- 1General Practice Ward/International Medical Center Ward, General Practice Medical Center, National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 2Health Promotion and Food Nutrition & Safety Key Laboratory of Sichuan Province, Chengdu, China
- 3Chengdu Second People's Hospital, Chengdu, Sichuan, China
- 4School of Computing, Ulster University, Belfast, United Kingdom
- 5School of Health Policy and Management, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China
- 6Jin-cheng Community Health Service Center, Chengdu, Sichuan, China
- 7Fang-cao Community Health Service Center, Chengdu, Sichuan, China
- 8Department of Endocrinology and Metabolism, Laboratory of Diabetes and Metabolism Research, West China Hospital, Sichuan University, Chengdu, China
- 9MAGIC China Center, Cochrane China Center, Chinese Evidence-Based Medicine Center, West China Hospital, Sichuan University, Chengdu, China
Background: Primary health care (PHC) is the cornerstone of the healthcare system in China. The medical and health consortia (medical consortia) integrate resources of continuing medical education (CME) to bridge competency gaps among healthcare providers. This narrative review aims to explore the innovative models of CME within the framework of medical consortia.
Methods: Searches were conducted in both Chinese and English databases to broaden the scope of the review, including China National Knowledge Infrastructure, Wanfang Data, and PubMed. Chinese policy documents were retrieved from official websites of China’s National Health Commission. The review analyzed existing policy documents (2010–2025) and relevant literature, supplemented by an institutional application example of the West China Hospital–Fangcao Community Health Service Center Medical Consortium to explore challenges and recommendations.
Results: China developed a series of policies to promote the construction of medical consortia, with a focus on resource-sharing between tertiary and PHC institutions. A literature search yielded 196 articles, including qualitative studies, quantitative studies, and reviews, of which 48 met inclusion criteria in the review. Seven policy documents were included in the analysis. The synergy between medical consortia and CME brought benefits to both healthcare providers and the health system. Key innovations included clinical scenario-oriented training, remote consultation, and flexible training modalities. However, the reviewed literature highlighted persistent challenges, including regional disparities in resources, limited financial incentives for general practitioners (GPs), and a shortage of qualified trainers. Overcoming barriers such as regional resource disparities and improving the intrinsic motivation of GPs remained critical to the implementation of CME.
Conclusion: Medical consortia offer platforms for the delivery of CME, while CME supports the development of medical consortia. These innovations enhance collaboration between specialists and GPs, thereby optimizing patient referrals and follow-up care.
Background
Primary health care (PHC) is the first element of the care continuum. In China, PHC system provides outpatient clinics, inpatient wards, and continuous preventive through general practitioner teams for community and village residents, focusing on managing common and chronic diseases (1). The goal of Healthy China 2030 aims to establish a universal basic healthcare system that provides safe, effective, convenient, and affordable PHC services to all by 2030 (2–4). However, current healthcare services in China have not yet fully achieved these objectives.
The dilemma of China’s healthcare system
The ongoing expansion of tertiary hospitals has led to a “siphon effect,” drawing both medical professionals and patients away from primary care. The root of the dilemma lies in the unequal distribution of medical resources (5–8). There is a small difference in medical costs and basic insurance reimbursement rates across different healthcare levels (9, 10). Patients exhibited a strong preference for seeking care at tertiary hospitals, regardless of the severity of conditions (11, 12). Tertiary hospitals are currently overburdened, expanding both outpatient and inpatient services to manage not only complex and critical illnesses but also common diseases, initial diagnoses, and chronic disease management (13, 14). This patient flow imbalance leads to a disproportionate allocation of health insurance funds toward tertiary hospitals. Meanwhile, PHC facilities remain underutilized, leading to significant inefficiencies and resource wastage (see Figure 1a) (15, 16). This imbalance is further evident in hospital admissions: in 2023, tertiary hospitals accounted for 245.001 million admissions (81.2% of the total), whereas PHC institutions managed only 45.451 million admissions (15.1%) (17). In addition, tertiary hospitals reported bed occupancy rates of 91.1%, compared to just 54.1% in PHC institutions (17).
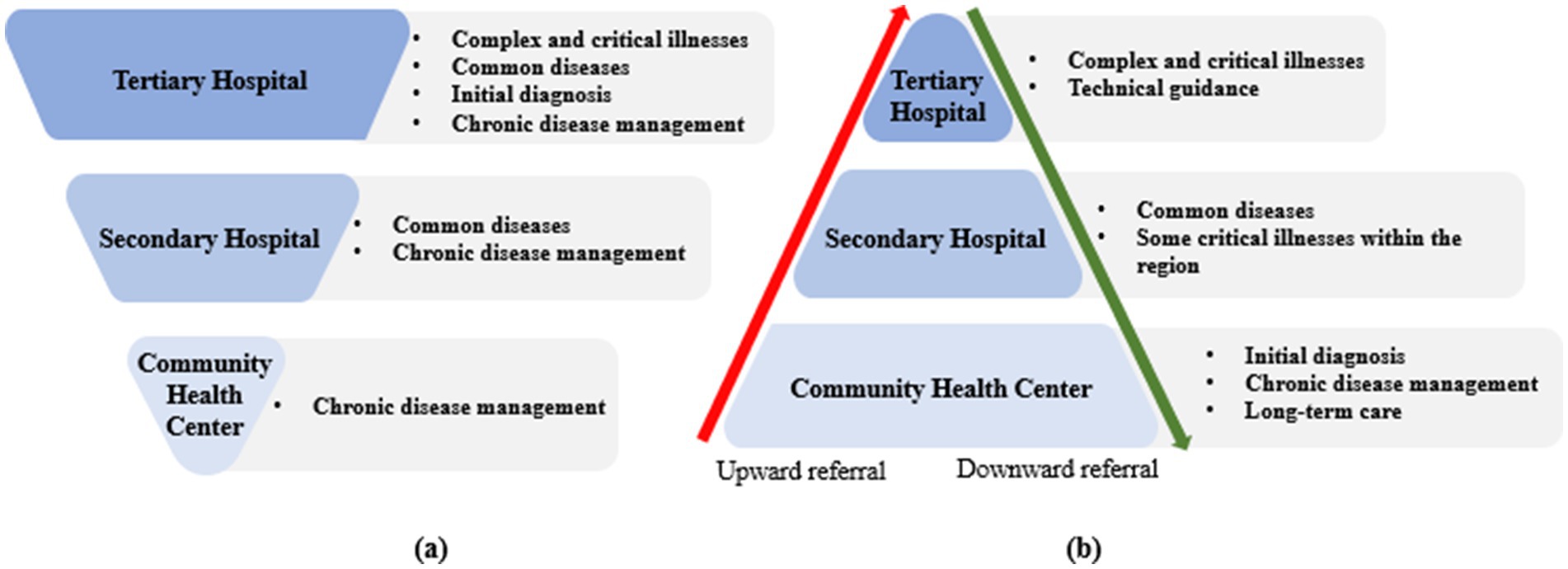
Figure 1. Transition from the current healthcare system to the graded diagnosis and treatment system. a: Current healthcare system; b: Graded diagnosis and treatment system.
Structure and function of medical consortia
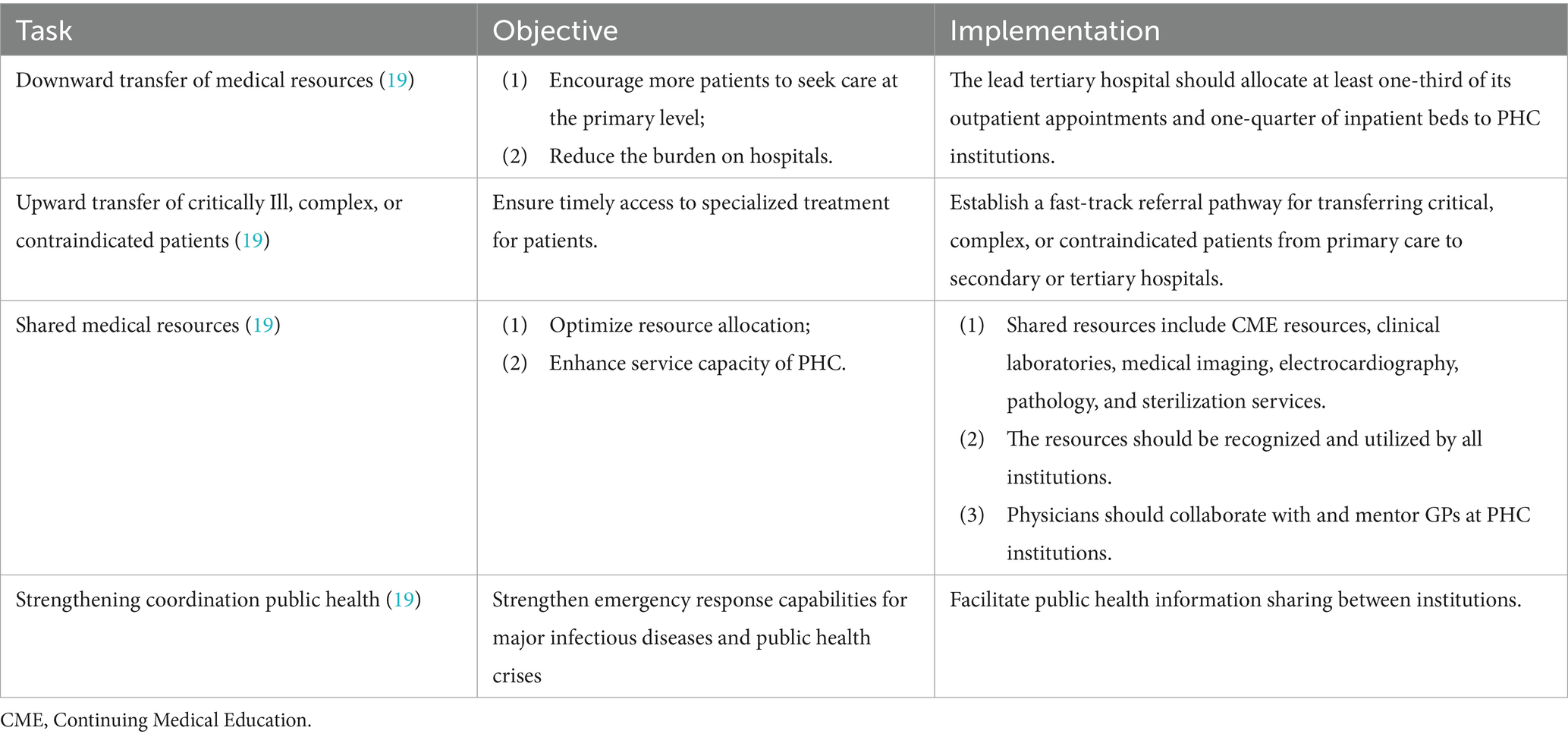
To eliminate the siphon effect, medical and health consortia (medical consortia) represent a key strategy to accelerate progress toward the Healthy China 2030 goals (18). Medical consortia typically consist of healthcare institutions across all three levels (tertiary, secondary, and primary care facilities). The leading institutions are usually tertiary hospitals with affiliated departments of medical education. This system allocated responsibilities appropriately across different healthcare levels (see Table 1) (19). GPs managed common and chronic diseases, while tertiary hospitals specialized in complex and critical conditions. Patients could be referred upward for advanced treatment or downward for rehabilitation and follow-up, ensuring a continuum of care (depicted in Figure 1b). The core objective of medical consortia was to direct high-quality medical resources to primary care, including continuing medical education (CME) resources (16, 20). As of the end of 2023, more than 18,000 various types of medical consortia had been established nationwide (21). While previous studies assessed the system’s management efficiency, little attention had been paid to the mechanisms of inter-institutional CME.
Overview of CME in China
CME is organized and carried out by national, provincial, and municipal health authorities, as well as hospitals, universities, and medical associations. The content covers new developments and advances in medicine, professional theories, treatment and management of common diseases, health policies and laws, new skills and practices and research capabilities (22, 23).
Prior to 2019, GPs in China were required to earn 25 CME credits, primarily for annual evaluations and professional title applications (24). The traditional approach was often characterized by seminars, hospital-based training, and self-directed learning (25). CME courses were typically conducted in large conference or seminar formats, delivering continuing education through on-the-job learning (23). Studies identified several challenges associated with CME, including fragmented learning experiences, outdated curricula, lack of learner initiative, irregular scheduling, and an excessive focus on earning credits (26). Hospital-based training was another alternative that focused on clinical skills and was typically offered at larger medical centers. However, these programs frequently failed to address the specific needs of PHC. CME activities conducted during personal time without compensation tend to reduce motivation and engagement (27). Financial barriers, such as travel costs, loss of income, and accommodation expenses, can also hindered participation in high-quality CME programs (28). The majority of GPs relied on medical textbooks for guidance in diagnosing and treating patients (29). Textbooks contained outdated or inaccurate recommendations.
Given the rapid development of medical consortia, there is an urgent need for strategies to advance CME in China. This narrative review focuses on innovative CME practices within the medical consortia and explores the interconnections.
Methods
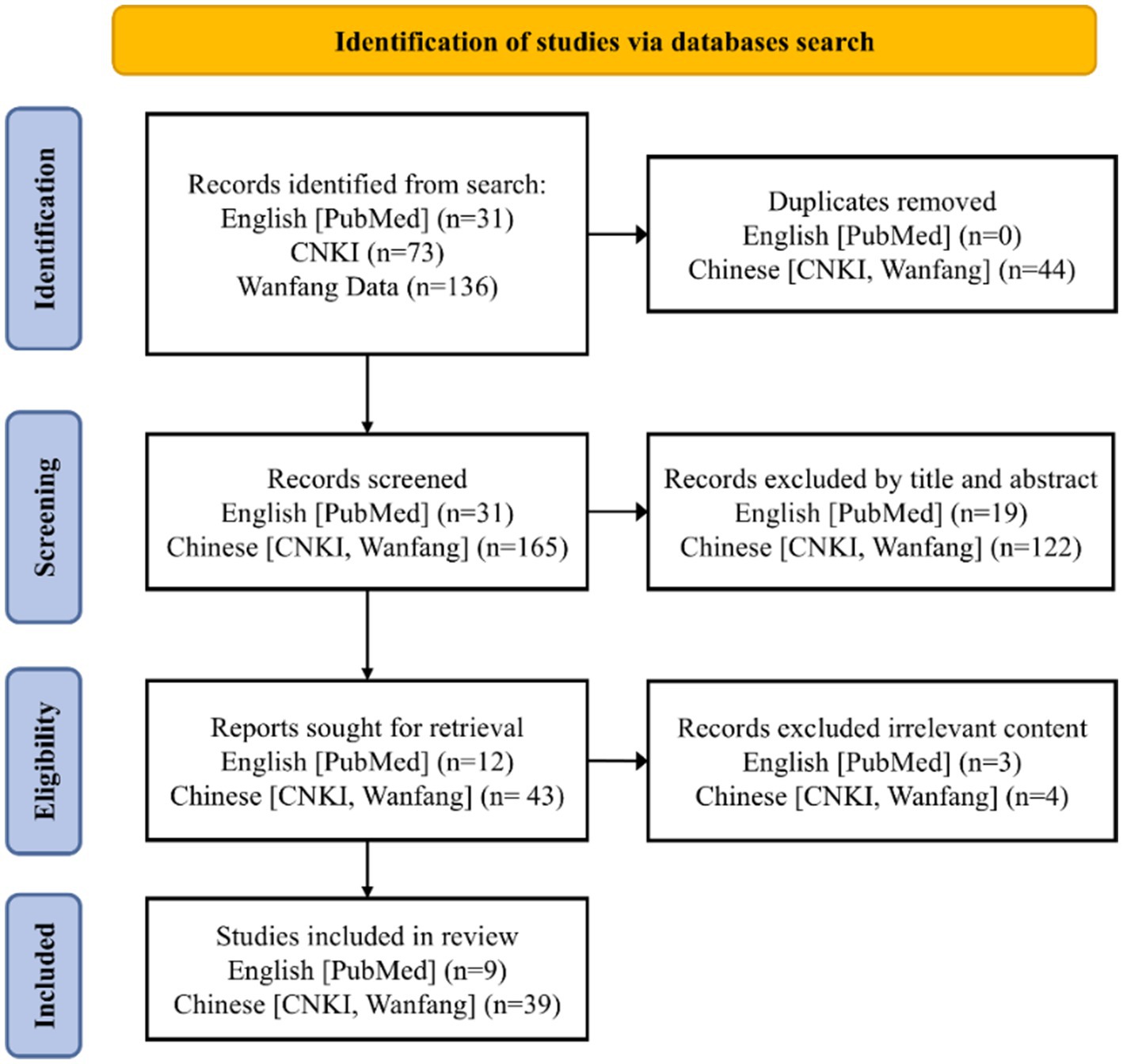
This narrative review analyzed existing policy documents and relevant literature, supplemented by an illustrative example of the West China Hospital–Fangcao Community Health Service Center Medical Consortium (Huaxi-Fangcao Medical Consortium), to explore the challenges and recommendations. The review employed the Joanna Briggs Institute PCC framework (population, concept, and context) to define the objectives and eligibility criteria. Searches were conducted to expand the review’s scope in both Chinese and English databases: China National Knowledge Infrastructure (CNKI), Wanfang Data, and PubMed. The primary search terms included ‘medical consortia,’ ‘medical alliance,’ ‘healthcare alliance,’ ‘medical coalition,’ ‘medical consortium,’ ‘training,’ ‘education,’ ‘learning,’ and MeSH term ‘Education.’ The search covered articles published between January 1, 2014, and April 14, 2025, because significant policy developments and pilot programs started around 2015. The inclusion criteria were: (1) publications in English or Chinese; (2) articles or reviews; (3) studies related to continuing medical education in China; (4) studies on doctor training, including general practitioners, family doctors. Exclusion criteria were: (1) studies focused on standardized training for residents, undergraduate students, postgraduates, pharmacists, or nurses; (2) articles such as conference papers, theses, commentaries, editorials, and letters. The details of the literature search were presented in Figure 2.
To identify relevant national policies and directives, we systematically searched official websites of China’s National Health Commission. These websites represent the authoritative source of healthcare policies in China. We focused on documents published between January 2010 and December 2024, corresponding to the period of major policy reforms in medical consortia and CME. We used advanced search functionalities with keywords such as medical consortia, tiered healthcare, and continuing medical education. Policy documents unrelated to CME or lacking clear directives on medical consortia implementation were excluded. The included documents were analyzed using content analysis. The institutional experiences described in the illustrative example of the Huaxi-Fangcao Medical Consortium were derived from internal practice records and routine operational documentation. It was not based on empirical research data. These records captured day-to-day operational details and administrative insights that were not typically included in research studies.
Results
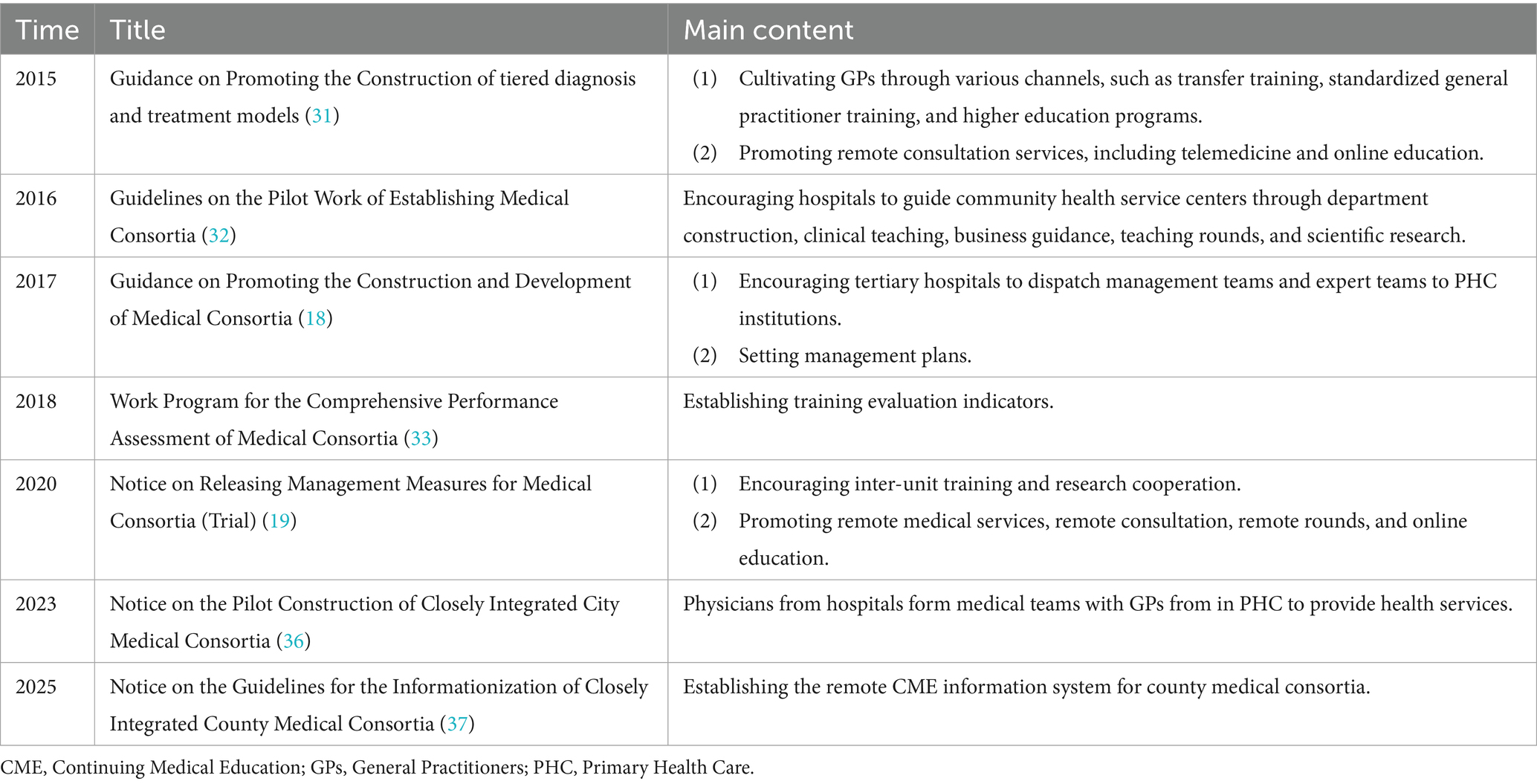
National Policies in advancing CME within medical consortia
The search retrieved 14 policies, of which seven were included in this review. Since 2015, China has made significant strides in developing medical consortia. Initially, hospitals were encouraged to provide consultations and training to PHC institutions, particularly in rural areas. Rural doctors and specialist physicians were offered opportunities to transition to general practice through training programs at medical consortia training bases (30). From 2015 to 2018, national policies gradually established the framework for medical consortia (See Table 2). These policies mandated that tertiary hospitals dispatch experts, conduct joint ward rounds, and participate in case discussions to train GPs, with a focus on diagnosing and treating common and chronic diseases (18, 31–33).
In 2018, performance evaluation mechanisms were introduced (33). CME completion and improvements in service capabilities were incorporated as key evaluation criteria. Moreover, the use of online platforms to deliver CME courses was encouraged to resolve the conflict between clinical duties and training. From 2019 to 2024, medical consortia facilitated cross-institutional and cross-regional CME collaborations, relaxed CME credit requirements, and alleviated the training burdens on GPs (34, 35). Between 2022 and 2023, policies further promoted collaboration between GPs and specialists within medical teams (36). By 2025, the government began developing the standardized information systems for county-level medical consortia (37). The systems were designed to support remote consultations, enable the sharing of CME resources, and track training outcomes (37).
Innovations in CME within medical consortia
The synergy effect of medical consortia and CME
Mutual benefits were the primary driving force behind sustained CME training within medical consortia. CME was not merely an educational supplement but a critical element of healthcare improvement (38). PHC facilities benefited from specialist support and resource-sharing mechanisms, such as CME, imaging, and pathology services (38–40). Trained GPs were better equipped to make accurate referrals and conduct post-discharge follow-ups (41). The improved reputation of PHC fostered greater patient trust and led to increased local healthcare utilization (42). Tertiary hospitals reduced overcrowding by referring recovered patients back to PHC, thus reserving medical resources for complex cases. Training and collaboration within medical consortia significantly reduced professional burnout among rural GPs, enhancing clinical competence and well-being (43). A well-functioning medical consortia operated effectively without extensive government subsidies (44). Each stakeholder had an inherent incentive to uphold and grow the collaboration (44). A cohort study found that 71.3% of post-training GPs saw 10–30% more outpatients, 57.5% had 10–30% more patients who signed family-doctor contracts, and 83.8% reported higher levels of patient satisfaction (42).
Six components formed the core of the CME model in medical consortia (see Figure 3): (1) Teaching outpatient clinics / Clinical rounds, (2) Clinical skills training, (3) Theoretical lectures, (4) Research collaboration, (5) Online education, and (6) Advanced clinical training. The CME model in medical consortia integrated diverse teaching methods (Table 2), combining theory with practice to address the limitations of traditional approaches (42, 45, 46). It overcame geographical barriers and better met the needs of healthcare professionals across regions and specialties (25, 47).
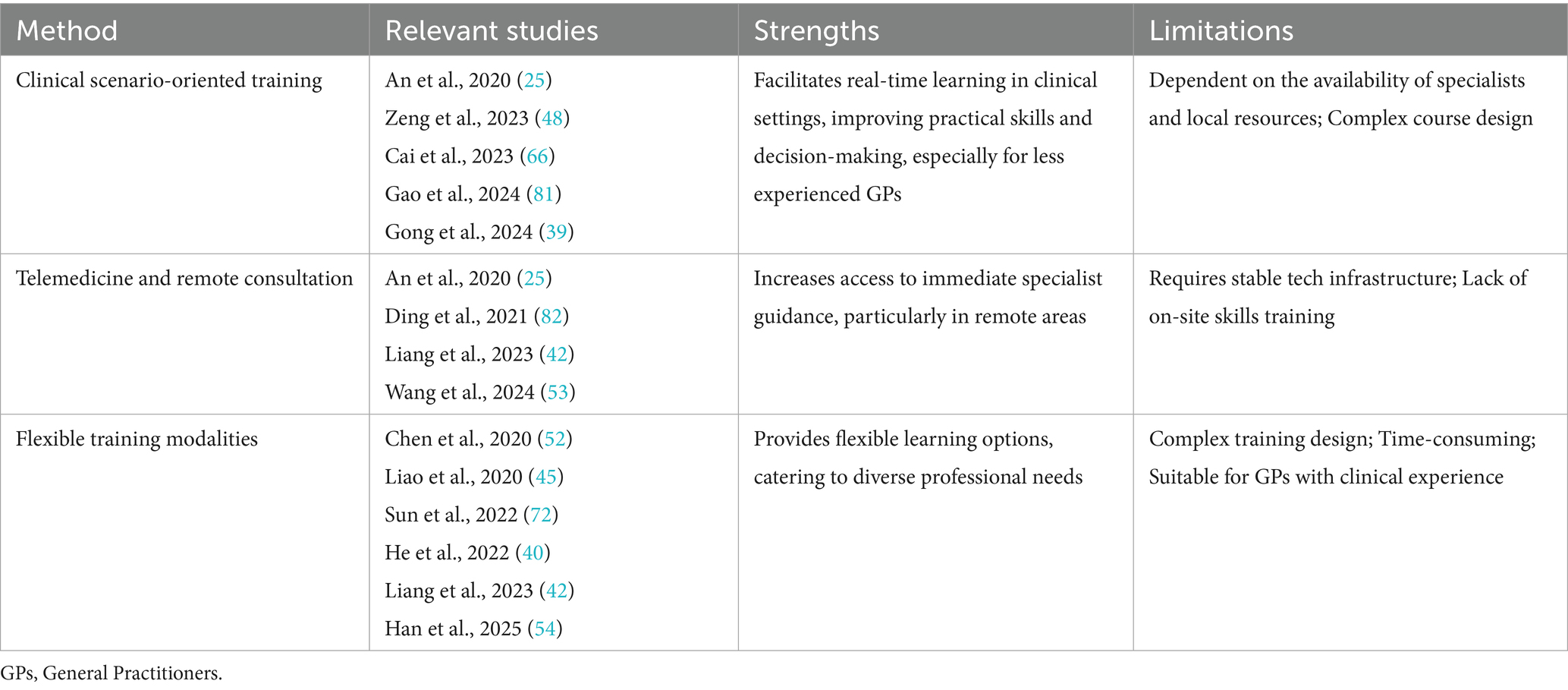
Clinical scenario-oriented training
The CME model within medical consortia emphasized training in realistic clinical settings. PHC centers were the main training hubs, with specialists from tertiary hospitals visiting regularly to conduct outpatient clinics, clinical rounds, and on-site teaching (25, 48). This arrangement allowed GPs to learn in real-time, enhancing both their practical skills and clinical decision-making (49). It also fostered specialist involvement in local patient care, thereby reducing unnecessary referrals (39).
Telemedicine and remote consultation
Comprehensive online education platforms offering a variety of learning modules, interactive sessions, and real-time consultations have improved the accessibility of CME (23, 50). Existing evidence indicated that online education reduced costs, improved access to education, and provided greater flexibility for learners with work and family commitments (28, 51). Many consortia integrated telemedicine platforms to facilitate real-time specialist consultations (25, 37, 42, 52). This approach enabled GPs to receive immediate guidance on diagnosis, treatment options, and patient management, especially in underserved regions (37). GPs benefited from a continuous learning pathway tailored to their specific professional needs, which in turn promoted ongoing professional development (25, 37).
Flexible training modalities
CME integrated both online and in-person learning (see Table 3). Online platforms broadened access to CME resources, particularly for GPs practicing in rural or remote areas (45, 53). Research collaboration and advanced clinical training further enriched the learning experience (42, 54). This blended-learning model provided flexibility, accommodating varying levels of prior knowledge and expertise (40).
Training content in medical consortia
CME programs tailored to the specific needs of GPs not only enhanced retention but also improved patient clinical outcomes (51). CME content focused on managing complex and chronic conditions through collaboration within medical consortia. It enhanced GPs’ clinical knowledge and adherence to evidence-based guidelines, improving patient referrals and follow-up care (28, 55). Research indicated that GPs often sought training that directly enhanced their clinical skills rather than administrative or policy-related content (56–58). Key chronic conditions covered include hypertension, dyslipidemia, type 2 diabetes, coronary heart disease, stroke, chronic obstructive pulmonary disease, osteoporosis, rehabilitation, and periodontal disease (56, 59). Training in clinical skills prioritized essential examinations, common care techniques, doctor-patient communication, shared decision-making, emergency care, cardiopulmonary resuscitation, and wound management (50, 60). New technologies, including wearable devices and artificial intelligence, were increasingly incorporated into the curriculum, improving diagnostic accuracy and healthcare delivery (61).
The public health component addressed vaccination programs, health screening strategies, infectious disease prevention, and maternal and child healthcare (62, 63). Health screenings aimed to identify and refer patients with conditions such as congenital heart disease in children, growth and developmental disorders, hypertension, diabetes, COPD, and common cancers (64, 65). Collaborative frameworks supported prompt responses to infectious disease outbreaks.
Institutional example: West China hospital-Fangcao community health service center medical consortium
The innovation of West China Hospital—Fangcao Community Health Service Center Medical Consortium (Huaxi-Fangcao medical consortium) was evident in three key areas: organization (staffing), administrative system, mechanism implementation, and four aspects of sharing: personnel, technology, equipment, and information (47). Fangcao Community Health Service Center (Fangcao) provided the necessary infrastructure, medical equipment, and financial support, while West China Hospital offered new medical technology, continuous CME, extensive teaching experience, and management expertise (47). Specialist physicians in endocrinology, respiratory medicine, oncology, dermatology, cardiology, neurology, hematology, nutrition, hepatology, rehabilitation, and mental health conducted daily consultations, teaching clinics, ward rounds, skills training, and research at Fangcao. Trained GPs were able to accurately refer complex cases either to specialist outpatient clinics or directly to West China Hospital for advanced care. Following clinical stabilization, patients were transferred back to Fangcao for ongoing management. Outpatient visits increased from approximately 102,000 in 2021 to approximately 138,000 in 2023, and the number of bidirectional referrals rose from 394 in 2021 to 2,300 in 2023.
Beyond the on-site collaborations, the Huaxi-Fangcao medical consortium jointly organized monthly CME sessions that combined online and face-to-face learning. By April 2025, 48 such training sessions had been conducted, incorporating theoretical lectures, practical skill workshops, and case discussions. GPs and other consortium members were also invited to attend West China Hospital’s regular academic activities, including seminars on frontier research and conferences on complex cases. In parallel, West China Cloud Classroom App was a mobile education platform, providing live broadcasts and recorded lectures to accommodate varied learning needs (25). GPs could additionally pursue advanced clinical training at West China Hospital to further develop their expertise.
Challenges in implementing CME within medical consortia
The insufficient support and lack of internal training incentives within medical consortia further hindered GPs’ effective participation in CME (66, 67). Training programs largely depended on external incentives, such as CME credits (34, 35). Although some institutions had implemented clinical skill competitions, regular competency assessments, and reward systems to encourage participation, these initiatives proved inadequate (48, 53, 66). Additionally, many GPs lacked clear career advancement pathways and financial incentives, limiting intrinsic motivation to engage in CME (68, 69). The increased workload required to acquire new skills, without corresponding financial remuneration, exacerbated GPs’ reluctance to participate in training (68).
There was a significant shortage of experienced and skilled GP trainers in medical consortia (30). Trainers in China only needed to complete a five-day theoretical course and a course design assignment to be certified (30, 51). Most GP trainers were hospital specialists who lacked experience in managing common medical conditions within the community. This issue was compounded by a limited understanding of the people-centered integrated care (PCIC) concept, which resulted in teaching content that was overly specialized and misaligned with the practical needs of GPs (70, 71). The teaching methods employed rely heavily on traditional and one-dimensional theoretical lectures with little emphasis on interactive and practical approaches, such as problem-based learning, case-based learning, and scenario simulation (45, 66, 72). Specialist doctors involved in mentoring GPs could lack appropriate incentives or performance recognition, which reduced motivation to invest time and resources in CME activities (71).
Several factors hindered the extension of face-to-face CME programs to township areas. There were notable regional disparities in the distribution of medical consortia, with the eastern regions being more developed (23, 73). In rural and remote areas, hospitals capable of providing CME resources were typically unavailable (8, 23). GPs faced constraints such as inadequate transport, limited funding, and a lack of awareness about the need for CME (73, 74). While online CME education has made rapid development in China (37), the practical application of telemedicine infrastructure may be insufficient (75). A survey of 84 PHC institutions across 23 counties in Sichuan Province found that although information hardware facilities were installed, only 47 institutions (56.0%) were connected to other units. Additionally, 34 institutions (41.0%) lacked information technology staff (75).
Recommendations
The positive performance feedback fosters a sense of accomplishment among GPs, including improvements in patient satisfaction and changes in income (43). From an organizational behavior perspective, existing studies in China showed that intrinsic motivators derived from job characteristics (such as professional growth, training opportunities, and task significance) exerted stronger influence on work outcomes than external incentives like administrative requirements or financial rewards (76). Enhancing CME quality was considered more effective in promoting active participation than relying on mandatory credit systems (76). When GPs perceive work as meaningful, it enhances intrinsic motivation to participate in CME (43). (1) Structured Incentive Mechanisms: CME teaching awards or opportunities of promotions should be conferred upon specialists or GPs who demonstrate excellence in training. (2) Intrinsic motivation reinforcement: Encouraging specialists to engage in multiple-site clinical practice within medical consortia enhances income sources and expands career development opportunities (77). Providing feedback on patient satisfaction and health improvements could help GPs perceive the direct impact of CME participation on their clinical work. (3) Expert-driven training: Inviting renowned experts with medical consortia to deliver training on emerging technologies can increase the credibility and appeal of CME (48, 78).
Training needs assessment is a crucial component for the development of training programs (30, 56). The training needs and skill requirements of GPs vary across different regions of China (79). Medical consortia should evaluate the teaching capabilities of specialists, as well as the satisfaction and effectiveness of training (30). Training content should be tailored to the practical needs of GPs, avoiding excessive specialization (56). Contemporary educational approaches, such as Problem-Based Learning (PBL), Case-Based Learning (CBL), and scenario-based simulations, foster active learning among GPs (80). Specialists mentoring GPs should be proficient in teaching methodologies and understand the core principles of PHC.
To address the low utilization of information equipment in CME, the following strategies are recommended: (1) Establish the online education platform to provide remote courses, thereby reducing reliance on equipment (25). (2) Facilitate equipment sharing among institutions within medical consortia (45, 66). (3) Prioritize the allocation of equipment to PHC institutions with high usage rates and demand, ensuring optimal utilization (75).
Strengths and limitations
The narrative review not only summarized the synergy and innovation between medical consortia and CME but also analyzed their advantages, challenges, and prospects. This review had several deficiencies. Firstly, the literature search focused on GPs as the primary trainees in CME programs, excluding pharmacists and nurses. Training needs and educational frameworks for pharmacists and nurses were distinct and varied. Secondly, the Huaxi-Fangcao Medical Consortium served as a practical example and policy application, rather than being based on empirically validated research findings. There was little published literature on CME with medical consortia. It was an important and understudied area of medical education. Future implementation science research is needed to advance CME strategies in medical consortia.
Conclusion
Medical consortia integrate resources and develop innovative CME models, such as scenario-based education, telemedicine, and flexible learning platforms. These models create synergy with medical consortia. However, several challenges remain, including insufficient incentives, a shortage of skilled trainers, and regional disparities. To address these challenges, it is important to strengthen GPs’ intrinsic motivation, promote career development, and adapt strategies to local contexts.
Author contributions
KA: Conceptualization, Writing – original draft. JZ: Validation, Writing – original draft. XW: Validation, Writing – original draft. YS: Writing – review & editing. SqL: Supervision, Writing – review & editing. SyL: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the 1.3.5 Projects for Disciplines of Excellence, West China Hospital, Sichuan University (grant no. ZYYC24001), the Community Health Association of China (grant no. 2021–2-045), and the National Natural Science Foundation of China (grant no. 72342014).
Acknowledgments
The study team is grateful to all colleagues participating in practices at Fang-cao Community Health Service Center (Chengdu, Sichuan, China) and Jin-cheng Community Health Service Center (Chengdu, Sichuan, China) who supported this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang, Y, Jin, H, Yang, H, Zhao, Y, Qian, Y, and Yu, D. Primary care functional features and their health impact on patients enrolled in the Shanghai family doctor service: a mixed-methods study. J Glob Health. (2025) 15:04007. doi: 10.7189/jogh.15.04007
2. Chen, P, Li, F, and Harmer, P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. (2019) 4:e447. doi: 10.1016/s2468-2667(19)30160-4
3. Zhang, C, and Gong, P. Healthy China: from words to actions. Lancet Public Health. (2019) 4:e438–9. doi: 10.1016/s2468-2667(19)30150-1
4. World Health Organization. (2016). Universal health coverage and health reform in China. Available online at: https://www.who.int/china/health-topics/universal-health-coverage (Accessed 2025.01.20).
5. Zhang, T, Xu, Y, Ren, J, Sun, L, and Liu, C. Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health. (2017) 16:42. doi: 10.1186/s12939-017-0543-9
6. Qin, A, Qin, W, Hu, F, Wang, M, Yang, H, and Li, L. Does unequal economic development contribute to the inequitable distribution of healthcare resources? Evidence from China spanning 2001-2020. Glob Health. (2024) 20:20. doi: 10.1186/s12992-024-01025-z
7. Dong, E, Xu, J, Sun, X, Xu, T, Zhang, L, and Wang, T. Differences in regional distribution and inequality in health-resource allocation on institutions, beds, and workforce: a longitudinal study in China. Archives of public health = Archives belges de sante publique. (2021) 79:78. doi: 10.1186/s13690-021-00597-1
8. Zhao, S, Wang, Y, Chen, Y, and Zhou, M. Healthcare resource allocation and patient choice: evidence from rural China. Int J Equity Health. (2025) 24:87. doi: 10.1186/s12939-025-02450-1
9. Lin, Y, Li, L, and Liu, B. Assessing the price levels of medical service and influential factors: evidence from China. BMC Public Health. (2024) 24:119. doi: 10.1186/s12889-024-17639-2
10. Li, L, and Liu, B. Spatial price differences of medical services: evidence from the Yangtze River Delta in China. BMC Health Serv Res. (2023) 23:761. doi: 10.1186/s12913-023-09774-0
11. Yu, W, Li, M, Ye, F, Xue, C, and Zhang, L. Patient preference and choice of healthcare providers in Shanghai, China: a cross-sectional study. BMJ Open. (2017) 7:e016418. doi: 10.1136/bmjopen-2017-016418
12. Yu, M, Yang, Z, Jiang, C, and Shi, L. Relationship between outpatients' sociodemographic and belief characteristics and their healthcare-seeking behavioral decision-making: evidence from Jiaxing city, China. PLoS One. (2022) 17:e0270340. doi: 10.1371/journal.pone.0270340
13. Yip, WN, Fu, HQ, Chen, AT, Zhai, TM, Jian, WY, Xu, RM, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. (2019) 394:1192–204. doi: 10.1016/S0140-6736(19)32136-1
14. Tu, J, Wang, C, and Wu, S. Skilled doctors in tertiary hospitals are already overworked in China--authors' reply. Lancet Glob Health. (2015) 3:e738. doi: 10.1016/s2214-109x(15)00190-4
15. Chai, Y, Liu, Y, Li, S, Zhang, L, Chen, D, and Yin, W. Can public hospital reform reduce medical resource mismatches? Evidence from China. Heal Econ Rev. (2024) 14:88. doi: 10.1186/s13561-024-00567-7
16. Xiao, Y, Wu, XH, Chen, J, and Xie, FF. Challenges in establishing a graded diagnosis and treatment system in China. Fam Pract. (2022) 39:214–6. doi: 10.1093/fampra/cmab089
17. National Health Commission of the People's Republic of China. 2023 Statistical Bulletin on the Development of Health and Healthcare in China. (2024) Available online at: https://www.gov.cn/lianbo/bumen/202408/content_6971241.htm. (Accessed 2025.01.02).
18. General Office of the State Council of the People's Republic of China. Guidance on Promoting the Construction and Development of Medical consortia. (2017) Available online at: https://www.gov.cn/gongbao/content/2017/content_5191699.htm. (Accessed 2024.12.23).
19. National Health Commission of the People's Republic of China. (2020) Notice on Releasing Management Measures for Medical consortia (Trial). Available online at: https://www.gov.cn/zhengce/zhengceku/2020-07/18/content_5528009.htm. (Accessed 2024.12.20).
20. Jiang, Q, Lou, Y, Chen, F, Lu, Z, and Cao, S. Keys to promoting the graded diagnosis and treatment system based on the integrated health care system in China. Fam Pract. (2022) 39:217–8. doi: 10.1093/fampra/cmab102
21. The State Council of the People's Republic of China. (2024) More than 18,000 medical consortia of various forms have been established nationwide. Available online at: https://www.gov.cn/lianbo/bumen/202402/content_6934829.htm. (Accessed 2025.08.31).
22. Yan, H, Han, Z, Nie, H, Yang, W, Nicholas, S, and Maitland, E. Continuing medical education in China: evidence from primary health workers' preferences for continuing traditional Chinese medicine education. BMC Health Serv Res. (2023) 23:1200. doi: 10.1186/s12913-023-10153-y
23. Hou, S, Zeng, X, Wang, T, Mou, B, Lei, Y, Wu, F, et al. A systematic evaluation of research on continuing education for general practitioners in China in the last decade. Chin Gen Pract. (2024) 27:3476–82. doi: 10.12114/j.issn.1007-9572.2023.0532
24. Wong, WCW, Zhu, S, Ong, JJ, Peng, M, Lam, CLK, and Kidd, MR. Primary care workforce and continuous medical education in China: lessons to learn from a nationwide cross-sectional survey. BMJ Open. (2017) 7:e015145. doi: 10.1136/bmjopen-2016-015145
25. An, K, Su, Q, Xu, J, Zhu, Y, Zhou, Y, Qu, F, et al. Training needs of general practitioners in the community health center within a compact medical consortium. Chin Gen Pract. (2020) 23:2825–30. doi: 10.12114/j.issn.1007-9572.2020.00.387
26. Liang, S, Deng, H, Liu, S, Wang, G, Li, L, and Wang, M. Competency building for lay health workers is an intangible force driving basic public health services in Southwest China. BMC Health Serv Res. (2019) 19:596. doi: 10.1186/s12913-019-4433-2
27. Wang, X, Qin, H, Zhu, Y, Wang, Z, Ye, B, and Zhu, X. Association of off-the-job training with work performance and work-family conflict among physicians: a cross-sectional study in China. BMJ Open. (2022) 12:e053280. doi: 10.1136/bmjopen-2021-053280
28. Lyu, X, and Li, S. Professional medical education approaches: mobilizing evidence for clinicians. Front Med (Lausanne). (2023) 10:1071545. doi: 10.3389/fmed.2023.1071545
29. Zeng, L, Li, Y, Zhang, L, Liu, G, Zhang, Y, and Zhen, S. Guideline use behaviours and needs of primary care practitioners in China: a cross-sectional survey. BMJ Open. (2017) 7:e015379. doi: 10.1136/bmjopen-2016-015379
30. An, K, Zhang, R, Zhu, B, Liu, L, Tang, J, and Ma, Y. Familiarity of teaching skills among general practitioners transfer training trainers in China: a cross-sectional survey. BMC Med Educ. (2023) 23:949. doi: 10.1186/s12909-023-04945-3
31. General Office of the State Council of the People's Republic of China. (2015) Guidance on Promoting the Construction of tiered diagnosis and treatment models. Available online at: https://www.gov.cn/zhengce/content/2015-09/11/content_10158.htm. (Accessed 2025.01.05).
32. National Health Commission of the People's Republic of China. (2017). Guidelines on the Pilot Work of Establishing Medical consortias. Available online at: http://www.nhc.gov.cn/yzygj/s3594q/201701/4a39ec35c70a4899b3e415b51e821464.shtml. (Accessed 2017.01.23).
33. National Health Commission of the People's Republic of China. (2018). Work Program for the Comprehensive Performance Assessment of a Medical consortia. Available online at: http://www.nhc.gov.cn/yzygj/s3594q/201808/570358dbf0af41238f46bb89e4af538b.shtml. (Accessed 2024.12.13).
34. National Health Commission of the People's Republic of China. (2024). Notice from the National Health Commission of the People's Republic of China on implementing measures to reduce the burden on primary healthcare and improve continuing medical education.
35. National Health Commission of the People's Republic of China. (2024) Notice from the National Health Commission of the People's Republic of China on Issuing the Management Measures for Continuing Medical Education Credits (Trial). Available online at: https://www.gov.cn/zhengce/zhengceku/202411/content_6985846.htm. (Accessed 2025.04.20).
36. National Health Commission of the People's Republic of China. (2023) Notice on the Pilot Construction of Closely Integrated City Medical Groups. Available online at: https://www.gov.cn/zhengce/zhengceku/2023-02/10/content_5740985.htm. (Accessed 2024.12.08).
37. National Health Commission of the People's Republic of China. (2025) Notice on the guidelines for the Informationization of closely Integrated County medical consortia. Available online at: http://www.nhc.gov.cn/guihuaxxs/gongwen12/202503/88e00b1afb4448ffb0d9391059bb1449.shtml. (Accessed 2025.04.23).
38. Cao, H, Yin, G, Bao, X, and Tao, H. Patient-centered evaluation of integrated care and health equity: evidence from county medical alliances in Henan province. Int J Equity Health. (2025) 24:101. doi: 10.1186/s12939-025-02468-5
39. Gong, F, Zhou, Y, Luo, J, Hu, G, and Lin, H. Health resource allocation within the close-knit medical consortium after the Luohu healthcare reform in China: efficiency, productivity, and influencing factors. Front Public Health. (2024) 12:1395633. doi: 10.3389/fpubh.2024.1395633
40. He, W, and Deng, G. Multi-mode joint application of remote electrocardiogram diagnosis and treatment base in continuing education. China Contin Med Educ. (2022) 14:146–149. doi: 10.3969/j.issn.1674-9308.2022.18.037
41. Peng, M, Li, L, Shi, X, and Wang, Z. Does integrated health management within a county medical consortium improve rural type 2 diabetic patients' self-management behavior and quality of life? An empirical analysis from eastern China. BMC Public Health. (2024) 24:1439. doi: 10.1186/s12889-024-18885-0
42. Liang, LB, Li, X, Liu, XP, Li, CZ, Luo, D, and Liu, F. Evaluation of the star family doctors training program: an observational cohort study of a novel continuing medical education program for general practitioners within a compact medical consortium: a quantitative analysis. BMC Med Educ. (2023) 23:250. doi: 10.1186/s12909-023-04210-7
43. Zhu, X, Chen, Y, and Liao, X. Factors underlying burnout among rural village physicians in southwestern China. Health Care Sci. (2023) 2:233–41. doi: 10.1002/hcs2.62
44. Li, H, Lu, Y, Wu, Z, Li, C, Wang, Q, and Tao, H. Construction strategy of medical resource integration in regional medical alliance based on grounded theory. Chin J Hosp Adm. (2021) 37:617–22. doi: 10.3760/cma.j.cn111325-20200928-01985
45. Liao, K, Liu, W, Peng, Z, Guan, N, and Zhang, Y. Case analysis of the role of regional medical association in promoting continuous medical education. Medical Educ Res Prac. (2020) 29:566–9. doi: 10.13555/j.cnki.c.m.e.2020.04.003
46. Ge, J, Geng, S, Jing, L, Jiang, H, and Sun, X. Exploration and practice of the "1 + 10 + 1100000" model. Int J Health Plann Manag. (2019) 34:1065–72. doi: 10.1002/hpm.2875
47. An, K, Su, Q, Li, S, Liao, X, and Jia, D. Practice and exploration of resource integration platform of general practice department in general hospitals. J Chengdu Medical College. (2022) 17:656–659,663. doi: 10.3969/j.issn.1674-2257.2022.05.024
48. Zeng, W, Tao, W, Yang, Y, Li, Y, Lu, B, and Zhao, Q. Perceived knowledge, attitudes and practices regarding the medical consortium among medical staff in Sichuan, China: a cross-sectional survey. BMC Health Serv Res. (2023) 23:1318. doi: 10.1186/s12913-023-10146-x
49. Luo, J, Dancel, E, Bains, S, Fanikos, P, and Fischer, MA. Academic detailing in the new era of diabetes medication management. Curr Diab Rep. (2019) 19:140. doi: 10.1007/s11892-019-1252-0
50. Lyu, X, Li, J, and Li, S. Approaches to reach trustworthy patient education: a narrative review. Healthcare (Basel, Switzerland). (2024) 12:2322. doi: 10.3390/healthcare12232322
51. You, C, Wang, L, Zhang, J, and Yao, M. China's national continuing medical education program for general practitioners: a cross-sectional survey (2016-2023). BMC Med Educ. (2025) 25:72. doi: 10.1186/s12909-025-06682-1
52. Chen, W, and Ma, L. Exploration and practice of intelligent family doctor studio in Beijing Fengtai district. Chin J Gen Pract. (2020) 19:1059–62. doi: 10.3760/cma.j.cn114798-20200303-00219
53. Wang, L, Wei, LJ, Zheng, WT, Liu, YJ, Xu, Y, and Wang, MZ. Exploration and contemplation of homogenized education of specialists in pulmonary and critical care medicine at member hospitals of a hospital consortium. Zhonghua Jie He He Hu Xi Za Zhi. (2024) 47:490–3. doi: 10.3760/cma.j.cn112147-20231011-00216
54. Han, X, Wei, J, and Yu, X. Research on the role of university-affiliated traditional Chinese medicine hospitals in enhancing primary healthcare service capacity through medical consortia. China rural health. (2025) 17:17–20. doi: 10.20126/j.cnki.1674-361X.2501-003
55. Liu, C, Tang, S, An, K, Zhang, S, Zhou, Y, and Su, N. Knowledge, attitude, and practice of metformin extended-release tablets among clinicians in China: a cross-sectional survey. Front Pharmacol. (2021) 12:634561. doi: 10.3389/fphar.2021.634561
56. An, K, Zhang, L, Qiao, RJ, Li, CZ, Zhong, Q, and Ma, YR. Training needs and curriculum of continuing medical education among general practitioners in Tibet, China: a cross-sectional survey. Front Public Health. (2022) 10:914847. doi: 10.3389/fpubh.2022.914847
57. An, K, Wu, Z, Zhang, L, Li, Y, An, Z, and Li, S. Knowledge, attitude, and practice of chronic insomnia management among general practitioners in China: a cross-sectional survey. BMC primary care. (2024) 25:365. doi: 10.1186/s12875-024-02615-x
58. Zhong, Q, An, K, Wu, Z, Zhang, H, Li, S, Zhang, L, et al. Knowledge and awareness of nicotine, nicotine replacement therapy, and electronic cigarettes among general practitioners with a special interest in respiratory medicine in China. Front Med (Lausanne). (2023) 10:1236453.
59. Wang, S, and Li, S. Type 2 diabetes, heart failure and the treatment of their comorbidity. Minerva Med. (2024) 116:141–155. doi: 10.23736/S0026-4806.24.09264-4
60. An, K, Wu, Z, Qiu, Y, Pan, M, Zhang, L, and An, Z. Shared decision making in sarcopenia treatment. Front Public Health. (2023) 11:1296112. doi: 10.3389/fpubh.2023.1296112
61. Ma, M, Li, Y, Gao, L, Xie, Y, Zhang, Y, and Wang, Y. The need for digital health education among next-generation health workers in China: a cross-sectional survey on digital health education. BMC Med Educ. (2023) 23:541. doi: 10.1186/s12909-023-04407-w
62. Meng, Q. Strengthening public health systems in China. Lancet Public Health. (2022) 7:e987–8. doi: 10.1016/s2468-2667(22)00206-7
63. Li, X, Lu, J, Hu, S, Cheng, KK, De Maeseneer, J, Meng, Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
64. Gong, W, and Cheng, KK. Challenges in screening and general health checks in China. Lancet Public Health. (2022) 7:e989–90. doi: 10.1016/s2468-2667(22)00207-9
65. Xia, C, Basu, P, Kramer, BS, Li, H, Qu, C, and Yu, XQ. Cancer screening in China: a steep road from evidence to implementation. Lancet Public Health. (2023) 8:e996–e1005. doi: 10.1016/s2468-2667(23)00186-x
66. Cai, L, and Sheng, Q. Practical exploration of building a compact medical consortium. Chin Prim Health Care. (2023) 37:23–6. doi: 10.3969/j.issn.1001-568X.2023.06.0007
67. Chen, D, Ma, Y, Chen, Y, and Huang, H. Analysis on key aspects of cultural integration for cross-region specialists alliances of closed cooperation. Chin J Hosp Adm. (2020) 36:184–7. doi: 10.3760/cma.j.issn.1000-6672.2020.03.003
68. Pan, D, and Yu, L. Study on the career development of clinical medicine graduates in township hospitals guided by the healthy China strategy. Chin J Med Educ. (2019) 39:236–40. doi: 10.3760/cma.j.issn.1673-677X.2019.03.019
69. Zou, C, Liao, XY, Spicer, J, and Hayhoe, B. Ten years' GP training in China: progress and challenges. Br J Gen Pract. (2020) 70:511–2. doi: 10.3399/bjgp20X712961
70. Zhang, B, Qian, Y, Ling, B, Li, X, and Wang, G. Effectiveness of integrated teaching methods in the training of general practitioners' surgical-related professional competencies. China Health Industry. (2023) 20:176–9. doi: 10.16659/j.cnki.1672-5654.2023.10.176
71. Shan, Y, Yuan, L, Fan, C, Tang, S, Lu, J, and Huang, X. Survey on cognition of general practice residency training and willingness of teaching among specialists. Chin J Gen Pract. (2022) 21:349–54. doi: 10.3760/cma.j.cn114798-20210928-00734
72. Sun, S, Wei, Q, Qiu, X, Yang, Y, and Zhang, H. Practical insights and reflections on the management of continuing medical education in traditional Chinese medicine hospitals under the trustee mode. Modern Hospital Manag. (2022) 20:58–60. doi: 10.3969/j.issn.1672-4232.2022.02.016
73. Shan, L, Gan, Y, Yan, X, Wang, S, Yin, Y, and Wu, X. Uneven primary healthcare supply of rural doctors and medical equipment in remote China: community impact and the moderating effect of policy intervention. Int J Equity Health. (2024) 23:97. doi: 10.1186/s12939-024-02183-7
74. Chen, Y, Yang, K, Jing, T, Tian, J, Shen, X, and Xie, C. Use of text messages to communicate clinical recommendations to health workers in rural China: a cluster-randomized trial. Bull World Health Organ. (2014) 92:474–81. doi: 10.2471/blt.13.127076
75. Chen, L, Wu, Y, Li, J, and Zhu, L. Development of informatization in primary care in China's regions inhabited by ethnic minorities. Chin Gen Pract. (2022) 25:2003–7. doi: 10.12114/j.issn.1007-9572.2022.0139
76. Zhao, S, Ping, J, Zhu, H, Ji, W, Wang, Y, and Wang, Y. Job characteristics model-based study of the intrinsic incentive mechanism for primary health workers. Chin Gen Pract. (2023) 26:3118–26. doi: 10.12114/j.issn.1007-9572.2022.0642
77. Xu, L, and Zhang, M. Regulated multi-sited practice for physicians in China: incentives and barriers. Global Health Journal. (2018) 2:14–31. doi: 10.1016/S2414-6447(19)30117-4
78. Cui, GY, Yao, ML, Zhang, X, Guo, YK, Li, HM, and Yao, XP. The effects of initial participation motivations on learning engagement in transition training for future general practitioners in rural China: perceived deterrents as mediator. Med Educ Online. (2016) 21:30998. doi: 10.3402/meo.v21.30998
79. Li, X, Krumholz, HM, Yip, W, Cheng, KK, De Maeseneer, J, and Meng, Q. Quality of primary health care in China: challenges and recommendations. Lancet. (2020) 395:1802–12. doi: 10.1016/s0140-6736(20)30122-7
80. Yan, J, Wen, Y, Liu, X, Deng, M, Ye, B, and Li, T. The effectiveness of problem-based learning and case-based learning teaching methods in clinical practical teaching in TACE treatment for hepatocellular carcinoma in China: a bayesian network meta-analysis. BMC Med Educ. (2024) 24:665. doi: 10.1186/s12909-024-05615-8
81. Gao, H, Wang, Y, and Wang, Z. Application of PBL teaching method in cultivating talents in pediatric specialty alliances. Jiangsu Healthcare Admin. (2024) 35:1647–9. doi: 10.3969/j.issn.1005-7803.2024.11.035
Keywords: medical and health consortia, telemedicine, general practitioner, primary care, continuing medical education
Citation: An K, Zhang J, Wang X, She Y, Li S and Li S (2025) Integration and innovation: medical and health consortia improving continuing medical education in China. Front. Public Health. 13:1633363. doi: 10.3389/fpubh.2025.1633363
Edited by:
Lei Shi, Guangzhou Medical University, ChinaReviewed by:
Shenshen Gao, Shanghai Jiao Tong University, ChinaAnil Kumar Marapaka, Purdue University, United States
Copyright © 2025 An, Zhang, Wang, She, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheyu Li, bGlzaGV5dUBnbWFpbC5jb20=; Shuangqing Li, bHNxaHhqa0AxMjYuY29t
†These authors have contributed equally to this work
 Kang An
Kang An Jinyi Zhang
Jinyi Zhang Xingyou Wang
Xingyou Wang Yi She
Yi She Shuangqing Li
Shuangqing Li Sheyu Li
Sheyu Li