- 1Fuzhou Center for Disease Control and Prevention, Affiliated with Fujian Medical University, Fuzhou, China
- 2Gulou District Center for Disease Control and Prevention, Fuzhou, China
- 3Fuqing Center for Disease Control and Prevention, Fuzhou, China
- 4Minqing County Center for Disease Control and Prevention, Fuzhou, China
- 5Yongtai County Center for Disease Control and Prevention, Fuzhou, China
Background: Children are vulnerable to influenza virus due to their developing immune systems, particularly children aged 6 months-5 years (preschool children). To improve the uptake of influenza vaccine in preschool children, it is important to determine the influencing factors of Chinese parents/guardians’ (P/Gs) intention and behavior for children to receive. We implemented an investigation to determine coverage of influenza vaccination in preschool children and the influencing factors of being vaccinated against influenza among preschool children in Fuzhou.
Methods: This is a cross-sectional study. Using a hierarchical approach, based on the coverage of influenza vaccination in preschool children, the 12 districts/counties in Fuzhou were divided into two levels. In each level, two urban districts and two counties were selected, including 2 randomly selected vaccination clinics and 2 kindergartens. A standardized anonymous questionnaire was used to collect information on P/Gs. Chi-square testing and multivariate logistic regression were used to analyze factors that may be associated with influenza.
Results: The coverage rate of influenza vaccination was 7.38% among preschool children in 2022 in Fuzhou City. A total of 8,768 guardians completed the questionnaire. 54.70% of the responders had received at least one dose of flu. Only 23.56% of the P/Gs involved were able to correctly list the influenza clinical feature. Higher education status had higher coverage (p-values < 0.05). Multivariate analysis showed birth order [odds ratio (OR) = 0.76, 95% confidence interval (CI): 0.63, 0.92], medical insurance [OR = 1.42, 95% CI: 1.22, 1.65], occupation [OR = 0.84, 95% CI: 0.75, 0.93], average monthly household income ≥ 10,000 [OR = 0.66, 95% CI: 0.56, 0.79], vaccine prices > 200 [OR = 1.66, 95% CI: 1.41, 1.97], and total duration of each vaccination session [OR = 0.49, 95% CI: 0.42, 0.58] were associated with flu vaccination.
Conclusion: Influenza vaccination coverage among preschoolers was low, and parental/guardian knowledge regarding influenza prevention was inadequate. Enhanced awareness, vaccine understanding, and recommendation policies correlated with higher coverage. Authorities should implement sustainable financing and incentives to ensure access and affordability, while promoting education to convert vaccination intentions into actual uptake.
Introduction
Influenza remains a major cause of morbidity, mortality, and economic burden worldwide each year. There are approximately 1 billion cases of influenza worldwide each year, of which 3 to 5 million are severe cases, resulting in 290,000–650,000 deaths globally (1). Children are relatively immunologically naive to influenza virus, leading to increased morbidity on infection (2). Among children under 5 years globally, there were an estimated one hundred million influenza virus episodes, and results in a substantial burden on health services worldwide (3). Lai et al. (4) indicated that the average economic burden of children due to influenza-like illness was 1,647 yuan (237.2 dollars) per episode, and the indirect economic burden due to the loss of caregivers’ labor time also was fairly large. The estimated overall attack rate in China was reported to be approximately 5.5% in all age groups, with the highest attack rate observed in 0–4 years old preschool children (31.9%). However, influenza vaccination coverage among children in China is low, remaining at approximately 25% (5).
World Health Organization (WHO) and European Union targets for immunization rates for at-risk populations are 75% (6). Both the Advisory Committee on Immunization Practices and Chinese Center for Disease Control and Prevention were simultaneously recommending universal influenza vaccination for preschool children (between the ages of 6 and 59 months), as well as those with high-risk conditions (7, 8). Vaccinating children against influenza could not only protect children themselves but also protect the whole community and reduce influenza incidence in the general population (9).
Parents/guardians (P/Gs) are the primary decision-makers for all family behaviors, it is critical to understand the factors that influence P/Gs’ intentions to vaccinate their children. Low MSF’s article showed that P/Gs’ willingness to vaccinate is a strong predictor of child influenza vaccination (10). Thus, a comprehensive survey of P/Gs is warranted to assess vaccination willingness and identify potential determinants influencing their decision-making.
In order to better control the influenza prevalent among preschool children, Fuzhou Health Commission and Fuzhou Center for Disease Control and Prevention provide health reminders and recommend getting vaccinated against influenza each year. However, the actual vaccination willingness of preschool children and the factors influencing their vaccination remain unclear. During 2022 through 2023, we conducted a field investigation to evaluate the knowledge, attitudes of P/Gs regarding this influenza vaccination, and assess their status of influenza vaccination. This study was designed to identify factors affecting influenza vaccination among preschool children and provide evidence increasing influenza vaccination rates among preschool children.
Methods
Study design and setting
Data on influenza vaccinations of children aged 6 months-5 years (preschool children) in 2022 were obtained from the Fujian Province Immunization Information System, which contains vaccination data for all citizens living in Fuzhou. Population data used in this study were obtained from the China Information System for Disease Control and Prevention.
Setting and subjects
Fuzhou area is made of 12 urban districts (counties). Based on the coverage of influenza vaccination in preschool children, the 12 districts/counties in Fuzhou were divided into two levels A and B (A: high coverage rate > 8.0%; B: low coverage rate < 8.0%) In each level, two urban districts and two counties were selected, including 2 randomly selected vaccination clinics and 2 kindergartens. There was no specific influenza vaccination campaign during the investigation period. At least 2,700 P/Gs of preschool children were investigated in each level. P/Gs who were unwilling to participate in the study and children with contraindications of influenza vaccines were excluded.
Data collection
A standardized anonymous questionnaire designed specifically for the study was used to collect information, including fundamental demographic details concerning the infants and their families (sex, age, household composition, education status of the P/Gs, health status of children, health insurance status, P/Gs occupation, average monthly household income, birth information of children), influenza vaccination status of children, health-related beliefs and attitudes to influenza vaccination knowledge to influenza and influenza vaccination, and the demand for vaccination services (trust and satisfaction with vaccination staff, schedule of clinics, medical service environment). The questionnaire was distributed by investigators, filled in, and retrieved immediately at the field.
Data analysis
Knowledge of influenza and influenza vaccination: Assign 1 point to each question, 1 point for correct answers, and 0 points for errors, the total score is 14. The scores were categorized into three groups: 0–5 unknown, 6–10 general know, 11–14 good know, with a hierarchy describing the respondent’s state of knowledge. We established a database for analysis with SPSS version 26.0. Coverage of influenza vaccination, demographics, knowledge about influenza and influenza vaccination, and health-related beliefs and attitudes to influenza vaccination were analyzed descriptively. Chi-square testing and multivariate logistic regression were used to analyze factors that may be associated with influenza vaccination. We used a 2-tail p-value (p) significance level of 0.05.
Results
Vaccination rates for flu in Fuzhou
Data obtained from the Fujian province immunization information system showed the total coverage of influenza vaccination (at least one dose) among preschool children in 2022 was 7.38%. The coverage was between 4.38–10.76% among 12 urban districts (counties). The coverage of influenza vaccination in preschool children among A (8.77%) was higher than in level B (6.10%) (p < 0.05).
Demographic characteristics
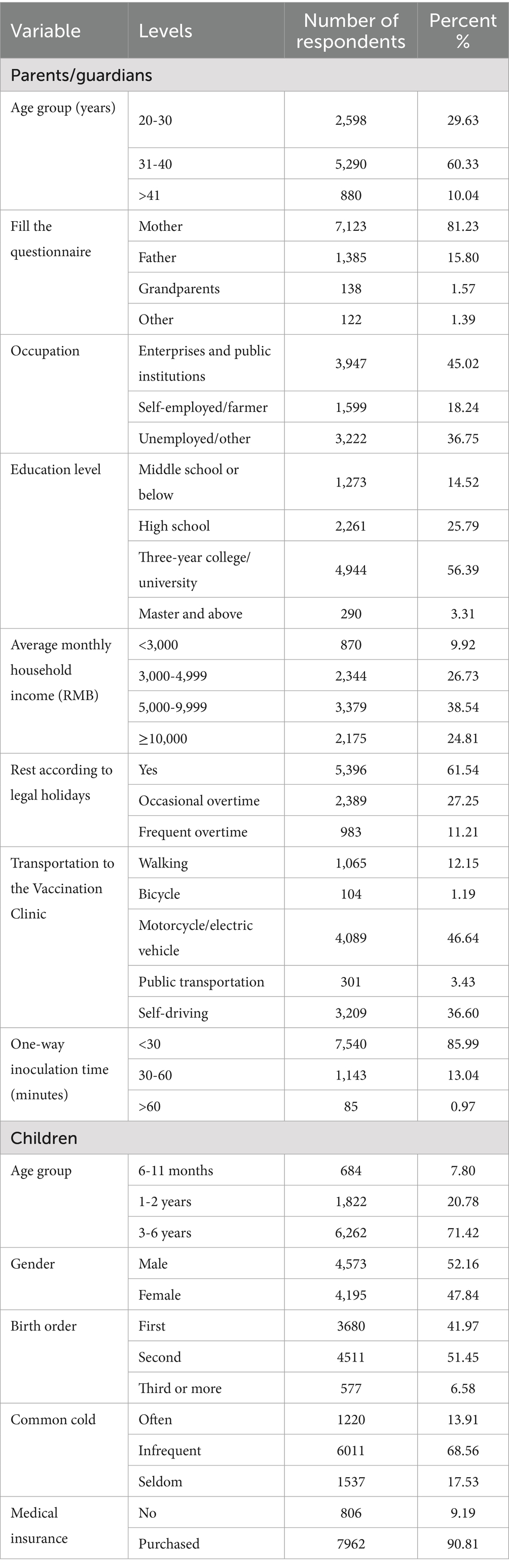
A total of 8,768 P/Gs were surveyed, their median age was 33 years (range: 20–99), and most participants were mothers (81.23%). According to occupational categorization, 45.02% of the respondents were enterprises and institutions, 59.39% were three-year college/university, and 61.54% had legal holidays.
7.80% (684) were 6–11 months children, 20.78% (1,822) were between 1–2 years, 71.42% (6,262) were 3–6 years, 52.16% (4,573) were males. 51.45% of these were from the second birth, 90.81% had health insurance. Demographics and other characteristics are illustrated in Table 1.
Knowledge regarding influenza
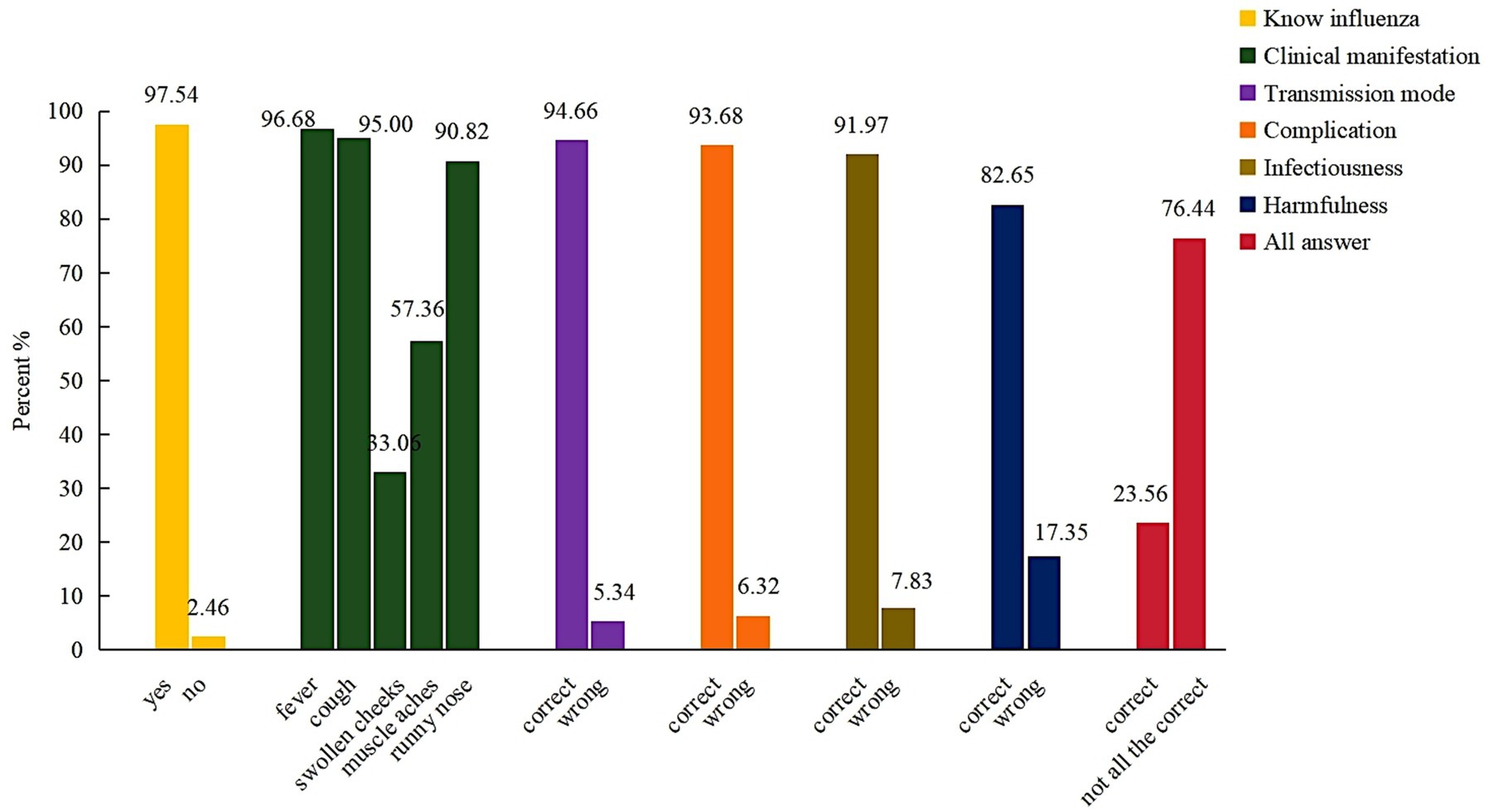
Almost all of the respondents (97.54%) answered they knew the flu, however, 23.56% of the P/Gs involved were able to correctly list the influenza clinical feature. And the percentage with correct knowledge of transmission mode, complication, and the infectiousness of influenza were 94.66, 93.68, and 91.97%, respectively (Figure 1).
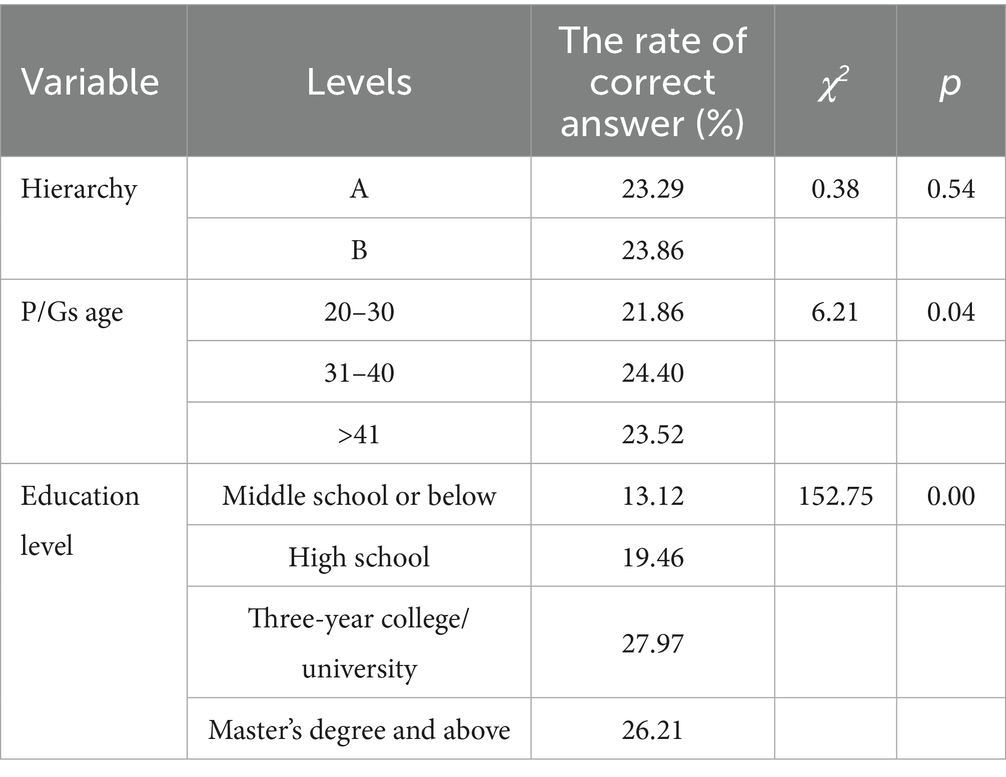
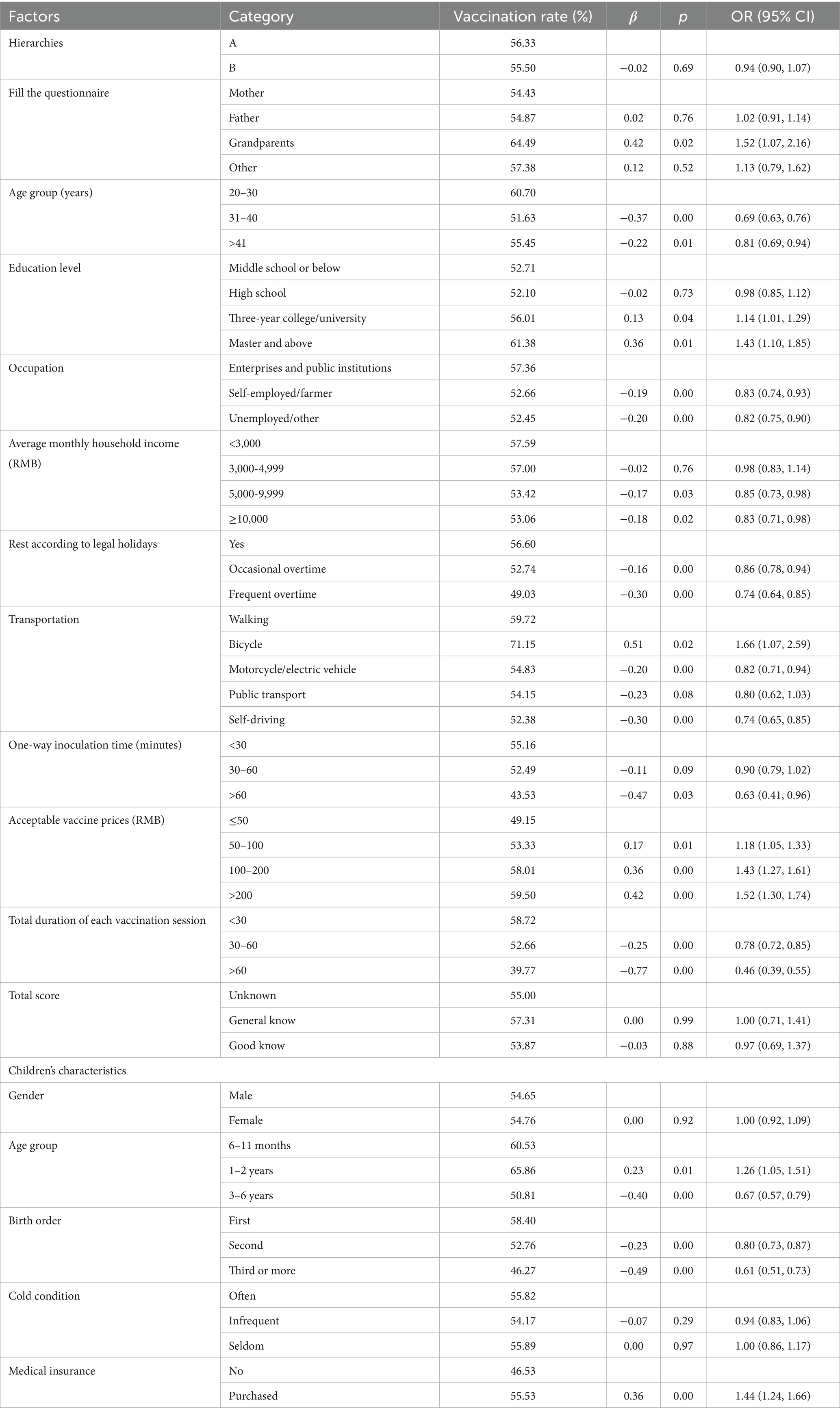
31–40 years old P/Gs had better knowledge about influenza than younger P/Gs and older P/Gs (24.40, 21.86, and 23.52%, respectively, p < 0.05). When we compared the education status, there were differences among P/Gs, 28% of P/Gs with Three-year college/university and above had answered correctly, which was higher than those with a high school education (19.46%) and middle school or below (13.12%; p < 0.05) (Table 2).
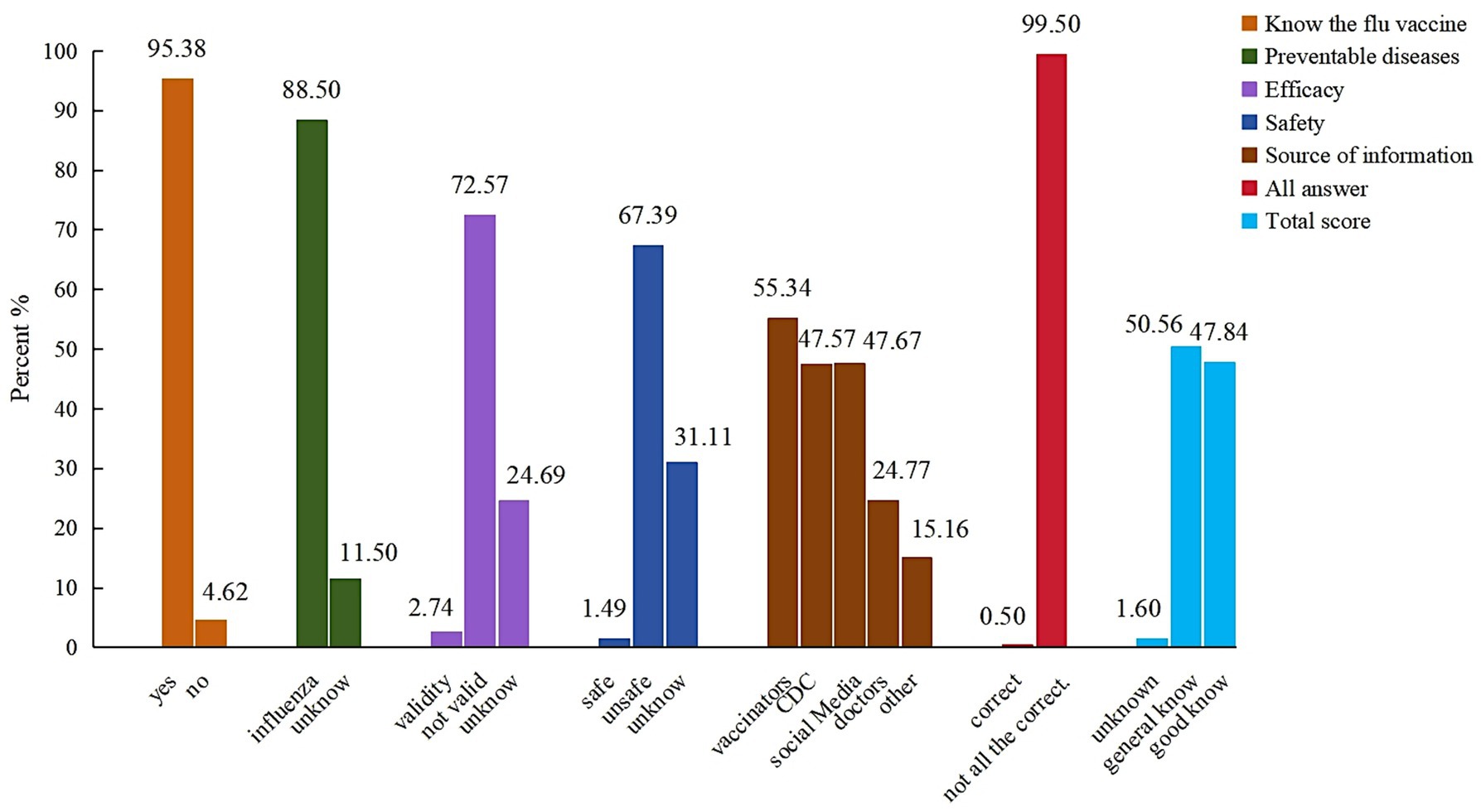
Influenza vaccination and vaccination rates for flu
Figure 2 showed almost P/Gs knew the flu vaccine (95.38%), and knew that it protects against the flu (88.50%). However, only 1.49% P/Gs and 2.74% P/Gs answered “YES” about the safety and effectiveness of the influenza vaccine. When asked about the source of knowledge of flu vaccine, the main source of information about flu was vaccinators (55.34%), followed by Center for Disease Control and Prevention (CDC) (47.57%), and social media (47.67%).
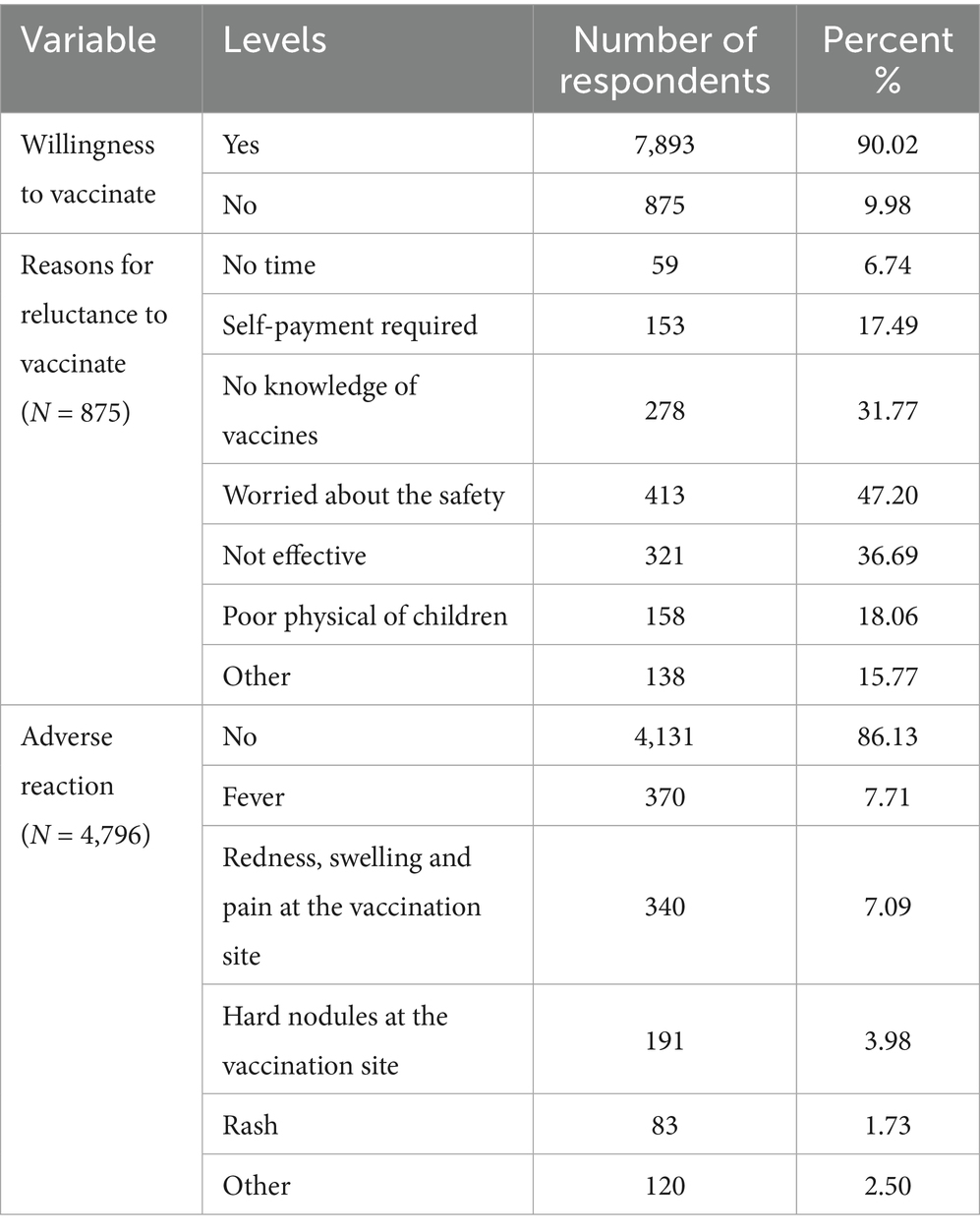
Table 3 showed that almost all of P/Gs were willing to vaccinate against influenza (90.02%), main reasons for refusing the flu vaccine were concerns about the safety (47.20%), not effective (36.69%), no knowledge of vaccines (31.77%), and adverse reactions have occurred of the influenza vaccine (13.87%).
Factors associated with influenza uptake
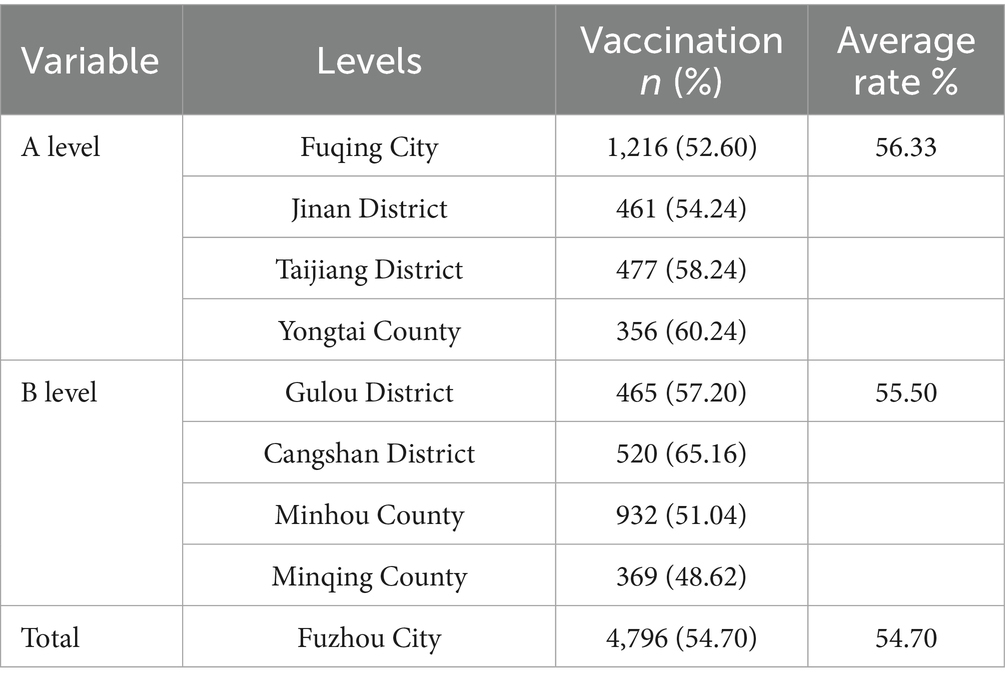
Among preschool children respondents, 4,796 (54.70%) had received at least one dose of flu vaccine (Table 4).
The coverage rate of preschool children was no significant difference between strata A and B (56.33 and 55.50%, p > 0.05). 20–30 years old (60.70%) have higher vaccination rate for their children than 31–40 years old (51.63%) and older P/Gs (55.45%) (p < 0.05). The higher the education level of parents, the higher the flu vaccination rate of their children (the detailed data are in Tables 5, p < 0.05). The P/Gs working in state enterprises and public institutions (57.36%) had higher coverage for their children than self-employed/farmer (52.66%) and unemployed/other occupations (52.45%, p < 0.05). However, when we compared the household income, it showed the lower household income had higher coverage rate (p < 0.05). Total duration of each vaccination session < 30 min (58.72%) had a higher vaccination rate than 30–60 (52.66%) and > 60 (39.77%, p < 0.05) (Table 5).
Summary of children characteristics is shown in Table 5. 1–2 years old had higher vaccination rate than 6–11 months and 3–6 years old (65.86, 60.53, and 50.81%, respectively, p < 0.05). Furthermore, the first-born child had a higher vaccination rate than second-born and born later (58.40, 52.76, and 46.27%, respectively, p < 0.05). The coverage of preschool children with medical insurance was higher than that of children without (55.53 and 46.53%, respectively, p < 0.05).
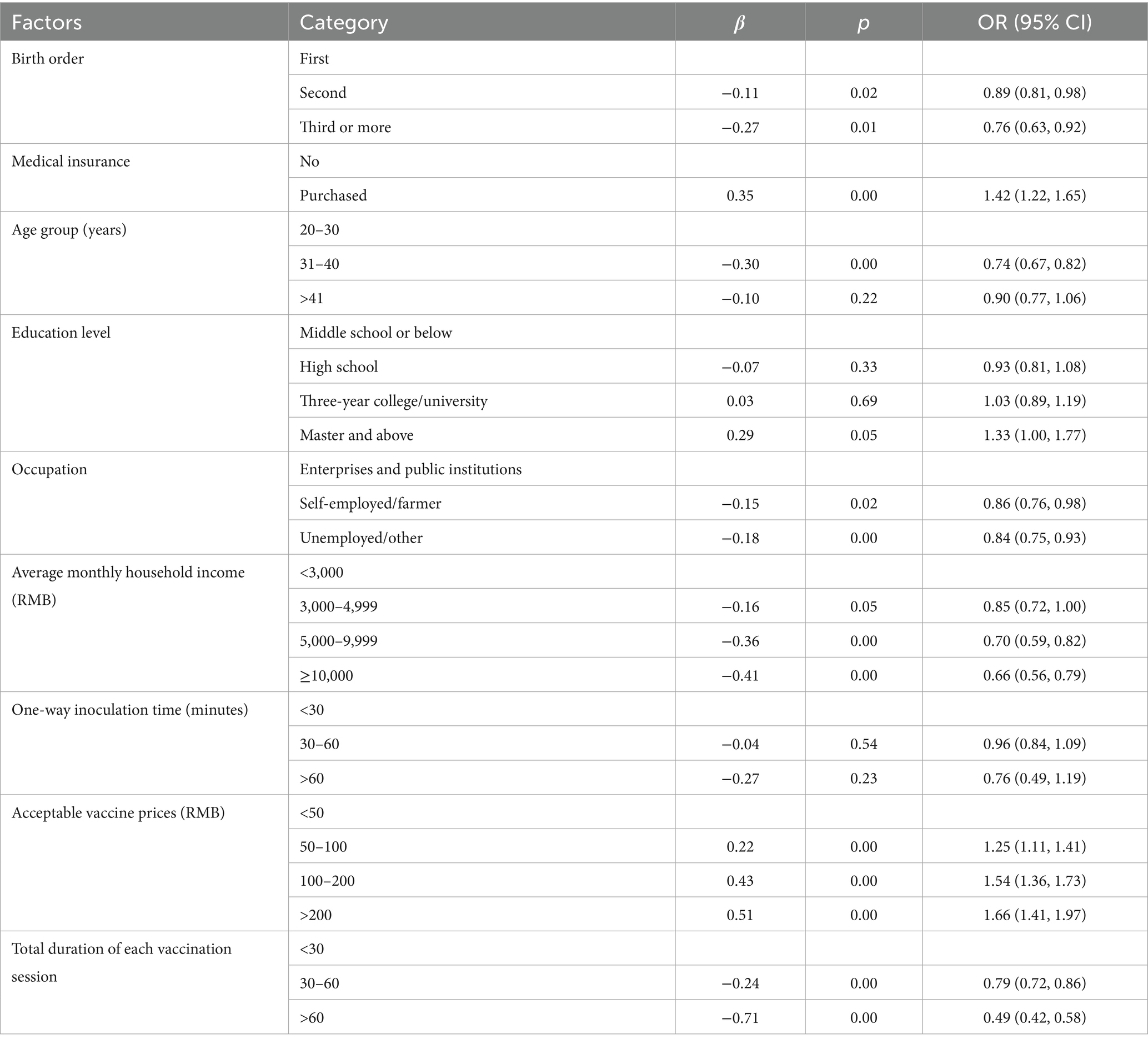
The multivariate analysis of factors influencing flu vaccination showed that children’s birth order, medical insurance, P/G’s occupation, average monthly household income, vaccine prices, and total duration of each vaccination session were associated with flu vaccination.
Children birthed third or late [odds ratio (OR) = 0.76, 95% confidence interval (CI): 0.63, 0.92]; medical insurance [OR = 1.42, 95% CI: 1.22, 1.65]; P/Gs occupation [OR = 0.86, 95% CI: 0.76, 0.98 and OR = 0.84, 95% CI: 0.75, 0.93]; average monthly household income ≥ 10,000 [OR = 0.66, 95% CI: 0.56, 0.79]; acceptable vaccine prices > 200 [OR = 1.66, 95% CI: 1.41, 1.97]; total duration of each vaccination session > 60 min [OR = 0.49, 95% CI: 0.42, 0.58] (Table 6).
Discussion
Our study showed the total coverage of influenza vaccination (at least one dose) among preschool children in 2022 was 7.38%. The coverage was between 4.38–10.76% among 12 urban districts (counties). 31–40 years old P/Gs had better knowledge about influenza than younger P/Gs and older P/Gs (24.40, 21.86, and 23.52%, respectively, p < 0.05), but almost P/Gs were unaware of the safety and effectiveness of the influenza vaccine. This investigation showed children’s age, birth order, medical insurance, P/G’s age, occupation, average monthly household income, overtime work, transportation, vaccine prices, and total duration of each vaccination session were associated with flu vaccination.
Data obtained from the Fujian Province Immunization Information System showed the total coverage of influenza vaccination (at least one dose) among preschool children in 2022 was 7.38%, which is far below Germany (40%) (11), and England (48%) (12) who provide specialized and effective policy support for vaccination. Currently, influenza vaccination in Fuzhou operates solely on a voluntary, self-paid basis without any complementary support measures such as government subsidies or insurance coverage. This suggested deficiencies in establishing or implementing influenza vaccine policies for Fuzhou.
This investigation showed 54.70% children had received at least one dose of the influenza vaccine, which was far below the WHO’s target of 75% and domestic of 28% (13) flu vaccination coverage. However, almost P/Gs (90.02%) were willing to have their children vaccinated against the flu, which suggested they knew it’s good to get vaccinated. If all P/Gs implemented the “Willingness,” children can be protected against flu through vaccination. In this study. Higher-degree of parental had higher influenza vaccination rates among preschoolers. Larson HJ’s article indicated that parental education level is a significant predictor of vaccine uptake (14). P/Gs with high education are more likely to vaccinate their children against influenza (15). However, European study reported that lower influenza vaccination rates among highly educated individuals in Ireland, Italy, and Spain (16). This discrepancy may be attributed to cultural and cognitive differences across regions. Extensive research has established that P/Gs knowledge significantly influences childhood influenza vaccination rates (17–19). Enhancing parental understanding of influenza may consequently improve vaccination rates among children. Our research showed only 1.49% P/Gs and 2.74% P/Gs answered “YES” about the safety and effectiveness of the influenza vaccine, indicating a substantial gap in influenza- and vaccine-related knowledge. When asked about the source of knowledge of flu vaccine, the main source of information about flu was vaccinators (55.34%), followed by CDC (47.57%), and social media (47.67%). So vaccinators must provide strong advice and vaccine knowledge to P/Gs who visit vaccination clinics. Above results showed influenza coverage among preschool children was low, good knowledge of influenza and influenza vaccine were linked to improved immunization coverage. These hinted that there was still a lack of publicity about influenza.
In addition to knowledge, the convenience and feasibility of influenza vaccination are also important influencing factors. Multivariate regression analyses showed that extended vaccination time negatively impacted compliance (β = −0.71, p < 0.05). The vaccination rate was higher among the respondents who could be vaccinated within 30 min. This disparity may reflect logistical challenges P/Gs face when coordinating clinic visits with children’s schedules. Distance between outpatient clinic and home also affect the convenience of vaccination (p < 0.05). Furthermore, parental occupational constraints and overtime status were identified as additional barriers, Goldman (20) and Ding’s (21) articles show that it is more difficult for P/Gs to coordinate the time of vaccination for children and their work leading to low vaccination.
Furthermore, some P/Gs also showed dissatisfaction with the vaccination process, including difficulties in making vaccine appointments, long queues, and cumbersome processes. These findings suggest current influenza vaccination procedures in Fuzhou create accessibility barriers. If individuals perceive the process of getting vaccinated to be complicated or cumbersome, they may be less likely to seek it out or delay it (22, 23). To boost children influenza vaccination coverage, public health authorities should prioritize service optimization through streamlined scheduling systems, extended clinic hours, digital appointment platforms, and strengthen cooperation with the school authorities (getting vaccinated before the flu season or strengthening the promotion of flu vaccination in schools).
Our results showed there was a significant inverse correlation between household income and influenza vaccination rates (β = −0.41, p < 0.05), which coincides with previous findings that vaccination rates among children tend to be higher in families with lower economic status (24). This phenomenon may be attributed to the greater perceived cost-effectiveness of immunization for economically disadvantaged families, where disease prevention represents a more substantial economic benefit. Health insurance coverage among preschool children is significantly associated with increased influenza vaccination uptake (p < 0.05). In addition, Fuzhou’s self-funded vaccination policy makes socially and economically disadvantaged groups have the burden of vaccination. The price of vaccines is an important deterrent to vaccination behavior. Comparative analyses of vaccination policies reveal that regions implementing free vaccination programs, such as Beijing and Hong Kong, achieve significantly higher coverage rates. Comparative analyses of vaccination policies reveal that regions such as Beijing (25) and Hong Kong (26), which implement free vaccination policy achieved significantly higher coverage rates than Fuzhou. Empirical evidence from national policy evaluations confirms that free vaccination policies yield the highest coverage rates, followed by medical insurance reimbursement systems (27, 28). These findings underscore the critical role of policy interventions and financial support mechanisms in enhancing vaccination uptake. In order to comprehensively increase influenza vaccine coverage among school-aged children in Fuzhou, we recommend implementing comprehensive strategies including: (1) establishment of free or subsidized vaccination programs, (2) integration with existing healthcare insurance systems, and (3) development of targeted initiatives for vulnerable populations.
Our study had a few limitations. First, the data on vaccination were self-reported, and not verified by immunization certificate, document, or serological testing. Second, the survey is a self-administered questionnaire by the respondents, we relied on respondents to fill out the questionnaire themselves to complete the survey, which may have limited a small percentage of P/Gs from responding.
In conclusion, our study offers valuable insights into the determinants influencing Chinese P/Gs’ willingness to vaccinate influenza vaccine for their children. The findings demonstrate that as factors such vaccine knowledge, medical insurance, occupation, household income, overtime work, transportation, vaccine prices, and total duration of each vaccination session play a pivotal role in shaping P/Gs’ intentions to influenza vaccine. Public health campaigns and educational initiatives should emphasize the benefits associated with the influenza vaccine. First, public health authorities should establish sustainable financing mechanisms and incentive programs to ensure vaccine accessibility and affordability, health and education departments can do a good job of health education on influenza and vaccination in advance, improve the corresponding cognitive level of the target population, convert vaccination intentions into actual uptake. These integrated measures, when implemented prior to influenza seasons, could significantly improve vaccination rates among preschool children, thereby establishing herd immunity and reducing influenza-related morbidity.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Fuzhou Center for Disease Control and Prevention’s Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
HJ: Writing – review & editing, Investigation, Project administration, Writing – original draft, Data curation, Methodology. WG: Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. XH: Project administration, Writing – review & editing, Investigation. QW: Project administration, Writing – review & editing, Investigation. YH: Project administration, Writing – review & editing, Investigation. LC: Investigation, Data curation, Writing – review & editing. DZ: Investigation, Data curation, Writing – review & editing. YZ: Investigation, Data curation, Writing – review & editing. LX: Investigation, Data curation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research received funding came from Vaccine and Immunization Young Talent Promotion Project of Chinese Preventive Medicine Association grant number CPMAQT_YM0320.
Acknowledgments
We thank the respondents, the vaccinators, and investigation teams, in Fuzhou CDC, Gulou District CDC, Fuqing CDC, Minqing County CDC, Minhou County CDC, and Yongtai County for their support and assistance with this investigation. We would also like to kindly thank all the participants for their time and contribution to this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization . Global influenza strategy 2019–2030. WHO. (2023). Available online at: https://apps.who.int/iris/handle/10665/311184. (Accessed 18 February 2023).
2. Nayak, J, Hoy, G, and Gordon, A. Influenza in Children. Cold Spring Harb Perspect Med. (2021) 11:a038430. doi: 10.1101/cshperspect.a038430
3. Wang, X, Li, Y, O'Brien, KL, Madhi, SA, Widdowson, MA, Byass, P, et al. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. Lancet Glob Health. (2020) 8:e497–510. doi: 10.1016/S2214-109X(19)30545-5
4. Lai, X, Rong, H, Ma, X, Hou, Z, Li, S, Jing, R, et al. The economic burden of influenza-like illness among children, chronic disease patients, and the elderly in China: a National Cross-Sectional Survey. Int J Environ Res Public Health. (2021) 18:6277. doi: 10.3390/ijerph18126277
5. Wu, S, VAN Asten, L, Wang, L, SA, MD, Pan, Y, Duan, W, et al. Estimated incidence and number of outpatient visits for seasonal influenza in 2015-2016 in Beijing. China Epidemiol Infect. (2017) 145:3334–44. doi: 10.1017/S0950268817002369
6. World Health Assembly . Resolution WHA56.19. Prevention and control of influenza pandemics and annual epidemics (2003) Available online at: http://apps.who.int/gb/archive/pdf_files/WHA56/ea56r19.pdf. (Accessed February 8, 2013).
7. Grohskopf, LA, Alyanak, E, Ferdinands, JM, Broder, KR, Blanton, LH, Talbot, HK, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2021-22 influenza season. MMWR Recomm Rep. (2021) 70:1–28. doi: 10.15585/mmwr.rr7005a1
8. National Immunization Advisory Committee Technical Working Group IVTWG . Technical guidelines for seasonal influenza vaccination in China (2021-2022). Zhonghua Liu Xing Bing Xue Za Zhi. (2021) 42:1722–49. doi: 10.3760/cma.j.cn112338-20210913-00732
9. Shono, A, and Kondo, M. Factors associated with seasonal influenza vaccine uptake among children in Japan. BMC Infect Dis. (2015) 18:72. doi: 10.1186/s12879-015-0821-3
10. Low, MSF, Tan, H, Hartman, M, Tam, CC, Hoo, C, Lim, J, et al. Parental perceptions of childhood seasonal influenza vaccination in Singapore: a cross-sectional survey. Vaccine. (2017) 35:6096–102. doi: 10.1016/j.vaccine.2017.09.060
11. Molnar, D, Anastassopoulou, A, Poulsen Nautrup, B, Schmidt-Ott, R, Eichner, M, Schwehm, M, et al. Cost-utility analysis of increasing uptake of universal seasonal quadrivalent influenza vaccine (QIV) in children aged 6 months and older in Germany. Hum Vaccin Immunother. (2022) 18:2058304. doi: 10.1080/21645515.2022.2058304
12. Boddington, NL, Mangtani, P, Zhao, H, Verlander, NQ, Ellis, J, Andrews, N, et al. Live-attenuated influenza vaccine effectiveness against hospitalization in children aged 2-6 years, the first three seasons of the childhood influenza vaccination program in England, 2013/14-2015/16. Influenza Other Respir Viruses. (2022) 16:897–905. doi: 10.1111/irv.12990
13. Wang, Q, Yue, N, Zheng, M, Wang, D, Duan, C, Yu, X, et al. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: a meta-analysis. Vaccine. (2018) 36:7262–9. doi: 10.1016/j.vaccine.2018.10.045
14. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DM, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
15. Ghazy, RM, Ibrahim, SA, Taha, SHN, Elshabrawy, A, Elkhadry, SW, Abdel-Rahman, S, et al. Attitudes of parents towards influenza vaccine in the eastern Mediterranean region: a multilevel analysis. Vaccine. (2023) 41:5253–64. doi: 10.1016/j
16. Endrich, MM, Blank, PR, and Szucs, TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. (2009) 27:4018–24. doi: 10.1016/j.vaccine.2009.04.029
17. Zhao, M, Liu, H, Qu, S, He, L, and Campy, KS. Factors associated with parental acceptance of influenza vaccination for their children: the evidence from four cities of China. Hum Vaccin Immunother. (2021) 17:457–64. doi: 10.1080/21645515.2020.1771988
18. Li, P, Qiu, Z, Feng, W, Zeng, H, Chen, W, Ke, Z, et al. Analysis of factors influencing parents' willingness to accept the quadrivalent influenza vaccine for school-aged children in the Nanhai District, China. Hum Vaccin Immunother. (2020) 16:1078–85. doi: 10.1080/21645515.2019.1644881
19. Hofstetter, AM, Opel, DJ, Stockwell, MS, Hsu, C, de Hart, MP, Zhou, C, et al. Influenza-related knowledge, beliefs, and experiences among caregivers of hospitalized children. Hosp Pediatr. (2021) 11:815–32. doi: 10.1542/hpeds.2020-003459
20. Goldman, RD, McGregor, S, Marneni, SR, Katsuta, T, Griffiths, MA, Hall, JE, et al. Willingness to vaccinate children against influenza after the coronavirus disease 2019 pandemic. J Pediatr. (2021) 228:87–93.e2. doi: 10.1016/j.jpeds.2020.08.005
21. Ding, X, Tian, C, Wang, H, Wang, W, and Luo, X. Associations between family characteristics and influenza vaccination coverage among children. J Public Health. (2020) 42:e199–205. doi: 10.1093/pubmed/fdz101
22. Zhao, X, Hu, X, Wang, J, Shen, M, Zhou, K, Han, X, et al. A cross-sectional study on the understanding and attitudes toward influenza and influenza vaccines among different occupational groups in China. Hum Vaccin Immunother. (2024) 20:2397214. doi: 10.1080/21645515.2024.2397214
23. Flood, EM, Rousculp, MD, Ryan, KJ, Beusterien, KM, Divino, VM, Toback, SL, et al. Parents' decision-making regarding vaccinating their children against influenza: a web-based survey. Clin Ther. (2010) 32:1448–67. doi: 10.1016/j.clinthera.2010.06.020
24. Zeng, Y, Yuan, Z, Yin, J, Han, Y, Chu, CI, and Fang, Y. Factors affecting parental intention to vaccinate kindergarten children against influenza: a cross-sectional survey in China. Vaccine. (2019) 37:1449–56. doi: 10.1016/j.vaccine.2019.01.071
25. Lv, M, Fang, R, Wu, J, Pang, X, Deng, Y, Lei, T, et al. The free vaccination policy of influenza in Beijing, China: the vaccine coverage and its associated factors. Vaccine. (2016) 34:2135–40. doi: 10.1016/j.vaccine.2016.02.032
26. Lau, YL, Wong, WHS, Hattangdi-Haridas, SR, and Chow, CB. Evaluating impact of school outreach vaccination programme in Hong Kong influenza season 2018-2019. Hum Vaccin Immunother. (2020) 16:823–6. doi: 10.1080/21645515.2019.1678357
27. Yang, J, Atkins, KE, Feng, L, Pang, M, Zheng, Y, Liu, X, et al. Seasonal influenza vaccination in China: landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine. (2016) 34:5724–35. doi: 10.1016/j.vaccine.2016.10.013
Keywords: influenza, preschool children, parental attitudes, influenza vaccination coverage, questionnaire survey
Citation: Jia H, Gao W, Huang X, Wang Q, Huang Y, Chen L, Zheng D, Zhang Y and Xu L (2025) Exploring influenza vaccination coverage and barriers to influenza vaccine uptake among preschool children in Fuzhou in 2022: a cross-sectional study. Front. Public Health. 13:1588760. doi: 10.3389/fpubh.2025.1588760
Edited by:
Sneha Vishwanath, University of Cambridge, United KingdomReviewed by:
Daniele Melo Sardinha, Evandro Chagas Institute, BrazilSruthika K. Ashokan, Diosynvax Ltd., United Kingdom
Copyright © 2025 Jia, Gao, Huang, Wang, Huang, Chen, Zheng, Zhang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haimei Jia, aGFpbWVpMTEwM0AxMjYuY29t
 Haimei Jia
Haimei Jia Wenyan Gao
Wenyan Gao Xun Huang1
Xun Huang1