- 1Department of Comprehensive Dentistry, San Antonio Refugee Health Clinic, School of Dentistry, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 2Department of Emergency Medicine, University of Virginia, Charlottesville, VA, United States
- 3School of Dentistry, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 4Joe R. & Teresa Lozano Long School of Medicine, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 5South Central AHEC (Area Health Education Center), University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 6Department of Family & Community Medicine, Joe R. & Teresa Lozano Long School of Medicine, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 7Department of Pediatrics, Joe R. & Teresa Lozano Long School of Medicine, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
- 8Office for Faculty Excellence, School of Nursing, University of Texas Health Science Center at San Antonio, San Antonio, TX, United States
Introduction: Ongoing socio-political instability has resulted in a growing influx of Afghan women with limited literacy skills resettling in the United States (U.S.). These women face considerable barriers in accessing oral and general healthcare services, exacerbated by limited literacy. This study aimed to explore Afghan women’s challenges in accessing healthcare services and develop a technology-enabled intervention to enhance their health.
Methods: An interprofessional (IP) team of researchers collaborated with community advocates and leaders to gather participants’ insights about preventive health. Participants identified WhatsApp as their preferred platform for receiving health information. Trained interpreters were employed to bridge cultural and linguistic gaps. The first phase involved conducting pre-intervention surveys to assess participants’ experiences with the availability, accessibility, and affordability of healthcare services. Culturally tailored oral health messages were developed using the interactive Canva platform. These videos incorporated messages in English, Pashto, and Farsi that were shared through WhatsApp, to accommodate varying literacy levels. The second phase emphasized hands-on demonstrations to illustrate oral hygiene techniques, and a customized rubric was used to assess participants’ competency. Pre- and post-surveys for the pilot study assessed changes in knowledge and behavior, which helped refine the intervention protocol. Follow-up interviews were conducted six months post-intervention, assessing variations in outcome.
Results: Forty-three Afghan women aged 19 to 57 participated in the study. Demographic data revealed that 58% identified Pashto as their primary language, 46% had received little to no formal education, and 77% were homemakers. Key barriers to healthcare access included financial constraints (91%), limited English proficiency (70%), low literacy levels (63%), and transportation challenges (56.3%). Post-intervention data revealed statistically significant improvements in participants’ oral hygiene and dietary knowledge (p < 0.05). Assessment of brushing and flossing techniques indicated increased performance scores from pre-to post-intervention (p < 0.001). At the six-month post-intervention follow-up, 20 women participated. 80% (n = 16) reported reduced consumption of sugary beverages, while 95% (n = 19) indicated improved oral hygiene practices.
Conclusion: This study supports the effectiveness of a culturally responsive, technology-facilitated oral health intervention in enhancing self-care behaviors among Afghan refugee women. The findings suggest that healthcare providers should adopt patient-centered, community-engaged approaches to advance health outcomes. Technology-based interventions can effectively address constraints in health literacy.
1 Introduction
Refugees resettling in a new country often encounter numerous stressors, including conflicting cultural norms, unfamiliar religious customs, and disrupted social support systems. These stressors significantly impact their overall health and wellbeing, including their oral health, as they navigate complex healthcare systems while facing financial, linguistic, and systemic barriers (1). In the United States (U.S.), despite existing resettlement support services (2), refugees face environmental challenges such as unfamiliar healthcare practices, dietary adjustments, sociocultural misunderstandings, and limited health literacy. These factors hinder self-care, restrict access to dental services, and contribute to inadequate oral hygiene practices (3, 4).
Such barriers are particularly relevant for the over 100,000 Afghans who have resettled in the U.S., many of whom have endured significant physical and emotional trauma during their displacement (5, 6). Between 2010 and 2022, the Afghan immigrant population in the U.S. nearly quadrupled, from approximately 54,000 to 195,000. In 2021 alone, 76,000 evacuated Afghans received humanitarian parole status to enter the United States (6).
Afghan cultural norms are deeply rooted in religious practices, which in turn shape daily oral hygiene practices (7). One such normalized practice is using chewing sticks as a traditional toothbrushing technique. The sticks are chewed on one end to create a frayed, brush-like tip used to clean teeth, while flossing is less familiar (7, 8).
Offering culturally sensitive oral health education and information about the U.S. healthcare system requires a comprehensive approach that addresses transportation, financial, and language barriers (9). Healthcare providers face unique challenges when treating patients from other cultures (10). Prioritizing oral health as a core, integral component of wellbeing and actively empowering marginalized groups, especially women, directly aligns with the United Nations’ Sustainable Development Goals of SDG 3 (good health and wellbeing), 5 (equality), and 10 (reduced inequalities) (11).
While previous studies have examined oral health disparities among refugees (12), few have implemented or evaluated culturally tailored and technology-driven interventions designed explicitly for Afghan women with limited literacy and English proficiency.
Emerging evidence supports the use of informed health advisors to enhance oral health knowledge and attitudes among Culturally and Linguistically Diverse (CLD) communities, effectively bridging communication gaps (13). However, educational outreach to Afghan women is hindered by low literacy levels and limited formal education (14, 15).
Health literacy refers to an individual’s ability to access, understand, evaluate, and apply health information to make informed decisions about their health (16). Strong health literacy skills are closely linked to better health outcomes, while limited health literacy is associated with poor health outcomes, higher healthcare costs, and greater health disparities (17). Similarly, digital literacy is the ability to locate, assess, and effectively communicate information using digital technologies (18). Emerging research highlights the critical role that digital communication tools play in enhancing health literacy, ultimately empowering individuals to take a more active and informed role in managing their health (19).
Digital communication tools, such as WhatsApp Messenger, present promising opportunities for delivering health outreach by facilitating rapid, multimodal communication through text messages, images, and video calls. Such platforms can enhance patients’ comprehension of general and oral health concepts; hence, improving clinical outcomes (20, 21). Technology-based interventions such as YouTube and other social media platforms have proven effective in delivering health education, raising awareness, and encouraging positive health behavior change (22, 23). This study sought to identify the factors that enhance Afghan women’s access to oral healthcare services and to promote improvements in their oral health literacy and practices.
2 Materials and methods
2.1 Intervention design and development
This quasi-experimental intervention utilized digital technology platforms and community engagement to address oral health disparities among Afghan women. Digital content was crafted with a focus on preventive empowerment self-care (21–23), emphasizing three critical components: comprehensibility (cognitive), manageability (behavioral), and meaningfulness (motivational). These pillars align with the framework proposed by Eriksson et al. (24), ensuring that the intervention addresses the multidimensional process of health knowledge acquisition and behavior change.
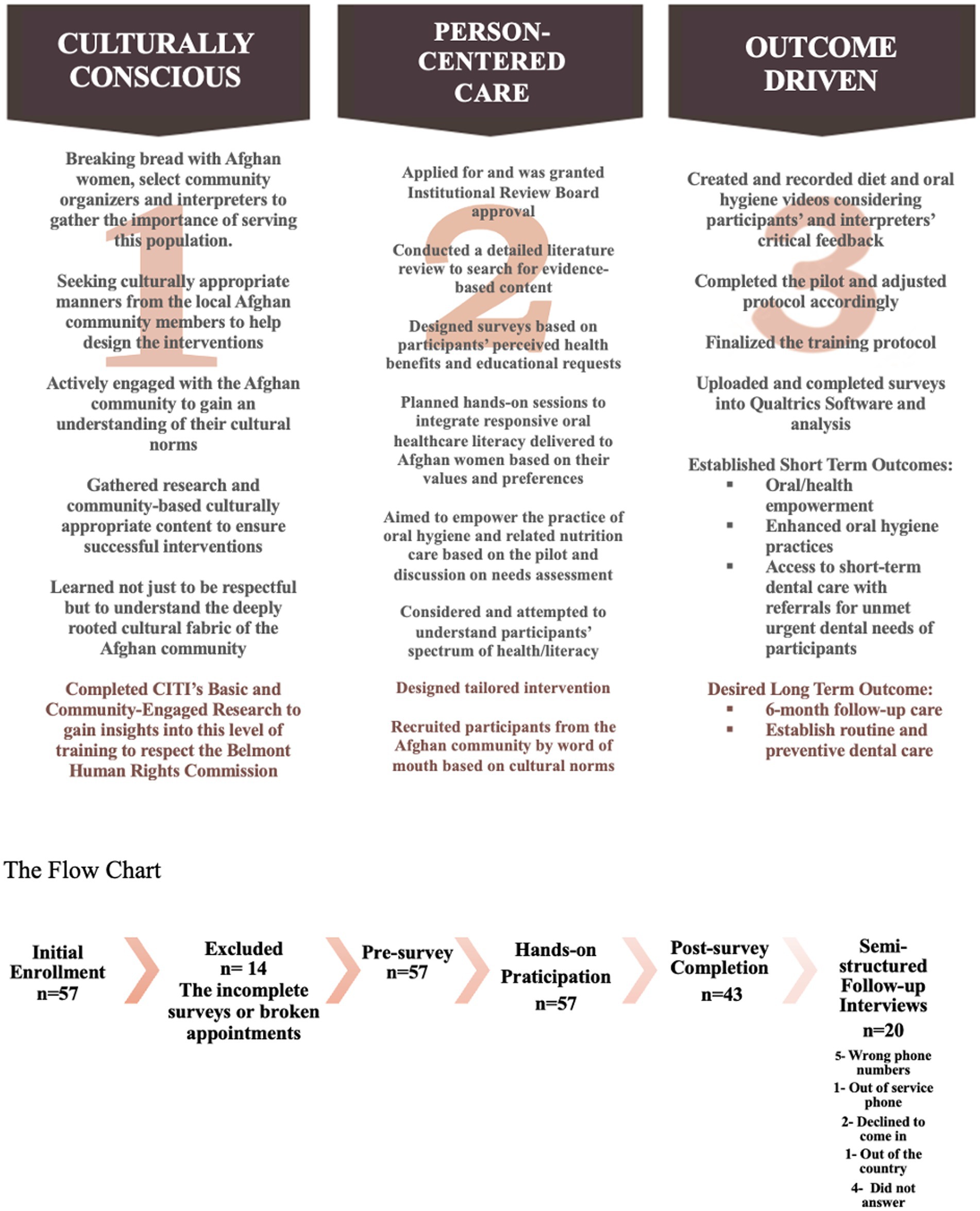
Motivational interviewing style interventions were developed in collaboration with the local Afghan community leaders. Afghan women guided the research questions and evaluation metrics during “breaking bread” lunches that promoted relationship-building and trust (Figure 1). Community events, including English as a Second Language (ESL) classes and oral health roundtables, provided opportunities for socialization and needs assessment. The study was pilot tested at such gatherings to refine the research design and uncover potential problems with the intervention protocol, the study procedure, or data collection through participant feedback.
Community events, including English as a Second Language (ESL) classes and oral health roundtables, provided opportunities for socialization and needs assessment. To minimize interpretation confusion, a simplified Likert scale with two response options (agree/disagree) addressed literacy and education limitations.
2.2 Participant recruitment and interventional design
Participants were recruited at our Refugee Health Clinic (Clinic, 9), which has provided services in the local community for over a decade. Inclusion criteria were adult Afghan women. This interventional study enrolled a convenience sample of 43 Afghan women (Figure 1) seeking urgent oral healthcare at the Clinic. During the study phase, 346 Afghan resettled women attended the Clinic, and 57 elected to participate.
Each participant received one-on-one training focused on oral hygiene instructions, and nutrition. IP providers applied a kinesthetic learning approach using tooth models or typodonts to demonstrate proper oral hygiene instructions. They also played two Canva videos in English, Pashto, and Farsi with narrations in Pashto and Farsi to reinforce the connections between general and oral health and diet as related to toothbrushing and adequate flossing.
• Video 1 demonstrated proper brushing and flossing techniques.
• Video 2 covered nutritional health: food group portion sizes, fresh versus processed foods, meal timing, and diet tips for cavity prevention.
The videos were used as training tools during the session and disseminated as WhatsApp links for take-away messages.
Using a rubric-based evaluation, calibrated providers, including the dental faculty, dental students, and medical students, assessed participants’ tactical oral hygiene skills immediately after the hands-on training (Appendix A) (25). The 3-point scale measured the amount of toothpaste, brush bristle stiffness, brushing time, and technique, coverage of tooth surfaces, and flossing techniques. The author developed Rubric Form (Appendix A), assessed, evaluated, and tracked participants’ progress with their oral hygiene skills.
2.3 Measurement and instruments
Calibrated interpreters facilitated the administration of the surveys for participants with limited English proficiency and literacy limitations.
2.3.1 Pre-intervention measures
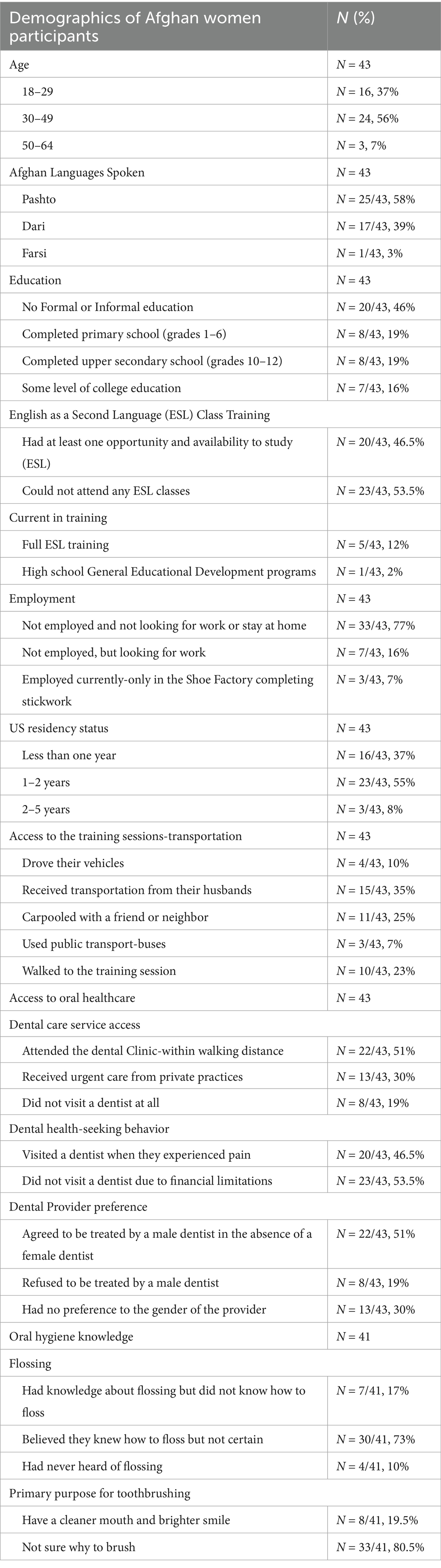
After providing informed consent, the participants completed pre-intervention surveys, including validated tools (26–28) to assess the quality of life, oral health perceptions, and access to care. The World Health Organization (WHO) WHOQOL-BREF measured the domains such as physical health, environmental context, and perceived wellbeing (26). Survey questions, co-developed with interpreters and community organizers, also evaluated culturally informed practices and baseline knowledge of oral and nutritional health (Tables 1, 2) (29–31). The pre-survey, consisting of 27 questions, focused on sociodemographics, education, and employment status (Table 1), access to oral healthcare (4), oral health and hygiene (10), nutritional health (11, Table 2), healthcare availability (5), accessibility (6), and affordability (2, Table 3). It also examined participants’ barriers to both oral and general health (3), Figure 2).
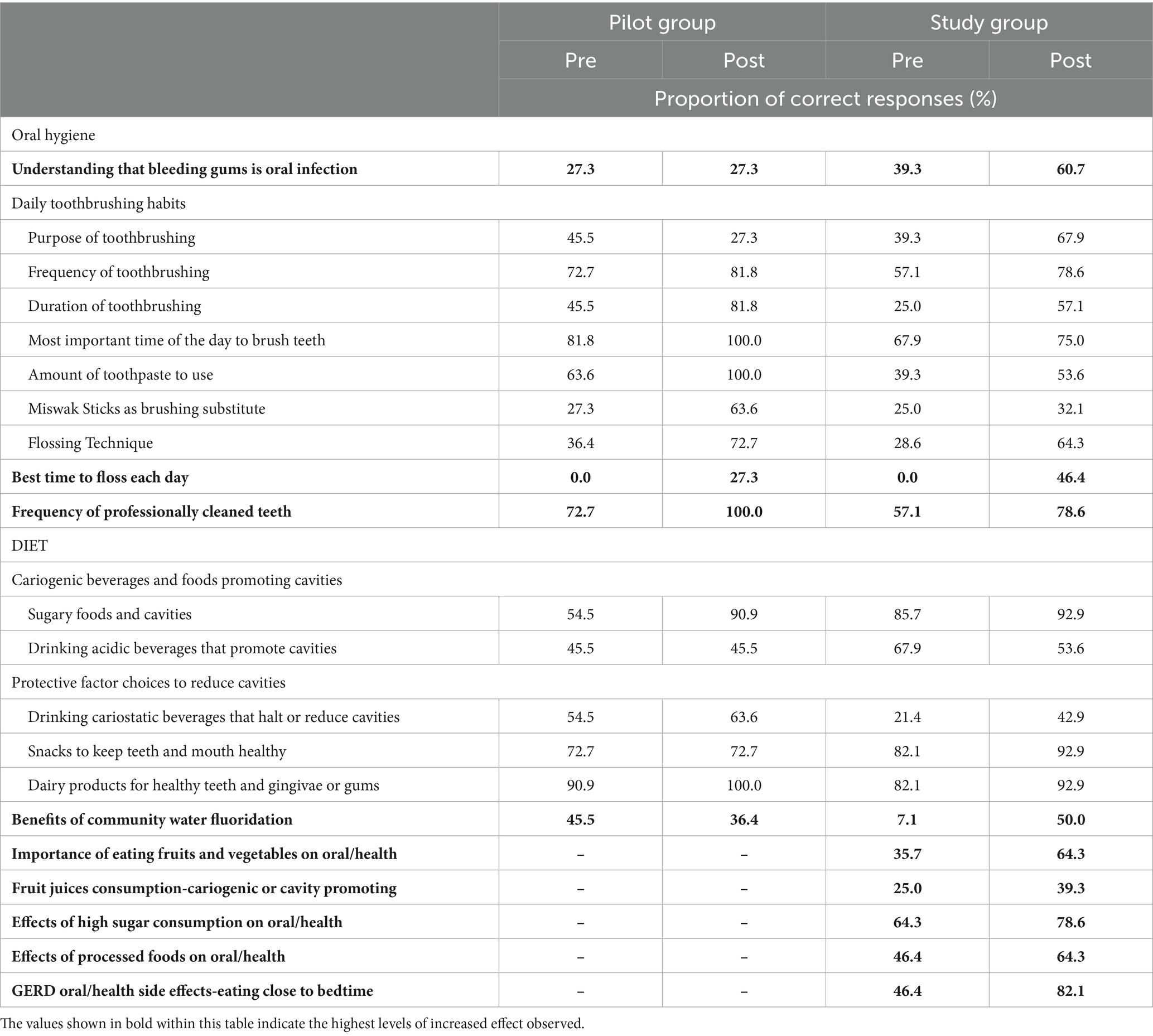
Table 2. Proportion of correct responses for the oral and health related assessment of knowledge among participants in the Pilot (n = 11) and Study (n = 32) groups Pre and Post the intervention.
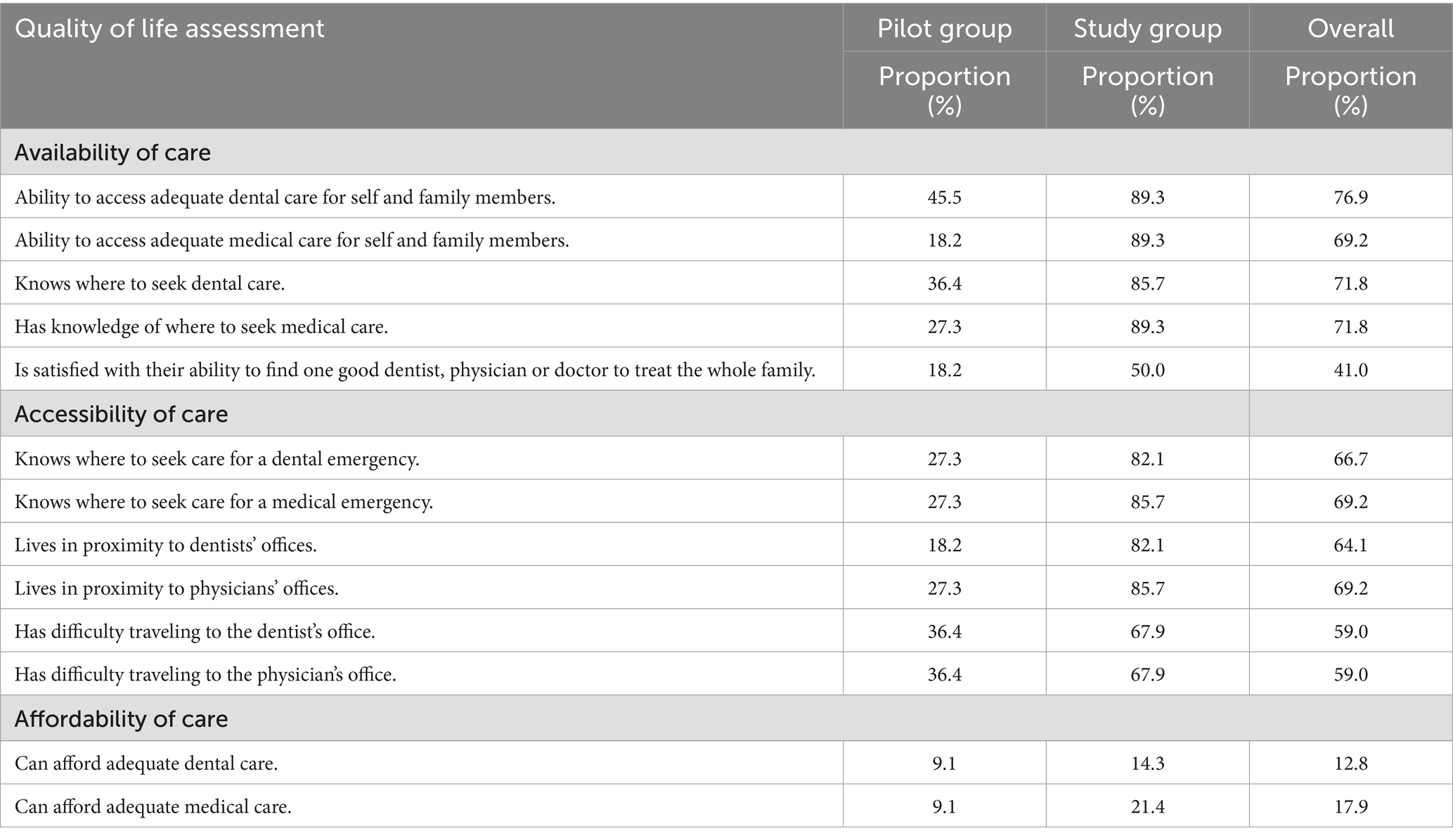
Table 3. Proportion of responses to the quality of life assessment questions by Pilot group (n = 11) and Study group (n = 32).
2.3.2 Post-intervention measures
The post-intervention survey, excluding sociodemographic questions (Tables 1, 2), was administered immediately after the intervention training. The post-survey assessed changes in knowledge and behavior using the same simplified Likert format.
Six months post-intervention, semi-structured interviews were conducted for 20 of the participants. Interviews explored participants’ (1) the capacity of the intervention outcomes, (2) the relative benefit/s of the intervention (28), and (3) the ability to be self-reliant (32).
2.4 Data management and analysis
The IP providers and interpreters recorded survey responses directly into a password-protected Qualtrics system. Responses were de-identified to ensure confidentiality. Descriptive statistics were used to summarize (1) quality of life, (2) oral health knowledge, and (3) healthcare access barriers. The pre-and post-interventional surveys were administered digitally using password-protected Qualtrics links. Wilcoxon matched-pairs signed-rank tests compared pre-and post-survey results. Analyses were performed using Stata 18.0 (StataCorp LLC, College Station, TX). Informed consent was obtained verbally and in writing at each session, as IRB approval of HSC-20230224NRR.
3 Results
3.1 Access to oral healthcare services
3.1.1 Participant demographics and barriers to accessing oral healthcare
The sociodemographic information of the participants is reported in Table 1. A total of 43 Afghan women participated in the intervention. Generally, participants were Afghan women ranging in age from 19–57 years old who mostly spoke Pashto (58%), presented with established U.S. residency status of 1–2 years (55%), had limited formal education (46%), and were not employed and not looking for work (77%). Few participants (23%) reported working outside the home as teachers, school principals, physicians, medical assistants, midwives, or tailors when they lived in Afghanistan. Transportation to training sessions emerged as a significant barrier, with participants relying on husbands or friends for carpooling.
Participants’ barriers to accessing oral healthcare (Table 1; Figure 2) ranked by the participants included cost (91%), limited English proficiency (70%), low oral health literacy (63%), transportation challenges (56.3%), and childcare responsibilities (50%).
3.1.2 Dental care utilization and treatment-seeking behavior
Access, as the lack of dental care, was a primary study objective. The majority (51%) of participants attended the Clinic’s urgent dental care services because of of walking or availability to access, 46.5% visited a dentist only when they experienced pain in an emergency, and the majority (70%) preferred female dental providers (Table 1).
The in-depth interviews revealed that the participants’ husbands play a significant role in their healthcare experiences, highlighting their influence on decisions and support system. Additionally, the study uncovered critical insights into the healthcare behaviors of Afghan refugee women, whose oral hygiene practices were often deprioritized due to overwhelming household responsibilities, particularly extensive childcare duties.
3.1.3 Healthcare availability, accessibility, and affordability trends
The availability, accessibility, and affordability of healthcare evaluations based on the Quality of Life Assessment are reported in Table 3. Overall, participants reported moderate availability of resources such as personnel and technology to address their oral health needs, and moderate accessibility in receiving timely and appropriate healthcare services to achieve optimal health outcomes. However, only 41% were satisfied with their ability to find a single provider to treat the whole family, and 59% reported having difficulty traveling to both a dentist’s and a physician’s office. The participant level of affordability of healthcare services was also low, with 12.8% reporting they could not afford dental care and 17.9% reporting they could not afford medical care. Comparing dental and medical groups, the Study group reported more availability and access to dental and medical care. However, dental and medical affordability of healthcare services was low for both the Pilot and Study groups (dental: 9.1 and 14.3%, respectively; medical: 9.1 and 21.4%, respectively).
3.2 Oral health literacy
3.2.1 Oral hygiene practices and knowledge gained
Participant knowledge improved notably from pre-to post-survey in several areas, including (1) understanding of gingivitis, proper brushing and flossing techniques, and the benefits of fluoride, and (2) recognition of Miswak stick usage as a traditional oral hygiene tool.
A tremendous increase in knowledge was in identifying the best time to floss daily, rising from 0 to 46% in the Study group to 0 to 3% in the Pilot group (Table 2).
Oral hygiene practices and diet knowledge were assessed using a survey administered before and after the intervention and scored based on the number of correct responses (Table 2). In both the Pilot and Study groups, increases in the proportion of correct responses were observed for several knowledge questions. For the Pilot group, the largest increases in the proportion of correct responses were seen in the amount of toothpaste to use (63.6 to 100%), sugary foods as cavity promoting agents (54.5 to 90.9%), the recommended duration of toothbrushing (45.5 to 81.8%), and the benefits of flossing teeth (36.4 to 72.7%). The data indicates a notable decline in knowledge scores about health-related practices, specifically toothbrushing, which decreased from 45.5 to 27.3%. Additionally, awareness of the benefits of community water fluoridation also experienced a reduction, dropping from 45.5 to 36.4%. These findings highlight the difficulties related to effectively communicating intricate health information. For the Study group, the highest increases in the proportion of correct responses were observed for daily flossing (0 to 46.4%), benefits of community water fluoridation (7.1 to 50.0%), and flossing technique (28.6 to 64.3%). Pre-intervention surveys revealed that 80.5% of participants were unaware of the primary purpose of toothbrushing (Table 2).
3.2.2 Dietary knowledge
For the Study group, the highest increases in the proportion of correct responses about diet were observed for the Gastroesophageal Reflux Disease (GERD) condition (GERD) and oral/health side effects from eating close to bedtime (46.4 to 82.1%). The knowledge score decreased for the question about drinking acidic beverages and cavities, likely due to participants’ positive perceptions of drinking juices’ health benefits. Post-intervention dietary knowledge significantly improved as participants’ understanding of the importance of fruit and vegetable intake increased from 9.4 to 43.8%, a 34.4% increase. The Knowledge about fluoride benefits improved from 18.8 to 50%, a 32% increase. The median knowledge scores increased significantly for the Study group (9 to 14) and the Pilot group (9 to 11).
Both pre-and post-surveys were scored for each participant to evaluate the intervention’s effectiveness. A Wilcoxon matched-pairs signed-rank statistical test was performed and reported in Table 4. For the Pilot group, a significant increase in median oral hygiene knowledge and overall knowledge was observed (p = 0.01 and p < 0.01, respectively). For the Study group, median knowledge scores for oral hygiene (p < 0.01), diet (p < 0.01), and overall (p < 0.01) significantly increased after the intervention.
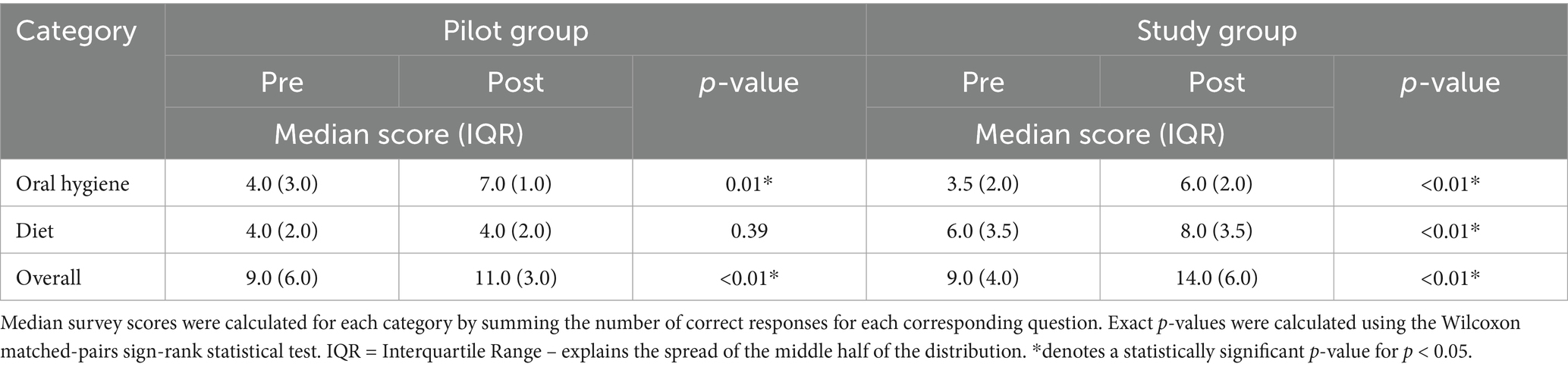
Table 4. Comparison of pre-and post-intervention median knowledge assessment scores among participants in the Pilot (n = 11) and Study (n = 32) groups.
3.3 Six month follow-up to assess oral health behavior
Of the 43 participants, 20 completed the follow-up interviews six months post-intervention. Of the 20, 80% (n = 16) reported occasional sugary drink consumption, while 20% (n = 4) reported none, 75% (n = 15) consumed sugary foods occasionally, and 25% (n = 5) abstained entirely. 85% (n = 17) brushed at least once daily, and 40% (n = 8) flossed at least once daily. 80% (n = 16) used fluoridated toothpaste once or more per day, and 65% (n = 13) had visited a dentist since the intervention; 35% (n = 7) had not. During the follow-up process, participants identified their remaining dental needs, which included pain (n = 4), restorations or fillings (n = 5), and professional tooth cleanings (n = 3).
4 Discussion
This community-engaged, person-centered intervention illuminated the barriers Afghan refugee women face in accessing and utilizing oral and general healthcare services in the United States. The key challenges identified include conflicting cultural norms, transportation barriers, limited proficiency in the dominant language, low health literacy, and financial constraints, which impacted the participants’ ability to access and understand healthcare services (9, 33–35).
4.1 Cultural norms and language access
This study highlighted that, despite participants’ high perceived access to oral health care, many encountered financial barriers that impeded their ability to afford such care. These findings imply that the cost of dental services plays a critical role in shaping participants’ health-related behaviors and care-seeking patterns among individuals. Limited language proficiency emerged as a significant factor impacting participants’ integration and perception of overall wellbeing. Participants faced challenges navigating the U.S. healthcare system due to unfamiliarity with its structure, services, and expectations (Table 3) (36). These barriers frequently led to delayed treatment-seeking, with care sought only when the pain became intolerable—a trend consistent with oral health behavior observed in other refugee communities (5, 10).
4.2 Person-centered and culturally responsive strategies
The novelty of this interventional study was its intentional alignment with participants’ religious, cultural, and logistical realities. Given most participants’ substantial homemaking responsibilities, training and interviewing sessions were deliberately scheduled outside prayer and meal preparation periods. Mothers were permitted to bring children to training sessions, reducing participants’ childcare barriers, as providers helped connect participants to local clinics and establish a “dental or medical home,” for them.”
Childcare burdens significantly impacted participants’ ability to attend appointments and complete surveys, echoing a common theme across low-income and refugee populations (37, 38). This insight reinforces the necessity of integrating childcare support and flexible scheduling into health interventions and the interconnectedness of factors that impact vulnerable populations. Participants also reported relying on informal networks of friends, neighbors, or family for childcare services during health visits (38). The main reason 23 women could not complete their longitudinal six-month follow-up care was childcare restrictions.
4.3 Family dynamics and decision-making
Afghan men traditionally hold financial and logistical responsibilities for their families and are often consulted regarding healthcare decisions. While this dynamic may initially appear at odds with Western ideals of autonomy, many participants described their husbands as supportive allies rather than authoritative decision-makers. This notion emphasizes that providers should avoid cultural assumptions and recognize context-specific gender dynamics (39, 40) when treating such population. For these reasons, the videos included English text so the husbands and English-speaking participants could be fully informed.
Moreover, significant literacy and language gaps amplified participants’ reliance on their husbands’ opinions. Hence, traditional gender dynamics should be considered, particularly how these roles could inhibit access to care. Providers adapted by ensuring that the content delivery was interpreter-assisted, delivered in Pashto and Farsi, and accessible via the WhatsApp platform suggested by the participants.
4.4 Oral health promotion and practice model
This study considered the traditional Afghan oral hygiene habits with Islamic practices like mouth rinsing during ablution, while incorporating science-backed preventive measures of fluoride toothpaste. Educational materials provided instruction on brushing, flossing, diet, and fluoride use, aligning with WHO recommendations of Basic Package of Oral Care, which promotes Affordable Fluoride Toothpaste (AFT), and indicating it’s significant reduction in the incidence of dental caries and periodontal disease (41).
4.5 Empowerment through interpretation
A notable success of this study was its use of trained community organizers and interpreters, many of whom had prior experience serving as cultural mediators in Afghanistan while working with the U.S. Troops. Their contributions were invaluable in both content delivery and trust-building. By incorporating participant voices into the message design, the intervention reduced cultural miscommunication and enhanced the relevance and uptake of oral health messages (42).
5 Implications
The structural burdens contributed to poor self-care routines and underutilization of preventive dental services. One of the most significant findings was the participants’ strong preference for receiving health education content via WhatsApp to be viewed again within the comfort of their home environments.
The successful use of multimedia content delivered through mobile platforms highlights the need for healthcare providers to invest in accessible and culturally appropriate educational tools. Such tools reflect the social contexts and support oral and nutritional health promotion beyond clinical settings that bridge the digital divide and circumvent the social isolation often experienced by refugee women while fostering engagement and autonomy.
Through relationship-building efforts with interpreters, community organizers, and participants, the providers created efforts extending well beyond health education, such as trust, empowerment, and long-term health advocacy.
Aligned with the World Health Organization’s Basic Package of Oral Care and the United Nations Sustainable Development Goals as SDGs 3, 5, and 10 (11), this interventional study design contributed to a broader global agenda of improving and promoting health. Notably, during the urgent care dental exam and triage phase, dental conditions observed by the provider dentist included fractured teeth, the reported frequent consumption of cariogenic foods, and lack of preventive care. Psychosocial stressors, often overlooked, emerged as hidden but powerful drivers of health behaviors. Such stressors, compounded by emotional and environmental distress, can lead individuals to feel a loss of self-identity and disconnection from traditional values (43).
The model of care used in this study highlights the value of community engagement as a mechanism for sustainable change. Technology becomes more than a communication tool; it becomes a dignified communication bridge to health promotion, integration, and content sharing. Despite challenges related to literacy and access to preventive care, routine follow-up metrics, such as health outcomes, could offer a more comprehensive evaluation.
Initially focused on increasing oral healthcare and preventive care outreach, the IP team recognized a deeper opportunity to transform this intervention into an empowerment strategy. As the process evolved, the strategy shifted to a community-engaged advocacy approach, with tools, knowledge, and a platform to reclaim participant agency over their oral and overall health.
6 Lessons learned and limitations
This intervention offered valuable insights into Afghan refugee women’s oral health needs and lived experiences by utilizing motivational interviewing and patient-provider cultural humility encounters while promoting oral and general health. Language and literacy barriers were addressed through tailored communication tools or visual aids. The intervention also enhanced the providers’ depth of cultural humility training and engagement.
A key lesson learned was the critical role of creative, culturally appropriate resources in helping refugee women adapt to unfamiliar healthcare systems and social environments. Many participants reported feeling isolated and overwhelmed when navigating complex health systems while managing extensive domestic and childcare responsibilities. These experiences are consistent with broader refugee literature that identifies structural exclusion and social disconnection as significant challenges for resettled populations (44, 45).
The lack of childcare support during interviews frequently led to overcrowded and occasionally chaotic environments, which could impact participants’ ability to focus. However, this challenge also produced unexpected positive outcomes: older children who observed the interviews became informal learners, absorbing health information alongside their mothers. This intergenerational exposure represents a subtle, indirect benefit, signaling the potential for family-centered health promotion approaches.
While the findings identify barriers for this population in a specific U.S. resettlement context, their applicability to other refugee communities or geographic areas should be cautiously approached.
Despite the relatively small size (n = 43) and the application of a convenience sample, depth of engagement and a comprehensive approach enhanced the outcome impact—one-on-one interviews allowed for a personalized and respectful data collection process. Hence, reliance on scripted and calibrated interpreters was the only alternative, it may present as response bias. While the study focuses on Afghan refugee women, it may not fully account for the experiences of other refugee groups facing similar barriers. Nonetheless, it could be adapted for populations with literacy challenges. Finally, to achieve equitable and effective implementation, careful consideration of accessibility, digital literacy, and data privacy is essential.
7 Conclusion
This community-driven interventional study highlighted the powerful intersection of grassroots outreach and digital engagement in reaching underserved populations. By leveraging existing networks, partnering with local organizations, and utilizing accessible platforms such as WhatsApp, the initiative effectively disseminated multimedia health content. This model of care outlined the impact of collective community-engaged action in promoting health and improving the wellbeing of resettled communities; however, ongoing education and support mechanisms are essential for long-term success.
This humanistic and upstream interventional model of care not only met immediate health needs but also initiated critical, broader conversations about integrating oral and general health services within vulnerable communities. The interventional study presented a scalable model suitable for displaced or linguistically challenged populations.; however, addressing the language, childcare, and cultural barriers encountered before implementation is critical.
Technology platforms, such as digital health tools and virtual consultation deliverables for refugees and other marginalized populations, can overcome structural barriers to healthcare, leading to improved oral and general health outcomes and potentially addressing language barriers, and geographical limitations (46).
Ultimately, by fostering a multi-agency interprofessional collaboration for this (46) interventional study this interventional study reinforces that empowering refugee women through education, engagement, and person-centered strategies can serve as a blueprint for responsive, inclusive healthcare that honors the dignity and resilience of displaced communities.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by UTHSA Institutional Review Board-HSC 20230224NRR. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their verbal and written informed consent to participate in this study.
Author contributions
MF: Visualization, Project administration, Validation, Resources, Writing – review & editing, Methodology, Supervision, Writing – original draft, Investigation, Conceptualization. AM: Validation, Writing – review & editing, Investigation, Resources, Methodology, Writing – original draft, Funding acquisition. HN: Methodology, Writing – review & editing, Supervision, Investigation, Data curation, Project administration, Validation. JY: Methodology, Supervision, Investigation, Data curation, Project administration, Conceptualization, Resources, Writing – review & editing. AE: Formal analysis, Methodology, Writing – review & editing, Software, Resources. RS: Resources, Project administration, Validation, Investigation, Writing – review & editing, Supervision. MS: Methodology, Formal analysis, Investigation, Funding acquisition, Project administration, Writing – review & editing. NM: Writing – review & editing, Funding acquisition, Resources, Project administration, Supervision, Validation. HW: Validation, Writing – review & editing, Supervision, Writing – original draft, Resources, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Morris, MD, Popper, ST, Rodwell, TC, Brodine, SK, and Brouwer, KC. Healthcare barriers of refugees post-resettlement. J Community Health. (2009) 34:529–38. doi: 10.1007/s10900-009-9175-3
2. U.S. Department of Health and Human Services, Office of Refugee Resettlement. Accessed March 12, 2025. Available online at: https://www.acf.hhs.gov/orr/about-refugee-program
3. Mangrio, E, and Sjögren Forss, K. Refugees' experiences of healthcare in the host country: a scoping review. BMC Health Serv Res. (2017) 17:814. doi: 10.1186/s12913-017-2731-0
4. Geltman, PL, Hunter Adams, J, Penrose, KL, Cochran, J, Rybin, D, Doros, G, et al. Health literacy, acculturation, and the use of preventive oral health care by Somali refugees living in Massachusetts. J Immigr Minor Health. (2014) 16:622–30. doi: 10.1007/s10903-013-9846-0
5. Asfari, E, Rodriguez, A, Dakessian, A, and Yuan, S. Exploring refugees' experience of accessing dental health services in host countries: a scoping review. Front Oral Health. (2024) 5:1328862. doi: 10.3389/froh.2024.1328862
6. Migration Policy Institute (MPI), Migration Data Hub. U.S. immigrant population by state and county. Accessed March 12, 2025. Available online at: https://www.migrationpolicy.org/article/afghan-immigrants-united-states-2022
7. Thapa, P, Aryal, KK, Mehata, S, Vaidya, A, Jha, BK, Dhimal, M, et al. Oral hygiene practices and their sociodemographic correlates among Nepalese adult: evidence from non communicable diseases risk factors STEPS survey Nepal 2013. BMC Oral Health. (2016) 16:105. doi: 10.1186/s12903-016-0294-9
8. Redzepagić, S. Oral hygiene in the hadiths of the holy prophet Mohammed (S.A.V.S). Med Arh. (1997) 51:35–9.
9. Farokhi, MR, Muck, A, Lozano-Pineda, J, Boone, SL, and Worabo, H. Using Interprofessional education to promote Oral health literacy in a faculty-student collaborative practice. J Dent Educ. (2018) 82:1091–7. doi: 10.21815/JDE.018.110
10. Ponomarenko, M, and Kaifie, A. Oral health, stress and barriers accessing dental health care among war-affected Ukrainian refugees in Germany. BMC Oral Health. (2023) 23:804. doi: 10.1186/s12903-023-03513-x
11. Huang, YK, and Chang, YC. Oral health: the first step to sustainable development goal 3. J Formos Med Assoc. (2022) 121:1348–50. doi: 10.1016/j.jfma.2021.10.018
12. Keboa, MT, Hiles, N, and Macdonald, ME. The oral health of refugees and asylum seekers: a scoping review. Global Health. (2016) 12:59. doi: 10.1186/s12992-016-0200-x
13. Balla, SB, Angelakopoulos, N, Tadakamadla, J, and Tadakamadla, SK. A systematic review and meta-analysis of interventions targeted to parents for improving the oral health of children from culturally and linguistically diverse (CALD) backgrounds. J Immigr Minor Health. (2025) 27:313–28. doi: 10.1007/s10903-024-01650-1
14. Hawkins, MM, Schmitt, ME, Adebayo, CT, Weitzel, J, Olukotun, O, Christensen, AM, et al. Promoting the health of refugee women: a scoping literature review incorporating the social ecological model. Int J Equity Health. (2021) 20:45. doi: 10.1186/s12939-021-01387-5
15. United Nations Educational, Scientific and Cultural Organization (UNESCO). "Let Girls and Women in Afghanistan Learn!" Updated April 20, 2023. Accessed March 12, 2025. Available online at: https://www.unesco.org/en/articles/let-girls-and-women-afghanistan-learn
16. World Health Organization (WHO). Improving health literacy. (2023). Accessed March 12, 2025. Available online at: https://www.who.int/activities/improving-health-literacy
17. Keene Woods, N, Ali, U, Medina, M, Reyes, J, and Chesser, AK. Health literacy, health outcomes and equity: a trend analysis based on a population survey. J Prim Care Community Health. (2023) 14:21501319231156132. doi: 10.1177/21501319231156132
18. Reddy, P, Chaudhary, K, Sharma, B, and Hussein, S. Essaying the design, development and validation processes of a new digital literacy scale. Online Inf Rev. (2023) 47:371–97. doi: 10.1108/OIR-10-2021-0532
19. Clifford, C. My health, my language—multilingual video messages on health in Ireland. Rural Remote Health. (2023) 23:8173. doi: 10.22605/RRH8173
20. Giordano, V, Koch, H, Godoy-Santos, A, Dias Belangero, W, Esteves Santos Pires, R, and Labronici, P. Whats app messenger as an adjunctive tool for telemedicine: an overview. Interact J Med Res. (2017) 6:e11. doi: 10.2196/ijmr.6214
21. Sharma, S, Mohanty, V, Balappanavar, AY, Chahar, P, and Rijhwani, K. Role of digital Media in Promoting Oral Health: a systematic review. Cureus. (2022) 14:e28893. doi: 10.7759/cureus.28893
22. Langford, A, and Loeb, S. Perceived patient-provider communication quality and sociodemographic factors associated with watching health-related videos on you tube: a cross-sectional analysis. J Med Internet Res. (2019) 21:e13512. doi: 10.2196/13512
23. Hassona, Y, Taimeh, D, Marahleh, A, and Scully, C. You tube as a source of information on mouth (oral) cancer. Oral Dis. (2016) 22:202–8. doi: 10.1111/odi.12434
24. Eriksson, M, and Lindström, B. Antonovsky's sense of coherence scale and its relation with quality of life: a systematic review. J Epidemiol Community Health. (2007) 61:938–44. doi: 10.1136/jech.2006.056028
25. Hancock, AB, and Brundage, SB. Formative feedback, rubrics, and assessment of professional competency through a speech-language pathology graduate program. J Allied Health. (2010) 39:110–9.
26. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28:551–8. doi: 10.1017/s0033291798006667
27. Sischo, L, and Broder, HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res (2011). 90:1264-70. doi: 10.1177/0022034511399918
28. Yaghoubi, Z, Khajedaluee, M, and Mohammadi, TM. Introducing a Valid Questionnaire for Assessment of Perceived Oral Health Care Needs, Barriers to Accessing Oral Health Care Services and Its Utility. Int J Dent Oral Health. (2017) 3. doi: 10.16966/2378-7090.239
29. Mahmoodi, Z, Bahrami, G, Ghavidel, N, and Seddighi, H. The effect of social determinants of health on quality of life among afghan refugees in Iran during the COVID-19 pandemic: a path analysis. BMC Psychiatry. (2023) 23:11. doi: 10.1186/s12888-022-04502-0
30. Petersen, PE. Global policy for improvement of oral health in the 21st century--implications to oral health research of world health assembly 2007, World Health Organization. Community Dent Oral Epidemiol. (2009) 37:1–8. doi: 10.1111/j.1600-0528.2008.00448.x
31. Wallace, BB, and Macentee, MI. Access to dental care for low-income adults: perceptions of affordability, availability and acceptability. J Community Health. (2012) 37:32–9. doi: 10.1007/s10900-011-9412-4
32. The United Nations High Commissioner for Refugees, Division of Program Support and Management OSTS. (2011). Promoting livelihoods and self-reliance operational guidance on refugee protection and solutions in urban areas. Geneva, Switzerland, Accessed March 12, 2025. Available online at: https://www.hsph.harvard.edu/wp-content/uploads/sites/134/2017/02/For-Jacobsen-UNHCR-Promoting-self-reliance.pdf
33. Rowe, J, and Paterson, J. Culturally competent communication with refugees. Home Health Care Manag Pract. (2010) 22:334–8. doi: 10.1177/1084822309353152
34. Hill, KG, Woodward, D, Woelfel, T, Hawkins, JD, and Green, S. Planning for long-term follow-up: strategies learned from longitudinal studies. Prev Sci. (2016) 17:806–18. doi: 10.1007/s11121-015-0610-7
35. Handtke, O, Schilgen, B, and Mo¨sko, M. Culturally competent healthcare – a scoping review of strategies implemented in healthcare organizations and a model of culturally competent healthcare provision. PLoS One. (2019) 14:e0219971. doi: 10.1371/journal.pone.0219971
36. The United Nations High Commissioner for Refugees, Integration programmes. Accessed March 12, 2025. Available online at: https://www.unhcr.org/handbooks/ih/
37. Gaur, P, Ganguly, AP, Kuo, M, Martin, R, Alvarez, KS, Bhavan, KP, et al. Childcare needs as a barrier to healthcare among women in a safety-net health system. BMC Public Health. (2024) 24:1608. doi: 10.1186/s12889-024-19125-1
38. Alvarez, KS, Bhavan, K, Mathew, S, Johnson, C, McCarthy, A, Garcia, B, et al. Addressing childcare as a barrier to healthcare access through community partnerships in a large public health system. BMJ Open Qual. (2022) 11:e001964. doi: 10.1136/bmjoq-2022-001964
39. Szaflarski, M, and Bauldry, S. The effects of perceived discrimination on immigrant and refugee physical and mental health. Adv Med Sociol. (2019) 19:173–204. doi: 10.1108/S1057-629020190000019009
40. Moghadam, VM. Patriarchy and the politics of gender in modernising societies: Iran, Pakistan and Afghanistan. Int Sociol. (1992) 7:35–53. doi: 10.1177/026858092007001002
41. Helderman, W, and Benzian, H. Implementation of a basic package of oral care: towards a reorientation of dental NGOs and their volunteers. Int Dent J. (2006) 56:44–8. doi: 10.1111/j.1875-595x.2006.tb00073.x
42. Swihart, DL, Yarrarapu, SNS, and Martin, RL. Cultural religious competence in clinical practice In: StatPearls. Treasure Island (FL): StatPearls Publishing (2023) 2025
43. Alemi, Q, Weller, SC, Montgomery, S, and James, S. Afghan refugee explanatory models of depression: exploring Core cultural beliefs and gender variations. Med Anthropol Q. (2017) 31:177–97. doi: 10.1111/maq.12296
44. Northcote, J, Hancock, P, and Casimiro, S. Breaking the isolation cycle: the experience of Muslim refugee women in Australia. Asian Pac J. (2006) 15:177–99. doi: 10.1177/01171968060150020
45. Dovigo, F. Beyond the vulnerability paradigm: fostering inter-professional and multi-agency cooperation in refugee education in Italy. Int J Incl Educ. (2021) 25:166–81. doi: 10.1080/13603116.2019.1707301
Keywords: cultural practices, health communication, refugee health, health literacy, stakeholder participation
Citation: Farokhi MR, Muck AE, Nathan H, Yan J, Estacio A, Su R, Stone M, Mandlik N and Worabo H (2025) Harnessing technology to enhance oral health literacy among Afghan women: an interprofessional community-engaged initiative. Front. Public Health. 13:1594767. doi: 10.3389/fpubh.2025.1594767
Edited by:
Dhelfeson Willya Douglas-de-Oliveira, Federal University of Jequitinhonha and Mucuri Valleys, BrazilReviewed by:
Ashek Elahi Noor, Atlantic Technological University, IrelandRomana Muller, A.T. Still University—Missouri School of Dentistry and Oral Health, United States
Copyright © 2025 Farokhi, Muck, Nathan, Yan, Estacio, Su, Stone, Mandlik and Worabo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moshtagh R. Farokhi, ZmFyb2toaUB1dGhzY3NhLmVkdQ==
†These authors share first authorship
 Moshtagh R. Farokhi
Moshtagh R. Farokhi Andrew E. Muck
Andrew E. Muck Hamsini Nathan
Hamsini Nathan James Yan
James Yan Alvin Estacio
Alvin Estacio Ruoxuan Su4
Ruoxuan Su4 Heidi Worabo
Heidi Worabo