- 1The University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 2City of Hope National Medical Center, Duarte, CA, United States
- 3Emory University, Atlanta, GA, United States
- 4University of Washington, Seattle, WA, United States
- 5University of Miami, Coral Gables, FL, United States
- 6University of Puerto Rico, San Juan, Puerto Rico
- 7San Diego State University, San Diego, CA, United States
- 8University of California, Davis, Davis, CA, United States
- 9Louisiana State University School of Public Health, New Orleans, LA, United States
Cancer disparities among Latinos in the United States persist as a significant public health challenge, characterized by inequitable outcomes throughout the cancer continuum. Latinos experience elevated rates and poorer prognoses in certain cancers compared to other populations, driven by complex, multilevel interactions involving environmental exposures, genetic factors, cultural practices, and systemic inequalities. Recognizing the substantial heterogeneity among Latinos—including differences in national origin, immigration experiences, socioeconomic status, language, and race—is crucial, as oversimplification risks masking key disparities. To comprehensively understand these dynamics, the Task Force: Latino Researchers Against Cancer (TFLRAC) convened specialists in oncology, public health, and behavioral sciences to systematically examine the multiple influences contributing to these disparities. Findings highlight environmental hazards, genetic susceptibilities, cultural stigmas, and linguistic barriers as significant drivers. Systemic issues such as discrimination, colorism, inadequate healthcare coverage, workforce disparities, socioeconomic challenges, and underrepresentation in clinical trials further compound these inequities. Addressing these disparities requires a multifaceted strategy, including targeted research, culturally tailored interventions, and comprehensive policy reforms to improve healthcare access, workforce diversity, and clinical trial inclusion. Collaborative efforts across academia, healthcare systems, community organizations, governmental agencies, and industry partners are imperative to achieve equitable cancer outcomes among Latinos.
Introduction
The Latino population is the largest minority in the United States (US), with 63.7 million individuals accounting for 19.1% of the total US population (1). It is important to recognize that “Latino” is an ethno-racial category primarily used for demographic and public health purposes within the US context. This socio-political construct encompasses a highly diverse population with varied ancestries, cultural heritages, countries of origin (such as Mexican, Cuban, Puerto Rican, Salvadoran, Dominican, Colombian, and others), immigration histories, languages, generational statuses, and socioeconomic conditions—differences that significantly influence health outcomes.
Spanish is widely spoken in Latino homes and is the second-most common language in the US (2). The Latino community experiences lower educational attainment and reduced median income, with a higher rate of poverty compared to the general population. Cancer disproportionately affects the Latino population and is the leading cause of death in the US Latino community, making cancer a critical issue to address in this growing population. An estimated 176,600 new cancer cases and 46,500 cancer deaths were expected to occur among US Latino individuals in 2021. Breast cancer is the leading cause of cancer death among US Latina women, and lung cancer is the leading cause of cancer death among Latino men (3).
Compared to non-Hispanic White patients, Latino men and women have higher rates of some less common cancers, such as gallbladder cancer and infection-related cancers of the liver, stomach, and cervix (3). Latino children also have the highest rates of acute lymphoblastic leukemia, the most common cancer in children (4). Cancer is often diagnosed at a later stage in Latino patients, making treatment more challenging, and they are less likely to receive timely and appropriate care (3). Participation in clinical trials is also lower among Latino patients, contributing to reduced survival rates for some cancers. However, cancer incidence and mortality vary widely within the heterogeneity Latino population (5), highlighting the need to identify specific drivers of these disparities and propose targeted solutions.
This heterogeneity extends across national origins, socioeconomic statuses, immigration backgrounds, and notably, racial and phenotypic diversity, including individuals who identify as Afro-Latino (6–9). Acknowledging this diversity—particularly differences in racial identity and skin tone—is essential, as these factors shape unique experiences of discrimination and health inequity, especially among subgroups affected by colorism. Understanding these internal differences and disaggregating data accordingly is crucial for identifying specific health burdens (10–12).
Although this article does not present new empirical data, it synthesizes consensus perspectives from Latino experts with lived experience, cultural fluency, and domain expertise in Latino cancer disparities. The qualitative insights reflect community-grounded understandings informed by extensive research, clinical practice, and policy engagement. As a Perspective Article, it aims to frame current issues, identify research gaps, and call for future empirical and qualitative research—including patient testimonies, ethnographic inquiry, and community-based research—to further develop and validate the framework presented.
Methods
Task force: Latino researchers against cancer
Considering the current state of the Latino cancer experience, a task force was established (Task Force: Latino Researchers Against Cancer, TFLRAC) with the goal to explore the causes and multilevel drivers of health impacting the Latino cancer experience.
Throughout 2023, the Task Force conducted structured meetings, focusing on distinct elements of the Latino cancer continuum. These sessions featured detailed agendas and facilitated in-depth discussions among members, who brought specialized expertise and diverse informational sources. This format ensured a focused examination of cancer disparities within the Latino community, allowing for an effective integration of insights and resources pertinent to the task force’s objectives.
Rather than collecting new empirical data, this process prioritized knowledge integration from existing literature, clinical experience, and community engagement. Members of TFLRAC include Latino scholars, clinicians, and public health professionals with cultural familiarity and insider perspectives. The collaborative nature of these discussions enabled the distillation of key themes and contextual factors affecting Latino cancer care, which form the basis of this Perspective.
Results
The TFLRAC identified environmental, genetic, cultural, and linguistic, behavioral, and systemic and access-related factors contributing to the Latino cancer experience. Figure 1 illustrates these factors mapped across the cancer control continuum and categorized by overarching social drivers of health, providing a visual framework for the subsequent discussion.
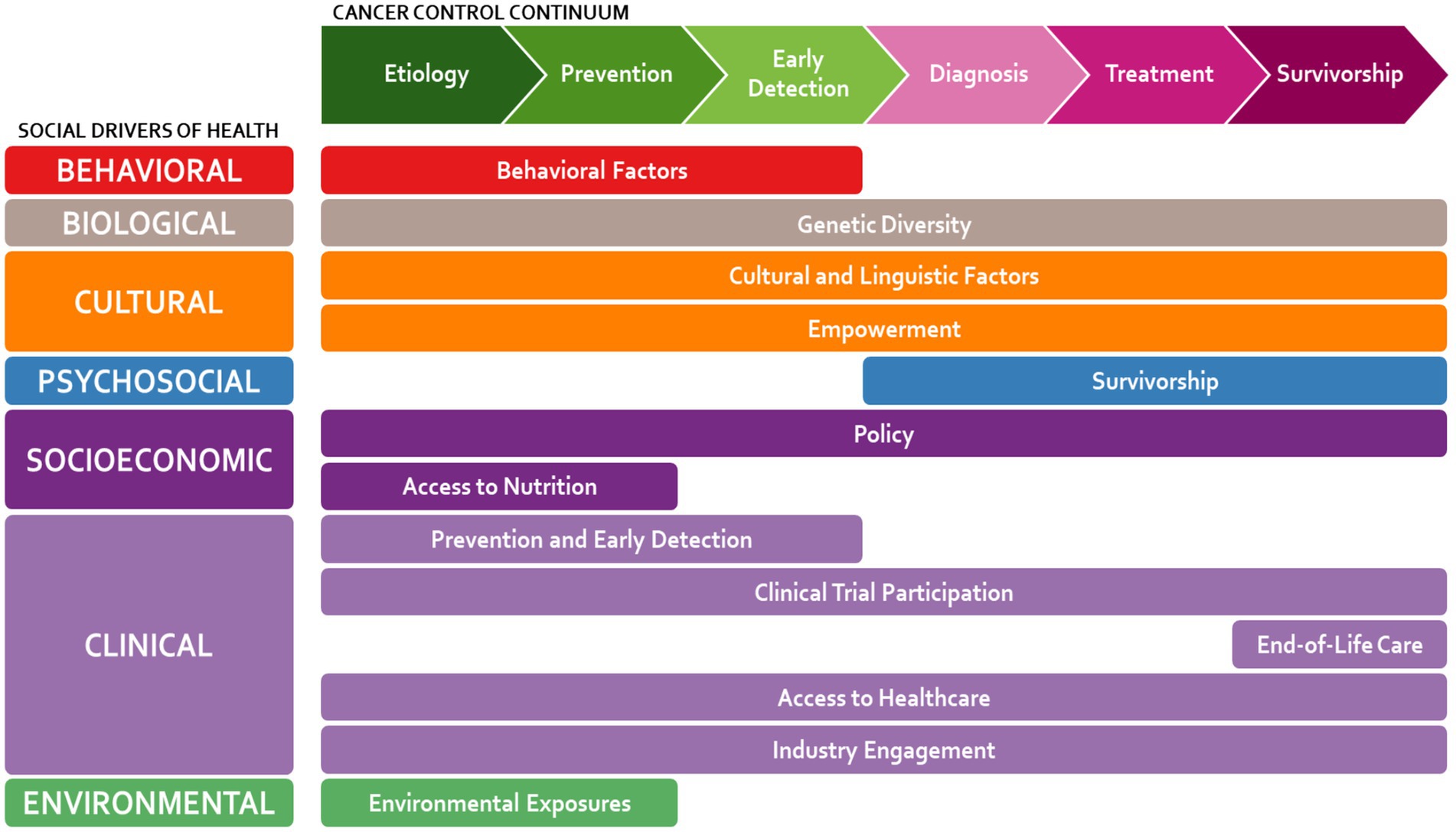
Figure 1. Factors affecting the state of cancer among Latinos, identified by the task force: Latino researchers against cancer (TFLRAC).
As each topic was discussed, two main questions pertaining to Latino cancer inequity and solutions-based interventions were considered:
1. Why do we think cancer has become the leading cause of mortality among US Latinos?
2. How can we address the unique cultural, linguistic, and socioeconomic barriers contributing to disparities in cancer incidence, mortality, and survivorship among US Latinos?
The discussion for each topic is summarized.
Environmental exposures
Environmental factors are a major cause of cancer disparities in Latino communities. Many Latino communities are in areas with higher pollution rates leading to elevated cancer risk. Latinos are exposed to higher levels of dangerous fine particulate air pollution and live in some of the most ozone-polluted cities (13, 14). The interplay between rising temperatures and altered precipitation patterns due to climate change profoundly impacts water quality. Living near toxic waste sites can also expose individuals to various carcinogens (15).
Many Latinos work in the agriculture (16) and construction industries (17), both of which increase the risk of exposure to carcinogens. Studies have shown that Latino agricultural workers are frequently exposed to insecticides and pesticides (18) Aflatoxin, another environmental toxin found in Latin America and southern US. can increase cancer risk (19) Other environmental factors include second-hand smoke and limited access to green spaces (20).
Climate change is a major contributor to increased environmental exposure among Latino individuals, who often live in areas where severe effects of climate change occur: droughts and fires, record-breaking heat, and hurricanes (21).
Despite what is known about the connection between environmental factors and cancer among Latino populations, there is still a missing link in many specific situations, highlighting the need for more research. The association between pesticide exposure and cancer in largely Latino workforces may differ across varied working conditions, climates, local regulations, and worker heritage. Other associations are clearer, such as increased rates of lung cancer associated with poor air quality due to wildfires. Chemicals in some plastics may increase the risk of breast cancer. Much more research is needed to fully understand these connections.
Genetic diversity
The genetic diversity among Latinos is vast, with various degrees of Native, African, and European ancestry represented in different populations. Genetic origin may be associated with higher risk of certain cancers. Higher rates of nonalcoholic fatty liver disease and alcohol related disease among Latino populations may contribute to a greater risk of liver cancer (22). This increased risk is not homogenous across Latino subgroups and varies based on country of origin (23). The patatin-like phospholipase domain containing 3 (PNPLA3) gene is associated with the development of nonalcoholic fatty liver disease, and the high-risk allele is found more commonly in the Mexican indigenous population (24). Studies have shown genetic heterogeneity with regard to prognosis among Latino gastric cancer patients (25).
Heterogeneity by country of origin, immigration status, and nativity
Data from population-based cancer registries reveal substantial heterogeneity within the Latino population across multiple dimensions. Subgroups defined by self-reported national origin—such as Mexican, Cuban, Puerto Rican, Central American, and South American—show distinct patterns in cancer incidence, stage at diagnosis, survival, and mortality (26). These differences are further influenced by nativity (US-born vs. foreign-born) (27) and geographic region (California vs. Florida).
Cultural and linguistic factors
Cultural beliefs and reliance on traditional medicine are major factors in the Latino healthcare experience. Insights presented here are informed by members of our Task Force—Latino cancer experts with both lived experience and cultural familiarity—and reflect emic (insider) perspectives on sociocultural dynamics.
Latino cultural beliefs significantly impact decisions and interactions with the healthcare system (28). Beliefs such as familismo (strong family orientation), fatalismo (a sense of fatalism regarding illness), machismo, and marianismo (gender role expectations) have been widely discussed in anthropological and sociological literature as influential factors in Latino health behaviors. These values are not monolithic across the Latino community but vary by geography, generation, migration history, and personal context.
Familismo can serve as both a source of support and a source of burden, particularly in resource-limited settings where caregiving responsibilities may delay care-seeking. Fatalismo, sometimes viewed as a barrier to preventive care, may coexist with proactive health behaviors when interpreted through a spiritual or faith-based lens. Traditional gender roles associated with machismo and marianismo can shape attitudes toward medical care and influence when and how care is sought. These patterns require careful navigation by healthcare providers to avoid assumptions.
A lack of education among some foreign-born Latinos and a strong belief in natural medicine may prevent some patients from understanding certain medical treatments, such as chemotherapy, antibody-based therapies, and immunotherapies. Language barriers represent one of the highest hurdles to meaningful cancer care for the Latino population. The entirety of the Latino cancer continuum is impacted by language.
Behavioral factors
When cultural beliefs collide with American culture, health can be compromised. A decline in physically demanding work, and the increase in availability of processed foods high in fat, sugar, and salt can result in a decrease in overall health of the community. This phenomenon may contribute to certain health issues (29). Unfavorable diets and increasing rates of obesity contribute to the high prevalence of colorectal cancer among Latinos. Increased rates of liver cancer could be associated with increased alcohol consumption (30), drug use and needle sharing (31), and sexually transmitted diseases (32).
Beyond healthy habits, Latino individuals also use less healthcare and social services than the average American. Health insurance is a concern, with difficulties obtaining and retaining insurance. Some Latino individuals prefer to pay cash for health costs and remain suspicious of health insurance companies.
Access to nutrition
Food sources also play a role in cancer risks. The cascading effect of climate change on agricultural productivity has culminated in diminished access to fresh and nutritious alimentary sources. Diets replete with processed foods and deficient in fruits and vegetables have been linked to an elevated risk of malignancies, notably colorectal and stomach cancers. Latino communities are particularly susceptible to this, And over 10% of Hispanic individuals have difficulty accessing fresh produce (33). This is exacerbated by government subsidies that make unhealthy foods less expensive.
Access to healthcare
Healthcare itself poses many difficulties for many Latinos, with lack of a diverse, culturally competent workforce, health insurance coverage, and language barriers. There are disproportionately fewer Latino workers across the entire healthcare workforce when compared to the general population, including medical oncologists (34). This lack of representation should be addressed throughout the medical training pipeline. Part of the problem with underrepresentation in healthcare is that tests in the US are given in English. For this reason, there is a great need for Latino practitioners to mentor young students.
Health insurance is also a challenge for many Latinos, with a high percentage lacking health insurance (35). A disruption in coverage for a cancer patient has been shown to adversely affect the receipt of cancer care and survival (36). Furthermore, some states have not expanded Medicaid, resulting in high rates of uninsured individuals (37). The burden of supporting multi-generational families and a distrust of government policy, make the idea of paying for an uncertain future benefit unappealing. Type of insurance also makes a key difference in outcome. Underinsurance can be a big problem, with large copays and coinsurance making costs untenable.
Clinical trial participation
There is vast disparity in cancer clinical trial participation among minorities in the US, particularly in the Latino population (38–40). As shown in Figure 2, which is adapted from Reopell et al. (38), these barriers can be broadly categorized into issues of access, awareness, systemic racism, and workforce diversity. Studies show that representation of Hispanic participation was the lowest overall when compared to other racial and ethnic groups (41, 42). Clinical trial design must be methodical and inclusive of diversity among potential minority recruits. Even clinical trials with thousands of Latino participants may yield questionable data if Hispanic/Latino subgroups, ancestry, and culture are not considered.
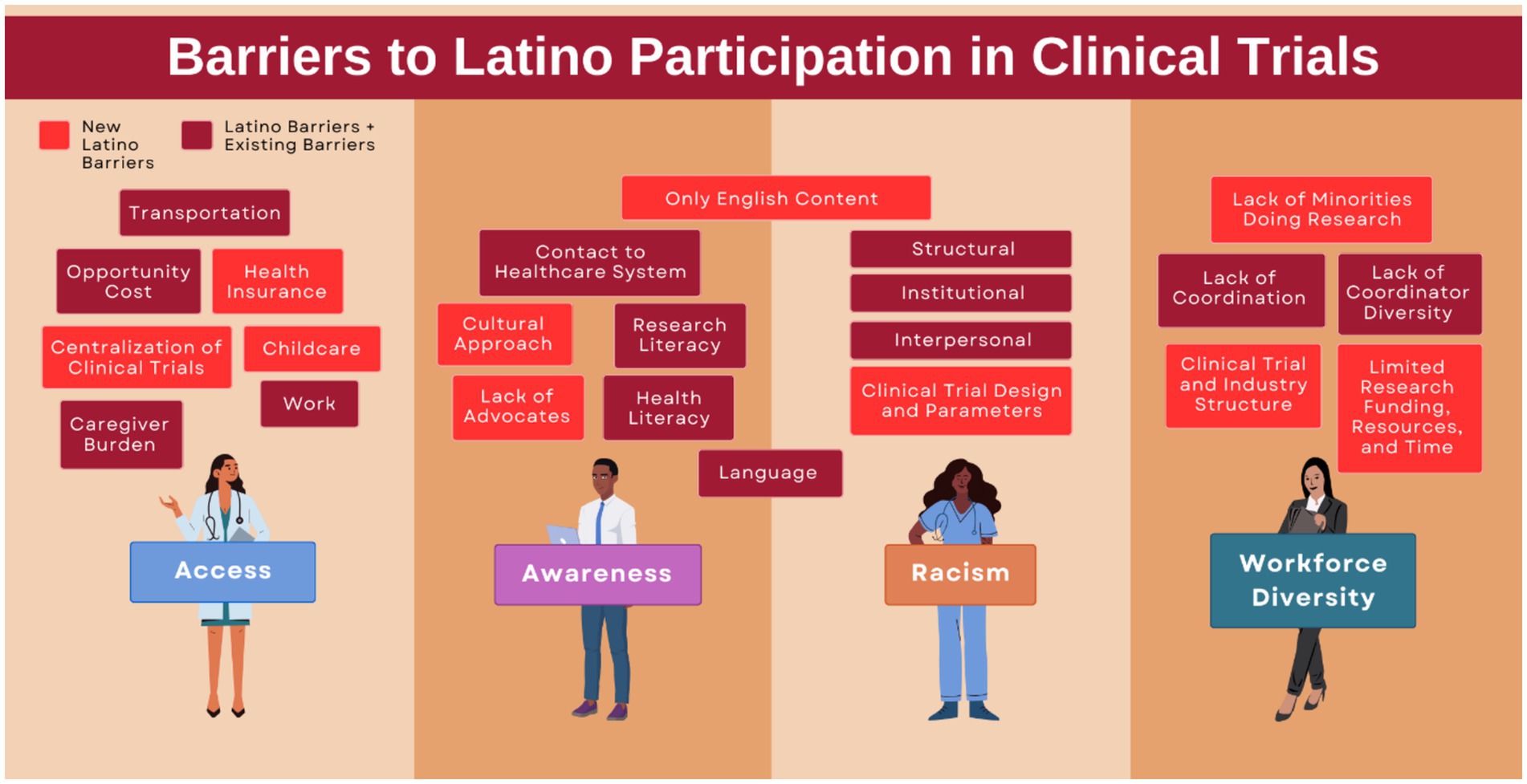
Figure 2. Barriers to Latino participation in clinical trials. Adapted from community engagement and clinical trial diversity: navigating barriers and co-designing solutions – a similar report from the “Health Equity through Diversity” series (38).
Clinical trials often require multiple, sometimes lengthy visits, preventing patients from working or caring for family members. This difficulty is exacerbated by limited paid sick days and a lack of medical insurance coverage for some clinical trials. Another barrier may be the lack of Latino patients living in areas surrounding most traditional research centers. Patients also tend to find the idea of clinical trials foreign. Others are ineligible based on stringent exclusion criteria for conditions that are highly prevalent among US-based Latinos (43).
Prevention and early detection
Patient education, cancer screenings, and enrollment in insurance programs are also best achieved at the community level. Churches and other community organizations, which have already established trust, are currently being used to great effect (44). Some organizations have even begun to focus on health education in elementary schools (45). The main barrier to prevention and early detection strategies is cost.
Empowerment
Before a discussion can be had concerning Latino empowerment, it is important to note that many Latino patients might not respond positively to the word “empowerment” at all. Instead, “understanding” and “communication” are concepts that might be more readily received. Then, through deeper understanding, patients might become more engaged and take a more active, informed role in their cancer care, making use of available resources to navigate the healthcare system. Cultural fluency training and standardized language training for providers warrant further consideration (46).
Survivorship
By 2030, the number of cancer survivors in the US is projected to reach 22.2 million, with Latino survivors accounting for approximately 20% of that number (47). This number reflects a rise in cancer survivorship in Latino communities, a testament to advancements in early detection and treatment. However, the post-treatment journey is often complicated by cultural beliefs, language barriers, and socio-economic constraints. Latino cancer survivors are more likely to report suboptimal physical well-being. Health behaviors and access to health care are associated with quality of life (48). The stress of a cancer diagnosis can also result in mental health issues. A cultural stigma may prevent many from seeking help for mental health concerns (49, 50). Like all cancer survivors, Latino patients face potential long-term and late effects of cancer and its treatment. Social support is a crucial component of survivorship, but many Latino patients face the challenge of social isolation. There is a critical need for interventions that support caregivers. However, the lack of bilingual counselors and Spanish-speaking survivor role models in the media can limit openness among survivors. The needs of caregivers are often overlooked, with these individuals carrying the major burdens. These caregivers carry a large psychosocial burden (51). Research is needed to further understand the needs of caregivers and the interventions that could be most impactful (52).
End-of-life care
Some Latino patients originating from other countries wish to go home at the end of their lives. This presents difficulties for travel and coordination of care in their home countries. A frequently overlooked consequence of this travel is that many US-based Latino cancer patients die in another country, which may affect morbidity and mortality calculations. Palliative care and hospice care are vital for the care of cancer survivors but are often difficult to obtain (53). Insurance coverage for hospice care and home equipment can give patients dignity and relief. Part of the problem for cancer patients trying to obtain hospice care is the difficulty in navigating a disjointed healthcare system. Advanced care planning is often underutilized in Latino patients, partially due to a lack of understanding that these decisions can ease the burden placed on the patient’s family. Latino cultures tend to be less control-focused, and there is often a stigma around discussing end-of-life.
Policy
Political participation is lower among Latino voters compared to the general population (54). Many of the systemic inequities impacting Latino cancer care are supported by government policy. Some policies are counter to the safety of individuals, such as state-initiated incentives that relax regulations and jeopardize the safety of nearby residents.
Discussion
The state of cancer in the US Latino population is concerning, and its causes are multifactorial. Our findings align with previous research highlighting a higher incidence of specific cancers in this group, later-stage diagnoses, and a notable absence of targeted research on both factors and outcomes (55, 56). Importantly, Latino communities in the US are internally diverse, encompassing a spectrum of cultural identities, immigration experiences, and socioeconomic conditions. These differences shape cancer risk, presentation, and treatment outcomes.
In its inaugural year, the Task Force: Latino Researchers Against Cancer (TFLRAC) has undertaken a comprehensive exploration of the multifaceted factors influencing cancer disparities among US Latinos. This foundational work has identified key areas such as environmental and genetic influences, cultural and linguistic barriers, health behavior patterns, and systemic and access-related issues.
The task force’s exploration of cultural beliefs, including familismo, fatalismo, machismo, and marianismo, emphasized the nuanced ways in which these values inform health decisions. For instance, familismo may bolster care adherence through strong social support, yet also discourage individual prioritization of preventive care. Fatalismo is not necessarily a passive belief but often integrates spiritual dimensions that can coexist with treatment engagement. A deeper understanding of these dynamics—grounded in insider perspectives and acknowledging their complexity and variation within diverse Latino subgroups—is essential to effective care.
The underrepresentation of Latinos in clinical trials remains a pressing issue, limiting generalizability of findings and contributing to inequities in evidence-based care. Greater attention to inclusion, cultural relevance, and accessibility is necessary in research and care delivery. Immediate efforts must also focus on educating patients about prevention and early detection, improving survivorship resources, and expanding culturally and linguistically aligned support systems.
To effectively address the complexity of cancer disparities within Latino populations, it is critical to disaggregate data by subgroups such as national origin, migration history, primary language, generational status, race, skin color, and socioeconomic background (7, 9, 11, 12). Aggregated data that treats Latinos as a single, uniform group can obscure significant differences in cancer incidence, risk factors, access to care, and treatment outcomes. Without attention to these intra-group variations and the complex realities shaped by political and social contexts, public health strategies risk being overly generalized and less effective. Tailoring interventions to reflect the specific needs, assets, and contexts of diverse Latino subgroups enhances both the cultural relevance and the efficacy of cancer prevention and care initiatives.
A limitation of this report is the absence of direct, primary qualitative data from Latino patients or community members themselves, such as in-depth interviews or personal narratives. While the Task Force members bring lived experience and community-grounded understanding, future research should incorporate direct qualitative data collection to more fully capture the nuanced experiences, perspectives, and priorities of the diverse Latino population regarding cancer care and disparities.
TFLRAC seeks to create a more equitable healthcare landscape for Latinos, understanding that this is a progressive journey requiring concerted efforts from various sectors. Changing the course of cancer care among Latinos is a task that requires partnership, not only in academia, healthcare, and Latino communities, but in government and industry as well (56, 57).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. EM: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. PC: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. LR-R: Writing – original draft, Writing – review & editing. LB-M: Writing – original draft, Writing – review & editing. JL: Writing – original draft, Writing – review & editing. PP: Writing – original draft, Writing – review & editing. BS-V: Writing – original draft, Writing – review & editing. GT: Writing – original draft, Writing – review & editing. LC-C: Writing – original draft, Writing – review & editing. AD: Writing – original draft, Writing – review & editing. CD: Visualization, Writing – original draft, Writing – review & editing. ET: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This Task Force is funded by the generous support of Genentech and its team, including Veronica Sandoval and Meghan McKenzie; Bristol Myers Squibb and the Organization for Latino Achievement represented by Lore Kuri, Nataly Manjarrez, and Ivan Reveles; and Gilead’s Latino/Hispanic health efforts spearheaded by Jesse Garcia, Stacey Bledsoe, and Tiffany Bratts. The authors declare that this project received funding from Bristol Myers Squibb, Genentech, and Gilead. The funder was not involved in the project design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction note
27 October 2025 A correction has been made to this article. Details can be found at: 10.3389/fpubh.2025.1686736.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. U.S. Census Bureau . America is getting older. (2023). Available online at: https://www.census.gov/newsroom/press-releases/2023/population-estimates-characteristics.html (Accessed on 2024 Aug 7)
2. Funk, C , and Lopez, MH . Hispanic Americans’ trust in and engagement with science. (2022). Available online at: https://www.pewresearch.org/science/2022/06/14/hispanic-americans-trust-in-and-engagement-with-science/ (Accessed on 2024 Aug 28)
3. American Cancer Society . Cancer Facts & Figures for Hispanic/Latino people 2021-2023. (2021). Available online at: https://www.cancer.org/research/cancer-facts-statistics/hispanics-latinos-facts-figures.html (Accessed on 2024 Aug 7)
4. Rivera-Luna, R , Perez-Vera, P , Galvan-Diaz, C , Velasco-Hidalgo, L , Olaya-Vargas, A , Cardenas-Cardos, R, et al. Triple-hit explanation for the worse prognosis of pediatric acute lymphoblastic leukemia among Mexican and Hispanic children. Front Oncol. (2022) 12:1–6. doi: 10.3389/fonc.2022.1072811
5. Zamora, SM , Pinheiro, PS , Gomez, SL , Hastings, KG , Palaniappan, LP , Hu, J, et al. Disaggregating Hispanic American cancer mortality burden by detailed ethnicity. Cancer Epidemiol Biomarkers Prev. (2019) 28:1353–63. doi: 10.1158/1055-9965.EPI-18-0872
6. Borrell, LN , and Viladrich, A . The Hispanic/Latino population in the United States: our black identity, our health and well-being. Am J Public Health. (2024) 114:S444–9. doi: 10.2105/AJPH.2024.307682
7. Charles, J . Colorism and the afro-Latinx experience: a review of the literature. Hisp J Behav Sci. (2021) 43:8–31. doi: 10.1177/07399863211027378
8. Cuevas, AG . How should health equity researchers consider intersections of race and ethnicity in afro-Latino communities? AMA J Ethics. (2022) 24:283–8. doi: 10.1001/amajethics.2022.283
9. Mendez, F , Urrea-Giraldo, F , and Ortega, D . Skin color, social inequalities and health in older adults: an analysis based on the SABE survey in Colombia. Cad Saude Publica. (2020) 36:e00121419. doi: 10.1590/0102-311x000121419
10. Almaguer, T . Race, racialization, and Latino populations in the United States In: DM HoSang , O LaBennett , and L Pulido , editors. Racial formation in the twenty-first century. [Internet]. Oakland, CA: University of California Press (2012) doi: 10.1525/california/9780520273436.003.0008
11. Cuevas, AG , Dawson, BA , and Williams, DR . Race and skin color in Latino health: an analytic review. Am J Public Health. (2016) 106:2131–6. doi: 10.2105/AJPH.2016.303452
12. Patterson, J , and Grob, K . Health implications of colorism: a narrative review of the literature. J Racial Ethn Health Disparities. (2025) doi: 10.1007/s40615-025-02369-x
13. Fleischman, L , Kingland, D , Maxwell, C , and Rios, E . Latino communities at risk the impact of air pollution from the oil and gas industry. Boston, MA: Clean Air Task Force (2016).
14. Jbaily, A , Zhou, X , Liu, J , Lee, TH , Kamareddine, L , Verguet, S, et al. Air pollution exposure disparities across US population and income groups. Nature. (2022) 601:228–33. doi: 10.1038/s41586-021-04190-y
15. Rainosek, C. (2022). Superfund sites: an environmental injustice for Latinos and all people. Salud America. Available online at: https://salud-america.org/superfund-sites-an-environmental-injustice-for-latinos-and-all-people/ (Accessed on 2024 Aug 7)
16. Varghese, JV , Sebastian, EM , Iqbal, T , and Tom, AA . Pesticide applicators and cancer: a systematic review. Rev Environ Health. (2021) 36:467–76. doi: 10.1515/reveh-2020-0121
17. Zippia,. Construction worker demographics and statistics in the US. (2021). Available online at: https://www.zippia.com/construction-worker-jobs/demographics/ (Accessed on 2024 Aug 7)
18. Arcury, TA , Laurienti, PJ , Talton, JW , Chen, H , Howard, TD , Barr, DB, et al. Pesticide urinary metabolites among Latina farmworkers and non-farmworkers in North Carolina. J Occup Environ Med. (2018) 60:e63:–71. doi: 10.1097/JOM.0000000000001189
19. Groopman, JD , Smith, JW , Rivera-Andrade, A , Alvarez, CS , Kroker-Lobos, MF , Egner, PA, et al. Aflatoxin and the aetiology of liver cancer and its implications for Guatemala. World Mycotoxin J. (2021) 14:305–17. doi: 10.3920/WMJ2020.2641
20. U.S. Centers for Disease Control and Prevention [CDC] . Hispanic and Latino people need more protection from secondhand smoke exposure. [Internet]. Tobacco - Health Equity. (2024) Available at: https://www.cdc.gov/tobacco-health-equity/collection/hispanic-latino-secondhand-smoke.html
21. Environmental Defense Fund . Latinos communities and climate change. (2017). Available online at: https://www.edf.org/sites/default/files/content/latinos_and_climate_change_factsheet_0317_refresh.pdf (Accessed on 2024 Aug 7).
22. Pinheiro, PS , Jones, PD , Medina, H , Cranford, HM , Koru-Sengul, T , Bungum, T, et al. Incidence of etiology-specific hepatocellular carcinoma: diverging trends and significant heterogeneity by race and ethnicity. Clin Gastroenterol Hepatol. (2024) 22:e8:562–571.e8. doi: 10.1016/j.cgh.2023.08.016
23. Kallwitz, ER , Daviglus, ML , Allison, MA , Emory, KT , Zhao, L , Kuniholm, MH, et al. Prevalence of suspected nonalcoholic fatty liver disease in Hispanic/Latino individuals differs by heritage. Clin Gastroenterol Hepatol. (2015) 13:569–76. doi: 10.1016/j.cgh.2014.08.037
24. Chinchilla-López, P , Ramírez-Pérez, O , Cruz-Ramón, V , Canizales-Quinteros, S , Domínguez-López, A , Ponciano-Rodríguez, G, et al. More evidence for the genetic susceptibility of Mexican population to nonalcoholic fatty liver disease through PNPLA3. Ann Hepatol. (2018) 17:250–5. doi: 10.5604/01.3001.0010.8644
25. Toal, TW , Estrada-Florez, AP , Polanco-Echeverry, GM , Sahasrabudhe, RM , Lott, PC , Suarez-Olaya, JJ, et al. Multiregional sequencing analysis reveals extensive genetic heterogeneity in gastric tumors from Latinos. Cancer Res Commun. (2022) 2:1487–96. doi: 10.1158/2767-9764.CRC-22-0149
26. Pinheiro, PS , Williams, M , Miller, EA , Easterday, S , Moonie, S , and Trapido, EJ . Cancer survival among Latinos and the Hispanic paradox. Cancer Causes Control. (2011) 22:553–61. doi: 10.1007/s10552-011-9727-6
27. Pinheiro, PS , Zhang, J , Setiawan, VW , Cranford, HM , Wong, RJ , and Liu, L . Liver cancer etiology in Asian subgroups and American Indian, black, Latino, and white populations. JAMA Netw Open. (2025) 8:e252208. doi: 10.1001/jamanetworkopen.2025.2208
28. Ramirez, A. (2023). Latino cancer survivorship: 2022 advancing the science of cancer in Latinos. Salud America. Available online at: https://salud-america.org/latino-cancer-survivorship-2022-advancing-the-science-of-cancer-in-latinos/ (Accessed on 2024 Aug 7)
29. CDC . Health disparities in Hispanic or Latino people. Health disparities in HIV, viral hepatitis, STDs, & tuberculosis. (2024) Available online at: https://www.cdc.gov/health-disparities-hiv-std-tb-hepatitis/populations/hispanic-latino.html (Accessed on 2024 Aug 7)
30. Yanez, B , McGinty, HL , Buitrago, D , Ramirez, AG , and Penedo, FJ . Cancer outcomes in Hispanics/Latinos in the United States: an integrative review and conceptual model of determinants of health. J Latina-o Psychol. (2016) 4:114–29. doi: 10.1037/lat0000055
31. Pinheiro, PS , Sherman, RL , Trapido, EJ , Fleming, LE , Huang, Y , Gomez-Marin, O, et al. Cancer incidence in first generation U.S. Hispanics: Cubans, Mexicans, Puerto Ricans, and new Latinos. Cancer Epidemiol Biomarkers Prev. (2009) 18:2162–9. doi: 10.1158/1055-9965.EPI-09-0329
32. CDC . Health disparities in HIV, viral hepatitis, STDs, and tuberculosis. Health disparities in HIV, viral hepatitis, STDs, & tuberculosis. (2024) Available online at: https://www.cdc.gov/health-disparities-hiv-std-tb-hepatitis/index.html (Accessed on 2024 Aug 7)
33. Cardiometabolic Health Congress [CMHC] . Persisting food deserts in Latino communities. Hispanic Heritage Month. (2020) Available online at: https://www.cardiometabolichealth.org/hispanic-heritage-month-persisting-food-deserts-in-latino-communities/ (Accessed on 2024 Aug 7)
34. Association of American Medical Colleges [AAMC] . Diversity in medicine: facts and figures 2019. Percentage of all active physicians by race/ethnicity, 2018. (2019) Available online at: https://www.aamc.org/data-reports/workforce/data/figure-18-percentage-all-active-physicians-race/ethnicity-2018 (Accessed on 2024 Aug 7)
35. U.S. Department of Health and Human Services Office of Minority Health . Hispanic/Latino health. Hispanic/Latino health. (2021) Available online at: https://minorityhealth.hhs.gov/hispaniclatino-health (Accessed on 2024 Aug 7)
36. Yabroff, KR , Reeder-Hayes, K , Zhao, J , Halpern, MT , Lopez, AM , Bernal-Mizrachi, L, et al. Health insurance coverage disruptions and cancer care and outcomes: systematic review of published research. JNCI J Natl Cancer Inst. (2020) 112:671–87. doi: 10.1093/jnci/djaa048
37. Richie, S , and Adriano, JL Texas has the highest share of uninsured in the country. Governing. (2023) Available online at: https://www.governing.com/health/texas-has-the-highest-share-of-uninsured-in-the-country (Accessed on 2024 Aug 7)
38. Reopell, L , Nolan, TS , Gray, D , Williams, A , Brewer, LC , Bryant, AL, et al. Community engagement and clinical trial diversity: navigating barriers and co-designing solutions—a report from the “health equity through diversity” seminar series. PLoS One. (2023) 18:e0281940. doi: 10.1371/journal.pone.0281940
39. Loree, JM , Anand, S , Dasari, A , Unger, JM , Gothwal, A , Ellis, LM, et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol. (2019) 5:e191870. doi: 10.1001/jamaoncol.2019.1870
40. Pittell, H , Calip, GS , Pierre, A , Ryals, CA , Altomare, I , Royce, TJ, et al. Racial and ethnic inequities in US oncology clinical trial participation from 2017 to 2022. JAMA Netw Open. (2023) 6:e2322515. doi: 10.1001/jamanetworkopen.2023.22515
41. American Association for Cancer Research . AACR cancer disparities progress report 2022. Philadelphia: American Association for Cancer Research (2022).
42. Camidge, DR , Park, H , Smoyer, KE , Jacobs, I , Lee, LJ , Askerova, Z, et al. Race and ethnicity representation in clinical trials: findings from a literature review of phase I oncology trials. Future Oncol. (2021) 17:3271–80. doi: 10.2217/fon-2020-1262
43. Mapes, D . Cancer clinical trials exclude too many patients: that’s changing. Fred Hutch Cancer Center. [Internet] (2021) Available at: https://www.fredhutch.org/en/news/center-news/2021/08/cancer-clinical-trials-exclude-patients-eligibility-criteria.html
44. Slater, A , Cantero, PJ , Alvarez, G , Cervantes, BS , Bracho, A , and Billimek, J . Latino health access: comparative effectiveness of a community-initiated promotor/a-led diabetes self-management education program. Fam Community Health. (2022) 45:34. doi: 10.1097/FCH.0000000000000311
45. Parada, H Jr, Vu, AH , Pinheiro, PS , and Thompson, CA . Comparing age at cancer diagnosis between Hispanics and non-Hispanic whites in the United States. Cancer Epidemiol Biomarkers Prev. (2021) 30:1904–12. doi: 10.1158/1055-9965.EPI-21-0389
46. Escobedo, LE , Cervantes, L , and Havranek, E . Barriers in healthcare for Latinx patients with limited English proficiency—a narrative review. J Gen Intern Med. (2023) 38:1264–71. doi: 10.1007/s11606-022-07995-3
47. Kronenfeld, JP , Graves, KD , Penedo, FJ , and Yanez, B . Overcoming disparities in cancer: a need for meaningful reform for Hispanic and Latino cancer survivors. Oncologist. (2021) 26:443–52. doi: 10.1002/onco.13729
48. Samuel, CA , Mbah, OM , Elkins, W , Pinheiro, LC , Szymeczek, MA , Padilla, N, et al. Calidad de Vida: a systematic review of quality of life in Latino cancer survivors in the USA. Qual Life Res. (2020) 29:2615–30. doi: 10.1007/s11136-020-02527-0
49. Substance Abuse and Mental Health Services Administration [SAMHSA] . (2022). Key substance use and mental health indicators in the United States: results from the 2021 national survey on drug use and health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Substance Abuse and Mental Health Services Administration; report no.: HHS publication no. PEP22-07-01-005, NSDUH series H-57. Available online at: https://www.samhsa.gov/data/sites/default/files/reports/rpt39443/2021NSDUHFFRRev010323.pdf (Accessed on 2024 Aug 7).
50. U.S. Department of Health and Human Services . Mental health: culture, race, and ethnicity: a supplement to mental health: a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services: Substance Abuse and Mental Health Services Administration; (2001) Available online at: http://www.ncbi.nlm.nih.gov/books/NBK44243/ (Accessed on 2024 Aug 7)
51. Sun, V , Raz, DJ , and Kim, JY . Caring for the informal cancer caregiver. Curr Opin Support Palliat Care. (2019) 13:238. doi: 10.1097/SPC.0000000000000438
52. Bisht, J , Rawat, P , Sehar, U , and Reddy, PH . Caregivers with cancer patients: focus on Hispanics. Cancer. (2023) 15:626. doi: 10.3390/cancers15030626
53. Glied, SA , and Weiss, MA . Impact of the Medicaid coverage gap: comparing states that have and have not expanded eligibility. Commonwealth Fund. [Internet] (2023). doi: 10.26099/vad1-s645
54. Morris, K , and Grange, C . Brennan center for justice. Large racial turnout gap persisted in 2020 election. (2023) Available online at: https://www.brennancenter.org/our-work/analysis-opinion/large-racial-turnout-gap-persisted-2020-election (Accessed on 2024 Aug 8)
55. Fejerman, L , Ramirez, AG , Nápoles, AM , Gomez, SL , and Stern, MC . Cancer epidemiology in Hispanic populations: what have we learned and where do we need to make progress? Cancer Epidemiol Biomarkers Prev. (2022) 31:932–41. doi: 10.1158/1055-9965.EPI-21-1303
56. Elena, JW , Gallicchio, L , Pottinger, CA , Akif, KE , Hanisch, R , Kennedy, AE, et al. Cancer epidemiology in Hispanic populations: an analysis of funded observational research at the National Cancer Institute. Cancer Epidemiol Biomarkers Prev. (2023) 32:653–8. doi: 10.1158/1055-9965.EPI-22-0815
57. Ramirez, A. Research: Latino communities lack accessible green space. San Antonio, TX: Salud America. (2019) Available online at: https://salud-america.org/research-latino-communities-lack-accessible-green-space/ (Accessed on 2024 Aug 7).
Keywords: cancer disparities, Latinos, health equity, cultural barriers, clinical trial diversity, environmental health
Citation: Ramirez AG, Munoz E, Rodriguez-Rodriguez L, Bernal-Mizrachi L, Chalela P, Lopez JA, Pinheiro PS, Segarra-Vasquez B, Talavera G, Carvajal-Carmona LG, Duque AD, Despres C and Trapido EJ (2025) Uncovering multilevel drivers of cancer disparities among Latinos in the United States. Front. Public Health. 13:1591074. doi: 10.3389/fpubh.2025.1591074
Edited by:
Cyrille Delpierre, INSERM Public Health, FranceReviewed by:
Francesca Randazzo Eisemann, National Autonomous University of Honduras, HondurasCopyright © 2025 Ramirez, Munoz, Rodriguez-Rodriguez, Bernal-Mizrachi, Chalela, Lopez, Pinheiro, Segarra-Vasquez, Talavera, Carvajal-Carmona, Duque, Despres and Trapido. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amelie G. Ramirez, b3JvemNvbkB1dGhzY3NhLmVkdQ==
 Amelie G. Ramirez
Amelie G. Ramirez Edgar Munoz
Edgar Munoz Lorna Rodriguez-Rodriguez
Lorna Rodriguez-Rodriguez Leon Bernal-Mizrachi
Leon Bernal-Mizrachi Patricia Chalela1
Patricia Chalela1
 Jose Aron Lopez
Jose Aron Lopez Paulo S. Pinheiro
Paulo S. Pinheiro Barbara Segarra-Vasquez
Barbara Segarra-Vasquez Gregory Talavera
Gregory Talavera Luis G. Carvajal-Carmona
Luis G. Carvajal-Carmona Edward J. Trapido
Edward J. Trapido