- 1School of Public Health, Karaganda Medical University, Karaganda, Kazakhstan
- 2Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia
Introduction: Hand hygiene is a fundamental public health measure that plays a crucial role in preventing the spread of infectious diseases, particularly in communal settings such as schools. The COVID-19 pandemic heightened awareness of hygiene practices, emphasizing the need for sustained interventions to ensure long-term adherence and improved health outcomes among students. This research aims to examine the key factors that shaped students’ hygiene behaviors during the COVID-19 pandemic and evaluate strategies for reinforcing and sustaining these practices over time.
Methods: This study utilized a cross-sectional design to evaluate hand hygiene practices and influencing factors among 3,980 students from grades 5, 9, and 11 in the Karaganda region of Kazakhstan during the COVID-19 pandemic. Data were analyzed using IBM SPSS Statistics 26.0, with Chi-square tests assessing group differences and binary logistic regression identifying factors associated with students’ handwashing behaviors.
Results: The results revealed that several factors, including school discussions on handwashing, school type (urban vs. rural), gender, grade level, and parental occupation and education, were significantly associated with improved handwashing behavior among students. Urban students, females, higher-grade students, and those with highly educated or employed parents demonstrated better hand hygiene practices, with school-based discussions on handwashing increasing the odds by 38%.
Conclusion: This study underscores the critical role of educational interventions, sociodemographic factors, and infrastructure in shaping students’ hand hygiene behaviors, emphasizing the need for sustained efforts to reinforce proper handwashing practices through school-based education, policy support, and improved hygiene facilities.
1 Introduction
Hygiene plays a critical role in public health, serving as a foundational element in the prevention of disease and the promotion of overall well-being. The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) emphasize that effective handwashing with soap and clean water is a key intervention in reducing disease transmission (1, 2). The COVID-19 pandemic significantly increased awareness and adherence to hand hygiene practices, emphasizing their importance not only in preventing COVID-19, but also in reducing the transmission of other infectious diseases (3, 4). Beyond COVID-19 prevention, improved handwashing practices have contributed to a decline in various infectious diseases such as gastrointestinal infections and respiratory infections, underscoring the long-term benefits of hygiene awareness (5).
Hand hygiene is particularly critical in school environments, where students interact closely, creating opportunities for disease transmission (6). Studies have shown that proper handwashing can reduce respiratory infections by up to 21% and gastrointestinal infections by 31% among schoolchildren (7, 8). Additionally, interventions promoting hand hygiene in schools have been effective in reducing Escherichia coli contamination and lowering incidences of diarrheal diseases and respiratory infections (9–11). Despite these benefits, many schools, especially in low- and middle-income countries, lack the necessary infrastructure, such as handwashing stations and consistent access to clean water, to support effective hygiene practices (12, 13). The COVID-19 pandemic further exacerbated these challenges, particularly in disadvantaged area, where schools struggled to maintain hygiene facilities and supplies (14).
Behavioral factors also play a crucial role in students’ adherence to hand hygiene. Studies suggest that children are more likely to wash their hands if they perceive it as a social norm among their caregivers, highlighting the impact of peer influence (15, 16). Additionally, structured hygiene curricula, strategically placed handwashing stations, and teacher-led demonstrations have been shown to significantly improve handwashing frequency among students (17, 18). However, despite increased awareness during the COVID-19 pandemic, sustaining improved hygiene behaviors remained challenging, especially among younger students, who may not fully grasp the long-term health benefits of handwashing (19, 20).
Although hygiene’s role in preventing infectious diseases is well-documented, there is a lack of comprehensive research evaluating school students’ hygiene behaviors in Central Asian countries, particularly during the COVID-19 pandemic. Existing studies have primarily focused on general public health measures, rather than the behavioral responses of students to pandemic-driven hygiene interventions. Moreover, little is known about the factors influencing students’ long-term adherence to hygiene practices once emergency health measures are removed. Kazakhstan, as one of the largest and most socioeconomically diverse countries in Central Asia, serves as a valuable case study for understanding these dynamics (21, 22). The findings of this study can contribute to a broader understanding of hygiene behaviors in the Karaganda region in Central Kazakhstan and inform the development of effective, long-term hygiene interventions in educational settings.
This research aims to identify the key factors that influenced students’ hygienic behavior during the COVID-19 pandemic and assess how these behaviors can be reinforced, and sustained over time. By providing evidence-based insights, the study will contribute to school-based public health interventions and broader hygiene promotion strategies, ensuring that the benefits of heightened hygiene awareness during the pandemic translate into lasting public health improvements.
2 Materials and methods
2.1 Study area
The Karaganda Region is one of the largest administrative divisions of Kazakhstan, situated in the center of the Eurasian continent (Figure 1). Geographically, the region is equidistant from the Arctic, Indian, Atlantic, and Pacific Oceans, which determines its sharply continental climate. The region covers the most elevated part of the Kazakh Hills—Saryarka (23).

Figure 1. The location and borders of the Karaganda region (selected area) on Kazakhstan map (before the 8 June, 2022). NB - the study was conducted before the division of the region.
The administrative center of the region is the city of Karaganda, founded in 1934. Today, the Karaganda region is one of the industrial regions of Kazakhstan, as it is rich in minerals and raw materials. It occupies 239,045 square km, which contains 8.7 of the whole territory of the Republic. As of January 1, 2025, the population of the region was 1,134.0 thousand people, of whom 929.8 thousand (82%) resided in urban areas, while 204.2 thousand (18%) lived in rural areas (24). 504 public schools operate in the Karaganda region. The number of students was about 204 thousand (204,174) in 2020 (25).
The region comprises eight cities, including six of regional significance and two of district significance. Additionally, there are eight settlements and 349 rural localities within the region.
The climate is sharply continental, characterized by 5.5 months of long cold winter and highly arid, with 3 months of hot summer. Temperature is about −16–17 °C in winter and 20–21 °C in summer. On summer days, the temperature can rise to 37 degrees. The coldest month is January. Frosts reach up to 40 degrees. Annual precipitation in the region’s north is 250–300 mm; in the south – 150–210 mm; in the low mountainous areas – 300–400 mm. It rains mainly from April to October.
2.2 Study population
This study employed a cross-sectional design to assess hand hygiene practices and associated factors among students in grades 5, 9, and 11 during the COVID-19 pandemic. The study population comprised 3,980 students enrolled in schools within the Karaganda region of Kazakhstan. Inclusion criteria specified students from grades 5, 9, and 11, attending either rural or urban schools within the region. A simple random sampling method was employed to select participants, ensuring an equal chance of inclusion for all eligible students. The overall response rate was 88%; however, 523 responses were excluded from the analysis due to incomplete data submission.
The study was conducted online among students attending schools in Karaganda region, Central Kazakhstan, between April 2 and May 20, 2021. An electronic questionnaire was disseminated to teachers through school administrations and subsequently completed by students. It was carried out during the resumption of face-to-face education in schools across Kazakhstan amid the COVID-19 pandemic (26). According to the resolution, in regions classified as high-risk zones, combined-format education was implemented. This included face-to-face instruction for preschool students and grades 1 to 5 with class sizes limited to 25 children, and a hybrid format for graduating classes (grades 9 and 11), with 70% of lessons conducted in person and 30% online. Strict sanitary, disinfection, and mask compliance measures were followed, with a limit of 15 students per class and adherence to the “1 class - 1 room” principle.
Prior to data collection, informed consent forms were distributed to parents through students in sealed envelopes to obtain written parental consent. The signed forms were returned to the teachers via the students. A collaboration plan was coordinated with school administrators to facilitate data collection. Participation in the study was voluntary, and students were informed about the study’s purpose before verbal assent was obtained. Data were collected online within the classroom environment, following a prearranged schedule. Completing the survey took approximately 10–15 min per participant.
2.3 Data analysis
The socio-demographic characteristics of the participants were assessed through seven questions, which addressed age, gender, grade level, and the educational and employment status of their parents. Hand Hygiene Behavior Form consisted of nine items designed based on existing literature (19, 27–29). The questions aimed to evaluate participants’ hand hygiene behaviors during the COVID-19 pandemic. The form was based on the WHO/UNICEF framework “Surveillance of Water, Sanitation and Hygiene in Schools,” with selected items from the hygiene section adapted for use in this study (27). The questions were modified to reflect the local school context and to ensure cultural appropriateness. Content validity was assessed through expert review by public health professionals and school administrators. The instrument was translated into both Kazakh and Russian, followed by back-translation to ensure linguistic accuracy and conceptual consistency. A pilot test was conducted with a small group of students to evaluate the clarity and comprehensibility of the items. Minor revisions were made based on the pilot feedback prior to full-scale implementation. The items focused on specific handwashing circumstances and procedures. Respondents were asked to indicate whether they washed their hands in particular situations, including, when hands were visibly dirty, before meals, after using the toilet, after playing with pets, after contact with an unwell individual, after using public transportation, upon returning home, and when washing hands with soap and water. Issues associated with inadequate handwashing were also explored. Responses were scored on a binary scale, with “Yes” assigned 1 point and “No” assigned 0 points, yielding a total possible score range of 0 to 9. The internal consistency reliability of the Hand Hygiene Behavior Form was determined to be 0.79, indicating acceptable reliability for this assessment tool.
Statistical analysis was performed using IBM SPSS Statistics 26.0 package program. Group differences were assessed using the Chi-square test (χ2) to evaluate statistical significance. A binary logistic regression was conducted to identify factors associated with hand hygiene practices. The dependent variable was students’ handwashing behavior, with independent variables comprising a range of demographic factors. The statistical significance level was taken as 0.05 in all tests. In order to obtain statistical results.
2.4 The ethical principles of the study
To conduct the study, ethical approval was obtained from the Bioethics Committee at Karaganda Medical University (approval dated 12/04/2021, No 18), with legal permission from the Department of Education of the Karaganda Region. The survey was administered in both Kazakh and Russian to accommodate the linguistic diversity of students in the region’s schools.
Following the collection of written parental consent, students were informed about the purpose and voluntary nature of the study. It was emphasized that participation was entirely optional, and students could withdraw from the study at any time without facing any consequences. Confidentiality of personal information was guaranteed, and students were assured that non-participation would not affect their grades or academic standing.
3 Results
3.1 Scenarios for assessing handwashing behavior
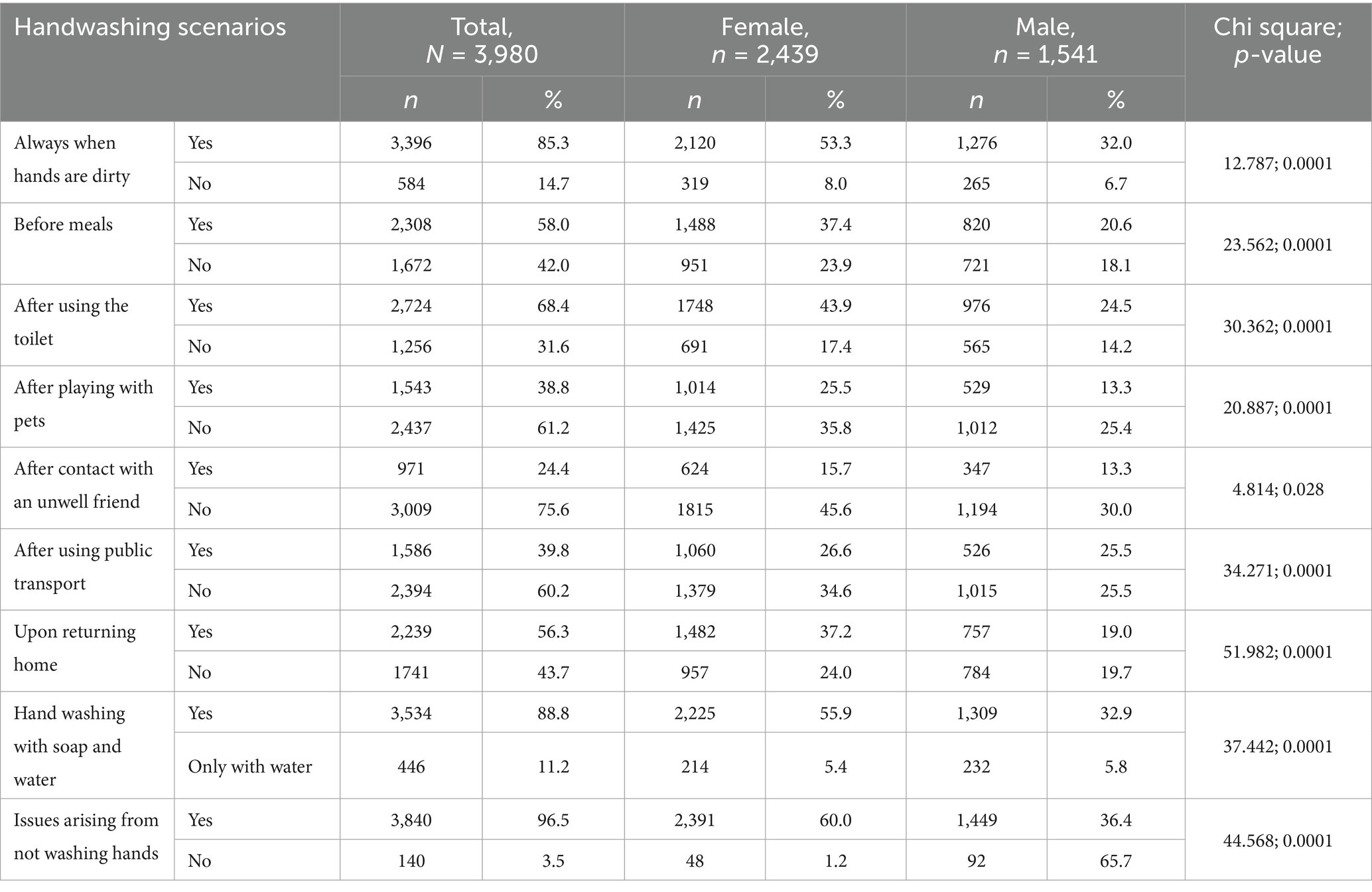
Nine survey items were used to assess handwashing practices among students (Table 1). The findings revealed that 85.3% of respondents consistently wash their hands, when visibly dirty and 90% reported regular handwashing with soap and water. The majority of participants demonstrated an understanding of the potential health risks associated with inadequate hand hygiene. Additionally, 60% of students reported washing their hands before meals, upon returning home, and after using the toilet. In contrast, 40% of students reported handwashing after interacting with pets or using public transportation. Only 24.4% of students practiced hand hygiene following contact with an unwell individual.
A significant disparity in handwashing practices was identified between female and male students. Female students demonstrated a higher frequency of handwashing across various situations, with chi-square test results indicating statistically significant differences between the girls and boys (p ≤ 0.05). Handwashing behavior was classified as “adequate” when respondents affirmed at least seven of the assessed items. Conversely, responses with fewer than seven affirmative answers were categorized as “inadequate” handwashing behavior. This threshold is consistent with scoring approaches used in prior cross-sectional studies on student hygiene behavior during COVID-19, where engaging in at least two-thirds to three-quarters of recommended practices was treated as sufficient for classification as “adequate” hygiene [19, 28, 29].
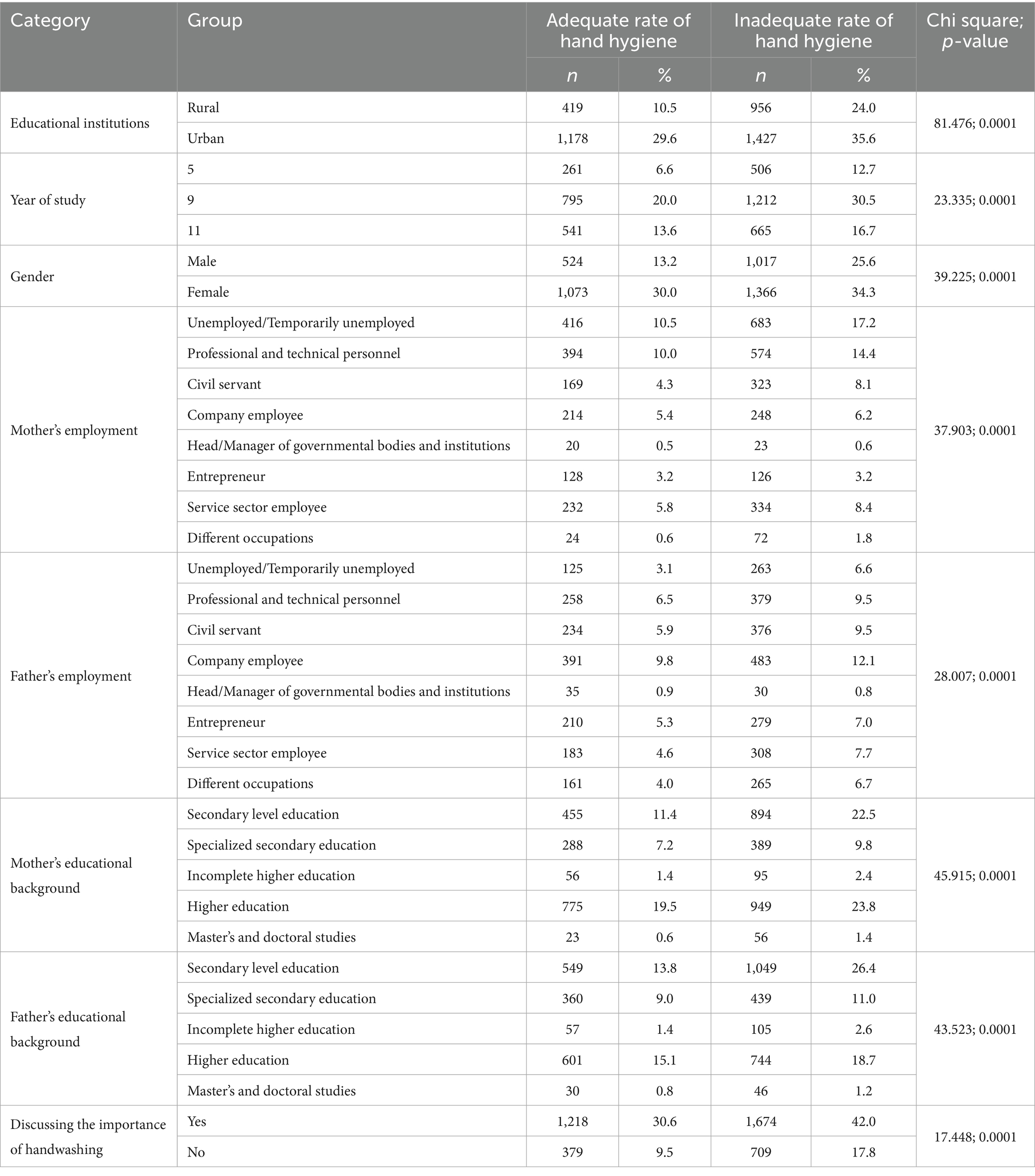
Overall, 40.1% of students demonstrated adequate hand hygiene practices (n = 1,597). Results from the chi-square analysis indicated statistically significant associations between hand hygiene adequacy and variables, such as school location (χ2 = 81.476, p < 0.01), gender (χ2 = 39.225, p < 0.01), grade level (χ2 = 23.335, p < 0.01), father’s occupation (χ2 = 28.007, p < 0.01), mother’s occupation (χ2 = 37.903, p < 0.01), mother’s educational level (χ2 = 45.915, p < 0.01), father’s educational level (χ2 = 43.523, p < 0.01), and discussions on handwashing at school (χ2 = 17.448, p < 0.01).
3.2 Demographic characteristics and comparative analysis of hand hygiene practices among school children
The analysis included data from 3,980 students, with a 63.9% being female (n = 2,439) and 36% (n = 1,375) from urban schools. The distribution across grade levels showed that half of the respondents were from the 9th grade (50.5%, n = 2007) (Table 2).
Regarding parental occupation, 27.7% of students’ mothers were unemployed, including housewives, while 24.4% were professional and technical personnel. Fathers showed higher occupational diversity: 21.9% were company employees, 16% were professional and technical personnel, and 12.3% each were businessmen and service sector employees.
In terms of education, 43.3% of mothers and 33.8% of fathers have higher education, with fathers more likely to have lower or upper secondary education (40.2%) compared to mothers (33.9%). Postgraduate education was rare, with only 2% of mothers and 1.9% of fathers attaining this level.
3.3 Factors associated with hand hygiene
In the binary logistic regression analysis, several factors, including handwashing discussions at school, school type (urban or rural), gender, grade level, and parental occupation and education showed significant associations with improved handwashing behavior (Table 3).
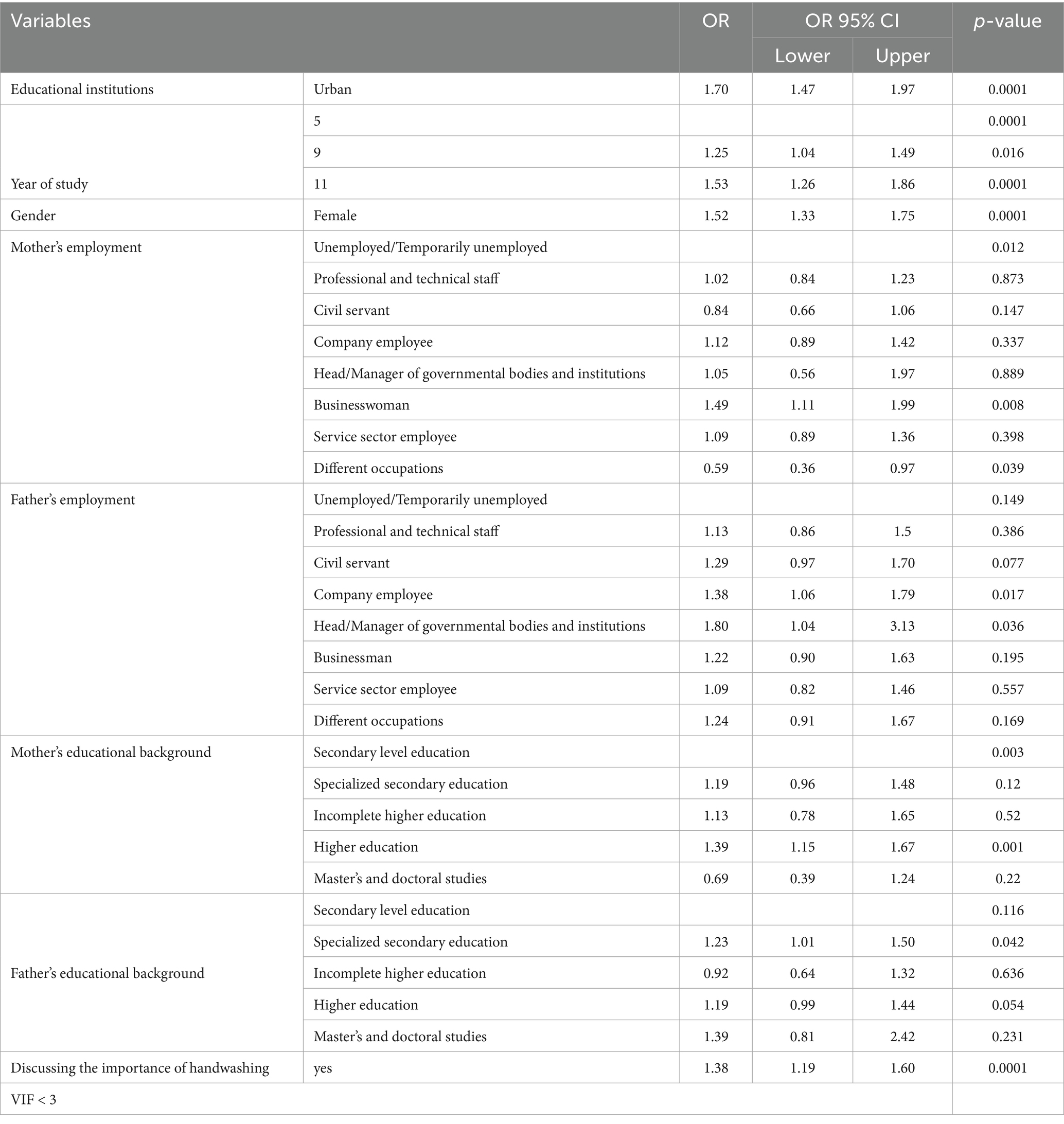
Table 3. Binary logistic regression analysis of factors influencing hand hygiene compliance (n = 3,980).
Urban school students demonstrated 1.70 times (95% CI = 1.47–1.97, p < 0.01) better handwashing behavior than those in rural schools. Gender differences were also evident, with female students being 1.52 times (95% CI = 1.33–1.75, p < 0.01) more likely to practice better handwashing compared to male students.
Grade level had a notable impact, as students in grade 9 were 1.25 times (95% CI = 1.04–1.49, p < 0.05) and those in grade 11 were 1.53 times (95% CI = 1.26–1.86, p < 0.01) more likely to exhibit good handwashing habits compared to students in grade 5.
Parental occupation also played a significant role. Students, whose mothers were businesswomen demonstrated 1.49 times (95% CI = 1.11–1.99, p < 0.01) better handwashing behavior than those with temporarily unemployed mothers. In contrast, students whose mothers selected “other” for occupation were 41% less likely to exhibit good handwashing behavior (OR = 0.59, 95% CI = 0.36–0.97, p < 0.05) compared to those whose mothers were unemployed.
Similarly, students whose fathers were company employees or held managerial positions in governmental bodies were more likely to have better handwashing behavior, with ORs of 1.38 (95% CI = 1.06–1.79, p < 0.05) and 1.80 (95% CI = 1.04–3.13, p < 0.05), respectively, compared to students with temporarily unemployed fathers.
Parental education was another determinant, with students whose mothers had a high level of education 1.39 times (95% CI = 1.15–1.67, p < 0.01) more likely to report good handwashing habits than those whose mothers had only secondary education. Fathers with secondary special education (OR = 1.23, 95% CI = 1.01–1.50, p < 0.05) and higher education (OR = 1.19, 95% CI = 0.99–1.44, p < 0.05) were also associated with better handwashing behavior among students, compared to those with secondary education.
The OR for students, who reported discussions about the importance of handwashing at school was 1.38 (95% CI = 1.19–1.60, p < 0.01), indicating a 38% higher odds of better handwashing behavior compared to students without such discussions.
4 Discussion
This study provides valuable insights into hand hygiene practices among school students in Kazakhstan, highlighting key demographic, behavioral, and educational factors that influence compliance.
The majority of students demonstrated appropriate hand hygiene practices, consistently washing their hands when visibly dirty and using soap and water. This high compliance aligns with public health guidelines, as proper handwashing is one of the most effective measures for reducing the spread of infectious diseases, including respiratory and gastrointestinal infections (30–32). Additionally, nearly all students exhibited awareness of the health risks associated with inadequate hand hygiene, reinforcing the link between knowledge and hygiene behaviors. Prior research suggests that awareness of disease transmission pathways and the protective role of handwashing significantly contributes to sustained behavioral improvements (33–35). Despite this awareness, gaps in routine hygiene behaviors persist. Only 60% of students practiced handwashing before meals and after returning home, and just three out of five students washed their hands after playing with pets or using public transportation. These findings highlight inconsistencies in compliance, particularly in contexts where students may not perceive an immediate health risk. The Health Belief Model (HBM) provides a useful framework for interpreting this behavior, as it suggests that individuals are more likely to adopt preventive measures when they perceive a high susceptibility to illness and believe that the benefits outweigh the barriers (36).
A particularly concerning is that only 25% of students in Karaganda region practiced hand hygiene after contact with a sick friend, posing a significant risk for disease transmission, particularly in school environments where close interactions facilitate the spread of infections (37–39). This discrepancy between knowledge and practice suggests that interventions should focus not only on education, but also on behavioral reinforcement strategies, such as habit formation techniques and peer modeling, to enhance adherence to critical hygiene practices. The study also identified notable gender differences, with female students exhibiting significantly better hand hygiene practices than males. This finding is consistent with global research suggesting that girls tend to engage in hygiene behaviors more diligently than boys (40–42). Several factors may contribute to this trend, including social norms, parental reinforcement, and gendered health perceptions, which often encourage hygiene-conscious behaviors more strongly among girls than boys.
It appeared that urban students demonstrated better hand hygiene practices than their rural counterparts. A similar trend has also observed in previous studies from Ethiopia and other regions (43). This disparity may be attributed to differences in access to water, sanitation infrastructure, and hygiene education programs. Schools in urban settings in Kazakhstan typically benefit from better hygiene facilities, structured health curricula, and stronger public health initiatives, whereas rural schools often face resource constraints.
The findings of this study indicate that handwashing behavior improves with increasing grade level, as older students demonstrated greater adherence to proper hygiene practices compared to younger students (28, 44). Prior research has also established a positive correlation between educational level and hygiene compliance, indicating that students in higher grades are more likely to internalize and consistently practice proper handwashing habits (45).
Parental education emerged as a key determinant of students’ hand hygiene behaviors. Students with more highly educated parents—particularly mothers—demonstrated significantly better hygiene compliance, aligning with existing research suggesting that higher parental educational attainment correlates with improved health behaviors among children (46, 47). Educated parents are more likely to emphasize hygiene at home, provide access to proper sanitation resources, and model good handwashing behavior of children. Additionally, maternal occupation was linked to students’ hand hygiene habits, potentially reflecting differences in health literacy, exposure to hygiene-related information, and household health priorities across occupational groups (48).
Students who engaged in discussions about handwashing at school demonstrated higher compliance, emphasizing the importance of education and awareness in shaping hygiene behaviors. Research consistently highlights that structured hygiene education—whether delivered through school curricula, peer discussions, or teacher-led initiatives—significantly improves adherence to hand hygiene practices (49–52). Integrating hand hygiene education into school programs and ensuring that teachers actively reinforce these lessons can help sustain long-term behavioral change. Moreover, behavioral interventions such as habit formation strategies, nudges (e.g., reminder posters near sinks), and positive reinforcement techniques can help bridge the gap between knowledge and practice. Empirical evidence suggests that motivational strategies, combined with accessible infrastructure (readily available soap and water), enhance compliance and long-term sustainability of hygiene behaviors (53).
The integration of behavioral theories provides a valuable lens for interpreting the determinants of handwashing behavior among school-aged children. The Theory of Planned Behavior (TPB) posits that behavioral intention is shaped by attitudes, subjective norms, and perceived behavioral control—all of which are relevant in the school context (54, 55). Positive attitudes toward hand hygiene, often fostered through health education, have been associated with greater compliance (48, 56). Similarly, subjective norms—reinforced through peer influence and support from educators—play a pivotal role in shaping normative beliefs and behavior (57, 58). Perceived behavioral control, including the availability of handwashing facilities and opportunities for skill reinforcement, enhances self-efficacy and behavioral consistency (8, 59). Complementing TPB, Social Cognitive Theory (SCT) emphasizes self-efficacy, observational learning, and social influences as core constructs influencing behavior. Evidence suggests that modeling, peer-led demonstrations, and environmental cues can significantly enhance hand hygiene practices (11, 16, 60). Together, TPB and SCT underscore the importance of multifaceted, theory-driven interventions that combine individual motivation, peer dynamics, and structural facilitators to support sustained handwashing behavior in school settings.
At a policy level, implementing comprehensive WASH programs in schools, particularly in underserved areas in Kazakhstan, is essential for improving public health outcomes (61, 62). Investments in hygiene infrastructure, teacher training, and community-based awareness campaigns can help ensure that hygiene promotion becomes a sustained public health priority rather than a reactive response to health crises. This study makes a significant contribution to public health research by examining hand hygiene behaviors among school students during the COVID-19 pandemic, a period of heightened awareness but also considerable logistical challenges in data collection. Despite these challenges, the study successfully gathered data from nearly 4,000 students, offering a large and representative dataset that provides valuable insights into hygiene behaviors in a high-risk context in Central Asia.
However, certain limitations and targeted recommendations for future research must be acknowledged. A notable aspect is the higher proportion of female students in the sample, which does not align with the overall gender distribution of children in Kazakhstan, where male children slightly outnumber female children (24). Additionally, urban students were overrepresented compared to their rural counterparts, a trend that reflects Kazakhstan’s population distribution. The overrepresentation of female students and urban schools in the sample may have biased the results, particularly if hygienic behaviors or access to hygiene facilities differ systematically by location. Female students may be more likely to report or engage in certain health-related behaviors, and urban schools may have better hygiene infrastructure and awareness programs compared to rural counterparts. As a result, the findings may overestimate the overall level of hygienic behavior among schoolchildren in Kazakhstan. Future research should aim to address these disparities by employing stratified sampling strategy to ensure representative inclusion of male and rural students. Moreover, future research should consider employing multilevel or hierarchical modeling to account for potential school-level clustering, which may influence student behavior and associated predictors. The reliance on self-reported data introduces the potential for social desirability bias and recall bias, as students may have over-reported their adherence to hygiene practices due to perceived social expectations. Although measures were taken to mitigate this bias—such as ensuring respondent anonymity and emphasizing the confidentiality of responses—some inflation of reported compliance is likely. Future research should consider the use of objective assessment methods, including direct observation or sensor-based monitoring, to enhance the validity and reliability of behavioral data. Additionally, as a cross-sectional study, the findings capture hygiene behaviors at a single point in time, limiting the ability to assess long-term behavioral changes. Specifically, while associations with variables such as parental education or school location may suggest influences on behavior, we cannot determine the directionality or permanence of these effects. As such, interpretations regarding sustained behavior change over time should be made with caution. Future research should consider longitudinal studies to examine how hand hygiene behaviors evolve over time and identify socio-cultural factors that influence sustained compliance. Additionally, qualitative research could provide deeper insight into the motivations, contextual influences, and barriers affecting student hygiene practices. Although no formal knowledge translation initiatives were implemented, preliminary findings were informally shared with participating schools and discussed with local education staff, and a WASH course was developed and distributed in select institutions. While these efforts contributed to initial engagement, the lack of a structured dissemination strategy limits broader impact. Future studies should prioritize systematic knowledge translation approaches to support policy translation and sustainable school-based interventions.
5 Conclusion
Current study highlights positive trends and areas for improvement in the hand hygiene behaviors of school students in Kazakhstan. While self-reported awareness of handwashing is high, significant gaps remain in routine practices. The study identifies key factors influencing students’ handwashing behavior, highlighting the role of sociodemographic and educational determinants. Students from urban schools, female students, those in higher grade levels, and those with parents who are employed and have higher education levels demonstrated significantly better handwashing practices. Furthermore, school-based discussions on handwashing were strongly associated with improved hygiene behavior, underscoring the importance of educational interventions in promoting proper hand hygiene among students.
Strengthening hand hygiene requires a combination of education, behavioral reinforcement, and infrastructure improvements. Schools should integrate structured hygiene education, peer-led discussions, and teacher reinforcement, while community-based awareness programs can further support hygiene promotion. Investments in WASH infrastructure, particularly in underserved areas, and longitudinal research on sustainable behavior change are essential for long-term impact.
The COVID-19 pandemic reinforced the importance of hand hygiene in preventing disease transmission, underscoring the need for sustained interventions beyond the crisis. Handwashing must be ingrained as a lifelong habit through education, policy support, and behavioral reinforcement. Schools, policymakers, and health authorities must collaborate to ensure access to hygiene facilities and structured education programs. Investing in hygiene education and infrastructure not only reduces infection risks but also fosters a healthier, more resilient generation. The lessons learned must drive permanent improvements in hygiene practices, ensuring that clean hands save lives every day, not just in times of crisis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Bioethics Committee at Karaganda Medical University (approval dated 12/04/2021, No 18). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
ZB: Conceptualization, Investigation, Formal analysis, Writing – review & editing, Methodology, Writing – original draft. MK: Writing – review & editing, Supervision, Investigation. KN: Writing – review & editing, Formal analysis. OZ: Writing – review & editing, Data curation. ZD: Writing – review & editing, Validation. GK: Resources, Writing – review & editing. NY: Visualization, Writing – review & editing. HO: Writing – review & editing, Supervision, Conceptualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of thisarticle.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1593579/full#supplementary-material
References
1. UN-Water. Global handwashing day 2020: Hand hygiene for all (2020). Available online at:https://www.unwater.org/news/global-handwashing-day-2020-hand-hygiene-all#:~:text=Global%20Handwashing%20Day%20is%20October,of%20hand%2Dwashing%20with%20soap [accessed January 1, 2025]
2. Han, M. Hand hygiene practices among adults with diabetes living in communities: the 2015 Korea community health survey. Int J Environ Res Public Health. (2019) 16:1279. doi: 10.3390/ijerph16071279
3. Głąbska, D, Skolmowska, D, and Guzek, D. Population-based study of the influence of the covid-19 pandemic on hand hygiene behaviors—polish adolescents’ covid-19 experience (place-19) study. Sustainability. (2020) 12:4930. doi: 10.3390/su12124930
4. Frederic, B. Assessment of knowledge about hygiene during covid-19 pandemic in catchment area of kaziba health Centre. Texila Int J Acad Res. (2022) 9:76–88. doi: 10.21522/tijar.2014.09.04.art007
5. Ali, AS, Yohannes, MW, and Tesfahun, T. Hygiene behavior and COVID-19 pandemic: opportunities of COVID-19-imposed changes in hygiene behavior. Inquiry. (2023) 60:469580231218421. doi: 10.1177/00469580231218421
7. Luby, SP, Halder, AK, Huda, T, Unicomb, L, and Johnston, RB. The effect of handwashing on child diarrhea in rural Bangladesh: an observational study. PLoS Med. (2011) 8:e1001052. doi: 10.1371/journal.pmed.1001052
8. Pasewaldt, S, Baller, S, Blackstone, S, and Malenke, L. Impact of a hand hygiene curriculum and group handwashing station at two primary schools in East Africa. Int Q Community Health Educ. (2018) 39:175–87. doi: 10.1177/0272684x18819968
9. Idris, H, Syakurah, R, and Safriantini, D. Hand hygiene knowledge among hospital health workers in Palembang during COVID-19 era. J Adm Kesehat Indones. (2021) 9:218–25. doi: 10.20473/jaki.v9i2.2021.218-225
10. McGuinness, S, Barker, F, O'Toole, J, Cheng, A, Forbes, A, Sinclair, M, et al. Effect of hygiene interventions on acute respiratory infections in childcare, school and domestic settings in low- and middle-income countries: a systematic review. Trop Med Int Health. (2018) 23:816–33. doi: 10.1111/tmi.13080
11. Watson, J, Ensink, J, Ramos, M, Benelli, P, Holdsworth, E, Dreibelbis, R, et al. Does targeting children with hygiene promotion messages work? The effect of handwashing promotion targeted at children, on diarrhoea, soil-transmitted helminth infections and behaviour change, in low- and middle-income countries. Trop Med Int Health. (2017) 22:526–38. doi: 10.1111/tmi.12861
12. Poague, KIHM, Blanford, JI, and Anthonj, C. Water, sanitation and hygiene in schools in low- and middle-income countries: a systematic review and implications for the covid-19 pandemic. Int J Environ Res Public Health. (2022) 19:3124. doi: 10.3390/ijerph19053124
13. Zuthi, MFR, Hossen, MA, Pal, SK, Mazumder, MH, Hasan, SF, and Hoque, MM. Evaluating knowledge, awareness and associated water usage towards hand hygiene practices influenced by the current covid-19 pandemic in Bangladesh. Groundw Sustain Dev. (2022) 19:100848. doi: 10.1016/j.gsd.2022.100848
14. Toleubekov, B, Bolatova, Z, and Stafström, M. Assessing access to wash in urban schools during covid-19 in Kazakhstan: case study of Central Kazakhstan. Int J Environ Res Public Health. (2022) 19:6438. doi: 10.3390/ijerph19116438
15. Watson, J, Cumming, O, and Dreibelbis, R. Nongovernmental organization practitioners' perspectives on the challenges and solutions to changing handwashing behavior in older children: a qualitative study. Global Health Sci Practice. (2023) 11:e2200231. doi: 10.9745/GHSP-D-22-00231
16. Jetha, Q, Bisserbe, C, McManus, J, Waldroop, D, Naliponguit, EC, Villasenor, JM, et al. Can social motivators improve handwashing behavior among children? Evidence from a cluster randomized trial of a school hygiene intervention in the Philippines. Am J Trop Med Hyg. (2020) 104:756–65. doi: 10.4269/ajtmh.20-0174
17. Luby, S, Rahman, M, Arnold, B, Unicomb, L, Ashraf, S, Winch, P, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob Health. (2018) 6:e302–15. doi: 10.1016/s2214-109x(17)30490-4
18. Mbakaya, B, Lee, P, and Lee, R. Hand hygiene intervention strategies to reduce diarrhoea and respiratory infections among schoolchildren in developing countries: a systematic review. Int J Environ Res Public Health. (2017) 14:371. doi: 10.3390/ijerph14040371
19. Chen, X, Li, R, Liu, Q, Hu, Q, Du, X, and Tan, X. Hand hygiene, mask-wearing behaviors and its associated factors during the covid-19 epidemic: a cross-sectional study among primary school students in Wuhan, China. Int J Environ Res Public Health. (2020) 17:2893. doi: 10.3390/ijerph17082893
20. Huang, H, Le, N, Battle, M, Villasenor, J, and Maule, L. Nudging handwashing among primary school students in the Philippines: evidence from a cluster randomized trial. Am J Trop Med Hyg. (2021) 105:1806–15. doi: 10.4269/ajtmh.20-0673
21. Cornell, SE, Engvall, J, and Starr, SF. Kazakhstan 2041: The next twenty-five years (2016). Available online at:https://isdp.eu/wp-content/uploads/2016/11/2016-cornell-engvall-starr-kazakhsta-n-2041-1.pdf |
22. Bohr, A. Relations with other central Asian states (2023). Available online at: https://www.chathamhouse.org/2019/11/kazakhst/an-tested-transition/6-relations-other-central-asian-states
23. Kiyasov, E. Akimat of Karaganda region. Available online at: https://www.gov.kz/memleket/entities/karaganda?lang=ru [accessed January 1, 2025]
24. Bureau of National statistics Agency for Strategic planning and reforms of the Republic of Kazakhstan Available online at: https://stat.gov.kz/ru/region/karagandy/dynamic-tables/38/ [accessed January 1, 2025]
25. Agency for Strategic planning and reforms of the Republic of Kazakhstan Bureau of National statistics Available online at: https://bala.stat.gov.kz/ [accessed January 1, 2025]
26. Kiyasov, E. Resolution of the chief state sanitary doctor of the Republic of Kazakhstan №12, dated march 25, (2021).
27. Dodos, J, Grossi, V, Andronic, C, Shinee, E, and Schmoll, O. Surveillance of water, sanitation and hygiene in schools. A practical tool. Copenhagen: WHO Regional (2019).
28. Ayran, G, Köse, S, Sarıalioğlu, A, and Çelebioğlu, A. Hand hygiene and mask-wearing behaviors and the related factors during the COVID 19 pandemic: a cross-sectional study with secondary school students in Turkey. J Pediatr Nurs. (2022) 62:98–105. doi: 10.1016/j.pedn.2021.10.001
29. Skolmowska, D, Glabska, D, and Guzek, D. Hand hygiene behaviors in a representative sample of polish adolescents in regions stratified by COVID-19 morbidity and by confounding variables (place-19 study): ıs there any association? Pathogens. (2020) 9:1–22. doi: 10.3390/pathogens9121011
30. Firdaus, OH, Syabariyah, S, and Fatmawati, A. Optimizing handwashing practices through audiovisual-based health education. J Public Health Sci. (2024) 3:46–56. doi: 10.56741/jphs.v3i01.457
31. Gidado, S, Awosanya, EJ, Haladu, S, Ayanleke, HB, Idris, SH, Mamuda, I, et al. Cholera outbreak in a naïve rural community in northern Nigeria: the importance of hand washing with soap, September 2010. Pan Afr Med J. (2018) 30:5. doi: 10.11604/pamj.2018.30.5.12768
32. Berhanu, A, Mengistu, DA, Temesgen, LM, Mulat, S, Dirirsa, G, Alemu, FK, et al. Hand washing practice among public primary school children and associated factors in Harar town, eastern Ethiopia: an institution-based cross-sectional study. Front Public Health. (2022) 10:975507. doi: 10.3389/fpubh.2022.975507
33. Sharma, P, Aggarwal, T, Kalita, M, Kumar, A, Mukherjee, A, and Chaubey, DK. Knowledge and practice of handwashing by school students in kamrup metropolitan, Assam, India: a cross sectional survey. Homœopathic Links. (2023) 36:016–9. doi: 10.1055/s-0042-1758678
34. Mbakaya, BC. Associations between health education, hygiene facilities, handwashing knowledge and practice related to diarrheal disease prevention among schoolchildren after typhoid outbreak in Rumphi district, Malawi: a cross sectional survey. Biomed J Scientific Technical Res. (2019) 16:002908. doi: 10.26717/bjstr.2019.16.002908
35. Almoslem, M., Alshehri, T., Althumairi, A., Aljassim, M. T., Hassan, M. E., and Berekaa, M. M. Handwashing knowledge, attitudes, and practices among students in eastern province schools, Saudi Arabia. J Environ Public Health, (2021):6638443. doi: 10.1155/2021/6638443
36. Becker, MH. The health belief model and personal health behavior. Health Educ Monogr. (1974) 2:324–508.
37. Jalloh, A, Edo, GI, Onyibe, PN, Nwosu, LC, and Agbo, JJ. Prevalence and associated risk factors of hookworm infection among primary school children in three selected schools in Moriba town, southern Sierra Leone. Applied Microbiol Theory Technol. (2023) 4:21–32. doi: 10.37256/amtt.4120232050
38. Lavelle, F, McKernan, C, Murphy, B, and Dean, M. Food safety and convenience meals: consumers' actual and perceived behaviours – a mixed methods study. Br Food J. (2023) 125:2838–57. doi: 10.1108/bfj-05-2022-0429
39. Tripathy, RM, Acharya, GC, and Karmee, N. Assessment of wash practices among women in urban slums of Berhampur, Odisha: a cross sectional study. Int J Res Med Sci. (2017) 5:4846. doi: 10.18203/2320-6012.ijrms20174931
40. Song, IH, Kim, S, and Park, W. Family factors associated with children's handwashing hygiene behavior. J Child Health Care. (2012) 17:164–73. doi: 10.1177/1367493512456106
41. Melaku, A, and Addis, T. Handwashing practices and associated factors among school children in kirkos and Akaki kality sub-cities, Addis ababa, Ethiopia. Environ Health Insights. (2023) 17:11786302231156299. doi: 10.1177/11786302231156299
42. Dajaan, DS, Addo, HO, Ojo, L, Amegah, KE, Fiagbe, L, Bechala, BD, et al. Hand washing knowledge and practices among public primary schools in the Kintampo municipality of Ghana. Int J Community Med Public Health. (2018) 5:2205. doi: 10.18203/2394-6040.ijcmph20182146
43. Admasie, A, Guluma, A, and Feleke, FW. Handwashing practices and its predictors among primary school children in damote woide district, South Ethiopia: an institution based cross-sectional study. Environ Health Insights. (2022) 16:11786302221086795. doi: 10.1177/11786302221086795
44. Öncü, E, Vayısoğlu, SK, Lafçı, D, Yurtsever, D, Bulut, ER, and Peker, E. Comparison of interactive education versus fluorescent concretization on hand hygiene compliance among primary school students: a randomized controlled trial. J Sch Nurs. (2018) 35:337–47. doi: 10.1177/1059840518785447
45. Sultana, M, Mahumud, RA, Sarker, AR, and Hossain, SM. Hand hygiene knowledge and practice among university students: evidence from private universities of Bangladesh. Risk Manag Healthc Policy. (2016) 9:13–20. doi: 10.2147/rmhp.s98311
46. Simelane, MS. A multilevel analysis of the determinants of handwashing behavior among households in Eswatini: a secondary analysis of the 2014 multiple indicator cluster survey. Afr Health Sci. (2020) 20:1996–2006. doi: 10.4314/ahs.v20i4.58
47. Harmon, OA, Howe, TS, Schaeffer, JD, Adeboyejo, R, and Eichelberger, L. Impact of in-home handwashing stations on hand hygiene during the covid-19 pandemic in unpiped rural Alaska native homes. Public Health Rep. (2024) 139:81S–8S. doi: 10.1177/00333549241255260
48. McMichael, C. Water, sanitation and hygiene (wash) in schools in low-income countries: a review of evidence of impact. Int J Environ Res Public Health. (2019) 16:359. doi: 10.3390/ijerph16030359
49. Herbert, V, Schlumm, P, Kessler, HH, and Frings, V. Knowledge of and adherence to hygiene guidelines among medical students in Austria. Interdiscip Perspect Infect Dis. (2013) 2013:1–6. doi: 10.1155/2013/802930
50. Kadi, AA, and Salati, SA. Hand hygiene practices among medical students. Interdiscip Perspec Infectious Dis. (2012) 2012:1–6. doi: 10.1155/2012/679129
51. Nawajah, I, Radwan, E, Abuharb, M, Jabareen, H, Jazzar, M, Rebai, WK, et al. Principal component analysis of the environmental attitudes of students at faculty of economics during the COVID-19 pandemic: a cross-sectional study from Palestine. Multidiscip Sci J. (2024) 7:2025033. doi: 10.31893/multiscience.2025033
52. Nygyzbayeva, RZ, Imanbayeva, GN, Tussupbekova, MM, Stabayeva, LM, and Abiyeva, SS. Interactive training in the organization of independent work of students in universities of Kazakhstan. Med Ecology. (2023) 2:32–40. doi: 10.59598/ME-2305-6045-2023-107-2-32-40
53. Akter, T, and Ali, AM. Factors influencing knowledge and practice of hygiene in water, sanitation and hygiene (wash) programme areas of Bangladesh rural advancement committee. Rural Remote Health. (2014) 14:2628. doi: 10.22605/rrh2628
54. Ajzen, I. The theory of planned behavior. Organ Behav Hum Decis Process. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
55. Radwan, E, Alattar, E, Radwan, A, and Jebreen, K. Palestine and the COVID-19 vaccine Infodemic on social media In: M Lewis, E Govender, and K Holland, editors. Communicating COVID-19. Cham: Palgrave Macmillan (2024)
56. Sun, CY, Wang, Q, Adhikari, SP, Ye, R, Sha, M, Wu, Y, et al. Correlates of school children’s handwashing: a study in Tibetan primary schools. Int J Environ Res Public Health. (2019) 16:3217. doi: 10.3390/ijerph16173217
57. Solehati, T, Kosasih, CE, Susilawati, S, Lukman, M, and Paryati, SPY. Effect of school community empowerment model towards handwashing implementation among elementary school students in Dayeuhkolot subdistrict. Kesmas Natl Public Health J. (2017) 11:111–116. doi: 10.21109/kesmas.v11i3.1171
58. Ramos, MM, Schrader, R, Trujillo, R, Blea, M, and Greenberg, C. School nurse inspections improve handwashing supplies. J Sch Health. (2011) 81:355–8. doi: 10.1111/j.1746-1561.2011.00602.x
59. Kim, EJ, Pai, AJ, Kang, N, Kim, WK, Kim, YS, Moon, H, et al. The effects of food safety education on adolescents' hand hygiene behavior: an analysis of stages of change. Nutr Res Pract. (2012) 6:169. doi: 10.4162/nrp.2012.6.2.169
60. Bandura, A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. (2001) 52:1–26. doi: 10.1146/annurev.psych.52.1.1
61. Fatajo, E, and Barrow, M. Water, sanitation, and hygiene policies and the enhancement of quality education in lower and upper basic schools within region one education directorate, the Gambia. AKSU Journal of Administration and Corporate Governance. (2023) 3:14–25. doi: 10.61090/aksujacog.2023.002
Keywords: handwashing, hygiene, students, COVID-19, behavior
Citation: Bolatova Z, Kalishev M, Nukeshtayeva K, Zhamantayev O, Dauletkaliyeva Z, Kayupova G, Yerdessov N and Orru H (2025) Factors influencing hygienic behavior among students in Central Kazakhstan during COVID-19. Front. Public Health. 13:1593579. doi: 10.3389/fpubh.2025.1593579
Edited by:
Antonio Sarría-Santamera, Nazarbayev University, KazakhstanReviewed by:
Kamel A. K. Jebreen, UMR8120 Génétique Quantitative et Evolution Le Moulon, FranceBalnur Omarova, Ahmet Yesevi University, Kazakhstan
Copyright © 2025 Bolatova, Kalishev, Nukeshtayeva, Zhamantayev, Dauletkaliyeva, Kayupova, Yerdessov and Orru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhanerke Bolatova, Ym9sYXRvdmF6aGFuZXJrZTkzQGdtYWlsLmNvbQ==; Marat Kalishev, S2FsaXNoZXZAcW11Lmt6
 Zhanerke Bolatova
Zhanerke Bolatova Marat Kalishev1*
Marat Kalishev1* Karina Nukeshtayeva
Karina Nukeshtayeva Olzhas Zhamantayev
Olzhas Zhamantayev Gaukhar Kayupova
Gaukhar Kayupova Hans Orru
Hans Orru