- 1School of Nursing, Bengbu Medical University, Bengbu, Anhui Province, China
- 2Department of Human Resources, The Third Affiliated Hospital of Anhui Medical University, Hefei First People's Hospital, Hefei, Anhui Province, China
- 3The School of Nursing, The Philippine Women's University Manila, Manila, Philippines
Background: China faces escalating challenges in older care because of rapid population ageing and the high prevalence of multimorbidity among urban older adults. Traditional family-based and institutional care models are increasingly inadequate, necessitating innovative solutions like mutual aid older care. However, research gaps persist in understanding the prioritised needs of urban older with multimorbidity within mutual aid older care frameworks. This study evaluates and prioritises mutual aid older care needs for older adults with multimorbidity in urban Chinese communities, by integrating Maslow’s Hierarchy of Needs with the Kano Model.
Methods: A cross-sectional survey was conducted among 240 older adults (aged ≥65, with ≥2 chronic conditions) across 25 urban communities in Hefei, China. Using a validated questionnaire, 43 service items across safety/health, daily life, learning/socialisation, spiritual, and entertainment domains were assessed. Kano Model categorisation and better-worse coefficient analysis were applied to classify needs (must-be, one-dimensional, attractive, indifferent) and rank priorities via sensitivity calculations.
Results: Key must-be needs included cooking, washing hair, and psychological counselling, while one-dimensional priorities emphasised exercise and travelling. Attractive needs featured telemedicine and cultural activities (e.g., Red Song Club). Indifferent items, such as pest control, had minimal impact on satisfaction. The analysis highlighted the centrality of physical health services, mental health support, and social engagement in enhancing quality of life.
Discussion: Urban older adults with multimorbidity prioritise integrated care models addressing both basic survival needs and higher-order psychosocial well-being. Mutual aid older care frameworks must therefore balance healthcare accessibility with opportunities for social participation and emotional fulfilment. Future policies should adopt evidence-based, culturally tailored strategies to optimise resource allocation and foster sustainable ageing-in-place solutions. Limitations include geographic specificity and cross-sectional design, warranting broader longitudinal and mixed-method research.
1 Introduction
Population ageing has emerged as a global challenge, profoundly impacting socio-economic systems, healthcare infrastructure, and intergenerational dynamics (1). China, with over 209 million individuals aged 65 and above—accounting for 14.9% of its population—in 2022, faces accelerated demographic shifts, as it is expected to transition into a ‘moderately ageing society’ by 2030 (2). This demographic shift coincides with the increasing incidence of long-term health conditions and overlapping chronic illnesses (individuals living with multiple persistent medical issues), which particularly impact older populations (3). Studies indicate that 44.1% of older Chinese citizens experience multiple chronic conditions, worsening risks of physical limitations, diminished life quality, and earlier mortality (4, 5). Simultaneously, traditional family-based care systems face pressures owing to urban migration, smaller household sizes, and differing lifestyle expectations between generations, creating an urgent need for new solutions to older care gaps (6).
In response, mutual aid older care—arrangements that involve older adults assisting each other through shared resources and local community networks—has emerged as a viable alternative. This model emphasises active ageing, enabling older adults to shift from being passive care receivers to engaged contributors (7). International models—for instance, multigenerational households in Germany and community-based initiatives in the United States, demonstrate the potential to strengthen social connections and reduce reliance on formal institutions (8, 9). In China, trial programmes in cities and rural areas have revealed positive outcomes in addressing isolation, enhancing psychological well-being, and easing family care responsibilities (10). However, existing research primarily examines rural settings or general groups of older adults; thus, urban communities, especially those dealing with multiple health conditions, have been hitherto overlooked (11, 12).
Current studies identify structural obstacles limiting the expansion of mutual aid models in urban China, including inadequate policy frameworks, financial resource limitations, supply–demand imbalance, and limited engagement of older adults owing to scepticism or insufficient awareness (13, 14). Furthermore, while research recognises the specific difficulties posed by multiple chronic conditions—such as complicated care requirements and greater resource needs—a notable gap remains in understanding how these challenges interact with mutual aid systems (15). Existing analyses often use qualitative methods or overlook variations between older adult subgroups, leading to oversimplified suggestions that lack practical depth (16).
Therefore, the present study aims to employ Maslow’s Hierarchy of Needs as the primary theoretical framework to comprehensively assess the mutual support needs of older adults with multiple chronic conditions through a multidimensional questionnaire survey. This investigation systematically examines five critical dimensions—safety and health requirements, life requirements, learning and social needs, spiritual needs, and entertainment needs—while conducting an internal prioritisation analysis to identify hierarchical demand patterns. The ultimate objective is to establish an evidence-based hierarchy that addresses the most urgent requirements for multimorbid older adults in mutual-aid older care scenarios, thereby providing empirical guidance for targeted service optimisation.
This study adopted Maslow’s Hierarchy of Needs as the theoretical foundation for qualitative data collection. The framework conceptualises human needs as a five-tiered hierarchical pyramid, progressing from physiological needs (base level) to safety needs, love/belonging, esteem needs, and self-actualisation (apex level). As a seminal psychological theory of motivation, it posits that human needs follow a sequential hierarchy, with survival-oriented physiological requirements forming the foundational layer, while self-actualisation—the pursuit of personal potential—occupying the highest tier (17). Building on this framework, the research investigates mutual aid needs among urban-dwelling older adults with multimorbidity. It not only emphasises the fulfilment of basic physiological necessities but also addresses higher-order needs, such as emotional support, cultural engagement, and recreational activities. By prioritising these needs based on urgency, the study proposes stratified intervention strategies to address the most critical older care gaps.
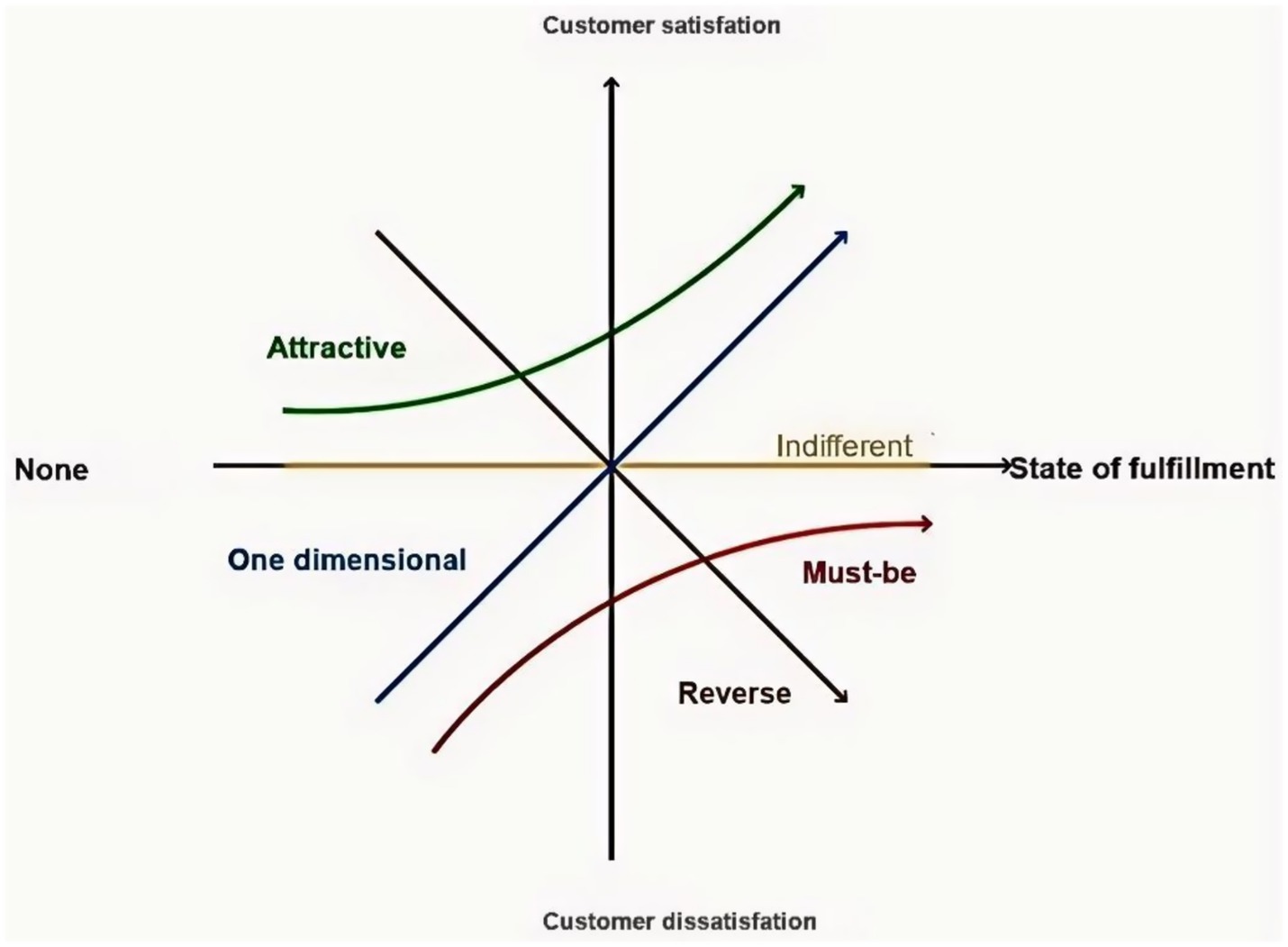
The Kano Model is a method proposed by Noriaki Kano to identify quality, customer needs, and customer satisfaction attributes in quality management, industrial engineering, and business administration (Figure 1). Considered an effective tool for identifying and prioritising the individual needs of patients, it has been extended to medical quality management studies such as patient satisfaction, the need for remote care services for older adults in the community, and more (18). In this study, the Kano Model guides the prioritisation of strategies, ensuring that resource allocation aligns with the mutual aid older care needs of older adults with multimorbidity in urban China.
2 Materials and methods
2.1 Participants
The participants in this study were older adults living in 25 urban communities in Hefei, Anhui Province, China. The inclusion criteria of the study were: (1) voluntary participation after signing the informed consent form; (2) age ≥ 65 years; (3) at least 1 year of residence within the community; (4) multimorbidity with two or more chronic diseases; (5) mentally and intellectually normal, with the ability to understand and answer questions correctly; and (6) no limitation to physical mobility. The exclusion criteria were older adults with multimorbidity within the urban community who do not meet the above inclusion criteria. Such participants were automatically excluded from the study.
2.2 Sampling method and sample size
Purposive sampling was the method employed in the study. In multivariate analyses, the sample size should ideally be 5–10 times that of the study factor. A total of 43 influencing factors were included in the questionnaire used in this study. The estimated minimum sample size was 43 × 5 = 215 cases, while the estimated maximum sample size was 43 × 10 = 430 cases. We collected not less than 215 cases, considering time and conditions. A total of 244 participants were selected for the first phase of the survey study. Ultimately, 240 valid questionnaires were collected.
2.3 Research instruments
2.3.1 Demographic questionnaire
A self-designed instrument was used administered to collect participants’ basic information (e.g., age, gender, health status). Reliability and validity tests were deemed unnecessary owing to the instrument’s descriptive nature.
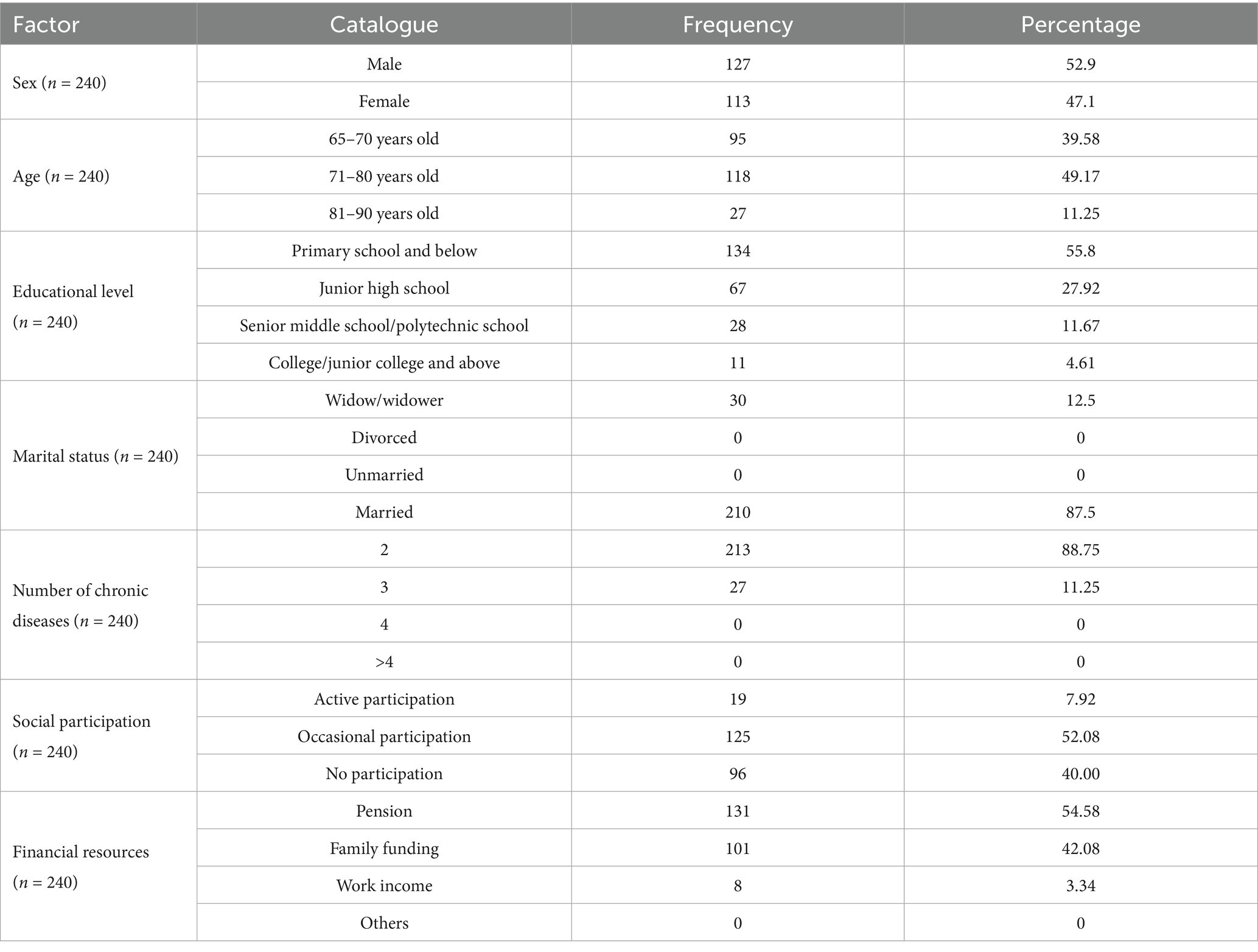
2.3.2 Mutual aid older care service demand questionnaire
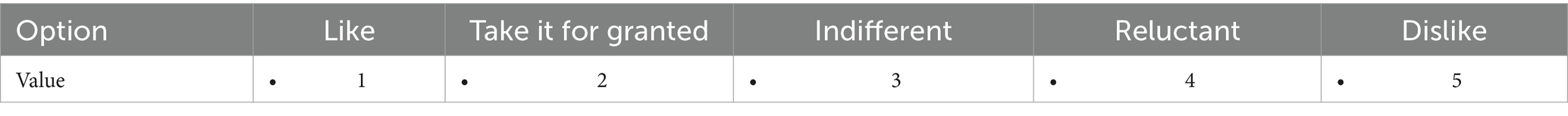
Adapted from Zhou et al. (19) with written authorisation, the Mutual Aid Older Care Service Demand Questionnaire assessed five categories (safety/health, daily life, learning/socialisation, spiritual, and entertainment needs) aligned with Maslow’s Hierarchy of Needs. It comprised 43 paired items (positive and negative sub-questions), each rated on a 5-point Likert scale (ranging from “like” to “dislike”), as shown in Table 1. Responses were mapped to Kano attributes to classify service preferences. For example, paired questions—such as “How would you feel about having/ not having a home hair wash service?”—allowed the identification of critical, attractive, or indifferent needs.
2.4 Reliability and validity analysis
The questionnaire’s reliability and validity were rigorously tested. Cronbach’s α coefficients were interpreted as follows: 0.6–0.7 (acceptable), 0.7–0.8 (good), and >0.8 (excellent). Values below 0.6 necessitated scale revision. An SPSS 25.0 analysis revealed an overall Cronbach’s α of 0.905, confirming high internal consistency. To determine validity, the Kaiser-Meyer-Olkin (KMO) measure (>0.9 = excellent; 0.8–0.9 = good; 0.7–0.8 = acceptable) and Bartlett’s sphericity test were applied. The questionnaire revealed a KMO value of 0.759 and a significant Bartlett’s test (χ2 = 6830.828, p < 0.001), indicating adequate validity for factor analysis at p < 0.05.
2.5 Analysis and interpretation
2.5.1 Descriptive statistics
Demographic data were analysed using SPSS 26.0, with categorical variables presented as frequencies (percentages).
2.5.2 Kano model classification
The evaluation of the Mutual Aid Elderly Care Needs Questionnaire was based on the results of the questionnaire for the classification of service needs. Statistical analyses were performed based on these results, and the attribute with the largest proportion was considered the requirement classification. A total of 25 permutations and combinations of each set of forward and negative problems were counted, as shown in Table 2.
2.5.3 Better-worse coefficient analysis
Satisfaction (Better/SI) and dissatisfaction (Worse/DSI) coefficients were calculated to rank service priorities, as follows:
Higher better values indicated stronger satisfaction enhancement, while higher worse values reflected greater risk of dissatisfaction.
2.5.4 Sequencing mutual aid older care service demands
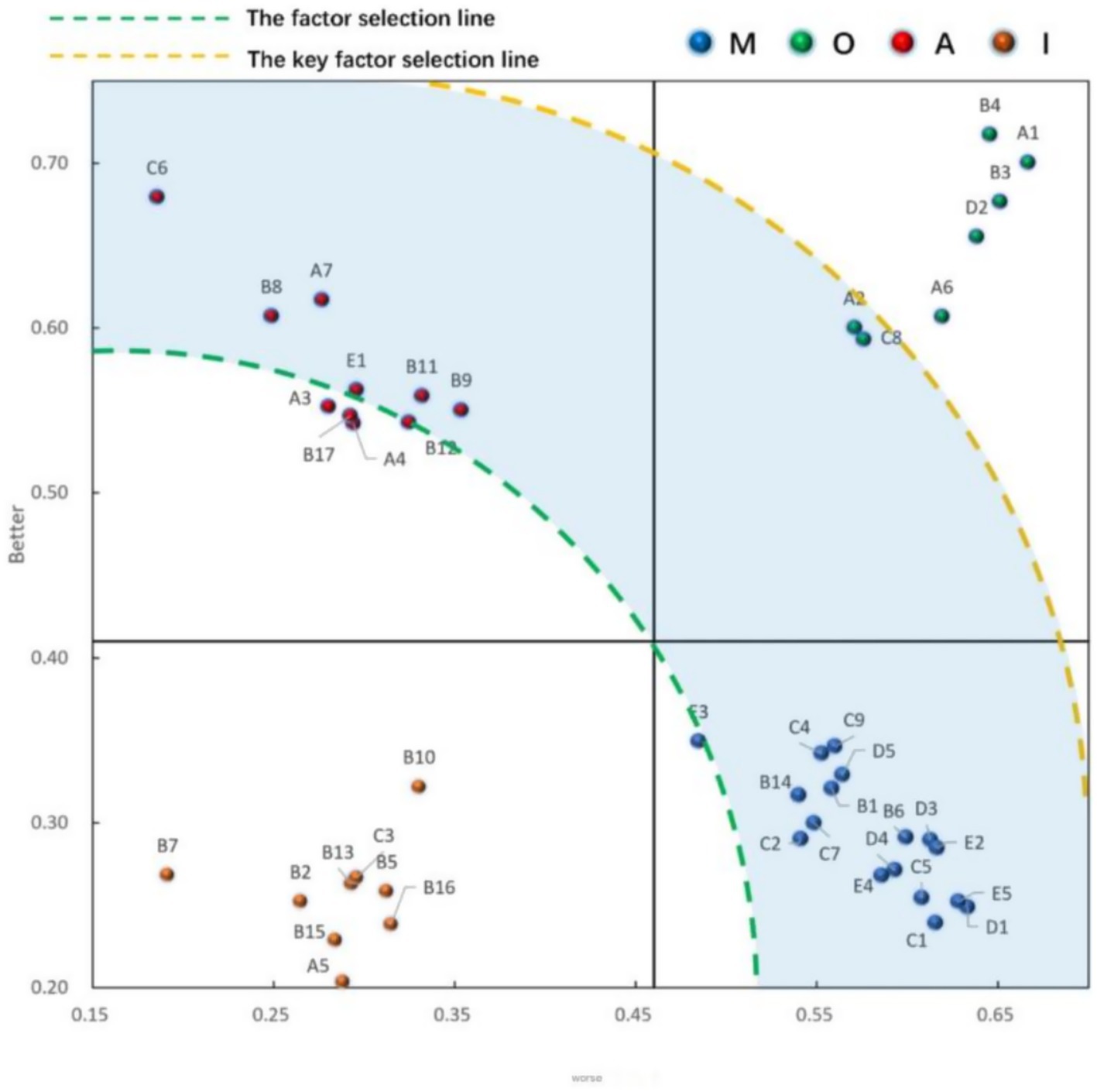
The mutual older care demand prioritisation model, based on the element screening method, constructs an SI (better value) versus DSI (absolute worse value) matrix. Element (radius 0.707) and key element (radius 1.061) selection lines are plotted as quarter-arc boundaries from the origin. Demand priorities are classified by calculating the sensitivity (R-value)—the perpendicular distance from discrete points to the element selection line: right-side demands (points to the right of the key element line) require immediate improvement (highest priority); left-side demands can be deferred based on practical conditions. Higher sensitivity values indicate greater urgency, guiding resource allocation to address critical needs first. This spatial positioning system quantifies demand hierarchy, optimising resource distribution for older care services.
2.6 Ethical considerations
This study was approved by the Ethics Review Committee of the Philippine Women’s University. It adhered to the ethical standards pertaining to obtaining informed consent in writing and reading and checking the questionnaire before the participant completes it, especially if the participant chooses to remain anonymous. The considerations respected participants’ intention or reason for participating in the study, included an explanation of the study process, and affirmed the participants’ right to refuse to join the study and voluntarily withdraw from the study for any reason, at any stage, without penalty.
3 Results
3.1 General information
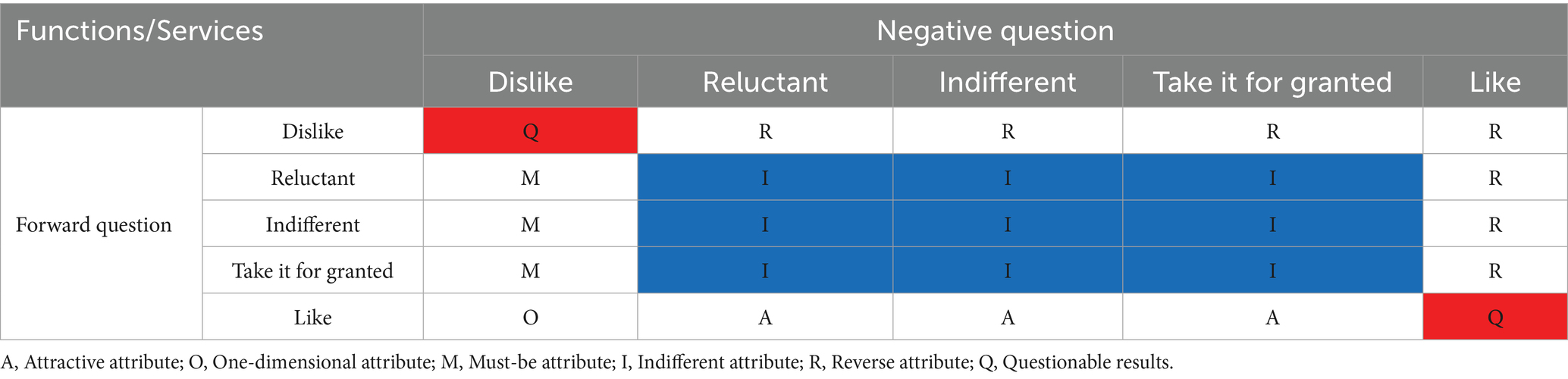
The demographic profile of older adults with multimorbidity in urban China reveals a male-dominated cohort (52.9%), predominantly aged between 65 and 80 years (88.75%), with limited educational attainment (55.8% primary education or below). This aligns with studies linking low health literacy to challenges in chronic disease management among less-educated seniors (20). Marital status reveals a potential familial support system (87.5% married), although widowed individuals (12.5%) highlight isolation risks, compounded by low social participation, with 40% never having engaged in social activities and 52.08% participating only occasionally. Such disconnection exacerbates mental and physical health decline, particularly in multimorbidity contexts (21).
Financial vulnerability is evident, with 54.58% relying on pensions and 42.08% on family support, reflecting systemic gaps in economic security amid rising healthcare costs (22). These challenges mirror broader trends in urban older care, with ageing populations facing intersecting burdens of health decline, social isolation, and financial strain (Table 3).
3.2 Kano attributes and calculation of the better-worse coefficient
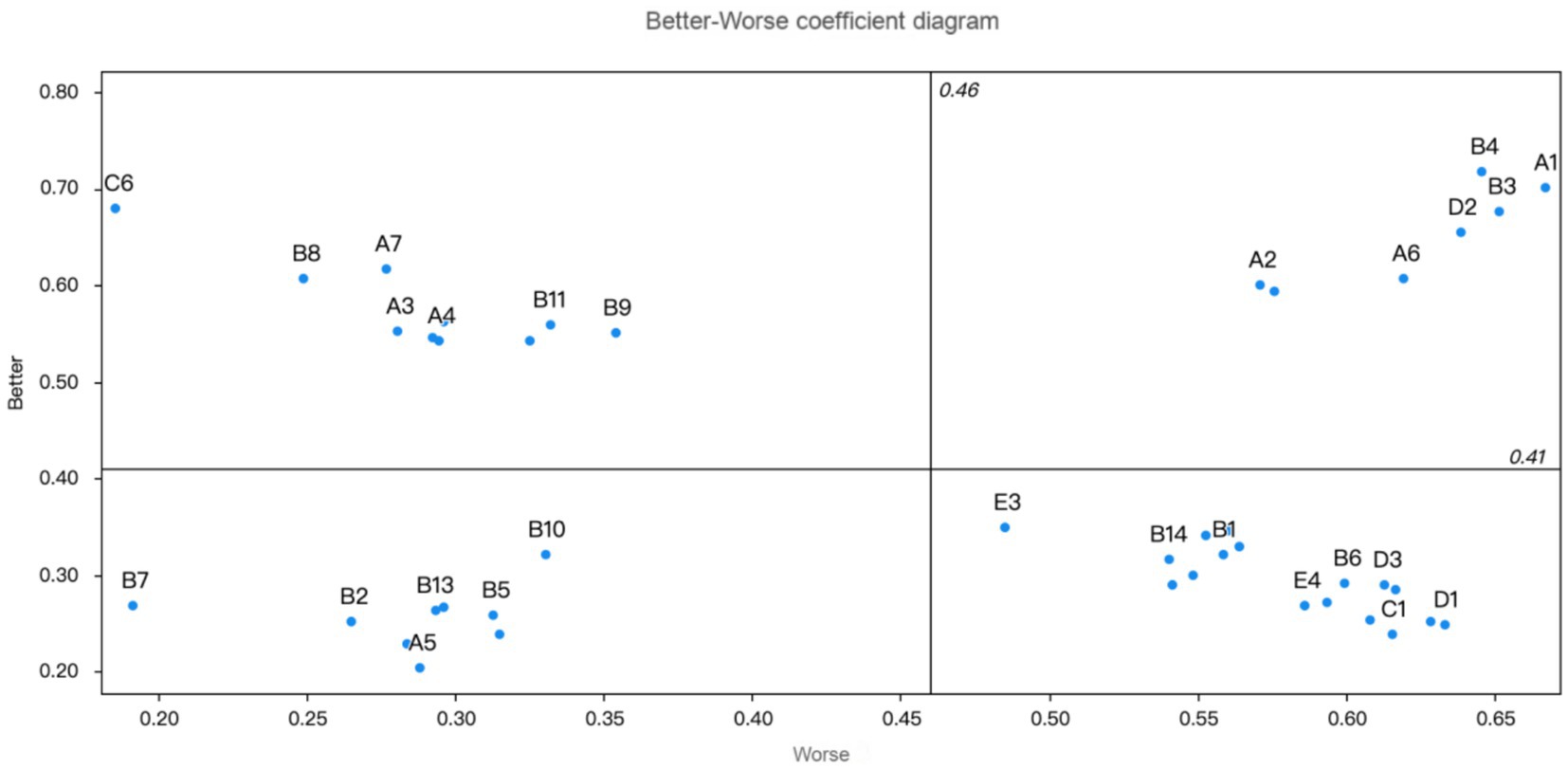
The priority order of mutual aid older care needs for older adults with multimorbidity in urban communities, as depicted in Table 4, categorises care needs into four groups: must-be (M), one-dimensional (O), attractive (A), and indifferent (I), emphasising the relative importance of various services in enhancing the quality of life for older adults, as determined by the better–worse coefficient analysis. Specifically, B1, B6, B14, C1, C2, C5, C4, C7, C9, D1, D3, D4, D5, E2, E3, E4, and E5 were identified as must-be qualities; A1, A2, A6, B3, B4, C6, and C8 as one-dimensional qualities; A3, A4, A7, B8, B9, B11, B12, B17, C6, and E1 as attractive qualities; and A5, B2, B5, B7, B10, B13, B15, B16, and C3 as indifferent qualities (Table 4; Figure 2).

Table 4. Kano attributes and better–worse coefficients of demand for older care older adults with multimorbidity.
3.3 Internal priority order calculation results
Finally, we derived the internal priority of each function/service item by using the important sensitivity calculation:
The internal priority calculation results for each function/service item are presented in Table 5 and Figure 3. The top five improvement elements are exercise, boiling traditional Chinese medicine, travelling, haircutting, and psychological counselling. These findings suggest that community managers should concentrate on these five needs of older adults with multiple chronic conditions and prioritise enhancements based on the community department’s actual situation.
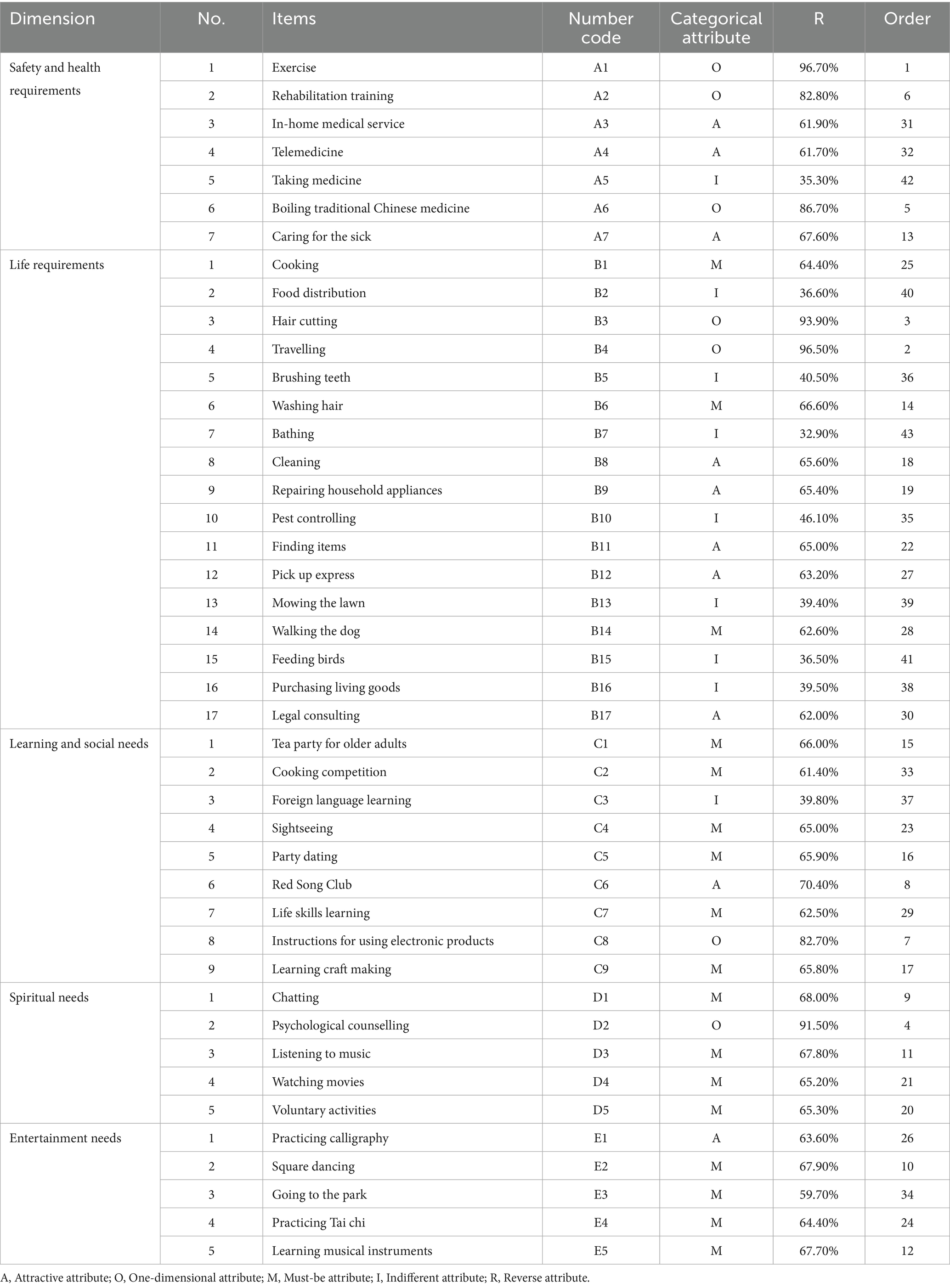
Table 5. The internal priority order calculation results of demand for older care among older adults with multimorbidity.
4 Discussion
The findings of this study provide critical insights into the prioritised needs of older adults with multimorbidity in urban Chinese communities under the mutual aid older care framework. Our investigation identified 17 must-be demands, 7 one-dimensional demands, 10 attractive demands, and 9 indifferent demands. We also identified five factors that urgently require improvement while sorting internal priorities. By integrating the Kano Model with Maslow’s Hierarchy of Needs, this analysis highlights the multidimensional nature of older care requirements, emphasising the interplay between basic survival needs and higher-order psychosocial well-being.
4.1 Safety and health requirements
Exercise and rehabilitation training emerged as one-dimensional (O) attributes, indicating their direct correlation with satisfaction. This aligns with existing research, which emphasises the importance of physical activity in maintaining older adults’ health and mobility, particularly for those with multiple chronic conditions. Exercise programmes help manage conditions such as hypertension, arthritis, and diabetes, all of which are common among older adult populations (23, 24). Notably, in-home medical services and telemedicine were categorised as attractive (A) attributes, reflecting their growing role in urban older care. Research reveals that telemedicine has become an increasingly important tool in managing chronic diseases remotely, especially in urban settings where healthcare infrastructure can support such technology (25). However, medication management, classified as indifferent (I), suggests that older individuals perceive it as routine rather than as a service requiring external support, underscoring the need for targeted health literacy programmes.
4.2 Life requirements
Must-be (M) attributes, such as cooking and hair washing, underscore the foundational role of daily living assistance. Research reveals that older adults, particularly those with multimorbidity, heavily rely on such basic care activities to maintain their quality of life, as these tasks become harder to manage independently with advancing age and chronic illness (26). Conversely, attractive attributes such as cleaning and repairing appliances underscore the value of convenience-enhancing services, which align with the provision of a clean and functional home environment. This is crucial to maintain the comfort and safety of older adults, contributing to their overall sense of security and well-being (27). The indifferent response to pest control and food distribution suggests that such tasks may already be managed informally, emphasising the need for community needs assessments to avoid resource misallocation.
4.3 Learning and social needs
Social activities such as tea parties for older adults and cooking competitions were classified as must-be attributes, reinforcing the critical role of social engagement in mitigating isolation. Although their presence does not significantly elevate satisfaction, their absence leads to considerable dissatisfaction, suggesting that these activities are crucial to maintain social engagement and prevent isolation among older adults (28). The Red Song Club, an attractive attribute. Highlights the cultural significance of activities that involve engaging in nostalgic and collective experiences, which provides a strong sense of community and emotional satisfaction. Such social activities help older adults relive shared histories and foster social bonds, contributing to emotional well-being and social connection (29, 30). Meanwhile, the indifferent response to foreign language learning suggests a preference for practical, health-focused interventions over skill acquisition. This aligns with broader findings that older adults in urban communities with multimorbidity prioritise social and recreational activities that are more immediately relevant to their cultural and social lives, rather than learning new skills they do not deem essential (20).
4.4 Spiritual needs
Psychological counselling, categorised as one-dimensional, highlights the unmet demand for mental health support in ageing populations. This aligns with existing research that highlights psychological support needs, particularly for older adults dealing with multiple chronic health issues, to help them manage stress, depression, and anxiety (31, 32). Listening to music and watching movies are important must-have attributes. The positive effect of music can lower anxiety levels and help with mental abilities, while watching movies offers stimulation and enjoyment, according to recent findings (33, 34). Volunteer work and casual conversations, both of which are essential attributes, reveal the necessity of ongoing social contact to fight loneliness and preserve purpose. In other words, volunteering helps older adults stay active while contributing to their communities, which research indicates boosts self-esteem and decreases feelings of isolation (35). Meanwhile, chatting is an easy but vital way to connect socially, addressing loneliness concerns common among those managing multiple health problems (36).
4.5 Entertainment needs
Among entertainment-related needs, calligraphy practice emerges as an appealing attribute owing to its creative expression and mental involvement. Studies suggest that activities like this can reduce anxiety levels, promote relaxation states, and support cognitive functions among older adults (37). As an art form with deep cultural roots, calligraphy strengthens cultural connections and feelings of personal accomplishment. Square dancing, classified as a fundamental attribute, remains widely popular among urban Chinese older adults, providing health benefits and social interaction chances. Moreover, regular practice is key for sustaining both body fitness and emotional wellness, as evidenced in recent analyses (38). Similarly, Tai chi exercises and musical instrument learning reveal positive impacts on well-being, although their effects differ across individuals. These observations underline how combining physical activities with mental engagement approaches can enhance the quality of life for seniors facing complex health challenges (24, 25).
Internal priority assessments identified five key need areas as urgent priorities for mutual aid older care among older adults with multiple chronic conditions: exercise, boiling traditional Chinese medicine, psychological counselling, travelling, and haircutting. The strong focus on exercise and boiling traditional Chinese medicine, both of which relate to basic health and safety requirements, reveals the need for expert guidance in physical recovery while simultaneously highlighting the lasting role of traditional medicinal practices in caring for older adults. The ongoing challenges of financial pressures combined with the emotional strain caused by long-term health issues underline the importance of supportive psychological services. Travelling, which serves as bridges between people, demonstrates potential benefits in reducing loneliness and stress through community interactions. The mention of haircutting services, which help maintain personal dignity, further illustrates how basic care needs intersect with emotional well-being.
The findings align with Maslow’s Hierarchy of Needs, showing that older adults prioritise survival needs while still valuing social belonging and personal growth opportunities. This dual focus challenges conventional care approaches that concentrate only on medical treatment for older adults, suggesting combined strategies that address whole-person wellness instead. Policy makers should consider practical solutions while developing community-based social initiatives to strengthen sustainable mutual aid older care models.
This research has several noteworthy limitations. First, the study design based on single-timepoint data collection limits cause–effect conclusions. Second, the geographical limitation to urban centres affects the generalisability of these findings to rural areas or regions with different cultural backgrounds. Third, reliance on self-reported information may lead to response inaccuracies, particularly among participants with memory challenges. Future studies should use long-term observation methods combined with multiple data types to not only track changing needs over time but also examine urban–rural differences. Moreover, exploring technology-based solutions could help address scalability issues in community-led older care systems.
5 Conclusion
This research seeks to identify the care requirements for older adults dealing with multiple chronic conditions in urban Chinese communities through the integration of Maslow’s Hierarchy of Needs and the Kano Model. The findings from this investigation highlight a hierarchical structure in need prioritisation, such as exercise programmes and rehabilitation training, psychological support areas including counselling sessions and opportunities for social interaction, as well as culturally meaningful activities such as participation in Red Song Club groups or Tai chi practice. These elements collectively contribute to improving life quality among older adults with multimorbidity and provide precise guidance for the formulation of policies linked to mutual aid older care needs.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Philippine Women’s University Research Ethics Review Board reviewed the above-named research project. The Philippine Women’s University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZZ: Data curation, Writing – original draft, Investigation, Writing – review & editing. YC: Data curation, Funding acquisition, Writing – review & editing, Writing – original draft. MO: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Health Research Project of Anhui Province (Grant No. AHW2023A20195) and the Program for Advancing Basic-Clinical Research Collaboration, The Third Affiliated Hospital of Anhui Medical University (Grant No. 2022sfy011). These funding bodies had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to thank the participants for their supports in making this study possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dai, K, and Guo, YC. Population aging, social security expenditure and economic growth. Stat. Theory Pract. (2024) 3:40–46. doi: 10.13999/j.cnki.tjllysj.2024.03.006
2. China National Bureau of Statistics (2023). Statistical public report of the people’s republic of China on National Economic and social development in 2022. Available online at: https://www.stats.gov.cn/sj/zxfb/202302/t20230228_1919011.html (Accessed March 20, 2025).
3. Skou, ST, Mair, FS, Fortin, M, Guthrie, B, Nunes, BP, Miranda, JJ, et al. Multimorbidity. Nat Rev Dis Primers. (2022) 8:48. doi: 10.1038/s41572-022-00376-4
4. Han, S, Mo, G, Gao, T, Sun, Q, Liu, H, and Zhang, M. Age, sex, residence, and region-specific differences in prevalence and patterns of multimorbidity among older Chinese: evidence from Chinese longitudinal healthy longevity survey. BMC Public Health. (2022) 22:1116. doi: 10.1186/s12889-022-13506-0
5. Yu, X, and Zhang, W. Neighborhood’s locality, road types, and residents’ multimorbidity: evidence from China’s middle-aged and older adults. BMC Public Health. (2020) 20:1728. doi: 10.1186/s12889-020-09876-y
6. Yan, GX, Yan, J, and Yuan, WX. Challenges and countermeasures of elderly care in the context of population aging. J Nurs. (2023) 38:117–20. doi: 10.3870/j.issn.1001-4152.2023.10.117
7. Fan, YX, Zhao, L, Zeng, HJ, Xie, Y, Luo, M, Luo, WY, et al. Research progress on mutual elderly care for the elderly in the context of active aging. J Nurs. (2023) 21:038. doi: 10.3870/j.issn.1001-4152.2023.21.122
8. Hünteler, B. A new perspective on the generational structures of families–generational placements over the life course. Adv Life Course Res. (2022) 51:100450. doi: 10.1016/j.alcr.2021.100450
9. Aziiza, AA, and Susanto, TD. “The smart village model for rural area (case study: Banyuwangi regency).” In: IOP Conference Series: Materials Science and Engineering (722, 1, p. 012011). IOP Publishing (2020).
10. Yang, HY. Research hotspots and trends of mutual elderly care for the elderly. Coop Econ Sci Technol. (2023) 20:173–5. doi: 10.13665/j.cnki.hzjjykj.2023.20.033
11. Zhang, J. Dilemma and Path for Rural Mutual Aid Elderly Care Model in Underdeveloped Areas—A Case Study of Dazhou City in Sichuan Province. Asian Agric. Res. (2019) 11:5–9. doi: 10.19601/j.cnki.issn1943-9903.2019.1.002
12. Zhang, WL. The Essence of “Contract” in China’s Rural Mutual Aid for the Aged: A Discussion Based on Transaction Cost Theory. Popul. Econ. (2022) 5:1–15. doi: 10.3969/j.issn.1000-4149.2022.00.028
13. Bao, PP, and Liu, H. The Status Quo, Problems and Countermeasures of Mutual Aid for the Elderly in Ningbo’s Urban Communities: From the Perspective of Future Community Construction. Commer. Exhib. Econ. (2022) 24:100–102. doi: 10.19995/j.cnki.CN10-1617/F7.2022.24.100
14. Liu, XM, and Liu, BB. Research on the Internal Behavioral Logic and Practical Path of Rural Mutual Aid for the Elderly from the Perspective of Social Exchange Theory. Iss. Agric. Econ. (2021) 9:80–89. doi: 10.13246/j.cnki.iae.2021.09.009
15. Quiñones, AR, Hwang, J, Heintzman, J, Huguet, N, Lucas, JA, Schmidt, TD, et al. Trajectories of chronic disease and multimorbidity among middle-aged and older patients at community health centers. JAMA Netw Open. (2023) 6:e237497. doi: 10.1001/jamanetworkopen.2023.7497
16. Fu, NY, He, JJ, and Shan, B. Investigation on Participation Willingness and Influencing Factors of Rural Mutual Aid for the Elderly in Hainan Province under the Background of Rural Revitalization. Soft Sci. Health. (2024) 38:36–41. doi: 10.3969/j.issn.1003-2800.2024.11.008
17. Huang, W. An Exploration of Needs within Maslow’s Hierarchy of Motivation. Adv. Soc. Behav. Res. (2024) 14:41–44. doi: 10.54254/2753-7102/2024.19284
18. Yao, X, Li, J, He, J, Zhang, Q, Yu, Y, He, Y, et al. A Kano model-based demand analysis and perceived barriers of pulmonary rehabilitation interventions for patients with chronic obstructive pulmonary disease in China. PLoS One. (2023) 18:e0290828. doi: 10.1371/journal.pone.0290828
19. Zhou, Z, Wang, L, and Dong, Y. Research on innovative design of community mutual aid elderly care service platform based on Kano model. Heliyon. (2023) 9:e15546. doi: 10.1016/j.heliyon.2023.e15546
20. van der Gaag, M, Heijmans, M, Spoiala, C, and Rademakers, J. The importance of health literacy for self-management: a scoping review of reviews. Chronic Illn. (2022) 18:234–54. doi: 10.1177/17423953211035472
21. Luster, JE, Ratz, D, and Wei, MY. Multimorbidity and social participation is moderated by purpose in life and life satisfaction. J Appl Gerontol. (2022) 41:560–70. doi: 10.1177/07334648211027691
22. Singh, A, Contreras Suarez, D, You, E, Fleitas Alfonzo, L, and King, T. Role of social support in the relationship between financial hardship and multimorbidity-a causal mediation analysis. Eur J Pub Health. (2021) 31:482–7. doi: 10.1093/eurpub/ckab015
23. Edwards, JJ, Coleman, DA, Ritti-Dias, RM, Farah, BQ, Stensel, DJ, Lucas, SJE, et al. Isometric exercise training and arterial hypertension: an updated review. Sports Med. (2024) 54:1459–97. doi: 10.1007/s40279-024-02036-x
24. Valenzuela, PL, Saco-Ledo, G, Morales, JS, Gallardo-Gómez, D, Morales-Palomo, F, López-Ortiz, S, et al. Effects of physical exercise on physical function in older adults in residential care: a systematic review and network meta-analysis of randomised controlled trials. Lancet Healthy Longev. (2023) 4:e247–56. doi: 10.1016/S2666-7568(23)00057-0
25. Ghouchan Nezhad Noor Nia, R, Arzehgar, A, Dehdeleh, V, and Eslami, S. Telemedicine based on human activity recognition in elderly healthcare. Stud Health Technol Inform. (2023) 302:987–91. doi: 10.3233/SHTI230323
26. Storeng, SH, Vinjerui, KH, Sund, ER, and Krokstad, S. Associations between complex multimorbidity, activities of daily living and mortality among older Norwegians. A prospective cohort study: the HUNT study, Norway. BMC Geriatr. (2020) 20:21. doi: 10.1186/s12877-020-1425-3
27. Kivimäki, T, Stolt, M, Charalambous, A, et al. Safety of older people at home: An integrative literature review. Int J Older People Nurs. (2020). 15:e12285. doi: 10.1111/opn.12285
28. Kim, YM, Jang, SN, and Cho, SI. Working hours, social engagement, and depressive symptoms: an extended work-life balance for older adults. BMC Public Health. (2023) 23:2442. doi: 10.1186/s12889-023-17072-x
29. Zhou, TH. (2023). Research on social support for rural-urban migrating elderly populations [master's thesis]. [Guizhou]: Guizhou University of Finance and Economics.
30. Wang, CF (2020). Research on aging adaptability of outdoor activity spaces in residential areas from the perspective of health promotion [doctoral dissertation, Hebei University of Technology].
31. Ren, T, Liang, SX, Guo, ZY, and Liu, MQ. Research progress on the status and influencing factors of medical and nursing needs in elderly patients with multimorbidity. Evid Based Nurs. (2025) 11:234–8. doi: 10.12102/j.issn.2095-8668.2025.02.008
32. Hung, HY, Azman, A, and Jamir Singh, PS. The impact of counseling on the dignity of older people: protocol for a mixed methods study. JMIR Res Protoc. (2023) 12:e45557. doi: 10.2196/45557
33. Lorber, M, and Divjak, S. Music therapy as an intervention to reduce blood pressure and anxiety levels in older adults with hypertension: a randomized controlled trial. Res Gerontol Nurs. (2022) 15:85–92. doi: 10.3928/19404921-20220218-03
34. Brown Wilson, C, Arendt, L, Nguyen, M, Scott, TL, Neville, CC, and Pachana, NA. Nonpharmacological interventions for anxiety and dementia in nursing homes: a systematic review. Gerontologist. (2019) 59:e731–42. doi: 10.1093/geront/gnz020
35. Hsu, HF, Chen, KM, and Belcastro, F. Types of voluntary work and influence of participation for older volunteers: a systematic review of qualitative studies. J Gerontol Soc Work. (2023) 66:1019–42. doi: 10.1080/01634372.2023.2205908
36. Martínez, RA, Aguilar, AT, Moreno, CJ, and Jiménez-Delgado, JJ. Qualitative analysis of conversational chatbots to alleviate loneliness in older adults as a strategy for emotional health. Health. (2023) 12:62. doi: 10.3390/healthcare12010062
37. Han, YL. (2024). Aging-friendly design of Xi’an Labor Park from a health promotion perspective [master’s thesis]. [Xi’an]: Xi’an University of Architecture and Technology.
Keywords: mutual aid, older care needs, multimorbidity, Kano model, population ageing
Citation: Zhang Z, Chen Y and Ochoa MC (2025) Assessment of mutual aid older care needs for older adults with multimorbidity in urban China: a Kano model-based study. Front. Public Health. 13:1612187. doi: 10.3389/fpubh.2025.1612187
Edited by:
Lawrence Ejike Ugwu, Renaissance University, NigeriaReviewed by:
Matthew Aplin-Houtz, Brooklyn College, United StatesKelly Gleason, Johns Hopkins University, United States
Bruno Basil, David Umahi Federal University of Health Sciences, Nigeria
Copyright © 2025 Zhang, Chen and Ochoa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongqian Chen, MzUzODc2MzRAcXEuY29t
†These authors have contributed equally to this work
 Zhe Zhang
Zhe Zhang Yongqian Chen2*†
Yongqian Chen2*† Marcos C. Ochoa
Marcos C. Ochoa