- 1Faculty of Kinesiology, University of Calgary, Calgary, AB, Canada
- 2School of Public Policy, University of Calgary, Calgary, AB, Canada
- 3Departamento de Kinesiología, Pontificia Universidad Católica de Chile, Santiago, Chile
- 4Faculty of Social Work, University of Calgary, Calgary, AB, Canada
- 5Department of Psychiatry, University of Calgary, Calgary, AB, Canada
Introduction: Youth with Neurodevelopmental Disabilities (NDD) who are transitioning to adulthood often struggle with accessing services. This limited access can result in poorer health, reduced ability to perform daily activities and engage in independent living and decreased levels of participation in society. Despite Canada’s commitment to the UN Convention on the Rights of Persons with Disabilities, British Columbia (BC) youth with NDD face additional barriers.
Methods: This study investigated service providers’ and decision-makers’ perspectives on barriers, facilitators and policy recommendations for accessing BC’s health, education and disability services for youth with NDD. We conducted a qualitative descriptive study with 15 semi-structured interviews. We conducted inductive thematic coding to generate themes, which we then organized and interpreted using Bronfenbrenner’s ecological model.
Results: Findings revealed that fragmented organizational structures, eligibility criteria, limited and unstable funding and enduring stigma impede service access, while coordinated inter-agency collaboration, clear transition planning and early, family-centered interventions may improve outcomes.
Discussion: Targeted policy reforms across multiple ecological levels are essential to reduce inequities in service access and strengthen the continuum of support for youth with NDD as they transition to adulthood.
1 Introduction
Youth with neurodevelopmental disability (NDD) are a heterogeneous group with chronic conditions that originate during the developmental period affecting the central nervous system, resulting in impact on daily functioning (1). In Canada, an estimated 75% of youth with a disability have a NDD, with prevalence ranging from 5 to 9% and up to 15% in developed countries (2–4). Youth with NDD often encompass conditions affecting their cognition, communication, motor skills, social interaction and behavior which leads to barriers in full participation in society (5). Moreover, youth with NDD often require extensive healthcare and support services and require continuous support as they transition into adulthood (6, 7).
The transition to adulthood is a crucial developmental phase focused on emotional, psychosocial growth and independent living (8), requiring youth to establish new relationships with service providers and navigate new systems of care (9). In Canada, it involves the transition from pediatric to adult healthcare, special education to adult life and a shift from pediatric to adult disability supports, as well as caregiver to self-income supports (10, 11). This critical phase is often characterized as navigating a “support cliff” (12), leading to a considerable decrease in support service utilization after reaching adulthood (13).
There are considerable gaps in the availability and quality of transition service systems for youth with NDD. These challenges include poor communication between pediatric and adult services, limited resources, a lack of understanding about transition practices among adult care providers, insufficient planning for transitions and the anxiety young adults feel when facing new healthcare systems (9, 14).
While challenges in the transition from pediatric to adult services have been widely discussed (9–11), little is known about how these factors operate across systems simultaneously. Youth with NDD often encounter poorly coordinated care and service gaps at the intersections of health, education and social services (15). Much of the existing literature remains siloed, addressing barriers within a single domain. For example, inadequate preparation for transfer in healthcare or transition tools developed for one sector (16). A smaller body of work demonstrates the value of cross-system perspectives. Hoffman et al. applied Bronfenbrenner’s ecological model to parents’ accounts of transition experiences for autistic youth, showing influences at multiple levels (17). Similarly, Mirzaian et al. mapped the “bouncing” of young people with intellectual and developmental disabilities between disability and mental health systems, illustrating how multi-level barriers accumulate (18). Despite these advances, cross-system analyses remain rare, and most studies continue to conceptualize barriers as isolated rather than interdependent processes. This gap also extends to understanding the unique needs of youth with NDD, strategies for supporting their transition and the systemic and organizational barriers that hinder successful outcomes (18). The consequences of these service gaps are severe: youth with NDD face higher risks of homelessness, greater involvement in the criminal justice system, lower graduation rates, reduced participation in post-secondary education, limited workforce engagement and higher rates of poverty than peers without disabilities (19–21). These findings highlight the urgent need for coordinated, multi-system approaches to ensure appropriate support for youth with NDD transitioning to adulthood.
To address this gap, we draw on Bronfenbrenner’s ecological systems theory as a framework (22). Transitions across service systems are not shaped by isolated factors but by the interaction of influences spanning multiple levels. At the microsystem level, youth and families navigate daily encounters with clinicians, educators and case managers; at the mesosystem level, interactions between schools, health providers and community agencies determine whether supports are aligned or fragmented; at the exosystem level, organizational rules and service delivery structures often create barriers; and at the macrosystem level, provincial funding schemes and eligibility criteria establish the policy barriers for access (22). Unlike narrower health transition frameworks, the ecological model explicitly foregrounds how these nested layers interact over time, a perspective particularly suited to the complex, cross-sectoral nature of transitions for youth with NDD (17, 18). This framing allows us to situate qualitative accounts of transition within a multi-level policy context, ensuring that findings not only capture lived experience but also illuminate the structural dynamics that either constrain or enable access to adult disability supports.
Service providers and decision-makers are important key informants regarding barriers and facilitators to accessing services when transitioning from pediatric to adult supports. Through daily engagement with policy and program implementation, service providers and decision-makers come to know what works and under what conditions (23). By centering service providers and decision makers, we illuminate the implementation layer of transition policy: how eligibility rules are operationalized, how organizational constraints drive triage and wait listing, and how inter agency relationships either enable or obstruct continuity.
Therefore, this paper focuses on describing decision makers’ and service providers’ perspectives in British Columbia, Canada to better understand barriers and facilitators in accessing services for youth with NDD based on two core research questions:
RQ1: How do barriers and facilitators operate across Bronfenbrenner’s ecological levels (micro, meso, exo, macro, chrono) to shape service access during transitions from pediatric to adult services for youth with NDD in British Columbia?
RQ2: Which multi-level policy levers can reduce inequities and improve service continuity during the transition to adulthood?
The aim is to describe the barriers and facilitators within systems and how they influence one another, so that interventions and support services can be tailored to facilitate a smooth transition for youth with NDD, promoting their successful integration into adult life. We apply Bronfenbrenner’s ecological systems theory as an organizing lens to map inductively derived themes across micro-, meso-, exo-, macro- and chrono-levels and to surface cross-level interactions. Findings from one provincial jurisdiction in Canada provide important context for other systems, including policy implications, resource allocation and the coordination of services.
2 Materials and methods
2.1 Study design
This study utilized a qualitative research design to gain a deeper understanding of the perspectives service providers and decision-makers have on barriers and facilitators that youth with NDD encounter in the transition from pediatric to adult services. Semi-structured interviews were employed to capture participants’ perspectives, grounded in their firsthand experiences working within systems serving youth with NDD and their families. This design allowed for an exploration of nuanced insights from those directly involved in the delivery of services and system design.
We adopted a qualitative descriptive approach within a pragmatic paradigm. Inductive coding generated themes that were subsequently organized using Bronfenbrenner’s ecological model (24, 25). This approach was well-suited to capture the range of experiences, challenges and facilitators perceived by service providers and decision-makers from various fields, including health, special education and disability supports (25). The research design was part of a broader, multi-method project focused on exploring service access for children and youth with NDD. Ethical approval for the study was obtained from The University of Calgary’s Research Ethics Board (REB20-1872).
2.2 Participant recruitment
Participant recruitment took place from January 2023 to November 2023. A combination of purposeful and snowball sampling methods was used to identify and recruit participants (26). We used purposeful sampling to recruit service providers and decision-makers with direct experience in supporting youth with NDD during the transition from pediatric to adult services. This approach ensured participants had situated knowledge of the systems and policies under study (26). Snowball sampling was also employed, as participants were well-positioned to identify additional colleagues across health, education and social service sectors whose perspectives were essential for capturing the cross-system nature of transitions (26). To be eligible, participants had to meet the following inclusion criteria: they were either actively working in a decision-making or service provider role in health, special education or disability services at the time of data collection, or they had previous experience with organizations providing services and supports to youth with NDD transitioning to adulthood in British Columbia. Eligible participants who expressed interest were invited by the researchers via email to participate in interviews. The email included a link to the informed consent form and a brief demographics survey to gather participant characteristics. Once the completed consent form was received, participants were provided with a link to join the interviews via Zoom Video Conferencing Software.
2.3 Data collection
Semi-structured interviews was the primary method of data collection for this study. The interview guide was developed based on previous research (27), which explored the experiences of children with NDD and their families in accessing services across Canada. The interview guide included questions regarding eligibility criteria, barriers and facilitators to accessing services and supports, changing needs and waitlists (Supplementary material A). The guide was pilot tested with a service provider and subsequent modifications were made to enhance its quality and clarity.
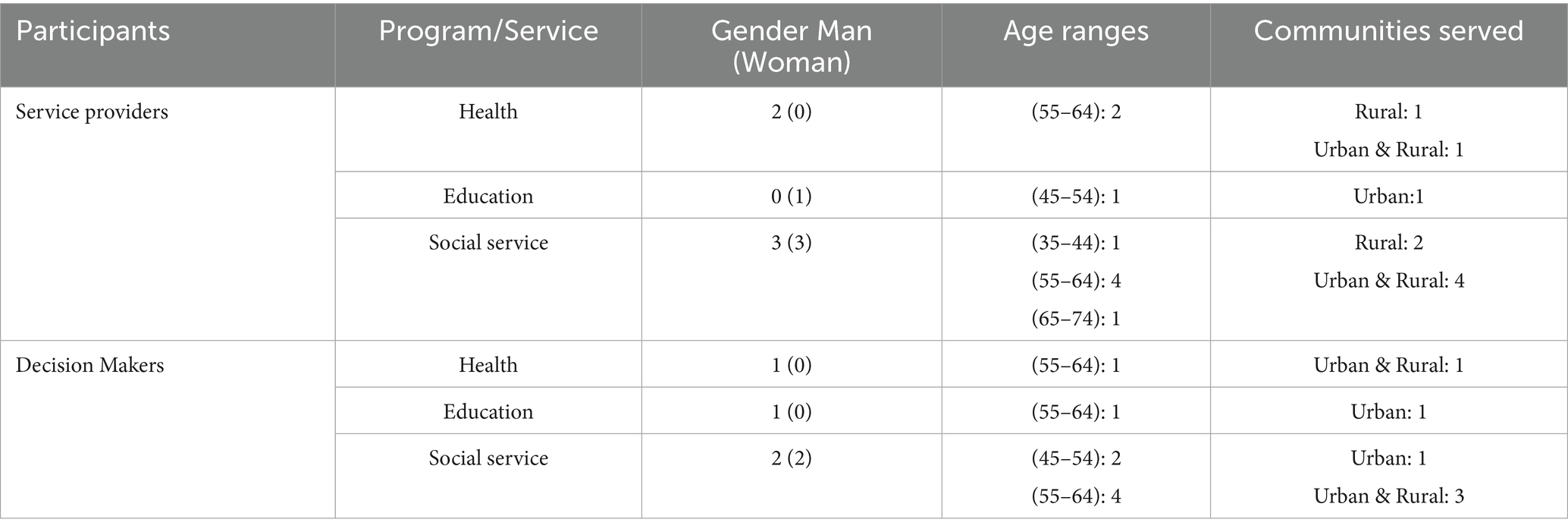
Feedback on the interview questions was obtained from the multidisciplinary research team and the advisory council, which included individuals with lived experience, knowledge users and community partners, to ensure the questions were appropriate and comprehensive. Interviews were conducted virtually using Zoom Video Conferencing, were audio-recorded and transcribed verbatim using ReV software. Each interview lasted up to 90 min and involved one interviewer and one note-taker. The audio recordings were stored in a secure encrypted drive provided by the University of Calgary. A total of 15 interviews were conducted (nine service providers and six decision-makers), representing both urban and rural communities across the province of British Columbia. Participant characteristics are outlined in Table 1.
2.4 Data analysis
The qualitative data analysis followed a six-stage thematic analysis process; familiarization with the data, generating initial codes, searching for themes, reviewing themes, defining and naming themes and writing the final report (28). Ten transcripts were read multiple times to gain familiarity with the data. We then conducted initial line-by-line inductive coding, staying close to participants’ words to capture barriers, facilitators and transition experiences as they were described. The iterative codebook approach was used to ensure consistency in coding across interviews (Supplementary material B). Then the codebook was applied to all transcripts, with ongoing comparison and refinement. New inductive codes were added when data did not align with existing categories. Codes were clustered into broader sub-themes that described patterns across participants’ accounts. These inductively derived sub-themes were then mapped to ecological levels to locate each theme within the model (organization/interpretation), not to generate themes. The deductive analysis offered a structured way to situate participants’ accounts within a rigorously theorized framework, ensuring system-level mechanisms were captured alongside lived experiences. Post-coding ecological mapping provided a structured way to organize and interpret participants’ accounts. This hybrid approach of inductive/deductive thematic analysis ensured that lived experiences remain central while also informing policy and organizational responses (29). This approach enabled the researchers to capture emergent insights while structuring interpretation through the ecological framework (29, 30).
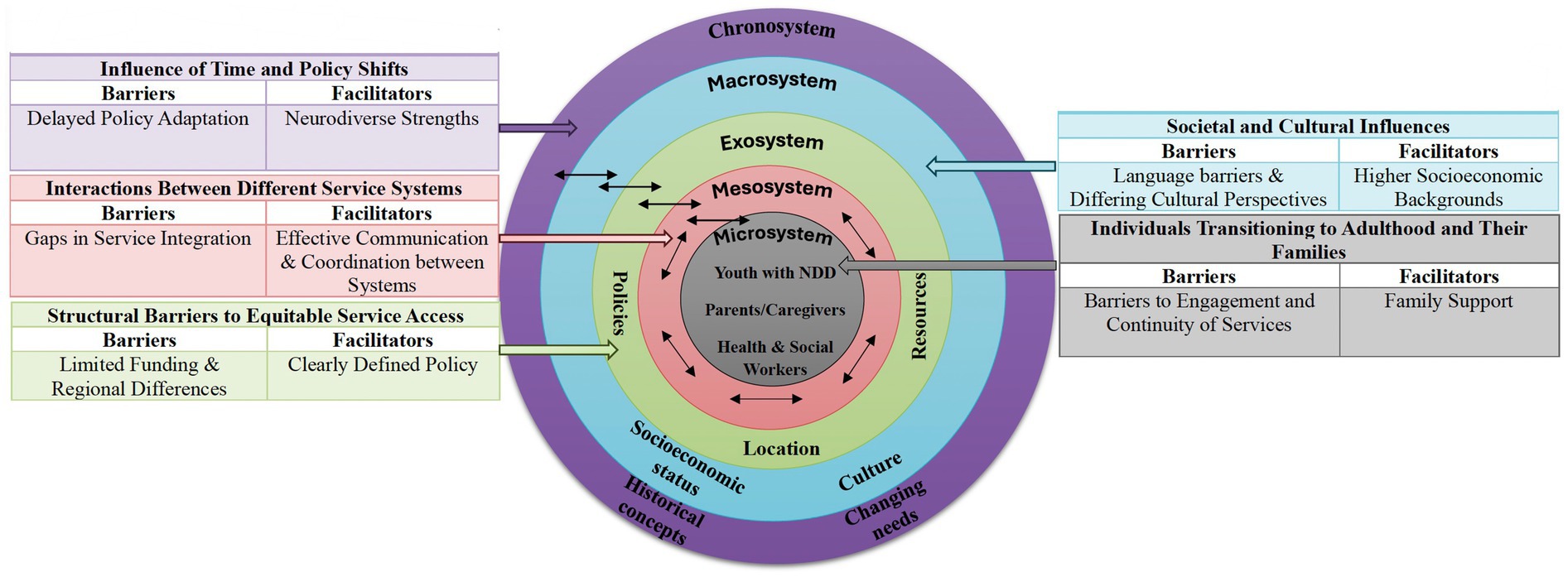
The deductive analysis of the data was situated in Bronfenbrenner’s ecological systems theory (22), which provided a conceptual framework for understanding the transition of youth with NDD into adulthood. This model emphasizes the complex interactions between individual and social and systemic factors, including the microsystem, mesosystem, exosystem, macrosystem and chronosystem. Youth and families navigate not only immediate clinical or educational encounters but also organizational policies, professional cultures and interagency relationships, as well as broader provincial funding structures and eligibility criteria. By applying this model, we critically examine how multi-layered environments interact to produce both barriers and facilitators for service access. Unlike alternative frameworks that focus narrowly on health care delivery or individual behavior, the ecological model foregrounds the cross-system interactions that are central to policy design in disability services (Figure 1). However, the analysis was conducted within a qualitative descriptive design; while inductively generated themes were mapped to ecological systems theory, the study was not theory-driven.
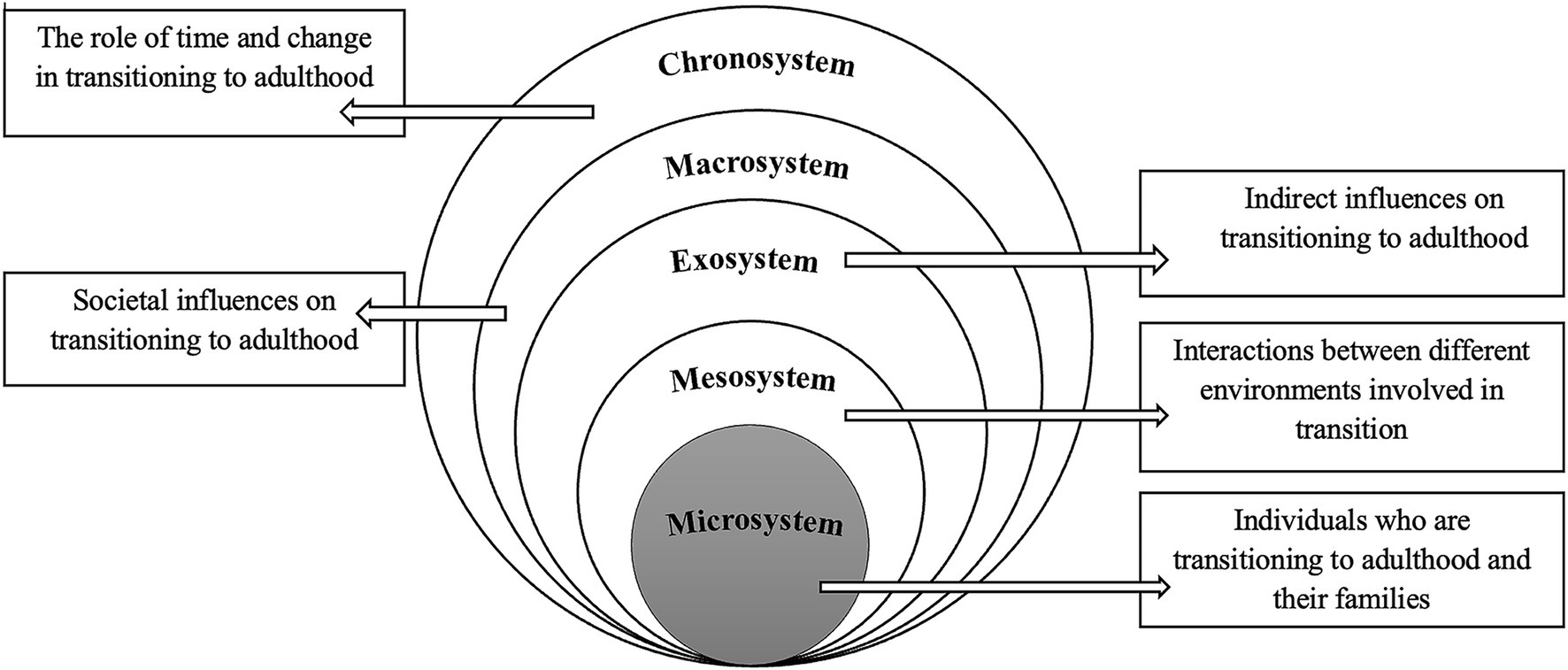
Figure 1. Interactions between systems using Bronfenbrenner’s ecological model to organize and interpret inductively derived themes.
Initial coding was led by the doctoral researcher, with supervisory team members independently reviewing a subset of transcripts to refine the coding framework. Differences in interpretation were discussed in team meetings until consensus was reached.
As qualitative research is shaped by researchers’ social positions, disciplinary training and prior experiences, reflexivity was practiced as an ongoing team process. The team brought complementary perspectives of health policy and health-economics expertise (supervisory role), clinical and social work practice expertise in child and youth navigation (supervisory role) and a doctoral researcher in health policy with ongoing training in disability policy and service access. These backgrounds, including prior collaborations with disability service systems, oriented us toward system and policy-level interpretations and an emphasis on equity. To mitigate bias, two researchers independently reviewed the transcripts to become familiar with the data and generate codes, with oversight and support from the qualitative lead. Initial findings were presented to senior researchers for peer debriefing to enhance the rigor and credibility of the analysis (31, 32). Following the coding process, the researchers exchanged transcripts and collaboratively resolved any discrepancies, ensuring validity through consensus (33). Themes were then developed from the codes and group discussions were held to refine these themes (34). Insights from these discussions were documented to maintain a transparent and rigorous process.
The final sample of 15 interviews was considered adequate to answer the aim and research questions based on the concept of “information power” (35), which suggests that the data provided sufficient depth and breadth for meaningful conclusions. While the final sample of 15 interviews may appear modest, sufficiency was demonstrated by the recurrence of central themes across participants and the redundancy of perspectives after approximately 12 interviews. Importantly, the sample included a range of roles and organizations, which provided variation in context while still allowing thematic convergence. This aligns with qualitative guidance that emphasizes adequacy of information richness and diversity of perspectives over numerical thresholds (35, 36).
To further ensure the validity and relevance of the findings, preliminary results were shared with the advisory council for feedback, ensuring alignment with the perspectives of those familiar with the topic (31–33).
3 Results
3.1 Demographics
A total of nine service providers and six decision-makers were selected and interviewed for the study. Participant characteristics reflected a diverse range of perspectives, including variation across provider type, ministry type, age and service area (Table 1).
3.2 Findings
Inductively derived themes were organized and interpreted using Bronfenbrenner’s ecological model to examine how barriers and facilitators interact across systems. We identified key influences at multiple ecological levels, highlighting the complex interplay between individual, family, service and policy factors that affect service access and continuity. The findings included a series of policy recommendations aimed at improving service delivery, increasing equity in access and enhancing coordination between systems. Figure 2 provides an overview of the findings. Quotes are presented as illustrative evidence embedded within analytic text, consistent with qualitative description. Headings by ecological level reflect organizational choices; themes were derived inductively from the data.
3.2.1 Microsystem: individuals transitioning to adulthood and their families
At the microsystem level, youth with NDD and their immediate support networks, including family members, caregivers and healthcare providers, play a pivotal role in shaping access to services. Family support emerged as an existing critical facilitator in navigating service systems for some youth. Parents and caregivers often acted as advocates, securing necessary services and ensuring continuity of care. However, barriers to engagement and continuity were prominent. Youth frequently disengaged from support services due to stigma and a lack of understanding of their future needs:
“The older the youth with support needs, they do not feel they need the support [.] they do not want to be labeled disabled” (SP10).
Families who were unfamiliar with transition planning faced challenges in identifying and accessing adult supports. For instance, in British Columbia, without proper guidance, the adult support system can be complex and daunting for families and youth seeking support and the intricacies of application processes and available services can be difficult to understand and navigate:
“One of the biggest and scariest things for (our) families is the persons with disabilities application” (SP06).
3.2.2 Mesosystem: interactions between different service systems
The mesosystem reflects the interactions between various support systems, including pediatric and adult service providers. Effective communication and coordination between these systems were key facilitators for smooth transitions. However, participants identified significant gaps in service integration and coordination, resulting in fragmented care and service discontinuities. For example, the shift from Children and Youth with Special Needs (CYSN) services to adult services like Community Living British Columbia (CLBC) was not always seamless:
“CLBC relies on other systems to create access pathways to ours, but those systems do not know sometimes that we are relying on them” (DM04).
According to participants, the current attempts to improve collaboration between systems include the creation of internal resources to enhance service literacy and promote coordinated care. One participant described that they developed an internal webpage with information on CLBC to help staff better understand its scope and limitations, noting that:
“it’s our effort to try and increase literacy on these services within our organization” (SP02).
Despite these efforts, siloed service structures with rigid eligibility criteria continued to pose barriers for families:
“It’s a very rigid criteria. You either are or are not eligible” (DM04).
3.2.3 Exosystem: structural barriers to equitable service access
At the exosystem level, decisions made by government agencies and policymakers indirectly influenced service access. The policy for CLBC’s eligibility is clearly defined, an individual qualifies if a psychologist determines they meet the requirements:
“You (either) meet the threshold requirements and have a developmental disability, autism or FASD you are then eligible to receive services from CLBC” (DM08).
Structural barriers, including limited funding and regional differences in service availability, were key challenges. Participants described financial constraints that limited-service provision and created lengthy waitlists:
“CLBC has a finite budget [.]. So we try to manage within the parameters and then prioritize individuals who have the greatest needs” (DM02).
Geographic location also created disparities in access, with youth in rural and remote communities facing additional barriers. Participants highlighted that even when individuals were deemed eligible for CLBC, services were often unavailable in isolated regions. In some cases, communities could only be reached by air for part of the year, leaving families without consistent access to supports.
“Not just rural that you can drive to, but remote where it’s fly in, fly out for part of the year and there may or may not be any services in the community at all” (DM04).
3.2.4 Macrosystem: societal and cultural influences
The macrosystem encompasses broader societal values and socioeconomic factors that shape service access. Families from higher socioeconomic backgrounds were better able to navigate service systems and secure necessary supports:
“People with intellectual disabilities who are born into affluent privileged families have by far a better situation, receive better services, have better housing” (SP04).
Cultural beliefs and practices also influenced service utilization, with immigrant families encountering language barriers and differing cultural perspectives on disability. One participant explained that service use often depended on how disability was understood within a family’s cultural background and in some cases, those perspectives could discourage engagement:
“it depends on your cultural background and maybe those perspectives on disability and sometimes that might prevent you from accessing” (SP08).
3.2.5 Chronosystem: influence of time and policy shifts
The chronosystem reflects how transition experiences evolve over time in response to policy changes and shifting societal norms. There was increased recognition of the strengths and contributions of neurodiverse individuals to society, leading to a shift toward more inclusive models of support:
“Kids that are transitioning into adulthood, we are seeing changing needs as we become more aware of the strengths and contributions that neurodiverse people can make to society” (SP08).
Historical comparisons further underscored the scale of change. Whereas past systems often segregated individuals with NDD from community life, participants noted a shift toward inclusive approaches:
“Young people are included in schools in a way that they were not 30 years ago, so a much greater need to just be part of the community, to get away from the more segregated models of support to much more inclusive models” (SP04).
Consistent with our design, these observations reflect participants’ perceptions rather than longitudinally demonstrated trends.
3.2.6 Policy and system level implications
Participants emphasized several policy priorities to strengthen transitions for youth with NDD. A consistent theme was the importance of case management to ensure continuity, with one noting that:
“Case management would be a helpful thing [.] you need that one person to help hold the story as they go from child and youth to adults” (SP02).
In addition, stronger collaboration between systems was viewed as essential. It was suggested that CLBC could improve:
“How, when and who we engage with [and] pursue it more actively than historically” (DM04).
Gaps in regional coordination were also raised, with participants pointing out that:
“CLBC has missed that middle gap[.] we need to be in the local networks, but also in the regional network” (DM04).
Resourcing was another prominent theme, with participants stressing the need for expanded capacity to support adults:
“It would be great if we could increase the ability to support adults” (SP08).
Equity concerns further underscored the importance of targeted outreach, as participants described the need for:
“Making sure organizations are aware of our services” (DM01).
Finally, participants identified emerging needs such as co-occurring substance use, describing this as:
“An emerging area” (DM02).
Requiring greater attention.
4 Discussion
4.1 Summary of findings
The transition from youth to adulthood is a formative time for everyone, but for individuals with NDD, it presents unique challenges. This study highlights how service providers’ and decision-makers’ perspectives reveal individual and systemic barriers and facilitators in the transition from pediatric to adult services for youth with NDD. Additionally, the findings offered policy recommendations aimed at improving transition services and addressing these challenges. In our analysis, the perspectives of service providers and decision-makers were largely convergent, emphasizing common priorities such as the need for case management, stronger interagency collaboration and increased resourcing to support transitions. Service providers more frequently highlighted the day-to-day challenges of navigating fragmented systems and supporting families with limited resources, while decision-makers focused on structural issues such as policy gaps, regional coordination and strategic planning. Despite these differences in emphasis, divergences were minimal.
Previous research has consistently documented the barriers that youth with NDD encounter when transitioning to adulthood. Studies highlight how stigma (37) and lack of support networks (37, 38) discourage service engagement, leading many young people to disengage from needed supports and experience social isolation. The transition is further complicated by simultaneous changes in healthcare, education and social networks, alongside heightened expectations for independence (9, 38). Socioeconomic resources play a crucial role in shaping outcomes. Families with financial means are better able to secure assessments, consultants and timely services, while lower-income families face systemic disadvantages (37, 38). Rigid diagnostic criteria exacerbate these inequities, excluding youth whose needs do not align neatly with established categories, especially those with overlapping or co-occurring conditions (39, 40). Fragmentation between pediatric and adult systems, often operating in silos, compounds these challenges and undermines continuity of care (23, 41, 42). Structural barriers, such as limited funding, is found to be another barrier for accessing services (43). Geographic disparities further limit access, as youth in rural and remote communities have fewer specialized services compared to their urban peers (13, 44). Finally, cultural and linguistic barriers disproportionately affect immigrant families, who may face stigma within their communities or lack familiarity with service systems, leaving them less likely to seek formal support (45, 46). While prior research has underscored some barriers, our findings extend this work by showing how these dynamics emerge not in isolation but through interactions across ecological levels.
Bronfenbrenner’s ecological model was a useful way to organize our findings. The model treats systems as layers that surround the individual, yet our results show these systems are not neutral. They actively shape who gets access to services and who is left out. Rules about eligibility, funding decisions and how services are organized across regions act as gatekeeping tools that can exclude people (47). As Prince (2012) argues, disability policies often follow neoliberal logics, approaches that prioritize efficiency, cost-cutting and individual responsibility over equity and inclusion, which deepens marginalization (48). Participants’ accounts suggest processes through which exclusion may be produced through how systems interact.
First, the participants described how youth disengagement at the microsystem level, often shaped by stigma and lack of family support, and intersects with rigid eligibility rules at the exosystem level and broader societal inequities at the macrosystem level, producing compounded exclusion. Second, it showed that failures in interagency collaboration at the mesosystem level cannot be separated from resource scarcity and political priorities at the exosystem level. Fragmentation reflects not only weak communication but structural underfunding. Third, it applied the ecological framework to situate participants’ accounts, highlighting that systems are not neutral contexts but sites of governance and power, where eligibility rules, budgetary decisions and geographic structures function as gatekeeping mechanisms (46–48).
4.2 Inter-level interactions
Participants described disengagement, which they linked to older teens resisting being “labeled disabled” (49). This disengagement intersected with rigid exosystem eligibility rules that required categorical diagnoses. Youth who resisted services thus faced double exclusion, first by stepping away and second by systems with rigid eligibility pathways. Previous research has shown similar dynamics where stigma drives youth to avoid disability labels, while rigid eligibility criteria act as structural gatekeepers (50). Cheak-Zamora et al. describe this as the “service cliff,” where young people simultaneously disengage and age out (51). Our findings reinforce that stigma is not only interpersonal but institutionally reproduced, as systems fail to provide flexible, youth-centered re-engagement options.
The interviews revealed the overwhelming complexity of disability benefit applications for youth and families. These microsystem-level burdens were intensified by the absence of case management or consistent supports across the systems. Without a single point of contact, families carried responsibility for coordination, increasing stress and risking youth disengagement. Prior studies show that the absence of navigation supports disproportionately disadvantages families with fewer resources (52). Evidence from Canada and internationally indicates that case management improves continuity and outcomes by ensuring that one actor “holds the story” during transitions (53–55). Our findings align with this literature, underscoring that the absence of mesosystem supports transforms administrative complexity into structural exclusion.
The lack of interagency collaboration (mesosystem) was linked to broader exosystem constraints. Participants described finite budgets that forced prioritization of “greatest needs,” limiting capacity for proactive collaboration. Thus, fragmentation was not only a product of communication failure but also the political economy of scarcity. Previous studies confirm this link. Beresford et al. observed that service fragmentation reflected resource shortages, while US studies highlight how underfunded systems foster agency competition rather than collaboration (56, 57). Canadian evidence similarly shows that collaboration frameworks require not only will but also resources and accountability (16). Our findings suggest that mesosystem collaboration cannot succeed without exosystem investment.
Rigid eligibility criteria and funding limits (exosystem) interacted with macrosystem inequities of socioeconomic and cultural factors (58). Affluent families secured private assessments and leveraged social networks, while immigrant families faced linguistic barriers and cultural stigma (59). Research across international contexts shows that socioeconomic privilege translates into smoother navigation (60, 61), while immigrant families encounter systemic barriers tied to cultural framings of disability (58). Canadian research argues that disability systems reproduce broader inequities by rewarding those with financial and cultural capital (62, 63). Our findings reinforce that eligibility and funding rules are not neutral and they interact with macrosystem inequities to stratify outcomes.
Geographic disparities (exosystem) further illustrated inter-level entanglements. Families in remote communities were eligible but had no services available locally (64). Here, exosystem structures (lack of regional delivery models) intersected with macrosystem inequities (urban-centric policy design) and translated into microsystem struggles for families left unsupported. Australian research on the NDIS documents similar rural service gaps (65) and Nordic countries face professional shortages in rural areas despite universalist policies (66). These findings highlight that geography is not only logistical but also reflects structural decisions about resource distribution.
Furthermore, emerging challenges such as co-occurring substance use revealed how chronosystem shifts in population needs collide with static exosystem rules. Eligibility frameworks designed in the early 2000s had not adapted, leaving families navigating disconnected disability and mental health systems. Participants also noted evolving societal understandings of neurodiversity, showing how macrosystem values change more slowly than youth realities. Studies of policy inertia confirm that adolescent mental health and co-occurring conditions are poorly accommodated in static service frameworks and transitions fail when systems cannot adapt to shifting needs (51, 53, 62, 67). Our findings add that time itself becomes a site of exclusion. Participants perceived that policy lag can leave youth unsupported in evolving contexts.
However, some considerations need to be undertaken. Although Bronfenbrenner’s ecological systems theory offers a valuable lens for structuring multi-level influences on transition, it does not fully capture structural exclusion or the ways inequities are reproduced through policy design, eligibility criteria and socio-political ideologies. Other frameworks, such as Andersen’s behavioral model of health services use (68) and the Life course health development (LCHD) model (69), emphasize the dynamic interactions between individual characteristics, service systems and broader social determinants of health. These perspectives foreground how system level characteristics such as policies, healthcare facilities and personal characteristics such as education, social background, shape service access, particularly for marginalized youth.
The interactions identified in this study such as how resource shortages intersect with cultural barriers and restrictive eligibility policies, illustrate that barriers cannot be understood in isolation. Instead, they accumulate and interact to create compounded exclusion over time, reinforcing the importance of examining transitions as embedded in intersecting systems rather than discrete challenges. By situating our findings in relation to these broader frameworks, we underscore the unique insight of this study. That transition barriers for youth with NDD emerge not only from isolated characteristics but also from the interaction of ecological levels with structural inequities, highlighting the need for integrated, equity-oriented policy reform.
4.3 Study limitations
This study’s strength lies in capturing perspectives across multiple systems, offering insight into how policy is enacted in practice. The ecological framework facilitated analysis of inter-level interactions, though it required adaptation. Limitations include the BC-specific sample, which may limit transferability and the absence of youth and family voices, which are critical for future research. Although purposive and snowball sampling enabled access to a diverse group of providers and decision-makers, we acknowledge that these approaches may have over-represented individuals who are well connected within service networks and under-represented dissenting or marginalized voices (70). We sought to mitigate these risks by recruiting through multiple sectors and organizational levels, but we recognize that the absence of certain perspectives remains a limitation that should temper the transferability of our findings. At the same time, the recurrence of key themes across participants and the breadth of organizational vantage points represented provide confidence that the study identifies system-level patterns and policy-relevant mechanisms that are unlikely to hinge on a single perspective. Because data were cross-sectional, chronosystem inferences reflect participants’ retrospective accounts (e.g., policy shifts, evolving norms) rather than longitudinal observation.
4.4 Practice recommendations
Policy recommendation 1: implement person-centered transition planning with case management supports.
Transition planning for youth with NDD should move beyond diagnostic and IQ thresholds to emphasize functional abilities, strengths and personal goals. In BC, this could be advanced by strengthening CLBC’s cross-ministerial protocol for transition planning for youth with special needs (71). Embedding case managers within CLBC regional offices would provide families with a single point of contact and improve continuity across education, health and social care as evidence from Alberta’s transition planning initiatives and international studies supports case management as a way to reduce fragmentation and promote smoother transitions (72).
Policy recommendation 2: establish proactive interagency collaboration frameworks.
Systemic barriers in the transition process are often reinforced by fragmented communication and unclear responsibilities between pediatric and adult service systems (73). A proactive collaboration framework should outline when, how and by whom engagement occurs across agencies, ensuring that responsibility for information sharing does not fall passively on individual families or disconnected systems (74). By embedding active mechanisms for interagency coordination, rather than relying on ad hoc efforts, such a framework would reduce service gaps, promote consistency in communication and strengthen continuity of care for youth with NDD.
Policy recommendation 3: develop regional support networks to strengthen rural service delivery.
Geographic disparities remain a significant barrier for families in rural and remote parts of BC, where services are often sparse or unavailable. Establishing regional support networks would bridge the “middle gap” between provincial structures and local providers, embedding CLBC fully into both local and regional systems (75). Frameworks for rural health care planning emphasize community-specific approaches, multidisciplinary team-based care, expanded use of telehealth, systematic evaluation and strategies to recruit and retain providers (76). Incorporating these principles into disability service planning would improve outreach, expand availability and ensure families in remote communities have more consistent access to supports.
Policy recommendation 4: increase funding for transition services and housing supports.
Resource constraints limit service availability, generate long waitlists and deepen inequities for youth and families. In BC, expanding funding through targeted streams such as CLBC’s personalized supports initiative and partnerships with BC housing’s supported independent living programs would help ensure that transition planning and housing supports are not delayed or inaccessible (77). Dedicated allocations would allow agencies to expand service options and reduce inequities in access, particularly for low-income and underserved populations (47, 71).
Policy Recommendation 5: Strengthen outreach and culturally responsive supports for marginalized communities.
Immigrant families and other marginalized groups often face language barriers, stigma and cultural perspectives on disability that limit service uptake (78). In BC, stronger partnerships between CLBC and community-based organizations, including settlement and integration services, could expand outreach and ensure families are informed about available supports. Embedding cultural competence and linguistic accessibility into provider training would reduce barriers, build trust and promote more equitable access.
Policy recommendation 6: implement a complex care model to address co-occurring needs.
Youth with NDD are increasingly presenting with emerging challenges such as substance use and mental health concerns, yet current transition structures remain siloed and ill-equipped to respond (79). Developing a complex care model that integrates disability, mental health and addictions services would ensure these needs are addressed within the transition process (80). In BC, this could build on initiatives such as the Integrated Child and Youth Teams (77) being rolled out across the province, expanding their scope to include developmental disability supports. Embedding multidisciplinary expertise and coordinated pathways into such models would reduce fragmentation and provide more responsive, holistic care.
4.5 Conclusion
This study shows that transition barriers for youth with NDD are not isolated but produced through interlocking dynamics such as stigma, eligibility rigidity, resource scarcity, inequities of privilege and culture, geographic divides and policy. We use the ecological model to synthesize participant perspectives on inter-level interactions and we situate BC’s findings within international debates on disability policy. We intentionally kept the practice recommendations section distinct, to ensure that these recommendations were presented as a synthesis of participant perspectives.
Our findings underscore that reforms targeting single levels are insufficient. Anti-stigma programs cannot succeed if eligibility remains rigid. Additional funding will not resolve inequities if services remain siloed. Outreach to immigrant communities will fail if eligibility and geographic barriers remain unchanged. And static frameworks cannot meet the needs emerging over time. Addressing these barriers requires integrated, cross-level reforms that are person-centered, equity-focused and adaptive to emerging needs. In doing so, disability transition policies can move beyond fragmented, exclusionary models toward inclusive pathways to adulthood.
Data availability statement
The datasets generated or analyzed during the current study are not publicly available due to the confidential nature of qualitative interview data and the ethical obligations to protect participant privacy. Participants did not consent to the public sharing of their transcripts. Requests for de-identified excerpts may be considered on a case-by-case basis and subject to approval by the appropriate research ethics board. Requests to access the datasets should be directed to YW5nZWxhLnNlbmV2aXJhdGhuYUB1Y2FsZ2FyeS5jYQ==.
Ethics statement
The studies involving humans were approved by The University of Calgary’s Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants.
Author contributions
AMS: Investigation, Data curation, Visualization, Formal analysis, Conceptualization, Software, Project administration, Methodology, Writing – original draft, Writing – review & editing, Funding acquisition. PB: Data curation, Writing – review & editing. AS: Data curation, Writing – review & editing. GD: Supervision, Writing – review & editing, Validation. JZ: Resources, Validation, Writing – review & editing, Funding acquisition, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. AMS is supported by the Canadian Institutes of Health Research (CIHR), grant number PJT-173325, the Alberta SPOR SUPPORT Unit (AbSPORU) and the Alberta Children’s Hospital Research Institute (ACHRI). JZ is supported by a Tier II Canada Research Chair in Disability Policy for Children and Youth and Kids Brain Health Network.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1612509/full#supplementary-material
SUPPLEMENTARY TABLE 1 | Summary of themes, subthemes, illustrative codes and example participant quotations identified through qualitative analysis of service provider and decision-maker interviews. This table outlines the analytical structure supporting the key findings.
SUPPLEMENTARY DATA SHEET 1 | Interview guide.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. US: American Psychiatric Publishing Inc. (2013).
2. Ogundele, MO, and Morton, M. Classification, prevalence and integrated care for neurodevelopmental and child mental health disorders: a brief overview for paediatricians. World J Clin Pediatr. (2022) 11:120–35. doi: 10.5409/wjcp.v11.i2.120
3. Russell, MJ, Zhang, Y, Cui, X, Tough, S, and Zwicker, JD. Use of family disability service by families with young children with disabilities. Dev Med Child Neurol. (2021) 63:81–8. doi: 10.1111/dmcn.14478
4. Zwicker, J, Zaresani, A, and Emery, JCH. Describing heterogeneity of unmet needs among adults with a developmental disability: an examination of the 2012 Canadian survey on disability. Res Dev Disabil. (2017) 65:1–11. doi: 10.1016/j.ridd.2017.04.003
5. Weitzman, C, Nadler, C, and Blum, NJ, Supporting Access for Everyone Consensus Panel. Health care for youth with neurodevelopmental disabilities: a consensus statement. Pediatrics. (2024) 153:e2023063809. doi: 10.1542/peds.2023-063809
6. Canadian Association of Pediatric Health Centres (CAPHC) NTCoP (2016) A guideline for transition from Paediatric to adult health Care for Youth with special health care needs: A national approach. Available at: https://www.childrenshealthcarecanada.ca/media/yoenvhq1/2017-05-10-caphc-transition-to-adult-hc-guidelinev2f.pdf#:~:text=Herein%20referred%20to%20as%20the%20Guideline%2C%20this%20document,consultation%20through%20a%20consensus%20building%20set%20of%20surveys\
7. Cogswell, ME, Coil, E, Tinker, SC, Ryerson, AB, Maenner, MJ, et al. Health needs and use of services among children with developmental disabilities - United States, 2014-2018. MMWR Morb Mortal Wkly Rep. (2022) 71:453–8. doi: 10.15585/mmwr.mm7112a3
8. Campbell, F, Biggs, K, Aldiss, SK, O'Neill, PM, Clowes, M, McDonagh, J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. (2016) 4. doi: 10.1002/14651858.CD009794.pub2
9. Thanalingam, Y, Langridge, F, Gordon, I, Russell, J, Muir, C, and Hamm, LM. Strategies and tools to aid the transition between paediatric and adult health services for young adults with neurodevelopmental disorders: a scoping review protocol. BMJ Open. (2022) 12:e065138. doi: 10.1136/bmjopen-2022-065138
10. Hepburn, CM, Cohen, E, Bhawra, J, Weiser, N, Hayeems, RZ, and Guttmann, A. Health system strategies supporting transition to adult care. Arch Dis Child. (2015) 100:559–64. doi: 10.1136/archdischild-2014-307320
11. Toulany, A, Willem Gorter, J, and Harrison, M. A call for action: recommendations to improve transition to adult care for youth with complex health care needs. Paediatr Child Health. (2022) 27:297–302. doi: 10.1093/pch/pxac047
12. Government of Alberta (2014). Alberta government support for families of children and youth with disabilities.
13. Arim, R. A profile of persons with disabilities among Canadians aged 15 years or older, 2012. Minister responsible for statistics Canada (2015).
14. Babajide, A, Ortin, A, Wei, C, Mufson, L, and Duarte, CS. Transition cliffs for young adults with anxiety and depression: is integrated mental health care a solution? J Behav Health Serv Res. (2020) 47:275–92. doi: 10.1007/s11414-019-09670-8
15. World Health Organization, United Nations Children’s Fund (UNICEF). Global report on children with developmental disabilities: from the margins to the mainstream. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF)(2023).
16. Reiss, JG, Gibson, RW, and Walker, LR. Health care transition: youth, family, and provider perspectives. Pediatrics. (2005) 115:112–20. doi: 10.1542/peds.2004-1321
17. Hoffman, JM, and Kirby, AV. Parent perspectives on supports and barriers for autistic youth transitioning to adulthood. J Autism Dev Disord. (2022) 52:4044–55. doi: 10.1007/s10803-021-05273-5
18. Mirzaian, CB, Deavenport-Saman, A, Hudson, SM, and Betz, CL. Barriers to mental health care transition for youth and Young adults with intellectual and developmental disabilities and co-occurring mental health conditions: stakeholders’ perspectives. Community Ment Health J. (2024) 60:1104–16. doi: 10.1007/s10597-024-01262-x
19. Dudley, C, Nicholas, DB, and Zwicker, J. What do we know about improving employment outcomes for individuals with autism spectrum disorder? SPP Research Paper. (2015):8.
20. Izakian, H, Russell, MJ, Zwicker, J, Cui, X, and Tough, S. Trajectory of service use among Albertan youth with complex service need. Child Youth Serv Rev. (2019) 100:229–38. doi: 10.1016/j.childyouth.2019.03.001
21. Russell, MJ, Michael Scott, CW, Murias, K, Ben Gibbard, W, Cui, X, Tough, S, et al. Cross-ministry data on service use and limitations faced by children in special education. Disabil Health J. (2021) 14:101118. doi: 10.1016/j.dhjo.2021.101118
22. Bronfenbrenner, U. Ecology of human development: experiments by nature and design. 1st ed. Cambridge: Harvard University Press (1979).
23. Head, BW. Reconsidering evidence-based policy: key issues and challenges. Polic Soc. (2010) 29:77–94. doi: 10.1016/j.polsoc.2010.03.001
24. Morgan, D. Paradigms lost and pragmatism regained: methodological implications of combining qualitative and quantitative methods. J Mixed Methods Res. (2007) 1:48–76. doi: 10.1177/2345678906292462
25. Sandelowski, M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23:334–40.
26. Valerio, MA, Rodriguez, N, Winkler, P, Lopez, J, Dennison, M, Liang, Y, et al. Comparing two sampling methods to engage hard-to-reach communities in research priority setting. BMC Med Res Methodol. (2016) 16:146. doi: 10.1186/s12874-016-0242-z
27. Finlay, B, Wittevrongel, K, Materula, D, Hebert, ML, O'Grady, K, Lach, LM, et al. Pan-Canadian caregiver experiences in accessing government disability programs: a mixed methods study. Res Dev Disabil. (2023) 134:104420. doi: 10.1016/j.ridd.2022.104420
28. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
29. Fereday, J, and Muir-Cochrane, E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. (2006) 5:80–92. doi: 10.1177/160940690600500107
30. Proudfoot, K. Inductive/deductive hybrid thematic analysis in mixed methods research. J Mixed Methods Res. (2022) 17:308–26. doi: 10.1177/15586898221126816
31. Timmermans, S, and Tavory, I. Theory construction in qualitative research. Sociol Theory. (2012) 30:167–86. doi: 10.1177/0735275112457914
32. Stahl, NA, and King, JR. Expanding approaches for research: understanding and using trustworthiness in qualitative research. J Dev Educ. (2020) 44:26–8.
33. Korstjens, I, and Moser, A. Series: practical guidance to qualitative research. Part 4: trustworthiness and publishing. Eur J Gen Pract. (2018) 24:120–4. doi: 10.1080/13814788.2017.1375092
34. Tobin, GA, and Begley, CM. Methodological rigour within a qualitative framework. J Adv Nurs. (2004) 48:388–96. doi: 10.1111/j.1365-2648.2004.03207.x
35. Malterud, K, Siersma, VD, and Guassora, AD. Sample size in qualitative interview studies. Qual Health Res. (2016) 26:1753–60. doi: 10.1177/1049732315617444
36. Saunders, B, Sim, J, Kingstone, T, Baker, S, Waterfield, J, Bartlam, B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
37. Serchuk, MD, Corrigan, PW, Reed, S, and Ohan, JL. Vicarious stigma and self-stigma experienced by parents of children with mental health and/or neurodevelopmental disorders. Community Ment Health J. (2021) 57:1537–46. doi: 10.1007/s10597-021-00774-0
38. Sonneveld, HM, Strating, MMH, van Staa, AL, and Nieboer, AP. Gaps in transitional care: what are the perceptions of adolescents, parents and providers? Child Care Health Dev. (2012) 39:69–80. doi: 10.1111/j.1365-2214.2011.01354.x
39. Joo, JY, and Huber, DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. (2019) 41:111–33. doi: 10.1177/0193945918762135
40. Ono, E, Friedlander, R, and Salih, T. Falling through the cracks: how service gaps leave children with neurodevelopmental disorders and mental health difficulties without the care they need. Br Columbia Med J. (2019) 61:114–24.
41. Biswas, S, Tickle, A, Golijani-Moghaddam, N, and Almack, K. The transition into adulthood for children with a severe intellectual disability: parents’ views. Int J Dev Disabil. (2016) 63:99–109. doi: 10.1080/20473869.2016.1138598
42. Harwick, RM, Unruh, D, and Lindstrom, L. Transition to adulthood for youth with disabilities who experienced foster care: an ecological approach. Child Abuse Negl. (2020) 99:104310. doi: 10.1016/j.chiabu.2019.104310
43. Evans, K, Afsharnejad, B, Finlay-Jones, A, Downs, J, Strumpher, E, Freeman, J, et al. Improving the journey before, during and after diagnosis of a neurodevelopmental condition: suggestions from a sample of Australian consumers and professionals. Adv Neurodev Disord. (2022) 6:397–406. doi: 10.1007/s41252-022-00289-z
44. Miller, AR, Masse, LC, Shen, J, Schiariti, V, and Roxborough, L. Diagnostic status, functional status and complexity among Canadian children with neurodevelopmental disorders and disabilities: a population-based study. Disabil Rehabil. (2013) 35:468–78. doi: 10.3109/09638288.2012.699580
45. Gray, WN, Schaefer, MR, Resmini-Rawlinson, A, and Wagoner, ST. Barriers to transition from pediatric to adult care: a systematic review. J Pediatr Psychol. (2017) 43:488–502. doi: 10.1093/jpepsy/jsx142
46. Salminen, J, Laasanen, M, Leinonen, L, Karukivi, M, Vornanen, R, Alin, M, et al. Professional collaboration for children and adolescents with neurodevelopmental disorders: a scoping review. Eur J Spec Needs Educ. (2025) 40:16–34. doi: 10.1080/08856257.2024.2314422
47. Fleming, P, McGilloway, S, Hernon, M, Furlong, M, O'Doherty, S, Keogh, F, et al. Individualized funding interventions to improve health and social care outcomes for people with a disability: a mixed-methods systematic review. Campbell Syst Rev. (2019) 15:e1008. doi: 10.4073/csr.2019.3
48. Prince, MJ. Canadian disability activism and political ideas: in and between neo-liberalism and social liberalism. Can J Disabil Stud. (2012) 1:1. doi: 10.15353/cjds.v1i1.16
49. Corrigan, PW, Kosyluk, KA, and Rüsch, N. Reducing self-stigma by coming out proud. Am J Public Health. (2016) 106:873–80. doi: 10.2105/AJPH.2015.302912
50. Corrigan, PW, Druss, BG, and Perlick, DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. (2014) 15:37–70. doi: 10.1177/1529100614531398
51. Cheak-Zamora, NC, Teti, M, and First, J. “Transitions are scary for our kids, and they’re scary for us”: family member and youth perspectives on the challenges of transitioning to adulthood with autism. J Appl Res Intellect Disabil. (2015) 28:548–60. doi: 10.1111/jar.12150
52. Shattuck, PT, Narendorf, SC, Cooper, B, Sterzing, PR, Wagner, M, and Taylor, JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. (2011) 129:1042–9. doi: 10.1542/peds.2011-2864
53. Arribas-Ayllon, M. Autism diagnosis in Wales: the case of governance-driven medicalisation in care pathways. Soc Sci Med. (2025) 382:118333. doi: 10.1016/j.socscimed.2025.118333
54. Mestre, TD, Lopes, MJ, Mestre, DM, Ferreira, RF, Costa, AP, and Caldeira, EV. Impact of family-centered care in families with children with intellectual disability: a systematic review. Heliyon. (2024) 10:e28241. doi: 10.1016/j.heliyon.2024.e28241
55. Young, NL, Barden, WS, Burke, TA, Law, M, and Boydell, KM. Evaluation of a youth-to-adult transition program for young people with disabilities in Alberta. Canada Child Care Health Dev. (2021) 47:310–8. doi: 10.1111/cch.12813
56. Beresford, B, Moran, N, Sloper, P, and Mitchell, W. Transition to adult services and adulthood for young people with autistic spectrum conditions: Final report. York: Social Policy Research Unit, University of York (2013).
57. Fortuna, RJ, Robbins, BW, Mani, N, and Halterman, JS. Dependence on emergency care among young adults in the United States. J Gen Intern Med. (2016) 31:663–71. doi: 10.1007/s11606-016-3606-2
58. Durbin, A, Sirotich, F, Lunsky, Y, and Durbin, J. Unmet needs of adults in community mental health care with and without intellectual and developmental disabilities: a cross-sectional study. Community Ment Health J. (2017) 53:15–26. doi: 10.1007/s10597-015-9961-6
59. Durbin, A, Jung, JKH, Chung, H, Lin, E, Balogh, R, and Lunsky, Y. Prevalence of intellectual and developmental disabilities among first generation adult newcomers, and the health and health service use of this group: a retrospective cohort study. PLoS One. (2019) 14:e0215804. doi: 10.1371/journal.pone.0215804
60. Harris, P. Culturally competent disability support: putting it into practice: a review of the international and Australian literature on cultural competence. NSW: Patrick Harris Multicultural Disability Advocacy Association of NSW (2004).
61. Blackburn, C, Spencer, N, and Read, J. Prevalence of childhood disability and the characteristics and circumstances of disabled children in the UK: secondary analysis of the family resources survey. BMC Pediatr. (2010) 10:1–13. doi: 10.1186/1471-2431-10-21
62. Goodley, D. Disability studies: An interdisciplinary introduction. 2nd ed. London: SAGE Publications (2017).
63. Stienstra, D. Canadian disability policies in a world of inequalities. Societies. (2018) 8:36. doi: 10.3390/soc8020036
64. Arakelyan, M, Freyleue, SD, Schaefer, AP, Austin, AM, Moen, EL, O'Malley, AJ, et al. Rural–urban disparities in health care delivery for children with medical complexity and moderating effects of payer, disability, and community poverty. J Rural Health. (2024) 40:326–37. doi: 10.1111/jrh.12827
65. Dintino, R, Wakely, L, Wolfgang, R, Wakely, K, and Little, A. Powerless facing the wave of change: the lived experience of providing services in rural areas under the National Disability Insurance Scheme. Rural Remote Health. (2019) 19:5337. doi: 10.22605/RRH5337
66. Tøssebro, J. Disabled children and welfare policy in the Nordic countries: historical notes In: R Traustadóttir, B Ytterhus, ST Egilson, and B Berg, editors. Childhood and disability in the Nordic countries. Studies in childhood and youth. London: Palgrave Macmillan (2015). 51–68.
67. Singh, SP, Paul, M, Ford, T, Kramer, T, Weaver, T, McLaren, S, et al. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. Br J Psychiatry. (2010) 197:305–12. doi: 10.1192/bjp.bp.109.075135
68. Meade, MA, Mahmoudi, E, and Lee, SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil. (2015) 37:632–41. doi: 10.3109/09638288.2014.938176
69. Halfon, N, and Hochstein, M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. (2002) 80:433–79. doi: 10.1111/1468-0009.00019
70. Etikan, I, Musa, SA, and Alkassim, RS. Comparison of convenience sampling and purposive sampling. Am J Theor Appl Stat. (2016) 5:1–4. doi: 10.11648/j.ajtas.20160501.11
71. Government of British Columbia. Cross-ministry transition planning protocol for youth with support needs. Victoria (BC): Government of British Columbia (2012).
72. Government of Alberta. Transition planning: Supporting youth with disabilities in transitioning to adulthood. Edmonton (AB): Government of Alberta (2014).
73. Varty, M, Speller-Brown, B, Phillips, L, and Kelly, KP. Youths’ experiences of transition from pediatric to adult care: an updated qualitative metasynthesis. J Pediatr Nurs. (2020) 55:201–10. doi: 10.1016/j.pedn.2020.08.021
74. Huang, KY, Kwon, SC, Cheng, S, Kamboukos, D, Shelley, D, Brotman, LM, et al. Unpacking partnership, engagement, and collaboration research to inform implementation strategies development: theoretical frameworks and emerging methodologies. Front Public Health. (2018) 6:190. doi: 10.3389/fpubh.2018.00190
75. Doucet, S, Splane, J, Luke, A, Cassie, J, Klassen, M, Marshall, D, et al. Programmes to support paediatric to adult healthcare transitions for youth with complex care needs and their families: a scoping review. Child Care Health Dev. (2022) 48:659–92. doi: 10.1111/cch.12984
76. Vu, T, and MacDougall, D. Rural Health Care Planning Initiatives and Frameworks. Canadian J Health Technol. (2022):2. doi: 10.51731/cjht.2022.484
77. Government of British Columbia. Integrated child and youth teams. Victoria (BC): Government of British Columbia (2023).
78. Arfa, S, Solvang, PK, Berg, B, and Jahnsen, R. Disabled and immigrant, a double minority challenge: a qualitative study about the experiences of immigrant parents of children with disabilities navigating health and rehabilitation services in Norway. BMC Health Serv Res. (2020) 20:134. doi: 10.1186/s12913-020-5004-2
79. Köck, P, Meyer, M, Elsner, J, Dürsteler, KM, Vogel, M, and Walter, M. Co-occurring mental disorders in transitional aged youth with substance use disorders: a narrative review. Front Psychol. (2022) 13:827658. doi: 10.3389/fpsyt.2022.827658
Keywords: neurodevelopment, transition, access, disability, stakeholders, barriers, facilitators, policy
Citation: Senevirathna AM, Basualto P, Seth A, Dimitropoulos G and Zwicker JD (2025) Service access for youth with neurodevelopmental disabilities transitioning to adulthood: service providers’ and decision-makers’ perspectives on barriers, facilitators and policy recommendations. Front. Public Health. 13:1612509. doi: 10.3389/fpubh.2025.1612509
Edited by:
Aline Bogossian, Université de Montréal, CanadaReviewed by:
Gaurav Singhal, University of Wisconsin-Madison, United StatesRicardo De Moraes E. Soares, Naval School, Portugal
Ertila Druga, Universitat Bremen Sonderforschungsbereich, Germany
Copyright © 2025 Senevirathna, Basualto, Seth, Dimitropoulos and Zwicker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer D. Zwicker, endpY2tlcjFAdWNhbGdhcnkuY2E=
 Angela M. Senevirathna
Angela M. Senevirathna Patricia Basualto
Patricia Basualto Ashish Seth
Ashish Seth Gina Dimitropoulos
Gina Dimitropoulos Jennifer D. Zwicker
Jennifer D. Zwicker