- 1Department of Emergency, The First People's Hospital of Yunnan Province, The Affiliated Hospital of Kunming University of Science and Technology, Kunming, China
- 2Department of Emergency, Yunnan Provincial Hospital of Traditional Chinese Medicine, The First Affiliated Hospital of Yunnan University of Traditional Chinese Medicine, Kunming, China
- 3Department of Hematology, The First People’s Hospital of Yunnan Province, Affiliated Hospital of Kunming University of Science and Technology, Kunming, China
- 4Yunnan Province Clinical Research Center for Hematologic Disease, The First People’s Hospital of Yunnan Province, Kunming, China
- 5Yunnan Provincial Clinical Medical Center for Blood Diseases and Thrombosis Prevention and Treatment, The First People’s Hospital of Yunnan Province, Kunming, China
- 6Yunnan Atherosclerosis Cooperation Base of Chinese and Western Medicine, The First People’s Hospital of Yunnan Province, Kunming, China
Global climate change, urbanization, and environmental pollution have significantly altered the ecosystem and socio-economic structure, while also promoting a new disease risk pattern that has markedly affected human physical and mental health, increasing the complexity and uncertainty of disease control and prevention. This review aims to summarize the correlation between unique public health vulnerabilities and disease distribution in different regions of China by investigating the national and regional personalized response strategies and research progress.
Introduction
China is located in East Asia, with a vast territory, a complex geographical environment, diverse climate types, and significant altitude differences. It is not only challenging to immediately restore equilibrium when the complex ecosystem composition is altered by extreme weather, air pollution, globalization, and other correlated factors, but it also has major repercussions, particularly the dynamic evolution of the illness spectrum. The typical ecosystem vulnerability characteristics include three dimensions: sensitivity, exposure, and adaptability. An imbalance in any of these dimensions negatively affects the system’s vulnerability. China has unique topography and landforms (the frozen Qinghai-Tibet Plateau, the towering Himalayas, the arid Tarim Basin, and the fertile Northeast Plain of China) and water distribution (the Yangtze and the Yellow Rivers), which establishes the foundation for disease distribution (1–4). Furthermore, climate differences and changes substantially affect the temporal and spatial scope of vector-borne diseases (5). Moreover, the industrialization and urbanization of emerging economies have exacerbated pollution problems (6), reduced the burden of some diseases, and promoted the prevalence of chronic diseases and environmental health risks. Comprehensive evaluation of globalization, particularly its association with the Southwestern border and Southeast Asia, as well as coastal ports such as Guangdong, China, has been under constant pressure due to the emergence of infectious diseases from other countries and cross-regional transmission. It has also increased the risk of infectious disease outbreaks (7–9). Although technological progress is crucial for disease prevention and control, it has several challenges, such as drug resistance and biosafety (10, 11). The significant changes in China’s ecosystem and socioeconomic structure have profoundly influenced the spread and distribution of diseases, forming a unique regional health risk pattern, indirectly making health issues particularly prominent.
Several epidemiological studies have shown that the causes of diseases are no longer simple and are often closely related to complex extreme weather events (such as heavy rain, high temperature, floods, cyclones, hurricanes, etc.). This can increase the incidence and mortality rates of acute and chronic diseases, as well as accelerate the incidence of severe mental health conditions (12, 13). In recent years, air pollution has caused > 1 million deaths in China each year (14), and some infectious diseases have re-emerged or even increased in certain regions (15). For instance, SARS-CoV-2 was first discovered in Wuhan in late 2019, then spread rapidly throughout China and worldwide (16). The Chikungunya virus was first discovered in Africa in 1952, and since then has caused unexpected large-scale outbreaks in Africa, Asia, Europe, and the Americas, becoming a major global health issue. On July 8, 2025, a local outbreak of Chikungunya fever was monitored in Shunde District, Foshan City, Guangdong Province, caused by an imported case.1 As of 24:00 on July 26, 2025, Guangdong Province reported 2,940 local cases of Chikungunya fever.2 Extreme weather events not only affect China, but also other developed countries like the United States. In 2020, the United States experienced 22 such events, with annual losses reaching 1 billion US dollars (17). The United Nations report (18) states that global climate change is currently the most urgent common concern. In addition to becoming the subject of international public health concern, disease and health issues are also a significant factor in China’s rapid development. The “Healthy China 2030 Strategy” guides China’s health care development, aiming to comprehensively improve the health level of the entire population and promote the coordinated development of health, economy, and society (19). To create a more sustainable and resilient society, address the challenges posed by climate change, and understand the ambitious goal of universal and global health, it is imperative to fully integrate various resources, overcome governance bottlenecks, and develop individualized and reasonable long-term strategic decisions and response measures by comprehensively understanding the characteristics of climate vulnerability and disease distribution in recent years.
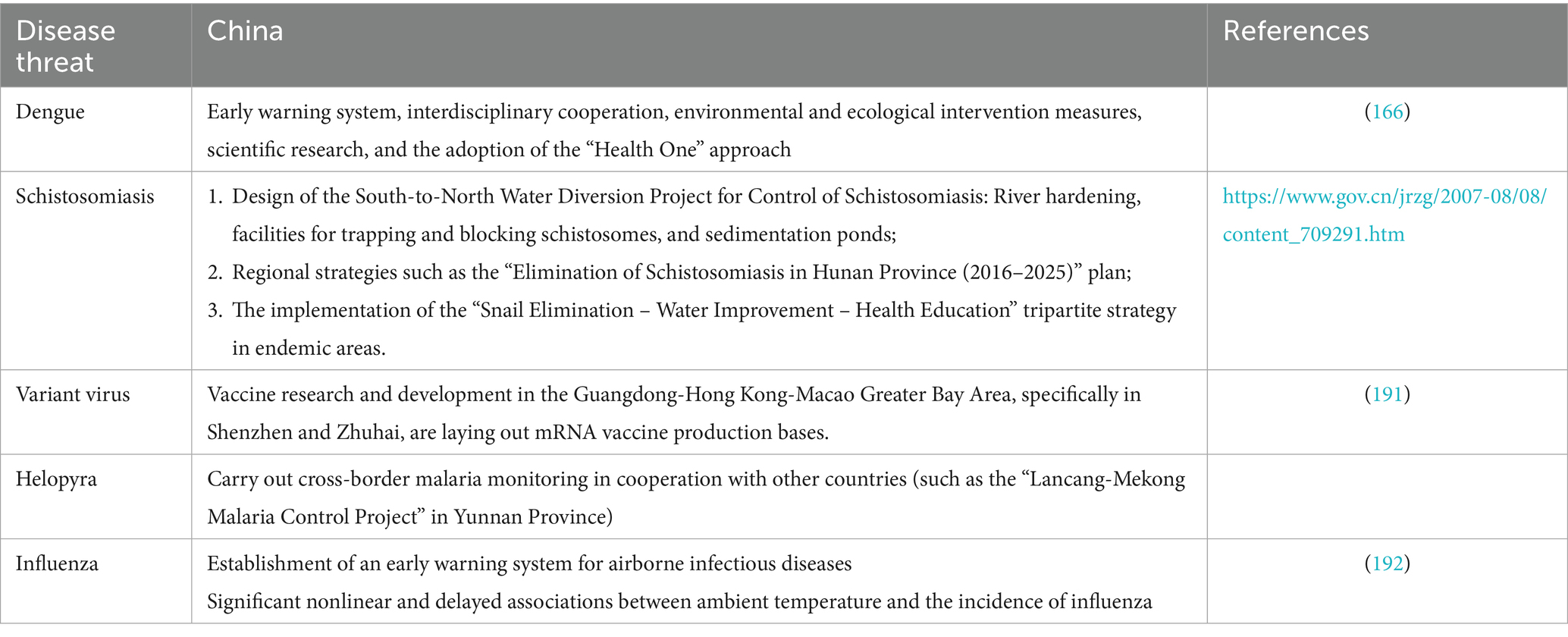
There are significant regional differences in the many component characteristics associated with extreme climate events like droughts, wildfires, and floods, including the primary categories of catastrophes and the financial losses and mortality costs (20). Geospatial analysis indicates that certain regions are particularly prone to specific types of disasters. Factors such as terrain, local climate, and population density have a significant impact on the location where disasters occur (21). China is now one of the countries that are most frequently hit by disasters because of its varied temperature zones, complicated geographic setting, significant urban–rural divides, and delicate ecosystems (22). Therefore, the seven major regions of China (Northeast Region, North China Region, Central China Region, East China Region, South China Region, Southwest Region, and Northwest Region) may experience different issues related to ecosystem vulnerability, indicating health problems and economic losses. This study summarizes the representative cases of systemic vulnerability in public health issues in the seven central regions of China, as well as the common problems that exist in some areas of the country, to provide practical and feasible suggestions and measures. It also summarizes some strategic measures for each region and highlights China’s experience through particular implementation cases. By lowering exposure risk factors at their source, the goal is to control the incidence of illnesses successfully. The findings can provide a guideline to prevent and control systemic vulnerability diseases worldwide.
Search strategy and selection criteria
For this review, PubMed was employed to search English articles published between 2000 and 2025. The search terms included combinations of “China” or “Northeast region” or “North China region” or “Central China region” or “East China region” or “South China region” or “Southwest region” or “Northwest region,” “system vulnerability” or “natural disasters” or “globalization” or “air pollution” or “ecosystem” or “extreme weather events,” “infectious diseases” or “chronic diseases” or “mental disorders” or “health issues,” “response strategies” or “strategic measures.” Furthermore, websites from different regions in China were also searched using Xinhuanet. Moreover, the official websites of various regions were investigated for data on “extreme weather events,” “natural disasters,” “infectious diseases,” and “response strategies.”
Vulnerability of China’s regional system
China is separated into seven geographical regions based on its different characteristics, resource distribution, and economic development, including the regions of Northeast, North, Central, East, South, Southwest, and Northwest China. Diseases in different regions have different characteristics. The vertical distribution ranges from the plain areas below 500 meters above sea level to the Qinghai-Tibet Plateau with an average altitude of over 4,000 meters, spanning the Tarim Basin, Junggar Basin, Qaidam Basin, and Sichuan Basin. The distinctive regional diseases with Chinese characteristics are determined by the karst, Danxia, Yardang, and volcanic landforms found there (Figure 1).
1. Northeast China (118°-135°05′E, 38°-53°33′N): including Heilongjiang, Jilin, Liaoning, and eastern Inner Mongolia, with mainly plain terrain and a cold climate, is China’s substantial agricultural and heavy industry base. The local cold climate and agrarian production mode determine the distribution characteristics of the disease in this area
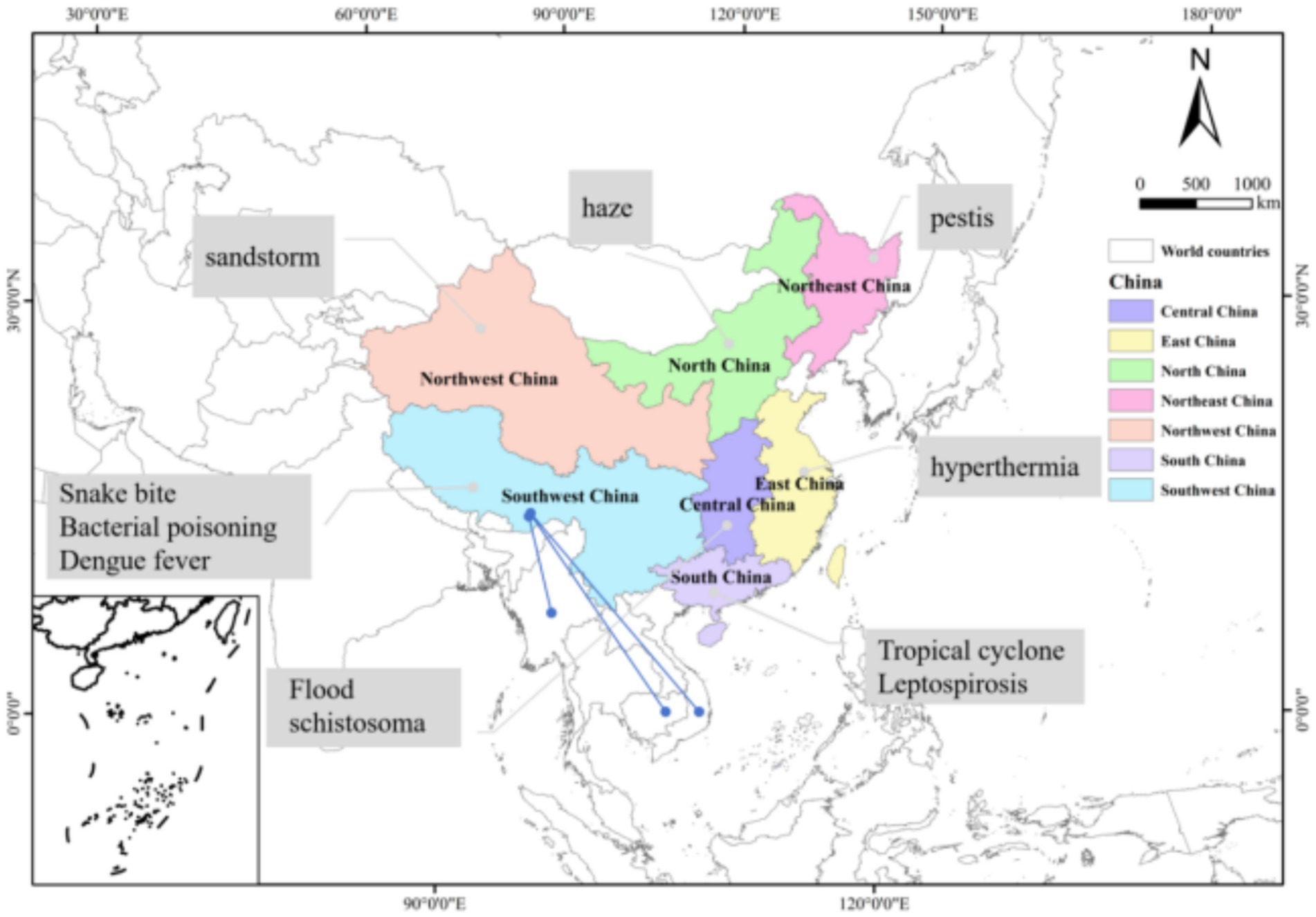
Figure 1. The seven geographical regions of China are represented by different colors. Each region’s representative system vulnerability and disease conditions are marked, respectively (It indicates the interaction of animal-borne diseases between southwest China and neighboring countries).
In Northeast China, greenhouse cultivation, indoor fuel combustion, and outdoor straw burning are the main production and living methods (23). The resultant environmentally persistent free radicals (EPFRs) (24) are considered the major risk factors for respiratory diseases, such as chronic obstructive pulmonary disease (COPD). A recent study revealed that COPD has a relatively high prevalence in Northeast China on a national scale (25). Furthermore, solid fuel combustion increased the risk of lung cancer (26). The primary strategies for preventing disease depend on the disease’s exposure factors. Residents’ lifestyles are altered and their living conditions are improved by pertinent public health laws and policies, such as the use of biogas in place of coal and the burning of straw (27). The government places a strong emphasis on addressing the health issues caused by COPD. China has made it a goal to lower the death rate associated with COPD and other chronic respiratory diseases among individuals under 70 to 8.1/100,000 or fewer by 2030. The “Implementation Plan for the Prevention and Control of Chronic Respiratory Diseases” was released concurrently by the relevant departments, which calls for actively reducing the COPD risk factors, enhancing the prevention and control system, standardizing the diagnosis and treatment procedure, and improving support for comprehensive guarantees and scientific research. Coal use has declined, car emissions have been successfully managed, and nitrogen deposition in Northeast China has significantly decreased thanks to the tireless efforts of the government and everyone else, as well as because of the change in agricultural methods (28).
Inner Mongolia is home to a world-renowned dairy cluster and a well-developed livestock industry. It is the nation’s top producer of wool and mutton. Although the industry sector is expanding, it has promoted certain disease-related issues. Human brucellosis is most common in Inner Mongolia and the provinces or autonomous regions that surround it (29, 30). Large-scale sheep farming, frequent animal trading, cross-regional circulation of dairy products, and a weak grassroots epidemic prevention system all increase the risk of brucellosis transmission and resurgence. Strengthening personal protection, early detection, and early treatment can effectively control the trend of brucellosis (31).
Plague is a zoonotic disease that spreads through fleas and is transmitted by rodents carrying the pathogen (32). Historically, it has caused three major pandemics, resulting in over 200 million deaths (33). There are indications that the prevalence of plague is increasing in the Americas, Asia, and Africa as a result of climate change (34). The Siberian marmot (Marmota sibirica) is widely distributed in the grasslands of Northeast China (35), whereas the Marmota himalayana is widely distributed in the Qinghai-Tibet Plateau (QTP) (33); these two together form the largest natural infection area in China. The literature has indicated that plague spreads faster in areas with low population density and a high proportion of grassland or forest (36). Furthermore, the warming trend in the QTP region (37) and the developed tourism industry (38) further increase the risk of plague transmission. Some studies have indicated that an increase of 1 °C in spring temperature elevates the risk of pathogen infection in gerbils by 59% (39). Further, heavy rainfall also increases the risk of plague transmission (40). Various fleas can survive in the Alxa Desert in Inner Mongolia, China, which is a typical arid region of Asia with a hot, dry climate. Fleas are the primary carriers of various zoonotic diseases and frequently parasitize rodents (22, 41). Therefore, novel strategies are required for the prevention and control of diseases like plague.
2 North China (110.22°-119.85°E, 34.58°-42.37°N): covers Beijing, Tianjin, Hebei, Shanxi, and central Inner Mongolia, has diverse terrain and a temperate monsoon climate, and is the political and cultural center of China
In China, non-communicable illnesses have progressively become the major cause of early mortality and disability (41), with air pollution listed as one of the four major risk factors. In recent years, the environment, human health, and economy have all suffered due to deteriorating dust weather in northern China. The number of cross-border sandstorms from Mongolia to China has been increasing from 1987 to 2022 (42). The concentration of PM10 (particles with a diameter of less than 10 μm) in Beijing increased to over 7,000 μg M-3 on March 15, 2021, due to a super sandstorm (43). Furthermore, the spring of 2023 had the highest frequency of spring dust weather in the previous 10 years due to a protracted sandstorm outbreak caused by the cold front of the Mongolian cyclone and the dust source area (44). Sandstorms have oxidation potential (OP) and EPFR, inducing oxidative stress. They are closely related to the incidence of circulatory system disorders (45–47) and respiratory system diseases (48). Moreover, the incidence of hospitalization among patients was significantly correlated with exposure to sandstorms (49). Moreover, recent studies have discovered that exposure to PM2.5 directly induces nephrotoxicity, which is linked to five different forms of kidney disorders (50). A meta-analysis indicated that PM2.5 exposure is significantly associated with liver dysfunction, chronic liver diseases, liver cancer, and colorectal cancer (51), as well as an increase in the incidence of lung cancer (52). In addition to threatening the environment and public health in northern China, sandstorms are progressively spreading to the center and southern parts of the country, endangering the environment and public health worldwide, and 150 nations have been directly impacted thus far (53). Despite the initiatives proposed by the United Nations, it is still influenced by various factors. Therefore, international cooperation and multidisciplinary health research are still needed.
As China’s economy expanded quickly, a significant increase was observed in air pollution between 2012 and 2017. The green finance index of Liaoning experienced extreme smog pollution, and the Beijing-Tianjin-Hebei region exhibited an overall negative trend between 2010 and 2017 (54). Smog not only has a significant negative impact on the economy and society, but also poses a considerable threat to people’s health.
Urban greening is a valuable strategy that is being employed to reduce the premature mortality rate caused by non-communicable diseases by one-third by 2030. Green spaces can alleviate environmental pollution, restore energy consumption of the body, and help people build health capabilities (55). A systematic study revealed a positive association between green spaces and mental health, cardiovascular outcomes, and overall health (56).
3 Central China (108°21′-116°39′E, 24°38′-36°22′N): includes Henan, Hubei, and Hunan provinces, has plain and hilly terrain, developed water systems, and is an important agricultural and industrial base in China
Floods have become more frequent and longer in duration due to global warming, which has had a negative influence on China’s social and economic structure as well as the health of the environment. The most catastrophic disaster since 1998 occurred in 2016, when the Yangtze River Basin experienced a devastating flood brought on by the El Niño phenomenon.
Hunan Province in China is regarded as one of the provinces most severely affected by floods in recent years (57). Water-borne illnesses include bacillary dysentery, cholera, and typhoid/paratyphoid. The risk of disease transmission rises when floodwaters contaminate drinking water (58). A study found that after the flash flood and waterlogging in Changsha City, the incidence of typhoid/paratyphoid and bacillary dysentery, which are related to intestinal infections, increased. The higher the level of storm floods, the higher the risk of disease outbreaks (59).
The saying “The danger of the Yangtze River lies in Jingjiang” refers to the distinctive geographic setting of the Jingjiang stretch of the Yangtze River in Hubei Province, which has historically been vulnerable to recurrent floods. In 2016, 20.8 million people in Hubei Province were impacted by the flood (60). Floods not only cause direct losses to people and facilities but also increase the risk of new infectious diseases. Hemorrhagic fever with renal syndrome (HFRS) is a zoonotic disease mainly transmitted by rodents carrying the Hantavirus (61). Previous literature suggests a positive correlation between hydrological conditions and the incidence of HFRS (62). According to some studies, HFRS will be a major threat to mainland China during the 21st century, particularly in the country’s northeast, east, and center. Furthermore, since the rodent population density may increase after floods, the risk of HFRS in low-altitude and flat terrain locations close to rivers should be assessed, and short-term HFRS preventative strategies should be formulated (60).
Schistosomiasis is a disease transmitted through the intermediate host, the Oncomelania snail (63). Although it has been successfully managed through extensive preventative and control methods, the central China region (Dongting Lake, Poyang Lake) has found it extremely challenging to prevent and control schistosomiasis due to the regular occurrence of floods (64). Comprehensive transformation of agriculture, water conservancy, forestry, health, and the environment is beneficial for the prevention and control of schistosomiasis (65). Of them, controlling the water levels at the Three Gorges Dam (TGD) to limit the population of Oncomelania snails has been considered a successful and effective case, as it has considerably decreased the snails’ density, infection rate, and potential for human interaction with (66).
4 East China (113.55°-122.87°E, 21.9°-38.32°N): It covers Shandong, Jiangsu, Anhui, Shanghai, Zhejiang, Jiangxi, Fujian, and Taiwan. The terrain is mainly hilly, with basins and plains. The climate is diverse, and the economy is developed
The increase in global warming and carbon emissions directly increases the surface temperature. High temperatures can lead to heatstroke and increase the risk of circulatory and respiratory system failure (67). The COVID-19 pandemic and hot weather are no coincidence, as unprecedented heatwaves increase the number of infectious diseases (68, 69). The urban heat island effect may be more pronounced in the more economically developed eastern coastal districts, potentially intensifying and prolonging heatwaves (70, 71). It has been estimated that nationally, the attributable fraction of non-accidental deaths due to high temperatures will increase from 1.9% in the 2010s to 5.5% in the 2090s, with an estimated attributable fraction of 6.3% for cardiovascular system deaths and 7.7% for respiratory system deaths (72). The literature suggests that the annual heat stress index (HSI) in China has generally risen, and by 2,100, will increase by 7.96 °C based on the SSP5-8.5 scenario (73). Furthermore, heatwaves have been found to significantly increase the risk of death among the older adults suffering from Alzheimer’s disease and other dementias (74). To prevent infectious diseases under the influence of high temperatures, government policies and individual protection awareness need to work together. The number and length of case encounters can be decreased by non-pharmaceutical intervention techniques (NPIs). According to recent studies, the effective creation of biodegradable and sustainable filter materials offers a fresh, alternative approach to air quality control (75). Moreover, strengthening drug intervention can control the epidemic and reduce the risk of transmission (76, 77). A study showed that high temperatures can increase the burden of cardiovascular diseases. Therefore, reducing emissions and implementing strategies can mitigate health risks related to human-induced climate change (78).
Poyang Lake is the largest freshwater lake in China. The microbial population in the marshes around Poyang Lake’s shore experienced substantial alterations during the severe and quick drought event in 2022. The diversity of denitrifying and DNRA bacteria declined (79). The increase in nitrous oxide emissions and nitrogen retention increased the greenhouse gas emissions and raised the risk of lake eutrophication, intensifying the positive feedback between climate change and nitrous oxide emissions (80).
5 South China region (105°29′-117°14′E, 18°10′-26°15′N): includes Guangdong, Guangxi, Hainan, Hong Kong, and Macao. The terrain is mainly composed of hills with a humid and hot climate. It is the forefront of China’s opening up to the outside world
China borders the Northwest Pacific Ocean and is situated in the eastern region of the Eurasian continent. Therefore, she is one of the nations that is most severely impacted by tropical cyclones worldwide (81). Since tropical cyclones often make landfall in Guangdong Province, the losses caused by tropical cyclones in Guangdong Province are greater than those in any other province (82). In addition to their direct effects on the environment, economy, and society, tropical cyclones can have an indirect effect on public health. Studies have indicated that acute hemorrhagic conjunctivitis, diarrheal infectious diseases, leptospirosis, and hand-foot-mouth disease are among the infectious diseases that have been linked to tropical cyclones (83–85). A study showed that tropical cyclones may increase diarrheal infectious diseases in Guangdong Province (86). Another study revealed that tropical cyclones may increase the risk of hand-foot-mouth disease in children under 6 years old (87). The danger of mosquito-borne illnesses like dengue fever rises in conjunction with the temperature fluctuations and precipitation brought on by tropical storms, which may be suitable for mosquito reproduction. Since an unprecedented dengue fever outbreak occurred in Guangdong Province in 2014 (88), from 2007 to 2017, about 94% of dengue fever cases in China occurred in Guangdong Province (89). Furthermore, it has been observed that in the Pearl River Delta, tropical cyclones are linked to a higher prevalence of primary dengue fever, with the risk peaking 5–9 days following the occurrence. The risk is greatest when lagging 5–9 days (90).
Leptospirosis is an animal-source disease (91), and the risk of leptospirosis outbreak is significantly increased by flood events (92). Leptospirosis has historically been more common in the Southwestern and Southeast regions. The disease is mainly linked with farmland and marshes in the Yangtze River Basin and its Southern areas, flood exposure in the Yellow River Basin and Northern China, and the buildup of water following heavy rains in low-lying plains (93). The transmission of leptospirosis is promoted by climatic variables such as heavy rain, floods, humidity, and high temperature (94). Studies have found that leptospirosis outbreaks can be avoided in locations that are vulnerable to extreme weather events like floods and heavy rain by implementing prevention and control measures (95).
6 Southwest Region (78°-110°E, 21°-34°N): covers Sichuan, Guizhou, Yunnan, Tibet, and Chongqing. The terrain is mainly composed of plateaus and basins, with diverse climates and rich cultures
Since the COVID-19 pandemic in 2019, animal hosts have attracted much attention, including bats, civets, pangolins, and other species (96). Zoonotic infectious illnesses have increased as a result of the varied effects of climate change on the species diversity of animal hosts. Bat species richness has increased significantly in southern Yunnan, Myanmar, and Laos as a result of climate change, and bats are currently thought to be the source or intermediate host of Middle East Respiratory Syndrome (MERS) (97), Ebola (98), SARS-CoV-1 and SARS-CoV-2 Rift Valley fever (RVF) (99), etc. At present, the coronavirus strain found in bats in southern Yunnan is the closest to SARS-CoV-1 and SARS-CoV-2 (100). Hunting, eating patterns, and agricultural practices that involve intimate contact with pathogen-carrying wild animals are all linked to the zoonotic disease outbreak (101). Therefore, it is crucial to protect natural habitats, implement strict regulations on wildlife hunting and trade, establish appropriate animal welfare standards, and adjust dietary and medicinal customs (96, 102).
Dengue fever is a mosquito-borne disease that is prevalent worldwide (103). The invasion of alien species and changes in the global environment have become major contributors to the development of dengue disease and have made its prevention and control extremely difficult (104, 105). However, China’s public health prevention and control efforts continue to prioritize preventing local dengue fever transmission; thus, environmental intervention and risk area identification are essential. It has been observed that Southeast Asia is the primary source of dengue fever invasions, and Yunnan, China, which borders Laos, Vietnam, and Myanmar, is under intense pressure to prevent the invasion and reduce dengue fever prevalence (106). Temperature affects the physiological process of the dengue virus-mosquito-host chain, thus becoming one of the important driving factors for dengue fever (107). Aedes aegypti and Aedes albopictus are the primary vectors for dengue fever transmission, which can survive at 10 °C–40 °C and spread diseases in a temperature range from 16.2 °C to 34.5 °C. Higher temperatures may increase the expected lifespan of mosquitoes, promoting a longer exposure time to dengue fever. The Southeastern part of China is affected by the East Asian monsoon, with higher summer temperatures (108); therefore, this region has a significant impact of dengue fever (106). Due to climate change, the suitable environment for vector insects is expanding (109), and the risk of dengue fever transmission is increasing.
One of the highest-altitude towns in the world, Lhasa is situated in the middle of the Tibetan Plateau and experiences significant intensities of ultraviolet (UV) radiation. The literature has indicated that UV radiation is one of the major risk factors for three pigmentary skin illnesses, which are far more common in high-altitude regions than in low-altitude ones (110). Due to climate warming and the prolonged duration of ozone, earlier seasonal snowfall and ice melting, more and more people are exposed to ultraviolet radiation, which seriously affects human health (111).
Yunnan, situated in the tropics and subtropics, boasts rich biodiversity, earning it the title of having one of the richest plant communities in the world, which in turn makes its fungal resources abundant (112). Edible mushrooms come in many different varieties and are both tasty and nourishing. The living environment of mushrooms has altered as a result of ecological changes, and both their poisonous and nutritious components have changed as well. Mushroom poisoning incidents are one of the main causes of death from foodborne diseases in China (113, 114). Due to its unique climate and topography, it is the province with the most extensive variety of snake species in the country and a high incidence area of snakebite poisoning in China. Furthermore, this region borders the frontier, with ethnic minorities and poverty-stricken areas (115).
1. 7 Northwest Region (73°-111°E, 31°-49°N): includes Shaanxi, Gansu, Qinghai, Ningxia, and Xinjiang. The terrain is mainly composed of plateaus and deserts, with an arid climate and abundant resources
Severe air pollution has been associated with sandstorms. Several studies have indicated that during sandstorms, the hospitalization and mortality rates increase significantly (116, 117). Asian sandstorms mainly originate from the arid regions in the northwest and north of China and Mongolia, and spread to East Asian countries (118). Furthermore, sandstorm events have been positively correlated with the number of visits for asthma (119), stroke (120), congestive heart failure (121), and conjunctivitis (122).
Climate warming is melting the glaciers in the Asian mountainous regions (123), and the permafrost layer on the Qinghai-Tibet Plateau. When the frozen viruses are discharged, there are more chances for the viruses to propagate throughout the habitats and migrations of wild migratory birds. When the frozen viruses are discharged, there are more chances for the viruses to propagate in the wild migratory birds’ habitats and migrations (124). In 2005, a large-scale H5N1 avian influenza epidemic broke out in the Qinghai Lake area, resulting in the death of thousands of migratory birds (125). This indicates that the Qinghai Lake area has become a significant source of H5N1 avian influenza.
1. 8 Common Systemic Vulnerable Diseases in China
Cryptosporidiosis is a zoonotic disease transmitted through the fecal-oral route (126), which can cause abdominal pain, diarrhea, and acute gastroenteritis in infected hosts (127). It is highly contagious and has become a globally highly concerning acute infectious disease (128). Research has indicated a strong correlation between climate change and Cryptosporidium’s biological adaptability, and climate change may be a major factor influencing the species’ survival, resulting in its extinction, re-distribution, resurgence, or re-emergence (129). Furthermore, regions in Northeast China (Jilin Province and Heilongjiang Province), Southwest China (Yunnan Province), and Northwest China (Xinjiang Uygur Autonomous Region) are significantly affected by climate change and may be suitable for the survival of Cryptosporidium. Future climate change may provide China with more favorable habitats for Cryptosporidium (130). The Maxent model can predict the distribution of Cryptosporidium and formulate a public health strategy covering “parasite–host-environment,” strengthening real-time monitoring, increasing information exchange and communication, improving the monitoring reporting system, and improving interdisciplinary linkage mechanisms (130).
China’s rainfall is influenced by various large-scale ocean–atmosphere patterns, including El Niño-Southern Oscillation (ENSO), Pacific Decadal Oscillation (PDO), Indian Ocean Dipole (IOD), and Atlantic Multidecadal Oscillation (AMO) (131). These patterns play an important role in the occurrence of extreme drought events (87, 132). Wildfires are becoming more frequent as a result of drought and global warming, which is extremely dangerous for human life, health, and productivity (133, 134). Carbon-containing gases and tiny particulate matter are released when wildfires burn, polluting the air and raising the risk of cancer, heart disease, and respiratory ailments for firefighters who fight fires (135). The development of new protective technologies against wildfire combustion pollutants is of vital importance.
Under the influence of multiple pollutants such as PM2.5, PM10, O3, NO2, CO, PAHs (Polycyclic Aromatic Hydrocarbons), SPM (Suspended Particulate Matter), SO2, NO, radon gas (136–139), multiple organ systems such as the cardiovascular system (45), respiratory system (48, 140), digestive system (51) nervous system (141–143), eye-related diseases (144, 145), urinary system (50, 146), and mental health (147, 148) are all affected to varying degrees. The air pollution levels in many Asian nations, particularly China and India, are far greater than those in wealthy nations. In a white paper, the Allergy, Asthma and Clinical Immunology Association of Asia-Pacific highlights the current state of air pollution in the Asia-Pacific area and urges national and international health and environmental organizations to take action (149).
The connection between China and international characteristic systemic vulnerability diseases
The total length of China’s land borders is approximately 22,000 km, making it one of the countries with the longest land borders in the world, bordering 14 countries. The “Belt and Road Initiative” has had a tremendous impact on trade openness and tourism expansion in recent years, which has greatly boosted people’s mobility both domestically and globally. Moreover, this has raised the possibility of infectious illness transmission. China is not the only country experiencing climate change. Some ecosystem-related diseases are determined by the unique geographical location. Therefore, there is a certain correlation among global system-related diseases in different countries.
Food security is severely compromised by Schistocerca gregaria, which has caused famine, particularly in South Asia, the Middle East, and Africa, important regions of the world. The biological behavior of locusts is strongly influenced by hydrological and climatic factors, with temperature, wind direction, and rainfall all having distinct effects (150). Studies have shown that a warmer climate promotes locust outbreaks, and new hotspots will emerge in central and western Asia. Early cross-regional cooperation is helpful for global coordinated control of the food security threat brought by locusts (151). It has been identified that the El Niño (Southern) oscillation (ENSO) is the primary climate oscillation in southern China. ENSO leads to a higher incidence of crop pests. EnSO-driven cyclic patterns identify the pests’ source locations, which makes it easier for them to migrate to China. Early cross-regional collaboration is beneficial for the global coordinated management of pest risks to food security (152).
Measures for responding to vulnerable diseases in the Chinese system
Ecological vulnerability and adaptation measures
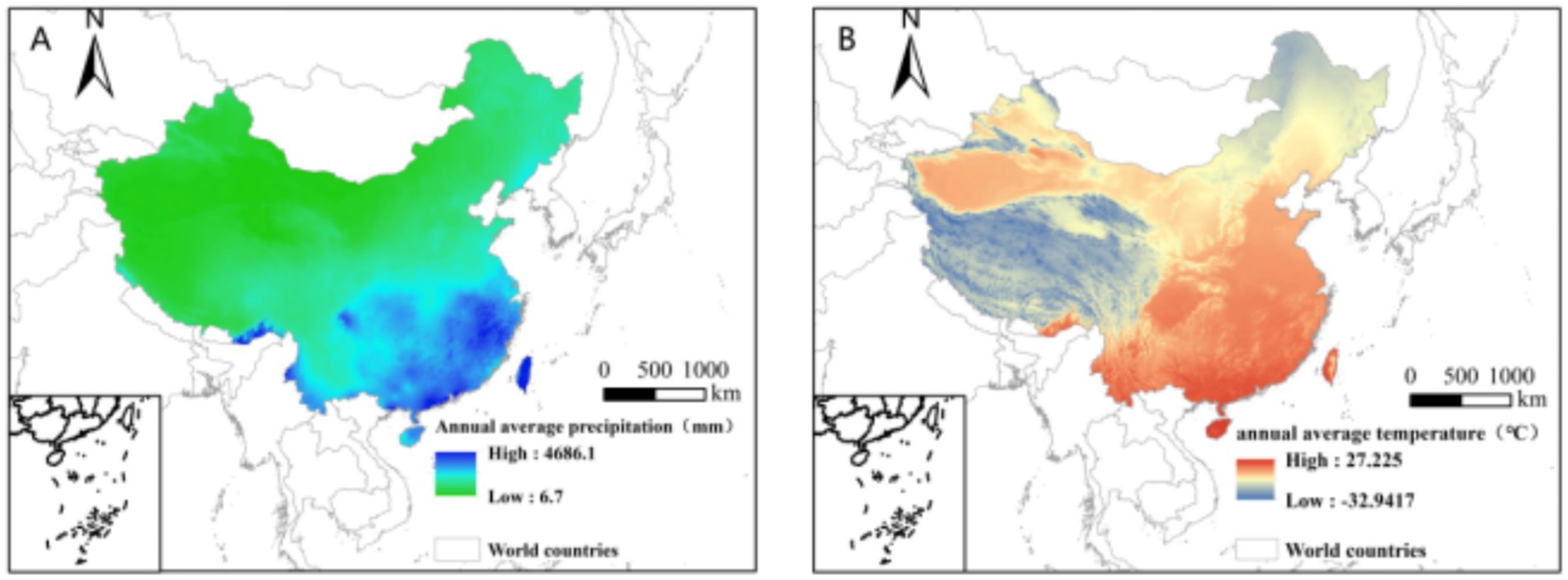
The primary and most obvious effects of climate change in China over the last three years have been an increase in yearly precipitation and a temperature rise (Figure 2). The incidence of natural disasters has increased to different degrees in each region (Table 1). Certain areas have put in place specific emergency response procedures and precautions for various extreme weather occurrences (Table 2).
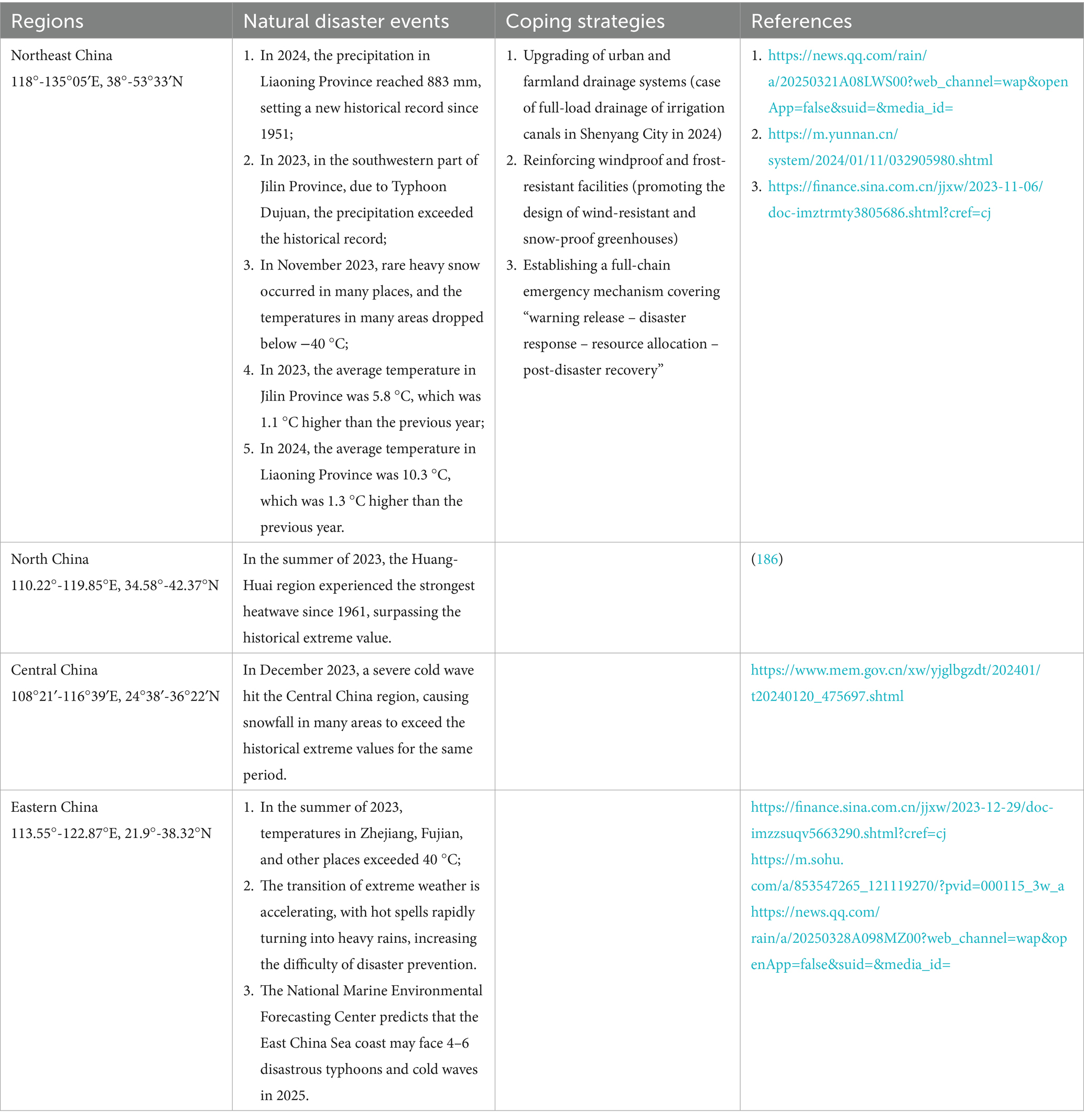
Table 1. The manifestations of system vulnerability in some regions of China over the past 3 years due to climate change.
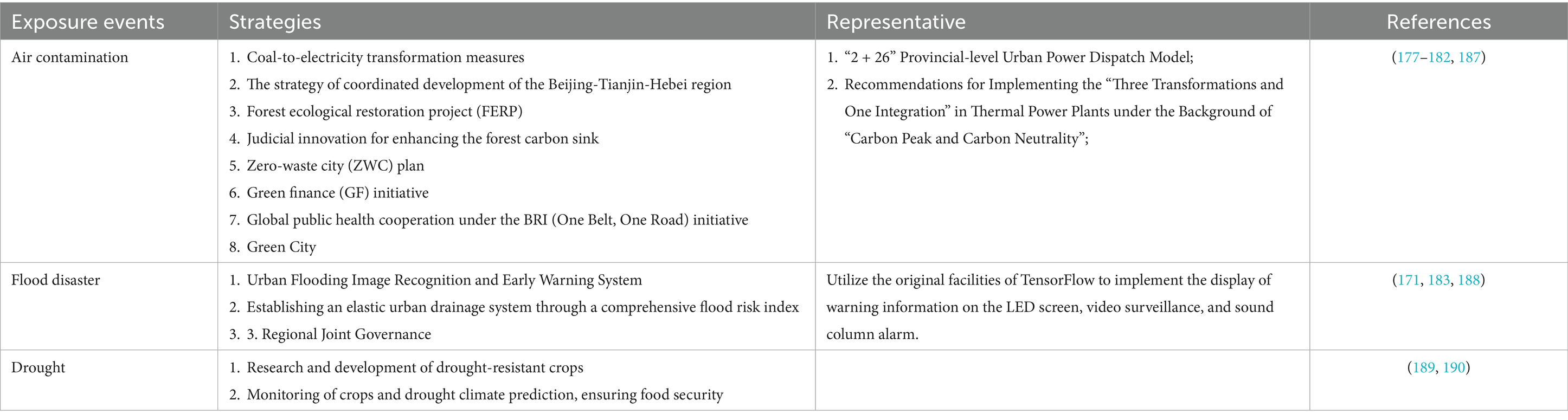
Table 2. The manifestations of some characteristic system vulnerabilities in China and the corresponding countermeasures.
Strategies for addressing the gaps in the health system and infrastructure
For the outbreak of infectious diseases, not only does the health system need to respond actively, but also infrastructure construction needs to respond promptly. China has its tailored response strategies for communication with the world (Table 3). However, China currently lacks extensive practical experience in coping with several infectious diseases around the world, and it must continue to learn from and draw on other nations’ experiences (Table 4). From the standpoint of public health policies, no nation can effectively address the issue of global climate change. Thus, international cooperation is crucial (153).
Regional adaptability ecosystem prediction model
Significant temporal and spatial disparities, severe wealth disparity, and differing levels of resource usage all make it harder to achieve unified governance and increase the ecosystem’s susceptibility in China. There are significant disparities in economic status and urbanization development between the eastern and western regions. Thus, they may face different health issues and ecosystem vulnerabilities, and there are also significant differences in the emergency response capabilities of the health systems. Based on the modified gravity model social network analysis, a study evaluated the network structure characteristics of China’s urban ecological resilience (UER) and revealed that the economically developed areas along the eastern coast had a significant “radiation effect” in spatial correlation. Furthermore, they indicated the importance of strengthening coordination and cooperation among regions to enhance UER (154). Extreme disaster events occur differently in coastal and plain areas due to significant climate changes, and each region has different priorities for emergency response. A study evaluated the patterns of flood resilience over 3 years using ArcGIS software to dynamically track each city’s level of resilience. The flood resilience level in the Pearl River Delta was very different, with the levels in the central and southern cities being higher than those in the eastern and western regions. Moreover, an innovative method was constructed to comprehensively assess the flood resilience of cities, which is suitable for quickly and accurately evaluating the short-term spatial and temporal evolution trends of urban flood resilience (155). Further research is needed to confirm that widespread adoption of this approach will effectively assess the temporal and spatial evolution patterns of floods in each region, improving flood prevention capacities, reducing health risks, and minimizing economic losses.
Southwest region
As an ecologically barrier and an underdeveloped area in the southwest, Yunnan’s social and economic development mainly relies on agriculture. Therefore, its ecosystem is susceptible to climate change (such as droughts and floods). However, Yunnan’s climate zones are complicated, and its altitude range is broad, allowing for exact classification of various places based on sensitivity levels. The ecosystem’s high sensitivity could have more negative effects. The ecosystem’s risk characteristics must be thoroughly evaluated, and appropriate action must be taken to guarantee the sustainable development strategy’s seamless implementation. A research group constructed a “climate-livelihood” framework by theoretical integration (IPCC + sustainable livelihood + human-environment coupling) and indicators localization, to build a vulnerability assessment system applicable to rural areas in Yunnan (156). This framework’s limitations include the absence of policy frameworks and the challenge of gathering subjective data. However, it takes into account the comprehensive variables of ecology, livelihood, and climate, and hence is appropriate to most rural locations (such as the southwestern mountainous regions).
Central China region
Hunan Province has a subtropical monsoon climate and is situated in China’s Yangtze River Basin. This region experiences flooding often (on average, 1 to 3 times a year between 2004 and 2011), which is followed by a significant rise in infectious diarrhea cases. This also seriously threatens the lives, health, and property safety of the people. A study found that focusing on precise intervention (water source guarantee, sanitation facilities), phased response (during and after the flood for 2 weeks), and resource allocation (in economically backward areas) can reduce the risk of diarrhea outbreaks after floods (157). Although the above research results considers the disease-related risk factors, this approach can still be employed in most southern regions. Furthermore, the flood resilience assessment system of Lagos Metropolis can be borrowed to provide a scientific basis for emergency response before and after major floods in various cities (158). Some researchers have modeled and conducted dynamic analysis of flood events in China and the UK. More real-world experiments and the development of flood-health risk warning systems might be required in the future to modify the preventative and control tactics on the fly (159).
East China region
Shanghai is one of the representative areas of economically developed China. Due to urbanization, the population’s morbidity has been affected in multiple ways by the extremely hot and muggy weather resulting from the combination of high temperatures and humidity. Studies have used the wet-bulb globe temperature (WBGT) to assess health risks, providing an operational basis for climate adaptation strategies (such as warning systems, urban planning) (160). For areas with severe, extremely hot, and humid weather (Chongqing, Guangdong), the WBGT can be included in the early warning system of public health, and the urban heat island effect can be alleviated through green space planning and building ventilation optimization to adapt to the inevitable climate warming trend in the future. However, further scientific investigation is required to validate this finding.
China’s strategy and cross-regional cooperation strategy
To address the problems caused by the vulnerability of China’s and the global public health systems, professionals across China are actively seeking, innovating, and optimizing various prediction models to formulate strategies that are highly operational and beneficial. Currently, initial results have been acquired from areas affected by the urban heat island effect, focusing on dengue fever prevention and control, as well as flood prevention after heavy rain. Other areas of China and other nations can refer to and learn from the cross-regional cooperation cases. However, in the face of the unpredictability of the future, there is still much room for improvement.
Blue-green spaces (BGS)
Extreme weather events, such as droughts, high temperatures, and floods, are increasingly common due to the urban heat island effect and global warming, significantly impacting the lives and health of local communities. Studies have shown that blue-green spaces (BGS) and urban green spaces (UGS) can mitigate the adverse effects of extreme climates on the urban environment. Research in Changchun and Ningbo of China indicates that UGS have a strong cooling effect on the surrounding environment, which is concurrent with the increase in Land Surface Temperature (LST) (161, 162).
Yunnan has a suitable climate and has natural simulated BGS. Furthermore, this region has large bodies of water, which increases air humidity through evaporation and controls temperature by absorbing heat waves. The forest coverage rate in Yunnan exceeds 60%, and tropical rainforests, evergreen broad-leaved forests, and other vegetation release water through transpiration, maintaining air humidity, absorbing dust, and purifying the air. It is one of the zones with the highest worldwide climate diversity and species richness because of the proper proportion of BGS that act in concert to prevent the extreme heat in the low latitudes and to reduce the extreme cold at high elevations.
All regions around the world have recognized that BGS offers multiple benefits, including reducing floods and heat, and increasing biodiversity. The potential of blue-green infrastructure (BGI) to convert urban areas into sustainable and adaptable environments can be observed in several projects in Spain (163). Governments in regions affected by extreme climates can formulate targeted measures based on these research findings, such as increasing vegetation, maintaining green areas, optimizing green space forms, and paying attention to the ratio of BGS.
The prevention and control project for dengue fever
By 2023, there had been several dengue fever outbreaks in China’s Guangdong and Yunnan provinces. Incomplete statistics show that there were 114,853 instances in total, including cases that were imported and those that were transmitted locally (164). The prevalent dengue virus serotypes include DENV-1, DENV-2, DENV-3, and DENV-4. Furthermore, the diversity of virus types has also presented a great challenge for disease prevention and control (165). Despite the difficult path of dengue prevention and control, China still perseveres. The Ministry of Health and the Chinese Center for Disease Control and Prevention published the crucial document “Dengue Fever Monitoring Plan (Trial) and Dengue Fever Prevention Technical Guidelines” following the main “Healthy China” policy. The central and local governments jointly formulated the “National Dengue Fever Prevention and Control Guidelines.” During the outbreak of the epidemic, the state and various administrative departments demonstrated extraordinary leadership, immediately activating the emergency response mechanism and organizing multi-departmental coordination and cooperation. Multiple department levels demonstrated exceptional coordination capabilities: disease control departments at all levels improved case management and epidemic monitoring, ensuring that higher-level departments were able to rapidly grasp epidemic trends and make real-time adjustments to prevention and control strategies while also providing front-line staff with professional knowledge, guiding vector control, and educating the public about health issues. Furthermore, various medical and health departments responded quickly, assembling medical staff and medical supplies to support the epidemic front, as well as expert teams conducting disease research, creating guidelines for diagnosis and treatment, developing detection techniques, and developing therapeutic drugs. Moreover, other community administration departments carried out their assigned tasks, guaranteeing the smooth operation of food, hygiene, and transportation while supporting pertinent agencies with health education and epidemic surveillance. The inspection and quarantine departments collaborated to improve the screening and monitoring of imported and exported goods, as well as border ports, circulating goods, and mobile personnel for diseases. The financial department also ensured the support of epidemic prevention funds, and people from all walks of life and various fund organizations assisted, ensuring sufficient epidemic materials and funds (166).
China has achieved considerable progress in controlling dengue fever, as evidenced by the fact that, from 2005 to 2023, the country reported only 15 dengue fever-related deaths, with a fatality rate of fewer than 0.01 cases per 100,000 people (167). When the COVID-19 pandemic broke out in 2019, successful practical experience led to the “dynamic zero case” of the epidemic. The lessons that can be drawn include:
1. The government’s capable leadership: In addition to swiftly creating workable policies, plans, and action plans, the government was able to temporarily designate responsible individuals to oversee cross-departmental cooperation and successfully execute reward and punishment systems. These departments included public security, health, finance, and social welfare organizations.
2. Community organizations are strong forces for control and prevention: Community organizations can achieve a role transformation from passive acceptance of policies to active guidance of residents in prevention and control, with high efficiency in vector control and strong acceptability of health education, which can fully mobilize the enthusiasm of the masses to make up for the shortage of professional personnel.
3. Innovation in vector control: Based on traditional human trapping and light trapping, innovative measures such as chemical, biological, and environmental control are adopted to reduce mosquito density, interrupt virus transmission, including remote sensing and geographic space analysis (168).
Because of the significant experience in prevention and control, the epidemic has been effectively controlled. However, there are still many areas that require improvement and the adoption of advanced international technologies and experiences. Although the disease control department places a high priority on vector control management, and public awareness of mosquito prevention has grown, human health is still seriously threatened by mosquito-borne diseases. A recent study shows that using Wolbachia bacteria may inhibit the vectors or reduce their ability to spread various vector-borne viruses through solutions that induce conditional egg infertility and compete for survival with wild-type male mosquitoes (169). This novel modeling is crucial for the current global context of health issues.
Joint prevention and control project for flood-affected areas
In 2020, severe rainstorms occurred frequently in some areas of China, and a total of 37 floods were recorded (170). The regulation of water conservation facilities in urban areas is frequently restricted due to the dense population, flat terrain, and limited living environment in China’s vast territory, as well as the disparate economic development of different cities and significant geographical differences. To effectively reduce flood risks, it is crucial to develop a well-coordinated joint flood regulation model in cities, which is highly challenging. However, Chinese water experts are still actively analyzing the temporal and spatial clustering characteristics of China and formulating a storage and drainage joint regulation model suitable for urban areas in China’s plains.
To evaluate the flood storage and discharge management models of cities and to distribute the urban flood risk levels and storage-discharge capabilities of cities, recent studies presented a unique concept based on “jointly regulated urban agglomerations” by building multi-layer tree rules (171). The research results is as follows: First, risk assessment of jointly regulated urban agglomerations. A thorough evaluation of flood hazards is carried out, and the flood risk levels of cities are categorized based on the features of the regulating cities and their surrounding cities. The cities’ capacity to store and release floodwaters is fully understood. Second, analysis of flood coordination models. Through multi-layer tree rules, the storage-after-release (SD), release-after-storage (DS), and release-and-storage-at-the-same-time (DWS) models are allocated. For instance, a city with a large water storage capacity can use the SD model to reduce regional flood pressure while ensuring its own low risk. The DS model should be utilized to reduce flood pressure in towns with strong storage capacity, whereas the DWS model should be adopted for cities with weak storage capacity. Coastal cities can adopt the DS model to assist neighboring cities with high flood risks, while non-coastal cities can adopt the DWS model. Furthermore, the role of the urban agglomeration needs to be adjusted in real time according to the precipitation characteristics in the early, middle, and late stages of the rainstorm to better coordinate the flood diversion pressure. Third, an innovative management model. As a novel approach to rainwater management, green infrastructure (172) creates thorough and long-lasting evaluation metrics to address urban flooding and climate change.
For floods, different countries have proposed plans and policies that are suitable for them. For instance, Japan has constructed the world’s largest drainage channel to regulate floods (173). The urban area control policies of different countries vary, and to improve the flood control models, we should share and learn from one another.
Cross-regional joint ecological vulnerability response strategies
China-Myanmar border: Based on China’s “Malaria Elimination Action Plan (2010–2020)” and the actual needs of Myanmar, Health Poverty Action (HPA) was established in the border area of Yunnan Province. In the border region of Yunnan Province, a sustainable network for malaria prevention and control has been established thanks to the HPA’s tripartite model of multi-level management, local implementation, and cross-border cooperation (7). However, political unpredictability, poor staff subsidies, significant family responsibilities, and a lack of professional technical experience in multi-drug resistant malaria all have an impact on sustainability because HPA relies on outside funding; its work is extremely challenging. This model can serve as a valuable guide for future international cross-border health collaboration, but it must address problems, such as technical sustainability, staffing, and funding.
Environmental safety in the karst border region between Guangxi and Vietnam: The Ecological Security Pattern (ESP) solves the three main problems of ecological connectivity, human activity interference, and cultural adaptability in delicate ecological areas like karst by combining scientific quantification (such as the MCR model, circuit theory) with traditional ecological knowledge (TEK) (174). In cross-border ecological governance, the optimized “technology + tradition” model (such as the “three axes, two belts, six zones” framework in Guangxi) provides a reusable paradigm for the karst regions worldwide. ESP needs to seek a balance between “ecological rigidity protection” (such as the core area of karst) and “development elasticity demand” (such as border trade), and cross-border coordination and the modernization of TEK are the core levers to solve the problem. In the ecological security patterns study, the Minimum Cumulative Resistance (MCR) model and the Gravity model are the core methods for identifying and screening important ecological corridors. In addition to offering cross-regional coordination solutions, the MCR model also gives “physical connectivity” and “functional importance” based on the “physical connectivity” it provides. By combining the two, ecological corridors can be precisely screened, and vulnerable areas (like the Xiliu Ditch in the Yellow River Basin, China) can receive scientific support for ecological restoration (175).
Recommendations
Recommendations on the vulnerability of the health system
The urban public health system (U-PHS) vulnerability is a complex system that requires a comprehensive and holistic assessment. The recent study employed a combined assessment model that integrates the “human-machine-environment-process” four-dimensional framework and the “Bayesian best-worst method (B-BWM) + cloud model” to comprehensively evaluate factors that affect the vulnerability of U-PHS, and identified 18 factors. Among these, the most significant issues are the poor coordination and cooperation among personnel, insufficient information assurance, low public awareness, and low competence among employees of relevant departments and institutions (176). In the Southwestern region of China (especially Yunnan), infrastructure construction is challenging, the information network is not complete, the public health system is vulnerable, and health vulnerability is significant due to the underdeveloped economic level, complex geographic environment and climatic conditions, and a lack of public awareness and cognition. Yunnan’s flora and animal resources are abundant. According to an analysis of the public health system’s vulnerability issues, the frequent occurrence of wild mushroom and snake-bite poisoning incidents is attributed to the joint effect of the “human-machine-environment-management” four-dimensional factors. Currently, our other team members are thoroughly studying the two scientific research directions of snake bites and mushroom poisonings via epidemiological investigations, clinical treatment challenges analysis, networked construction to improve treatment levels and public cognition, and by establishing clinical prediction models, etc. We hope that future research successes can provide new scientific evidence for the challenges of ecosystem vulnerability in Yunnan.
Recommendations on systemic vulnerable diseases
Zoonotic diseases
Formulate corresponding laws and regulations: Strengthen the reporting, control, and implementation of emergency response plans for zoonotic infectious diseases (177).
Upgrade the infectious disease reporting system: Various organizations, including hospitals, community health centers, the Ministry of Health, the Ministry of Forestry, and the Ministry of Agriculture, should work together and exchange information online to respond to infectious disease emergencies effectively and efficiently (178, 179).
Implementation of special projects for major infectious diseases: The effective integration of technology sharing platforms, professional academic alliances, typical demonstration areas, and high-quality forces can establish a multi-link network technology system and a strong support system for infectious disease prevention and control, as well as improve the emergency response capabilities for infectious diseases (180).
Monitoring of abnormal diseases: The monitoring of cross-border transmission of exotic diseases should be strengthened, and a cross-border animal disease control joint mechanism should be established between China and neighboring countries (181).
Emphasize interdisciplinary and international cooperation: An international early warning system should be established to timely monitor unknown infectious diseases in international public health (182).
Health education: Living habits should be changed, the living environment should be improved, and public awareness should be increased (183).
Common systemic vulnerable diseases
Strengthening the monitoring and early warning system
a. Climate Adaptation Warning: The climate model predictions should be combined to forecast the risk of vector-borne diseases (such as the early warning system for African malaria).
Improving the healthcare system
a. Resource Fair Distribution: Vaccine coverage should be improved in low-income countries through international assistance (Global Alliance for Vaccines and Immunization, GAVI).
b. Innovative Health Financing Mechanism: Disease burden should be included in major policy evaluation systems by controlling the Health Impact Assessment (HIA) system. The primary barriers to action are a lack of resources and a shortage of workers. It is recommended that climate change be integrated into the development of primary health care, and that sustainable government should provide funding and resource support.
c. Primary Service: The community medical worker model (such as the “Health Promotion Program” in Ethiopia) should be promoted.
d. Integrate Traditional Chinese and Western Medicine: The prevention and treatment integration training bases should be established in regions with abundant traditional Chinese medicine resources (such as Gansu and Guangxi).
Cross-sectoral collaborative governance
a. (a)Environmental and Health Linkage: Sanitation facilities should be improved (such as the “Clean India Movement” in India to reduce waterborne infectious diseases), environmental pollution during urbanization should be controlled, and meteorological and health data should be integrated to establish an early warning system.
b. Economic Policy Intervention: The risk of infectious diseases should be reduced through poverty reduction (United Nations Sustainable Development Goal SDG1).
Public health education and behavioral intervention
a. Health Education: The public should be educated on mosquito prevention measures, safe drinking water, and vaccination.
b. Chronic Disease Control: High-risk behaviors should be changed through taxation (Mexican “Sugar-Sweetened Beverage Tax Law”) and legislation (anti-smoking policies).
Climate adaptation and resilience building
a. Climate-Sensitive Disease Response: Adaptive technologies such as heat-resistant vaccines and anti-malaria nets should be developed.
b. Disaster Emergency Response: A rapid response mechanism for cholera after floods (such as the case in Bangladesh) should be established.
Technological innovation and application
a. Digital Healthcare: Artificial intelligence (AI) to predict disease outbreaks (such as modeling by Metabiota in the United States), mobile healthcare to cover remote areas, AI-assisted drug resistance prediction, microfluidic chip rapid detection, etc., should be employed to improve diagnosis efficiency, establish an environment-genome monitoring database, and promote region-specific disease prevention and control plans.
b. Genetic Technology: Genetic editing should be performed to control malaria transmission (such as Targe Malaria).
c. Application of Geographic Information Technology: A Geographic Information System (GIS) should be adopted to draw disease risk maps, such as the malaria transmission risk spatial model established by the Chinese Center for Disease Control and Prevention.
Global cooperation
Chinese experience in chronic disease prevention and control should be promoted, international vaccine distribution and monitoring network governance measures should be established, and guidelines by the WHO and Global Infectious Disease Monitoring Network (GOARN) should be followed to share epidemic data, such as virus genome tracking observed during the COVID-19 pandemic.
Future challenges
Ecosystems are changing due to climate change, and the effects of this change on human health are profound and far-reaching. Monitoring across time and space, using predictive models, studying the influencing mechanisms, formulating response strategies, implementing feasible plans, and achieving desired results are all lengthy and complex processes. Disease distribution occurs because of natural, economic, and social factors, and the policy response should integrate the concept of “One Health” (human-animal-environmental health integration) (184, 185), and achieve comprehensive management through multidisciplinary cooperation, international assistance, and localized deployment strategies. Therefore, establishing a more resilient public health system to meet the long-term challenges of climate change would require multifaceted and cross-scale structural adjustments.
Author contributions
YT: Methodology, Writing – original draft. YC: Methodology, Writing – original draft. SF: Formal analysis, Resources, Writing – original draft. BH: Validation, Writing – original draft. QG: Methodology, Writing – review & editing. ZL: Funding acquisition, Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by grants from The Yunnan Provincial Department of Science and Technology—Kunming Medical University Joint Special Project on Applied Basic Research (202301AY070001-064). Yunnan Fundamental Research Projects (202501AT070046). Hu Yu expert workstation (202305AF150149). Joint Fund of Yunnan University of Traditional Chinese Medicine (XYLH2024029).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^http://www.news.cn/20250715/e1cfa95744124efeb46966aa3bfbc66a/c.html
2. ^https://www.news.cn/politics/20250727/d2d840908baa489580f36723c8733f7b/c.html
References
1. Yao, T, Thompson, L, Yang, W, Yu, W, Gao, Y, Guo, X, et al. Different glacier status with atmospheric circulations in Tibetan Plateau and surroundings. Nat Clim Chang. (2012) 2:663–7. doi: 10.1038/nclimate1580
2. Cheng, T, Chen, D, Wang, B, Cheng, TF, Ou, T, and Lu, M. Human-induced warming accelerates local evapotranspiration and precipitation recycling over the Tibetan Plateau. Commun Earth Environ. (2024) 5. doi: 10.1038/s43247-024-01563-9
3. Lingxiao, S, Yang, Y, Yuting, G, Jing, H, Xiang, Y, Ireneusz, M, et al. Remote Sensing Monitoring and Evaluation of the Temporal and Spatial Changes in the Eco-Environment of a Typical Arid Land of the Tarim Basin in Western China Land (Basel) (2021) 10:868. doi: 10.3390/land10080868
4. Afshar, E, Yarnia, M, Bagherzadeh, A, Sadrabadi Haghighi, R, and Mirshekari, B. The effects of cropping systems on soil erosion risks and crop productivity using ImpelERO model and GIS in northeast of Iran. Model Earth Syst Environ. (2016) 2. doi: 10.1007/s40808-016-0142-6
5. Yang, H, Gou, X, and Yin, D. Response of biodiversity, ecosystems, and ecosystem services to climate change in China: a review. Ecologies. (2021) 2:313–31. doi: 10.3390/ecologies2040018
6. Tran, HM, Tsai, FJ, Lee, YL, Chang, JH, Chang, LT, Chang, TY, et al. The impact of air pollution on respiratory diseases in an era of climate change: A review of the current evidence. Sci Total Environ. (2023) 898:166340. doi: 10.1016/j.scitotenv.2023.166340
7. Zhang, J, Dong, JQ, Li, JY, Zhang, Y, Tian, YH, Sun, XY, et al. Effectiveness and impact of the cross-border healthcare model as implemented by non-governmental organizations: case study of the malaria control programs by health poverty action on the China-Myanmar border. Infect Dis Poverty. (2016) 5:80. doi: 10.1186/s40249-016-0175-0
8. Zhao, C, Chen, J, Su, G, and Yuan, H. Assessment of the climate change adaptation capacity of urban agglomerations in China. Mitig Adapt Strateg Glob Change. (2019) 25:221–36. doi: 10.1007/s11027-019-09874-5
9. Li, C, Cai, R, and Yan, X. Assessment of the future changes in the socio-economic vulnerability of China’s coastal areas. Sustainability. (2023) 15:5794. doi: 10.3390/su15075794
10. Pan, X, Fu, W, and Yang, Y. Occurrence, ecological, and health risk assessment of antibiotics in water from the Karst River during influenza season. River. (2024) 3:389–98. doi: 10.1002/rvr2.107
11. Allen, L. Biosecurity and non-communicable diseases. J Bioterror Biodef. (2016) 7. doi: 10.4172/2157-2526.1000145
12. Rocque, RJ, Beaudoin, C, Ndjaboue, R, Cameron, L, Poirier-Bergeron, L, Poulin-Rheault, RA, et al. Health effects of climate change: an overview of systematic reviews. BMJ Open. (2021) 11:e046333. doi: 10.1136/bmjopen-2020-046333
13. Musacchio, A, Andrade, L, O'Neill, E, Re, V, O'Dwyer, J, and Hynds, PD. Planning for the health impacts of climate change: Flooding, private groundwater contamination and waterborne infection – A cross-sectional study of risk perception, experience and behaviours in the Republic of Ireland. Environ Res. (2021) 194:110707. doi: 10.1016/j.envres.2021.110707
14. Hong, C, Zhang, Q, Zhang, Y, Davis, SJ, Tong, D, Zheng, Y, et al. Impacts of climate change on future air quality and human health in China. Proc Natl Acad Sci USA. (2019) 116:17193–200. doi: 10.1073/pnas.1812881116
15. Tong, MX, Hansen, A, Hanson-Easey, S, Cameron, S, Xiang, J, Liu, Q, et al. Infectious Diseases, Urbanization and Climate Change: Challenges in Future China. Int J Environ Res Public Health. (2015) 12:11025–36. doi: 10.3390/ijerph120911025
16. Zhu, N, Zhang, D, Wang, W, Li, X, Yang, B, Song, J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
17. NOAA. U.S. Billion-dollar Weather and Climate Disasters, 1980 – Present; (2020). Natl Centers Environ Inf Published. doi: 10.25921/STKW-7W73
18. World Health Organization. Ageing and Health. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (Accessed 15 February 2023)
19. Chen, P, Li, F, and Harmer, P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. (2019) 4:e447. doi: 10.1016/S2468-2667(19)30160-4
20. Zhou, Y, Liu, Y, Wu, W, and Li, N. Integrated risk assessment of multi-hazards in China. Nat Hazards. (2015) 78:257–80. doi: 10.1007/s11069-015-1713-y
21. El Mougher, MMA, Abu Sharekh, SAM, Abu Ali, RF, and Zuhud, AAM. Risk management of gas stations that urban expansion crept into in the Gaza Strip. Int J Disaster Risk Manag. (2023) 5:13–26. doi: 10.18485/ijdrm.2023.5.1.2
22. Haque, CE, and Burton, I. Adaptation options strategies for hazards and vulnerability mitigation: an international perspective. Mitig Adapt Strateg Glob Change. (2005) 10:335–53. doi: 10.1007/s11027-005-0050-y
23. Liu, S, Ren, Y, Wen, D, Chen, Y, Chen, D, Li, L, et al. Prevalence and risk factors for COPD in greenhouse farmers: a large, cross-sectional survey of 5, 880 farmers from northeast China. Int J Chron Obstruct Pulmon Dis. (2015) 10:2097. doi: 10.2147/COPD.S79264
24. Jia, SM, Chen, MH, Yang, PF, Wang, L, Wang, GY, Liu, LY, et al. Seasonal variations and sources of atmospheric EPFRs in a megacity in severe cold region: Implications for the influence of strong coal and biomass combustion. Environ Res. (2024) 252:119067. doi: 10.1016/j.envres.2024.119067
25. Fang, L, Gao, P, Bao, H, Tang, X, Wang, B, Feng, Y, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. (2018) 6:421–30. doi: 10.1016/S2213-2600(18)30103-6
26. Ji, C, Lv, J, Zhang, J, Zhu, M, Yu, C, Ma, H, et al. Household air pollution and risk of incident lung cancer in urban China: A prospective cohort study. Int J Cancer. (2023) 153:1592–601. doi: 10.1002/ijc.34646
27. Yu, Y, Tian, XC, Zhang, H, Hu, D, Lyu, J, Yu, CQ, et al. Association of solid fuel use for heating and smoking with respiratory diseases: a prospective cohort study. Zhonghua Liu Xing Bing Xue Za Zhi. (2024) 45:1356–61. doi: 10.3760/cma.j.cn112338-20240508-00246
28. Wang, Y, Zhu, F, Li, J, Gurmesa, GA, Huang, S, Fang, X, et al. Evidence and causes of recent decreases in nitrogen deposition in temperate forests in Northeast China. Sci Total Environ. (2024) 929:172472. doi: 10.1016/j.scitotenv.2024.172472
29. Tian, Z, Wan, L, Pei, J, Li, T, Wang, X, Yuan, P, et al. Brucellosis seroprevalence in cattle in China during 2014-2024: a systematic review and meta-analysis. Emerg Microbes Infect. (2024) 13:2417859. doi: 10.1080/22221751.2024.2417859
30. Sun, ZX, Wang, Y, Li, YJ, Yu, SH, Wu, W, Huang, DS, et al. Socioeconomic, meteorological factors and spatiotemporal distribution of human brucellosis in China between 2004 and 2019-A study based on spatial panel model. PLoS Negl Trop Dis. (2023) 17:e0011765. doi: 10.1371/journal.pntd.0011765
31. Ni, H, Dai, H, Yang, X, Zhao, J, He, Y, Yi, S, et al. Effective intervention of brucellosis prevention in developing countries: a dynamic modelling study. One Health. (2024) 19:100840. doi: 10.1016/j.onehlt.2024.100840
32. Gage, KL, and Kosoy, MY. Natural history of plague: perspectives from more than a century of research. Annu Rev Entomol. (2005) 50:505. doi: 10.1146/annurev.ento.50.071803.130337
33. Perry, RD, and Fetherston, JD. Yersinia pestis--etiologic agent of plague. Clin Microbiol Rev. (1997) 10:35–66. doi: 10.1128/CMR.10.1.35
34. Sarah, NB, John, AB, Dale, LN, Min, Z, and Hongxuan, H. Yersinia pestis: examining wildlife plague surveillance in China and the USA. Integr Zool. (2012) 7:99–109. doi: 10.1111/j.1749-4877.2011.00277.x
35. Galdan, B, Baatar, U, Molotov, B, and Dashdavaa, O. Plague in Mongolia. Vector Borne Zoonotic Dis. (2010) 10:69–75. doi: 10.1089/vbz.2009.0047
36. Xu, L, Stige, LC, Leirs, H, Neerinckx, S, Gage, KL, Yang, R, et al. Historical and genomic data reveal the influencing factors on global transmission velocity of plague during the third pandemic. Proc Natl Acad Sci USA. (2019) 116:11833–8. doi: 10.1073/pnas.1901366116
37. Zhang, M, Liu, S, Chen, M, Chen, J, Cao, X, Xu, G, et al. The below-ground carbon and nitrogen cycling patterns of different mycorrhizal forests on the eastern Qinghai-Tibetan Plateau. Peer J. (2022) 10:e14028. doi: 10.7717/peerj.14028
38. Wang, L, Zeng, Y, and Zhong, L. Impact of climate change on tourism on the Qinghai-Tibetan Plateau: research based on a literature review. Sustainability. (2017) 9:1539. doi: 10.3390/su9091539
39. Stenseth, NC, Samia, NI, Viljugrein, H, Kausrud, KL, Begon, M, Davis, S, et al. Plague dynamics are driven by climate variation. Proc Natl Acad Sci USA. (2006) 103:13110–5. doi: 10.1073/pnas.0602447103
40. Eads, DA, and Hoogland, JL. Precipitation, climate change, and parasitism of prairie dogs by fleas that transmit plague. J Parasitol. (2017) 103:309–19. doi: 10.1645/16-195
41. Yan, H, Bu, F, Wu, X, Zhang, H, Sun, S, Bai, W, et al. Host selection and influencing factors of parasitic fleas on the body surface of desert rodents, Inner Mongolia, China. Int J Parasitol Parasites Wildl. (2024) 25:100993. doi: 10.1016/j.ijppaw.2024.100993
42. Zhou, M, Wang, H, Zeng, X, Yin, P, Zhu, J, Chen, W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
43. Huo, Q, Yin, Z, Ma, X, and Wang, H. Distinctive dust weather intensities in North China resulted from two types of atmospheric circulation anomalies. Atmos Chem Phys. (2025) 25:1711–24. doi: 10.5194/acp-25-1711-2025
44. Chen, Z, Zhou, Z, Ji, C, Yao, Z, Mao, J, Wang, Z, et al. Comparison of the polluted dust plume and natural dust air mass in a spring dust event in Beijing 2023. J Environ Sci (China). (2024) 154:760. doi: 10.1016/j.jes.2024.07.003
45. Hao, J, Liu, Z, Hu, B, Tse, LA, Rangarajan, S, Wang, C, et al. Interactive effects of outdoor fine particulate matter and metabolic, behavioural, and psychosocial risk factors on cardiovascular disease: analysis of the PURE-China cohort study. Eur Heart J. (2024) 45:ehae666-2941. doi: 10.1093/eurheartj/ehae666.2941
46. Zhang, J, Luo, L, Chen, G, Ai, B, Wu, G, Gao, Y, et al. Associations of ambient air pollution with incidence and dynamic progression of atrial fibrillation. Sci Total Environ. (2024) 951:175710. doi: 10.1016/j.scitotenv.2024.175710
47. Jing, D, Shao, B, Gao, Y, Zaihua Wei, Y, Zhang, HL, et al. Relationship between exposure to fine particulate matter and cardiovascular risk factors and the modifying effect of socioeconomic status: a cross-sectional study in Beijing, China. Front. Public Health. (2024) 12:1398396. doi: 10.3389/fpubh.2024.1398396
48. Niu, Y, Niu, H, Meng, X, Zhu, Y, Ren, X, He, R, et al. Associations between air pollution and the onset of acute exacerbations of COPD: a time-stratified case-crossover study in China. Chest. (2024) 166:998–1009. doi: 10.1016/j.chest.2024.05.030
49. Qin, L, Yang, L, Liu, L, Tong, S, Liu, Q, Li, G, et al. Oxidative potential and persistent free radicals in dust storm particles and their associations with hospitalization. Nat Commun. (2024) 15:10827. doi: 10.1038/s41467-024-55151-8
50. Hou, T, Jiang, Y, Zhang, J, Hu, R, Li, S, Fan, W, et al. Kidney injury evoked by fine particulate matter: risk factor, causation, mechanism and intervention study. Adv Sci (Weinh). (2024) 11:e2403222. doi: 10.1002/advs.202403222
51. Zhao, H, Zheng, X, Lin, G, Wang, X, Lu, H, Xie, P, et al. Effects of air pollution on the development and progression of digestive diseases: an umbrella review of systematic reviews and meta-analyses. BMC Public Health. (2025) 25:183. doi: 10.1186/s12889-024-21257-3
52. Hu, J, Yang, L, Kang, N, Wang, N, Shen, L, Zhang, X, et al. Associations between long-term exposure to fine particulate matter and its constituents with lung cancer incidence: Evidence from a prospective cohort study in Beijing, China. Environ Pollut. (2025) 368:125686. doi: 10.1016/j.envpol.2025.125686
53. Li, T, Cohen, AJ, Krzyzanowski, M, Zhang, C, Gumy, S, Mudu, P, et al. Sand and dust storms: a growing global health threat calls for international health studies to support policy action. Lancet Planet Health. (2025) 9:e34–40. doi: 10.1016/S2542-5196(24)00308-5
54. Zhou, Y, and Zhou, J. Study on the impact of green finance and environmental regulations on haze pollution in China. Atmosphere. (2024) 15:1548. doi: 10.3390/atmos15121548
55. Markevych, I, Schoierer, J, Hartig, T, Chudnovsky, A, Hystad, P, Dzhambov, AM, et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ Res. (2017) 158:301. doi: 10.1016/j.envres.2017.06.028
56. Rahimi-Ardabili, H, Astell-Burt, T, Nguyen, PY, Zhang, J, Jiang, Y, Dong, GH, et al. Green space and health in mainland China: a systematic review. Int J Environ Res Public Health. (2021) 18:9937. doi: 10.3390/ijerph18189937
57. Liu, X, Liu, Z, Zhang, Y, and Jiang, B. Quantitative analysis of burden of bacillary dysentery associated with floods in Hunan, China. Sci Total Environ. (2016) 547:190. doi: 10.1016/j.scitotenv.2015.12.160
58. Xu, X, Ding, G, Zhang, Y, Liu, Z, Liu, Q, and Jiang, B. Quantifying the impact of floods on bacillary dysentery in Dalian city, China, from 2004 to 2010. Disaster Med Public Health Prep. (2016) 11:190–5. doi: 10.1017/dmp.2016.90
59. Luo, PY, Chen, MX, Kuang, WT, Ni, H, Zhao, J, Dai, HY, et al. Hysteresis effects of different levels of storm flooding on susceptible enteric infectious diseases in a central city of China. BMC Public Health. (2023) 23:1874. doi: 10.1186/s12889-023-16754-w
60. Ji, H, Li, K, Shang, M, Wang, Z, and Liu, Q. The 2016 severe floods and incidence of hemorrhagic fever with renal syndrome in the Yangtze River Basin. JAMA Netw Open. (2024) 7:e2429682. doi: 10.1001/jamanetworkopen.2024.29682
61. Vial, PA, Ferrés, M, Vial, C, Klingström, J, Ahlm, C, López, R, et al. Hantavirus in humans: a review of clinical aspects and management. Lancet Infect Dis. (2023) 23:e371–82. doi: 10.1016/S1473-3099(23)00128-7
62. Wang, Y, Zhang, C, Gao, J, Chen, Z, Liu, Z, Huang, J, et al. Spatiotemporal trends of hemorrhagic fever with renal syndrome (HFRS) in China under climate variation. Proc Natl Acad Sci USA. (2024) 121:e2312556121. doi: 10.1073/pnas.2312556121
63. Gryseels, B, Polman, K, Clerinx, J, and Kestens, L. Human schistosomiasis. Lancet. (2006) 368:1106–18. doi: 10.1016/S0140-6736(06)69440-3
64. Li-Juan, Z, Zhi-Min, X, Ying-Jun, Q, Hui, D, Shan, L, Jing, X, et al. Endemic status of schistosomiasis in People's Republic of China in 2015. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. (2016) 28:611–7. doi: 10.16250/j.32.1374.2016246
65. Yang, Y, Zhou, YB, Song, XX, Li, SZ, Zhong, B, Wang, TP, et al. Integrated Control Strategy of Schistosomiasis in The People’s Republic of China: Projects Involving Agriculture, Water Conservancy, Forestry, Sanitation and Environmental Modification. ADV PARASIT. (2016) 92:237–68. doi: 10.1016/bs.apar.2016.02.004
66. Yang, Y, Gao, J, Cheng, W, Pan, X, Yang, Y, Chen, Y, et al. Three Gorges Dam: polynomial regression modeling of water level and the density of schistosome-transmitting snails Oncomelania hupensis. Parasit Vectors. (2018) 11:183. doi: 10.1186/s13071-018-2687-x
67. Robine, JM, Cheung, SL, Le Roy, S, Van Oyen, H, Griffiths, C, Michel, JP, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. CR BIOL. (2007) 331:171–8. doi: 10.1016/j.crvi.2007.12.001
68. Luo, M, Ning, G, Xu, F, Wang, S, Liu, Z, and Yang, Y. Observed heatwave changes in arid northwest China: physical mechanism and long-term trend. Atmos Res. (2020) 242:242 105009. doi: 10.1016/j.atmosres.2020.105009
69. Robine, JM, Cheung, SL, Le Roy, S, Van Oyen, H, Griffiths, C, Michel, JP, et al. A Year of Unprecedented Climate Extremes in Eastern Asia. North America, and Europe ADV ATMOS SCI. (2021) 2022. doi: 10.1007/s00376-022-2063-9
70. Hui-Yi, Y, Kou-Huang, C, and Kow-Tong, C. Cause-specific mortality and burden attributable to temperature variability in China. SCI TOTAL ENVIRON. (2023) 896:165267. doi: 10.1016/j.scitotenv.2023.165267
71. Cheng, J, Xu, Z, Zhu, R, Wang, X, Jin, L, Song, J, et al. Impact of diurnal temperature range on human health: a systematic review. Int J Biometeorol. (2014) 58:2011–24. doi: 10.1007/s00484-014-0797-5
72. Yang, J, Zhou, M, Ren, Z, Li, M, Wang, B, Liu, DL, et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat Commun. (2021) 12:1039. doi: 10.1038/s41467-021-21305-1
73. Zhang, G, Han, L, Yao, J, Yang, J, Xu, Z, Cai, X, et al. Assessing future heat stress across China: combined effects of heat and relative humidity on mortality. Front Public Health. (2023) 11:1282497. doi: 10.3389/fpubh.2023.1282497
74. Zhang, R, Sun, L, Jia, A, Wang, S, Guo, Q, Wang, Y, et al. Effect of heatwaves on mortality of Alzheimer's disease and other dementias among elderly aged 60 years and above in China, 2013-2020: a population-based study. Lancet Reg Health West Pac. (2024) 52:52 101217. doi: 10.1016/j.lanwpc.2024.101217
75. Tang, X, Zhang, Z, Jing, L, Luan, K, Zhang, T, Zhou, S, et al. Synthesis of a quaternary ammonium-halamine and preparation on the modified nanofibrous filter with superior sterilization, air filtration, and biodegradability. ACS Appl Mater Interfaces. (2024) 16:59245–55. doi: 10.1021/acsami.4c12239
76. Oraby, T, Tyshenko, MG, Maldonado, JC, Vatcheva, K, Elsaadany, S, Alali, WQ, et al. Modeling the effect of lockdown timing as a COVID-19 control measure in countries with differing social contacts. Sci Rep. (2021) 11:3354. doi: 10.1038/s41598-021-82873-2
77. Sun, K, Wang, W, Gao, L, Wang, Y, Luo, K, Ren, L, et al. Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. SCIENCE. (2020) 371. doi: 10.1126/science.abe2424
78. Zhu, Q, Zhou, M, Zare Sakhvidi, MJ, Yang, S, Chen, S, Feng, P, et al. Projecting heat-related cardiovascular mortality burden attributable to human-induced climate change in China. EBioMedicine. (2024) 103:105119. doi: 10.1016/j.ebiom.2024.105119
79. Candry, P, Abrahamson, B, Stahl, DA, and Winkler, M-KH. Microbially mediated climate feedbacks from wetland ecosystems. Glob Change Biol. (2023) 29:5169–83. doi: 10.1111/gcb.16850
80. Su, R, Zhao, D, Zhang, X, Zhang, H, Cheng, J, Xu, L, et al. Dissimilatory nitrate reduction pathways drive high nitrous oxide emissions and nitrogen retention under the flash drought in the largest freshwater lake in China. Water Res. (2024) 274:123075. doi: 10.1016/j.watres.2024.123075
81. China Meteorological Administration. Yearbook of Meteorological Disasters in China 2019. China Meteorological Press (2019).
82. Xu, WD. Characteristics of tropic cyclones landing in Guangdong province and their impacts. Marine Forecasts. (2020) 37:11–8. doi: 10.11737/j.issn.1003-0239
83. Zheng, J, Han, W, Jiang, B, Ma, W, and Zhang, Y. Infectious diseases and tropical cyclones in southeast China. Int J Environ Res Public Health. (2017) 14:494. doi: 10.3390/ijerph14050494
84. Giribabu, D, Muvva, VR, Joshi, NK, and Rao, SS. Assessment of epidemiological implications due to serial tropical cyclones in India: introspecting the recent sanitation interventions. Disaster Med Public Health Prep. (2020) 15:181–90. doi: 10.1017/dmp.2019.129
85. Deng, Z, Xun, H, Zhou, M, Jiang, B, Wang, S, Guo, Q, et al. Impacts of tropical cyclones and accompanying precipitation on infectious diarrhea in cyclone landing areas of Zhejiang Province, China. Int J Environ Res Public Health. (2015) 12:1054–68. doi: 10.3390/ijerph120201054
86. Kang, R, Xun, H, Zhang, Y, Wang, W, Wang, X, Jiang, B, et al. Impacts of different grades of tropical cyclones on infectious diarrhea in Guangdong, 2005-2011. PLoS One. (2015) 10:e0131423. doi: 10.1371/journal.pone.0131423
87. Awange, J, Forootan, E, Kuhn, M, Awange, JL, Kusche, J, and Heck, B. Water storage changes and climate variability within the Nile Basin between 2002 and 2011. Adv Water Resour. (2014) 73:1–15. doi: 10.1016/j.advwatres.2014.06.010
88. Sanna, M, Wu, J, Zhu, Y, Yang, Z, Lu, J, and Hsieh, YH. Spatial and temporal characteristics of 2014 dengue outbreak in Guangdong, China. Sci Rep. (2018) 8:2344. doi: 10.1038/s41598-018-19168-6
89. Li, Q, Ren, H, Zheng, L, Cao, W, Zhang, A, Zhuang, D, et al. Ecological niche modeling identifies fine-scale areas at high risk of dengue fever in the Pearl River Delta, China. Int J Environ Res Public Health. (2017) 14:619. doi: 10.3390/ijerph14060619
90. Li, C, Zhao, Q, Zhao, Z, Liu, Q, and Ma, W. The association between tropical cyclones and dengue fever in the Pearl River Delta, China during 2013-2018: A time-stratified case-crossover study. PLoS Negl Trop Dis. (2021) 15:e0009776. doi: 10.1371/journal.pntd.0009776
91. Vasylieva, N, Andreychyn, M, Kravchuk, Y, Chervinska, О, and Iosyk, I. Changes in leptospirosis etiology in animals and humans. Ann Agric Environ Med. (2017) 24:671–5. doi: 10.26444/aaem/78031
92. Casanovas-Massana, A, Costa, F, Riediger, IN, Cunha, M, de Oliveira, D, Mota, DC, et al. Spatial and temporal dynamics of pathogenic Leptospira in surface waters from the urban slum environment. WATER RES. (2017) 130:176–84. doi: 10.1016/j.watres.2017.11.068
93. Shao, JW, Wei, YH, Yao, XY, Chen, HY, Liu, H, Sun, J, et al. Pathogenic leptospira species are widely disseminated among wild rodents in urban areas of Guangzhou, southern China. Microorganisms. (2022) 10:873. doi: 10.3390/microorganisms10050873
94. Dhewantara, PW, Lau, CL, Allan, KJ, Hu, W, Zhang, W, Mamun, AA, et al. Spatial epidemiological approaches to inform leptospirosis surveillance and control: a systematic review and critical appraisal of methods. Zoonoses Public Health. (2018) 66:185–206. doi: 10.1111/zph.12549
95. Wang, Z, Li, K, Liu, Y, Ward, MP, Chen, Y, Li, S, et al. Changing epidemiology of leptospirosis in China from 1955 to 2022. Infect Dis Poverty. (2025) 14:17. doi: 10.1186/s40249-025-01284-x
96. Petrovan, SO, Aldridge, DC, Bartlett, H, Bladon, AJ, Booth, H, Broad, S, et al. Post COVID-19: a solution scan of options for preventing future zoonotic epidemics. Biol Rev. (2021) 96:2694–715. doi: 10.1111/brv.12774
97. Mohd, HA, Al-Tawfiq, JA, and Memish, ZA. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) origin and animal reservoir. Virol J. (2016) 13:87. doi: 10.1186/s12985-016-0544-0
98. Marí Saéz, A, Weiss, S, Nowak, K, Lapeyre, V, Zimmermann, F, Düx, A, et al. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Mol Med. (2015) 7:17–23. doi: 10.15252/emmm.201404792
99. Wang, Z, Pei, S, Ye, R, Chen, J, Cheng, N, Zhao, M, et al. Increasing evolution, prevalence, and outbreaks for rift valley fever virus in the process of breaking geographical barriers. Sci Total Environ. (2024) 917:170302. doi: 10.1016/j.scitotenv.2024.170302
100. Beyer, RM, Manica, A, and Mora, C. Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS-CoV-1 and SARS-CoV-2. Sci Total Environ. (2021) 767:145413. doi: 10.1016/j.scitotenv.2021.145413
101. Gibb, R, Franklinos, LHV, Redding, DW, and Jones, KE. Ecosystem perspectives are needed to manage zoonotic risks in a changing climate. BMJ. (2020) 371:371 m3389. doi: 10.1136/bmj.m3389
102. Nabi, G, and Khan, S. Corrigendum to "Preventing bat-born viral outbreaks in future using ecological interventions" [Environ. Res. 185 (2020) 109460]. Environ Res. (2020) 189:109929. doi: 10.1016/j.envres.2020.109929
103. Wilder-Smith, A, Lindsay, SW, Scott, TW, Ooi, EE, Gubler, DJ, and das, P. The Lancet commission on dengue and other Aedes-transmitted viral diseases. Lancet. (2020) 395:1890–1. doi: 10.1016/S0140-6736(20)31375-1
104. Franklinos, LHV, Jones, KE, Redding, DW, and Abubakar, I. The effect of global change on mosquito-borne disease. Lancet Infect Dis. (2019) 19:e302–12. doi: 10.1016/S1473-3099(19)30161-6
105. Baker, RE, Mahmud, AS, Miller, IF, Rajeev, M, Rasambainarivo, F, Rice, BL, et al. Infectious disease in an era of global change. Nat Rev Microbiol. (2021) 20:193–205. doi: 10.1038/s41579-021-00639-z
106. Zhao, Z, Yue, Y, Liu, X, Li, C, Ma, W, and Liu, Q. The patterns and driving forces of dengue invasions in China. Infect Dis Poverty. (2023) 12:42. doi: 10.1186/s40249-023-01093-0
107. Reinhold, JM, Lazzari, CR, and Lahondère, C. Effects of the environmental temperature on Aedes Aegypti and Aedes albopictus mosquitoes: a review. Insects. (2018) 9:158. Published 2018 Nov 6. doi: 10.3390/insects9040158
108. Zhang, J, Huan, X, Lü, H, Wang, C, Shen, C, He, K, et al. Crossing of the Hu line by Neolithic population in response to seesaw precipitation changes in China. Sci Bull (Beijing). (2022) 67:844–52. doi: 10.1016/j.scib.2021.12.011
109. Kraemer, MUG, Reiner, RCJr, Brady, OJ, Messina, JP, Gilbert, M, Pigott, DM, et al. Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat Microbiol. (2019) 4:854–63. doi: 10.1038/s41564-019-0376-y
110. Xu, M, Zhen, Z, Chen, Y, Zhang, S, Li, J, Li, N, et al. Pigmented skin disorders in high-altitude: cross-sectional epidemiological analysis in the general population of Lhasa, China. J Cosmet Dermatol. (2025) 24:e70030. doi: 10.1111/jocd.70030
111. Neale, PJ, Hylander, S, Banaszak, AT, Häder, DP, Rose, KC, Vione, D, et al. Environmental consequences of interacting effects of changes in stratospheric ozone, ultraviolet radiation, and climate: UNEP Environmental Effects Assessment Panel, Update 2024. Photochem Photobiol Sci. (2025) 24:357–92. doi: 10.1007/s43630-025-00687-x
112. Tang, SM, Zhao, G, Niu, KY, Li, RY, Yu, FM, Karunarathna, SC, et al. Species diversity of edible mushrooms I-four new Laccaria species from Yunnan Province, China. J Fungi (Basel). (2025) 11:189. doi: 10.3390/jof11030189
113. Yuan, Y, Zhang, Y, Zhou, J, Lang, N, Jiang, S, Li, H, et al. Detection and identification in reported mushroom poisoning incidents – China, 2012-2023. China CDC Wkly. (2024) 6:1360–4. doi: 10.46234/ccdcw2024.270
114. Li, H, Zhang, Y, Zhang, H, Zhou, J, Chen, Z, Liang, J, et al. Mushroom poisoning outbreaks – China, 2023. China CDC Wkly. (2024) 6:64–8. doi: 10.46234/ccdcw2024.014
115. Zhong, GH, Chen, WD, Liu, Q, Zhu, F, Peng, PH, and Guo, P. Valid or not? Yunnan mountain snake Plagiopholis unipostocularis Serpentes: Colubridae: Pseudoxenodontinae. ZOOTAXA. (2015) 4020:390–6. doi: 10.11646/zootaxa.4020.2.9
116. Chen, Q, Wang, M, Sun, H, Wang, X, Wang, Y, Li, Y, et al. Enhanced health risks from exposure to environmentally persistent free radicals and the oxidative stress of PM2.5 from Asian dust storms in Erenhot, Zhangbei and Jinan, China. Environ Int. (2018) 121:260–8. doi: 10.1016/j.envint.2018.09.012
117. Guan, Q, Li, F, Yang, L, Zhao, R, Yang, Y, and Luo, H. Spatial-temporal variations and mineral dust fractions in particulate matter mass concentrations in an urban area of northwestern China. J Environ Manag. (2018) 222:95–103. doi: 10.1016/j.jenvman.2018.05.064
118. Liu, CM, Young, CY, and Lee, YC. Influence of Asian dust storms on air quality in Taiwan. Sci Total Environ. (2006) 368:884–97. doi: 10.1016/j.scitotenv.2006.03.039
119. Yang, CY, Tsai, SS, Chang, CC, and Ho, SC. Effects of Asian dust storm events on daily admissions for asthma in Taipei, Taiwan. Inhal Toxicol. (2005) 17:817–21. doi: 10.1080/08958370500241254
120. Yang, CY, Chen, YS, Chiu, HF, and Goggins, WB. Effects of Asian dust storm events on daily stroke admissions in Taipei, Taiwan. Environ Res. (2005) 99:79–84. doi: 10.1016/j.envres.2004.12.009
121. Yang, CY, Cheng, MH, and Chen, CC. Effects of Asian dust storm events on hospital admissions for congestive heart failure in Taipei, Taiwan. J Toxicol Environ Health A. (2009) 72:324–8. doi: 10.1080/15287390802529880
122. Yang, CY. Effects of Asian dust storm events on daily clinical visits for conjunctivitis in Taipei, Taiwan. J Toxicol Environ Health A. (2006) 69:1673–80. doi: 10.1080/15287390600630096
123. Hu, S, Zhou, T, and Wu, B. Accelerated warming of high mountain Asia predicted at multiple years ahead. Sci Bull. (2024) 70:419–28. doi: 10.1016/j.scib.2024.09.023
124. Canavan, BC. Opening Pandora's box at the roof of the world: landscape, climate and avian influenza (H5N1). Acta Trop. (2019) 196:93–101. doi: 10.1016/j.actatropica.2019.04.021
125. Bourouiba, L, Wu, J, Newman, S, Takekawa, J, Natdorj, T, Batbayar, N, et al. Spatial dynamics of bar-headed geese migration in the context of H5N1. J R Soc Interface. (2010) 7:1627–39. doi: 10.1098/rsif.2010.0126
126. Liu, J, Platts-Mills, JA, Juma, J, Kabir, F, Nkeze, J, Okoi, C, et al. Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: a reanalysis of the GEMS case-control study. Lancet. (2016) 388:1291–301. doi: 10.1016/S0140-6736(16)31529-X
127. O'Donoghue, PJ. Cryptosporidium and cryptosporidiosis in man and animals. Int J Parasitol. (1995) 25:139–95. doi: 10.1016/0020-7519(94)e0059-v
128. Gururajan, A, Rajkumari, N, Devi, U, and Borah, P. Cryptosporidium and waterborne outbreaks – A mini review. Trop Parasitol. (2021) 11:11–5. doi: 10.4103/tp.TP_68_20
129. Young, I, Smith, BA, and Fazil, A. A systematic review and meta-analysis of the effects of extreme weather events and other weather-related variables on Cryptosporidium and Giardia in fresh surface waters. J Water Health. (2015) 13:1–17. doi: 10.2166/wh.2014.079
130. Wang, X, Jiang, Y, Wu, W, He, X, Wang, Z, Guan, Y, et al. Cryptosporidiosis threat under climate change in China: prediction and validation of habitat suitability and outbreak risk for human-derived Cryptosporidium based on ecological niche models. Infect Dis Poverty. (2023) 12:35. doi: 10.1186/s40249-023-01085-0
131. Gao, T, Xu, Y, Wang, H, Wang, HJ, Sun, Q, Xie, L, et al. Combined impacts of climate variability modes on seasonal precipitation extremes over China. Water Resour Manag. (2022) 36:2411–31. doi: 10.1007/s11269-022-03150-z
132. Xiao, M, Zhang, Q, and Singh, V. Influences of ENSO, NAO, IOD and PDO on seasonal precipitation regimes in the Yangtze River basin, China. Int J Climatol. (2014) 35:3556–67. doi: 10.1002/joc.4228
133. Prestemon, J, Shankar, U, Xiu, A, Prestemon, JP, Talgo, K, Yang, D, et al. Projecting wildfire area burned in the south-eastern United States, 2011–60. Int J Wildland Fire. (2016) 25:715–29. doi: 10.1071/wf15124
134. Flannigan, M, Krawchuk, M, de Groot, W, Wotton, B, and Gowman, L. Implications of changing climate for global wildland fire. Int J Wildland Fire. (2009) 18:483. doi: 10.1071/wf08187
135. Tian, X, Cheng, Y, Chen, S, Liu, S, Wang, Y, Niu, X, et al. The emission characteristics and health risks of firefighter-accessed fire: a review. Toxics. (2024) 12:739. doi: 10.3390/toxics12100739
136. Tian, Y, Zhang, J, Huang, C, Ma, Y, Sun, Y, Zhang, C, et al. Ambient polycyclic aromatic hydrocarbons and cardiovascular disease in China. J Hazard Mater. (2025) 491:137948. doi: 10.1016/j.jhazmat.2025.137948
137. Xiao, Y, Zeng, Y, Huang, Y, You, A, Yu, L, Shu, J, et al. The effect of tropospheric low-value ozone exposure on the mortality risk of ischemic heart disease and stroke on the example of Yibin (southwestern China). Int J Biometeorol. (2025) 69:1167–79. doi: 10.1007/s00484-025-02886-8
138. Cui, X, Tian, Y, Yin, Z, Huang, S, and Yin, P. The impact of ambient PM2.5 on emergency ambulance dispatches due to circulatory system disease modified by season and temperature in Shenzhen, China. Atmosphere. (2025) 16:198. doi: 10.3390/atmos16020198
139. Miao, X, Su, Y, Hou, C, Song, Y, Ding, B, Cui, H, et al. Indoor radon survey in 31 provincial capital cities and estimation of lung cancer risk in urban areas of China. Biomed Environ Sci. (2024) 37:1294–302. doi: 10.3967/bes2024.165
140. D'Amato, G, Holgate, ST, Pawankar, R, Ledford, DK, Cecchi, L, Al-Ahmad, M, et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. (2015) 8:25. doi: 10.1186/s40413-015-0073-0
141. Xie, C, Xia, X, Wang, K, Yan, J, Bai, L, Guo, L, et al. Ambient air pollution and Parkinson's disease and Alzheimer's disease: an updated meta-analysis. Toxics. (2025) 13:139. doi: 10.3390/toxics13020139
142. Zhou, Y, Jin, Y, and Zhang, Z. Short-term exposure to nitrogen dioxide and emergency department visits for cause-stroke: a time-series study in Shanghai, China, 2013-2022. Environ Health Prev Med. (2024) 29:67. doi: 10.1265/ehpm.24-00304
143. Deng, X, Zhao, L, Xiao, C, Dai, R, Xu, Q, Yao, Y, et al. Heatstroke characteristics and meteorological conditions in Hefei, China: thresholds and driving factors. BMC Public Health. (2025) 25:352. doi: 10.1186/s12889-025-21577-y
144. Gu, Y, Sheng, F, Gao, M, Zhang, L, Hao, S, Chen, S, et al. Acute and continuous exposure of airborne fine particulate matter (PM2.5): diverse outer blood-retinal barrier damages and disease susceptibilities. Part Fibre Toxicol. (2023) 20:50. doi: 10.1186/s12989-023-00558-2
145. Chen, X, Ren, Y, Zheng, T, Cheng, H, Shen, Y, Liu, Y, et al. The effect of airborne particulate matter 2.5 (PM2.5) on meibomian gland. Exp Eye Res. (2024) 245:109956. doi: 10.1016/j.exer.2024.109956
146. Okoye, O, Carnegie, E, and Mora, L. Ambient air pollution and chronic kidney disease risk in Deltan communities: a policy brief, 2023. F1000Res. (2025) 13:265. doi: 10.12688/f1000research.145904.3
147. Go, TH, Kim, MH, Choi, YY, Han, J, Kim, C, and Kang, DR. The short-term effect of ambient particulate matter on suicide death. Environ Health. (2024) 23:3. doi: 10.1186/s12940-023-01042-2
148. Chen, S, Oliva, P, and Zhang, P. Air pollution and mental health: evidence from China. AEA Pap Proc. (2024) 114:423–8. doi: 10.1257/pandp.20241062
149. Pawankar, R, Wang, JY, Wang, IJ, Thien, F, Chang, YS, Latiff, AHA, et al. Asia Pacific Association of Allergy Asthma and Clinical Immunology White Paper 2020 on climate change, air pollution, and biodiversity in Asia-Pacific and impact on allergic diseases. Asia Pac Allergy. (2020) 10:e11. doi: 10.5415/apallergy.2020.10.e11
150. Meynard, CN, Lecoq, M, Chapuis, MP, and Piou, C. On the relative role of climate change and management in the current desert locust outbreak in East Africa. Glob Change Biol. (2020) 26:3753–5. doi: 10.1111/gcb.15137
151. Liu, X, Zhang, D, and He, X. Unveiling the role of climate in spatially synchronized locust outbreak risks. Sci Adv. (2024) 10:eadj1164. doi: 10.1126/sciadv.adj1164
152. Wang, C, Wang, X, Sang, Y, Müller, C, Huang, Y, Li, L, et al. Oscillation-induced yield loss in China partially driven by migratory pests from mainland Southeast Asia. Nat Food. (2025) 6:681–91. doi: 10.1038/s43016-025-01158-3
153. Dilaver, I, Karakullukcu, S, Gurcan, F, Topbas, M, Ursavas, OF, and Beyhun, NE. Climate change and non-communicable diseases: a bibliometric, content, and topic modeling analysis. Sustainability. (2025) 17:2394. doi: 10.3390/su17062394
154. Liu, Z, and Liu, T. Temporal and spatial evolution and network analysis of urban ecological resilience considering natural influences. J Ind Ecol. (2025) 29:863–77. doi: 10.1111/jiec.70025
155. Xu, W, Han, P, Proverbs, DG, and Guo, X. A study of the temporal and spatial evolution trends of urban flood resilience in the Pearl River Delta. China. Int J Build Pathol. (2025). doi: 10.1108/ijbpa-11-2024-0228
156. He, Y, Zhou, C, and Ahmed, T. Vulnerability assessment of rural social-ecological system to climate change: a case study of Yunnan Province, China. Int J Clim Chang Str. (2021) 13:162–80. doi: 10.1108/ijccsm-08-2020-0094
157. Liu, Z, Zhang, F, Zhang, Y, Li, J, Liu, X, Ding, G, et al. Association between floods and infectious diarrhea and their effect modifiers in Hunan province, China: A two-stage model. Sci Total Environ. (2018) 626:630. doi: 10.1016/j.scitotenv.2018.01.130
158. Orimoogunje, O, and Aniramu, O. Systematic review of flood resilience strategies in Lagos Metropolis: pathways toward the 2030 sustainable development agenda. Front Clim. (2025) 7:1603798. doi: 10.3389/fclim.2025.1603798
159. Falconer, RA. Modelling and forecasting processes in urban environments: particularly in the UK and China. Hydrology. (2025) 12:82. doi: 10.3390/hydrology12040082
160. Liang, C, Yuan, J, Tang, X, Kan, H, Cai, W, and Chen, J. The influence of humid heat on morbidity of megacity Shanghai in China. Environ Int. (2024) 183:108424. doi: 10.1016/j.envint.2024.108424
161. Yang, H, and Zeng, H. Impact of changes in—blue and green spaces on the spatiotemporal evolution of the urban heat island effect in Ningbo and its implications for sustainable development. Sustainability. (2025) 17:4156. doi: 10.3390/su17094156
162. Yu, H, and Piao, Y. The cooling effect and its stability in urban green space in the context of global warming: a case study of Changchun, China. Sustainability. (2025) 17:2590. doi: 10.3390/su17062590
163. Polo-Martín, B. The potential of blue–green infrastructures (BGIs) to boost urban resilience: examples from Spain. Urban Sci. (2025) 9:102. doi: 10.3390/urbansci9040102
164. Ni, H, Cai, X, Ren, J, Dai, T, Zhou, J, Lin, J, et al. Epidemiological characteristics and transmission dynamics of dengue fever in China. Nat Commun. (2024) 15:8060. doi: 10.1038/s41467-024-52460-w
165. Meng, JX, Hu, QM, Zhang, LM, Li, N, He, Y-W, Yang, Z-X, et al. Isolation and genetic evolution of dengue virus from the 2019 outbreak in Xishuangbanna, Yunnan Province, China. Vector-Borne Zoonotic Dis. (2023) 23:331–40. doi: 10.1089/vbz.2022.0091
166. Feng, X, Jiang, N, Zheng, J, Zhu, Z, Chen, J, Duan, L, et al. Advancing knowledge of One Health in China: lessons for One Health from China's dengue control and prevention programs. Sci One Health. (2024) 3:100087. doi: 10.1016/j.soh.2024.100087
167. Du, J, Zhang, L, Hu, X, Peng, R, Wang, G, Huang, Y, et al. Phylogenetic Analysis of the Dengue Virus Strains Causing the 2019 Dengue Fever Outbreak in Hainan. China. Virol Sin. (2021) 36:636–43. doi: 10.1007/s12250-020-00335-x
168. Zhang, Y, Wang, M, Huang, M, and Zhao, J. Innovative strategies and challenges mosquito-borne disease control amidst climate change. Front Microbiol. (2024) 15:15 1488106. doi: 10.3389/fmicb.2024.1488106
169. Moretti, R, Lim, JT, Ferreira, AGA, Ponti, L, Giovanetti, M, Yi, CJ, et al. Exploiting wolbachia as a tool for mosquito-borne disease control: pursuing efficacy, safety, and sustainability. Pathogens. (2025) 14:285. doi: 10.3390/pathogens14030285
170. CMA. Yearbook of Meteorological Disasters in China, vol. 2021. Beijing: Meteorological Press (2022). 3 p.
171. Liu, Q, Zhang, Z, Liangrui, Y, and Zhe, W. Regional joint regulation mode for flood control in plain cities: addressing extensive heavy rainfall. Water Sci Technol. (2025) 91:714–30. doi: 10.2166/wst.2025.027
172. Zhang, Y, Yin, H, Liu, M, Kong, F, and Xu, J. Evaluating the effectiveness of environmental sustainability indicators in optimizing green-grey infrastructure for sustainable stormwater management. Water Res. (2024) 272:122932. doi: 10.1016/j.watres.2024.122932
173. EDOGAWA River Office. About the Metropolitan Outer Area Underground Discharge Channel; (2023), Kanto Regional Development Bureau: Japan
174. Teng, M, Liu, S, Cao, W, Huang, C, Huang, Y, and Long, C. Harnessing traditional ecological knowledge for ecological security optimization in karst border regions: a case study of Guangxi–Vietnam. Sustainability. (2025) 17:2858. doi: 10.3390/su17072858
175. Xu, X, Wang, S, Yan, G, and He, X. Ecological Security Assessment Based on the “Importance–Sensitivity–Connectivity” Index and Pattern Construction: A Case Study of Xiliu Ditch in the Yellow River Basin, China. Land. (2023) 12:1296. doi: 10.3390/land12071296
176. Fu, L, Wang, Z, Zhu, Y, Liang, B, Qian, T, and Ma, H. Assessing the vulnerability of urban public health system based on a hybrid model. Front Public Health. (2025) 13:1576214. doi: 10.3389/fpubh.2025.1576214
177. Xiao, Z, Li, H, and Gao, Y. Analysis of the impact of the Beijing-Tianjin-Hebei coordinated development on environmental pollution and its mechanism. Environ Monit Assess. (2022) 194:91. doi: 10.1007/s10661-021-09720-9
178. Que, Z, Zhang, Y, and Cheng, X. Judicial innovation in enhancing forest carbon sinks: evidence from China. Forests. (2025) 16:369. doi: 10.3390/f16020369
179. Zhu, F, Hunjra, AI, Roubaud, D, Zhao, S, and Grebinevych, O. Assessment of synergistic governance of pollution and carbon reduction. J Environ Manag. (2025) 375:124226. doi: 10.1016/j.jenvman.2025.124226
180. Huang, H, Mbanyele, W, Zhang, L, Chen, XL, and Song, M. Nonnegligible transition risks towards net-zero economy: Lessons from green finance initiatives in China. J Environ Manag. (2025) 375:124132. doi: 10.1016/j.jenvman.2025.124132
181. Tambo, E, Khayeka-Wandabwa, C, Muchiri, GW, Liu, YN, Tang, S, and Zhou, XN. China's Belt and Road Initiative: Incorporating public health measures toward global economic growth and shared prosperity. Glob Health J. (2019) 3:46–9. doi: 10.1016/j.glohj.2019.06.003
182. Aishan, T, Sun, Y, Halik, Ü, Betz, F, Yusup, A, and Rezhake, R. Spatiotemporal changes in fine particulate matter and ozone in the oasis city of Korla, northeastern Tarim Basin of China. Sci Rep. (2024) 14:12904. doi: 10.1038/s41598-024-63856-5
183. Feng, X. Image recognition and early warning system of urban waterlogging based on Tensorflow. J Phys Conf Ser. (2021) 1992:022055. doi: 10.1088/1742-6596/1992/2/022055
184. Bruno, G, and Buccoliero, GB. Antivirals against Monkeypox (Mpox) in humans: an updated narrative review. Life (Basel). (2023) 13:1969. doi: 10.3390/life13101969
185. Zhang, XX, Li, XC, Zhang, QY, Liu, JS, Han, LF, Lederman, Z, et al. Tackling global health security by building an academic community for one health action. Infect Dis Poverty. (2023) 12:70. doi: 10.1186/s40249-023-01124-w
186. Zhu, XY, Sun, LH, Zhong, HL, Zhi, R, Ai, WX, Jiang, YD, et al. Characteristics of climate anomalies and major meteorological events over China in 2023 (in Chinese). Meteor Mon. (2024) 50:246–56. doi: 10.7519/j.issn.1000-0526.2024.010501
187. Zhu, L, Liang, Z, Zhang, L, Meng, W, Yao, X, Su, B, et al. Assessing the impacts of coal-to-electricity transition in China's regional power system and "2 + 26" cities. iScience. (2025) 28:111775. doi: 10.1016/j.isci.2025.111775
188. Ahmad, S, Peng, X, Ashraf, A, Yin, D, Chen, Z, Ahmed, R, et al. Building resilient urban drainage systems by integrated flood risk index for evidence-based planning. J Environ Manag. (2025) 374:124130. doi: 10.1016/j.jenvman.2025.124130
189. Chowdhury, TA, Ahmed, Z, Laskor, MAH, Kadir, A, and Zhang, F. How monitoring crops and drought, combined with climate projections, enhances food security: Insights from the Northwestern regions of Bangladesh. Environ Monit Assess. (2025) 197:430. doi: 10.1007/s10661-025-13907-9
190. Zhang, T, Zhang, Y, Ding, Y, Yang, Y, Zhao, D, Wang, H, et al. Research on the regulation mechanism of drought tolerance in wheat. Plant Cell Rep. (2025) 44:77. doi: 10.1007/s00299-025-03465-2
191. Zhang, T, Jian, Z, Chen, J, Xu, D, Yang, X, Lu, Y, et al. Efficiency enhancement in main path extraction in mRNA vaccine field: A novel approach leveraging intermediate patents, with shielding origin and terminus patent edges. Hum Vaccin Immunother. (2025) 21:2454078. doi: 10.1080/21645515.2025.2454078
192. Li, Y, Wu, J, Hao, J, Dou, Q, Xiang, H, and Liu, S. Short-term impact of ambient temperature on the incidence of influenza in Wuhan, China. Environ Sci Pollut Res Int. (2021) 29:18116–25. doi: 10.1007/s11356-021-16948-y
193. Zinnah, MA, Uddin, MB, Hasan, T, das, S, Khatun, F, Hasan, MH, et al. the re-emergence of Mpox: old illness, modern challenges. Biomedicine. (2024) 12:1457. doi: 10.3390/biomedicines12071457
194. El-Bushra, H, Izzoddeen, A, Haroun, A, ElBushra, E, Abualgasim, H, Abasher, M, et al. Multistate cholera outbreak in Sudan amid ongoing armed conflict, 2023-2024. Int J Infect Dis. (2025) 153:107788. doi: 10.10.1016/j.ijid.2025.107788
195. Izzoddeen, A, Abualgasim, H, Abasher, M, Elnoor, H, Magbol, M, Fadlelmoula, S, et al. Cholera in conflict: outbreak analysis and response lessons from Gadaref state, Sudan (2023-2024). BMC Public Health. (2025) 25:881. doi: 10.1186/s12889-025-22128-1
196. George, CM, Namunesha, A, Endres, K, Felicien, W, Sanvura, P, Bisimwa, JC, et al. Epidemiologic and genomic surveillance of Vibrio cholerae and effectiveness of single-dose oral cholera vaccine, Democratic Republic of the Congo. Emerg Infect Dis. (2025) 31:288–97. doi: 10.3201/eid3102.241777
197. Chen, Y, Wang, P, Zhang, FN, Dai, H, Jiao, XY, Wang, XY, et al. Sensors for surveillance of RNA viruses: a one health perspective. Lancet Microbe. (2024) 6:101029. doi: 10.1016/j.lanmic.2024.101029.81
198. Krammer, F, Hermann, E, and Rasmussen, AL. Highly pathogenic avian influenza H5N1: history, current situation, and outlook. J Virol. (2025) 99:e0220924. doi: 10.1128/jvi.02209-24
199. Owusu, H, and Sanad, YM. Comprehensive insights into highly pathogenic avian influenza H5N1 in dairy cattle: transmission dynamics, milk-borne risks, public health implications, biosecurity recommendations, and one health strategies for outbreak control. Pathogens. (2025) 14:278. doi: 10.3390/pathogens14030278
Keywords: vulnerability of public health system, disease distribution, adaptation strategy, China, environment
Citation: Teng Y, Cao Y, Feng S, Han B, Gao Q and Li Z (2025) Vulnerability characteristics and adaptation strategies of public health systems in different regions of China. Front. Public Health. 13:1609377. doi: 10.3389/fpubh.2025.1609377
Edited by:
Rachael Piltch-Loeb, Harvard University, United StatesReviewed by:
Monica Ewomazino Akokuwebe, University of the Witwatersrand, South AfricaGoran Trbic, University of Banjaluka, Bosnia and Herzegovina
Copyright © 2025 Teng, Cao, Feng, Han, Gao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qinfen Gao, Z2FvcWlucm9uZ2ZmMjAyMUAxNjMuY29t; Zengzheng Li, bGl6ZW5nemhlbmdAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Yajun Teng
Yajun Teng Yue Cao2†
Yue Cao2† Shuai Feng
Shuai Feng Zengzheng Li
Zengzheng Li