- 1Department of Children’s Health Care, Jiangsu Province Hospital, Jiangsu Women and Children’s Health Hospital, Nanjing, Jiangsu, China
- 2The First Clinical Medical College of Nanjing Medical University, Nanjing, Jiangsu, China
- 3Nanjing Pukou People’s Hospital, Liangjiang Hospital Southeast University, Nanjing, Jiangsu, China
Introduction: Understanding parental knowledge, attitudes, and practices (KAP) regarding metabolically healthy obesity (MHO) in children and adolescents is crucial. This study aimed to assess the KAP levels of parents concerning MHO and identify factors influencing these levels.
Methods: A cross-sectional study was conducted at Jiangsu Provincial People’s Hospital (June 28, 2023–August 3, 2023). 534 valid questionnaires were collected. Data analysis included descriptive statistics, univariable/multivariable regression, and Spearman correlation to determine KAP levels and influencing factors. Cronbach’s α was 0.890.
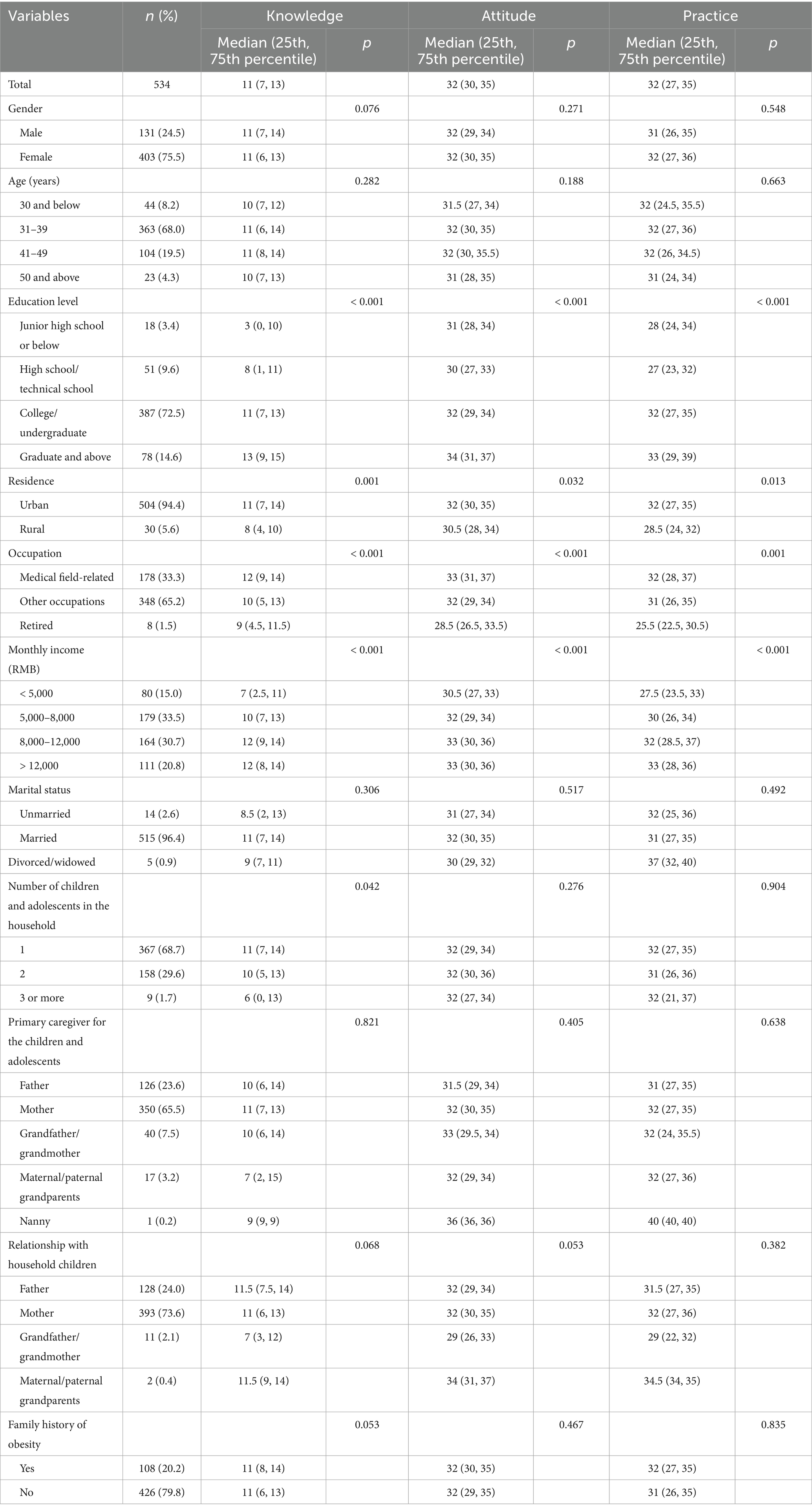
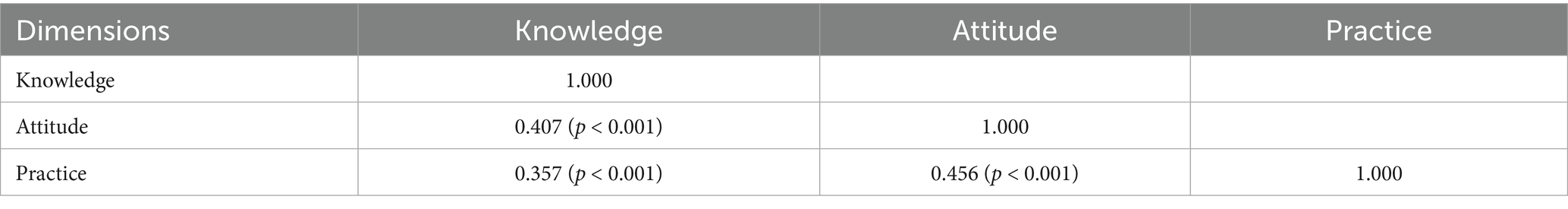
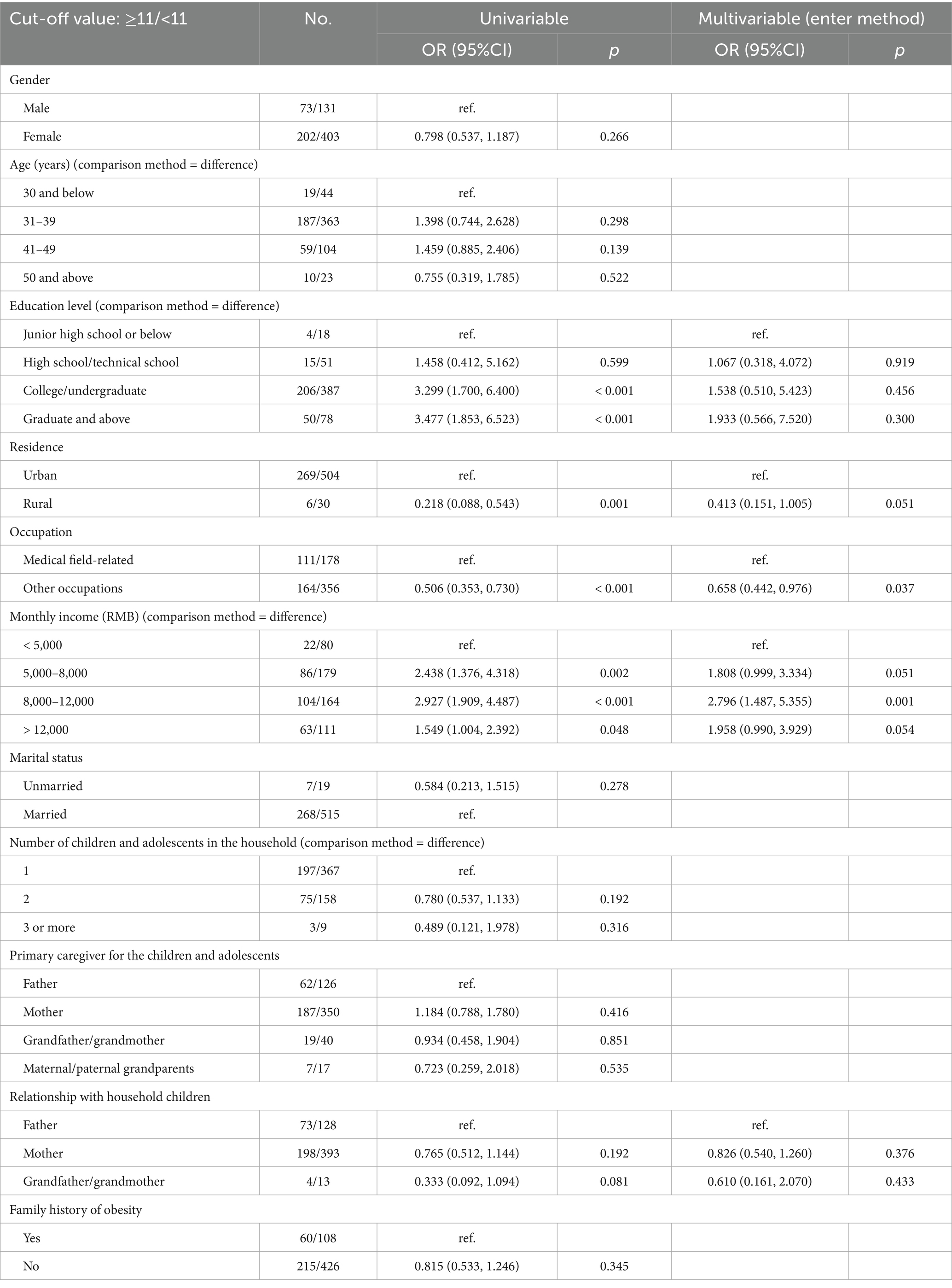
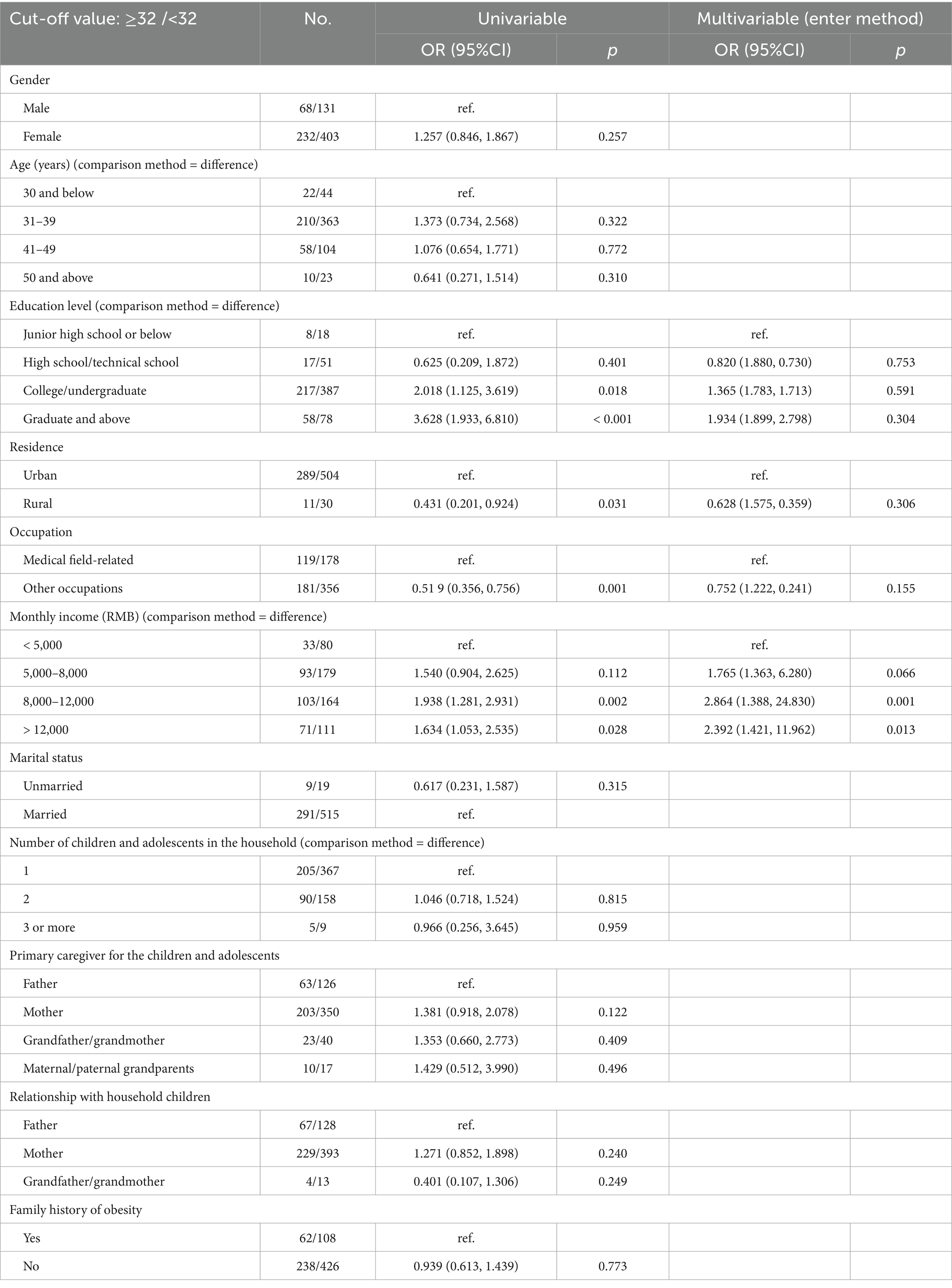
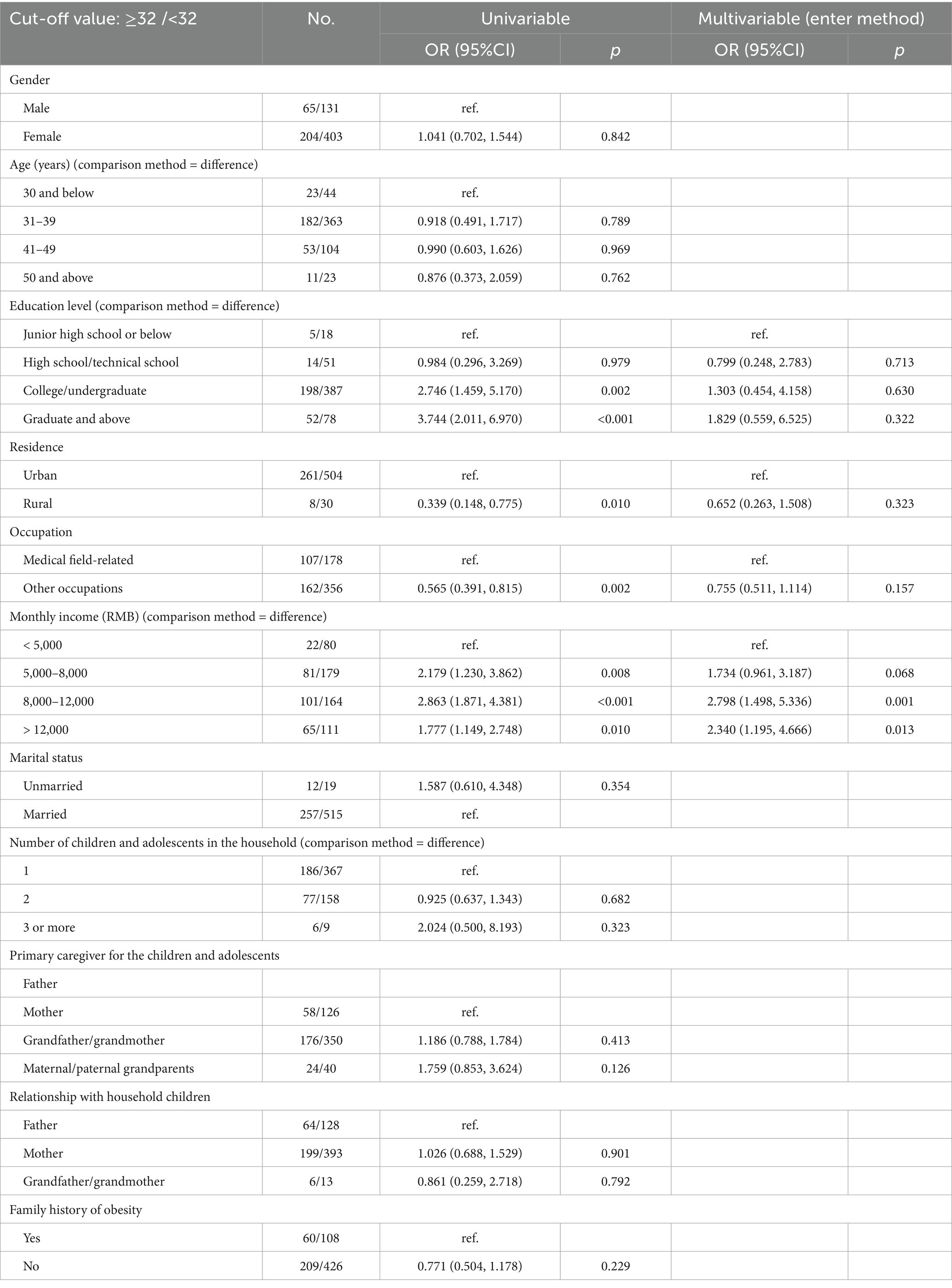
Results: Median scores were 11 (IQR: 7–13; maximum 18) for knowledge, 32 (IQR: 30–35; maximum 40) for attitude, and 32 (IQR: 27–35; maximum 40) for practice. Significant positive correlations were found between knowledge and attitude (r = 0.407, p < 0.001), knowledge and practice (r = 0.357, p < 0.001), and attitude and practice (r = 0.456, p < 0.001). Non-medical occupations (OR = 0.658, p = 0.037) and income 8,000–12,000 (OR = 2.796, p = 0.001) were linked to knowledge. Income 5,000–8,000 (OR = 2.864, p = 0.001) and 8,000–12,000 (OR = 2.392, p = 0.013) related to attitude, while income 8,000–12,000 (OR = 2.798, p = 0.001) and >12,000 (OR = 2.340, p = 0.013) related to practice.
Conclusion: Parents showed moderate knowledge but good attitudes/practices toward MHO. KAP dimensions were positively correlated. Socioeconomic status, particularly income, significantly associated with knowledge/practice.
Introduction
Overweight and obesity are emerging as a global public health crisis and are related to the rapid economic growth and changes in lifestyles (1, 2). Obesity and overweight have more than doubled in the past 30 years, with obesity alone affecting over 1 billion people globally as of 2024 (3). China has the largest number of overweight and obese individuals worldwide, and approximately 20% of Chinese children and adolescents have excess weight (4). Obesity not only impacts the normal growth and development of children and adolescents but also stands as a primary risk factor for non-communicable diseases in this age group, including cardiovascular diseases, type 2 diabetes mellitus (T2DM), musculoskeletal disorders, cancer, and mental health issues, leading to an increased likelihood of premature death and disability in adulthood (5, 6).
Still, not all overweight/obese individuals are equal, and research has revealed that individuals with obesity who have unhealthy metabolic profiles are more prone to cardiovascular diseases and overall mortality than those with a healthier metabolic profile (7, 8). Hence, it has been recommended to classify obesity into distinct phenotypes based on body mass index (BMI) and metabolic status, including metabolically healthy obesity (MHO) and metabolically unhealthy obesity (MUO), and to adopt different management strategies (9, 10). People with MHO do not appear to have cardiometabolic abnormalities despite a BMI in the obesity range, while patients with MUO display T2DM, fatty liver disease, hypertension, dyslipidemia, and cardiovascular diseases (10). In 2019, China issued an expert consensus that clearly defines MHO as individuals whose BMI qualifies as obese but does not exhibit metabolic abnormalities such as high blood pressure, high blood glucose, lipid disorders, or insulin resistance (11). Still, the data regarding the overall prevalence of MHO and MUO in Chinese children and adolescents according to the criteria mentioned above is poorly known.
“The ‘Healthy China 2030’ Blueprint,” the “Healthy Children Action Enhancement Plan (2021–2025),” and the “China Children’s Development Program (2021–2030)” all emphasize the need to address and control childhood obesity from a national strategic perspective (12). Identifying the risk factors for childhood and adolescent obesity is a crucial approach to preventing and managing obesity, and the concept of MHO brings new insights to the treatment and management of childhood obesity (13). Currently, the principles of treating childhood and adolescent obesity involve reducing energy intake and increasing energy expenditure to reduce body fat while promoting normal growth and health in the affected children (14–16). Treatment methods primarily encompass (1) lifestyle interventions, (2) psychological and behavioral interventions, (3) medication, and (4) metabolic weight reduction surgery. Lifestyle interventions, which include diet, exercise, and sleep management, should be family-based, integrated into daily life, and involve the active participation of children, parents, teachers, and healthcare professionals, with a duration of at least 1 year (14–16). Previous studies commonly acknowledge that genetic and environmental factors contribute to obesity (17–19). Therefore, the World Health Organization (WHO) specifically urges improvements in children’s and adolescents’ obesity through parental behaviors, early life conditions, individual diet, and physical activity (20, 21). Parents play a crucial role in recognizing and managing childhood and adolescent obesity, through early recognition and health monitoring, modeling and shaping healthy behaviors, engagement in behavior change interventions, and long-term maintenance (22, 23). Even among children with MHO, parents should ensure the maintenance of protective behaviors (high physical activity, healthy diet, reduced sedentary time). Regular health check-ups are needed to detect any changes in metabolic profile. Encouraging healthy habits, such as high fruit/vegetable intake and low screen time, directly relates to a more favorable metabolic profile and slower progression to metabolic syndrome (24).
There is currently limited direct research specifically focused on parental awareness, attitudes, and behaviors regarding metabolically healthy obesity (MHO) in children and adolescents. Most existing studies address parental perceptions, knowledge, and practices concerning childhood obesity more broadly, with only indirect relevance to the MHO phenotype (25–27). Therefore, this study aims to explore the levels of parental awareness, attitudes, and behaviors regarding MHO in children and adolescents, which holds significant implications for preventing and managing obesity-related health issues. Particularly in the context of the escalating obesity epidemic, understanding parental perceptions and actions toward MHO provides valuable insights for devising effective health education and intervention strategies. Moreover, the study can unveil factors influencing parental awareness and behavioral practices, including socioeconomic status, thereby offering more targeted recommendations for future health promotion initiatives. This research holds crucial practical and policy implications for fostering the health development of children and adolescents, as well as preventing and managing obesity-related health problems.
Materials and methods
The study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (28).
Study design and participants
This cross-sectional study was conducted at Jiangsu Provincial People’s Hospital from June 28, 2023, to August 3, 2023. Established in 1936 as the affiliated clinic to Jiangsu Provincial Medical College, Jiangsu Provincial People’s Hospital is the largest comprehensive hospital in Jiangsu Province. It is designated as a Grade 3A hospital, representing the highest tier in China’s hospital classification system for comprehensive service and advanced medical capabilities. It houses approximately 4,200 beds with a daily patient volume approaching 9,000. The staff exceeds 6,800 employees, including specialists in multiple nationally and provincially recognized key clinical disciplines. The hospital serves the population of Nanjing municipality and the wider Jiangsu Province, regions that include both highly urbanized areas and vast rural communities. Jiangsu itself is one of China’s most economically developed provinces, but it exhibits strong urban–rural socioeconomic diversity and health inequality. Over 95% of the population has basic medical security, but out-of-pocket health spending remains a significant burden for the lowest-SES and high-cost families, especially those with chronic diseases and older adults.
The participants were the parents of children and adolescents, enrolled at the General outpatient clinic of child health department (i.e., obese/overweight patients found in general physical examination screening), the pediatric nutrition clinic, and the pediatric child weight management clinic (i.e., patients who are seen for obesity). The study was approved by the Medical Ethics Committee of Jiangsu Provincial People’s Hospital. Each participant provided written informed consent before completing the questionnaire.
The inclusion criteria were (1) parents of children or adolescents who could be encountered in routine outpatient work, (2) individuals with clear consciousness, normal cognitive function, and the ability to complete the questionnaire (in Chinese) without communication barriers, and (3) participants who provided informed consent for this study and voluntarily agreed to participate. The exclusion criteria were (1) participants who did not consent to participate in the study, (2) respondents with completion time >1,800 s or < 150 s (the minimum time to answer the questionnaire was calculated as 2 s for a single-choice question and 3 s for a multiple-choice question; the maximum was set arbitrarily to exclude those who might be checking for answers on the internet or other sources), (3) incomplete or duplicate questionnaire responses, or (4) questionnaires with logical errors in the responses.
Questionnaires and data collection
Since no questionnaire was available to answer the research question in the specific study population, a new KAP questionnaire was designed based on the literature (10, 29, 30) and the Expert Consensus on the Definition and Screening of Metabolically Healthy Obesity in Chinese Children (11). The questionnaire was refined based on the feedback of 15 experts in pediatric endocrinology, child growth and development, and the child healthcare field. A pilot study was conducted with 49 participants, and the Cronbach’s α coefficient was 0.872.
The questionnaire consisted of four sections (Supplementary materials): demographic characteristics (11 items), knowledge (15 items), attitudes (eight items), and practices (eight items) related to MHO. The scores were computed individually for each subcategory. In the knowledge section, the responses were coded as 1 = correct, 0 = incorrect, and 0 = uncertain. The attitude section used a five-point Likert scale, ranging from “totally agree” (5 points) to “totally disagree” (1 point). The scores for negative topics were reverse-coded before calculation. The practice section also used a five-point Likert scale, ranging from “always” (5 points) to “never” (1 point). Hence, the total scores for the knowledge, attitude, and practice dimensions were 0–15, 8–40, and 8–40, respectively.
Data was collected through an online questionnaire using a QR code generated with the WeChat-based Questionnaire Star applet. The parents were approached for participation when they visited the hospital. Data are collected using the Questionnaire Star applet. The participants accessed the questionnaire by scanning the QR code via WeChat and completing it. The questionnaire tool 2–30 min to complete. The research assistants were available to provide guidance and answer questions when the questionnaire was completed on-site. Once enrolled and the QR code was scanned, the participants could complete the questionnaire at their leisure. All items were mandatory. A given IP address could be used only once to submit a questionnaire.
Sample size
The sample size calculation was performed using the Open Epi calculator tool, using the following formula (31, 32):
where n is the required sample size, z is the Z statistic for the confidence level (e.g., 1.96 for a 95% confidence level or 2.58 for a 99% confidence level), p is the estimated proportion (generally set at 0.5), and e is the margin of error (typically set at 5%). A smaller margin of error increases the reliability of the conclusions. Hence, using the formula.
a minimum of 384 valid questionnaires were needed to be collected to ensure the required level of confidence in the research findings.
Statistical analysis
The data were analyzed using SPSS 22.0 (IBM, Armonk, NY, USA). The continuous data were tested for normal distribution using the Kolmogorov–Smirnov test. The continuous data following the normal distribution were presented as means ± standard deviations and analyzed using Student’s t-test or ANOVA. Those with a non-normal distribution were presented as medians [interquartile ranges (IQRs)] and analyzed using the Mann–Whitney U-test or Wilcoxon’s test. Categorical data were presented as n (%) and analyzed using the chi-squared test. Correlations between scores were analyzed using Pearson correlation coefficients (normal distribution) or Spearman correlation coefficients (non-normal distribution). Univariate logistic regression analyses were performed to determine the factors associated with the KAP scores. Variables with p-values < 0.10 were included in the multivariable logistic regression analyses. In this study, the p-values were reported with three decimals, and p-values < 0.05 were considered statistically significant.
Results
Demographics characteristics
This study collected 632 questionnaires, but three participants did not agree to the use of the collected data for scientific research, and 95 questionnaires took less than 150 s or more than 1,800 s to fill in. Therefore, 534 questionnaires were included in the analysis. The results confirmed the questionnaire’s good reliability and validity, with a Cronbach’s α coefficient of 0.890 and a Kaiser-Meyer-Olkin (KMO) value of 0.893. The Cronbach’s α coefficients for knowledge, attitudes, and practices were 0.868, 0.723, and 0.882, respectively. The knowledge, attitude, and practice scores did not meet the normal distribution (Supplementary Table S1).
The characteristics of the participants are shown in Table 1. Most participants were female (75.5%), aged 31–39 years (68.0%), had a college/undergraduate education (72.5%), were living in urban areas (94.4%), were working in non-medical occupations (65.2%), had a monthly income of 5,000–8,000 RMB (33.5%), were married (96.4%), had one child or adolescent in the household (68.7%), and showed no family history of obesity (79.8%). The primary caregiver of the child or adolescent was the mother (65.5%).
Knowledge
The median knowledge score was 11 (61.1%; IQR: 7–13; range: 0–18) (Supplementary Table S2). Higher knowledge scores were observed with higher education (p < 0.001), urban residence (p = 0.001), medical occupation (p < 0.001), higher income (p < 0.001), and only one child or adolescent in the household (p = 0.042) (Table 1). The item with the highest score was K1 (88.0%; “Overweight and obesity are defined as the excessive or abnormal accumulation of fat that poses health risks, and they are chronic metabolic diseases caused by the interaction of various factors, including genetics and the environment.”), while the item with the lowest score was K7 (13.9%; “MHO, as a form of obesity with normal metabolism, is no different from other health states”) (Supplementary Table S3).
Attitudes
The median attitude score was 32 (80.0%; IQR: 30–35; range: 16–40) (Supplementary Table S2). Higher attitude scores were observed with higher education level (p < 0.001), urban residence (p = 0.032), medical occupation (p < 0.001), and higher income (p < 0.001) (Table 1). The item with the highest score was A3 (87.0%; “I believe it is necessary to control and improve the diet of children and adolescents to manage MHO.”), while the lowest score was seen for A6 (46.7%; “I believe MHO will resolve naturally or transform into metabolically healthy normal-weight individuals as children and adolescents develop.”) (Supplementary Table S4).
Practices
The median practice score was 32 (80.0%; IQR: 27–35; range: 8–40) (Supplementary Table S2). Higher practice scores were seen with higher education level (p < 0.001), urban residents (p = 0.013), medical occupation (p = 0.001), and a higher income (p < 0.001) (Table 1). The highest practice score was observed with P5 (79.2%; “I will educate MHO children and adolescents to develop healthy sleep hygiene habits, such as maintaining a regular sleep schedule and avoiding stimulating activities before bedtime.”) and the lowest score was seen with P8 (53.3%; “I will collaborate with teachers and healthcare professionals to participate in intervention programs for MHO children and adolescents.”) (Supplementary Table S5).
Correlations
The knowledge scores were positively correlated with the attitude (r = 0.407, p < 0.001) and practice (r = 0.357, p < 0.001) scores, while the attitude scores were positively correlated to the practice scores (r = 0.456, p < 0.001) (Table 2).
Multivariable analyses
All multivariable analyses used the median score as the cutoff value. Non-medical occupations (OR = 0.658, 95%CI: 0.442–0.976, p = 0.037) and income 8,000–12,000 (OR = 2.796, 95%CI: 1.487–6.355, p = 0.001) were independently associated with the knowledge scores (Table 3). Income 5,000–8,000 (OR = 2.864, 95%CI: 1.388–24.830, p = 0.001) and income 8,000–12,000 (OR = 2.392, 95%CI: 1.421–11.962, p = 0.013) were independently associated with the attitude scores (Table 4). Income 8,000–12,000 (OR = 2.798, 95%CI: 1.498–5.336, p = 0.001) and income >12,000 (OR = 2.340, 95%CI: 1.195–4.666, p = 0.013) were independently associated with the practice scores (Table 5).
Discussion
This cross-sectional study analyzed the KAP levels of parents of children and adolescents regarding MHO. The KAP dimensions were positively correlated to each other. Socioeconomic status was associated with knowledge and practice scores.
The present study showed moderate parental knowledge (61.1%) toward MHO but positive attitudes and proactive practice (both 80.0%). No previous studies examined the KAP of parents toward MHO specifically. Available studies mostly examined obesity in general and only brushed the subject of MHO (25–27). Previous studies among Chinese university students showed poor knowledge of obesity and its complications (33, 34). Straughan and Xu showed that the parental KAP toward childhood obesity was moderate in Singapore (35). Similar results were observed in Congo (36) and even in developed countries like the United States of America (37). In the present study, participants with non-medical occupations had lower knowledge of MHO. Indeed, medical workers are more likely to have learnt about MHO in the course of their occupation or continuing education. Healthcare providers are primary sources of medical and health information for patients and the general population. Studies showed that the KAP toward obesity can be low or moderate among healthcare providers in specific parts of the world (38). The KAP of healthcare providers was not examined in the present study, and future studies should involve such professionals. Indeed, improving the parental KAP could involve improving the KAP upstream, especially given that parent-physician communication plays an important role in KAP toward obesity and its prevention/management (39).
Socioeconomic conditions are well-known to be related to health literacy, health risk behaviors, and health status (40). Accordingly, in the present study, parents with a higher income had higher knowledge scores, as did those involved in medical professions. Only a higher income was associated with better attitude and practice scores. In the study area, an income of < 5,000 yuan is a lower income level, covering some graduates, grassroots service workers, or part-time workers who have just joined the workforce. An income of 5,000–8,000 yuan is a lower middle/mainstream wage, which is the typical income range of white-collar workers and ordinary employees in many cities, and is the backbone of society, but life pressure may be greater. An income of 8,000–12,000 yuan is a middle/upper middle income, usually for more experienced professionals, grassroots managers, or technical backbones with relatively affordable lives. An income of > 12,000 yuan represents the high-income group, including senior managers, senior experts, business owners, etc., with strong consumption and savings ability. Those results are globally supported by Straughan and Xu (35), who showed that parents with higher KAP scores toward obesity were younger, had a higher income, were not working full-time, and were living in a separate household from the children’s grandparents. Similar results were also reported in various countries (41–43). Nevertheless, all three dimensions were positively correlated to each other. Based on the KAP theory, knowledge is the basis for practice, but attitude is the force driving practice (44, 45). Hence, improving knowledge and attitudes through educational and motivational interventions could also improve practice (46, 47). Future studies should also examine such interventions.
This study had limitations. The study met the calculated sample size, but it was performed at a single center and thus represents only a small proportion of the parents in China, limiting generalizability. The study was cross-sectional and, therefore, represents a single point in time, preventing causality analysis and the changes over time. Nevertheless, the results could serve as a historical baseline to evaluate the effect of future educational activities on MHO. All KAP studies are at risk of social desirability bias, i.e., the participants might be tempted to answer what they know they should think/do instead of what they are actually thinking/doing (48, 49). Considering the high attitude and practice scores, that bias is a possibility. Future studies should involve multiple centers and cover larger areas of the country. Finally, the sparse effect raises the odds ratio’s confidence interval. It refers to the phenomenon that when the sample size is small, and there are many variables, the parameter estimation in the so-called “separated data” tends to be infinite (50–52). We acknowledge that the statistical analysis may have resulted in some inflation of the Type I error rate. However, given the exploratory nature of this study, the primary aim was hypothesis generation rather than definitive hypothesis testing. Accordingly, the acceptance of a slightly elevated risk of false-positive findings was considered justifiable, with the understanding that these results require confirmation in future, adequately powered confirmatory studies (53, 54). Therefore, pending confirmation, the results should be interpreted with caution.
Conclusion
In conclusion, this study showed that the parents of children and adolescents had moderate knowledge but good attitudes and practices toward MHO. The KAP dimensions were positively correlated to each other. The socioeconomic status (living in an urban area, income, and working in a medical profession) was generally associated with the KAP scores. The results could be used to optimize educational strategies for parents and provide guidance and references for preventing and managing childhood and adolescent obesity. Policymakers should be made aware of the results and participate in the development of an intervention to improve the KAP of the parents toward MHO. Better practice could translate into patient outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was carried out after the protocol was approved by the Medical Ethics Committee of Jiangsu Provincial People’s Hospital (2023-SR-514). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
FZ: Writing – original draft. JF: Writing – original draft. LZ: Writing – original draft. LL: Writing – original draft. HY: Writing – original draft. JL: Writing – original draft. TT: Writing – original draft. YH: Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the General Project of Jiangsu Province Maternal and Child Health Research Project (F202112).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1591300/full#supplementary-material
References
1. McGrosky, A, Luke, A, Arab, L, Bedu-Addo, K, Bonomi, AG, and Bovet, P. Energy expenditure and obesity across the economic spectrum. Proc Natl Acad Sci. (2025) 122:e2420902122. doi: 10.1073/pnas.2420902122
2. Abud Alanazi, Y. Implications of lifestyle changes on the incidence of childhood obesity – a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. (2023) 27:7700–9. doi: 10.26355/eurrev_202308_33424
3. Ahmed, SK, and Mohammed, RA. Obesity: prevalence, causes, consequences, management, preventive strategies and future research directions. Metabolism Open. (2025) 27:100375. doi: 10.1016/j.metop.2025.100375
4. Peng, W, Zhang, J, Zhou, H, Zhang, A, Wang, Y, Tian, X, et al. Obesity intervention efforts in China and the 2022 world obesity day. Glob Health J. (2022) 6:118–21. doi: 10.1016/j.glohj.2022.07.007
5. Chung, ST, Krenek, A, and Magge, SN. Childhood obesity and cardiovascular disease risk. Curr Atheroscler Rep. (2023) 25:405–15. doi: 10.1007/s11883-023-01111-4
6. Goel, A, Reddy, S, and Goel, P. Causes, consequences, and preventive strategies for childhood obesity: a narrative review. Cureus. (2024) 16:e64985. doi: 10.7759/cureus.64985
7. Kim, S-A, Lim, K, Lee, J-K, Kang, D, and Shin, S. Metabolically healthy obesity and the risk of all-cause and cardiovascular disease mortality in a Korean population: a prospective cohort study. BMJ Open. (2021) 11:e049063. doi: 10.1136/bmjopen-2021-049063
8. Wei, D, González-Marrachelli, V, Melgarejo, JD, Liao, C-T, Hu, A, Janssens, S, et al. Cardiovascular risk of metabolically healthy obesity in two European populations: prevention potential from a metabolomic study. Cardiovasc Diabetol. (2023) 22:82. doi: 10.1186/s12933-023-01815-6
9. Smith, GI, Mittendorfer, B, and Klein, S. Metabolically healthy obesity: facts and fantasies. J Clin Invest. (2019) 129:3978–89. doi: 10.1172/JCI129186
11. Association for Maternal Child Health Study, Expert committee on obesity controlling for women children, Expert committee on definition of metabolically healthy obesity, Screening metabolically unhealthy obesity in Chinese children. The expert consensus on definition of metabolically healthy obesity and screening metabolically healthy obesity in Chinese children. Chin J Woman Child Health Res. (2019) 30:1487–90. doi: 10.3969/j.issn.1673-5293.2019.12.001
12. Tan, X, Liu, X, and Shao, H. Healthy China 2030: a vision for health care. Value Health Reg Issues. (2017) 12:112–4. doi: 10.1016/j.vhri.2017.04.001
13. Shaban Mohamed, MA, AbouKhatwa, MM, Saifullah, AA, Hareez Syahmi, M, Mosaad, M, Elrggal, ME, et al. Risk factors, clinical consequences, prevention, and treatment of childhood obesity. Children (Basel). (2022) 9:1975. doi: 10.3390/children9121975
14. Maffeis, C, Olivieri, F, Valerio, G, Verduci, E, Licenziati, MR, and Calcaterra, V. The treatment of obesity in children and adolescents: consensus position statement of the Italian Society of Pediatric Endocrinology and Diabetology, Italian Society of Pediatrics and Italian Society of Pediatric surgery. Ital J Pediatr. (2023) 49:69. doi: 10.1186/s13052-023-01458-z
15. Hampl, SE, Hassink, SG, Skinner, AC, Armstrong, SC, Barlow, SE, Bolling, CF, et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics. (2023) 151:e2022060640. doi: 10.1542/peds.2022-060640
16. Chrissini, MK, and Panagiotakos, DB. Public health interventions tackling childhood obesity at European level: a literature review. Prev Med Rep. (2022) 30:102068. doi: 10.1016/j.pmedr.2022.102068
17. Kansra, AR, Lakkunarajah, S, and Jay, MS. Childhood and adolescent obesity: a review. Front Pediatr. (2020) 8:581461. doi: 10.3389/fped.2020.581461
18. Xi, Y, Gao, W, Zheng, K, Lv, J, Yu, C, Wang, S, et al. The roles of genetic and early-life environmental factors in the association between overweight or obesity and hypertension: a population-based twin study. Front Endocrinol (Lausanne). (2021) 12:743962. doi: 10.3389/fendo.2021.743962
19. Pledger, SL, and Ahmadizar, F. Gene-environment interactions and the effect on obesity risk in low and middle-income countries: a scoping review. Front Endocrinol (Lausanne). (2023) 14:1230445. doi: 10.3389/fendo.2023.1230445
20. World Health Organization (2025). Obesity. Available online at: https://www.who.int/health-topics/obesity#tab=tab_1 (Accessed August 9, 2025)
21. World Health Organization (2016). Report of the commission on ending childhood obesity. Available online at: https://www.who.int/publications/i/item/9789241510066 (Accessed November 5, 2023)
22. Bean, MK, LaRose, JG, Raynor, HA, Adams, EL, Evans, RK, Farthing, S, et al. The role of parents in adolescent obesity treatment: results of the teens+ randomized clinical pilot trial. Pediatr Obes. (2022) 17:e12858. doi: 10.1111/ijpo.12858
23. Kim, HS, Park, J, Park, K-y, Lee, M-N, and Ham, OK. Parent involvement intervention in developing weight management skills for both parents and overweight/obese children. Asian Nurs Res. (2016) 10:11–7. doi: 10.1016/j.anr.2015.07.006
24. Vukovic, R, Dos Santos, TJ, Ybarra, M, and Atar, M. Children with metabolically healthy obesity: a review. Front Endocrinol (Lausanne). (2019) 10:865. doi: 10.3389/fendo.2019.00865
25. Onay, T, Beyazıt, U, Uçar, A, and Bütün Ayhan, A. Obesity in childhood: associations with parental neglect, nutritional habits, and obesity awareness. Front Nutr. (2024) 11:1430418. doi: 10.3389/fnut.2024.1430418
26. Abbas, N, Rouaiheb, H, Saliba, J, and El-Bikai, R. Childhood obesity: facts and parental perceptions. World Acad Sci J. (2023) 5:38. doi: 10.3892/wasj.2023.215
27. Fisher, K, Palmateer, L, Nelson, R, and Chandler, J. Does increasing parental knowledge of healthy behaviors lead to lifestyle changes for overweight or obese children? A prospective study. Inter J Sport Exer Health Res. (2022) 6:1–6. doi: 10.31254/sportmed.6101
28. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gotzsche, PC, Vandenbroucke, JP, et al. The strengthening the reporting of observational studies in epidemiology (Strobe) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
29. Cai, S, Dang, J, Zhong, P, Ma, N, Liu, Y, Shi, D, et al. Sex differences in metabolically healthy and metabolically unhealthy obesity among Chinese children and adolescents. Front Endocrinol (Lausanne). (2022) 13:980332. doi: 10.3389/fendo.2022.980332
30. Ooi, DSQ, Toh, JY, Ng, LYB, Peng, Z, Yang, S, Rashid, N, et al. Dietary intakes and eating behavior between metabolically healthy and unhealthy obesity phenotypes in Asian children and adolescents. Nutrients. (2022) 14:4796. doi: 10.3390/nu14224796
31. Gebeyehu, DT, Bekele, D, Mulate, B, Gugsa, G, and Tintagu, T. Knowledge, attitude and practice of animal producers towards antimicrobial use and antimicrobial resistance in Oromia zone, north eastern Ethiopia. PLoS One. (2021) 16:e0251596. doi: 10.1371/journal.pone.0251596
32. Al-Qahtani, AM. Clean hands, safe care: how knowledge, attitude, and practice impact hand hygiene among nurses in Najran, Saudi Arabia. Front Public Health. (2023) 11:1158678. doi: 10.3389/fpubh.2023.1158678
33. Diao, X, Gao, L, Yang, Y, Chen, X, Gong, J, Qian, Y, et al. Knowledge and attitudes towards obesity and bariatric surgery in university students: a National Survey. Obes Surg. (2022) 32:2869–79. doi: 10.1007/s11695-022-06157-y
34. Xue, B, Zhang, X, Li, T, Gu, Y, Wang, R, Chen, W, et al. Knowledge, attitude, and practice of obesity among university students. Ann Palliat Med. (2021) 10:4539–46. doi: 10.21037/apm-21-573
35. Straughan, PT, and Xu, C. Parents’ knowledge, attitudes, and practices of childhood obesity in Singapore. SAGE Open. (2022) 12. doi: 10.1177/21582440221144436
36. Mabiala Babela, JR, Nika, ER, Nkounkou Milandou, KG, Missambou Mandilou, SV, Bouangui Bazolana, SB, Monabeka, HG, et al. Knowledge, attitudes, and practices of parents facing child and adolescent obesity in Brazzaville, Congo. Glob Pediatr Health. (2016) 3:2333794X16675546. doi: 10.1177/2333794X16675546
37. Rausch, JC, Berger-Jenkins, E, Nieto, AR, McCord, M, and Meyer, D. Effect of a school-based intervention on parents’ nutrition and exercise knowledge, attitudes, and behaviors. Am J Health Educ. (2015) 46:33–9. doi: 10.1080/19325037.2014.977411
38. Somannavar, MS, and Appajigol, JS. Knowledge, attitudes, and practices of public sector primary health care physicians of rural North Karnataka towards obesity management. J Family Med Prim Care. (2014) 3:400–3. doi: 10.4103/2249-4863.148126
39. Zoghby, HB, Sfeir, E, Akel, M, Malaeb, D, Obeid, S, and Hallit, S. Knowledge, attitude and practice of Lebanese parents towards childhood overweight/obesity: the role of parent-physician communication. BMC Pediatr. (2022) 22:209. doi: 10.1186/s12887-022-03279-1
40. Svendsen, MT, Bak, CK, Sorensen, K, Pelikan, J, Riddersholm, SJ, Skals, RK, et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large National Population-Based Survey among Danish adults. BMC Public Health. (2020) 20:565. doi: 10.1186/s12889-020-08498-8
41. Case, A, and Paxson, C. Parental behavior and child health. Health Aff (Millwood). (2002) 21:164–78. doi: 10.1377/hlthaff.21.2.164
42. Flores, G, Bauchner, H, Feinstein, AR, and Nguyen, US. The impact of ethnicity, family income, and parental education on children's health and use of health services. Am J Public Health. (1999) 89:1066–71. doi: 10.2105/ajph.89.7.1066
43. Gibbs, BG, and Forste, R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr Obes. (2014) 9:135–46. doi: 10.1111/j.2047-6310.2013.00155.x
44. Andrade, C, Menon, V, Ameen, S, and Kumar Praharaj, S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J Psychol Med. (2020) 42:478–81. doi: 10.1177/0253717620946111
45. World Health Organization. (2008) Advocacy, communication and social mobilization for tb control: a guide to developing knowledge, attitude and practice surveys. Available online at: http://whqlibdoc.who.int/publications/2008/9789241596176_eng.pdf (Accessed November 22, 2022)
46. Lyu, Y, Hu, CY, Sun, L, Qin, W, Xu, PP, Sun, J, et al. Impact of an intervention programme on knowledge, attitudes and practices of population regarding severe fever with thrombocytopenia syndrome in endemic areas of Lu’an. China Epidemiol Infect. (2018) 146:125–36. doi: 10.1017/s0950268817002679
47. Pham, HT, Tran Doan, M-T, Dang Thi, T, Nguyen Tuan, D, Tran, M-H, and Nguyen, TNP. Impact of multifaceted interventions on the knowledge, attitude, and practice of adverse drug reactions reporting among healthcare workers in Vietnam: a comparative intervention study. Front Pharmacol. (2024) 15:1420914. doi: 10.3389/fphar.2024.1420914
48. Bergen, N, and Labonte, R. Everything is perfect, and we have no problems: detecting and limiting social desirability Bias in qualitative research. Qual Health Res. (2020) 30:783–92. doi: 10.1177/1049732319889354
49. Latkin, CA, Edwards, C, Davey-Rothwell, MA, and Tobin, KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. (2017) 73:133–6. doi: 10.1016/j.addbeh.2017.05.005
50. Tzeng, IS. To handle the inflation of odds ratios in a retrospective study with a profile penalized log-likelihood approach. J Clin Lab Anal. (2021) 35:e23849. doi: 10.1002/jcla.23849
51. Tzeng, IS. Examination of matching methods, sparse effects, and limitations in a nationwide database study on Alzheimer’s disease. J Alzheimer’s Dis. (2023) 96:73–5. doi: 10.3233/JAD-230701
52. Tzeng, IS. Dealing with the problem of monotone likelihood in the onflation of estimated effects in clinical studies. comment on hasegawa et al. impact of blood type O on mortality of sepsis patients: a multicenter retrospective observational study. diagnostics 2020, 10, 826. Diagnostics (Basel). (2022) 12:2295. doi: 10.3390/diagnostics12102295
53. Sullivan, GM, and Feinn, RS. Facts and fictions about handling multiple comparisons. J Grad Med Educ. (2021) 13:457–60. doi: 10.4300/jgme-d-21-00599.1
Keywords: children, adolescents, obesity, metabolically, obesity, health knowledge, attitude, practice, cross-sectional studies
Citation: Zhong F, Feng J, Zhang L, Lu L, Yuan H, Li J, Tian T and Hu Y (2025) Parents of children and adolescents knowledge, attitude, and practice toward metabolically healthy obesity: a cross-sectional survey. Front. Public Health. 13:1591300. doi: 10.3389/fpubh.2025.1591300
Edited by:
Ana Mª García-Muñoz, UCAM Universidad Católica de Murcia, SpainReviewed by:
Antonio Di Lorenzo, University of Bari Aldo Moro, ItalyGizem Öztürk, Fenerbahçe University, Türkiye
Copyright © 2025 Zhong, Feng, Zhang, Lu, Yuan, Li, Tian and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youfang Hu, MTMxODI4MjM5MDNAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Fengyu Zhong1†
Fengyu Zhong1† Tian Tian
Tian Tian Youfang Hu
Youfang Hu