- 1School of Nursing, Bouvé College of Health Sciences, Northeastern University, Boston, MA, United States
- 2Department of Psychological Sciences Texas Tech University, Department of Pharmacology and Neuroscience, Texas Tech University Health Sciences Center, Lubbock, TX, United States
- 3LIFE Research Institute, University of Ottawa, Ottawa, ON, Canada
- 4Department of Community and Behavioral Health, College of Public Health, East Tennessee State University, Johnson City, TN, United States
- 5Institute for Engaged Aging, Department of Psychology, Clemson University, Clemson, SC, United States
- 6Department of Health and Wellness Design, School of Public Health-Bloomington, Indiana University, Bloomington, IN, United States
- 7Steve Hicks School of Social Work, University of Texas at Austin, Austin, TX, United States
- 8School of Social Work, University of Texas at Arlington, Arlington, TX, United States
- 9School of Nursing, Thompson Rivers University, Kamloops, BC, Canada
- 10Department of Human Development, Connecticut College, New London, CT, United States
- 11Connell School of Nursing, Boston College, Chestnut Hill, MA, United States
- 12College of Social Work, University of Tennessee, Knoxville, TN, United States
- 13Department of Environmental and Occupational Health, School of Public Health, Texas A&M University, College Station, TX, United States
- 14Center for Community Health and Aging, Texas A&M University, College Station, TX, United States
- 15Department of Health Behavior, School of Public Health, Texas A&M University, College Station, TX, United States
Background: Older unpaid caregivers often face social isolation and loneliness, yet risk factors for social disconnection remain largely unexplored. As the demand for unpaid caregiving rises with an aging population, there is a need for targeted interventions to reduce social disconnectedness in this vulnerable group. This study aimed to identify determinants of social disconnectedness.
Methods: Data came from a sample of 701 unpaid caregivers aged 60 + who completed an internet-based survey assessing sociodemographics, health status, financial strain, social environment, and social disconnectedness. Four sequential regression models were used to identify the unique contribution of these factors related to social disconnectedness.
Results: The first model (F = 3.94, p < 0.001, aR2 = 0.030) showed that older age (β = −0.15, p < 0.001), self-identifying as being Black (β = −0.10, p = 0.008), and higher education (β = −0.11, p = 0.041) were associated with lower social disconnectedness. Adding health factors in the second model (F = 15.33, p < 0.001, aR2 = 0.170) revealed that, in addition to age and education, chronic conditions (β = 0.12, p = 0.001) and possible depression (β = 0.35, p < 0.001) were associated with social disconnectedness. Including financial strain in the third model (F = 15.52, p < 0.001, aR2 = 0.212) showed that household income (β = −0.10, p = 0.012) and financial stress (β = 0.18, p < 0.001) were additionally associated with social disconnectedness. The final model (F = 23.42, p < 0.001, aR2 = 0.366) that included social environmental factors showed that age (β = −0.07, p = 0.033), possible depression (β = 0.22, p < 0.001), financial stress (β = 0.16, p < 0.001), and levels of community belonging (β = −0.20–0.58, p < 0.001) were significantly related to the risk of disconnectedness.
Conclusion: Findings highlight possible intervention targets that have the potential to reduce social disconnectedness among older unpaid caregivers. Particularly, addressing depressive symptoms, reducing financial stress, and enhancing community belonging are essential components to mitigate social disconnectedness risk in this population.
Introduction
Unpaid caregivers, also known as informal, family, or friend caregivers, play an essential role in supporting individuals with chronic illnesses, disabilities, or age-related conditions (1, 2) by providing care to them without professional training or compensation (3). As such, unpaid caregiving often entails considerable physical, emotional, and financial burdens (1). Many unpaid caregivers dedicate substantial amounts of time providing care, which can limit their ability to engage in social activities, nurture relationships, and participate in community gatherings (4). This risk of social disconnectedness is particularly pronounced for older unpaid caregivers as they face their own age-related challenges, such as physical limitations, declining health, and reduced mobility, which further isolate them from social interactions, leaving them especially vulnerable as they balance their caregiving responsibilities with their personal well-being (5).
Social disconnectedness is the state characterized by a lack of social connection—an umbrella term that encompasses various dimensions of social relationships, including structural (e.g., size of social networks, marital status, living situation, social isolation), functional (e.g., received and perceived social support, loneliness), and quality-related (e.g., satisfaction with relationships, conflict) aspects of an individual’s world (6, 7). Social disconnectedness has a significant impact on health and overall well-being across all age groups (8, 9). The consequences of social isolation and loneliness in caregivers, as well as its influence on the care recipients are well documented (10). While extensive research exists on the risks of social isolation among the older adult population at large, there remains a significant gap in understanding its prevalence and implications among older unpaid caregivers. Furthermore, most studies on social disconnectedness in this group have focused on one aspect of social disconnectedness that generally taps into either structural or functional dimension (11–13) and have not considered diverse aspects of social disconnectedness simultaneously, limiting a comprehensive understanding of the social disconnectedness risk faced by unpaid caregivers.
Caregiving for older adults can negatively affect unpaid caregivers financially due to decreased work hours and household income, high costs of care, and reduced capacity to work (14, 15). A recent review noted that unpaid caregivers face both direct financial costs (i.e., out-of-pocket expenses) and indirect financial costs (i.e., changes in household finances due to reduced labor participation) resulting in significant financial strain on this population (16). Financial strain is a robust predictor of social isolation across the life course, particularly for older adults (17), due to a lack of resources and/or increased labor commitments that result in an inability to engage in leisure and social activities (18). The resulting lack of engagement exacerbates social disconnectedness, creating a vicious cycle of isolation. Given that unpaid caregivers often provide support for extended periods (i.e., years), they are at particular risk for chronic social disconnectedness. However, access to community resources and strong connections within the community can serve as protective factors against the dual burdens of financial strain and social disconnectedness faced by unpaid caregivers.
Social environment plays an important role in health and well-being and is directly related to social disconnectedness (19). Social environment refers to the physical and social contexts in which individuals live, work, or interact, including workplaces, parks, or neighborhoods (including urban, rural or remote areas) (20). This environment influences unpaid caregiver’s lives, including their sense of belonging and access to community resources (21). For example, caregivers in rural or remote areas may have limited access to health care services and community programs, which can exacerbate the effects of an already challenging caregiving role and possibly increase the risk of social disconnectedness.
Understanding the factors that contribute to the risk of social disconnectedness in older unpaid caregivers is crucial for designing targeted interventions that can effectively mitigate isolation and reduce its negative impact on health and well-being. To address this gap in the literature, the purpose of this study was to identify different types of factors associated with social disconnectedness risk among unpaid caregivers aged 60 and older.
Methods
Data source
Data were analyzed from a cross-sectional, internet-delivered questionnaire targeting adults ages 60 years and older residing in the United States (22). Participants were recruited nationwide through a Qualtrics Internet Panel (23) between June 2019 and September 2019. To address potential sampling bias introduced by online convenience sampling, quota sampling parameters were employed to diversify the sample across key demographic characteristics, including age, sex, race, and geographic location (22, 24). After participants were identified by Qualtrics, they were presented with a link to the online questionnaire, which required acknowledgment of an Institutional Review Board (IRB)-approved information sheet. Participation in the study was voluntary, and participants could choose to stop taking the survey at any time. Participants were compensated by Qualtrics for their participation, not the research team, in accordance with the Qualtrics Internet Panel policy. A total of 4,101 older adults completed the survey, of which 19 were omitted for missing data on all questions. To align with the study’s focus on unpaid caregivers, participants who indicated “yes” to a question about providing unpaid regular care or assistance to a friend or family member with a health problem or disability were included in the analyses. The resulting analytic sample was 701 unpaid caregivers ages 60 years and older. All survey procedures were approved by the Texas A&M University IRB (IRB2019-0375).
Variables and measures
Sociodemographics
Measures used to identify participant characteristics included self-reported age (i.e., range from 60 to 94 years), sex (i.e., male, female), ethnicity (i.e., non-Hispanic, Hispanic), race (i.e., White or Caucasian, Black or African American, Another Race), education level (i.e., high school education or less, some college, college graduate or more), and whether the participant lived alone (i.e., no, yes).
Health factors
Health factors included the number of chronic conditions and possible depression. Participants were asked to report if a healthcare provider told them they had any of 19 chronic conditions (e.g., arthritis, diabetes, high cholesterol, high blood pressure, cancer, chronic pain, osteoporosis, urinary incontinence). The number of self-reported chronic conditions were summed to create a composite score. Depressive symptoms were measured by the two-item version of the Patient Health Questionnaire (PHQ-2) (25, 26). This brief assessment contains the first two items of the PHQ-9 (27), which measures the two cardinal symptoms of depression: depressed mood and anhedonia. The PHQ-2 asks participants to report the frequency they “felt down, sad, or hopeless” and “had little interest or pleasure in doing things” in the past 2 weeks. Response choices were on a 4-point Likert scale that ranged from “not at all” (scored 0) to “nearly every day” (scored 3). These items were summed, with a total score ranging from 0 to 6. The scores were dichotomized using the recommended cutoff of ≥3, indicating those with possible depression (28).
Financial strain
Financial strain was assessed using annual household income, current employment status, and a four-item financial stress scale. Participants were asked to self-report their annual household income [i.e., ranging from “less than $10,000” (scored 1) to “$60,001 or more” (scored 6) in $10,000 increments] and if they were currently employed (i.e., “no” or “yes”). Further, participants were asked a series of four items to determine whether they were worried or stressed about having enough money regarding (a) paying their rent or mortgage; (b) buying nutritious meals; (c) buying medications; and (d) meeting their basic needs. Response choices for each item were on a 5-point Likert scale that ranged from “never” to “always.” Based on the frequency distribution, each item was dichotomized as “never/rarely” (scored 0) and “sometimes/usually/always” (scored 1). These four items were summed to create a composite score ranging from 0 to 4 (Cronbach’s alpha = 0.84), with higher scores indicating more financial stress.
Social environment
Social environment included rurality/urbanicity of participant’s residence, access to resources, and community belonging. Participants’ county of residence was geocoded based on the 2013 Rural–Urban Continuum Codes (RUCC), which were the most current at the time of data collection. These codes indicate population density within a given county and range from 1 to 9, where higher values indicate residing in more rural areas (29). To capture access to local resources, participants were asked to indicate if “it is easy for me get to appointments, grocery stores, places of worship, and other locations.” Response choices for this item were “yes” (scored 0) and “no” (scored 1), with higher scores indicating more access to resources. Finally, participants were also asked to rate their sense of belonging to their local community, using a 4-point Likert scale. Response choices were “very weak” (scored 1), “somewhat weak” (scored 2), “somewhat strong” (scored 3), and “very strong” (scored 4).
Social disconnectedness risk
The primary outcome of interest was the risk of social disconnectedness among participants, measured by the Upstream Social Interaction Risk Scale (U-SIRS-13) (22, 30). This 13-item scale asked participants to report the frequency of feeling disconnected in terms of physical opportunities to interact with others and the emotional fulfillment of such interactions (or lack thereof). Response choices were on a 3-point Likert scale and included “none of the time” (scored 1), “some of the time” (scored 2), and “often” (scored 3). Each item was then dichotomized based on the directionality of the wording to create items scored as “no risk” (scored 0) and “risk” (scored 1). Items were then summed to generate a continuous score from 0 to 13, with higher scores indicating higher risk for social disconnectedness. Cronbach’s alpha for the U-SIRS-13 in the sample was 0.80, which aligns with the strength of reliability coefficients identified in other studies (22).
Data analysis
All analyses were performed using IBM SPSS Statistics (Version 29). First, descriptive statistics were computed for the sample. Then, we fitted a series of sequential ordinary least squares regression models to examine the relative importance of participants’ sociodemographic characteristics, health factors, financial strain, and social environments on the risk for social disconnectedness. Variable sets were sequentially added as blocks into each subsequent regression model (i.e., a total of four blocks). The proportion of error variance controlled for by each model (i.e., Adjusted R Square) was compared across the four regression models. Regression diagnostics were conducted to assess the assumptions of multivariable linear regression, including the absence of multicollinearity among the variables by checking the variance inflation factor (VIF). For all statistical tests, effects were considered significant at p < 0.05.
Results
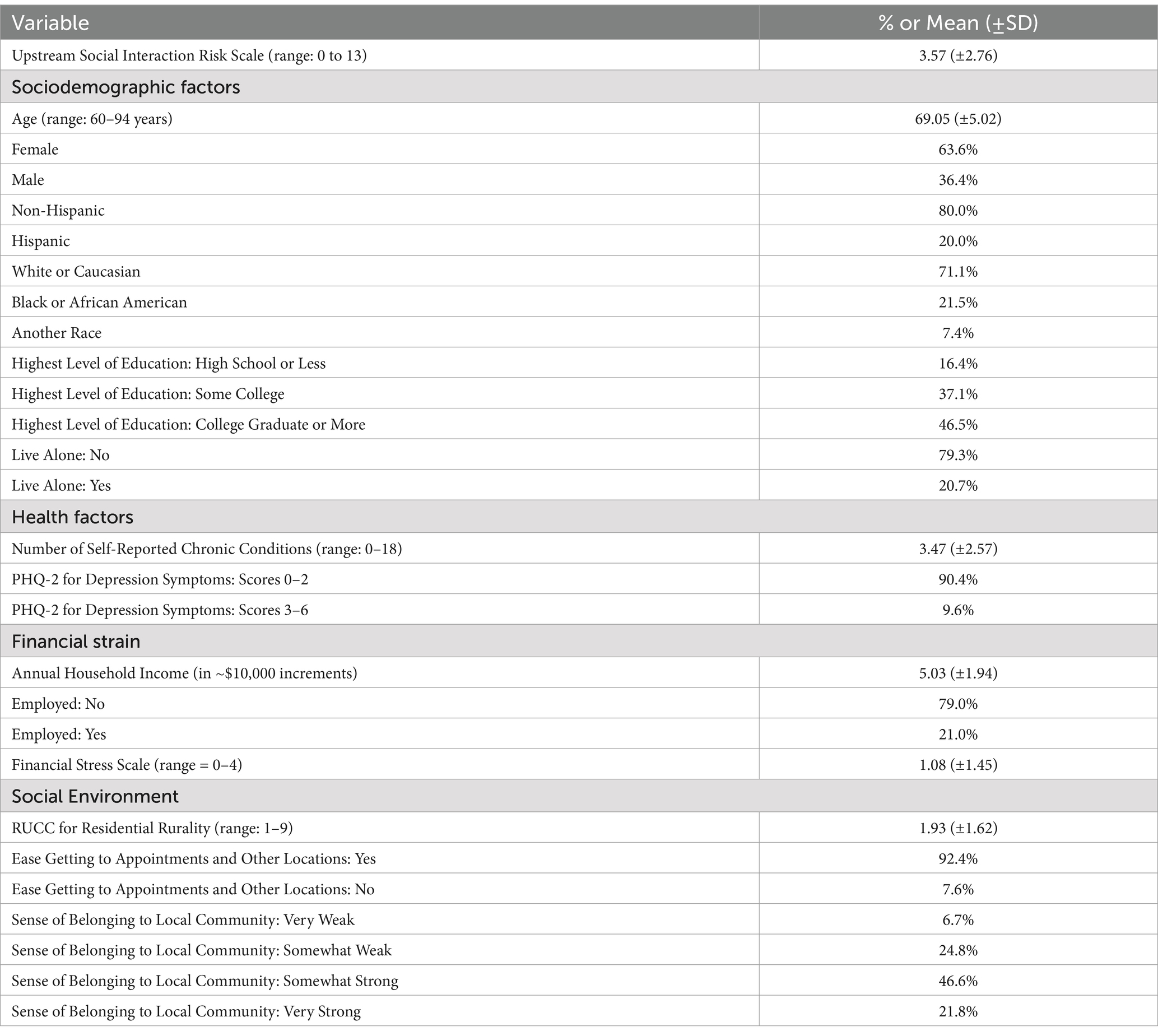
Table 1 provides demographic information about participants. The average age was 69.05 (±5.02) years. Most participants were female (63.6%), non-Hispanic (80.0%), and White or Caucasian (71.1%). Most participants reported either having some college education (37.1%) or a college degree or more (46.5%). About 21.0% of participants lived alone. Participants reported 3.47 (±2.57) chronic conditions on average, and 9.6% screened positive for possible depression (PHQ-2 ≥ 3). Participants’ average household income was between $40,000 and $50,000, 79.0% were not employed, and had low worry/stress about money (i.e., average score of 1.08). Participants primarily resided in metropolitan areas (i.e., average RUCC of 1.93), with 92.4% reporting being able to easily get to appointments, grocery stores, places of worship, and other locations. About 31% of participants reported having a “somewhat weak” or “weak” sense of belonging to their local community.
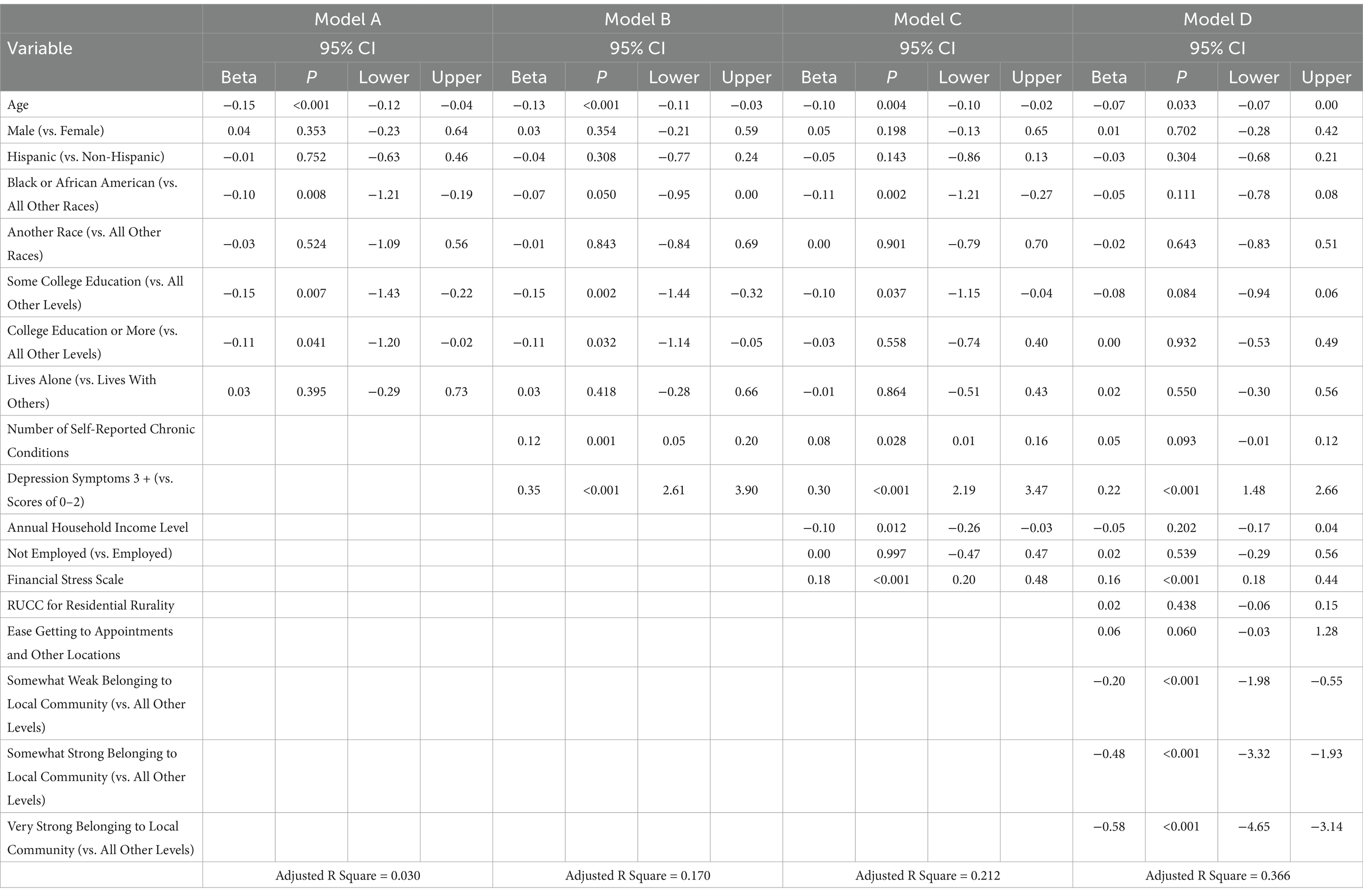
Table 2 reports findings from the sequential ordinary least squares regression models. The first model (Model A: sociodemographic factors only; F = 3.94, p < 0.001, aR2 = 0.030) showed that each additional year of age (β = −0.15, p < 0.001) and self-identifying as being Black/AA (β = −0.10, p = 0.008) were associated with lower risk for social disconnectedness. Participants who attended some college (β = −0.15, p = 0.007) or had college education or more (β = −0.11, p = 0.041) had lower risk for social disconnectedness compared to high school or less than high school levels of education.
The second model added health factors to the analysis (Model B: sociodemographics + health factors; F = 15.33, p < 0.001, aR2 = 0.170) and showed that age and education remained significant predictors of lower social disconnectedness risk. Further, self-reported chronic condition (β = 0.12, p = 0.001) and having possible depression (β = 0.35, p < 0.001) were additionally associated with higher risk for social disconnectedness.
The third model (Model C: sociodemographics + health factors + financial burden; F = 15.52, p < 0.001, aR2 = 0.212) showed that, in addition to the significant findings from Models A and B, higher annual household income was associated with lower risk for social disconnectedness (β = −0.10, p = 0.012), whereas being more worried or stressed about money was associated with higher risk for social disconnectedness (β = 0.18, p < 0.001).
The final model (Model D: sociodemographics + health factors + financial burden + social environment; F = 23.42, p < 0.001, aR2 = 0.366) showed that age (β = −0.07, p = 0.033), possible depression (β = 0.22, p < 0.001), and financial stress (β = 0.16, p < 0.001) remained significantly associated with higher social disconnectedness. Compared to those with very weak belonging to their local community, participants who reported somewhat weak (β = −0.20, p < 0.001), somewhat strong (β = −0.48, p < 0.001), or very strong (β = −0.58, p < 0.001) community belonging had lower risk for social disconnectedness.
Figure 1 illustrates the additive contributions of each block of variables in terms of model fit (i.e., higher Adjusted R Square values indicate stronger models in that that the included variables explain more variance in social disconnectedness) for Models A through D (i.e., starting with sociodemographic characteristics and sequentially adding, health factors, financial strain, and social environment variables). Each block meaningfully increases the model’s explanatory power, with the final model accounting for 36.6% of the variance in social disconnectedness.

Figure 1. Sequential contribution to explained variance in social disconnectedness. Bar chart displays adjusted R Square values for each sequential regression model. Model A includes sociodemographics; Model B adds health factors; Model C adds financial strain; and Model D adds social environment variables. Each block meaningfully increases the model’s explanatory power, with the final model accounting for 36.6% of the variance in social disconnectedness.
Discussion
This study identified the unique contributions of sociodemographic, health, financial, and social environmental factors to social disconnectedness risk among older unpaid caregivers aged 60 and above. The findings underscore critical areas for both prevention and intervention strategies to mitigate social disconnectedness in this population. One of the most significant findings was the strong and consistent association between probable depression and increased risk of social disconnectedness across all three models in which it was included. This finding aligns with previous research indicating that mental health, such as depression, can exacerbate feelings of isolation and hinder the ability to engage in social activities (31, 32). Depressive symptoms may lead to withdrawal from social networks, reduced motivation to seek social support, and a diminished sense of belonging (32). Given that caregivers often experience emotional strain due to their caregiving responsibilities, it is critical for health care professionals to screen for depressive symptoms early and address depression using evidence-based interventions, such as behavioral activation (33), and cognitive-behavioral therapy (34, 35). However, caregivers are often “hidden patients” making it difficult for healthcare providers to identify them and intervene on their behalf. To address this concern, Holiday and colleagues (2022) developed the C.A.R.E. framework (36) – Caregiver well-being, Advanced care planning, Respite, and Education—which is designed to educate clinicians about the need to support family caregivers and connect them to interventions and support. Dissemination of the C.A.R.E. framework could enhance clinicians’ efforts to screen for depression and social disconnectedness in this population. Ultimately, reducing depressive symptoms could result in improved emotional well-being, greater engagement in social interactions, and reduced social disconnectedness risk.
Financial stress was another significant factor associated with social disconnectedness risk among unpaid caregivers. The financial burden associated with caregiving responsibilities, including out-of-pocket costs such as health care expenses for care recipients, can significantly limit the caregivers’ ability to use resources for participating in social activities to maintain connections (15). This financial strain is particularly pronounced among spousal caregivers, who are more vulnerable compared to adult children caring for parents. This is important to highlight particularly among older caregivers who are retired and reliant on fixed incomes (37). Further, caregiving responsibilities may reduce working hours for unpaid caregivers who are still in the workforce (38). Strategies to address financial stress should extend beyond providing financial assistance to include employment support programs for unpaid caregivers to help them balance work and caregiving responsibilities. As individuals increasingly remain in the workforce beyond traditional retirement age, sustaining employment may provide caregivers with financial stability, social engagement opportunities, and a sense of purpose. Promoting caregiver-inclusive institutional policies (e.g., such as flexible work hours, expanded caregiving leave, and remote work options) may play a critical role in mitigating financial stress and preserving social connection, especially among those providing ongoing unpaid care while working. In addition, providing free or low-cost respite services could allow unpaid caregivers to engage in more social activities or re-enter the workforce, which can mitigate the risk of social disconnectedness.
A strong sense of community belonging was identified as a significant factor mitigating the risk of social disconnectedness among older unpaid caregivers, underscoring the importance of social integration and community involvement in reducing isolation within this population. Research demonstrates that a sense of belonging to one’s community may serve as a protective buffer against caregiving burden (39) through collective efforts in problem solving and inducing a greater sense of identity (40). Community-based interventions that promote social inclusion, such as neighborhood programs, support groups, and local activities, could foster a stronger sense of belonging and reduce the risk of social disconnectedness. Interpersonal strategies such as peer mentoring may help reduce isolation and foster a sense of community, which could help reduce social disconnectedness risk (41, 42). Technology-based interventions may help to facilitate social participation for caregivers who have impaired physical functioning or no longer drive, as well as for individuals who are in a high intensity caregiving context (43). Taking an upstream approach to intervention by targeting unpaid caregivers that are living in certain high risk social environments, such as those in isolated areas or with limited access to resources, is critical.
Caregivers who self-identify as Black or African American had reduced risk of social disconnectedness. This contrasts with existing literature that shows higher levels of social isolation in racial and ethnic minorities due to structural inequities and discrimination (44) but aligns with the evidence on protective effects of being a racial/ethnic minority caregiver through increased access to social support (45). Caregivers who self-identify as Black or African American may benefit from stronger ties to family, friends, fictive kin, and community (46) which provide emotional and social support that enhances social connections. Previous studies suggest that Black or African American communities may have more robust unpaid caregiving networks and a cultural emphasis on collective support, which can foster a sense of community (45). However, this finding warrants further exploration to better understand the complex interplay between race, caregiving, and social connection. It also highlights the need for culturally tailored interventions that build upon existing strengths within communities (47).
Several limitations should be considered when interpreting the findings. First, the study relied on a non-probabilistic, internet-based sample, which may introduce selection bias. While the study attracted participants from a range of sociodemographic backgrounds, participants with internet access and the ability to complete online surveys may not fully represent the broader population of older unpaid caregivers, particularly those who are more socially isolated or economically disadvantaged. This study may have also excluded unpaid caregivers experiencing higher levels of burden who lacked the time or capacity to engage in this study. Similarly, the sampling methodology may have inadvertently excluded individuals who are less digitally connected—such as those with limited internet access, lower digital literacy, or greater social isolation. These individuals may represent a particularly vulnerable subgroup of caregivers who face compounded barriers to social engagement and support. As a result, our findings may underestimate the true prevalence or severity of social disconnectedness among the broader population of older unpaid caregivers. Future research should consider using mixed-modal recruitment strategies to ensure inclusion of digitally disconnected individuals and to more comprehensively assess social risks across the caregiving spectrum. Second, we did not collect information about the care recipients or specific caregiving contexts, including the types or intensities of caregiving. For example, caring for an individual with Alzheimer’s disease or related dementias differs significantly from caring for someone with mobility challenges. As such, the potential influence of these distinct caregiving contexts on the risk of social disconnectedness among unpaid caregivers warrants further investigation. Future research should incorporate more detailed measures of caregiving roles and responsibilities to better understand how specific caregiving contexts contribute to social disconnectedness among older unpaid caregivers. Differentiating between caregiving subtypes may also help tailor interventions to those at greatest risk of social isolation. Third, the study did not assess whether participants were the primary caregivers or part of a broader caregiving network. Understanding whether additional caregivers co-provide care could offer valuable insights into how caregiving networks influence social connectedness. Fourth, the cross-sectional design of the study limits the ability to infer causal and direction of the relationships between identified risk factors and social disconnectedness. Longitudinal studies are needed to clarify the directionality and temporal dynamics of how sociodemographic characteristics, health factors, and caregiving contexts influence social connectedness as older unpaid caregivers age. Lastly, since the current study used the PHQ-2 to assess depressive symptoms (27), our findings should be interpreted with caution, recognizing that they reflect screening-level indicators rather than formal diagnoses.
Conclusion
This study contributes to the growing body of knowledge on social disconnectedness risk among older unpaid caregivers by identifying key risk factors reflecting intervention targets. Through sequential regression modeling, this study assessed the unique contributions of various factors related to social disconnectedness risk in older unpaid caregivers. Addressing depressive symptoms, reducing financial stress, and enhancing community belonging are essential components to mitigate social disconnectedness risk in this population. Given the projected growth of older unpaid caregivers, this research highlights an urgent need to provide resources and services that promote social connection, strengthen supportive networks, and improve overall well-being among older unpaid caregivers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) at Texas A&M University (IRB2019-0375). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because procedures were reviewed and approved by the Institutional Review Board (IRB) at Texas A&M University (IRB2019-0375). Given the cross-sectional and anonymous nature of the survey, the IRB determined that this research meets the criteria for U.S. Human Research Protection (HRPP) Exemption in accordance with 45 CFR 46.104. Instead of written consent, participants were provided with information sheet presented in the first page of the Survey Participants needed to click ‘I agree’ to acknowledge receipt and continue taking the actual survey. The study was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author contributions
MY-J: Conceptualization, Writing – original draft, Writing – review & editing. JS: Writing – review & editing. CB: Writing – review & editing. JLS: Writing – review & editing. HC: Writing – review & editing. AP: Writing – review & editing. YZ: Writing – review & editing. CEV: Writing – review & editing. J-DB: Writing – review & editing. KK: Writing – review & editing. WJ: Writing – review & editing. TW: Writing – review & editing. MO: Writing – review & editing. MLS: Formal Analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the participants for their time in completing the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Leykum, LK, Penney, LS, Dang, S, Trivedi, RB, Noël, PH, Pugh, JA, et al. Recommendations to improve health outcomes through recognizing and supporting caregivers. J Gen Intern Med. (2022) 37:1265–9. doi: 10.1007/s11606-021-07247-w
2. Wolff, JL, Mulcahy, J, Roth, DL, Cenzer, IS, Kasper, JD, Huang, J, et al. Long-term nursing home entry: a prognostic model for older adults with a family or unpaid caregiver. J Am Geriatr Soc. (2018) 66:1887–94. doi: 10.1111/jgs.15447
3. Stall, NM, Campbell, A, Reddy, M, and Rochon, PA. Words matter: the language of family caregiving. J Am Geriatr Soc. (2019) 67:2008–10. doi: 10.1111/jgs.15988
4. Beach, B, Bélanger-Hardy, L, Harding, S, Rodrigues Perracini, M, Garcia, L, Tripathi, I, et al. Caring for the caregiver: why policy must shift from addressing needs to enabling caregivers to flourish. Front Public Health. (2022) 10:997981. doi: 10.3389/fpubh.2022.997981
5. Theng, B, Tran, JT, Serag, H, Raji, M, Tzeng, HM, Shih, M, et al. Understanding caregiver challenges: a comprehensive exploration of available resources to alleviate caregiving burdens. Cureus. (2023) 15:e43052. doi: 10.7759/cureus.43052
6. Donovan, NJ, and Blazer, D. Social isolation and loneliness in older adults: review and commentary of a National Academies Report. Am J Geriatr Psychiatry. (2020) 28:1233–44. doi: 10.1016/j.jagp.2020.08.005
7. Holt-Lunstad, J. Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications. World Psychiatry. (2024) 23:312–32. doi: 10.1002/wps.21224
8. Umberson, D, and Montez, JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. (2010) 51:S54–66. doi: 10.1177/0022146510383501
9. Cornwell, EY, and Waite, LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. (2009) 50:31–48. doi: 10.1177/002214650905000103
10. Hajek, A, Kretzler, B, and König, HH. Informal caregiving, loneliness and social isolation: a systematic review. Int J Environ Res Public Health. (2021) 18:12101. doi: 10.3390/ijerph182212101
11. Wang, J, Liu, W, Li, X, Ma, Y, Zhao, Q, Lü, Y, et al. Examining the social networks types and their effects on caregiving experience of family caregivers for individuals with dementia: a mixed-methods study. Innov Aging. (2024) 8:igae040. doi: 10.1093/geroni/igae040
12. Roth, AR. Informal caregiving and social capital: a social network perspective. Res Aging. (2020) 42:272–80. doi: 10.1177/0164027520912659
13. Lee, J, Baik, S, Becker, TD, and Cheon, JH. Themes describing social isolation in family caregivers of people living with dementia: a scoping review. Dementia. (2022) 21:701–21. doi: 10.1177/14713012211056288
14. Lai, DWL. Effect of financial costs on caregiving burden of family caregivers of older adults. SAGE Open. (2012) 2:2158244012470467. doi: 10.1177/2158244012470467
15. Lee, Y, and Zurlo, KA. Spousal caregiving and financial strain among middle-aged and older adults. Int J Aging Hum Dev. (2014) 79:302–21. doi: 10.1177/0091415015574181
16. Watkins, M, and Overton, L. The cost of caring: a scoping review of qualitative evidence on the financial wellbeing implications of unpaid care to older adults. Ageing Soc. (2024) 1–28. doi: 10.1017/S0144686X24000382
17. Kahn, JR, and Pearlin, LI. Financial strain over the life course and health among older adults. J Health Soc Behav. (2006) 47:17–31. doi: 10.1177/002214650604700102
18. Drost, MA, Snyder, AR, Betz, M, and Loibl, C. Financial strain and loneliness in older adults. Appl Econ Lett. (2024) 31:845–8. doi: 10.1080/13504851.2022.2152421
19. Zahnow, R. Social infrastructure, social cohesion and subjective wellbeing. Wellbeing Space Soc. (2024) 7:100210. doi: 10.1016/j.wss.2024.100210
20. Yen, IH, and Syme, SL. The social environment and health: a discussion of the epidemiologic literature. Annu Rev Public Health. (1999) 20:287–308. doi: 10.1146/annurev.publhealth.20.1.287
21. Choi, H, Reblin, M, and Litzelman, K. Conceptualizing family Caregivers' use of community support services: a scoping review. Gerontologist. (2024) 64:1–11. doi: 10.1093/geront/gnad039
22. Smith, ML, and Barrett, ME. Development and validation of the upstream social interaction risk scale (U-SIRS-13): a scale to assess threats to social connectedness among older adults. Front Public Health. (2024) 12:1454847. doi: 10.3389/fpubh.2024.1454847
23. Qualtrics. Available online at: https://www.qualtrics.com/research-services/online-sample/.
24. Lehdonvirta, V, Oksanen, A, Räsänen, P, and Blank, G. Social media, web, and panel surveys: using non-probability samples in social and policy research. Policy Internet. (2021) 13:134–55. doi: 10.1002/poi3.238
25. Kroenke, K, Spitzer, RL, and Williams, JB. The patient health Questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
26. Spitzer, RL, Kroenke, K, and Williams, JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
27. Arroll, B, Goodyear-Smith, F, Crengle, S, Gunn, J, Kerse, N, Fishman, T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. (2010) 8:348–53. doi: 10.1370/afm.1139
28. Levis, B, Sun, Y, He, C, Wu, Y, Krishnan, A, Bhandari, PM, et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and meta-analysis. JAMA. (2020) 323:2290–300. doi: 10.1001/jama.2020.6504
29. 2013 Rural-Urban Continuum Codes. (2020). Available online at: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.
30. Smith, ML, Steinman, LE, and Casey, EA. Combatting social isolation among older adults in a time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health. (2020) 8:403. doi: 10.3389/fpubh.2020.00403
31. Dahlberg, L, McKee, KJ, Frank, A, and Naseer, M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment Health. (2022) 26:225–49. doi: 10.1080/13607863.2021.1876638
32. Elmer, T, and Stadtfeld, C. Depressive symptoms are associated with social isolation in face-to-face interaction networks. Sci Rep. (2020) 10:1444. doi: 10.1038/s41598-020-58297-9
33. Zabihi, S, Lemmel, FK, and Orgeta, V. Behavioural activation for depression in informal caregivers: a systematic review and meta-analysis of randomised controlled clinical trials. J Affect Disord. (2020) 274:1173–83. doi: 10.1016/j.jad.2020.03.124
34. Kang, SY. Predictors of emotional strain among spouse and adult child caregivers. J Gerontol Soc Work. (2006) 47:107–31. doi: 10.1300/J083v47n01_08
35. Hopkinson, MD, Reavell, J, Lane, DA, and Mallikarjun, P. Cognitive behavioral therapy for depression, anxiety, and stress in caregivers of dementia patients: a systematic review and meta-analysis. Gerontologist. (2019) 59:e343–62. doi: 10.1093/geront/gnx217
36. Holliday, AM, Quinlan, CM, and Schwartz, AW. The hidden patient: the CARE framework to care for caregivers. J Family Med Prim Care. (2022) 11:5–9. doi: 10.4103/jfmpc.jfmpc_719_21
37. Kang, S-Y. Financial strain among unpaid family caregivers of frail elders in community. J Hum Behav Soc Environ. (2021) 31:582–98. doi: 10.1080/10911359.2020.1799900
38. Keita Fakeye, MB, Samuel, LJ, Drabo, EF, Bandeen-Roche, K, and Wolff, JL. Caregiving-related work productivity loss among employed family and other unpaid caregivers of older adults. Value Health. (2023) 26:712–20. doi: 10.1016/j.jval.2022.06.014
39. Sargent, J, Williams, RA, Hagerty, B, Lynch-Sauer, J, and Hoyle, K. Sense of belonging as a buffer against depressive symptoms. J Am Psychiatr Nurses Assoc. (2002) 8:120–9. doi: 10.1067/mpn.2002.127290
40. Michalski, CA, Diemert, LM, Helliwell, JF, Goel, V, and Rosella, LC. Relationship between sense of community belonging and self-rated health across life stages. SSM Popul Health. (2020) 12:100676. doi: 10.1016/j.ssmph.2020.100676
41. Fleisher, JE, Suresh, M, Klostermann, EC, Lee, J, Hess, SP, Myrick, E, et al. IN-HOME-PDCaregivers: the effects of a combined home visit and peer mentoring intervention for caregivers of homebound individuals with advanced Parkinson’s disease. Parkinsonism Relat Disord. (2023) 106:105222. doi: 10.1016/j.parkreldis.2022.11.014
42. Liu, J, Cheung, ESL, Lou, Y, and Wu, B. A peer mentoring program for Chinese American dementia caregivers: a pilot randomized controlled trial. Aging Ment Health. (2024) 28:1479–88. doi: 10.1080/13607863.2024.2346599
43. Lindeman, DA, Kim, KK, Gladstone, C, and Apesoa-Varano, EC. Technology and caregiving: emerging interventions and directions for research. Gerontologist. (2020) 60:S41–9. doi: 10.1093/geront/gnz178
44. Umberson, D, and Donnelly, R. Social isolation: an unequally distributed health Hazard. Ann Rev Sociol. (2023) 49:379–99. doi: 10.1146/annurev-soc-031021-012001
45. Ellis, KR, Koumoutzis, A, Lewis, JP, Lin, Z, Zhou, Y, Chopik, WJ, et al. Conceptualizing and operationalizing collaboration among multiple caregivers of older adults. J Gerontol B Psychol Sci Soc Sci. (2023) 78:S27–s37. doi: 10.1093/geronb/gbac139
46. Taylor, RJ, Chatters, LM, Woodward, AT, and Brown, E. Racial and ethnic differences in extended family, friendship, fictive kin and congregational informal support networks. Fam Relat. (2013) 62:609–24. doi: 10.1111/fare.12030
Keywords: unpaid caregivers, older adults, social environment, financial strain, social disconnectedness
Citation: Yoo-Jeong M, Singer J, Bergeron CD, Southerland JL, Chai HW, Pickett AC, Zhou Y, Vazquez CE, Bacsu J-D, Kwong K, Jung W, Washington TR, Ory MG and Smith ML (2025) Factors related to social disconnectedness among older unpaid caregivers. Front. Public Health. 13:1589103. doi: 10.3389/fpubh.2025.1589103
Edited by:
María Cantero-García, Universidad a Distancia de Madrid, SpainReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesSandra Gómez-Martínez, Valencian International University, Spain
Copyright © 2025 Yoo-Jeong, Singer, Bergeron, Southerland, Chai, Pickett, Zhou, Vazquez, Bacsu, Kwong, Jung, Washington, Ory and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moka Yoo-Jeong, bS55b28tamVvbmdAbm9ydGhlYXN0ZXJuLmVkdQ==
 Moka Yoo-Jeong
Moka Yoo-Jeong Jonathan Singer
Jonathan Singer Caroline D. Bergeron
Caroline D. Bergeron Jodi L. Southerland
Jodi L. Southerland Hye Won Chai5
Hye Won Chai5 Andrew C. Pickett
Andrew C. Pickett Yuanjin Zhou
Yuanjin Zhou Christian E. Vazquez
Christian E. Vazquez Juanita-Dawne Bacsu
Juanita-Dawne Bacsu Marcia G. Ory
Marcia G. Ory Matthew Lee Smith
Matthew Lee Smith