- 1Department of Family Medicine, Radiology, and Emergency Medicine, Faculty of Medicine, Hashemite University, Zarqa, Jordan
- 2Faculty of Medicine, Hashemite University, Zarqa, Jordan
Exclusive breastfeeding (EBF) is a crucial public health strategy that reduces infant morbidity and mortality, yet rates remain suboptimal among refugee populations. This study examines breastfeeding practices and determinants of EBF among long-standing Palestinian refugees in Jordan through a cross-sectional survey of 249 mothers at the UNRWA Zarqa Camp Health Center. The prevalence of EBF among infants under 6 months was 38.2%, declining with age. Key predictors included birth order, mode of delivery, labor analgesia, and breastfeeding initiation timing. Mothers who delivered vaginally avoided analgesia, and initiated breastfeeding within the first hour had significantly higher EBF rates. Perceived insufficient milk supply was the primary reason for formula introduction. Breastfed infants experienced fewer acute illnesses, antibiotic use, and allergic conditions. Despite moderately positive maternal attitudes toward breastfeeding, fewer than half of the mothers received breastfeeding education, with no significant association between maternal knowledge and feeding methods. These findings underscore the need for interventions promoting early breastfeeding initiation, reducing unnecessary cesarean sections and analgesia, and strengthening breastfeeding education to improve EBF rates and infant health in refugee settings.
1 Introduction
Breastfeeding is regarded as the optimal source of nutrition for infants (1), providing unparalleled health benefits. The World Health Organization and the American Academy of Pediatrics recommend exclusive breastfeeding (EBF) for the first 6 months of life to achieve optimal growth, development, and health (2).
By 2030, the Sustainable Development Goals (SDG) target to end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal and under-five mortality (3). Unfortunately, as of 2022, we are still off-track to achieve the 2030 agenda (4). Globally, infectious diseases – mainly pneumonia, malaria, and diarrhea-accounted for 30% of under-five deaths beyond the neonatal period in 2022 (5). Exclusive breastfeeding is linked in literature with lower incidences of diarrhea, otitis media, UTIs, allergic diseases, and pneumonia in infants (6, 7). Furthermore, EBF promotes effective weight gain, cognitive development (8, 9), and may reduce the risk of chronic diseases such as asthma, allergies, diabetes, and obesity (10). Breastfeeding also offers significant benefits to mothers, including protection against breast cancer, improved birth spacing, and potential protection against ovarian cancer and type 2 diabetes (10).
Despite its proven benefits, the rate of EBF globally is still below the goal set by the World Health Assembly Resolution with the target that at least half of infants should be exclusively breastfed for the first 6 months of life by 2025 (11). In Jordan, the rate of exclusive breastfeeding as reported by the United Nations International Children’s Emergency Fund (UNICEF) in 2017 for infants 0 to 5 months was 25% (12). Common barriers to EBF include the lack of maternal knowledge about EBF and its benefits (13), low maternal confidence in the ability to breastfeed (14), perception of insufficient breastmilk (15), and lack of family and community support for EBF (16). Understanding the factors influencing EBF practices remains critical for designing effective interventions.
In acute and long-term emergencies, infants and young children are particularly vulnerable, where risks of malnutrition, infectious diseases, and mortality are significantly increased for children under 2 who are not breastfed and for infants under 6 months who are not exclusively breastfed (17). Among refugee populations, these vulnerabilities are exacerbated. A systematic review found higher mortality rates among children born to refugee parents, with socio-economic disadvantage and infectious diseases playing significant roles (18). In such contexts, EBF emerges as a critical survival intervention.
By the end of 2023, the United Nations High Commissioner for Refugees (UNHCR) reported 117.3 million forcibly displaced people worldwide, most of them were displaced in countries neighboring their country of origin and live in urban areas outside of camps (19).
Jordan is a lower-middle-income country (12) that hosts the second-highest share of refugees per capita in the world from different nationalities (20). In the middle governorate of Jordan, Zarqa camp—the oldest Palestinian refugee camp established in 1949 — hosts long-standing Palestinian refugees who left Palestine as a result of the 1948 War. While many of these refugees are accommodated in camps, the majority live alongside other Jordanians in cities, towns, and villages, and hold Jordanian citizenship (21).
While government hospitals are the main provider of services to Palestinian refugees in Jordan, UNRWA (United Nations Relief and Works Agency for Palestine Refugees) remains an important healthcare provider particularly for the poorest population, offering mother–child care services to both camp and non-camp residents (21).
Breastfeeding practices are influenced by diverse and multifaceted factors that include medical conditions, hospital protocols, socioeconomic status, cultural beliefs, media and marketing influence, workplace support, and individual factors (22). However, studies that investigated infant feeding practices among long-standing refugees in Jordan are limited. This study aims to fill that gap by investigating breastfeeding and infant feeding practices among infants aged 0–6 months in long-standing Palestinian refugee communities within the middle governorate of Jordan. This research also explores predictors of exclusive breastfeeding and its association with the infant’s health. As such, it may serve as a valuable contribution to the scientific literature on the challenges faced by these vulnerable populations.
2 Materials and methods
2.1 Study design and setting
A cross-sectional study was conducted using a face-to-face interview with mothers of infants 6 months old or below who attended the UNRWA Zarqa Camp Health Center (ZCHC) during the period June 4th to August 3rd, 2023.
The study outcomes are expected to find the prevalence of breastfeeding among these infants and determine the predictors of exclusive breastfeeding and its association with infant’s health.
All mothers to infants aged 6 months or younger who attended maternal and child health services at UNRWA ZCHC during the period of the survey, and who were willing to participate were recruited.
2.2 Sample size
The sample size was calculated based on the following formula: (23).
Since exclusive breastfeeding for the first 6 months is the recommended feeding practice by all health organizations, we relied on this indicator for calculating the sample size.
Based on the results of a recent study (24) about exclusive breastfeeding among Palestinian refugees in Jordan which included 307 infants aged 6 months or younger in 2017 at UNRWA health centers, the prevalence of exclusive breastfeeding among these infants was 34%. Hence the sample size to achieve a precision of ±5% with a 95% Confidence Interval (CI) was 344, which was not achieved in the time available for data collection according to the timetable of the study, a total of 249 participants were included in this study.
2.3 Data collection tools
A validated, constructed, anonymous, and confidential questionnaire was employed to measure different underlying constructs. It was formulated in Arabic and was carefully designed to avoid leading or biased questions. It was filled by the researchers during face-to-face interviews with participating mothers. The interview was initiated by asking the mother to fill a consent form, and a participant information sheet was given to the participant which included explanation about the aim and importance of the study, assuring the safety and privacy of their data, and what to do and whom to contact if they decided to withdraw from the study at any time.
The first part of the questionnaire asked about sociodemographic information like the mother’s age, nationality, level of education, occupation, the family’s place of residence (inside or outside the refugee camp), the source of family income as well as the amount of monthly income (voluntary question), and maternal chronic diseases and smoking status. In addition to information about the infant (age, gender, and birth order).
The next section enquired about the birth conditions (term or preterm, place and mode of delivery, analgesia used, postpartum hemorrhage, and infant’s birth weight).
The following section included questions about maternal height, pre-pregnancy and pre-delivery weight, the timing of the first breastfeeding, skin-to-skin practice, rooming-in during birth hospitalization, and current infant feeding method.
The next question was specific for breastfed babies and asked about breastfeeding practices like frequency of breastfeeding, scheduled or upon request, and signs of infant’s satiety following breastfeeding session.
Then, a section asked about the infant’s diet like the type and reason for introducing milk other than breastmilk to infant’s diet, solid foods, juices and sweets, in addition to questions about signs of sufficient milk intake like the number of daily wet and soiled diapers as well as daily sleep hours.
The following two sections enquired about the mother’s knowledge and attitude toward breastfeeding, and the last section asked about infant’s health issues like attending regular well-child visits, vaccination, number of healthcare visits for acute illnesses, number of episodes of diarrhea and acute respiratory illnesses, use and frequency of antibiotics, hospitalizations, allergic conditions, and infant growth parameters which were recruited from the infant’s health record for the current visit.
2.4 Ethical approval
Ethical approval for this study was obtained from the Institutional Review Board Committee of Hashemite University on October 31, 2022, and the Research Review Board Committee of the UNRWA on April 20, 2023.
2.5 Data management
The data collected was analyzed using SPSS (Statistical Package for Social Science) version 25. Descriptive statistics such as mean and standard deviation were used for quantitative/continuous data while frequencies and percentages were used for qualitative/categorical data. The chi-square test was employed to assess differences between categorical variables. The independent sample t-test and one-way ANOVA were conducted to identify independent determinants. A p-value of <0.05 was considered statistically significant with a confidence level of 95%.
3 Results
A total of 249 mothers were interviewed and answered the questionnaire. All of them were married. Most of them were younger than 40 years (97.2%), had Jordanian nationality (87.1%), live outside the refugee camp (90%), were housewives (93.2%), had secondary school or lower level of education (79.9%), had four or fewer children (84.3%), were multiparous (75%), had vaginal delivery in their last birth (65.1%), had delivered at hospital (98.4%), and did not receive analgesia during delivery (60.5%). Half of them had normal weight status before pregnancy while 40.2% of them were either overweight or obese, and less than a third of them had normal gestational weight gain during the last pregnancy (31%) (Table 1).
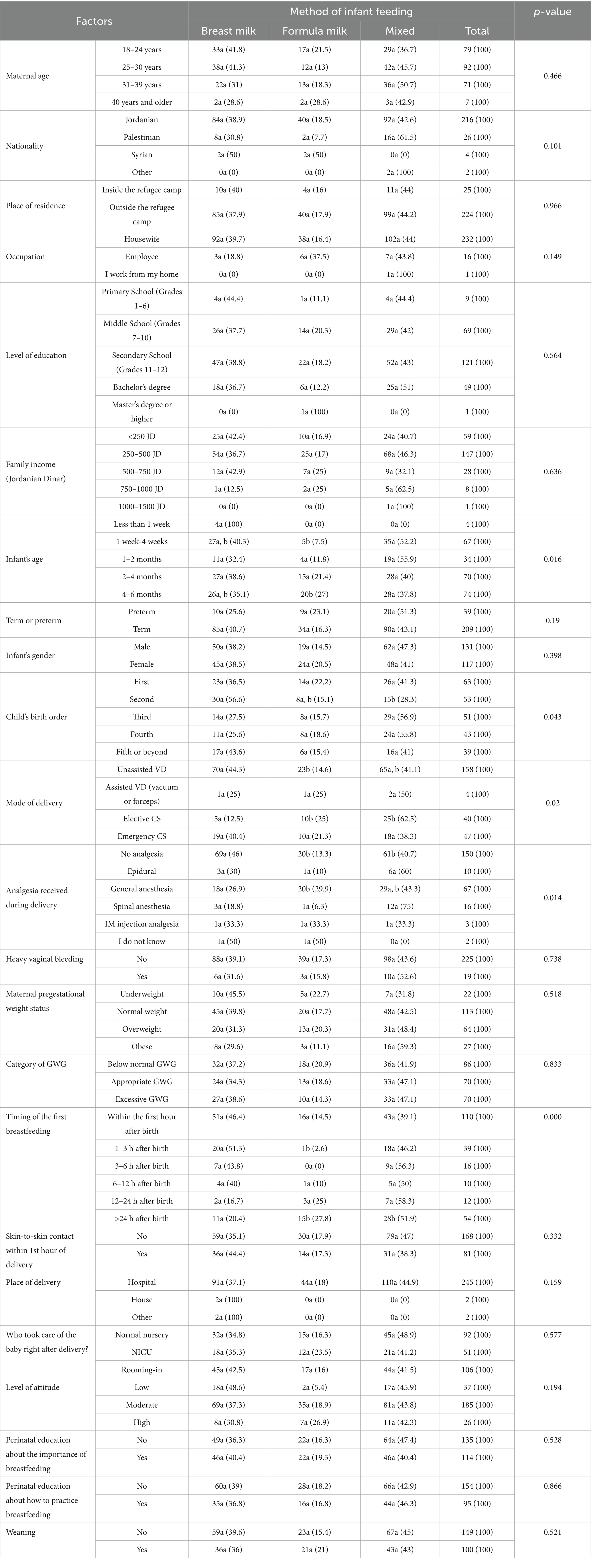
Table 1. Sociodemographic, maternal, and infant-related factors and their associations with breastfeeding practices.
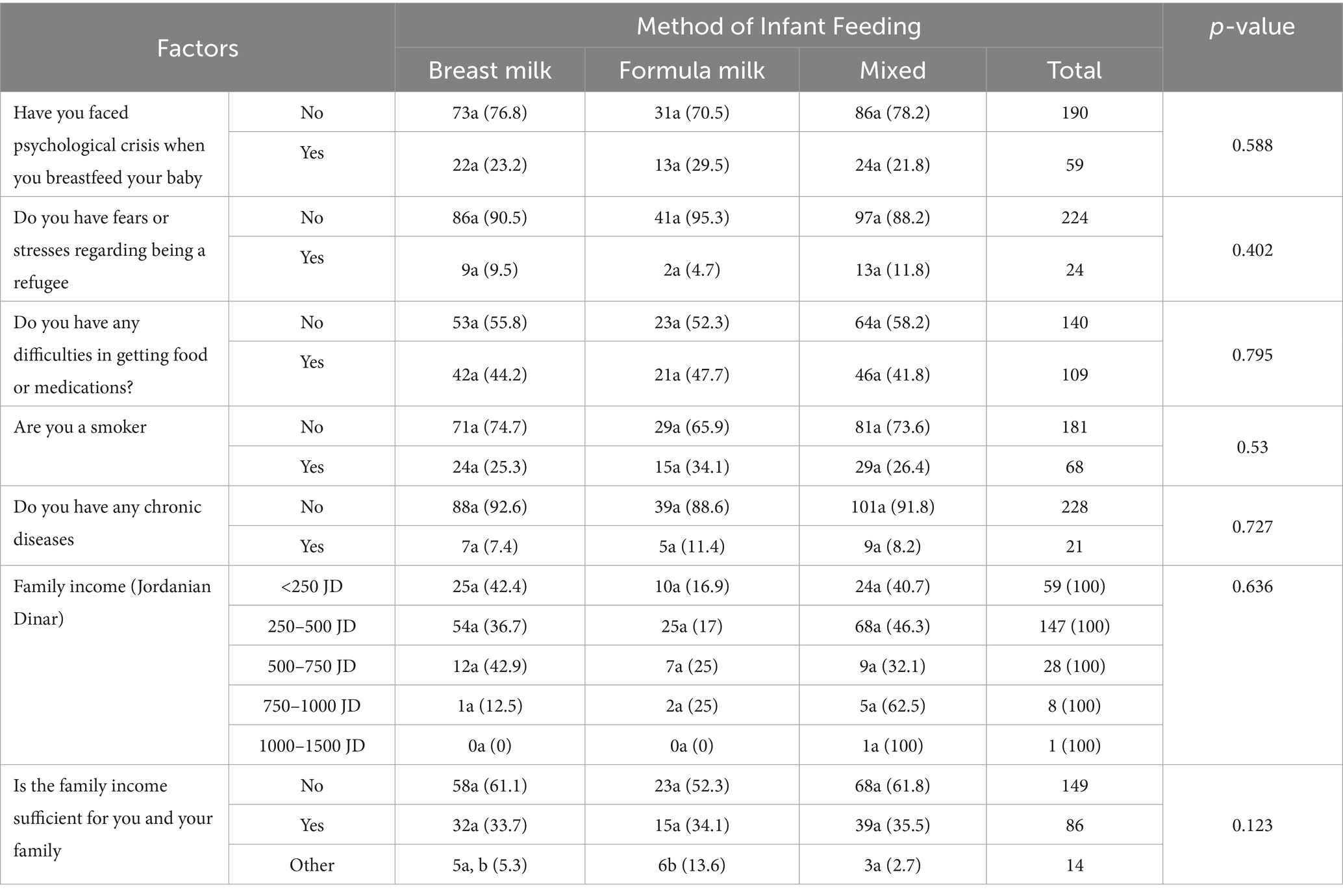
More than one-fourth (27.3%) were smokers, 21 mothers had one or more chronic medical conditions (8.4%) (Table 2). Nineteen mothers (7.8%) had postpartum hemorrhage, 10 of them (4%) had blood transfusions and one mother required surgical intervention to stop bleeding (Table 1).
Most participants had a monthly income of 500 JDs or below (84.8%), 43.8% reported having difficulties in getting food or medications, and 59.8% mentioned that the family’s monthly income is not sufficient to meet their daily needs (Table 2).
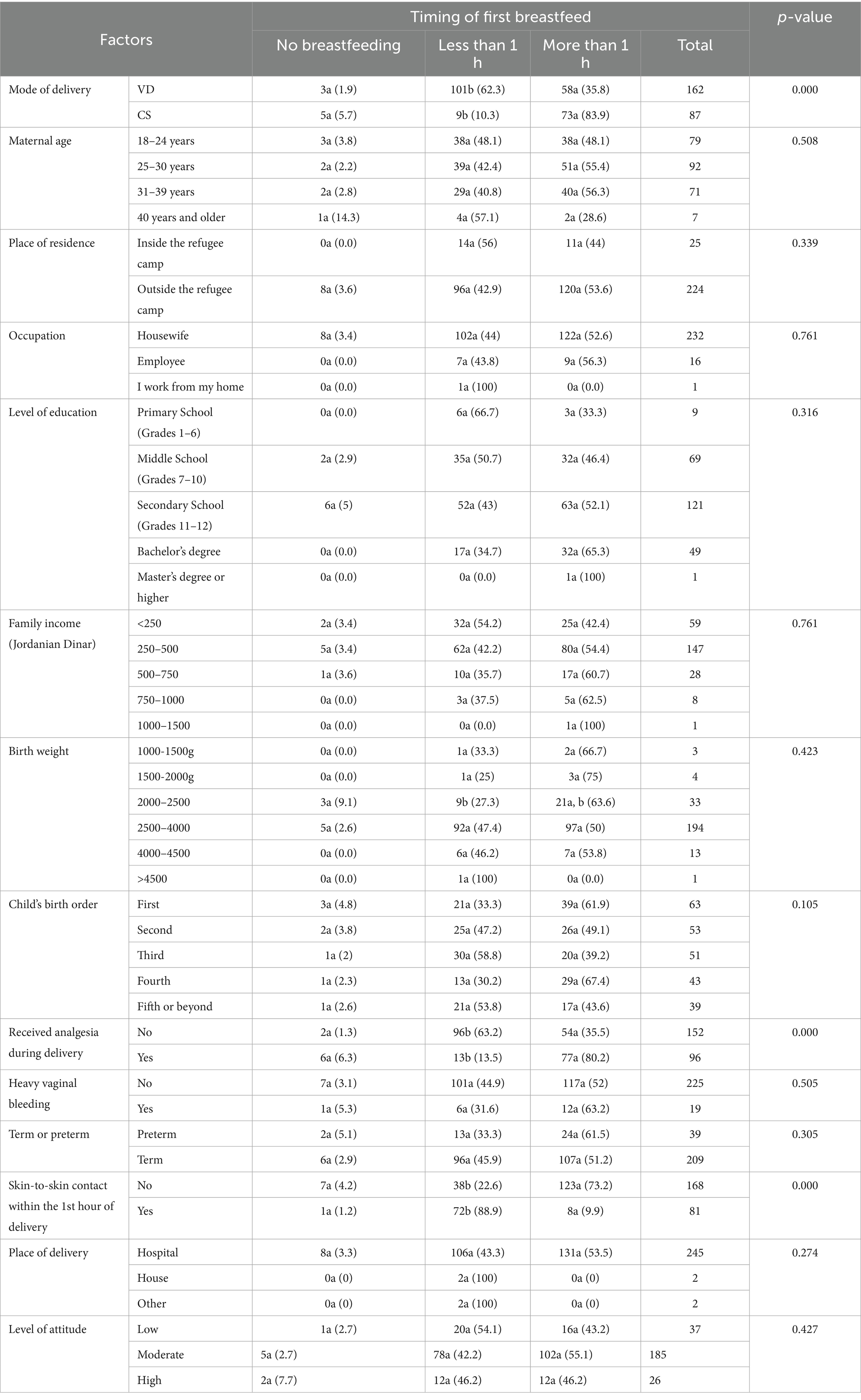
Most of the infants were born at term (84.3%), had normal birth weight (2,500–4,000 gm) (78.2%), 52.8% were male, 44.2% had their first breastfeeding within the first hour after birth, 32.5% had skin-to-skin contact with their mothers within the first hour after birth, and 42.6% had rooming-in with their mothers during the birth hospitalization.
At the time of the survey, the mean age of the infants was 11.3 weeks (median 12, min. 0, max. 29 weeks, SD: 7.985).
The current method of infant feeding was reported to be exclusive breastfeeding, formula feeding, and mixed feeding by 38.2, 17.7, and 44.2%, respectively.
Exclusive breastfeeding was reported by all mothers and by 40% of mothers to infants less than 1 week of age and 1–4 weeks of age, respectively, while almost only one-third of infants aged 4–6 months were exclusively breastfed (35.1%).
Most breastfed babies were fed upon request (77.6%), had at least 6 breastfeeding sessions daily (82.4%) during the week preceding the interview, had signs of satiety after breastfeeding sessions like sleeping and looking calm and relaxed after the end of the feed (71.7 and 95.1%, respectively).
All infants with mixed feeding were given an infant formula. In addition to infant formula, one infant had received cow’s milk powder not intended for infant feeding, and 4 infants (2.4%) received breastmilk from another mother. The additional milk was introduced since birth in 59.2% of the cases. The reason for the introduction of the additional milk was the mother’s feeling of insufficient breastmilk supply as reported by 52.1% of mothers, poor infant growth (15.9%), to reduce the efforts imposed on the mother (31.5%), lack of time for breastfeeding (22.3%), pediatrician advice (19.4%), advice from other health professionals (6.7%), and medical reasons related to the mother (7.2%).
In addition to milk, other foods were introduced into infants’ diets such as vegetables (14.9%), dairy products (17.4%), fruits (19.8%), rice (12%), and sweets (18.9%).
Factors that were significantly associated with exclusive breastfeeding included infant’s age, infant’s birth order, mode of delivery, analgesia used during delivery, and the timing of the first breastfeed after delivery (Table 1).
As the infant gets older breastfeeding rate declined and formula feeding increased, p = 0.016. In addition, the second baby was significantly more likely than the first, the third or higher birth orders to be exclusively breastfed, p = 0.043.
Mothers who underwent elective CS were significantly less likely to breastfeed their infants exclusively compared to mothers with normal delivery or emergency CS, p = 0.02.
Only mothers who did not receive any analgesia during delivery were significantly more likely to exclusively breastfeed their infants, compared to mothers who received any kind of analgesia during delivery, p = 0.014.
Infants who had their first breastfeeding beyond the first 12 h of life were significantly less likely to be exclusively breastfed, p = 0.000.
Early initiation of breastfeeding (within the first hour after birth) was reported by 44.2% of mothers and was significantly associated with practicing skin-to-skin contact, not receiving any kind of analgesia during birth, and having a vaginal birth, p = 0.000 (Table 3).
Overall, mothers had a moderately positive attitude toward breastfeeding (mean 2.95, min. 1, max. 4, SD. 0.515), with no significant association between mothers’ attitude and the method of infant feeding, p = 0.194 (Table 1).
During antepartum or postpartum periods, less than half of mothers (45.8%) reported receiving education about the importance of breastfeeding, and only 38.2% received education about how to practice breastfeeding. Receiving education about the importance of breastfeeding and how to practice it had no significant association with the method of infant feeding, p = 0.528, and 0.866, respectively (Table 1).
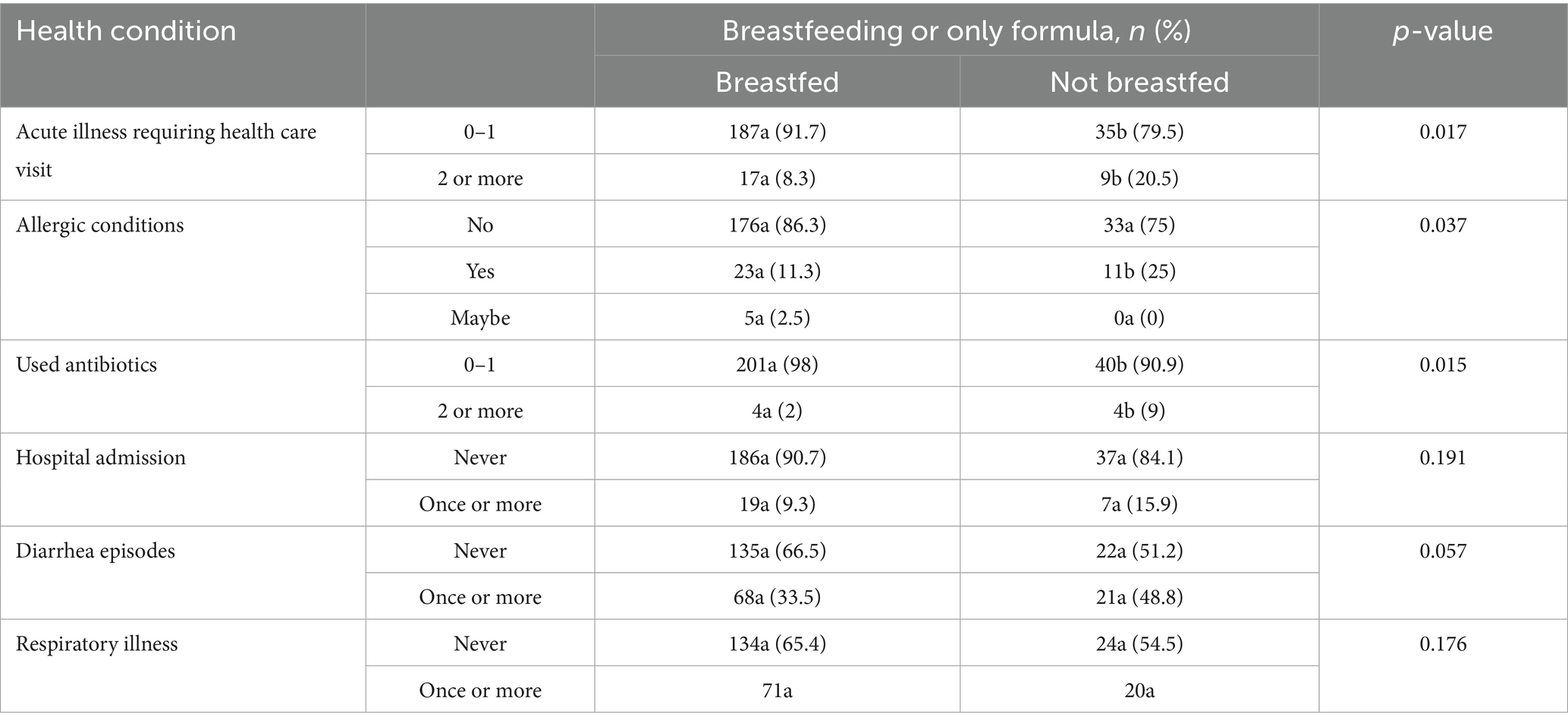
Breastfed infants compared to wholly formula-fed infants were significantly less likely to have acute illnesses requiring health care visits twice or more, to receive antibiotics twice or more in their life, and less likely to have allergic conditions, p = 0.017, 0.015, and 0.037, respectively (Table 4).
4 Discussion
In our sample, most families had a limited monthly income of 500 JDs or below, and nearly 60% reported insufficient income to meet daily needs. These socioeconomic challenges may impact access to healthcare, breastfeeding support, and nutritional resources, potentially influencing breastfeeding practices and infant health outcomes.
Globally, the prevalence of EBF among infants under 6 months of age has reached 48% (25), close to achieving the World Health Assembly 2025 target of 50% (11).
However, the rate of EBF in the Middle East and North Africa regions is still far below global trends. In 2019, the reported rate of EBF in these regions was 30.2% (26). Studies suggest that the drivers of these trends include the poor implementation of the Baby-Friendly Hospital Initiative and of the Code of Marketing of Breastmilk Substitutes, which allows formula companies to expand their markets (27), as well as the high prevalence of prelacteal feeds (mostly water-based), which negatively affect breastfeeding practices (28).
The situation in refugee camps mirrors the regional trends. A study performed in refugee camps in Algeria reported 33.3% exclusive or predominant breastfeeding among infants aged less than 6 months (29). This is comparable to what we found in our study; as only 38% of infants younger than 6 months were exclusively breastfed, with a small improvement to the prevalence that was reported by a similar study among long-standing Palestinian refugees in Jordan in 2017; as the prevalence was 34% (24), and even higher than what was reported among the general population in Jordan in 2017 also, where only 26% of infants younger than 6 months were exclusively breastfed (30). This higher prevalence of EBF compared to the general population could be influenced by several factors, including limited access to formula or other supplementary foods due to economic constraints among refugees, and community health initiatives within refugee camps promoting and supporting breastfeeding as a cost-effective and health-protective practice. In addition, the improvement in social and financial status has paradoxically been associated with a decline in the rate of EBF in certain cultural contexts (31).
In this study, most mothers practiced breastfeeding upon infant demand (77.6%) and reported indicators of adequate feeding, such as satiety (95.1%), suggesting a general understanding of infant hunger and satiety cues among breastfeeding mothers.
4.1 Exclusive breastfeeding influencing factors
The EBF was significantly associated with the infant’s age, birth order, mode of delivery, analgesia used during delivery, and the timing of the first breastfeed after delivery.
4.2 Infant’s age and birth order
EBF declined sharply from 40% in infants less than 4 weeks old to 35.1% by 4–6 months. This trend aligns with global findings where breastfeeding rates often decline as infants age, largely due to the introduction of formula and other foods. This is despite the EBF recommendations for the first 6 months of life by the World Health Organization (WHO) and other health organizations worldwide (2). Perceived insufficient milk supply (52.1%) was the most common reason for introducing formula, highlighting the need for support and education to address this concern, which was also reported in the literature as the major reason for early introduction of solid foods (32).
Several studies suggest children with earlier birth orders are more likely to be breastfed (33, 34). In our results, the second baby was more likely to be exclusively breastfed which may be attributed to previous experience, as breastfeeding self-efficacy was linked in the literature with prior experience (35–37). First-time mothers often perceive more breastfeeding obstacles (35, 36) and report lower self-efficacy during breastfeeding. On the other hand, with increasing birth orders, mothers experience more distractions when feeding their infants. This is supported by a study that included multiparous mothers (38), as well as another study that found a statistically significant higher percentage of EBF continuation when distractions were reduced (39). These reports may explain, in part, our finding that the second baby was more likely to be exclusively breastfed compared to subsequent babies.
4.3 Labor method and analgesia use
Mothers who did not receive any kind of analgesia during labor were found more likely to be exclusively breastfeeding. Neuraxial analgesia during labor has been associated with less likelihood of breastfeeding postpartum and thereafter, as reported in the literature (40, 41).
Intramuscular meperidine and morphine are commonly used for labor analgesia. However, Intrapartum pethidine administration may have a detrimental effect on neonatal behavior, reducing infant alertness, suppressing the rooting and sucking reflex, and may shorten breastfeeding duration as well (42).
Also, cesarean birth is associated with decreased breastfeeding initiation and continuation globally (43, 44). The lower rate of breastfeeding initiation and increased difficulties with breastfeeding in women with cesarean section (CS) deliveries may be attributed to a disruption of the hormonal pathway that stimulates lactogenesis (45).
In our findings, mothers who underwent elective CS were significantly less likely to breastfeed their infants exclusively compared to mothers with normal delivery or emergency CS. Similar findings have been reported in the literature; planned c-sections negatively affect breastfeeding initiation and continuation (46, 47), which may be attributed to the timing of planned cesarean sections, which typically occur before the onset of labor, further disrupting the process of lactogenesis.
One contributing factor to the rising number of CS is maternal request, as documented in the literature (48, 49). Encouraging natural birthing practices, minimizing unnecessary interventions, reducing the number of non-medically indicated CS, and developing targeted strategies for women planning cesarean deliveries, starting from the perinatal period and extending into postpartum, could foster the initiation and continuation of breastfeeding.
4.4 Early initiation of breastfeeding
The World Health Organization (WHO) recommends early, and uninterrupted skin-to-skin contact between mothers and infants as soon as possible after birth, along with early initiation of breastfeeding (EIBF), within 1 h of birth (50). These practices have been shown to reduce newborn mortality (51) and positively impact the prevalence and duration of exclusive breastfeeding (52, 53). However, achieving this goal can be challenging due to several factors such as maternal pain after CS delivery, exhaustion, suboptimal hospital environment, and insufficient breastfeeding support.
Research also highlights the association between EIBF (within 24 h of birth) and reduced risks of all-cause neonatal mortality among all live births (54). Despite these benefits, global estimates suggest that fewer than half (42%) of all newborns are breastfed within the first hour of birth (55). Reasons for breastfeeding delays included extended recovery time from spinal anesthesia, maternal fatigue, and uncomfortable breastfeeding position due to post-cesarean pain (56).
In our sample, EIBF was reported by less than half of the mothers (44.2%), a figure consistent with findings from studies conducted in India (56, 57). It was significantly associated with practicing skin-to-skin contact, vaginal delivery, and the absence of analgesia during delivery. Moreover, infants who began breastfeeding more than 12 h after birth were significantly less likely to be exclusively breastfed. These findings emphasize the critical window for breastfeeding initiation and underscore the importance of hospital practices and birth interventions in promoting successful breastfeeding initiation and continuation.
4.5 Breastfeeding impact on infant health
Our findings revealed that infants fed on breast milk, whether exclusively or partially, were significantly less likely to experience allergic conditions, to have acute illnesses requiring health care visits, and to receive antibiotics compared to formula-fed infants. These findings reaffirm the protective effects of breastfeeding against infections and allergies, consistent with the established benefits of human milk (7, 58).
4.6 Maternal education and attitudes regarding breastfeeding
Step 3 of the Baby Friendly Hospital Initiative (BFHI) underscores the need for all pregnant women to be informed about the benefits and techniques of breastfeeding (50). Evidence suggests that comprehensive breastfeeding counseling and support during the prenatal and postpartum periods can significantly improve breastfeeding outcomes (59). Despite that, our data show that less than half of mothers in our sample have received education during antepartum or postpartum periods, about the importance of breastfeeding. Additionally, only 38.2% received education about how to practice breastfeeding. Limited breastfeeding education in this population may reflect resource constraints, healthcare access issues, or gaps in breastfeeding support within the community. Increasing breastfeeding education in these settings could improve the rates of exclusive breastfeeding and better infant health outcomes.
Despite moderately positive maternal attitudes toward breastfeeding, no significant association was found between maternal attitude and infant feeding method. This indicates that external factors, such as healthcare support and socioeconomic constraints, may play a larger role in influencing feeding practices than maternal preferences alone.
4.7 Limitations
Data collection relied on self-reported information from mothers, which may be subject to recall bias. In addition, future longitudinal studies could better identify causal relationships between predictors and breastfeeding outcomes. The representativeness of the sample is also a potential limitation, as the sample was recruited from a single UNRWA health center, which may not fully represent the broader population of Palestinian refugees in Jordan or other refugee settings, and the total number of participants was limited because of the tight time frame of the study. Future studies should include larger and more diverse samples to improve generalizability.
5 Conclusion
The findings underline the need for comprehensive strategies to promote breastfeeding in these vulnerable situations, including early initiation, addressing concerns about milk insufficiency, supporting natural delivery practices, and improving breastfeeding education during antenatal and postnatal care. Interventions should also consider socioeconomic barriers and cultural factors influencing feeding practices. In addition, EBF indicators should be adopted as part of routine follow-up and quality assurance mechanisms in primary care centers serving refugee populations. This would help translate research into action, enabling health workers to identify at-risk mothers early, offer targeted support, and continuously improve care quality based on real-time data. Future research should explore in-depth the interplay between individual, familial, and systemic factors influencing EBF practices in similar settings globally.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board Committee of Hashemite University on October 31, 2022 the Research Review Board Committee of the UNRWA on April 20, 2023. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
NQ: Conceptualization, Methodology, Supervision, Writing – review & editing, Formal analysis, Writing – original draft. AA-S: Writing – review & editing, Resources, Methodology. DA-K: Conceptualization, Methodology, Writing – original draft, Data curation. SJ: Methodology, Conceptualization, Data curation, Writing – review & editing. JA: Conceptualization, Methodology, Writing – review & editing, Data curation. LS: Methodology, Data curation, Conceptualization, Writing – review & editing. LA: Data curation, Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Special thanks to UNRWA and the UNRWA Zarqa camp health center for their collaboration and support in facilitating data collection. Sincere thanks also to Faten Tamim, Ph.D, IBCLC for her valuable efforts in reviewing the questionnaire.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lessen, R, and Kavanagh, K. Position of the academy of nutrition and dietetics: promoting and supporting breastfeeding. J Acad Nutr Diet. (2015) 115:444–9. doi: 10.1016/j.jand.2014.12.014
2. Meek, JY, and Noble, L. Policy statement: breastfeeding and the use of human Milk. Pediatrics. (2022) 150:7988. doi: 10.1542/peds.2022-057988
3. Sustainable Development Goals | United Nations development Programme [internet]. [cited 2024 Dec 3]. Available online at: https://www.undp.org/sustainable-development-goals
4. United Nations Department for General Assembly and Conference Management. Sustainable development high-level political forum on sustainable development, convened under the auspices of the economic and social council Progress towards the sustainable development goals. United Nations, New York. (2023).
5. United Nations Inter-Agency Group for Child Mortality Estimation [UNIGME]. Levels and trends in child mortality: Report 2023. New York; (2024).
6. Oddy, WH. Breastfeeding in the first hour of life protects against neonatal mortality. J Pediatr. (2013) 89:109–11. doi: 10.1016/j.jped.2013.03.012
7. Mohamed Ahmed, SO, Ashgar, RI, Mohammed Abdelgader, AA, Abdalla Hamid, HI, Mathkor, DM, Abdelsadig Ali, MA, et al. Exclusive breastfeeding: impact on infant health. Clinical Nutrition Open Science. (2023) 51:44–51. doi: 10.1016/j.nutos.2023.08.003
8. Kim, KM, and Choi, JW. Associations between breastfeeding and cognitive function in children from early childhood to school age: a prospective birth cohort study. Int Breastfeed J [Internet]. (2020) 15:1–9. doi: 10.1186/s13006-020-00326-4
9. El-Asheer, OM, Darwish, MM, Abdullah, AM, and Mohamad, HA. Complementary feeding pattern and its impact on growth and development of under 2-years infants in upper Egypt. Egypt Pediatr Assoc Gazette. (2021) 69:1–6. doi: 10.1186/s43054-021-00061-3
10. Victora, CG, Bahl, R, Barros, AJD, França, GVA, Horton, S, Krasevec, J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 387:475–90. doi: 10.1016/S0140-6736(15)01024-7
11. World Health Organization. Comprehensive implementation plan on maternal. Geneva: Infant and Young Child Nutrition (2014).
13. Maonga, AR, Mahande, MJ, Damian, DJ, and Msuya, SE. Factors affecting exclusive breastfeeding among women in Muheza District Tanga northeastern Tanzania: a mixed method community based study. Matern Child Health J. (2016) 20:77–87. doi: 10.1007/s10995-015-1805-z
14. Babakazo, P, Donnen, P, Akilimali, P, Ali, NMM, and Okitolonda, E. Predictors of discontinuing exclusive breastfeeding before six months among mothers in Kinshasa: a prospective study. Int Breastfeed J. (2015) 10:19. doi: 10.1186/s13006-015-0044-7
15. Suresh, S, Sharma, KK, Saksena, M, Thukral, A, Agarwal, R, and Vatsa, M. Predictors of breastfeeding problems in the first postnatal week and its effect on exclusive breastfeeding rate at six months: experience in a tertiary care Centre in northern India. Indian J Public Health. (2014) 58:270–3. doi: 10.4103/0019-557X.146292
16. Khanal, V, Lee, AH, Karkee, R, and Binns, CW. Postpartum breastfeeding promotion and duration of exclusive breastfeeding in Western Nepal. Birth. (2015) 42:329–36. doi: 10.1111/birt.12184
17. UNHCR. Infant and young child feeding practices: standard operating procedures for the handling of breastmilk substitutes (BMS) in refugee situations for children 0-23 months | UNHCR. (2015). Available online at: https://www.unhcr.org/media/infant-and-young-child-feeding-practices-standard-operating-procedures-handling-breastmilk-0
18. Wallace, M, Hiam, L, and Aldridge, R. Elevated mortality among the second-generation (children of migrants) in Europe: what is going wrong? A review. Brit Med Bull. (2023) 148:5–21. doi: 10.1093/bmb/ldad027
19. United Nations High Commissioner for Refugees. Global Trends: Forced Displacement in 2023. Copenhagen, Denmark: United Nations High Commissioner for Refugees. (2024).
20. Jordan | UNHCR [Internet]. [cited 2024 Dec 3]. Available online at: https://www.unhcr.org/countries/jordan (Accessed December 3, 2024).
21. Tiltnes, ÅA, and Zhang, H. Progress, challenges, diversity insights into the socio-economic conditions of Palestinian refugees in Jordan [internet]. Fafo Report, editor Norway; (2013). Available online at: www.fafo.no/english/ (Accessed December 3, 2024).
22. Rollins, NC, Bhandari, N, Hajeebhoy, N, Horton, S, Lutter, CK, Martines, JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. (2016) 387:491–504. doi: 10.1016/S0140-6736(15)01044-2
23. Daniel, WW. Biostatistics: a foundation for analysis in the health sciences. (1999). 7th Edition, Hoboken: John Wiley & Sons, Inc.
24. Takai, K, Kamiya, Y, Hababeh, M, Khader, A, Kitamura, A, Zeidan, W, et al. Prevalence of exclusive breastfeeding and associated factors among refugees from Palestine in Jordan: a cross-sectional study. Lancet. (2019) 393:S51. doi: 10.1016/S0140-6736(19)30637-3
25. UNICEF, World Health Organization. Global breastfeeding scorecard 2023 rates of breastfeeding increase around the world through improved protection and support. Geneva, Switzerland: World Health Organization. (2023).
26. Neves, PAR, Vaz, JS, Maia, FS, Baker, P, Gatica-Domínguez, G, Piwoz, E, et al. Rates and time trends in the consumption of breastmilk, formula, and animal milk by children younger than 2 years from 2000 to 2019: analysis of 113 countries. Lancet Child Adolesc Health [Internet]. (2021) 5:619. doi: 10.1016/S2352-4642(21)00163-2
27. Baker, P, Santos, T, Neves, PA, Machado, P, Smith, J, Piwoz, E, et al. First-food systems transformations and the ultra-processing of infant and young child diets: the determinants, dynamics and consequences of the global rise in commercial milk formula consumption. Matern Child Nutr. (2021) 17:97. doi: 10.1111/mcn.13097
28. Al-Jawaldeh, A. Trends in infant feeding in countries of the eastern Mediterranean region 1995 to 2020: time for action [internet]. 2020 [cited 2024 Dec 17]. Available online at: https://www.academia.edu/97432404/Trends_in_Infant_Feeding_in_Countries_of_the_Eastern_Mediterranean_region_1995_to_2020_Time_for_action (Accessed December 17, 2024).
29. Aakre, I, Lilleengen, AM, Lerseth Aarsand, M, Strand, TA, Barikmo, I, and Henjum, S. Infant feeding practices in the Saharawi refugee camps Algeria, a cross-sectional study among children from birth to six months of age. Int Breastfeed J. (2017) 12:1–10. doi: 10.1186/s13006-016-0098-1
30. Department of Statistics [Jordan], ICF. Jordan population and family health survey 2017-2018 [internet]. Amman-Jordan; (2019). Available online at: www.DHSprogram.com (Accessed December 17, 2024).
31. Ryan, AS, Zhou, W, and Arensberg, MB. The effect of employment status on breastfeeding in the United States. Womens Health Issues. (2006) 16:243–51. doi: 10.1016/j.whi.2006.08.001
32. Ricci, C, Otterman, V, Bennett, TL, Metcalfe, S, Darling, E, Semenic, S, et al. Rates of and factors associated with exclusive and any breastfeeding at six months in Canada: an analysis of population-based cross-sectional data. BMC Pregnancy Childbirth. (2023) 23:56–11. doi: 10.1186/s12884-023-05382-2
33. Buckles, K, and Kolka, S. Prenatal investments, breastfeeding, and birth order. Soc Sci Med. (2014) 118:66–70. doi: 10.1016/j.socscimed.2014.07.055
34. Der, G, Batty, GD, and Deary, IJ. Effect of breast feeding on intelligence in children: prospective study, sibling pairs analysis, and meta-analysis. BMJ. (2006) 333:945–8. doi: 10.1136/bmj.38978.699583.55
35. Kronborg, H, and Væth, M. The influence of psychosocial factors on the duration of breastfeeding. Scand J Public Health. (2004) 32:210–6. doi: 10.1080/14034940310019218
36. Yang, X, Gao, L-L, Ip, W-Y, and WCS, C. Predictors of breast feeding self-efficacy in the immediate postpartum period: a cross-sectional study. Midwifery [Internet]. (2016) 41:1–8. doi: 10.1016/j.midw.2016.07.011
37. Sutherland, T, Pierce, CB, Blomquist, JL, and Handa, VL. Breastfeeding practices among first-time mothers and across multiple pregnancies. Matern Child Health J. (2012) 16:1665–71. doi: 10.1007/s10995-011-0866-x
38. Golen, RB, and Ventura, AK. Mindless feeding. Is maternal distraction during bottle-feeding associated with overfeeding? Appetite. (2015) 91:385–92. doi: 10.1016/j.appet.2015.04.078
39. Arezi, E, Maleki, A, and Jafari, E. Investigating the influence of family-oriented counselling on breastfeeding continuity in mothers experiencing distractions: a randomized controlled trial. Heliyon. (2024) 10:e30687. doi: 10.1016/j.heliyon.2024.e30687
40. Wetzl, RG, Delfino, E, Peano, L, Gogna, D, Vidi, Y, Vielmi, F, et al. A priori choice of neuraxial labour analgesia and breastfeeding initiation success: a community-based cohort study in an Italian baby-friendly hospital. BMJ Open. (2019) 9:e025179. doi: 10.1136/bmjopen-2018-025179
41. Orbach-Zinger, S, Landau, R, Davis, A, Oved, O, Caspi, L, Fireman, S, et al. The effect of labor epidural analgesia on breastfeeding outcomes: a prospective observational cohort study in a mixed-parity cohort. Anesth Analg. (2019) 129:784–91. doi: 10.1213/ANE.0000000000003442
42. Burchell, T, Coster, S, and Norman, I. The effect of intrapartum pethidine on breastfeeding: a scoping review. Evid Based Midwifery. (2016) 14:49–56.
43. Wiklund, I, Edman, G, and Andolf, E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. (2007) 86:451–6. doi: 10.1080/00016340701217913
44. Zanardo, V, Svegliado, G, Cavallin, F, Giustardi, A, Cosmi, E, Litta, P, et al. Elective cesarean delivery: does it have a negative effect on breastfeeding? Birth. (2010) 37:275–9. doi: 10.1111/j.1523-536X.2010.00421.x
45. Scott, JA, and Binns, CW. Oddy WH. Predictors of delayed onset of lactation. Matern Child Nutr. (2007) 3:186–93. doi: 10.1111/j.1740-8709.2007.00096.x
46. Hobbs, AJ, Mannion, CA, McDonald, SW, Brockway, M, and Tough, SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. (2016) 16:1–9. doi: 10.1186/s12884-016-0876-1
47. Li, L, Wan, W, and Zhu, C. Breastfeeding after a cesarean section: a literature review. Midwifery. (2021) 103:103117. doi: 10.1016/j.midw.2021.103117
48. Chien, P. Global rising rates of caesarean sections. BJOG. (2021) 128:781–2. doi: 10.1111/1471-0528.16666
49. Jenabi, E, Khazaei, S, Bashirian, S, Aghababaei, S, and Matinnia, N. Reasons for elective cesarean section on maternal request: a systematic review. J Matern Fetal Neonatal Med. (2020) 33:3867–72. doi: 10.1080/14767058.2019.1587407
50. WHO, UNICEF. Implementation guidance: protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative 2018. World Health Organization and United Nations Children’s Fund Geneva; (2018). Available online at: https://www.who.int/publications/i/item/9789241513807 (Accessed December 3, 2024).
51. Shane, AL, Sánchez, PJ, and Stoll, BJ. Neonatal sepsis. Lancet. (2017) 390:1770–80. doi: 10.1016/S0140-6736(17)31002-4
52. Mikiel-Kostyra, K, Mazur, J, and Bołtruszko, I. Effect of early skin-to-skin contact after delivery on duration of breastfeeding: a prospective cohort study. Acta Paediatr [Internet]. (2002) 91:1301–6. doi: 10.1111/j.1651-2227.2002.tb02824.x
53. Giang, HTN, Duy, DTT, Vuong, NL, Ngoc, NTT, Pham, TT, Tuan, LQ, et al. Prevalence of early skin-to-skin contact and its impact on exclusive breastfeeding during the maternity hospitalization. BMC Pediatr. (2022) 22:395. doi: 10.1186/s12887-022-03455-3
54. Debes, AK, Kohli, A, Walker, N, Edmond, K, and Mullany, LC. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health. (2013) 13:S19. doi: 10.1186/1471-2458-13-S3-S19
55. WHO. Health in 2015: from MDGs, millennium development goals to SDGs, sustainable development goals [internet]. GENEVA; (2015) Available online at: https://iris.who.int/handle/10665/200009 (Accessed December 3, 2024).
56. Mary, JJF, Sindhuri, R, Kumaran, AA, and Dongre, AR. Early initiation of breastfeeding and factors associated with its delay among mothers at discharge from a single hospital. Clin Exp Pediatr. (2022) 65:201–8. doi: 10.3345/cep.2021.00129
57. Ahmed, AE, and Salih, OA. Determinants of the early initiation of breastfeeding in the Kingdom of Saudi Arabia. Int Breastfeed J. (2019) 14:1–13. doi: 10.1186/s13006-019-0207-z
58. Lamberti, LM, Fischer Walker, CL, Noiman, A, Victora, C, and Black, RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. (2011) 11:1–12. doi: 10.1186/1471-2458-11-S3-S15
Keywords: exclusive breastfeeding, infant feeding practices, Palestinian refugees, maternal health, breastfeeding determinants, refugee health
Citation: Qasem N, Al-Shdaifat A, Abu-Khader D, Jaraa S, AlOthman J, Shatat L and Alsaif L (2025) Breastfeeding practices among long-standing refugees in Jordan: insights from a cross-sectional study. Front. Public Health. 13:1644659. doi: 10.3389/fpubh.2025.1644659
Edited by:
Raymond Akawire Aborigo, Navrongo Health Research Centre, GhanaCopyright © 2025 Qasem, Al-Shdaifat, Abu-Khader, Jaraa, AlOthman, Shatat and Alsaif. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nuha Qasem, bnVoYXFhc2VtQGh1LmVkdS5qbw==
 Nuha Qasem
Nuha Qasem Amjad Al-Shdaifat
Amjad Al-Shdaifat Deema Abu-Khader
Deema Abu-Khader Sajeda Jaraa
Sajeda Jaraa Jelan AlOthman
Jelan AlOthman Lina Shatat
Lina Shatat Lara Alsaif
Lara Alsaif