- 1Medical Oncology, University of Rome “La Sapienza”, Rome, Italy
- 2Oncological Orthopaedics Unit, IRCCS Regina Elena National Cancer Institute (IRE), Rome, Italy
- 3UOSD Sarcomas and Rare Tumours, IRCCS Regina Elena National Cancer Institute (IRE), Rome, Italy
- 4Oncology and Oncohematology Unit, Regional General Hospital “F. Miulli”, Bari, Italy
Background: Due to their rarity and complexity sarcomas require specialized multidisciplinary team management. COVID-19 pandemic brought to a rapid implementation of telemedicine and activation of digital tools. This study evaluates the perception of virtual disease multidisciplinary team among healthcare professionals of an European rare cancer referral center.
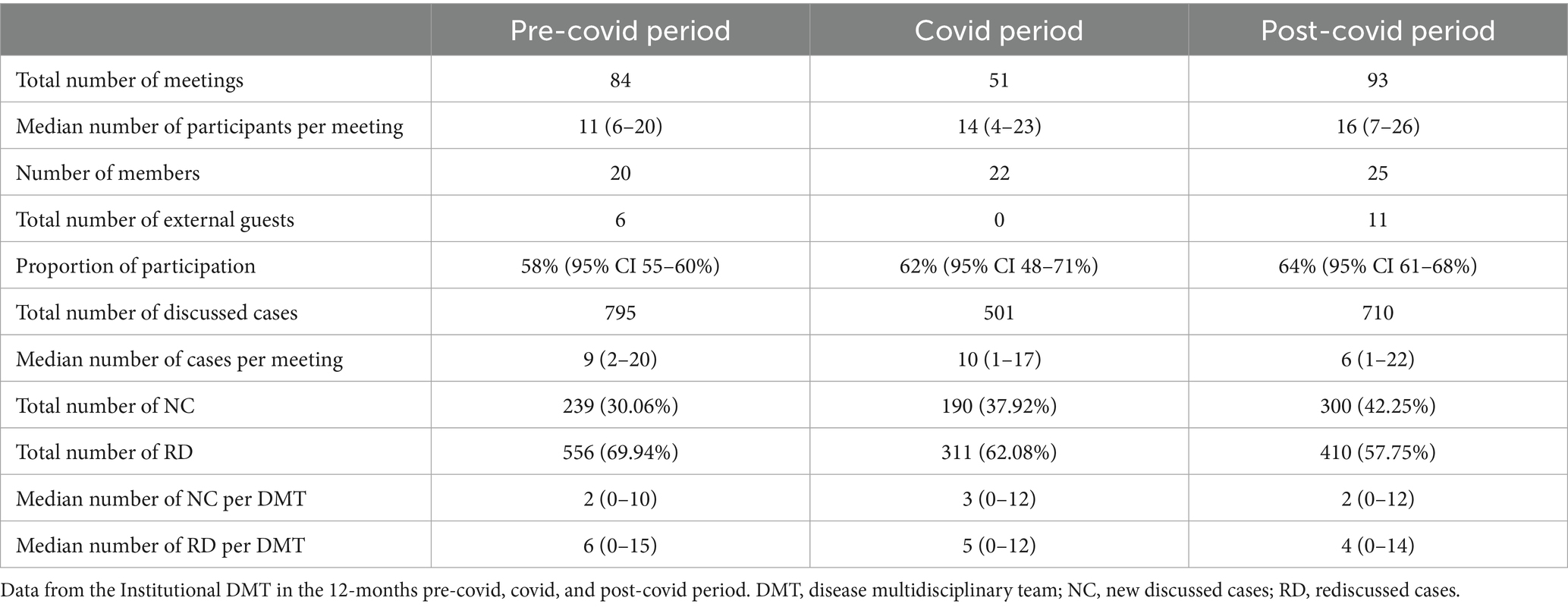
Methods: An online survey was administered to the participants of Regina Elena National Cancer Institute’s Sarcoma disease multidisciplinary team meetings held between 2020 and 2022. It was composed of 40 questions comparing face-to-face and virtual meetings. Data from the Institutional disease multidisciplinary team from 2019 to 2022 were also analyzed retrospectively to compare the pre-covid, covid, and post-covid phases.
Results: Twenty-two healthcare professionals answered the survey. In their opinion, decision-making process was not affected by virtual modality (86.0%). Regarding virtual meetings 90.0% were highly/moderately satisfied with depth of discussion, 95.0%–100% were able to interact adequately and access all relevant data. The most important improvements of virtual disease multidisciplinary team were better quality of clinical approach/research (22.7%–31.8%), technological innovations (50.0%), and logistical setting (95.5%). 90.0% to 100% thought that virtual disease multidisciplinary team could be approved thereafter. We observed an increase in participation rate from 58.0, to 62.0%, to 64.0% (p = 0.0159) and a rise in the new cases discussed at meetings compared to the re-discussed ones from 30.1% to 37.9% to 42.3% (p < 0.0001) in the pre-covid, covid, and post-covid phases, respectively.
Conclusion: Virtual disease multidisciplinary team enhances participation and discussion quality without compromising patient care.
1 Introduction
Sarcomas are extremely rare malignant tumors and represent less than 1% of all new malignancies’ diagnosis (1). The 5th edition of World Health Organization (WHO) classification recognizes more than 80 different histological types of sarcomas categorized as soft tissue (STS) or bone sarcomas (BS) (2).
STS incidence increases with age, with a peak between 80 and 89 years and a mean age of diagnosis around 60 years. BS have a bimodal age distribution, with peaks between ages 10 and 30 and 60 and 90 (1).
In Europe, the incidence of STS is 4–5 new cases/100,000 people, which is six times more common than BS, whose incidence is around 0.8 new cases/100,000 people (3). In Italy, in 2021 about 2,300 new cases were detected (1,400 among men and over 900 in women), with a prevalence of about 29,000 people living with a diagnosis of sarcoma (4).
Besides being rare, they are also sneaky tumors as they are ubiquitous with often non-specific symptoms and consequently a diagnosis more complex and challenging, often leading to a delay (5–7). Prognosis varies greatly and European countries follow different indications on trying to establish the best-possible care. Many countries have their own sarcoma networks and collaborate on several European-funded research projects. In Italy, cancer treatment is performed in various general hospitals or cancer centres throughout the country, but most of these are not highly specialised in the treatment of sarcomas, which are therefore referred to centres recognised by European Reference Network on Rare Adult Cancers (EURACAN) (8–10).
Disease multidisciplinary team (DMT) meetings represent a crucial step in decision-making process, with the aim of defining an optimal therapeutic strategy in relation to shared guidelines (11). Nowadays it constitutes the standard of care as it optimizes the coordination between all the necessary professionals involved in patients’ care and several national guidelines (12). DMT should be composed by a core of experts including all the necessary key professionals: surgeon with experience in cancer treatment, medical oncologist, radiologist, pathologist, radiotherapist, case manager, and data manager. Other professionals both internal to the institute and external consultants can be involved, according to the needs and the complexity of the individual case discussion (13). Multidisciplinary meetings make the clinician feel more confident with the therapeutic decision, significantly shortens the interval from diagnosis to treatment, leads to a better patient experience and an increase in the quality of care for patients (14). Some evidences suggest that implementing DMT discussions improves patients’ outcomes and reduced cancer-related mortality, although it remains difficult to evaluate the real effect on survival (15–17). All studies concluded that a multidisciplinary setting resulted in improved patient outcomes in terms of diagnosis and/or treatment planning, improvements in survival, patient satisfaction, and clinician satisfaction as a consequence of teamwork communication and cooperation (18).
The COVID-19 pandemic due to SARS-CoV-2 infection has imposed a sudden and rapid reorganization in care management and affected the professional life of the entire healthcare sector, including the Centres dedicated to the treatment of oncological diseases (19–23). This resulted in the adherence of all health professionals to the preventive measures recommended by WHO and government measures, including social distancing, logistical limitations, and restrictions on interpersonal exchanges (24). It also gave the opportunity to activate digital health tools such as the transition from face-to-face (FTF) DMT meetings to virtual ones (vDMT).
The aim of this study is to examine and describe the experience of the Institutional Sarcoma DMT in carrying out virtual meetings, comparing this new modality with the previous FTF one, and to investigate how DMT participants perceive the introduction of the virtual modality by administering a survey to them. Some aspects in terms of advantages, disadvantages and effectiveness of virtual modality are discussed in order to see if the adoption of this procedure is valuable in the decision-making process and in amelioration of clinical practice.
2 Materials and methods
We administered an online survey (Table 1) to the participants of the biweekly Sarcoma DMT meetings held at Regina Elena National Cancer Institute of Rome, an EURACAN referral centre.
We formulated 40 questions, divided in four sections: the first section (14 questions) was about the experience of individual professional in DMT; the second section (10 questions) asked opinions about FTF meetings; the third (11 questions) about the virtual one; the last section (5 questions) inquires about the future perspectives of the online modality. Questions contemplated 12 yes/no answers, 15 multiple choice answers with one or more items to be selected, two 5-points Likert scale, and 11 open answers. The survey was conceived by one medical doctor participating in DMT meetings and independently reviewed by three other medical doctors participants in sarcoma DMT meetings, before starting the study.
We also analysed in a retrospective way the registries of all the DMT meetings held from 9 March 2019 to 8 March 2022 including data about numbers of participants, numbers of external participants, and numbers of discussed cases (new cases vs. known cases discussed several times).
We performed a descriptive statistic for the survey responses. Subsequently, we analysed data from the institutional DMT. We defined three different time periods by using the date of National lockdown beginning in Italy (9 March 2020) as cutoff: a pre-covid phase extending from 9 March 2019 to 8 March 2020; a covid phase extending from 9 March 2020 to 8 March 2021, and post-covid phase extending from 9 March 2021 to 8 March 2022. We analysed all the data from the institutional DMT focusing on time periods, without calculating a sample size.
We checked normality by Kolmogorov–Smirnov test for all the continuous variables. The study groups were compared using Kruskal–Wallis test, followed by Dunn’s multiple comparison test, or Mann–Whitney U test as appropriate. The number of new cases and re-discussed cases per time-period were analysed by Chi Square test. Statistical analysis was performed by means of Prism GraphPad v.9 software, Insightful Science.
3 Results
3.1 Survey results
A total of 22 out of 25 healthcare professionals participating to the DMT, corresponding to a response rate of 88.0%, have answered to the survey: seven orthopaedics, four oncologists, one radiotherapist, two pathologists, one radiologist, one nuclear medicine physician, one psychologist, two residents in training, two data managers, and one case manager. Thirteen of the participants have been working in their specialty for more than 10 years, seven between 5 and 10 years, and two for less than 5 years. Thirty-six percent of them usually join other DMT meetings (otorhinolaryngology, melanoma, thyroid, breast, hematologic, gastrointestinal, head & neck, and gynecologic DMT); 18.0% had already participated in a virtual meeting before this experience.
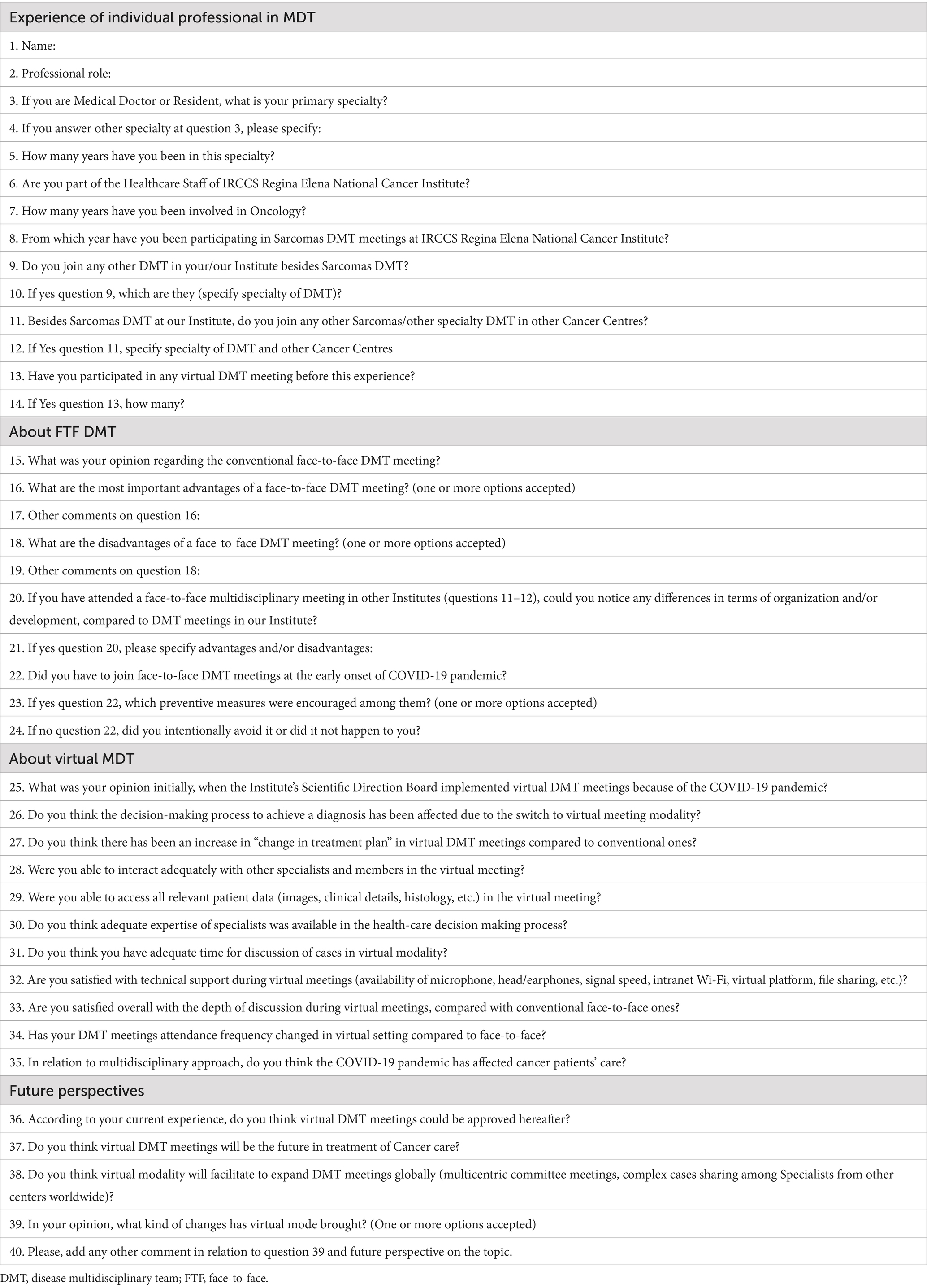
Overall, 91.0% answered that FTF modality was good or very good and that the most important advantages were the facilitation in interaction with other participants (68.0%) and greater attention to discussion because of the predefined duration (50.0%). However, the disadvantages observed by the participants were various: less attention to discussion for 27.3% of the participants; the possibility of attendance only on site for 27.3%; the difficulty in interaction and data sharing for 22.7%; and the poor imaging resolution and evaluation for 36.4% (Figure 1A).
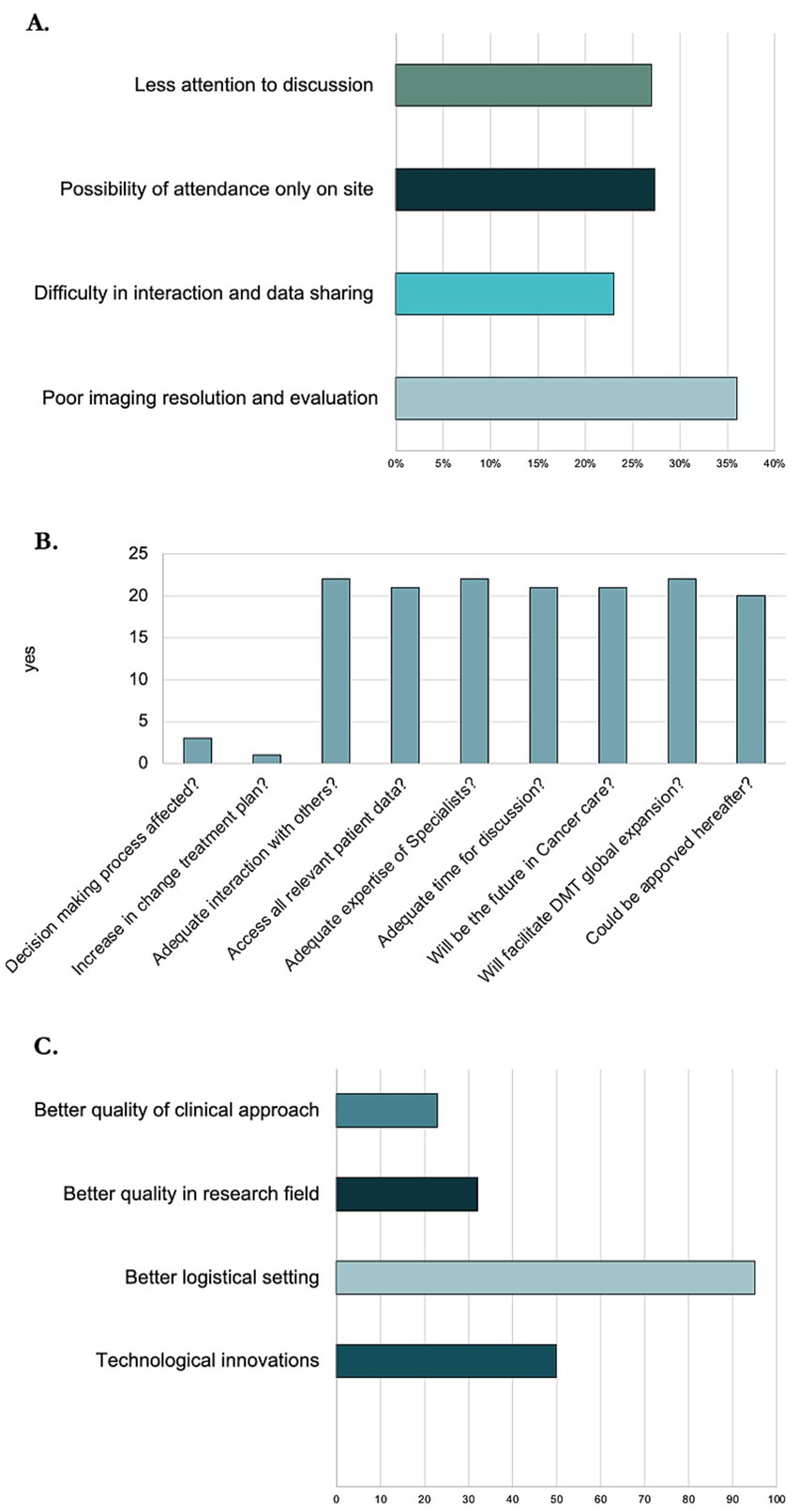
Figure 1. Survey data about opinion on virtual and face-to-face DMT. (A) Bar chart representing disadvantages of face-to-face DMT. (B) Bar chart representing opinions about virtual DMT. (C) Bar chart representing changes that virtual DMT has brought.
About the vDMT (Figure 1B): 86.0% thought that the decision-making process had not been affected and 95.0% stated that there was not a change in the treatment plans; 100% were still able to interact adequately with other specialists and members and to access all relevant patient data (images, clinical details, histology, etc.) and affirmed that an adequate expertise of specialists was available in the decision-making process. For the majority (95.0%) the time available for the discussion of cases was adequate.
In general, 90.0% were highly or moderately satisfied overall with the depth of discussion and above all with the technical support (availability of microphone, head/earphones, signal speed, intranet Wi-Fi, virtual platform, file sharing, etc.). Participants declared that the attendance at the meetings with the new modality was similar (68.0%) or increased (32.0%).
In the opinion of the participants, the most important change that the virtual mode brought was better quality of clinical approach (22.7%) and of the research field (31.8%). Moreover, there has been a notable important technological innovation (50.0%), and a better logistical setting, like the possibility to connect outside the hospital (95.5%) (Figure 1C).
Finally, 91.0% thought that vDMT could be approved hereafter and 100% stated that it would facilitate the global expansion of DMT meetings (multicentre committee meetings, complex case sharing among specialists from other centres worldwide).
3.2 Institutional DMT data
Analysing data from the Institutional DMT (Table 2), in the 12-months pre-covid period we held 84 meetings, and the median number of participants was 11 (range: 6–20) over 20 members and we had only six external guests in a few meetings. During the 12-months covid period we held 51 meetings with a median number of participants of 14 (range: 4–23) over 22 members with no external guests. In the 12-months post-covid period we held 93 meetings, and the median number of participants was 16 (range: 7–26) over 25 members and we had 11 external guests in many meetings. The median proportion of participation (Figure 2A) in the three different periods was, respectively, in the pre-covid, covid, and post-covid periods of 58.0% (95% CI 55.0%–60.0%), 62.0% (95% CI 48.0%–71.0%), and 64.0% (95% CI 61.0%–68.0%), with an increase in participation rate statistically significant from the pre-covid to the post-covid period (p = 0.0159). The multiple comparison analysis showed that only the difference between the median participation rate during pre- and post-covid period was statistically different (p = 0.0127).
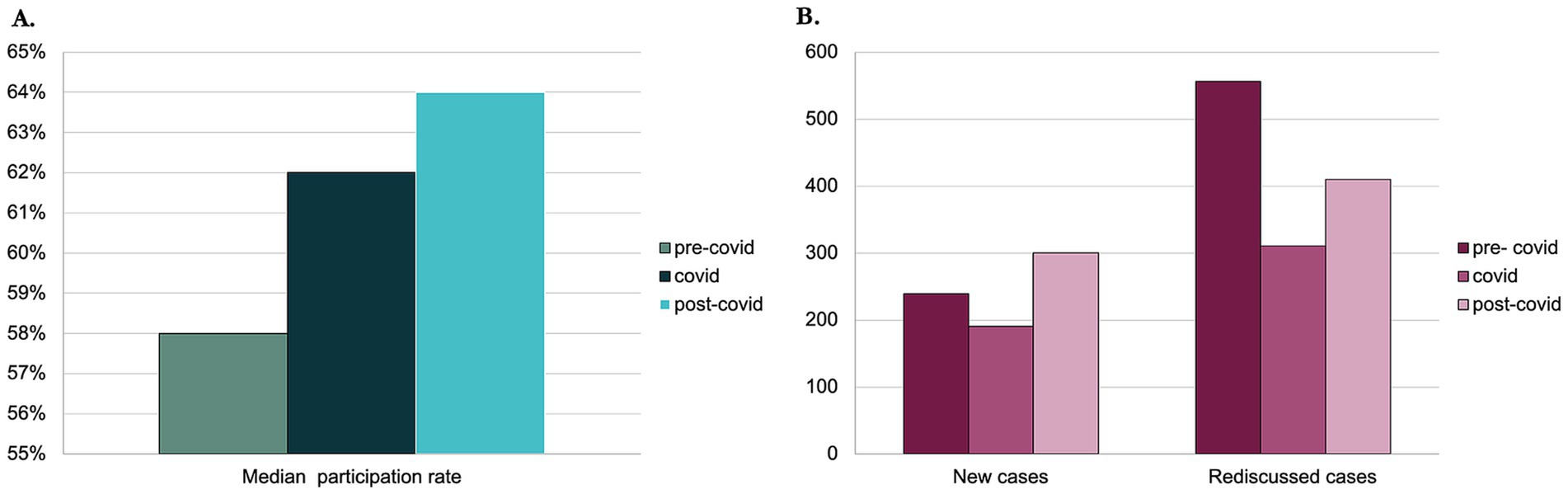
Figure 2. Data from Institutional DMT. (A) Bar chart representing the rise of participation rate between the pre-covid, covid, and post-covid periods. (B) Bar chart representing the number of new cases and re-discussed ones between pre-covid, covid, and post-covid periods.
The number of discussed cases was 795 in the pre-covid period with a median of nine cases per meeting, 501 cases with a median of 10 cases per meeting in the Covid period, and 710 with a median of six cases per meeting in the post-covid period. The proportion of new discussed cases as compared to the re-discussed ones (Figure 2B) raised from 30.1% (239 cases) in the pre-covid period, to 37.9% (190) in the covid period, and 42.3% (300) in the post-covid period (p < 0.0001).
4 Discussion
With the onset of the COVID-19 pandemic, telemedicine has rapidly spread throughout the medical field in various contexts, from remote consultations to conferences and online meetings. Teleconsultation between professionals via validated platforms will be the virtual mode of interaction between predefined national reference centres (all of which are already EURACAN centres and so-called “provider centres”) and local centres (so-called “user centres”) within the Italian National Rare Tumors Network (RNTR) (25). In this Network, which is currently being implemented and is in the pilot phase in some Italian regions, clinical cases can be discussed at a multidisciplinary level to ensure the correct diagnostic and therapeutic approach, avoiding unnecessary travel for patients as far as possible.
Virtual DMT for musculoskeletal oncology care has been reported, following the pandemic, as a valuable and effective tool with the aim to simplify a satisfying interaction between specialists (26). Similarly, to other few experiences reported in literature, the results of our survey showed that virtual DMT gives the possibility to break the geographical barriers. It can optimize the work because of the lack of need for a fixed place of meeting increases the flexibility of the work, with no additional travel requirements, which is a factor that may improve attendance (27).
In fact, our results have shown that with the virtualization of the meetings, the attendance was similar or even increased with a median participation that shifted from 58.0% in the pre-covid period to 64.0% in the post-covid one. While in the pre-covid period we observed occasionally the participation of external guests and no one in the covid period, in the post-covid period we registered 11 external guests in total with almost always one guest at every meeting. From our point of view, this data is important, as the participation of external guests, facilitated by the possibility of connecting online, allows for cooperation in the management of patients in the community, and is especially important for a rare disease such as sarcoma, where it is essential that patients are referred to specialist centres. The experience reported shows an increase in the number of meetings from pre-covid period to the post-covid one (from 84 to 51 to 93 meetings in a year). These numbers dropped during the covid period due to the temporary interruption of DMT meetings before the introduction of the virtual modality. A possible reason for the rise in the post-covid period was the gradual recovery of clinical activity and the reduction of sanitary limitations, but it could be linked also to a more organized and simple way of organizing meetings.
From the results of the survey, the introduction of virtual modality has not had any impact on the depth or attention to discussion but rather improved it and there was not a change in treatment plan. The survey results show that 27.3% considered a disadvantage to only be able to participate on site. Twenty-two point 7 % of participants perceived difficulties in interacting and sharing data, and 36.4% believed that image resolution was poorer in the FTF DMT. On the contrary, 90% of participants were highly or moderately satisfied with the technological support provided by the virtual mode. Ninety-one percent of survey participants believed that virtual DMT could be approved in the future, and all participants agreed that the virtual format could encourage the expansion of meetings. Reflecting the survey results, DMT continues to be virtual in our institute, despite the fact that there are no longer any pandemic restrictions. Furthermore, since 2021, our institute has implemented online platforms for recording discussed cases and the attendance of healthcare professionals. As proof that virtual DMT is a valid method for discussing cases, over 800 cases were discussed in 2024.
The survey presented in this article was proposed to assess the degree of appreciation within the multidisciplinary working group dedicated to the treatment of sarcomas at our institute. For this reason, the number of participants is small, that is the principal limitation of this study. Another limitation of the study is that the survey was designed and evaluated by members of the same working group to which it was then proposed, and was not subjected to a validation process.
5 Conclusion
Five years after the COVID-19 spread, literature data regarding vDMT meetings remains scarce. Results from this experience showed that the vDMT have been accepted by healthcare professionals with high satisfaction level, due to a better quality of clinical approach/research, technological innovations, and especially logistical setting. In fact, analysing data from institutional DMT we observed an increase in participation rate.
Results from this experience should be extended to all institutional DMT meetings and/or to other reference centres for the treatment of sarcomas. Given the results of our survey, the implementation of virtual DMT or, alternatively, a hybrid form combining in-person and virtual meetings, could become the standard.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
FS: Writing – original draft, Writing – review & editing. BR: Investigation, Data curation, Visualization, Validation, Methodology, Conceptualization, Writing – original draft, Supervision, Writing – review & editing, Project administration, Formal analysis, Funding acquisition. CO: Supervision, Software, Visualization, Investigation, Conceptualization, Formal analysis, Writing – review & editing, Validation, Data curation, Writing – original draft, Methodology. SV: Investigation, Writing – review & editing, Writing – original draft, Conceptualization. SC: Writing – review & editing, Investigation, Writing – original draft. EC: Investigation, Resources, Writing – review & editing, Writing – original draft, Software. AC: Writing – review & editing, Writing – original draft. FR: Writing – review & editing, Writing – original draft. DR: Writing – review & editing, Writing – original draft. RB: Writing – original draft, Supervision, Conceptualization, Writing – review & editing. VF: Funding acquisition, Writing – original draft, Investigation, Writing – review & editing, Methodology, Project administration, Supervision, Validation, Conceptualization, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by Ricerca Corrente from Italian Ministry of Health. This work was financially supported through funding from the institutional “Ricerca Corrente” granted by the Italian Ministry of Health.
Acknowledgments
We acknowledge all the participants to the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gronchi, A, Miah, AB, Dei Tos, AP, Abecassis, N, Bajpai, J, Bauer, S, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN-GENTURIS clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. (2021) 32:1348–65. doi: 10.1016/j.annonc.2021.07.006
2. WHO Classification of Tumours Editorial Board. Soft tissue and bone tumours. In C. Fletcher, J. A. Bridge, P. C. W. Hogendoorn, and F. Mertens, (eds). International Agency for Research on Cancer, editor WHO classification of tumours, 5th; Lyon, France: World Health Organization, (2020); Volume 3.
3. Stiller, CA, Trama, A, Serraino, D, Rossi, S, Navarro, C, Chirlaque, MD, et al. Descriptive epidemiology of sarcomas in Europe: report from the RARECARE project. Eur J Cancer. (2013) 49:684–95. doi: 10.1016/j.ejca.2012.09.011
4. AIOM/AIRTUM. I numeri del cancro in Italia (2023). Available online at: https://www.aiom.it/wp-content/uploads/2023/12/2023_AIOM_NDC-web.pdf. (Accessed July 12, 2024).
5. Brasme, JF, Morfouace, M, Grill, J, Martinot, A, Amalberti, R, Bons-Letouzey, C, et al. Delays in diagnosis of paediatric cancers: a systematic review and comparison with expert testimony in lawsuits. Lancet Oncol. (2012) 13:e445–59. doi: 10.1016/S1470-2045(12)70361-3
6. Foersch, S, Eckstein, M, and Wagner, DC. Deep learning for diagnosis and survival prediction in soft tissue sarcoma. Ann Oncol. (2021) 32:1178–87. doi: 10.1016/j.annonc.2021.06.007
7. AIOM. Linee guida sarcomi dei tessuti molli e GIST. Edizione (2021). Available online at: https://www.iss.it/documents/20126/8403839/LG+492+AIOM_Sarcomi+2024.pdf/9215b6f4-a396-0d19-731a-8d027e964f02?t=1715072292467. (Accessed July 12, 2024).
8. Casali, PG, Bielack, S, Abecassis, N, Aro, HT, Bauer, S, Biagini, R, et al. Bone sarcomas: ESMO-PaedCan-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. (2018) 29:iv79–95. doi: 10.1093/annonc/mdy310
9. Casali, PG, Abecassis, N, Aro, HT, Bauer, S, Biagini, R, Bielack, S, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. (2018) 29:iv51–67. doi: 10.1093/annonc/mdy096
10. EURACAN. (2024). Available online at: https://euracan.eu/. (Accessed July 12, 2024).
11. Disease Multidisciplinary Team. DELIBERAZIONE N. 311 DEL 30/06/2022. OGGETTO: Adozione del Regolamento del Disease Multidisciplinary Team (DMT) (2022).
12. Walvaer, JEW, Van der Hel, OL, Van der Hoeven, JJM, VEPP, L, RHA, V, and IME, D. Factors influencing the quality and functioning of oncological multidisciplinary team meetings: results of a systematic review. BMC Health Serv Res. (2022) 22:829. doi: 10.1186/s12913-022-08112-0
13. Regolamento DMT- Istituti Fisioterapici Ospitalieri - Roma. (Delibera IFO n. 72 del s Febbraio 2016) (2016).
14. Gebbia, V, Guarini, A, Piazza, D, Bertani, A, Spada, M, Verderame, F, et al. Virtual multidisciplinary tumor boards: a narrative review focused on lung Cancer. Pulm Ther. (2021) 7:295–308. doi: 10.1007/s41030-021-00163-8
15. Kočo, J, Weekenstroo, HHA, Lambregts, DMJ, JPM, S, Prokop, M, Fütterer, JJ, et al. The effects of multidisciplinary team meetings on clinical practice for colorectal, lung, prostate and breast cancer: a systematic review. Cancers. (2021) 13:4159. doi: 10.3390/cancers13164159
16. Askelin, B, Hind, A, and Paterson, C. Exploring the impact of uro-oncology multidisciplinary team meetings on patient outcomes: a systematic review. Eur J Oncol Nurs. (2021) 54:102032. doi: 10.1016/j.ejon.2021.102032
17. Basta, YL, Baur, OL, Van Dieren, L, Klinkenbijl, JH, Fockens, P, and Tytgat, KM. Is there a benefit of multidisciplinary cancer team meetings for patients with gastrointestinal malignancies? Ann Surg Oncol. (2016) 23:2430–7. doi: 10.1245/s10434-016-5178-3
18. Prades, J, Remue, E, Van Hoof, E, and Borras, JM. Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes. Health Policy. (2015) 119:464–74. doi: 10.1016/j.healthpol.2014.09.006
19. Rossi, B, Zoccali, C, Baldi, J, Scotto di Uccio, A, Biagini, R, De Luca, A, et al. Reorganization tips from a sarcoma unit at time of the COVID-19 Pandemie in ltaly: early experience from a regional referral oncologic center. J Clin Med. (2020) 9:1868. doi: 10.3390/jcm9061868
20. Onesti, CE, Vari, S, Nardozza, F, Maggi, G, Minghelli, D, Rossi, B, et al. The impact of the COVID-19 pandemic on diagnosis and treatment of patients with soft tissue and bone sarcomas or aggressive benign musculoskeletal diseases: a single-center retrospective study (SarCorD study). Front Oncol. (2022) 12:1000056. doi: 10.3389/fonc.2022.1000056
21. Onesti, CE, Vari, S, Minghelli, D, Nardozza, F, Rossi, B, Sperati, F, et al. Quality of life and emotional distress in sarcoma patients diagnosed during COVID-19 pandemic: a supplementary analysis from the SarCorD study. Front Psychol. (2023) 14:1078992. doi: 10.3389/fpsyg.2023.1078992
22. Jazieh, AR, Akbulut, H, Curigliano, G, Rogado, A, Alsharm, AA, Razis, ED, et al. Impact of the COVID-19 pandemic on cancer care: a global collaborative study. JCO Glob Oncol. (2020) 6:1428–38. doi: 10.1200/GO.20.00351
23. Amador, M, Matias-Guiu, X, Sancho-Pardo, G, Contreras Martinez, J, de la Torre-Montero, JC, Peñuelas Saiz, A, et al. Impact of the COVID-19 pandemic on the care of cancer patients in Spain. ESMO open. (2021) 6:100157. doi: 10.1016/j.esmoop.2021.100157
24. Rebecca, E, Parkhill, A, and Schinfeld, L. What are relevant, feasible and effective approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID-19 prevention and control? Copenhagen: WHO Regional Office for Europe (2021).
25. Rete Nazionale Tumori Rari. Available online at: http://eonc.istitutotumori.mi.it/RTR/
26. Rajasekaran, RB, Whitwell, D, Cosker, TDA, Gibbons, CLMH, and Carr, A. Will virtual multidisciplinary team meetings become the norm for musculoskeletal oncology care following the COVID-19 pandemic? - experience from a tertiary sarcoma Centre. BMC Musculoskelet Disord. (2021) 22:18. doi: 10.1186/s12891-020-03925-8
27. Bonanno, N, Cioni, D, Caruso, D, Cyran, CC, Dinkel, J, Fournier, L, et al. Attitudes and perceptions of radiologists towards online (virtual) oncologic multidisciplinary team meetings during the COVID-19 pandemic-a survey of the European Society of Oncologic Imaging (ESOI). Eur Radiol. (2022) 33:1194–204. doi: 10.1007/s00330-022-09083-w
Keywords: COVID-19, sarcoma, telemedicine, disease multidisciplinary team, virtual disease multidisciplinary team
Citation: Salvatori F, Rossi B, Onesti CE, Vari S, Ceddia S, Checcucci E, Cosimati A, Riva F, Renna D, Biagini R and Ferraresi V (2025) Virtual sarcoma disease multidisciplinary team: a successful experience in the era of telemedicine and COVID-19 in Italy. Front. Public Health. 13:1636095. doi: 10.3389/fpubh.2025.1636095
Edited by:
Santosh Kumar Sharma, University of Limerick, IrelandReviewed by:
Luigi Di Biasi, University of Salerno, ItalyBenson Ncube, University of KwaZulu-Natal, South Africa
Copyright © 2025 Salvatori, Rossi, Onesti, Vari, Ceddia, Checcucci, Cosimati, Riva, Renna, Biagini and Ferraresi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Concetta Elisa Onesti, ZWxpc2Eub25lc3RpQGlmby5pdA==
 Francesca Salvatori1
Francesca Salvatori1 Concetta Elisa Onesti
Concetta Elisa Onesti Sabrina Vari
Sabrina Vari Federica Riva
Federica Riva Virginia Ferraresi
Virginia Ferraresi