- 1Institute of Developmental Psychology, Beijing Normal University, Beijing, China
- 2Affiliated Mental Health Center and Hangzhou Seventh Peoples Hospital, Zhejiang University School of Medicine, Zhejiang, China
- 3Department of Health Sciences, College of Health and Rehabilitation Sciences, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
- 4Beijing Key Laboratory of Applied Experimental Psychology, Faculty of Psychology, Beijing Normal University, Beijing, China
Background: Infant mortality remains a critical public health concern, necessitating a comprehensive understanding of its determinants. This investigation aimed to examine associations between social determinants, lifestyle factors, and maternal mental health in relation to infant mortality.
Methods: A cross-sectional survey was conducted among 500 mothers (250 rural, 250 urban) in Khyber Pakhtunkhwa (KPK), Pakistan. The Depression Anxiety Stress Scales (DASS-21) were employed to evaluate symptoms of anxiety, depression, and stress, while a Lifestyle and Habits Questionnaire collected data on physical activity and dietary patterns. Data was collected via questionnaires and demographic information from 500 mothers using purposive sampling. Key variables included rural/urban residence, age at marriage, socio-economic status, access to healthcare, type of delivery attendant, and under-5 mortality rates.
Results: Rural mothers had significantly lower infant mortality rates (p = 0.000) compared to urban mothers. Physical activity and diet were negatively correlated with depression, anxiety, and stress (p < 0.05). Rural mothers reported higher physical activity (M = 23.46 vs. 21.79, p = 0.001) and healthier diets (M = 16.01 vs. 14.85, p = 0.001). Urban mothers exhibited significantly higher levels of depression (M = 6.59 vs. 1.63, p = 0.000), anxiety (M = 7.68 vs. 2.18, p = 0.000), and stress (M = 9.65 vs. 2.32, p = 0.000). Early marriage was linked to increased anxiety and stress (p = 0.000).
Conclusion: Findings underscored the importance of addressing social determinants and fostering healthy lifestyles to improve maternal and child health outcomes. Interventions that promote access to healthcare, physical activity or healthy dietary habits can help make the infant mortality rates and the overall state of health of the mother better.
Background
Infant death refers to the death of children under the age of one year and remains a key socioeconomic development indicator. UNICEF (1) reported 4.9 million child deaths, with most being infants. These are largely preventable and linked to nutrition, maternal education, essential services, and health inequalities. Globally, 90% of infant deaths occur in low- and middle-income countries where poverty and poor health infrastructure dominate (2). In South Asia, Pakistan ranks among the highest with 57 deaths per 1,000 live births, despite policy interventions (1), highlighting the need to study social factors influencing mortality.
Determinants where people are born and live like socioeconomic, environmental, cultural, income, education, and healthcare access are critical (3, 4). Poverty and low maternal education consistently predict higher mortality (5–7). Infants of uneducated mothers face greater death risk than those with educated mothers (8). Inequalities are not limited to developing nations; in the U.S., African-American newborns have higher mortality due to racialized healthcare, income gaps, and neighborhood deprivation (9–11).
Urban–rural divides remain persistent. Rural areas lack trained attendants and facilities, forcing reliance on traditional birth attendants (12, 13). Urban settings, despite better access, face overcrowding, pollution, and poor sanitation (14). In Pakistan, mountainous terrain, marginalization, and tribal norms cause delays in care, poor rural staffing, and fatal complications (15–17). Urban slums mirror many rural disadvantages (14, 18).
Maternal lifestyle is also crucial. Prenatal physical activity reduces preterm births, low birth weight, and gestational diabetes, with meta-analyses showing a 15–30% reduction in adverse outcomes (19, 20). Yet cultural barriers, safety concerns, and misconceptions restrict activity in Pakistan (21–24). Antenatal education promoting safe activity could improve outcomes. Nutrition is equally vital. Undernutrition contributes to intrauterine growth restriction, anemia, and LBW (25, 26). Over 40% of Pakistani pregnant women are anemic, and one in five underweight (27, 28). Food insecurity reduces antenatal care and nutrition counseling (29, 30). Diet diversity and supplementation with iron and folic acid remain essential (31).
Maternal mental health is a significant but often neglected determinant. Stress, anxiety, and depression predict preterm birth, poor postnatal care, and LBW (32, 33). Untreated illnesses reduce visits, breastfeeding, and bonding (34). In Pakistan, stigma and lack of services lead to underdiagnosed perinatal depression, particularly in rural areas (35). Such mothers often lack emotional support, nutrition, and antenatal care, with long-term cognitive and emotional risks for infants (36).
In Khyber Pakhtunkhwa (KPK), early marriages and adolescent childbirth pose risks including obstructed labor, hemorrhage, LBW, and infant mortality (37, 38). Girls married under 18 face reduced education, limited autonomy, and poor reproductive health access (39, 40). Nearly one-third in rural Pakistan marry before 18, worsening malnutrition and neonatal complications (41, 42). Addressing this requires legal enforcement, education, and culturally adapted outreach.
Existing studies document national determinants: disparities in Punjab (43), cultural impacts in Sindh (44), and links between maternal education, income, and outcomes (45). However, literature on KPK is scarce, despite its unique cultural practices and geographical barriers. This study therefore investigates how social determinants like maternal mental health, physical activity, and dietary patterns shape infant survival in rural and urban KPK.
Conceptual framework: web of causation
Methods
Research design
The current study was correlational and cross-sectional in nature utilizing questionnaire survey targeting mothers residing in rural and urban areas of Khyber Pakhtunkhwa (KPK), Pakistan. KPK was chosen as the study location due to its distinct socio-economic, geographical, and cultural characteristics, as well as the region’s historically elevated rates of infant mortality. The study period spanned from February 15, 2024, to September 1, 2024. This design was chosen to explore potential associations between maternal lifestyle factors, mental health, and infant mortality outcomes across different settings (Figure 1).
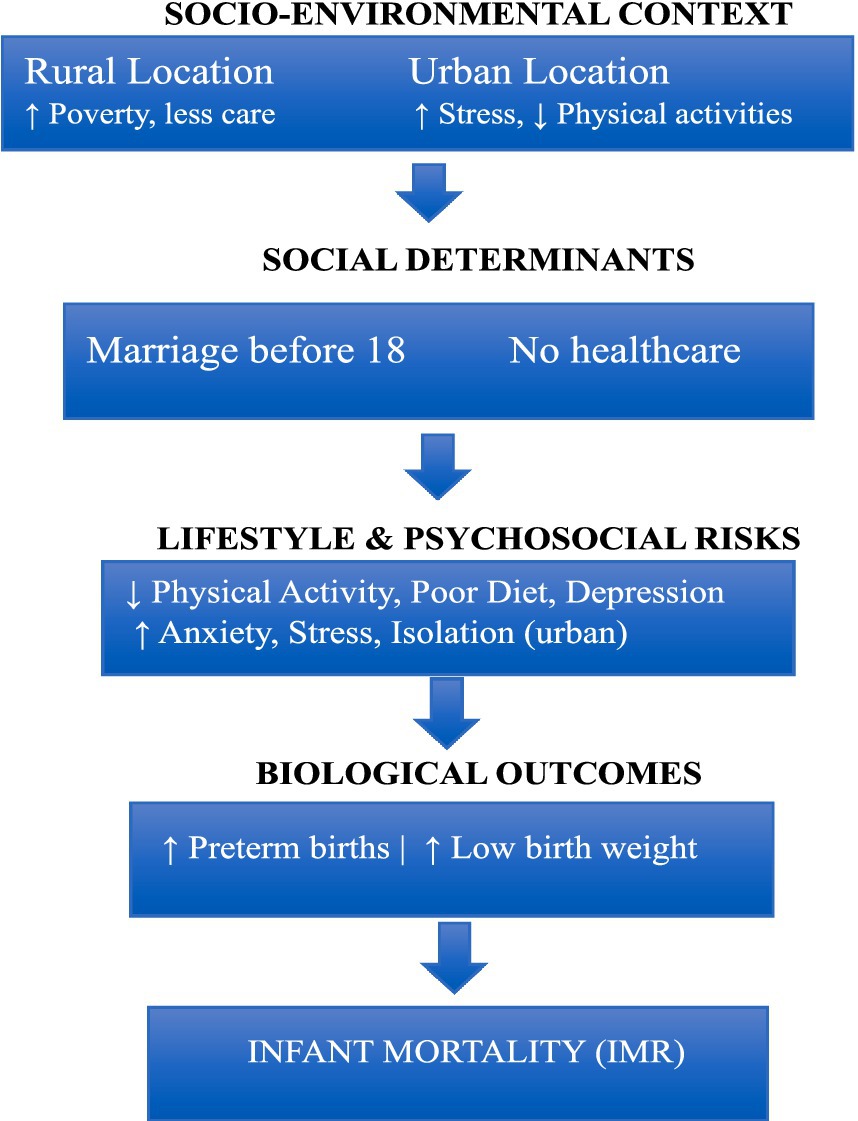
Figure 1. Web of causation model for infant mortality in rural and urban Pakistan (43).
Population
In the study ethical guidelines were strictly adhered to, with approval obtained from the Institutional Ethics Review Board. Informed consent was collected from all participants, and confidentiality was maintained by anonymizing responses and securely storing all data to ensure privacy throughout the study. The population was mothers of rural and urban areas who had experienced infant mortality. There were 500 samples chosen via purposive sampling techniques from rural and urban areas with 250 from rural and 250 from urban areas. The inclusion criteria were mothers from rural and urban areas, mothers married before or after the age of 18 years, and participants who voluntarily agreed to participate and provide informed consent. The exclusion criteria were, excludes mothers who have had stillbirths or no live births, excludes mothers with severe uncontrolled medical conditions or psychiatric disorders. Excludes mothers who do not comply with study protocols or refuse participation and exclude participants with missing data on key variables (e.g., neonatal deaths, SES, delivery, healthcare access).
Instruments
Demographic sheet
Demographic information contains age, area, marriage before 18 years, Socioeconomic status (lower, middle & Higher), access to health care, attendant, delivery at home or hospital, number of neonatal deaths, and under 5 mortalities. Socioeconomic status was assessed using income categories outlined in a Dawn newspaper report dated April 2, 2024: 4,000–20,000 PKR as lower, 50,000–100,000 PKR as middle, and above as upper class (44).
Depression Anxiety Stress Scale (DASS)
The Depression Anxiety Stress Scales (DASS-21) is a popular self-report tool for gauging the intensity of depressive, anxious, and stress-related symptoms experienced in the previous seven days. The Depression Anxiety Stress Scale (DASS-21) was created by Lovibond and Lovibond and has a Cronbach Alpha of 0.91 for Depression, 0.81 for Anxiety, and 0.89 for Stress (45). It is a valid and efficient way to measure emotional discomfort in these three areas.
The lifestyle and habits questionnaire-B (LHQ-B)
It was developed by Dinzeo et al. (46), which has 42-items with 5-points response range strongly disagree to strongly agree. It has 8 subscales, but we used only physical activity and diet with Cronbach Alpha ranging from 0.65 to 0.91.
Statistical analysis
Statistical methods, chi-square tests were used to examine whether there is a significant association or difference between variables and for comparison. t-tests were used to compare the means (averages) of two groups to see if they are significantly different from each other. These tests were used to analyze the relationships between socio-economic factors, physical activity, diet, and mental health.
Results
The current study tended to explore social determinants of infant mortality and compared rural and urban mothers. The results generated and tabulated are given below.
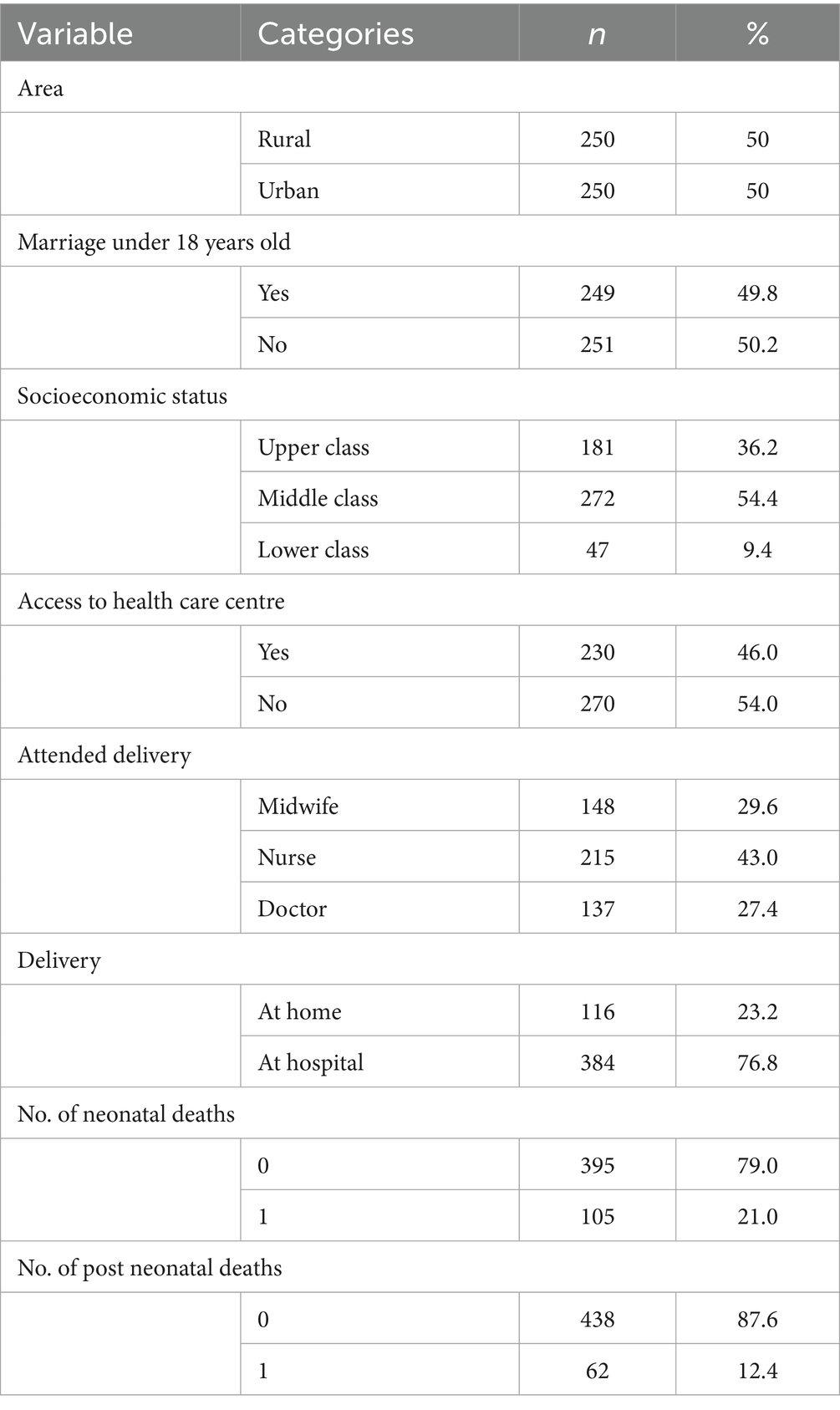
Table 1 presents the characteristics of 500 mothers from Khyber Pakhtunkhwa, with a balanced representation from rural and urban areas. Key findings include a high percentage of young mothers married before the age of 18 (49.8%) and a clear trend toward middle-class socioeconomic status (54.4%) among the participants. Access to healthcare centers was notably low, with 54% of the participants reporting limited access. The majority of deliveries took place in hospitals (76.8%), and neonatal mortality was relatively low, with 79% of mothers reporting no neonatal deaths. These findings underscore the importance of healthcare access and early medical intervention in reducing infant mortality rates (Table 2).
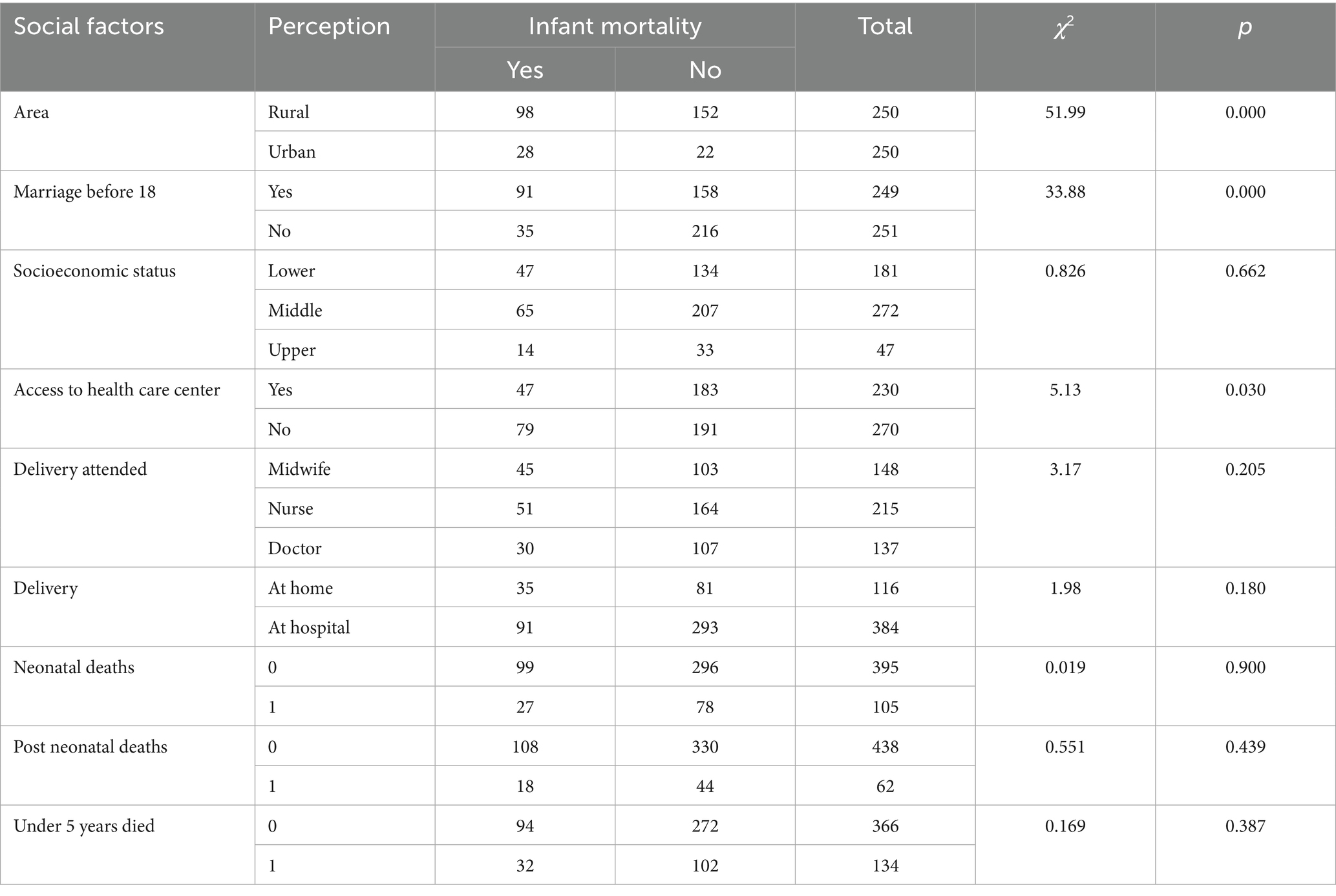
The analysis of social determinants of infant mortality revealed significant associations with certain factors. Areas with rural populations showed significantly higher rates of infant mortality compared to urban areas (χ2 = 51.99, p = 0.000). Additionally, early marriage (before 18 years) was linked to a higher incidence of infant mortality (χ2 = 33.88, p = 0.000), and lack of access to health care centers also contributed to higher mortality rates (χ2 = 5.13, p = 0.030). On the other hand, no significant associations were found for other social determinants. Socioeconomic status did not appear to affect infant mortality (χ2 = 0.826, p = 0.662), and the type of birth attendant (midwife, nurse, or doctor) showed no significant difference in mortality rates (χ2 = 3.17, p = 0.205). Delivery location (home or hospital), neonatal deaths, post-neonatal deaths, and under-5-year deaths were also not significantly associated with infant mortality, as indicated by their respective p-values (all > 0.05).
Table 3 presents Pearson correlation coefficients exploring the relationships between lifestyle factors (physical activity and diet) and mental health outcomes (depression, anxiety, and stress) among rural and urban mothers (n = 500). A statistically significant negative correlation was found between physical activity and depression (r = −0.149, p < 0.01), anxiety (r = −0.146, p < 0.01), and stress (r = −0.135, p < 0.05), indicating that higher levels of physical activity are associated with lower levels of psychological distress. Similarly, diet was negatively correlated with depression (r = −0.139, p < 0.05), anxiety (r = −0.130, p < 0.05), and stress (r = −0.152, p < 0.01), suggesting that healthier dietary habits are linked to better mental health. Strong positive correlations were also observed among the mental health variables themselves: depression with anxiety (r = 0.660, p < 0.01), depression with stress (r = 0.623, p < 0.01), and anxiety with stress (r = 0.682, p < 0.01).
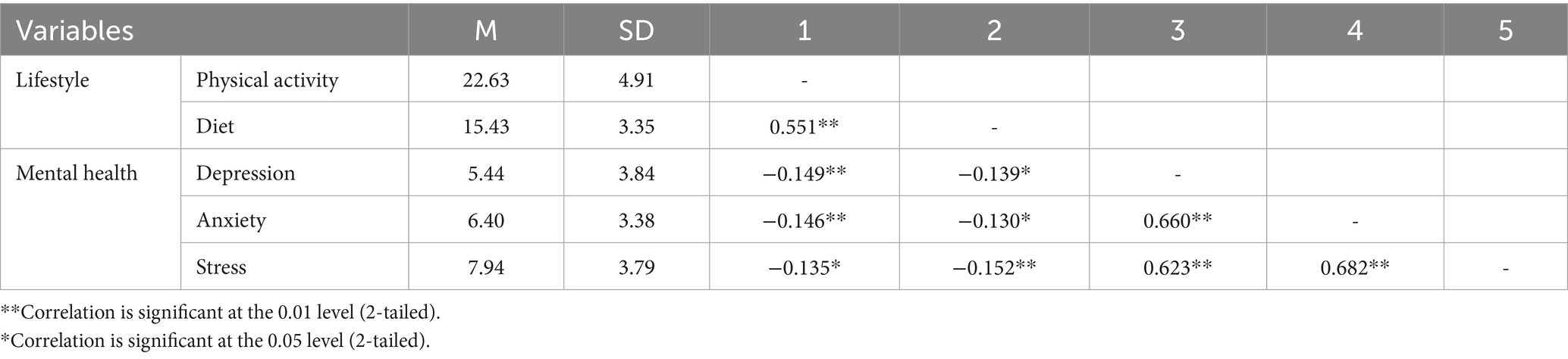
Table 3. Correlation among lifestyles (physical activity, diet), and mental health (depression, anxiety and stress) among rural and urban mothers (n = 500).
Table 4 shows rural mothers showed significantly better lifestyles compared to their urban counterparts. They engaged in more physical activity (M = 23.46 vs. 21.79, p = 0.001) and followed a healthier diet (M = 16.01 vs. 14.85, p = 0.001). These differences were statistically significant, indicating better lifestyle habits in rural areas. However, urban mothers reported significantly worse mental health outcomes. They experienced much higher levels of depression (M = 6.59 vs. 1.63, p = 0.000), anxiety (M = 7.68 vs. 2.18, p = 0.000), and stress (M = 9.65 vs. 2.32, p = 0.000) compared to rural mothers, with all differences being highly significant.
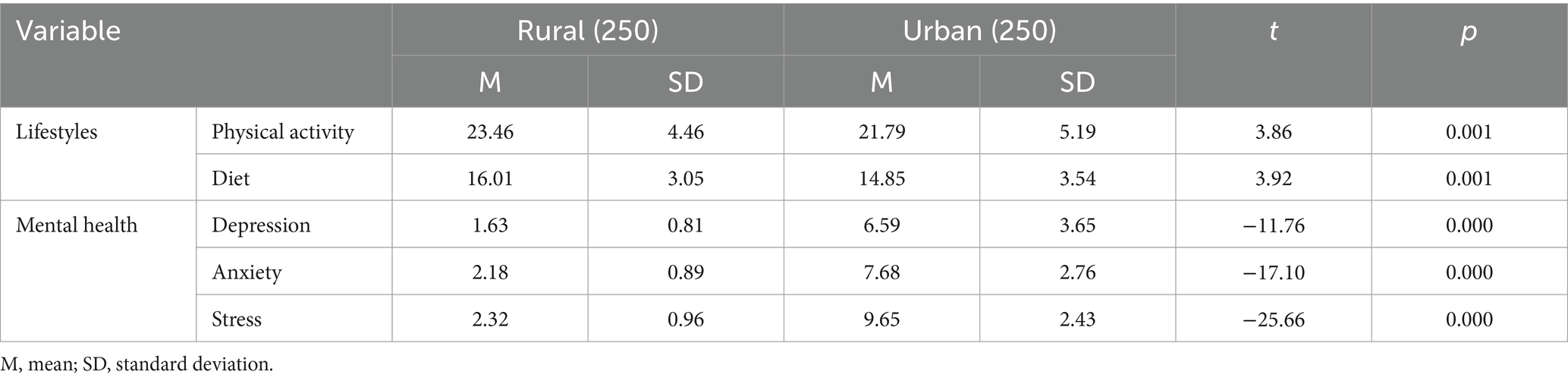
Table 4. Mean difference along area on lifestyles (physical activity, diet), and mental health (depression, anxiety and stress) among rural and urban mothers (n = 500).
Table 5 shows that mothers who married before 18 showed no significant differences in lifestyles like physical activity (M = 22.84 vs. 22.42, p = 0.72) and diet (M = 15.67 vs. 15.2, p = 0.25) and depression (M = 6.08 vs. 4.32, p = 0.13) compared to those who married later. However, significant differences were found in mental health, with those who married early reporting higher levels of anxiety (M = 7.14 vs. 5.12, p = 0.00) and stress (M = 8.87 vs. 6.32, p = 0.00).
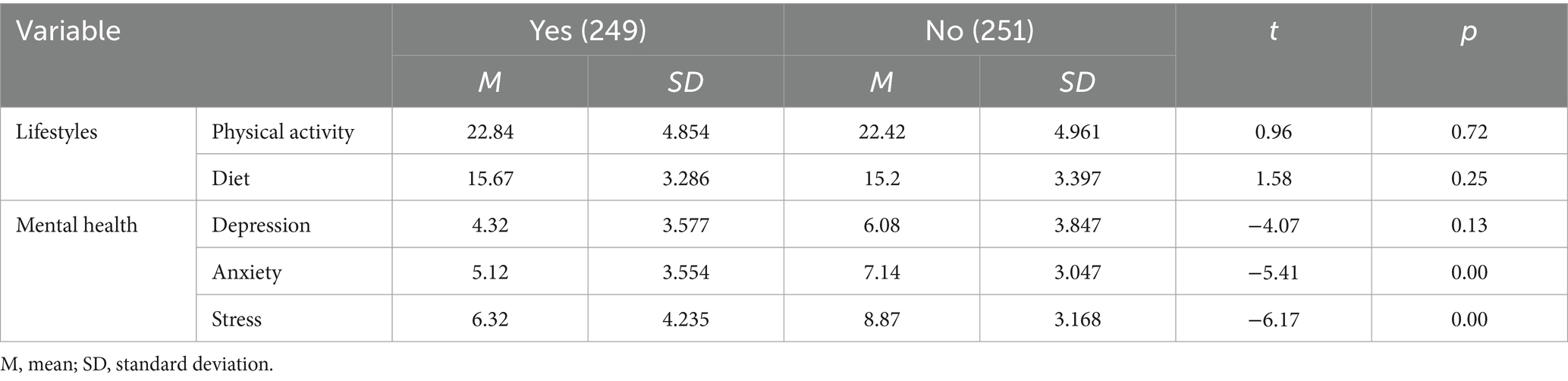
Table 5. Mean Difference along marriage before 18 on lifestyles (physical activity, diet), and mental health (depression, anxiety and stress) among rural and urban mothers (n = 500).
Discussion
In this study, the social determinants of infant mortality among rural and urban mothers were analyzed, focusing on factors such as physical activity, diet, and mental health. The result of the present study indicates that higher infant mortality tends to be correlated to rural residence and early marriage.
The descriptive data shown in Table 1 on neonatal and post-neonatal mortality is supported by recent studies emphasizing the importance of socioeconomic status, healthcare access, and delivery conditions. For instance, Izulla et al. (47) highlight that skilled birth attendance and facility delivery are critical in reducing neonatal mortality, aligning with the higher mortality rates observed for home births in the data. Similarly, Kibret (48) points out how socioeconomic disparities in healthcare access contribute to higher neonatal mortality. Additionally, Chauhan and Verma (49) confirm that skilled delivery significantly reduces neonatal and post-neonatal mortality in India. Ogbo et al. (50) also demonstrate that factors like maternal education and place of residence affect neonatal survival, with facility-based deliveries yielding better outcomes. Furthermore, Temporin (51) highlights how socioeconomic factors in Bolivia, including access to skilled birth attendants, contribute to better neonatal survival. These studies strengthen the findings from the descriptive data, indicating that socioeconomic inequalities and access to healthcare significantly impact neonatal and post-neonatal outcomes.
Our results revealed that Areas with rural populations showed significantly higher rates of infant mortality compared to urban areas (χ2 = 51.99, p = 0.000), supported by both international and Pakistani literature. Numerous studies support our findings presenting various reasons, i.e., limited access to maternal healthcare, poor infrastructure and lower literacy in rural areas. For example, limited access to skilled birth attendants in rural Ethiopia (52), studies in the United States (53, 54), and China (55, 56) consistently found that rural regions suffer from higher infant mortality due to socioeconomic disadvantages, inadequate healthcare access, and systemic inequities. These trends are echoed by Singh et al. (57), who highlighted growing disparities between Appalachia and more urban U.S. regions, and by Dagher and Linares (3), who stressed the impact of social determinants of health. However, evidence also indicates that targeted reforms can mitigate these disparities: Aidoo (58) reported reductions in mortality through community-based rural health interventions, while well-designed regional policies can significantly narrow the rural–urban mortality gap (59).
Additionally, adolescents who get married early have been found to have higher infant mortality rates due to teen pregnancy, less access to healthcare, and fewer opportunities for education due to being young mothers (60, 61). On the other hand, some studies have not demonstrated a connection between infant mortality ratios and delivery related risk factors or socio-economic status and suggest that other factors, such as age of mother and georeferential location might outweigh those (62–64). In the rural areas, mothers or women who will bear children have more unfavorable systems for healthcare such as, low income, education, and very less availability of health services to make is easier to the women to bear children so; these conditions lead to infant mortality because these women are not able to handle their pregnancy or the issues relating to pregnancy properly. These issues are now reflected as the studies on rural urban difference map these issues and have proved the existence of these issues (59, 65).
Among rural and urban mothers, our findings showed notable negative relationships between physical activity and diet with mental health indicators (depression, anxiety, and stress). Studies supporting this one have found that physical activity lowers anxiety and stress; one study found that regular exercise helps to lower postpartum depression (66, 67). Studies have also shown that a balanced diet helps to alleviate depressive and anxious symptoms in mothers (68, 69). Some studies, meanwhile, question these links and argue that other variables such as healthcare and socioeconomic level might be more important predictors of mental health results than physical activity or diet alone (70, 71). Regular exercise and good nutrition’s physiological and psychological advantages explain these correlations; they lower inflammation and enhance hormonal balance, both of which have been connected to improved mental health (70, 72).
Moreover, our findings underlined the different physical activity, dietary and mental health markers (i.e., depression, anxiety, and stress) between rural and urban mothers, with rural mothers indicating more physical activity and better diets, and lower levels of mental health distress. Previous supporting studies have found that rural mothers demonstrate healthier lifestyle behavior, such as nutrition and physical activity (both of which could related to increased community involvement and less artificial nature) (73, 74). While urban areas are often perceived as having a wider variety of health promoting resources such as gyms, and dietary diversity, as is revealed by contradictory research (75, 76), they may also actually provide a better place for mothers to engage in physical activity and nutrition despite having reported mental health issues. In explaining rural urban disparities on mental health, Singh et al. (76) attributed it to the different environmental stressors, urban mothers having greater socioeconomic stress and less access to green spaces, in comparison to rural mothers who experience other challenges of limited healthcare but report high amount of community support and less stress from urban conditions in living (77).
Conclusion
The results showed notable links between demographic variables and newborn death; rural areas and early marriage before 18 indicated higher infant death rates. Mental health indicators including sadness, anxiety, and stress were negatively correlated with lifestyle choices including physical activity and diet. Rural mothers had better lifestyle decisions and far less mental health problems than urban mothers as well. Though it did not affect lifestyle decisions, early marriage was linked to poorer mental health results, especially anxiety and stress. Moreover, healthcare access emerged as a significant factor, with limited healthcare resources in rural areas contributing to higher infant mortality rates. This underscores the need for better healthcare access, especially in underserved areas, as a means to improve maternal and child health outcomes.
Limitations and future recommendations
Among the shortcomings of the study are its cross-sectional design due to its reliance on self-reported data, which could skew results. The sample was also restricted to Khyber Pakhtunkhwa mothers, so the results might not be applicable to other areas. Future studies should use objective lifestyle and mental health measurements to lower bias, include a more varied sample from several areas of Pakistan, and examine longitudinal designs to prove causality. Additional research could look at how other social factors including education and employment affect maternal and child health results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Beijing Normal University ethical committee and the ethical committee number is 202003310034. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SS: Writing – original draft, Visualization, Resources, Software, Validation, Methodology, Conceptualization. ZZ: Resources, Data curation, Writing – review & editing, Investigation. MJ: Data curation, Investigation, Validation, Writing – review & editing. FA: Resources, Data curation, Writing – review & editing, Investigation, Funding acquisition. WZ: Investigation, Validation, Data curation, Writing – review & editing. XL: Conceptualization, Supervision, Funding acquisition, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The study was funded by the National Major Educational Research project of National Science Planning (VBA230010); and the Cultivation Program for Leading Talents of Beijing Normal University (1233200016): The authors extend their appreciation to the Deanship of Scientific Research and Libraries in Princess Nourah bint Abdulrahman University for funding this research work through the program for supporting publication in Top-impact journals, Grant No. SPTIF-2025-2.
Acknowledgments
We appreciate the parents, and researchers who participated in our study and people who assisted in the data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. UNICEF. Levels and trends in child mortality report 2023. New York: United Nations Children’s Fund (2023).
3. Dagher, RK, and Linares, DE. A critical review on the complex interplay between social determinants of health and maternal and infant mortality. Children. (2022) 9:394. doi: 10.3390/children9030394
4. Jang, CJ, and Lee, HC. A review of racial disparities in infant mortality in the US. Children. (2022) 9:257. doi: 10.3390/children9020257
5. Atkins, R, Pontes, NM, Patterson, NA, Hinckson, A, Aromolaran, D, McCray, A, et al. The effects of race, ethnicity, and maternal education on infant mortality. Nurs Res. (2024) 73:37–45. doi: 10.1097/NNR.0000000000000700
6. Fishman, SH, Hummer, RA, Sierra, G, Hargrove, T, Powers, DA, and Rogers, RG. Race/ethnicity, maternal educational attainment, and infant mortality in the United States. Biodemography Soc Biol. (2021) 66:1–26. doi: 10.1080/19485565.2020.1793659
7. Sedig, MB, and Pacquaio, DF. Action on social determinants of black maternal and infant mortality in the United States. J Nursing Practice Applications Reviews Research. (2021) 11:67–75. doi: 10.13178/jnparr.2021.11.02.1108
8. Elder, TE, Goddeeris, JH, and Haider, SJ. Racial and ethnic infant mortality gaps and the role of socio-economic status. Labour Econ. (2016) 43:42–54. doi: 10.1016/j.labeco.2016.04.001
9. Matoba, N, and Collins, JW Jr. Racial disparity in infant mortality. Semin Perinatol. (2017) 41:354–9. doi: 10.1053/j.semperi.2017.07.003
10. Singh, GK, and Stella, MY. Infant mortality in the United States, 1915-2017: large social inequalities have persisted for over a century. Int J Matern Child Health AIDS. (2019) 8:19. doi: 10.21106/ijma.271
11. Lorch, SA, and Enlow, E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr Res. (2016) 79:141–7. doi: 10.1038/pr.2015.199
12. Mustafa, K, Nosheen, M, and Khan, AU. Dynamic reflections of multidimensional health poverty in Pakistan. PLoS One. (2021) 16:e0258947. doi: 10.1371/journal.pone.0258947
13. Nawaz, R, Khalid, N, Ajmal, F, Akbary, MF, Gong, S, and Zhou, Z. The nexus between healthcare provider distribution and neonatal mortality based on the context of maternal and child healthcare services in Pakistan. J Health Popul Nutr. (2025) 44:219. doi: 10.1186/s41043-025-00971-7
14. Zainab, U, Abbas, M, Urooj, A, Rabia, M, Sun, H, and Ahmed Shehzad, M. Undesired nexus poor health status of child under-five: a case study of Pakistan. PLoS One. (2025) 20:e0323845. doi: 10.1371/journal.pone.0323845
15. Khan, NU, Asif, N, Zehrh, I, Mg, G, Arshad, S, and Changez, MIK. Fertility patterns in Pakistan: a comparative analysis of family planning trends across different geographic regions. Rural Remote Health. (2024) 24:1–8. doi: 10.3316/informit.T2024110600006300410766222
16. Shakeel, A, Kamal, A, Tesema, GA, and Siddiqa, M. Analysis of spatial patterns and associated factors of stillbirth in Pakistan, PDHS (2017–18): a spatial and multilevel analysis. J Stat Theory Pract. (2023) 17:19. doi: 10.1007/s42519-022-00308-1
17. Memon, Z, Fridman, D, Soofi, S, Ahmed, W, Muhammad, S, Rizvi, A, et al. Predictors and disparities in neonatal and under 5 mortality in rural Pakistan: cross sectional analysis. Lancet Regional Health. (2023) 15:1–11. doi: 10.1016/j.lansea.2023.100231
18. Maryam, BIBI, Khan, FA, and Irshad, I. Women empowerment and infant mortality in Pakistan: micro data evidence. Pak J Appl Econ. (2020) 30:181–201. Available at: https://www.aerc.edu.pk/wp-content/uploads/2021/01/Paper-914-MARYAM-BIBI-II.pdf
19. Dodd, JM, Deussen, AR, and Louise, J. A randomised trial to optimise gestational weight gain and improve maternal and infant health outcomes through antenatal dietary, lifestyle and exercise advice: the OPTIMISE randomised trial. Nutrients. (2019) 11:2911. doi: 10.3390/nu11122911
20. Hayes, L, McParlin, C, Azevedo, LB, Jones, D, Newham, J, Olajide, J, et al. The effectiveness of smoking cessation, alcohol reduction, diet and physical activity interventions in improving maternal and infant health outcomes: a systematic review of meta-analyses. Nutrients. (2021) 13:1036. doi: 10.3390/nu13031036
21. Fatima, H, Yasmin, S, Fernandes, NA, Afzal, A, Arif, B, Shah, SNA, et al. The impact of physical activity on maternal and fetal well-being during pregnancy. J Health Wellness Community Research. (2025) 3:e397. doi: 10.61919/0et8q268
22. Nuruddin, R, Vadsaria, K, Mohammed, N, and Sayani, S. The efficacy of a personalized mHealth coaching program during pregnancy on maternal diet, supplement use, and physical activity: protocol for a parallel-group randomized controlled trial. JMIR Research Protocols. (2021) 10:e31611. doi: 10.2196/31611
23. Collings, PJ, Farrar, D, Gibson, J, West, J, Barber, SE, and Wright, J. Associations of pregnancy physical activity with maternal cardiometabolic health, neonatal delivery outcomes and body composition in a biethnic cohort of 7305 mother–child pairs: the born in Bradford study. Sports Med. (2020) 50:615–28. doi: 10.1007/s40279-019-01193-8
24. Iqbal, H, West, J, McEachan, RR, and Haith-Cooper, M. Identifying the health concerns of pregnant British Pakistani women living in deprived areas: a qualitative study. Matern Child Health J. (2024) 28:489–95. doi: 10.1007/s10995-023-03797-z
25. Khan, HA, Qamar, K, Salman, Y, Shakir, A, Butt, MS, Tharwani, ZH, et al. Exploring the relationship between anemia in pregnancy and infant mortality: a narrative review. Int J Surgery. (2024) 7:e0412. doi: 10.1097/GH9.0000000000000412
26. Kiran, W, Babar, H, Noor, M, Hussain, M, and Ibrahim, M. Association between maternal anemia and the anthropometric measurements of full-term newborns. Indus J Bioscience Research. (2025) 3:318–22. doi: 10.70749/ijbr.v3i4.1091
27. Fatima, N, Khan, MS, Fatima, M, Khalid, M, Salomon, I, and Abro, MT. Food insecurity characteristics and related factors among pregnant women attending antenatal care in Karachi. BMC Pregnancy Childbirth. (2025) 25:669. doi: 10.1186/s12884-025-07795-7
28. Fazal, S, Shahid, Y, Nadhman, A, Amjad, N, Naeem, M, Khan, S, et al. Maternal malnutrition and its associated adverse pregnancy outcomes and childbirth in Dadu district, Sindh, Pakistan. Pak J Public Health. (2024) 14:127–33. doi: 10.32413/pjph.v14iSpecial.ni.1374
29. Iqbal, S, and Ali, I. Maternal food insecurity in low-income countries: revisiting its causes and consequences for maternal and neonatal health. J Agriculture Food Research. (2021) 3:100091. doi: 10.1016/j.jafr.2020.100091
30. Sajid, I, Khan, SA, Hussain, S, Rehman, MU, and Adnan, MS. Maternal nutrition and its impact on low birth weight in newborns. Indus J Biosci Research. (2025) 3:236–44. doi: 10.70749/ijbr.v3i1.482
31. Thaver, I, Ahmad, AM, Ashraf, M, Asghar, SK, and Mirza, MS. Effect of multi-pronged interventions in reducing low birth weight and maternal anaemia among pregnant women. A community-based interventions research in non-agrarian resource constrained setting of rural Pakistan. JPMA. (2020) 70:2092–101. doi: 10.47391/JPMA.1218
32. Field, T. Prenatal depression effects on early development: a review. Infant Behav Dev. (2011) 34:1–14. doi: 10.1016/j.infbeh.2010.09.008
33. Grote, NK, Bridge, JA, Gavin, AR, Melville, JL, Iyengar, S, and Katon, WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. (2010) 67:1012–24. doi: 10.1001/archgenpsychiatry.2010.111
34. Zubrick, SR, Shepherd, C, Dudgeon, P, Gee, G, Paradies, Y, Scrine, C, et al. Social determinants of social and emotional wellbeing In: t Working, editor. Aboriginal and Torres Strait islander mental health and wellbeing principles and practice : Telethon Institute for Child Health Research, Kulunga Research Network (2014). 93–112.
35. Rahman, A, Malik, A, Sikander, S, Roberts, C, and Creed, F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. (2008) 372:902–9. doi: 10.1016/S0140-6736(08)61400-2
36. Amato, PR. The impact of family formation change on the cognitive, social, and emotional well-being of the next generation. Futur Child. (2005) 15:75–96. doi: 10.1353/foc.2005.0012
37. Agha, N, and Rind, RD. Experiences of teenage pregnancy and its consequences on adolescent girls in rural Sindh, Pakistan. JPMA. (2024) 74:1968–72. doi: 10.47391/JPMA.11356
38. Bari, K, Sadik, F, and Faraz, N. Child marriage and its effect on maternal and child health in Pakistan In: Research and reflections on child wellbeing in Pakistan. Cham: Springer Nature Switzerland (2025). 93–116.
39. Naz, S, Aslam, M, and Karim, R. Social and cultural factors influencing maternal mortality in Khyber Pakhtunkhwa-Pakistan. J Posit Sch Psychol. (2022) 6:453–65. Available at: https://journalppw.com/index.php/jpsp/article/view/
40. Shabbar, SZ, and Manzoor, A. An analytical study on early marriage in Pakistan: impact on education and health. Pak J Educ Res. (2022) 5:25–41. doi: 10.52337/pjer.v5i2.515
41. Atif, M, Farooq, M, Shafiq, M, Ayub, G, and Ilyas, M. The impact of partner’s behaviour on pregnancy related outcomes and safe child-birth in Pakistan. BMC Pregnancy Childbirth. (2023) 23:516. doi: 10.1186/s12884-023-05814-z
42. Nasrullah, M, Zakar, R, Zakar, MZ, and Krämer, A. Girl-child marriage and its association with morbidity and mortality of children under 5 years of age in a nationally-representative sample of Pakistan. J Pediatr. (2014) 164:639–46. doi: 10.1016/j.jpeds.2013.11.017
43. Tharwani, ZH, Bilal, W, Khan, HA, Kumar, P, Butt, MS, Hamdana, AH, et al. Infant & child mortality in Pakistan and its determinants: a review. Inquiry. (2023) 60:00469580231167024. doi: 10.1177/00469580231167024
44. Dawn. (2024). Defining income groups. Dawn Newspaper. Available online at: https://www.dawn.com/news/219652/defining-income-groups.
45. Lovibond, PF, and Lovibond, SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
46. Dinzeo, TJ, Thayasivam, U, and Sledjeski, EM. The development of the lifestyle and habits questionnaire-brief version: relationship to quality of life and stress in college students. Prev Sci. (2014) 15:103–14. doi: 10.1007/s11121-013-0370-1
47. Izulla, P, Muriuki, A, Kiragu, M, Yahner, M, Fonner, V, Nitu, SNA, et al. Proximate and distant determinants of maternal and neonatal mortality in the postnatal period: a scoping review of data from low-and middle-income countries. PLoS One. (2023) 18:e0293479. doi: 10.1371/journal.pone.0293479
48. Kibret, GD. Maternal and newborn health services accessibility, utilisation and neonatal mortality in Ethiopia. Australia: University of Technology Sydney (2023).
49. Chauhan, BG, Verma, RK, Alagarajan, M, and Chauhan, SK. Effect of maternal healthcare utilization on early neonatal, neonatal and post-neonatal mortality in India. Community Health Equity Research Policy. (2022) 43:31–43. doi: 10.1177/0272684X211004925
50. Ogbo, FA, Ezeh, OK, Awosemo, AO, Ifegwu, IK, Tan, L, Jessa, E, et al. Determinants of trends in neonatal, post-neonatal, infant, child and under-five mortalities in Tanzania from 2004 to 2016. BMC Public Health. (2019) 19:1243. doi: 10.1186/s12889-019-7547-x
51. Temporin, F. What matters most for newborns' survival? Patterns of socioeconomic determinants of neonatal and post-neonatal mortality in Bolivia. (Doctoral dissertation, London: London School of Economics and Political Science (2019).
52. Mekuria, YA, Zeleke, BG, Mekonen, GW, and Chekol, TM. Spatial variation and determinants of skilled birth attendant delivery among women of reproductive age in Ethiopia: a spatial and multilevel analysis. BMC Pregnancy Childbirth. (2025) 25:48. doi: 10.1186/s12884-025-07164-4
53. Womack, LS, Rossen, LM, and Hirai, AH. Urban–rural infant mortality disparities by race and ethnicity and cause of death. Am J Prev Med. (2020) 58:254–60. doi: 10.1016/j.amepre.2019.09.010
54. Vilda, D, Hardeman, R, Dyer, L, Theall, KP, and Wallace, M. Structural racism, racial inequities and urban–rural differences in infant mortality in the US. J Epidemiol Community Health. (2021) 75:788–93. doi: 10.1136/jech-2020-214260
55. Wang, Y, Zhu, J, He, C, Li, X, Miao, L, and Liang, J. Geographical disparities of infant mortality in rural China. Arch Dis Child Fetal Neonatal Ed. (2012) 97:F285–90. doi: 10.1136/archdischild-2011-300412
56. Yu, X, Wang, Y, Kang, L, Miao, L, Song, X, Ran, X, et al. Geographical disparities in infant mortality in the rural areas of China: a descriptive study, 2010–2018. BMC Pediatr. (2022) 22:264. doi: 10.1186/s12887-022-03332-z
57. Singh, GK, Kogan, MD, and Slifkin, RT. Widening disparities in infant mortality and life expectancy between Appalachia and the rest of the United States, 1990–2013. Health Aff. (2017) 36:1423–32. doi: 10.1377/hlthaff.2016.1571
58. Aidoo, EM. Community based healthcare interventions and their role in reducing maternal and infant mortality among minorities. Int J Research Publication Reviews. (2024) 5:4620–36. doi: 10.55248/gengpi.6.0325.1177
59. Ehrenthal, DB, Kuo, HHD, and Kirby, RS. Infant mortality in rural and nonrural counties in the United States. Pediatrics. (2020) 146:1–11. doi: 10.1542/peds.2020-0464
60. Defo, BK. Areal and socioeconomic differentials in infant and child mortality in Cameroon. Soc Sci Med. (1996) 42:399–420. doi: 10.1016/0277-9536(95)00107-7
61. Mustafa, H. (2007). Socioeconomic determinants of infant mortality in Kenya (Doctoral dissertation).
62. Ding, Y, Li, G, Shi, X, Wang, M, Peng, Y, Deng, H, et al. Correlation of lifestyle behaviors during pregnancy with postpartum depression status of puerpera in the rural areas of South China. Front Public Health. (2023) 11:1304226. doi: 10.3389/fpubh.2023.1304226
63. Raj, A, and Boehmer, U. Girl child marriage and its association with national rates of HIV, maternal health, and infant mortality across 97 countries. Violence Against Women. (2013) 19:536–51. doi: 10.1177/1077801213487747
64. Van de Poel, E, O'donnell, O, and Van Doorslaer, E. What explains the rural-urban gap in infant mortality: household or community characteristics? Demography. (2009) 46:827–50. doi: 10.1353/dem.0.0074
65. Dongarwar, D, and Salihu, HM. Place of residence and inequities in adverse pregnancy and birth outcomes in India. Int J Maternal Child Health AIDS. (2019) 9:53–63. doi: 10.21106/ijma.291
66. Firth, J, Solmi, M, Wootton, RE, Vancampfort, D, Schuch, FB, Hoare, E, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. (2020) 19:360–80. doi: 10.1002/wps.20773
67. Yang, C, Zhao, A, Lan, H, Ren, Z, Zhang, J, Szeto, IMY, et al. Association between dietary quality and postpartum depression in lactating women: a cross-sectional survey in urban China. Front Nutr. (2021) 8:705353. doi: 10.3389/fnut.2021.705353
68. Brumby, S, Chandrasekara, A, McCoombe, S, Torres, S, Kremer, P, and Lewandowski, P. Reducing psychological distress and obesity in Australian farmers by promoting physical activity. BMC Public Health. (2011) 11:362. doi: 10.1186/1471-2458-11-362
69. Jacka, FN, Pasco, JA, Mykletun, A, Williams, LJ, Hodge, AM, O'Reilly, SL, et al. Association of western and traditional diets with depression and anxiety in women. Am J Psychiatry. (2010) 167:305–11. doi: 10.1176/appi.ajp.2009.09060881
70. Herba, CM, Glover, V, Ramchandani, PG, and Rondon, MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry. (2016) 3:983–92. doi: 10.1016/S2215-0366(16)30148-1
71. McEachan, RRC, Prady, SL, Smith, G, Fairley, L, Cabieses, B, Gidlow, C, et al. The association between green space and depressive symptoms in pregnant women: moderating roles of socioeconomic status and physical activity. J Epidemiol Community Health. (2016) 70:253–9. doi: 10.1136/jech-2015-205954
72. Hackett, KM, Mukta, US, Jalal, CS, and Sellen, DW. A qualitative study exploring perceived barriers to infant feeding and caregiving among adolescent girls and young women in rural Bangladesh. BMC Public Health. (2015) 15:771. doi: 10.1186/s12889-015-2115-5
73. Brown, WJ, Mishra, G, Lee, C, and Bauman, A. Leisure time physical activity in Australian women: relationship with well being and symptoms. Res Q Exerc Sport. (2000) 71:206–16. doi: 10.1080/02701367.2000.10608901
74. Molnar, BE, Gortmaker, SL, Bull, FC, and Buka, SL. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. Am J Health Promot. (2004) 18:378–86. doi: 10.4278/0890-1171-18.5.378
75. Gopalakrishnan, L, Acharya, B, Puri, M, and Diamond-Smith, N. A longitudinal study of the role of spousal relationship quality and mother-in-law relationship quality on women’s depression in rural Nepal. SSM Mental Health. (2023) 3:100193. doi: 10.1016/j.ssmmh.2023.100193
76. Singh, GK, Daus, GP, Allender, M, Ramey, CT, Martin, EK, Perry, C, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS. (2017) 6:139–64. doi: 10.21106/ijma.236
Keywords: mental health, depression, anxiety, physical activities, diet, infant mortality, rural mothers, urban mothers
Citation: Shah SM, Zhang Z, Jahangir M, Alharbi FS, Zhang W and Lin X (2025) Associations among parental mental health, lifestyle factors and infant mortality in rural and urban mothers. Front. Public Health. 13:1622333. doi: 10.3389/fpubh.2025.1622333
Edited by:
Raymond Akawire Aborigo, Navrongo Health Research Centre, GhanaReviewed by:
Davi Rumel, Retired, São Paulo, BrazilAmira Shalaby, Assiut University, Egypt
Winda Ayu Fazraningtyas, Universitas Sari Mulia, Indonesia
Bimal Kumar Sahoo, SJMCH, India
Copyright © 2025 Shah, Zhang, Jahangir, Alharbi, Zhang and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fatimah Sayer Alharbi, ZnNhYWxoYXJiaUBwbnUuZWR1LnNh; Xiuyun Lin, bGlueHlAYm51LmVkdS5jbg==
 S. Mudasser Shah
S. Mudasser Shah Zijin Zhang1
Zijin Zhang1 Muhammad Jahangir
Muhammad Jahangir