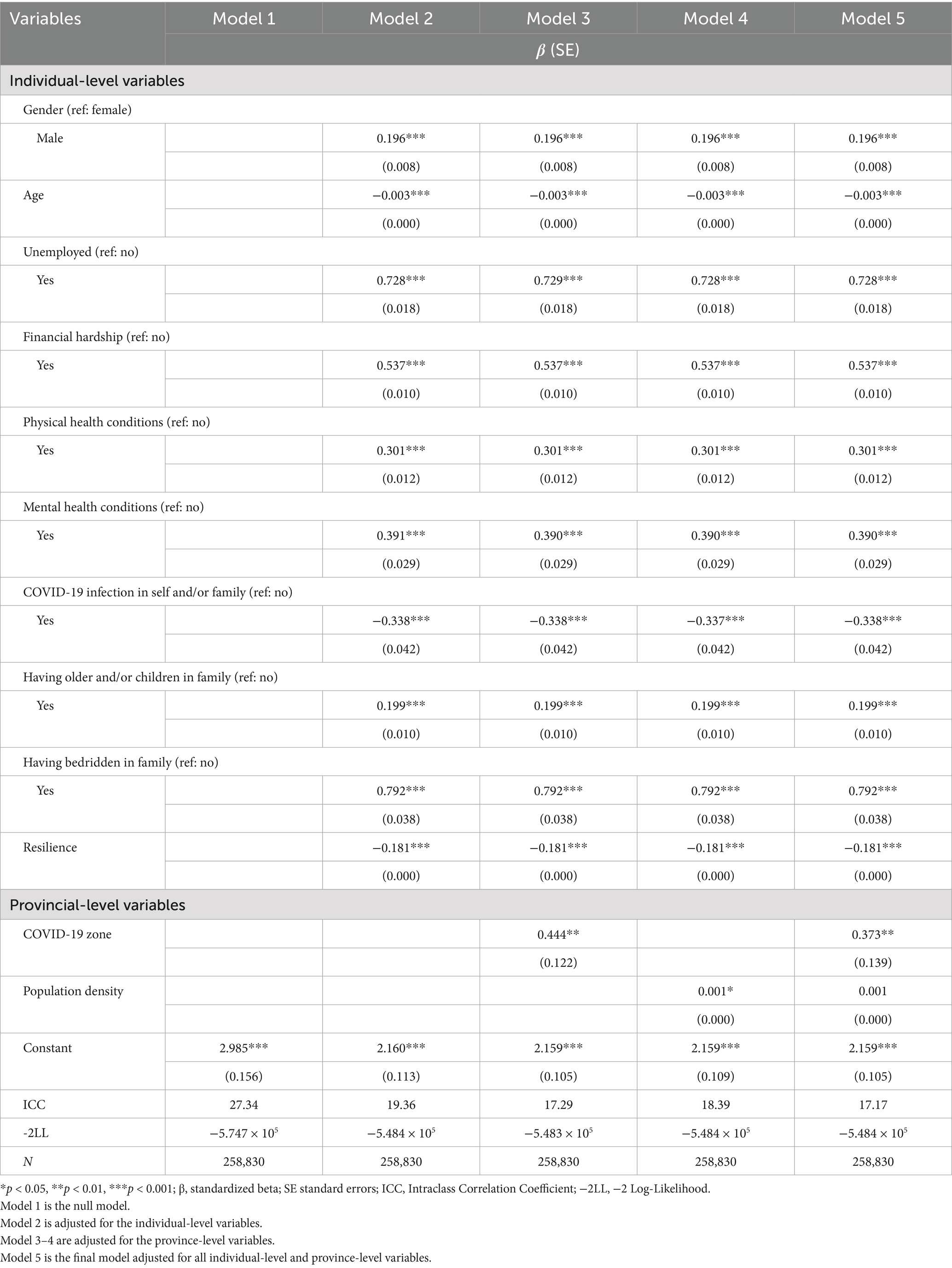
The modeling process of this study is as follows: the first step in the analysis is to estimate a null model. The null model (Model 1) is constructed, which only includes a constant term to detect potential contextual variation in stress across provinces. In Model 2, we add individual-level variables. Models 3 and 4 sequentially incorporate province-level variables. Finally, Model 5 includes all individual-level and province-level variables. Statistical significance is set at p < 0.05 for all analyses.
3 Results
3.1 Characteristic of the sample
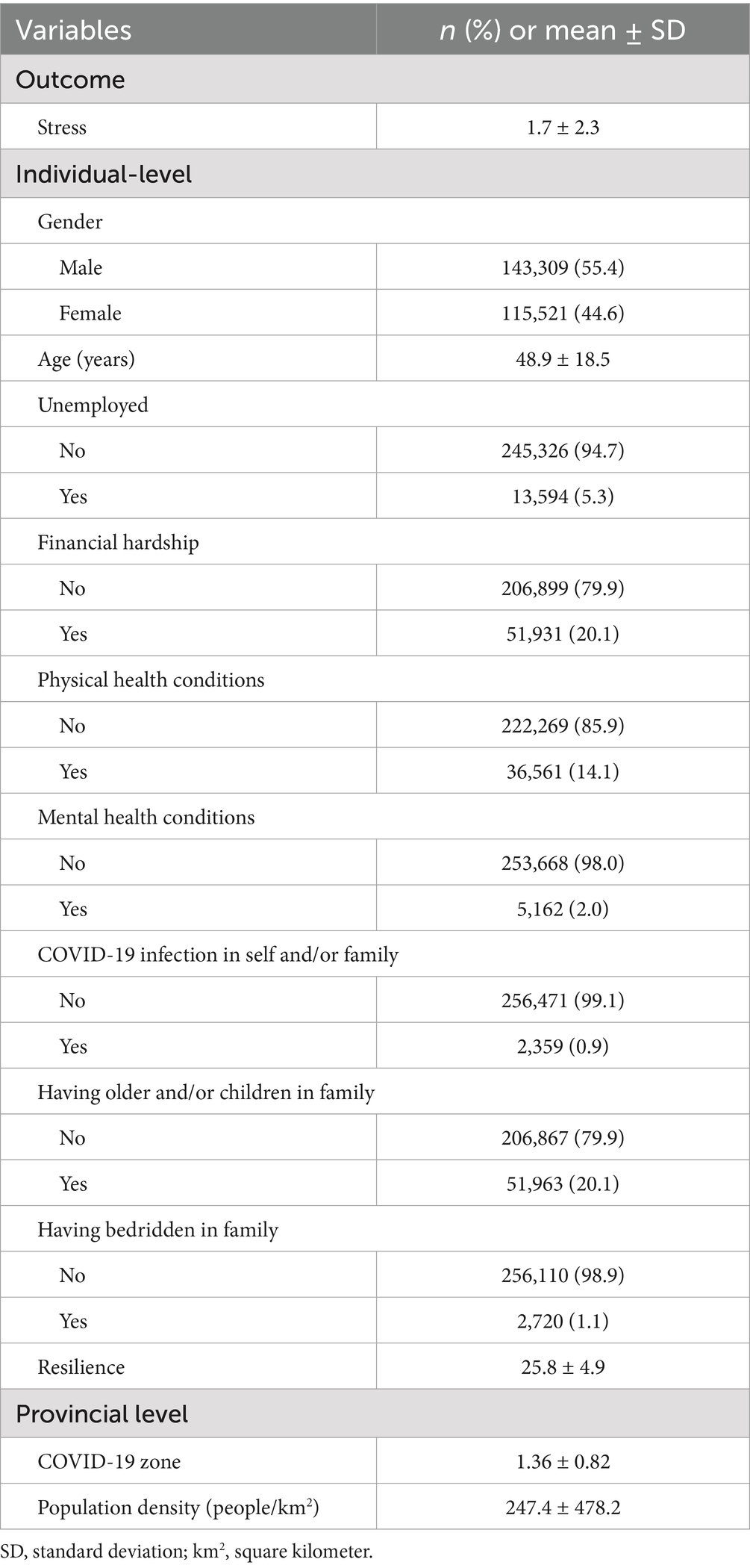
The study analyzed both individual and provincial-level variables among the 258,830 respondents. Of these 143,309 (55.4%) were male, with a mean age of 48.9 years (SD = 18.5), ranging from 18 to 99 years. The sample included 5.3% who were unemployed, 20.1% facing financial hardship, 14.1% with physical health conditions, 2.0% with mental health conditions, 0.9% from COVID-19 infection in self and/or family, 20.1% from families with older adults and children, and 1.1% with bedridden patients. The average stress score among respondents was 1.7 (from the range of 0 to 15 score), while the average resilience score was 25.8 (from the range of 3 to 30). At the provincial level, the mean COVID-19 zone score was 1.36, and the mean population density was 247.4 people/km2 (Table 1).
3.2 Multilevel analysis of stress
The multilevel analysis (Table 2) showed that in the initial model (Model 1) where the dependent variable was included. When individual-level variables were added (Model 2), the analysis showed that higher stress scores were significantly associated with being male (β = 0.196, p < 0.001), unemployed (β = 0.728, p < 0.001), experiencing financial hardship (β = 0.537, p < 0.001), having physical health conditions (β = 0.301, p < 0.001), having mental health conditions (β = 0.391, p < 0.001), having older adults and/or children in the family (β = 0.199, p < 0.001), and having bedridden patients in the family (β = 0.792, p < 0.001). In contrast, COVID-19 infection in self and/or family (β = −0.338, p < 0.001), older age (β = −0.003, p < 0.001) and higher resilience (β = −0.181, p < 0.001) were associated with lower stress scores. When provincial-level variables were added (Models 3 and 4), the results indicated that living in higher and stricter control areas was associated with higher stress scores (β = 0.444, p < 0.01). Additionally, higher population density was linked to increased stress scores (β = 0.001, p < 0.05). In the final model (Model 5), which included all individual and provincial-level variables, most remained significantly associated with stress, except for population density. The intraclass correlation coefficient value of 0.172 in this final model suggests that 17.2% of the variance in stress scores was explained by the combined effects of individual and provincial-level factors.
4 Discussion
This study was designed to examine how individual-level and provincial-level factors influenced stress among the Thai general population during the second wave of the COVID-19 pandemic by integrating the SDOH conceptual framework into a multi-level model. This study highlights the significant role of the SDOH in individuals’ stress levels during the COVID-19 pandemic, emphasizing on both individual and provincial factors in Thailand. At the individual level, sociodemographic characteristics such as gender, employment status, and financial strain were linked to higher stress, with financial hardship being a particularly important contributor. Physical and mental health conditions, along with caregiving responsibilities, further exacerbated stress, reflecting the compounded burden on vulnerable groups during the pandemic. However, resilience emerged as a crucial protective factor, reducing the impact of stress and underscoring the importance of psychological support during crises. At the provincial level, population density and COVID-19 zone classification played a significant role in influencing stress. Residents in high-density areas and regions with stricter control measures faced increased stress due to the heightened risk of virus transmission and the economic and social restrictions implemented to control the outbreak.
While multiple studies in Canada, Spain, and India reported higher stress in women than men (29–31), we found that Thai men reported higher stress than Thai women, similar to an Israeli study (32). This suggests that traditional gender roles, particularly the expectation for men to be primary financial providers, may have intensified stress during the COVID-19 pandemic. Financial hardship were a key stressor, particularly for individuals experiencing income loss, exacerbated by factors such as low savings and high consumer debt, which led to feelings of powerlessness (33, 34). Thailand’s tourism-dependent economy was especially impacted, with unemployment rates tripling during the pandemic, contributing to a surge in stress levels, especially among young adults (35–37). The link between unemployment and stress underscores the urgent need for accessible mental health services for the unemployed (38, 39). The strong link between financial insecurity, job loss, and stress emphasizes the critical need for accessible mental health services and government-led financial assistance programs to address the mental health impacts of economic instability during crises.
In addition to socioeconomic stressors, caregiving responsibilities and biological vulnerabilities also increased stress levels. Families with older adults or children faced compounded stress due to health concerns and increased caregiving demands, while family caregivers of bedridden individuals experienced significant psychological distress, often due to the loss of external support during the pandemic. Interestingly, contrary to findings from other studies (40–42), individuals in Thailand who were directly affected by COVID-19—either personally or through infected family members—reported lower stress levels compared to those without such exposure. This paradox may be explained by Thailand’s comprehensive pandemic response, which likely played a crucial role in mitigating stress. The government’s multi-faceted strategy included daily updates on COVID-19 cases and regulations through various media channels (43), the implementation of mobile applications for disease tracking (44), and the provision of extensive healthcare coverage through public health insurance programs (45). Additionally, the availability of low-cost COVID-19 insurance policies may have provided financial security, further alleviating stress among the affected population (46). Community-based initiatives were also pivotal in reducing stress. The Village Health Volunteers program, which delivered door-to-door education and support (43), and the Mental Health Crisis Assessment and Treatment Team (MCATT), which offered crucial counseling services, played key roles in offering reliable information and emotional support at the community level (8).
Our study revealed that families with older adults and children experienced higher stress levels during the COVID-19 pandemic, aligning with global trends. The increased vulnerability of older adults to severe COVID-19 outcomes resulted in heightened anxiety and stress for their caregivers (47). Simultaneously, parents faced multiple stressors, including concerns about their children’s health and the challenges of remote learning. The shift to home-based education expanded parental roles, often leading to additional financial pressures. This combination of health concerns, financial strain, and expanded educational responsibilities collectively contributed to elevated stress levels among parents (19, 48). During the pandemic, family caregivers faced additional challenges, such as restricted access to external support and growing concerns about their loved ones’ health (49). During the COVID-19 pandemic, family caregivers faced unique challenges, including restricted access to external support and heightened concerns about their loved ones’ health (50). Pandemic-related restrictions forced caregivers to adjust routines and assume new responsibilities, particularly for high-risk individuals. Research showed that during the early phase of the pandemic, family caregivers reported significantly higher levels of psychological distress and fatigue compared to non-caregivers (51–54). The increased caregiving demands, along with reduced social support, created an environment conducive to elevated stress and mental health issues. Addressing these challenges requires early psychological support for family caregivers, including timely stress assessments, flexible interventions, and establishing trust-based relationships with healthcare providers to help caregivers adapt more effectively, especially during crises like the COVID-19 pandemic.
Individuals with chronic underlying diseases experienced heightened stress, consistent with previous research linking pre-existing conditions to more severe COVID-19 cases and higher mortality rates. In Thailand, the government prioritized vaccination for seven high-risk groups, including those with diabetes, chronic respiratory disease, cardiovascular disease, chronic kidney disease, cancer, obesity, and stroke, to mitigate illness severity among these vulnerable populations. Research consistently shows that COVID-positive patients with chronic conditions, such as psoriasis, multiple sclerosis, and kidney transplant recipients, were more likely to experience higher stress levels compared to those without such conditions (55, 56). Studies from Mexico further highlighted the elevated mortality risk among COVID-19 patients with underlying health conditions, who face a fourfold increased risk of death (57). On the other hand, psychological resilience, the capacity to effectively cope with and recover from challenges, emerged as a crucial factor in mitigating stress during the pandemic (58). Similar to another study (21), we found that high resilient individuals were less likely to experience stress. This aligns with previous research showing that resilience plays a protective role against pandemic-related stress. Resilient individuals exhibited adaptive behaviors, such as recognizing health risks and adhering to preventive measures like mask-wearing (59). A study in Thailand during the early stages of the pandemic also found a link between moderate resilience and lower perceived stress (60), supporting findings from the UK where individuals either maintained resilience or recovered from initial distress within the first 6 months of the pandemic (61). These findings highlight the significant role chronic illnesses play in worsening COVID-19 outcomes and intensifying psychological stress, as individuals with such conditions are acutely aware of their heightened risk. However, the remarkable resilience observed in this study’s population demonstrates an impressive capacity to adapt and recover in the face of adversity, likely helping to mitigate many of the pandemic’s negative psychological effects.
For provincial level factors, population density has been a significant factor in COVID-19 transmission and related stress. Our study found that densely populated areas and stricter COVID control zones were associated with higher stress levels, likely due to increased risk interpersonal interactions and the combination effects of social distancing measures, movement restrictions, and reduced access to public spaces (62). Previous studies, including those from Thailand and South Korea, confirm that densely populated regions saw higher infection rates and more pronounced mental health issues (2, 63). Social isolation, reduced interactions, and limited physical activity during the pandemic further contributed to elevated stress (64, 65). Moreover, residents in densely populated areas may face ongoing challenges in readapting to post-pandemic life, such as returning to work and coping with increased traffic, which could prolong stress even as restrictions ease.
A notable strength of this study is its multilevel approach, which allows for the analysis of both individual- and provincial-level factors influencing stress during the second wave of COVID-19 in Thailand. As one of the first studies to investigate this issue in the Thai context, it provides valuable insights into the interaction between personal characteristics, such as gender, employment status, and chronic illness, and broader structural factors like population density and COVID-19 zone classifications. This approach offers a deeper understanding of how both individual vulnerabilities and environmental conditions contribute to elevated stress levels, informing targeted mental health interventions. Another strength is the use of secondary data from a nationwide mental health survey, which provided a large sample from all provinces, giving the study a comprehensive view of stress across the country. Methodologically, the study employed multilevel analysis to validate findings across different regions, providing robust evidence on factors influencing stress during the pandemic.
However, this study has several limitations. One notable limitation is its reliance on self-reported stress data, which may introduce bias due to subjective interpretation or social desirability effects. Additionally, the cross-sectional study design restricts the ability to establish causal relationships or assess changes in stress levels over time, limiting the capacity to capture the long-term psychological impact of the pandemic. Moreover, the analysis is constrained by the availability of variables in the secondary dataset, potentially omitting other significant factors influencing stress. The online nature of the survey further limits its applicability to short-term assessments, underscoring the need for future longitudinal studies to better understand the prolonged effects of COVID-19-related stress on mental health. Furthermore, the reliance on online data collection poses accessibility concerns, as not all individuals in Thailand have reliable internet access. This digital divide may result in demographic disparities between those who could participate and those who could not, potentially underrepresenting vulnerable populations, including the older adults and individuals with limited access to technology.
The study findings emphasize the need for the government to develop and implement comprehensive policies that mitigate the effects of stress on both physical and psychological well-being, particularly in preparation for future pandemics or emerging public health crises. National mental health education initiatives expanded access to remote healthcare, and integrating stress management techniques into public health programs is essential to enhancing the population’s mental health and resilience. Furthermore, creating support systems for at-risk groups—such as families with vulnerable members, frontline workers, and residents of densely populated areas—should be a priority. Policies should also mandate workplace mental health programs, provide funding for community-based mental health services, and ensure the availability of emergency psychological support during crises. By adopting these measures, governments can more effectively alleviate the adverse impacts of stress, reduce the risk of severe physical and psychological conditions, and enhance the population’s overall well-being. This approach will strengthen preparedness for future public health challenges and improve the nation’s ability to respond to unforeseen outbreaks.
Future research should prioritize establishing a robust and comprehensive national data collection plan, particularly in studying the long-term consequences of post COVID-19 conditions. This plan should include systematic and well-coordinated data gathering efforts that allow for the accurate assessment of prevalence, severity, and varied manifestations across diverse populations. To further enhance the value of research findings, it is also crucial to incorporate additional variables that influence outcomes at higher levels, such as those related to healthcare providers-level and regional-level. By examining these factors before compiling data on a national scale, researchers can gain a more detailed understanding of individuals’ access to health services across various regions, thereby enhancing the development of evidence-based public health strategies and interventions.
5 Conclusion
This study demonstrates that during Thailand’s second wave of the COVID-19 pandemic, reported stress levels among the general population were relatively low. However, stress outcomes were significantly shaped by provincial-level characteristics, including COVID-19 risk zone classifications and population density. These results highlight the necessity of integrating regional disparities into public health planning to more effectively safeguard both physical and mental well-being in future health crises. Furthermore, the findings contribute to progress toward the Sustainable Development Goals (SDGs), specifically SDG 3 (Good Health and Well-being) by reinforcing the role of mental health in holistic health promotion, and SDG 10 (Reduced Inequalities) by drawing attention to the importance of addressing geographic and social inequalities in health-related outcomes.
Data availability statement
The datasets presented in this article are not publicly available because they were obtained from the Department of Mental Health, Ministry of Public Health, Thailand, and restrictions apply to their availability. Requests to access the datasets should be directed to the corresponding author, with permission from the Department of Mental Health, Ministry of Public Health, Thailand.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
PT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TM: Conceptualization, Methodology, Visualization, Writing – original draft, Writing – review & editing. AP: Data curation, Writing – original draft, Writing – review & editing. NL: Conceptualization, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
This research project was supported by the Second Century Fund (C2F), Chulalongkorn University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Novel Coronavirus (2019-nCoV) situation reports. (2023). Available online at: https://data.who.int/dashboards/covid19/cases?n=c (accessed January 5, 2024)
2. Ruksakulpiwat, S, Zhou, W, Chiaranai, C, Saengchut, P, and Vonck, J. Age, sex, population density and COVID-19 pandemic in Thailand: a nationwide descriptive correlational study. J Health Sci Med Res. (2022) 40:281–91. doi: 10.31584/jhsmr.2021836
3. Uansri, S, Tuangratananon, T, Phaiyarom, M, Rajatanavin, N, Suphanchaimat, R, and Jaruwanno, W. Predicted impact of the lockdown measure in response to coronavirus disease 2019 (COVID-19) in greater Bangkok, Thailand, 2021. Int J Environ Res Public Health. (2021) 18:12816. doi: 10.3390/ijerph182312816
4. Rajatanavin, N, Tuangratananon, T, Suphanchaimat, R, and Tangcharoensathien, V. Responding to the COVID-19 second wave in Thailand by diversifying and adapting lessons from the first wave. BMJ Glob Health. (2021) 6:e006178. doi: 10.1136/bmjgh-2021-006178
5. Nochaiwong, S, Ruengorn, C, Awiphan, R, Ruanta, Y, Boonchieng, W, Nanta, S, et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine. (2020) 99:e20751. doi: 10.1097/md.0000000000020751
6. Pothisiri, W, and Vicerra, PMM. Psychological distress during COVID-19 pandemic in low-income and middle-income countries: a cross-sectional study of older persons in Thailand. BMJ Open. (2021) 11:e047650. doi: 10.1136/bmjopen-2020-047650
7. Tantirattanakulchai, P, Hounnaklang, N, Pongsachareonnont, PF, Khambhiphant, B, Hounnaklang, S, Win, N, et al. Impact of COVID-19 on depressive symptoms among patients with low vision and blindness. Clin Ophthalmol. (2023) 17:789–96. doi: 10.2147/opth.S401714
8. Ministry of Public Health (MOPH). (2021). Strategic plan: COVID-19; Strategy: Managing the new wave of the COVID-19 Epidemic. Available online at: https://ddc.moph.go.th/viralpneumonia/eng/file/main/en_Thailand%20Covid-19%20plan_MOPH_2021.pdf (accessed 3 January, 2024)
9. World Health Organization. Social determinants of health. (2024). Available online at: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (accessed July 14 2024)
10. Marmot, M. Social determinants of health inequalities. Lancet. (2005) 365:1099–104. doi: 10.1016/s0140-6736(05)71146-6
11. Tay, WWY, Jesuthasan, J, Wan, KS, Ong, T, and Mustapha, F. Eighteen months into the COVID-19 pandemic: the prevalence of depression, anxiety, and stress symptoms in Southeast Asia and the associated demographic factors. Front Public Health. (2022) 10:863323. doi: 10.3389/fpubh.2022.863323
12. Acharya, S, Sharma, S, and Bhatta, J. An online survey of factors associated with self-perceived stress during the initial stage of the COVID-19 outbreak in Nepal. Ethiop J Health Dev. (2020) 34:84–9.
13. Gayatri, M, and Puspitasari, MD. The impact of COVID-19 pandemic on family well-being: a literature review. Fam J. (2022) 31:606–13. doi: 10.1177/10664807221131006
14. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
15. Braveman, P, and Gottlieb, L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. (2014) 129:19–31. doi: 10.1177/00333549141291s206
16. Cockerham, WC, Hamby, BW, and Oates, GR. The social determinants of chronic disease. Am J Prev Med. (2017) 52:S5–S12. doi: 10.1016/j.amepre.2016.09.010
17. Kittiprapas, S. Socioeconomic impacts of the COVID-19 pandemic on the vulnerable households: empirical evidence from slum areas of Bangkok city. Cogent Soc Sci. (2022) 8:2074111. doi: 10.1080/23311886.2022.2074111
18. Singhal, S, Kumar, P, Singh, S, Saha, S, and Dey, AB. Clinical features and outcomes of COVID-19 in older adults: a systematic review and meta-analysis. BMC Geriatr. (2021) 21:321. doi: 10.1186/s12877-021-02261-3
19. Lebow, JL. The challenges of COVID-19 for divorcing and post-divorce families. Fam Process. (2020) 59:967–73. doi: 10.1111/famp.12574
20. Kermott, CA, Johnson, RE, Sood, R, Jenkins, SM, and Sood, A. Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS One. (2019) 14:e0218092. doi: 10.1371/journal.pone.0218092
21. Vannini, P, Gagliardi, GP, Kuppe, M, Dossett, ML, Donovan, NJ, Gatchel, JR, et al. Stress, resilience, and coping strategies in a sample of community-dwelling older adults during COVID-19. J Psychiatr Res. (2021) 138:176–85. doi: 10.1016/j.jpsychires.2021.03.050
22. Kadi, N, and Khelfaoui, M. Population density, a factor in the spread of COVID-19 in Algeria: statistic study. Bull Natl Res Cent. (2020) 44:138. doi: 10.1186/s42269-020-00393-x
23. Department of Disease Control Thaialnd. The coronavirus disease 2019 situation by emergency operation center, Department of Disease Control. (2020). Available online at: https://ddc.moph.go.th/viralpneumonia/eng/situation_more.php (accessed January 2, 2024)
24. Aiewsakun, P, Jamsai, B, Phumiphanjarphak, W, Sawaengdee, W, Palittapongarnpim, P, and Mahasirimongkol, S. Spatiotemporal evolution of SARS-CoV-2 in the Bangkok metropolitan region, Thailand, 2020-2022: implications for future outbreak preparedness. Microb Genom. (2023) 9:001170. doi: 10.1099/mgen.0.001170
25. Department of Provincial Administration Thailand. Official statstics registration sytstems (2020). Available online at: https://stat.bora.dopa.go.th/stat/statnew/statMenu/newStat/sumyear.php (accessed December 5, 2023)
26. Neti, N, Pimsri, A, Boonsopon, S, Tesavibul, N, and Choopong, P. Triggering factors associated with a new episode of recurrent acute anterior uveitis. Sci Rep. (2021) 11:12156. doi: 10.1038/s41598-021-91701-6
28. Dechkhong, TKP, Tipchot, T, and Wuttihan, P. Reliability and validity of resilience inventory 3-item version. J Mental Health Thai. (2022) 30:297–306.
29. Arcand, M, Bilodeau-Houle, A, Juster, RP, and Marin, MF. Sex and gender role differences on stress, depression, and anxiety symptoms in response to the COVID-19 pandemic over time. Front Psychol. (2023) 14:1166154. doi: 10.3389/fpsyg.2023.1166154
30. Bethencourt, JM, and Estefanía Lorenzo, D. Stressful events, psychological distress and well-being during the second wave of COVID-19 pandemic in Spain: a gender analysis. Appl Res Qual Life. (2022) 18:1–29. doi: 10.1007/s11482-022-10140-1
31. Afridi, F, Dhillon, A, and Roy, S. The gendered crisis: livelihoods and well-being in India during COVID-19. Fem Econ. (2023) 29:40–74. doi: 10.1080/13545701.2023.2186461
32. Levy, I. Stress, anxiety, and depression in times of COVID-19: gender, individual quarantine, pandemic duration and employment. Front Public Health. (2022) 10:999795. doi: 10.3389/fpubh.2022.999795
33. Khademian, F, Delavari, S, Koohjani, Z, and Khademian, Z. An investigation of depression, anxiety, and stress and its relating factors during COVID-19 pandemic in Iran. BMC Public Health. (2021) 21:275. doi: 10.1186/s12889-021-10329-3
34. Simonse, O, Van Dijk, WW, Van Dillen, LF, and Van Dijk, E. The role of financial stress in mental health changes during COVID-19. Npj Ment Health Res. (2022) 1:15. doi: 10.1038/s44184-022-00016-5
35. Open Development Thailand. (2020). COVID-19 impact on Thai Labor market. Available online at: https://thailand.opendevelopmentmekong.net/topics/covid-19-impact-on-thai-labor-market/#ref-10227-1 (accessed June 15, 2024)
36. Mojtahedi, D, Dagnall, N, Denovan, A, Clough, P, Hull, S, Canning, D, et al. The relationship between mental toughness, job loss, and mental health issues during the COVID-19 pandemic. Front Psych. (2020) 11:607246. doi: 10.3389/fpsyt.2020.607246
37. Ganson, KT, Tsai, AC, Weiser, SD, Benabou, SE, and Nagata, JM. Job insecurity and symptoms of anxiety and depression among U.S. young adults during COVID-19. J Adolesc Health. (2021) 68:53–6. doi: 10.1016/j.jadohealth.2020.10.008
38. Mamun, MA, Akter, S, Hossain, I, Faisal, MTH, Rahman, MA, Arefin, A, et al. Financial threat, hardship and distress predict depression, anxiety and stress among the unemployed youths: a Bangladeshi multi-city study. J Affect Disord. (2020) 276:1149–58. doi: 10.1016/j.jad.2020.06.075
39. de Miquel, C, Domènech-Abella, J, Felez-Nobrega, M, Cristóbal-Narváez, P, Mortier, P, Vilagut, G, et al. The mental health of employees with job loss and income loss during the COVID-19 pandemic: the mediating role of perceived financial stress. Int J Environ Res Public Health. (2022) 19:3158. doi: 10.3390/ijerph19063158
40. Prakash, J, Dangi, A, Chaterjee, K, Yadav, P, Srivastava, K, and Chauhan, VS. Assessment of depression, anxiety and stress in COVID-19 infected individuals and their families. Med J Armed Forces India. (2021) 77:S424–9. doi: 10.1016/j.mjafi.2021.06.013
41. Saeed, BA, Ismael, SK, Amin, RM, Mahmud, NM, Al-Banna, DA, and Shabila, NP. Prevalence and determinants of anxiety and stress in the general population during COVID-19 pandemic in Iraq: a cross-sectional study. PLoS One. (2023) 18:e0283260. doi: 10.1371/journal.pone.0283260
42. Rodríguez-Rey, R, Garrido-Hernansaiz, H, and Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. (2020) 11:1540. doi: 10.3389/fpsyg.2020.01540
43. Marome, W, and Shaw, R. COVID-19 response in Thailand and its implications on future preparedness. Int J Environ Res Public Health. (2021) 18:1089. doi: 10.3390/ijerph18031089
44. Chuenyindee, T, Ong, AKS, Prasetyo, YT, Persada, SF, Nadlifatin, R, and Sittiwatethanasiri, T. Factors affecting the perceived usability of the COVID-19 contact-tracing application "Thai Chana" during the early COVID-19 omicron period. Int J Environ Res Public Health. (2022) 19:4383. doi: 10.3390/ijerph19074383
45. Tangcharoensathien, V, Sachdev, S, Viriyathorn, S, Sriprasert, K, Kongkam, L, Srichomphu, K, et al. Universal access to comprehensive COVID-19 services for everyone in Thailand. BMJ Glob Health. (2022) 7:e009281. doi: 10.1136/bmjgh-2022-009281
46. Phoonphingphiphat, A. (2022). Thai insurers sink into bankruptcy due to COVID claims. Available online at: https://asia.nikkei.com/Spotlight/Coronavirus/Thai-insurers-sink-into-bankruptcy-due-to-COVID-claims (accessed June 1, 2024)
47. Brooke, J, and Jackson, D. Older people and COVID-19: isolation, risk and ageism. J Clin Nurs. (2020) 29:2044–6. doi: 10.1111/jocn.15274
48. Patrick, SW, Henkhaus, LE, Zickafoose, JS, Lovell, K, Halvorson, A, Loch, S, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. (2020) 146:e2020016824. doi: 10.1542/peds.2020-016824
49. Bekdemir, A, and Ilhan, N. Predictors of Caregiver Burden in Caregivers of Bedridden Patients. J Nurs Res. (2019) 27:e24. doi: 10.1097/jnr.0000000000000297
50. Irani, E, Niyomyart, A, and Hickman, RL Jr. Family caregivers' experiences and changes in caregiving tasks during the COVID-19 pandemic. Clin Nurs Res. (2021) 30:1088–97. doi: 10.1177/10547738211014211
51. Park, SS. Caregivers' mental health and somatic symptoms during COVID-19. J Gerontol B Psychol Sci Soc Sci. (2021) 76:e235–40. doi: 10.1093/geronb/gbaa121
52. Truskinovsky, Y, Finlay, JM, and Kobayashi, LC. Caregiving in a pandemic: COVID-19 and the well-being of family caregivers 55+ in the United States. Med Care Res Rev. (2022) 79:663–75. doi: 10.1177/10775587211062405
53. Borges-Machado, F, Barros, D, Ribeiro, Ó, and Carvalho, J. The effects of COVID-19 home confinement in dementia care: physical and cognitive decline, severe neuropsychiatric symptoms and increased caregiving burden. Am J Alzheimers Dis Other Dement. (2020) 35:1533317520976720. doi: 10.1177/1533317520976720
54. Irani, E, Niyomyart, A, and Zauszniewski, JA. Caregiving stress and self-rated health during the COVID-19 pandemic: the mediating role of resourcefulness. Issues Ment Health Nurs. (2021) 42:982–8. doi: 10.1080/01612840.2021.1924324
55. Sukumaran, S, and Achambattu, S. Assessment of depression, anxiety, and stress in COVID-19-positive patients with chronic illness – a comparative study. Natl J Physiol Pharm Pharmacol. (2023) 13:1293–8. doi: 10.5455/njppp.2023.13.04220202302052023
56. Łuc, M, Pawłowski, M, Jaworski, A, Fila-Witecka, K, Szcześniak, D, Augustyniak-Bartosik, H, et al. Coping of chronically-ill patients during the COVID-19 pandemic: comparison between four groups. Int J Environ Res Public Health. (2023) 20:4814. doi: 10.3390/ijerph20064814
57. Choi, WY. Mortality rate of patients with COVID-19 based on underlying health conditions. Disaster Med Public Health Prep. (2021) 16:2480–5. doi: 10.1017/dmp.2021.139
58. American Psychological Association. (2014). The road to resilience. Available online at: https://www.apa.org/topics/resilience (accessed June 8, 2024)
59. Álvarez, MA, and Pinto, NS. Experiential COVID-19 factors predicting resilience among Spanish adults. BMC Psychol. (2023) 11:118. doi: 10.1186/s40359-023-01131-4
60. Ruengorn, C, Awiphan, R, Phosuya, C, Ruanta, Y, Wongpakaran, N, Wongpakaran, T, et al. Psychological resilience and adverse mental health issues in the Thai population during the coronavirus disease 2019 pandemic. Int J Environ Res Public Health. (2022) 19:13023. doi: 10.3390/ijerph192013023
61. Pierce, M, McManus, S, Hope, H, Hotopf, M, Ford, T, Hatch, SL, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. (2021) 8:610–9. doi: 10.1016/s2215-0366(21)00151-6
62. Bhadra, A, Mukherjee, A, and Sarkar, K. Impact of population density on Covid-19 infected and mortality rate in India. Model Earth Syst Environ. (2021) 7:623–9. doi: 10.1007/s40808-020-00984-7
63. Min, J, Kwon, D, Lee, W, Kang, C, Park, C, Heo, S, et al. Individual and regional characteristics associated with changes in mental health before and during the COVID-19 pandemic in South Korea. Sci Rep. (2022) 12:14189. doi: 10.1038/s41598-022-18493-1
64. Loades, ME, Chatburn, E, Higson-Sweeney, N, Reynolds, S, Shafran, R, Brigden, A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–39.e3. doi: 10.1016/j.jaac.2020.05.009
65. Chekroud, SR, Gueorguieva, R, Zheutlin, AB, Paulus, M, Krumholz, HM, Krystal, JH, et al. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. (2018) 5:739–46. doi: 10.1016/s2215-0366(18)30227-x
Keywords: stress, COVID-19, individual-level, provincial-level, multilevel analysis, Thailand
Citation: Tantirattanakulchai P, Hounnaklang N, Mahaprom T, Polrak A and Lukkahatai N (2025) Effect of individual and provincial levels on stress among general population during the COVID-19 pandemic: a multilevel analysis using mental health survey in Thailand. Front. Public Health. 13:1587819. doi: 10.3389/fpubh.2025.1587819
Edited by:
Aliya Naheed, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), BangladeshReviewed by:
Saranraj Loganathan, Mepco Schlenk Engineering College, IndiaMiguel Vasconcelos Da Silva, King's College London, United Kingdom
Copyright © 2025 Tantirattanakulchai, Hounnaklang, Mahaprom, Polrak and Lukkahatai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nuchanad Hounnaklang, TnVjaGFuYWQuSEBjaHVsYS5hYy50aA==
 Pankaew Tantirattanakulchai
Pankaew Tantirattanakulchai Nuchanad Hounnaklang1*
Nuchanad Hounnaklang1* Tiwa Mahaprom
Tiwa Mahaprom Nada Lukkahatai
Nada Lukkahatai