- 1Fujian Medical University Clinical Skills Teaching Center, Fuzhou, Fujian, China
- 2Fujian Medical University Union Hospital, Fuzhou, Fujian, China
Background: Medical Simulation Centers have become integral to filling the gaps between theoretical learning and clinical practice as part of modern medical education. Traditional clinical teaching is often restricted by ethical constraints, limited patient contacts, and variable quality of training; there is a need for structured, simulation-based approaches to fill those gaps.
Objective: This study is intended to identify effective approaches to developing and optimizing Medical Simulation Centers based on the New Medical Sciences principles, and the Fujian Medical University institutional experience is proposed as a model.
Methods: A descriptive institutional study was designed to collect data from Fujian Medical University’s Medical Simulation Center from 2020 to 2024. Key elements of infrastructure development, management components, faculty development, and curriculum development were considered, emphasizing principles of competency-based medical education.
Results: Developing a structured simulation-based program improved students’ clinical preparedness, procedural skills, and performance in objective structured clinical examinations (OSCE). The Fujian model shows that positive results related to faculty development, sustainable funding, and curriculum integrations are important to the success of Medical Simulation Centers.
Conclusion: Medical Simulation Centers are essential to bridging theory and practice in medical education. Creating a structured and governed simulation program improves educational quality, educators’ capacities, and sustainability, benefiting long-term education and clinical outcomes in health care.
1 Introduction
In recent years, the concept of New Medical Sciences has emerged as a transformative initiative in medical education, aiming to align healthcare training with the demands of modern medicine, scientific innovation, and interdisciplinary integration. Against this backdrop, Medical Simulation Centers have emerged as essential platforms for bridging the gap between theoretical education and practical clinical training. Traditional medical education often relies on real patient interactions, but with the increasing number of students, ethical concerns, and limited patient availability, it has become imperative to adopt alternative teaching methods. Simulation-based learning enables medical students to develop critical skills in a controlled environment, improving their confidence and clinical decision-making abilities before transitioning to real-world settings (1, 2). Additionally, competency-based medical education (CBME) frameworks increasingly integrate simulation-based training to provide structured, measurable learning experiences (3).
Despite its advantages, the establishment and operation of Medical Simulation Centers face several challenges. Many institutions struggle with inadequate funding, a lack of trained faculty, and inconsistent integration of simulation-based learning into the curriculum. Studies have shown that while some well-funded institutions possess state-of-the-art simulation facilities, these resources are often underutilized due to scheduling inefficiencies and insufficient faculty training (4, 5). Furthermore, disparities in Medical Simulation Center access across different medical schools raise concerns about the equitable distribution of high-quality clinical training (6). Addressing these challenges requires a strategic approach to Medical Simulation Center management, including investment in faculty development, resource allocation, and curriculum integration.
This manuscript explores the significance of Medical Simulation Centers and the challenges associated with their development. Drawing from the experience of Fujian Medical University, we propose strategies for optimizing Medical Simulation Center construction, including strengthening infrastructure, implementing effective management systems, and incorporating simulation-based learning into medical education. By addressing these issues, institutions can enhance the quality of medical education, improve clinical competency among students, and ultimately contribute to better patient care outcomes.
Recent research has identified that training using simulations serves a significant purpose of connecting educational theory with clinical competency transfer, providing an opportunity for skill standardization and professional preparation development (7–9).
However, there is a gap in strategic and systematic models regarding the construction and management of Medical Simulation Centers in the context of New Medical Sciences in China.
Thus, this paper contributes a grounded optimized institutional model based on Fujian Medical University’s experience to incorporate an enterprise of infrastructure, faculty policy, and curricular innovation into improving the sustainability and quality of Medical Simulation Centers.
2 Materials and methods
This research utilized a descriptive institutional design grounded in the practical experiences of Fujian Medical University’s Medical Simulation Center, which is envisioned to become a model under the New Medical Science framework. The research aimed to explore the processes, approaches, and challenges to developing and improving a modern Medical Simulation Center. This study investigated and contributed to developing and improving a sustainable simulation-based education center by examining the structural, management, and learning perspectives that underpin a Medical Simulation Center and whether a combination of infrastructure, faculty development, and curricular alignment improves the quality of medical education (10, 11).
2.1 Study settings and data sources
The study setting and data sources were developed based on institutional documents of Fujian Medical University maintained through official means for the years 2020–2024. Data sources included institutional teaching and training reports for each academic year, documentation of simulation session reports, faculty development documentation and records, and construction and management documentation of the Medical Simulation Center. Additional supporting documentation was also acquired, which included quality-assurance reports, documentary assessments of student assessments and performance, and assessments of clinical skills. These documents provided a rich source of institutional data for exploring the development, intent, and outcomes of research-based on the Medical Simulation Center in medical education (12–14).
2.2 Analysis process
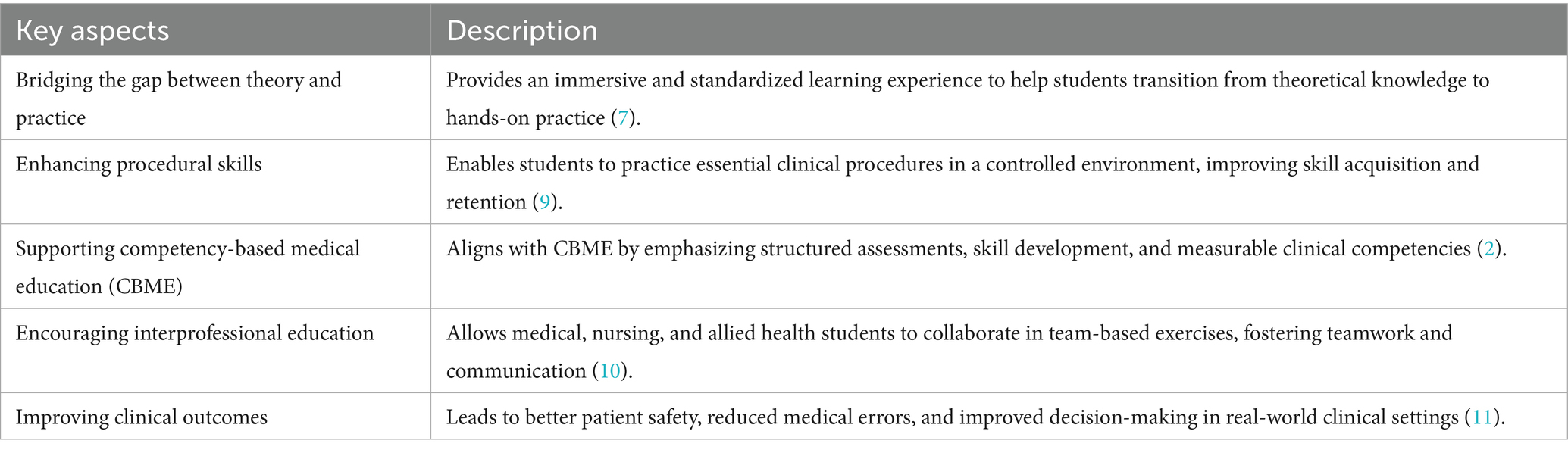
A qualitative narrative synthesis was used for analysis of the institution documents. The narrative synthesis was necessary as it allows for the triangulation of quantitative indicators (e.g., number of simulations or hours of faculty training) with qualitative indicators (e.g., commentaries, policy, reports, or evaluations) into terms. The narrative synthesis intended to elicit significant themes and effective practices relating to infrastructure development, faculty capacity building, curricular alignment, and evaluation systems. The outcomes of thematic analysis of documents are reconstructed in Table 1, with recommendations related to key aspects and educational value of the research Medical Simulation Center that emerged from the study. Using iterative reading techniques and clumping techniques upon themes, effective practices gleaned from the Fujian Medical University model effectively practices, and participating concepts of consensus and widely held international commentary on a framework for medical education, effective practice (15, 16).
2.3 Conceptual and theoretical framework
The analysis framework provided in the study drew from previous work undertaken as part of the study of Saratila et al. (17) and Romancenco et al. (33); the work found refers to the notion of simulation-based education being an opportunity to enhance the transfer of clinical competencies and to bring together theory-based content and practical applications. These frameworks were claimed and conceptually located in Competency-Based Medical Education (CBME), which outlines measurable outcomes, structured assessment, and the progressive nature of skill acquisition and assessment. The analytical process made sense of institutional reports and commentary into four categories of infrastructure and resources, faculty training and professional development, curricular alignments, and quality assurance networks. The analysis phenomena adhered to the original purpose of current best practices, while ensuring a sound conceptual analysis of the study within CBME (18–22).
2.4 Ethical considerations
No human or animal subjects participate in this study. All data were harvested from research-based documents held at Fujian Medical University, which did not compromise the confidentiality of participating human subjects, nor did the documents constitute any identifiable information about individuals used as data sources. This study did not contrive formal ethics committee recommendations; consequently, all facets of the process of data collection and analysis adhered to policies of the Fujian Medical University and Chinese national guidelines for transparency in educational research and confidentiality of research projects (23, 24).
3 Results
3.1 Achievements of the Medical Simulation Center
Between 2020 and 2024, the Medical Simulation Center at Fujian Medical University reached several significant milestones to advance simulation-based education. During this time, the number of simulation-based training labs increased from 8 to 14 in key areas, including emergency medicine, surgical skills, obstetrics and gynecology, and nursing. Regarding utilization, the increase in student participation grew from about 1,200 to more than 2,800 students per year, a growth of 133%. Additionally, the summers of 2023 include a successful institutional accreditation from the Fujian Provincial Department of Education, which recognized it as a program of best practices using competency-based medical education. In the summer of 2024, the center coordinated formal agreements with 2 regional teaching hospitals to begin to standardize simulation curriculum for clinical students to ensure equitable exposure (10–12).
3.2 Outcomes of training and student feedback
The systematic implementation of simulation training has resulted in measurable increases in student performance and satisfaction. Institutional data indicated that students who participated in at least three modules improved Objective Structured Clinical Examination (OSCE) scores between 15 and 20% above baseline scores (13, 14). Faculty also commented on an observable increase in accuracy when completing procedures, and also noted a reduction in demonstrating common technical errors during clinical placements. In more depth, for example, student satisfaction surveys (n = 650) collected in the summer of 2023–2024 indicated 94.3% of the students agreed that simulation helped students feel more confident in their skills, and 89.6% of students improved in timing and team communication after simulation training. After the internal “Simulation Instructor Development Program” was implemented, faculty involvement increased by 45% demonstrating greater institutional capacity (15, 16, 18).
3.3 Technology and innovations
To increase realism and learner engagement, the Medical Simulation Center has added digital tools that utilize the latest technology. This includes high-fidelity manikins for critical care training, virtual-reality (VR)-assisted surgical modules, and AI-assisted learning performance tracking systems. In addition to the educational residency program, more than one-third of simulation sessions involved the use of VR and AI by 2024, which adhered to worldwide standards for adaptive learning and learners’ personal skills assessment (19, 20). Student comments confirmed that technology was effective in enhancing engagement and scenario recall by over 30 % compared to non-electronic learning experiences.
3.4 Accreditation and quality assurance
To ensure consistency in evaluations of students, the institution adopted standardized evaluation tools, including OSCEs, Direct Observation of Procedural Skills (DOPS), and structured debriefing protocols. Accreditation requirements were aligned with standards established by the Society for Simulation in Healthcare (SSH) and the International Nursing Association for Clinical Simulation and Learning (INACSL) to ensure a worldwide perspective and authority of credibility.
Between the years of 2021 through 2024, the institution performed annual internal audits, and over 90% compliance was achieved to establish safety and scenario integrity, as well as learning evaluations (21–23).
3.5 Interprofessional and collaborative training
Interprofessional education (IPE) was achieved, and all curricular elements embrace collaborative activities where medical students and the school of nursing and pharmacy, and rehabilitation science education programs are represented. From 2022, the institution implemented team-based simulation sessions focused on scenarios of emergency response, perioperative collaboration, and patient communication.
Survey data demonstrated that 92% of respondents reported increased interprofessional understanding, and team performance during simulation multi-role scores increased by, on average, 18%. All evidence suggested that the Model was capable of strengthening teamwork and reducing team variability across professions (24–26).
3.6 Scalability and sustainability
To better ensure continued sustainability, in 2024, the center established a “shared-resource consortium” with three partnered teaching institutions providing risk-shared access to the simulator and educator resources. This consortium decreased the relative costs of simulator learning by approximately 28% per student while increasing accessibility of simulation learning experiences in rural teaching sites.
The educators also established the “Train-the-Trainer” program with the primary purpose of expanding the number of qualified instructors from 15 to 29 certified simulation educators within 2 years. As a result of the shared-resource consortium and the train-the-train program, the simulation program was established to promote ongoing maintenance and expansion for both education and clinical contexts.
The combination of long-term budget and financial planning and agreements to share resources elevates the Fujian Medical University Medical Simulation Center into a scalable and replicable model for medical education reform.
3.7 Medical Simulation Center achievements
The center successfully obtained institutional accreditation from the Fujian Provincial Department of Education in 2023, recognizing it as a model for competency-based medical education. In 2024, the center-initiated a collaboration with two regional teaching hospitals to standardize simulation curricula, ensuring consistent exposure for clinical students (10–12). A summary of key institutional outcomes from 2020 to 2024 is presented in Table 2.
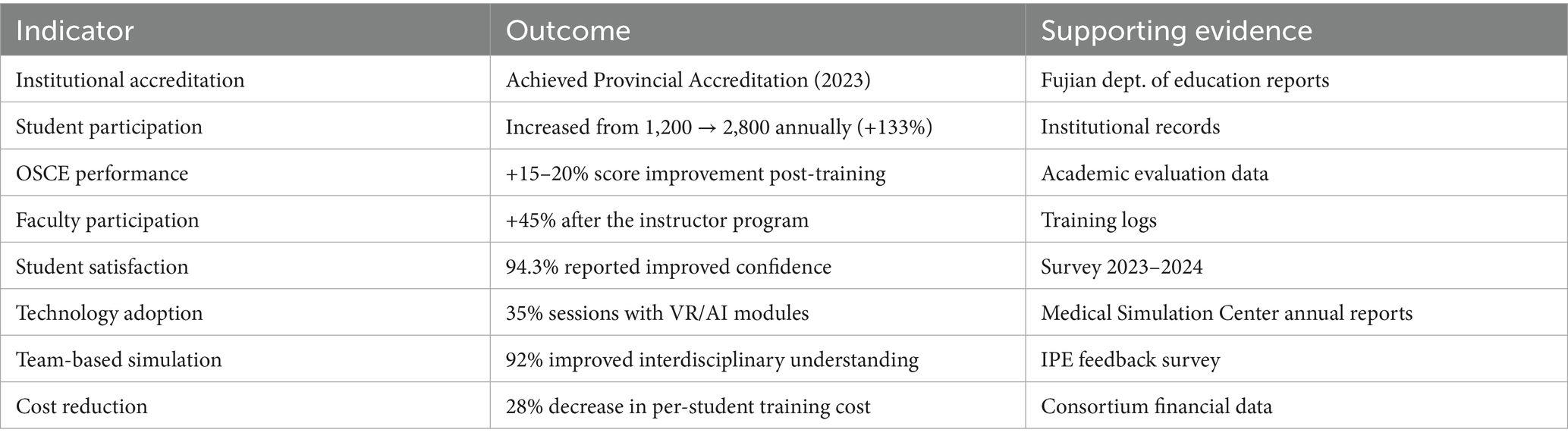
Table 2. Summary of key outcomes from the Fujian Medical University Medical Simulation Center (2020–2024).
4 Discussion
This article provides a detailed descriptive evaluation of Fujian Medical University’s Medical Simulation Center as a case of a simulation-based learning model incorporated into medical education through the New Medical Sciences perspective. The results illustrated the effectiveness of leveraging investment in infrastructure, faculty development, and curriculum innovation to enhance learner engagement and program sustainability.
4.1 Comparing with the literature
This study’s findings correlate well with the current literature available on simulation-based medical education. Saratila et al. (17) discussed that simulation-based learning results in significantly improved skill transfer and decision-making, which absolutely correlates with improvements in performance on the OSCE and with the student satisfaction measured in this study. Romancenco et al. (33) also highlighted faculty training and standardizing training scenarios as key ingredients to the quality of simulation programs, which was observed in this study as the model made incredible approaches through the “Simulation Instructor Development Program.” Furthermore, the reference to sustainability and interprofessional learning expands the work of Romancenco et al. (33), who suggested inter-institutional partnerships and shared resources to promote efficiency and sustainability for longer periods. By introducing a consortium framework, the model demonstrated how Fujian Medical University is utilizing partnerships in the region to maximize resources while taking care to maintain the quality of training (24–26).
On the other hand, the current study distinctly discusses the institutional management aspects, or administration, in utilizing alignment and ongoing quality checks to strengthen the effectiveness of learning.5.2 Implications for Institutions.
The Fujian model offers a replicable approach to Medical Simulation Centers, especially for medical schools in underdeveloped or resource-limited environments. Its integrated framework—across infrastructure, faculty, and curriculum—represents a well-balanced model for the institution that seeks to adopt competency-based medical education (CBME).
The findings demonstrate that ongoing faculty development, structured evaluation, and interprofessional training are all important to creating practice-ready outcomes for graduates. Evaluation systems that integrated accreditation required assessments suggested a shift from simulation being just a form of teaching, but now it has developed into the institution’s strategic asset.
Additionally, achieved 28% cost savings of the consortium model and generated enough certified educators, suggesting that institutional growth is sustainable without sacrificing educational quality, and provides a scale model (18, 27).
4.2 Limitations
There are limitations to this study despite its strengths. It was a single-center descriptive study, rather than multi-center comparative work, reliant on reports at the institution rather than comparative multi-center data. Therefore, while the findings give insight into structural and pedagogical effectiveness, the findings apply to the local context and need to be interpreted with caution.
The study lacked a longitudinal cohort for validating outcome measures for extending outcomes from simulation training into clinical practice.
Finally, the data in this study were primarily descriptive; theoretical performance was limited to fractionating and statistical summarizing, and future research aims should incorporate mixed methods or quasi-experimental designs to clarify or develop stronger causal links (17, 28, 29).
4.3 Future directions
Novel technologies, such as virtual reality (VR) or artificial intelligence (AI), and tele-simulation, are changing medical education in a global context. Implementation of these modalities can support educational experiences by enhancing realism, differentially adapting training levels while maintaining forward progress, and extending access to remotely located learners.
In a Fujian context, implementation of performance analytics could further individualize simulation learning based on overall performance trends, and tele-simulation could create space for inter-campus center training across entities (7, 30–32).
In the future, as education evolves, simulation-based learning will establish a back-and-forth relationship between technological technology and pedagogical integrity. Institutions will still need to be learner-focused, making sure that simulation is a complement—not a substitute for clinical experience.
5 Conclusion
The establishment of a well-organized, faculty-led Medical Simulation Center enhances the outcomes of competency-based medical education. The experience from Fujian Medical University demonstrates that systematic faculty management, continuous professional development, and curricular integration are key strategies for achieving sustainable simulation-based training. This model provides a practical reference for institutions seeking to modernize medical education and strengthen clinical competence among learners.
Collaboration should continue to expand across multiple universities and disciplines, accompanied by the integration of innovative technologies such as virtual reality, artificial intelligence, and tele-simulation to further advance educational reform.
Future studies should evaluate the long-term impact of simulation-based training on graduates’ clinical competence and patient outcomes. Comparative and longitudinal analyses across institutions would help determine whether simulation exposure translates into improved clinical performance, safety practices, and sustained professional development. Such evidence will be critical for establishing national standards and policy frameworks that support competency-based medical education.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AZ: Writing – original draft, Investigation, Formal analysis, Methodology, Data curation. XC: Formal analysis, Writing – original draft, Data curation. QW: Writing – review & editing, Investigation. XL: Methodology, Writing – original draft. XP: Data curation, Writing – original draft. QY: Conceptualization, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Special Project Support for Higher Education Science Research Laboratory of Fujian Higher Education Association in 2022 (22FJSYZD006) and Graduate Education and Teaching Research Project of Fujian Medical University (Y23015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Campbell, KK, Wong, KE, Kerchberger, AM, Lysikowski, J, Scott, DJ, and Sulistio, MS. Simulation-based education in US undergraduate medical education: a descriptive study. Simul Healthc. (2023) 18:359–66. doi: 10.1097/SIH.0000000000000705
2. Archana, S, Nilakantam, SR, Hathur, B, and Dayananda, M. The need and art of establishing skill and medical medical simulation center s to strengthen skill-based medical education: learning insights and experience. Ann Afr Med. (2021) 20:247–54. doi: 10.4103/aam.aam_53_20
3. Griswold, S, Fralliccardi, A, Boulet, J, Moadel, T, Franzen, D, Auerbach, M, et al. Simulation-based education to ensure provider competency within the health care system. Acad Emerg Med. (2018) 25:168–76. doi: 10.1111/acem.13322
4. Pirie, J, Fayyaz, J, Gharib, M, Simone, L, Glanfield, C, and Kempinska, A. Development and implementation of a novel, mandatory competency-based medical education simulation program for pediatric emergency medicine faculty. Adv Simul. (2021) 6:17. doi: 10.1186/s41077-021-00170-4
5. Garofalo, M, and Aggarwal, R. Competency-based medical education and assessment of training: review of selected National Obstetrics and Gynaecology curricula. J Obstet Gynaecol Can. (2017) 39:534–44.e1. doi: 10.1016/j.jogc.2017.01.024
6. Chacko, TV. Simulation-based medical education: using best practices and curriculum mapping to maximize educational benefits in the context of shift toward competency-based medical education. Arch Med Health Sci. (2017) 5:9–15. doi: 10.4103/2321-4848.208217
7. Elendu, C, Amaechi, DC, Okatta, AU, Amaechi, EC, Elendu, TC, Ezeh, CP, et al. The impact of simulation-based training in medical education: a review. Medicine. (2024) 103:e38813. doi: 10.1097/MD.0000000000038813
8. Daneshfar, M, and Moonaghi, HK. The impact of clinical simulation on bridging the theory-practice gap in nursing education: a systematic review. BMC Med Educ. (2025) 25:1216. doi: 10.1186/s12909-025-07790-8
9. Saragih, ID, Suarilah, I, Hsiao, CT, Fann, WC, and Lee, BO. Interdisciplinary simulation-based teaching and learning for healthcare professionals: a systematic review and meta-analysis of randomized controlled trials. Nurse Educ Pract. (2024) 76:103920. doi: 10.1016/j.nepr.2024.103920
10. Wu, Z, Huang, Y, Lyu, L, Huang, Y, and Ping, F. The efficacy of simulation-based learning versus non-simulation-based learning in endocrinology education: a systematic review and meta-analysis. BMC Med Educ. (2024) 24:1069. doi: 10.1186/s12909-024-06010-z
11. AlHaqwi, AI, and Taha, WS. Promoting excellence in teaching and learning in clinical education. J Taibah Univ Med Sci. (2015) 10:97–101. doi: 10.1016/j.jtumed.2015.02.005
12. Alharbi, A, Nurfianti, A, Mullen, RF, McClure, JD, and Miller, WH. The effectiveness of simulation-based learning (SBL) on students’ knowledge and skills in nursing programs: a systematic review. BMC Med Educ. (2024) 24:1099. doi: 10.1186/s12909-024-06080-z
13. Yu, H, Zhao, J, Su, L, and Zhang, J. Application of simulation-based education in the instruction of medical students from non-radiology specialties. BMC Med Educ. (2025) 25:966. doi: 10.1186/s12909-025-07572-2
14. Lateef, F, Suppiah, M, Chandra, S, Yi, TX, Darmawan, W, Peckler, B, et al. Medical simulation center s and simulation-based education during the time of COVID 19: a multi-center best practice position paper by the World Academic Council of Emergency Medicine. J Emerg Trauma Shock. (2021) 14:3–13. doi: 10.4103/JETS.JETS_185_20
15. Kothari, LG, Shah, K, and Barach, P. Simulation based medical education in graduate medical education training and assessment programs. Prog Pediatr Cardiol. (2017) 44:33–42. doi: 10.1016/j.ppedcard.2017.02.001
16. Kumar, EJS, Parameswari, A, Manickam, A, and Purva, M. Establishment of a simulation Centre: challenges and solutions. Indian J Anaesth. (2024) 68:45–51. doi: 10.4103/ija.ija_1232_23
17. Saratila, I, Romancenco, A, and Spinei, L. Evaluating the efficacy of simulation-based training on clinical competency transfer. One Health Risk Manag. (2024) 5:21–32. doi: 10.38045/ohrm.2024.3.03
18. Diaz-Navarro, C, Armstrong, R, Charnetski, M, Freeman, KJ, Koh, S, Reedy, G, et al. Global consensus statement on simulation-based practice in healthcare. Adv Simul. (2024) 9:19. doi: 10.1186/s41077-024-00288-1
19. Gómez-Pérez, V, Escrivá Peiró, D, Sancho-Cantus, D, and Casaña Mohedo, J. In situ simulation: a strategy to restore patient safety in intensive care units after the COVID-19 pandemic? Systematic review. Healthcare. (2023) 11:263. doi: 10.3390/healthcare11020263
20. Chernogorova, Y, Zanev, A, and Grancharov, D. Systematizing strategies to overcome challenges in medical simulation center management. Pol J Manag Stud. (2024) 30:75–90. doi: 10.17512/pjms.2024.30.2.05
21. Leiphrakpam, PD, Armijo, PR, and Are, C. Incorporation of simulation in graduate medical education: historical perspectives, current status, and future directions. J Med Educat Curri Develop. (2024) 11:7329. doi: 10.1177/23821205241257329
22. Nagarajappa, A, and Kaur, S. Simulation in contemporary medical education: current practices and the way forward. Indian J Anaesth. (2024) 68:17–23. doi: 10.4103/ija.ija_1203_23
23. Dow, AW, Salas, E, and Mazmanian, PE. Improving quality in Systems of Care: solving complicated challenges with simulation-based continuing professional development. J Contin Educ Health Prof. (2012) 32:230–5. doi: 10.1002/chp.21150
24. Gardner, AK, Ritter, EM, Dunkin, BJ, Smink, DS, Lau, JN, Paige, JT, et al. Leaders by example: best practices and advice on establishing a state-of-the art surgical medical medical simulation center that optimizes available resources. Am J Surg. (2018) 215:259–65. doi: 10.1016/j.amjsurg.2017.11.007
25. Sittner, BJ, Aebersold, ML, Paige, JB, Graham, LLM, Schram, AP, Decker, SI, et al. INACSL standards of best practice for simulation: past, present, and future. Nurs Educ Perspect. (2015) 36:294–8. doi: 10.5480/15-1670
26. Cooke, JM, Rooney, DM, Fernandez, GL, and Farley, DR. Medical medical simulation center best practices: a review of ACS-accredited educational institutes' best practices, 2011 to present. Surgery. (2018) 163:916–20. doi: 10.1016/j.surg.2017.11.004
27. Khan, M, and Sasso, RA. Obtaining medical medical medical simulation center accreditation. Treasure Island, FL: StatPearls Publishing (2023).
28. Svendsen, BT, Petersen, LF, Skjelsager, A, Lippert, A, and Østergaard, D. Using simulation scenarios and a debriefing structure to promote feedback skills among interprofessional team members in clinical practice. Adv Simul. (2024) 9:39. doi: 10.1186/s41077-024-00303-5
29. Salahuddin, MF. Bridging theory and practice: enhancing pharmacology education through simulation-based learning and statistical analysis training. Curr Pharm Teach Learn. (2025) 17:102440. doi: 10.1016/j.cptl.2025.102440
30. Cristina, DN, Robert, A, Matthew, C, Kirsty, FJ, Sabrina, K, Gabriel, R, et al. Global consensus statement on simulation-based practice in healthcare. Simul Healthc. (2024) 19:e52–9. doi: 10.1097/SIH.0000000000000804
31. Thim, S, Henriksen, TB, Laursen, H, Schram, AL, Paltved, C, and Lindhard, MS. Simulation-based emergency team training in pediatrics: a systematic review. Pediatrics. (2022) 149:e2021054305. doi: 10.1542/peds.2021-054305
32. McCarrick, CA, Moynihan, A, Khan, MF, Lennon, F, Stokes, M, Donnelly, S, et al. Impact of simulation training on core skill competency of undergraduate medical students. J Surg Educ. (2024) 81:1222–8. doi: 10.1016/j.jsurg.2024.06.006
Keywords: medical simulation, competency-based education, simulation-based learning, healthcare training, objective structured clinical examination
Citation: Zeng A, Chen X, Wu Q, Lin X, Peng X and Ye Q (2025) Exploration and practice of Medical Simulation Center construction under the background of New Medical Sciences. Front. Public Health. 13:1619348. doi: 10.3389/fpubh.2025.1619348
Edited by:
Shaidah Jusoh, Xiamen University, MalaysiaReviewed by:
Katarzyna Tomaszewska, Państwowa Akademia Nauk Stosowanych im. ks. B. Markiewicza w Jarosławiu, PolandLarisa Spinei, Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova, Moldova
Copyright © 2025 Zeng, Chen, Wu, Lin, Peng and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qinyong Ye, eWVxaW55b25nMGFAMTYzLmNvbQ==
 Aiying Zeng1
Aiying Zeng1 Qinyong Ye
Qinyong Ye