- 1Sports and Health Research Center, Department of Physical Education, Tongji University, Shanghai, China
- 2International College of Football, Tongji University, Shanghai, China
- 3Department for Quality-of-Life Studies, Bologna University, Bologna, Italy
Aim: Non-depressed college students with high perceived stress represent a distinct preclinical population at elevated risk for psychological deterioration. While Tai Chi is established as a mind–body exercise for improving well-being in clinical and older populations, its targeted efficacy in this specific at-risk subgroup—particularly regarding integrated physical and mental health benefits—remains inadequately explored. This study aimed to investigate the effects of a 16-week Tai Chi program on comprehensive fitness outcomes in this population.
Methods: Eighty-eight non-depressed students with high perceived stress (Perceived Stress Scale scores between 38 and 56, Self-Rating Depression Scale scores below 50) were randomly assigned to a Tai Chi group (n = 47), which underwent a 16-week supervised program (3 sessions/week, 90 min/session), or a control group (n = 41) that maintained usual activities. Assessments pre- and post-intervention covered health-related physical fitness and mental health status (Perceived Stress Scale, Self-Rating Depression Scale, Pittsburgh Sleep Quality Index, Fatigue Scale-14, Hamilton Anxiety Scale, and SF-36).
Results: Compared to controls, the Tai Chi group showed significant between-group improvements in lower-limb muscular endurance (squat test), perceived stress, sleep quality, somatic anxiety, role limitations due to physical health, and social functioning (all p < 0.05). Significant enhancements were also observed in physical functioning, fatigue, and general mental health (all p < 0.05).
Conclusion: The 16-week Tai Chi intervention yielded concurrent benefits in physical and mental health among non-depressed college students with high perceived stress. These findings support Tai Chi as a feasible, multi-targeted preventive strategy against stress-related morbidity in this at-risk campus population.
Clinical trial registration: Identifier ChiCTR2400089594, http://www.chictr.org.cn/index.html.
1 Introduction
College students navigate a critical developmental transition, facing a confluence of academic pressures, career uncertainties, and complex social dynamics that significantly elevate their risk for chronic stress (1, 2). The high prevalence of perceived stress and anxiety in this population is a global concern, with reported rates ranging from 32% to over 55% (3, 4), a trend exacerbated by recent societal challenges such as the COVID-19 pandemic (5, 6). Chronic exposure to such stressors is not merely a subjective discomfort; it is robustly linked to measurable declines in sleep quality, physical health, and psychological well-being, thereby increasing the susceptibility to clinical disorders like anxiety and depression (7). Consequently, the World Health Organization has identified stress management as a paramount public health priority for student populations (8).
Within this broad context, a specific preclinical subgroup warrants particular attention: non-depressed students experiencing high perceived stress. These individuals, while not meeting the clinical threshold for depression, represent an at-risk population in the prodromal stage of potential psychological deterioration (9, 10). Sustained high stress is a known correlate of depression pathogenesis, potentially inducing neuroplastic alterations that pave the way for depressive onset (11). For this subgroup, prolonged stress already impairs daily functioning and academic performance (12, 13), creating a vulnerable state that, without timely intervention, can escalate to major depressive disorder or other adverse outcomes (9, 14). This positions them as a critical target for early, preventive interventions aimed at curbing the progression along the stress-depression continuum.
Exercise is widely recognized as a viable non-pharmacological intervention to mitigate stress-related risks (15). Meta-analytic evidence supports the efficacy of aerobic exercise in reducing depressive symptoms in student populations (16). Among various forms, Tai Chi, a low-intensity mind–body aerobic exercise, demonstrates particular promise due to its unique integration of physical activity with meditative focus and diaphragmatic breathing (17). A growing body of evidence documents its benefits for multidimensional effects, including physical, psychological and quality of life benefits (17–22). Systematic reviews and randomized controlled trials, conducted mainly in older adults and clinical populations, indicate that Tai Chi consistently improves functional fitness (including BMI, body fat, vital capacity, lower limb strength, balance/dynamic stability, and flexibility) and yields cardiometabolic benefits, including reductions in blood pressure and improvements in glycemic control (23). In parallel, its mental health benefits, such as reducing stress (17), anxiety (18), and depressive symptoms (24), are attributed to its proposed mechanisms of regulating autonomic function (e.g., reducing cortisol, increasing heart rate variability) and fostering psychological self-regulation through mindful movement (17, 23–29).
However, a significant literature gap remains. While the effects of Tai Chi are well-documented in older or clinically ill cohorts, its mechanisms and efficacy are underexplored in the specific, preclinical subgroup of non-depressed college students with high perceived stress. This population faces a distinct set of challenges and possesses different resilience resources compared to older or clinical groups. The question of whether Tai Chi’s documented physical and mental benefits can be translated to confer preventive, dual-domain protection in this young, high-risk, yet non-clinical population has not been systematically investigated. Their underrepresentation in targeted exercise intervention research highlights a missed opportunity for early prevention.
To address this gap, the present study aimed to examine the effects of a 16-week Tai Chi intervention on a comprehensive set of mental and health-related physical fitness outcomes within this target population. We hypothesized that Tai Chi would yield significant improvements in both domains compared to a control group. Furthermore, the study concurrently evaluated its feasibility as a practical, campus-based stress management tool. By pursuing these objectives, this research provides novel insights into Tai Chi’s preventive potential against stress-related morbidity in higher education contexts, offering empirical support for institutional well-being initiatives.
2 Methods
2.1 Participants
All interventions were approved by the University Ethics Committee (2021tjdx024). Participants were recruited via flyers, social media, and printed notices posted on campus. A total of 116 respondents were initially invited to visit the research department. The study protocol and objectives were explained in detail to all potential participants prior to data collection. Written informed consent was obtained from all participants before registration.
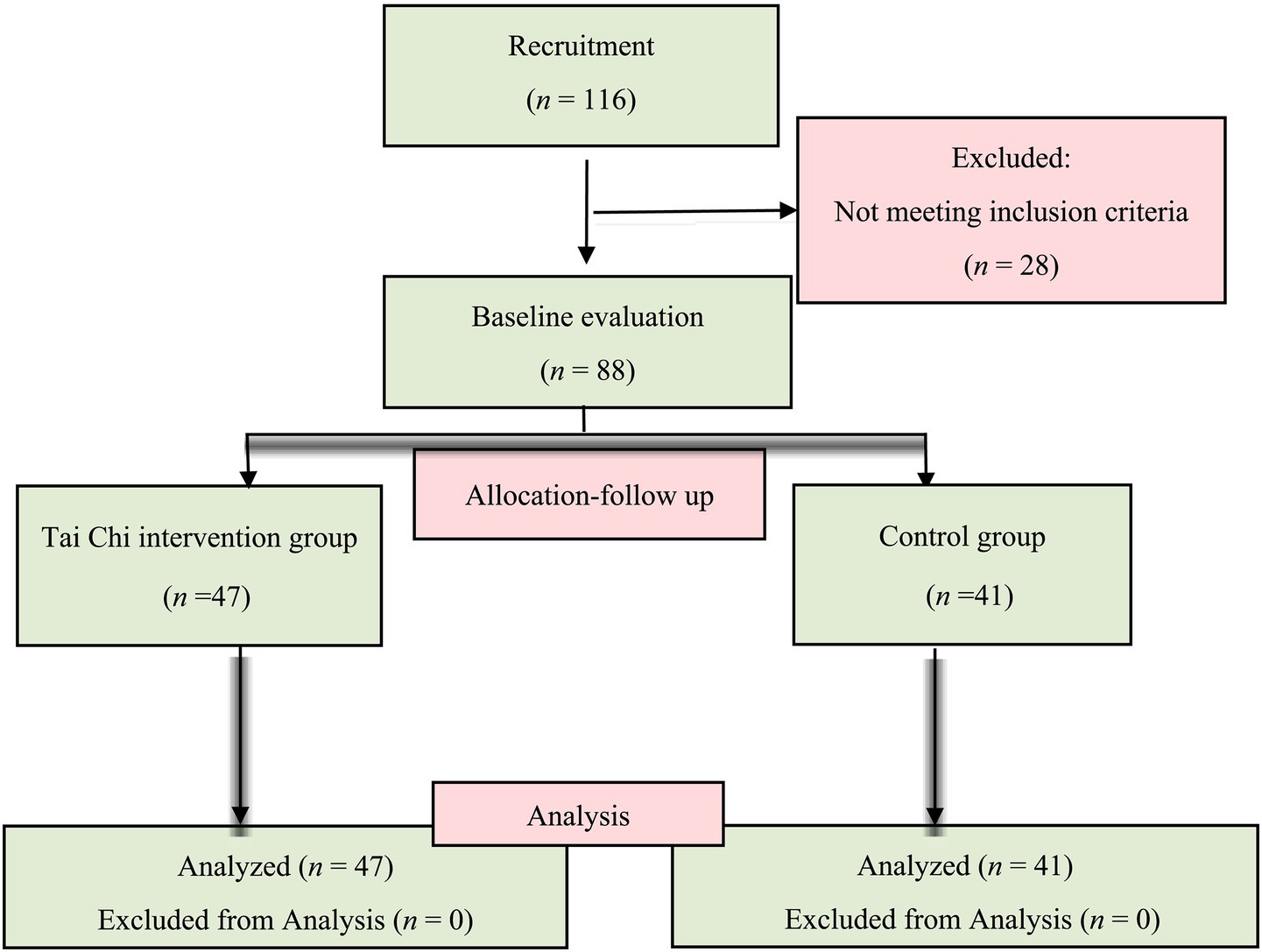
Participants were all undergraduate students from colleges, aged between 18 and 23. Participants were subjected to an initial screening that included completion of questionnaires to collect background information (e.g., sedentary behavior, medical history, current health status, etc.), and a physical examination. Based on the following inclusion exclusion criteria: (1) participants aged 18–23 years; (2) Perceived Stress Scale (PSS) scores between 38 and 56, confirming high perceived stress status (30); (3) Self-Rating Depression Scale (SDS) scores below 50 to ensure absence of depression; and (4) Kessler Psychological Distress Scale (K10) scores below 30 (excluding severe psychological distress), thereby maintaining relative psychological homogeneity in the sample and minimizing potential confounding effects of extreme psychological distress on primary outcomes; (5) Willing to accept the principle of randomization; (6) Willing to take the tests and sign an informed consent form. Those participants who satisfied the following criteria were excluded: (1) Suffering from a disease that affects their athletic performance; (2) Had a history of heart disease, severe arrhythmia, or pacemaker use; (3) Regular smokers or heavy drinkers of alcohol or other stimulating beverages; and (4) Taking medications that may affect their emotional responses, such as anxiolytics or antidepressants, at least 1 month before this study. A total of 88 students were eventually retained in the experiment (Figure 1).
2.2 Experimental procedures
Participants completed baseline assessments consisting of demographic questionnaires and standardized psychometric instruments: Pittsburgh Sleep Quality Index (PSQI), Hamilton Anxiety Scale (HAMA), the 14-item Fatigue Scale (FS-14) and 36-Item Short Form Health Survey (SF-36). Health-related physical fitness evaluations included eight standardized measures: (1) body weight and BMI, (2) resting heart rate, (3) vital capacity, (4) blood pressure, (5) one-minute sit-up test, (6) standing long jump, (7) one-minute squat test, and (8) eyes-closed single-leg balance test.
Sample size was determined from prior evidence (PMID: 25686304) indicating that a standardized mindful awareness practices intervention produced significant improvements in sleep quality, a stress-related outcome. Using G*Power for a two-tailed test (α = 0.05, Cohen’s d = 0.80), we estimated that 26 participants per group would be required. To ensure adequate power, we set a target sample size of 88 and subsequently randomized 88 university students to either a Tai Chi intervention group (n = 47), assigned to regular 24-form Yang-style Tai Chi practice, or a control group (n = 41) instructed to maintain their usual lifestyles (19). The intervention group received 4 weeks of foundational training from a senior Tai Chi instructor (20 years’ teaching experience), followed by a structured 16-week intervention (3 sessions/week, 90 min/session). Each session comprised: (1) 10-min warm-up (gentle stretching and breathing exercises), (2) 70-min core Tai Chi practice, and (3) 10-min cool-down (meditation and slow walking). All participants resided within the same closed-campus community. Adherence was ensured through dual oversight: a certified Tai Chi master/research assistant supervised all sessions, and participants signed standardized attendance sheets at every meeting.
2.3 Health-related physical fitness measurement
All assessments were administered between 14:00 and 17:00 in a temperature-controlled laboratory (24–26 °C) under standardized lighting. Participants abstained from caffeine and alcohol for at least 24 h before testing and rested quietly for at least 10 min upon arrival. To minimize fatigue carryover, tests followed a fixed sequence: (1) anthropometrics and vitals, (2) lung function, (3) balance, (4) muscular strength/power, and (5) muscular endurance. Unless otherwise specified, three trials were permitted with 1–2 min of passive rest between trials and ~3 min between different items; the best performance was retained for analysis.
Pulmonary function was indexed by forced vital capacity (FVC) (31), measured with a portable spirometry device (HK6000/6800 FH; Hengkang Jiaye, Shenzhen, China). During testing, participants grasped the mid-section of the mouthpiece with both hands, refrained from placing their lips on the tube during inspiration, and took care not to occlude the air outlet with their hands while exhaling.
Muscle strength was assessed using handgrip dynamometry and the standing long jump (SLJ) (32). Maximal voluntary grip strength was obtained with an electronic dynamometer (CAMRY-EH101; Hengkang Jiaye, Shenzhen, China) across three trials per hand. The SLJ was performed three times, and the greatest distance achieved was retained for analysis.
Muscular endurance was evaluated with one-minute sit-up and one-minute squat tests (33). For sit-ups, participants lay supine on a mat with feet at shoulder width, knees flexed, and arms crossed over the chest; a valid repetition required elbow-to-knee contact on the ascent and the shoulder blades touching the mat on the descent. The count of correct repetitions completed within 60 s was documented. For squats, participants adopted a natural stance with feet externally rotated about 30°. Throughout the movement, knees did not travel beyond the toes and were aligned with the direction of the toes; repetitions completed in 1 min were tallied.
Static balance was examined using a single-leg stance with eyes closed (34). Barefoot on a level surface, participants elevated one leg—maintaining approximately a 90° bend—while the contralateral foot remained on the floor. They were instructed to keep an upright posture and minimize sway. The trial ended if the eyes opened, the lifted foot touched down, or the arms were used for support. Time to loss of balance was recorded, with longer durations indicating superior static balance.
2.4 Questionnaire assessments
All questionnaires were administered in their validated Chinese versions between 14:00 and 17:00 in a quiet laboratory under standardized lighting with trained proctor supervision. Participants rested quietly for at least 10 min before testing and received uniform instructions. To reduce respondent burden and maintain consistency, a fixed sequence was used: (1) PSS, (2) SDS, (3) PSQI, (4) HAMA, (5) FS-14, and (6) SF-36. Brief intervals of approximately 1–2 min were provided between instruments. Proctors checked forms on site for completeness and clarity; any missing or multiple responses were corrected immediately before scoring.
This study employed internationally recognized standardized instruments—the PSS (35), SDS (36), PSQI (37), HAMA (38), FS-14 (39), and SF-36 (40)—all of which have well-documented reliability, validity, and responsiveness. These measures have been repeatedly used as primary or key secondary endpoints in randomized controlled trials and large cohort studies published in high-impact journals (41–45), thereby ensuring the scientific rigor, methodological standardization, and cross-study comparability of our outcome assessments. The PSS is a well-established psychometric instrument designed to evaluate an individual’s subjective experience of stress (35). Scores between 38 and 56 are classified as indicative of high stress, with progressively higher scores reflecting more severe perceived stress levels (46). The SDS quantifies the presence and intensity of depressive symptomatology (36). Each item is rated on a 4-point scale (1 = none or a little of the time to 4 = most or all of the time), yielding a total score from 20 to 80, with higher scores indicating greater symptom severity (36). PSQI score is derived from the sum of seven component scores, yielding a total ranging from 0 to 21 (47). Lower scores reflect better sleep quality, while higher scores indicate poorer sleep. A score above 5 typically signifies significant sleep disturbances (48). The HAMA widely applied in clinical and research settings, assesses anxiety severity across both psychological and somatic domains (49). The instrument comprises 14 items graded from 0 to 4, where 0 denotes no anxiety and 4 indicates marked severity. The aggregate score ranges from 0 to 56, providing a quantitative index of anxiety burden. Conventional interpretive bands are: values >17 suggest mild anxiety; scores of 17–23 indicate moderate anxiety; and scores of 25–30 denote severe anxiety (50). The FS14 is a fatigue perception questionnaire that assesses two key dimensions: physical fatigue and psychological fatigue. The total score ranges from 0 to 33, with higher scores indicating greater fatigue severity (51). The SF-36 is a widely used instrument for assessing health-related quality of life, measuring self-reported physical and mental health across eight domains (52): physical functioning (PF), role limitations due to physical health (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). Additionally, this questionnaire was utilized to evaluate changes in perceived health status over the preceding year (53).
Questionnaires were administered in their validated Chinese versions (50, 51, 54–58).
2.5 Statistical analysis
Statistical analyses of all data were performed using the SPSS statistical package (IBM SPSS Statistics, version 25). Extracted data included health-related physical fitness measures (anthropometrics and vitals, lung function, balance, muscular strength/power, and muscular endurance) and questionnaire scores (PSS, SDS, PSQI, HAMA, FS-14, and SF-36). For each outcome, means and standard deviations (SD) were calculated at baseline and after the 16-week intervention. Levene’s and Shapiro–Wilk tests were used to check the homogeneity of variance and normality of data, respectively. Between-group differences in change scores (Δ = Baseline – Post) were examined with independent-samples t-tests, and within-group pre–post changes were evaluated with paired t-tests for both physical and psychological outcomes. Two-sided p-values with 95% confidence intervals are reported, and statistical significance was set at α = 0.05.
3 Results
3.1 Baseline characteristics of non-depressed college students with high perceived stress
There was no significant difference in age (p = 0.062), sex distribution (p = 0.45), PSS (p = 0.31), SDS (p = 0.16) and K10 (p = 0.72) between the two groups (Table 1).
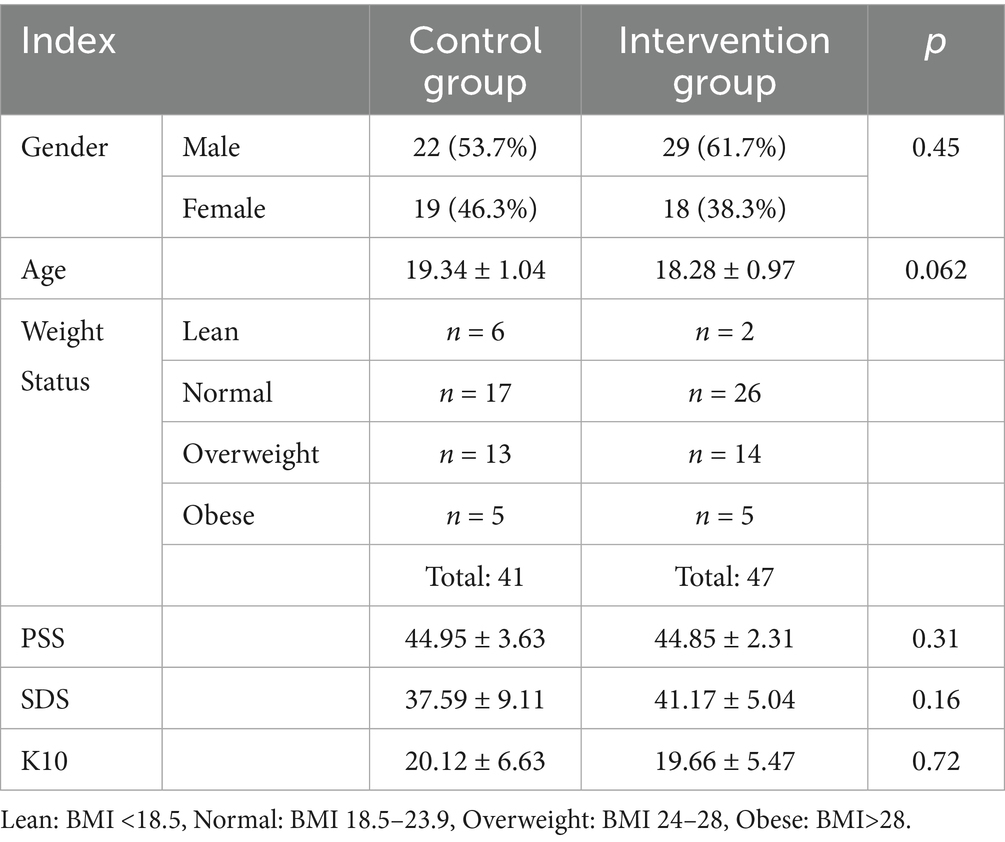
Table 1. Summary of basic characteristics of high perceived stress in non-depressed college students with high perceived stress.
3.2 Effects of tai chi exercise on physical outcomes in non-depressed college students with high perceived stress
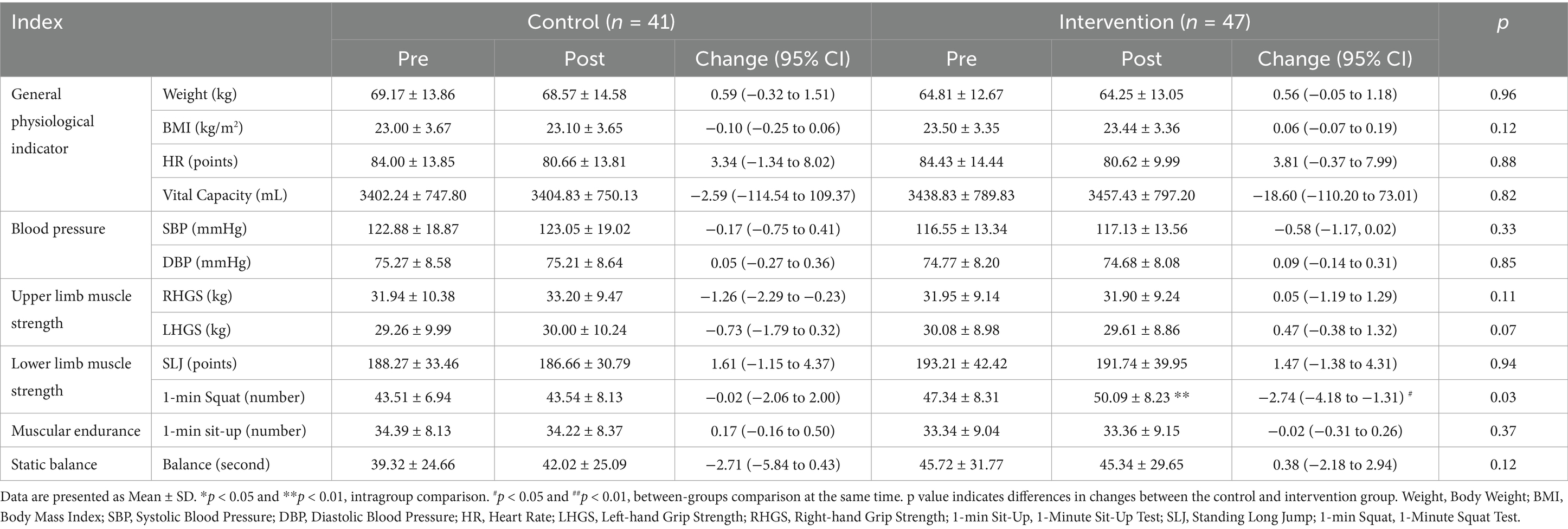
As shown in Table 2, within-group comparisons showed significant changes in the Tai Chi intervention group for the 1-min deep-squat test (p < 0.05); However, the participants in the control group did not show such changes (p > 0.05).
The between-group comparisons indicated that, following the 16-week Tai Chi intervention, participants in the intervention group exhibited a significant improvement in lower-limb muscle strength, as evidenced by a significant increase in the number of deep-squat repetitions completed in 1 min (p < 0.05).
3.3 Effects of tai chi exercise on mental outcomes in non-depressed college students with high perceived stress
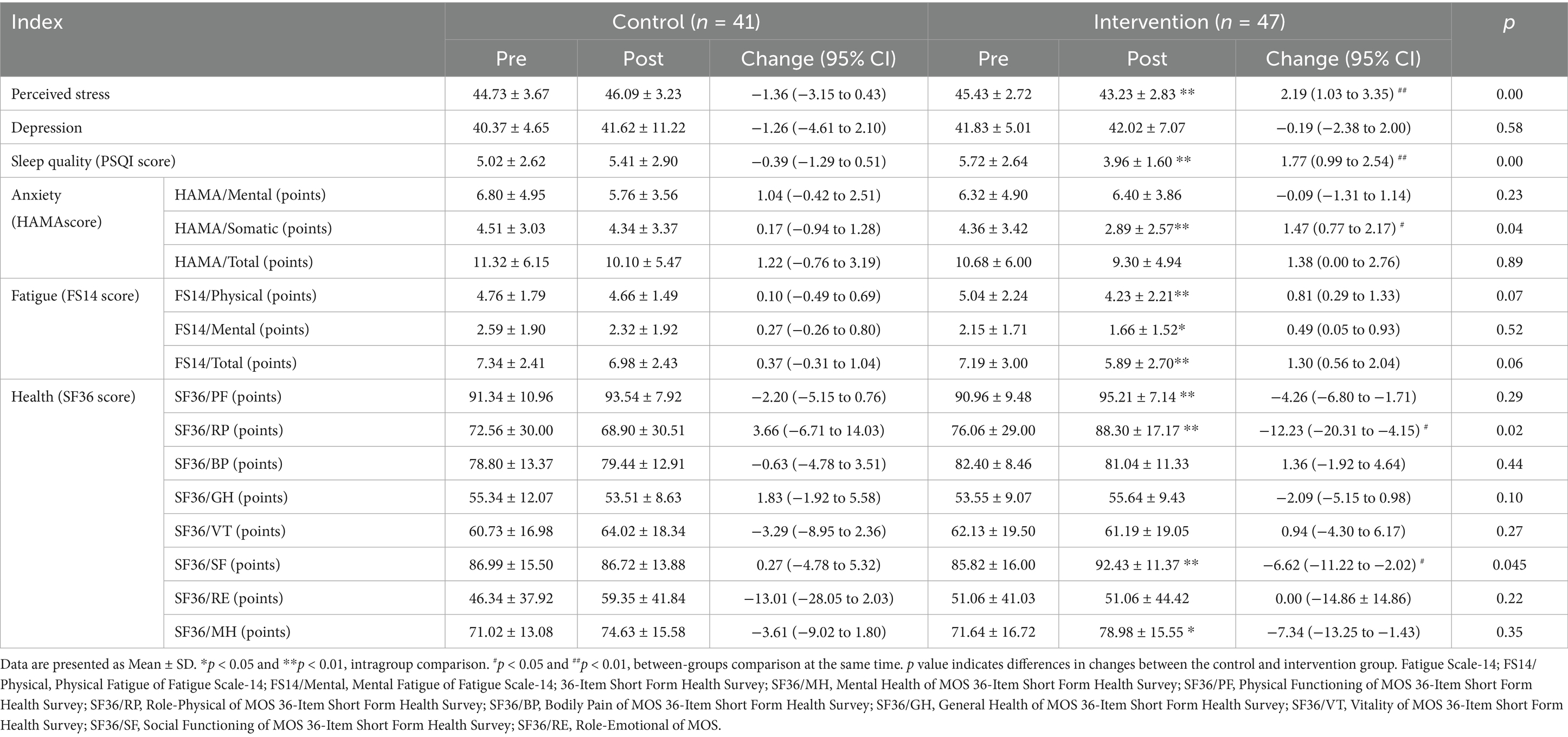
As shown in Table 3, within-group comparisons revealed significant improvements in the Tai Chi intervention group in perceived stress scores measured by the PSS questionnaire, sleep quality scores assessed by the PSQI questionnaire, body anxiety scores from the HAMA questionnaire, physical and mental fatigue scores as well as total scores in the FS-14 questionnaire, and physical functioning, social functioning, role limitations due to physical health, and mental health scores in the SF-36 questionnaire (p < 0.05). In contrast, no significant changes were observed in the control group (p > 0.05).
Between-group comparisons indicated that, following the 16-week Tai Chi intervention, participants in the intervention group demonstrated significant improvements in perceived stress, sleep quality, somatic anxiety, role limitations due to physical health, and social functioning, as reflected in the scores of the PSS, PSQI, the somatic anxiety subscale of the HAMA, and the role-physical and social functioning domains of the SF-36 (p < 0.05).
4 Discussion
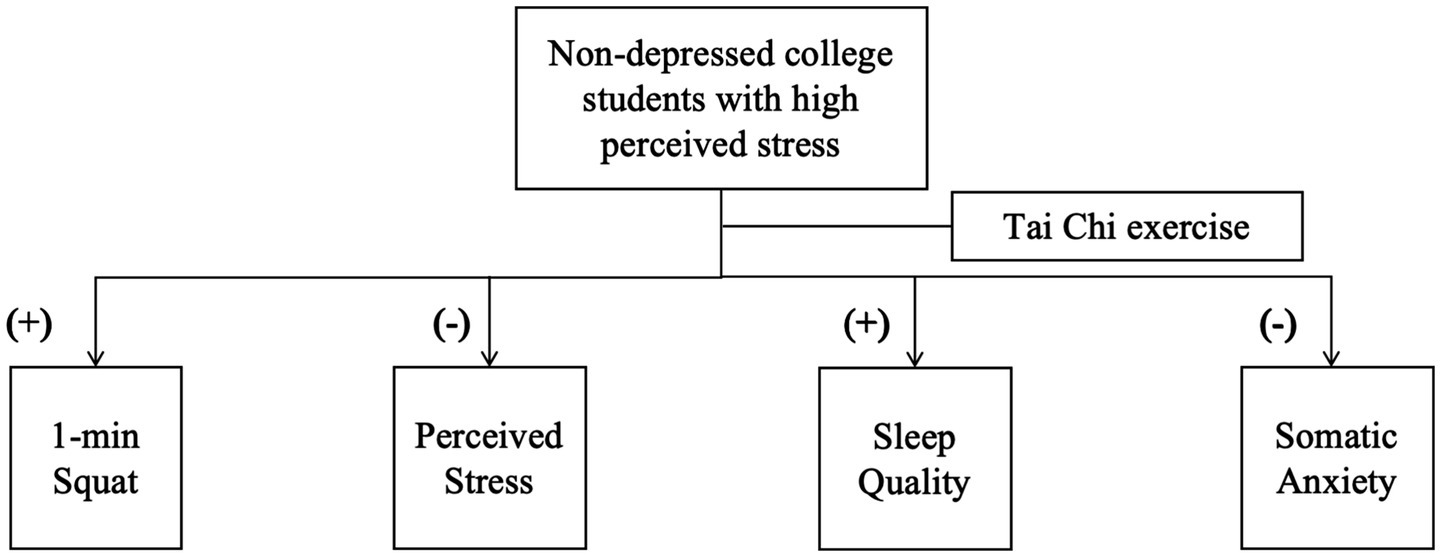
This study demonstrates that a 16-week Tai Chi intervention led to significant and concurrent improvements across multiple health domains in non-depressed college students with high perceived stress—a preclinical subgroup at elevated risk for stress-related morbidity. As illustrated in Figure 2, participants in the Tai Chi group showed enhanced lower-limb muscular endurance (reflected by 1-min squat performance), reduced perceived stress (PSS), improved sleep quality (indicated by lower PSQI total scores), and decreased somatic anxiety (HAMA-Somatic subscale). These findings provide evidence supporting the utility of Tai Chi as an integrated intervention that concurrently enhances health-related physical fitness and alleviates key stress-related symptoms in this younger, non-clinical yet high-risk population, which has been underrepresented in previous research focusing primarily on older or clinical cohorts.
To interpret these findings, a multidimensional framework encompassing biomechanical, neurophysiological, and psychosocial pathways can be proposed. While the present design does not allow for causal inference, the interrelationships between these pathways offer a plausible, theoretical model for understanding Tai Chi’s potential effects. First, on a biomechanical level, the significant improvement in lower-limb muscular endurance is consistent with the demands of Tai Chi’s characteristic sustained, knee-flexed postures, which engage the quadriceps and related muscle groups (59). We speculate that this physical adaptation may be particularly beneficial for college students, as it could help counteract the physical fatigue and musculoskeletal discomfort that often accompanies chronic academic stress (60, 61). It is plausible that alleviating such somatic strain may, in turn, contribute to the observed reductions in global perceived stress and somatic anxiety, potentially by modulating the physical manifestations of stress.
Second, the observed reductions in perceived stress and somatic anxiety may be understood through neurophysiological perspectives. The integration of mindful movement, breath regulation, and meditative focus in Tai Chi is theorized to promote autonomic nervous system regulation, potentially favoring parasympathetic dominance (17, 62). Such a shift could be associated with the stabilization of physiological stress responses, offering a possible explanation for the parallel improvements in sleep quality (63). The fact that significant improvement was specific to somatic anxiety, rather than emotional anxiety (HAMA), might suggest that the intervention’s initial effects are more pronounced on the physiological and somatic level, possibly through enhancing body awareness and regulation, before significantly influencing core affective dimensions (64, 65).
Third, the enhancements in social functioning, and fewer physical health-related role limitations point to potentially important psychosocial processes. The group-based delivery of the intervention inherently created a context for social support and interaction, which may have been particularly beneficial for high-stress individuals who might otherwise experience social withdrawal (66). Furthermore, the process of mastering movement sequences and perceiving physical improvements may foster a strengthened sense of self-efficacy and perceived control—a process that could be termed “mind–body fortification” (66, 67). This enhanced self-efficacy might empower students to engage more fully in daily activities, thereby improving physical health-related role limitations and social functioning. The reduction in both physical and mental fatigue (FS-14) could be understood as a downstream effect of this process, where increased bodily stamina and the practice-induced relaxation may collectively alleviate exhaustion and its cognitive burden (68, 69).
Collectively, these findings position Tai Chi as a holistic intervention with relevance for the embodied experience of stress in a high-risk, preclinical student population. The co-occurrence of benefits across diverse domains suggests potentially synergistic effects. For instance, gains in physical endurance may support reductions in fatigue and somatic anxiety, which could then facilitate lower stress perception and greater social participation, thereby collectively building resilience. This profile highlights the innovative preventive value of Tai Chi as a campus-based strategy, specifically aimed at mitigating risk factors and promoting protective factors in a group that remains underrepresented in exercise intervention research, thereby potentially altering the trajectory toward more severe stress-related morbidity (62, 70, 71). Future research should prioritize longer-term trials to assess the sustainability of benefits and their impact on affective anxiety. Crucially, mechanistic studies incorporating physiological biomarkers and psychological mediators are needed to empirically validate the theoretical pathways proposed in this framework.
5 Limitation
Although this study provides valuable insights into the effects of Tai Chi training among non-depressed college students with high perceived stress, several limitations warrant acknowledgment. First, we recognize the multidimensional nature of stress assessment—while the PSS remains the gold standard for measuring perceived stress, future research would benefit from complementing PSS scores with physiological biomarkers (e.g., cortisol assays) or autonomic nervous system markers (e.g., heart rate variability) to achieve more comprehensive stress characterization, as noted in our revised discussion. Second, the single-intervention timepoint design limits our understanding of temporal effects; subsequent studies should incorporate multiple intervention timepoints to examine dose–response relationships. Future dose- and frequency-matched trials with active exercise comparators (e.g., brisk walking, flexibility training, or non-mindful calisthenics) are warranted to further distinguish Tai Chi–specific effects from general effects of physical activity. Third, the homogeneous sample of Chinese college students constrains generalizability, highlighting the need for cross-cultural validation across diverse ethnicities, regions, and populations (including non-depressed individuals with high stress from varying socioeconomic backgrounds). Finally, the underlying mechanisms through which Tai Chi improves psychological outcomes in this population remain unclear, necessitating multidisciplinary investigations integrating neurobiological, physiological, and psychological measures to elucidate the pathways of action.
6 Conclusion
This study investigated the effects of Tai Chi exercise on non-depressed college students experiencing high perceived stress—a preclinical population at elevated risk for psychological deterioration. The 16-week Tai Chi intervention resulted in significant improvements compared to the control group across multiple domains, including lower-limb muscular endurance (as assessed by the deep-squat test), perceived stress levels, sleep quality, somatic anxiety, and the role limitations due to physical health and social functioning domains of the SF-36 questionnaire. These findings provide robust evidence that Tai Chi is an effective, feasible campus-based intervention for enhancing both mental and health-related physical fitness in this high-risk student subgroup. By mitigating key stress-related impairments and fostering resilience, Tai Chi holds significant promise as a valuable public health strategy for preventing the progression toward stress-related morbidity, including depression, within college populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Tongji University (2021tjdx024). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JS: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. KY: Methodology, Software, Writing - original draft, Writing - review & editing. RZ: Investigation, Writing - original draft. HL: Formal analysis, Writing - original draft. MZ: Validation, Writing - review & editing. HY: Visualization, Writing - review & editing. AC: Project administration, Writing - original draft, Writing - review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Creed, PA, French, J, and Hood, M. Working while studying at university: the relationship between work benefits and demands and engagement and well-being. J Vocat Behav. (2015) 86:48–57. doi: 10.1016/j.jvb.2014.11.002
2. Cheng, H. Research on the current situation and strategies of college students' psychological crisis work. Appl Educ Psychol. (2023) 4:57–62. doi: 10.23977/appep.2023.040709
3. Tan, GX, Soh, XC, Hartanto, A, Goh, AY, and Majeed, NM. Prevalence of anxiety in college and university students: an umbrella review. J Affect Disord Rep. (2023) 14:100658. doi: 10.1016/j.jadr.2023.100658
4. Oliveira Carvalho, P, Hülsdünker, T, and Carson, F. The impact of the COVID-19 lockdown on European students’ negative emotional symptoms: a systematic review and meta-analysis. Behav Sci. (2021) 12:3. doi: 10.3390/bs12010003
5. Alemany-Arrebola, I, Rojas-Ruiz, G, Granda-Vera, J, and Mingorance-Estrada, ÁC. Influence of COVID-19 on the perception of academic self-efficacy, state anxiety, and trait anxiety in college students. Front Psychol. (2020) 11:570017. doi: 10.3389/fpsyg.2020.570017
6. Wang, X, Hegde, S, Son, C, Keller, B, Smith, A, and Sasangohar, F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2020) 22:e22817. doi: 10.2196/22817
7. Wang, X, and Liu, Q. Prevalence of anxiety symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Heliyon. (2022) 8:e10117. doi: 10.1016/j.heliyon.2022.e10117
8. Waterhouse, P, and Samra, R. University students’ coping strategies to manage stress: a scoping review. Educ Rev. (2024) 12:1–41. doi: 10.1080/00131911.2024.2438888
9. Deng, Y, Cherian, J, Khan, NUN, Kumari, K, Sial, MS, Comite, U, et al. Family and academic stress and their impact on students' depression level and academic performance. Front Psych. (2022) 13:869337. doi: 10.3389/fpsyt.2022.869337
10. Zhang, J, Peng, C, and Chen, C. Mental health and academic performance of college students: knowledge in the field of mental health, self-control, and learning in college. Acta Psychol. (2024) 248:104351. doi: 10.1016/j.actpsy.2024.104351
11. Liu, Y, Chen, J, Chen, K, Liu, J, and Wang, W. The associations between academic stress and depression among college students: a moderated chain mediation model of negative affect, sleep quality, and social support. Acta Psychol. (2023) 239:104014. doi: 10.1016/j.actpsy.2023.104014
12. Pascoe, MC, Hetrick, SE, and Parker, AG. The impact of stress on students in secondary school and higher education. Int J Adolesc Youth. (2020) 25:104–12. doi: 10.1080/02673843.2019.1596823
13. Barbayannis, G, Bandari, M, Zheng, X, Baquerizo, H, Pecor, KW, and Ming, X. Academic stress and mental well-being in college students: correlations, affected groups, and COVID-19. Front Psychol. (2022) 13:886344. doi: 10.3389/fpsyg.2022.886344
14. Lee, YY, Stockings, EA, Harris, MG, Doi, SAR, Page, IS, Davidson, SK, et al. The risk of developing major depression among individuals with subthreshold depression: a systematic review and meta-analysis of longitudinal cohort studies. Psychol Med. (2019) 49:92–102. doi: 10.1017/S0033291718000557
15. Huang, X, Wang, Y, and Zhang, H. Effects of physical exercise intervention on depressive and anxious moods of college students: a meta-analysis of randomized controlled trials. Asian J Sport Exerc Psychol. (2023) 3:206–21. doi: 10.1016/j.ajsep.2023.01.001
16. Lin, J, Gao, YF, Guo, Y, Li, M, Zhu, Y, You, R, et al. Effects of qigong exercise on the physical and mental health of college students: a systematic review and meta-analysis. BMC Complement Med Ther. (2022) 22:287. doi: 10.1186/s12906-022-03760-5
17. Kraft, J, Waibl, PJ, and Meissner, K. Stress reduction through taiji: a systematic review and meta-analysis. BMC Complement Med Ther. (2024) 24:210. doi: 10.1186/s12906-024-04493-3
18. Kuang, X, Dong, Y, Song, L, Dong, L, Chao, G, Zhang, X, et al. The effects of different types of Tai Chi exercise on anxiety and depression in older adults: a systematic review and network meta-analysis. Front Public Health. (2023) 11:1295342. doi: 10.3389/fpubh.2023.1295342
19. Nan, L, Grunberg, D, De Silva, S, and Sivaramakrishnan, D. Evaluating the effectiveness of Tai Chi in short-term, medium-term, and long-term on balance and strength among the elderly: a systematic review and meta-analysis. Arch Gerontol Geriatr Plus. (2024) 1:100080. doi: 10.1016/j.aggp.2024.100080
20. Li, X, Chang, P, Wu, M, Jiang, Y, Gao, Y, Chen, H, et al. Effect of Tai Chi vs aerobic exercise on blood pressure in patients with prehypertension: a randomized clinical trial. JAMA Netw Open. (2024) 7:e2354937. doi: 10.1001/jamanetworkopen.2023.54937
21. Yang, GY, Hunter, J, Bu, FL, Hao, WL, Zhang, H, Wayne, PM, et al. Determining the safety and effectiveness of Tai Chi: a critical overview of 210 systematic reviews of controlled clinical trials. Syst Rev. (2022) 11:260. doi: 10.1186/s13643-022-02100-5
22. Solloway, MR, Taylor, SL, Shekelle, PG, Miake-Lye, IM, Beroes, JM, Shanman, RM, et al. An evidence map of the effect of Tai Chi on health outcomes. Syst Rev. (2016) 5:126. doi: 10.1186/s13643-016-0300-y
23. Song, J, Liu, Z-z, Huang, J, Wu, J-s, and Tao, J. Effects of aerobic exercise, traditional Chinese exercises, and meditation on depressive symptoms of college student: a meta-analysis of randomized controlled trials. Medicine (Baltimore). (2021) 100:e23819. doi: 10.1097/MD.0000000000023819
24. Chen, S, Luo, L, and Yuan, Y. Optimal Tai Chi dose for improving anxiety, depression, and sleep quality in older adults: a Bayesian meta-analysis. Clin Rehabil. (2025) 39:1170–80. doi: 10.1177/02692155251355083
25. Kucukosmanoglu, HS, Cramer, H, Tavakoly, R, Moosburner, A, and Bilc, MI. Mind-body medicine in the treatment of depression: a narrative review of efficacy, safety and mechanisms. Curr Psychiatry Rep. (2024) 26:729–40. doi: 10.1007/s11920-024-01548-7
26. Wu, J, Song, J, He, Y, Li, Z, Deng, H, Huang, Z, et al. Effect of Tai Chi on young adults with subthreshold depression via a stress-reward complex: a randomized controlled trial. Sports Med Open. (2023) 9:90. doi: 10.1186/s40798-023-00637-w
27. Qu, P, Zhu, X, Zhou, H, Kang, Z, Li, R, Wen, J, et al. The effects of mindfulness enhanced Tai Chi Chuan training on mental and physical health among beginners: a randomized controlled trial. Front Psychol. (2024) 15:1381009. doi: 10.3389/fpsyg.2024.1381009
28. Guo, S, Sun, W, Liu, C, and Wu, S. Structural validity of the Pittsburgh sleep quality index in Chinese undergraduate students. Front Psychol. (2016) 7:1126. doi: 10.3389/fpsyg.2016.01126
29. Lei, L, Chang, S, and Cheng, L. At least 150 min per week of Tai Chi practice improves sleep quality in the older people: evidence from a meta-analysis. Eur Geriatr Med. (2025) 16:293–303. doi: 10.1007/s41999-024-01125-4
30. Lee, EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. (2012) 6:121–7. doi: 10.1016/j.anr.2012.08.004
31. Moon, SM, Lim, JH, Hong, YS, Shin, KC, Lee, CY, Kim, DJ, et al. Clinical impact of forced vital capacity on exercise performance in patients with chronic obstructive pulmonary disease. J Thorac Dis. (2021) 13:837–46. doi: 10.21037/jtd-20-1098a
32. Vaishya, R, Misra, A, Vaish, A, Ursino, N, and D'Ambrosi, R. Hand grip strength as a proposed new vital sign of health: a narrative review of evidences. J Health Popul Nutr. (2024) 43:7. doi: 10.1186/s41043-024-00500-y
33. Ojeda, ÁH, Maliqueo, SG, and Barahona-Fuentes, G. Validity and reliability of the muscular fitness test to evaluate body strength-resistance. Apunts Med Esport. (2020) 55:128–36. doi: 10.1016/j.apunsm.2020.08.002
34. Novaes, M, Carvalho, A, Sauer, JF, Brech, GC, Helito, CP, and João, SMA. Postural control during single leg stance in individuals with clinical indication for combined reconstruction of the anterior cruciate and the anterolateral ligaments of the knee: a cross-sectional study. BMC Musculoskelet Disord. (2022) 23:383. doi: 10.1186/s12891-022-05347-0
35. Kupst, MJ, Butt, Z, Stoney, CM, Griffith, JW, Salsman, JM, Folkman, S, et al. Assessment of stress and self-efficacy for the NIH toolbox for neurological and behavioral function. Anxiety Stress Coping. (2015) 28:531–44. doi: 10.1080/10615806.2014.994204
36. Dunstan, DA, and Scott, N. Clarification of the cut-off score for Zung's self-rating depression scale. BMC Psychiatry. (2019) 19:177. doi: 10.1186/s12888-019-2161-0
37. Buysse, DJ, Reynolds, CF 3rd, Monk, TH, Berman, SR, and Kupfer, DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213.
38. Maier, W, Buller, R, Philipp, M, and Heuser, I. The Hamilton anxiety scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. (1988) 14:61–8. doi: 10.1016/0165-0327(88)90072-9
39. Jing, MJ, Lin, WQ, Wang, Q, Wang, JJ, Tang, J, Jiang, ES, et al. Reliability and construct validity of two versions of Chalder fatigue scale among the general population in mainland China. Int J Environ Res Public Health. (2016) 13:147. doi: 10.3390/ijerph13010147
40. Velanovich, V. Behavior and analysis of 36-item short-form health survey data for surgical quality-of-life research. Arch Surg. (2007) 142:473–7. doi: 10.1001/archsurg.142.5.473
41. Black, DS, O'Reilly, GA, Olmstead, R, Breen, EC, and Irwin, MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Intern Med. (2015) 175:494–501. doi: 10.1001/jamainternmed.2014.8081
42. Pande, AC, Crockatt, JG, Feltner, DE, Janney, CA, Smith, WT, Weisler, R, et al. Pregabalin in generalized anxiety disorder: a placebo-controlled trial. Am J Psychiatry. (2003) 160:533–40. doi: 10.1176/appi.ajp.160.3.533
43. Zhao, Y, Liang, Q, Jiang, Z, Mei, H, Zeng, N, Su, S, et al. Brain abnormalities in survivors of COVID-19 after 2-year recovery: a functional MRI study. Lancet Reg Health West Pac. (2024) 47:101086. doi: 10.1016/j.lanwpc.2024.101086
44. Yan, S, Jiang, H, Yang, Z, Tang, X, Chen, Z, Chen, Z, et al. Physical activity trajectory during pregnancy and associations with maternal fatigue using a growth mixture modeling approach. Sci Rep. (2024) 14:1020. doi: 10.1038/s41598-024-51648-w
45. Eisenman, DP, Gelberg, L, Liu, H, and Shapiro, MF. Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA. (2003) 290:627–34. doi: 10.1001/jama.290.5.627
46. Ali, S, Tauqir, S, Farooqi, FA, Al-Jandan, B, Al-Janobi, H, Alshehry, S, et al. Psychological impact of the COVID-19 pandemic on students, assistants, and Faculty of a Dental Institute of Saudi Arabia. Int J Environ Res Public Health. (2021) 18:3366. doi: 10.3390/ijerph182413366
47. Ho, KY, Lam, KKW, Xia, W, Chung, JOK, Cheung, AT, Ho, LLK, et al. Psychometric properties of the Chinese version of the Pittsburgh sleep quality index (PSQI) among Hong Kong Chinese childhood cancer survivors. Health Qual Life Outcomes. (2021) 19:176. doi: 10.1186/s12955-021-01803-y
48. Yan, DQ, Huang, YX, Chen, X, Wang, M, Li, J, and Luo, D. Application of the Chinese version of the Pittsburgh sleep quality index in people living with HIV: preliminary reliability and validity. Front Psych. (2021) 12:676022. doi: 10.3389/fpsyt.2021.676022
49. Thompson, E. Hamilton rating scale for anxiety (HAM-A). Occup Med (Lond). (2015) 65:601. doi: 10.1093/occmed/kqv054
50. Zimmerman, M, Martin, J, Clark, H, McGonigal, P, Harris, L, and Holst, CG. Measuring anxiety in depressed patients: a comparison of the Hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. (2017) 93:59–63. doi: 10.1016/j.jpsychires.2017.05.014
51. Ho, KY, Li, WH, Lam, KW, Chui, SY, and Chan, CF. Psychometric properties of the Chinese version of the fatigue scale-adolescent. BMC Cancer. (2015) 15:938. doi: 10.1186/s12885-015-1945-y
52. Dyer, K, Hooke, G, and Page, AC. Development and psychometrics of the five item daily index in a psychiatric sample. J Affect Disord. (2014) 152-154:409–15. doi: 10.1016/j.jad.2013.10.003
53. Brody, T. Chapter 23 - health-related quality-of-life tools—immune disorders In: T Brody, editor. Clinical trials. Boston: Academic Press (2016). 469–77.
54. Li, L, Wang, HM, and Shen, Y. Chinese SF-36 health survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health. (2003) 57:259–63. doi: 10.1136/jech.57.4.259
55. Yılmaz Koğar, E, and Koğar, H. A systematic review and meta-analytic confirmatory factor analysis of the perceived stress scale (PSS-10 and PSS-14). Stress Health. (2024) 40:e3285. doi: 10.1002/smi.3285
56. She, Z, Li, D, Zhang, W, Zhou, N, Xi, J, and Ju, K. Three versions of the perceived stress scale: psychometric evaluation in a nationally representative sample of Chinese adults during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:8312. doi: 10.3390/ijerph18168312
57. Tsai, PS, Wang, SY, Wang, MY, Su, CT, Yang, TT, Huang, CJ, et al. Psychometric evaluation of the Chinese version of the Pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res. (2005) 14:1943–52. doi: 10.1007/s11136-005-4346-x
58. Leung, KK, Lue, BH, Lee, MB, and Tang, LY. Screening of depression in patients with chronic medical diseases in a primary care setting. Fam Pract. (1998) 15:67–75. doi: 10.1093/fampra/15.1.67
59. Wang, F, Lee, E-KO, Wu, T, Benson, H, Fricchione, G, Wang, W, et al. The effects of Tai Chi on depression, anxiety, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med. (2014) 21:605–17. doi: 10.1007/s12529-013-9351-9
60. Wang, L, Zhai, Y, and Sun, Q. Enhancing career adaptability in college students: a Tai Chi-based sports intervention study. Front Psychol. (2024) 15:1455877. doi: 10.3389/fpsyg.2024.1455877
61. Leuzzi, G, Giardulli, B, Pierantozzi, E, Recenti, F, Brugnolo, A, and Testa, M. Personality traits and levels of anxiety and depression among martial artists: a cross-sectional study. BMC psychology. (2024) 12:607. doi: 10.1186/s40359-024-02096-8
62. Wei, GX, Li, YF, Yue, XL, Ma, X, Chang, YK, Yi, LY, et al. Tai Chi Chuan modulates heart rate variability during abdominal breathing in elderly adults. PsyCh J. (2016) 5:69–77. doi: 10.1002/pchj.105
63. Oh, B, Bae, K, Lamoury, G, Eade, T, Boyle, F, Corless, B, et al. The effects of Tai Chi and qigong on immune responses: a systematic review and meta-analysis. Medicine. (2020) 7:39. doi: 10.3390/medicines7070039
64. Yin, J, Yue, C, Song, Z, Sun, X, and Wen, X. The comparative effects of Tai Chi versus non-mindful exercise on measures of anxiety, depression and general mental health: a systematic review and meta-analysis. J Affect Disord. (2023) 337:202–14. doi: 10.1016/j.jad.2023.05.037
65. Qi, F, Soh, KG, Nasiruddin, NJM, Leong, OS, He, S, and Liu, H. Effect of Taichi chuan on health-related physical fitness in adults: a systematic review with meta-analysis. Complement Ther Med. (2023) 77:102971. doi: 10.1016/j.ctim.2023.102971
66. Sani, NA, Yusoff, SSM, Norhayati, MN, and Zainudin, AM. Tai Chi exercise for mental and physical well-being in patients with depressive symptoms: a systematic review and meta-analysis. Int J Environ Res Public Health. (2023) 20:2828. doi: 10.3390/ijerph20042828
67. Chen, M-Y, Bai, W, Zhang, L, Sha, S, Su, Z, Cheung, T, et al. Associations of Tai Chi with depression and anxiety among older adults: Nationwide study findings from a network perspective. J Geriatr Psychiatry Neurol. (2025) 38:241–53. doi: 10.1177/08919887241313248
68. Cui, H, Wang, Q, Pedersen, M, Wang, Q, Lv, S, James, D, et al. The safety of Tai Chi: a meta-analysis of adverse events in randomized controlled trials. Contemp Clin Trials. (2019) 82:85–92. doi: 10.1016/j.cct.2019.06.004
69. Marcora, SM, Staiano, W, and Manning, V. Mental fatigue impairs physical performance in humans. J Appl Physiol. (2009) 106:857–64. doi: 10.1152/japplphysiol.91324.2008
70. Choo, YT, Jiang, Y, Hong, J, and Wang, W. Effectiveness of Tai Chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. (2020) 111:103737. doi: 10.1016/j.ijnurstu.2020.103737
Keywords: Tai Chi exercise, high perceived stress, non-depressed, mental and physical outcomes, college students
Citation: Sun J, Yao K, Zhao R, Li H and Cicchella A (2025) Tai Chi as a preventive intervention for improving mental and physical health in non-depressed college students with high perceived stress. Front. Public Health. 13:1613384. doi: 10.3389/fpubh.2025.1613384
Edited by:
Jason H. Huang, Baylor Scott and White Health, United StatesReviewed by:
Yuke Teng, Chengdu University of Traditional Chinese Medicine, ChinaYi Wang, Weinan Normal University, China
Copyright © 2025 Sun, Yao, Zhao, Li and Cicchella. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonio Cicchella, YW50b25pby5jaWNjaGVsbGFAdW5pYm8uaXQ=
 Jingyu Sun
Jingyu Sun Ke Yao1
Ke Yao1 Rongji Zhao
Rongji Zhao Antonio Cicchella
Antonio Cicchella