- 1Department of Implementation Science, Wake Forest University School of Medicine, Winston-Salem, NC, United States
- 2Institute for Global Health and Infectious Diseases, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 3Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 4Bouvé College of Health Sciences, Institute for Health Equity and Social Justice Research, Northeastern University, Boston, MA, United States
- 5School of Public Health, Georgia State University, Atlanta, GA, United States
- 6College for Health Community and Policy, University of Texas at San Antonio, San Antonio, TX, United States
- 7Department of Medical Social Sciences, Center for Dissemination and Implementation Science, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
- 8Brown School of Social Work, Washington University in St. Louis, St. Louis, MO, United States
- 9Department of Psychological Sciences, University of Missouri, Columbia, MO, United States
- 10Division of Infectious Diseases, Washington University School of Medicine in St. Louis, St. Louis, MO, United States
- 11College for Public Health and Social Justice, Saint Louis University, St. Louis, MO, United States
- 12Clinical Sciences Department, Nigerian Institute of Medical Research, Lagos, Nigeria
- 13Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, CT, United States
Background: Expanding HIV research capacity among the global majority (individuals identifying as Black/African American, American Indian and Alaska Native, Asian, Native Hawaiian and Other Pacific Islander, Multiracial, and Hispanic/Latino) is important. However, achieving national goals to increase the pool of implementation science and HIV early-stage investigators from underrepresented backgrounds remains elusive, largely due to limited investment in training and mentoring these individuals. To address this issue, we launched the Stimulating Training and Access to HIV Research Experiences (STAR) program, a partnership led by Saint Louis University and the University of North Carolina at Chapel Hill in collaboration with Georgia State University and Texas A&M University. The STAR program aims to establish a pathway for Underrepresented minority (UREM) students to engage in HIV and implementation science research.
Methods: We launched a crowdsourcing open call from November 30, 2022, to January 22, 2023, to identify potential trainees at the four participating institutions (Prompt: “How might we promote HIV prevention among youth aged 13–24 years in your community?”). The finalists from the crowdsourcing call participated in a 2-day designathon, which included didactic introductory lectures on HIV, dissemination and implementation science. The finalists participated in a 6-week innovation bootcamp, including modules on HIV research, implementation science, research ethics, and fieldwork experience with community partners. We assessed the acceptability of the STAR program through participant self-reported surveys on their experience and evaluation of the lectures.
Findings: Twenty-four individuals applied to the STAR program by completing the crowdsourcing open call, 12 were selected for the designathon, and 10 completed the fellowship. The first cohort of STAR trainees (10 students—6 undergraduate and 4 graduate students) successfully completed the STAR innovation bootcamp. The innovation bootcamp culminated in seven proposals that the trainees implemented and evaluated over 12 months, with support from the research team, mentors, and participatory learning community. The implementation strategies proposed by the trainees include the use of peer engagement, storytelling, digital engagement tools, and artificial intelligence to promote awareness of HIV and increase the uptake of HIV testing. All the participants were satisfied with the STAR program (90% very satisfied and 10% satisfied) and indicated enthusiasm for pursuing academic and research careers in HIV and/or implementation science.
Conclusion: Building a pathway for UREM investigators is crucial to ending the HIV epidemic. The STAR program may enhance interest, build research capacity, and increase the UREM talent pool retained in this field.
Background
People of the global majority (individuals identifying as Black/African American, American Indian and Alaska Native, Asian, Native Hawaiian and Other Pacific Islander, Multiracial, and Hispanic/Latino) in the United States make up a significant proportion of newly diagnosed individuals with HIV (1, 2). The proportion of the global majority newly diagnosed with HIV is inversely correlated to the global majority workforce or researchers in the HIV field (1, 2). Racial and ethnic inequities persist along the HIV prevention and care continuum - poor indicators for HIV testing, HIV prevention, linkage to and retention in care, antiretroviral therapy (ART) uptake and adherence, and viral suppression (3). While evidence-based interventions (EBIs) and strategies exist to address these issues, the problem lies in individual, structural, and social barriers that impede their uptake and reach (4).
The field of dissemination and implementation (D&I) science can potentially reduce these translational gaps, but it requires transformative approaches that are community-engaged, equitable, and reflective of the needs of individuals most affected by the problem—i.e., people from the global majority (5). Therefore, it is especially important to have a workforce and researchers who are representative of the communities most affected by HIV. The current workforce does not mirror that. The number of investigators who identify as the global majority in biomedical research, including HIV, is suboptimal (1, 6–8). A well-trained and diverse pool of researchers represents a crucial component towards equitable implementation and addressing the persistent disparities along the HIV prevention and care continuum (7, 9).
The global majority, comprising over 30% of the US population, accounts for less than 9% of individuals in health and biomedical professions (10). Underrepresented groups are a critical resource of talent that could be nurtured to expand the HIV research workforce and elucidate cultural assets and resources for HIV prevention/care that may not be accessible to individuals outside the community (7, 11). HIV research led by investigators who are part of the affected community offers an opportunity to understand cultural and contextual factors that can enhance the utility of the research work (7). Therefore, it is important that the research space is diverse and includes individuals of various backgrounds. However, existing training programs are limited, and few academic and research institutions have innovative skills development, research experiences, and mentoring activities to support high-quality HIV training for racial and ethnic minorities (9).
To address this issue, we launched the Stimulating Training and Access to HIV Research Experiences (STAR) program, funded by the National Institute of Allergy and Infectious Diseases (NIAID). The program is a partnership led by Saint Louis University and the University of North Carolina at Chapel Hill, in collaboration with Georgia State University and Texas A&M University. The protocol manuscript is currently under journal review. The STAR program aims to establish a pathway to increase entry into and retention of trainees in HIV and D&I research, particularly those from backgrounds underrepresented in biomedical research. STAR incorporates elements of participatory action research to provide hands-on HIV research experience, skills development, and mentoring opportunities to undergraduate and graduate students. This manuscript describes the STAR program’s structure and core components, as well as its impact on trainees’ self-reported scientific proficiency and project outcomes.
Methods
The STAR program used a multi-phase approach to recruit and train scholars. This included a crowdsourcing open call, a designathon, and an innovation bootcamp.
Eligibility criteria
Students who identified as underrepresented minorities from the four participating institutions (Saint Louis University, University of North Carolina at Chapel-Hill, Georgia State University, and Texas A & M University) were eligible to participate in the STAR program. Undergraduate and graduate students were eligible to participate in the program. Participants had the option to apply as individuals or teams. The application to the STAR program included completion of a crowdsourcing open call application packet, which included a response to the crowdsourcing open call prompt, demographics information, resume/CV, and transcripts.
The crowdsourcing open call
Crowdsourcing is a process whereby a group of people attempt to solve all or part of a problem and then shares their solutions with the communities of interest (12, 13). Crowdsourcing takes a bottom-up approach for problem-solving, and has been successfully used to solicit innovative ideas in several areas, including developing strategies to promote the uptake of HIV testing (14–16), antimicrobial drug discovery (17), and STI testing (18). The STAR crowdsourcing open call aimed to identify STAR participants and provide an opportunity for them to develop HIV prevention research ideas. The crowdsourcing open call was launched on November 30th, 2022, through January 22nd, 2023. We disseminated the open call via flyers on social media, direct emails to professors in relevant programs at the participating institutions, webinar events, and announcements by campus liaisons. The campus liaisons were student representatives from participating institutions who acted as intermediaries between the program leaders and the STAR participants. They assisted with participant recruitment, coordinated program activities such as designathons and bootcamps, scheduled meetings, and supported the development and implementation of participants’ ideas. The open call entry required: (a) response to the prompt—“How might we promote HIV prevention services among youth aged 14–24 years old in your community? We are particularly interested in communities with populations who are Black, Latine, Asian, Brown, Indigenous, and/or dual- or multi-heritage, also known as the global majority (Response must not exceed 500 words)”; (b) personal statement; (c) CV or Resume; and (d) faculty letter of recommendation (at least one and at most two). Each category was scored on a scale from 0 to 5 points. The open call question was scored using the following criteria: (1) clear and concise description; (2) relevance; (3) novelty; (4) feasibility, scalability/ replicability, and sustainability; and (5) promotion of equity and fairness, with 5 being the highest possible score. The scores were also weighed, with the Open Call Response worth 50%, the Personal Statement 20%, the CV/Resume 15%, and the Letter of Recommendation 15%.
The virtual designathon
A designathon is a three-step process informed by design thinking that includes preparation with end-users and others (open call for ideas to engage end-users and other key individuals to identify ideas to prepare for collaboration), intensive collaboration (interaction between participants and mentors to foster cross-disciplinary problem-solving and refinement of team ideas), and follow-up activities for implementation and research (plans for implementation of solutions beyond designathons, mentorship for participants to support implementation, and plans for monitoring and evaluation) (19). A systematic review of designathons provides evidence for the effectiveness of this approach (20). The STAR designathon was hosted virtually from February 17 to 19, 2023. Top entries (N = 12) from the crowdsourcing open call were invited to participate in the designathon to further develop their ideas. The designathon used a workshop-style format where participants learned about design-thinking concepts, such as rapid prototyping and co-creation, to strengthen their ideas. At the end of the designathon, participants pitched their solutions to an expert panel of 5 judges. The panel of judges consisted of public health and implementation science researchers, practitioners, and representatives from community organizations. The contest question for the designathon was similar to the open call: “How might we promote HIV prevention services among youth aged 14–24 in your community?” At the end of the designathon, the participants presented three key deliverables: (1) a PLAN (People, Learning, Adapting, Nurturing) (21) on how to engage and sustain engagement with their community partners; (2) A specific aims page introducing their solution, main objective, and potential impact, and (3) a 5- min pitch, which were evaluated by the judges based on these five criteria: (a) clear and concise description; (b) relevance; (c) novelty; (d) feasibility, scalability/replicability, and sustainability; and (e) promotion of equity and fairness.
The hybrid innovation bootcamp
Following the designathon, the STAR cohort participated in a 6-week hybrid summer innovation bootcamp. An innovation boot camp is an accelerated training program designed to build capacity for implementing solutions and typically follows a designathon to provide participants with research and project strategy skills (22). The bootcamp comprised of 3-weeks synchronous and asynchronous sessions, 2 weeks of fieldwork at a collaborating community partner organization (during this phase, the scholars gained feedback on their ideas from their community partners. It was also an opportunity to understand the feasibility of implementing their proposed solutions in collaboration with the community partners), and 1 week of in-person activities.
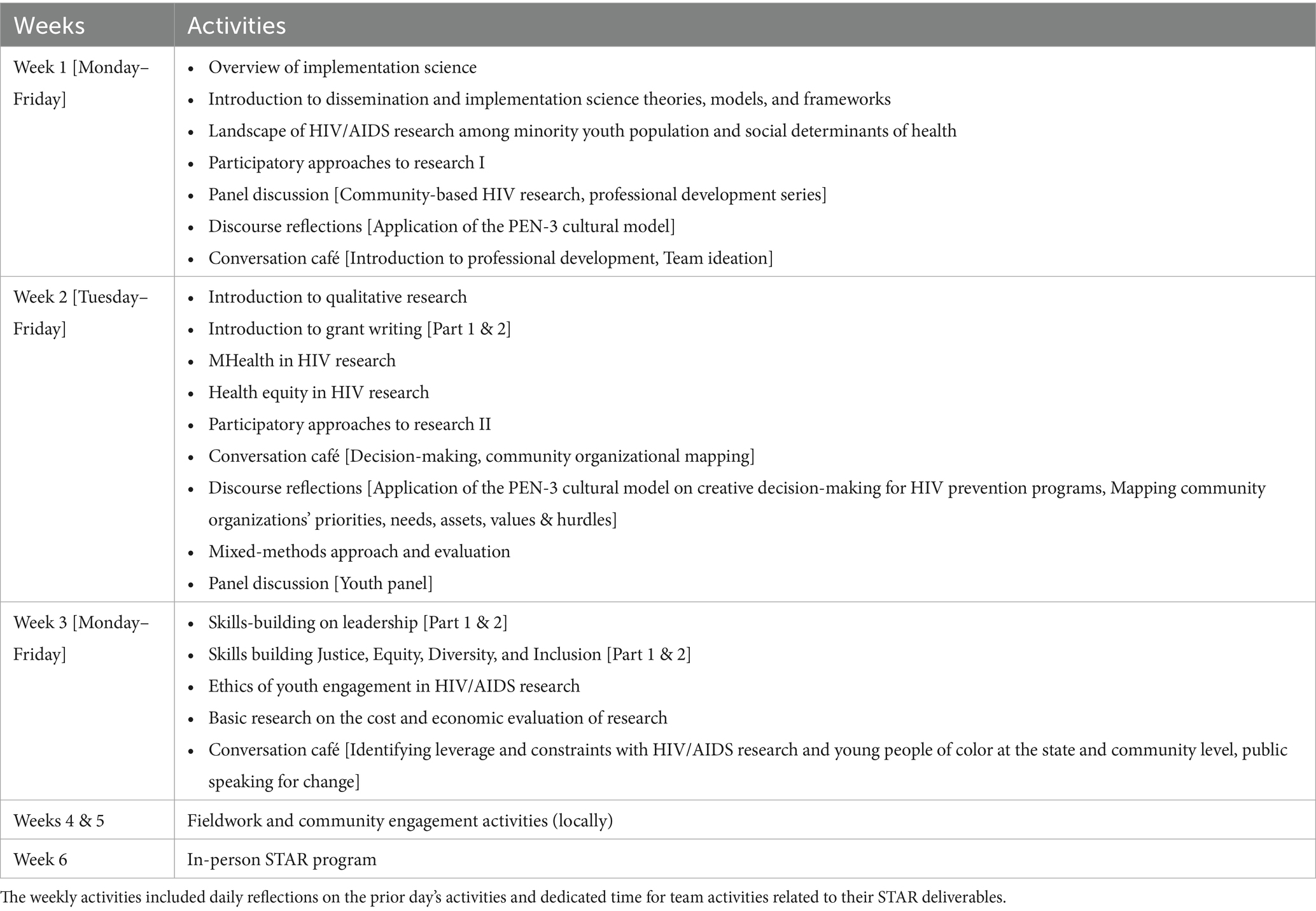
The program was framed to build general knowledge of HIV/AIDS and D&I and cross-cutting topics such as practices in grant preparation, community participatory research, JEDI (justice, equity, diversity, and inclusion), and leadership principles among the STAR fellows. A compressed curriculum for the innovation bootcamp is shown in Table 1. At the end of the innovation bootcamp, the participants presented three key deliverables: a project protocol that included a description of the solution, significance, innovation, and proposed implementation approach, a project PLAN (21) on how to engage and sustain engagement with their community partner for the proposed solution, and a 10-min pitch presentation. The bootcamp culminated with participants pitching their final ideas to a panel of six expert judges during the final week of in-person activities. The judges comprised public health and implementation science researchers, practitioners, and representatives from community organizations. The ideas were judged based on the 5 criteria that were used in the designathon phase: (a) clear and concise description; (b) relevance; (c) novelty; (d) feasibility, scalability/replicability, and sustainability; and (e) promotion of equity and fairness.
Follow-up activities
Beyond the bootcamp, the STAR scholars had access to their faculty mentors at their respective institutions and the participatory learning community. The participatory learning community was designed to be a collaborative space for STAR scholars to share progress on their pilot work, and brainstorm challenges with implementing their solutions. In addition, we held quarterly virtual meetings with the STAR scholars; this was an opportunity to share updates on the work and get feedback from their peers and program faculty. Outside the STAR-wide meetings, the campus liaisons and institution directors held periodic meetings with the scholars.
Data collection
Feedback on the STAR bootcamp was obtained through surveys designed to collect quantitative and qualitative responses before and after the innovation bootcamp related to the fellow’s overall experience. The questions were related to their experience with the program logistics, program faculty, presentations, didactic sessions, and recommendations for improvement. Closed-ended questions consisted of five-point Likert-type scales from “very dissatisfied” to “strongly satisfied.” At the beginning of the bootcamp, participants were provided with a survey to rate their knowledge of the core competencies of the program: (a) dissemination and implementation science, (b) clinical sciences, (c) leadership, and (d) Justice, Equity, Diversity, and Inclusion (JEDI), on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). The implementation science competencies were informed by the work of Padek and colleagues (23). The survey included questions related to participants’ skills and competencies in the topic areas, including definitions of key terminologies in the field, guiding theories and approaches, methods, designs, and analysis, and practice-based considerations (23). The participants completed the same questions at the end of the innovation bootcamp. Open-ended questions gathered feedback on participants’ satisfaction with the program, perceptions of its components and logistics, mentorship opportunities, networking experiences, learning outcomes, and program delivery and organization.
Analysis
Quantitative data
Demographic data collected from participants during the crowdsourcing open call, designathon, and bootcamp phases of the program, including their age, sex, race, ethnicity, level in school, and institution affiliation, were compiled and analyzed using descriptive statistics (frequencies and proportions). For Likert scale questions, the frequencies of the responses were calculated. To compare changes from the pretest to the posttest at the bootcamp, paired sample t-tests with Cohen’s d effect sizes were used. A p-value <0.05 was considered statistically significant. All analyses were performed using SPSS (version 22; IBM Corp).
Qualitative data
Data from the crowdsourcing open call and designathon
The qualitative data from the crowdsourcing open call and designathon were deidentified for analysis. A thematic analysis was conducted using open coding, which assigns themes to capture specific ideas, and axial coding, which explores linkages between concepts and categories and determines common themes (24). The thematic analysis involved two members of the team (COU and UN) initially reading through the data to familiarize themselves with the responses, after which they extracted texts to generate a codebook that identified recurring categories and themes across the data set independently. The two coders (COU and UN) then compared, discussed, and synthesized their coding process, which was merged into the final codebook. The two coders then tested the codebook against three submissions, made revisions, and resolved discrepancies before moving to the stage of complete coding. All submissions were then characterized using the codebook, and overarching categories were closely examined to identify analytic themes. Qualitative Survey data: Due to the exploratory nature of the open-ended questions included in the survey, we analyzed the text responses using an inductive thematic approach (25, 26). One member of the team (COU) collated the responses to the open-ended questions for data cleaning and quality checks. Following this, two members of the research team (UN and COU) independently read the texts to become familiar with the data before developing codes. Then the open-ended questions were manually coded independently by two members of the team (UN and COU) to determine emerging themes. The two reviewers compared their themes for consistency, and differences were resolved by consensus. The findings are organized based on emerging themes and corresponding quotations from written open-ended responses.
Ethics
This study was determined to be non-human subjects research by the Saint Louis University Review Board.
Results
Crowdsourcing open-call
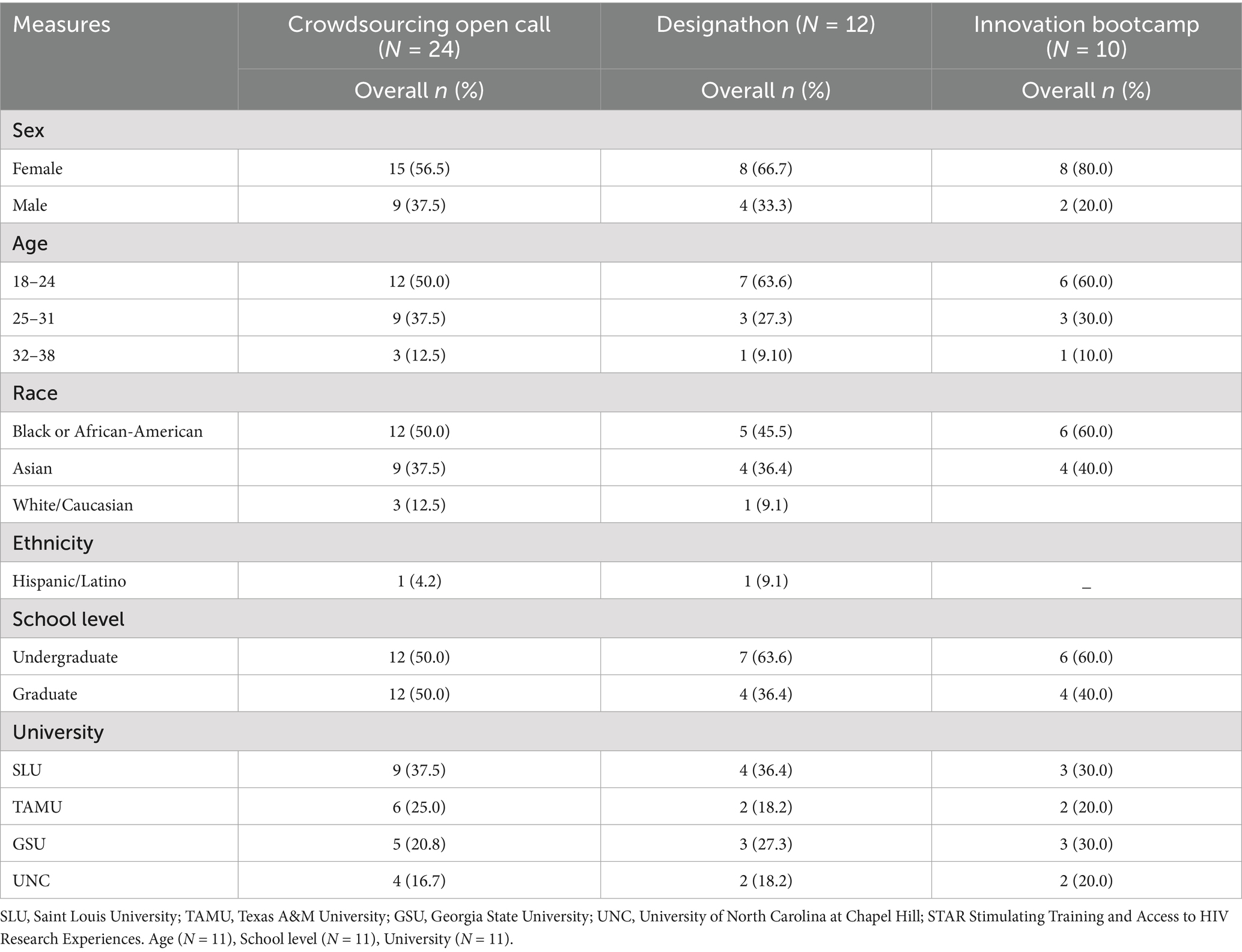
We received 24 fully completed submissions (SLU = 9; TAMU = 6; GSU = 5; and UNC = 4). The majority of the entries were from individuals who identified as women (56.5%) and Black or African-American (50.0%). The mean age of applicants was 24.5 years. Table 2 provides the demographics of eligible submissions to the crowdsourcing open call and details of who progressed on to the designathon and bootcamp phases.
In addition to providing strategies for promoting HIV prevention services among youth in their communities, 54% (n = 13) of the entries outlined barriers to HIV prevention. The key barriers to the uptake of HIV preventive services include (a) Limited access to comprehensive HIV education and materials, (b) Stigma and misconceptions that prevent open conversations about HIV or accessing necessary preventive services, (c) Structural barriers such as poverty, discrimination, and violence that may impede access to healthcare services, (d) Political determinants that influence the availability of sexual and reproductive knowledge and services, and (e) Limited youth-friendly strategies. Conventional methods of programming and promotion of HIV knowledge and information may not be engaging and appealing to youth. See Appendix 1 for barriers to the uptake of HIV prevention services emerging from the crowdsourcing open call.
Themes from the crowdsourcing open call entry on strategies to promote HIV prevention services among youth aged 14–24 years old in the respondents’ communities included: (a) Use of storytelling to make the information relatable to youth, (b) Use of social media and digital technologies for campaigns and dissemination of accurate and reliable HIV information, (c) Use of competitions and incentive-driven programs, (d) Youth engagement in program delivery-engaging youth as peer navigators, champions, or implementors of HIV prevention programs for youth, and (e) Partnering with existing organizations that serve youth, such as youth community-based organizations, student clubs, and after-school programs to deliver HIV prevention programs for youth. See Appendix 2 for the emerging themes on strategies to promote HIV prevention among youth aged 14–24 years from the crowdsourcing open call.
Designathon
We selected 12 participants from the open call to move on to the designathon. After 2 days of strengthening their solutions and a pitch presentation to the judging panel, all participants were selected to join the STAR innovation boot camp (see Table 2).
Themes from the solutions on strategies to promote HIV prevention services among youth aged 14–24 years in their respondents’ communities included: (a) promoting awareness and education on HIV prevention through youth engagement. This included utilizing sex-positive approaches, utilizing art to foster engagement and appeal among youth, and using interactive and informational videos for education. (b) Partnership with youth-serving organizations and youth in implementing HIV services. This included collaborations with schools, after-school programs, and community-based organizations to deliver HIV programs. In addition, utilizing peer-to-peer delivery of HIV services or for health promotion, (c) building trust among youth and addressing stigma. This included fostering conversations in safe spaces and (d) using social media and digital technology. This included leveraging social media and digital technologies such as websites and software applications to deliver HIV prevention information and for demand creation. Additional information about the solutions at the designathon is provided in Appendix 3. The teams from the designathon were then invited to join the innovation bootcamp to build on their implementation pilot solutions.
STAR innovation bootcamp
Ten out of the twelve participants from the designathon participated in the STAR bootcamp as STAR scholars (Table 2 provides demographics). The other two participants from the designathon could not proceed to the bootcamp due to scheduling conflicts. Most of the STAR first cohort were undergraduate students (60%).
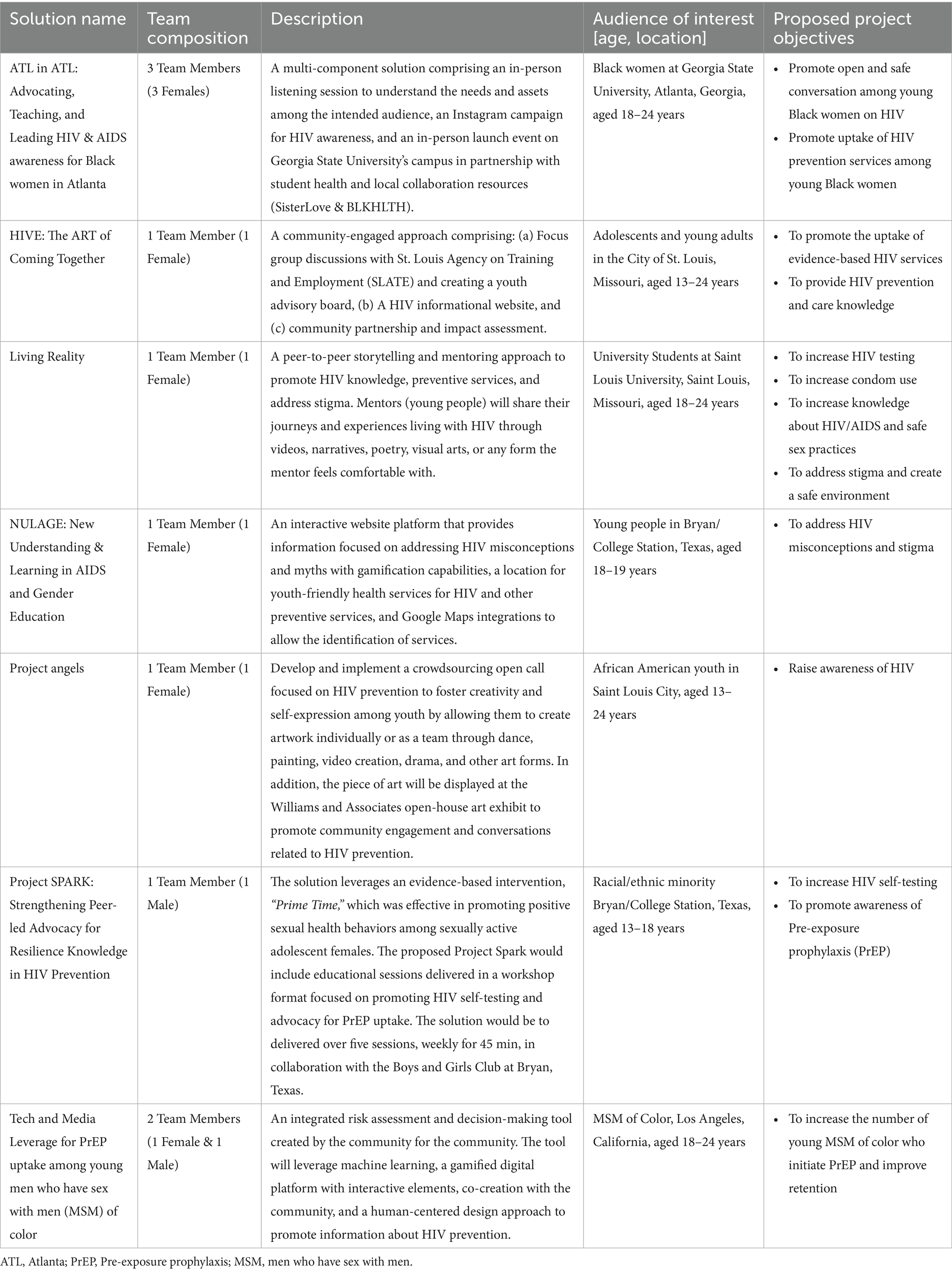
Emerging pilot projects
The STAR bootcamp culminated in seven proposals led by the STAR scholars, with support from the research team, mentors, and participatory learning community engagements. The various teams proposed diverse strategies to promote HIV prevention and awareness and address stigma among youth and minoritized populations. Most of the solutions involved some community-engagement components through activities such as listening sessions with a community interested in learning about their needs, resources, and assets; peer engagement through youth advisory boards; crowdsourcing open calls to generate innovative and creative solutions from young people for HIV prevention; art exhibits; and storytelling. In addition, technology-driven solutions were also suggested, including leveraging machine learning for risk assessment and tailoring of health information, using social media campaigns, gamified platforms for HIV education, and an interactive website for the geolocation of youth-friendly services for HIV. Overall, the solutions focused on some HIV prevention objectives, including reducing HIV stigma, promoting HIV knowledge, or the uptake of preventive services such as HIV testing and PrEP. The proposed solutions by the STAR scholars are provided in Table 3. Judges scores of the teams’ solutions are provided in Appendix 4.
STAR bootcamp evaluation
Quantitative evaluation
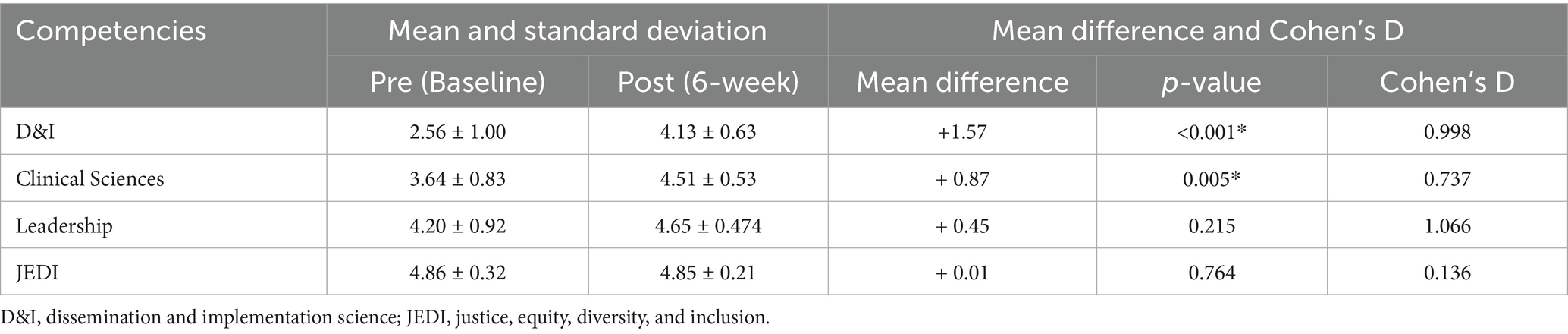
A pre-post assessment of the core competencies of the STAR program showed an overall improvement in the four areas: (a) dissemination and implementation science (D &I), (b) clinical sciences, (c) leadership, and (d) JEDI. However, only the increase in D&I and clinical sciences knowledge was statistically significant. The difference in D & I knowledge at baseline and the completion of the boot camp had a large effect size (Cohen’s d = 0.99). The difference in Clinical sciences knowledge at baseline and the completion of the boot camp had a moderate effect size (Cohen’s d = 0.74). Table 4 provides a summary of this assessment.
In general, 90% of the participants were “very satisfied” with the STAR program, and 10% were “satisfied.” Further, 90% of the participants indicated they would recommend the STAR program to their peers. Regarding the mentorship experience, most of the STAR scholars found the support from their peers helpful (80%), and 90% indicated that the feedback from their faculty on their ideas and the final project was helpful, respectively. Additional reports are provided in Appendix 5.
Qualitative evaluation
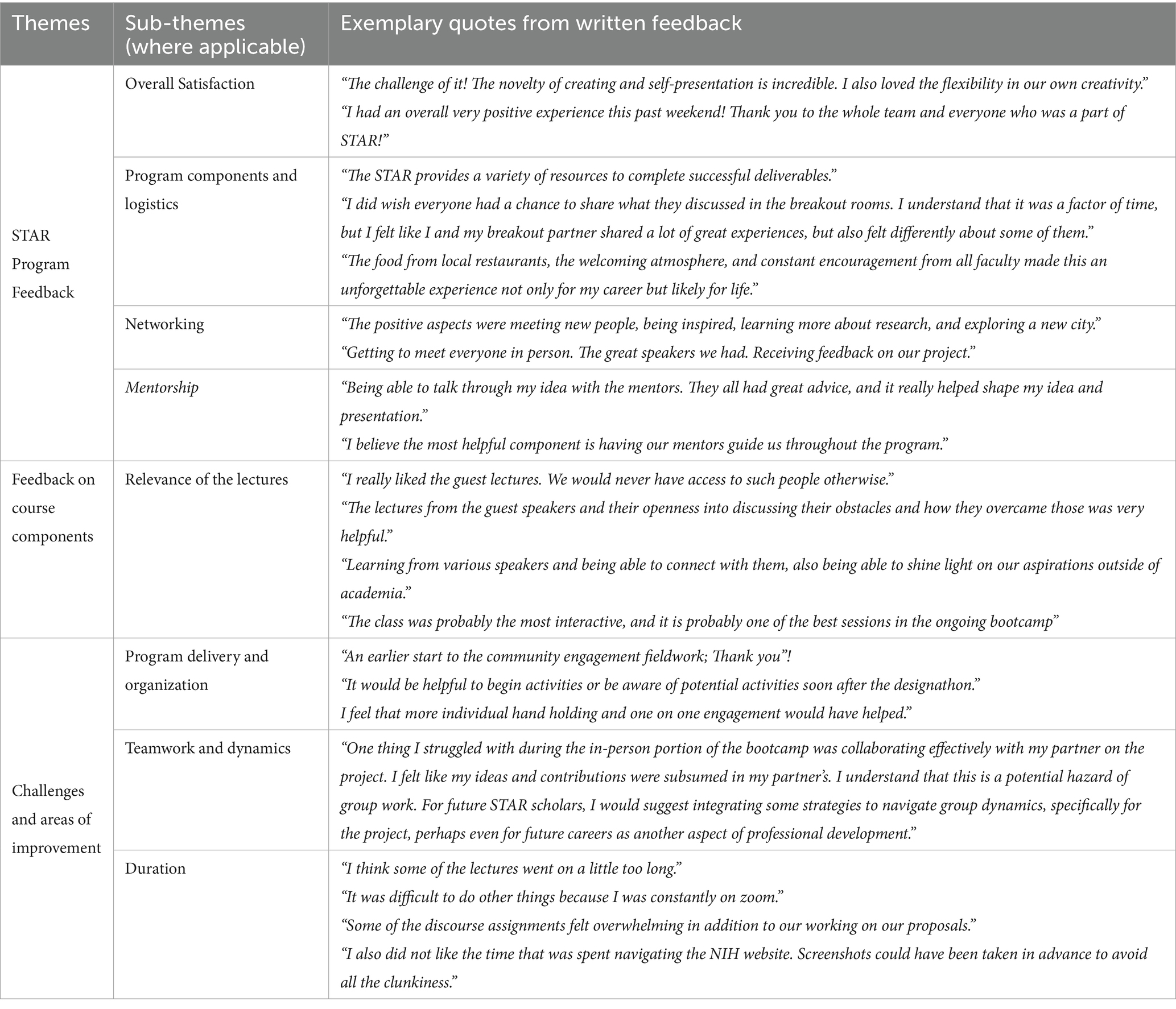
A qualitative evaluation of the innovation bootcamp among the STAR scholars shows an overall positive experience with the STAR program and its contents. In addition, the scholars highlighted some areas for improvement in the boot camp experience. Three main qualitative themes emerged from our analysis of the scholars’ responses to open-ended questions on pre- and post-program evaluation surveys: (a) STAR boot camp feedback. This included feedback on overall satisfaction with the program, program components and logistics, networking, and mentoring components, (b) feedback on course components, and (c) some challenges experienced and areas of improvement. This included some challenges experienced in program delivery and organization, teamwork, dynamics, and course durations. The emerging themes and corresponding sub-themes, where applicable, and quotes from the written feedback on the survey are provided in Table 5.
Discussion
We report on the first year of the implementation of the STAR program. The program seeks to support the development of HIV and D&I research skills among students to increase the pipeline of underrepresented researchers focused on HIV and D&I research. The STAR program utilized an innovative multi-phase, participatory approach to recruiting and training scholars to develop solutions for promoting HIV prevention services among youth aged 14–24 years old. The success of the STAR program was evident from feedback from the STARs. The program evaluation suggests overall satisfaction and acceptability among the STAR scholars. The participants valued peer interactions and the support from the STAR faculty and mentors. The use of participatory approaches, such as crowdsourcing and designathons, also expands the literature by providing innovative strategies for recruiting and engaging individuals in training.
The evaluation of the core competencies of the STAR program indicated gains by the end of the bootcamp. However, only the gains in D&I (e.g., lectures on D&I theories, methods, and frameworks) and clinical sciences (e.g., lectures on research study design and methodologies, identifying and measuring clinically relevant outcomes, and community engagement in research) components were statistically significant. These findings are congruent with other training programs for students who reported gains in research skills and academic knowledge (27). This highlights the value of the STAR program in enriching student content knowledge and research skills. Notably, leadership and JEDI areas were the highest rated at pretest; it is possible that a ceiling effect impacted the lack of change in those areas. Future iterations of STAR may want to improve the pretest measure or deepen skills in these areas since participants joined with such high knowledge at the outset.
Beyond the research and course materials, the program provided scholars with experiential research opportunities with the community partners they intended to work with. The scholars received robust research experience in idea/solution conceptualization and community engagement through implementation. The scholars learned the importance of community engagement and a strength-based approach to intervention, development, and implementation through this process. By centering community engagement and strength-based inquiry through the lecture format and the assignments, the STAR program cultivated and reinforced the capabilities and strengths of young people and communities toward leading an HIV-free generation (28). This builds on the consideration for inclusive co-creation of knowledge and strategies in D &I to improve health and create transformational change in systems that influence health (29).
At the end of the bootcamp, the scholars developed seven proposals to be implemented within their respective communities. The solutions generated by the scholars included community-engagement components to create demand for and promote the uptake of HIV prevention services among young people. Engaging communities to support HIV prevention research has been highlighted as critical to developing robust and locally relevant strategies (30). The strategies developed by the participants may have significant implications for designing HIV prevention interventions focused on elevating youth assets, leveraging digital technologies, building trust, and collaborating with existing organizations to optimize the delivery of youth-centered interventions.
Findings suggest that students and trainees can be involved in the co-production of knowledge and activities for HIV prevention in the early stage of their training. This can inform future training programs, fostering participatory strategies for engaging trainees and steering trainees towards developing competencies on centering people and communities in their research and projects.
Notably, mentorship was highlighted as an important aspect of the STAR program. This aligns with the WHO HEalth Research MEntorship in Low and Middle-Income CountrieS (HERMES) guide on institutionalizing research mentorship (31). The guide highlights the importance of supportive mentoring practices that elevate the strengths and capabilities of mentees. In addition, the high satisfaction with the multi-mentorship opportunity through peers and faculty members has been reported as an important attribute of training programs to enhance diversity and inclusion in research (32). Mentorship has been shown to be a very influential component of successful training experiences, career pathway development, and workforce development for trainees (32, 33).
Constructive feedback from the scholars revealed concerns about the lengthy nature of the online engagement component of the training during the 3 weeks of online lectures. While the online modality for lecture delivery was effective in engaging students in different locations simultaneously, there were some challenges with continually engaging the trainees for an extended period. This challenge is similar to other training programs that have utilized virtual platforms to deliver the training, which have shared concerns with continued engagement and retaining participants’ attention over an extended period of time (34). Future STAR trainings could reduce online time and increase active engagement with trainees through interactive activities. In addition, some of the participants indicated the need for an earlier engagement with their community partners to plan and implement their ideas. Looking forward to maximizing the impact of the STAR program, we will partner with community organizations from the onset to co-develop the open call prompt. This would ensure that solutions generated through the open call would be responsive to the immediate needs of community partners.
Limitations
There are some limitations worth noting. One notable limitation is that there is a potential for selection bias. The participants were likely individuals already exposed to or interested in HIV or implementation science research. To minimize selection bias, we utilized several promotion strategies to enhance a wider reach, such as social media promotion, classroom announcements, and webinars. Nonetheless, involvement in training requires a level of interest in expanding their knowledge in the proposed area. This evaluation is based on an immediate assessment of the program. This is critical information to assess the program’s success in meeting the short-term goals. Future studies should follow students over time to assess the impact of the STAR program on their career and research trajectories. Lastly, reliance on self-reported measures may have introduced social desirability bias. Despite these limitations, the evaluation of the STAR program is highly acceptable among STAR scholars. The format of the STAR program can be replicated to improve core competencies on HIV and implementation science among undergraduate and graduate students, and develop a pathway for diverse researchers and professionals in the field.
Future directions for the STAR program include building community engagement and expanding the curriculum. Potential future curriculum topics include how to develop and implement demonstration projects within community organizations. We would incorporate novel strategies to keep participants engaged during the 3 weeks of lectures and participatory learning communities, such as including book clubs and journal clubs to introduce scholars to emerging research and topics in the field. In addition, given the challenges some participants faced with teamwork, the STAR curriculum and activities would include strategies to foster team cohesion and collaboration.
Conclusion
In summary, findings from this work highlight the success of the STAR program in recruiting and training students in HIV and D&I research while centering the roles of community engagement, diversity, equity, and inclusion. This first iteration of the STAR program holds promise in fostering HIV research with an equity and implementation science lens among global majority scholars, which could help narrow gaps in health disparities in their respective communities. By training scholars who are underrepresented in the HIV field, we are nurturing the next generation of researchers and professionals who will contribute to innovation and excellence in HIV and D&I research. Partnering with community-based organizations and including fieldwork experiences elevated scholars’ experiences by allowing them to experience the real-world implementation of their solutions. The STAR participatory recruitment and training process could serve as an innovative model to foster interest and build research capacity, educational training, and mentorship for the next generation of HIV and D&I scientists.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
UN: Formal analysis, Writing – original draft, Project administration, Writing – review & editing. JDT: Formal analysis, Writing – review & editing, Funding acquisition, Resources, Conceptualization, Supervision. IBT: Supervision, Writing – review & editing, Funding acquisition, Resources, Conceptualization. COA: Supervision, Writing – review & editing, Conceptualization, Funding acquisition, Resources. RB: Formal analysis, Methodology, Writing – review & editing. WT: Writing – review & editing, Methodology, Supervision, Resources. CO-U: Project administration, Supervision, Writing – review & editing, Formal analysis, Methodology. OA: Project administration, Writing – review & editing. KA: Writing – review & editing, Supervision, Project administration. CH: Supervision, Writing – review & editing, Project administration. AE: Writing – review & editing. TP: Writing – review & editing. UO: Writing – review & editing. DO: Writing – review & editing. BPT: Writing – review & editing, Project administration. OO: Writing – review & editing. TO: Writing – review & editing. JI: Methodology, Resources, Investigation, Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Institute of Allergy and Infectious Diseases (NIAID) R25 AI170379-01.
Acknowledgments
The authors would like to thank all the STAR staff, scholars, liaisons, mentors, faculty members, and advisory committee who assisted with the program. We want to thank and acknowledge all the STAR scholars, open-call participants, judges, mentors, community partners, and the STAR team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author (UN) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The reviewer DH declared a shared affiliation with the author BT to the handling editor at the time of review.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1637752/full#supplementary-material
References
1. Stoff, DM, Bowleg, L, del Río-González, AM, Rodriguez-Diaz, CE, and Zea, MC. Critical perspectives on expanding racial/ethnic diversity in the HIV research workforce: comorbidities and mentoring. Health Educ Behav. (2023) 50:10901981231157795. doi: 10.1177/10901981231157795
2. Crepaz, N, Dong, X, Hess, KL, and Bosh, K. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons aged 13–29 years living with diagnosed HIV infection, United States, 2016. J Acquir Immune Defic Syndr. (2020) 83:334–9. doi: 10.1097/QAI.0000000000002277
3. Crepaz, N, Dong, X, Wang, X, Hernandez, AL, and Hall, HI. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care—United States, 2014. MMWR Morb Mortal Wkly Rep. (2018) 67:113–8. doi: 10.15585/mmwr.mm6704a2
4. Brownson, RC, Kumanyika, SK, Kreuter, MW, and Haire-Joshu, D. Implementation science should give higher priority to health equity. Implement Sci. (2021) 16:1–16. doi: 10.1186/s13012-021-01097-0
5. Gustafson, P, Abdul Aziz, Y, Lambert, M, Bartholomew, K, Rankin, N, Fusheini, A, et al. A scoping review of equity-focused implementation theories, models and frameworks in healthcare and their application in addressing ethnicity-related health inequities. Implement Sci. (2023) 18:51. doi: 10.1186/s13012-023-01304-0
6. Oh, SS, Galanter, J, Thakur, N, Pino-Yanes, M, Barcelo, NE, White, MJ, et al. Diversity in clinical and biomedical research: a promise yet to be fulfilled. PLoS Med. (2015) 12:e1001918. doi: 10.1371/journal.pmed.1001918
7. Stoff, DM, and Cargill, VA. Building a more diverse workforce in HIV/AIDS research: the time has come. AIDS Behav. (2016) 20:222–30. doi: 10.1007/s10461-016-1501-z
8. Nguyen, M, Chaudhry, SI, Desai, MM, Dzirasa, K, Cavazos, JE, and Boatright, D. Gender, racial, and ethnic inequities in receipt of multiple National Institutes of Health research project grants. JAMA Netw Open. (2023) 6:e230855–5. doi: 10.1001/jamanetworkopen.2023.0855
9. Vermund, SH, Hamilton, EL, Griffith, SB, Jennings, L, Dyer, TV, Mayer, K, et al. Recruitment of underrepresented minority researchers into HIV prevention research: the HIV prevention trials network scholars program. AIDS Res Hum Retrovir. (2018) 34:171–7. doi: 10.1089/aid.2017.0093
10. Wiley, K, Dixon, BE, Grannis, SJ, and Menachemi, N. Underrepresented racial minorities in biomedical informatics doctoral programs: graduation trends and academic placement (2002–2017). J Am Med Inform Assoc. (2020) 27:1641–7. doi: 10.1093/jamia/ocaa206
11. Stoff, DM, Zea, MC, and Rodriguez-Diaz, CE. Mentoring programs by and for a new generation of Latino investigators in behavioral-social science HIV research. Ethn Dis. (2020) 30:305–12. doi: 10.18865/ed.30.2.305
12. World Health Organization and UNICEF. Crowdsourcing in health and health research: a practical guide. Switzerland: Social Innovation in Health Initiative (2018).
13. Tucker, JD, Day, S, Tang, W, and Bayus, B. Crowdsourcing in medical research: concepts and applications. PeerJ. (2019) 7:e6762. doi: 10.7717/peerj.6762
14. Tang, W, Ritchwood, TD, Wu, D, Ong, JJ, Wei, C, Iwelunmor, J, et al. Crowdsourcing to improve HIV and sexual health outcomes: a scoping review. Curr HIV/AIDS Rep. (2019) 16:270–8. doi: 10.1007/s11904-019-00448-3
15. Iwelunmor, J, Ezechi, O, Obiezu-Umeh, C, Gbaja-Biamila, T, Nwaozuru, U, Oladele, D, et al. The 4 youth by youth HIV self-testing crowdsourcing contest: a qualitative evaluation. PLoS One. (2020) 15:e0233698. doi: 10.1371/journal.pone.0233698
16. Mathews, A, Conserve, D, Mason, H, Alston, LM, Rennie, S, and Tucker, J. ‘Informed and empowered’: a mixed-methods study of crowdsourcing contests to promote uptake of HIV self-testing kits among African Americans. J Virus Erad. (2020) 6:74–80. doi: 10.1016/S2055-6640(20)30020-0
17. Desselle, MR, Neale, R, Hansford, KA, Zuegg, J, Elliott, AG, Cooper, MA, et al. Institutional profile: community for open antimicrobial drug discovery–crowdsourcing new antibiotics and antifungals. Future Science OA. (2017) 3:FSO171. doi: 10.4155/fsoa-2016-0093
18. Davis, A, Kpokiri, E, Li, C, Day, S, Yan, X, Marley, G, et al. Using crowdsourcing at an academic conference to develop STI testing messaging for public dissemination. Sex Transm Infect. (2024) 100:110–2. doi: 10.1136/sextrans-2023-056002
19. World Health Organization (2024) Participatory health research and action: a practical guide on designathons. Available online at: https://socialinnovationinhealth.org/health-designathon-guide/ (Accessed October 3, 2025).
20. Tieosapjaroen, W, Chen, E, Ritchwood, T, Li, C, Conklin, JL, Babatunde, AO, et al. Designathons in health research: a global systematic review. BMJ Glob Health. (2024) 9, 1–10. doi: 10.1136/bmjgh-2023-013961
21. Iwelunmor, J, Tucker, JD, Ezechi, O, Nwaozuru, U, Obiezu-Umeh, C, Gbaja-Biamila, T, et al. Sustaining HIV research in resource-limited settings using PLAN (people, learning, adapting, nurturing): evidence from the 4 youth by youth project in Nigeria. Curr HIV/AIDS Rep. (2023) 20:111–20. doi: 10.1007/s11904-023-00652-2
22. Nwaozuru, U, Obiezu-Umeh, C, Tahlil, KM, Gbaja-Biamila, T, BeLue, R, Idigbe, I, et al. An innovation bootcamp model for developing youth-led HIV self-testing delivery strategies in Nigeria: post-designathon capacity building. Front Public Health. (2024) 12:1454304. doi: 10.3389/fpubh.2024.1454304
23. Padek, M, Colditz, G, Dobbins, M, Koscielniak, N, Proctor, EK, Sales, AE, et al. Developing educational competencies for dissemination and implementation research training programs: an exploratory analysis using card sorts. Implement Sci. (2015) 10:1–9. doi: 10.1186/s13012-015-0304-3
24. Braun, V, Clarke, V, Hayfield, N, and Terry, G. Thematic analysis In: P. Liamputtong (ed.). Handbook of research methods in health social sciences. Singapore: Springer (2019). 843–60.
25. Gibbs, GR. Thematic coding and categorizing In: Analyzing qualitative data, Thousand Oaks, California: SAGE Publications. vol. 703 (2007). 38–56.
26. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
27. Salto, LM, Riggs, ML, Delgado De Leon, D, Casiano, CA, and De Leon, M. Underrepresented minority high school and college students report STEM-pipeline sustaining gains after participating in the Loma Linda University summer health disparities research program. PLoS One. (2014) 9:e108497. doi: 10.1371/journal.pone.0108497
28. Knibbs, K, Underwood, J, MacDonald, M, Schoenfeld, B, Lavoie-Tremblay, M, Crea-Arsenio, M, et al. Appreciative inquiry: a strength-based research approach to building Canadian public health nursing capacity. J Res Nurs. (2012) 17:484–94. doi: 10.1177/1744987110387472
29. Ramanadhan, S, Donaldson, ST, Siqueira, CE, Rackard-James, C, Miller, E, Tappin, J, et al. Connecting implementation science, community-engaged research, and health promotion to address cancer inequities in Massachusetts: the UMB/DF-HCC U54 outreach Core. Am J Health Promot. (2022) 36:597–601. doi: 10.1177/08901171211062800
30. Sahay, S, and Mehendale, S. Engaging community to support HIV prevention research. East J Med. (2011) 16:168.
31. Social and Economic Situation of Health in Ethiopia and World Health Organization. Health research mentorship in low-and middle-income countries (HERMES): a TDR global practical guide to spur mentorship institutionalization. Geneva: World Health Organization (2022).
32. Howell, LP, Wahl, S, Ryan, J, Gandour-Edwards, R, and Green, R. Educational and career development outcomes among undergraduate summer research interns: a pipeline for pathology, laboratory medicine, and biomedical science. Acad Pathol. (2019) 6:2374289519893105. doi: 10.1177/2374289519893105
33. McSweeney, JC, Hudson, TJ, Prince, L, Beneš, H, Tackett, AJ, Miller Robinson, C, et al. Impact of the INBRE summer student mentored research program on undergraduate students in Arkansas. Adv Physiol Educ. (2018) 42:123–9. doi: 10.1152/advan.00127.2017
34. Kumar, ABV, McGinnis, GG, Jones, L, Hager, ER, Wright, SL, Felter, C, et al. A feasibility study describing the successes and challenges of implementing a virtual community health worker training among high school students participating in a summer STEM enrichment program. J STEM Outreach. (2024) 7, 1–18. doi: 10.15695/jstem/v7i1.01
Keywords: capacity-building, implementation science, HIV, participatory approaches, mentorship
Citation: Nwaozuru U, Tucker JD, Thurston IB, Airhihenbuwa CO, BeLue R, Tang W, Obiezu-Umeh C, Anikamadu O, Ameen K, Herrara C, Engelhart A, Patrick T, Onyeama U, Oladele D, Takenaka BP, Olusanya OA, Ojo T and Iwelunmor J (2025) Building capacity for HIV and implementation science among students in the United States: the stimulating training and access to HIV research experiences (STAR) program. Front. Public Health. 13:1637752. doi: 10.3389/fpubh.2025.1637752
Edited by:
Jeremiah Brown, Dartmouth College, United StatesReviewed by:
Debbie L. Humphries, Yale University, United StatesKimberly Evans, Centers for Disease Control and Prevention (CDC), United States
Copyright © 2025 Nwaozuru, Tucker, Thurston, Airhihenbuwa, BeLue, Tang, Obiezu-Umeh, Anikamadu, Ameen, Herrara, Engelhart, Patrick, Onyeama, Oladele, Takenaka, Olusanya, Ojo and Iwelunmor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ucheoma Nwaozuru, dW53YW96dXJAd2FrZWhlYWx0aC5lZHU=; Juliet Iwelunmor, aWp1bGlldEB3dXN0bC5lZHU=
 Ucheoma Nwaozuru
Ucheoma Nwaozuru Joseph D. Tucker
Joseph D. Tucker Idia B. Thurston
Idia B. Thurston Collins O. Airhihenbuwa5
Collins O. Airhihenbuwa5 Rhonda BeLue
Rhonda BeLue Weiming Tang
Weiming Tang Chisom Obiezu-Umeh
Chisom Obiezu-Umeh Onyekachukwu Anikamadu
Onyekachukwu Anikamadu Bryce Puesta Takenaka
Bryce Puesta Takenaka