- 1School of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2School of Management, Beijing University of Chinese Medicine, Beijing, China
- 3Guang’anmen Hospital, China Academy of Chinese Medicine Sciences, Beijing, China
- 4School of Health Management, Gansu University of Chinese Medicine, Lanzhou, China
- 5Gansu Health and Population Development Research Center, Gansu Provincial Health and Wellness Commission, Lanzhou, China
- 6School of Public Health, Lanzhou University, Lanzhou, China
- 7National Institute of Chinese Medicine Development and Strategy, Beijing University of Chinese Medicine, Beijing, China
Objectives: Lumbar disc herniation (LDH) presents a significant economic burden globally, worsening in China due to an aging population. Traditional Chinese Medicine (TCM) offers effective treatment options for LDH, making its integration with Diagnosis-Related Groups (DRG) payment reform crucial for reducing medical costs and enhancing healthcare quality.
Methods: We analyzed data from hospitalized patients at Qingyang City Hospital of Chinese Medicine, Gansu Province, from 2017 to 2022. Univariate analysis was conducted to examine changes in patient demographics before and after the DRG reform. A single group interrupted-time series analysis (ITSA) model was used to compare key indicators of medical costs and length of stay pre- and post-reform.
Results: A total of 2,857 LDH patients were included in the study. Pre-DRG reform, 1,294 patients were recorded, with males comprising 46.06% and a mean age (SD) of 58.29 (14.22) years. Post-DRG reform, 1,563 patients were observed, with males accounting for 40.88% and a mean age (SD) of 60.64 (14.25) years. No significant differences were found in nationality, marital status, use of Chinese medicine diagnostic and therapeutic equipment, use of Chinese medicine diagnostic and treatment techniques or diagnosis and treatment based on Chinese medicine evidence (p > 0.05). However, significant differences were noted in sex, age, visit times, admission pathways, admission disease status, complications and comorbidities, and surgeries and operations (p < 0.05). Healthcare-related costs and length of stay are associated with sex, age, visit times, and other factors, showing a positive correlation among different costs and length of stay (p < 0.05). Post-reform, average monthly hospitalization cost decreased by CNY 36.78 (
Conclusion: The DRG reform is associated with lower hospitalization cost and reduced costs for both Chinese medicine and Western medicine. However, its impact on overall medical services cost, diagnosis cost, TCM treatment cost, and length of stay is limited. Future DRG reform should leverage the distinctive advantages of TCM, enhance the payment system, improve treatment outcomes, and further reduce healthcare costs while shortening hospitalization times.
1 Introduction
Low back pain is one of modern society’s most common orthopedic conditions (1). Currently, over 600 million people suffer from low back pain worldwide, and this number is projected to exceed 800 million by 2050 (2–4). Low back pain attributable solely to occupational ergonomic factors contributed to global economic losses of US$216.1 billion. Recent Chinese healthcare statistics revealed an average hospitalization cost of ¥11,085.9 (US$1,604) per low back pain episode. Both China and the global community face substantial economic burdens from low back pain, with China experiencing particularly accelerated growth in this burden due to its rapidly aging population (5, 6). Low back pain ranks among the top causes of disability globally, with long recovery times that impose a significant economic burden on patients and their families. LDH has emerged as a primary contributor to low back pain, leg pain, and mobility impairments (7, 8), with its incidence climbing each year due to an aging population, evolving work patterns, lifestyle shifts, and increasingly sedentary behavior (9). Research from countries such as the United States (10, 11), the United Kingdom (12), Brazil (13), New Zealand (14), and Spain underscores the substantial healthcare burden posed by LDH (15, 16). Given China’s large population and accelerating aging process, healthcare costs associated with LDH are expected to continue rising soon.
TCM demonstrates unique advantages in treating LDH. It utilizes various modalities, including acupuncture, tuina (Chinese massage), herbal medicine, and moxibustion. By adopting a holistic approach and differential diagnosis, TCM effectively alleviates pain and enhances the body’s self-repair capabilities (17, 18). Furthermore, exercises such as Tai Chi and Wuqinxi have demonstrated significant effectiveness in preventing low back pain, as highlighted in several studies (19, 20). In contrast, conventional treatments like medication and surgery often carry numerous complications and side effects (21–23). TCM’s conservative, non-surgical methods typically result in fewer complications and better recovery outcomes (24–27). Reforming the DRG payment system in Chinese medicine hospitals to harness TCM strengths can significantly reduce hospitalization cost and length of stay for LDH patients, making this an important practical consideration.
DRG introduced by Fetter et al. in the 1980s, classify cases based on similarities in clinical processes and resource consumption (28). DRG has been adopted by various countries (29–33) for its benefits in hospital management and healthcare costs, achieving notable results (30, 34–36). Through decades of practice-oriented research and development, China has established several regional pilot DRG systems, including BJ-DRG, CN-DRG, CR-DRG, and C-DRG. These initiatives aim to address China’s rapidly growing healthcare expenditures while positively impacting the quality of medical services. On June 18, 2020, the China National Healthcare Security Administration officially promulgated the “China Healthcare Security Diagnosis Related Groups (CHS-DRG) Fine Classification Scheme (Version 1.0),” initiating nationwide pilot implementation and subsequent progressive rollout. The CHS-DRG framework adopts China’s national health insurance versions of ICD-10 (comprising 2,048 diagnostic categories, 10,172 subcategories, and 33,324 specific entries) and ICD-9-CM-3 (including 890 surgical procedure subcategories, 3,666 detailed items, and 12,995 entries). Following the grouping principles of “clinical process similarity” and “resource consumption similarity,” the system established 376 Adjacent Diagnosis-Related Groups (ADRGs), consisting of 167 surgical procedure groups, 22 non-operating room procedure groups, and 187 medical diagnosis groups, comprehensively covering all acute and severe short-term hospitalization cases (37, 38). While traditional Chinese medicine hospitals are required to implement the unified CHS-DRG standards alongside other medical institutions, a gradual transition period is permitted. For certain TCM-dominant disease categories with demonstrated treatment efficacy and stable cost structures, specially designated reimbursement standards may be alternatively applied. As a vital part of healthcare in China, the reform of DRG payment systems in Chinese medicine hospitals is important, particularly for LDH, a condition where TCM shows distinct advantages.
This study focuses on LDH patients at Qingyang City Hospital of Chinese Medicine, Gansu Province, examining the impact of DRG payment reform on healthcare-related costs and length of stay. The findings aim to provide insights for Chinese health policymakers to advance DRG reforms, leveraging TCM’s strengths to alleviate the economic burden of diseases like LDH in China.
2 Materials and methods
2.1 Data sources
Data were sourced from the Gansu Provincial Health and Health Commission, covering case records from January 2017 to June 2022 for Qingyang City Hospital of Chinese Medicine. Inclusion criteria included TCM diagnosis code International Classification of Disease (ICD)-10 M51.202 and TCM coding BNS150 (1995 version) or A03.06.04.06.01 (2021 version). Exclusion criteria involved length of stay less than 1 day or greater than 90 days, zero hospitalization cost, and logically inconsistent visit information, resulting in a final dataset of 2,857 valid cases.
The data were regularly validated and cleaned by qualified personnel, ensuring reliable quality for analysis. The dataset encompasses patient demographics, including sex, age, and marital status, alongside medical information including visit times, surgeries and operations, complications and comorbidities, medical costs, and length of stay.
To evaluate the impact of DRG reform on medical costs and length of stay for LDH patients in Chinese medicine hospitals, our study employed a quasi-experimental model for data analysis. As one of the pioneering tertiary Chinese medicine hospitals in Northwest China to implement DRG payment reform, this research is instrumental in advancing DRG reimbursement systems in the TCM sector.
2.2 Statistical analysis
To address healthcare economic costs, we used 2016 as the base year and adjusted relevant costs based on the Consumer Price Index (CPI) for healthcare in Gansu Province from 2017 to 2022, minimizing potential biases in the study. It is worth highlighting that Qingyang City in Gansu Province, began trial implementation of the DRG reimbursement system in October 1, 2019. Accordingly, the period from January 1, 2017 to September 30, 2019 is designated as the pre-reform phase, during which the medical insurance payment was implemented under the fee-for-service (FFS) model. In contrast, the period from October 1, 2019 to June 30, 2022 is defined as the post-reform phase, with the implementation of the DRG-based medical insurance payment method.
Next, we compared the basic characteristics of patient visits before and after the DRG reform. For normally distributed numerical variables, paired sample t-tests were used, reporting data as means and standard deviations. For non-normally distributed numerical variables, we applied the Wilcoxon rank-sum test, expressing results in median and quartiles. Categorical variables were analyzed using chi-square tests, with frequencies and percentages reported. Moreover, multiple linear regression and Spearman correlation analyses were performed to investigate determinants of hospitalization expenditures and length of stay, as well as inter-variable relationships.
Finally, we employed an interrupted time-series analysis (ITSA) model - a quasi-experimental method specifically designed to assess causal effects of interventions (e.g., policy changes, clinical practice implementations) on longitudinal data. This approach compares pre- versus post-intervention trends while controlling for underlying temporal patterns, thereby providing robust effect estimation (39–41). We applied ITSA to evaluate key healthcare cost indicators for LDH patients in Chinese medicine hospitals. The analysis included hospitalization cost, medical service cost, diagnostic cost, TCM treatment cost, Chinese medicine cost, Western medicine cost, and length of stay. This methodology facilitated a comprehensive investigation of the changes in these indicators before and after the DRG reform, with the model equation expressed as follows:
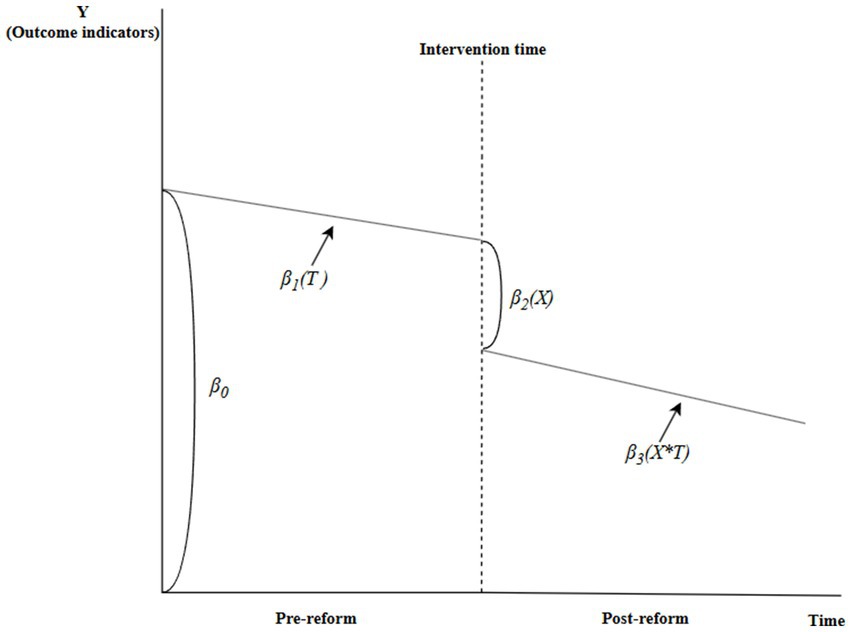
In this equation, is the dependent variable (the primary outcome), β0 is the intercept, β1 reflects the pre-reform trend, β2 indicates the level change at the reform, and β3 represents the difference in slopes between the post-reform and pre-reform periods, with the post-reform slope being the sum of β1 and β3. denotes the time series spanning January 2017 to June 2022, with T ranging from 1 to 66. Interaction terms include ,, , and , while denotes random error. To address the skewed distributions of healthcare costs and length of stay, we selected the median values for each month as the data for the interrupted time series analysis, ensuring the rigor of the analysis. A schematic of the model is shown in Figure 1.
We used the Cumby-Huizinga tests to assess the autocorrelation of the dependent variable and adjusted calculations using the ‘lag (#)’ command along with the Newey-West method (39, 40, 42). All statistical analyses were conducted using Excel 2019, SPSS 26.0, and Stata 15.0, with a significance level set at α = 0.05.
3 Results
3.1 General information of LDH hospitalized patients in Qingyang City Hospital of Chinese medicine in pre- and post-DRG reform
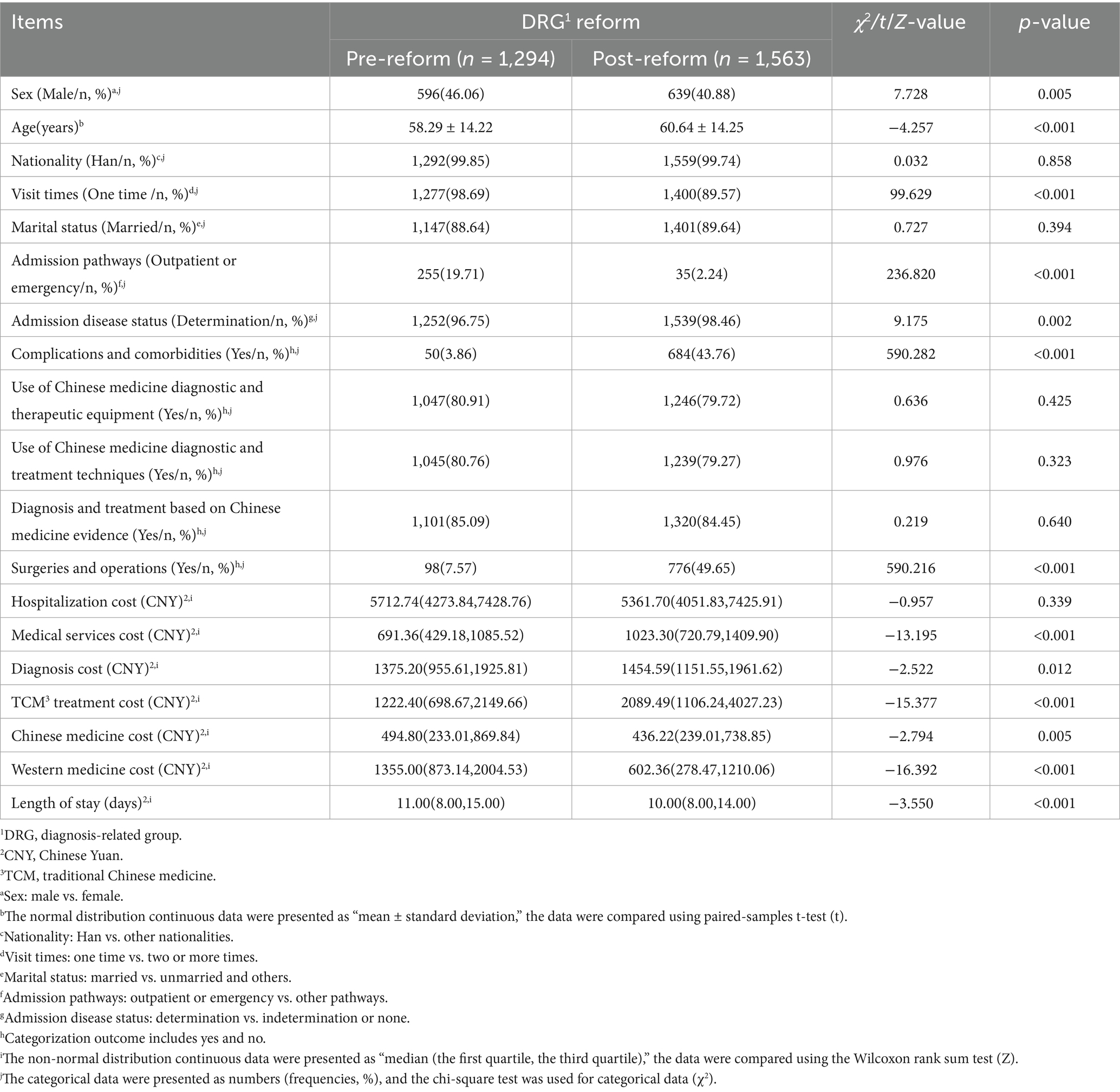
We included a total of 2,857 LDH patients in our analysis. Before the implementation of the DRG reform, there were 1,294 cases, with 46.06% of the patients being male and an average age (SD) of 58.29 (14.22) years. Following the DRG reform, the sample comprised 1,563 cases, with a male proportion of 40.88% and an average age (SD) of 60.64 (14.25) years. Further demographic details are provided in Table 1.
As shown in Table 1 and Figure 2, there were no statistical differences in nationality, marital status, use of Chinese medicine diagnostic and treatment techniques, use of Chinese medicine diagnostic and treatment techniques, diagnosis and treatment based on Chinese medicine evidence, and hospitalization cost among LDH patients pre- and post-DRG reforms (p > 0.05), but there were significant differences in sex, age, visit times, admission pathways, admission disease status, complications and comorbidities, surgeries and operations, medical services cost, diagnosis cost, TCM treatment cost, Chinese medicine cost, Western medicine cost and length of stay among LDH patients pre- and post-DRG reforms (p < 0.05).
3.2 Results of factors affecting LDH patients’ healthcare-related costs and length of stay in Qingyang City Hospital of Chinese medicine
To further investigate the factors influencing healthcare-related costs and length of stay in LDH patients, we constructed multiple linear regression models using hospitalization cost, medical service cost, diagnostic cost, TCM treatment cost, Chinese medicine cost, and Western medicine cost, and length of stay as dependent variables, with sex, age, nationality, and other general information as independent variables. Stepwise regression was employed for the analysis.
The regression results (Table 2) revealed that: hospitalization cost was significantly lower in patients using Chinese medicine diagnostic and therapeutic equipment (p < 0.05); medical service cost increased with complications, two or more times hospitalizations, use of Chinese medicine diagnostic and treatment technique, and post-DRG reform (p < 0.05); diagnostic cost decreased for patients with complications, younger patients, outpatient or emergency admissions, use of Chinese medicine diagnostic and therapeutic equipment, and no diagnosis and treatment based on Chinese medicine evidence (p < 0.05); TCM treatment cost was higher for complicated cases, females, two or more times hospitalizations, other pathways, determination disease status, use of Chinese medicine diagnostic and treatment techniques, and pre-DRG reform (p < 0.05); Chinese medicine cost decreased for uncomplicated cases, males, younger patients, no use of Chinese medicine diagnostic and treatment techniques, and post-DRG reform (p < 0.05); Western medicine cost increased for uncomplicated cases, older adults patients, one time hospitalizations, outpatient or emergency admissions, indetermination or none disease status, no use of Chinese medicine diagnostic and therapeutic equipment, and pre-DRG reform (p < 0.05); and length of stay was shorter for uncomplicated cases, older adults patients, one time hospitalizations, use of Chinese medicine diagnostic and therapeutic equipment, no use of Chinese medicine diagnostic and treatment techniques, and post-DRG reform (p < 0.05).
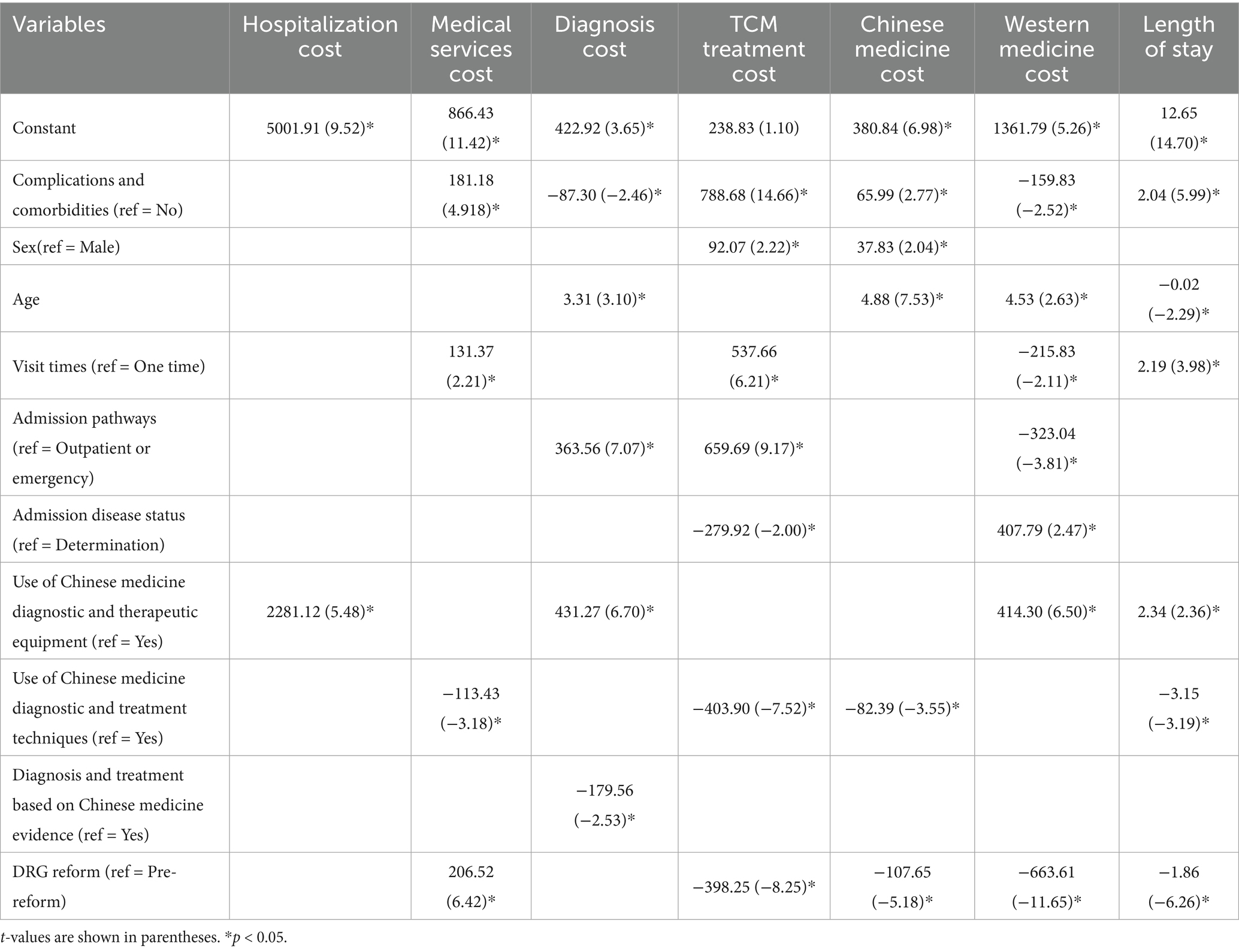
Table 2. Results of multiple linear regression analysis for healthcare-related costs and length of stay in LDH patients.
To further elucidate the correlations between hospitalization-related costs and length of stay, we conducted Spearman correlation analyses. The results demonstrated statistically significant positive correlations (p < 0.05) among all measured variables, including hospitalization cost, medical service cost, TCM treatment cost, Chinese medicine cost, Western medicine cost, and length of stay, indicating consistent directional trends across these parameters. Complete results are presented in Table 3.
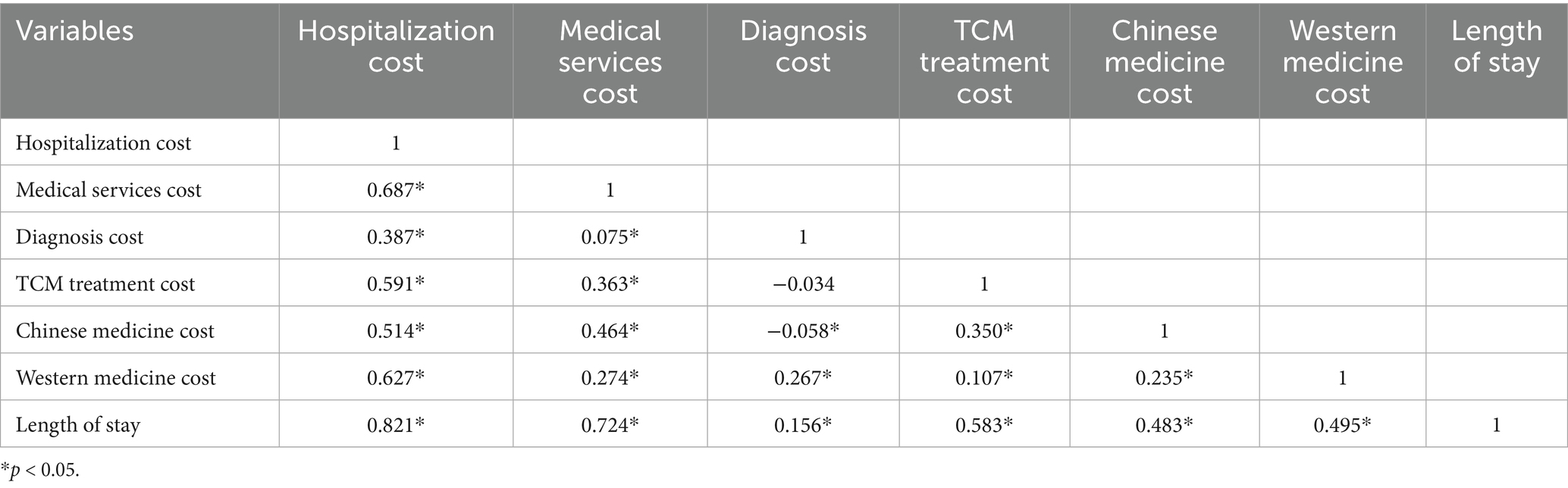
Table 3. Results of correlation analysis for healthcare-related costs and length of stay in LDH patients.
3.3 Results of ITSA of DRG reform on LDH patients’ healthcare-related costs in Qingyang City Hospital of Chinese medicine
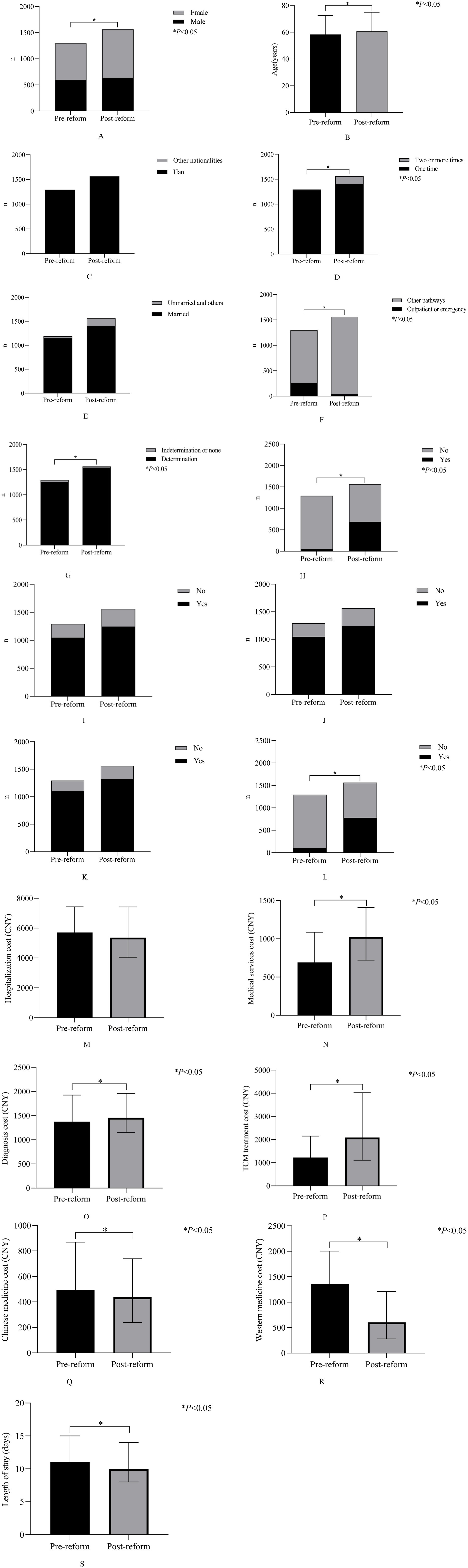
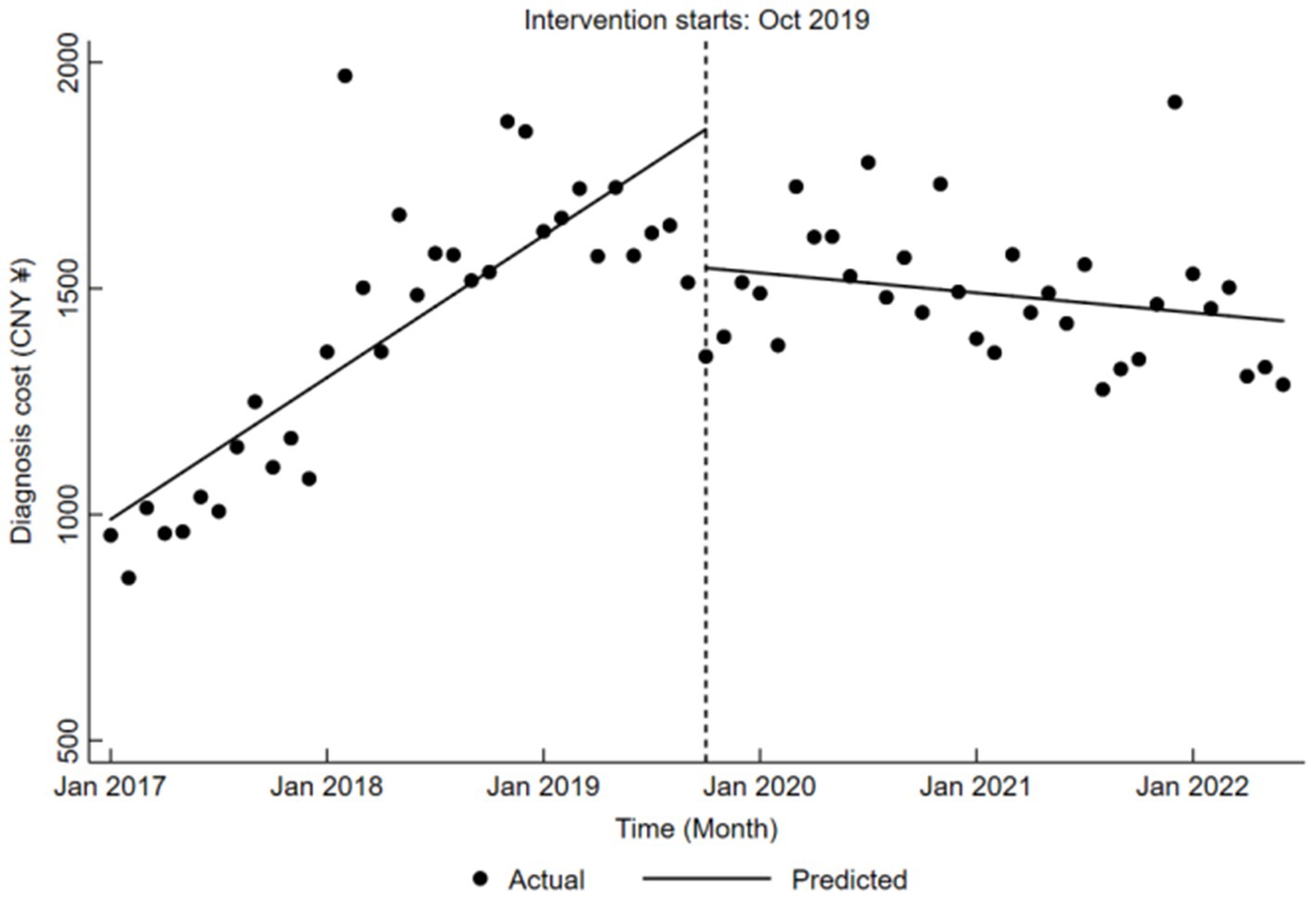
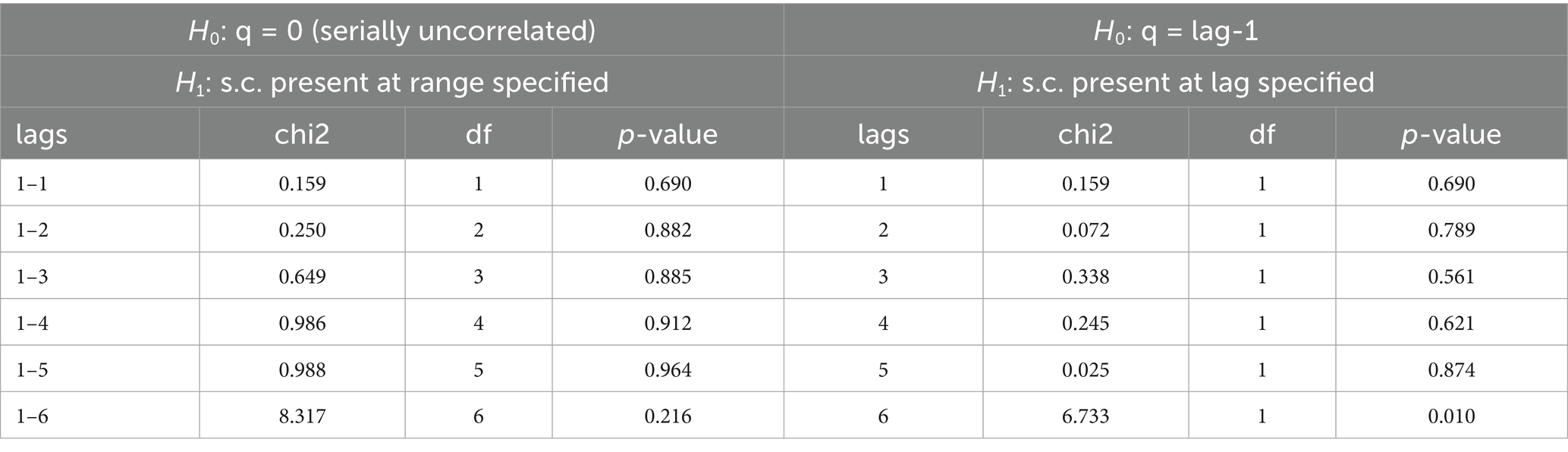
We performed Cumby-Huizinga autocorrelation tests on hospitalization cost, medical service cost, diagnostic cost, TCM treatment cost, Chinese medicine cost, and Western medicine cost. The results indicated that hospitalization cost, TCM treatment cost, and Chinese medicine cost exhibited no autocorrelation. However, diagnostic cost and Western medicine cost may demonstrate first-order autocorrelation, while medical service cost could indicate second-order autocorrelation, as summarized in Table 4. To ensure the robustness of our interrupted time-series analysis, we employed the ‘lag (1)’or ‘lag (2)’ command to adjust for autocorrelation effects in the medical costs analysis.
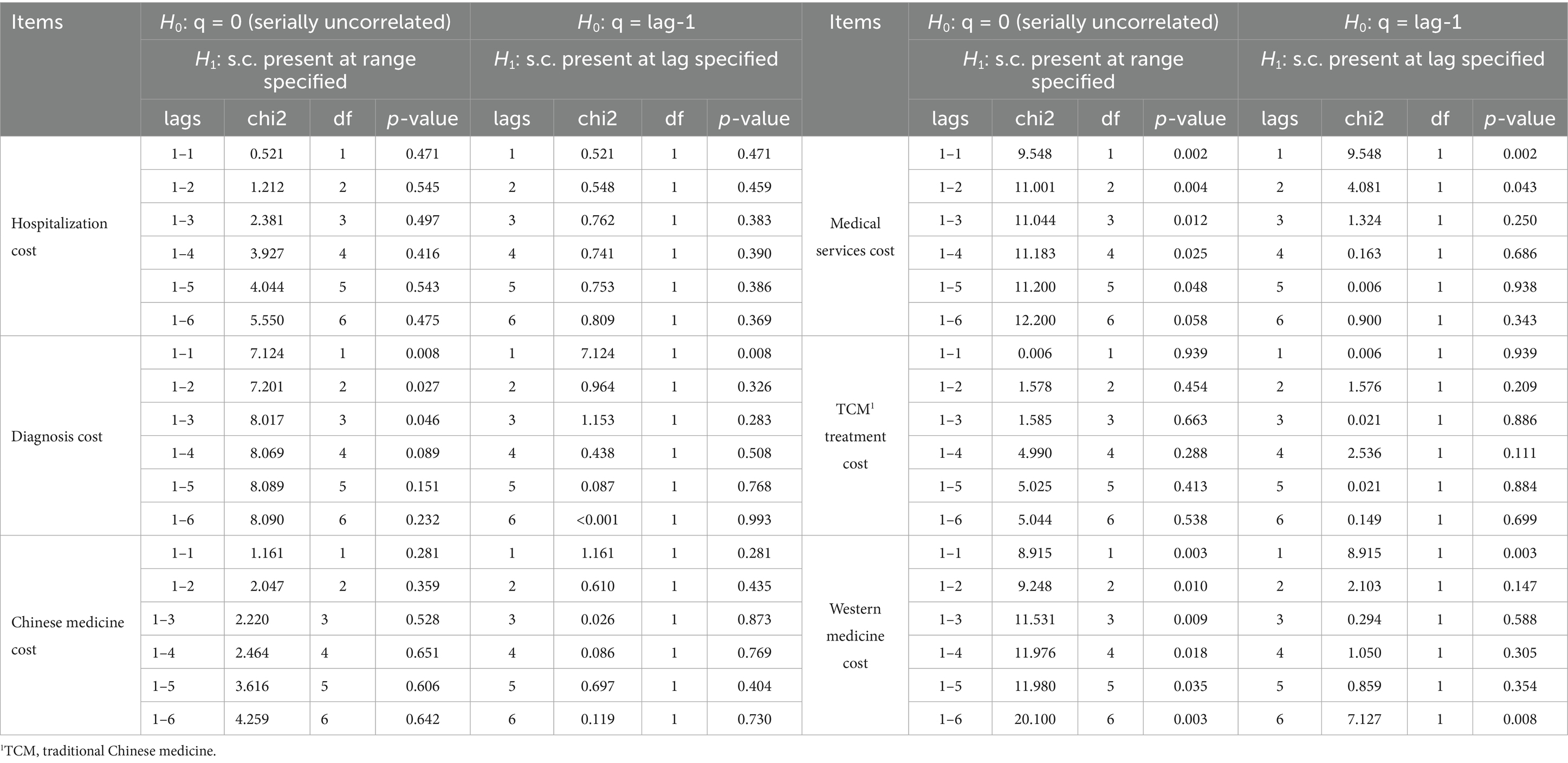
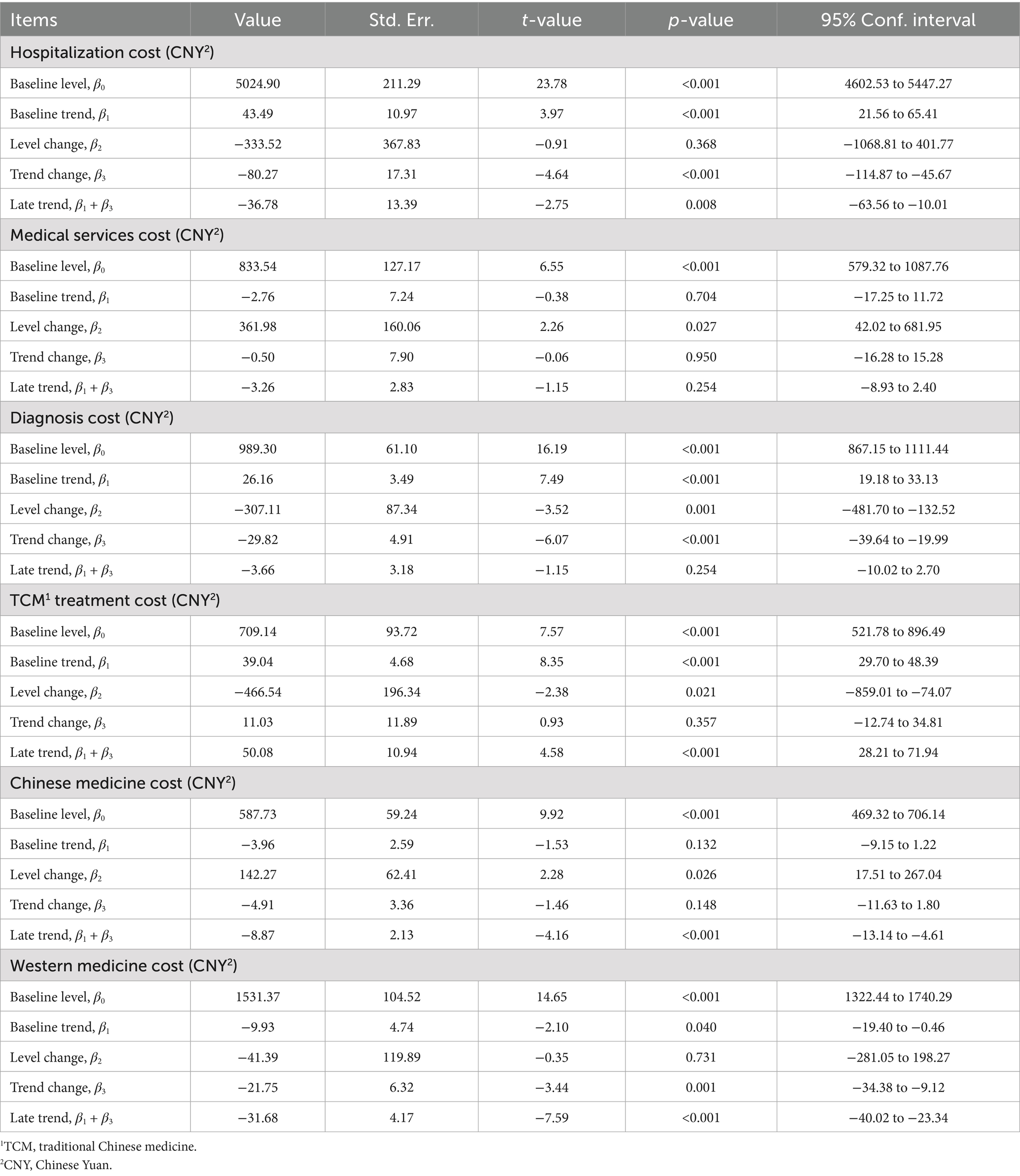
Before the DRG reform at Qingyang City Hospital of Chinese Medicine, hospitalization cost exhibited a significant upward trajectory, with an average monthly increase of CNY 43.49 (β₁ = 43.49, p < 0.05). Conversely, during the reform, fluctuations in hospitalization cost were not statistically significant (β₂ = −333.52, p > 0.05). Following the reform, however, cost demonstrated a pronounced downward trend, decreasing by an average of CNY 36.78 per month (β₁ + β₃ = −36.78, p < 0.05). Comprehensive results are presented in Table 5, and the corresponding trend changes are illustrated in Figure 3.
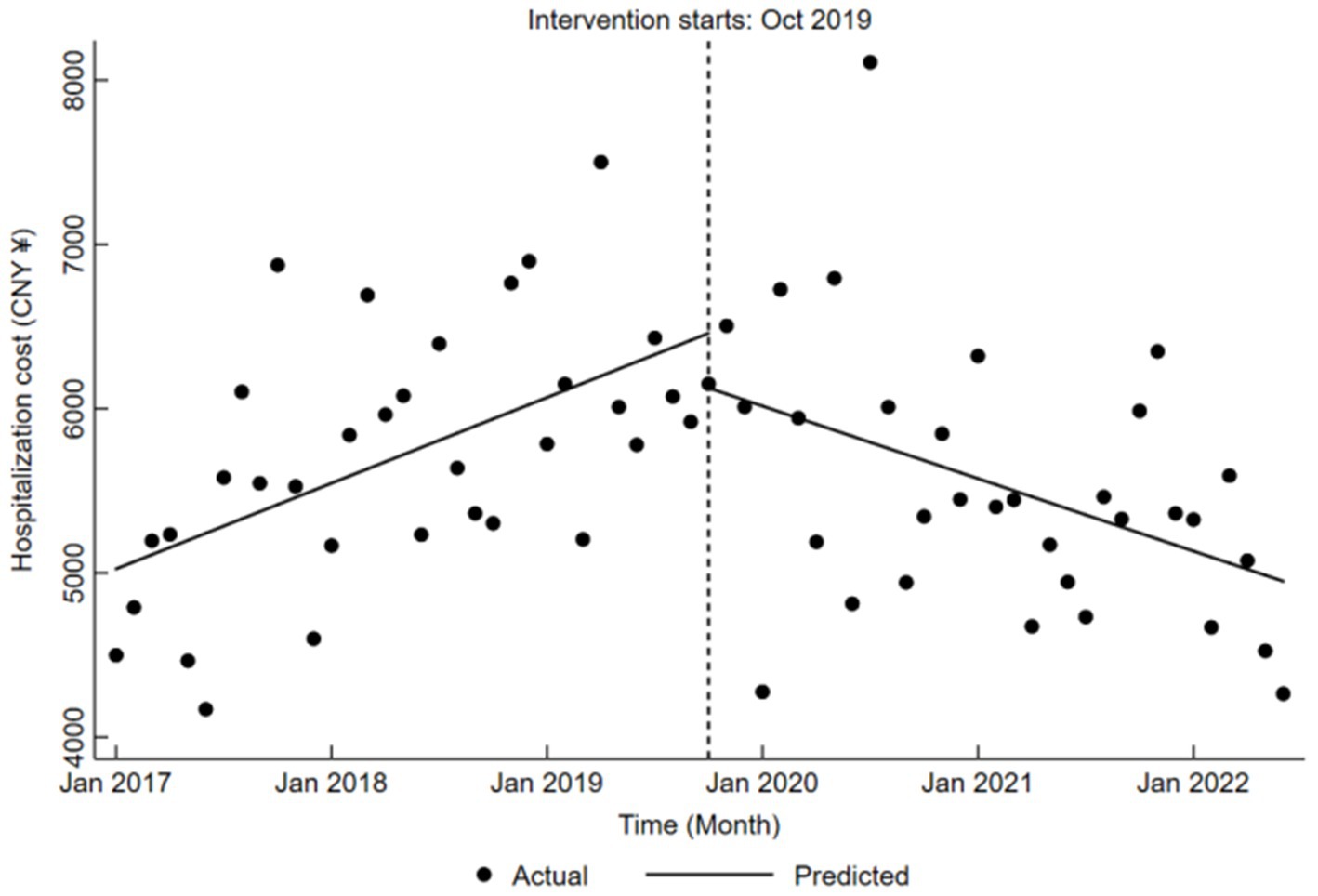
In terms of medical services cost, the pre-reform trend was not significant (β₁ = −2.76, p > 0.05). Nevertheless, during the reform, there was a substantial increase of CNY 361.98 (β₂ = 361.98, p < 0.05), while post-reform changes remained insignificant (β₁ + β₃ = −3.26, p > 0.05), as detailed in Table 5 and depicted in Figure 4.
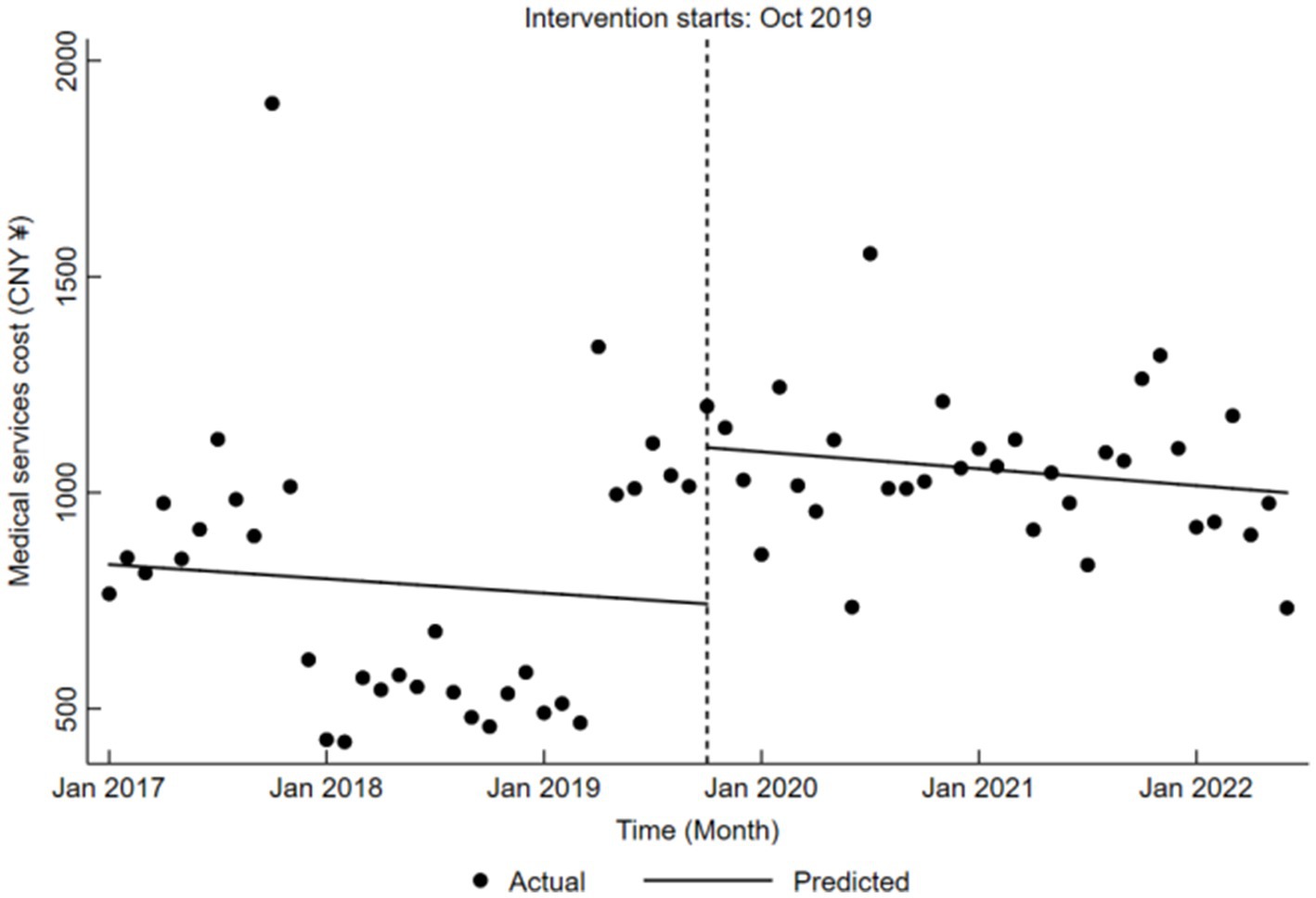
Regarding diagnosis cost, a clear upward trend was evident before the reform, with an average monthly increase of CNY 26.16 (β₁ = 26.16, p < 0.05). During the reform, diagnosis cost significantly decreased by CNY 307.11 (β₂ = −307.11, p < 0.05), yet the post-reform trend was again not significant (β₁ + β₃ = −3.66, p > 0.05), as outlined in Table 5 and shown in Figure 5.
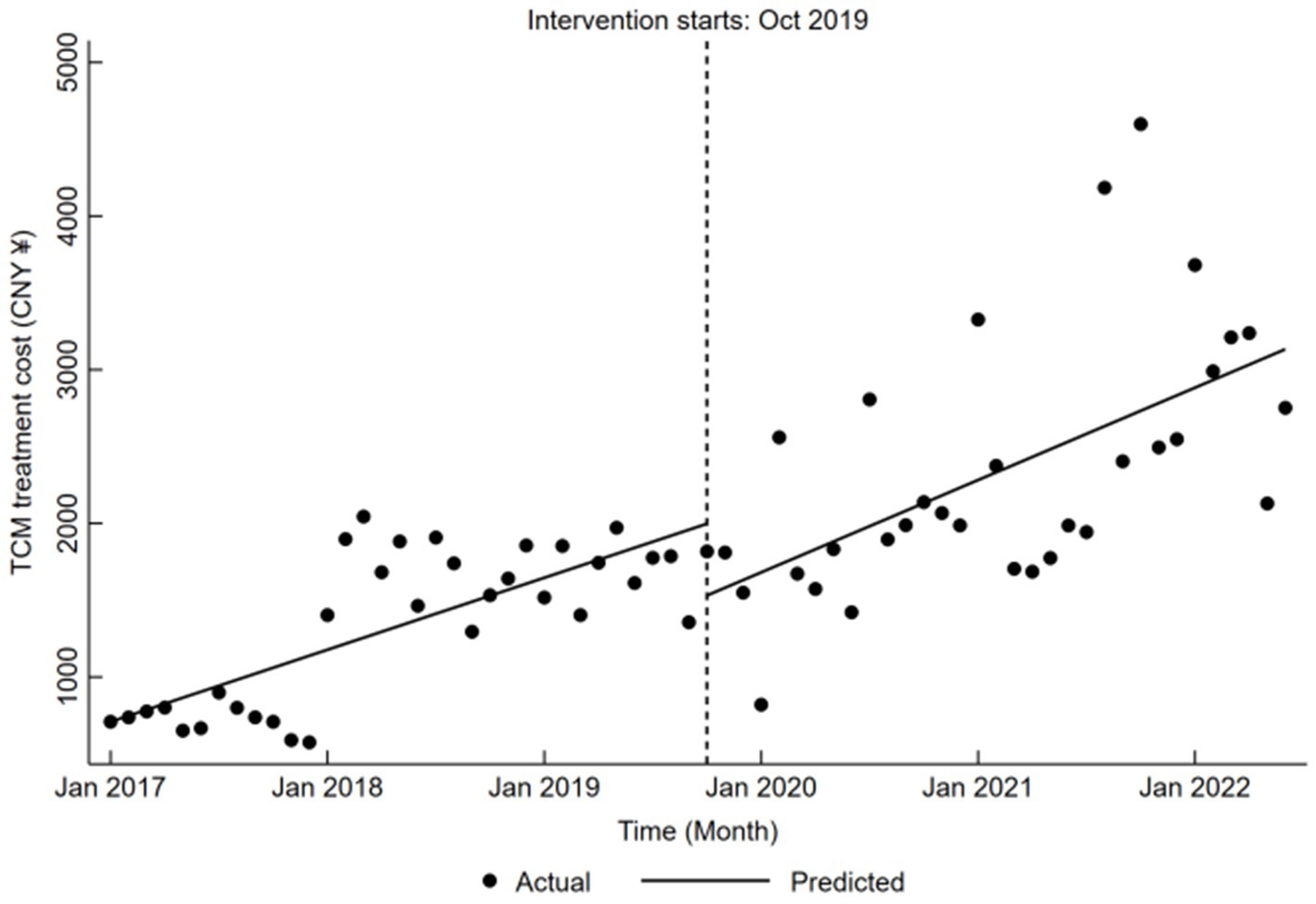
Concerning TCM treatment cost, there was a notable increase before the reform, averaging CNY 39.04 per month (β₁ = 39.04, p < 0.05). Following a significant decrease of CNY 466.54 during the reform (β₂ = −466.54, p < 0.05), the cost rebounded, displaying a clear upward trend post-reform, with an average increase of CNY 50.08 (β₁ + β₃ = 50.08, p < 0.05), as detailed in Table 5 and represented in Figure 6.
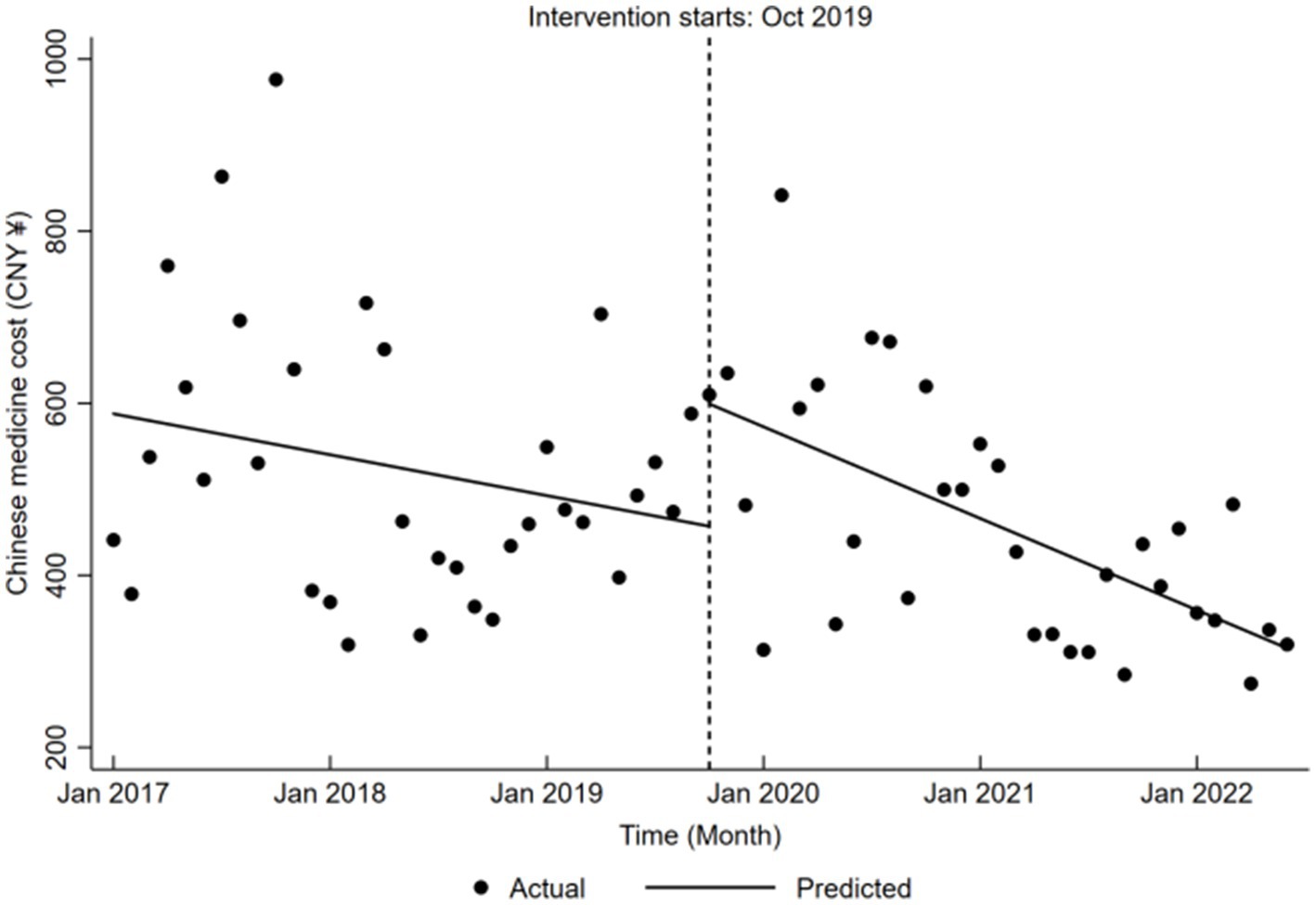
Chinese medicine cost exhibited no significant trend before the reform (β₁ = −3.96, p > 0.05). However, during the reform, the cost rose significantly by CNY 142.27 (β₂ = 142.27, p < 0.05), while post-reform expenses revealed a significant downward trend, decreasing by an average monthly of CNY 8.87 (β₁ + β₃ = −8.87, p < 0.05), as presented in Table 5 and illustrated in Figure 7.
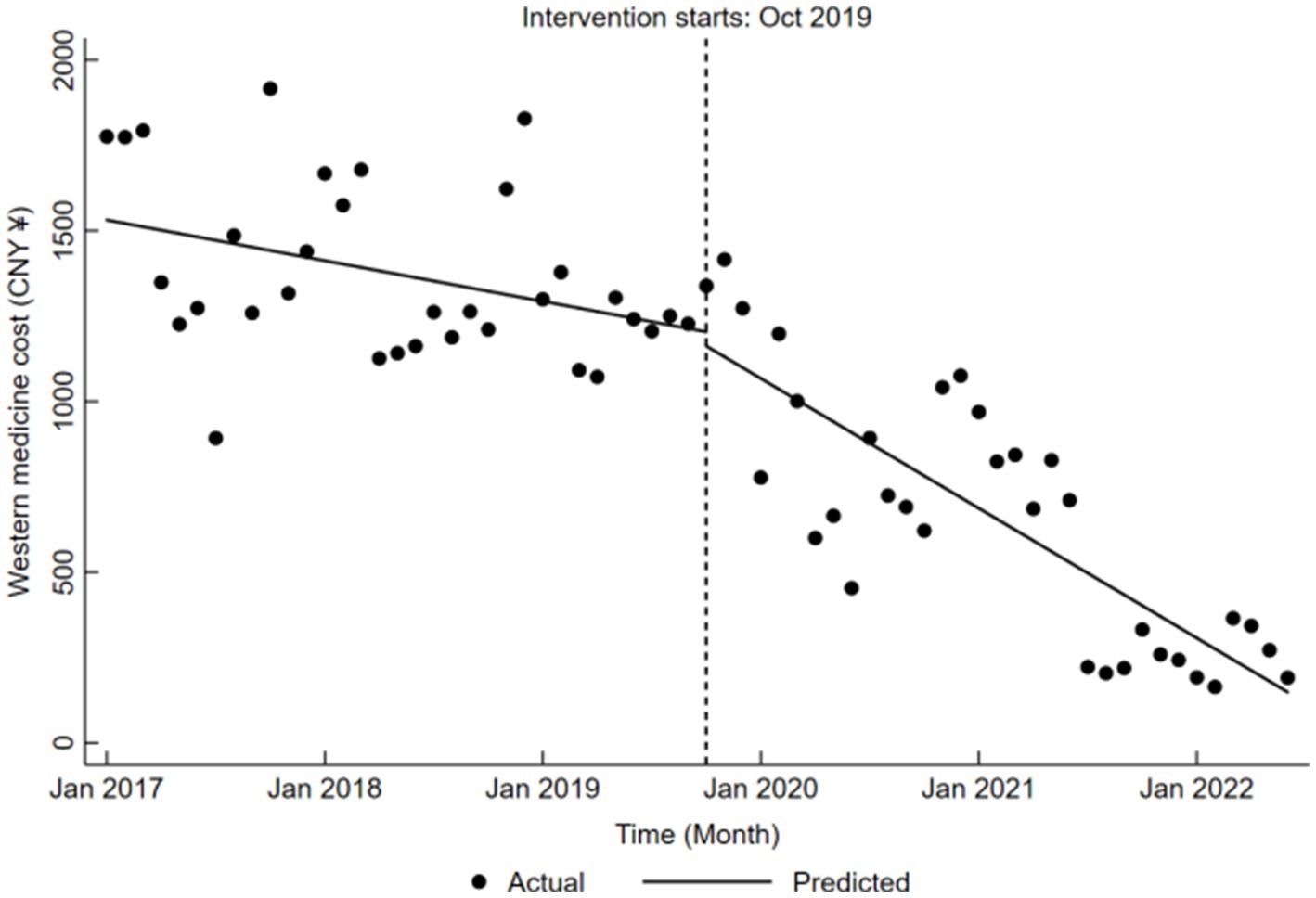
Finally, Western medicine cost showed a significant downward trend before the reform, decreasing by an average of CNY 9.93 (β₁ = −9.93, p < 0.05). Changes during the reform were not statistically significant (β₂ = −41.39, p > 0.05). However, the cost exhibited a marked downward trend, with an average monthly decrease of CNY 31.68 (β₁ + β₃ = −31.68, p < 0.05) post-reform, which was notably more pronounced than the pre-reform trend. Detailed results can be found in Table 5, with trend changes depicted in Figure 8.
3.4 Results of ITSA of DRG reform on length of stay in Qingyang City Hospital of Chinese medicine
We conducted a Cumby-Huizinga autocorrelation test on the length of stay, which revealed no evidence of autocorrelation, as presented in Table 6. This finding underscores the stability of the data regarding length of stay.
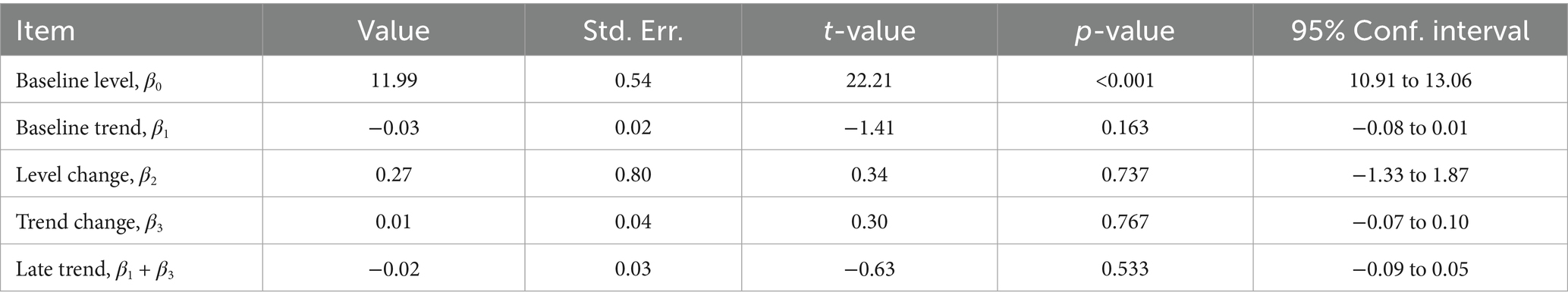
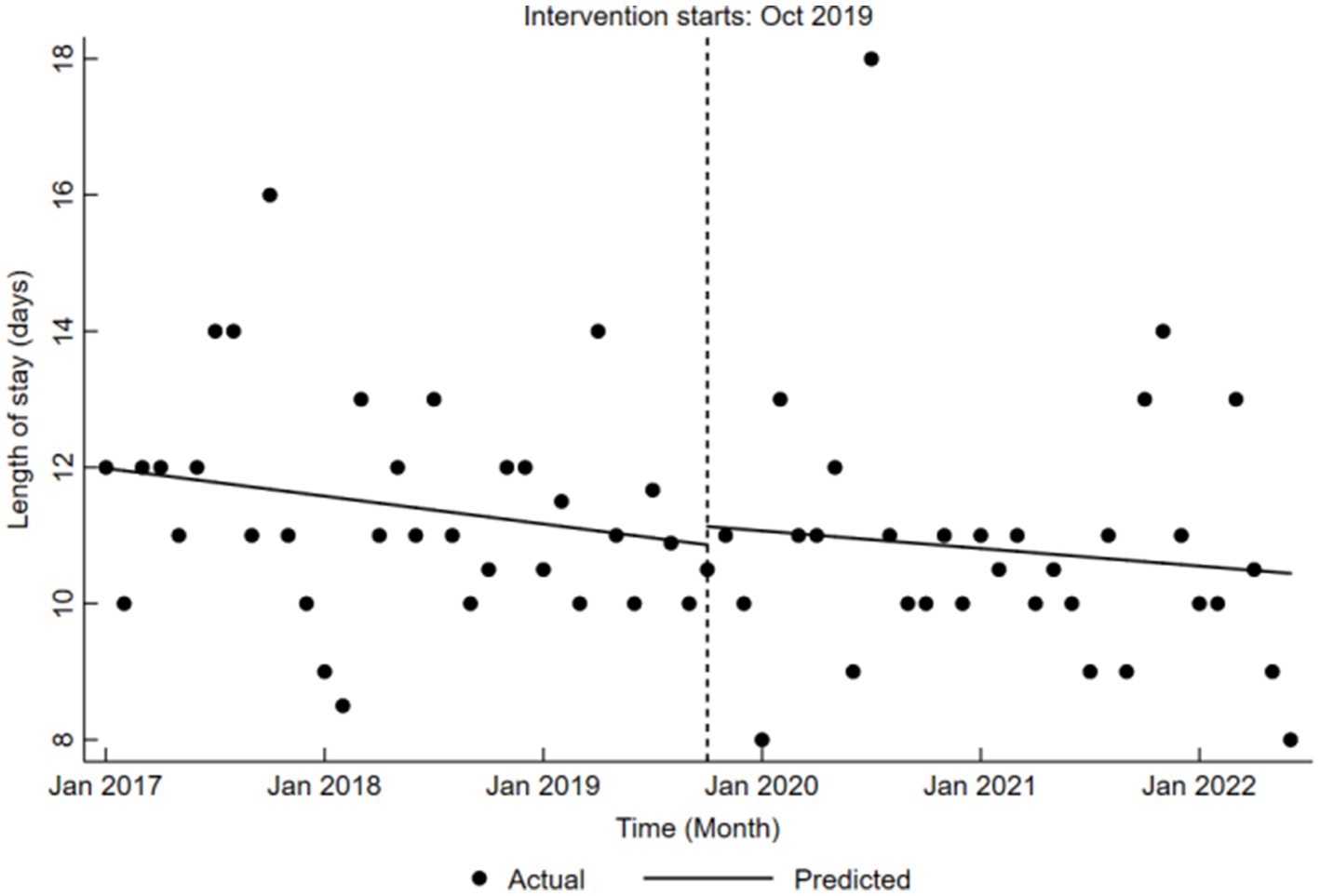
Pre-DRG reform, the trend in length of stay was not statistically significant, with a coefficient of β₁is −0.03 (p > 0.05). This lack of significance indicates that there were no noteworthy changes in the average length of stay during this period.
Similarly, the analysis of length of stay during the reform period also yielded insignificant results (β₂ = 0.27, p > 0.05), and post-reform trends remained unremarkable, as reflected in the combined coefficient (β₁ + β₃ = −0.02, p > 0.05). Detailed results are provided in Table 7, and the corresponding trend changes are illustrated in Figure 9, further emphasizing the consistency of length of stay across the study periods.
4 Discussion
We are the first to investigate the effects of the DRG reform on medical costs and length of stay for LDH patients in Chinese medicine hospitals. This study provides valuable insights into the ongoing reforms of DRG payment systems in TCM. Our univariate analysis revealed differences in patient characteristics before and after the reform, including sex, age, visit times, admission pathways, admission disease status, complications and comorbidities, and surgeries and operations. Post-reform, there was an increase in female patients, older patients, those admitted through other pathways, and patients with defined disease status, complications and comorbidities, and surgical needs. Notably, the proportion of patients admitted through other pathways and those with repeated hospitalizations also increased, suggesting that the reform measures have successfully attracted more patients and fostered repeat admissions to the hospital. The higher number of patients with defined disease status aligns with the reform’s objective of improving diagnostic precision. Additionally, the increase in patients with complications and operations needs suggests a rise in case complexity, potentially leading to higher reimbursement standards, which benefits the hospital departments during cost settlement.
Integrating the results of multiple linear regression and correlation analyses, we identified significant associations between healthcare-related costs and multiple factors including patient age, sex, complications and comorbidities, visit times, admission pathways, admission disease status, use of Chinese medicine diagnostic and therapeutic equipment, use of Chinese medicine diagnostic and treatment techniques, diagnosis and treatment based on Chinese medicine evidence, and DRG reform. Comprehensive analysis revealed that advanced age, presence of complications and comorbidities, and no use of Chinese medicine diagnostic and therapeutic equipment and use of Chinese medicine diagnostic and treatment techniques were associated with higher hospitalization costs, while DRG reform demonstrated cost-containment effects. Furthermore, a positive correlation was observed among healthcare-related costs and length of stay, suggesting that effective cost control for LDH patients requires comprehensive medication cost management coupled with appropriate reduction of length of stay.
The results from our interrupted time-series analysis indicate a significant downward trend in hospitalization cost, Chinese medicine cost, and Western medicine cost following the DRG reform. While the rising trend in diagnostic cost before the reform was curtailed, overall medical service cost increased post-reform, alongside a marked rise in TCM treatment cost. It is noteworthy that hospitalization cost for LDH patients changed significantly after the DRG reform, demonstrating a marked decrease that aligns with findings from various other studies (41, 43, 44). Certainly, the component costs of hospitalization, including those for Chinese and Western medicine, have concurrently declined alongside the overall reduction in hospitalization cost. However, diagnostic cost and medical service cost were higher post-reform than before, indicating that Chinese hospitals are leveraging their unique strengths by providing more specialized services to address patient needs. This aligns with the Chinese government’s objectives for DRG reform in TCM.
Interestingly, the length of stay for LDH patients did not decrease following the DRG reform, which stands in contrast to findings from several other studies (32, 45–47). What’s more, previous studies suggest that length of stay is a critical factor influencing hospitalization cost, implying that a significant cost reduction should typically accompany shorter stay (48–50). The absence of a reduction in length of stay, despite the cost reduction, may be related to the unique characteristics of TCM treatment, which often has a slower onset of effects and fewer side effects. The relatively prolonged treatment duration for LDH in TCM is inherently difficult to substantially reduce, which is fundamentally associated with TCM’s diagnostic and therapeutic paradigm. First, this stems from TCM’s holistic therapeutic philosophy that necessitates simultaneous management of both pain symptoms and underlying pathological mechanisms (e.g., kidney deficiency, qi-blood stagnation). Second, it reflects the characteristic therapeutic modalities of TCM: acupuncture requires cumulative sessions to activate the endogenous analgesic system, while Chinese herbal compounds need time for multi-target regulation of inflammation and tissue repair. Third, TCM manual therapies follow the natural tissue repair cycle requirements. Although TCM demonstrates a relatively slower onset of therapeutic effects, clinical evidence confirms its superior medium-to-long-term efficacy for LDH management. The majority of TCM treatment occurs in the initial days of hospitalization, suggesting that later cost may be lower, making it challenging to significantly reduce recovery times through DRG payment reforms alone. However, integrating and standardizing TCM treatment methods, along with reducing medication usage, could help achieve the goal of lowering hospitalization cost.
In conclusion, the reform of DRG payment system in TCM has a substantial impact on controlling overall medical costs for LDH patients, although its effectiveness in reducing the length of stay remains limited. Future refinements of the DRG payment system should account for the distinctive characteristics of TCM, optimizing treatment methods and enhancing the quality of healthcare. Establishing a unique and effective reimbursement framework for TCM will further reduce patient treatment cost and length of stay, ultimately benefiting a greater number of patients.
5 Conclusion
DRG reform is associated with lower hospitalization cost, as well as reduced costs for both Chinese and Western medicine among LDH patients in Chinese medicine hospitals. However, it does not correlate with reductions in medical services cost, diagnostic cost, TCM treatment cost, or length of stay. While the reform effectively leverages the unique strengths of TCM to alleviate the economic burden of illness, there is a need to deepen institutional reforms and enhance the quality and content of medical services, with the goal of further reducing healthcare costs and shortening hospitalization durations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
M-eC: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. Y-hW: Data curation, Writing – original draft, Formal analysis. JY: Data curation, Writing – original draft, Formal analysis. S-jX: Project administration, Writing – review & editing, Investigation, Methodology. X-xZ: Writing – original draft, Methodology, Data curation. YW: Data curation, Methodology, Writing – original draft, Project administration. Y-sY: Writing – original draft, Resources, Software. XJ: Writing – original draft, Software, Methodology. H-nS: Software, Resources, Writing – original draft. G-pW: Writing – review & editing, Data curation, Formal analysis. J-yW: Writing – original draft, Formal analysis, Data curation, Validation. T-zC: Investigation, Project administration, Writing – original draft. F-xK: Software, Writing – original draft, Supervision, Project administration. H-jH: Formal analysis, Data curation, Writing – original draft, Visualization. J-yY: Resources, Supervision, Writing – review & editing, Software. Z-wW: Software, Writing – review & editing, Conceptualization, Resources, Validation, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the State Administration of Traditional Chinese Medicine (SACM), China (grant no. ZYZB-2023-435 and no. GZY-FJS-2022-045).
Acknowledgments
We thank the Gansu Provincial Health and Wellness Commission for data support for our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1631872/full#supplementary-material
References
1. Hartvigsen, J, Hancock, MJ, Kongsted, A, Louw, Q, Ferreira, ML, Genevay, S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391:2356–67. doi: 10.1016/s0140-6736(18)30480-x
2. Manuela, LF, Katie, DL, Lydia, MH, Jaimie, DS, Garland, TC, Marita, C, et al. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. (2023) 5:e316–29. doi: 10.1016/s2665-9913(23)00098-x
3. Theo, V, Christine, A, Megha, A, Ryan, MB, Zulfiqar, AB, Alexandria, B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/s0140-6736(16)31678-6
4. Chen, S, Chen, M, Wu, X, Lin, S, Tao, C, Cao, H, et al. Global, regional and national burden of low back pain 1990-2019: a systematic analysis of the global burden of disease study 2019. J Orthop Translat. (2022) 32:49–58. doi: 10.1016/j.jot.2021.07.005
5. Chen, N, Fong, DYT, and Wong, JYH. The global health and economic impact of low-back pain attributable to occupational ergonomic factors in the working-age population by age, sex, and geography in 2019. Scand J Work Environ Health. (2023) 49:487–95. doi: 10.5271/sjweh.4116
6. China National Health Commission. China health statistics yearbook 2023. Beijing: Peking Union Medical College Press (2023).
7. Buchbinder, R, van Tulder, M, Öberg, B, Costa, LM, Woolf, A, Schoene, M, et al. Low back pain: a call for action. Lancet. (2018) 391:2384–8. doi: 10.1016/s0140-6736(18)30488-4
8. Hoy, D, March, L, Brooks, P, Blyth, F, Woolf, A, Bain, C, et al. The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. (2014) 73:968–74. doi: 10.1136/annrheumdis-2013-204428
9. Zhou, M, Theologis, AA, and O’Connell, GD. Understanding the etiopathogenesis of lumbar intervertebral disc herniation: from clinical evidence to basic scientific research. JOR Spine. (2024) 7:e1289. doi: 10.1002/jsp2.1289
10. Yang, H, Liu, H, Li, Z, Zhang, K, Wang, J, Wang, H, et al. Low back pain associated with lumbar disc herniation: role of moderately degenerative disc and annulus fibrous tears. Int J Clin Exp Med. (2015) 8:1634–44.
11. Dieleman, JL, Cao, J, Chapin, A, Chen, C, Li, Z, Liu, A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. (2020) 323:863–84. doi: 10.1001/jama.2020.0734
12. Katz, JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. (2006) 88:21–4. doi: 10.2106/jbjs.E.01273
13. Hong, J, Reed, C, Novick, D, and Happich, M. Costs associated with treatment of chronic low back pain: an analysis of the UK general practice research database. Spine (Phila Pa 1976). (2013) 38:75–82. doi: 10.1097/BRS.0b013e318276450f
14. Carregaro, RL, Tottoli, CR, Rodrigues, DDS, Bosmans, JE, da Silva, EN, and van Tulder, M. Low back pain should be considered a health and research priority in Brazil: lost productivity and healthcare costs between 2012 to 2016. PLoS One. (2020) 15:e0230902. doi: 10.1371/journal.pone.0230902
15. Lambeek, LC, van Tulder, MW, Swinkels, IC, Koppes, LL, Anema, JR, and van Mechelen, W. The trend in total cost of back pain in the Netherlands in the period 2002 to 2007. Spine (Phila Pa 1976). (2011) 36:1050–8. doi: 10.1097/BRS.0b013e3181e70488
16. Alonso-García, M, and Sarría-Santamera, A. The economic and social burden of low Back pain in Spain: a National Assessment of the economic and social impact of low Back pain in Spain. Spine (Phila Pa 1976). (2020) 45:E1026–e1032. doi: 10.1097/brs.0000000000003476
17. Yang, Y, Lai, X, Li, C, Yang, Y, Gu, S, Hou, W, et al. Focus on the impact of social factors and lifestyle on the disease burden of low back pain: findings from the global burden of disease study 2019. BMC Musculoskelet Disord. (2023) 24:679. doi: 10.1186/s12891-023-06772-5
18. Liang, H, and Huang, J. Case report: spontaneous regression of extruded lumbar disc herniation with acupuncture therapy. Front Neurol. (2024) 15:1381292. doi: 10.3389/fneur.2024.1381292
19. Chou, R, Côté, P, Randhawa, K, Torres, P, Yu, H, Nordin, M, et al. The global spine care initiative: applying evidence-based guidelines on the non-invasive management of back and neck pain to low- and middle-income communities. Eur Spine J. (2018) 27:851–60. doi: 10.1007/s00586-017-5433-8
21. Knezevic, NN, Candido, KD, Vlaeyen, JWS, Van Zundert, J, and Cohen, SP. Low back pain. Lancet. (2021) 398:78–92. doi: 10.1016/s0140-6736(21)00733-9
22. Skljarevski, V, Ossanna, M, Liu-Seifert, H, Zhang, Q, Chappell, A, Iyengar, S, et al. A double-blind, randomized trial of duloxetine versus placebo in the management of chronic low back pain. Eur J Neurol. (2009) 16:1041–8. doi: 10.1111/j.1468-1331.2009.02648.x
23. Chaparro, LE, Furlan, AD, Deshpande, A, Mailis-Gagnon, A, Atlas, S, and Turk, DC. Opioids compared to placebo or other treatments for chronic low-back pain. Cochrane Database Syst Rev. (2013) 2013:Cd004959. doi: 10.1002/14651858
24. Deyo, RA, Von Korff, M, and Duhrkoop, D. Opioids for low back pain. BMJ. (2015) 350:g6380. doi: 10.1136/bmj.g6380
25. Zhang, B, Xu, H, Wang, J, Liu, B, and Sun, G. A narrative review of non-operative treatment, especially traditional Chinese medicine therapy, for lumbar intervertebral disc herniation. Biosci Trends. (2017) 11:406–17. doi: 10.5582/bst.2017.01199
26. Wang, CA, Zhao, HF, Ju, J, Kong, L, Sun, CJ, Zheng, YK, et al. Reabsorption of intervertebral disc prolapse after conservative treatment with traditional Chinese medicine: a case report. World J Clin Cases. (2023) 11:2308–14. doi: 10.12998/wjcc.v11.i10.2308
27. Huang, SR, Pan, LD, Ma, YW, Wang, ZJ, Chen, YY, and Yu, ZX. Research on community promotion and application of single acupoint electroacupuncture therapy for lumbar intervertebral disc herniation. Zhongguo Zhen Jiu. (2021) 41:391–4. doi: 10.13703/j.0255-2930.20200409-k0001
28. Sun, C, Sun, K, Wang, S, Wang, Y, Yuan, P, Li, Z, et al. Effect of Baimai ointment on lumbar disc herniation: a multicentre, prospective, randomised, double-blind, placebo-controlled trial. Phytomedicine. (2024) 122:155138. doi: 10.1016/j.phymed.2023.155138
29. Fetter, RB, Shin, Y, Freeman, JL, Averill, RF, and Thompson, JD. Case mix definition by diagnosis-related groups. Med Care. (1980) 18:1–53.
30. Chok, L, Bachli, EB, Steiger, P, Bettex, D, Cottini, SR, Keller, E, et al. Effect of diagnosis related groups implementation on the intensive care unit of a Swiss tertiary hospital: a cohort study. BMC Health Serv Res. (2018) 18:84. doi: 10.1186/s12913-018-2869-4
31. Messerle, R, and Schreyögg, J. Country-level effects of diagnosis-related groups: evidence from Germany’s comprehensive reform of hospital payments. Eur J Health Econ. (2024) 25:1013–30. doi: 10.1007/s10198-023-01645-z
32. Cid, C, Dawson, N, Medina, C, Espinoza, A, and Bastías, G. Using diagnosis-related groups in Chile: lessons and challengesLições e desafios do uso de grupos de diagnósticos relacionados no Chile. Rev Panam Salud Publica. (2024) 48:e67. doi: 10.26633/rpsp.2024.67
33. Choi, JW, Kim, SJ, Park, HK, Jang, SI, Kim, TH, and Park, EC. Effects of a mandatory DRG payment system in South Korea: analysis of multi-year nationwide hospital claims data. BMC Health Serv Res. (2019) 19:776. doi: 10.1186/s12913-019-4650-8
34. Milstein, R, and Schreyögg, J. The end of an era? Activity-based funding based on diagnosis-related groups: a review of payment reforms in the inpatient sector in 10 high-income countries. Health Policy. (2024) 141:104990. doi: 10.1016/j.healthpol.2023.104990
35. Meng, Z, Hui, W, Cai, Y, Liu, J, and Wu, H. The effects of DRGs-based payment compared with cost-based payment on inpatient healthcare utilization: a systematic review and meta-analysis. Health Policy. (2020) 124:359–67. doi: 10.1016/j.healthpol.2020.01.007
36. Kahn, KL, Keeler, EB, Sherwood, MJ, Rogers, WH, Draper, D, Bentow, SS, et al. Comparing outcomes of care before and after implementation of the DRG-based prospective payment system. JAMA. (1990) 264:1984–8.
37. Busse, R, Geissler, A, Aaviksoo, A, Cots, F, Häkkinen, U, Kobel, C, et al. Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ. (2013) 346:f3197. doi: 10.1136/bmj.f3197
38. China National Healthcare Security Administration. Notice regarding the publication of the list of national pilot cities for DRG payment. (2019). Available online at: https://www.nhsa.gov.cn/art/2019/6/5/art_37_1362.html. Accessed Oct 25, 2024.
39. Baum, C, and Schaffer, M. ACTEST: Stata module to perform Cumby-Huizinga general test for autocorrelation in time series. Boston: Mark Schaffer (2015).
40. Linden, A. A comprehensive set of postestimation measures to enrich interrupted time-series analysis. Stata J. (2017) 17:73–88. doi: 10.1177/1536867x1701700105
41. Lin, K, Li, Y, Yao, Y, Xiong, Y, and Xiang, L. The impact of an innovative payment method on medical expenditure, efficiency, and quality for inpatients with different types of medical insurance: evidence from a pilot city, China. Int J Equity Health. (2024) 23:115. doi: 10.1186/s12939-024-02196-2
42. China National Healthcare Security Administration. Notice on the issuance of the three-year action plan for DRG/DIP payment reform. (2019). Available online at: https://www.gov.cn/zhengce/zhengceku/2021-11/28/content_5653858.htm#:~:text=DRG/DI. Accessed Oct 25, 2024.
43. Wang, S, Wu, N, Wang, H, Zhang, X, Li, F, Wang, X, et al. Impacts of a new diagnosis-related group point payment system on children’s medical services in China: length of stay and costs. Int J Health Plann Manag. (2024) 39:432–46. doi: 10.1002/hpm.3739
44. Liu, Y, Du, S, Cao, J, Niu, H, Jiang, F, and Gong, L. Effects of a diagnosis-related group payment reform on length and costs of hospitalization in Sichuan, China: a synthetic control study. Risk Manag Healthc Policy. (2024) 17:1623–37. doi: 10.2147/rmhp.S463276
45. Chen, YJ, Zhang, XY, Yan, JQ, Xue, T, Qian, MC, and Ying, XH. Impact of diagnosis-related groups on inpatient quality of health care: a systematic review and meta-analysis. Inquiry. (2023) 60:469580231167011. doi: 10.1177/00469580231167011
46. Hamada, H, Sekimoto, M, and Imanaka, Y. Effects of the per diem prospective payment system with DRG-like grouping system (DPC/PDPS) on resource usage and healthcare quality in Japan. Health Policy. (2012) 107:194–201. doi: 10.1016/j.healthpol.2012.01.002
47. Wu, Y, Fung, H, Shum, HM, Zhao, S, Wong, EL, Chong, KC, et al. Evaluation of length of stay, care volume, in-hospital mortality, and emergency readmission rate associated with use of diagnosis-related groups for internal resource allocation in public hospitals in Hong Kong. JAMA Netw Open. (2022) 5:e2145685. doi: 10.1001/jamanetworkopen.2021.45685
48. Chen, M, Kong, F, Su, B, Wei, X, and Yang, J. Factors influencing hospitalization cost for diabetic patients in traditional Chinese medicine hospitals in Qingyang City, China. Int J Environ Res Public Health. (2022) 19:13859. doi: 10.3390/ijerph192113859
49. Hou, HJ, Cong, TZ, Cai, Y, Ba, YH, Chen, ME, Yang, JY, et al. Influencing factors of hospitalization cost of hypertension patients in traditional Chinese medicine hospitals. Front Public Health. (2024) 12:1329768. doi: 10.3389/fpubh.2024.1329768
50. Chen, M, Yang, J, Hou, H, Zheng, B, Xia, S, Wang, Y, et al. Analysis of factors influencing hospitalization cost of patients with distal radius fractures: an empirical study based on public traditional Chinese medicine hospitals in two cities, China. BMC Health Serv Res. (2024) 24:605. doi: 10.1186/s12913-024-10953-w
Keywords: LDH, DRG, TCM, hospitalization cost, Chinese medicine hospitals
Citation: Chen M-e, Wang Y-h, Yu J, Xia S-j, Zhang X-x, Wang Y, Yuan Y-s, Jia X, Sun H-n, Wu G-p, Wang J-y, Cong T-z, Kong F-x, Hou H-j, Yang J-y and Wang Z-w (2025) Unpacking the cost implications of diagnosis-related groups reform for lumbar disc herniation patients in Chinese medicine: a closer look at evidence from China. Front. Public Health. 13:1631872. doi: 10.3389/fpubh.2025.1631872
Edited by:
Jing Yuan, Fudan University, ChinaReviewed by:
Yuehui Zhang, Shanghai Jiao Tong University, ChinaZhongcheng An, Zhejiang Chinese Medical University, China
Copyright © 2025 Chen, Wang, Yu, Xia, Zhang, Wang, Yuan, Jia, Sun, Wu, Wang, Cong, Kong, Hou, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhi-wei Wang, d3p3OTkwMkAxMjYuY29t
 Meng-en Chen
Meng-en Chen Yu-han Wang2
Yu-han Wang2 Jia-yi Wang
Jia-yi Wang Hao-jia Hou
Hao-jia Hou