- 1Department of First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 2School of Laboratory Animal & Shandong Laboratory Animal Center, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, China
- 3Department of Traditional Chinese Medicine, Jining First People's Hospital, Jining, Shandong, China
- 4Department of Cardiology, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 5Peripheral Vascular Department, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 6Department of Cardiology, Qufu Hospital of Traditional Chinese Medicine, Jining, Shandong, China
Background: As a new obesity-related index, the weight-adjusted waist circumference index (WWI) seems to be a good predictor of cognitive decline in hypertensive patients. This study aimed to verify the relationship between WWI and cognitive decline in Chinese hypertensive patients.
Methods: Data were obtained from the Hypertension Follow-up System of Shandong Province. WWI was calculated by dividing waist circumference by the square root of body weight, and cognitive decline was judged based on Mini-Mental State Examination (MMSE) scale scores. Multivariate logistic regression models and subgroup analyses were used to assess the relationship between WWI and cognitive decline in hypertensive patients.
Results: A total of 2,204 participants were included. There was a positive association between WWI and cognitive decline in hypertension (HCD). After adjusting for all covariates, a one-unit increase in WWI was associated with a 12% increase in the risk of cognitive decline in hypertensive patients (OR: 1.12, 95%CI: 1.04–1.21). In addition, the multivariable-adjusted OR for the highest quartile (11.16–16.76) compared with the lowest quartile of WWI (7.00–10.11) was 1.61 (95% CI: 1.30–2.00).
Conclusion: In Chinese hypertensive patients, high levels of WWI were significantly associated with an increased risk of cognitive decline. This finding suggests that WWI may be an indicator of the risk of cognitive decline affecting hypertensive patients.
Introduction
The relationship between hypertension and cognitive decline is garnering increasing attention. Hypertension is not only a significant risk factor for cardiovascular disease but may also contribute to cognitive deterioration. Research has demonstrated that hypertensive patients face a markedly elevated risk of cognitive decline attributable to various etiologies, encompassing vascular dementia and Alzheimer’s disease (1–3). In a study involving women, those with hypertension who did not effectively manage their blood pressure exhibited a 30% higher risk of cognitive decline compared to untreated patients with well-controlled blood pressure (4).
The social burden of hypertension accompanied by cognitive decline is significant and cannot be ignored. As ages, cognitive decline not only diminishes the quality of life for patients (5), but also places significant strain on families and the broader community (6). Moreover, hypertension associated with cognitive decline is recognized as a critical factor influencing all-cause mortality among the older adults. Studies have shown that patients with both cognitive impairment and hypertension have an increased risk of all-cause death compared to patients with only cognitive impairment or hypertension (7). Consequently, there is an urgent need to identify a variable and measurable indicator that can help reduce the incidence of cognitive decline in individuals with hypertension.
Park et al. proposed the weight-adjusted waist circumference index (WWI) as a novel measurement in 2018 (8, 9). Unlike the body mass index (BMI) or waist circumference (WC), WWI considers the relationship between waist circumference and body weight, offering a more comprehensive understanding of body fat distribution (10). WWI was calculated as WC (cm) divided by the square root of weight (kg) (9), because the calculation of WWI only needs to measure waist circumference and weight, and the data is easy to obtain, it is suitable for large-scale epidemiological investigation and clinical screening. Recent studies have indicated that WWI may be linked to the development of hypertension (8, 11) and dementia (12).
Therefore, the aim of this study was to evaluate the association between WWI and cognitive decline in a hypertensive population in China, thereby providing a foundation for the early identification of cognitive decline among hypertensive patients.
Methods
Study design and data sources
This study was a multicenter observational investigation involving hospitalized patients with hypertension. The Affiliated Hospital of Shandong University of Traditional Chinese Medicine collaborated with nine hospitals located in Jinan, Weifang, Yantai, Tai’an, Dongying, and Jining. Hypertensive patients underwent comprehensive evaluation of: (a) general health status, (b) physical activity levels, (c) sleep quality, and (d) cognitive function. A total of 6,098 patients were enrolled from May 2022 to July 2024. The subjects of this study were patients with essential hypertension aged over 40 years. Patients with secondary hypertension, renal impairment, comorbid mental disorders, and those with a history of alcohol or psychotropic drug abuse were excluded. After matching patients with hypertension and cognitive decline to cognitively normal hypertensive patients by age and sex in a 1:1 ratio, 2,726 patients were included in the final analysis, comprising 1,363 patients with cognitive decline and 1,363 cognitively normal patients.
Sample size calculation
Among them, α is the type I error, β is the type II error, p0, and p1 represent the estimated exposure values of the control and exposed groups of the target population, respectively, q1 = (1 − p1), q0 = (1 − p0), and p1 = p0OR/ [1 + p0(OR − 1)] (13).
In a previous meta-analysis of the relationship between hypertension and cognitive decline, the prevalence of cognitive decline in hypertensive patients was 30% (14), so p0 = 0.30, then p1 = 0.46, with an expected OR = 2.0, α = 0.05, and β = 0.10. Substituting into the above formula, and since this study used 1:1 for matching, a minimum of 186 case groups and 186 control samples. Considering the follow-up miss rate, a total of 2,726 patients were finally included in this study.
Diagnostic criteria
Hypertension is defined as a systolic blood pressure (SBP) of 140 mmHg or higher, a diastolic blood pressure (DBP) of 90 mmHg or higher, or the current use of antihypertensive medications (15). It is classified into three grades, Grade 1: SBP 140–159 mmHg and/or DBP 90–99 mmHg; Grade 2: SBP 160–179 mmHg and/or DBP 100–109 mmHg; Grade 3: SBP ≥ 180 mmHg and/or DBP ≥ 110 mmHg. Cognitive function was assessed using the Mini-Mental State Examination (MMSE), which evaluates five cognitive domains: orientation, attention, memory, language, and visuospatial abilities. The MMSE is a validated screening tool for cognitive decline and impairment that detects and differentiates between patients with cognitive decline and those with intact cognition (16, 17). The total score for the MMSE is 30, with higher scores reflecting better cognitive function. In this study, MMSE scores ranging from 18 to 27 were defined as early cognitive decline (18).
The WWI is determined by dividing the waist circumference (WC, measured in centimeters) by the square root of body weight (measured in kilograms) (10). Body weight and WC were assessed anthropometrically by trained healthcare professionals, whose proficiency was regularly verified. To ensure accuracy, subjects were advised to wear minimal clothing during weighing. Waist circumference was measured using a tape measured at specific anatomical landmarks.
Ascertainment of covariates
Blood pressure was measured by a qualified nurse in a quiet environment. Additionally, fasting blood glucose (FBG), triglycerides (TG), total cholesterol (TC), high-density lipoproteins (HDL-C), low-density lipoproteins (LDL-C), and serum creatinine (Scr) levels were assessed in all subjects after an overnight fast.
Physical activity levels were measured using the Chinese version of the International Physical Activity Questionnaire Long Form (IPAQ-LC), which is reliable and shows adequate evidence of validity (19, 20).
Statistical analysis
Continuous variables collected from participants were tested for normality according to the characteristics of the data; data conforming to a normal distribution were expressed as mean ± standard deviation (SD), and data not conforming to a normal distribution were expressed as median and interquartile range (IQR). Qualitative variables were expressed as relative numbers or percentages. WWI was transformed from a continuous variable to a categorical variable (quartile), and differences between subjects grouped by quartiles of WWI were compared in a multivariate logistic regression using quartile (Q1) as the reference group: Model 1 was not adjusted for any confounding variables and represented a univariate analysis. Model 2 was adjusted for sex, age, education level, marital status, type of work, smoking and drinking. The primary physiological and biochemical indicators (SBP, DBP, BMI, FBG, TG, TC, HDL-C, LDL-C, Scr) were incorporated into Model 2 to develop Model 3. Considering the impact of sleep disorders on HCD, Model 4 included the prevalence of sleep disorders in hypertensive patients. Data processing and analysis were performed using R version 4.4.0, along with Zstats 1.0.1
Results
Baseline clinical characteristics of subjects
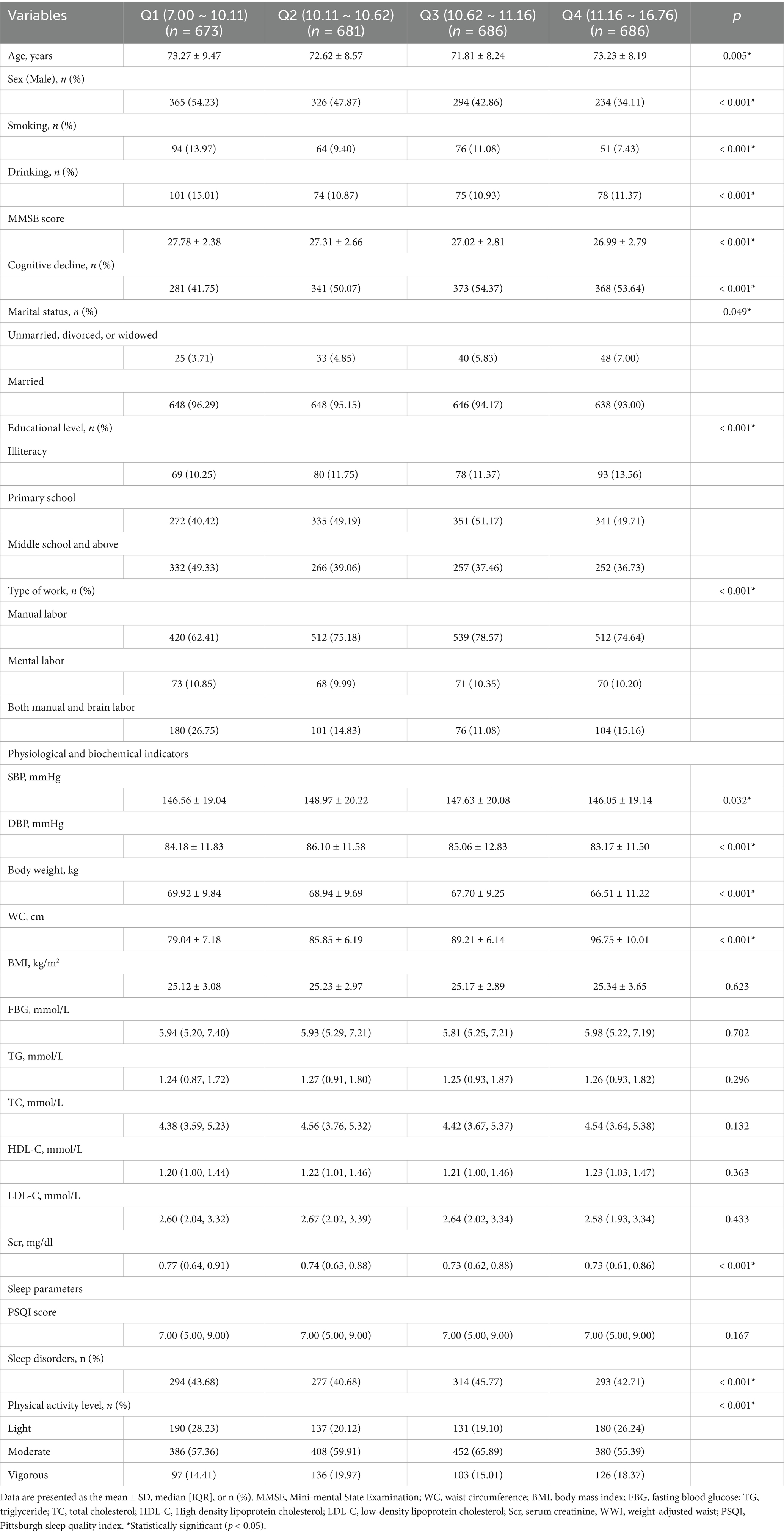
Table 1 summarizes the baseline characteristics of hypertensive patients with normal cognitive function and those with cognitive decline. The mean age of the participants in this study was 72 years. The gender distribution was 44.7% male and 55.3% female. The risk of cognitive decline was higher among the older adults with hypertensive patients (p < 0.05).
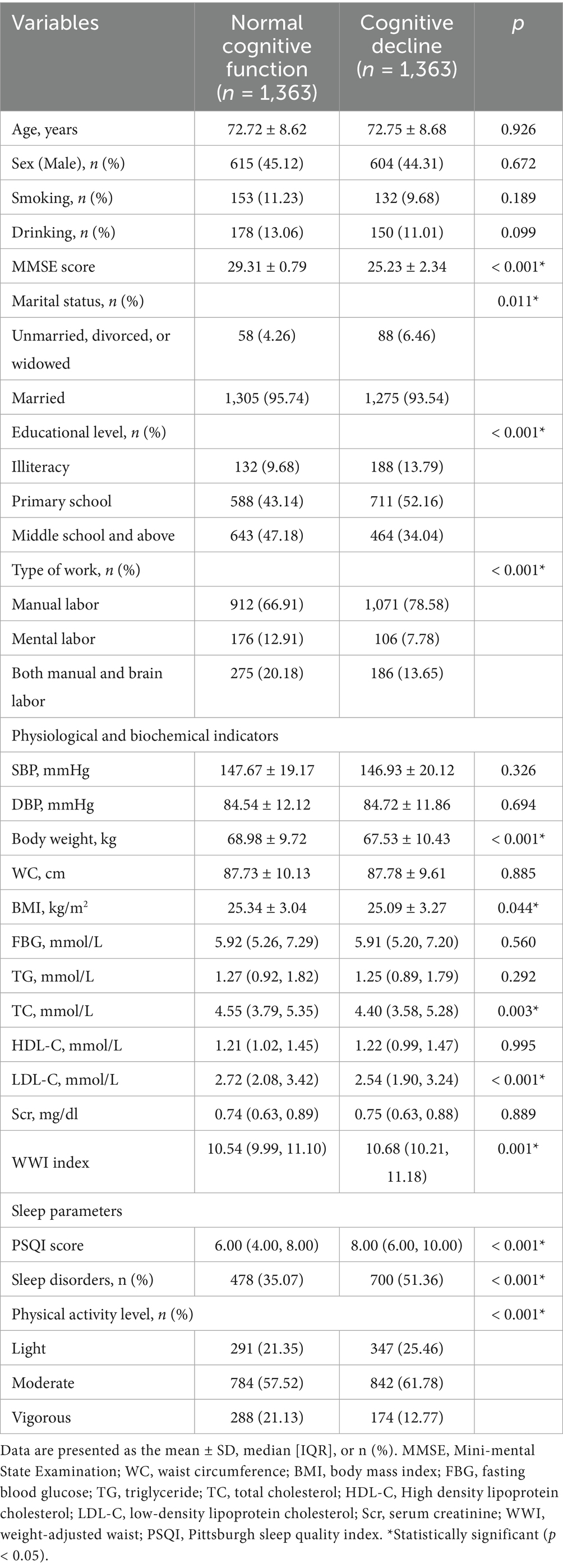
Table 1. Baseline characteristics of hypertensive patients with normal cognitive function and cognitive decline.
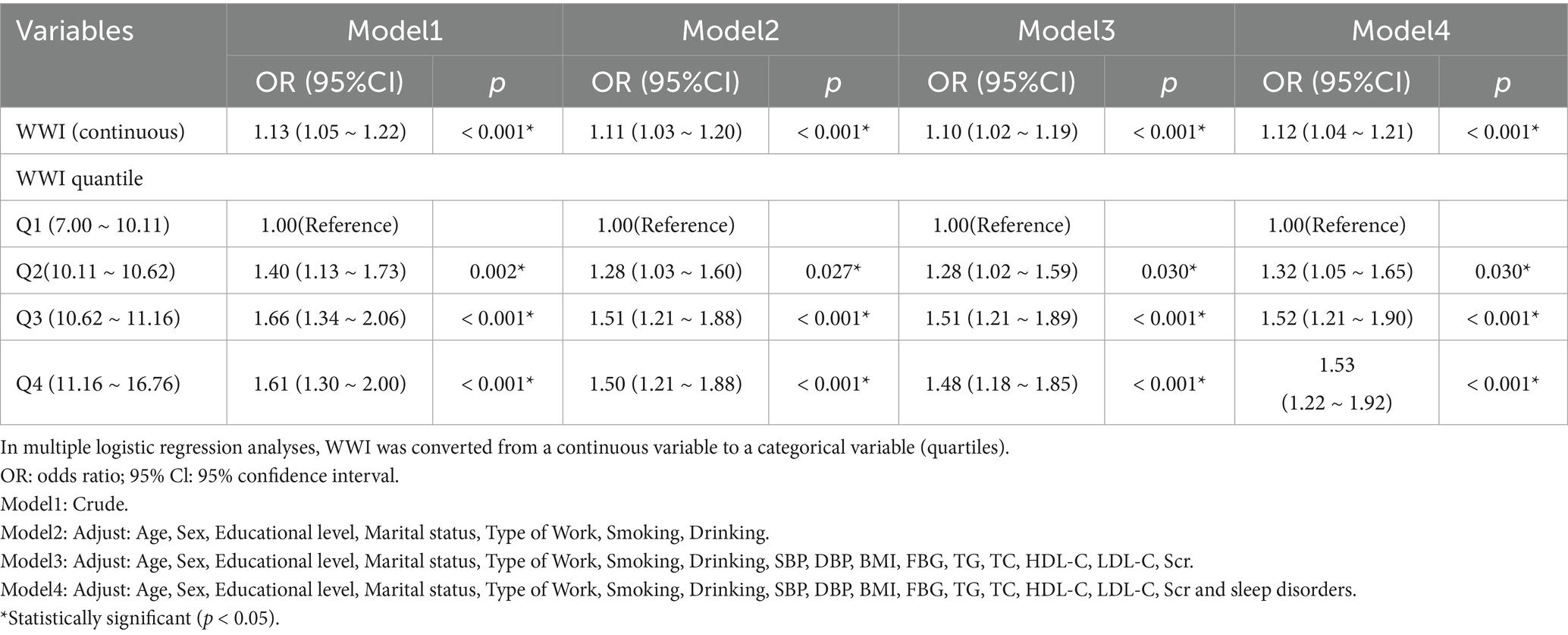
Table 2 categorizes the participants into quartiles based on their WWI values. Q1 corresponds to values ranging from 7.00 to 10.11, Q2 from 10.11 to 10.62, Q3 from 10.62 to 11.16, and Q4 from 11.16 to 16.76. The prevalence of cognitive decline significantly increased with higher WWI index among hypertensive patients (Q1: 41.75%; Q2: 50.07%; Q3: 54.37%; Q4: 53.64%, p < 0.001).
Associations between MMSE scores and multidimensional factors
Figure 1 shows a significant negative correlation between age, WWI, PSQI, and MMSE scores in this study (p < 0.001). Additionally, significant positive correlations were observed between TC, LDL-C and MMSE scores (p < 0.001). Although the correlations between these variables and MMSE scores were relatively weak, the findings suggest that increases in age, WWI, and PSQI scores may negatively impact cognitive functioning. On the contrary, higher TC and LDL-C levels were associated with better cognitive function. This finding seems to be contradictory because TC and LDL-C are usually associated with adverse cardiovascular outcomes. Previous studies have also obtained conflicting data on the relationship between blood lipids and cognitive function (21–24), suggesting that the effects of TC and LDL-C on cognitive function may be dual.
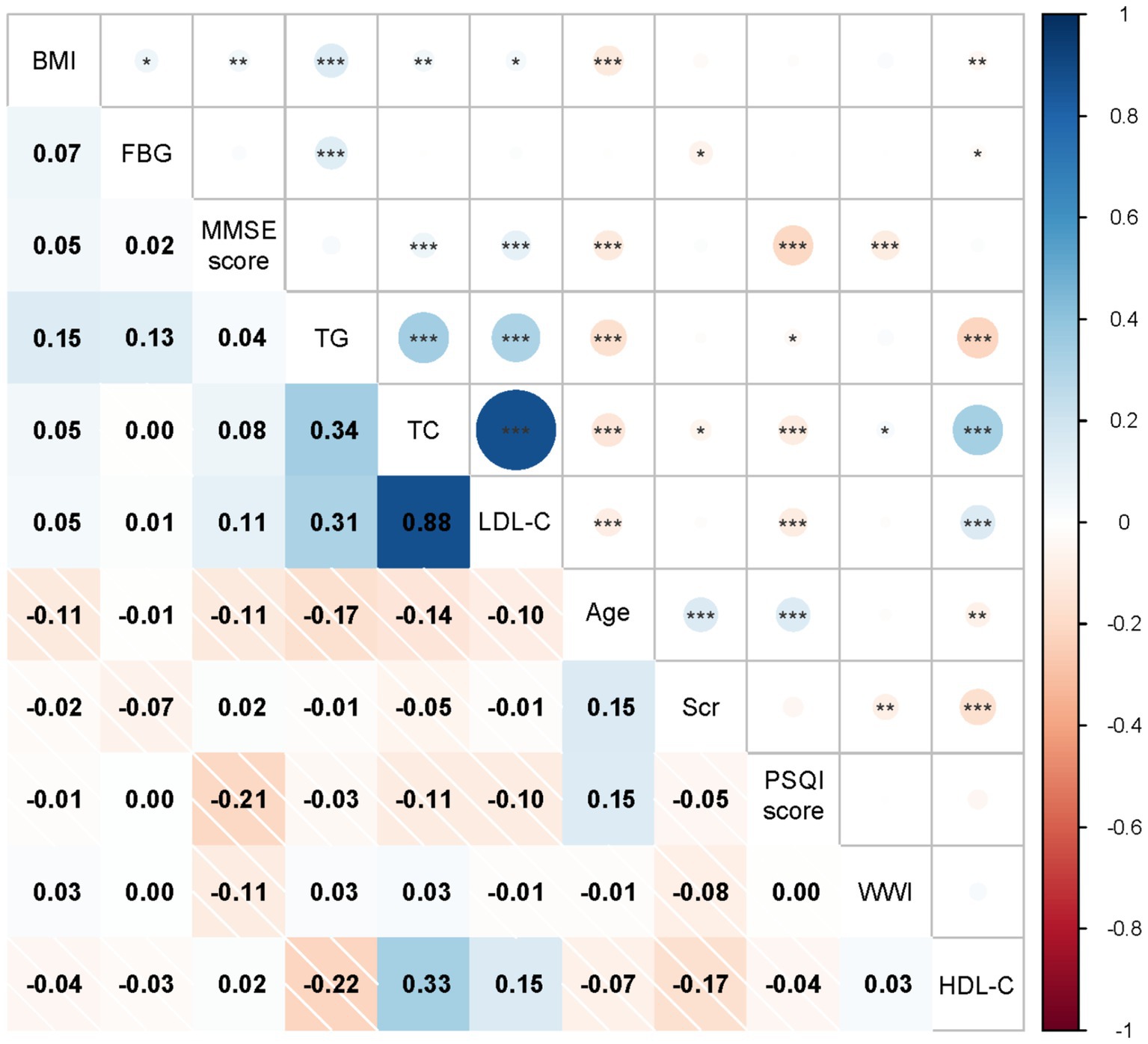
Figure 1. Associations between MMSE score and multidimensional factor, the x-axis and y-axis represent variable names, including BMI, FBG, MMSE score, TG, TC, LDL-C, Age, Scr, PSQI score, WWI, HDL-C. Each cell shows the correlation coefficient between the two variables, ranging from − 1 (dark red, indicating negative correlation) to 1 (dark blue, indicating positive correlation). *Indicates a significance level of p < 0.05, ** indicates a significance level of p < 0.01, *** indicates a significance level of p < 0.001.
Logistic regression analysis
Table 3 shows the relationship between WWI and HCD and the results of the multivariate logistic regression analysis. In the original model, there was a statistically significant positive correlation between WWI and HCD, with an OR of 1.13 (95% CI: 1.05 ~ 1.22; p < 0.001). In Model 2, after adjusting for factors such as age, sex, educational level, marital status, type of work, smoking and drinking, the positive association remained highly significant (OR = 1.11; 95% CI: 1.03 ~ 1.20; p < 0.001). In Model 3, even after adjusting for additional variables including BMI, FBG, TG, TC, HDL-C, LDL-C, and Scr, the correlation between WWI and HCD continued to be statistically significant (OR = 1.10; 95% CI: 1.02 ~ 1.19; p < 0.001). In Model 4, which was developed based on Model 3, this significant correlation persisted (OR = 1.12; 95% CI: 1.04 ~ 1.21; p < 0.001), even after accounting for sleep disorders. This indicates that the prevalence of cognitive decline among hypertensive patients increased by 12% with each unit increase in WWI. The statistical significance of the trend test showed that the strong correlation between WWI and cognitive decline in hypertensive patients persisted even after stratifying WWI into quartiles (p < 0.001). In Model 4, the prevalence of cognitive decline in hypertensive patients rose by 53% when comparing the highest quartile of WWI to the lowest quartile.
Discussion
In this case-control study based on a large sample size, we examined the association between a new obesity index WWI and cognitive decline in hypertensive populations. Cognitive decline involves multiple factors (25, 26). Therefore, understanding the risk factors associated with HCD is essential for effective prevention and treatment strategies, and WWI shows promise as a new predictor in the diagnosis of HCD.
With the rising prevalence of obesity and obesity-related diseases worldwide (27), it is essential to accurately assess obesity and identify individuals at risk for HCD in clinical practice. Previous studies have reported that the relationship between cognitive decline and obesity-related parameters is controversial, that is, the ‘obesity paradox’. Some studies have shown that the lower BMI, the better the cognitive function, and the higher BMI, the worse the cognitive function (28, 29). However, some other studies have shown that a higher BMI prevents cognitive decline, while a lower BMI increases the likelihood of poor cognitive performance (30, 31). The reason may be that anthropometric indicators related to obesity (such as BMI) have inherent limitations due to the inability to distinguish between muscle mass and fat mass (8, 32, 33). To better explore the correlation between obesity and cognitive decline, recent studies have tended to use non-traditional obesity indicators to measure obesity and test the exact relationship between the two. A meta-analysis showed that subjects with a high triglyceride-glucose index (TyG) index were significantly associated with a higher risk of cognitive impairment compared to subjects with a low TyG index [RR: 1.39, 95% CI: 1.22 to 1.59, p < 0.001; I2 = 45%] (34). In addition, another clinical study showed that a higher lipid accumulation product (LAP) (OR = 1.037, 95% CI = 1.025–1.050, p < 0.01) was associated with a higher risk of mild cognitive impairment (MCI). After correcting for age, gender, lifestyle risk factors, duration of diabetes mellitus, LDL, HbA1c, education, insulin use, statin use, and diabetic peripheral neuropathy, a high LAP index was still associated with an increased risk of MCI (OR = 1.047, 95% CI = 1.031–1.063, p < 0.01) (35). However, most of these non-traditional obesity indicators are computationally complex and are poorly operationalized in practical applications.
The weight-adjusted waist index, as a newly developed obesity parameter, combines the advantages of WC while weakening the correlation with BMI compared to traditional formulas based on BMI, enabling the assessment of fat and muscle mass components independent of BMI. Previously, Kim et al.’s cross-sectional study of 602 participants aged 65 years in the Anshan Geriatric Study found that WWI was better able to differentiate between adiposity and muscle mass components compared with BMI (36). Therefore, WWI may be more reliable for detecting cognitive decline than commonly used body composition indices such as BMI. A previous cross-sectional study has reported that WWI is positively associated with dementia in a population of hypertensive patients (12), which is highly consistent with our findings. Although the interaction effects between several subgroups (such as education level, marital status, type of work, and physical activity) were not statistically significant in our study, these findings do not completely rule out the possibility of subgroup differences.
The mechanism by which WWI is positively associated with cognitive decline may be related to obesity, inflammatory responses, and metabolic abnormalities. WWI was positively correlated with the abdominal fat area and visceral fat area but negatively correlated with the abdominal muscle area, suggesting that an increase in WWI may reflect a state of excessive fat accumulation in the body as well as dysfunction of adipose tissue (8, 36, 37). Obesity is a chronic, persistent inflammatory state. It increases the production of various pro-inflammatory cytokines and adipocytokines, leading to an inflammatory response, endothelial dysfunction, and consequent adverse effects on cognitive function (38–41); At the same time, excess pro-inflammatory factors can lead to insulin resistance, which in turn triggers metabolic syndrome, which is associated with an increased risk of cognitive decline (42–44). Secondly, obesity-related inflammation can lead to leptin resistance and decreased adiponectin secretion, and induce cerebral neurodegeneration and neurodegenerative diseases (44–47). Finally, obesity harms cerebrovascular function and the blood–brain barrier, thus affecting cognitive ability (48, 49). In addition, increased age may also partially explain the mechanism of the association between WWI and cognitive decline. As individuals age, changes in body composition, including increased visceral fat and changes in adipose tissue distribution, can affect cognitive function (50). Future studies involving larger and more diverse populations may help clarify the role of these factors in moderating the relationship between WWI and HCD.
Limitations and strengths
Our study is based on the hypertension follow-up system in Shandong Province, which is a hypertension sampling survey system in Shandong Province, following strict research programs and quality control measures. To enhance the reliability of our research results, we have adjusted multiple potential covariates to ensure the reliability of the results. Due to the simplicity and ease of calculation, WWI may become a practical tool for managing and intervening cognitive decline in patients with hypertension in clinical practice.
However, this study has several limitations. First, as a case-control study, it cannot establish a causal relationship between WWI and HCD. Second, although we adjusted to many important covariates, we could not completely exclude the effects of other potential confounders. While WWI predicted a decline in cognitive ability in our study, we recognized that other indicators derived from anthropometric indicators [e.g., TyG-body mass index (51)] may also complement cardiovascular risk prediction. Future studies should explore the combined utility of WWI and these indicators to better understand their influence on cognitive function in patients with hypertension.
Furthermore, we found that higher TC and LDL-C levels were associated with better cognitive performance. This finding seems contradictory, as high levels of these lipids are often associated with negative health outcomes, particularly cardiovascular risk (52, 53). However, combined with previous studies (21–24) and our findings, the relationship between TC, LDL-C, and cognitive function does not seem to be one-way but is influenced by a series of physiological and pathological factors. Therefore, the effect of blood lipid levels on cognitive function in patients with hypertension needs further study.
Finally, since the sample of this study is limited to individuals with hypertension in Shandong Province, the generalization of our results in the wider population of hypertension in China remains to be verified.
Conclusion
Our study demonstrated that elevated levels of WWI in hypertensive patients were significantly associated with an increased risk of cognitive decline. This finding suggests that WWI may serve as a potential intervention indicator for mitigating the risk of cognitive decline in hypertensive individuals. However, further longitudinal studies are necessary to clarify the precise causality of this relationship.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The datasets used and analysed during the current study available from the corresponding author on reasonable request. Requests to access these datasets should be directed to Huachen Jiao, bGl5aXh1YW4wNTMxQDE2My5jb20=.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine ((2023) Review No. (109) -KY). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MZ: Methodology, Visualization, Writing – original draft, Writing – review & editing. DL: Conceptualization, Formal analysis, Methodology, Supervision, Writing – review & editing. XY: Data curation, Project administration, Writing – original draft. ZN: Methodology, Visualization, Writing – review & editing. YZ: Data curation, Project administration, Writing – original draft. LH: Data curation, Project administration, Writing – original draft. HJ: Conceptualization, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 82474422).
Acknowledgments
I am grateful to all the participants in this study for their help in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Kim, JS, Sung Kim, J, Bin Bae, J, Won Han, J, Jong Oh, D, Wan Suh, S, et al. Association of estimated white matter hyperintensity age with cognition in elderly with controlled hypertension. Neuroimage Clin. (2023) 37:103323. doi: 10.1016/j.nicl.2023.103323
2. Poster viewing Session II. J Cereb Blood Flow Metab. (2017) 37:169–239. doi: 10.1177/0271678X17695989
3. Biernacki, M, Baranowska-Kuczko, M, Niklińska, GN, and Skrzydlewska, E. The FAAH inhibitor URB597 modulates lipid mediators in the brain of rats with spontaneous hypertension. Biomol Ther. (2020) 10:1022. doi: 10.3390/biom10071022
4. Haring, B, Wu, C, Coker, LH, Seth, A, Snetselaar, L, Manson, JAE, et al. Hypertension, dietary sodium, and cognitive decline: results from the women’s health initiative memory study. Am J Hypertens. (2016) 29:202–16. doi: 10.1093/ajh/hpv081
5. Su, J, and Xiao, X. Factors leading to the trajectory of cognitive decline in middle-aged and older adults using group-based trajectory modeling: a cohort study. Medicine (Baltimore). (2022) 101:e31817. doi: 10.1097/MD.0000000000031817
6. Wang, X, Li, T, Li, H, Li, D, Wang, X, Zhao, A, et al. Association of dietary inflammatory potential with blood inflammation: the prospective markers on mild cognitive impairment. Nutrients. (2022) 14:2417. doi: 10.3390/nu14122417
7. Gombojav, B, Yi, S-W, Sull, JW, Nam, CM, and Ohrr, H. Combined effects of cognitive impairment and hypertension on total mortality in elderly people: the kangwha cohort study. Gerontology. (2011) 57:490–6. doi: 10.1159/000323759
8. Xie, F, Xiao, Y, Li, X, and Wu, Y. Association between the weight-adjusted-waist index and abdominal aortic calcification in United States adults: results from the national health and nutrition examination survey 2013–2014. Front Cardiovasc Med. (2022) 9:948194. doi: 10.3389/fcvm.2022.948194
9. Park, Y, Kim, NH, Kwon, TY, and Kim, SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. (2018) 8:16753. doi: 10.1038/s41598-018-35073-4
10. Zhao, P, Shi, W, Shi, Y, Xiong, Y, Ding, C, Song, X, et al. Positive association between weight-adjusted-waist index and hyperuricemia in patients with hypertension: the China H-type hypertension registry study. Front Endocrinol. (2022) 13:1007557. doi: 10.3389/fendo.2022.1007557
11. Li, Q, Qie, R, Qin, P, Zhang, D, Guo, C, Zhou, Q, et al. Association of weight-adjusted-waist index with incident hypertension: the rural Chinese cohort study. Nutr Metab Cardiovasc Dis. (2020) 30:1732–41. doi: 10.1016/j.numecd.2020.05.033
12. Zhou, W, Xie, Y, Yu, L, Yu, C, Bao, H, and Cheng, X. Positive association between weight-adjusted-waist index and dementia in the Chinese population with hypertension: a cross-sectional study. BMC Psychiatry. (2023) 23:519. doi: 10.1186/s12888-023-05027-w
13. Wang, R, Zhao, H, and Li, B. Analytical clinical medicine research: key points of casecontrol study design. Shanghai Med. (2023) 44:23–5. doi: 10.3969/j.issn.1006-1533.2023.21.005
14. Qin, J, He, Z, Wu, L, Wang, W, Lin, Q, Lin, Y, et al. Prevalence of mild cognitive impairment in patients with hypertension: a systematic review and meta-analysis. Hypertens Res. (2021) 44:1251–60. doi: 10.1038/s41440-021-00704-3
15. Joint Committee for Guideline Revision. 2018 chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J geriatr cardiol: JGC. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
16. Croll, PH, Vinke, EJ, Armstrong, NM, Licher, S, Vernooij, MW, de Baatenburg Jong, RJ, et al. Hearing loss and cognitive decline in the general population: a prospective cohort study. J Neurol. (2020) 268:860. doi: 10.1007/s00415-020-10208-8
17. Tombaugh, TN, and McIntyre, NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. (1992) 40:922–35. doi: 10.1111/j.1532-5415.1992.tb01992.x
18. Zhong, X, Yu, J, Jiang, F, Chen, H, Wang, Z, Teng, J, et al. A risk prediction model based on machine learning for early cognitive impairment in hypertension: development and validation study. Front Public Health. (2023) 11:1143019. doi: 10.3389/fpubh.2023.1143019
19. Xue, B, Xue, Y, Dong, F, Zheng, X, Shi, L, Xiao, S, et al. The impact of socioeconomic status and sleep quality on the prevalence of multimorbidity in older adults. Front Public Health. (2022) 10:959700. doi: 10.3389/fpubh.2022.959700
20. Macfarlane, D, Chan, A, and Cerin, E. Examining the validity and reliability of the chinese version of the international physical activity questionnaire, long form (IPAQ-LC). Public Health Nutr. (2011) 14:443–50. doi: 10.1017/S1368980010002806
21. Zhou, F, Deng, W, Ding, D, Zhao, Q, Liang, X, Wang, F, et al. High low-density lipoprotein cholesterol inversely relates to dementia in community-dwelling older adults: the Shanghai aging study. Front Neurol. (2018) 9:952. doi: 10.3389/fneur.2018.00952
22. Liu, H, Zou, L, Zhou, R, Zhang, M, Gu, S, Zheng, J, et al. Long-term increase in cholesterol is associated with better cognitive function: evidence from a longitudinal study. Front Aging Neurosci. (2021) 13:691423. doi: 10.3389/fnagi.2021.691423
23. Stough, C, Pipingas, A, Camfield, D, Nolidin, K, Savage, K, Deleuil, S, et al. Increases in total cholesterol and low density lipoprotein associated with decreased cognitive performance in healthy elderly adults. Metab Brain Dis. (2019) 34:477–84. doi: 10.1007/s11011-018-0373-5
24. Guo, Y, Li, P, Ma, X, Huang, X, Liu, Z, Ren, X, et al. Association of Circulating Cholesterol Level with cognitive function and mild cognitive impairment in the elderly: a community-based population study. Curr Alzheimer Res. (2020) 17:556–65. doi: 10.2174/1567205017666200810165758
25. Zhang, T, Wu, X, Yuan, H, Huang, S, and Park, S. Mitigation of memory impairment with fermented fucoidan and λ-carrageenan supplementation through modulating the gut microbiota and their metagenome function in hippocampal amyloid-β infused rats. Cells. (2022) 11:2301. doi: 10.3390/cells11152301
26. A Armstrong, R. Risk factors for Alzheimer’s disease. Folia Neuropathol. (2019) 57:87–105. doi: 10.5114/fn.2019.85929
27. Verkouter, I, de Mutsert, R, Smit, RAJ, Trompet, S, Rosendaal, FR, van Heemst, D, et al. The contribution of tissue-grouped BMI-associated gene sets to cardiometabolic-disease risk: a Mendelian randomization study. Int J Epidemiol. (2020) 49:1246. doi: 10.1093/ije/dyaa070
28. Rubin, LH, Gustafson, D, Hawkins, KL, Zhang, L, Jacobson, LP, Becker, JT, et al. Midlife adiposity predicts cognitive decline in the prospective multicenter AIDS cohort study. Neurology. (2019) 93:e261–71. doi: 10.1212/WNL.0000000000007779
29. Gong, H-J, Tang, X, Chai, YH, Qiao, YS, Xu, H, Patel, I, et al. Relationship between weight-change patterns and cognitive function: a retrospective study. JAD. (2023) 91:1085–95. doi: 10.3233/JAD-220788
30. Zhang, W, Chen, Y, and Chen, N. Body mass index and trajectories of the cognition among chinese middle and old-aged adults. BMC Geriatr. (2022) 22:613. doi: 10.1186/s12877-022-03301-2
31. Aiken-Morgan, AT, Capuano, AW, Arvanitakis, Z, and Barnes, LL. Changes in body mass index are related to faster cognitive decline among african american older adults. J American Geriatrics Soc. (2020) 68:2662–7. doi: 10.1111/jgs.16814
32. Komici, K, D’Amico, F, Verderosa, S, Piomboni, I, D’Addona, C, Picerno, V, et al. Impact of body composition parameters on lung function in athletes. Nutrients. (2022) 14:3844. doi: 10.3390/nu14183844
33. Liu, J, Yang, F, Sun, Q, Gu, T, Yao, J, Zhang, N, et al. Fat mass is associated with subclinical left ventricular systolic dysfunction in patients with type 2 diabetes mellitus without established cardiovascular diseases. Diabetes Therapy. (2023) 14:1037. doi: 10.1007/s13300-023-01411-7
34. Han, Y, Meng, X, and Wang, D. Association between triglyceride glucose index with cognitive impairment and dementia in adult population: a meta-analysis. Horm Metab Res. (2024) 56:737–48. doi: 10.1055/a-2284-5667
35. Yu, Z-W, Li, X, Wang, Y, Fu, Y-H, and Gao, X-Y. Association between lipid accumulation product and mild cognitive impairment in patients with type 2 diabetes. J Alzheimers Dis. (2020) 77:367–74. doi: 10.3233/JAD-200332
36. Kim, NH, Park, Y, Kim, NH, and Kim, SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. (2021) 50:780–6. doi: 10.1093/ageing/afaa208
37. Kim, JY, Choi, J, Vella, CA, Criqui, MH, Allison, MA, and Kim, NH. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. (2022) 46:747–55. doi: 10.4093/dmj.2021.0294
38. Martinelli, I, Tayebati, SK, Roy, P, Micioni di Bonaventura, MV, Moruzzi, M, Cifani, C, et al. Obesity-related brain cholinergic system impairment in high-fat-diet-fed rats. Nutrients. (2022) 14:1243. doi: 10.3390/nu14061243
39. Choi, J, Joseph, L, and Pilote, L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. (2013) 14:232–44. doi: 10.1111/obr.12003
40. Guo, H, Zhang, Y, Ma, H, Gong, P, Shi, Y, Zhao, W, et al. T-stage-specific abdominal visceral fat, haematological nutrition indicators and inflammation as prognostic factors in patients with clear renal cell carcinoma. Adipocytes. (2022) 11:133. doi: 10.1080/21623945.2022.2048546
41. Shi, S, Ni, L, Tian, Y, Zhang, B, Xiao, J, Xu, W, et al. Association of obesity indices with diabetic kidney disease and diabetic retinopathy in type 2 diabetes: a real-world study. J Diabetes Res. (2023) 2023:1–11. doi: 10.1155/2023/3819830
42. Lindberger, E, Wikström, AK, Bergman, E, Eurenius, K, Mulic-Lutvica, A, Sundström Poromaa, I, et al. Association of maternal central adiposity measured by ultrasound in early mid pregnancy with infant birth size. Sci Rep. (2020) 10:19702. doi: 10.1038/s41598-020-76741-8
43. Hung, C-C, Cheng, Y-W, Chen, W-L, and Fang, W-H. Negative association between acrylamide exposure and metabolic syndrome markers in adult population. Int J Environ Res Public Health. (2021) 18:11949. doi: 10.3390/ijerph182211949
44. Wang, X-L, Feng, H-L, Xu, X-Z, Liu, J, and Han, X. Relationship between cognitive function and weight-adjusted waist index in people ≥ 60 years old in NHANES 2011-2014. Aging Clin Exp Res. (2024) 36:30. doi: 10.1007/s40520-023-02649-8
45. Chen, W-D, Lai, LJ, Lee, KL, Chen, TJ, Liu, CY, and Yang, YH. Is obesity a risk or protective factor for open-angle glaucoma in adults? A two-database, asian, matched-cohort study. J Clin Med. (2021) 10:4021. doi: 10.3390/jcm10174021
46. Flores-Cordero, JA, Pérez-Pérez, A, Jiménez-Cortegana, C, Alba, G, Flores-Barragán, A, and Sánchez-Margalet, V. Obesity as a risk factor for dementia and alzheimer’s disease: the role of leptin. Int J Mol Sci. (2022) 23:5202. doi: 10.3390/ijms23095202
47. Forny-Germano, L, De Felice, FG, and Vieira, MN d N. The role of leptin and adiponectin in obesity-associated cognitive decline and Alzheimer’s disease. Front Neurosci. (2018) 12:1027. doi: 10.3389/fnins.2018.01027
48. Rask, L, Bendix, L, Harbo, M, Fagerlund, B, Mortensen, EL, Lauritzen, MJ, et al. Cognitive change during the life course and leukocyte telomere length in late middle-aged men. Front Aging Neurosci. (2016) 8:300. doi: 10.3389/fnagi.2016.00300
49. Nguyen, JCD, Killcross, AS, and Jenkins, TA. Obesity and cognitive decline: role of inflammation and vascular changes. Front Neurosci. (2014) 8:375. doi: 10.3389/fnins.2014.00375
50. Brinkley, TE, Leng, I, Register, TC, Neth, BJ, Zetterberg, H, Blennow, K, et al. Changes in adiposity and cerebrospinal fluid biomarkers following a modified mediterranean ketogenic diet in older adults at risk for alzheimer’s disease. Front Neurosci. (2022) 16:906539. doi: 10.3389/fnins.2022.906539
51. Sodero, G, Rigante, D, Pane, LC, Sessa, L, Quarta, L, Candelli, M, et al. Cardiometabolic risk assessment in a cohort of children and adolescents diagnosed with hyperinsulinemia. Diseases. (2024) 12:119. doi: 10.3390/diseases12060119
52. Montalvan Sanchez, EE, Urrutia, SA, Rodriguez, AA, Duarte, G, Murillo, A, Rivera, R, et al. Cardiovascular risk assessment in the resource limited setting of Western Honduras: an epidemiological perspective. Int J Cardiol Heart Vasc. (2020) 27:100476. doi: 10.1016/j.ijcha.2020.100476
53. Yu, S, Wu, X, Ferguson, M, Simmen, RC, Cleves, MA, Simmen, FA, et al. Diets Containing Shiitake Mushroom Reduce Serum Lipids and Serum Lipophilic Antioxidant Capacity in Rats123. J Nutr. (2016) 146:2491–2496. doi: 10.3945/jn.116.239806
Glossary
HCD - cognitive decline in hypertension
WWI - waist circumference index
MMSE - Mini-mental State Examination
WC - waist circumference
BMI - body mass index
FBG - fasting blood glucose
TG - triglyceride
TC - total cholesterol
HDL-C - High density lipoprotein cholesterol
LDL-C - low-density lipoprotein cholesterol
Scr - serum creatinine
WWI - weight-adjusted waist
PSQI - Pittsburgh sleep quality index
ACEI - angiotensin-converting enzyme inhibitors
ARB - angiotensin receptor blocker
CCB - calcium channel blocker
IPAQ-L - International Physical Activity Questionnaire Long Form
TyG - triglyceride-glucose index
LAP - lipid accumulation product
MCI - mild cognitive impairment
Keywords: weight-adjusted-waist index, obesity, hypertension, cognitive decline, risk factors
Citation: Zhang M, Liu D, Yan X, Niu Z, Zhang Y, He L and Jiao H (2025) Association between weight-adjusted waist circumference index and risk of cognitive decline in Chinese hypertensive patients: a case-control study. Front. Public Health. 13:1632358. doi: 10.3389/fpubh.2025.1632358
Edited by:
Basil Nwaneri Okeahialam, University of Jos, NigeriaReviewed by:
Giorgio Sodero, Azienda Sanitaria Locale di Brindisi, ItalyBogdana Virgolici, Carol Davila University of Medicine and Pharmacy, Romania
Copyright © 2025 Zhang, Liu, Yan, Niu, Zhang, He and Jiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huachen Jiao, bGl5aXh1YW4wNTMxQDE2My5jb20=
 Mengdi Zhang
Mengdi Zhang Donghai Liu
Donghai Liu Xipeng Yan3
Xipeng Yan3 Zhenchao Niu
Zhenchao Niu Huachen Jiao
Huachen Jiao