- 1Department of Pediatric Dentistry, Faculty of Dentistry, Universitas Padjadjaran, Bandung, Indonesia
- 2Department of Pediatric Dentistry and Public Health, Kulliyah of Dentistry, International Islamic University Malaysia, Selayang, Malaysia
Background: Oral diseases remain a significant public health challenge worldwide, disproportionately impacting children in developing countries due to socioeconomic hardship and limited healthcare access.
Purpose: This rapid review evaluates the relationship between low household income and children’s oral health outcomes in developing countries.
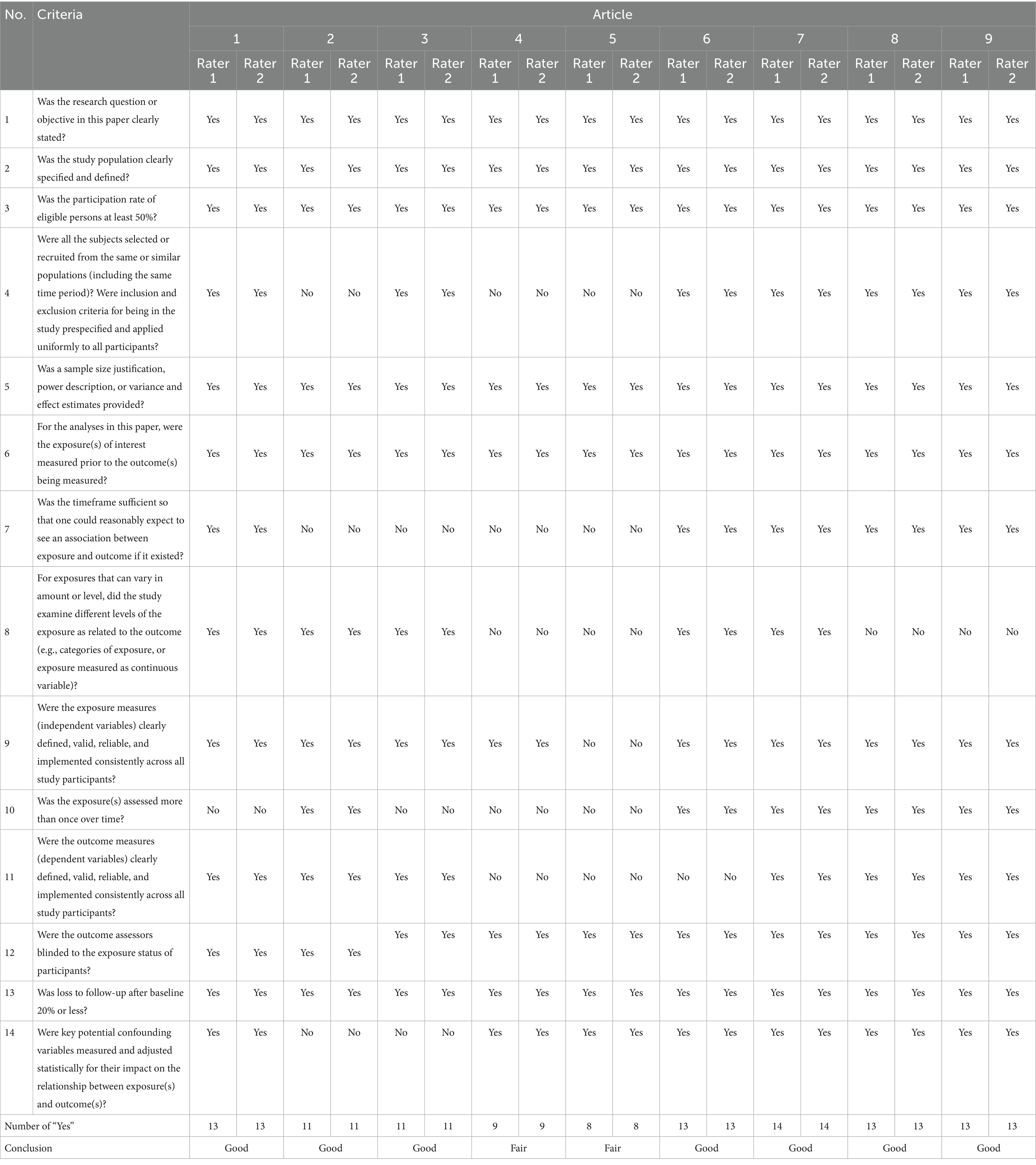
Method: We followed PRISMA 2020 and Cochrane Rapid Review guidelines. A systematic search of five databases (2012–2022) using refined keywords identified eligible studies. Quality assessment used the NIH tool.
Results: Of 1,574 articles identified, 13 met inclusion criteria. Most were cross-sectional studies from China, India, Nigeria, Brazil, and Syria. A consistent association was found between lower socioeconomic status and worse oral health outcomes, including higher DMFT/dmft scores, gingivitis, and early childhood caries (ECC).
Conclusion: Low socioeconomic status (SES) is associated with worse oral health outcomes in children in developing countries.
1 Introduction
Oral and dental health was a problem for nearly 3.5 billion people worldwide in 2020. Untreated dental caries in permanent teeth remain the most prevalent health condition globally, affecting an estimated 2.5 billion people. Severe periodontal disease affects approximately 10.8% of the global population. In addition, lip and oral cavity cancers rank among the 15 most common cancers worldwide (1). Untreated oral diseases can cause pain, infection, and reduced quality of life and productivity. Good oral health positively impacts nutrition, employment, self-confidence, and social participation (2).
Lower socioeconomic status is strongly linked to poorer oral health outcomes (2). Previous studies in developed countries have shown that low-income people have worse oral health compared to those with high-incomes (3). Economic inequalities affect healthcare access and utilization, influencing oral health outcomes (4). The link between economic factors and dental and oral health is reflected in the increasing prevalence of oral health problems among populations in low-income countries (2). Economic inequalities within the population continue to influence individuals’ decisions when healthcare facilities and services are chosen, ultimately affecting the outcomes of the care they receive (4).
According to the World Health Organization (WHO), oral health problems are more prevalent in low and middle-income countries (LMICs), with three-quarters of affected individuals residing in these regions (2). WHO indicates that developing nations endure a considerable burden of oral disorders, including dental caries, advanced periodontal disease, tooth loss, and oral malignancies. The WHO indicates that more than 45% of the global population is afflicted by oral disorders, with three-quarters of these individuals living in low- and middle-income nations (5).
Comprehensive data on the oral health of children from low-income households in developing countries are scarce, posing challenges for developing targeted interventions (2). Most existing literature focuses on adults in developed countries, leaving a research gap regarding children in developing nations. Understanding the relationship between poverty and oral health in childhood—a crucial phase for establishing lifelong habits—is essential. This rapid review aims to synthesize current evidence on how low household income influences children’s oral health outcomes in developing countries.
2 Method
This rapid review was conducted in accordance with Cochrane Rapid Review guidelines and PRISMA 2020. We used the PICO framework as follows: – Population: Children (0–18 years) from low-income families in developing countries – Intervention: Assessment of oral health status using indices (DMFT/ dmft, GI, OHI-S) – Comparison: Children from higher-income households – Outcome: Prevalence of caries and severity, ECC, gingivitis, and oral hygiene.
The research question was: “What is the impact of poverty on oral health status of children in developing countries?”.
We searched ScienceDirect, PubMed, Scopus, Web of Science, and Livivo using terms including “oral health,” “dental health survey,” “oral health status,” “socioeconomic factors,” and “children.” The term “low socioeconomic status” was not included as a primary keyword to avoid overly restrictive results and ensure broader retrieval. Boolean logic was adapted for each database (detailed in Table 1).
Articles published between January 2012 and August 2022, in English or Indonesian, were included. Dissertations, gray literature, and non-full-text papers were excluded. Screening was conducted independently by three reviewers. Quality appraisal used the NIH tool (6).
Duplicate articles were removed, and the remaining articles were checked on the basis of the relevance of the title and abstract and then selected on the basis of full-text availability and content consistency with the study objectives. Further screening was performed by checking the study location to ensure that the studies were conducted in developing countries according to the World Economic Situation and Prospects 2020 classification (7).
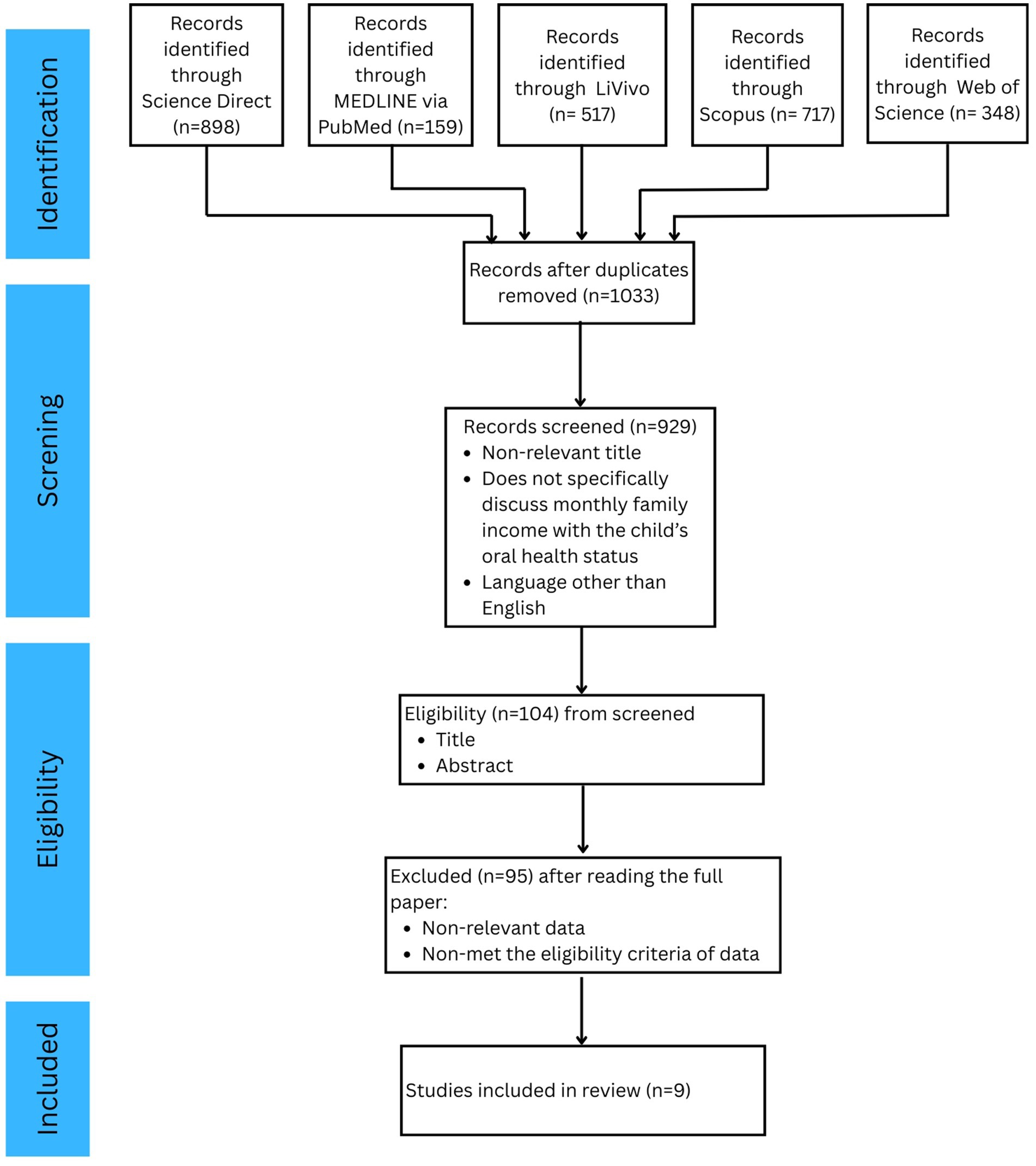
The results of the expedited review process, including identification, screening, eligibility evaluation, and final selection, are illustrated in the PRISMA flow diagram (Figure 1). A preliminary search employing specified keywords and filters for publication years ranging from 2012–2022 yielded 1,574 articles across three databases. Upon eliminating duplicates, 1,033 articles remained.
The remaining publications were subjected to title and abstract screening according to the inclusion criteria, which included relevancy, language (English or Indonesian), and study design. This procedure produced 104 articles for comprehensive assessment. After a comprehensive evaluation of the complete texts, 95 papers were removed due to factors such as irrelevant demographics, settings not located in developing nations, or incompatible study designs. As a result, nine papers were incorporated into the final synthesis.
3 Result
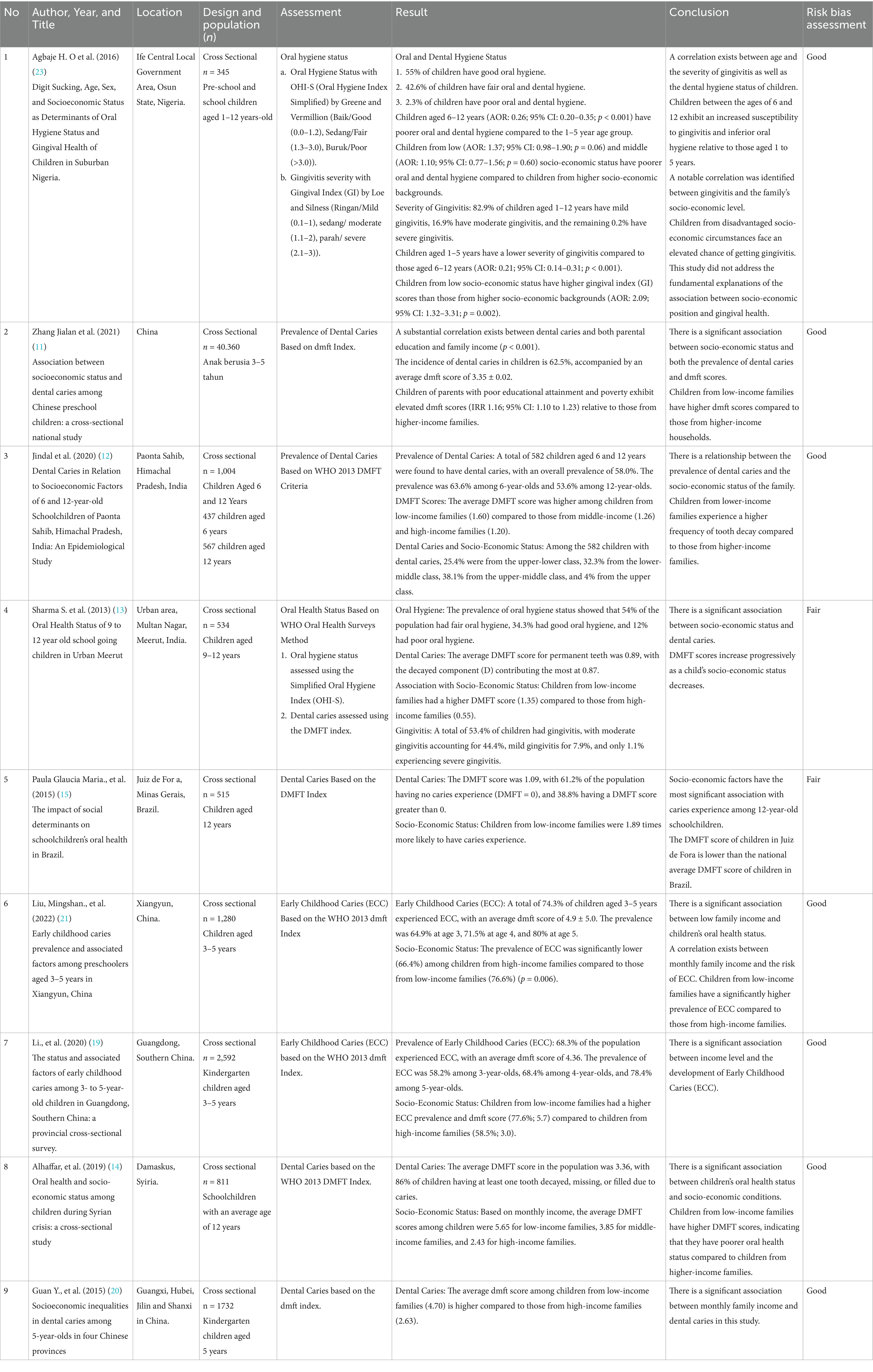
Following screening, 9 articles were included. Most were cross-sectional studies, with no randomized or interventional designs. Countries represented included China, India, Nigeria, Brazil, and Syria. Findings consistently showed that children from lower-income families had higher rates of: – Dental caries (via DMFT/dmft index): higher prevalence and severity – Early childhood caries: more frequent in low-SES families – Gingivitis: elevated GI scores among disadvantaged children – Oral hygiene: more poor/fair hygiene linked to economic disadvantage. Additional factors influencing outcomes included: – Parental education – Sugar consumption – Tooth brushing frequency – Access to dental services. Table 1 summarizes key findings. Table 2 reports the risk of bias assessment.
4 Discussion
This review highlights the persistent oral health gap between low- and high-income populations in developing countries. Despite methodological variation, all included studies support a strong association between poverty and poor dental outcomes.
Heterogeneity was observed in: – Age groups studied (1–5, 6–12, and 12 + years) – Oral health indices used – Definitions of income categories. Confounding variables—such as parental education, brushing habits, and sugar intake—were not consistently adjusted for, limiting causal inference.
All studies were observational. The lack of interventional or longitudinal data restricts conclusions about causality. Future studies should include these designs to assess the effectiveness of targeted public health intervention.
Socioeconomic factors, especially income level, play important roles in the dental and oral health status of individuals. The results revealed that people in low-income groups tend to have worse dental and oral health than those in high-income groups (8). This study revealed that oral health problems among children aged 0–18 years in developing countries included dental caries, early childhood caries, poor oral hygiene, and gingivitis are associated with low monthly household income.
4.1 Dental caries
A commonly used parameter for caries assessment is the decayed, missing, filled teeth (DMFT or dmft) index, which calculates the total number of decayed (D), missing (M), and filled teeth (F) (9). According to the World Health Organization (WHO), the DMFT index is primarily used to assess caries in permanent teeth, particularly among 12-year-old children, as a global indicator. The WHO classification includes five categories: very low (<1.2), low (1.2–2.6), medium (2.7–4.4), high (4.5–6.5), and very high (>6.5). However, this classification does not apply to primary teeth (dmft index), and there is no standardized WHO threshold for interpreting dmft scores across age groups. Therefore, caution is required when comparing caries severity across populations with different dentitions (10).
Five studies conducted in China (11), India (12, 13), Syiria (14), and Brazil (15) revealed a significant association between low socioeconomic status and high caries prevalence and severity in children from low-income families in developing countries. This association was demonstrated by the fact that children from low-income families had higher mean DMFT/dmft values than did children from high-income families. Studies conducted in China (3–5-year-old children) (11), India (12, 13) (6-, 9–12-, and 12-year-old children), and Syiria (14) (12-year-old children) have shown that more than 50% of the study population had caries. The dmft value in the Chinese study was 3.35 (11), whereas the DMFT values in the Indian study were 1.60 (12) and 1.35 (13), respectively, and the DMFT value in the Syrian study was 5.65 (14). These results support the impact of low family income on the prevalence and severity of caries among children in developing countries.
A Brazilian study of 12-year-old children reported a dental caries prevalence of 38.8%, which appears lower compared to the reported rates in studies from China, India, and Syria. However, direct comparison should be made with caution, as the Brazilian study focused on permanent dentition in adolescents, while the others primarily examined primary dentition in younger children. Differences in age, dentition type (DMFT vs. dmft), and epidemiological thresholds limit the comparability of these findings. Hence, it is more appropriate to compare studies with similar populations and dentition types. Nevertheless, among the 38.8% of children with dental caries, the risk of dental caries among children from low-income families was 1.89 times greater than that among children from high-income families (15).
The results of these five articles are consistent with those of previous studies showing that children from low-income families are more likely to experience severe toothaches and tooth decay (9). This finding supports the link between socioeconomic status and oral health and highlights that children from economically disadvantaged families are more likely to suffer from dental disease (9).
4.2 Early childhood caries
Early childhood caries (ECC) is a common oral health problem with a high prevalence in most countries (16, 17). This problem is more common in developing countries than in developed countries (18). The prevalence of ECC is usually assessed via the dmft index, which is similar to the method of assessing caries via the Caries Experience Classification established by the World Health Organization (WHO) in 2013 (10).
Multiple (multifactorial) factors contribute to the occurrence of early childhood caries (ECC), of which socioeconomic status is one of the most important influencing factors (16). A study conducted in Guangdong, China, reported that the prevalence of ECC in children aged 3–5 years was 68.3%. The overall mean dmft score was 3.72 ± 4.14, with children from families earning less than 3,000 yuan/month showing a higher mean dmft score (4.79 ± 4.49) compared to those from higher-income families (≥10,000 yuan/month) with a mean score of 2.34 ± 3.16 (19).
Another study conducted in four provinces in China (Guangxi, Hubei, Jilin, and Shanxi) reported similar results. The level of caries experience in this population was reflected in the dmft values of different monthly income groups. Children from low-income families had a dmft score of 3.29, children from middle-income families had a dmft score of 4.70, and children from high-income families had a lower DMFT score of 2.63 (20). A study in Xiangyun, China, also revealed a high prevalence of ECC in children aged 3–5 years (74.3%), with a dmft score of 4.9. Children from high-income families had a significantly lower prevalence of ECC (66.4%) than did those from low-income families (76.6%) (21).
These three studies conducted in China consistently revealed a significant association between oral health and socioeconomic inequality (19–21). The mean dmft scores among low-income children were significantly higher than in those from high-income families, suggesting a considerable caries burden in preschool-aged children.
The high prevalence of ECC in children from low-income families is closely related to the lack of awareness of the importance of healthy primary teeth. This lack of awareness remains a serious problem and further limits the access of families with lower socioeconomic status to optimal dentistry and dental care (18).
4.3 Gingivitis
Gingivitis is usually assessed via the gingival index (GI), which is considered a reliable indicator of the severity and extent of gingivitis (22). One study examined gingivitis in children aged 1–12 years in Nigeria and reported the prevalence of gingivitis in 983 children. The results revealed that 82.9% (815 children) had mild gingivitis, 16.9% had moderate gingivitis, and 0.2% had severe gingivitis. According to socioeconomic status, 75.5% of children from 21 low-income families had mild gingivitis, 24.1% had moderate gingivitis, and 0.3% had severe gingivitis (23).
A similar study in India reported that 53.4% of children had gingivitis. Among these patients, 44.4% had moderate gingivitis, and only 1.1% had severe gingivitis. The study also revealed that gingivitis was more common in children from low-income families than in children from high-income families (13).
4.4 Oral hygiene
A study in Nigeria examining children aged 1–12 years found no significant association between oral hygiene status and socioeconomic status (23). Another study in India on children aged 9–12 years reported varying levels of oral hygiene and noted that behavioral factors such as brushing frequency and sugar intake played a role (13). These findings highlight that oral hygiene may be influenced more by behavior than by socioeconomic status in some contexts.
4.5 Other factors influencing children’s dental and oral health
Other factors that influence children’s oral health include differences in parents’ education level (11, 14, 15), tooth brushing habits (19–21, 23), the consumption of sugary foods (12, 19, 20), and regular dental checkups (11, 14, 15, 19–21).
4.6 Limitations
The study included only publications in English or Indonesian. Gray literature, dissertations, and non-peer-reviewed studies were excluded. Most included studies were cross-sectional and limited in confounding control. No subgroup analysis by age group was conducted; future studies should stratify by developmental stage. The search strategy employed a combination of terms related to socioeconomic status and oral health to ensure comprehensive coverage of relevant literature. To balance specificity and inclusiveness, both general and specific terms related to poverty and oral health in children were incorporated.
5 Conclusion
This review consolidates evidence that low socioeconomic status (SES) is associated with poorer oral health in children in developing countries. Efforts to improve oral health equity should: – Prioritize early interventions in schools and community programs – Incorporate oral health into broader poverty-alleviation policies – Emphasize parent-focused education and access to preventive services.
Future research should adopt interventional or longitudinal designs, expand language and source inclusivity, and focus on age-specific strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AS: Supervision, Data curation, Methodology, Writing – review & editing, Software, Conceptualization, Investigation, Visualization, Writing – original draft, Formal analysis, Validation, Resources, Funding acquisition, Project administration. RI: Investigation, Data curation, Validation, Formal analysis, Writing – review & editing. SS: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Article Review Grant from Universitas Padjadjaran, Indonesia.
Acknowledgments
The authors would like to thank the Directorate of Research and Community Engagement (DRHPM), Universitas Padjadjaran, for their support in the completion of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. Generative AI was used to assist in Language editing and refinement of the manuscript draft. Structuring abstract and conclusion for clarity and conciseness. Translating and rephrasing specific sections from Indonesian to English. All content generated using AI was critically reviewed and edited by the authors to ensure accuracy, validity, and integrity in line with scholarly standards.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Management-screening D and T (MND). Global Oral health status report: towards universal health coverage for Oral health by 2030. World Health Organization, editor. Geneva: World Health Organization; (2022) 1–100W p.
2. World Health Organization (WHO). Oral health. Geneva: Achieving better oral health as part of the universal health coverage and noncommunicable disease agendas towards 2030. (2020); 1–6.
3. Armfield, JM, Mejía, GC, and Jamieson, LM. Socioeconomic and psychosocial correlates of oral health. Int Dent J. (2013) 63:202–9. doi: 10.1111/idj.12032
4. Steele, J, Shen, J, Tsakos, G, Fuller, E, Morris, S, Watt, R, et al. The interplay between socioeconomic inequalities and clinical oral health. J Dent Res. (2015) 94:19–26. doi: 10.1177/0022034514553978
5. World Health Organization. (2022). Global oral health status report: Towards universal health coverage for oral health by 2030. Geneva: World Health Organization; 100 p. Available online at: http://apps.who.int/bookorders (Accessed 04 April, 2025).
6. National Heart Lung and Blood Institute. Study quality assessment tools. Bethesda: National Heart, Lung, and Blood Institute (2013).
7. Zhenmin, L, Barcena, A, Kituyi, M, Alisjahbana, AS, Songwe, V, Dashti, R, et al. World economic situation and prospects 2020. New York: United Nations; (2020). Available online at: https://www.un.org/development/desa/dpad/ (Accessed 04 April, 2025).
8. Nutter, M. Disparities in Oral health: Socioeconomic status and policies to increase access to primary dental care. Omaha: University of Nebraska (2020).
9. Peres, MA, Macpherson, LMD, Weyant, RJ, Daly, B, Venturelli, R, Mathur, MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394:249–60. doi: 10.1016/S0140-6736(19)31146-8
10. Mitiche, A, and Ayed, IB. Oral health surveys basic methods. Springer Top Signal Process. (2013) 5:33–58.
11. Zhang, T, Hong, J, Yu, X, Liu, Q, Li, A, Wu, Z, et al. Association between socioeconomic status and dental caries among Chinese preschool children: a cross-sectional national study. BMJ Open. (2021) 11:e042908. doi: 10.1136/bmjopen-2020-042908
12. Jindal, L, Dua, P, Mangla, R, Gupta, K, Vyas, D, and Gupta, P. Dental caries in relation to socioeconomic factors of 6 and 12-year-old schoolchildren of Paonta sahib, Himachal Pradesh, India: an epidemiological study. Int J Clin Pediatr Dent. (2020) 13:395–8. doi: 10.5005/jp-journals-10005-1805
13. Sharma, S, Parashar, P, Srivastava, A, and Bansal, R. Oral health status of 9 to 12 year old school going children in urban Meerut. Indian J Community Health. (2013) 25:61–5.
14. Alhaffar, BA, Alawabdi, R, Barakat, L, and Kouchaji, C. Oral health and socio-economic status among children during Syrian crisis: a cross-sectional study. BMC Oral Health. (2019) 19:165. doi: 10.1186/s12903-019-0856-8
15. de Paula, JS, Ambrosano, GMB, and Mialhe, FL. The impact of social determinants on schoolchildren’s oral health in Brazil. Braz Oral Res. (2015) 29:1–9. doi: 10.1590/1807-3107BOR-2015.vol29.0098
16. Folayan, MO, El Tantawi, M, Aly, NM, Al-Batayneh, OB, Schroth, RJ, Castillo, JL, et al. Association between early childhood caries and poverty in low and middle income countries. BMC Oral Health. (2020) 20:1–8. doi: 10.1186/s12903-019-0997-9
17. Setiawan, AS, Indriyanti, R, Suryanti, N, Rahayuwati, L, and Juniarti, N. Neonatal stunting and early childhood caries: a mini-review. Front Pediatr. (2022):1–8. doi: 10.3389/fped.2022.871862/full
18. Kazeminia, M, Abdi, A, Shohaimi, S, Jalali, R, Vaisi-Raygani, A, Salari, N, et al. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: a systematic review and meta-analysis. Head Face Med. (2020) 16:1–21. doi: 10.1186/s13005-020-00237-z
19. Li, J, Fan, W, Zhou, Y, Wu, L, Liu, W, and Huang, S. The status and associated factors of early childhood caries among 3- to 5-year-old children in Guangdong, southern China: a provincial cross-sectional survey. BMC Oral Health. (2020) 20:265. doi: 10.1186/s12903-020-01253-w
20. Guan, Y, Zeng, X, Tai, B, Cheng, M, Huang, R, and Bernabé, E. Socioeconomic inequalities in dental caries among 5-year-olds in four Chinese provinces. Community Dent Health. (2015) 32:185–9.
21. Liu, M, Song, Q, Xu, X, and Lai, G. Early childhood caries prevalence and associated factors among preschoolers aged 3–5 years in Xiangyun, China: a cross-sectional study. Front Public Health. (2022) 10:959125. doi: 10.3389/fpubh.2022.959125
Keywords: oral health status, children, socioeconomic factors, poverty, developing countries
Citation: Setiawan AS, Indriyanti R and Sukmasari S (2025) Breaking the cycle: how poverty affects children’s oral health in developing nations—a rapid review. Front. Public Health. 13:1612026. doi: 10.3389/fpubh.2025.1612026
Edited by:
Callum Durward, University of Puthisastra, CambodiaReviewed by:
Sten Olof Martin Hellström, Karolinska Institutet (KI), SwedenAshek Elahi Noor, Atlantic Technological University, Ireland
Copyright © 2025 Setiawan, Indriyanti and Sukmasari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arlette Suzy Setiawan, YXJsZXR0ZS5wdXNwYUB1bnBhZC5hYy5pZA==
 Arlette Suzy Setiawan
Arlette Suzy Setiawan Ratna Indriyanti
Ratna Indriyanti Susi Sukmasari
Susi Sukmasari