- 1Department of Obstetrics and Gynecology, Olson Center for Women’s Health, University of Nebraska Medical Center, Omaha, NE, United States
- 2Department of Environmental, Agricultural, and Occupational Health, University of Nebraska Medical Center, Omaha, NE, United States
- 3Department of Veterans Affairs Nebraska-Western Iowa Health Care System, Omaha, NE, United States
Women have played a vital role in the U.S. military for decades, with their presence steadily increasing. However, despite this growth, research on the unique occupational and environmental exposures they face remains limited, highlighting the need for greater understanding to improve reproductive health outcomes. Chemical exposures such as burn pit emissions, airborne particulates, heavy metals, and pesticides can disrupt hormone regulation and pose risks for fertility, miscarriage, preterm birth, and congenital anomalies. Additional risks include unsafe water sources, contaminated soil, increased vaccinations, and extreme environmental conditions. However, studies on these exposures remain inconsistent, with some indicating significant reproductive risks while others show minimal or no impact. This mini review highlights what is currently known about the impact of military-related environmental and occupational exposures on women’s reproductive health and identifies key gaps in the literature. Further research is essential to determine high-risk exposures, guide policy development, and support early intervention strategies. Addressing the long-term impact of military-related environmental exposures is crucial for ensuring better health outcomes and facilitating access to care for female service members and veterans.
1 Introduction
Women have been an integral part of the military for decades, serving across various roles and operational environments. As of 2023, women constitute nearly 18% of the active-duty force and approximately 11.3% of the total U.S. Veteran population (1), marking them as the fastest growing subgroup among Veterans. By 2043, women are projected to make up 17.2% of all living Veterans (1). As the presence of women in the armed forces continues to grow, so does the need to understand the unique occupational and environmental exposures they face during their time of service. While much research has examined the health effects of military service on men, fewer studies have focused on the specific exposures and risks encountered by women, particularly in relation to environmental and occupational hazards.
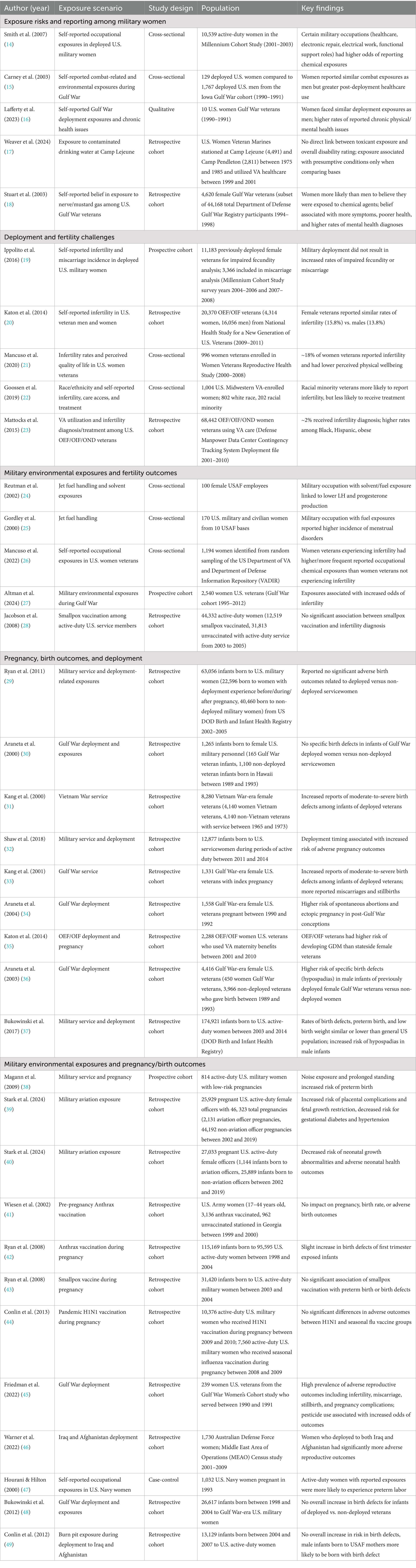
Military service inherently involves exposure to a variety of environmental and industrial hazards that can have lasting health consequences for both women and their offspring. Active-duty military women, who are often in their prime reproductive years, are particularly vulnerable to harmful chemical exposures that can disrupt hormone regulation and impair fertility (2–4). For women who become pregnant while serving, military exposures may pose increased risks for pregnancy complications including miscarriage, preterm birth, low birth weight, and congenital anomalies (4–8). These exposures include toxic substances such as burn pit emissions, airborne particulates, heavy metals, industrial solvents, fuel combustion byproducts, and pesticides (9–11) (Figure 1). Women serving in deployed settings may also encounter unsafe water sources, contaminated soil, increased routine and/or deployment-specific vaccinations, and prolonged exposure to extreme temperatures (9, 10), all of which may pose potential risks to reproductive health.
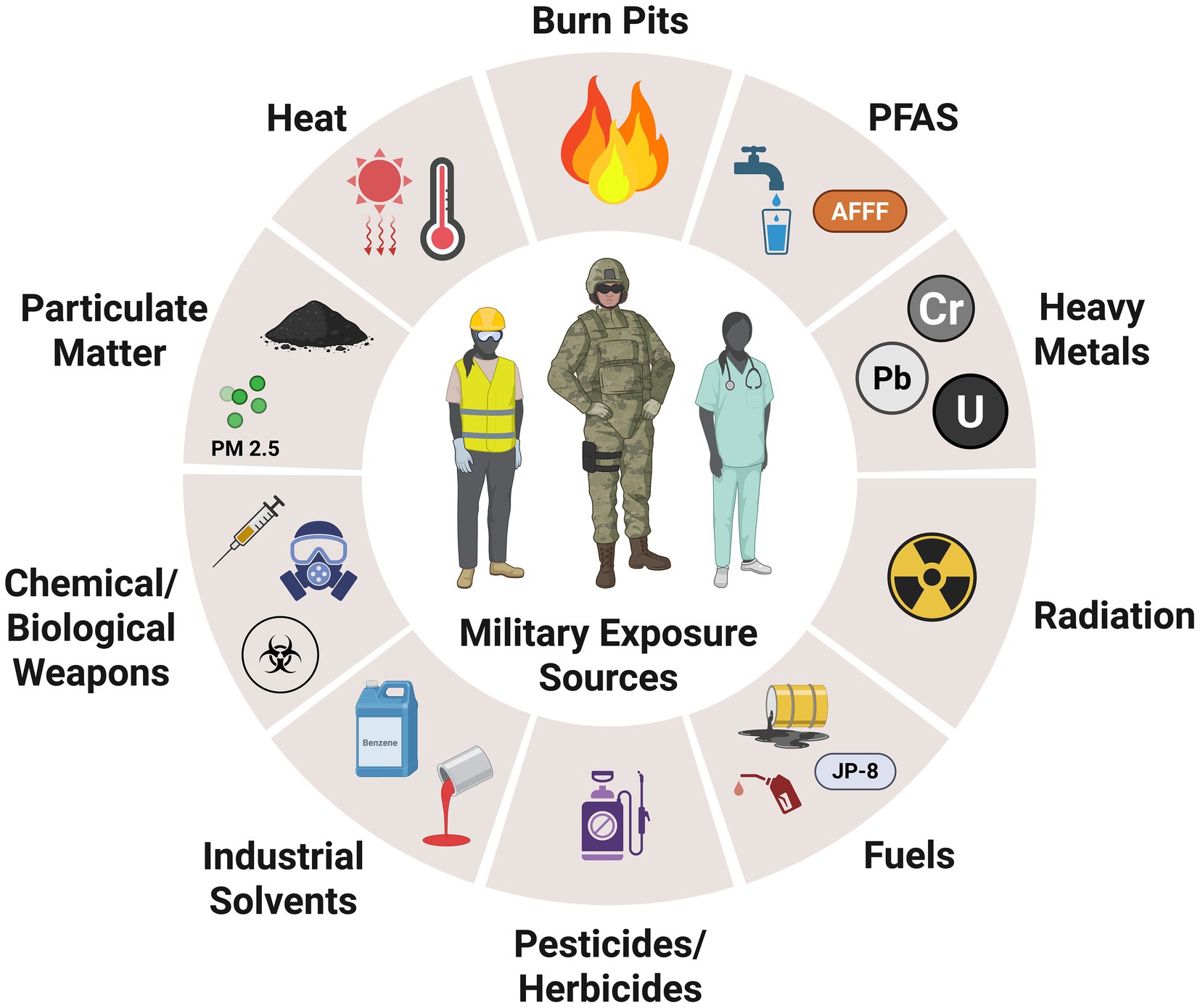
Figure 1. Potential occupational hazards, including chemical and physical exposures faced by female military personnel.
Understanding the lasting impact of military-related environmental exposures is essential for enhancing health outcomes and ensuring better access to care for servicewomen and veterans, especially during their transition to civilian life. As the Department of Veterans Affairs (VA) expands women-centered healthcare services (3, 12, 13), further research is needed to assess the reproductive effects of military service, identify high-risk exposures, and develop policies that mitigate potential health risks. Additionally, increasing awareness and education on these risks among both healthcare providers and service members will be essential in ensuring early intervention and targeted preventive measures. In this mini review, we examine studies on the impact of military environmental and occupational exposures on reproductive health outcomes in active-duty and veteran women (Table 1). Additionally, we identify gaps in understanding female-specific health concerns related to these exposures and highlight key areas for future research.
2 Military service and reproductive health: risks, exposures, and outcomes
2.1 Exposure risks and reporting among military women
Several studies have highlighted significant gender differences in exposure reporting and risks, perceived health impacts, and post-exposure healthcare usage. Thus, the accurate assessment of these exposures is crucial for understanding long-term health risks among female service members. Using data from women in the Millennium Cohort Study, researchers found that both active-duty and Reserve/National Guard women in occupations such as healthcare, electronic repair/electrical work, and functional support roles faced the highest exposure risks (14). These women frequently reported encounters with death, trauma, chemical and biological warfare agents, depleted uranium, and pesticides, highlighting the occupational hazards associated with these roles (14). Active-duty women, particularly those in the Army, experienced greater exposure risks compared to their counterparts in the Reserve or National Guard (14). Other studies of women who served during the Gulf War (GW) indicated that women and men reported similar rates of overall environmental exposures (15, 16). Women, however, were more likely to experience illness at the time of exposure, particularly those related to smoke from oil fires, burning trash/human waste, mustard gas, or food contaminated with smoke, oil, or chemical agents (15). Additional exposures reported by a smaller cohort of GW women veterans included extreme heat and sand, oil fires/burn pits, depleted uranium, chemical munitions, vaccinations, and pyridostigmine bromide pills (16). Notably, 5 years post-deployment, women demonstrated higher rates of both outpatient and inpatient healthcare utilization compared to men and were more likely to receive disability compensation from the VA (15). Among female veterans stationed at Marine Corps Base Camp Lejeune, where water contamination raised concerns about long-term health risks, a comparative study with women stationed at Camp Pendleton, an unexposed control site, found no direct association between toxicant exposure and higher disability ratings (17). However, women from Camp Lejeune were more likely to have service-connected disability claims for presumptive conditions linked to toxicant exposures (17). Additionally, reproductive health concerns, such as ovary removal, were reported more frequently among exposed women (17). Beyond documented exposures, belief in toxicant exposure also may influence health outcomes. Women GW veterans were more likely to report perceived exposure to nerve or mustard gas and reported greater encounters with other potentially toxic agents and traumatic combat experiences than male GW veterans (18). Further, such beliefs resulted in higher rates of physical symptoms, mental health diagnoses, and poorer self-reported health in GW women veterans (16, 18). These findings suggest that the psychological impact of perceived exposure, regardless of documented exposure status, may contribute to increased healthcare utilization and long-term illness risk. Addressing both real and perceived exposures in military healthcare settings is essential for improving health outcomes and reducing the burden of post-deployment illnesses.
2.2 Deployment and fertility challenges
The impact of military deployment on fertility remains a growing area of concern, particularly as more women serve. Another study using data from the Millennium Cohort Study examined whether deployment-related experiences, including combat exposure and stress, were associated with an increased risk of impaired fecundity among U.S. servicewomen. Their findings indicated that military deployment, regardless of combat exposure, was not significantly associated with increased rates of infertility or miscarriage (19). Similarly, a study that examined self-reported infertility among veterans who served during Operation Enduring Freedom/Operation Iraqi Freedom (OEI/OIF) found that while female veterans were no more likely than male veterans to report infertility, they were significantly more likely to seek medical help for fertility issues (20). Alternatively, survey data from VA-enrolled women aged 21–52 found that 18% reported a history of infertility, and those with a history of infertility reported lower perceived physical wellbeing and higher rates of chronic conditions such as fibromyalgia, persistent pain, and cancer (21). Further, racial minority veterans were more likely to report infertility but less likely to receive infertility treatment compared to their white counterparts (22, 23), citing reasons for not seeking fertility treatment including lack of awareness about available evaluations and treatments, as well as uncertainty or mixed feelings about becoming pregnant (22). While these studies suggests that military service may not significantly alter infertility prevalence compared to civilians, the demands of deployment may delay fertility. Further, these findings suggest that infertility may serve as an indicator of broader health concerns, which is likely to result in greater healthcare utilization for reproductive issues. However, given the limited scope and timespan of the data sets evaluated in the aforementioned studies, further research is needed to fully understand the long-term reproductive effects of military service, given that more women are currently serving in deployment situations than ever before.
2.3 Military environmental exposures and fertility outcomes
A small number of studies have explored the associations between chemical exposures, hazardous materials, and reproductive endocrine disruptions among female service members and veterans. Fuel handling is a common occupational exposure in the military, and a small number of studies have examined its impact on reproductive health among military women. Research on U.S. Air Force personnel exposed to jet fuel (JP-8) and organic solvents found that women with higher exposure to aliphatic (C6H14–C16H34) and aromatic (benzene, ethylbenzene, toluene, m,p,o-xylenes) hydrocarbons exhibited lower preovulatory luteinizing hormone (LH) levels, a key hormone for ovulation and fertility (24). Additionally, exposure to aromatic hydrocarbons was associated with a trend toward lower midluteal progesterone levels, further suggesting potential endocrine disruption (24). Another study on female U.S. Air Force personnel who reported occupational fuel handling, found an increased risk of menstrual disorders such as dysmenorrhea and abnormal cycle lengths (25). Further supporting the connection between military toxicant exposure and reproductive health, another study found that women experiencing infertility had higher exposure rates to petrochemicals, polychlorinated biphenyls (PCBs), sulfur fires, extreme heat, and receiving an anthrax vaccine compared to those not experiencing infertility (26). Women with infertility also reported a greater cumulative number of toxicant exposures (26), suggesting that the burden of multiple exposures may compound reproductive risks. Similarly, research on female GW veterans using data from the Gulf War Longitudinal Cohort Study found that deployment, environmental exposures, and Gulf War Illness (GWI) were associated with an increased likelihood of infertility (27). Finally, military service members undergo various vaccinations as part of their duty requirements, raising questions about potential impacts on reproductive health, including infertility. A study of active-duty U.S. military women who received a smallpox vaccine determined that while the proportion of infertility diagnosis was slightly higher in vaccinated versus unvaccinated women, these differences were not statistically significant, indicative of no causal relationship (28). Taken together, these studies highlight the potential reproductive risks associated with military occupational and environmental exposures, particularly fuel handling, chemical mixtures, and deployment-related toxicants and vaccinations. Given the cumulative impact of multiple exposures, further research is needed to fully understand the long-term reproductive consequences and to develop targeted healthcare interventions for military women.
2.4 Pregnancy, birth outcomes, and deployment
Research on deployment and its effects on pregnancy and birth outcomes has yielded mixed results. Pregnancies among women who deployed during early pregnancy showed no significant increase in preterm birth or birth defects compared to non-deployed servicewomen (29). Similarly, an analysis of birth defects surveillance records revealed no significant differences in the prevalence of 48 selected birth defects between infants of female GW veterans and those of non-deployed female veterans (30). Furthermore, birth defect rates were consistent among infants conceived both before and after deployment, indicating no clear link between GW service and an increased risk of congenital anomalies (30). Likewise, among women Vietnam veterans, military service in Vietnam was not linked to an increased risk of miscarriage, stillbirth, low birth weight, preterm birth, or infant death, however there was an increased risk of birth defects (31).
In contrast, other research has identified greater risks of pregnancy complications, and birth defects associated with military service. Deployment timing may play a role, as women who gave birth within 6 months of returning from deployment had an increased risk of spontaneous preterm birth compared to those who had not recently deployed (32). Female GW veterans also reported more miscarriages and stillbirths than non-deployed counterparts, though these outcomes were found not statistically significant (33). Spontaneous abortions and ectopic pregnancies were also elevated in post-GW conceptions (34). Additionally, rates of gestational diabetes during pregnancy were higher in women veterans that were deployed in OEF/OIF versus women who were stateside (35). Concerns about birth defects among children born to military women have also been raised. An increased prevalence of certain congenital anomalies, particularly hypospadias, was observed among male infants conceived post-deployment by female GW veterans (36). Similarly, another study identified hypospadias as the most common birth defect reported in male infants born to active-duty mothers (37). Additionally, another study of female GW veterans found a higher prevalence of birth defects among children born to deployed female GW veterans versus non-deployed female GW veterans (33). Overall, while some studies suggest minimal pregnancy and birth risks associated with military service and deployment, others highlight specific vulnerabilities that warrant further investigation. Continued research is necessary to identify modifiable risk factors, improve obstetric healthcare for military women, and ensure comprehensive monitoring of birth outcomes in female service members and veterans.
2.5 Military environmental exposures and pregnancy/birth outcomes
Military women face a range of occupational and environmental hazards that could impact pregnancy and birth outcomes, with factors such physical demands and service-related exposures potentially contributing to increased pregnancy risks. The effects of standing, lifting, and noise exposure among active-duty pregnant women were examined, revealing that prolonged standing and noise exposure was associated with an increased risk of preterm labor/birth (38). The impact of aviation-related military careers on pregnancy has also been studied, showing that while military aviation officers had a lower risk of gestational diabetes and hypertension, they faced an increased risk of placental complications and fetal growth restriction, potentially due to occupational stressors such as intermittent hypoxia, circadian disruption, excessive noise/vibration, and radiation exposure (39). Interestingly though, babies born to female aviation officers were reported to less likely experience neonatal growth abnormalities or adverse neonatal health outcomes such as cardiovascular, neurological, or pulmonary disorders (40).
Concerns about the potential reproductive effects of vaccination in military women have led to several studies evaluating their impact on pregnancy and birth outcomes. The relationship between pre-pregnancy anthrax vaccination and pregnancy outcomes was examined in a study analyzing pregnancy rates, birth rates, and adverse birth outcomes among U.S. Army women. Findings showed no significant differences in these outcomes between vaccinated and unvaccinated women, though the study lacked sufficient power to detect rare adverse effects (41). In contrast, an analysis of birth defects among infants born to military women who received anthrax vaccinations found a slight increase in birth defects among first trimester-exposed infants, but the association was not statistically significant (42). The impact of smallpox vaccination on preterm births and birth defects among infants born to military women has also been examined, with findings showing no significant association between maternal smallpox vaccination and an increased risk of these outcomes (43). Another study assessed the safety of the pandemic H1N1 vaccine among pregnant military women and their newborns. The analysis compared pregnancy loss, preeclampsia, preterm labor, preterm birth, birth defects, and fetal growth problems between those vaccinated with the H1N1 vaccine (2009–2010) and those who received the seasonal influenza vaccine (2008–2009), with no significant differences in these outcomes between the two groups (44). Overall, studies on vaccine exposures in military women provide reassuring evidence that anthrax, smallpox, and influenza vaccinations do not significantly impact pregnancy outcomes or increase the risk of birth defects. Given the critical role of vaccination in force readiness and protection against biological threats, these findings support continued immunization efforts while emphasizing the need for ongoing surveillance to monitor any potential long-term reproductive effects.
Similar to the aforementioned studies on deployment-related environmental exposures and fertility outcomes, the role of exposures on birth outcomes have also yielded conflicting results. Higher rates of miscarriage, stillbirth, and pregnancy complications have been reported among GW women veterans, with pesticide cream use during deployment increasing the likelihood of women experiencing these outcomes (45). Similarly, Australian Defense Force veterans who deployed to both Iraq and Afghanistan and reported exposure to reproductive toxicants including exhaust emissions, fumes, toxic industrial chemicals, noise, and radiation also reported higher rates of adverse pregnancy outcomes including miscarriage, birth defects, and ectopic pregnancies (46). Active-duty U.S. Navy women were more likely to report exposures to heavy metals, solvents, and petroleum products at work after their pregnancies were confirmed relative to their civilian counterparts (47). Further, they are more likely to experience preterm labor during pregnancy (47). Alternatively, no significant increase in birth defects was observed among infants born to 1990–1991 GW female veterans, either at birth or within the first year of life (48). Research on burn pit exposure has also been inconclusive, with findings showing no consistent association between burn pit exposure including deployment location relative to the burn pit, timing, and duration of exposure before pregnancy and an increased risk of birth defects or preterm birth (49). Interestingly though, the male infants born to active-duty military women were more likely to be diagnosed with a birth defect if their mother was in the Air Force (49), potentially due to differences in occupational exposure scenarios. These findings underscore the complex relationship between military occupational and environmental exposures and pregnancy outcomes. While certain exposures, such as prolonged standing, aviation-related stressors, and deployment toxicants have been linked to increased offspring health risks, research on vaccine safety and birth defect prevalence has provided reassuring results. Continued investigation is necessary to clarify conflicting findings and ensure comprehensive reproductive healthcare for military women.
3 Conclusions and future perspective
As the number of women in active-duty military roles continues to grow, it is increasingly important to address their unique reproductive health risks. This review highlights the complex relationship between military related occupational and environmental exposures and reproductive health outcomes among female service members and veterans. While military service provides unique career opportunities for women, it also presents distinct risks to reproductive health through exposure to hazardous chemicals, high physical demands, and deployment-related environmental conditions. Despite growing recognition of these risks, research on their long-term reproductive impacts remains limited. Inconsistencies across studies point to a need for more robust data to establish clearer causal links between military toxicant exposures and adverse reproductive outcomes, emphasizing the importance of comprehensive exposure assessments and longitudinal studies. Moreover, disparities in infertility diagnosis and access to reproductive care persist within the military healthcare system, underscoring the importance of addressing systemic barriers to reproductive health services for servicewomen and veterans. Ultimately, supporting the reproductive health of women in the military requires a stronger focus on research, improved healthcare access, and a deeper understanding of the effects of military-related exposure and their risks.
Author contributions
KC: Writing – review & editing, Data curation, Conceptualization, Writing – original draft, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by VA IK2BX006457 (KC). The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government and Olson Center for Women’s Health (KLC).
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript. Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Veteran population. National Center for Veterans Analysis and Statistics. (2024). Available online at: https://www.va.gov/vetdata/veteran_population.asp (Accessed March 3, 2025).
2. Braun, LA, Kennedy, HP, Womack, JA, and Wilson, C. Integrative literature review: U.S. military women's genitourinary and reproductive health. Mil Med. (2016) 181:35–49. doi: 10.7205/MILMED-D-15-00242
3. Assefa, MT, Adamson, MM, Proctor, LB, Moeder, S, Ashford, JW, and Jennings, JS. A multipronged approach to caring for women veterans with military environmental exposures. Womens Health Issues. (2024) 34:325–30. doi: 10.1016/j.whi.2024.05.002
4. Doyle, P, Maconochie, N, and Ryan, M. Reproductive health of Gulf War veterans. Philos Trans R Soc Lond Ser B Biol Sci. (2006) 361:571–84. doi: 10.1098/rstb.2006.1817
5. Mezwa, K, Adelsheim, L, and Markenson, G. Obstetric outcomes in military servicewomen: emerging knowledge, considerations, and gaps. Semin Reprod Med. (2019) 37:215–21. doi: 10.1055/s-0040-1712929
6. Khodr, ZG, Bukowinski, AT, Hall, C, Gumbs, GR, Wells, NY, and Conlin, AMS. The department of defense birth and infant health research program: assessing the reproductive health of U.S. active-duty women. Semin Reprod Med. (2018) 36:351–60. doi: 10.1055/s-0039-1678751
7. Lawrence-Wood, E, Kumar, S, Crompvoets, S, Fosh, BG, Rahmanian, H, Jones, L, et al. A systematic review of the impacts of active military service on sexual and reproductive health outcomes among servicewomen and female veterans of armed forces. J Mil Veterans Health. (2016) 24:34–55. Available online at: https://doi-ds.org/doilink/05.2021-28962829/JMVH
8. Krulewitch, CJ. Reproductive health of active duty women in medically austere environments. Mil Med. (2016) 181:63–9. doi: 10.7205/MILMED-D-15-00221
9. Nevin, RL, and Ritchie, EC. Toxic exposures from service in the US military: effects on reproductive and sexual health In: EC Ritchie editor. Intimacy post-injury: combat trauma and sexual health. New York, NY: Oxford University Press (2016). 165–78.
10. Geretto, M, Ferrari, M, De Angelis, R, Crociata, F, Sebastiani, N, Pulliero, A, et al. Occupational exposures and environmental health hazards of military personnel. Int J Environ Res Public Health. (2021) 18:5395. doi: 10.3390/ijerph18105395
11. Van De Graaff, J, and Poole, JA. A clinician's guide to occupational exposures in the military. Curr Allergy Asthma Rep. (2022) 22:259–64. doi: 10.1007/s11882-022-01051-0
12. Zephyrin, LC. Reproductive health management for the care of women veterans. Obstet Gynecol. (2016) 127:383–92. doi: 10.1097/AOG.0000000000001252
13. Wong, EP, and Yoon, J. Effects of veterans affairs access expansions on inpatient care for women veterans. Health Equity. (2025) 9:116–24. doi: 10.1089/heq.2024.0103
14. Smith, TC, Jacobson, IG, Smith, B, Hooper, TI, and Ryan, MA. The occupational role of women in military service: validation of occupation and prevalence of exposures in the Millennium Cohort Study. Int J Environ Health Res. (2007) 17:271–84. doi: 10.1080/09603120701372243
15. Carney, CP, Sampson, TR, Voelker, M, Woolson, R, Thorne, P, and Doebbeling, BN. Women in the Gulf War: combat experience, exposures, and subsequent health care use. Mil Med. (2003) 168:654–61. doi: 10.1093/milmed/168.8.654
16. Lafferty, M, Winchell, K, Cottrell, E, Knight, S, and Nugent, SM. Women of the Gulf War: understanding their military and health experiences over 30 years. Mil Med. (2023) 188:3191–8. doi: 10.1093/milmed/usac283
17. Weaver, FM, Cao, L, Stroupe, KT, Pratt, A, Tanner, CM, and Goldman, SM. Disability claims for female veterans exposed to contaminated water at Marine Base Camp Lejeune. Mil Med. (2024) 189:e2127–33. doi: 10.1093/milmed/usae237
18. Stuart, JA, Ursano, RJ, Fullerton, CS, Norwood, AE, and Murray, K. Belief in exposure to terrorist agents: reported exposure to nerve or mustard gas by Gulf War veterans. J Nerv Ment Dis. (2003) 191:431–6. doi: 10.1097/01.NMD.0000081634.28356.6B
19. Ippolito, AC, Seelig, AD, Powell, TM, Conlin, AMS, Crum-Cianflone, NF, Lemus, H, et al. Risk factors associated with miscarriage and impaired fecundity among United States servicewomen during the recent conflicts in Iraq and Afghanistan. Womens Health Issues. (2017) 27:356–65. doi: 10.1016/j.whi.2016.12.012
20. Katon, J, Cypel, Y, Raza, M, Zephyrin, L, Reiber, G, Yano, EM, et al. Self-reported infertility among male and female veterans serving during operation enduring freedom/operation Iraqi freedom. J Womens Health (Larchmt). (2014) 23:175–83. doi: 10.1089/jwh.2013.4468
21. Mancuso, AC, Summers, KM, Mengeling, MA, Torner, JC, Ryan, GL, and Sadler, AG. Infertility and health-related quality of life in United States women veterans. J Womens Health (Larchmt). (2020) 29:412–9. doi: 10.1089/jwh.2019.7798
22. Goossen, RP, Summers, KM, Ryan, GL, Mengeling, MA, Booth, BM, Torner, JC, et al. Ethnic minority status and experiences of infertility in female veterans. J Womens Health (Larchmt). (2019) 28:63–8. doi: 10.1089/jwh.2017.6731
23. Mattocks, K, Kroll-Desrosiers, A, Zephyrin, L, Katon, J, Weitlauf, J, Bastian, L, et al. Infertility care among OEF/OIF/OND women veterans in the Department of Veterans Affairs. Med Care. (2015) 53:S68–75. doi: 10.1097/MLR.0000000000000301
24. Reutman, SR, LeMasters, GK, Knecht, EA, Shukla, R, Lockey, JE, Burroughs, GE, et al. Evidence of reproductive endocrine effects in women with occupational fuel and solvent exposures. Environ Health Perspect. (2002) 110:805–11. doi: 10.1289/ehp.02110805
25. Gordley, LB, Lemasters, G, Simpson, SR, and Yiin, JH. Menstrual disorders and occupational, stress, and racial factors among military personnel. J Occup Environ Med. (2000) 42:871–81. doi: 10.1097/00043764-200009000-00005
26. Mancuso, AC, Mengeling, MA, Holcombe, A, and Ryan, GL. Lifetime infertility and environmental, chemical, and hazardous exposures among female and male US veterans. Am J Obstet Gynecol. (2022) 227:744.e1–e12. doi: 10.1016/j.ajog.2022.07.002
27. Altman, A, Gibson, C, Inslicht, S, Cao, G, Haas, C, and Dursa, E. Military exposures and reproductive health outcomes: findings from the Gulf War cohort study. Fertil Steril. (2024) 122:e212. doi: 10.1016/j.fertnstert.2024.07.694
28. Jacobson, IG, Gumbs, GR, Sevick, CJ, Smith, TC, and Ryan, MA. Smallpox vaccination is not associated with infertility in a healthy young adult population. Hum Vaccin. (2008) 4:224–8. doi: 10.4161/hv.4.3.5436
29. Ryan, MA, Jacobson, IG, Sevick, CJ, Smith, TC, Gumbs, GR, and Conlin, AM. Health outcomes among infants born to women deployed to United States military operations during pregnancy. Birth Defects Res A Clin Mol Teratol. (2011) 91:117–24. doi: 10.1002/bdra.20746
30. Araneta, MR, Destiche, DA, Schlangen, KM, Merz, RD, Forrester, MB, and Gray, GC. Birth defects prevalence among infants of Persian Gulf War veterans born in Hawaii, 1989–1993. Teratology. (2000) 62:195–204. doi: 10.1002/1096-9926(200010)62:4<>3.0.CO;2-5
31. Kang, HK, Mahan, CM, Lee, KY, Magee, CA, Mather, SH, and Matanoski, G. Pregnancy outcomes among U.S. women Vietnam veterans. Am J Ind Med. (2000) 38:447–54. doi: 10.1002/1097-0274(200010)38:4<447::AID-AJIM11>3.0.CO;2-J
32. Shaw, JG, Nelson, DA, Shaw, KA, Woolaway-Bickel, K, Phibbs, CS, and Kurina, LM. Deployment and preterm birth among US army soldiers. Am J Epidemiol. (2018) 187:687–95. doi: 10.1093/aje/kwy003
33. Kang, H, Magee, C, Mahan, C, Lee, K, Murphy, F, Jackson, L, et al. Pregnancy outcomes among U.S. Gulf War veterans: a population-based survey of 30, 000 veterans. Ann Epidemiol. (2001) 11:504–11. doi: 10.1016/S1047-2797(01)00245-9
34. Araneta, MR, Kamens, DR, Zau, AC, Gastañaga, VM, Schlangen, KM, Hiliopoulos, KM, et al. Conception and pregnancy during the Persian Gulf War: the risk to women veterans. Ann Epidemiol. (2004) 14:109–16. doi: 10.1016/j.annepidem.2003.08.006
35. Katon, J, Mattocks, K, Zephyrin, L, Reiber, G, Yano, EM, Callegari, L, et al. Gestational diabetes and hypertensive disorders of pregnancy among women veterans deployed in service of operations in Afghanistan and Iraq. J Womens Health (Larchmt). (2014) 23:792–800. doi: 10.1089/jwh.2013.4681
36. Araneta, MR, Schlangen, KM, Edmonds, LD, Destiche, DA, Merz, RD, Hobbs, CA, et al. Prevalence of birth defects among infants of Gulf War veterans in Arkansas, Arizona, California, Georgia, Hawaii, and Iowa, 1989–1993. Birth Defects Res A Clin Mol Teratol. (2003) 67:246–60. doi: 10.1002/bdra.10033
37. Bukowinski, AT, Conlin, AMS, Gumbs, GR, Khodr, ZG, Chang, RN, and Faix, DJ. Department of defense birth and infant health registry: select reproductive health outcomes, 2003–2014. MSMR. (2017) 24:39–49.
38. Magann, EF, Evans, SF, Chauhan, SP, Nolan, TE, Henderson, J, Klausen, JH, et al. The effects of standing, lifting and noise exposure on preterm birth, growth restriction, and perinatal death in healthy low-risk working military women. J Matern Fetal Neonatal Med. (2005) 18:155–62. doi: 10.1080/14767050500224810
39. Stark, CM, Sorensen, IS, Royall, M, Dorr, M, Brown, J, Dobson, N, et al. Maternal and fetal health risks among female military aviation officers. Aerosp Med Hum Perform. (2024) 95:675–82. doi: 10.3357/AMHP.6416.2024
40. Stark, CM, Sorensen, IS, Royall, M, Dorr, M, Brown, J, Dobson, N, et al. Neonatal Health Risks Among Children of Female Military Aviation Officers. Aerosp Med Hum Perform. (2024) 95:815–20. doi: 10.3357/AMHP.6417.2024
41. Wiesen, AR, and Littell, CT. Relationship between prepregnancy anthrax vaccination and pregnancy and birth outcomes among US Army women. JAMA. (2002) 287:1556–60. doi: 10.1001/jama.287.12.1556
42. Ryan, MA, Smith, TC, Sevick, CJ, Honner, WK, Loach, RA, Moore, CA, et al. Birth defects among infants born to women who received anthrax vaccine in pregnancy. Am J Epidemiol. (2008) 168:434–42. doi: 10.1093/aje/kwn159
43. Ryan, MA, Gumbs, GR, Conlin, AM, Sevick, CJ, Jacobson, IG, Snell, KJ, et al. Evaluation of preterm births and birth defects in liveborn infants of US military women who received smallpox vaccine. Birth Defects Res A Clin Mol Teratol. (2008) 82:533–9. doi: 10.1002/bdra.20470
44. Conlin, AMS, Bukowinski, AT, Sevick, CJ, DeScisciolo, C, and Crum-Cianflone, NF. Safety of the pandemic H1N1 influenza vaccine among pregnant U.S. military women and their newborns. Obstet Gynecol. (2013) 121:511–8. doi: 10.1097/AOG.0b013e318280d64e
45. Friedman, A, Janulewicz Lloyd, PA, Carlson, J, Quinn, E, Keating, D, Toomey, R, et al. Preliminary findings from the Gulf war women's cohort: reproductive and children's health outcomes among women veterans. Int J Environ Res Public Health. (2022) 19:8483. doi: 10.3390/ijerph19148483
46. Warner, R, Avery, JC, Neuhaus, SJ, and Davies, MJ. Associations between environmental exposures in the Middle East Area of Operations and pregnancy outcomes in Australian Defence Force veterans. Environ Res. (2022) 208:112688. doi: 10.1016/j.envres.2022.112688
47. Hourani, L, and Hilton, S. Occupational and environmental exposure correlates of adverse live-birth outcomes among 1032 US Navy women. J Occup Environ Med. (2000) 42:1156–65. doi: 10.1097/00043764-200012000-00006
48. Bukowinski, AT, DeScisciolo, C, Conlin, AM, Ryan, MAK, Sevick, CJ, and Smith, TC. Birth defects in infants born in 1998–2004 to men and women serving in the U.S. military during the 1990–1991 Gulf War era. Birth Defects Res A Clin Mol Teratol. (2012) 94:721–8. doi: 10.1002/bdra.23062
Keywords: environmental exposures, occupational exposures, women, military personnel, reproductive health
Citation: Clark KL (2025) Environmental and occupational risks to reproductive health in women service members and veterans. Front. Public Health. 13:1628858. doi: 10.3389/fpubh.2025.1628858
Edited by:
Terje Svingen, Technical University of Denmark, DenmarkReviewed by:
Laura N. Vandenberg, University of Massachusetts Amherst, United StatesCopyright © 2025 Clark. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kendra L. Clark, a2VuZHJhLmNsYXJrQHVubWMuZWR1
 Kendra L. Clark
Kendra L. Clark