- 1Institute of Epidemiology and Medical Biometry, Ulm University, Ulm, Germany
- 2German Center for Child and Adolescent Health (DZKJ), Partner Site Ulm, Ulm, Germany
- 3Pediatric Epidemiology, Department of Pediatrics, Medical Faculty, Leipzig University, Leipzig, Germany
- 4German Center for Child and Adolescent Health (DZKJ), Partner Site Leipzig, Leipzig, Germany
Introduction: The COVID-19 pandemic and associated preventive measures influenced family health and behavior, leading to diverse effects on sleep.
Methods: This study examined sleep characteristics before, during and after the COVID-19 pandemic in children (n = 558), mothers (n = 465), and fathers (n = 318) in Germany, using data from the prospective Ulm SPATZ Health Study. We compared the period from April 2017 to May 2023 (children aged 5–10 years) with the period from 15 March 2020 to 3 April 2022, defined as “COVID-19 pandemic.” Sleep quality was measured using the Children's Sleep Habits Questionnaire (CSHQ) and the Pittsburgh Sleep Quality Index (PSQI), among children and parents, respectively. Multivariable mixed models were used to assess the associations of the COVID-19 pandemic compared to before and after the pandemic with sleep characteristics among boys, girls, mothers, and fathers, separately.
Results: Child and parent sleep quality showed a weak correlation among 6-year-old boys and their mothers. A moderate correlation was observed between mothers' mental health and boys' sleep quality at ages 5, 6, and 9. Parents' mental health showed a moderate correlation with their sleep quality. Multivariable mixed models revealed better sleep quality (lower CSHQ total scores) among boys during the COVID-19 pandemic compared to before and after. Daytime sleepiness decreased among boys and girls, while no significant changes were found for sleep duration and sleep latency. Among mothers, sleep duration increased on free-days, while fathers experienced increased sleep duration on work-days, along with increased sleep efficiency.
Discussion: This study showed that family sleep quality (indexed with the CSHQ and PSQI) did not decrease during the COVID-19 pandemic compared to sleep quality measured at one (parents) or two (children) annual time points before the pandemic and up to one after it. Instead, parental sleep duration increased, children experienced reduced daytime sleepiness, and boys exhibited improved sleep quality. To effectively optimize public health during a pandemic, findings on sleep quality should be interpreted in conjunction with findings on mental health, given their interrelated nature, as also indicated by our study.
Introduction
The COVID-19 pandemic, along with the legally mandated preventive measures implemented to mitigate its spread, have affected the health and behavior of children and parents. Sleep is a critical aspect of health (1), and the pandemic has affected sleep characteristics in several ways (2–4). While sleep duration may increase (2, 4–11), it is important to note that poorer mental health (12–14), anxiety (15, 16), increased screen-time (2, 17–19), and altered and irregular sleep patterns (2, 8, 9, 20, 21) during a pandemic may negatively impact other important aspects of sleep (9, 22, 23), such as sleep disturbances or sleep latency. The underlying mechanism and family-specific pathways are described by Peltz et al. (24), Ballesio et al. (25) and Zhan et al. (26). These factors may contribute to the overall decline in subjective sleep quality observed among children, adolescents (2, 9, 27–30), and parents (30–32) during the pandemic. Studies investigating sleep characteristics within families and their association with the COVID-19 pandemic remain limited and have been rarely analyzed to date.
The current study aimed to investigate associations of the COVID-19 pandemic (compared to pre- and and post-pandemic periods) with sleep characteristics of children and parents using the Ulm SPATZ Health Study. This longitudinal birth cohort study has conducted annual follow-ups with children and parents since 2012, providing data spanning the pre-pandemic, pandemic, and post-pandemic.
Methods
Study participants
The current study was based on the Ulm SPATZ Health study, a population-based longitudinal birth cohort study conducted in Ulm, southern Germany. Participants were recruited at the Department of Gynecology and Obstetrics, University Hospital Ulm (at that time the only maternity hospital in Ulm). Mothers who had insufficient German language skills, had an outpatient childbirth, were under the age of 18, had a postpartum transfer to the intensive care unit, or experienced a stillbirth were excluded from participating in the study. A complete description of the Ulm SPATZ Health study can be found elsewhere (33). Briefly, 1,006 newborns from 970 mothers were recruited while hospitalized following delivery. Baseline data were collected between April 2012 and May 2013 (overall response rate, 49%). Children and parents have been followed up annually; resulting in the availability of pre-pandemic, COVID-19 pandemic and post-pandemic data.
In the present study, of the 1,006 newborns, a children's subgroup of 558 (55.5% of baseline), was included, for whom at least one questionnaire was completed at ages 5, 6, 7, 8, 9, or 10 years and for whom outcome data were available. The subgroups of mothers and fathers consist of participants who completed at least one questionnaire when the child was aged 6, 7, 8, or 9 years, and for whom outcome data were available. These subgroups included 465 mothers (45.1% of baseline) and 318 fathers (45.0% of baseline). Ethical approval was obtained from the Ethics Committee of the University of Ulm (no. 311/11).
COVID-19 pandemic
For this analysis, we examined the period from April 2017 to May 2023 (child ages 5-10 years), with the timeframe from March 15, 2020 to April 3, 2022, defined as “COVID-19 pandemic.” Since the questionnaires used assess sleep quality retrospectively over the “last 30 days,” Pittsburgh Sleep Quality Index (PSQI) or “last months,” Children's Sleep Habits Questionnaire (CSHQ), questionnaires completed up to April 15, 2022, were included in the “COVID-19 pandemic” category. Questionnaires completed outside this period were categorized as “before and after the pandemic.” This classification was used to create a dichotomous exposure variable.
Measurement of sleep characteristics and mental health
Sleep characteristics
Child sleep characteristics at ages 5, 6, 7, 8, 9, and 10 years were the primary outcome variables of interest. Sleep quality in children was evaluated using the validated German version of the Children's Sleep Habits Questionnaire (CSHQ) (34), which was completed annually by the parents, mostly the mothers. The CSHQ (35) includes 48 items, of which 33 are categorized into eight different subscales, namely (1) bedtime resistance, (2) sleep latency/sleep onset delay, (3) sleep duration, (4) sleep anxiety, (5) night wakings, (6) parasomnias, (7) sleep-disordered breathing, and (8) daytime sleepiness. Each subscale comprises multiple items, with higher scores indicating poorer sleep quality. The total CSHQ score was calculated by summing all subscale scores, providing a comprehensive measure of overall sleep quality, by incorporating key attributes of sleep quality in children (36). The total CSHQ score can range from 33–99, as each item is reported on a three-point scale. Internal consistency of the validated German version of the CSHQ, measured by Cronbach's alpha, is α = 0.68 (34).
Parent sleep characteristics, assessed when their child was aged 6, 7, 8, and 9 years, were the primary outcome variables of interest. Parent sleep quality was evaluated with the validated German version of the Pittsburgh Sleep Quality Index (PSQI) (37, 38), for work-days and free-days separately. This distinction was based on findings from Pilz et al. (39) and Reis et al. (40) suggesting that the original PSQI predominantly reflects sleep quality on work-days. The PSQI includes seven subscales capturing various characteristics of sleep quality: (1) subjective sleep quality (2) sleep latency, (3) sleep duration, (4) sleep efficiency, (5) sleep disturbance, (6) use of sleep medication, (7) daytime dysfunction. The total PSQI score is calculated by summing the 19 item scores, resulting in an overall sleep quality score ranging from 0 to 21. Internal consistency of the German version of the PSQI, measured by Cronbach's alpha, is α = 0.85 (38).
We also assessed sleep duration, defined as the time between 'falling asleep' and 'waking up', and sleep latency, defined as the time needed to fall asleep, analyzed separately for work-days (weekdays for children) and free-days for both children and parents. Additionally, bedtime was calculated for parents and defined as the actual time spent in bed, analyzed separately for work-days and free-days.
Mental health
The German version of the HADS was used to index maternal and paternal mental health at child ages 5, 6, and 9 years. The HADS questionnaire is a validated 14-item screening measure with two subscales that assess symptoms of anxiety (7 items) and depression (7 items) in the last week prior to assessment (41, 42). The questionnaire has also been validated in the German language (42, 43). The possible HADS score ranges from 0–42 (total score) (42). Internal consistencies, measured by Cronbach's alpha, is α = 0.72, and α = 0.82 for the subscales HADS-Anxiety, and HADS-Depression, respectively (44). We chose to use the total HADS score rather than analyzing the anxiety and depression subscales separately, as our primary interest was in the overall psychological distress experienced by participants.
Confounding variables
Information on parental sociodemographic variables were collected at childbirth through self-reported questionnaires. Child gender assigned at birth (male or female) was used for stratification of the analysis of children.
Confounders were selected based on a review of relevant literature (2, 4, 7, 12, 13, 17, 21, 24, 27, 45–51). For the model between the COVID-19 pandemic and child sleep characteristics; child age at time of the assessment, child age at school entry, maternal educational attainment (<12 or ≥12 years of school education), maternal nationality (German or non-German), and maternal age at childbirth were included to control for confounding. Additionally, the final model was adjusted for maternal mental health, measured using the Hospital Anxiety and Depression Scale (HADS) score when the child was 5 years old (the first longitudinal data point included in the analysis). This adjustment was made to evaluate the association between the COVID-19 pandemic and child sleep characteristics independently of maternal pre-pandemic mental health (we adjusted for maternal pre-pandemic mental health rather than paternal, due to greater completeness of maternal data). “Mental health during the pandemic” was considered a potential mediator, and therefore no adjustment was made for this variable.
For the model between the COVID-19 pandemic and maternal and paternal sleep quality; maternal and paternal age at childbirth, maternal and paternal educational attainment (<12 or ≥12 years of school education), maternal and paternal nationality (German or non-German), and child age at time of the outcome assessment were included to control for confounding. Additionally, the final model was adjusted for maternal and paternal mental health using the HADS score when the child was 6 years old (the first longitudinal data point included in the analysis). This adjustment was made to evaluate the association between the COVID-19 pandemic and maternal and paternal sleep characteristics independently of maternal and paternal pre-pandemic mental health.
Statistical analysis
Descriptive values of sleep characteristics were analyzed longitudinally and reported by means and standard deviation or n and percentages. Pearson correlation coefficients were calculated to evaluate the strength and direction of linear relationships between concurrent parent and child sleep quality when the child was aged 6 and 8 years (i.e., before and during the COVID-19 pandemic). Additionally, Pearson correlation coefficients were calculated between concurrent parental mental health and child sleep quality when the child was aged 5, 6, and 9 years. Data on parental mental health were unavailable for child ages 7 and 8 years; therefore, correlations for these time points could not be calculated. Lastly, Pearson correlation coefficients were calculated to evaluate the strength and direction of linear relationships between concurrent parental mental health and parental sleep quality when the child was aged 6 and 9 years. Correlations were not calculated for child age 5 years, as parents sleep quality was not assessed separately for work-days and free-days at that time point. These correlations were examined to inform potential associations and underlying patterns, providing insights into the relationship between child sleep quality, parent sleep quality and parental mental health.
We fitted multivariable linear mixed-effects models, assuming an unstructured covariance matrix, to estimate differences in means associated with the time during the COVID-19 pandemic vs. before and after the COVID-19 pandemic. The intercept represents the individual score at baseline (random effect). The models were analyzed separately for boys, girls, mothers, and fathers in order to account for potential effect modification of the COVID-19 pandemic with gender. Based on the availability of sleep data, the mixed models incorporated up to six time points for children (ages 5, 6, 7, 8, 9, and 10 years) and up to four time points for parents (ages 6, 7, 8, and 9 years of the child). Participants were included in the mixed-effects model if they had at least one measurement of the outcome variable available and complete data for all the covariates. Consequently, those with missing data for either the outcome and/or the covariates were excluded from the analysis (listwise deletion). The analysis was performed using SAS® 9.4 (The SAS Institute, Cary, NC, USA).
Results
Descriptive results
We analyzed data from 558 children (278 boys, 280 girls), 465 mothers, and 318 fathers with available follow-up data on sleep characteristics. Maternal and paternal age at childbirth did not differ substantially between the baseline sample (n = 970 families) and the analysis sample. However, the analysis sample included a slightly higher proportion of mothers with German nationality and a higher educational level compared to the baseline sample (Table 1). The mean age of the children in the analysis sample at school entry was 6.5 years (SD 0.28; rang: 5.97–6.96 years).
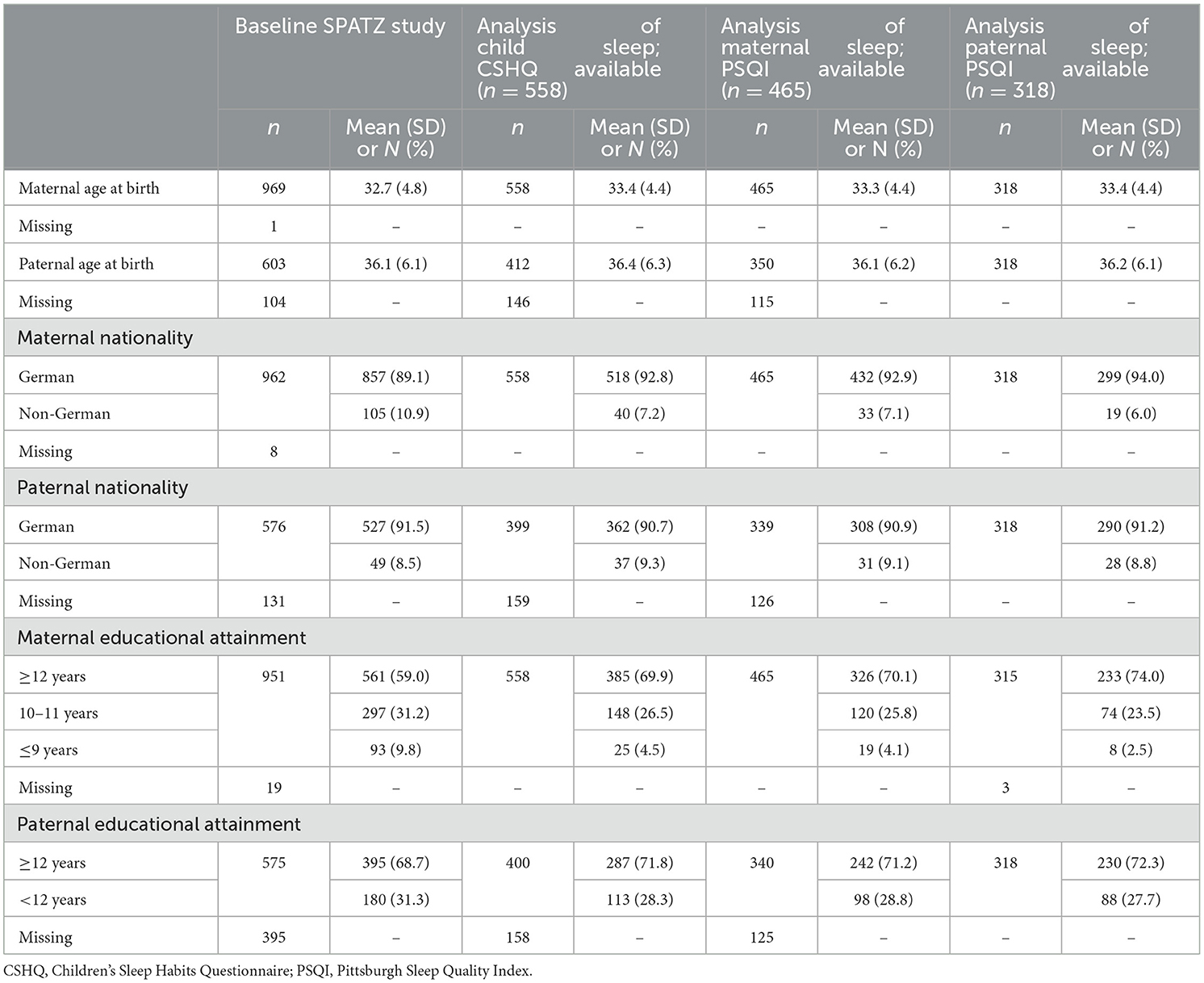
Table 1. Baseline characteristics of parental data included in the statistical analysis (n = 465 mothers, n = 318 fathers) vs. SPATZ cohort baseline (n = 970 mothers, and n = 707 fathers).
Table 2 presents descriptive data on sleep characteristics among children, mothers and fathers. The results indicate that girls generally exhibited better sleep quality (CSHQ) than boys at all time points, except during the early phase of the COVID-19 pandemic. Mothers reported slightly poorer sleep quality (PSQI) compared to fathers across the study period. Descriptive data suggest differences in sleep duration between boys and girls on week-days and free-days, with girls tending to sleep slightly more on free-days and slightly less on week-days compared to boys. Before the COVID-19 pandemic, when children were 6 years old, 71% of mothers and 73% of fathers reported good sleep quality (PSQI ≤ 5). During the COVID-19 pandemic, when children were 8 years old, these proportions increased slightly to 73% for mothers and 75% for fathers. However, it is important to note that there was a loss to follow up of 66 mothers and 59 fathers between these two time-points. Regarding mental health, 28% of mothers and 10% of fathers reported significant anxiety symptoms (HADS score ≥8) before the COVID-19 pandemic (child age 6 years), while 16% of mothers and 13% of fathers reported significant depressive symptoms. Sleep latency was shorter on free-days compared to work-days among parents. Additionally, descriptive results suggested a trend toward increased sleep latency among fathers during the COVID-19 pandemic.
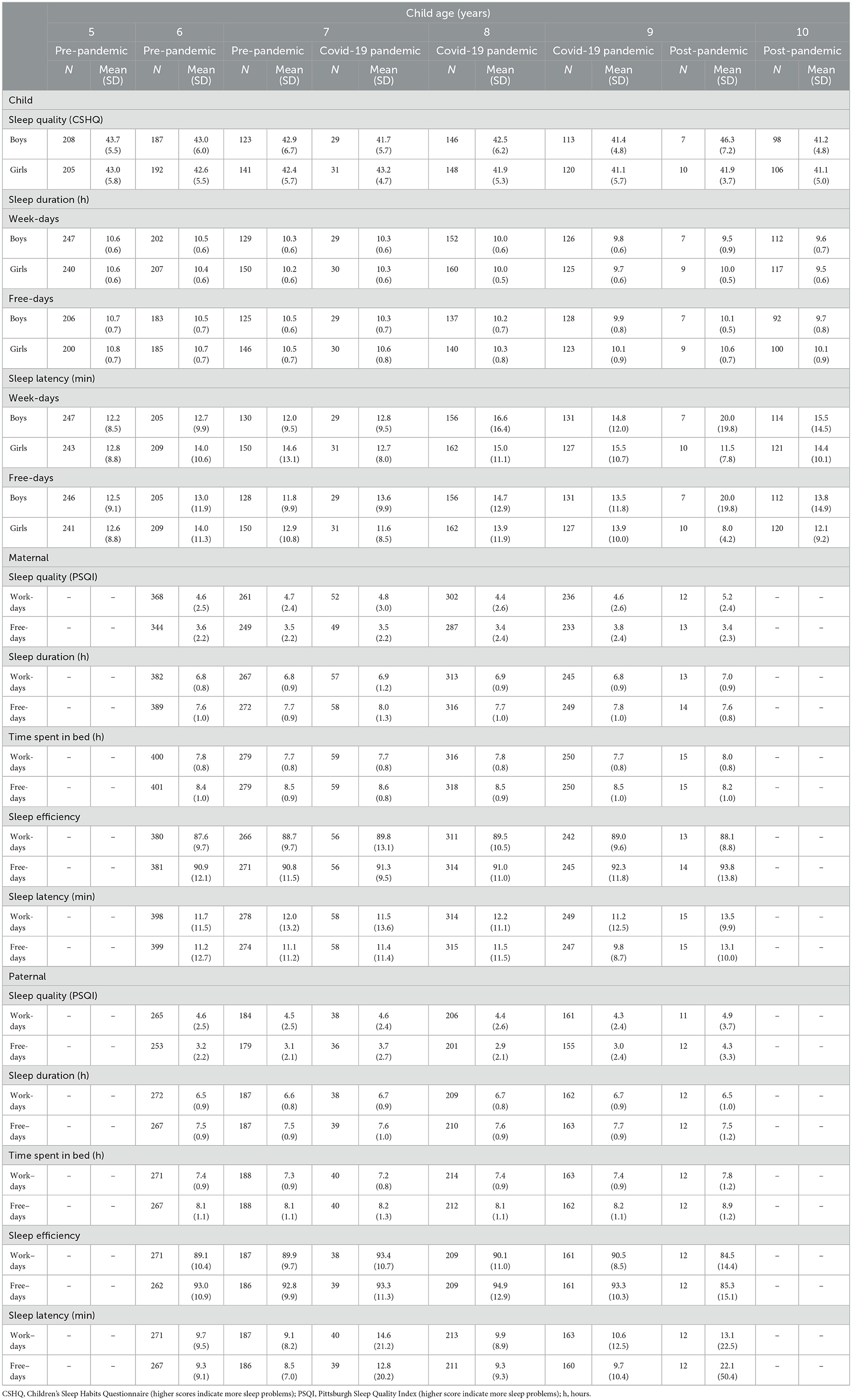
Table 2. Sleep characteristics of children, mothers and fathers by child age and COVID-19 pandemic periods.
Tables 3, Supplementary Tables S1, S2 summarize the results of the Pearson correlation analyses. Among 6-year-old boys, a slight positive correlation was observed between their sleep quality and maternal sleep quality on both weekdays (r = 0.19, p = 0.01) and free-days (r = 0.22, p = 0.005), whereas no statistically significant correlation was found for girls (weekdays: r = 0.14, p = 0.06; free-days: r = 0.10, p = 0.19) (Table 3). At child age 8 years, no statistically significant correlations were observed for either boys or girls (Table 3). Stronger correlations were identified between maternal mental health and children's sleep quality, particularly among boys at ages 5, 6, and 9 years (r = 0.33, p < 0.001; r = 0.28, p <0.001; r = 0.25, p = 0.01) and among 5-year-old girls (r = 0.25, p < 0.001) (Supplementary Table S1). Maternal mental health was also strongly correlated with parental sleep quality, as detailed in Supplementary Table S2.
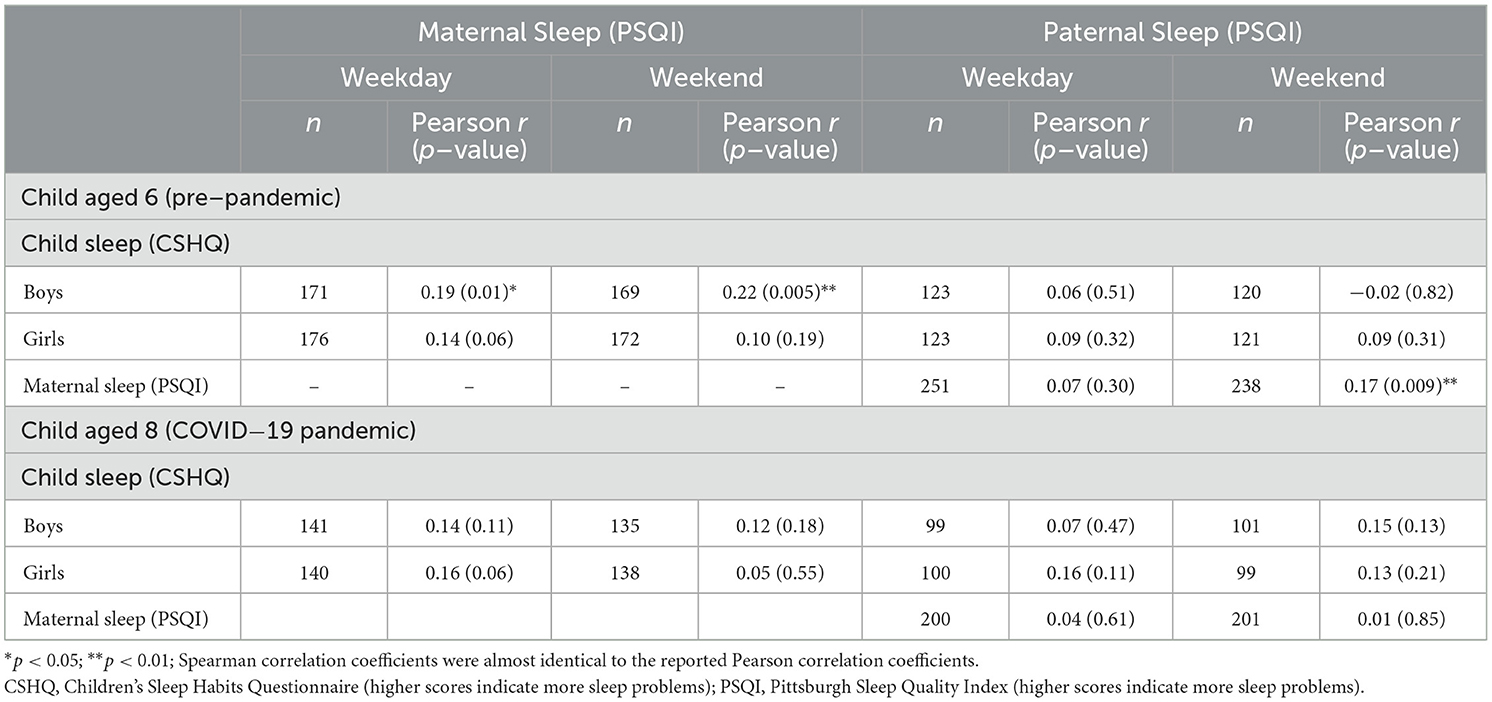
Table 3. Correlations between child sleep quality (by gender) and maternal and paternal sleep quality at child ages 6 and 8 years (pre–pandemic and during COVID−19 pandemic).
Analytical results
Table 5 presents the results of the mixed models. During the COVID-19 pandemic, boys exhibited improved sleep quality compared to pre- and post-pandemic periods, with a mean intra-individual difference of −1.52 (95% confidence interval (CI): −2.85, −0.19). Additionally, daytime sleepiness decreased in both boys (−1.24; 95% CI: −1.84, −0.63) and girls (−1.52; 95% CI: −2.85, −0.19). However, no significant changes were observed in sleep latency or sleep duration among children during the COVID-19 pandemic. Among parents, mothers experience a slight increase in sleep duration on free-days (+0.26 h; 95% CI: 0.06, 0.46), while fathers reported increased sleep duration on work-days (+0.18 h; 95% CI: 0.01, 0.35). Fathers also showed an improvement in sleep efficiency (+4.81; 95% CI: 2.15, 7.46). Sleep latency and overall sleep quality, as measured by the PSQI remained largely unchanged for both mothers and fathers during the COVID-19 pandemic, regardless of work-days or free-days.
Discussion
In this prospective study including data of 558 children, 465 mothers, and 318 fathers of the Ulm SPATZ Health study, we investigated the associations between the COVID-19 pandemic and various sleep characteristics. The analysis revealed that family sleep quality did not decline during the COVID-19 pandemic compared to pre- and post-pandemic periods. Notably, parental sleep duration increased, daytime sleepiness among children decreased, and boys experienced improved sleep quality during the COVID-19 pandemic.
Sleep quality
Our finding of improved sleep quality among boys during the COVID-19 pandemic (CSHQ total score −1.52; 95 % CI: −2.85, −0.19) contrasts with most previous literature, which report a decline in children's sleep quality during this period (27, 32, 52, 53). However, many studies are cross-sectional or rely on retrospective assessment of pre-pandemic data, which may limit their comparability to our longitudinal approach. Two studies, however, have reported improved sleep quality during the COVID-19 pandemic. Genta et al. (54) examined 94 high school students attending a private Rudolf Steiner Waldorf High School in Brazil and found that sleep quality improved during the COVID-19 pandemic, particularly among those with shorter sleep duration before the COVID-19 pandemic. While this study did not assess the pre-pandemic data retrospectively, its small sample size and lack of representativeness for adolescents in Brazil are notable limitations. The relatively high socioeconomic status in both Genta et al.'s sample and our cohort may partially explain the observed improvements. Similarly, Liu et al. (20) analyzed data from 1,619 Chinese preschoolers aged 4–6 years and reported higher sleep quality during the COVID-19 pandemic compared to a socio-demographically similar group of 436 preschoolers assessed in 2018. However, this study involved younger children than those in our cohort, and a key limitation was the lack of adjustment for potential confounders, which may have introduced bias. Together, these findings suggest that improved sleep quality in children during a pandemic period may be influenced by factors such as socioeconomic status and age. These results highlight the importance of clearly defining the study population, as certain demographic characteristics may play a crucial role in shaping sleep outcomes.
Our findings did not suggest substantial changes in sleep quality among parents during the COVID-19 pandemic (Table 4). In contrast, Olive et al. (30) reported decreased sleep quality in 2,365 Australian parents, while a systematic review and meta-analysis by Jahrami et al. (31) found an increased prevalence of sleep problems among adults globally during the COVID-19 pandemic, with prevalence rates varying by country. Notably, the prevalence in Germany aligned with the global prevalence ratio of ~35%. Similarly, Cui et al. (55) identified decreased sleep quality and increased sleep duration among adults in their meta-analysis, findings that were echoed by Alimoradi et al. (56) Silva et al. (32) further observed an association between parental and child sleep problems during the COVID-19 pandemic, though we did not adjust for child sleep problems in our analysis due to the unclear direction of this relationship. Kocevska et al. (57) highlighted the importance of pre-pandemic sleep patterns, noting an unexpected trend: individuals with pre-existing insomnia showed improved sleep quality during the COVID-19 pandemic, while those with good pre-pandemic sleep experienced a decline. Unlike many studies relying on retrospective pre-pandemic data or cross-sectional designs, our analysis incorporated longitudinal data using mixed models and up to four follow-up measurement points, which accounted for pre-pandemic sleep quality. This approach reduces potential biases and strengthens the causal interpretation of our findings. While numerous studies have reported adverse changes in adult sleep during the COVID-19 pandemic, methodological differences likely contribute to the variation in results. For example, Leone et al. (11) using a longitudinal study design, found no changes in sleep quality among adults (n = 1021) during the COVID-19 pandemic, consistent with our findings. Of note, our study examined the entire pandemic period in Germany, spanning ~2 years, whereas many studies focused specifically on the early confinement measures implemented in March 2020. This broader time frame may also explain the difference in findings.
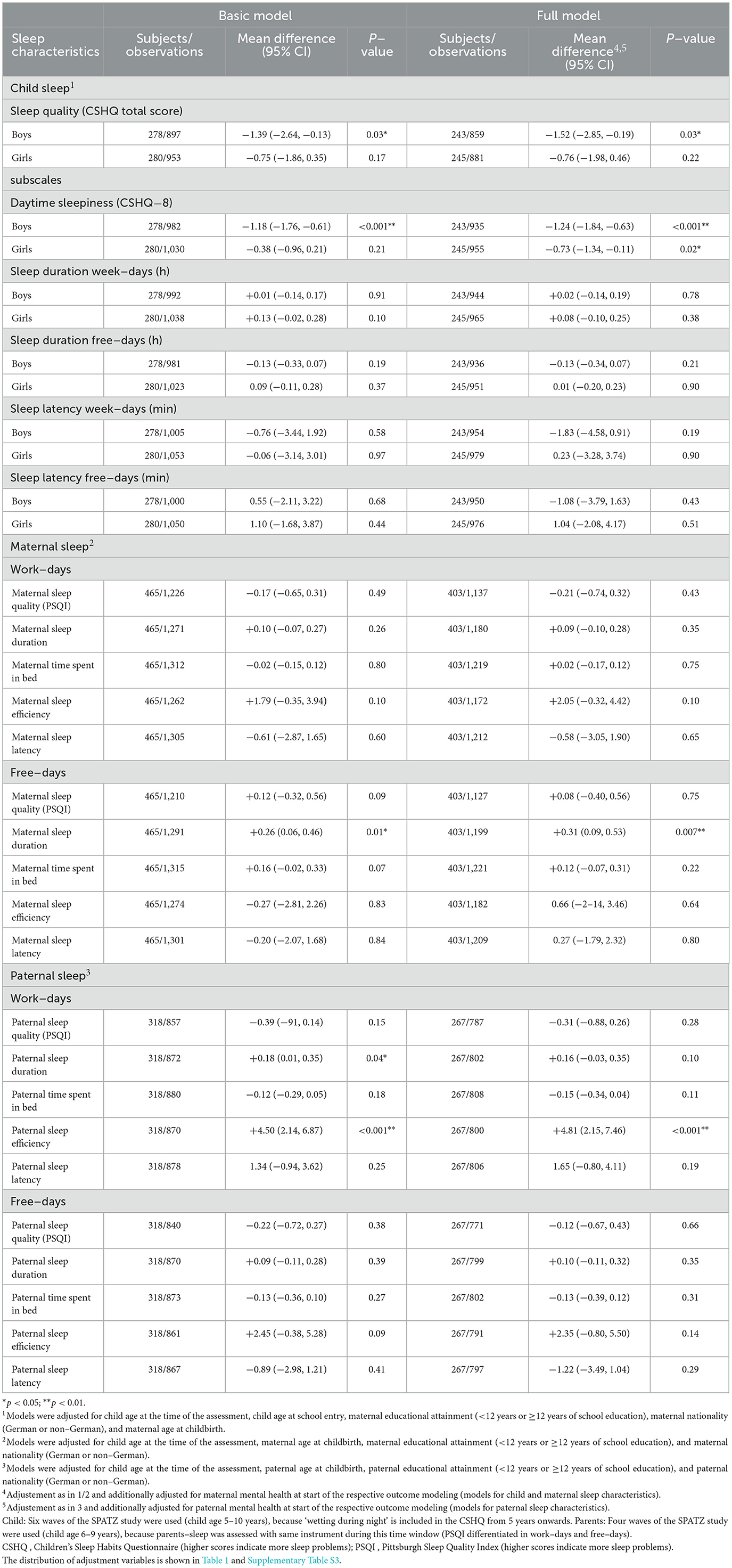
Table 4. Mean differences and 95% confidence intervals (CI) for sleep characteristics in children (by gender) and parents during the COVID−19 pandemic compared to pre– and post–pandemic periods.
Sleep duration
Our analysis indicated that sleep duration among children did not increase during the COVID-19 pandemic (Table 4). Similarly, Luchini et al. (58) reported no increase in sleep duration in their study of 528 children aged 4–12 years in the United States during the COVID-19 pandemic. However, Poirier et al. (18) found that among 28,307 Canadian adolescents, average sleep duration increased by 9.6 min between 2019 and 2022, alongside an increase in screen time by 129.2 min (95% CI: 120.5, 138.0). The differing age ranges of the study population may partly explain these contrasting findings. Additionally, while numerous studies have reported increased sleep duration among children and adolescents during the COVID-19 pandemic, (2, 4–10) our results did not align with this observation.
A multi-center study conducted in Bavaria, Germany, including 1,962 children (63.4% in primary schools and 36.6% in daycare centers), observed that children who experienced changes in sleep duration during the COVID-19 pandemic—whether an increase or decrease—reported worse health-related quality of life compared to those whose sleep duration remained stable (59). This finding aligns with numerous studies that have reported increased sleep duration during the COVID-19 pandemic accompanied by decreased sleep quality, which is often linked to mental health challenges. These observations are partially consistent with our findings among boys, where sleep duration remained unchanged, but sleep quality improved during the COVID-19 pandemic (Table 4).
We observed increased sleep duration among parents during the COVID-19 pandemic, specifically for mothers on weekends (difference in means +0.31 h; 95% CI 0.09, 0.53) and fathers on weekdays (difference in means +0.18 h; 95% CI 0.01, 0.35). These findings are consistent with numerous studies that have reported an increase in sleep duration among adults during the COVID-19 pandemic (11, 21, 60–62). However, results for adults remain mixed, as some studies found no change in sleep duration, (63, 64) while others reported divergent trends depending on work conditions—sleep duration increased with remote work and decreased for those continuing to work in person (65). Many studies, including ours, did not differentiate between these work settings. A further limitation of adult sleep studies is that large datasets often use time in bed as a proxy for actual sleep duration, which can lead to inaccuracies (61). For example, Hisler and Twenge (64) found no change in average sleep duration in a nationally representative sample of U.S. adults when comparing 2020 to 2018. However, they noted an increase in the prevalence of both shorter and longer sleep durations outside recommended ranges during the COVID-19 pandemic. Our analysis focused on intra-individual changes and predicted the mean of these changes, adjusted for covariates. While we identified increases in sleep duration among mothers on weekends and fathers on weekdays, our results do not exclude the possibility that these increases contributed to a higher prevalence of sleep durations falling outside the recommended ranges.
Daytime sleepiness
The reduction in daytime sleepiness observed among boys in this study may be linked to the delayed school start times during the COVID-19 pandemic, as later school start times have been shown to improve daytime sleepiness (66). This effect was also reported during the COVID-19 pandemic in a study of 45 Canadian adolescents (67).
Moreover, research has shown that daytime sleepiness is negatively associated with health related quality of life in schoolchildren (68). Our findings align with these observations to some extent. While boys experienced a significant reduction in daytime sleepiness during the COVID-19 pandemic, their health-related quality of life remained unchanged, as observed in a previous study of the same cohort (12, 17).
The results of our study, in conjunction with the research conducted by Maciel et al. (69) suggest that the implementation of flexible school start times may contribute to the enhancement of sleep characteristics in children and adolescents.
Correlations between sleep qualities in families
We did not observe a substantial correlation between maternal or paternal sleep quality and child sleep quality during the COVID-19 pandemic (Table 3). This contrasts with findings from Zreik et al. (70) who reported a strong association between maternal and child sleep. Specifically, mothers who reported improved sleep quality or longer sleep duration in their children during the COVID-19 pandemic were also more likely to experience a reduction in their own sleep problems. These findings are further supported by Tikotzky et al. (71) who demonstrated that maternal sleep is predictive of infant sleep during the first 6 months of life under non-pandemic conditions. As Zreik et al. studied children aged 0.5 to 6 years, and we found only a weak correlation between maternal and child sleep quality for 6 year old boys—an association that was no longer present when boys reached 8 years—it is possible that the relationship between maternal and child sleep diminishes as children grow older.
Mental health and sleep quality
In two earlier studies using the same cohort, we found that girls, but not boys, experienced poorer mental health during the COVID-19 pandemic compared to before (12, 17). This finding aligns with our observation of improved sleep quality among boys during the COVID-19 pandemic, suggesting that better sleep quality may have contributed to maintaining mental health in boys during this period. Improved sleep quality is causally linked to better mental health in adults (72), while increasing sleep disturbances are well-established risk factors for mental health issues (14). Conversely, poor mental health can also negatively affect sleep quality (45), highlighting the bidirectional and complex relationship between sleep and mental health, which may be further complicated during a pandemic (4, 21). In our cohort, the absence of poorer sleep quality among girls, despite their lower mental health, supports the hypothesis that sleep quality likely contributed to good mental health during the COVID-19 pandemic rather than being a consequence of it. If poor mental health were the primary driver of sleep disturbances, we would expect girls to exhibit worse sleep quality in this analysis.
We also identified a correlation between maternal mental health and boys' sleep quality at ages 5, 6 and 9 years, but this relationship was observed among girls at age 5 years (Supplementary Table S1). This suggests a possible gender difference in the associations between parental mental health and child sleep quality, although the direction of this association remains unclear. Additionally, we found strong correlations between parental sleep quality and their own mental health status (Supplementary Table S2), consistent with the bidirectional relationship between sleep and mental health (4, 21).
Additional adjustment for mental health in the analysis
Adjusting for pre-pandemic mental health did not substantially alter the associations between the COVID-19 pandemic and sleep characteristics, except for paternal sleep duration and girl's daytime sleepiness (Table 4).
After adjusting for the pre-pandemic HADS score (a summary score for mental health), the increase in sleep duration among fathers during the COVID-19 pandemic was no longer significant (Table 4). This suggests an inverse relationship between pre-pandemic HADS scores and sleep duration, as the model indicated that poorer pre-pandemic mental health (higher HADS scores) was associated with shorter sleep duration (data not shown). To explore this further, we stratified fathers based on their pre-pandemic HADS scores (<median vs. ≥ median, with a median HADS score of 7). Stratified analysis revealed that only fathers with good pre-pandemic mental health (HADS <7) experienced an increase in sleep duration during the COVID-19 pandemic (mean difference +0.22 h; 95% CI: 0.05, 0.40; p = 0.01), whereas fathers with HADS ≥ 7 showed no significant change (mean difference +0.13 h; 95% CI −0.15, 0.40; p = 0.36).
We observed reduced daytime sleepiness among girls during the COVID-19 pandemic, but only after adjusting for maternal pre-pandemic mental health. This adjustment likely reduced variability in the model and accounted for the positive association between maternal HADS scores and girls' daytime sleepiness observed in the analysis (data not shown). As such, the findings of reduced daytime sleepiness in girls' should be interpreted carefully, as they represent an association independent of maternal pre-pandemic mental health, and effect modification between pre-pandemic mental health and the COVID-19 pandemic cannot be ruled out.
Limitations
Our findings should be interpreted with caution given the study's limitations. First, the relatively small sample size limits statistical power and may affect the robustness of some associations. Second, our sample had a high proportion of families with mothers who had higher educational attainment at baseline. While this reflects the local population around a university city, families with lower educational attainment or migrant backgrounds were more likely to be lost to follow-up, particularly during the first year. Third, children's sleep quality was assessed using parent-proxy reports rather than self-reports. However, given that we adjusted for maternal mental health and found little to no association between parental sleep quality and child sleep quality, the use of a parent-proxy is unlikely to have introduced substantial bias, and the findings on children's sleep characteristics can be considered reliable. However, even though the CSHQ and PSQI are validated tools for assessing sleep quality, relying on self/parent-reported data may have introduced recall bias, affecting the accuracy of our findings. Moreover, our study did not include measurements of sleep characteristics by means of actigraphy, which could have introduced bias as we only relied on self-reported data on sleep characteristics. Further studies may validate reported sleep characteristics with a subsample of their study population using more objective measurements, such as actigraphy or daily sleep protocols. Another limitation is that our statistical model assumes no age-specific differences in the association between the pandemic and children's sleep characteristics across ages 7, 8 and 9 years. Effect modification by age was not tested, which could limit insights into potential age-related variability in pandemic effects.
Since our analysis treated the pandemic as a single event spanning 2 years, future research might consider multiple phases, such as the initial lockdown, phased reopening and vaccine rollout, if sample sizes allow. This would facilitate a deeper understanding of the pandemic and its associations with sleep health. Further, as our sample size was too small to divide the time before and after the pandemic into 'before' and 'after' time windows and compare these time windows separately with the time during the pandemic, our analysis is limited by this. Further research should aim to obtain more post-pandemic measurements in order to specifically explore the period after the pandemic compared to the period during the pandemic.
Moreover, as we considered the CHSQ and PSQI on a linear scale to explore potential associations between the COVID-19 pandemic and sleep quality, further research should also consider meaningful changes and clinically relevant thresholds for sleep quality.
Another limitation is that our analysis did not consider whether parents were working remotely or in person during the pandemic, even though this can influence changes to sleep duration during a pandemic.
The key strength of our study lies in its longitudinal design, which enabled the collection of routinely gathered data even during the unpredictable conditions of the COVID-19 pandemic. This design enhances the reliability of the findings and provides a valuable record of the possible associations of the pandemic with health of families and children in a natural experiment, as captured by the Ulm SPATZ Health study (73). As our analysis was exploratory rather than confirmatory, the results should be interpreted with caution. Further research involving specific hypothesis testing is necessary to gain a deeper understanding of the pandemic-related impact on sleep health.
Conclusion
Despite these limitations, our findings indicated that sleep quality of families did not generally decline during the COVID-19 pandemic compared to before and after the COVID-19 pandemic. However, we observed an increase in parental sleep duration, a decrease in daytime sleepiness among children, and an improvement in sleep quality among boys during this time. Further studies are required to assess the long-term implications of the pandemic on sleep characteristics, particularly among vulnerable groups or individuals with pre-existing mental health conditions.
Data availability statement
The datasets presented in this article are not readily available because the datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions regarding data protection issues and the study-specific consent text and procedure, but anonymized data are available from the corresponding author upon reasonable request. Supplementary results are available upon request. Requests to access the datasets should be directed to ZGVib3JhaC53ZXJuZWNrZUB1bmktdWxtLmRl.
Ethics statement
This study involving humans was approved by the ethics board of Ulm University (no. 311/11). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants or participants' legal guardians/next of kin.
Author contributions
DW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RP: Methodology, Software, Writing – review & editing. SB: Data curation, Project administration, Resources, Writing – review & editing. MZ: Methodology, Writing – review & editing. JG: Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – review & editing. DR: Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The Ulm SPATZ Health Study was funded through an unrestricted grant by the Medical Faculty of Ulm University, Ulm, Germany. These funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The contributing researchers are independent of the funders. None of the authors have financial relationships to disclose.
Acknowledgments
We thank the midwives, nurses, and obstetricians of the Department of Gynaecology and Obstetrics, University Medical Centre Ulm, the caring pediatricians, and the mothers and their families for their study support and participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1604195/full#supplementary-material
Abbreviations
CI, confidence interval; CSHQ, Children's Sleep Habits Questionnaire; FU, follow-up; h, hours; OR, odds ratio; PSQI, Pittsburgh Sleep Quality Index; SD, standard deviation; SPATZ, Ulm SPATZ Health Study; vs, versus.
References
1. Ramar K, Malhotra RK, Carden KA, Martin JL, Abbasi-Feinberg F, Aurora RN, et al. Sleep is essential to health: an American Academy of sleep Medicine position statement. J Clin Sleep Med. (2021) 17:2115–9. doi: 10.5664/jcsm.9476
2. Richter SA, Ferraz-Rodrigues C, Schilling LB, Camargo NF, Nunes ML. Effects of the COVID−19 pandemic on sleep quality in children and adolescents: a systematic review and meta-analysis. J Sleep Res. (2023) 32:e13720. doi: 10.1111/jsr.13720
3. Scarpelli S, Zagaria A, Ratti PL, Albano A, Fazio V, Musetti A, et al. Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: a systematic review, meta-analysis and meta-regression. Sleep Med. (2022) 100:89–102. doi: 10.1016/j.sleep.2022.07.012
4. Alfonsi V, Scarpelli S, Gorgoni M. COVID-19 and sleep disturbances: unraveling the connection. Brain Sci. (2024) 14:220. doi: 10.3390/brainsci14030220
5. Paterson DC, Ramage K, Moore SA, Riazi N, Tremblay MS, Faulkner G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: a scoping review of evidence after the first year. J Sport Health Sci. (2021) 10:675–89. doi: 10.1016/j.jshs.2021.07.001
6. Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. (2020) 17:85. doi: 10.1186/s12966-020-00987-8
7. Zhao J, Xu J, He Y, Xiang M. Children and adolescents' sleep patterns and their associations with mental health during the COVID-19 pandemic in Shanghai, China. J Affect Disord. (2022) 301:337–44. doi: 10.1016/j.jad.2021.12.123
8. Lim MTC, Ramamurthy MB, Aishworiya R, Rajgor DD, Tran AP, Hiriyur P, et al. School closure during the coronavirus disease 2019 (COVID-19) pandemic – Impact on children's sleep. Sleep Med. (2021) 78:108–14. doi: 10.1016/j.sleep.2020.12.025
9. Pfefferbaum B, Tucker P, Ekambaram V, Van Horn RL. Children's sleep and mental health during the COVID-19 Pandemic. Curr Psychiatry Rep. (2023) 25:847–56. doi: 10.1007/s11920-023-01475-z
10. Bussières EL, Malboeuf-Hurtubise C, Meilleur A, Mastine T, Hérault E, Chadi N, et al. Consequences of the COVID-19 pandemic on children's mental health: a meta-analysis. Front Psychiatry. (2021) 12:691659. doi: 10.3389/fpsyt.2021.691659
11. Leone MJ, Sigman M, Golombek DA. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. (2020) 30:R930–1. doi: 10.1016/j.cub.2020.07.015
12. Kurz D, Braig S, Genuneit J, Rothenbacher D. Trajectories of child mental health, physical activity and screen-time during the COVID-19 pandemic considering different family situations: results from a longitudinal birth cohort. Child Adolesc Psychiatry Ment Health. (2023) 17:36. doi: 10.1186/s13034-023-00581-3
13. Ravens-Sieberer U, Kaman A, Erhart M, Devine J, Schlack R, Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry. (2021) 31:1–11. doi: 10.1007/s00787-021-01726-5
14. Ng CSM, Ng SSL. Impact of the COVID-19 pandemic on children's mental health: a systematic review. Front Psychiatry. (2022) 13:975936. doi: 10.3389/fpsyt.2022.975936
15. Fortuna LR, Brown IC, Lewis Woods GG, Porche MV. The impact of COVID-19 on anxiety disorders in youth. Child Adolesc Psychiatr Clin N Am. (2023) 32:531–42. doi: 10.1016/j.chc.2023.02.002
16. Hossain MM, Nesa F, Das J, Aggad R, Tasnim S, Bairwa M, et al. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: an umbrella review. Psychiatry Res. (2022) 317:114814. doi: 10.1016/j.psychres.2022.114814
17. Kurz D, Braig S, Genuneit J, Rothenbacher D. Lifestyle changes, mental health, and health-related quality of life in children aged 6–7 years before and during the COVID-19 pandemic in South Germany. Child Adolesc Psychiatry Ment Health. (2022) 16:20. doi: 10.1186/s13034-022-00454-1
18. Poirier K, Gauvin L, Haddad S, Bélanger RE, Leatherdale ST, Turcotte-Tremblay AM. Evolution of sleep duration and screen time between 2018 and 2022 among canadian adolescents: evidence of drifts accompanying the COVID-19 pandemic. J Adolesc Health. (2024) 74:980-988. doi: 10.1016/j.jadohealth.2023.12.023
19. López-Bueno R, López-Sánchez GF, Casajús JA, Calatayud J, Gil-Salmerón A, Grabovac I, et al. Health-related behaviors among school-aged children and adolescents during the spanish covid-19 confinement. Front Pediatr. (2020) 8:573. doi: 10.3389/fped.2020.00573
20. Liu Z, Tang H, Jin Q, Wang G, Yang Z, Chen H, et al. Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J Sleep Res. (2021) 30:e13142. doi: 10.1111/jsr.13142
21. Neculicioiu VS, Colosi IA, Costache C, Sevastre-Berghian A. Clichici S. Time to Sleep?—A review of the impact of the COVID-19 pandemic on sleep and mental health. Int J Environ Res Public Health. (2022) 19:3497. doi: 10.3390/ijerph19063497
22. Nelson KL, Davis JE, Corbett CF. Sleep quality: an evolutionary concept analysis. Nurs Forum (Auckl). (2022) 57:144–51. doi: 10.1111/nuf.12659
23. Bacaro V, Chiabudini M, Buonanno C, De Bartolo P, Riemann D, Mancini F, et al. Insomnia in the Italian population during covid-19 outbreak: a snapshot on one major risk factor for depression and anxiety. Front Psychiatry. (2020) 11:579107. doi: 10.3389/fpsyt.2020.579107
24. Peltz JS, Daks JS, Rogge RD. COVID-related stressors and their impact on parental sleep, parenting behaviors, and child functioning. J Fam Psychol. (2023) 37:305–17. doi: 10.1037/fam0001061
25. Ballesio A, Zagaria A, Musetti A, Lenzo V, Palagini L, Quattropani MC, et al. Longitudinal associations between stress and sleep disturbances during COVID-19. Stress Health J Int Soc Investig Stress. (2022) 38:919–26. doi: 10.1002/smi.3144
26. Zhan N, Zhang Y, Xie D, Geng F. The associations of parental COVID-19 related worries, lifestyles, and insomnia with child insomnia during the COVID-19 outbreak. J Sleep Res. (2022) 31:e13590. doi: 10.1111/jsr.13590
27. Lopez-Iracheta R, Moreno-Galarraga L, Moreno-Villares JM, Bueso-Asfura OE, Martinez-Gonzalez MA, Martin-Calvo N. The effects of covid-19 lockdown on the sleep quality of children. Children. (2023) 10:944. doi: 10.3390/children10060944
28. Cai H, Chen P, Jin Y, Zhang Q, Cheung T, Ng CH, et al. Prevalence of sleep disturbances in children and adolescents during COVID-19 pandemic: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. (2024) 14:12. doi: 10.1038/s41398-023-02654-5
29. Pang JCY, Chan ELS, Lau HMC, Reeves KKL, Chung THY, Hui HWL, et al. The impacts of physical activity on psychological and behavioral problems, and changes in physical activity, sleep and quality of life during the COVID-19 pandemic in preschoolers, children, and adolescents: a systematic review and meta-analysis. Front Pediatr. (2023) 11:1015943. doi: 10.3389/fped.2023.1015943
30. Olive LS, Sciberras E, Berkowitz TS, Hoare E, Telford RM, O'Neil A, et al. Child and parent physical activity, sleep, and screen time during covid-19 and associations with mental health: implications for future psycho-cardiological disease? Front Psychiatry. (2022) 12:774858. doi: 10.3389/fpsyt.2021.774858
31. Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. (2021) 17:299–313. doi: 10.5664/jcsm.8930
32. Wearick-Silva LE, Richter SA, Viola TW, Nunes ML. Sleep quality among parents and their children during COVID-19 pandemic. J Pediatr (Rio J). (2022) 98:248–55. doi: 10.1016/j.jped.2021.07.002
33. Logan C, Zittel T, Striebel S, Reister F, Brenner H, Rothenbacher D, et al. Changing Societal and Lifestyle Factors and Breastfeeding Patterns Over Time. Pediatrics. (2016) 137:e20154473–e20154473. doi: 10.1542/peds.2015-4473
34. Schlarb AA, Schwerdtle B, Hautzinger M. Validation and psychometric properties of the German version of the Children's Sleep Habits Questionnaire (CSHQ-DE). Somnologie - Schlafforschung Schlafmed. (2010) 14:260–6. doi: 10.1007/s11818-010-0495-4
35. Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. (2000) 23:1043–51.
36. Phillips SR, Johnson AH, Shirey MR, Rice M. Sleep Quality in School-Aged Children: A Concept Analysis. J Pediatr Nurs. (2020) 52:54–63. doi: 10.1016/j.pedn.2020.02.043
37. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
38. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. (2002) 53:737–40. doi: 10.1016/S0022-3999(02)00330-6
39. Pilz LK, Keller LK, Lenssen D, Roenneberg T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep. (2018) 41:10.1093/sleep/zsy029. doi: 10.1093/sleep/zsy029
40. Reis C, Pilz LK, Keller LK, Paiva T, Roenneberg T. Social timing influences sleep quality in patients with sleep disorders. Sleep Med. (2020) 71:8–17. doi: 10.1016/j.sleep.2020.02.019
41. Herrmann C. International experiences with the hospital anxiety and depression scale-a review of validation data and clinical results. J Psychosom Res. (1997) 42:17–41. doi: 10.1016/S0022-3999(96)00216-4
42. Petermann F. Hospital anxiety and depression scale, deutsche version (HADS-D). Z Für Psychiatr Psychol Psychother. (2011) 59:251–3. doi: 10.1024/1661-4747/a000077
43. Hermann-Lingen C, Buss U, Snaith R. Hospital Anxiety and Depression Scale-Deutsche Version (HADS-D). 3rd Ed. Bern: Hans-Huber. (2011).
44. Hinz A, Schwarz R. Angst und Depression in der Allgemeinbevölkerung - Eine Normierungsstudie zur hospital anxiety and depression scale -. PPmP - Psychother · Psychosom · Med Psychol. (2001) 51:193–200. doi: 10.1055/s-2001-13279
45. Wallace DD, Boynton MH, Lytle LA. Multilevel analysis exploring the links between stress, depression, and sleep problems among two-year college students. J Am Coll Health. (2017) 65:187–96. doi: 10.1080/07448481.2016.1269111
46. Groenwold RHH, Klungel OH, Grobbee DE, Hoes AW. Selection of confounding variables should not be based on observed associations with exposure. Eur J Epidemiol. (2011) 26:589–93. doi: 10.1007/s10654-011-9606-1
47. VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. (2019) 34:211–9. doi: 10.1007/s10654-019-00494-6
48. Andruskiene J, Varoneckas G, Martinkenas A, Grabauskas V. Factors associated with poor sleep and health-related quality of life. Med Kaunas Lith. (2008) 44:240–6.
49. Greenland S. Quantifying biases in causal models: classical confounding vs collider-stratification bias.Epidemiology. (2003) 14:300–306. doi: 10.1097/01.EDE.0000042804.12056.6C
50. El Rafihi-Ferreira R, Lewis KM, McFayden T, Ollendick TH. Predictors of nighttime fears and sleep problems in young children. J Child Fam Stud. (2019) 28:941–9. doi: 10.1007/s10826-019-01332-9
51. McDonald L, Wardle J, Llewellyn CH, Van Jaarsveld CHM, Fisher A. Predictors of shorter sleep in early childhood. Sleep Med. (2014) 15:536–40. doi: 10.1016/j.sleep.2014.01.005
52. Bruni O, Malorgio E, Doria M, Finotti E, Spruyt K, Melegari MG, et al. Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Med. (2021) 2021:S1389945721000940. doi: 10.1016/j.sleep.2021.02.003
53. Dondi A, Fetta A, Lenzi J, Morigi F, Candela E, Rocca A, et al. Sleep disorders reveal distress among children and adolescents during the Covid-19 first wave: results of a large web-based Italian survey. Ital J Pediatr. (2021) 47:130. doi: 10.1186/s13052-021-01083-8
54. Genta FD, Rodrigues Neto GB, Sunfeld JPV, Porto JF, Xavier AD, Moreno CRC, et al. COVID-19 pandemic impact on sleep habits, chronotype, and health-related quality of life among high school students: a longitudinal study. J Clin Sleep Med. (2021) 17:1371–7. doi: 10.5664/jcsm.9196
55. Cui D, Zhang X, Guo J. The impact of the COVID-19 pandemic on physical activity and sleep among healthy adults: a systematic review and meta-analysis. Front Psychol. (2023) 14:1149215. doi: 10.3389/fpsyg.2023.1149215
56. Alimoradi Z, Gozal D, Tsang HWH, Lin C-Y, Broström A, Ohayon MM, et al. Gender-specific estimates of sleep problems during the COVID-19 pandemic: systematic review and meta-analysis. J Sleep Res. (2022) 31:e13432. doi: 10.1111/jsr.13432
57. Kocevska D, Blanken TF, Van Someren EJW, Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. (2020) 76:86–8. doi: 10.1016/j.sleep.2020.09.029
58. Lucchini M, Bekelman TA, Li M, Knapp EA, Dong Y, Ballard S, et al. Impact of the COVID-19 pandemic on children's sleep habits: an ECHO study. Pediatr Res. (2023) 93:586–94. doi: 10.1038/s41390-022-02309-z
59. Schillok H, Coenen M, Rehfuess EA, Zimmermann J, Gensichen J, von Schrottenberg V et al. Changes in behavior and quality of life in German young children during the COVID-19 pandemic—results from the COVID kids bavaria study. Front Pediatr. (2023) 11:1135415. doi: 10.3389/fped.2023.1135415
60. Barbouzas AE, Malli F, Daniil Z, Gourgoulianis K. Long-term impact of COVID-19 pandemic in sleep quality and lifestyle in young adults. Int J Environ Res Public Health. (2022) 19:12333. doi: 10.3390/ijerph191912333
61. Yuan RK, Zitting KM, Maskati L, Huang J. Increased sleep duration and delayed sleep timing during the COVID-19 pandemic. Sci Rep. (2022) 12:10937. doi: 10.1038/s41598-022-14782-x
62. Rezaei N, Grandner MA. Changes in sleep duration, timing, and variability during the COVID-19 pandemic: large-scale Fitbit data from 6 major US cities. Sleep Health. (2021) 7:303–13. doi: 10.1016/j.sleh.2021.02.008
63. Robillard R, Dion K, Pennestri M, Solomonova E, Lee E, Saad M, et al. Profiles of sleep changes during the COVID-19 pandemic: demographic, behavioural and psychological factors. J Sleep Res. (2021) 30:e13231. doi: 10.1111/jsr.13231
64. Hisler GC. Twenge JM. Sleep characteristics of US adults before and during the COVID-19 pandemic. Soc Sci Med. (2021) 276:113849. doi: 10.1016/j.socscimed.2021.113849
65. Conroy DA, Hadler NL, Cho E, Moreira A, MacKenzie C, Swanson LM, et al. The effects of COVID-19 stay-at-home order on sleep, health, and working patterns: a survey study of US health care workers. J Clin Sleep Med. (2021) 17:185–91. doi: 10.5664/jcsm.8808
66. Minges KE, Redeker NS. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med Rev. (2016) 28:86–95. doi: 10.1016/j.smrv.2015.06.002
67. Gruber R, Saha S, Somerville G, Boursier J, Wise MS. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. (2020) 76:33–5. doi: 10.1016/j.sleep.2020.09.015
68. Gustafsson M, Laaksonen C, Aromaa M, Asanti R, Heinonen OJ, Koski P, et al. Association between amount of sleep, daytime sleepiness and health-related quality of life in schoolchildren. J Adv Nurs. (2016) 72:1263–72. doi: 10.1111/jan.12911
69. Maciel GP, De Camargo R, Lopes MVV, de Oliveira BN, da Costa BGG, Chaput JP, et al. Sleep among Brazilian adolescents before and after the COVID-19 pandemic: repeated cross-sectional and longitudinal analyses. BMC Pediatr. (2025) 25:541. doi: 10.1186/s12887-025-05904-1
70. Zreik G, Asraf K, Haimov I, Tikotzky L. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. (2021) 30:e13201. doi: 10.1111/jsr.13201
71. Tikotzky L, Sadeh A, Volkovich E, Manber R, Meiri G, Shahar G. Infant sleep development from 3 to 6 months postpartum: links with maternal sleep and paternal involvement. Monogr Soc Res Child Dev. (2015) 80:107–24. doi: 10.1111/mono.12147
72. Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. doi: 10.1016/j.smrv.2021.101556
Keywords: Children's Sleep Habits Questionnaire (CSHQ), COVID-19 pandemic, school-aged children, longitudinal data, families, Pittsburgh Sleep Quality Index (PSQI), sleep quality
Citation: Wernecke D, Peter RS, Braig S, Zarco M, Genuneit J and Rothenbacher D (2025) Longitudinal associations between the COVID-19 pandemic and sleep characteristics in children and parents. Front. Public Health 13:1604195. doi: 10.3389/fpubh.2025.1604195
Received: 01 April 2025; Accepted: 25 August 2025;
Published: 25 September 2025.
Edited by:
Anikó Lovik, Leiden University, NetherlandsReviewed by:
Mustafa Kursat Sahin, Ondokuz Mayis University, TürkiyeAlicia Nevriana, Karolinska Institutet (KI), Sweden
Juan González Hijón, Université libre de Bruxelles, Belgium
Copyright © 2025 Wernecke, Peter, Braig, Zarco, Genuneit and Rothenbacher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deborah Wernecke, ZGVib3JhaC53ZXJuZWNrZUB1bmktdWxtLmRl
†These authors have contributed equally to this work
‡ORCID: Deborah Wernecke orcid.org/0000-0002-6934-9257
 Deborah Wernecke
Deborah Wernecke Raphael S. Peter1
Raphael S. Peter1 Stefanie Braig
Stefanie Braig Jon Genuneit
Jon Genuneit Dietrich Rothenbacher
Dietrich Rothenbacher