- 1Emergency and Evidence-Based Medicine Unit, Department of Medicine, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, Brazil
- 2Laboratory of Molecular and Translational Endocrinology, Department of Medicine, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, Brazil
- 3A.C.Camargo Cancer Center, São Paulo, Brazil
Cancer survivorship has become a critical global health issue, with survival rates on the rise in both high-income countries (HICs) and low- and middle-income countries (LMICs). Cancer survivors, encompassing individuals from diagnosis onward, face unique and complex health challenges that necessitate tailored care. In HICs, survival rates have increased due to advances in diagnosis and treatment, prompting robust survivorship programs addressing late effects and long-term quality of life. In LMICs, however, disparities in healthcare access, infrastructure, and support systems hinder comparable progress in survivorship care, particularly outside urban areas. LMIC survivors often contend with financial barriers, limited access to follow-up care, and significant psychosocial and rehabilitative gaps. Specialized survivorship centers are rare, and resources for addressing late effects are constrained, impacting survivors' long-term wellbeing. Emerging studies, primarily from middle-income nations, identify late effects such as endocrine and metabolic disorders, though robust, comprehensive data remain scarce. For childhood cancer survivors, late effects like chronic viral infections and cognitive impairments are documented, yet systematic follow-up remains limited. To bridge these gaps, LMICs require innovative care models, such as non-profit partnerships and community-based interventions, to meet the complex needs of survivors. In Brazil, we've highlighted successful programs including the Mais Médicos program for increased care capacity and DATA-SUS as a model registry. This review synthesizes available literature on cancer survivorship in LMICs, evaluating challenges and successful practices across diverse regions. Addressing these needs is crucial for improving survivorship care, particularly in regions where socioeconomic disparities amplify the challenges of post-cancer recovery.
Introduction
Cancer survivors—those living with cancer from diagnosis onward—represent a growing population (1). A cancer diagnosis marks a turning point in an individual's life, introducing health and social needs that require focused care (2). In high-income countries, 5-year survival rates have reached nearly 50%, thanks to advancements in therapy and early diagnostics, with even higher rates in pediatric and young adult cancers (1).
In low- and middle-income countries (LMICs), cancer survivorship presents additional challenges, such as limited oncologic care, early diagnostics, and effective treatments (3). Survival rates are generally lower in LMICs due to disparities in infrastructure, professional training, and financial barriers (4). Survivors in LMICs also face insufficient support, particularly in follow-up programs, rehabilitation, and psychosocial care—critical components of quality survivorship (5). This review examines cancer survivorship in LMICs, highlighting the challenges and successful strategies that can be adapted to meet local needs. This narrative review was conducted in accordance with the SANRA (Scale for the Assessment of Narrative Review Articles) guidelines, which provide a framework to ensure clarity, justification of the topic, scientific reasoning, appropriate referencing, and relevance to the field (6). Although this study is presented as a narrative review, we adopted a semi-structured and purposeful approach to identify relevant literature. We performed a comprehensive search of peer-reviewed publications across major databases, including PubMed, Scopus, and Web of Science, focusing on literature published between 2000 and 2024. Our search strategy combined terms related to “cancer survivorship,” “low- and middle-income countries,” “late effects,” and “health disparities.” Priority was given to studies that provided empirical data, cohort analyses, or policy insights relevant to LMIC contexts. We also included gray literature, such as reports from international health organizations, to capture region-specific initiatives and challenges not yet represented in indexed literature. We prioritized large cohort studies, global reports, and conceptual analyses relevant to LMICs, ultimately selecting approximately 90 sources based on thematic relevance, geographic diversity, and scientific rigor. This approach enabled us to integrate empirical findings with broader policy and systems-level considerations, in line with accepted principles of narrative synthesis in health sciences. While formal inclusion and exclusion criteria were not rigidly applied, we ensured thematic relevance, geographical diversity, and methodological quality in the selection process. The narrative review format was intentionally chosen to allow flexibility in synthesizing diverse sources and to accommodate the heterogeneity of survivorship models and health systems across LMICs.
While previous reviews have largely centered on survivorship in HICs, this review offers a novel and timely contribution by focusing specifically on LMICs—settings where the cancer burden is rising but survivorship remains a neglected area of study and policy. This review not only highlights gaps in survivorship data and service delivery in LMICs but also proposes strategies to inform future policy and practice.
A brief overview of cancer survivorship
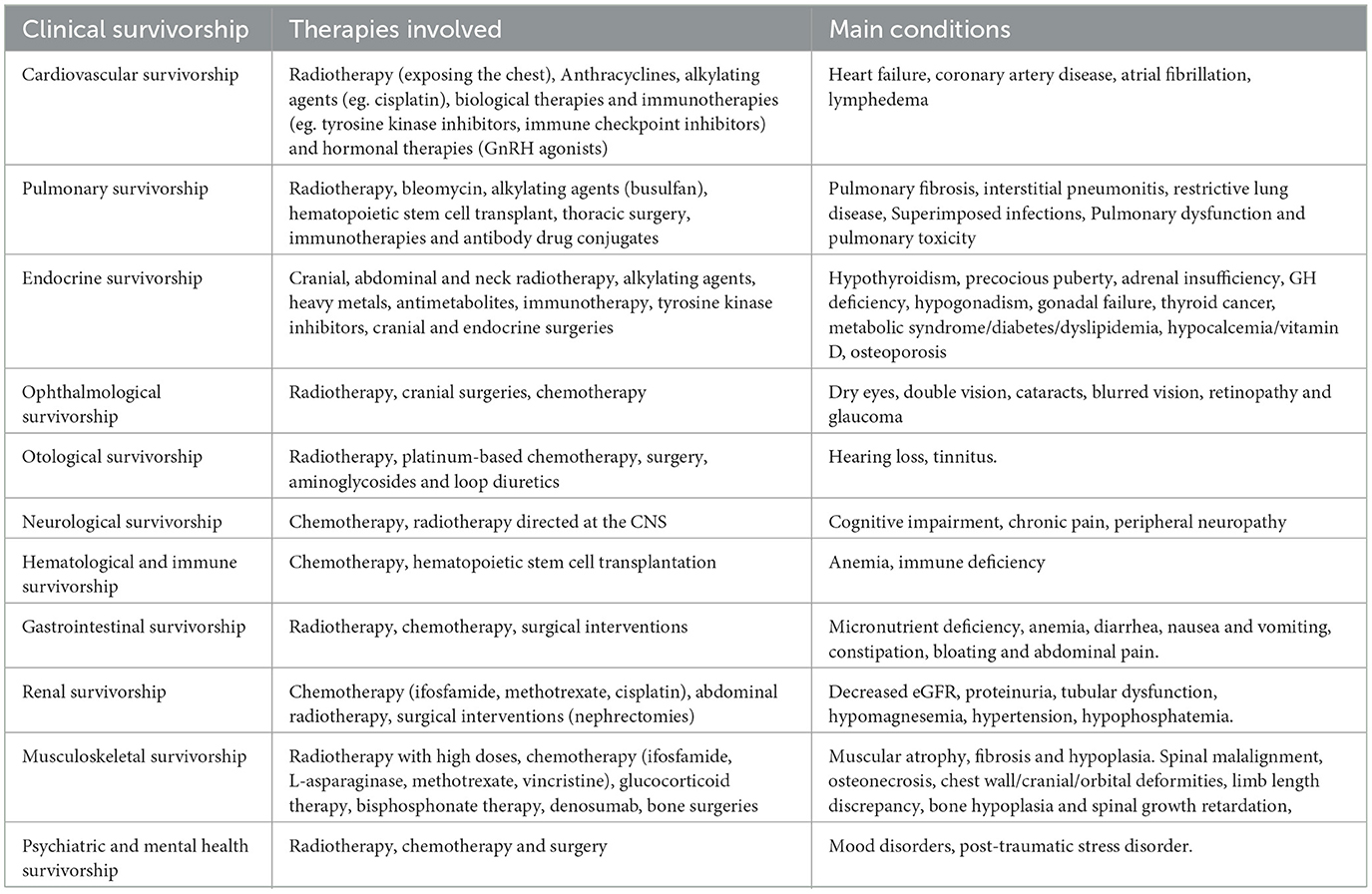
Cancer survivors require more than clinical care. Their needs include social, psychological, and economic support, as they may face stigma, workforce reintegration issues, and barriers to daily activities. Long-term complications, such as cardiovascular disease, metabolic dysfunction, and mental health issues, are often under-addressed. Survivorship challenges are grouped into several categories according to the affected system as can be seen in Table 1.
Cardiovascular survivorship
Survivors are at higher risk for heart failure (HF), coronary artery disease (CAD), and atrial fibrillation (AF). These risks depend on cancer type, treatment, genetics, inflammation, and common risk factors. Specific cancers linked to CAD include esophageal adenocarcinoma, lung cancer, and hematologic cancers (7). Radiotherapy, particularly for Hodgkin's lymphoma and breast cancer, increases CAD and HF risk (8, 9). Pediatric cancer survivors face a 15-fold higher risk of HF than their peers (9). Chemotherapies like anthracyclines and cisplatin contribute to cardiovascular complications, with cumulative anthracycline doses increasing HF risk (10). Lymphedema, especially in breast cancer survivors, can significantly affect quality of life (11).
Respiratory survivorship
Cancer treatments can cause lung damage, leading to symptoms like dyspnea and reduced exercise capacity (12). Post-treatment issues such as pulmonary fibrosis, interstitial pneumonitis, and restrictive lung diseases are common, especially in lung cancer survivors. Radiation to the chest increases risks of lung fibrosis and chronic pneumonia. Chemotherapies like bleomycin and alkylating agents also contribute to lung damage. Hematopoietic stem cell transplantation (HSCT) can cause severe pulmonary complications due to chemotherapy, radiotherapy, and immune reactions.
Endocrine survivorship
Endocrine sequelae from cancer treatments are diverse, including issues with the hypothalamic-pituitary axis, gonads, thyroid, bone density, and obesity. Radiotherapy, especially cranial, can cause growth hormone (GH) deficiency and early puberty. Chemotherapy and radiotherapy are linked to gonadal failure, and HSCT patients often experience hypogonadism, hypothyroidism, and GH deficiency. Treatment with immune checkpoint inhibitors can lead to hypothyroidism and type-1 diabetes (13). Diabetes risk increases, likely due to insulin resistance, obesity, and chemotherapy (14).
Ophthalmological and otological survivorship
Ocular side effects of cancer treatment include dry eyes, double vision, cataracts, and retinopathy. Radiation to areas near the eyes increases the risk of these effects, particularly in CNS cancer and leukemia survivors. Otological side effects, like hearing loss and tinnitus, result from radiation or chemotherapy (15). These conditions can be particularly challenging in children, affecting their language and communication development (16).
Neurological survivorship
Cognitive impairment, including memory and learning difficulties, is common in cancer survivors, particularly those treated with methotrexate or brain radiation (17). Peripheral neuropathy, often linked to chemotherapy, can persist as chronic pain syndrome (18). Chronic pain, a prevalent symptom, is associated with reduced quality of life and should be adequately managed (19).
Hematological and immunological survivorship
Anemia, common in cancer survivors, contributes to fatigue and other symptoms. Chemotherapy affects immune responses, increasing the risk of infections, especially in HSCT recipients (20).
Gastrointestinal survivorship
GI symptoms are frequent in survivors of colon and rectal cancers, often persisting after chemotherapy and radiation. Symptoms such as constipation, diarrhea, and abdominal pain are common but underreported (21). Chemotherapy disrupts gut microbiota, leading to inflammation and symptoms that affect psychosocial health. Upper GI cancer patients often suffer from altered gastrointestinal function, compromising their nutritional status (22).
Renal survivorship
Chronic kidney disease is common among cancer survivors, especially those who underwent abdominal radiation or chemotherapy (23). Nephrectomy patients also need long-term monitoring for kidney function (24).
Musculoskeletal survivorship
Radiotherapy causes long-term musculoskeletal effects, including muscular atrophy, bone malformations, and growth retardation. Chemotherapies like methotrexate and vincristine, combined with radiation, exacerbate these issues (25). Osteonecrosis can also develop, particularly in older patients or those receiving glucocorticoid therapy post-HSCT (26).
Psychiatric and mental health survivorship
Cancer survivors experience higher rates of mood and anxiety disorders. Depression and anxiety are prevalent in both pediatric and adult survivors, with children facing an increased risk of post-traumatic stress disorder (27). Female sex and older age are associated with worse mental health outcomes.
Social and economic impacts of cancer survivorship
Cancer survivors often face unemployment, with those diagnosed with childhood cancer being particularly affected (28). Cancer treatments can impair work productivity and reduce income (29). Social isolation is also a significant issue, negatively impacting psychological wellbeing, particularly in pediatric survivors (30, 31).
Overview of cancer in LMICs
Cancer has become an increasingly significant public health issue not only in high-income countries (HICs) but also in low- and middle-income countries (LMICs). Figure 1 shows the regional distribution of cancer types based on income levels. Countries with high Human Development Index (HDI) such as North America and Western Europe have higher cancer incidence rates, with improved survival outcomes due to better healthcare infrastructure and treatment. In contrast, regions with lower HDI like Latin America, Africa, Asia, and Eastern Europe tend to experience higher age-standardized mortality rates despite having lower crude incidence rates. This suggests that treatment effectiveness is lower, leading to poorer survival outcomes.
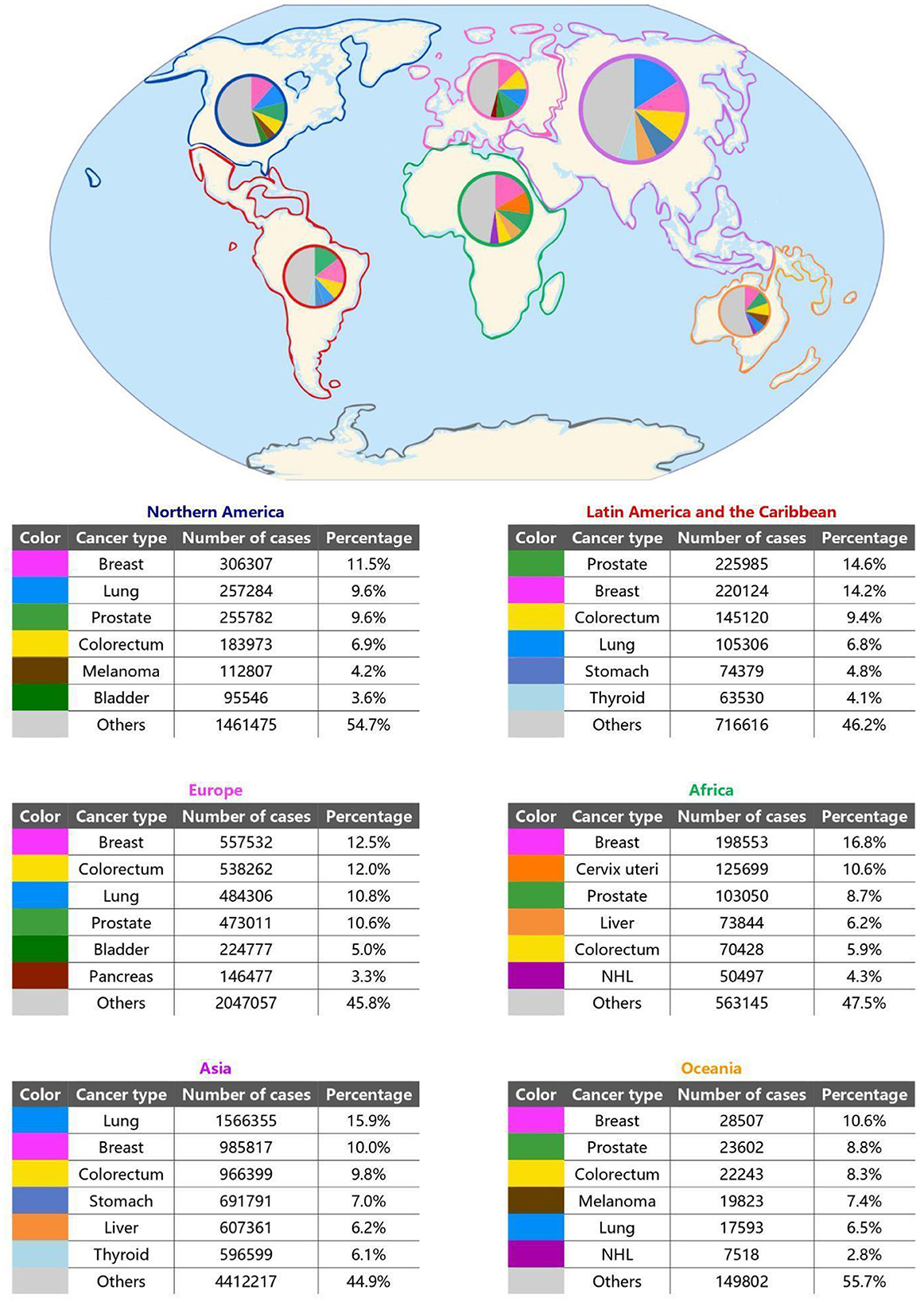
Figure 1. Global map with pie-charts presenting the most incident types of cancer by region (78–83). It's important to note that regions with higher Human Development Index (HDI) and high-income countries (HIC), such as Northern America, Europe and Oceania, have a predominance of lifestyle related malignancies (lung and colorectum cancer, for example); whereas regions with lower HDI and low- and middle-income countries (LMIC), such as Africa, Asia, Latin America and the Caribbean, have more infection-related malignancies (cervix uteri and liver cancer, in particular).
In Brazil, for example, cancer mortality rates have been surpassing cardiovascular disease mortality, reflecting a broader trend in many LMICs undergoing epidemiological transitions (32). Data from Brazil's 5,570 municipalities from 2000 to 2019 reveal that cancer mortality increased in over half of the states, particularly in higher-income areas. This shift emphasizes the rising importance of cancer in LMICs and the urgent need for targeted public health responses.
Globally, disparities in cancer outcomes between HICs and LMICs are striking. While HICs benefit from advanced diagnostic technologies, treatment options, and healthcare investments, LMICs struggle with systemic gaps that hinder cancer control, resulting in worse outcomes (33, 34). These disparities highlight the need for tailored approaches in LMICs to address their unique challenges, including limited resources and lack of specialized care.
Reliable cancer data collection is essential for effective public health strategies; however, many LMICs lack comprehensive cancer registries (35). Brazil's DATA SUS is an example of an established data collection system, but most LMICs still face gaps in data, hindering the development of targeted prevention and treatment programs. In contrast, HICs have robust cancer registries that support early detection and inform policy (36).
Delays in cancer diagnosis are common in LMICs, where patients often present with advanced-stage cancer due to limited access to diagnostic services and low awareness of cancer symptoms (37). Screening programs for breast, cervical, and colorectal cancers are often unavailable or inaccessible, and existing interventions lack clinically relevant measures (38, 39). Addressing these gaps is crucial to improve cancer control and patient outcomes.
Access to cancer treatment is another significant challenge in LMICs, where oncologic care is typically concentrated in urban centers, forcing rural patients to travel long distances and incur additional costs (40). Treatment facilities in LMICs often face staff shortages and inadequate resources (41). Even in HICs, geographical and financial barriers exist, leading to disparities in treatment access and quality (42).
Limited access to first-line cancer drugs is another barrier in LMICs, where the cost of medications, especially targeted therapies, is often prohibitive (43). Although efforts to increase access to generic drugs have been successful in HICs, LMICs continue to struggle with affordability and availability (44).
Additionally, social support systems in LMICs are often insufficient, leaving patients without financial, emotional, or logistical assistance during treatment (45). In contrast, HICs generally have more robust support networks, though inequalities remain, especially in private healthcare systems (46).
Addressing these challenges will require comprehensive strategies to improve health infrastructures, early detection, access to treatment, and social support for cancer patients in LMICs. Strengthening international collaborations and policies is essential to reduce the disparities in cancer outcomes between LMICs and HICs.
Particularities of cancer survivorship in low- and middle-income countries
Despite the growing body of literature on cancer survivorship in high-income countries (HICs), there remains a significant lack of data on late effects among cancer survivors in LMICs, where the cancer burden is substantial but long-term outcomes are largely unexplored (47). Research in LMICs is primarily focused on childhood cancer survivorship, with studies mostly originating from middle-income nations like India. Common late effects include secondary cancers, endocrine dysfunctions, reproductive issues, and cardiovascular problems, although their prevalence varies widely (5). Due to limited and heterogeneous study designs with small sample sizes, major gaps persist in understanding the types and risks of late effects in these regions, underscoring the need for systematic, comprehensive data on cancer survivorship in LMICs (5).
In LMICs, specialized centers for the long-term care of cancer survivors are scarce. However, some centers have conducted studies to shed light on this issue. For example, in India, one study examined 3,067 childhood cancer survivors and found that approximately two-thirds of the survivors experienced no late effects or only mild ones, while 15.6%, 16.2%, and 5.3% had grade 2, 3, and 4 late effects, respectively (89). Common late effects included chronic viral hepatitis (7.8%), thyroid dysfunction (7.5%), and other endocrine issues (13.6%). Notably, the incidence and severity of late effects have decreased over time, suggesting improvements in care and less aggressive treatments.
Another study of 300 survivors over 5 years identified that 23% had minimal disabilities, while 13% had moderate conditions, including cardiac problems and hypothyroidism (48). A comprehensive review of childhood cancer survivorship in India highlighted the prevalence of hepatitis B and C infections among survivors and the variability in research methodologies, making generalizations challenging (49). While many survivors report a good quality of life, there is an urgent need for monitoring strategies to detect late effects, particularly secondary cancers.
In Brazil, the Department of Pediatrics at the ACCamargo Cancer Center in São Paulo established a multidisciplinary team in 1999 to monitor long-term childhood cancer survivors (50). This team, consisting of oncologists, endocrinologists, cardiologists, and other specialists, found that 50% of patients had grade I late effects, while 22.5% had grade II, 35% had grade III, and 0.3% had grade IV. Among patients assessed for cardiac, gonadal, neurological, and renal function, a small percentage exhibited dysfunctions, highlighting the importance of multidisciplinary care for survivors.
Despite the progress made in LMICs, clinical characteristics of cancer survivors in these countries often mirror those seen in HICs, although social and financial disparities may exist. Metabolic disorders and endocrine dysfunctions are prevalent in both LMICs and HICs. In India, a study found high rates of dyslipidemia (61.8%), obesity (33%), and metabolic syndrome (12.2%) among children who had completed at least 2 years of cancer treatment (51). These findings are significant, as the coexistence of obesity and undernutrition in these children may create a unique metabolic profile. Another study indicated that childhood survivors of acute lymphoblastic leukemia (ALL) were more likely to be overweight or obese (30.8%), and had higher rates of hypertension, hypertriglyceridemia, and insulin resistance (52). Similarly, a study from Egypt found that childhood survivors of ALL had higher body mass indices and worse liver function markers than controls (53). In Brazil, children transplanted for acute leukemia, particularly those treated with total body irradiation, experienced a high prevalence of endocrinological late effects (54).
While endocrine and metabolic late effects are more common among cancer survivors, cardiovascular injuries remain the most lethal. A study in Mexico found that childhood cancer survivors treated with anthracyclines showed early signs of myocardial dysfunction, despite normal ejection fractions, and those treated with mediastinal radiotherapy were at risk for arrhythmias (55). In Brazil, studies report that approximately 10% of childhood cancer survivors in São Paulo experience late cardiovascular effects, with most being mild (56).
The current literature on cancer survivorship in LMICs highlights significant gaps in understanding compared to HICs, despite the high cancer burden in these regions. Studies on childhood cancer survivors reveal a variety of late effects that profoundly impact clinical management, such as chronic health issues. Data from urban and central areas suggest similar epidemiological trends in the late effects of cancer treatments. Therefore, there is a pressing need for innovative care models and targeted monitoring strategies to meet the unique needs of cancer survivors in LMICs. Addressing the systemic barriers to cancer survivorship care in these regions is crucial to improving outcomes for survivors.
From a global perspective, strengthening survivorship care in LMICs also aligns with WHO's broader strategic objectives in cancer control and non-communicable disease (NCD) management, which emphasize the continuity of care, integration into primary health systems, and the use of culturally relevant approaches (57).
Knowledge gaps in LMICs disproportionately affect certain populations. Gender-specific survivorship challenges—such as fertility preservation, early menopause, and the psychosocial burden of caregiving roles—are often under-addressed in LMICs, despite their substantial impact on quality of life, particularly for female survivors (58). Moreover, while survivorship data in LMICs predominantly focus on pediatric populations, limited attention has been given to the long-term needs of adult survivors, whose late effects and reintegration pathways often differ markedly. The transition from pediatric to adult care further complicates this landscape and remains a critical yet underexplored area (59).
Challenges and opportunities in cancer survivorship in LMICS
Cancer survivorship in LMICs faces significant challenges, including limited healthcare infrastructure, financial barriers, and psychological stigma. A 2022 survey by the Survivorship Special Interest Group of the International Psycho-Oncology Society highlighted that services such as reproductive health, genetic counseling, and distress management were more readily available in HICs compared to LMICs, with major barriers in LMICs including a focus on treatment rather than survivorship (60). Furthermore, a shortage of trained oncology professionals limits comprehensive survivorship care, particularly in rural areas, where survivors face high out-of-pocket costs and long travel distances to access care (61).
The social stigma surrounding cancer in LMICs exacerbates these challenges, leading to difficulties in survivors' relationships and limiting their access to mental health support (62). Survivors often face economic hardship due to direct treatment costs and indirect financial impacts, such as unemployment and discrimination. A Brazilian study revealed that 38% of survivors of childhood cancer still depended on their parents financially, while others faced social challenges, including smoking and drug use (50). These issues are particularly pronounced in LMICs, where financial instability and social vulnerability add to the burden.
Additionally, the availability of mental health services is limited, leaving many survivors without adequate psychological support. In Brazil, over a third of childhood cancer survivors reported cognitive impairments or pain, and a quarter had emotional difficulties (60). A study in Malaysia found that more than half of childhood cancer survivors experienced moderate or higher levels of anxiety, with diagnosis at advanced stages being a key predictor of poor health-related quality of life (63). These findings underscore the need for mental health resources and improved quality of life assessments in LMICs.
A major concern in cancer survivorship care is the identification and early diagnosis of secondary malignancies. Survivors of retinoblastoma, for example, are at an elevated risk of developing secondary cancers due to treatment. A study in Argentina found that 3.36% of retinoblastoma survivors developed secondary tumors, with radiation increasing the risk of certain cancers, such as Ewing sarcoma, by 700 times in hereditary survivors (64). This highlights the need for ongoing surveillance, genetic counseling, and early detection strategies for survivors at risk of secondary malignancies.
Improving cancer survivor care in LMICs requires strengthening community-based care models, like Brazil's Mais Médicos and Family Health Strategy, which bring healthcare professionals to underserved populations, fostering integrated care (65). Empowering local health workers and primary care providers to manage survivorship needs can ease the burden on oncology centers and improve care accessibility. Expanding telemedicine also offers a viable solution for remote symptom management, reducing the travel burden on survivors in rural areas (66).
Traditional and complementary medicine (T&CM) remains a key component of healthcare in many low- and middle-income countries (LMICs), where it often represents the most accessible or sole form of care, as noted by the World Health Organization (WHO) (67). However, cancer survivorship strategies seldom incorporate integrative approaches. Therapies such as mind-body interventions, phytotherapy, acupuncture, and nutritional support have demonstrated potential in managing common survivorship symptoms, including fatigue, anxiety, chronic pain, and gastrointestinal issues. While rigorous evaluation and regulation are necessary, integrating culturally relevant, evidence-informed T&CM into survivorship care may offer scalable, cost-effective solutions in resource-limited settings. Incorporating traditional healing within community care, primary care training, and policy frameworks could improve cultural acceptability, symptom management, and service accessibility. This approach supports WHO's recommendation to evaluate and integrate traditional medicine into health systems as part of universal health coverage efforts (68).
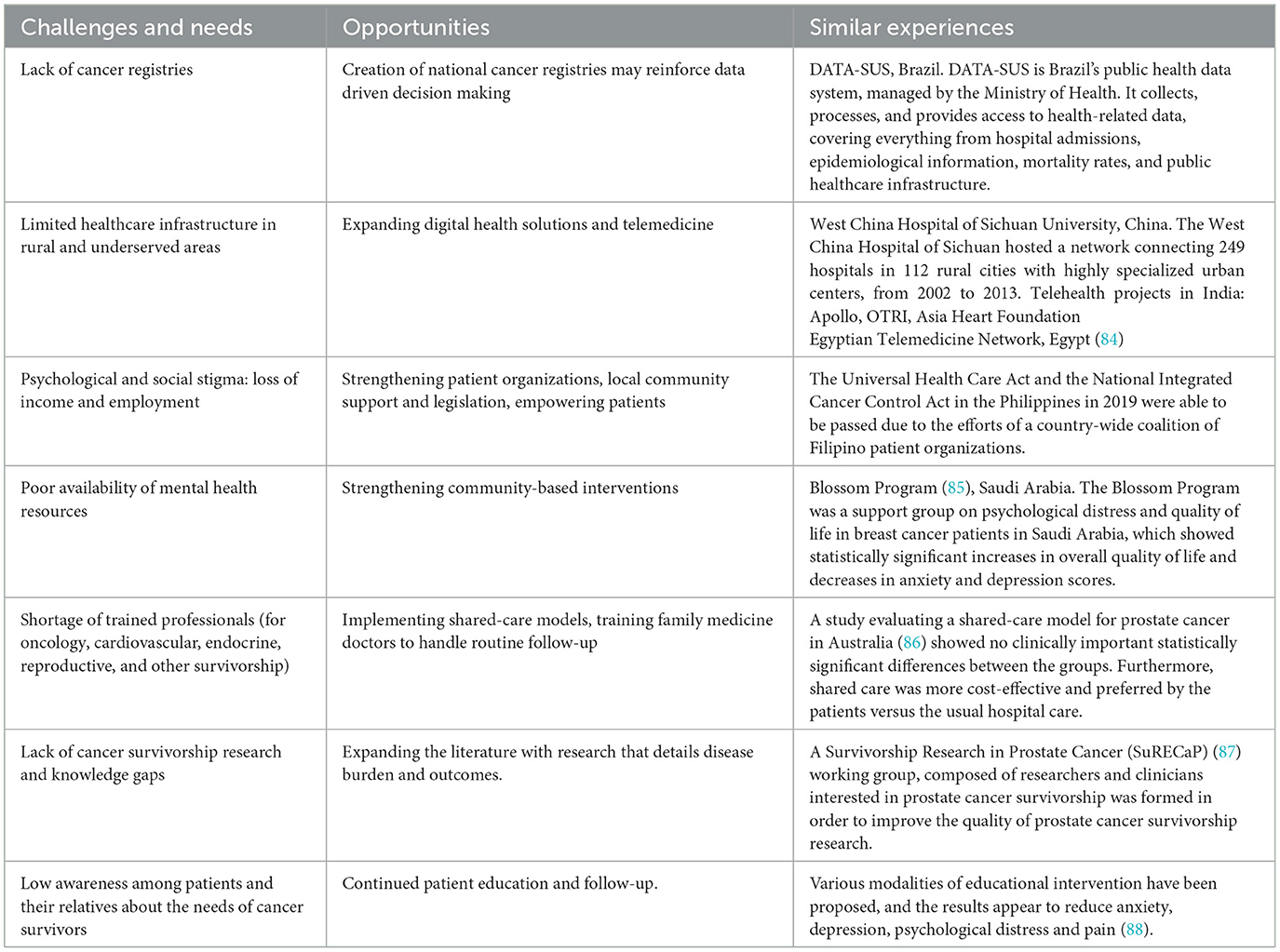
International collaborations and non-governmental organization support are crucial in building sustainable cancer survivorship programs in LMICs (69). These partnerships can provide essential resources, expertise, and infrastructure, enhancing care delivery. Task-shifting and shared-care models, where general practitioners manage routine follow-up care, can further decentralize survivorship care and improve patient-centered outcomes (70). Integrating survivorship care into national health policies and advocating for policy changes are also critical to ensuring long-term sustainability and adequate resources for cancer survivors (71). We have highlighted many opportunities for the various challenges faced by LMICs and cancer survivors in LMICs, as well as experiences worldwide, in a conceptual framework as seen in Figure 2.
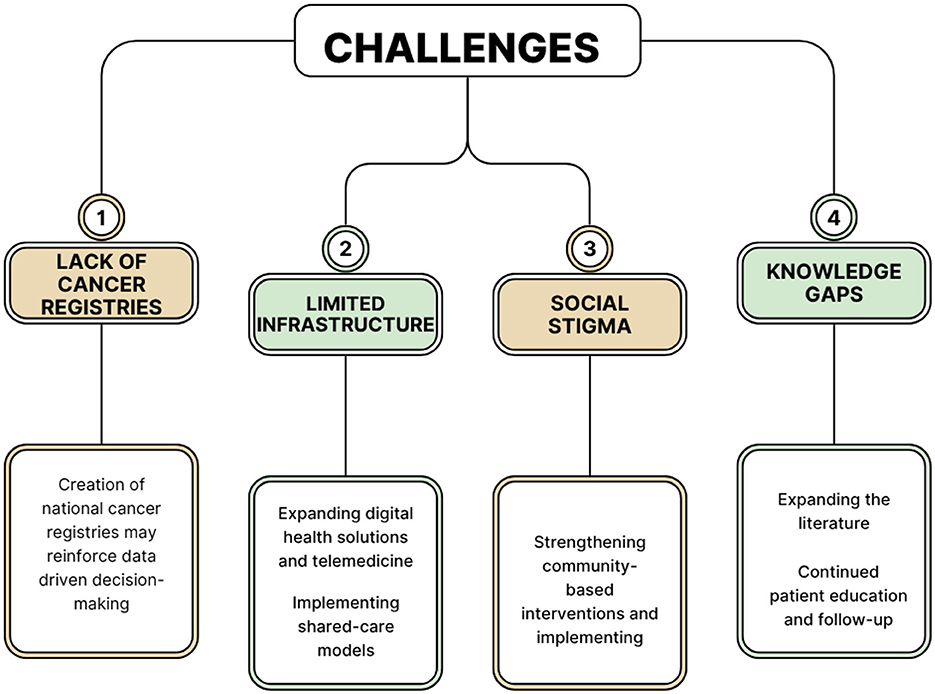
Figure 2. A conceptual diagram which summarizes the most important Challenges faced by cancer survivors in LMICs and the possible interventions that may improve care provided for patients.
Lastly, the development of comprehensive cancer registries can help identify gaps in care and inform region-specific interventions (72). By collecting detailed data on survivor outcomes, these registries can support evidence-based policies and improve care coordination, ensuring better long-term outcomes for cancer survivors.
By integrating findings from diverse geographic regions and levels of healthcare development, this review proposes a contextual framework for survivorship care in LMICs that includes community-based strategies, non-profit engagement, and scalable care models tailored to resource-limited settings. Moreover, this review proposes a contextualized framework for survivorship care in LMICs, emphasizing integrated primary care, local health worker engagement, and the inclusion of traditional medicine as potential tools for expanding survivorship support in low-resource settings. These insights provide a foundation for future research and policy efforts aimed at reducing global disparities in cancer survivorship. A summary of challenges and opportunities faced by LMICs can be seen in Table 2.
Comparison of cancer survivorship in HICS and LMICS
High-income countries (HICs) have made significant strides in managing the long-term sequelae of cancer and its treatment through the development of structured survivorship care frameworks. These include the implementation of survivorship care plans, multidisciplinary follow-up programs, and risk-based stratification models that allow for tailored surveillance and early intervention (73, 74). For instance, late effects such as cardiovascular disease, endocrine disorders, and cognitive impairment are routinely monitored in childhood and adult cancer survivors through well-integrated care pathways supported by national guidelines and electronic health records (75). Furthermore, the robust systems and care pathways present in HICs are often more cost-effective (73) than unstructured care, which is often present in LMICs.
In contrast, LMICs face persistent challenges in addressing these late effects due to fragmented health systems, limited access to specialized care, and the absence of standardized follow-up protocols. Some LMICs have initiated promising survivorship strategies. For example, survivorship clinics in Brazil have begun implementing follow-up protocols inspired by HIC guidelines but adapted to local resource constraints, often relying on nurse-led care or telemedicine platforms as alternatives (76). In India, the Indian Cancer Society's Project PICASSO (Partnership in Cancer Survivorship Optimization) helps to implement hospital-based survivorship clinics with success (77).
By comparing the structured, evidence-based models of survivorship care in HICs with the emerging, context-sensitive interventions in LMICs, it becomes evident that scalable and sustainable survivorship solutions require both innovation and policy commitment. Strategies such as task-shifting, mobile health interventions, and regional centers of excellence could bridge current gaps, particularly if supported by international collaborations and health system strengthening. Drawing from HIC experiences, LMICs have the opportunity to adapt survivorship frameworks in ways that are feasible, culturally appropriate, and equity-driven.
Limitations
This narrative review offers a broad synthesis of cancer survivorship in low- and middle-income countries (LMICs), yet several limitations must be acknowledged. First, the semi-structured and purposive literature search, while comprehensive, does not adhere to systematic review protocols, which may introduce selection bias. Without formal inclusion and exclusion criteria, there is a risk of omitting relevant studies, particularly those published in languages other than English or indexed in non-mainstream databases.
Additionally, the heterogeneity of the included studies, in terms of design, quality, and outcome measures, limits the ability to draw definitive conclusions or perform meta-analytic comparisons. Much of the existing research from LMICs focuses on pediatric populations, leaving a significant gap in data regarding adult cancer survivors, especially in rural and marginalized communities. Furthermore, survivorship studies from LMICs are often hospital-based and may not reflect the broader population of survivors who do not receive follow-up care or whose outcomes remain undocumented.
Lastly, survivorship experiences and health system responses are deeply influenced by sociocultural, economic, and political contexts that may not be fully captured in the existing literature. The absence of longitudinal studies and national cancer registries in many LMICs hinders efforts to assess long-term outcomes and the effectiveness of interventions.
Closing remarks
In conclusion, enhancing cancer survivorship care in LMICs requires tailored strategies that address specific challenges. Key approaches include conducting research to identify survivor needs, implementing community-based interventions, and advocating for policy changes to ensure equitable access to healthcare services. Collaborating with local organizations and stakeholders is essential for creating a supportive network that promotes the well-being of survivors. By prioritizing these strategies, we can improve healthcare systems and the quality of life for cancer survivors in LMICs. In this review, we offer novel contributions by centering the lived realities of cancer survivors in LMICs, a population often underrepresented in the global survivorship discourse. Unlike prior reviews that tend to generalize survivorship experiences or focus predominantly on high-income settings, our synthesis highlights region-specific challenges such as limited follow-up infrastructure, sociocultural barriers to care, and gaps in psychosocial support. Furthermore, we identify emerging patterns of late effects—particularly endocrine and metabolic disorders—in LMIC contexts and draw attention to the lack of systematic data collection and survivorship tracking. Future research should prioritize longitudinal investigations into the survivorship landscape within low- and middle-income countries (LMICs), with particular attention to the integration of survivors' experiences and findings. Additionally, efforts should be directed toward the design and evaluation of scalable, context-specific care models. Collaborative platforms that facilitate data exchange between countries could also be evaluated to assess how well they support innovation in the care of survivors.
Author contributions
GA: Formal analysis, Writing – original draft, Investigation, Writing – review & editing, Data curation, Methodology, Conceptualization, Visualization. GM: Writing – original draft, Writing – review & editing, Data curation. CB: Investigation, Methodology, Conceptualization, Writing – review & editing, Visualization, Formal analysis, Writing – original draft, Data curation. VA: Visualization, Writing – original draft, Writing – review & editing, Conceptualization. RM: Formal analysis, Writing – original draft, Writing – review & editing, Conceptualization. LC: Methodology, Investigation, Supervision, Writing – review & editing, Conceptualization, Project administration, Formal analysis, Writing – original draft, Visualization, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. We acknowledge FAPESP for funding and scholarships: Lucas Leite Cunha (2024/06697-8), Guilherme Falcão MAchado (2024/10933-4), and Rui Monteiro de Barros Maciel (2021/02752-6).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rowland JH, Kent EE, Forsythe LP, Loge JH, Hjorth L, Glaser A, et al. Cancer survivorship research in Europe and the United States: where have we been, where are we going, and what can we learn from each other? Cancer. (2013) 119:2094–108. doi: 10.1002/cncr.28060
2. Vázquez ML, Vargas I, Rubio-Valera M, Aznar-Lou I, Eguiguren P, Mogollón-Pérez AS, et al. Improving equity in access to early diagnosis of cancer in different healthcare systems of Latin America: protocol for the EquityCancer-LA implementation-effectiveness hybrid study. BMJ Open. (2022) 12:e067439. doi: 10.1136/bmjopen-2022-067439
3. Stefan DC, Tang S. Addressing cancer care in low- to middle-income countries: a call for sustainable innovations and impactful research. BMC Cancer. (2023) 23:756. doi: 10.1186/s12885-023-11272-9
4. Omotoso O, Teibo JO, Atiba FA, Oladimeji T, Paimo OK, Ataya FS, et al. Addressing cancer care inequities in sub-Saharan Africa: current challenges and proposed solutions. Int J Equity Health. (2023) 22:189. doi: 10.1186/s12939-023-01962-y
5. Wong KA, Moskalewicz A, Nathan PC, Gupta S, Denburg A. Physical late effects of treatment among survivors of childhood cancer in low- and middle-income countries: a systematic review. J Cancer Surviv. (2024) 19:1–17. doi: 10.1007/s11764-023-01517-8
6. Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. (2019) 4:5. doi: 10.1186/s41073-019-0064-8
7. Velusamy R, Nolan M, Murphy A, Thavendiranathan P, Marwick TH. Screening for coronary artery disease in cancer survivors: JACC: cardiooncology state-of-the-art review. JACC CardioOncol. (2023) 5:22–38. doi: 10.1016/j.jaccao.2022.12.007
8. van Dalen EC, Mulder RL, Suh E, Ehrhardt MJ, Aune GJ, Bardi E, et al. Coronary artery disease surveillance among childhood, adolescent and young adult cancer survivors: a systematic review and recommendations from the international late effects of childhood cancer guideline harmonization group. Eur J Cancer. (2021) 156:127–37. doi: 10.1016/j.ejca.2021.06.021
9. Wong J, Soh CH, Wang B, Marwick T. Long-term risk of heart failure in adult cancer survivors: a systematic review and meta-analysis. Heart. (2024) 110:1188–95. doi: 10.1136/heartjnl-2024-324301
10. Armenian SH, Gelehrter SK, Chow EJ. Strategies to prevent anthracycline-related congestive heart failure in survivors of childhood cancer. Cardiol Res Pract. (2012) 2012:713294. doi: 10.1155/2012/713294
11. Donahue PMC, MacKenzie A, Filipovic A, Koelmeyer L. Advances in the prevention and treatment of breast cancer-related lymphedema. Breast Cancer Res Treat. (2023) 200:1–14. doi: 10.1007/s10549-023-06947-7
12. Huang TT, Hudson MM, Stokes DC, Krasin MJ, Spunt SL, Ness KK. Pulmonary outcomes in survivors of childhood cancer: a systematic review. Chest. (2011) 140:881–901. doi: 10.1378/chest.10-2133
13. Bajwa R, Cheema A, Khan T, Amirpour A, Paul A, Chaughtai S, et al. Adverse effects of immune checkpoint inhibitors (programmed death-1 inhibitors and cytotoxic T-lymphocyte-associated protein-4 inhibitors): results of a retrospective study. J Clin Med Res. (2019) 11:225–36. doi: 10.14740/jocmr3750
14. Casano-Sancho P, Izurieta-Pacheco AC. Endocrine late effects in childhood cancer survivors. Cancers. (2022) 14:2630. doi: 10.3390/cancers14112630
15. Whelan KF, Stratton K, Kawashima T, Waterbor JW, Castleberry RP, Stovall M, et al. Ocular late effects in childhood and adolescent cancer survivors: a report from the childhood cancer survivor study. Pediatr Blood Cancer. (2010) 54:103–9. doi: 10.1002/pbc.22277
17. Ahles TA, Root JC, Ryan EL. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol. (2012) 30:3675–86. doi: 10.1200/JCO.2012.43.0116
18. Staff NP, Grisold A, Grisold W, Windebank AJ. Chemotherapy-induced peripheral neuropathy: a current review. Ann Neurol. (2017) 81:772–81. doi: 10.1002/ana.24951
19. Emery J, Butow P, Lai-Kwon J, Nekhlyudov L, Rynderman M, Jefford M. Management of common clinical problems experienced by survivors of cancer. Lancet. (2022) 399:1537–50. doi: 10.1016/S0140-6736(22)00242-2
20. Guilcher GMT, Rivard L, Huang JT, Wright NAM, Anderson L, Eissa H, et al. Immune function in childhood cancer survivors: a children's oncology group review. Lancet Child Adolesc Health. (2021) 5:284–94. doi: 10.1016/S2352-4642(20)30312-6
21. Deleemans JM, Toivonen K, Reimer RA, Carlson LE. The chemo-gut study: a cross-sectional survey exploring physical, mental, and gastrointestinal health outcomes in cancer survivors. Glob Adv Health Med. (2022) 11:2164957X221145940. doi: 10.1177/2164957X221145940
22. Tan SYC, Tsoukalas T, Javier K, Fazon T, Singh S, Vardy J. Recommendations on the surveillance and supplementation of vitamins and minerals for upper gastrointestinal cancer survivors: a scoping review. J Cancer Surviv. (2024). doi: 10.1007/s11764-024-01666-4. [Epub ahead of print].
23. Mudi A, Levy CS, Geel JA, Poole JE. Paediatric cancer survivors demonstrate a high rate of subclinical renal dysfunction. Pediatr Blood Cancer. (2016) 63:2026–32. doi: 10.1002/pbc.26132
24. Mansouri I, Schwartz B, Vu-Bezin G, Bejarano-Quisoboni D, Fresneau B, El-Fayech C, et al. Risk of renal or urinary related hospitalization in survivors of childhood cancer: results from the French childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev. (2023) 32:572–81. doi: 10.1158/1055-9965.EPI-22-0925
25. Gawade PL, Hudson MM, Kaste SC, Neglia JP, Wasilewski-Masker K, Constine LS, et al. A systematic review of selected musculoskeletal late effects in survivors of childhood cancer. Curr Pediatr Rev. (2014) 10:249–62. doi: 10.2174/1573400510666141114223827
26. Kadan-Lottick NS, Dinu I, Wasilewski-Masker K, Kaste S, Meacham LR, Mahajan A, et al. Osteonecrosis in adult survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. (2008) 26:3038–45. doi: 10.1200/JCO.2007.14.9088
27. Frederiksen LE, Erdmann F, Mader L, Mogensen H, Pedersen C, Kenborg L, et al. Psychiatric disorders in childhood cancer survivors in Denmark, Finland, and Sweden: a register-based cohort study from the SALiCCS research programme. Lancet Psychiatry. (2022) 9:35–45. doi: 10.1016/S2215-0366(21)00387-4
28. Godono A, Felicetti F, Conti A, Clari M, Dionisi-Vici M, Gatti F, et al. Employment among childhood cancer survivors: a systematic review and meta-analysis. Cancers. (2022) 14:4586. doi: 10.3390/cancers14194586
29. Stone DS, Ganz PA, Pavlish C, Robbins WA. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. (2017) 11:765–81. doi: 10.1007/s11764-017-0614-3
30. Fox RS, Armstrong GE, Gaumond JS, Vigoureux TFD, Miller CH, Sanford SD, et al. Social isolation and social connectedness among young adult cancer survivors: a systematic review. Cancer. (2023) 129:2946–65. doi: 10.1002/cncr.34934
31. Deegan A, Brennan C, Gallagher P, Lambert V, Dunne S. Social support and childhood cancer survivors: a systematic review (2006–2022). Psychooncology. (2023) 32:819–33. doi: 10.1002/pon.6128
32. Rache B, Rocha R, Medeiros LA, Okada LM, Ferrari G, Zeng H, et al. Transition towards cancer mortality predominance over cardiovascular disease mortality in Brazil, 2000-2019: a population-based study. Lancet Reg Health Am. (2024) 39:100904. doi: 10.1016/j.lana.2024.100904
33. Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends–an update. Cancer Epidemiol Biomarkers Prev. (2016) 25:16–27. doi: 10.1158/1055-9965.EPI-15-0578
34. GBD 2013 Risk Factors Collaborators, Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2015) 386:2287–323. doi: 10.1016/S0140-6736(15)00128-2
35. Siddiqui AH, Zafar SN. Global availability of cancer registry data. J Glob Oncol. (2018) 4:1–3. doi: 10.1200/JGO.18.00116
36. White MC, Babcock F, Hayes NS, Mariotto AB, Wong FL, Kohler BA, et al. The history and use of cancer registry data by public health cancer control programs in the United States. Cancer. (2017) 123:4969–76. doi: 10.1002/cncr.30905
37. Brand NR, Qu LG, Chao A, Ilbawi AM. Delays and barriers to cancer care in low- and middle-income countries: a systematic review. Oncologist. (2019) 24:e1371–80. doi: 10.1634/theoncologist.2019-0057
38. “Institute of Medicine (US) and National Research Council (US) National Cancer Policy Board.” In:Curry SJ, Byers T, Hewitt M, , editors. Fulfilling the Potential of Cancer Prevention and Early Detection. Washington (DC): National Academies Press (US) (2003).
39. Ginsburg O, Yip CH, Brooks A, Cabanes A, Caleffi M, Dunstan Yataco JA, et al. Breast cancer early detection: a phased approach to implementation. Cancer. (2020) 126:2379–93. doi: 10.1002/cncr.32887
40. Rehr M, Shoaib M, Ellithy S, Okour S, Ariti C, Ait-Bouziad I, et al. Prevalence of non-communicable diseases and access to care among non-camp Syrian refugees in northern Jordan. Confl Health. (2018) 12:33. doi: 10.1186/s13031-018-0168-7
41. Obeidat NA, Habashneh MA, Shihab RA, Hawari FI. Are Jordanian primary healthcare practitioners fulfilling their potential in cancer prevention and community health? Findings from a cross-sectional survey. BMJ Open. (2017) 7:e015269. doi: 10.1136/bmjopen-2016-015269
42. Barrios C, de Lima Lopes G, Yusof MM, Rubagumya F, Rutkowski P, Sengar M. Barriers in access to oncology drugs—a global crisis. Nat Rev Clin Oncol. (2023) 20:7–15. doi: 10.1038/s41571-022-00700-7
43. Ocran Mattila P, Ahmad R, Hasan SS, Babar ZU. Availability, affordability, access, and pricing of anti-cancer medicines in low- and middle-income countries: a systematic review of literature. Front Public Health. (2021) 9:628744. doi: 10.3389/fpubh.2021.628744
44. Fundytus A, Sullivan R, Vanderpuye V, Seruga B, Lopes G, Hammad N, et al. Delivery of global cancer care: an international study of medical oncology workload. J Glob Oncol. (2018) 4:1–11. doi: 10.1200/JGO.17.00126
45. WHO: Global Health Expenditure Database (2022). Available online at: https://apps.who.int/nha/database/country_profile/Index/en (Accessed January 28, 2025).
46. Zavala VA, Bracci PM, Carethers JM, Carvajal-Carmona L, Coggins NB, Cruz-Correa MR, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. (2021) 124:315–32. doi: 10.1038/s41416-020-01038-6
47. Denburg A, Wong KA, Moskalewicz A, Gupta S. Outcomes among survivors of childhood cancer in low- and middle-income countries: a systematic review. J Clin Oncol. (2023) 41:10057. doi: 10.1200/JCO.2023.41.16_suppl.10057
48. Seth R, Singh A, Seth S, Sapra S. Late effects of treatment in survivors of childhood cancers: a single-centre experience. Indian J Med Res. (2017) 146:216–23. doi: 10.4103/ijmr.IJMR_196_16
49. Arora RS, Arora PR, Seth R, Sharma S, Kumar C, Dhamankar V, et al. Childhood cancer survivorship and late effects: the landscape in India in 2020. Pediatr Blood Cancer. (2020) 67:e28556. doi: 10.1002/pbc.28556
50. Rigon H, Lopes LF, do Rosario Latorre M, de Camargo B. The GEPETTO program for surveillance of long-term survivors of childhood cancer: preliminary report from a single institution in Brazil. Med Pediatr Oncol. (2003) 40:405–6. doi: 10.1002/mpo.10146
51. Agarwal A, Kapoor G, Jain S, Malhotra P, Sharma A. Metabolic syndrome in childhood cancer survivors: delta BMI a risk factor in lower-middle-income countries. Support Care Cancer. (2022) 30:5075–83. doi: 10.1007/s00520-022-06910-0
52. Das G, Seth R, Ramakrishnan L, Jana M, Jain V, Gupta A, et al. Metabolic syndrome in childhood acute lymphoblastic leukemia/lymphoma survivors: a global cause for concern. Pediatr Blood Cancer. (2022) 69:S482–3. doi: 10.1002/pbc.29952
53. El-Rashedy FH, El-Hawy MA, El Hefnawy SM, Mohammed MM. Assessment of obesity and hepatic late adverse effects in the egyptian survivors of pediatric acute lymphoblastic leukemia: a single center study. Mediterr J Hematol Infect Dis. (2017) 9:e2017026. doi: 10.4084/mjhid.2017.026
54. Marinho DH, Ribeiro LL, Nichele S, Loth G, Koliski A, Mousquer RTG, et al. The challenge of long-term follow-up of survivors of childhood acute leukemia after hematopoietic stem cell transplantation in resource-limited countries: a single-center report from Brazil. Pediatr Transplant. (2020) 24:e13691. doi: 10.1111/petr.13691
55. Jiménez-Carbajal MG, Antúnez-Sánchez SP, Arreguín-González FE, Benito-Reséndiz AE. Evaluación cardiovascular de pacientes sometidos a tratamientos oncológicos en una clínica de supervivientes de cáncer infantil en México [Cardiovascular evaluation of patients undergoing cancer treatments at a clinic for childhood cancer survivors in Mexico]. Arch Cardiol Mex. (2020) 91:25–33. doi: 10.24875/ACM.20000401
56. Shimoda S, Horsman J, Furlong W, Barr R, de Camargo B. Disability and health-related quality of life in long-term survivors of cancer in childhood in Brazil. J Pediatr Hematol Oncol. (2008) 30:563–70. doi: 10.1097/MPH.0b013e31816e231c
57. World Health Organization. WHO Report on Cancer: Setting priorities, investing wisely and providing care for all. Geneva: WHO (2020). Available online at: https://www.who.int/publications/i/item/who-report-on-cancer-setting-priorities-investing-wisely-and-providing-care-for-all (Accessed January 28, 2025).
58. Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. (2012) 104:386–405. doi: 10.1093/jnci/djr541
59. Schwartz CL. Creating a bridge for transition: from pediatric cancer survival to life-long, risk-based health care of the adult cancer survivor. Cancer. (2020) 126:473–6. doi: 10.1002/cncr.32569
60. Signorelli C, Høeg BL, Asuzu C, Centeno I, Estapé T, Fisher P, et al. International survey of psychosocial care for cancer survivors in low-/middle- and high-income countries: current practices, barriers, and facilitators to care. JCO Glob Oncol. (2024) 10:e2300418. doi: 10.1200/GO.23.00418
61. Santos ATCD, Silva RPD, Almeida LM, et al. Cancer survivorship needs in Brazil: Patient and family perspective. PLoS One. 2020;15(10):e0239811. Published 2020 Oct 8. doi: 10.1371/journal.pone.0239811
62. Fereidouni Z, Dehghan Abnavi S, Ghanbari Z, Bosi MLM, Menezes MFB, Skaba MMVF, et al. The impact of cancer on mental health and the importance of supportive services. Galen Med J. (2024) 13:1–13. doi: 10.31661/gmj.v13i.3327
63. Subramaniam S, Kong YC, Chinna K, Kimman M, Ho YZ, Saat N, et al. Health-related quality of life and psychological distress among cancer survivors in a middle-income country. Psychooncology. (2018) 27:2172–9. doi: 10.1002/pon.4787
64. Villanueva G, Sampor C, Moreno F, Alderete D, Moresco A, Pinto N, et al. Subsequent malignant neoplasms in the pediatric age in retinoblastoma survivors in Argentina. Pediatr Blood Cancer. (2022) 69:e29710. doi: 10.1002/pbc.29710
65. Russo LX. Effect of more doctors (mais médicos) program on geographic distribution of primary care physicians. Cien Saude Colet. (2021) 26:1585–94. doi: 10.1590/1413-81232021264.26932020
66. Yadav K, Ginsburg O, Basu P, Mehrotra R. Telemedicine and cancer care in low- and middle-income countries during the SARS-CoV-2 pandemic. JCO Glob Oncol. (2021) 7:1633–8. doi: 10.1200/GO.21.00249
67. World Health Organization. WHO Traditional Medicine Strategy: 2014–2023. Geneva: WHO (2013). Available online at: https://www.who.int/publications/i/item/9789241506096
68. World Health Organization. Global Summit on Traditional Medicine – Summary Report. Geneva: WHO (2023). Available online at: https://www.who.int/publications/m/item/who-traditional-medicine-global-summit-2023
69. Blanchard C, Lubuzo B, Asirwa FC, Dlamini X, Msadabwe-Chikuni SC, Mwachiro M, et al. Multisector collaborations and global oncology: the only way forward. JCO Glob Oncol. (2021) 7:153–61. doi: 10.1200/GO.20.00492
70. Jefford M, Howell D, Li Q, Lisy K, Maher J, Alfano CM, et al. Improved models of care for cancer survivors. Lancet. (2022) 399:1551–60. doi: 10.1016/S0140-6736(22)00306-3
71. Nekhlyudov L, Mollica MA, Jacobsen PB, Mayer DK, Shulman LN, Geiger AM. Developing a quality of cancer survivorship care framework: implications for clinical care, research, and policy J Natl Cancer Inst. (2019) 111:1120–30. doi: 10.1093/jnci/djz089
72. Lee B, Gately L, Lok SW, Tran B, Lee M, Wong R, et al. Leveraging comprehensive cancer registry data to enable a broad range of research, audit and patient support activities. Cancers. (2022) 14:4131. doi: 10.3390/cancers14174131
73. Witteveen A, Otten JWM, Vliegen IMH, Siesling S, Timmer JB, IJzerman MJ. Risk-based breast cancer follow-up stratified by age. Cancer Med. (2018) 7:5291–8. doi: 10.1002/cam4.1760
74. Greenlee H, Molmenti CL, Crew KD, Awad D, Kalinsky K, Brafman L, et al. Survivorship care plans and adherence to lifestyle recommendations among breast cancer survivors. J Cancer Surviv. (2016) 10:956–63. doi: 10.1007/s11764-016-0541-8
75. Fidler-Benaoudia MM, Oeffinger KC. Childhood leukemia, late effects, and a person-centric model of follow-up. J Natl Cancer Inst. (2019) 111:880–1. doi: 10.1093/jnci/djz018
76. Dias CG, Duarte AM, Ibanez AdaS, Rodrigues DB, Barros DP, Soares JdosS, et al. Enfermeiro clínico especialista: um modelo de prática avançada de enfermagem em oncologia pediátrica no Brasil [clinical nurse specialist: a model of advanced nursing practice in pediatric oncology in Brazil]. Rev Esc Enferm USP. (2013) 47:1426–30. doi: 10.1590/S0080-623420130000600025
77. Kurkure PA, Dhamankar VS, Joshi S, Jha S, Nair S, Goswami S. Partnership in cancer survivorship optimization (PICASSO) project: an Indian Cancer Society (ICS) initiative for cancer survivorship program in India. JCO. (2018) 36:46. doi: 10.1200/JCO.2018.36.7_suppl.46
78. International Agency for Research on Cancer: Pie-chart of cancer incidence in Africa. (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=903 (Accessed January 4, 2025).
79. International Agency for Research on Cancer: Pie-chart of cancer incidence in Latin America and the Caribbean. (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=904 (Accessed January 4, 2025).
80. International Agency for Research on Cancer: Pie-chart of cancer incidence in Northern America (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=905 (Accessed January 4, 2025).
81. International Agency for Research on Cancer: Pie-chart of cancer incidence in Asia. (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=935 (Accessed January 4, 2025).
82. International Agency for Research on Cancer: Pie-chart of cancer incidence in Europe. (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=908 (Accessed January 4, 2025).
83. International Agency for Research on Cancer: Pie-chart of cancer incidence in Oceania. (2024). Available online at: https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&map_nb_color=8&types=0&key=total&populations=909 (Accessed January 4, 2025).
84. Combi C, Pozzani G, Pozzi G. Telemedicine for developing countries. a survey and some design issues. Appl Clin Inform. (2016) 7:1025–50. doi: 10.4338/ACI-2016-06-R-0089
85. Alshamsi HA, Aseel HA, Obeid DA, Aljohi A. The efficacy of psychoeducational support group for saudi breast cancer survivors. Asian Pac J Cancer Prev. (2023) 24:569–74. doi: 10.31557/APJCP.2023.24.2.569
86. Emery JD, Jefford M, King M, Hayne D, Martin A, Doorey J, et al. ProCare Trial: a phase II randomized controlled trial of shared care for follow-up of men with prostate cancer. BJU Int. (2017) 119:381–9. doi: 10.1111/bju.13593
87. Narayan V, Harrison M, Cheng H, Kenfield S, Aggarwal R, Kwon D, et al. Improving research for prostate cancer survivorship: a statement from the survivorship research in prostate cancer (SuRECaP) working group. Urol Oncol. (2020) 38:83–93. doi: 10.1016/j.urolonc.2019.10.006
88. Champarnaud M, Villars H, Girard P, Brechemier D, Balardy L, Nourhashémi F. Effectiveness of therapeutic patient education interventions for older adults with cancer: a systematic review. J Nutr Health Aging. (2020) 24:772–82. doi: 10.1007/s12603-020-1395-3
Keywords: cancer survivorship, low-and middle-income countries (LMICs), late effects, health disparities, quality of life
Citation: dos Anjos GR, Machado GF, de Barros CP, de Andrade VP, Maciel RMB and Cunha LL (2025) Cancer survivorship in low- and middle-income countries: challenges, needs, and emerging support strategies. Front. Public Health 13:1601483. doi: 10.3389/fpubh.2025.1601483
Received: 28 March 2025; Accepted: 27 June 2025;
Published: 16 July 2025.
Edited by:
Anna Santos Salas, University of Alberta, CanadaReviewed by:
Gabriel Madeira Werberich da Silva, National Cancer Institute (INCA), BrazilDaniel Krüerke, Klinik Arlesheim, Switzerland
Samvel Bardakhchyan, Hematology Center After Yeolyan, Armenia
Copyright © 2025 dos Anjos, Machado, de Barros, de Andrade, Maciel and Cunha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucas Leite Cunha, bHVjYXMubGVpdGVAdW5pZmVzcC5icg==
 Gustavo Rodrigues dos Anjos
Gustavo Rodrigues dos Anjos Guilherme Falcao Machado
Guilherme Falcao Machado Cassiano Pereira de Barros1,2
Cassiano Pereira de Barros1,2 Victor Piana de Andrade
Victor Piana de Andrade Rui Monteiro de Barros Maciel
Rui Monteiro de Barros Maciel Lucas Leite Cunha
Lucas Leite Cunha