- 1Health Technology Assessment India, Department of Health Research, Ministry of Health & Family Welfare, New Delhi, India
- 2Health Technology Assessment India, Regional Resource Hub, ICMR-Regional Medical Research Centre, Bhubaneswar, India
- 3Department of General Medicine, S.C.B. Medical College & Hospital, Cuttack, India
- 4Department of Medicine, Kalinga Institute of Medical Sciences, Bhubaneswar, India
- 5Department of Psychiatry, Kalinga Institute of Medical Sciences, Bhubaneswar, India
Multimorbidity presents major challenges to healthcare systems worldwide. Assessing health-related quality-of-life (HRQoL) in multimorbid patients is essential for understanding the overall impact of the patient’s health conditions on wellbeing and the complexities of patient management. This study assessed the HRQoL of multimorbid patients in India using the EQ-5D-5L value set. This observational study included 906 patients from tertiary healthcare facilities in Odisha, India, and used consecutive time-based sampling methods, conducted from January to April 2023. The study examined the relationship between HRQoL measures and utility scores using ordinary least squares regression and multiple regression analysis. The results showed that mean utility scores decreased as the number of health conditions increased, with scores of 0.677 for one condition, 0.577 for two conditions, 0.354 for three conditions, and 0.098 for four or more conditions. Combining stroke/paralysis with other health issues resulted in negative utility ratings. The findings showed that younger age (p = 0.003), urban residence (p = 0.027), higher education (p = 0.018), being married (p = 0.006), engaging in physical activity (p = 0.001), and having fewer health conditions were independently associated with higher utility scores. The study highlights the correlation between multimorbidity and HRQoL in older adults, highlighting implications for healthcare systems and clinical and policy decisions for multimorbid patients.
Introduction
Multimorbidity, characterised by the simultaneous presence of two or more chronic health conditions in an individual, has profound implications for the health-related quality of life (HRQoL) (1–3). The intricate interplay of multiple health issues often presents formidable challenges in the management of daily activities, exerting impacts on both physical and mental wellbeing (4). Individuals grappling with multimorbidity may encounter limitations in functional capacity, leading to an overall decline in their HRQoL (5). Managing the consequences of multiple health conditions, scheduling multiple medications, and navigating intricate healthcare systems can lead to increased stress levels and reduced satisfaction in daily activities. Furthermore, the cumulative effects of multiple chronic conditions may intensify symptoms, diminish resilience, and impede one’s ability to participate in social activities (6, 7). Understanding and appropriately addressing the various consequences of multimorbidity, specifically its influence on HRQoL, is essential for developing comprehensive healthcare strategies to enhance the overall wellbeing of individuals coping with the complexities of managing multiple chronic health conditions.
Currently, there is a growing emphasis on understanding diseases and healthcare from the perspective of patients, emphasising patient-reported outcome measures (8). Therefore, the importance of HRQoL data for patient-centred care has increased, offering a valuable understanding of individuals’ subjective experiences regarding their health and wellbeing (9). Furthermore, evaluating HRQoL enables healthcare practitioners to assess the influence of medical treatments and interventions on the overall wellbeing of patients (10, 11). The HRQoL data are crucial for informing healthcare decision-making processes by providing a comprehensive view of the physical, mental, and social dimensions of health (12–14). Additionally, previous studies have underscored the critical role of nurses’ awareness, attitude, and self-efficacy in ensuring patient safety (9–11). Collectively, these factors contribute to creating a safer healthcare environment, ultimately improving health outcomes and HRQoL for patients, including those with multimorbidity. This information is crucial for prioritising interventions, allocating resources effectively, and shaping policies to meet diverse patient populations’ needs.
The literature indicates that HRQoL among multimorbid patients is generally lower compared to individuals with single chronic conditions due to the cumulative burden of multiple conditions and complexity in the management of multiple conditions (8–12). Despite recognising the impact of multimorbidity on HRQoL, existing research in the Indian context is limited in exploring how specific combinations of chronic conditions influence HRQoL scores derived from the EQ-5D-5L. Additionally, there is a lack of comprehensive data on the prevalence and severity of multimorbidity across different demographic and socioeconomic groups in India (13–15). The EQ-5D-5L, a widely used instrument for measuring HRQoL, has been validated, utilising the EQ-5D-5L value set for India (16), highlighting the need for integrated healthcare approaches to improve the overall quality of life among multimorbid patients. Addressing these gaps is essential for designing targeted interventions and informing health policy, underscoring the need for further studies to elucidate the nuanced relationship between multimorbidity patterns and quality of life outcomes. However, there is a research gap in understanding how specific patterns of multimorbidity affect HRQoL among Indian patients, and therefore, further study is essential to fill that gap by assessing the relationship between multimorbidity combinations and EQ-5D-5L-based quality of life scores in the Indian context.
Multimorbidity can significantly affect patients’ relationships, lead to increased financial burdens due to ongoing healthcare costs, and pose challenges in accessing appropriate medical services, especially in resource-limited settings. Given India’s rising burden of chronic diseases and the growing prevalence of multimorbidity, understanding its impact on HRQoL is particularly relevant to inform targeted healthcare strategies and improve patient outcomes in the Indian context (3, 4). Addressing these social dimensions is essential for a comprehensive understanding of the true burden of multimorbidity and for developing holistic interventions to improve overall wellbeing. The HRQoL constitutes a crucial element in economic modelling, specifically within decision trees and Markov models. The EQ-5D-5L stands out as a widely employed generic tool for assessing and appraising health status (15). It furnishes a straightforward descriptive profile and a single index for health status, applicable in both clinical and economic evaluations of healthcare, as well as in population health surveys. Despite the prevalent use of EQ-5D-5L in health technology assessment in India, the country lacked a dedicated EQ-5D-5L value set. Recently, Jyani et al. (16) addressed this gap by providing utility scores for each health state within the Indian context (16). The hypothesis proposed that people with multiple chronic conditions may face more restrictions in physical and functional activities, lowering their overall HRQoL. Furthermore, it was hypothesised that the HRQoL for older people with multimorbidity would be lower than for their younger counterparts. Therefore, in this study, we assessed the self-perceived HRQoL of multimorbid patients in India using the EQ-5D-5L value set—utility score for each health state. This will provide information for health technology assessment as well as additional guidelines for future clinical and policy decision-making for the management of multimorbid patients in India.
Methods
Study design, participants, and setting
An observational study was conducted among patients aged ≥18 years who visited the medicine outpatient department (OPD) at two tertiary healthcare and teaching hospitals in the state of Odisha, India. We have included patients aged 18 years and above attending the medicine OPD; first-time attendees on the designated sampling days, and patients providing informed consent to participate in the study. We have excluded the patients unable to participate due to insufficient cognition or debilitating conditions, inpatients, repeat visitors previously interviewed in the current study, and patients unwilling to participate or who refused consent. The participating facilities were the Kalinga Institute of Medical Science, Bhubaneswar (private), and SCB Medical College in Cuttack (public), representing both private and public healthcare sectors.
Sample size and sampling frame
The complex multimorbidity prevalence in India was 34.5% (17). The calculation of the sample size was predicated on specific parameters, including the population size (N) with a finite population correction factor, a hypothesized 34.5% frequency of the outcome factor (p), 95% confidence limits (Z1 − α/2 = 1.96), precision (d = 0.1), and the design effect for cluster surveys (DEFF = 1). The sample size (n) was determined using the equation: n = [DEFF*Np(1-p)]/ [d2/Z21-α/2*(N-1) + p*(1-p)]. The resulting required sample size was determined to be 348 at each facility.
We used consecutive time-based sampling methods. Through discussions with healthcare professionals at each institution, it was determined that approximately 70–100 adult patients visited the medicine OPD daily. Among them, a minimum of 25 were first-time attendees. Consequently, the decision was made to include all first-time visitors on every alternate working day, totalling around 12 days per month. This approach aimed to enrol at least 10 patients per day over 4 months, to reach a sample size of 480 patients at each facility. We were able to collect 403 responses from private and 503 from public health facilities. Data collection took place from January to April 2023.
Study variables and data collection procedure
We used a pre-validated structured Multimorbidity Assessment Questionnaire for Primary Care (MAQ-PC) to collect data. This instrument has a high internal consistency (Cronbach’s alpha: 0.69), interrater reliability (Cohen’s Kappa: 0.78–1), and test–retest reliability (ICC: 0.970–0.741) (18). A tablet-based Open Data Kit (ODK) format was designed to efficiently capture information encompassing socio-demographic details, multimorbidity assessment, and EQ-5D-5L. The multimorbidity assessment section of the MAQ-PC included self-reported doctor-diagnosed chronic conditions such as diabetes, musculoskeletal disorders, acid peptic disease, disabilities, visual and hearing impairments, arthritis, neurological conditions, chronic lung disease, cancer, tumour, thyroid diseases, heart disease and stroke, chronic kidney diseases, hypertension, and certain chronic infectious diseases like tuberculosis, HIV, and filariasis.
To enhance data validity, these self-reported conditions were cross-validated using prescription records obtained from patient pharmacy data. A subset of the data was used to construct a misclassification matrix comparing self-reported diagnoses with prescription-based diagnoses. The sensitivity, specificity, and predictive values indicated high concordance (substantial agreement, kappa = 0.78). Conditions were selected based on their clinical relevance, prevalence in the population, and data availability. Conditions with very low prevalence or unreliable self-reporting were excluded to improve data quality and analytical robustness.
The EQ-5D-5L, a commonly employed health-related quality-of-life tool, entails a thorough evaluation of an individual’s health status across five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression (16, 19). Each dimension encompasses five response levels, providing a more detailed assessment. For each dimension, a single question is posed, with five options on a Likert scale ranging from 1 (indicating no problems) to 5 (signifying an inability to perform the activity or experiencing extreme pain, anxiety, or depression). The EQ5D tool was evaluated the validity, reliability, and responsiveness of in regional language (Odia) version (20).
Consenting participants were interviewed following consultation with the relevant physician in the medicine department, ensuring minimal disruption to the hospital’s system. Exit interviews facilitated a comprehensive recording of diagnoses by reviewing prescriptions. To prevent duplication, each of the patients received a unique identification number, and those previously interviewed in the current study were excluded later. Exclusions from the study comprised patients unable to participate, those with insufficient cognition, and individuals with debilitating conditions who were unwilling to take part. Four public health professionals with previous experience in multimorbidity data collection conducted the interviews. They were proficient in the local language and skilled in quantitative interviews.
The study received ethical approval from the Institutional Ethics Committee of ICMR-Regional Medical Research Centre, Bhubaneswar (ICMR-RMRCBB/IHEC-2021/93 Date 30/12/2021). Written informed consent was acquired from all participants, with measures in place to guarantee patient confidentiality and anonymity. When patients could not provide necessary information, caregivers were approached for relevant details. Additionally, the hospital and outpatient department’s approval was secured before initiating the data collection process.
Statistical analysis
The demographic attributes of the patients were depicted through descriptive statistics, specifically frequency and percentage. Recognizing the importance of age as a predictive factor for multimorbidity, as well as its impact on associated health outcomes and HRQoL, we chose to conduct all analyses with age stratification—categorizing individuals into three groups: 18–39 years, 40–59 years, and 60 years and above. Individuals aged 60 and above are officially classified as older people or senior citizens, according to the 1999 National Policy for Older People (20). Disease conditions with a prevalence exceeding 10 percent, such as Hypertension (HT), Diabetes (DB), Acid peptic disease (APD), Arthritis (AT), Chronic respiratory disease (CRD), and Stroke/paralysis (SP), were selected for the calculation of dyads and triads.
Data gathered by the EQ-5D-5L from participants undergo conversion into a health utility index, offering a quantitative assessment of the overall health state. The EQ-5D-5L score, derived from the five questions, spans a theoretical range from −0.923 (indicating a state worse than death) to 1 (representing the best possible health state). The utility values for all 3,125 conceivable health states were sourced from Jyani et al. (16) within the Indian context. The average utility score and standard deviation were computed for each disease condition. Likewise, the mean utility score with standard deviation for multimorbidity conditions—ranging from one to four, and four and above—as well as diverse combinations of dyad and triad among different age groups, was determined. For dyad and triad scenarios, conditions with at least five or more occurrences were taken into account for the calculation of the mean utility score.
In order to explore factors associated with HRQoL, the univariate association between independent variables and HRQoL measures (utility score) was examined using ordinary least squares regression. Additionally, a hierarchical multiple regression analysis was then conducted to determine the relationship between demographic variables, clinical outcomes (multimorbidity conditions) and lifestyle variables (physical activity – exercise) with utility score. In step 1, a linear regression model was constructed to evaluate the relationship between utility score (dependent variables) and demographic variables such as age, sex, residence, education, ethnicity, marital status and occupations. This approach allowed for the assessment of the independent effect of each demographic factor on utility scores while controlling for others. In step 2, the analysis was extended to include clinical outcomes (multimorbidity conditions) and lifestyle variables (physical activity – exercise) were added to the model. A multivariable linear regression model was used to examine the combined influence of these factors on utility scores, with all relevant variables entered simultaneously. The significance level was set at p < 0.05. Furthermore, using the distribution-based method, the standard deviation of the utility scores was calculated, and the minimally important difference (MID) was estimated. Statistical analyses were conducted using STATA 16 (Stata Corp, College Station, TX, USA).
Results
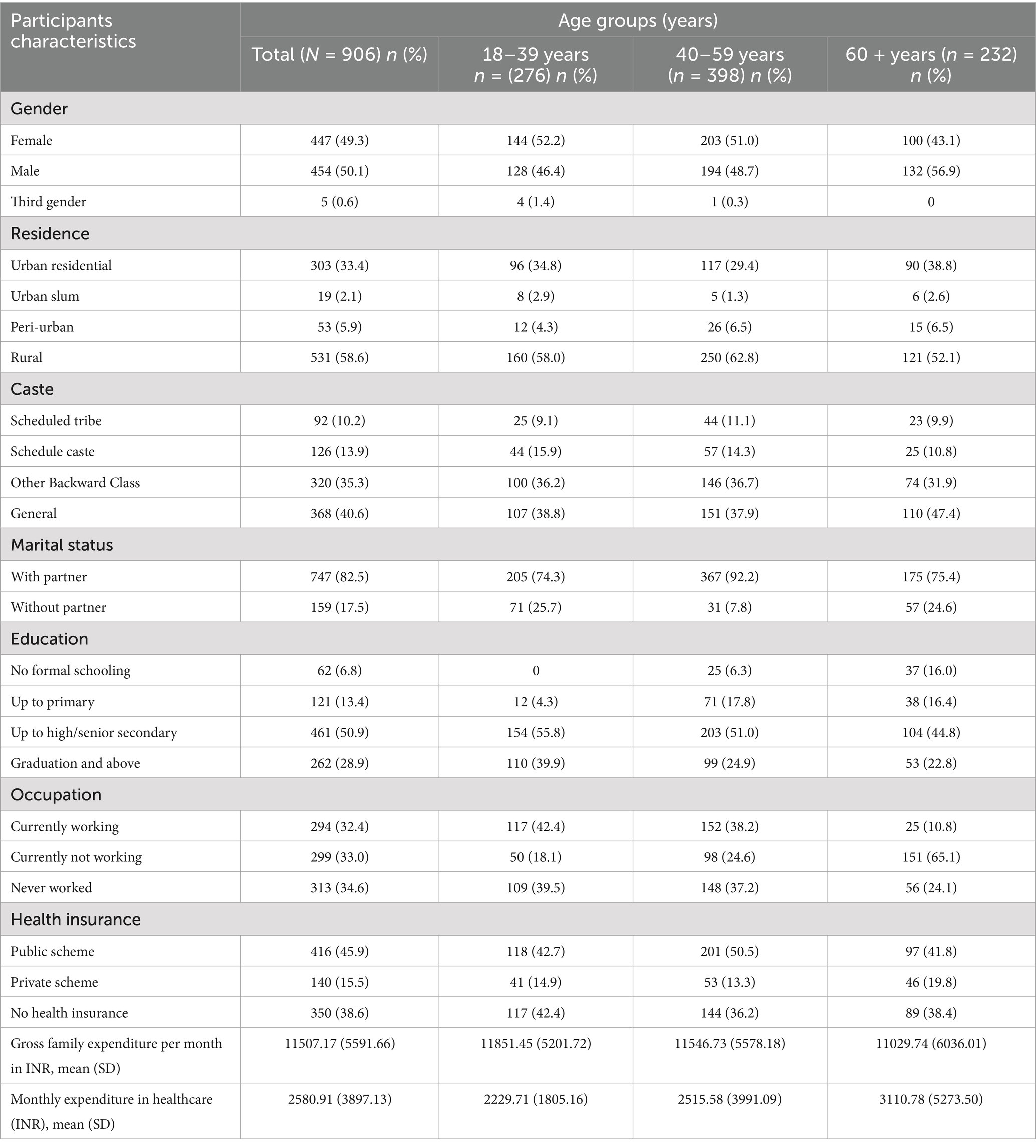
The study included 906 participants, with 276 in the 18–39 age group, 398 in the 40–59 age group, and 232 in the 60 and above age group. In the participant group, 49% were female, 50% were male, and approximately 1% identified as third-gender. Approximately 59% reside in rural areas, 40% belong to the general caste, and 51% have completed high school/senior secondary education. Approximately 39% lacked health insurance coverage, and the mean monthly healthcare expenditure was 2,581 INR (Indian Rupees). Table 1 provides an in-depth overview of the participants’ characteristics.
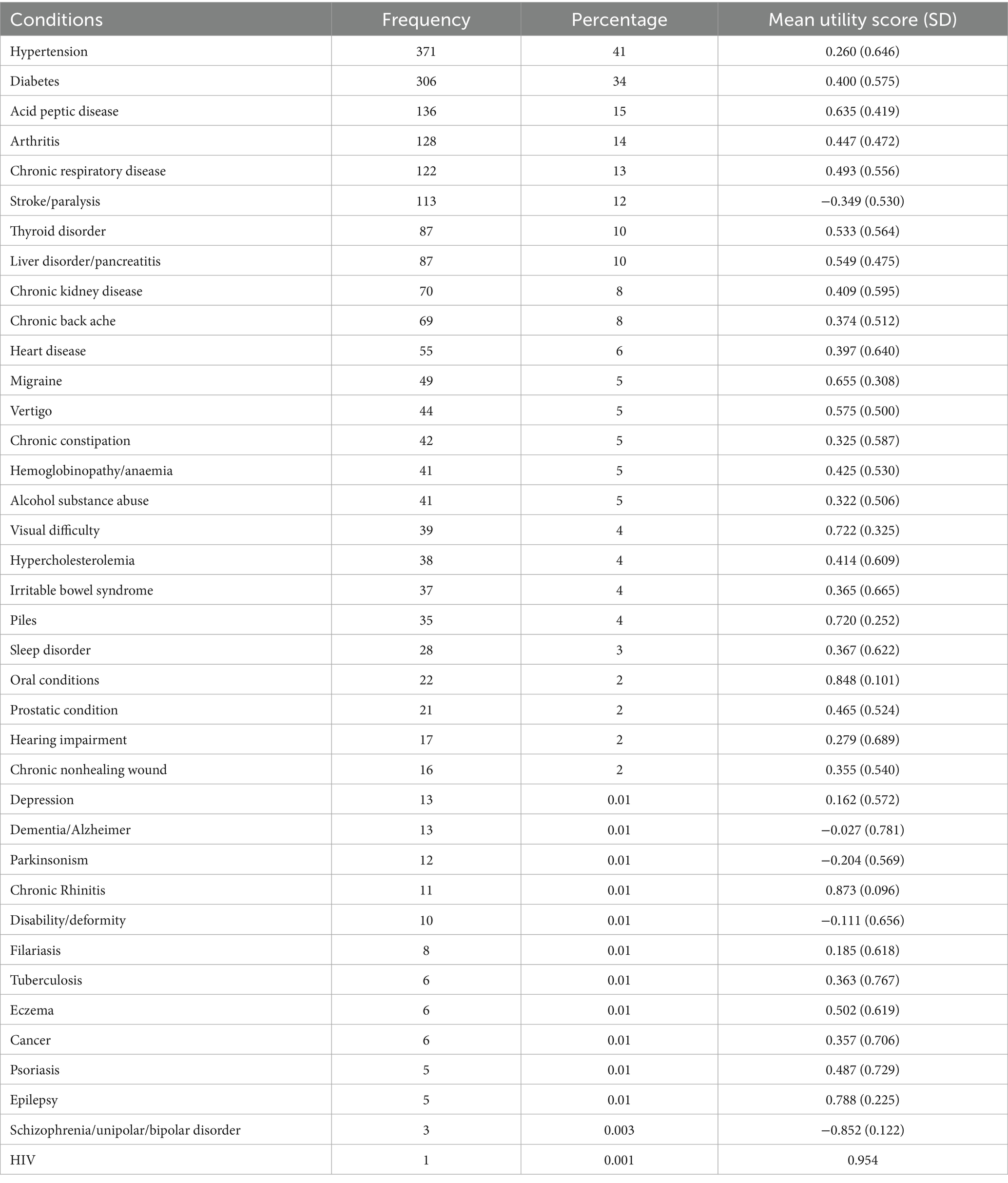
Table 2 details the reported conditions, encompassing a total of 38, with the six most frequently mentioned being hypertension (41%, mean utility score 0.260), diabetes (34%, mean utility score 0.4), acid peptic disease (15%, mean utility score 0.635), arthritis (14%, mean utility score 0.447), chronic respiratory disease (13%, mean utility score 0.493), and stroke/paralysis (12%, −0.349). Notably, conditions such as schizophrenia/unipolar/bipolar disorder (n = 3, mean utility score −0.852), stroke/paralysis (n = 113, mean utility score −0.349), parkinsonism (n = 12, mean utility score −0.204), disability/deformity (n = 10, mean utility score −0.111), and dementia/Alzheimer (n = 13, mean utility score −0.027) exhibited negative utility scores. Further specifics on disease-specific mean utility scores are presented in Table 2.
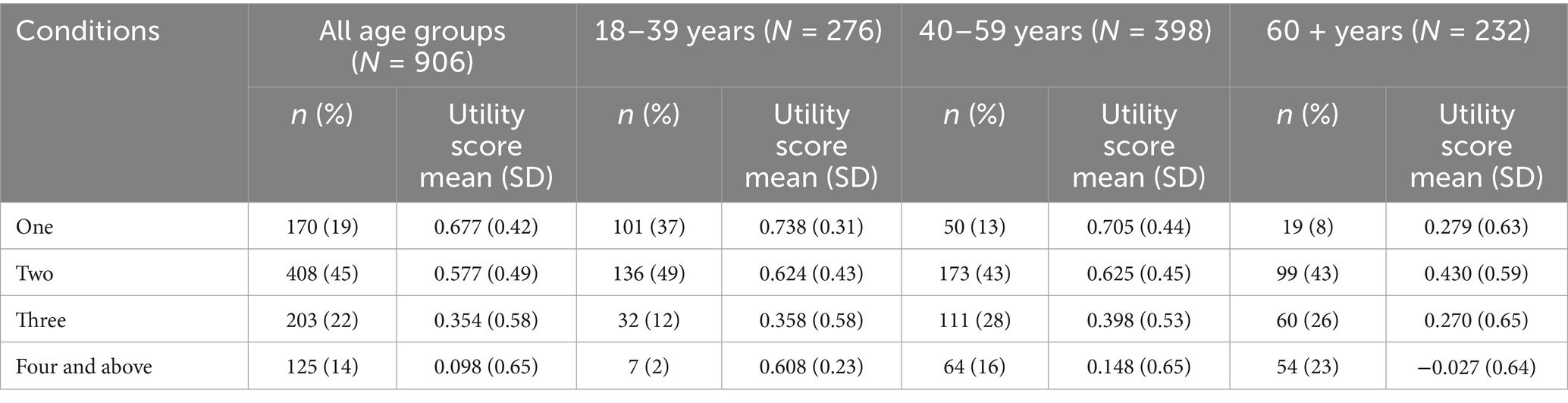
The comprehensive mean utility scores for multimorbidity conditions across different age groups are outlined in Table 3. Of the participants, 19% exhibited one condition with a utility score of 0.677, 45% presented with two conditions, registering a mean utility score of 0.577, 22% had three conditions with a mean utility score of 0.354, and 14% had four or more conditions, reflecting a mean utility score of 0.098 (Table 3). It was noted that across all age groups, as the number of conditions increased, the utility score exhibited a decline. Additionally, the overall utility score in the older age group was found to be lower compared to other age groups. Specifically, within the older age group, when the number of conditions reached four or more, the utility score was recorded as −0.027.
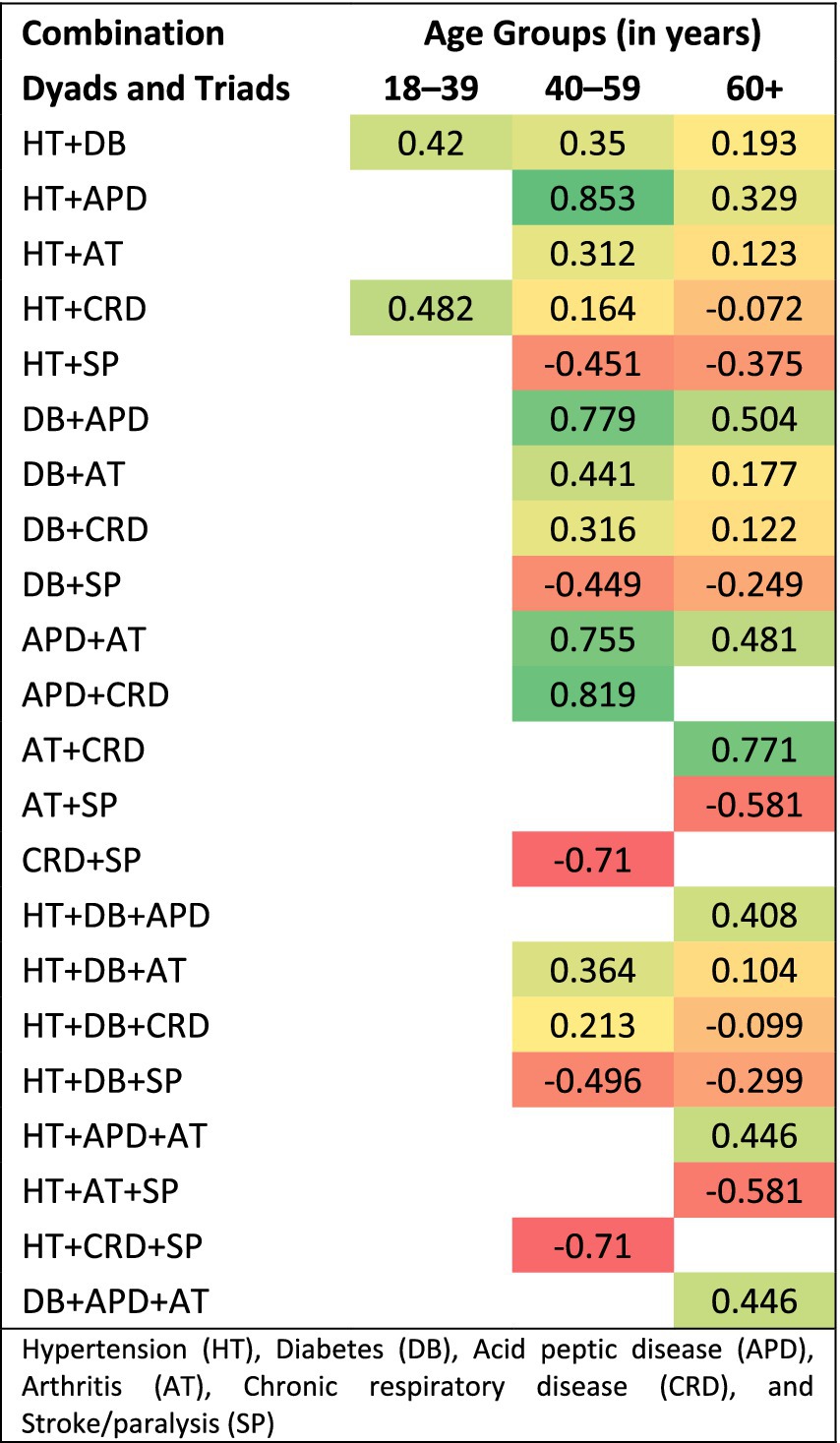
Table 4 presents the mean utility scores of multimorbidity, considering various combinations (dyad and triad) of conditions across different age groups. Within dyad conditions, the pairing of stroke/paralysis with other conditions like hypertension (mean utility score −0.403), diabetes (mean utility score −0.338), acid peptic disease (mean utility score −0.091), arthritis (mean utility score −0.519), and chronic respiratory disease (mean utility score −0.710) resulted in a negative value. Likewise, combining diabetes with chronic respiratory disease yielded a negative value, with a mean utility score of −0.636. Similarly, in triad conditions, combining stroke/paralysis with other health conditions led to a negative value. Within both dyad and triad combinations, the mean utility score for Quality of Life in older age groups was relatively lower than in other age groups. Figure 1 shows the heatmaps on the influence of dyads and triads on utility scores by age group.
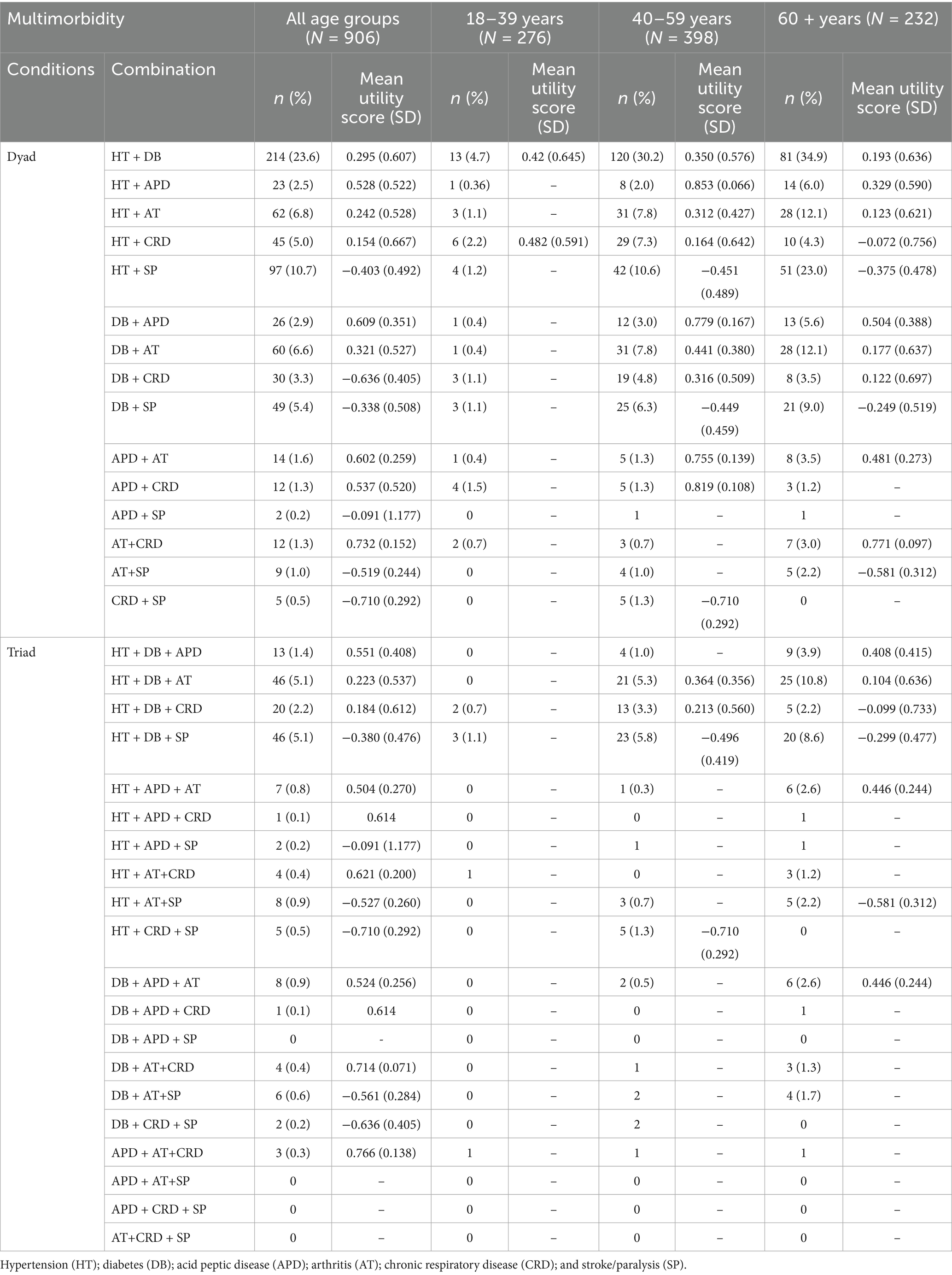
Table 4. Mean utility score of multimorbidity with various combinations (dyad and triad) of conditions among various age groups.
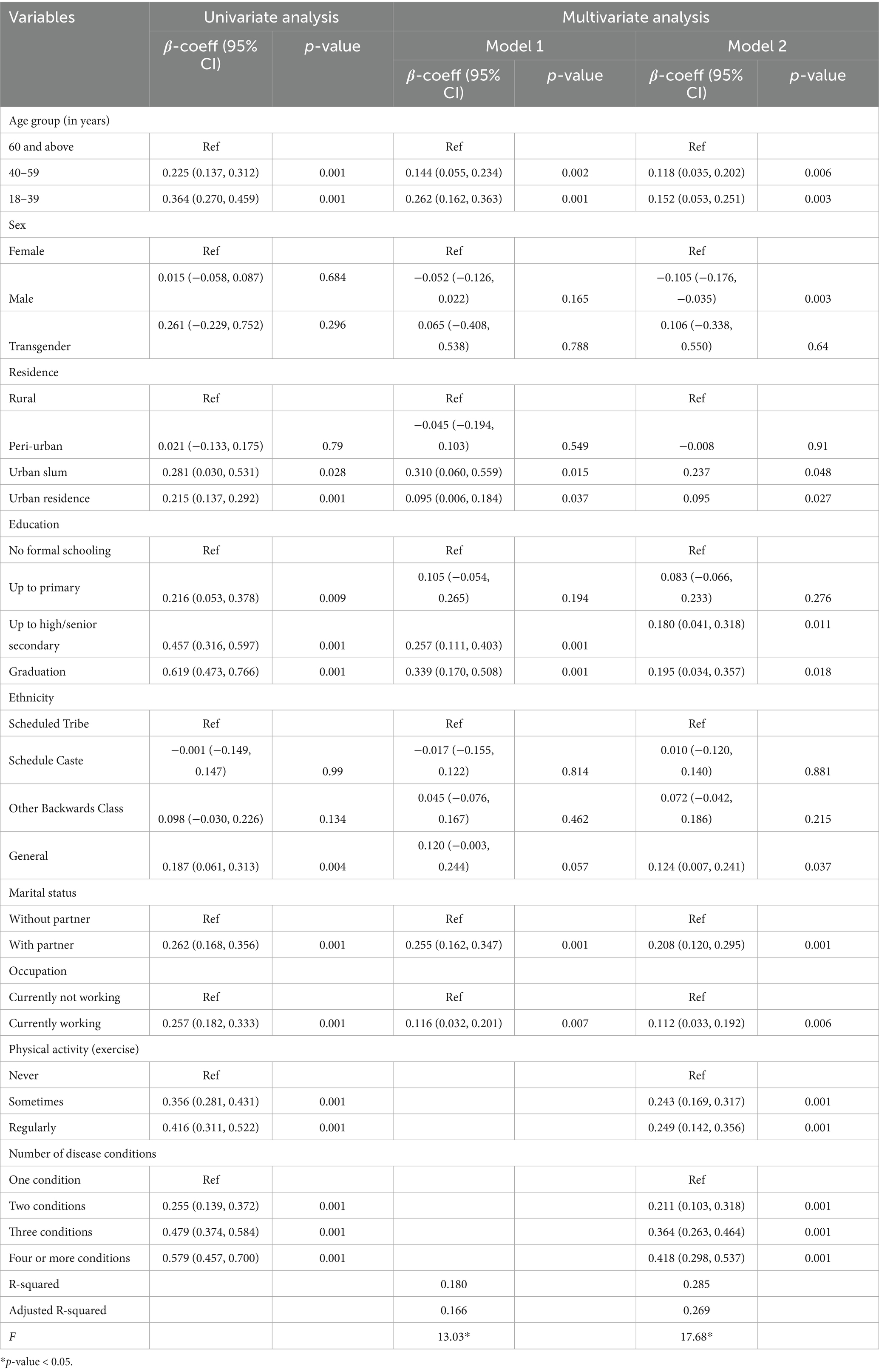
The univariate analysis results (Table 5) showed that younger groups (18–39 and 40–59) have significantly higher utility scores (better HRQoL) compared to the ≥60 reference group. The 18–39 age group shows the strongest positive association. Urban slum residents and urban residents generally have higher utility scores compared to rural residents, with urban slum residents showing a significant difference. Higher education levels (up to high/senior secondary and graduation) are significantly associated with higher utility scores. Having a partner was significantly associated with higher utility scores. Individuals who were currently employed had higher utility scores. Sometimes or regularly exercising was associated with higher utility scores. More health conditions were associated with lower utility scores. Males and females, as well as ethnicity, did not significantly differ in their utility scores.
When adjusted for basic demographics (model 1), such as age, residence, education, marital status, occupation, physical activity, and number of conditions, remain significantly associated with utility scores (Table 5). When the fully adjusted model, including all variables (model 2), includes physical activity and multimorbidity conditions, younger age groups still had higher utility scores, urban residents continue to show higher utility scores, and higher education remains positively associated. Having a partner continues to predict higher utility scores. Regular and sometimes exercising had been linked with better utility scores. However, more disease conditions reduce utility scores (Table 5). The full model explains about 27% (adjusted R2 ≈ 0.27) of the variation in utility scores, which was moderate. The F-test indicates the models were statistically significant overall.
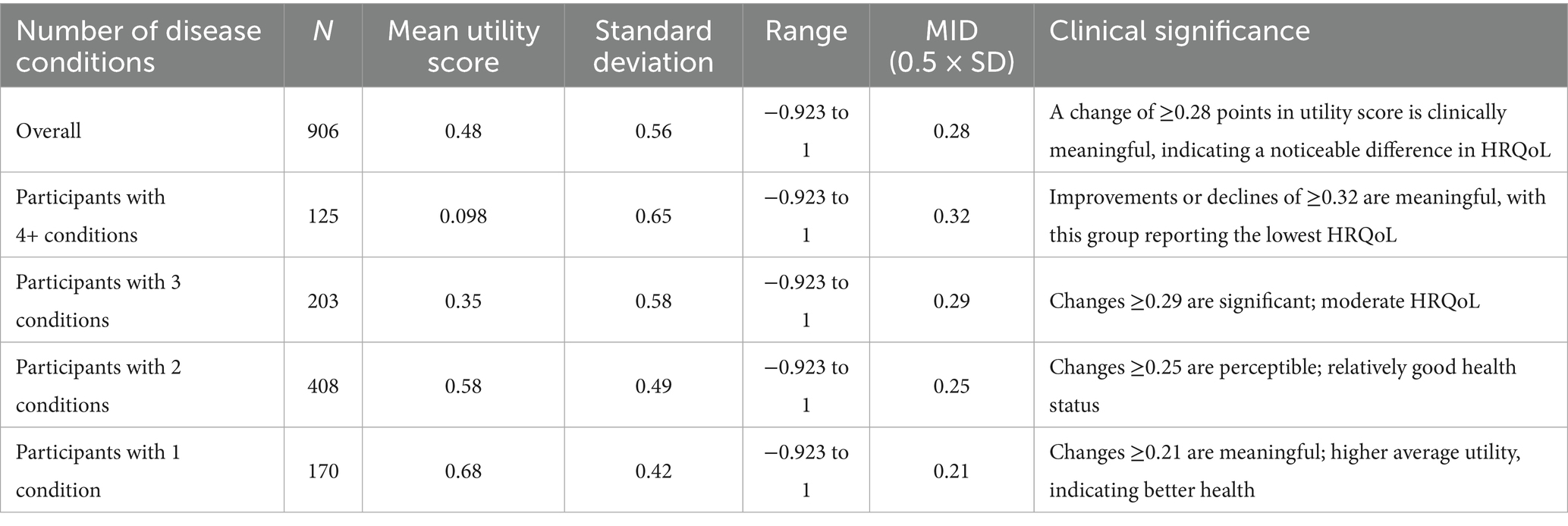
Across the sample, utility scores varied widely, with an overall mean of approximately 0.48, reflecting moderate health-related quality of life. Participants with multiple conditions tended to have lower average utility scores, while those with only one condition reported higher scores. The variability was substantial, with standard deviations ranging from about 0.42–0.65, and scores spanning from negative values (worse than death) up to perfect health (Table 6).
Discussion
The study evaluated the HRQoL of multimorbid patients using the EQ-5D-5L value set for India. It identified prevalent health conditions such as hypertension, diabetes, and stroke, revealing a significant decline in mean utility scores as the number of conditions increased. Specifically, utility scores declined from 0.677 for one condition to 0.098 for four or more conditions, with older adults particularly affected. Negative utility scores were associated with severe conditions like schizophrenia and stroke. The study found that younger age, urban living, higher education, marital status, regular physical activity, and fewer health conditions correlated with higher utility scores. The minimum important difference for perceived meaningful change in utility scores ranged from 0.21 to 0.32 points, indicating that more significant changes are necessary for those with multiple conditions.
Understanding the patterns of common health conditions is critical for healthcare professionals and policymakers in developing targeted interventions. Recognizing the specific conditions that are common in a population allows healthcare professionals to tailor their approaches to early detection, diagnosis, and treatment. This knowledge enables the development of specialised care plans and interventions that address the distinct challenges presented by each common health condition. As a result, the HRQoL measurement is critical for understanding how chronic conditions, multimorbidity, and polypharmacy affect patients’ health. Studies such as Bhadhuri et al. (21) and Wong et al. (22) emphasised the importance of using standardised instruments such as the EQ-5D-3L and EQ-5D-5L to assess self-reported health status among older patients with significant multimorbidity and polypharmacy (21–23). These studies highlight the need for comprehensive evaluation tools that can capture the complexities of health conditions and their impact on HRQoL, particularly in vulnerable populations. Furthermore, Peters et al.’s study sheds light on the impact of multimorbidity on HRQoL among primary care patients, emphasising the importance of self-efficacy in managing multiple health conditions (6, 24). Understanding the relationship between self-efficacy and HRQoL is critical for designing interventions that assist patients in dealing with their health issues and improving their overall wellbeing.
To improve responsiveness to the individual needs and experiences of patients with multiple health conditions, healthcare systems must take a holistic, patient-centred approach. Integrated care models, which encourage collaboration among various healthcare professionals, are critical for addressing the interconnected complexities of multimorbidity. Community collaboration addresses social determinants of health, and continuous monitoring and feedback systems enable timely adjustments to care plans. Previous research has highlighted the high healthcare costs associated with multimorbidity and its impact on HRQoL, particularly after hospitalisation (25–27). These findings emphasise the importance of integrated and patient-centred care models that address the complex needs of multimorbid patients while also considering the economic implications of their healthcare management. Furthermore, previous research has shed light on the catalogue of chronic conditions and psychosocial factors associated with HRQoL, contributing to our understanding of the multifaceted nature of HRQoL assessment in chronic disease patients (28–31). The findings highlight the importance of taking a comprehensive approach to assessing HRQoL in patients with multimorbidity, taking into account both clinical and psychosocial factors, to better inform healthcare interventions and outcomes.
Individuals with multimorbidity are more likely to use health-care services, require complex medications, and have polypharmacy than those without. As a result, recognising and addressing multimorbidity is critical in shaping the design of effective healthcare systems. Previous studies relied on value sets from Thailand and the United Kingdom because there was no India-specific EQ-5D-5L value set available. As a result, developing an India-specific EQ-5D-5L value set became critical to ensuring more transparent and consistent decision-making (16). This analysis improves understanding of individuals’ health-related quality of life, providing useful insights for healthcare professionals, researchers, and policymakers (32, 33). It makes it easier to assess the effects of interventions, allows for more informed decision-making, and contributes to population wellbeing.
This study examines the impact of identified health conditions on quality of life, particularly those with low utility scores, as well as the difficulties and implications of managing multiple conditions. The study expands on age disparities, focusing on lower mean utility scores in the older age group with multiple conditions, and investigates potential causes and implications for tailored healthcare strategies (31). The importance of holistic healthcare approaches is emphasised, recognising the complex interplay of multiple health conditions and proposing strategies for healthcare systems to better support individuals with multimorbidity, particularly in ageing populations. Policymakers can use this information to better allocate resources, design public health campaigns, and implement policies that address the identified health concerns. Furthermore, understanding these patterns helps predict future healthcare needs and design preventive strategies. This targeted approach not only optimises healthcare resource allocation but also improves intervention effectiveness, resulting in better health outcomes for both individuals and communities. In essence, a nuanced understanding of common health conditions enables healthcare professionals and policymakers to implement strategic and effective measures that address the specific health needs of the population they serve.
The results emphasise that conditions such as stroke/paralysis and schizophrenia/unipolar/bipolar disorder are associated with significantly negative utility scores, which suggests a significant decrease in quality of life. In contrast, diseases such as acid peptic disease and diabetes, despite their prevalence, have relatively higher mean utility scores, which implies a less significant impact on HRQoL (5). An analysis that is more nuanced and investigates the impact of specific disease combinations, such as stroke with hypertension or arthritis with chronic respiratory disease, on the overall decline in utility scores, would offer a more comprehensive understanding of the relative burden of various conditions. Furthermore, the interpretation of these results would be strengthened by an understanding of the reasons why certain conditions have a more profound impact, whether it be due to the severity of symptoms, disability, or psychological effects. Targeted interventions to enhance HRQoL among patients with multimorbidity would be informed by such an exhaustive investigation, which would also contextualise the quantitative findings.
The results have substantial implications for the geriatric populations of India and other LMICs. As the prevalence of multimorbidity increases, older individuals experience significant declines in HRQoL, with the mean utility decreasing by nearly four times (from 0.677 to 0.098). The low scores were linked to severe conditions, including schizophrenia and stroke, underscoring the necessity of targeted integrative interventions in the older adults population to enhance their quality of life. Moreover, the estimation of QALYs at the population level will be facilitated by quantified disease-specific HRQoL, which will be useful for cost-effectiveness research and the allocation of resources for any rehabilitation programs, assistive devices, and home-based care among the geriatric population in India. Additionally, early screening and care for anxiety and depression among older populations may enhance QALYs and their opportunities for social engagement.
Implications for policy and practices
• Promoting lifestyle modifications, recognizing multimorbidity’s social and psychological implications, and investing in community-based support programs, mental health services, and medication subsidies can improve access and affordability for patients.
• Nurses should promote lifestyle modifications such as regular physical activity and health education among patients, particularly in younger populations. Enhancing access to preventive and early diagnostic services, especially in rural and underserved areas. In order to address the holistic needs of patients, nurses should support community-based programs and mental health services.
• This study recommends clinicians for prioritizing integrated care models for managing multiple conditions through comprehensive care approaches. Incorporate utility score assessments into clinical evaluations to enhance comprehension of patient requirements. Recognizing the psychological effects of multimorbidity, including stress, anxiety, and depression, and integrating psychosocial support into care.
• Policymakers should improve access to preventive services, invest in community-based support programs, and subsidize essential medications. Addressing social determinants of health and supporting research on sociodemographic factors can improve healthcare access and quality of life.
Limitations of the study
The study faces limitations regarding its sampling method and sample size, which may affect the generalizability of its findings on India’s multimorbid patient population. Although efforts were made to include participants from both private and public healthcare sectors, the recruitment from two tertiary hospitals in a single state may not represent the diversity of multimorbid patients across the country. The sample size, calculated based on relevant parameters, was smaller than intended, particularly in the private sector, hindering comparisons of HRQoL between public and private facilities. Moreover, given the observational study design and the sampling strategy employed, several potential biases may influence the study findings. Selection bias could arise due to the inclusion of only patients attending the medicine outpatient departments on designated days, potentially excluding individuals with different health-seeking behaviors or those unable to visit the hospital, particularly the severely ill, disabled, or those from remote areas, which may limit the generalizability of the results. The patients with cognitive impairments or debilitating conditions were excluded, which could underestimate the prevalence or impact of multimorbidity in the broader patient population.
Additionally, the sample was insufficient to analyze disease combinations by burden and their impact on quality of life, potentially introducing bias and affecting precision. Exclusion criteria, such as cognitive ability and refusal to participate, may have omitted valuable insights. Although the findings have demonstrated that an increase in the number of diseases results in a decrease in the health utility score, however, the relationship between specific diseases and their severity of impact on HRQoL is not thoroughly examined. These limitations highlight the need for further research with larger, more diverse samples to enhance the robustness and applicability of the findings. The study reports disease-specific utility scores and explores combinations of conditions, but it does not conduct an in-depth analysis of the individual impact of each disease on HRQoL within the regression models. These limits understanding of how specific conditions, such as depression or diabetes, independently influence quality of life, which could be addressed in future analyses for more nuanced insights.
Conclusion
The findings reveal that multimorbidity significantly reduces HRQoL, particularly in older adults with multiple health conditions. Moreover, conditions like stroke, parkinsonism, and dementia notably worsen utility scores, especially when combined. The findings stress the necessity for comprehensive healthcare strategies aimed at improving wellbeing in complex medical scenarios. Furthermore, context-specific minimal important difference thresholds are crucial for interpreting utility scores; smaller changes are significant for those with fewer conditions, while larger shifts are needed for those with multiple ailments. This understanding is vital for clinicians and researchers in assessing interventions and monitoring disease progression effectively.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the study received ethical approval from the Institutional Ethics Committee of ICMR-Regional Medical Research Centre, Bhubaneswar (ICMR-RMRCBB/IHEC-2021/93 Date 30/12/2021). Written informed consent was acquired from all participants, with measures in place to guarantee patient confidentiality and anonymity. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KS: Project administration, Visualization, Methodology, Resources, Formal analysis, Investigation, Supervision, Data curation, Conceptualization, Writing – original draft. AS: Methodology, Writing – original draft, Formal analysis, Conceptualization, Data curation, Investigation. GD: Visualization, Methodology, Writing – review & editing, Investigation. RS: Investigation, Visualization, Writing – review & editing, Data curation, Methodology. DB: Project administration, Methodology, Investigation, Funding acquisition, Writing – review & editing. PD: Investigation, Resources, Data curation, Project administration, Writing – review & editing. LM: Writing – review & editing, Methodology, Investigation, Visualization, Project administration, Conceptualization. PM: Resources, Conceptualization, Project administration, Writing – review & editing, Methodology. KR: Investigation, Writing – review & editing, Resources, Methodology, Project administration. SP: Supervision, Writing – original draft, Investigation, Resources, Formal analysis, Data curation, Methodology, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The present research was funded by the Department of Health Research, Ministry of Health and Family Welfare, Government of India.
Acknowledgments
We thank the respondents who agreed to spare time and gave us the data for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
LMICs, low-and-middle income countries; HIC, high income countries; NCD, non-communicable diseases; HRQoL, health-related quality of life.
References
1. Lefèvre, T, d’Ivernois, JF, De Andrade, V, Crozet, C, Lombrail, P, and Gagnayre, R. What do we mean by multimorbidity? An analysis of the literature on multimorbidity measures, associated factors, and impact on health services organization. Rev Epidemiol Sante Publique. (2014) 62:305–14. doi: 10.1016/j.respe.2014.09.002
2. Agborsangaya, CB, Lau, D, Lahtinen, M, Cooke, T, and Johnson, JA. Health-related quality of life and healthcare utilization in multimorbidity: results of a cross-sectional survey. Qual Life Res. (2013) 22:791–9. doi: 10.1007/s11136-012-0214-7
3. Pati, S, Swain, S, Knottnerus, JA, Metsemakers, JF, and van den Akker, M. Health related quality of life in multimorbidity: a primary-care based study from Odisha, India. Health Qual Life Outcomes. (2019) 17:1. doi: 10.1186/s12955-019-1180-3
4. Pati, S, Mahapatra, P, Dwivedi, R, Athe, R, Sahoo, KC, Samal, M, et al. Multimorbidity and its outcomes among patients attending psychiatric care settings: an observational study from Odisha, India. Front Public Health. (2021) 8:616480. doi: 10.3389/fpubh.2020.616480
5. Makovski, TT, Schmitz, S, Zeegers, MP, Stranges, S, and van den Akker, M. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. (2019) 53:100903. doi: 10.1016/j.arr.2019.04.005
6. Peters, M, Kelly, L, Potter, CM, Jenkinson, C, Gibbons, E, Forder, J, et al. Quality of life and burden of morbidity in primary care users with multimorbidity. Patient Rel Outcome Meas. (2018) 9:103–13. doi: 10.2147/PROM.S148358
7. Pati, S, Pati, S, Van Den Akker, M, Schellevis, FF, Jena, S, and Burgers, JS. Impact of comorbidity on health-related quality of life among type 2 diabetic patients in primary care. Prim Health Care Res Dev. (2020) 21:e9. doi: 10.1017/S1463423620000055
8. Salisbury, C, Man, MS, Bower, P, Guthrie, B, Chaplin, K, Gaunt, DM, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet. (2018) 392:41–50. doi: 10.1016/S0140-6736(18)31308-4
9. Russell, AM, Sprangers, MA, Wibberley, S, Snell, N, Rose, DM, and Swigris, JJ. The need for patient-centred clinical research in idiopathic pulmonary fibrosis. BMC Med. (2015) 13:1–7. doi: 10.1186/s12916-015-0475-4
10. Feeny, D. Health-related quality-of-life data should be regarded as a vital sign. J Clin Epidemiol. (2013) 66:706–9. doi: 10.1016/j.jclinepi.2012.12.013
11. Revicki, DA, Osoba, D, Fairclough, D, Barofsky, I, Berzon, R, Leidy, NK, et al. Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Qual Life Res. (2000) 9:887–900. doi: 10.1023/A:1008996223999
12. Longworth, L, and Rowen, D. Mapping to obtain EQ-5D utility values for use in NICE health technology assessments. Value Health. (2013) 16:202–10. doi: 10.1016/j.jval.2012.10.010
13. Rowen, D, Azzabi Zouraq, I, Chevrou-Severac, H, and van Hout, B. International regulations and recommendations for utility data for health technology assessment. Pharmacoeconomics. (2017) 35:11–9. doi: 10.1007/s40273-017-0544-y
14. Kennedy-Martin, M, Slaap, B, Herdman, M, van Reenen, M, Kennedy-Martin, T, Greiner, W, et al. Which multi-attribute utility instruments are recommended for use in cost-utility analysis? A review of national health technology assessment (HTA) guidelines. Eur J Health Econ. (2020) 21:1245–57. doi: 10.1007/s10198-020-01195-8
15. Devlin, N, Parkin, D, and Janssen, B. Methods for analysing and reporting EQ-5D data. Cham, Switzerland: Springer Nature (2020).
16. Jyani, G, Sharma, A, Prinja, S, Kar, SS, Trivedi, M, Patro, BK, et al. Development of an EQ-5D value set for India using an extended design (DEVINE) study: the Indian 5-level version EQ-5D value set. Value Health. (2022) 25:1218–26. doi: 10.1016/j.jval.2021.11.1370
17. Sinha, A, Kerketta, S, Ghosal, S, Kanungo, S, Lee, JT, and Pati, S. Multimorbidity and complex multimorbidity in India: findings from the 2017–2018 longitudinal ageing study in India (LASI). Int J Environ Res Public Health. (2022) 19:9091. doi: 10.3390/ijerph19159091
18. Pati, S, Hussain, MA, Swain, S, Salisbury, C, Metsemakers, JF, Knottnerus, JA, et al. Development and validation of a questionnaire to assess multimorbidity in primary care: an Indian experience. Biomed Res Int. (2016) 2016:1–9. doi: 10.1155/2016/6582487
19. van Reenen, M, and Janssen, B. EQ-5D-5L user guide: basic information on how to use the EQ-5D-5L instrument. Rotterdam: EuroQol Research Foundation (2015).
20. Tripathy, S, Hansda, U, Seth, N, Rath, S, Rao, PB, Mishra, TS, et al. Validation of the EuroQol five-dimensions-three-level quality of life instrument in a classical Indian language (Odia) and its use to assess quality of life and health status of cancer patients in eastern India. Indian J Palliat Care. (2015) 21:282–8. doi: 10.4103/0973-1075.164896
21. Bhadhuri, A, Kind, P, Salari, P, Jungo, KT, Boland, B, Byrne, S, et al. Measurement properties of EQ-5D-3L and EQ-5D-5L in recording self-reported health status in older patients with substantial multimorbidity and polypharmacy. Health Qual Life Outcomes. (2020) 18:1–7. doi: 10.1186/s12955-020-01564-0
22. Wong, EL, Xu, RH, and Cheung, AW. Measuring the impact of chronic conditions and associated multimorbidity on health-related quality of life in the general population in Hong Kong SAR, China: a cross-sectional study. PLoS One. (2019) 14:e0224970. doi: 10.1371/journal.pone.0224970
23. Govt of India. Ministry of Social Justice and Empowerment. (1999). National Policy for Older Persons. New Delhi: 2020.
24. Peters, M, Potter, CM, Kelly, L, and Fitzpatrick, R. Self-efficacy and health-related quality of life: a cross-sectional study of primary care patients with multi-morbidity. Health Qual Life Outcomes. (2019) 17:1. doi: 10.1186/s12955-019-1103-3
25. Salari, P, Henrard, S, O’Mahony, C, Welsing, P, Bhadhuri, A, Jungo, KT, et al. Healthcare costs and health-related quality of life in older multimorbid patients after hospitalization. Health Serv Insights. (2023) 16:11786329231153278. doi: 10.1177/11786329231153278
26. Shah, S, Abbas, G, Aslam, A, Randhawa, FA, Khan, FU, Khurram, H, et al. Assessment of health-related quality of life among patients with obesity, hypertension and type 2 diabetes mellitus and its relationship with multimorbidity. PLoS One. (2023) 18:e0289502. doi: 10.1371/journal.pone.0289502
27. Gebreyohannes, EA, Gebresillassie, BM, Mulugeta, F, Dessu, E, and Abebe, TB. Treatment burden and health-related quality of life of patients with multimorbidity: a cross-sectional study. Qual Life Res. (2023) 32:3269–77. doi: 10.1007/s11136-023-03473-3
28. Hvidberg, MF, Petersen, KD, Davidsen, M, Witt Udsen, F, Frølich, A, Ehlers, L, et al. Catalog of EQ-5D-3L health-related quality-of-life scores for 199 chronic conditions and health risks in Denmark. MDM Policy Practice. (2023) 8:23814683231159023. doi: 10.1177/23814683231159023
29. Singh, K, Kondal, D, Shivashankar, R, Ali, MK, Pradeepa, R, Ajay, VS, et al. Health-related quality of life variations by sociodemographic factors and chronic conditions in three metropolitan cities of South Asia: the CARRS study. BMJ Open. (2017) 7:e018424. doi: 10.1136/bmjopen-2017-018424
30. Van Wilder, L, Vandepitte, S, Clays, E, Devleesschauwer, B, Pype, P, Boeckxstaens, P, et al. Psychosocial factors associated with health-related quality of life in patients with chronic disease: results of a cross-sectional survey. Chronic Illn. (2023) 19:743–57. doi: 10.1177/17423953221124313
31. Kanesarajah, J, Waller, M, Whitty, JA, and Mishra, GD. Multimorbidity and quality of life at mid-life: a systematic review of general population studies. Maturitas. (2018) 109:53–62. doi: 10.1016/j.maturitas.2017.12.004
32. Pati, S, Pati, S, van den Akker, M, Schellevis, FG, Sahoo, KC, and Burgers, JS. Managing diabetes mellitus with comorbidities in primary healthcare facilities in urban settings: a qualitative study among physicians in Odisha, India. BMC Fam Pract. (2021) 22:99. doi: 10.1186/s12875-021-01454-4
Keywords: multimorbidity, quality of life, EQ-5D-5L, utility score, Health Technology Assessment, multiple long-term conditions
Citation: Sahoo KC, Sinha A, Dash GC, Sahoo RK, Bhattacharya D, Dash PC, Mohanty L, Mahapatra P, Rajsekhar K and Pati S (2025) Health-related quality of life among multimorbid patients using the EQ-5D-5L value set for India. Front. Public Health. 13:1612512. doi: 10.3389/fpubh.2025.1612512
Edited by:
Priyank Shukla, Ulster University, United KingdomReviewed by:
Mehrnaz Ahmadi, Ahvaz Jundishapur University of Medical Sciences, IranBodhayan Prasad, University of Glasgow, United Kingdom
Copyright © 2025 Sahoo, Sinha, Dash, Sahoo, Bhattacharya, Dash, Mohanty, Mahapatra, Rajsekhar and Pati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krushna Chandra Sahoo, c2Fob29rcnVzaG5hQHlhaG9vLmNvbQ==; Sanghamitra Pati, ZHJzYW5naGFtaXRyYTEyQGdtYWlsLmNvbQ==
 Krushna Chandra Sahoo
Krushna Chandra Sahoo Abhinav Sinha
Abhinav Sinha Girish Chandra Dash
Girish Chandra Dash Rakesh Kumar Sahoo
Rakesh Kumar Sahoo Debdutta Bhattacharya
Debdutta Bhattacharya Purna Chandra Dash3
Purna Chandra Dash3 Pranab Mahapatra
Pranab Mahapatra