- 1Department of Nursing, Faculty of Nursing and Midwifery, Wroclaw Medical University, Wrocław, Poland
- 2Department of Health Care Services, Polish National Health Fund, Central Office in Warsaw, Warsaw, Poland
- 3Centre for Cardiovascular Health, Edinburgh Napier University, Edinburgh, United Kingdom
- 4Boston College William F. Connell School of Nursing, Chestnut Hill, MA, United States
- 5Department of Emergency Medical Services, Faculty of Nursing and Midwifery, Wroclaw Medical University, Wrocław, Poland
- 6Group of Research in Care (GRUPAC), Faculty of Health Science, University of La Rioja, Logroño, Spain
- 7Institute of Heart Diseases, University Hospital, Wrocław, Poland
- 8Department of Pharmacology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Zabrze, Poland
- 9Department of Internal Medicine and Clinical Pharmacology, Medical University of Silesia, Katowice, Poland
Background: Understanding smoking prevalence trends across demographic groups is crucial for effective public health interventions. Monitoring such trends helps tailor prevention strategies and allocate resources to the most affected populations. These insights support the design of more equitable and effective tobacco control policies.
Aim: This study analyzes data from the Comprehensive Cardiovascular Risk Prevention Program (CCRPP) in Poland (2012–2021) to assess smoking trends by age and gender among program participants.
Methods: A repeated cross-sectional observational design was used to analyze data collected from 2012 to 2021, including participants who met the predefined age criteria (35, 40, 45, 50, or 55 years) at the time of enrollment, based on their birth year. Smoking prevalence was examined across age groups and sex to identify trends and disparities.
Results: Smoking prevalence significantly declined from 28.91% in 2012 to 21.77% in 2021 (p < 0.001). The largest absolute reduction was seen in the 45-year age group (from 29.90 to 19.50%, p < 0.001). Across all age groups, men consistently had higher smoking rates than women, with the gap most pronounced in the 55-year group in 2012 (41.01% vs. 30.08%, p < 0.001). Although smoking rates decreased over time in both sexes, this male predominance persisted and remained statistically significant (p < 0.001).
Conclusion: Smoking prevalence declined significantly among participants of the CCRPP, particularly in middle-aged individuals. Persistent sex differences highlight the need for more targeted smoking cessation interventions tailored to men. The CCRPP’s large-scale, standardized data collection offers a valuable platform for monitoring national smoking trends and informing future tobacco control policies in Poland.
1 Introduction
Tobacco smoking remains one of the most important modifiable health risk factors (1); therefore, taking action to promote smoking cessation is one of the most important public health challenges. It is worth emphasizing that passive exposure to tobacco smoke is an equally important problem (2).
Tobacco smoke contains numerous carcinogens that affect various signal transduction pathways (3). Exposure to tobacco smoke is associated with increased heart rate, systolic blood pressure, myocardial contractility, and cardiac output (4), as well as development of atherosclerosis through an increase in oxidative stress (5), endothelial dysfunction (6), inflammation (7), thrombosis (8), and platelet activation (9).
Cardiovascular diseases remain the leading cause of morbidity and mortality worldwide (10, 11). Notably, only smoking cessation, not reduction, is associated with a significant reduction in cardiovascular risk (12). In 2017, the multi-center National Population Health Examination Survey (WOBASZ) results were presented. This study, conducted between 2003 and 2014, found that although the percentage of people smoking tobacco was decreasing, it still remained significant and above targeted prevalence (13). More recent data collected retrospectively on a large population in 2016–2020 were presented in 2022 (11.6% of women and 17.1% of men declared smoking). However, this study involved only professionally active adults (14).
There is insufficient data available on tobacco smoking in Polish society, therefore conducting scientific research that can contribute to obtaining additional data is very important. Expanding knowledge about the current epidemiology of tobacco smoking remains essential, taking into account the influence of gender and age for optimal identification of the group of people who should be covered by intensified educational and preventive activities. It should be emphasized that age and gender are factors that significantly influence cardiovascular risk [10.1016/j.atherosclerosis.2023.117269; 10.1016/j.cjca.2021.02.005; 10.3390/jcm14051444], hence, additionally, understanding the relationship with tobacco smoking is crucial in undertaking initiatives aimed at preventing cardiovascular diseases (15–17).
One of the initiatives addressing cardiovascular risk factors in Poland was the Comprehensive Cardiovascular Risk Prevention Program (CCRPP, org. ChUK), a nationwide cardiovascular prevention project conducted between 2012 and 2021 within primary healthcare services. The program aimed at early detection and management of cardiovascular risk factors, including smoking, through comprehensive screenings and preventive interventions. The program is addressed to middle-aged adults (35–65 years old), without diagnosed cardiovascular disease, diabetes, chronic disease, or familial hypercholesterolemia. As part of the program, blood pressure, blood glucose, and lipid profile determination as well as basic anthropometric measurements were performed. The CCRPP provides a unique opportunity to examine long-term smoking trends and their association with cardiovascular risk across different demographic groups from the entire Polish society (18). During similar period, other, smaller-scale cardiovascular disease prevention programs were also conducted. One example is KORDIAN: the nationwide prevention program for atherosclerosis and heart disease through education of people with elevated cardiovascular risk factors (19). Similar projects are also being conducted in other countries around the world, such as the National Public Health Prevention Programme in Greece (20) and Million Hearts 2022 or Well-Integrated Screening and Evaluation for Women Across the Nation (WISEWOMAN) in the United States (21, 22).
The purpose of this study was to analyze a decade of data (2012–2021) from the CCRPP to assess smoking trends by age and gender among program participants.
2 Methods
2.1 Study population
This study utilized a repeated cross-sectional observational design to analyze cross-sectional data collected annually from 2012 to 2021. The total sample size across all years was 880,136 participants, including 342,802 men (39.0%) and 537,334 women (61.0%). In 2012, the initial sample size was 83,974 participants, which declined to 44,797 by 2021. Participants, drawn from the Polish population, were enrolled in the CCRPP based on predefined age criteria (35, 40, 45, 50, or 55 years), determined by birth year, and were stratified by sex. Eligibility criteria included: age between 35 and 65 years; no prior diagnosis of diabetes mellitus, chronic kidney disease, familial hypercholesterolemia, or cardiovascular disease; and no participation in the CCRPP within the past 5 years (23). Data collection methods were standardized annually to ensure methodological consistency. Participants were invited through primary care physicians during routine visits or were recruited via local health initiatives. Smoking status was assessed according to the CCRPP criteria, defining a smoker as an individual who reported current use of tobacco products or regular smoking within the previous 12 months. Smoking status was recorded during a structured interview conducted by trained healthcare staff, with additional information collected on the number of cigarettes smoked per day and years of smoking. Data were entered into a uniform national electronic template (SIMP) and transferred to the National Health Fund database, ensuring methodological consistency across all participating sites and study years (23).
2.2 Ethical
All procedures were conducted in compliance with the relevant guidelines and regulations. Ethical review and approval were not required for this study, as no identifiable data were collected, nor were any laboratory tests or medical interviews conducted. Consequently, approval from a bioethics committee was not necessary under Polish national legislation.
2.3 Statistical analysis
The comparison of categorical variables between groups was performed using the chi-square test (with Yates’ correction for 2×2 tables) or Fisher’s exact test when low expected frequencies were observed in contingency tables. Smoking prevalence (%) was calculated annually for each sex and age group and used as the dependent variable in trend analyses, with calendar year as the independent variable.
Changes over time were analyzed using one of seven statistical models, selected based on the nature of the data. The linear model (y = a + bty = a + bty = a + bt) assumes a constant rate of change over time. The quadratic model (y = a + bt + ct2y = a + bt + ct^2y = a + bt + ct2) and the cubic model (y = a + bt + ct2 + dt3y = a + bt + ct^2 + dt^3y = a + bt + ct2 + dt3) allow for non-linear trends, incorporating squared and cubic terms to capture more complex changes. In cases where an exponential relationship was suspected, the exponential model (ln(y) = a0 + bt\ln(y) = a_0 + btln(y) = a0 + bt) was used, transforming the dependent variable logarithmically. Similarly, the logarithmic model (y = a + b·ln(t)y = a + b\cdot \ln(t)y = a + b·ln(t)) was applied when changes in the predictor variable influenced the outcome in a decreasing manner, while the power model (ln(y) = a0 + b·ln(t)\ln(y) = a_0 + b \cdot\ln(t)ln(y) = a0 + b·ln(t)) was used when the relationship followed a power function. If no significant trend was detected, a constant model (y = ay = ay = a) was assumed, indicating stability over time. For each subgroup (sex and age), the best-fitting model was selected individually. For example, a linear model described the overall smoking prevalence trend, whereas a quadratic model best fit the 55-year-old male subgroup. The selection of the appropriate model was based on the coefficient of determination (R2), with consideration given only to models where the highest-order term was statistically significant. A significance level of 0.05 was applied, meaning that all p-values below this threshold were interpreted as indicating statistically significant relationships. The statistical analysis was performed using the R software.
3 Results
The overall smoking rate decreased from 28.91% in 2012 to 21.77% in 2021, representing a relative reduction of 24.6%, with the most substantial reduction observed in the 45-year age group (a relative decrease of 34.8%; 10.40 percentage points). Sex differences persisted throughout the study period, with males showing consistently higher smoking rates.
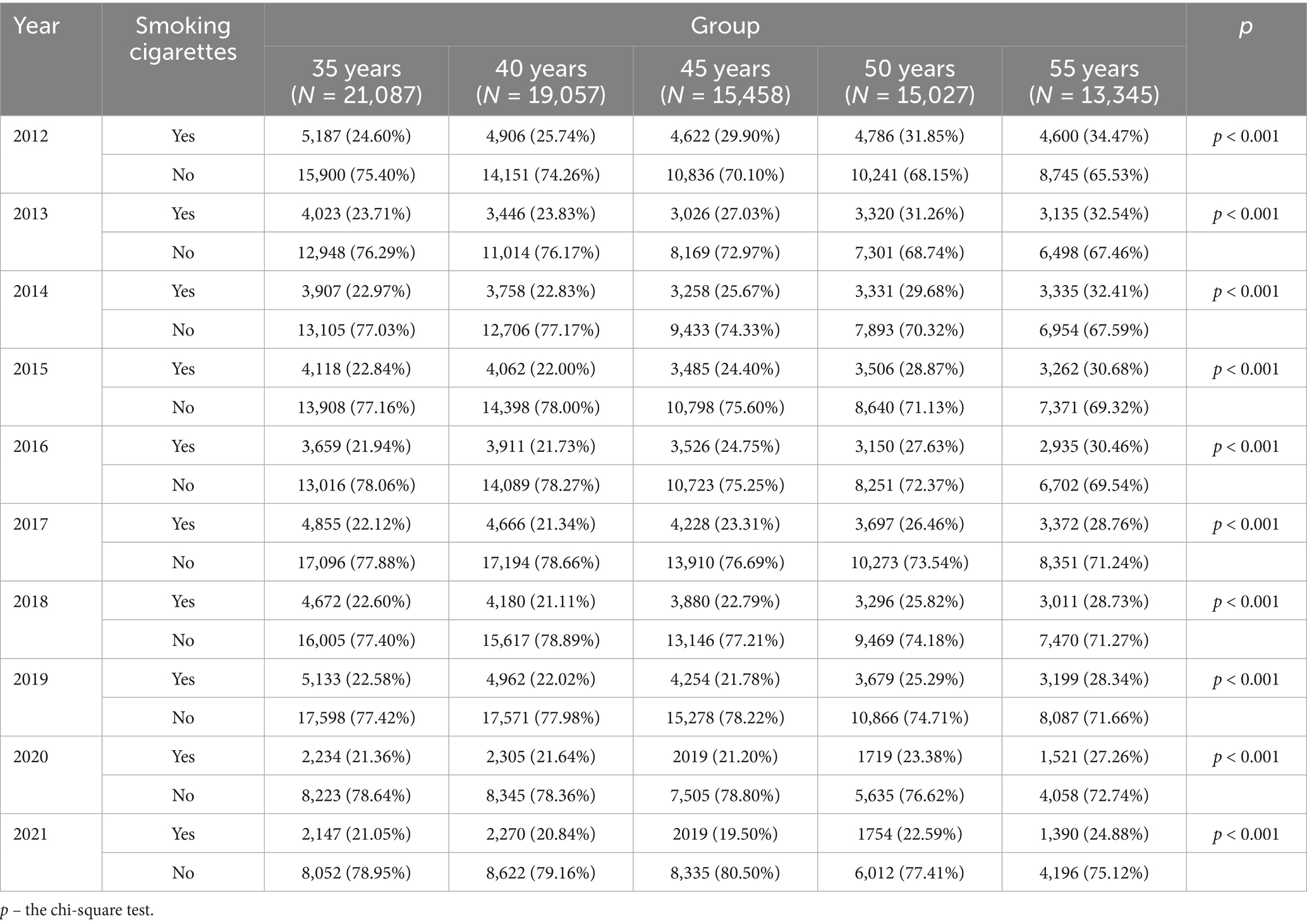
The prevalence of smoking varied significantly across age groups (p < 0.001). As shown in Table 1, older individuals consistently had a higher percentage of smokers compared to younger age groups. In 2012, smoking prevalence was highest among individuals aged 55 + years (34.47%) and lowest among those aged 35–39 years (24.60%). Over the study period, a general decline in smoking prevalence was observed across all age groups. By 2021, the proportion of smokers had decreased in each age category, with the most notable decline in the oldest group (from 34.47% in 2012 to 24.88% in 2021; a relative decrease of 27.8%). These findings suggest an overall reduction in smoking rates over time, with significant differences between age groups.
Table 2 presents the prevalence of smoking among women in different age groups between 2012 and 2021. A statistically significant association was observed (p < 0.001), with older women generally exhibiting higher smoking rates. In 2012, the highest prevalence was noted among 50-year-old women (27.83%) and 55-year-old women (30.08%), while the lowest was in the 35-year-old group (19.97%).
Over the study period, smoking prevalence declined in all female age groups. By 2021, the proportion of smokers decreased to 10.76% in the youngest group (35 years; a relative reduction of 46.1%) and 21.44% in the oldest group (55 years; a relative reduction of 28.7%). These findings indicate a downward trend in smoking rates among women, with significant differences between age groups.
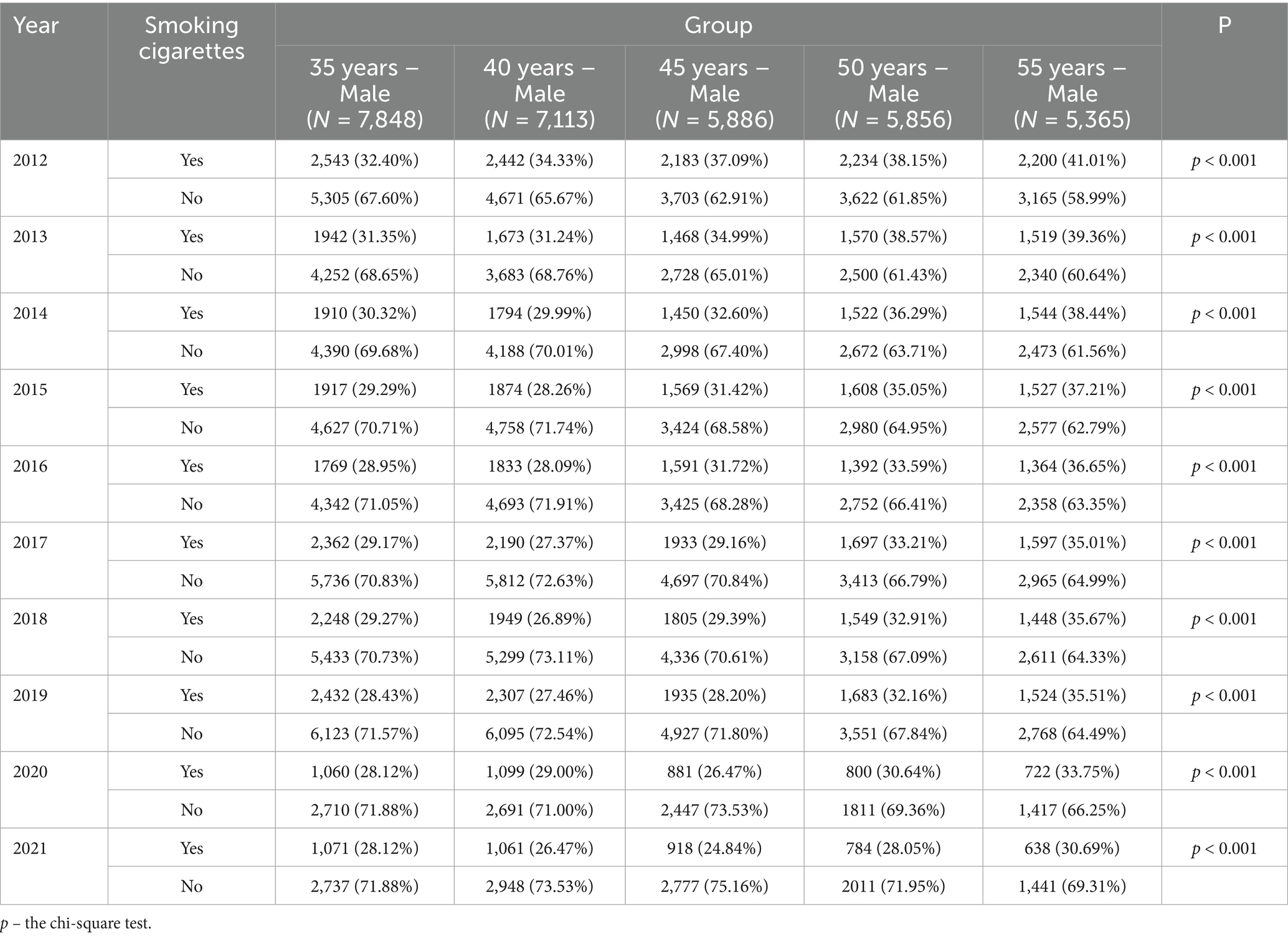
Table 3 presents the prevalence of smoking among male participants in different age groups between 2012 and 2021. A statistically significant association was observed (p < 0.001), with older males generally exhibiting higher smoking rates. In 2012, the highest prevalence was noted among 55-year-old males (41.01%) and 50-year-old males (38.15%), while the lowest was in the 35-year-old group (32.40%). Over the study period, smoking prevalence declined in all male age groups. By 2021, the proportion of smokers decreased to 28.12% in the youngest group (35 years; a relative reduction of 13.2%) and 30.69% in the oldest group (55 years; a relative reduction of 25.2%). These findings indicate a downward trend in smoking rates among males, with significant differences between age groups.
4 Discussion
The CCRPP was developed specifically for adults at risk for CVD to enhance patients’ knowledge and awareness of cardiovascular disease and healthy behaviors, with the primary goal of achieving a 20% relative reduction in CVD incidence and mortality in the Polish population. We have shown that the CCRPP program has caused a significant reduction in the number of people smoking cigarettes in the years 2012–2021 (from 28.91% in 2012 to 21.77% in 2021). The largest reduction in cigarette smoking concerned men aged 45–55 (10–12%) and women aged 45 (almost 9%). Over the years 2012–2021, in each age group, the percentage of smokers was higher among men. Thus, smoking prevalence declined by an average of about 7% among CCRPP participants between 2012 and 2021, which may reflect broader public health trends or increasing health awareness in this group.
A notably sharp decline in smoking prevalence among 45-year-olds may reflect a confluence of factors beyond programmatic intervention. Mid-life is often a transitional stage accompanied by increased healthcare engagement for screening and chronic disease detection, which may have amplified cessation motivation. National registry data indicate that the prevalence of diagnosed hypertension is particularly high and rising in early middle-aged men, with the highest incidence observed in those aged 55–59, and elevated prevalence in younger men under 55 years (24). In parallel, trends in premature cardiovascular mortality in Poland during 2008–2017 show the greatest relative decreases among individuals aged 40–44, suggesting heightened public awareness and responsiveness to health messaging in neighboring age cohorts (25). These converging factors — enhanced detection of risk factors and greater salience of health risks at mid-life — likely synergized with CCRPP activity, contributing to the disproportionate decline in smoking at age 45.
The consistently higher smoking rates among men throughout the decade may be linked to multiple factors: cultural norms, occupational exposures, and differential coping strategies related to stress (26). Data from Poland show that smoking prevalence remains considerably higher in men than women, including a higher proportion of “hardcore” smokers—with 13.0% of men compared to 7.3% of women identified in a national survey (27). Tailored interventions—including workplace-based cessation programs, male-focused communication strategies, and integration of cessation support into routine occupational health assessments—may help address this disparity (26, 28).
Our study showed that conducting comprehensive CVD prevention programs led to a significant reduction in the incidence of one of the main cardiovascular (CV) risk factors. According to the World Health Organization (WHO), the percentage of smokers worldwide decreased from 22 to 17% between 2007 and 2021. Cigarette smoking contributes not only to an increased risk of CVD, but also to a number of other diseases including metabolic, oncological, respiratory, endocrine and gastrointestinal disorders (29–31). The 2021 European Society of Cardiology (ESC) guidelines on CVD prevention clearly indicate that smoking cessation should be recommended (class I recommendation) (32). In Poland, according to a study by Jankowski et al., in the group of women aged 40–49 and 50–59, the percentage of smokers is 33.3 and 27.6%, respectively. Among men the percentage is 35.6 and 37.5%, respectively (33). Thus, it appears that people covered by the CCRPP program are more motivated to quit smoking. It is estimated that every year, more than 82,800 adults in Poland are killed by tobacco-related diseases (34). Given that tobacco use is one of the most preventable causes of cardiovascular morbidity and mortality, reducing smoking rates remains a critical public health goal (34). Despite the countless data indicating the harmfulness of smoking, cigarettes have remained at the forefront of cardiovascular risk factors worldwide for decades. In 1990, smoking was in fifth place, while in 2019 it was in 6th place in terms of the prevalence of cardiovascular risk factors. Epidemiological data estimate indicate that in 2050 smoking will rank 7th in this ranking (35, 36). Although this trend is positive, the rate of decline remains too slow.
It is also important to acknowledge that the observed decline in smoking prevalence over the decade may not be solely attributable to the CCRPP program. Other contributing factors could include increased public awareness of the harms of smoking, broader health promotion initiatives, gradual shifts in social norms, and evolving patterns of nicotine product use. While our analysis suggests that the CCRPP played a meaningful role, particularly given the absence of new national tobacco regulations during this period, these additional influences should be considered when interpreting the findings. Furthermore, during the study period Poland continued to fulfill its obligations as a signatory to the WHO Framework Convention on Tobacco Control (FCTC) (37), which has been progressively strengthened over the past two decades. Although no major new national tobacco control strategy or legislation was developed, existing measures — including public smoking bans, graphic health warnings, and restrictions on tobacco advertising and sponsorship — remained in force, with periodic public health campaigns reinforcing these provisions (38). These ongoing efforts, aligned with FCTC guidelines, may have contributed to the observed decline in smoking prevalence, acting in parallel with the CCRPP and other health promotion activities (39–41). The observed decline in smoking prevalence, despite the absence of new national tobacco legislation, suggests that sustained, structured, primary care–based interventions such as the CCRPP can be an effective driver of behavioral change. By integrating cardiovascular risk assessment, personalized counseling, and follow-up into routine healthcare encounters, CCRPP may have provided continuous motivation and opportunities for cessation that complemented existing legislative measures.
Therefore, implementing comprehensive programs such as CCRPP on a large scale can contribute to a faster reduction in the number of smokers, not only in Poland but also worldwide. The results of the meta-analysis by Bakhit et al. (42) emphasize the key role of implementing comprehensive programs such as CCRPP in CVD prevention. This meta-analysis showed that providing patients with information about the benefits of quitting smoking, both in primary and secondary prevention, did not translate into a significant reduction in smoking (42). It is worth emphasizing that education should clearly indicate: (1) never starting smoking; (2) quitting smoking as soon as possible; (3) using new forms of smoking (e-cigarettes, heat-not-burn [HnB] systems) only as a way to quit smoking and not as a substitute. It has been shown that only smoking cessation, but not reduction, was associated with reduced CVD risk (12). Cessation of smoking significantly contributes to the reduction of CV risk compared to individuals who continue smoking. The extent of risk reduction is positively correlated with the duration of smoking abstinence, with longer periods of cessation leading to a progressive decline in CV risk. Over time, this risk approaches that of individuals who have never smoked; however, it does not fully revert to baseline levels, indicating a persistent residual risk attributable to prior tobacco exposure (43). Therefore, the best form of prevention is to never smoke cigarettes.
Despite the fact that our analysis did not include new forms of smoking: e-cigarettes and heated tobacco systems (HnB), it is worth paying attention to them, as some people may have switched from traditional cigarettes to these modern forms. Furthermore, these new forms of smoking, particularly disposable e-cigarettes, are currently the primary method of nicotine initiation among children and adolescents (44). Unfortunately, despite a partially better safety profile, e-cigarettes and HnB are often used at the same time (double and triple smokers) (45). Simultaneous use of 2–3 forms of smoking is associated with a significantly higher cardiovascular risk compared to smoking, for example, only traditional cigarettes (46). Taking this into account, educational programs should emphasize that, for example, e-cigarettes, in a similar way to traditional ones, increase the risk of CVD and stroke (46). The use of e-cigarettes and HnB systems is associated with an increase in cardiovascular risk (47, 48). Therefore, it is recommended to conduct a more extensive medical interview regarding cigarette smoking, as some people may not recognize e-cigarettes and HnB as cigarettes.
Conducting comprehensive smoking cessation programs, such as CCRPP, significantly increases the likelihood of successfully quitting tobacco use. To enhance cessation success rates, a structured approach should be implemented, incorporating motivation by highlighting the benefits of quitting, thorough assessment, and, if necessary, additional education and encouragement, with recognition of previous quit attempts made by the patient. An essential component of this process is the use of nicotine replacement therapy, along with support from close family members (49, 50). Evidence suggests that a gradual, step-by-step approach to smoking cessation, based on education and motivation, is more effective in achieving long-term abstinence compared to abrupt quitting attempts (51). It is also worth mentioning that different factors influence smoking cessation in women and men. The main barriers to smoking cessation in women were psychological factors, such as emotion and stress, compared with environmental factors in men (26). Women despite smoking fewer cigarettes and being less nicotine dependent than men, women find it more difficult to quit. Especially in the group of women, a multidisciplinary approach involving a psychologist, dietitian, and physical activity specialist is important in the process of quitting smoking (52).
This study offers added value beyond confirming global declines in smoking prevalence by providing a decade-long, large-scale, program-based analysis drawn from the CCRPP in Poland. Unlike previous national surveys, our dataset includes over 880,000 participants stratified into fixed age cohorts and analyzed separately by sex, allowing the identification of trends not previously described in the Polish context. These include the most pronounced decline in smoking among individuals aged 45 years, the persistence of significant sex disparities despite overall reductions, and the observation that such changes occurred in the absence of major new national tobacco control legislation. These findings demonstrate the potential for structured, long-term prevention programs embedded in primary healthcare to drive measurable behavioral change, offering a model that can be adapted and applied in other countries. From a policy perspective, our findings reinforce the need to scale structured prevention programs like CCRPP within primary care, especially targeting middle-aged men. National strategies could incorporate smoking cessation counseling into routine health checks, increase access to pharmacotherapy, and expand surveillance to include alternative nicotine products (53, 54). Public campaigns should also address gender-specific barriers to quitting, with tailored messaging that resonates with men’s motivations and contexts.
In summary, our research has shown that the comprehensive CVD prevention program – CCRPP has led to a significant reduction in the percentage of smoking women and men in Poland over the past decade. Nevertheless, the number of smokers is still too high and it is necessary to promote even more knowledge about the harmfulness of smoking (taking into account the increasingly available new forms of smoking, which are increasingly used by children).
4.1 Study limitations
This study has several limitations that should be considered when interpreting the results. First, the data were obtained from the CCRPP, which may introduce selection bias, as participants were likely more health-conscious and motivated to engage in preventive healthcare compared to the general population. Second, smoking status was self-reported, which may have led to reporting bias, as individuals might have underreported or misreported their smoking habits. Third, the study lacked detailed socioeconomic and clinical data, preventing an in-depth analysis of potential confounders such as income, education level, and family history of cardiovascular disease, which could have influenced smoking behavior trends. In particular, the CCRPP dataset did not capture key determinants such as socioeconomic status, urban/rural residency, or comorbidities, which limited our ability to adjust for these potential confounders or to examine disparities in smoking prevalence across different population subgroups. Moreover, the dataset was available only in aggregated form (annual prevalence by sex and age group), without individual-level records. This precluded the use of multivariable statistical approaches such as logistic regression with interaction terms (e.g., age × sex, time × age) and the calculation of regression-based confidence intervals. This study spans a decade (2012–2021), during which public health policies and smoking regulations were already well-established. While previously established smoking restrictions and tobacco control measures remained in effect, no significant new regulations were introduced during this period. However, healthcare access, public awareness campaigns, and the continued enforcement of national tobacco control measures under the WHO Framework Convention on Tobacco Control (FCTC) evolved during this period, potentially affecting smoking trends. As the CCRPP dataset did not include information on participants’ exposure to these broader interventions, we could not disentangle their effects from the program’s impact. The COVID-19 pandemic (2020–2021) likely impacted both participation rates and smoking behaviors among CCRPP participants. Lockdowns and disruptions in healthcare services limited program coverage, and pandemic-related stress may have increased smoking in some individuals. However, data in this area are inconsistent, with some suggesting an increase in smoking due to stress, while others suggest a decrease because smoking was perceived as a risk factor for COVID-19 (55, 56). It is worth noting that the use of new forms of smoking increased significantly during the COVID-19 pandemic (57). Conversely, heightened public concerns about respiratory health and COVID-19-related messaging may have prompted others to attempt to quit (58). These conflicting influences make it difficult to discern the true impact of the CCRPP on smoking prevalence in the most recent years of observation. Despite these limitations, the study provides valuable insights into temporal trends in smoking prevalence in Poland and underscores the effectiveness of structured prevention programs in reducing smoking rates. Future research should incorporate additional demographic and behavioral variables, as well as objective biomarkers, to enhance the understanding of smoking patterns and improve targeted intervention strategies. The present study focused exclusively on smoking status, despite the availability of other relevant variables in the CCRPP dataset, such as education, physical activity, and alcohol use. While this approach allowed for a detailed analysis of one key modifiable cardiovascular risk factor, it does not account for the potential influence of these other factors on smoking prevalence and trends. Future analyses could incorporate these variables to provide a more comprehensive picture of smoking behaviors in the Polish population.
5 Conclusion
In this nationwide, repeated cross-sectional study of the CCRPP, smoking prevalence declined markedly between 2012 and 2021, most notably in middle-aged adults. Persistent sex disparities highlight an urgent need for targeted cessation strategies for men. These findings support the continuation and expansion of structured prevention programs within primary care, with integration of demographic-specific interventions and systematic monitoring of emerging tobacco products. Public health policy should prioritize sustained investment in such initiatives, coupled with enhanced surveillance to capture socioeconomic and geographic disparities. Future research using individual-level, representative data is essential to determine the causal impact of these programs and to guide more equitable, effective tobacco control. From a policy perspective, our findings imply that embedding structured smoking cessation and cardiovascular risk reduction interventions within primary care can yield measurable public health benefits, even in the absence of new national legislation. Such models could be replicated in settings where legislative change is delayed or politically challenging. The lessons learned from CCRPP may inform and inspire similar large-scale, evidence-based initiatives in other countries facing persistent tobacco-related health burdens.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
GK: Project administration, Writing – review & editing, Formal analysis, Methodology, Writing – original draft, Visualization, Investigation, Conceptualization. IU: Methodology, Supervision, Writing – review & editing, Writing – original draft, Funding acquisition. CL: Writing – original draft, Writing – review & editing. MC: Writing – original draft, Visualization, Writing – review & editing, Formal analysis. GJ: Writing – original draft, Writing – review & editing. SS: Writing – review & editing, Writing – original draft. ML: Writing – original draft, Writing – review & editing. MW: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Ministry of Science and Higher Education of Poland under the statutory grant of Wroclaw Medical University (SUBZ. L010.25.053).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. OpenAI’s ChatGPT 4.0o was utilized for language editing and proofreading to ensure clarity, coherence, and linguistic accuracy in the final manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hunt, LJ, Covinsky, KE, Cenzer, I, Espejo, E, Boscardin, WJ, Leutwyler, H, et al. The epidemiology of smoking in older adults: a National Cohort Study. J Gen Intern Med. (2023) 38:1697–704. doi: 10.1007/s11606-022-07980-w
2. Flor, LS, Anderson, JA, Ahmad, N, Aravkin, A, Carr, S, Dai, X, et al. Health effects associated with exposure to secondhand smoke: a burden of proof study. Nat Med. (2024) 30:149–67. doi: 10.1038/s41591-023-02743-4
3. Warren, GW, Sobus, S, and Gritz, ER. The biological and clinical effects of smoking by patients with cancer and strategies to implement evidence-based tobacco cessation support. Lancet Oncol. (2014) 15:e568–80. doi: 10.1016/S1470-2045(14)70266-9
4. Klein, LW. Pathophysiologic mechanisms of tobacco smoke producing atherosclerosis. Curr Cardiol Rev. (2022) 18:e110422203389. doi: 10.2174/1573403X18666220411113112
5. Taati, B, Arazi, H, and Suzuki, K. Oxidative stress and inflammation induced by Waterpipe tobacco smoking despite possible protective effects of exercise training: a review of the literature. Antioxidants. (2020) 9:777. doi: 10.3390/antiox9090777
6. Dikalov, S, Itani, H, Richmond, B, Arslanbaeva, L, Vergeade, A, Rahman, SMJ, et al. Tobacco smoking induces cardiovascular mitochondrial oxidative stress, promotes endothelial dysfunction, and enhances hypertension. Am J Physiol Heart Circ Physiol. (2019) 316:H639–46. doi: 10.1152/ajpheart.00595.2018
7. Choi, WJ, Lee, JW, Cho, AR, and Lee, YJ. Dose-dependent toxic effect of cotinine-verified tobacco smoking on systemic inflammation in apparently healthy men and women: a Nationwide population-based study. Int J Environ Res Public Health. (2019) 16:503. doi: 10.3390/ijerph16030503
8. Alarabi, AB, Lozano, PA, Khasawneh, FT, and Alshbool, FZ. The effect of emerging tobacco related products and their toxic constituents on thrombosis. Life Sci. (2022) 290:120255. doi: 10.1016/j.lfs.2021.120255
9. Lyytinen, G, Melnikov, G, Brynedal, A, Anesäter, E, Antoniewicz, L, Blomberg, A, et al. Use of heated tobacco products (IQOS) causes an acute increase in arterial stiffness and platelet thrombus formation.Atherosclerosis. (2024) 390:117335. doi: 10.1016/j.atherosclerosis.2023.117335
10. Gaidai, O, Cao, Y, and Loginov, S. Global cardiovascular diseases death rate prediction. Curr Probl Cardiol. (2023) 48:101622. doi: 10.1016/j.cpcardiol.2023.101622
11. Kocełak, P, Puzianowska-Kuźnicka, M, Olszanecka-Glinianowicz, M, and Chudek, J. Wnt signaling pathway and sclerostin in the development of atherosclerosis and vascular calcification. Adv Clin Exp Med. (2024) 33:519–32. doi: 10.17219/acem/169567
12. Jeong, SM, Jeon, KH, Shin, DW, Han, K, Kim, D, Park, SH, et al. Smoking cessation, but not reduction, reduces cardiovascular disease incidence. Eur Heart J. (2021) 42:4141–53. doi: 10.1093/eurheartj/ehab578
13. Polakowska, M, Kaleta, D, Piotrowski, W, Topór-Mądry, R, Puch-Walczak, A, Niklas, A, et al. Tobacco smoking in Poland in 2003–2014. Multi-Centre national population health examination survey (WOBASZ). Pol Arch Intern Med. 127:91–9. doi: 10.20452/pamw.3896
14. Rulkiewicz, A, Pilchowska, I, Lisik, W, Pruszczyk, P, and Domienik-Karłowicz, J. Prevalence of cigarette smoking among professionally active adult population in Poland and its strong relationship with cardiovascular co-morbidities-POL-O-CARIA 2021 study. J Clin Med. (2022) 11:4111. doi: 10.3390/jcm11144111
15. Kim, HJ, Choi, H, Ahn, HJ, Shin, SH, Kim, C, Lee, SH, et al. Machine learning–based analysis of lifestyle risk factors for atherosclerotic cardiovascular disease: retrospective case-control study. JMIR Med Inform. (2025) 13:e74415. doi: 10.2196/74415
16. Young, C, Courtenay, A, Rajiah, K, and Abuelhana, A. Unmasking cardiovascular risk in patients with COPD at primary care settings: the critical role of age, sex, and smoking. J Clin Med. (2025) 14:1444. doi: 10.3390/jcm14051444
17. Connelly, PJ, Azizi, Z, Alipour, P, Delles, C, Pilote, L, and Raparelli, V. The importance of gender to understand sex differences in cardiovascular disease. Can J Cardiol. (2021) 37:699–710. doi: 10.1016/j.cjca.2021.02.005
18. Profilaktyka chorób układu krążenia (CHUK). Pacjent. Available online at: http://pacjent.gov.pl/programy-profilaktyczne/program-profilaktyki-chorob-ukladu-krazenia-chuk (accessed December 11, 2024)
19. KORDIAN. Available online at: https://programkordian.pl/ (accessed August 12, 2025)
20. National Public Health Prevention Programme/Cardiovascular Risks Prevention – European Commission. Available online at: https://commission.europa.eu/projects/national-public-health-prevention-programme-cardiovascular-risks-prevention_en (accessed August 12, 2025)
21. Jun 5 LR, (2023). CDC Prevention Programs. Available online at: https://www.heart.org/en/get-involved/advocate/federal-priorities/cdc-prevention-programs (accessed August 12, 2025)
22. Vaid, I, Blum, E, and Nwaise, I. Women with blood pressure improvement in the well-integrated screening and evaluation for women across the nation program by race and ethnicity, 2014–2018. J Women's Health. (2024) 33:467–72. doi: 10.1089/jwh.2023.0612
23. Zarządzenie Nr 79/2022/DSOZ. Narodowy Fundusz Zdrowia (NFZ) – finansujemy zdrowie Polaków. Available online at: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz (accessed August 12, 2025)
24. Cegłowska, U, Burzyńska, M, Prejbisz, A, Stępińska, J, Gellert, R, Pinkas, J, et al. Incidence and prevalence of registered hypertension in Poland. Pol Arch Intern Med. (2024) 134:6746. doi: 10.20452/pamw.16746
25. Moryson, W, and Stawińska-Witoszyńska, B. Trends in premature mortality rates among the polish population due to cardiovascular diseases. Int J Occup Med Environ Health. (2022) 35:27–38. doi: 10.13075/ijomeh.1896.01798
26. Dieleman, LA, van Peet, PG, and Vos, HMM. Gender differences within the barriers to smoking cessation and the preferences for interventions in primary care a qualitative study using focus groups in the Hague, the Netherlands. BMJ Open. (2021) 11:e042623. doi: 10.1136/bmjopen-2020-042623
27. Kaleta, D, Usidame, B, Dziankowska-Zaborszczyk, E, Makowiec-Dąbrowska, T, and Leinsalu, M. Prevalence and factors associated with hardcore smoking in Poland: findings from the global adult tobacco survey (2009–2010). BMC Public Health. (2014) 14:583. doi: 10.1186/1471-2458-14-583
28. Moher, M, Hey, K, Lancaster, T, and Cahill, K. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. (2005) 2:CD003440. doi: 10.1002/14651858.CD003440.pub4
29. Chen, B, Yan, Y, Wang, H, and Xu, J. Association between genetically determined telomere length and health-related outcomes: a systematic review and meta-analysis of Mendelian randomization studies. Aging Cell. (2023) 22:e13874. doi: 10.1111/acel.13874
30. Mi, N, Liu, M, Meng, C, and Fu, F. Evaluation of the effects of vitamin D deficiency and cigarette smoking on insulin resistance in type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Adv Clin Exp Med. (2024) 33:679–89. doi: 10.17219/acem/171451
31. Chen, Q, Katsouras, CS, Liu, C, Shi, J, Luan, X, Ni, C, et al. Gender-specific risks for incident cancer in patients with different heart failure phenotypes. ESC Heart Fail. (2024) 12:497–507. doi: 10.1002/ehf2.15097
32. Visseren, FLJ, Mach, F, Smulders, YM, Carballo, D, Koskinas, KC, Bäck, M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2021) 42:3227–337. doi: 10.1093/eurheartj/ehab484
33. Jankowski, M, Ostrowska, A, Sierpiński, R, Skowron, A, Sytnik-Czetwertyński, J, Giermaziak, W, et al. The prevalence of tobacco, heated tobacco, and E-cigarette use in Poland: a 2022 web-based cross-sectional survey. Int J Environ Res Public Health. (2022) 19:4904. doi: 10.3390/ijerph19084904
34. Szymański, J, Ostrowska, A, Pinkas, J, Giermaziak, W, Krzych-Fałta, E, and Jankowski, M. Awareness of tobacco-related diseases among adults in Poland: a 2022 Nationwide cross-sectional survey. Int J Environ Res Public Health. (2022) 19:5702. doi: 10.3390/ijerph19095702
35. Chong, B, Jayabaskaran, J, Jauhari, SM, Chan, SP, Goh, R, Kueh, MTW, et al. Global burden of cardiovascular diseases: projections from 2025 to 2050. Eur J Prev Cardiol. (2024) 32:zwae281. doi: 10.1093/eurjpc/zwae281
36. Roth, GA, Mensah, GA, Johnson, CO, Addolorato, G, Ammirati, E, Baddour, LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
37. WHO Framework Convention on Tobacco Control. Available online at: https://fctc.who.int/ (accessed August 12, 2025)
38. Balwicki, Ł, Miller, M, Cedzyńska, M, Przepiórka, I, Pinkas, J, Tomczak, W, et al. Expert consensus statement on tobacco control sustainability in Poland. Nowotw J Oncol. (2023) 73:238–241. Available at: https://journals.viamedica.pl/biuletyn_pto/article/view/97280/73743
39. McHardy, J, Marquizo, AB, Bettcher, D, and Gakidou, E. Policy view: worldwide patterns of tobacco use with recommendations for tobacco control. Lancet Respir Med Published online 2025. Available online at: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(25)00172-9/abstract (accessed August 12, 2025)
40. Shelley, DR, Kyriakos, C, McNeill, A, Murray, R, Nilan, K, Sherman, SE, et al. Challenges to implementing the WHO framework convention on tobacco control guidelines on tobacco cessation treatment: a qualitative analysis. Addiction. (2020) 115:527–33. doi: 10.1111/add.14863
41. Benzian, H, Beltrán-Aguilar, E, and Mackay, J. The World Health Organization framework convention on tobacco control at 20 years: why oral health care professionals must stay in the fight. J Am Dent Assoc. (2025) 156:678–82. doi: 10.1016/j.adaj.2025.05.015
42. Bakhit, M, Fien, S, Abukmail, E, Jones, M, Clark, J, Scott, AM, et al. Cardiovascular disease risk communication and prevention: a meta-analysis. Eur Heart J. (2024) 45:998–1013. doi: 10.1093/eurheartj/ehae002
43. Ding, N, Sang, Y, Chen, J, Ballew, SH, Kalbaugh, CA, Salameh, MJ, et al. Cigarette smoking, smoking cessation, and long-term risk of 3 major atherosclerotic diseases. J Am Coll Cardiol. (2019) 74:498–507. doi: 10.1016/j.jacc.2019.05.049
44. Jester, JM, Glass, JM, Bohnert, KM, Nigg, JT, Wong, M, and Zucker, RA. Child and adolescent predictors of smoking involvement in emerging adulthood. Health Psychol. (2019) 38:133–42. doi: 10.1037/hea0000703
45. Knura, M, Kurowski, T, Lubanski, J, Majek, P, and Jankowski, M. E-cigarette: an effective tool to quit smoking or an. Porto Biomed J. Available online at: https://journals.lww.com/pbj/fulltext/2017/09000/e_cigarette__an_effective_tool_to_quit_smoking_or.41.aspx (accessed February 2, 2025)
46. Glantz, SA, Nguyen, N, and Oliveira da Silva, AL. Population-based disease odds for E-cigarettes and dual use versus cigarettes. NEJM Evid. (2024) 3:229. doi: 10.1056/EVIDoa2300229
47. Siddiqi, TJ, Rashid, AM, Siddiqi, AK, Anwer, A, Usman, MS, Sakhi, H, et al. Association of Electronic Cigarette Exposure on cardiovascular health: a systematic review and Meta-analysis. Curr Probl Cardiol. (2023) 48:101748. doi: 10.1016/j.cpcardiol.2023.101748
48. Fried, ND, and Gardner, JD. Heat-not-burn tobacco products: an emerging threat to cardiovascular health. Am J Physiol Heart Circ Physiol. (2020) 319:H1234–9. doi: 10.1152/ajpheart.00708.2020
49. Aung, MN, Yuasa, M, Moolphate, S, Lorga, T, Yokokawa, H, Fukuda, H, et al. Effectiveness of a new multi-component smoking cessation service package for patients with hypertension and diabetes in northern Thailand: a randomized controlled trial (ESCAPE study). Subst Abuse Treat Prev Policy. (2019) 14:10. doi: 10.1186/s13011-019-0197-2
50. Nian, T, Guo, K, Liu, W, Deng, X, Hu, X, Xu, M, et al. Non-pharmacological interventions for smoking cessation: analysis of systematic reviews and meta-analyses. BMC Med. (2023) 21:378. doi: 10.1186/s12916-023-03087-z
51. Li, WHC, Xia, W, Wang, MP, Cheung, DYT, Cheung, KY, Wong, CKH, et al. Effect of quitting immediately vs progressively on smoking cessation for smokers at emergency department in Hong Kong: a posteriori analysis of a randomized controlled trial. PLoS One. 18:925. doi: 10.1371/journal.pone.0280925
52. Allagbe, I, Thomas, D, Airagnes, G, Limosin, F, Chagué, F, Zeller, M, et al. Specific risk factors profile and abstinence rate of female smokers at high cardiovascular risk from the nationwide smoking cessation services cohort CDT-net. Arch Cardiovasc Dis Suppl. (2022) 14:102–3. doi: 10.1016/j.acvdsp.2021.09.235
53. Goszczyńska, E. Challenges for smoking cessation interventions targeted at women in Poland. Med Pr. (2012) 63:471–82.
54. Hitchman, SC, and Fong, GT. Gender empowerment and female-to-male smoking prevalence ratios. Bull World Health Organ. (2011) 89:195–202. doi: 10.2471/BLT.10.079905
55. Khamees, A, Awadi, S, Rawashdeh, S, Talafha, M, Alzoubi, M, Almdallal, W, et al. The impact of COVID-19 pandemic lockdown on smoking habits and lifestyle: a cross-sectional study. Health Sci Rep. (2023) 6:e1392. doi: 10.1002/hsr2.1392
56. Loui, HF, Li, J, Jackson, NJ, Romero, R, Wisk, LE, and Buhr, RG. Tobacco consumption behavior change during the COVID-19 pandemic is associated with perceived COVID threat. BMC Public Health. (2024) 24:2827. doi: 10.1186/s12889-024-20259-5
57. Didkowska, J, Wojciechowska, U, and Przewoźniak, K. Smoking behaviours in Poland before and after COVID-19 pandemic. Tob Prev Cessat. (2023) 9:172806. doi: 10.18332/tpc/172806
Keywords: smoking cessation, tobacco use disorder, cardiovascular disease prevention, public health intervention, sex differences
Citation: Kubielas G, Uchmanowicz I, Lee CS, Czapla M, Jakubiak GK, Surma S, Lisiak M and Wleklik M (2025) Smoking trends in Poland (2012–2021)—insights from the comprehensive cardiovascular risk prevention program. Front. Public Health. 13:1643059. doi: 10.3389/fpubh.2025.1643059
Edited by:
Margubur Rahaman, All India Institute of Medical Sciences Gorakhpur, IndiaReviewed by:
Anusha Manoharan, Ministry of Health Malaysia, MalaysiaRoomani Srivastava, AIIMS, New Delhi, India
Copyright © 2025 Kubielas, Uchmanowicz, Lee, Czapla, Jakubiak, Surma, Lisiak and Wleklik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michał Czapla, bWljaGFsLmN6YXBsYUB1bXcuZWR1LnBs
 Grzegorz Kubielas1,2
Grzegorz Kubielas1,2 Izabella Uchmanowicz
Izabella Uchmanowicz Michał Czapla
Michał Czapla Grzegorz K. Jakubiak
Grzegorz K. Jakubiak Stanisław Surma
Stanisław Surma Marta Wleklik
Marta Wleklik