- 1Intensive Care Unit, Shandong Public Health Clinical Center, Jinan, Shandong, China
- 2Surgical Intensive Care Unit, Shandong Public Health Clinical Center, Jinan, Shandong, China
Objective: Continuous renal replacement therapy (CRRT) is the primary treatment for severe sepsis and has been shown to reduce patient mortality. Patients with severe sepsis who receive CRRT frequently experience significant physical and psychological distress, manifesting as shame, social withdrawal, and abnormal cognitive moods. This study aimed to explore the relationship between psychological resilience, cognitive flexibility, and post-traumatic growth (PTG) levels in patients with severe sepsis treated with CRRT.
Methods: From January to October 2024, patients with severe sepsis who were treated with CRRT in our hospital were selected by convenience sampling as the research object. The Connor-Davidson Resilience Scale (CDRISC), Cognitive Flexibility Scale, and Post-Traumatic Growth Inventory (PTGI) were used to evaluate patients’ psychological resilience, cognitive flexibility, and PTG levels. Statistical methods included the independent sample t test, Pearson analysis, and linear regression analysis.
Results: The total scores of CDRISC, cognitive flexibility scale and PTGI in 205 patients was (42.98 ± 6.13), (95.04 ± 17.98) and (49.77 ± 9.92), respectively. There was a significant positive correlation between psychological resilience, cognitive flexibility, and PTG levels in patients with severe sepsis treated with CRRT (p < 0.05). Psychological resilience and cognitive flexibility had positive predictive effects on PTG, and there were significant positive predictive effects between psychological resilience and cognitive flexibility (p < 0.05). Psychological resilience directly and positively predicted PTG (β = 0.538, p < 0.05). The indirect effect of psychological resilience on cognitive flexibility was significant (β = 0.677, p < 0.05), and the indirect effect of cognitive flexibility on PTG was significant (β = 0.165, p < 0.05). The chain-mediating effect between psychological resilience, cognitive flexibility, and PTG was significant (β = 0.112, p < 0.05).
Conclusion: Psychological resilience can affect the PTG level of patients with severe sepsis treated with CRRT and can also indirectly affect PTG levels through direct chain mediation of cognitive flexibility. Targeted intervention strategies should be formulated to improve mental health and promote clinical prognosis.
1 Introduction
Severe sepsis is a systemic inflammatory response syndrome caused by pathogens invading the blood circulation and is one of the main diseases leading to the death of intensive care patients (1). Continuous renal replacement therapy (CRRT) is widely used in the clinical treatment of severe sepsis as it effectively eliminates inflammatory factors and metabolic waste from the blood while replacing compromised renal function (2). However, long-term clinical observations have revealed that patients with severe sepsis undergoing CRRT often experience significant physical and psychological distress, frequently manifesting issues such as shame, social withdrawal, and cognitive-emotional abnormalities (3).
Resilience, also termed psychological resilience, refers to the developmental phenomenon wherein individuals maintain or restore adaptive functioning following adversity or traumatic experiences (4). Psychological resilience can improve one’s ability to perform daily activities and reduce the adverse consequences of physical dysfunction. Empirical evidence shows a correlation between post-traumatic growth (PTG) and psychological resilience in gynecological cancer patients, pneumonia survivors, and accidental trauma populations (5, 6). However, there is a lack of research to confirm this relationship in patients with severe sepsis.
Cognitive flexibility is the ability of individuals to adjust their cognition flexibly to adapt to the environment in new situations (7). Empirical investigations have established a statistically significant positive correlation between psychological and cognitive flexibility. The development of cognitive flexibility can enhance an individual’s psychological resilience and promote confidence in the face of stress, frustration, and stress. At the same time, some scholars have proposed that the relationship between psychological resilience and PTG can be explained by cognitive flexibility, but the path is not clear (8).
Post-traumatic growth denotes the positive psychological changes that occur when an individual experiences trauma (9). Clinical evidence demonstrates that PTG facilitates the establishment of adaptive self-perception and optimal psychological functioning in patients, thereby improving clinical prognosis (10). Therefore, it is important to study the level of PTG and its related influencing factors in patients with severe sepsis who receive CRRT to improve their psychological state. At the same time, some scholars have proposed that the relationship between psychological resilience and PTG can be explained by cognitive flexibility, but the underlying pathways remain insufficiently elucidated (11, 12).
This study aimed to investigate the pathways through which psychological resilience and cognitive flexibility influence post-traumatic growth in patients with severe sepsis undergoing CRRT, with the goal of providing a scientific foundation for the development of targeted psychological training programs in clinical practice.
2 Materials and methods
2.1 Subjects
From January to October 2024, patients with severe sepsis who underwent CRRT in the Department of Nephrology of our hospital were recruited using convenience sampling. The inclusion criteria were as follows: patients diagnosed with severe sepsis based on clinical manifestations and auxiliary examinations, including imaging and pathology; patients who received CRRT; those with complete clinical data; and patients with sufficient listening, speaking, reading, and writing abilities to complete the study questionnaire during hospitalization. The exclusion criteria included patients with cognitive impairment, those who had previously participated in psychological counseling or other scientific research projects, patients with other serious physical illnesses, and those with a history of mental disorders, such as anxiety or depression, prior to study enrollment.
2.2 Assessment tools
The following assessment tools were used in this study. First, a general information questionnaire was administered to collect demographic and clinical characteristics including age, sex, education level, marital status, monthly household income, payment method, body mass index (BMI), and etiology.
Second, psychological resilience was evaluated using the Connor-Davidson Resilience Scale (CD-RISC), which comprises 25 items across three dimensions: optimism (4 items), strength (8 items), and resilience (13 items). The optimism dimension assesses positive attitudes and future expectations; the strength dimension measures self-confidence and perceived self-efficacy; and the resilience dimension evaluates the ability to cope with adversity and stress. Each item is rated on a 5-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, and 4 = almost always). For example, item 1, “I am able to adapt to change,” is scored from 0 to 4 based on the respondent’s selection. The total score ranges from 0 to 100, with higher scores indicating greater psychological resilience (13). In this study, Cronbach’s α coefficient for the CD-RISC was 0.912, indicating excellent internal consistency.
Third, cognitive flexibility was assessed using the Cognitive Flexibility Scale, which contains 20 items grouped into two dimensions: choice (13 items) and control (7 items). Responses are rated on a 5-point Likert scale (1 = never to 5 = always). Items 2, 4, 7, 9, 11, and 17 are reverse scored. Higher total scores reflect greater cognitive flexibility (14). The scale demonstrated good reliability in this study, with a Cronbach’s α coefficient of 0.896.
Lastly, PTG was measured using the Post-Traumatic Growth Inventory (PTGI), which includes 21 items across five dimensions: appreciation of life (six items), personal strength (three items), relating to others (three items), self-transformation (four items), and new possibilities (four items). Each item is rated on a 6-point Likert scale. PTG was present if the total score was ≥63 (15). The PTGI showed acceptable internal consistency in this study, with a Cronbach’s α coefficient of 0.831.
2.3 Quality control
All questionnaires were distributed and recovered by the researchers. Before filling in, the purpose of this study was explained to the patients, and the instructions were uniformly accepted during the filling process. All questionnaires were collected on the spot, 218 questionnaires were distributed, 13 invalid questionnaires were eliminated, and 205 questionnaires were collected.
2.4 Statistical methods
SPSS 24.0 was used to conduct the common method deviation test, descriptive statistical analysis, and correlation analysis. Counting data are expressed as frequency and rate (%). The measurement data were tested using the Shapiro–Wilk normal distribution, which conforms to the normal distribution and is expressed as the mean ± standard deviation ( ±s). Pearson correlation and multiple linear regression analyses were used for regression analysis. PROCESS was used to test the mediating effect, and the Harman single-factor test was used to check the degree of deviation of the common method in this study. The significance of mediation was tested using the nonparametric percentile bootstrap method. Sampling was repeated 5,000 times, and a confidence interval of 95% was estimated. If the confidence interval did not contain 0, then the mediation effect was significant.
3 Results
3.1 General information of the research object
A total of 218 questionnaires were sent, and 205 valid questionnaires were returned, with an effective recovery rate of 94.04%. The general characteristics of the 205 subjects are presented in Table 1.
3.2 Psychological resilience, cognitive flexibility, and PTG level of patients with severe sepsis treated by CRRT
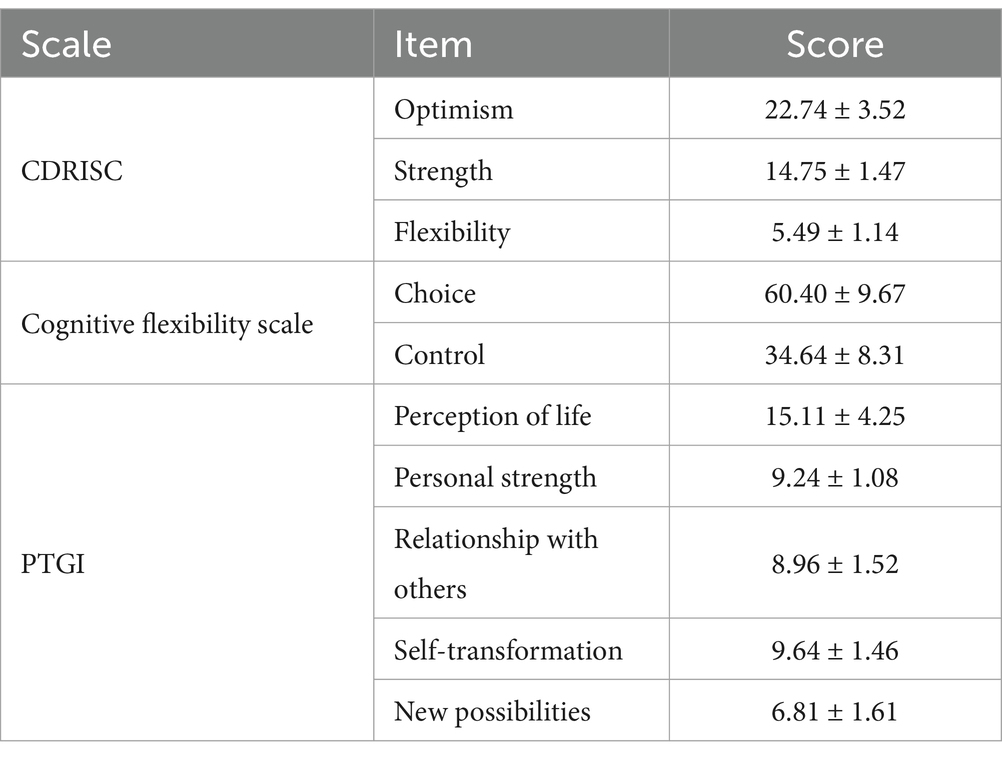
The total score of CDRISC, cognitive flexibility scale, and PTGI in 205 patients was (42.98 ± 6.13), (95.04 ± 17.98) and (49.77 ± 9.92), respectively. The scores for the remaining dimensions are presented in Table 2.
3.3 Correlation analysis of psychological resilience, cognitive flexibility, and PTG level
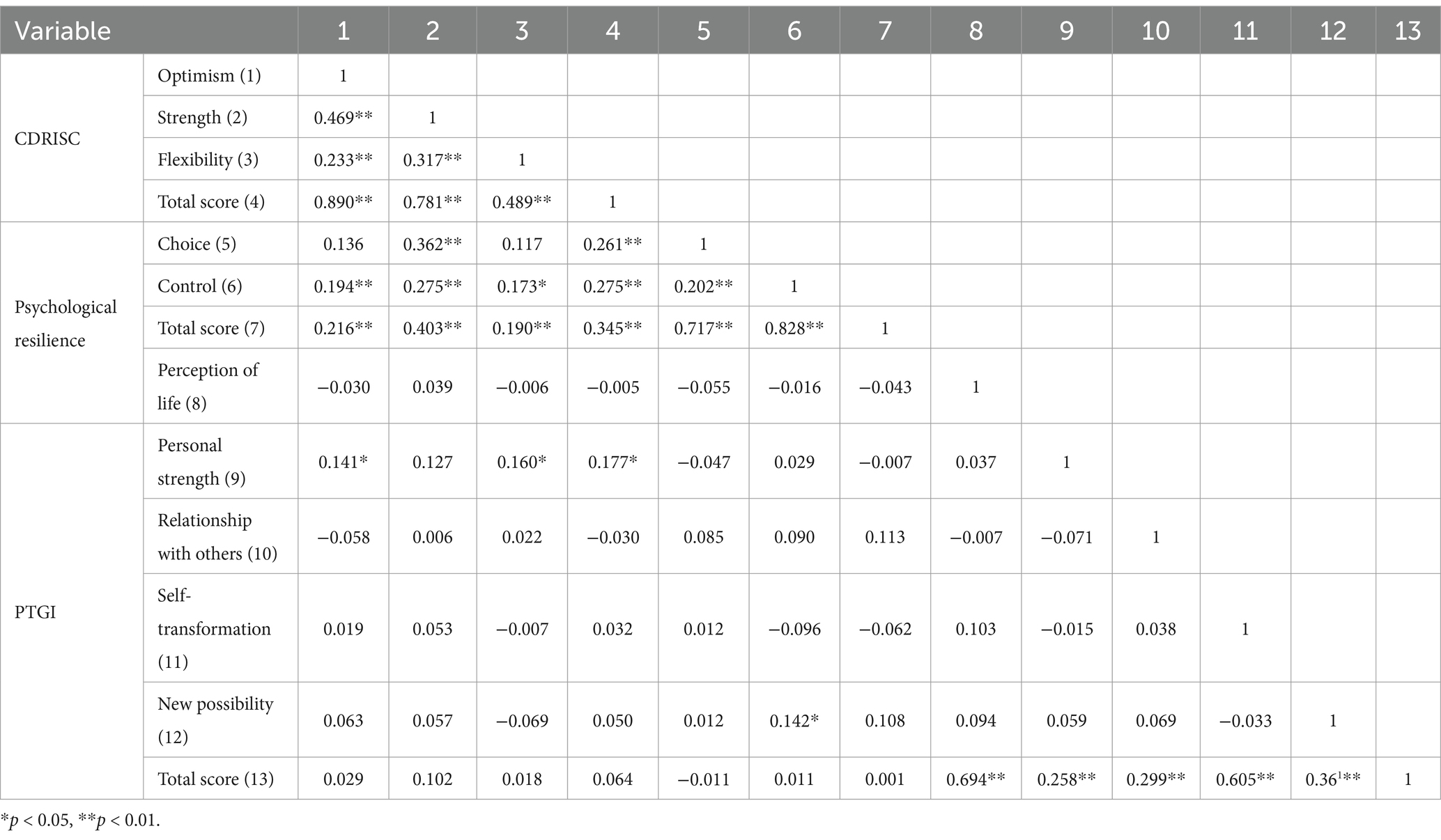
There was a significant positive correlation between psychological resilience, cognitive flexibility, and PTG levels in patients with severe sepsis treated with CRRT (p < 0.05). The correlations of the dimensions of psychological resilience, cognitive flexibility, and the PTG scale are shown in Table 3.
3.4 Analysis of the mediating effect of psychological resilience, cognitive flexibility, and PTG
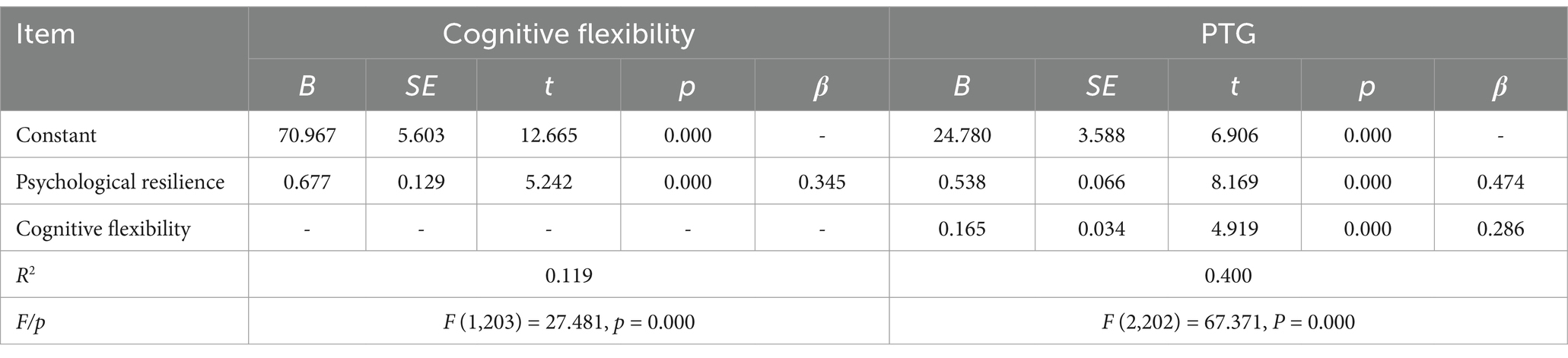
Regression analysis revealed that psychological resilience and cognitive flexibility significantly and positively predicted PTG. Additionally, psychological resilience was found to have a significant positive predictive effect on cognitive flexibility. Both psychological and cognitive resilience exhibited significant direct effects on PTG. Furthermore, cognitive flexibility partially mediated the relationship between psychological resilience and PTG (Table 4).
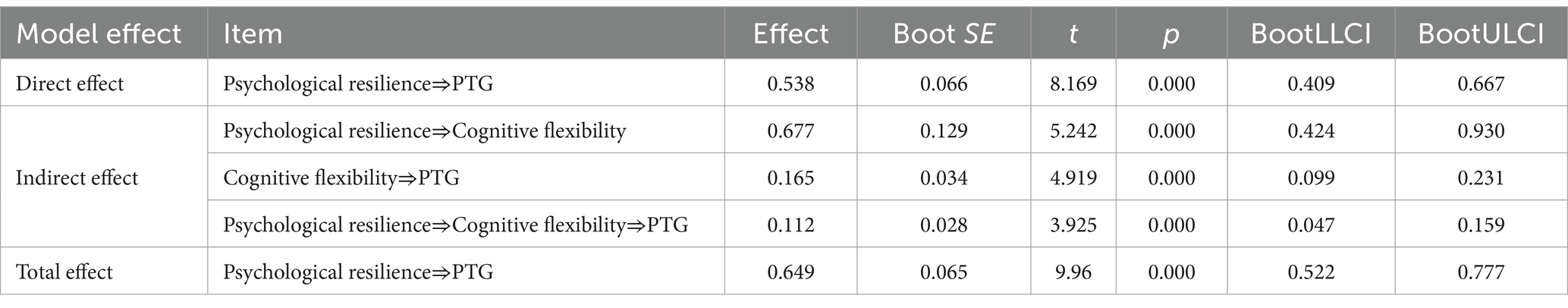
3.5 Mediating effect analysis
Psychological resilience demonstrated a significant direct effect on PTG (β = 0.538, p < 0.001), with a 95% confidence interval (CI) of (0.409, 0.667). An indirect effect was identified through the mediating pathway: psychological resilience → cognitive flexibility → PTG. The size of the indirect effect was calculated as 0.677 × 0.165 = 0.112. A bootstrap test further confirmed the significance of this mediating effect, with a 95% CI of (0.047, 0.159). The indirect effect accounted for 17.3% of the total effect of psychological resilience on PTG. The total effect of psychological resilience on PTG was also statistically significant (β = 0.649, p < 0.001), with a 95% CI of (0.522, 0.777) (Table 5 and Figure 1).

Figure 1. Path diagram of mediating effect of psychological resilience, cognitive flexibility, and PTG in patients with severe sepsis treated by CRRT.
4 Discussion
Sepsis is a significant public health concern in China. In recent years, with the advancement of the positive psychology movement, increasing attention has been directed toward fostering positive mental health in clinical settings (16, 17). In this study, the mean total scores of CD-RISC, the Cognitive Flexibility Scale, and PTGI among 205 patients with severe sepsis undergoing CRRT were 42.98 ± 6.13, 95.04 ± 17.98, and 49.77 ± 9.92, respectively. These scores approximated a median value of 50, indicating a moderate level. This finding aligns with those of previous studies conducted in critically ill populations, including patients undergoing kidney transplantation (18, 19). These results suggest that psychological resilience, cognitive flexibility, and PTG levels in patients with severe sepsis receiving CRRT remain suboptimal and warrant further enhancement.
A plausible explanation for these findings is that severe sepsis is commonly associated with intense physical suffering, high mortality rates, and prolonged medical expenses. These stressors create uncertainty regarding disease prognosis and future life outcomes, which may hinder the development of positive self-perception and thus negatively affect psychological resilience, cognitive flexibility, and PTG levels (20).
This study further explored the mediating and interrelated roles of psychological resilience, cognitive flexibility, and PTG in patients with severe sepsis who underwent CRRT. The findings revealed that psychological resilience and cognitive flexibility significantly and positively predicted PTG. Moreover, a mutually reinforcing relationship was observed between psychological and cognitive flexibilities. Higher levels of these traits were associated with enhanced PTG, which is consistent with previous research (21). This finding supports the conclusion that both psychological resilience and cognitive flexibility are critical contributors to PTG. Enhancing these traits may facilitate the recovery and psychological growth of patients with severe sepsis. Additionally, the results demonstrated that psychological resilience and cognitive flexibility exerted significant chain mediation effects on PTG. These effects were evident through three indirect pathways: the independent effects of psychological resilience and cognitive flexibility as well as their combined mediating role.
A deeper analysis revealed that PTG in patients with severe sepsis reflects their cognitive and emotional restructuring when confronted with life-threatening illness (22). Psychological resilience plays a pivotal role in this process, enabling patients to maintain a proactive outlook on illness management and prognosis, thereby exerting a strong positive influence on PTG (23–25). Furthermore, individuals with high psychological resilience are more likely to adopt adaptive and flexible thinking patterns, thus enhancing cognitive flexibility and reducing susceptibility to anxiety and depression (10). Conversely, individuals with low cognitive flexibility often display rigid thinking and a tendency toward negative cognition, which may cause emotional stagnation, hinder the rational processing of trauma, and obstruct PTG (26, 27). Therefore, cognitive flexibility plays an important role in predicting PTG.
Based on clinical observations, we propose several effective interventions to promote positive mental health among patients with severe sepsis: (1) healthcare providers can encourage patients to engage in meaningful activities within their capability during the recovery phase, helping them to rediscover their self-worth and rebuild self-confidence, thereby facilitating personal transformation; (2) establishing a robust social support system through interpersonal interaction can enhance PTG by providing emotional reinforcement; and (3) mindfulness meditation may also be beneficial, enabling patients to observe themselves and their surroundings objectively, and helping those with negative psychological patterns shift from mental rigidity to greater cognitive and emotional flexibility (28–30).
In summary, psychological resilience exerts both direct and indirect effects on PTG in patients with severe sepsis treated with CRRT, with cognitive flexibility serving as a key mediator. Clinically, the development of targeted psychological interventions is essential for improving mental health outcomes and promoting recovery. However, this study had several limitations. First, the cross-sectional design limits the ability to infer temporal or causal relationships among variables. Second, the sample was restricted to a single geographical region, which may have affected the generalizability of the findings. Future studies should employ longitudinal designs and multi-center recruitment strategies to enhance the robustness and applicability of the results, particularly across diverse patient populations with severe sepsis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Shandong Public Health Clinical Center. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. LZ: Conceptualization, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. HG: Conceptualization, Formal analysis, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. YL: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Writing – review & editing. MS: Conceptualization, Formal analysis, Methodology, Resources, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors wish to thank the research and administrative staff at their respective institutions for their support and contribution to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Srzić, I, Nesek Adam, V, and Tunjić Pejak, D. Sepsis definition: what's new in the treatment guidelines. Acta Clin Croat. (2022) 61:67–72. doi: 10.20471/acc.2022.61.s1.11
2. Zampieri, FG, Bagshaw, SM, and Semler, MW. Fluid therapy for critically ill adults with Sepsis: a review. JAMA. (2023) 329:1967–80. doi: 10.1001/jama.2023.7560
3. Jacobi, J. The pathophysiology of sepsis-2021 update: part 1, immunology and coagulopathy leading to endothelial injury. Am J Health Syst Pharm. (2022) 79:329–37. doi: 10.1093/ajhp/zxab380
4. Troy, AS, Willroth, EC, Shallcross, AJ, Giuliani, NR, Gross, JJ, and Mauss, IB. Psychological resilience: an affect-regulation framework. Annu Rev Psychol. (2023) 74:547–76. doi: 10.1146/annurev-psych-020122-041854
5. Wang, Y, Qiu, Y, Ren, L, Jiang, H, Chen, M, and Dong, C. Social support, family resilience and psychological resilience among maintenance hemodialysis patients: a longitudinal study. BMC Psychiatry. (2024) 24:76. doi: 10.1186/s12888-024-05526-4
6. Nash, RP, Loiselle, MM, Stahl, JL, Conklin, JL, Rose, TL, Hutto, A, et al. Post-traumatic stress disorder and post-traumatic growth following kidney transplantation. Kidney360. (2022) 3:1590–8. doi: 10.34067/KID.0008152021
7. Dell'Osso, L, Lorenzi, P, Nardi, B, Carmassi, C, and Carpita, B. Post traumatic growth (Ptg) in the frame of traumatic experiences. Clin Neuropsychiatry. (2022) 19:390–3. doi: 10.36131/cnfioritieditore20220606
8. Sierra-Murguía, M, Ml, G-S, Navarro-Contreras, G, Peralta-Castillo, G, Padilla-Rico, A, González-Alcocer, L, et al. Relationship between thought style, emotional response, post-traumatic growth (Ptg), and biomarkers in Cancer patients. Int J Environ Res Public Health. (2024) 21:763. doi: 10.3390/ijerph21060763
9. Grant, JE, and Chamberlain, SR. Impaired cognitive flexibility across psychiatric disorders. CNS Spectr. (2023) 28:688–92. doi: 10.1017/S1092852923002237
10. Henson, C, Truchot, D, and Canevello, A. Factors that hinder post-traumatic growth: a systematic review. Encéphale. (2022) 48:560–2. doi: 10.1016/j.encep.2022.02.001
11. Pais, T, Jorge, S, and Ja, L. Acute kidney injury in Sepsis. Int J Mol Sci. (2024) 25:5924. doi: 10.3390/ijms25115924
12. Desposito, L, and Bascara, C. Review: sepsis guidelines and core measure bundles. Postgrad Med. (2024) 136:702–11. doi: 10.1080/00325481.2024.2388021
13. Liu, YC, Yao, Y, Yu, MM, Gao, YL, Qi, AL, Jiang, TY, et al. Frequency and mortality of sepsis and septic shock in China: a systematic review and meta-analysis. BMC Infect Dis. (2022) 22:564. doi: 10.1186/s12879-022-07543-8
14. Lakbar, I, Maakaron, E, Leone, M, Delamarre, L, Dk, Y, Tran, B, et al. Severe mental illness and mortality in sepsis and septic shock: a systematic review and meta-analysis. Mol Psychiatry. (2024) 29:3857–64. doi: 10.1038/s41380-024-02603-8
15. Magne, H, Jaafari, N, and Voyer, M. Post-traumatic growth: some conceptual considerations. Encéphale. (2021) 47:143–50. doi: 10.1016/j.encep.2020.05.021
16. Miglani, M, Upadhyay, P, Mahajan, R, Mishra, BP, Sharma, T, Mohan, B, et al. Psychological resilience, coping, and distress in admitted patients with Covid-19 infection. Prim Care Companion CNS Disord. (2022) 24:21m03230. doi: 10.4088/PCC.21m03230
17. Chien, CH, Pang, ST, Chuang, CK, Liu, KL, Wu, CT, Yu, KJ, et al. Exploring psychological resilience and demoralisation in prostate cancer survivors. Eur J Cancer Care. (2022) 31:e13759. doi: 10.1111/ecc.13759
18. Wang, J, Li, S, Hu, Y, Ren, L, Yang, R, Jiang, Y, et al. The moderating role of psychological resilience in the relationship between falls, anxiety and depressive symptoms. J Affect Disord. (2023) 341:211–8. doi: 10.1016/j.jad.2023.08.060
19. Almutlaq, BA, Almohaimeed, LA, Kahin, SA, and Alsubaie, MS. Psychological resilience and well-being among a sample of Saudi. Saudi Med J. (2024) 45:963–7. doi: 10.15537/smj.2024.45.9.20240467
20. Cai, Z, and Qi, B. Cognitive flexibility as a protective factor for empathy. Front Psychol. (2022) 13:1064494. doi: 10.3389/fpsyg.2022.1064494
21. Wang, Z, Chen, X, Zhou, J, Ay, L, and Li, Q. Posttraumatic growth in colorectal cancer survivors: a systematic review. Clin Psychol Psychother. (2023) 30:740–53. doi: 10.1002/cpp.2838
22. Novak, LA, Carter, SP, JM, LC, Perera, KU, Neely, LL, Soumoff, A, et al. Cognitive flexibility and suicide risk indicators among psychiatric inpatients. Psychiatry Res. (2022) 313:114594. doi: 10.1016/j.psychres.2022.114594
23. HA, MP, Kim, KL, Seymour, KE, Wolff, J, Esposito-Smythers, C, Spirito, A, et al. Cognitive flexibility and impulsivity deficits in suicidal adolescents. Res Child Adolesc Psychopathol. (2022) 50:1643–56. doi: 10.1007/s10802-022-00952-y
24. Dell'Osso, L, Carpita, B, Nardi, B, Bonelli, C, Calvaruso, M, and Im, C. Biological correlates of post-traumatic growth (Ptg): a literature review. Brain Sci. (2023) 13:305. doi: 10.3390/brainsci13020305
25. Hao, R, Han, P, Wang, L, and Zhang, Y. The effect of the social support on Ptsd and Ptg about university student volunteers in the prevention and controlling of coronavirus: with coping style as the intermediary. Front Psychol. (2023) 14:1152823. doi: 10.3389/fpsyg.2023.1152823
26. Ning, J, Tang, X, Shi, H, Yao, D, Zhao, Z, and Li, J. Social support and posttraumatic growth: a meta-analysis. J Affect Disord. (2023) 320:117–32. doi: 10.1016/j.jad.2022.09.114
27. Park, YJ, and Lee, KS. Scoping review protocol of post-traumatic growth (Ptg) in Korean cancer survivors. BMJ Open. (2024) 14:e077896. doi: 10.1136/bmjopen-2023-077896
28. Gower, T, Pham, J, En, J, Rosenfield, D, and Hj, B. Cognitive biases in perceptions of posttraumatic growth: a systematic review and meta-analysis. Clin Psychol Rev. (2022) 94:102159. doi: 10.1016/j.cpr.2022.102159
29. Imran, A, Tariq, S, Kapczinski, F, and de Azevedo Cardoso, T. Psychological resilience and mood disorders: a systematic review and meta-analysis. Trends Psychiatry Psychother. (2024) 46:e20220524. doi: 10.47626/2237-6089-2022-0524
Keywords: severe sepsis, continuous renal replacement therapy, psychological resilience, cognitive flexibility, post-traumatic growth
Citation: Zhao C, Zhou L, Gao H, Lu Y and Shi M (2025) Relationship between psychological resilience, cognitive flexibility and post-traumatic growth level in patients with severe sepsis treated by continuous renal replacement therapy. Front. Public Health. 13:1589223. doi: 10.3389/fpubh.2025.1589223
Edited by:
Shusen Sun, Western New England University, United StatesReviewed by:
Long Meng, First Affiliated Hospital of Chongqing Medical University, ChinaChunhua Zhou, The First hospital of Hebei Medical University, China
Copyright © 2025 Zhao, Zhou, Gao, Lu and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: MiaoMiao Shi, MTM4NTMxNDI3MjBAMTYzLmNvbQ==
 Changzheng Zhao1
Changzheng Zhao1 MiaoMiao Shi
MiaoMiao Shi