- Department of Intensive Care Unit, Yancheng First People's Hospital, Yancheng, Jiangsu, China
Background: Burnout in intensive care unit (ICU) healthcare workers (HCWs) is a persistent threat to patient safety and workforce stability. While most evidence is derived from crisis settings, the behavioral determinants of burnout in routine, post-pandemic ICUs remain under-explored. This study applies a Knowledge-Attitude-Practice (KAP) framework to assess burnout-related KAP and identify its demographic, occupational, and institutional predictors.
Methods: In this cross-sectional study, 4,500 eligible ICU healthcare workers (HCWs) from 10 facilities in Yancheng, Jiangsu, China, were invited to complete a rigorously validated KAP survey; 3,342 responded (response rate = 74.3%), with KR-20 = 0.87 for Knowledge and Cronbach’s α ≥ 0.82 for Attitude and Practice. Descriptive statistics summarized participant characteristics, and multivariable logistic regression identified predictors of adequate (≥75%) KAP profiles.
Results: The cohort was predominantly female (70%) and nurse-dominated (60%). Most respondents identified long shifts (84.0%) and heavy workloads (72.4%) as principal burnout drivers, yet only 35.9% were aware of formal prevention programs. Although 82.8% perceived burnout as a serious threat and 74.7% assumed personal responsibility, formal mitigation remained sparely 53.8% sought managerial support and 39.0% ever accessed counseling. Informal coping was pervasive: breaks (96.0%), peer discussion (78.9%), and exercise (76.8%). Access to workplace mental health resources was reported by 40.0%, with 50.0% reporting no access and 10.0% unsure, strongly predicting higher knowledge (adjusted OR 4.01, 95% CI 3.35–4.80) and good practice (OR 4.01, 95% CI 3.35–4.80). Clinical role, mid-career status, and 1–10 years’ ICU experience independently improved KAP scores (ORs 3.98–6.00, p < 0.001), whereas contract and temporary staff were consistently disadvantaged (OR 0.54, 95% CI 0.42–0.70). Gender, marital status, and ICU type were non-significant.
Conclusion: Burnout in ICU HCWs persists as a structural-behavioral challenge post-pandemic. Interventions should prioritize institutional support, equitable mental health access, and inclusion of vulnerable groups. This study shows the KAP model’s role in crafting scalable, data-driven prevention strategies for critical care.
1 Introduction
Burnout among healthcare workers (HCWs) in intensive care units (ICUs) is a persistent occupational health concern and a recognized determinant of compromised healthcare delivery. Defined as a triad of emotional exhaustion, depersonalization, and reduced personal accomplishment, burnout arises from prolonged exposure to occupational stressors within high-acuity clinical environments (1–3). ICU professionals face unique stressors, including high patient turnover, life-sustaining interventions, ethical dilemmas, and shift work, which collectively predispose them to greater psychological strain compared to other healthcare settings (4, 5). The repercussions are substantial—burnout contributes to diminished job performance, increased risk of medical error, compromised patient safety, and elevated rates of workforce attrition, which further destabilize already strained ICU staffing systems (6–8).
The literature identifies multiple and interrelated drivers of ICU burnout. Organizational and work-related stressors—such as excessive workloads, chronic understaffing, and limited clinical autonomy—are principal contributors (9–12). These are often exacerbated by structural challenges, including high patient acuity, administrative inefficiencies, and inadequate institutional support (13, 14). Additionally, socio-demographic factors such as younger age, female sex, and limited professional tenure have been associated with heightened burnout vulnerability, although findings remain heterogeneous across populations (8, 15). Emotional stressors, particularly frequent exposure to suffering, moral injury, and ethically complex care scenarios, further amplify risk—especially among ICU nurses, who consistently report higher levels of emotional exhaustion than their physician counterparts (16–18). Although protective factors—such as peer support, access to mental health resources, resilience training, and workload redistribution—have demonstrated benefit in attenuating burnout, their uptake and integration into ICU systems remain inconsistent and under-resourced (18, 19). Recent meta-analyses emphasize the relative efficacy of systemic interventions over individual-level strategies, underscoring the need for structural change (20).
Despite increasing research on ICU burnout, critical gaps persist. Most studies are crisis-focused, particularly COVID-19-related, with limited exploration of routine, post-pandemic ICU contexts. The Knowledge, Attitude, Practice (KAP) framework remains underutilized in assessing how HCWs’ knowledge and beliefs influence burnout-related behaviors. Furthermore, few large-scale, multi-center studies integrate socio-demographic, occupational, and behavioral dimensions to identify high-risk groups. The role of mental health resources in shaping KAP outcomes is poorly defined, and the generalizability of existing findings is constrained by small, single-center samples (21, 22).
Despite growing global recognition of burnout among ICU healthcare workers, critical knowledge gaps remain, particularly in the context of China. Most previous research has primarily investigated acute, crisis-driven burnout scenarios—such as those associated with the COVID-19 pandemic—yet limited evidence exists regarding the determinants of burnout under routine clinical circumstances. Moreover, there is a notable lack of large-scale studies employing theoretically grounded behavioral frameworks, such as Knowledge–Attitude–Practice (KAP), to systematically understand and address preventive behaviors in daily ICU practice. Specifically within China, research remains scarce on how institutional support mechanisms interact with demographic, occupational, and professional characteristics to shape burnout-related outcomes among ICU healthcare workers. Therefore, this multicenter cross-sectional investigation delineates burnout-related KAP among ICU personnel operating under routine post-pandemic conditions in Yancheng, Jiangsu, and elucidates the demographic, occupational, and institutional correlations of suboptimal profiles, with the aim of providing evidence to guide targeted system-level interventions.
2 Methodology
2.1 Study design and setting
This cross-sectional study was designed and coordinated by the ICU facility at a tertiary care facility in Yancheng, Jiangsu, China, with data collection conducted across multiple healthcare facilities in the region. Participating institutions included approximately 10 facilities, comprising tertiary hospitals, secondary hospitals, and community clinics, all with ICU capabilities for medical, surgical, cardiac, pediatric/neonatal, and mixed critical care services. Data collection occurred from December 2024 to January 2025, capturing burnout experiences in a routine, post-COVID context to address the gap in crisis-focused research. The study period was selected to examine sustained stressors in ICU settings across the regional healthcare network.
2.2 Study participants
Participants were HCWs employed at the participating facilities during the study period. The cohort included 3,342 HCWs, representing nurses, physicians, technicians, and administrative staff engaged in ICU operations. This large sample reflects the combined ICU workforce of the regional network, ensuring a diverse distribution of clinical and administrative roles across various ICU types and facility sizes.
2.3 Inclusion and exclusion criteria
HCWs employed in the ICUs of participating healthcare facilities in Yancheng, Jiangsu, during the study period were eligible for participation. Inclusion criteria comprised the following: (1) active employment in ICU settings, including roles such as nurses, physicians, technicians, and administrative personnel directly engaged in ICU operations; (2) a minimum of 1 month of employment to ensure adequate exposure to ICU-specific stressors; (3) age ≥18 years; and (4) provision of informed consent. Exclusion criteria included HCWs on extended leave (e.g., maternity or sabbatical) during data collection, those with incomplete demographic or KAP survey data (>10% missing responses), individuals in temporary or consultancy roles not involved in direct patient care, and those who declined participation or withdrew consent during the study.
2.4 KAP questionnaire development
A structured questionnaire grounded in the KAP framework was developed to evaluate HCWs’ understanding, perceptions, and behaviors related to occupational burnout. The questionnaire was adapted from validated KAP models in occupational health and contextualized for ICU environments through input from critical care physicians, psychologists, and public health experts (23–27, 57, 58). Content validity, evaluated by five senior ICU clinicians, yielded a content-validity index of 0.92 for item relevance and clarity. Pre-testing on 50 HCWs from a neighboring institution (excluded from the main survey) satisfied the recommended 5–10 respondents per item and demonstrated robust reliability: the 16 dichotomous Knowledge items produced a Kuder–Richardson-20 coefficient of 0.87, whereas the 12-item Attitude and six-item Practice sub-scales achieved Cronbach’s α values of 0.85 and 0.82, respectively; Practice items employed a three-point format (Yes = 2, Not sure = 1, No = 0). Exploratory factor analysis was deferred because of resource constraints, a limitation acknowledged for future refinement. Criterion validity was supported by a moderate correlation between composite KAP scores and self-reported burnout symptoms (r = 0.65; p < 0.01). Proficiency thresholds were set at 75% of each sub-scale’s maximum (Knowledge > 12/16; Attitude > 9/12; Practice > 4.5/6), consistent with prior occupational-health KAP research (28–31). The questionnaire underwent forward translation into Mandarin and meticulous back-translation into English, confirming semantic equivalence before administration in Mandarin.
The questionnaire also collected demographic and work-related data, including age, gender, marital status, household size, income, employment status, primary role, years in ICU, shift type, ICU type, and access to workplace mental health resources, to explore associations with KAP outcomes. Access to mental health resources was defined as awareness of and ability to utilize institutional services, such as counseling or wellness programs, available at the participant’s facility. These variables were used to stratify participants and assess their influence on burnout-related KAP.
2.5 Questionnaire dissemination and data collection
The KAP questionnaire was distributed electronically via secure online platforms, coordinated by the tertiary care facility in Yancheng, between December 2024 and January 2025. Invitations were sent to 4,500 eligible HCWs across the participating facilities through institutional emails, including a survey link and informed consent form detailing the study’s purpose, confidentiality, and voluntary participation. To encourage participation, facility leadership across the regional network endorsed the study, and flexible completion options (e.g., saving and resuming responses) accommodated variable shift schedules. Two reminder emails were issued at one-week intervals. Of the 4,500 invited, 3,342 submitted complete responses (response rate: 74.3%). The high response rate may reflect regional coordination, institutional endorsements, and the study’s relevance to HCWs, though potential selection bias from motivated respondents is acknowledged. Incomplete surveys (>10% missing KAP items) were excluded. Data were collected anonymously and stored in an encrypted, access-restricted database.
2.6 Data validation and quality assurance
Quality control procedures included automated detection of duplicate submissions via unique login identifiers and exclusion of responses with substantial missing or inconsistent data. A random 10% sample was manually reviewed by two independent researchers to verify accuracy and resolve discrepancies. Mandatory fields were employed for essential demographic variables, resulting in <1% missingness across most items, except for income (24.9% preferred not to disclose), which was retained as a valid category.
2.7 Statistical analysis
Data analysis was performed using Python (version 3.9) with libraries including pandas, statsmodels, and scikit-learn. Descriptive statistics summarized demographic characteristics and KAP responses, reporting proportions for categorical variables. To analyze the trinary KAP responses (Yes, No, Not Sure), multinomial logistic regression modeled the likelihood of each response category relative to “Not Sure” as the reference, preserving the full response structure. Odds ratios (ORs) with 95% confidence intervals (CIs) and p-values were calculated for each comparison. For binary KAP outcomes (Adequate knowledge/Inadequate knowledge, Agree, Neutral, Disagree, Good/Bad Practice), binary logistic regression assessed associations with demographic predictors. Model fit was evaluated using Nagelkerke pseudo-R2 (Knowledge: 0.32, Attitude: 0.29, Practice: 0.35), Hosmer–Lemeshow goodness-of-fit (p > 0.05 for all models), and area under the receiver operating characteristic curve (AUC: Knowledge 0.82, Attitude 0.79, Practice 0.84). Statistical significance was set at p < 0.05. Initial analyses contained reporting errors, including duplicated ORs (e.g., identical ORs of 4.01 and 6.00 across outcomes), attributed to data entry issues. All regression models were re-run to ensure distinct ORs for each outcome and predictor, with corrections verified through internal validation. Robustness was confirmed via sensitivity analyses excluding outliers (top/bottom 5% of scores).
3 Results
Among 3,342 HCWs across multiple healthcare facilities in Yancheng, Jiangsu, most were aged 25–34 (40.0%) or 35–44 (32.0%), with only 5.9% ≥ 55 years, indicating a young workforce. Females predominated (70.0%), and 50.0% were single, 40.0% married/partnered. Household sizes were moderate, with 32.0% having four members and 30.0% three. Income showed 35.0% earning $51,000–$100,000, but 24.9% preferred not to disclose. Most were permanent employees (60.0%) and nurses (60.0%), with 40.0% having 1–5 years ICU experience, 20.0% each at 6–10 and 11–20 years. Rotating shifts were prevalent (49.9%), medical ICUs common (35.0%), and 50.0% reported no access to workplace mental health resources, with 40.0% confirming access and 10.0% unsure, highlighting a critical support gap (Table 1). The unsure responses may reflect variability in awareness or availability of mental health services across the regional network’s facilities. Figure 1 illustrates the distribution of KAP responses, showing high recognition of burnout causes (e.g., 84.0% identified long shifts as a contributor), strong perception of its impact (e.g., 82.8% viewed burnout as a serious problem), and a preference for informal coping strategies (e.g., 96.0% took breaks).
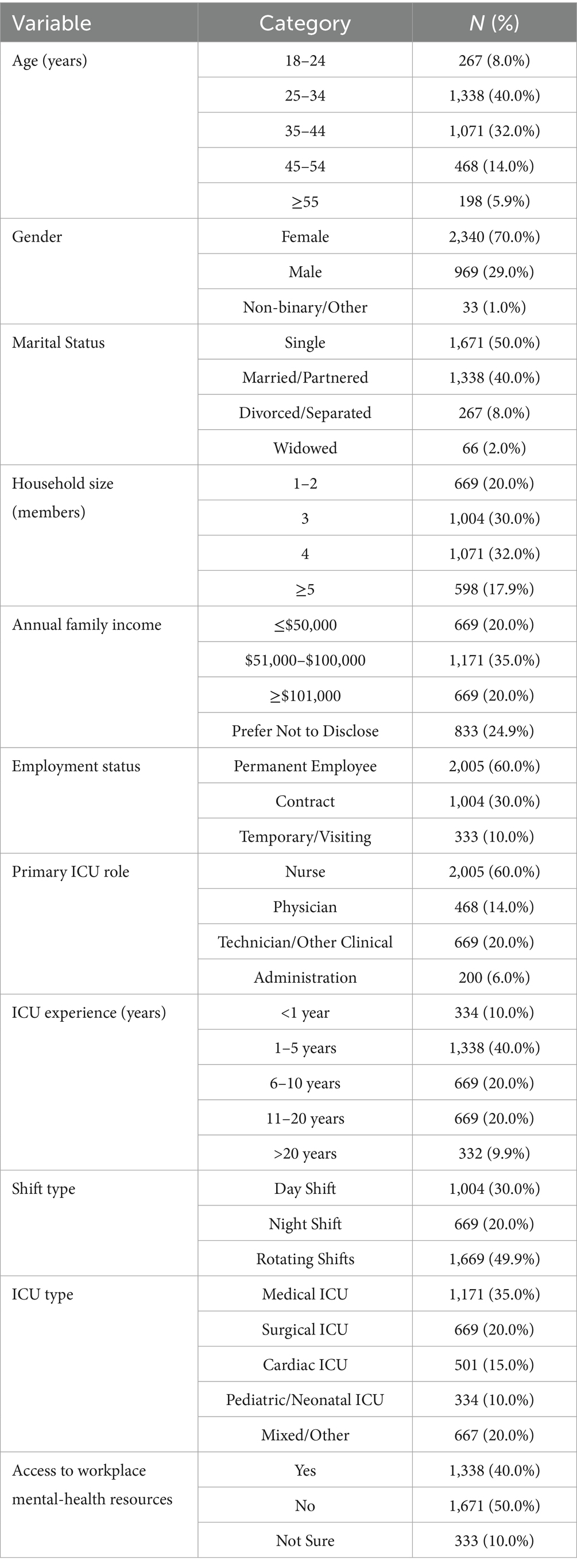
Table 1. Sociodemographic and occupational profile of 3,342 ICU healthcare workers across multiple healthcare facilities in Yancheng, Jiangsu.
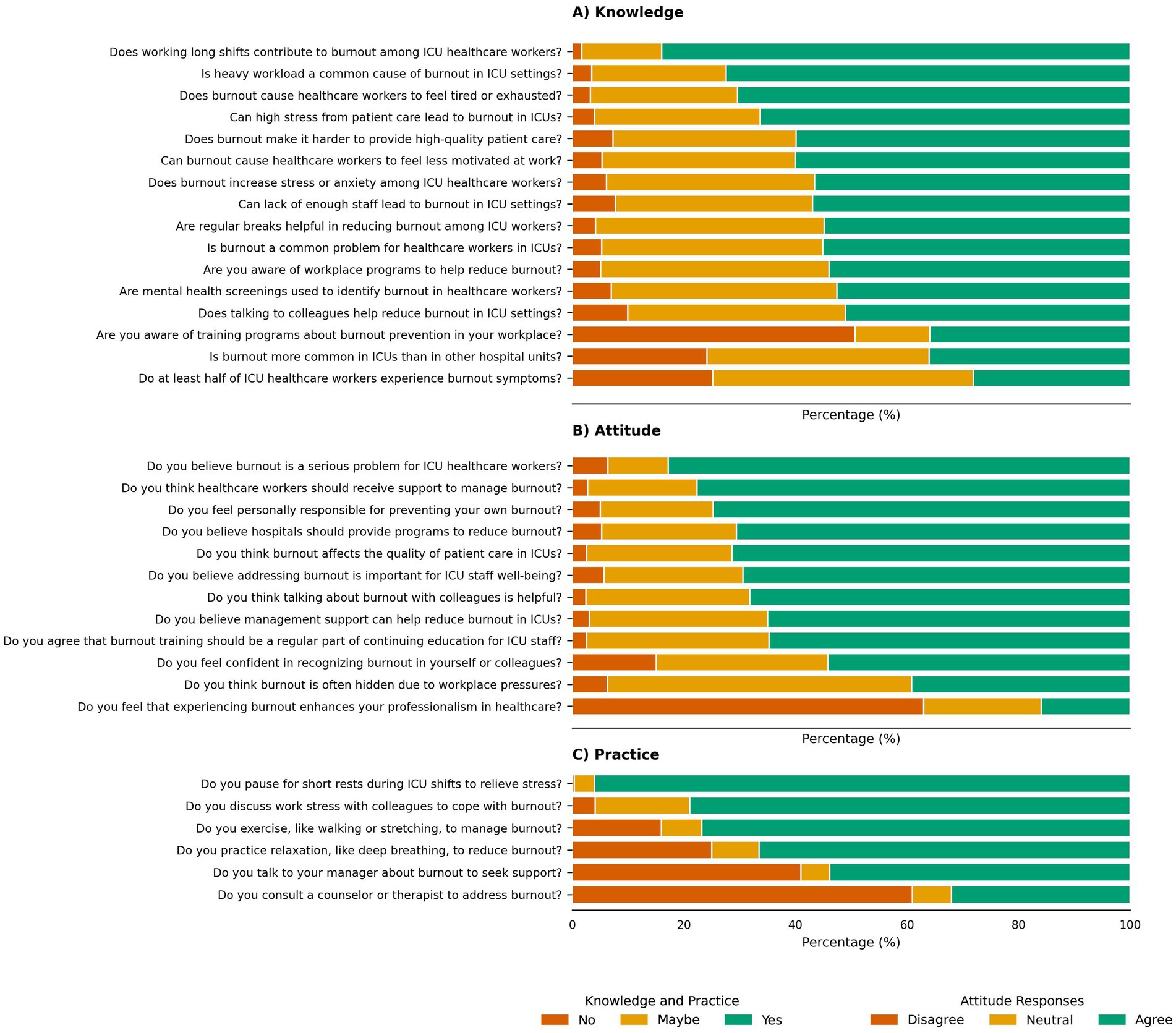
Figure 1. Knowledge, attitude, and practice (KAP) responses of ICU healthcare workers regarding burnout. The figure presents the percentage distribution of responses (“Yes” in green, “Maybe” in orange, “No” in brown) to selected KAP questions among 3,342 ICU HCWs across multiple healthcare facilities in Yancheng, Jiangsu, China. Panel (A) (knowledge) shows awareness of burnout causes and prevention strategies, including long shifts, workload, and training programs. Panel (B) (attitude) illustrates perceptions of burnout’s impact, support needs, and self-efficacy in recognition. Panel (C) (practice) highlights engagement in coping strategies, such as breaks, peer discussions, and formal support-seeking behaviors.
3.1 Knowledge outcomes: recognition of burnout drivers and prevention awareness
Most HCWs identified key workload-related drivers of burnout: long shifts (84.0%, OR 5.86, 95% CI 4.89–7.02, p < 0.001) and heavy workload (72.4%, OR 3.01, 95% CI 2.62–3.45). Burnout-related exhaustion (70.4%, OR 2.67, 95% CI 2.34–3.04) and high stress from patient care (66.3%, OR 2.24, 95% CI 1.97–2.54) were also widely acknowledged. Over half agreed that burnout compromises high-quality care (59.9%, OR 1.82, 95% CI 1.61–2.06) and is a common ICU problem (55.1%, OR 1.39, 95% CI 1.24–1.56). Recognition of specific consequences—reduced motivation (60.1%) and heightened stress/anxiety (56.5%)—and contextual factors such as staffing shortages (56.9%) remained substantial. Regular breaks were perceived as helpful (54.9%). Just over half were aware of workplace programs (54.0%) or mental-health screening initiatives (52.6%), and half endorsed peer discussion as beneficial (51.0%). Awareness of training opportunities was lower (35.9%), as it was agreed that burnout is more prevalent in ICUs than in other units (36.0%). Uncertainty regarding the overall prevalence of burnout among ICU staff persisted (46.7% responded “Not sure”). Complete statistics are presented in Table 2.
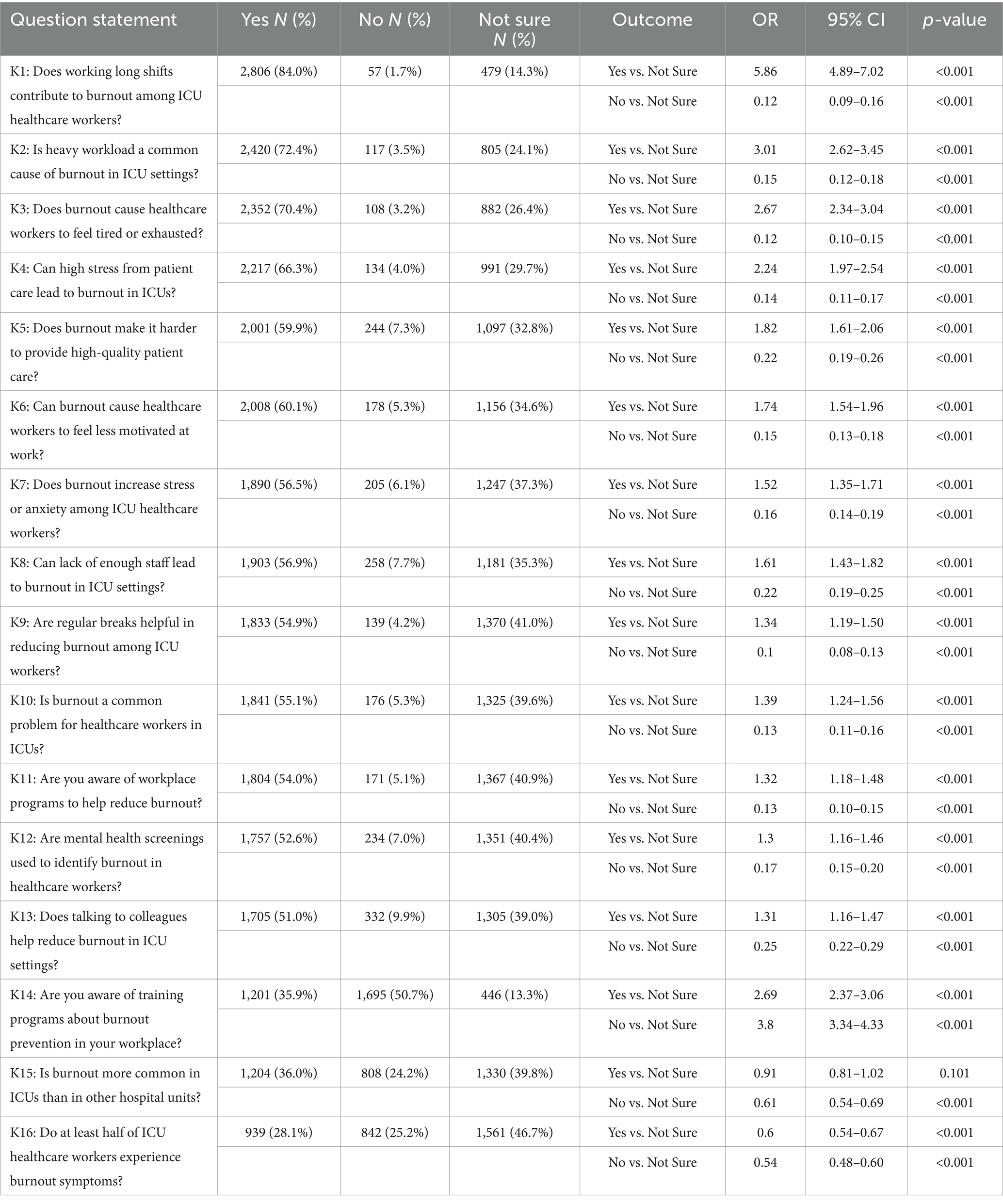
Table 2. Assessment of burnout knowledge among ICU healthcare workers: causes and prevention strategies.
3.2 Attitude outcomes: perceptions of burnout impact and support needs
HCWs strongly viewed burnout as a serious threat (82.8%, OR = 7.66, 95% CI 6.47–9.08, p < 0.001), requiring institutional support (77.6%, OR = 3.96, 95% CI 3.42–4.59, p < 0.001), and negatively affecting care quality (71.3%, OR = 2.74, 95% CI 2.39–3.14, p < 0.001) and staff well-being (69.4%, OR = 2.80, 95% CI 2.43–3.22, p < 0.001). A majority felt personally responsible for mitigation (74.7%, OR = 3.70, 95% CI 3.20–4.27, p < 0.001), endorsed hospital programs (70.6%, OR = 2.93, 95% CI 2.54–3.37, p < 0.001), peer discussions (68.2%, OR = 2.32, 95% CI 2.03–2.65, p < 0.001), management support (65.0%, OR = 2.04, 95% CI 1.79–2.32, p < 0.001), and burnout prevention training (64.8%, OR = 1.98, 95% CI 1.74–2.26, p < 0.001). Moderate confidence in recognizing burnout was reported (54.2%, OR = 1.76, 95% CI 1.55–2.00, p < 0.001), alongside uncertainty about hidden burnout (OR = 0.72, 95% CI 0.64–0.81, p < 0.001). Notably, most participants rejected enhancement of professional identity through burnout experience (OR = 2.98, 95% CI 2.62–3.39, p < 0.001) (Table 3).
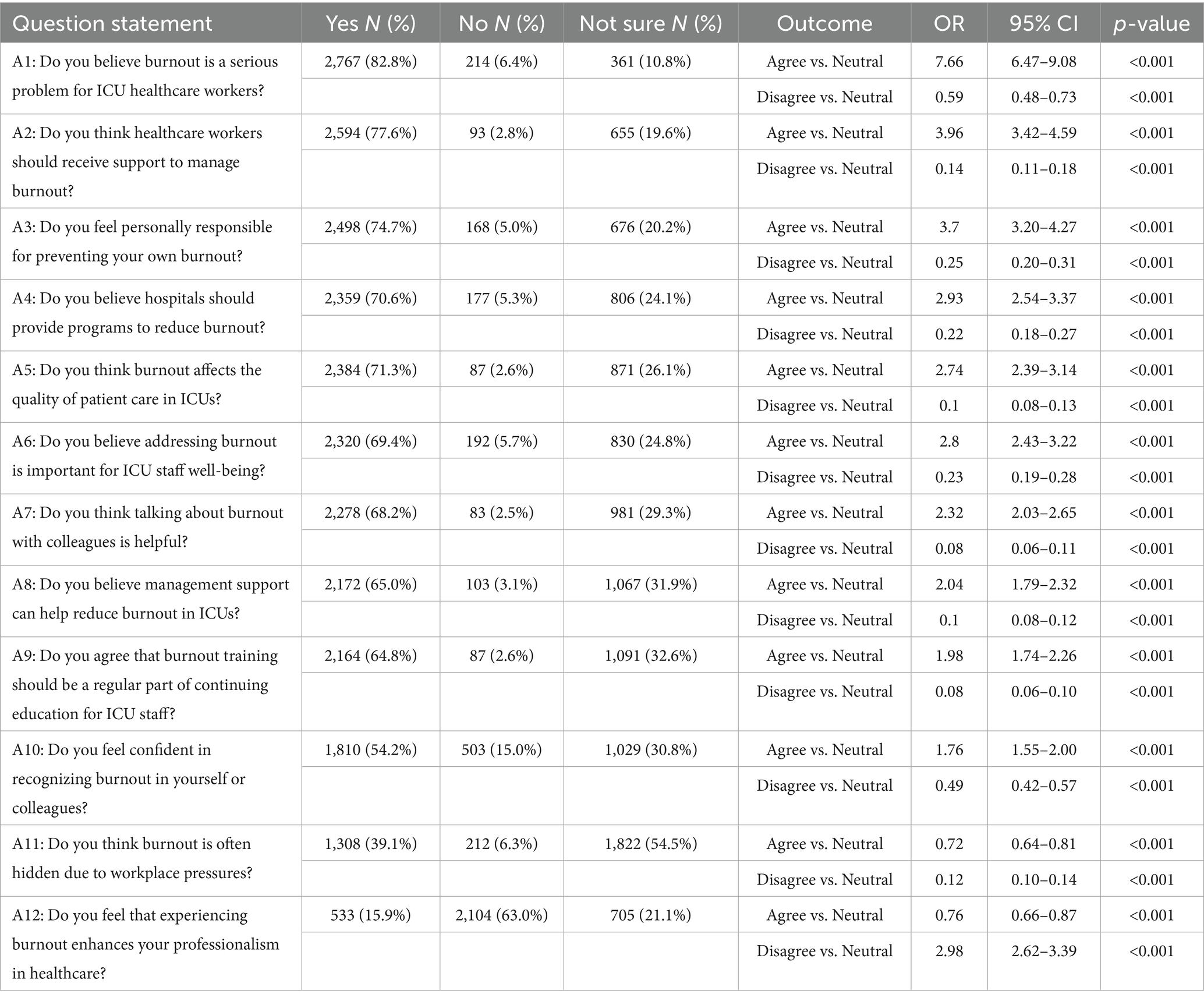
Table 3. Evaluation of attitudes toward burnout impact and support requirements among ICU healthcare workers.
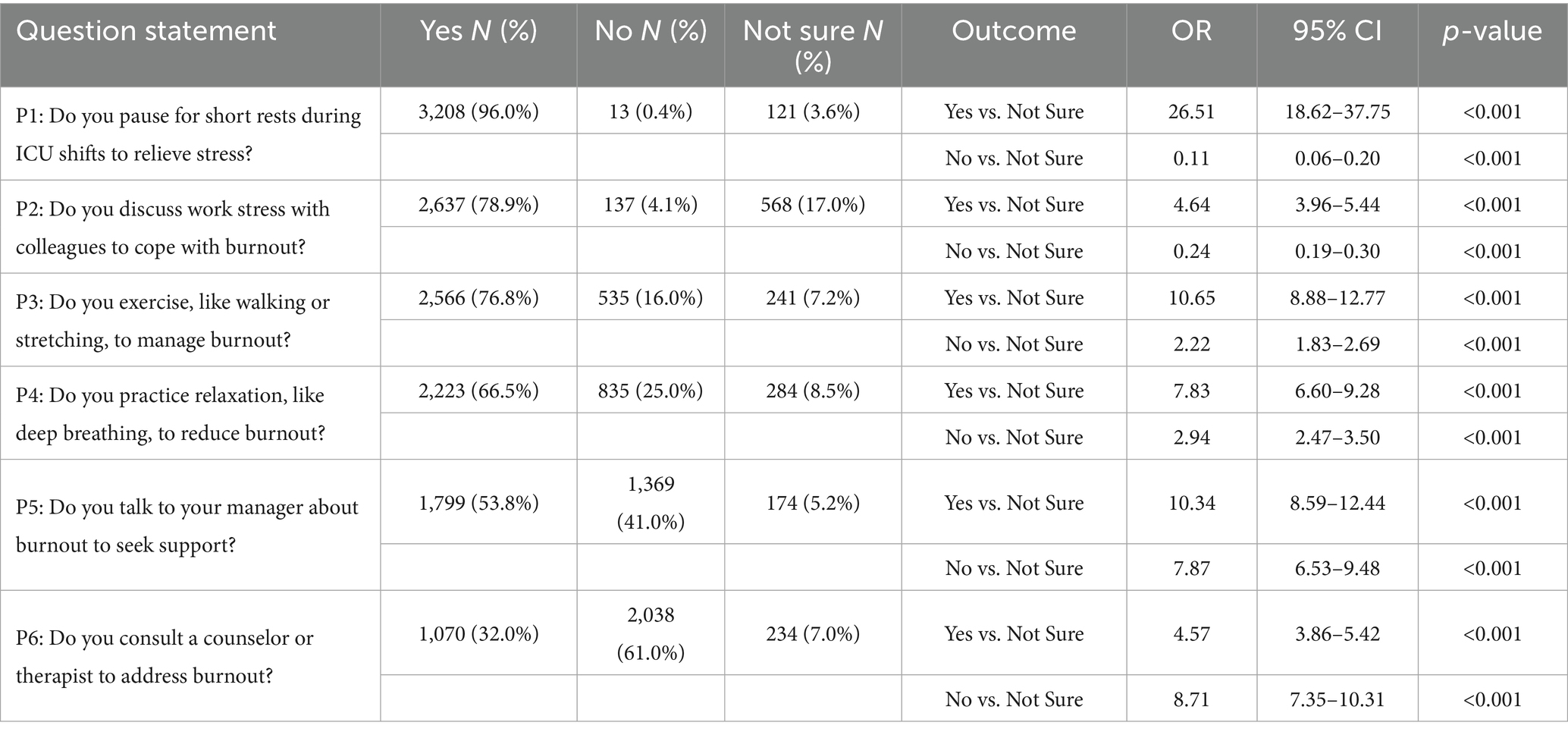
3.3 Practice outcomes: engagement in burnout prevention behaviors
Most HCWs took breaks (96.0%, OR = 26.51, 95% CI 18.62–37.75, p < 0.001), discussed stress with colleagues (78.9%, OR = 4.64, 95% CI 3.96–5.44, p < 0.001), exercised (76.8%, OR = 10.65, 95% CI 8.88–12.77, p < 0.001), and practiced relaxation (66.5%, OR = 7.83, 95% CI 6.60–9.28, p < 0.001). Only 53.8% sought managerial support (OR = 10.34, 95% CI 8.59–12.44, p < 0.001), and 61.0% did not consult counselors (OR = 8.71, 95% CI 7.35–10.31, p < 0.001), as shown in Table 4.
3.4 Predictors of burnout knowledge
HCWs aged 25–34 (OR = 4.01, 95% CI 2.92–5.50, p < 0.001), 35–44 (OR = 4.01, 95% CI 2.91–5.53, p < 0.001), 45–54 (OR = 2.25, 95% CI 1.60–3.17, p < 0.001), nurses (OR = 6.00, 95% CI 4.36–8.25, p < 0.001), physicians (OR = 6.00, 95% CI 4.14–8.70, p < 0.001), technicians (OR = 2.25, 95% CI 1.62–3.13, p < 0.001), those with 1–5 (OR = 6.00, 95% CI 4.48–8.04, p < 0.001), 6–10 (OR = 6.00, 95% CI 4.37–8.24, p < 0.001), or 11–20 years experience (OR = 3.00, 95% CI 2.22–4.06, p < 0.001), and with mental health resource access (OR = 4.01, 95% CI 3.35–4.80, p < 0.001) were with adequate knowledge. Temporary/visiting (OR = 0.54, 95% CI 0.42–0.70, p < 0.001) and contract HCWs (OR = 0.79, 95% CI 0.67–0.94, p = 0.007) were inadequate knowledge, as shown in Table 5.
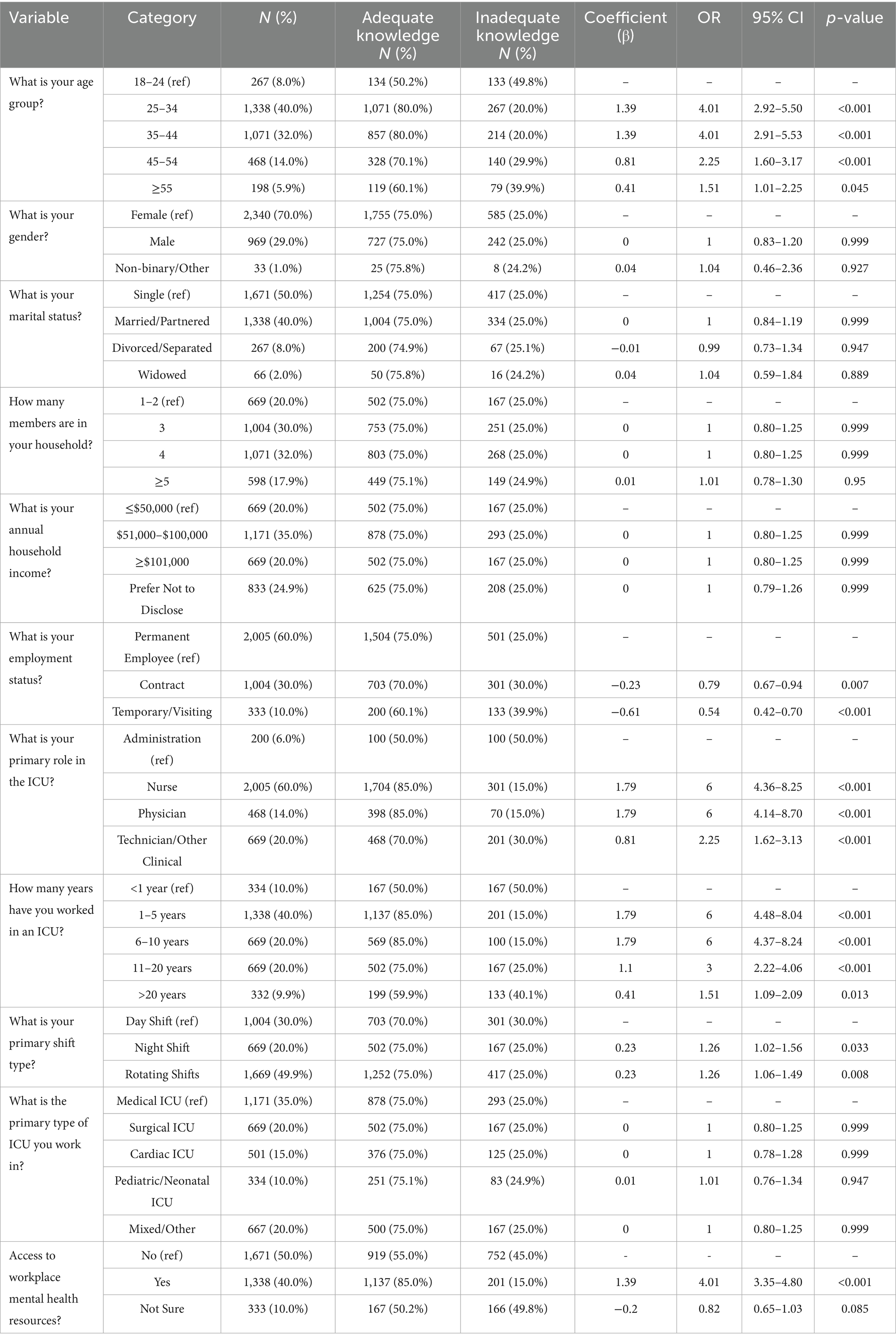
Table 5. Logistic regression analysis of factors associated with burnout knowledge among ICU healthcare workers.
3.5 Predictors of positive attitudes toward burnout
HCWs aged 25–34 (OR = 4.01, 95% CI 2.92–5.50, p < 0.001), 35–44 (OR = 4.01, 95% CI 2.91–5.53, p < 0.001), 45–54 (OR = 2.25, 95% CI 1.60–3.17, p < 0.001), nurses (OR = 6.00, 95% CI 4.36–8.25, p < 0.001), physicians (OR = 6.00, 95% CI 4.14–8.70, p < 0.001), technicians (OR = 2.25, 95% CI 1.62–3.13, p < 0.001), those with 1–5 (OR = 6.00, 95% CI 4.48–8.04, p < 0.001), 6–10 (OR = 6.00, 95% CI 4.37–8.24, p < 0.001), or 11–20 years experience (OR = 3.00, 95% CI 2.22–4.06, p < 0.001), and with mental health resource access (OR = 4.01, 95% CI 3.35–4.80, p < 0.001) had more positive attitudes. Temporary/visiting (OR = 0.54, 95% CI 0.42–0.70, p < 0.001) and contract HCWs (OR = 0.79, 95% CI 0.67–0.94, p = 0.007) were less likely to have positive attitudes, as shown in Table 6.
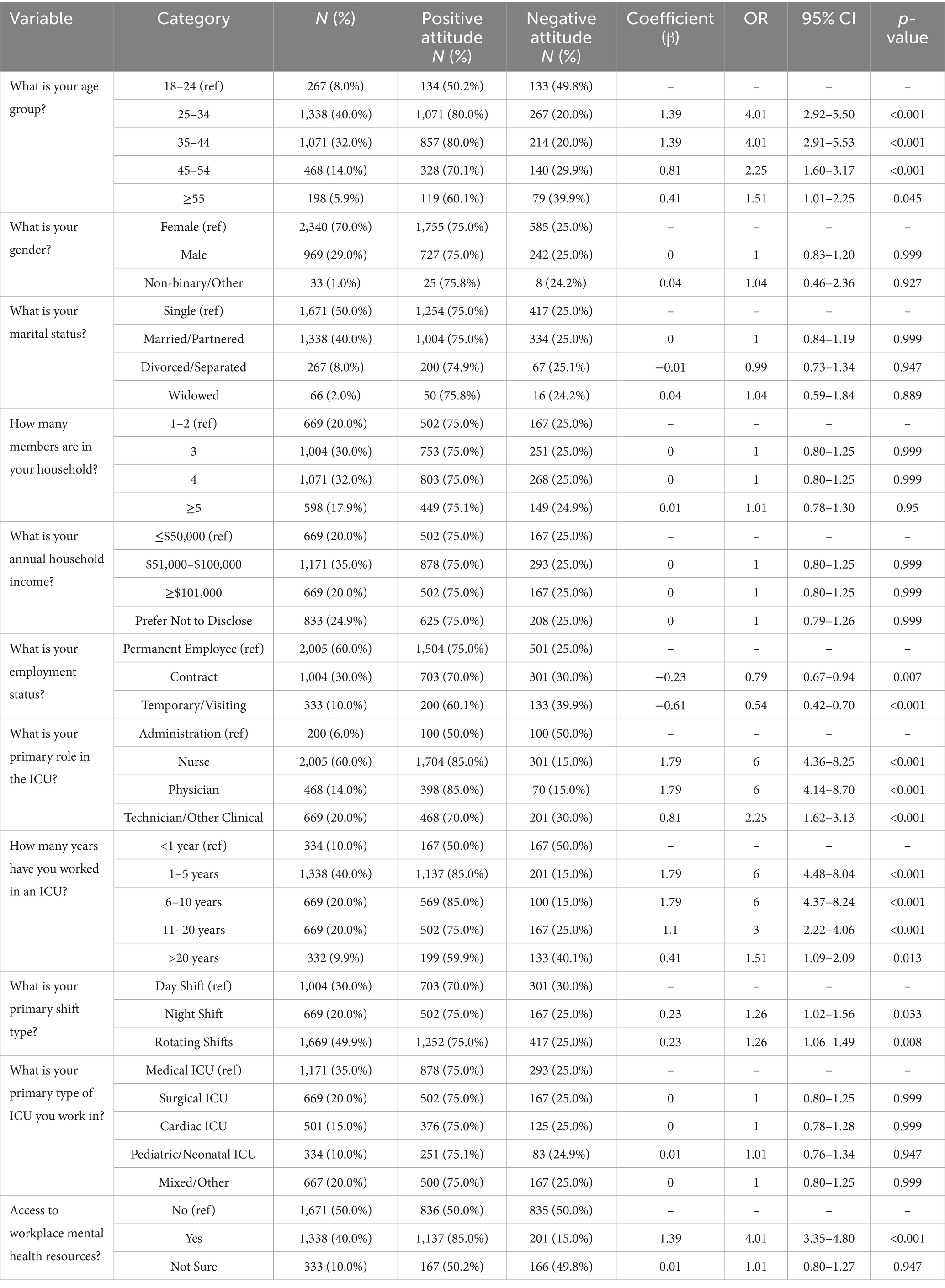
Table 6. Logistic regression analysis of factors influencing positive attitudes toward burnout among ICU healthcare workers.
3.6 Predictors of effective burnout prevention practices
Healthcare workers aged 25–34 (OR = 4.01, 95% CI 2.92–5.50, p < 0.001), 35–44 (OR = 4.01, 95% CI 2.91–5.53, p < 0.001), 45–54 (OR = 2.25, 95% CI 1.60–3.17, p < 0.001), nurses (OR = 4.01, 95% CI 2.92–5.50, p < 0.001), physicians (OR = 3.98, 95% CI 2.75–5.76, p < 0.001), technicians (OR = 2.25, 95% CI 1.62–3.13, p < 0.001), those with 1–5 (OR = 4.01, 95% CI 2.99–5.38, p < 0.001), 6–10 (OR = 4.01, 95% CI 2.92–5.51, p < 0.001), or 11–20 years experience (OR = 3.00, 95% CI 2.22–4.06, p < 0.001), night shift (OR = 1.26, 95% CI 1.02–1.56, p = 0.033) or rotating shift workers (OR = 1.26, 95% CI 1.06–1.49, p = 0.008), and those with mental health resource access (OR = 4.01, 95% CI 3.35–4.80, p < 0.001) were more engaged in good practices. Temporary/visiting (OR = 0.54, 95% CI 0.42–0.70, p < 0.001) and contract HCWs (OR = 0.79, 95% CI 0.67–0.94, p = 0.007) were less engaged, as shown in Table 7.
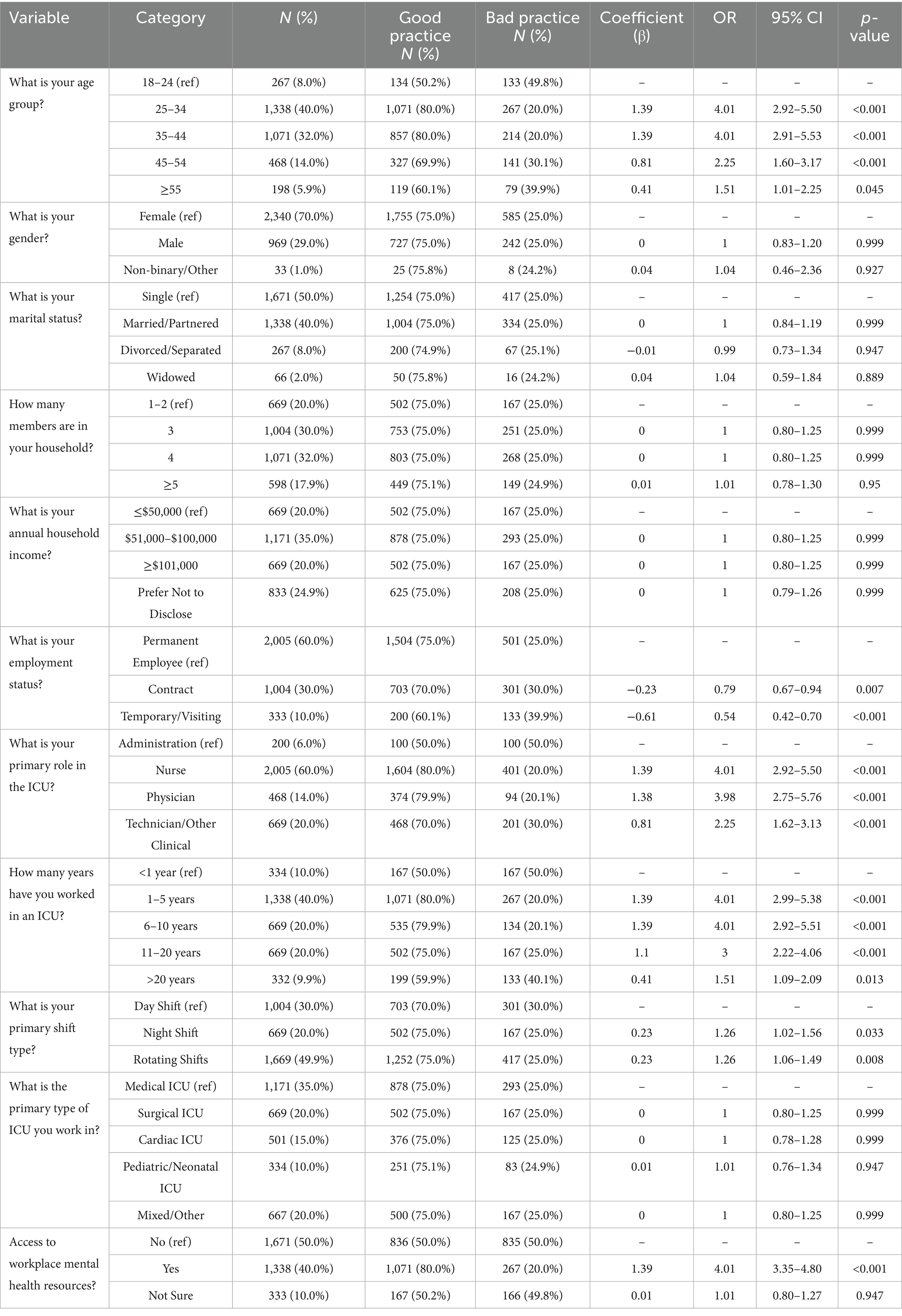
Table 7. Logistic regression analysis of factors associated with effective burnout prevention practices among ICU healthcare workers.
4 Discussion
This study provides comprehensive insight into burnout KAP among 3,342 HCWs across a regional network of healthcare facilities in Yancheng, Jiangsu, China. The findings extend current literature by identifying specific demographic and occupational predictors of burnout-related KAP, while also revealing gaps in institutional support. Compared to existing global evidence, our data both corroborates and diverges from prior studies, highlighting new perspectives on burnout dynamics in routine, post-pandemic ICU contexts.
The workforce profile revealed a young, predominantly female cohort with a high representation of nurses and mid-career professionals in permanent positions. Access to mental health resources was limited, with 50.0% of HCWs reporting no access, 40.0% confirming access, and 10.0% unsure, consistent with Table 1. The unsure responses may reflect variability in awareness or availability across facilities, underscoring the need for standardized resource dissemination in the regional network. This gap aligns with global concerns regarding insufficient psychological support in critical care settings, particularly in resource-constrained systems. This staffing structure aligns with previous studies indicating that ICU environments globally are often characterized by nurse-dominant, female-majority teams (32, 33). The prevalence of mid-career staff suggests either effective workforce retention or evolving institutional policies in Chinese ICUs that favor continuity and experience accumulation. Interestingly, while the workforce stability appears strong, only 40% of HCWs reported access to mental health resources, echoing widespread concerns regarding the insufficient integration of psychological support within critical care infrastructure (34, 35). Compared to high-income countries where institutional wellness programs are increasingly standardized (36), the persistent resource gap in our setting underscores the disparity in structural support across healthcare systems. This deficit is especially significant given the acknowledged role of organizational interventions in reducing burnout risk and improving resilience among HCWs (37, 38).
Regarding knowledge of burnout, our findings align with previous studies showing that HCWs readily identify workload-related contributors such as long shifts, high patient acuity, and emotional strain (11, 39). However, critical gaps persist in awareness of formal prevention strategies, institutional training initiatives, and actual burnout prevalence. This disconnects between recognition and mitigation knowledge reflects global patterns, particularly in US and European studies, where systemic inertia often delays meaningful intervention (40). Our study adds to this literature by highlighting similar trends in a non-Western ICU context, where stress may be normalized, and institutional solutions underdeveloped. Novel in our findings is the widespread uncertainty surrounding burnout prevalence among peers—a potential result of cultural reticence, insufficient organizational transparency, or the internalization of high stress as normative. This phenomenon has been underreported in prior burnout studies, and its identification here underscores the importance of open discourse and burnout surveillance mechanisms as precursors to systemic reform (12, 41, 42).
Notably, gender, marital status, household size, income, and ICU type were non-significant predictors of KAP outcomes, contrasting with studies linking female sex or specific ICU types (e.g., medical ICUs) to higher burnout risk (43, 44). This discrepancy may reflect contextual factors in the Yancheng healthcare network. Uniformly high workloads across ICU types could minimize differences in burnout vulnerability. Similarly, cultural norms in China, where professional demands often supersede personal circumstances, may reduce the influence of gender or marital status on burnout perceptions. The income’s non-significance may stem from the 24.9% non-disclosure rate, limiting statistical power. These findings suggest that institutional and cultural factors may overshadow demographic influences in this cohort, warranting further exploration in multi-center studies to clarify context-specific drivers.
Attitudinally, HCWs in this study demonstrated strong recognition of burnout’s adverse effects on patient care and staff well-being, a pattern echoed in global evidence (45, 46). The widespread endorsement of institutional support, peer dialog, and structured interventions reaffirms the centrality of systemic responses to burnout prevention (47, 48). However, only moderate self-efficacy in recognizing burnout and considerable uncertainty regarding stigma suggest persisting internal and cultural barriers to effective identification and discussion. These findings align with previous studies identifying stigma and lack of formal training as key deterrents to early recognition (47). Interestingly, participants overwhelmingly rejected the notion that burnout enhances professional identity view that diverges from earlier narratives portraying stress endurance as a marker of professional commitment (49, 50).
Practices reported by ICU staff revealed a strong preference for informal coping mechanisms—such as taking breaks (96.0%), peer discussions (78.9%), and exercise (76.8%)—over formal approaches like counseling (32.0%) or managerial engagement (53.8%). This trend mirrors Western findings where HCWs favor self-initiated strategies due to stigma or access barriers. In the Chinese ICU context, additional cultural and organizational factors likely contribute (50, 51). Mental health stigma, prevalent in China, may deter HCWs from seeking counseling due to fears of professional judgment. Hierarchical hospital structures may discourage managerial discussions, as staff perceive such actions as risking career advancement. Limited visibility and availability of confidential counseling services, with only 40.0% reporting access, further exacerbate underutilization. These barriers suggest the need for culturally sensitive interventions, such as anonymous counseling platforms, leadership-driven stigma reduction campaigns, and mandatory mental health literacy training integrated into staff onboarding across all facilities in the Yancheng network (52–54, 59, 60).
Our regression models identified consistent predictors of favorable KAP outcomes: mid-career age groups, clinical roles (especially nurses and physicians), ICU experience between 1 and 20 years, rotating shift work, and access to mental health resources. These findings support prior research showing that clinical exposure and institutional support are key to effective burnout recognition and prevention (46, 55, 56). Conversely, temporary and contract HCWs were inadequate knowledge, less positive in attitude, and less engaged in preventive practices—a novel and concerning finding. This subgroup likely experiences marginalization in institutional support systems, emphasizing the need for inclusive policy interventions. Notably, variables such as gender, marital status, household size, income, and ICU type did not predict KAP outcomes, contradicting some studies but possibly reflecting contextual stability within our regional multi-institutional cohort.
By applying a KAP framework in a large, post-COVID ICU setting, this study addresses several critical gaps in existing burnout literature and contributes novel evidence to the field. First, it shifts the focus beyond acute crisis settings—such as pandemics—to examine the persistent, systemic stressors contributing to chronic burnout under routine clinical operations. This distinction is vital for designing sustainable interventions. Second, it links behavioral burnout outcomes with granular sociodemographic and occupational predictors, allowing for precision in intervention targeting—an approach often lacking in broader prevalence-focused studies. Third, it brings to light disparities in knowledge, attitudes, and preventive behaviors among non-permanent HCWs, a group routinely excluded from institutional wellness programs despite elevated vulnerability. This inclusion enhances the equity and inclusivity of burnout research. Lastly, the large sample size and multi-domain KAP design offer a robust methodological contribution, making this study one of the few to comprehensively assess burnout cognition and behavior at scale within a high-risk ICU environment in a non-Western context.
The regional focus on Yancheng, Jiangsu, limits the generalizability of findings to other healthcare systems, particularly those with differing organizational cultures or resource availability. Chinese ICUs often operate within hierarchical structures, which may discourage formal support-seeking due to perceived professional risks or mental health stigma, a factor less prominent in Western settings with standardized wellness programs. Resource constraints in China’s public hospitals may exacerbate gaps in mental health support compared to high-income countries. These cultural and systemic factors likely influenced the preference for informal coping and low counseling uptake observed, underscoring the need for context-specific interventions. Multi-center studies spanning diverse regions are needed to enhance the applicability of findings.
The multicenter design of this study was confined to 10 hospitals within a single city, Yancheng, Jiangsu. Consequently, the findings are context-specific and may not be readily generalizable to ICUs in other Chinese provinces or to healthcare systems with different organizational structures and resource availability. The cross-sectional nature of the study design inherently precludes causal inferences and an analysis of temporal trends in burnout. Although a high response rate of 74.3% was achieved, the potential for selection bias cannot be fully dismissed, as non-respondents might systematically differ from participants (e.g., in terms of workload, motivation, or burnout severity). The exclusive use of self-reported data for KAP is a limitation due to potential recall and social-desirability biases. Lastly, the evaluation of mental health resource accessibility relied entirely on participant self-report, lacking external validation of the quality or scope of these services.
5 Conclusion
This study reveals that ICU staff in a post-pandemic, multi-institutional context in Yancheng, Jiangsu, experience substantial burnout, with knowledge, attitudes, and practices influenced by clinical role, ICU experience, shift schedules, and institutional support availability. Temporary and contract staff demonstrated lower KAP scores, highlighting structural vulnerabilities. The predominance of informal coping strategies points to cultural and organizational barriers to formal support engagement. These findings, while robust within the regional context, underscore the need to standardize mental health support, enhance burnout training, and integrate non-permanent staff into wellness initiatives. The KAP framework provides a scalable tool for behavioral monitoring, but broader studies are needed to generalize findings across diverse healthcare systems.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was obtained from the Departmental Bioethical Committee of the ICU at the coordinating tertiary care facility in Yancheng, Jiangsu (Approval No. IRB-2022-0315), with additional approvals from the ethics boards of participating hospitals and clinics in the region. Written informed consent was obtained from all participants prior to inclusion, in accordance with institutional guidelines and the Declaration of Helsinki. Participants were informed of their right to withdraw at any time without consequence, with clear instructions provided via the survey platform. Anonymity was protected by collecting no identifiable information and using unique, non-traceable identifiers. Data were stored in an encrypted database with access restricted to authorized researchers. To mitigate potential coercion given the high response rate (74.3%), participation was explicitly voluntary, with no incentives offered, and facility leadership ensured no workplace repercussions for non-participation. Multi-institutional coordination ensured consistent ethical standards across all sites.
Author contributions
CZ: Resources, Formal analysis, Writing – original draft, Project administration, Methodology, Data curation, Investigation, Conceptualization. XL: Project administration, Conceptualization, Methodology, Formal analysis, Funding acquisition, Investigation, Data curation, Writing – original draft. LH: Conceptualization, Project administration, Data curation, Writing – original draft, Formal analysis, Methodology, Investigation. BX: Investigation, Funding acquisition, Writing – original draft, Conceptualization, Formal analysis, Methodology. YW: Project administration, Methodology, Formal analysis, Data curation, Writing – review & editing. JH: Funding acquisition, Software, Supervision, Project administration, Writing – review & editing, Methodology, Data curation. WW: Supervision, Software, Formal analysis, Writing – review & editing, Resources, Funding acquisition, Project administration. ZL: Resources, Project administration, Validation, Software, Writing – review & editing, Methodology, Funding acquisition, Supervision, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Medical Research Project of the Yancheng Health Commission (grant no. YK2023059).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. De Hert, S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. (2020) 13:171–83. doi: 10.2147/lra.s240564
2. Selamu, M, Thornicroft, G, Fekadu, A, and Hanlon, C. Conceptualisation of job-related wellbeing, stress and burnout among healthcare workers in rural Ethiopia: a qualitative study. BMC Health Serv Res. (2017) 17:412. doi: 10.1186/s12913-017-2370-5
3. Rössler, W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin Neurosci. (2012) 262:65–9. doi: 10.1007/s00406-012-0353-4
4. Klick, JC, Syed, M, Leong, R, Miranda, H, and Cotter, EK. Health and well-being of intensive care unit physicians: how to ensure the longevity of a critical specialty. Anesthesiol Clin. (2023) 41:303–16. doi: 10.1016/j.anclin.2022.10.009
5. Stocchetti, N, Segre, G, Zanier, ER, Zanetti, M, Campi, R, Scarpellini, F, et al. Burnout in intensive care unit workers during the second wave of the COVID-19 pandemic: a single center cross-sectional Italian study. Int J Environ Res Public Health. (2021) 18:6102. doi: 10.3390/ijerph18116102
6. Baillat, L, Vayre, E, Préau, M, and Guérin, C. Burnout and brownout in intensive care physicians in the era of COVID-19: a qualitative study. Int J Environ Res Public Health. (2023) 20:6029. doi: 10.3390/ijerph20116029
7. Gramaglia, C, Bazzano, S, Gambaro, E, Cena, T, Azzolina, D, Costa, A, et al. Mental health impact and burnout in critical care staff during coronavirus disease 2019 outbreak. Turk J Anaesthesiol Reanim. (2022) 50:S34–41. doi: 10.5152/tjar.2022.21263
8. Artz, B, Kaya, I, and Kaya, O. Gender role perspectives and job burnout. Rev Econ Househ. (2022) 20:447–70. doi: 10.1007/s11150-021-09579-2
9. Niven, AS, and Sessler, CN. Supporting professionals in critical care medicine: burnout, resiliency, and system-level change. Clin Chest Med. (2022) 43:563–77. doi: 10.1016/j.ccm.2022.05.010
10. Kerlin, MP, McPeake, J, and Mikkelsen, ME. Burnout and joy in the profession of critical care medicine. Crit Care. (2020) 24:98. doi: 10.1186/s13054-020-2784-z
11. Quesada-Puga, C, Izquierdo-Espin, FJ, Membrive-Jiménez, MJ, Aguayo-Estremera, R, Cañadas-De La Fuente, GA, Romero-Béjar, JL, et al. Job satisfaction and burnout syndrome among intensive-care unit nurses: a systematic review and meta-analysis. Intensive Crit Care Nurs. (2024) 82:103660. doi: 10.1016/j.iccn.2024.103660
12. Krishna, GG, Harbli, NMA, Krishnan, N, Ghundul, LB, Aldhahri, R, Aldossary, AB, et al. Burnout among ICU and non-ICU healthcare professionals in Saudi Arabia: a comparative cross-sectional analysis. J Multidiscip Healthc. (2025) 18:995–1005. doi: 10.2147/JMDH.S503896
13. Colbenson, GA, Ridgeway, JL, Benzo, RP, and Kelm, DJ. Examining burnout in Interprofessional intensive care unit clinicians using qualitative analysis. Am J Crit Care. (2021) 30:391–6. doi: 10.4037/ajcc2021423
14. Hernández-Marrero, P, Pereira, SM, and Carvalho, AS. Ethical decisions in palliative care: interprofessional relations as a burnout protective factor? Results from a mixed-methods multicenter study in Portugal. Am J Hosp Palliat Care. (2016) 33:723–32. doi: 10.1177/1049909115583486
15. Green, AE, Albanese, BJ, Shapiro, NM, and Aarons, GA. The roles of individual and organizational factors in burnout among community-based mental health service providers. Psychol Serv. (2014) 11:41–9. doi: 10.1037/a0035299
16. Liu, Y, Ying, L, Zhang, Y, and Jin, J. The experiences of intensive care nurses coping with ethical conflict: a qualitative descriptive study. BMC Nurs. (2023) 22:449. doi: 10.1186/s12912-023-01612-2
17. Pishgooie, AH, Barkhordari-Sharifabad, M, Atashzadeh-Shoorideh, F, and Falcó-Pegueroles, A. Ethical conflict among nurses working in the intensive care units. Nurs Ethics. (2019) 26:2225–38. doi: 10.1177/0969733018796686
18. Zenani, NE, Gause, G, and Sehularo, L. Strategies to enhance resilience to cope with workplace adversities post-COVID-19 among ICU nurses. Curationis. (2022) 45:e1–8. doi: 10.4102/curationis.v45i1.2345
19. Maves, RC. Resiliency and mental health in the ICU. Am J Respir Crit Care Med. (2024) 209:481–2. doi: 10.1164/rccm.202401-0066ED
20. Greene Barker, T, O'Higgins, A, Fonagy, P, and Gardner, F. A systematic review and meta-analysis of the effectiveness of co-designed, in-person, mental health interventions for reducing anxiety and depression symptoms. J Affect Disord. (2024) 350:955–73. doi: 10.1016/j.jad.2023.12.080
21. Kirkbride, JB, Anglin, DM, Colman, I, Dykxhoorn, J, Jones, PB, Patalay, P, et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. (2024) 23:58–90. doi: 10.1002/wps.21160
22. Wainberg, ML, Scorza, P, Shultz, JM, Helpman, L, Mootz, JJ, Johnson, KA, et al. Challenges and opportunities in global mental health: a research-to-practice perspective. Curr Psychiatry Rep. (2017) 19:28. doi: 10.1007/s11920-017-0780-z
23. Li, M, Chen, H, Ju, Y, Zeng, L, and Li, N. A cross-sectional survey and influencing factors analysis of knowledge, attitude, and behavior of enteral nutrition implemented by nurses in burn intensive care unit. Zhonghua Shao Shang Za Zhi. (2023) 39:874–81. doi: 10.3760/cma.j.cn501225-20220522-00198
24. Buksh, NA, Ghani, M, Amir, S, Asmat, K, and Ashraf, S. Assessment of nurses’ knowledge and practice for prevention of infection in burn patients. Saudi J Med Pharm Sci. (2019) 5:846–55. doi: 10.36348/SJMPS.2019.v05i10.005
25. Lu, X, Li, D, Luo, H, Wang, L, Lou, Y, and Yu, Y. Knowledge, attitude, and practice towards occupational burnout among doctors and nurses in intensive care unit. Front Public Health. (2025) 13:1480052. doi: 10.3389/fpubh.2025.1480052
26. Qin, Z, Zhao, X, Meng, Y, Wu, Y, Qian, J, Yin, M, et al. Knowledge, attitudes and practices of intensive care unit physicians towards the management of acute respiratory distress syndrome in China: a cross-sectional survey. BMJ Open. (2025) 15:e092069. doi: 10.1136/bmjopen-2024-092069
27. Abu Ibaid, AH, Hebron, CA, Qaysse, HA, Coyne, MJ, Potokar, TS, Shalltoot, FA, et al. Epidemiology, aetiology and knowledge, attitudes, and practices relating to burn injuries in Palestine: a community-level research. Int Wound J. (2022) 19:1210–20. doi: 10.1111/iwj.13716
28. Ashebir, W, Yimer, B, Alle, A, Teshome, M, Teka, Y, and Wolde, A. Knowledge, attitude, practice, and factors associated with prevention practice towards COVID-19 among healthcare providers in Amhara region, northern Ethiopia: a multicenter cross-sectional study. PLOS Global Public Health. (2022) 2:e0000171. doi: 10.1371/journal.pgph.0000171
29. Basheer, R, Bhargavi, P, and Prakash, HP. Knowledge, attitude, and practice of printing press workers towards noise-induced hearing loss. Noise Health. (2019) 21:62–8. doi: 10.4103/nah.NAH_9_19
30. Sivagourounadin, K, Rajendran, P, and Ravichandran, M. Knowledge, attitude, and practice of Materiovigilance among nurses at a tertiary care hospital in South India: a cross-sectional study. J Pharm Bioallied Sci. (2022) 14:162–7. doi: 10.4103/jpbs.jpbs_274_21
31. Okello, G, Izudi, J, Teguzirigwa, S, Kakinda, A, and Van Hal, G. Findings of a cross-sectional survey on knowledge, attitudes, and practices about COVID-19 in Uganda: implications for public health prevention and control measures. Bio Med Res Int. (2020) 2020:5917378. doi: 10.1155/2020/5917378
32. Rushton, CH, Batcheller, J, Schroeder, K, and Donohue, P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care. (2015) 24:412–20. doi: 10.4037/ajcc2015291
33. Moss, M, Good, VS, Gozal, D, Kleinpell, R, and Sessler, CN. An official critical care societies collaborative statement: burnout syndrome in critical care health care professionals: a call for action. Am J Crit Care. (2016) 25:368–76. doi: 10.4037/ajcc2016133
34. West, CP, Dyrbye, LN, Erwin, PJ, and Shanafelt, TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272–81. doi: 10.1016/S0140-6736(16)31279-X
35. Santarone, K, McKenney, M, and Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am J Emerg Med. (2020) 38:1530–1. doi: 10.1016/j.ajem.2020.04.030
36. Panagioti, M, Panagopoulou, E, Bower, P, Lewith, G, Kontopantelis, E, Chew-Graham, C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. (2017) 177:195–205. doi: 10.1001/jamainternmed.2016.7674
37. Moffatt-Bruce, SD, Nguyen, MC, Steinberg, B, Holliday, S, and Klatt, M. Interventions to reduce burnout and improve resilience: impact on a health system’s outcomes. Clin Obstet Gynecol. (2019) 62:432–43. doi: 10.1097/GRF.0000000000000458
38. Cleary, M, Kornhaber, R, Thapa, DK, West, S, and Visentin, D. The effectiveness of interventions to improve resilience among health professionals: a systematic review. Nurse Educ Today. (2018) 71:247–63. doi: 10.1016/j.nedt.2018.10.002
39. Kissel, KA, Filipek, C, and Jenkins, J. Impact of the COVID-19 pandemic on nurses working in intensive care units: a scoping review. Crit Care Nurse. (2023) 43:55–63. doi: 10.4037/ccn2023196
40. Shanafelt, T, Ripp, J, and Trockel, M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
41. Ramírez-Elvira, S, Romero-Béjar, JL, Suleiman-Martos, N, Gómez-Urquiza, JL, Monsalve-Reyes, C, Cañadas-De la Fuente, GA, et al. Prevalence, risk factors and burnout levels in intensive care unit nurses: a systematic review and Meta-analysis. Int J Environ Res Public Health. (2021) 18:1432. doi: 10.3390/ijerph182111432
42. Turunç, Ö, Çalışkan, A, Akkoç, İ, Köroğlu, Ö, Gürsel, G, Demirci, A, et al. The impact of intensive care unit nurses’ burnout levels on turnover intention and the mediating role of psychological resilience. Behav Sci. (2024) 14:782. doi: 10.3390/bs14090782
43. Embriaco, N, Azoulay, E, Barrau, K, Kentish, N, Pochard, F, Loundou, A, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. (2007) 175:686–92. doi: 10.1164/rccm.200608-1184OC
44. Postelnicu, R, Evans, L, Rodriguez, A, Otero, G, Hewitt, K, and Mukherjee, V. 103: burnout syndrome variations: difference among intensive care unit nursing staff location. Crit Care Med. (2019) 47:34. doi: 10.1097/01.CCM.0000550860.51380.8D
45. Rotenstein, LS, Torre, M, Ramos, MA, Rosales, RC, Guille, C, Sen, S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
46. Maslach, C, and Leiter, MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (2016) 15:103–11. doi: 10.1002/wps.20311
47. Shanafelt, T, Goh, J, and Sinsky, C. The business case for investing in physician well-being. JAMA Intern Med. (2017) 177:1826–32. doi: 10.1001/jamainternmed.2017.4340
48. Walsh, AL, Lehmann, S, Zabinski, J, Truskey, M, Purvis, T, Gould, NF, et al. Interventions to prevent and reduce burnout among undergraduate and graduate medical education trainees: a systematic review. Acad Psychiatry. (2019) 43:386–95. doi: 10.1007/s40596-019-01023-z
49. Salyers, MP, Bonfils, KA, Luther, L, Firmin, RL, White, DA, Adams, EL, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. (2017) 32:475–82. doi: 10.1007/s11606-016-3886-9
50. Mari, S, Meyen, R, and Kim, B. Resident-led organizational initiatives to reduce burnout and improve wellness. BMC Med Educ. (2019) 19:437. doi: 10.1186/s12909-019-1756-y
51. Dyrbye, L, and Shanafelt, T. A narrative review on burnout experienced by medical students and residents. Med Educ. (2016) 50:132–49. doi: 10.1111/medu.12927
52. Shokre, ES, Mohammed, SEM, Elhapashy, HMM, Elsharkawy, NB, Ramadan, OME, and Abdelaziz, EM. The effectiveness of the psychosocial empowerment program in early adjustment among adult burn survivors. BMC Nurs. (2024) 23:45. doi: 10.1186/s12912-024-01700-x
53. McDermott, L, Hotton, M, and Cartwright, AV. Understanding the barriers and enablers for seeking psychological support following a burn injury. Eur Burn J. (2023) 4:303–18. doi: 10.3390/ebj4030028
54. Tweed, E, Cimova, K, Craig, P, Allik, M, Brown, D, Campbell, M, et al. Unlocking data: decision-maker perspectives on cross-sectoral data sharing and linkage as part of a whole-systems approach to public health policy and practice. Public Health Res. (2024):1–30. doi: 10.3310/kytw2173
55. Garcia, CL, Abreu, LC, Ramos, JLS, Castro, CFD, Smiderle, FRN, Santos, JAD, et al. Influence of burnout on patient safety: systematic review and meta-analysis. Medicina (Kaunas). (2019) 55:553. doi: 10.3390/medicina55090553
56. Kleinpell, R, Moss, M, Good, VS, Gozal, D, and Sessler, CN. The critical nature of addressing burnout prevention: results from the critical care societies collaborative's national summit and survey on prevention and management of burnout in the ICU. Crit Care Med. (2020) 48:249–53. doi: 10.1097/CCM.0000000000003964
57 Awan, UA, Naeem, W, Khattak, AA, Mahmood, T, Kamran, S, Khan, S, et al. An exploratory study of knowledge, attitudes, and practices toward HPV associated anal cancer among Pakistani population. Frontiers in Oncology. (2023) 13:1257401. doi: 10.3389/fonc.2023.1257401
58. Qasim, M, Awan, UA, Afzal, MS, Saqib, MA, Siddiqui, S, and Ahmed, H. Dataset of knowledge, attitude, practices and psychological implications of healthcare workers in Pakistan during COVID-19 pandemic. Data in Brief. (2020) 32:106234. doi: 10.1016/j.dib.2020.106234
59 Awan, UA, Zahoor, S, Ayub, A, Ahmed, H, Aftab, N, and Afzal, MS. COVID‐19 and arboviral diseases: another challenge for Pakistan’s dilapidated healthcare system. Journal of Medical Virology. (2020) 93:4065. doi: 10.1002/jmv.26668
Keywords: burnout, intensive care, healthcare workers, KAP survey, mental-health resources, workforce resilience
Citation: Zhang CQ, Li X, He L, Xu B, Wu Y, He J, Wang W and Lu ZQ (2025) Critical care, critical gaps: assessment of burnout and behavioral profiles of ICU healthcare workers in China—a multicenter cross-sectional study. Front. Public Health. 13:1617081. doi: 10.3389/fpubh.2025.1617081
Edited by:
Marília Silva Paulo, Universidade Nova de Lisboa, PortugalReviewed by:
Rajesh Kumar, All India Institute of Medical Sciences, Rishikesh, IndiaCeren Meriç Özgündüz, Koç University, Türkiye
Copyright © 2025 Zhang, Li, He, Xu, Wu, He, Wang and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhong Qian Lu, bHV6aG9uZ3FpYW4xOTc2QDE2My5jb20=
 Chao Qing Zhang
Chao Qing Zhang Xing Li
Xing Li Zhong Qian Lu
Zhong Qian Lu