- 1Department of Nursing, West China Second University Hospital, Sichuan University/ West China School of Nursing, Sichuan University, Chengdu, China
- 2Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, China
- 3Department of Obstetric Nursing, West China Second University Hospital, Sichuan University/ West China School of Nursing, Sichuan University, Chengdu, China
Background: Fear of childbirth is a common concern among pregnant women, potentially affecting maternal physical and mental health as well as birth outcomes. However, the factors influencing fear of childbirth are still being explored. This study aims to assess the prevalence of fear of childbirth among women in late pregnancy and identify associated factors, with a particular focus on pregnancy comorbidities, complications, and specific obstetric conditions.
Methods: A cross-sectional study was conducted from October 2022 to March 2024 at a tertiary women’s and children’s hospital in western China. A total of 6,335 pregnant women were recruited. The Childbirth Attitude Questionnaire was used to measure fear of childbirth. Data on pregnancy comorbidities, complications, and specific obstetric conditions were extracted from the hospital information system. Ordinal logistic regression was performed to analyze factors associated with different levels of fear of childbirth.
Results: The mean score of the Childbirth Attitude Questionnaire was 34.69 ± 8.15. 79.8% of the participants reported mild to severe fear of childbirth in late pregnancy. Ordinal logistic regression analysis identified several significant risk factors for severe fear of childbirth, including lower education level, primiparity, no history of uterine scarring, natural conception, intention to have a cesarean section, high myopia, and urinary disease.
Conclusion: Fear of childbirth is highly prevalent among women in late pregnancy and is influenced by multiple factors, including pregnancy comorbidities and complications. Obstetric healthcare providers should be aware of fear of childbirth and consider both sociodemographic and obstetric characteristics when implementing targeted interventions and counseling to support high-risk groups.
1 Introduction
Pregnancy and childbirth are significant stages in a woman’s life. During this period, women transition into motherhood while experiencing significant physiological and psychological changes. In addition to routine prenatal care for pregnant women, the identification and timely management of psychological issues should not be neglected. Fear of childbirth (FOC) is a psychological condition characterized by anxiety or unease during pregnancy and birth, which can significantly impact the physical and psychological well-being of pregnant women during pregnancy and childbirth (1), even in the postpartum period (2). Epidemiological data show that the prevalence of FOC varies widely, ranging from 12 to 58.6% across different countries and regions (2, 3), which is influenced by cultural factors, healthcare standards, and the tools used to measure FOC (4). Despite varying rates, studies consistently highlight the widespread prevalence and severity of FOC. Approximately 33% of pregnant women experience FOC in late pregnancy, with 11–14% experiencing severe fear and requiring medical intervention (2).
Research shows that FOC in pregnant women changes as pregnancy progresses (5, 6), and the prevalence of FOC significantly increases in late pregnancy (7). FOC in late pregnancy may have varying degrees of short-term and long-term effects on maternal and neonatal outcomes. In the short term, FOC influences pregnant women’s preferences for birth methods, the progression of birth, and the childbirth experience. Evidence suggests that FOC is a significant factor contributing to the increase in unnecessary cesarean sections (8, 9) because of the declining willingness of women to undergo vaginal birth (10). Severe FOC may lower the pain threshold, heighten pain perception, and magnify the sensation of labor pain (11, 12), leading many women to select cesarean sections as a safer and less painful choice. In terms of the progression of birth, FOC can result in increased plasma catecholamine levels, which may cause insufficient uterine contractions and prolong the stages of birth (13, 14). An extended duration of birth often increases discomfort, further reinforcing pregnant women’s demand for medical interventions, including cesarean sections and epidural analgesia (15, 16). FOC can significantly impact maternal and neonatal outcomes, as well as future pregnancies. If women experience severe FOC during their current pregnancy, that experience can result in adverse fetal outcomes, including abnormal heart rhythms, low APGAR scores, and low birth weight (14). Additionally, women may experience post-traumatic stress disorder after birth, which could recur in subsequent pregnancies (17). Women who experience FOC are more likely to develop psychological disorders in the postpartum period, such as postpartum depression and anxiety, which may further impact their willingness and breastfeeding behavior (18). The severity of FOC varies between individuals, and the duration of its long-term effects also differs. Therefore, identifying factors influencing FOC in late pregnancy, providing accurate childbirth information, and implementing targeted interventions are crucial for decreasing the impact of FOC.
Previous research on factors influencing FOC primarily focuses on sociodemographic or psychological variables, such as maternal age, educational level, anxiety, or depression (19, 20), while the impact of pregnancy comorbidities, complications, or specific obstetric conditions remains underexplored. Therefore, we conducted a large-scale cross-sectional study to (1) investigate the prevalence of FOC in late pregnancy and (2) identify its associated factors, particularly pregnancy comorbidities, complications, and specific obstetric conditions, which may aid obstetric healthcare providers in accurately identifying and managing high-risk individuals with severe FOC.
2 Methods
2.1 Setting
The study was conducted from October 2022 to March 2024 at a women’s and children’s tertiary hospital in Sichuan Province, China. As a leading referral center in western China, the hospital receives a high volume of deliveries each year and provides care for pregnant and postpartum women from a wide catchment area, including both urban and rural regions across multiple provinces. It specializes in the management of high-risk and critically ill pregnancies, offering services for a broad range of obstetric conditions and diverse demographic groups. This setting provides a valuable foundation for investigating maternal health issues, including fear of childbirth, in regional and under-resourced populations. Pregnant women who undergo routine prenatal checks at this hospital have a unique identification number, which helps distinguish individuals by their names and allows healthcare staff to identify them accurately.
2.2 Participants
This study used a consecutive sampling strategy, enrolling all eligible pregnant women who met the inclusion criteria and provided informed consent. The inclusion criteria were as follows (1): Age ≥18 years (2); Gestational age ≥28 weeks (3); Participants with singleton pregnancies (4); Absence of mental illness; and (5) Participants were required to communicate effectively in Mandarin and complete the questionnaires independently. In this study, “primiparous” refers to women who have not previously given birth to a viable infant, which may include those who have had prior pregnancies but no deliveries. This is distinct from “first-time pregnant” women, who are experiencing their first pregnancy. As the study design involved the full inclusion of all eligible participants during the data collection period, no formal a priori sample size calculation was conducted. However, the final sample of 6,335 participants provided a sufficiently large and representative dataset for robust multivariable analysis.
2.3 Measurement
Sociodemographic and selected obstetric information were collected through a self-designed questionnaire. Sociodemographic information included age, ethnicity, residence, education level, employment status, and monthly per capita family income. Selected obstetric information included gestational age, number of pregnancies, whether conceived by in vitro fertilization-embryo transfer (IVF-ET), and intended mode of childbirth. Additional obstetric information, such as pregnancy comorbidities, complications, and specific obstetric conditions, was obtained from the hospital information system by matching each participant’s identification number. Participants’ FOC was assessed with the Childbirth Attitude Questionnaire (CAQ). This instrument was originally designed by Areskog et al. (21), further developed by Lowe (22), and Tanglakmankhong (23). It was subsequently translated and validated for use in Chinese populations by Juan et al. (24). The translation process followed standard procedures, including forward and backward translation, expert review, and pilot testing. The CAQ contains 16 items and is scored using a 4-point Likert scale from 1 (not afraid) to 4 (very afraid). Scores ranging from 16 to 27, 28 to 39, 40 to 51, and 52 to 64 represent low, mild, moderate, and severe FOC, respectively. A high score indicates that a woman is fearful. The Chinese version of the CAQ has been widely used in studies involving Chinese pregnant women and has demonstrated good applicability and measurement properties in this context (25, 26). In the present study, the scale also showed excellent internal consistency, with a Cronbach’s alpha coefficient of 0.902.
2.4 Data collection
We used paper questionnaires for data collection. Four investigators, trained by the principal researchers, recruited pregnant women in late pregnancy during routine antenatal checks at the obstetric clinic to complete the questionnaires. Before participation, all participants were required to sign an informed consent form and offer their correct identification number, then they could receive the questionnaires. To protect participant privacy, the identification number was used solely for matching questionnaire data with the Hospital Information System and was not linked to names, phone numbers, or other personally identifiable information. No identifiable data were collected on the paper questionnaires. Only authorized members of the research team had access to the ID-hospital data mapping file, which was securely stored in a password-protected system. Participants had the right to decline participation or withdraw from the study at any time. Investigators reviewed the questionnaires on the spot. If any items were left blank, participants were prompted to fill them in immediately. However, questionnaires with more than 20% missing data were considered invalid and excluded. Following data collection, two investigators independently cross-checked the questionnaires to ensure accuracy. Subsequently, the main researcher and another researcher entered the data into the Epidata software. Pregnancy comorbidities, complications, and obstetric information were retrieved from the Hospital Information System using the participants’ identification number. These clinical diagnoses were recorded in the Hospital Information System by attending physicians. The diagnoses followed the International Classification of Diseases, 10th Revision (ICD-10) coding system and were based on established national clinical guidelines. The hospital employs a standardized multi-level quality control process for medical records to ensure diagnostic accuracy and consistency, including physician verification, departmental audits, and periodic reviews by the medical records department. To enhance analytical reliability, we categorized clinically related conditions into broader diagnostic groups as described in Table 1, which helped address potential variations in specific coding practices. Finally, data from the paper questionnaires were matched with the corresponding hospital records. We received a total of 6,335 valid questionnaires.
2.5 Data statistics
All statistical analyses were performed using IBM SPSS 27.0 software. The total score of the Childbirth Attitude Questionnaire, as a continuous variable, was normally distributed and presented as mean ± standard deviation (SD). Sociodemographic, obstetric information, and levels of FOC were categorical variables, shown as frequencies (n) and percentages (%). As the categorical variables did not follow normal distributions, non-parametric tests were used to identify potential factors influencing levels of FOC. The Mann–Whitney U test was used for two-group comparisons, and the Kruskal-Wallis H test was applied for comparisons among multiple groups. To further explore factors independently associated with different levels of FOC, variables that were significantly associated with FOC in the univariate analysis (p < 0.05) were simultaneously entered into an ordinal logistic regression model. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to assess the strength of association while controlling for potential confounding among predictors. The proportional odds assumption was tested using the test of parallel lines in SPSS. The results showed that this assumption was not violated (p > 0.05), indicating that the ordinal logistic regression model was appropriate for the data. A two-tailed p-value of less than 0.05 was considered statistically significant.
2.6 Ethics approval
This study was approved by the Ethics Committee of West China Second University Hospital, Sichuan University, with ethics approval number 2022 (191). Informed consent was obtained from all participants. Participants identified as having a severe FOC based on questionnaire responses were not directly intervened with by the research team. However, their results were flagged and communicated to their designated obstetricians during antenatal care. A corresponding note was placed in their medical records to prompt closer emotional observation. In cases where obstetricians observed signs of significant psychological distress (e.g., anxiety or depression), a referral to the hospital’s psychological counseling clinic was advised, following standard clinical pathways.
3 Result
3.1 Sociodemographic and obstetric characteristics of participants
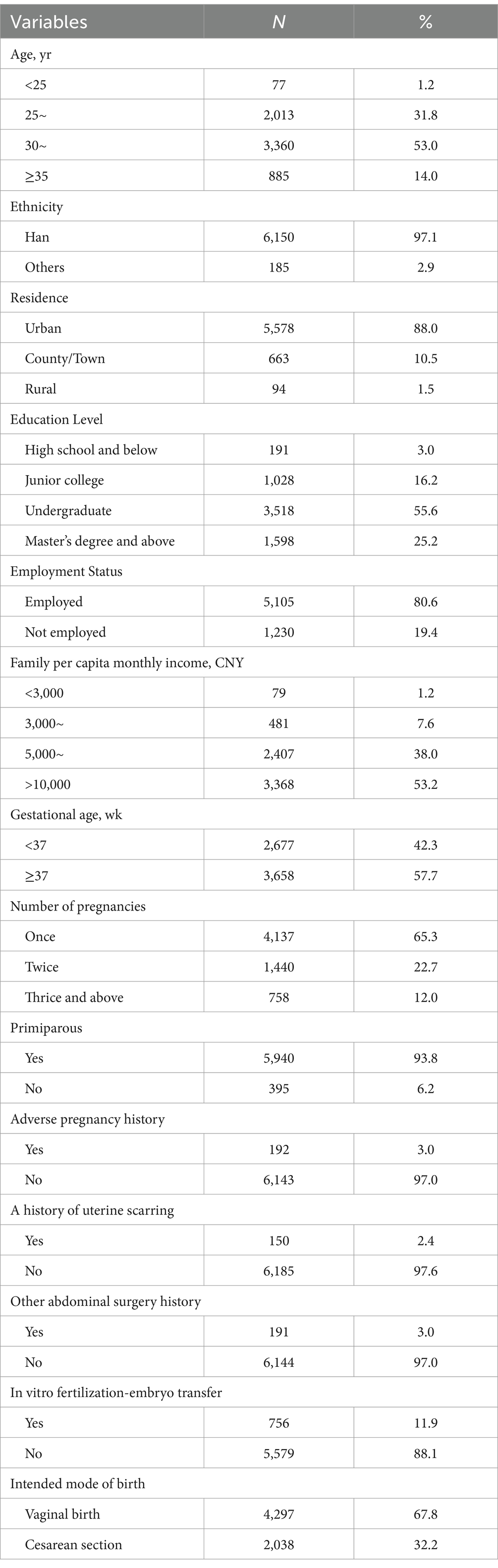
A total of 14.0% of participants were of advanced maternal age (≥35 years). Approximately 57.7% (n = 3,658) of the participants were at or beyond 37 weeks of gestation. A total of 65.3% of participants were pregnant for the first time, while 93.8% were primiparous. Additionally, 192 participants had a history of adverse pregnancy outcomes. 11.9% (n = 756) of participants conceived through IVF-ET. Furthermore, 67.8% (n = 4,297) of the participants intended to have a vaginal birth. The specific demographic and obstetric characteristics are presented in Table 2.
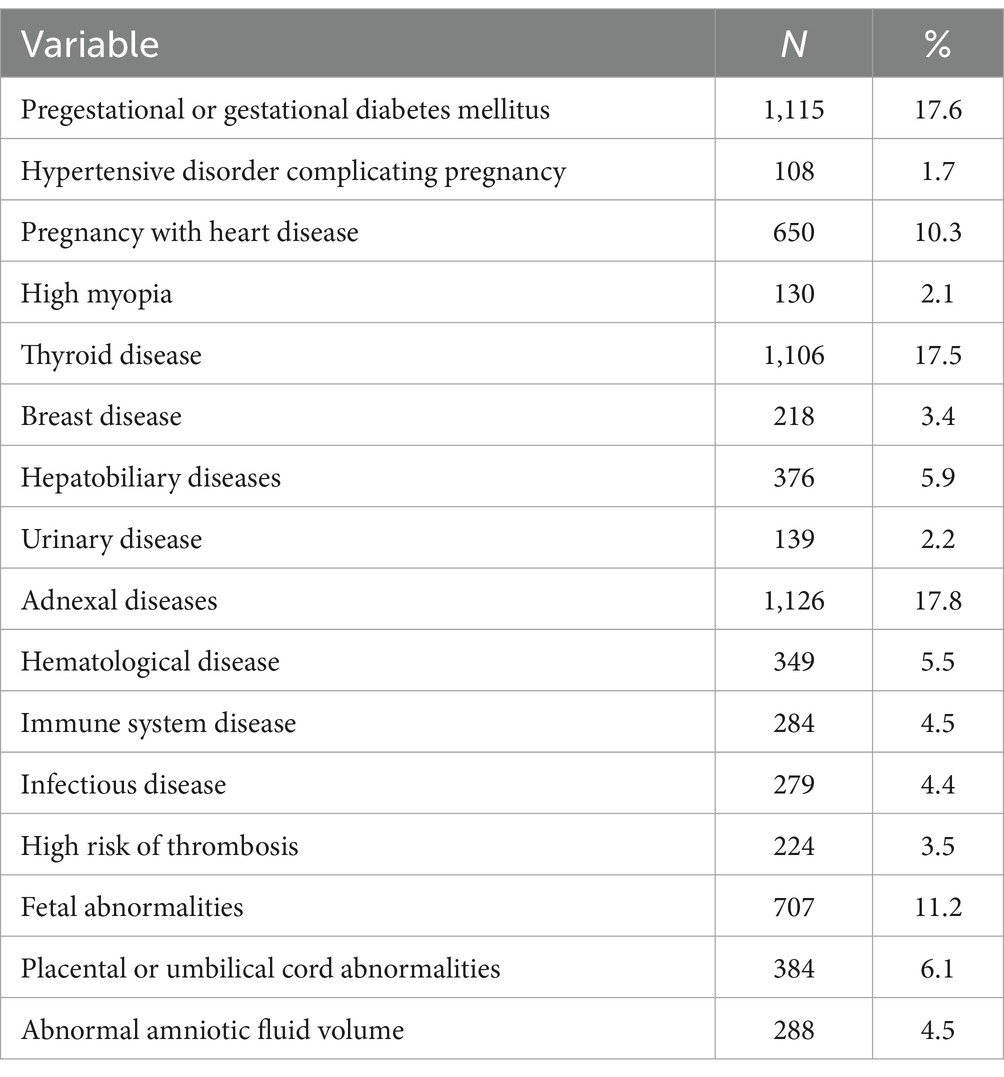
3.2 Pregnancy comorbidities, complications, and specific obstetric conditions of participants
We retrieved all participants’ pregnancy comorbidities, complications, and related abnormalities from the hospital information system and categorized these conditions as shown in Table 1. Thyroid diseases in the classification included hypothyroidism, hyperthyroidism, Hashimoto’s thyroiditis, and thyroid cancer. Breast diseases comprised hyperplasia of mammary glands, breast cysts, and breast cancer. Hepatobiliary diseases included hepatic cysts, liver hemangiomas, hepatitis, intrahepatic cholestasis of pregnancy, cholecystolithiasis, gallbladder polyps, and cholecystitis. Urinary diseases included hydronephrosis, renal cysts, nephrolithiasis, and ureteral calculi. Adnexal diseases encompassed cervical cancer, uterine fibroids, adenomyosis, ovarian cysts, and polycystic ovary syndrome. Hematological diseases included iron deficiency anemia, Mediterranean anemia, and thrombocytopenia. Immune system diseases included antiphospholipid syndrome and systemic lupus erythematosus. Infectious diseases included viral hepatitis and syphilis. Pregestational or gestational diabetes mellitus (17.6%), thyroid disease (17.5%), and adnexal disease (17.8%) were the most prevalent comorbidities. Hypertensive disorders complicating pregnancy (1.7%), high myopia (2.1%), and urinary disease (2.2%) had the lowest prevalence.
Among other special obstetric conditions, fetal abnormalities were the most prevalent, accounting for 11.2%. These mainly included fetal growth restriction, congenital heart disease, renal collecting system separation, or abnormalities in the appearance. Placental and umbilical cord abnormalities included velamentous cord insertion, placenta previa, and single umbilical artery. Amniotic fluid abnormalities included polyhydramnios and oligohydramnios.
3.3 Participants’ levels of fear of childbirth
The mean total score of the questionnaires was 34.69 ± 8.15. Based on these scores, 79.8% (n = 5,060) of the pregnant women experienced varying degrees of FOC during late pregnancy. Specifically, 53.5% (n = 3,391) of the participants reported mild FOC, 1,466 (23.1%) reported moderate fear, and 203 (3.2%) reported severe FOC.
3.4 Individual participant characteristics and fear of childbirth
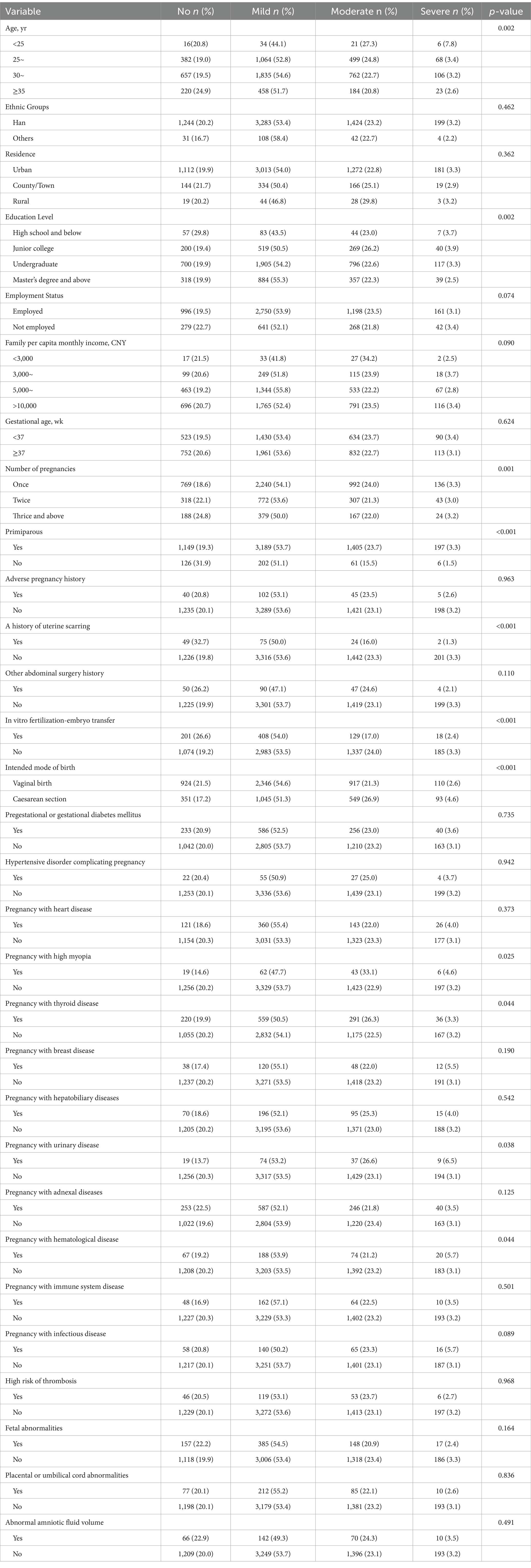
Table 3 compares the levels of FOC among participants with different characteristics. Older pregnant women (≥35 years) reported a higher proportion of no FOC (24.9%) compared to younger groups (p = 0.002). The level of FOC differed significantly among participants with different educational levels (p = 0.002). First-time pregnant women reported higher levels of fear than women who had two or more pregnancies (p = 0.001). Primiparous women reported higher levels of FOC compared to multiparous women (p < 0.001). Women with a history of uterine scarring showed lower levels of FOC compared to those without (p < 0.001). Women who conceived via IVF-ET had lower levels of fear compared with women who had natural pregnancies (p < 0.001). A statistically significant difference (p < 0.001) was observed in the level of FOC between participants intending to have a vaginal birth and those intending to have a cesarean section. Statistically significant differences in FOC were also observed among participants with certain complications. These included high myopia (p = 0.025), thyroid disease (p = 0.044), urinary disease (p = 0.038), and hematological disease (p = 0.044).
3.5 Factors influencing the level of fear of childbirth in late pregnancy
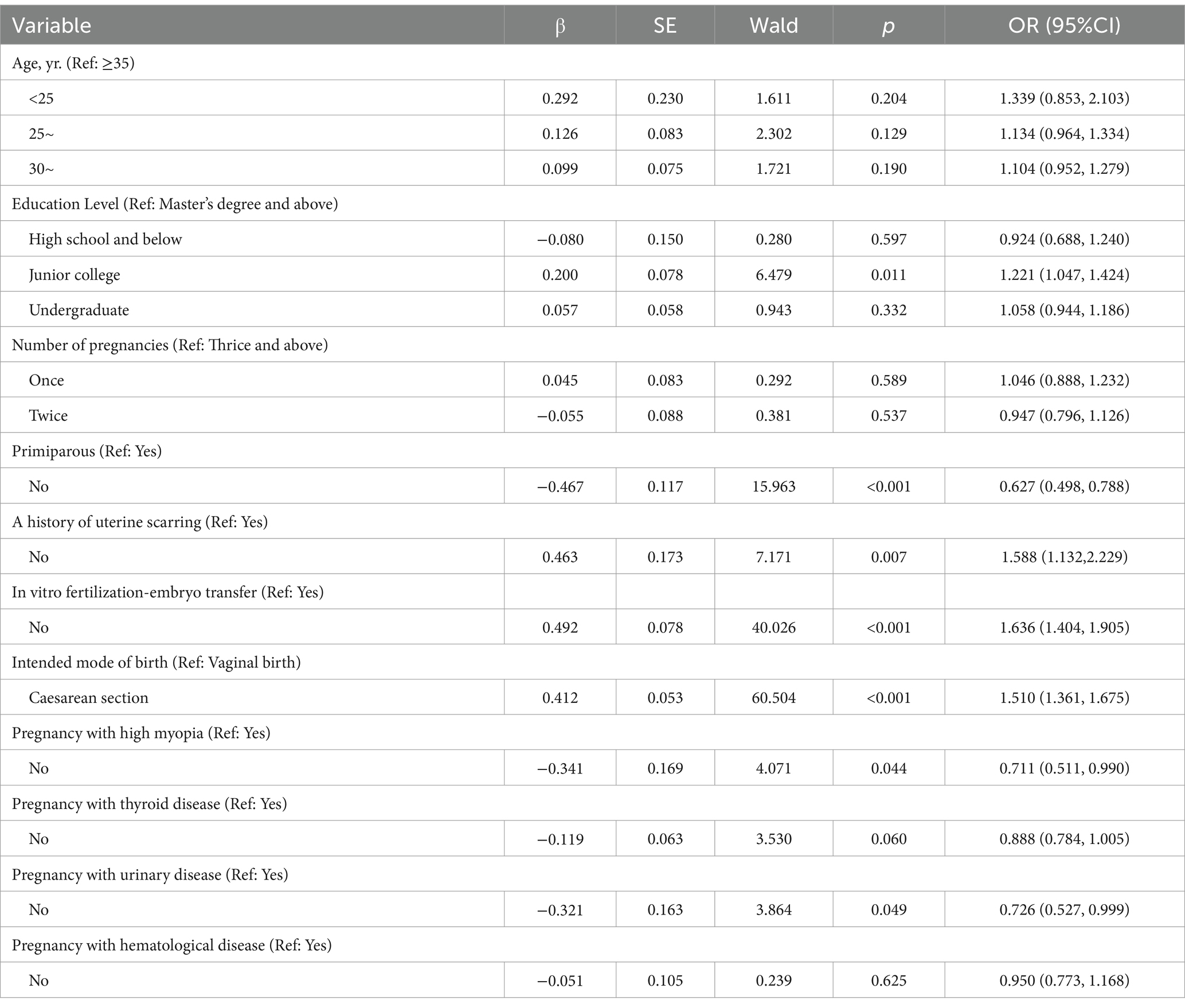
The aforesaid statistically significant variables were used as inputs for ordinal logistic regression analysis (Table 4). Age, number of pregnancies, pregnancy with thyroid disease, and hematological disease were not statistically significant in the regression equation (p > 0.05). Participants with a junior college education had significantly higher levels of FOC than those with a master’s degree and above (OR = 1.221, 95%CI: 1.047, 1.424), while no significant difference was observed in other education levels. Primiparous women had a high risk of severe FOC levels compared to multiparous women (OR = 0.627, 95%CI: 0.498, 0.788). Women without a history of uterine scarring had higher levels of FOC compared to those with a history of uterine scarring (OR = 1.588, 95%CI: 1.132, 2.229). Women who conceived naturally had higher levels of FOC compared to those who conceived via IVF-ET (OR = 1.636, 95%CI: 1.404, 1.905). Participants intending to have a cesarean section had higher levels of FOC compared to those intending a vaginal birth (OR = 1.510, 95%CI: 1.361, 1.675). Pregnant women without high myopia (OR = 0.711, 95%CI: 0.511, 0.990) and urinary disease (OR = 0.726, 95%CI: 0.527, 0.999) had a lower level of FOC compared to those with these conditions.
4 Discussion
4.1 The fear of childbirth prevalence among women in late pregnancy
In this cross-sectional study, we investigated the prevalence and influencing factors of FOC among 6,335 women in late pregnancy. We focused on pregnancy comorbidities, complications, and specific obstetric conditions. We found that 1,669 participants (26.3%) experienced moderate to severe FOC during late pregnancy. The mean FOC score was 34.69 (SD = 8.15), which was higher than those reported in similar studies using the same tool in other regions of China (25–27). This difference might be due to differences in gestational age or previous childbirth experience, which significantly affect levels of FOC (25, 28, 29). The score in our study was higher than that reported in Greece (30), but lower than that of women in Pakistan (31). It is important to recognize that countries may differ significantly in living conditions, ethnicity, religion, and social structures, all of which may influence the perception and assessment of the FOC (27). Additionally, questionnaire scores may not fully capture the complexity of FOC. Consequently, we further analyzed the prevalence of FOC and found that 79.8% of women in late pregnancy experienced varying levels of fear. This percentage was calculated by combining the proportions of participants categorized as having mild, moderate, or severe FOC based on the CAQ scoring criteria. The result is similar to a study conducted in Chongqing, also a city in western China, in which the reported prevalence of 75.15% was measured with the same assessment tool (32). However, it was higher than the level reported in a coastal city in eastern China (20). This variation may be associated with differences in healthcare quality, socioeconomic factors, and access to healthcare between eastern and western China; healthcare quality is known to affect FOC (33). Additionally, our study setting as a tertiary referral center in western China may have contributed to the higher prevalence, as our population included more high-risk pregnancies and patients from diverse socioeconomic backgrounds and underserved areas. Moreover, the prevalence of FOC in our study was slightly higher than that reported in Middle Eastern countries, such as Egypt and Iran, where prevalence ranged from 70.4 to 71.5% (14, 34). These differences could be attributed to differences in religious and cultural norms (4). The fact that prevalence exceeds 70% regardless of geographic, cultural, or social conditions emphasizes the fact that FOC is a common issue among women in late pregnancy.
In our study, 3.2% of participants experienced severe FOC, a proportion comparable to that reported in a study from Finland (35), but lower than the 8.1% reported in Turkey and 12% in Brazil (36, 37). These differences may be related to the use of different measurement tools, but they also reflect the widespread prevalence and potential clinical implications of FOC. It is important for obstetric healthcare providers to be attentive to the FOC, particularly among women with severe FOC, and to implement targeted interventions.
4.2 Influencing factors of fear of childbirth in late pregnancy
On the basis of demographic factors, we identified numerous variations in FOC among women in late pregnancy, and we examined the presence of pregnancy comorbidities, complications, and special obstetric conditions. Our findings show that young women are more likely to experience moderate to severe FOC. These findings are similar to research by Elsharkawy et al., and they suggest that young women may be more prone to high levels of fear because of their lack of experience and uncertainty in the childbirth process (34). Our results contradict reports of Huang et al. and Räisänen et al., who found that older pregnant women had higher levels of fear, possibly because of concerns about their own health or potential pregnancy complications (25, 28). However, our regression analysis revealed that age was not a statistically significant factor influencing the level of FOC in late pregnancy (p > 0.05); thus, factors other than age may be more influential. Nevertheless, women of all ages experience FOC. Therefore, it is essential to ensure that pregnant women of all age groups receive adequate attention and support to alleviate their fears. We found that women with a junior college education, compared with women having a master’s degree and above, were more likely to experience a higher level of FOC (OR = 1.221, 95%CI: 1.047, 1.424). An association between low educational level and severe fear in late pregnancy is consistent with the findings of Gao et al. and Laursen et al. (38, 39). Such an association may exist because women with low education lack knowledge about childbirth or have limited access to comprehensive health information (40), making them more prone to anxiety or worry. In contrast, women with high education levels tend to experience less fear, possibly because they easily obtain and understand information related to childbirth (41), which enhances their confidence. Thus, there may be a need to provide better support and health information to women who have more limited education (42).
First-time pregnant women, particularly primiparas, had a high prevalence of moderate to severe fear. The regression analysis demonstrated that being a primipara was statistically significant (p < 0.001), establishing it as an important factor influencing the level of FOC in late pregnancy. This finding is similar to research by Adams et al., and it suggests that primiparas have a higher FOC because of their lack of practical childbirth experience and uncertainty about the birth process (13), particularly labor pain (43). These results revealed the need for obstetric healthcare professionals to provide enhanced support and education to primiparas, instructing them in acquiring knowledge about childbirth. We found that pregnant women with a history of uterine scarring experienced less FOC in late pregnancy, and this condition was a significant influence in regression analyses (p = 0.007, OR = 1.588, 95%CI: 1.132, 2.229). A scarred uterus is usually the result of a cesarean section or other uterine surgery. Women who have experienced such surgery may have a greater awareness of the risks of birth; thus, they have more realistic expectations of subsequent births. However, our finding contrasts with the findings of Sluijs and Hou (44, 45). Phunyammalee et al. found that the level of childbirth fear of women with a history of uterine scarring due to previous cesarean sections was similar to that of women without cesarean sections (46). This finding may be attributed to the fact that experienced women received better care during their previous cesarean sections, which resulted in reduced fear of subsequent childbirth. Although there are some differences in results, they all suggested that healthcare providers need to ensure that appropriate support and attention is provided to this group. Our results showed that women with natural pregnancies had higher fear levels than women who conceived via IVF-ET, and planned vaginal childbirth was a significant factor influencing FOC in late pregnancy. This finding may be due to the fact that women who conceive via IVF-ET usually receive more medical monitoring and psychological support because of the longer treatment process, which could enhance their understanding of pregnancy and birth. Women with natural pregnancies may have lacked this intensive medical support, leading to more anxiety about birth. Women intending to have cesarean section had higher fear levels than women planning vaginal births (OR = 1.510, 95%CI = 1.361, 1.675), which is similar to findings by Størksen and Haines (47, 48). The preference of pregnant women for cesarean section may exist because of a strong fear of labor pain (49), the prolonged duration of birth (50), and the belief that natural birth is more unpredictable (51). Additionally, the intended mode of birth is a significant factor in the FOC, suggesting that understanding a woman’s birth intention and providing targeted psychological support and information about birth options may help to alleviate the FOC.
Pregnant women with high myopia, thyroid disease, urinary disease, or hematological disease had higher levels of FOC in late pregnancy, with high myopia and urinary disease identified as influencing factors of FOC in this study. Our results show that pregnant women without myopia had 0.711 times (95%CI = 0.511, 0.990) lower risk of severe FOC in late pregnancy compared with women who had myopia. Some pregnant women fear that exertion during vaginal birth could lead to retinal detachment, but there is no evidence that high myopia increases the risk of retinal detachment during birth (52). Among our study participants, urinary disease was mainly nephritis or hydronephrosis. Birth may increase the burden on the kidneys (53), which may be a plausible explanation for why pregnant women with urinary disease fear that childbirth could harm their urinary health. Although thyroid disease and hematological diseases were not identified as factors influencing FOC, they are still worth considering. Pregnant women with thyroid disease may need to continue medication during pregnancy; fluctuations in thyroid hormone levels can affect emotions, leading to anxiety or depression (54), which may increase FOC. Furthermore, some pregnant women had anemia, which could raise concerns about the risk of blood loss during vaginal birth or cesarean section, thereby raising FOC. Although these conditions do not directly influence FOC, they may indirectly increase anxiety and fear related to childbirth. Therefore, based on the analysis of these pregnancy comorbidities, complications, and specific obstetric conditions, our findings suggest that certain maternal health conditions may be associated with a higher risk of severe FOC. This may provide a basis for identifying potentially high-risk groups in late pregnancy. These findings do not serve as direct intervention recommendations, but rather highlight theoretical risk patterns that may assist clinicians in identifying patients who warrant additional attention during antenatal care. Further prospective and interventional studies are needed to determine whether such risk-based approaches can be translated into effective support strategies.
4.3 Limitation
There are several limitations to this study. First, the single-center design and regional setting in a tertiary referral hospital in western China may limit the generalizability of the findings. The study population included a high proportion of high-risk pregnancies and women in late gestation, which could contribute to the relatively high prevalence of FOC. In addition, factors such as family support, prior counseling, and cultural differences were not examined and may further influence the patterns of FOC. Second, the study sample was predominantly primiparous (93.8%), and the number of participants with certain comorbidities, such as high myopia or urinary disease, was relatively small. Although we statistically adjusted for parity and other covariates, the sample structure may limit generalization to more diverse obstetric populations. Further studies with more balanced and diagnosis-specific samples are warranted. Third, we focused on the independent effects of each variable and did not assess potential interaction effects among predictors. Additionally, the use of self-reported measures may introduce subjective bias. Future studies should explore the combined effects of risk factors and consider integrating qualitative methods for a more comprehensive assessment of FOC.
5 Conclusion
Fear of childbirth is highly prevalent among women in late pregnancy and is influenced by a combination of demographic, obstetric, and clinical factors. In this large cross-sectional study, primiparity, lower education levels, natural conception, and a preference for cesarean delivery were all significantly associated with higher levels of FOC. Additionally, specific comorbidities and complications, such as high myopia and urinary diseases, were identified as independent predictors of severe FOC. These findings highlight the importance of integrating FOC screening into routine prenatal care, particularly among high-risk groups. By recognizing the multidimensional nature of FOC, obstetric healthcare providers can offer more personalized counseling and support strategies to alleviate maternal fear, promote informed birth choices, and potentially improve maternal psychological well-being and birth outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of West China Second University Hospital, Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DH: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft. JZ: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. GW: Data curation, Formal analysis, Software, Visualization, Writing – review & editing. YH: Investigation, Resources, Validation, Writing – review & editing. NL: Data curation, Investigation, Validation, Writing – review & editing. MZ: Investigation, Resources, Writing – review & editing. YM: Conceptualization, Project administration, Validation, Writing – review & editing. BL: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Thanks to Yonghong Wang, Juan Li, Feng Chen, and Chuanrong Liu for their support in the data collection process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FOC, Fear of childbirth; CAQ, Childbirth Attitude Questionnaire; IVF-ET, In vitro fertilization-embryo transfer.
References
1. Hübner, T, Wolfgang, T, Theis, AC, Steber, M, Wiedenmann, L, Wöckel, A, et al. The impact of the COVID-19 pandemic on stress and other psychological factors in pregnant women giving birth during the first wave of the pandemic. Reprod Health. (2022) 19:189. doi: 10.1186/s12978-022-01493-9
2. Nilsson, C, Hessman, E, Sjöblom, H, Dencker, A, Jangsten, E, Mollberg, M, et al. Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy Childbirth. (2018) 18:28. doi: 10.1186/s12884-018-1659-7
3. Onchonga, D. Prenatal fear of childbirth among pregnant women and their spouses in Kenya. Sex Reprod Healthc. (2021) 27:100593. doi: 10.1016/j.srhc.2020.100593
4. O'Connell, MA, Leahy-Warren, P, Khashan, AS, Kenny, LC, and O'Neill, SM. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. (2017) 96:907–20. doi: 10.1111/aogs.13138
5. Ji, KM, Li, ZZ, Min, H, Sun, LP, and Zhao, Y. The trajectory and influencing factors of fear of childbirth in third trimester primiparas: a prospective longitudinal study. J Adv Nurs (2024). doi: 10.1111/jan.16636 [Epub ahead of print].
6. Hildingsson, I, Haines, H, Karlström, A, and Nystedt, A. Presence and process of fear of birth during pregnancy-findings from a longitudinal cohort study. Women Birth. (2017) 30:e242–7. doi: 10.1016/j.wombi.2017.02.003
7. Alemu, C, Wudu, H, and Lakew, S. Fear of childbirth and its associated factors among pregnant women in Dejen Woreda, east Gojjam zone, Northwest Ethiopia: a community-based cross-sectional study. Sci Rep. (2024) 14:9319. doi: 10.1038/s41598-024-58855-5
8. Rúger-Navarrete, A, Vázquez-Lara, JM, Antúnez-Calvente, I, Rodríguez-Díaz, L, Riesco-González, FJ, Palomo-Gómez, R, et al. Antenatal fear of childbirth as a risk factor for a bad childbirth experience. Healthcare (Basel). (2023) 11:297. doi: 10.3390/healthcare11030297
9. Chen, I, Opiyo, N, Tavender, E, Mortazhejri, S, Rader, T, Petkovic, J, et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. (2018) 2018:CD005528. doi: 10.1002/14651858.CD005528.pub3
10. Handelzalts, JE, Becker, G, Ahren, MP, Lurie, S, Raz, N, Tamir, Z, et al. Personality, fear of childbirth and birth outcomes in nulliparous women. Arch Gynecol Obstet. (2015) 291:1055–62. doi: 10.1007/s00404-014-3532-x
11. Junge, C, von Soest, T, Weidner, K, Seidler, A, Eberhard-Gran, M, and Garthus-Niegel, S. Labor pain in women with and without severe fear of childbirth: a population-based, longitudinal study. Birth. (2018) 45:469–77. doi: 10.1111/birt.12349
12. Sanni, KR, Eeva, E, Noora, SM, Laura, KS, Linnea, K, and Hasse, K. The influence of maternal psychological distress on the mode of birth and duration of labor: findings from the FinnBrain birth cohort study. Arch Womens Ment Health. (2022) 25:463–72. doi: 10.1007/s00737-022-01212-0
13. Adams, SS, Eberhard-Gran, M, and Eskild, A. Fear of childbirth and duration of labour: a study of 2206 women with intended vaginal delivery. BJOG. (2012) 119:1238–46. doi: 10.1111/j.1471-0528.2012.03433.x
14. Khosravi, P, Pirdadeh Beiranvand, S, Beiranvand, B, and Khalesi, ZB. Relationship between Primigravid women's awareness, attitude, fear of childbirth, and mode of delivery preference. Eur J Obstet Gynecol Reprod Biol X. (2022) 14:100143. doi: 10.1016/j.eurox.2022.100143
15. Vaajala, M, Kekki, M, Mattila, VM, and Kuitunen, I. Fear of childbirth and use of labor analgesia: a nationwide register-based analysis in Finland. Int J Gynaecol Obstet. (2023) 162:945–9. doi: 10.1002/ijgo.14781
16. Elgzar, WT, Alshahrani, MS, and Ibrahim, HA. Mode of delivery preferences: the role of childbirth fear among nulliparous women. Front Psychol. (2023) 14:1221133. doi: 10.3389/fpsyg.2023.1221133
17. Gökçe İsbir, G, İnci, F, Önal, H, and Yıldız, PD. The effects of antenatal education on fear of childbirth, maternal self-efficacy and post-traumatic stress disorder (PTSD) symptoms following childbirth: an experimental study. Appl Nurs Res. (2016) 32:227–32. doi: 10.1016/j.apnr.2016.07.013
18. Yin, A, Shi, Y, Heinonen, S, Räisänen, S, Fang, W, Jiang, H, et al. The impact of fear of childbirth on mode of delivery, postpartum mental health and breastfeeding: a prospective cohort study in Shanghai, China. J Affect Disord. (2024) 347:183–91. doi: 10.1016/j.jad.2023.11.054
19. Kalok, A, Kamisan Atan, I, Sharip, S, Safian, N, and Shah, SA. Factors influencing childbirth fear among Asian women: a scoping review. Front Public Health. (2024) 12:1448940. doi: 10.3389/fpubh.2024.1448940
20. Zhang, T, Liu, M, Min, F, Wei, W, Liu, Y, Tong, J, et al. Fear of childbirth and its determinants in pregnant women in the third trimester: a cross-sectional study. BMC Psychiatry. (2023) 23:574. doi: 10.1186/s12888-023-05070-7
21. Areskog, B, Kjessler, B, and Uddenberg, N. Identification of women with significant fear of childbirth during late pregnancy. Gynecol Obstet Investig. (1982) 13:98–107. doi: 10.1159/000299490
22. Lowe, NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. (2000) 21:219–24. doi: 10.3109/01674820009085591
23. Tanglakmankhong, K, Perrin, NA, and Lowe, NK. Childbirth self-efficacy inventory and childbirth attitudes questionnaire: psychometric properties of Thai language versions. J Adv Nurs. (2011) 67:193–203. doi: 10.1111/j.1365-2648.2010.05479.x
24. Wei, J, Liu, J, Zhang, L, Wu, Y, and Fu, C. Reliability and validity of the Chinese version of childbirth attitudes questionnaire [in Chinese]. J Nurs Sci. (2016) 31:81–3. doi: 10.3870/j.issn.1001-4152.2016.02.081
25. Huang, J, Huang, J, Li, Y, and Liao, B. The prevalence and predictors of fear of childbirth among pregnant Chinese women: a hierarchical regression analysis. BMC Pregnancy Childbirth. (2021) 21:643. doi: 10.1186/s12884-021-04123-7
26. Qiu, L, Sun, N, Shi, X, Zhao, Y, Feng, L, Gong, Y, et al. Fear of childbirth in nulliparous women: a cross-sectional multicentre study in China. Women Birth. (2020) 33:e136–41. doi: 10.1016/j.wombi.2019.04.005
27. Zhou, X, Liu, H, Li, X, and Zhang, S. Fear of childbirth and associated risk factors in healthy pregnant women in northwest of China: a cross-sectional study. Psychol Res Behav Manag. (2021) 14:731–41. doi: 10.2147/PRBM.S309889
28. Räisänen, S, Lehto, SM, Nielsen, HS, Gissler, M, Kramer, MR, and Heinonen, S. Fear of childbirth in nulliparous and multiparous women: a population-based analysis of all singleton births in Finland in 1997-2010. BJOG. (2014) 121:965–70. doi: 10.1111/1471-0528.12599
29. Rouhe, H, Salmela-Aro, K, Halmesmäki, E, and Saisto, T. Fear of childbirth according to parity, gestational age, and obstetric history. BJOG. (2009) 116:67–73. doi: 10.1111/j.1471-0528.2008.02002.x
30. Gourounti, K, Kouklaki, E, and Lykeridou, K. Validation of the childbirth attitudes questionnaire in Greek and psychosocial characteristics of pregnant women with fear of childbirth. Women Birth. (2015) 28:e44–51. doi: 10.1016/j.wombi.2015.02.004
31. Shahid, A, Malik, NI, Shahid, F, Ullah, I, and Abbass, Z. Psychosocial predictors of mental health among pregnant women. Perspect Psychiatr Care. (2022) 58:1071–6. doi: 10.1111/ppc.12900
32. Hu, Y, Zhou, M, and Wan, Y. Study on the current situation and influencing factors of pregnant women's fear of childbirth in late pregnancy [in Chinese]. J Nurs Adm. (2020) 20:768–73.
33. Arfaie, K, Nahidi, F, Simbar, M, and Bakhtiari, M. The role of fear of childbirth in pregnancy related anxiety in Iranian women: a qualitative research. Electron Physician. (2017) 9:3733–40. doi: 10.19082/3733
34. Elsharkawy, NB, Alruwaili, MM, Mohamed Elsayed Ramadan, O, Alruwaili, AN, Ouda, MMA, Oraby, FA, et al. Prevalence and determinants of fear of childbirth among pregnant women in Egypt: a cross-sectional study. Midwifery. (2024) 136:104088. doi: 10.1016/j.midw.2024.104088
35. Kemppainen, V, Mentula, M, Seppälä, T, Gissler, M, Rouhe, H, Terhi, S, et al. Fear of childbirth after induced abortion in primiparous women: population-based register study from Finland. Acta Obstet Gynecol Scand. (2024) 103:241–9. doi: 10.1111/aogs.14718
36. Yıldırım, YE, Çetinay Aydın, P, İnan Ünlü, A, Karaca, İ, and Ekin, M. Comparison of state-trait anxiety and fear of childbirth according to attachment styles of pregnant women. J Perinat Neonatal Nurs (2024). doi: 10.1097/JPN.0000000000000844 [Epub ahead of print].
37. Dal Moro, APM, Soecki, G, de Fraga, FS, Petterle, RR, and Rückl, SZ. Fear of childbirth: prevalence and associated factors in pregnant women of a maternity hospital in southern Brazil. BMC Pregnancy Childbirth. (2023) 23:632. doi: 10.1186/s12884-023-05948-0
38. Gao, LL, Liu, XJ, Fu, BL, and Xie, W. Predictors of childbirth fear among pregnant Chinese women: a cross-sectional questionnaire survey. Midwifery. (2015) 31:865–70. doi: 10.1016/j.midw.2015.05.003
39. Laursen, M, Hedegaard, M, and Johansen, C. Fear of childbirth: predictors and temporal changes among nulliparous women in the Danish National Birth Cohort. BJOG. (2008) 115:354–60. doi: 10.1111/j.1471-0528.2007.01583.x
40. Albayrak, M, and Arslan, HF. Health literacy levels of women attending a perinatology outpatient Clinic for High-Risk Pregnancy Follow-up. Cureus. (2024) 16:e68267. doi: 10.7759/cureus.68267
41. Sabetghadam, S, Keramat, A, Goli, S, Malary, M, and Rezaie, CS. Maternal health literacy, health information-seeking behavior and pregnancy outcomes among Iranian pregnant women: a cross-sectional study. Community Health Equity Res Policy. (2023) 44:77–87. doi: 10.1177/0272684X221095659
42. Khwepeya, M, Lee, GT, Chen, SR, and Kuo, SY. Childbirth fear and related factors among pregnant and postpartum women in Malawi. BMC Pregnancy Childbirth. (2018) 18:391. doi: 10.1186/s12884-018-2023-7
43. Takegata, M, Haruna, M, Morikawa, M, Yonezawa, K, Komada, M, and Severinsson, E. Qualitative exploration of fear of childbirth and preferences for mode of birth among Japanese primiparas. Nurs Health Sci. (2018) 20:338–45. doi: 10.1111/nhs.12571
44. Sluijs, AM, Cleiren, MP, Scherjon, SA, and Wijma, K. No relationship between fear of childbirth and pregnancy−/delivery-outcome in a low-risk Dutch pregnancy cohort delivering at home or in hospital. J Psychosom Obstet Gynaecol. (2012) 33:99–105. doi: 10.3109/0167482x.2012.685905
45. Hou, Y, Zhou, X, Yao, M, and Liu, S. Fear of childbirth and its predictors in re-pregnant women after cesarean section: a cross-sectional multicenter study in China. BMC Pregnancy Childbirth. (2022) 22:393. doi: 10.1186/s12884-022-04721-z
46. Phunyammalee, M, Buayaem, T, and Boriboonhirunsarn, D. Fear of childbirth and associated factors among low-risk pregnant women. J Obstet Gynaecol. (2019) 39:763–7. doi: 10.1080/01443615.2019.1584885
47. Størksen, HT, Garthus-Niegel, S, Adams, SS, Vangen, S, and Eberhard-Gran, M. Fear of childbirth and elective caesarean section: a population-based study. BMC Pregnancy Childbirth. (2015) 15:221. doi: 10.1186/s12884-015-0655-4
48. Haines, H, Pallant, JF, Karlström, A, and Hildingsson, I. Cross-cultural comparison of levels of childbirth-related fear in an Australian and Swedish sample. Midwifery. (2011) 27:560–7. doi: 10.1016/j.midw.2010.05.004
49. Safari-Moradabadi, A, Alavi, A, Pormehr-Yabandeh, A, Eftekhaari, TE, and Dadipoor, S. Factors involved in selecting the birth type among primiparous women. J Educ Health Promot. (2018) 7:55. doi: 10.4103/jehp.jehp_150_17
50. Beigi, SM, Valiani, M, Alavi, M, and Mohamadirizi, S. The relationship between attitude toward labor pain and length of the first, second, and third stages in primigravida women. J Educ Health Promot. (2019) 8:130. doi: 10.4103/jehp.jehp_4_19
51. Saisto, T, and Halmesmäki, E. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand. (2003) 82:201–8. doi: 10.1034/j.1600-0412.2003.00114.x
52. Karska-Basta, I, Tarasiewicz, M, Kubicka-Trząska, A, Miniewicz, J, and Romanowska-Dixon, B. Cesarean section and eye disorders. Ginekol Pol. (2016) 87:217–21. doi: 10.17772/gp/61752
53. Jesudason, S, Safi, N, Li, Z, Brown, M, Hague, W, Makris, A, et al. Significant kidney disease in pregnancy: feasibility and outcomes of a national population-based study using the Australasian maternity outcomes surveillance system. Aust N Z J Obstet Gynaecol (2024). doi: 10.1111/ajo.13885 [Epub ahead of print].
Keywords: fear of childbirth, mental health, maternal health, prenatal care, late pregnancy
Citation: He D, Zhang J, Wang G, Huang Y, Li N, Zhu M, Meng Y and Luo B (2025) Prevalence and factors associated with fear of childbirth in late pregnancy: a cross-sectional study. Front. Public Health. 13:1589568. doi: 10.3389/fpubh.2025.1589568
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Saba Amin, Shri Venkateshwara University, IndiaZhenwei Dai, National Clinical Research Center for Mental Disorders, China
Copyright © 2025 He, Zhang, Wang, Huang, Li, Zhu, Meng and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinling Zhang, empsLWh4ZGV5eTEwMDdAc2N1LmVkdS5jbg==; Yangxue Meng, aHh5YW5neHVlbWVuZ0AxMjYuY29t
 Dongning He
Dongning He Jinling Zhang2,3*
Jinling Zhang2,3*