- 1Department of Geriatrics, The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, China
- 2Department of Emergency, The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, China
Background: Malnutrition is a prevalent but underrecognized health issue among older adults in China. Inadequate awareness may delay detection and intervention, especially in cognitively vulnerable populations. To assess the level of malnutrition awareness and its association with sociodemographic, cognitive, and nutritional factors in a representative sample of older Chinese adults.
Methods: We conducted a cross-sectional survey among 1,227 individuals aged ≥60 years in Zhejiang Province. Malnutrition awareness was measured using a validated 7-item questionnaire. Cognitive status, nutritional risk, frailty, sarcopenia risk, and fall risk were assessed using standard tools. Multivariate logistic regression was used to identify independent predictors of awareness.
Results: Overall, 49.1% of participants demonstrated adequate malnutrition awareness. While most recognized general nutrition concepts (93.5%) and protein supplementation (92.7%), awareness of psychosocial risk factors (e.g., depression) was limited (41.7%). Higher awareness was significantly associated with higher education (OR = 1.38, 95% CI: 1.23–1.55), cohabitation (OR = 1.33, 95% CI: 1.13–1.56), and better cognitive function (p < 0.0001). Age, BMI, and frailty were not independent predictors.
Conclusion: Malnutrition awareness among older Chinese adults remains suboptimal, particularly regarding psychological contributors. Targeted education strategies should be stratified by cognitive ability and living context to bridge awareness gaps and support national healthy aging initiatives.
1 Introduction
China has entered a stage of deep population aging, with adults aged 65 years and older comprising 15.4% of the total population by the end of 2023 (1). In response, national health policies have increasingly emphasized the development of age-friendly health service systems and support structures (2, 3). Recent government initiatives have launched comprehensive campaigns to promote older adults health, prioritizing domains such as cognitive function, malnutrition, and oral health, which are now recognized as key determinants of functional decline in later life (4–6).
Malnutrition is a common but frequently overlooked condition in the older population, associated with higher risks of frailty, sarcopenia, infection, disability, and mortality (7, 8). In China, the prevalence of malnutrition or nutritional risk ranges from 10% to over 40%, depending on care setting and assessment tool (9, 10). Despite its clinical consequences, public awareness of malnutrition remains underexplored—especially among older adults who are also facing cognitive and sensory decline. Moreover, recent evidence shows that psychosocial factors such as depression, social isolation, and loss of autonomy are often overlooked as contributors to malnutrition, even though they play a central role in geriatric nutrition deterioration (11, 12). For example, the European MAnu study demonstrated that undernutrition in older adults is closely linked with mental health deterioration, yet only a minority of individuals could identify psychological distress as a risk factor (13). In China, while awareness of conditions such as hypertension or diabetes is relatively high among the older adults, awareness of malnutrition remains poorly characterized (14, 15).
Against this backdrop, understanding how older adults perceive the symptoms, causes, and consequences of malnutrition is critical. While most existing research focuses on nutritional screening or intervention outcomes, there is a lack of data on the awareness of malnutrition itself, particularly in relation to cognitive ability, education level, and living situation (16–18). These factors directly affect how older adults access, process, and act on nutrition-related information.
In 2025, China launched the “Weight Management Year” national initiative, reflecting a growing national commitment to promoting healthy aging. This initiative aims to improve population-wide nutritional education, encourage healthy body composition, and prevent chronic diseases, with older adults identified as a priority group. Crucially, the prevention, early recognition, and management of malnutrition among older adults constitute a key element of this broader agenda. However, the effectiveness of such top-down public health strategies depends on a clear understanding of the current level of public awareness regarding malnutrition and its limitations—particularly in vulnerable subgroups (19). Raising awareness about malnutrition—its symptoms, risk factors, and preventive measures—is foundational for the success of national campaigns like “Weight Management Year.” Our study directly supports this national initiative by systematically assessing malnutrition awareness and its associated sociodemographic and health-related determinants in a representative sample of older adults in Zhejiang Province, China. Specifically, we explore how awareness varies according to cognitive function, educational background, living situation, and chronic disease burden. The findings provide actionable evidence to inform targeted, cognition-adapted, and community-based nutrition education strategies, thereby helping to realize the goals of the “Weight Management Year” and China’s broader healthy aging policies.
2 Materials and methods
2.1 Study design and setting
This was a cross-sectional, questionnaire-based study conducted from communities in Zhejiang, China, who completed questionnaires and somatic function assessments between February 2024 and February 2025. The study aimed to evaluate the awareness of malnutrition and its association with nutritional and health-related parameters among older adults. The Ethics Committee of Zhejiang Provincial Hospital of Chinese Medicine approved this study (Approval No. 2023-KLS-398-02). The clinical trial number is not applicable. Participants who took part in screening for geriatric syndrome were given written informed consent before participating in the study.
2.2 Participants
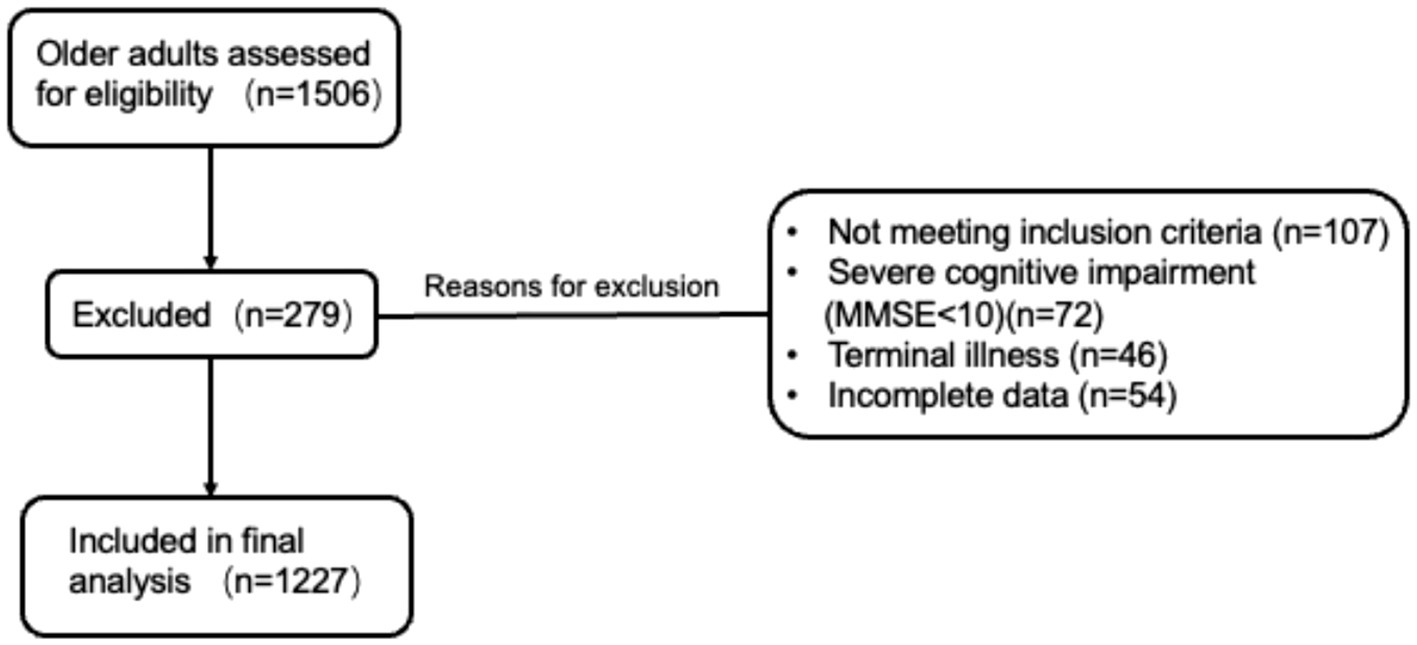
Participants were consecutively enrolled from both inpatient and outpatient settings of the Department of Geriatrics, Zhejiang Provincial Hospital of Chinese Medicine. The study population thus comprised a mix of older adults with and without chronic diseases, including those attending for routine health screening and comprehensive geriatric assessment. Inclusion criteria were: (1) age 60 or older; (2) ability to provide informed consent and complete the survey independently or with assistance. Exclusion criteria included severe cognitive impairment (MMSE <10), terminal illness (defined as a medical condition with an estimated life expectancy of less than 3 months, including advanced cancer, end-stage organ failure (heart, lung, and kidney), or other severe conditions deemed by clinicians to be beyond active treatment), or incomplete data for key variables. A total of 1,506 older adults were assessed for eligibility. Of these, 279 were excluded for the following reasons: not meeting inclusion criteria (n = 107), severe cognitive impairment (MMSE <10; n = 72), terminal illness (n = 46), or incomplete data (n = 54). Finally, 1,227 participants were included in the analysis. The detailed screening and inclusion process is illustrated in Figure 1.
2.3 Measurements
Sociodemographic information collected included age, gender, marital status, living arrangement, educational attainment, and employment status. Malnutrition knowledge was assessed using a 7-item questionnaire developed based on our previous work (20), encompassing general nutritional concepts, clinical symptoms, risk factors, and intervention strategies. Consistent with prior methodology, a score of ≥4 correct responses were defined as adequate awareness.
Nutritional Status: Assessed using the Mini Nutritional Assessment–Short Form (MNA-SF) which integrates both subjective and objective indicators, but does not include laboratory or direct muscle strength measurements (21). 12–14: Normal nutritional status; 8–11: At risk of malnutrition; 0–7: Malnutrition.
Cognitive Function: Measured using the Mini-Mental State Examination (MMSE) (22). 27–30: Normal cognitive function; 24–26: Mild cognitive impairment; 18–23: Moderate cognitive impairment; 0–17: Severe cognitive impairment (note: Cut-off values may be adjusted for education level in some studies; in our analysis, MMSE <10 was used as the exclusion criterion for severe impairment).
Frailty: Evaluated by the Fried Frailty Phenotype Scale (23). 0: Robust; 1–2: Prefrail; ≥3: Frail.
Sarcopenia Risk: Assessed by the SARC-F questionnaire (24). 0–3: Low risk of sarcopenia; ≥4: At risk of sarcopenia.
Fall Risk: Estimated with the Morse Fall Risk Scale (25). 0–24: Low risk; 25–44: Moderate risk; ≥45: High risk.
Body Mass Index (BMI) was calculated as weight (kg) divided by height squared (m2). <18.5: Underweight; 18.5–23.9: Normal; ≥24: Overweight (per Chinese guidelines).
Data on major chronic diseases (hypertension, diabetes, cardiovascular and cerebrovascular diseases, etc.) were collected for all participants. The presence of these comorbidities was included as an independent variable in multivariate analyses to control for their potential confounding effects on malnutrition awareness and status.
2.4 Statistical analysis
All statistical analyses and visualizations were performed using R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria), including the use of tidyverse, stats, and ggplot2 packages. Descriptive statistics were presented as means ± standard deviation (SD) for continuous variables and counts (percentages) for categorical variables. Group comparisons between participants who were aware vs. unaware of malnutrition were conducted using: Independent samples t-tests for continuous variables (e.g., MMSE, MNA-SF, and BMI), Chi-square tests for categorical variables (e.g., marital status, education), Multivariate logistic regression was performed with age, cognition (MMSE), BMI, education, living situation, and other significant variables as independent covariates, to control for potential confounding effects, including that of age, to identify independent predictors of malnutrition awareness, with odds ratios (OR) and 95% confidence intervals (CI) reported. Statistical significance was set at p < 0.05.
3 Results
3.1 Participant characteristics
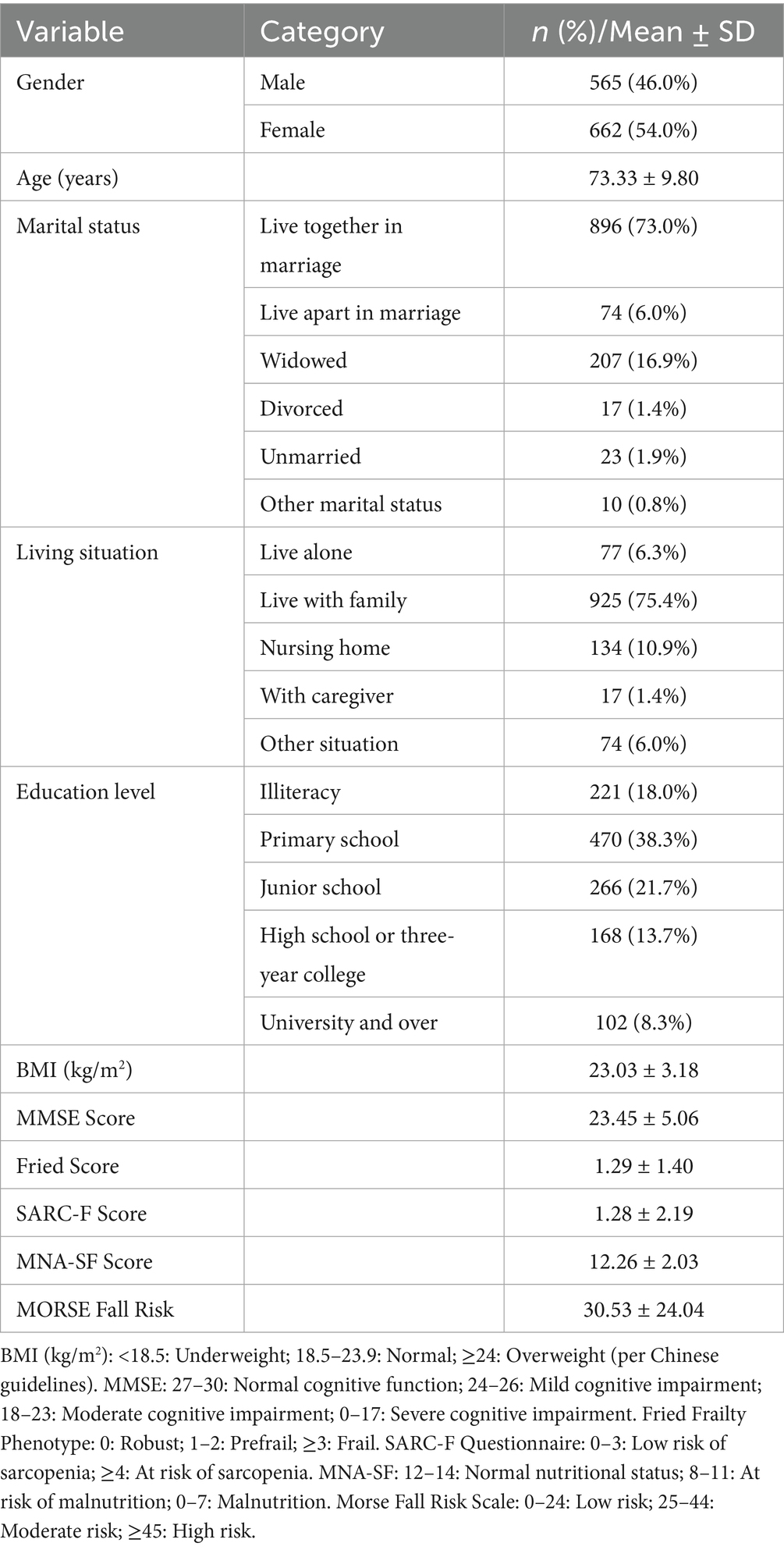
A total of 1,227 older adults were included in the final analysis. The mean age of participants was 73.3 ± 9.8 years, with 54.0% being male. Most participants were married and living with others (73.0%), and the majority were retired. Regarding educational background, a large proportion had received only primary education or were illiterate, whereas a smaller percentage had completed secondary or higher education (Table 1). The mean body mass index (BMI) was 23.0 ± 3.2 kg/m2, and the mean Mini-Mental State Examination (MMSE) score was 23.5 ± 5.1. Nutritional assessment indicated a generally good status, with a mean Mini Nutritional Assessment–Short Form (MNA-SF) score of 12.3 ± 2.0. The average Fried frailty score was 1.3 ± 1.4, and the SARC-F score was 1.3 ± 2.2, suggesting low overall prevalence of severe frailty or sarcopenia. The average Morse Fall Risk Score was 30.5 ± 24.0. Multiple chronic diseases were prevalent, with hypertension, diabetes, coronary artery disease, stroke, and osteoporosis being the most frequently reported.
3.2 Awareness of malnutrition
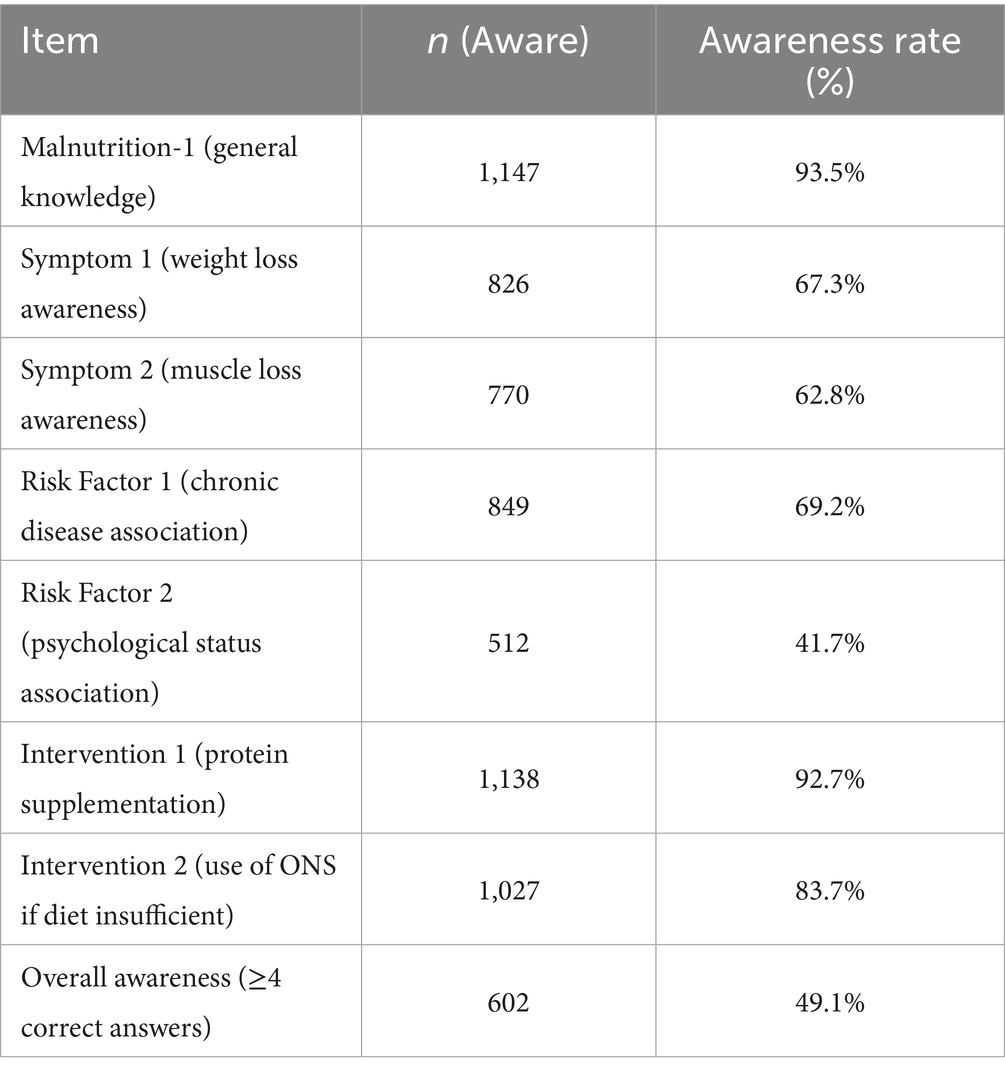
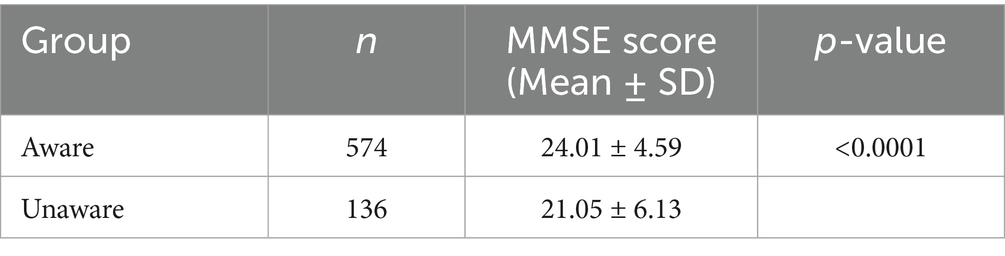
The overall awareness rate of malnutrition was 49.1%, as defined by correctly answering ≥4 out of 7 items in the knowledge assessment scale (Table 2). As shown in Figure 2, the highest awareness was observed for the general concept of malnutrition (93.5%) and recommended interventions such as protein supplementation (92.7%) and use of oral nutrition supplements when dietary intake is inadequate (83.7%). Conversely, awareness was lower for the identification of muscle loss (62.8%) and weight loss (67.3%) as key symptoms, and especially low for recognition of mental health conditions (e.g., depression) as a risk factor (41.7%).
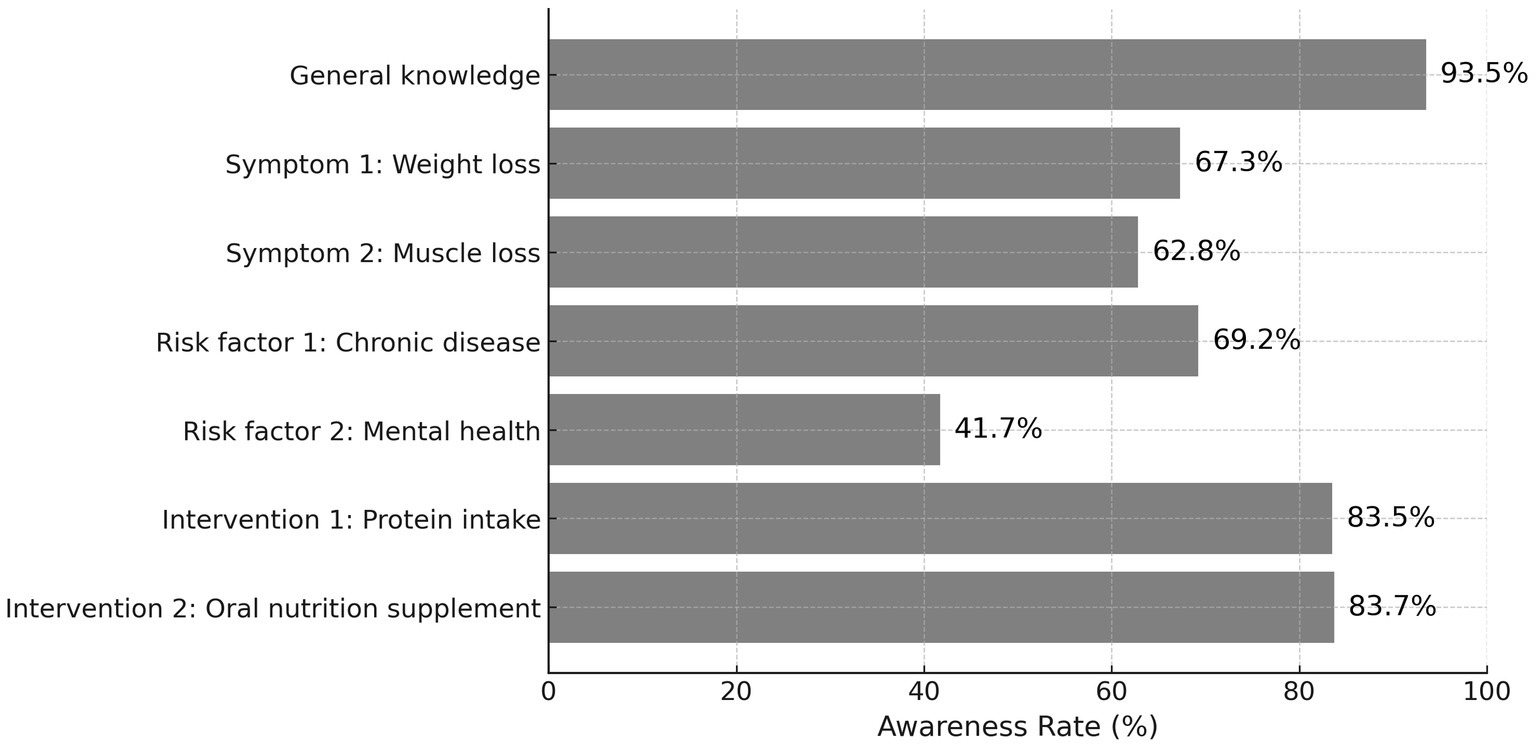
Figure 2. Awareness rate of malnutrition-related items among older adults. Awareness rate of specific malnutrition-related knowledge items among older adults (n = 1,227). Items included general understanding, symptom recognition (weight and muscle loss), risk factors (chronic disease, mental health), and recommended interventions (protein intake, oral nutritional supplements). The lowest awareness was seen in psychological risk factors (41.7%), while knowledge of general concept and protein intervention exceeded 90%.
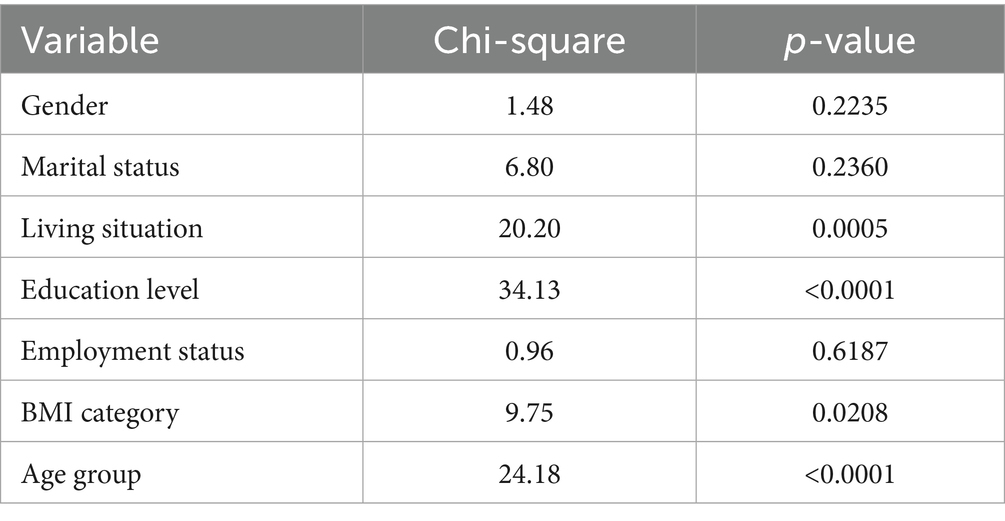
3.3 Univariate analysis of factors associated with awareness
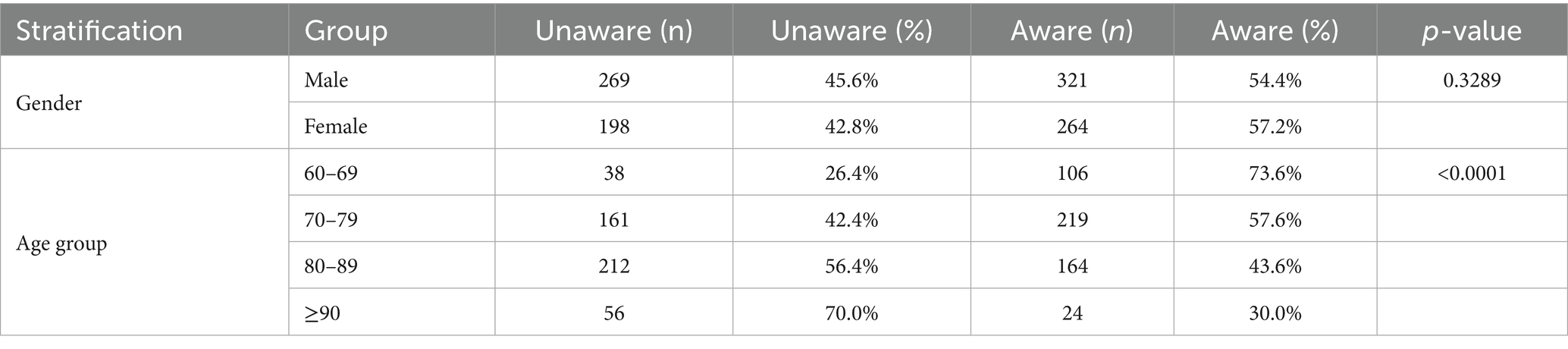
As shown in Table 3, univariate analysis indicated that several sociodemographic variables were significantly associated with malnutrition awareness. Awareness was significantly higher in participants with greater educational attainment (χ2 = 34.13, p < 0.0001) and those living with others (χ2 = 20.20, p = 0.0005). Awareness was also associated with age group (χ2 = 24.18, p < 0.0001) and BMI category (χ2 = 9.75, p = 0.0208). No significant associations were found with gender (p = 0.2235), marital status (p = 0.2360), or employment status (p = 0.6187).
3.4 Multivariate logistic regression analysis
Multivariate logistic regression (Table 4 and Figure 3) identified education level and living situation as independent predictors of malnutrition awareness. Specifically, participants with higher education had significantly greater odds of being aware (OR = 1.38, 95% CI: 1.23–1.55, p < 0.0001). Similarly, those living with others had increased odds of awareness compared to those living alone (OR = 1.33, 95% CI: 1.13–1.56, p = 0.0008). BMI category and age group, though significant in univariate analyses, were not independently associated after adjustment.
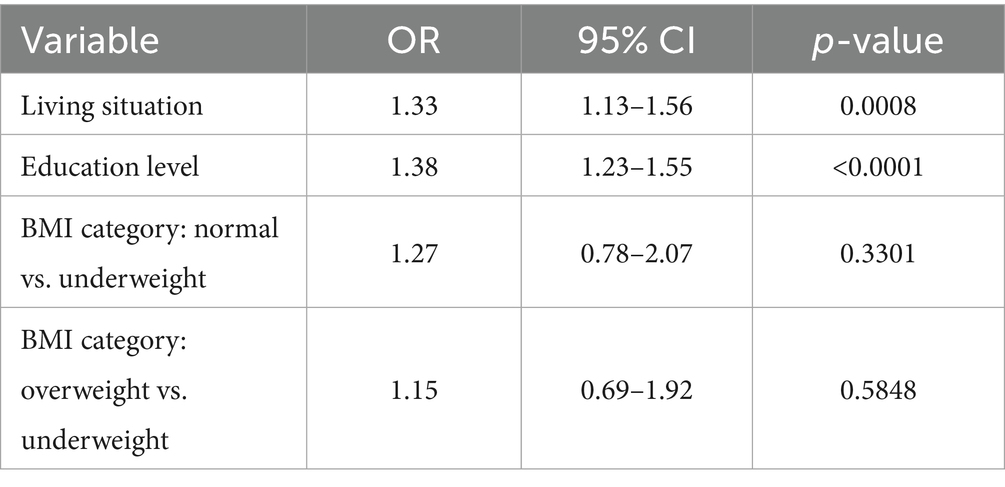
Table 4. Multivariate logistic regression analysis of factors associated with malnutrition awareness.
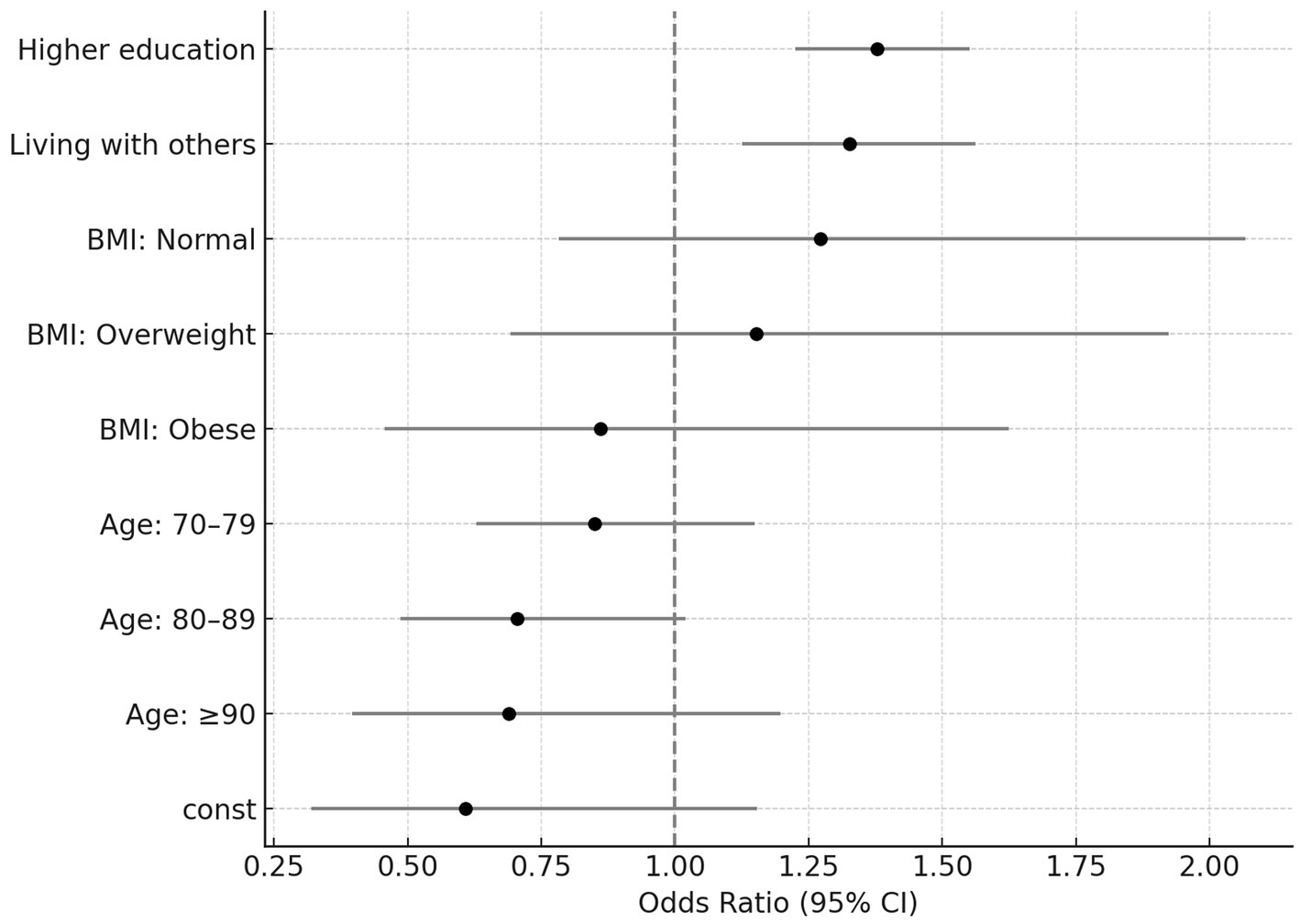
Figure 3. Adjusted odds ratios for malnutrition awareness. Forest plot showing adjusted odds ratios (ORs) and 95% confidence intervals (CI) from multivariate logistic regression for factors associated with malnutrition awareness. Higher educational level and living with others were significantly associated with greater awareness. BMI category and age group were not significantly associated with awareness (p > 0.05).
3.5 Stratified analysis by gender and age
As shown in Table 5 and Figure 4, stratified analysis by gender revealed no statistically significant differences in malnutrition awareness (male: 54.4%, female: 57.2%, p = 0.3289). In contrast, there was a clear and significant inverse trend between age and awareness (p < 0.0001). The highest awareness rate was found in participants aged 60–69 years (73.6%), followed by those aged 70–79 (57.6%) and 80–89 (43.6%), with the lowest rate observed among those aged 90 and above (30.0%).
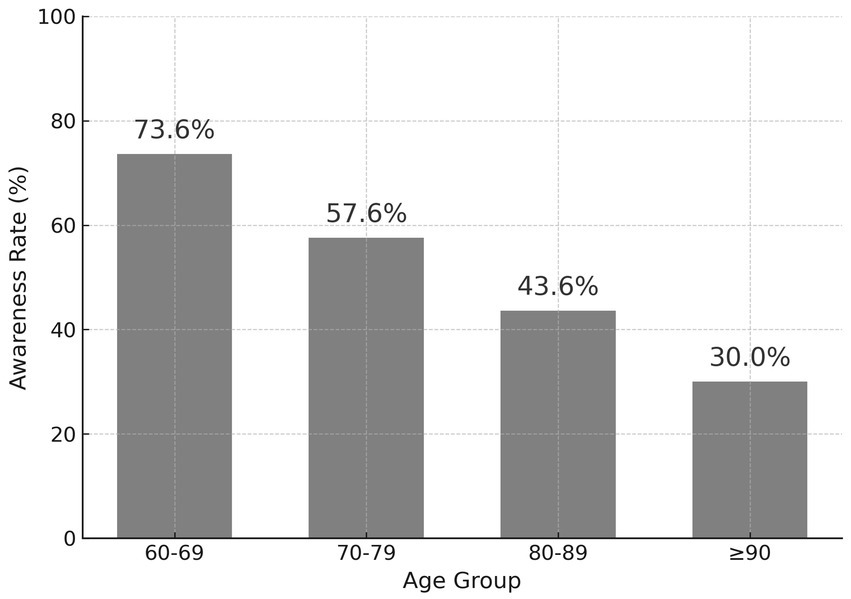
Figure 4. Awareness rate by age group. Awareness rate of malnutrition among older adults by age group (n = 1,227). Awareness significantly decreased with increasing age. The highest rate was observed in participants aged 60–69 (73.6%), while the lowest was in those aged 90 and above (30.0%). The trend was statistically significant (p < 0.0001).
3.6 Association between awareness and cognitive status
The association between malnutrition awareness and cognitive function was examined using MMSE scores. As presented in Table 6 and Figure 5, the mean MMSE score was significantly higher in the aware group (24.01 ± 4.59) compared to the unaware group (21.05 ± 6.13, p < 0.0001). This suggests that individuals with better cognitive status may have a greater capacity to acquire and retain nutrition-related knowledge.

Figure 5. MMSE scores by malnutrition awareness. Comparison of MMSE scores between participants aware and unaware of malnutrition (n = 710). Participants with awareness showed significantly higher cognitive function scores (mean MMSE = 24.01 ± 4.59) than those unaware (mean MMSE = 21.05 ± 6.13), p < 0.0001.
4 Discussion
This study is among the first in China to systematically evaluate malnutrition awareness among older adults and identify its associations with cognitive, educational, and social factors. Our findings reveal that fewer than half (49.1%) of community-dwelling older individuals demonstrated adequate knowledge of malnutrition. While general concepts such as protein supplementation were widely recognized, key clinical symptoms (e.g., unintentional weight loss, muscle wasting) and psychosocial contributors (e.g., depression) were often overlooked. These results underscore a critical knowledge gap that may compromise early recognition and management of malnutrition in aging populations.
4.1 International comparison and psychosocial dimensions
Our results are consistent with previous international and Chinese studies that suggest awareness of malnutrition is low among older adults. A nationwide survey in Germany revealed that fewer than half of older adults participants could identify basic signs of malnutrition, such as unintended weight loss or appetite reduction (26). Similarly, a systematic review covering low- and middle-income countries highlighted that most older adults lack accurate knowledge regarding malnutrition symptoms, risk conditions, and treatment options (27). In China, although awareness of chronic diseases like hypertension is high, malnutrition remains a neglected issue in public health education (14, 15).
Particularly noteworthy is the low awareness of psychological contributors to malnutrition. In our study, only 41.7% of participants recognized mental health as a relevant risk factor. This is concerning given robust evidence that depression, loneliness, and cognitive impairment are strongly linked to nutritional decline in older populations (11, 12). The observed cognitive-nutritional interplay emphasizes the need for integrated health education addressing both physical and psychosocial dimensions.
4.2 Cognitive and social determinants of nutritional literacy
Our multivariate model confirmed that higher educational attainment, intact cognitive function, and cohabitation with others were significant independent predictors of malnutrition awareness. These results align with previous research indicating that educational attainment enhances health literacy and access to reliable nutrition information (28). Similarly, living with others may increase exposure to health messages and social encouragement for healthy behaviors (29). Our findings support the call for socially contextualized interventions targeting isolated or less-educated older adults (30, 31). While age group and BMI category were significant in univariate models, they did not remain independent predictors after adjustment. This may reflect underlying confounding with cognitive function and education level, which were not evenly distributed across age strata.
We found a statistically significant association between cognitive status and malnutrition awareness, with higher MMSE scores observed in the aware group. This finding is in line with previous research and can be explained by several interrelated mechanisms (32, 33). First, individuals with better cognitive function generally possess higher health literacy, allowing them to more effectively process, understand, and retain health information, including knowledge about nutrition and malnutrition prevention. Second, intact cognitive abilities—such as memory, attention, and executive function—facilitate planning, decision-making, and self-management, enabling older adults to recognize symptoms, understand risk factors, and act on nutrition-related guidance. Furthermore, cognitively healthy older adults are more likely to participate in community and social activities, increasing their exposure to health education and peer support. Conversely, cognitive decline impairs these capacities, reducing one’s ability to acquire and recall health knowledge, recognize early signs of malnutrition, and adhere to dietary recommendations (34). In addition, memory loss, impaired judgment, and eating difficulties may directly contribute to undernutrition. These findings underscore the need to tailor educational strategies to the cognitive abilities of older adults. Public health interventions should consider simplified, visual, or repetitive messaging and actively involve caregivers or family members for those with cognitive impairment. Addressing these cognitive barriers is essential for the effective delivery of nutrition education and for maximizing the reach and impact of healthy aging policies at the population level. Evidence suggests that deficiencies in specific micronutrients, particularly vitamin D, may negatively impact cognitive function, which in turn may increase the risk of malnutrition among older adults. While our study did not assess vitamin D or other micronutrient status, the potential role of such deficiencies in the cognitive-nutritional pathway warrants further investigation. Future research should incorporate objective measures of key micronutrients (such as vitamin D) to better understand their mediating effects between cognition and nutrition, and to inform more targeted intervention strategies.
4.3 Policy implications: toward cognition-stratified nutrition education
China’s 2025 “Weight Management Year” initiative provides a timely national framework for addressing malnutrition. However, our findings indicate that universal nutrition messaging may fail to reach subgroups with cognitive or educational vulnerabilities. To maximize impact, we propose a cognition-stratified nutrition education model guided by the following principles:
1. Cognitive tiering: Education delivery formats (e.g., digital modules, pictorial handbooks, and group sessions) should be matched to cognitive ability and literacy level. For cognitively intact individuals, app-based self-learning tools may be appropriate, while those with mild impairment may benefit from simplified visuals or family-assisted sessions. Those with significant decline may require direct caregiver-targeted education.
2. Social integration: Family caregivers and community health workers should be mobilized as co-educators, particularly for isolated or homebound older adults. Education can be embedded into existing community outreach programs or long-term care assessments.
3. Mental health inclusion: Nutrition education content should explicitly address emotional health, appetite suppression from depression, and socially embedded risks. This would align with current evidence that psychological distress is a major, yet underrecognized, contributor to undernutrition.
4. Monitoring and feedback: We recommend incorporating a brief, validated nutrition knowledge screening tool—such as the 7-item scale used in this study—into routine geriatric health evaluations. This would allow public health programs to track awareness trends and evaluate the effectiveness of interventions over time.
Furthermore, we advocate the creation of a risk stratification framework to guide prioritization of interventions. Our results suggest that individuals with (1) MMSE score <22, (2) educational attainment below primary level, and (3) living alone status may constitute a high-risk triad for poor nutrition literacy. These criteria can be operationalized into community-level screening algorithms to triage education efforts efficiently.
4.4 Relevance to older adults health system reform
This study supports the national agenda of building elder-friendly health systems by offering data-driven, tiered intervention strategies that reflect real-world heterogeneity in older adults’ cognitive and social functioning. Our findings emphasize that knowledge inequities are not merely informational but structurally rooted in cognitive capacity, education, and living arrangements.
From a health systems perspective, we recommend the integration of nutrition knowledge assessment into standardized geriatric screening protocols. In community health centers, pairing tools such as the MNA-SF with a brief cognitive screen (e.g., MMSE or MoCA) and a simplified malnutrition knowledge test could enhance early detection of “hidden risk” individuals—those who are not yet malnourished but lack the awareness needed to prevent it.
Moreover, public health authorities could consider embedding nutrition knowledge indicators into national aging surveillance systems, particularly within programs like the Healthy Aging Strategy or regional electronic health record platforms. This would enable systematic tracking of population-level awareness gaps and guide longitudinal policy adjustments.
To ensure long-term sustainability, we also advocate investment in neuro-adaptive education technologies, such as touchscreen kiosks in community centers with animated guidance, or voice-assisted modules for visually or cognitively impaired individuals. These tools should be designed in alignment with behavior change theories, using reinforcement and repetition to optimize retention. By transitioning from a reactive to a proactive prevention model, and by embedding educational sensitivity into public health architecture, China’s response to malnutrition in aging societies can become both more precise and equitable.
4.5 Strengths and limitations
This study’s strengths include its large representative sample, use of validated tools (e.g., MMSE, MNA-SF, SARC-F), and integration of multidimensional geriatric health indicators. Nevertheless, several limitations should be acknowledged. Due to the cross-sectional nature of our study, we cannot infer causality or the directionality of the relationship between cognitive decline and malnutrition. Evidence suggests a bidirectional association: cognitive impairment may contribute to nutritional decline, while poor nutritional status may in turn accelerate cognitive deterioration. Future prospective and interventional studies are needed to elucidate these mechanisms and inform targeted prevention strategies. As all subjects were recruited from hospital-based services, this may limit the generalizability of findings to the broader healthy community-dwelling older adults population. And In our study, 78.8% of participants were outpatients and 21.2% were inpatients. While including both groups helps capture a wider range of older adults, these differences may introduce selection bias. For instance, inpatients often have lower functional status and greater health needs, which could influence their awareness of malnutrition. Future research should use stratified analyses or population-based samples to better address these potential biases. Lastly, in China, rapid socioeconomic changes have created substantial generational, cultural, and regional differences in education, nutrition knowledge, dietary habits, and access to food among older adults. Malnutrition awareness may therefore vary widely, especially between urban and rural areas. Although we adjusted for education and some socioeconomic factors, residual confounding from unmeasured variables such as dietary culture and region may remain. As our study mainly involved urban and peri-urban participants, with few from rural areas, future research should include more diverse samples and detailed dietary and socioeconomic data to better assess these generational and regional differences in malnutrition awareness.
5 Conclusion
This study highlights that malnutrition awareness among older adults in China is insufficient, especially regarding clinical symptoms and psychosocial risk factors. While general nutrition knowledge is relatively widespread, deficits remain in recognizing early warning signs of undernutrition. Cognitive function, education level, and cohabitation status emerged as key determinants of awareness, indicating the need for stratified, cognition-sensitive education strategies. Standardized health messaging alone may not effectively reach vulnerable subgroups, such as those with cognitive decline or low literacy. Future research should move beyond cross-sectional associations to rigorously evaluate, through longitudinal and interventional studies, whether improving malnutrition awareness among older adults leads to measurable improvements in clinical outcomes, such as nutritional status, functional ability, quality of life, and morbidity. Moreover, it is crucial to test the effectiveness and scalability of cognition-stratified nutrition education models in diverse real-world settings—including urban, rural, and minority communities—to provide robust, evidence-based recommendations for national and regional health policies. Only through such translational research can we bridge the gap from descriptive findings to actionable public health strategies that promote healthy aging at scale.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Ethics Committee of Zhejiang Provincial Hospital of Chinese Medicine approved this study (Approval No.2023-KLS-398-02). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FL: Funding acquisition, Conceptualization, Data curation, Writing – original draft, Writing – review & editing, Methodology. JZ: Conceptualization, Writing – review & editing, Methodology. DW: Writing – review & editing, Conceptualization, Methodology. XY: Writing – review & editing, Conceptualization, Methodology. XC: Supervision, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was financially supported by the Zhejiang Province Medical and Health Science and Technology Plan Project (2024KY001), the Zhejiang Province Traditional Chinese Medicine Science and Technology Plan Project (2024ZL002), the Zhejiang Provincial Department of Science and Technology’s Major Social Welfare Program (2023C03162), and the Zhejiang Provincial Program for the Cultivation of High-Level Innovative Health Talents (2022–01).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Xu, W, Zhu, J, Xi, W, and Cui, J. Creating age-friendly environments in a smart society in China: a policy review. J Aging Soc Policy. (2025) 37:216–35. doi: 10.1080/08959420.2023.2284058
3. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The path to healthy ageing in China: a Peking University–lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
4. Zhang, J, Song, PK, Zhao, LY, Sun, Y, Yu, K, Yin, J, et al. Malnutrition in relation with dietary, geographical, and socioeconomic factors among older Chinese. Biomed Environ Sci. (2021) 34:337–47. doi: 10.3967/bes2021.045
5. Wang, Z, Pang, Y, Liu, J, Wang, J, Xie, Z, and Huang, T. Association of healthy lifestyle with cognitive function among Chinese older adults. Eur J Clin Nutr. (2021) 75:325–34. doi: 10.1038/s41430-020-00785-2
6. Zhi, QH, Si, Y, Wang, X, Tai, BJ, Hu, DY, Wang, B, et al. Determining the factors associated with oral health-related quality of life in Chinese elders: findings from the fourth national survey. Community Dent Oral Epidemiol. (2022) 50:311–20. doi: 10.1111/cdoe.12674
7. Norman, K, Haß, U, and Pirlich, M. Malnutrition in older adults—recent advances and remaining challenges. Nutrients. (2021) 13:2764. doi: 10.3390/nu13082764
8. Roberts, S, Collins, P, and Rattray, M. Identifying and managing malnutrition, frailty and sarcopenia in the community: a narrative review. Nutrients. (2021) 13:2316. doi: 10.3390/nu13072316
9. Liu, R, Shao, W, Sun, N, Lai, JK, Zhou, L, Ren, M, et al. Prevalence and the factors associated with malnutrition risk in elderly Chinese inpatients. Aging Med. (2021) 4:120–7. doi: 10.1002/agm2.12143
10. Mao, Y, Wu, J, Liu, G, Yu, Y, Chen, B, Liu, J, et al. Chinese expert consensus on prevention and intervention for the elderly with malnutrition. Aging Med. (2022) 5:191–203. doi: 10.1002/agm2.12226
11. Walker-Clarke, A, Walasek, L, and Meyer, C. Psychosocial factors influencing the eating behaviours of older adults: a systematic review. Ageing Res Rev. (2022) 77:101597. doi: 10.1016/j.arr.2022.101597
12. Nho, J-H, and Kim, EJ. Mediating effects of depression on relationships between nutritional status and quality of life among older adults: a cross-sectional study. J Korean Gerontol Nurs. (2022) 24:47–54. doi: 10.17079/jkgn.2022.24.1.47
13. Zhang, Z, Pereira, SL, Luo, M, and Matheson, EM. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and meta-analysis. Nutrients. (2017) 9:829. doi: 10.3390/nu9080829
14. Yan, Y, Wu, T, Zhang, M, Li, C, Liu, Q, and Li, F. Prevalence, awareness and control of type 2 diabetes mellitus and risk factors in Chinese elderly population. BMC Public Health. (2022) 22:1382. doi: 10.1186/s12889-022-13759-9
15. Zhang, H-Z, Wang, Y-H, Ge, Y-L, Wang, S-Y, Sun, J-Y, Chen, L-L, et al. Obesity, malnutrition, and the prevalence and outcome of hypertension: evidence from the National Health and nutrition examination survey. Front Cardiovasc Med. (2023) 10:1043491. doi: 10.3389/fcvm.2023.1043491
16. Schuetz, P, Seres, D, Lobo, DN, Gomes, F, Kaegi-Braun, N, and Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet. (2021) 398:1927–38. doi: 10.1016/S0140-6736(21)01451-3
17. Bellanti, F, Lo Buglio, A, Quiete, S, and Vendemiale, G. Malnutrition in hospitalized old patients: screening and diagnosis, clinical outcomes, and management. Nutrients. (2022) 14:910. doi: 10.3390/nu14040910
18. Chew, STH, Tan, NC, Cheong, M, Oliver, J, Baggs, G, Choe, Y, et al. Impact of specialized oral nutritional supplement on clinical, nutritional, and functional outcomes: a randomized, placebo-controlled trial in community-dwelling older adults at risk of malnutrition. Clin Nutr. (2021) 40:1879–92. doi: 10.1016/j.clnu.2020.10.015
19. Sun, X, Sun, Z, Peng, W, Zhang, J, Gou, B, Tian, X, et al. Expert consensus and call on actions for weight Management in China: advancing healthy China initiative through strategic actions. China CDC Wkly. (2024) 6:1347–53. doi: 10.46234/ccdcw2024.268
20. Wu, D, Yu, X, Li, F, Qiao, W, and Chen, X. Geriatric syndrome awareness and its determinants in China: a cross-sectional study. BMC Geriatr. (2024) 24:712. doi: 10.1186/s12877-024-05291-9
21. Kaiser, MJ, Bauer, JM, Ramsch, C, Uter, W, Guigoz, Y, Cederholm, T, et al. Validation of the mini nutritional assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. (2009) 13:782–8. doi: 10.1007/s12603-009-0214-7
22. Folstein, MF, Folstein, SE, and McHugh, PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
23. Bieniek, J, Wilczyński, K, and Szewieczek, J. Fried frailty phenotype assessment components as applied to geriatric inpatients. Clin Interv Aging. (2016) 11:453–9. doi: 10.2147/CIA.S101369
24. Malmstrom, TK, and Morley, JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. (2013) 14:531–2. doi: 10.1016/j.jamda.2013.05.018
25. Morse, JM, Morse, RM, and Tylko, SJ. Development of a scale to identify the fall-prone patient. Can J Aging. (1989) 8:366–77. doi: 10.1017/S0714980800008576
26. Kiesswetter, E, Colombo, MG, Meisinger, C, Peters, A, Thorand, B, Holle, R, et al. Malnutrition and related risk factors in older adults from different health-care settings: an enable study. Public Health Nutr. (2020) 23:446–56. doi: 10.1017/S1368980019002271
27. Bardon, LA, Corish, CA, Lane, M, Bizzaro, MG, Loayza Villarroel, K, Clarke, M, et al. Ageing rate of older adults affects the factors associated with, and the determinants of malnutrition in the community: a systematic review and narrative synthesis. BMC Geriatr. (2021) 21:1–39. doi: 10.1186/s12877-021-02583-2
28. Nutbeam, D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
29. Volkert, D, Beck, AM, Cederholm, T, Cruz-Jentoft, A, Goisser, S, Hooper, L, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. (2019) 38:10–47. doi: 10.1016/j.clnu.2018.05.024
30. Cho, JH-J, Olmstead, R, Choi, H, Carrillo, C, Seeman, TE, and Irwin, MR. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging Ment Health. (2019) 23:1130–8. doi: 10.1080/13607863.2018.1481928
31. Hildon, ZJ-L, Tan, CS, Shiraz, F, Ng, WC, Deng, X, Koh, GCH, et al. The theoretical and empirical basis of a BioPsychoSocial (BPS) risk screener for detection of older people’s health related needs, planning of community programs, and targeted care interventions. BMC Geriatr. (2018) 18:1–15. doi: 10.1186/s12877-018-0739-x
32. Jackson, HM, Calear, AL, Batterham, PJ, Ohan, JL, Farmer, GM, and Farrer, LM. Skill enactment and knowledge acquisition in digital cognitive behavioral therapy for depression and anxiety: systematic review of randomized controlled trials. J Med Internet Res. (2023) 25:e44673. doi: 10.2196/44673
33. Miller, LMS. Cognitive and motivational factors support health literacy and acquisition of new health information in later life. Calif Agric. (2010) 64:189–94. doi: 10.3733/ca.v064n04p189
Keywords: geriatric assessment, malnutrition, nutrition education, older adults, awareness
Citation: Li F, Zhang J, Wu D, Yu X and Chen X (2025) Malnutrition awareness and its determinants among Chinese older adults: findings from a cross-sectional survey. Front. Public Health. 13:1638285. doi: 10.3389/fpubh.2025.1638285
Edited by:
Florencia Ceriani, Universidad de la República, UruguayReviewed by:
Lingqiong Meng, University of Arizona, United StatesJuan Carlos Perez-Ycaza, Catholic University of Cuenca, Ecuador
Copyright © 2025 Li, Zhang, Wu, Yu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xujiao Chen, bGlseTE5NzQ1OUAxNjMuY29t
†These authors have contributed equally to this work
 Fangzhou Li
Fangzhou Li Jingmei Zhang1†
Jingmei Zhang1† Xiyan Yu
Xiyan Yu