- 1Department of Health Sciences, University of York, Heslington, United Kingdom
- 2Nottingham Clinical Trials Unit, University of Nottingham, Nottingham, United Kingdom
- 3Department of Life Sciences, University of Lincoln, Lincoln, United Kingdom
- 4Dogs for Good, The Frances Hay Centre, Banbury, United Kingdom
- 5Foss Park Hospital, Tees, Esk and Wear Valleys NHS Foundation Trust, York, United Kingdom
Introduction: In England, dog-assisted interventions (DAIs) are increasingly used to support the health and wellbeing of individuals with mental and physical health conditions. Although research in this area is increasing, little is known about the national prevalence and characteristics of DAIs in practice. Advancing knowledge is important to inform development of research, policy and practice in the field.
Methods: An online survey of DAI providers in England was conducted to collect data on DAI service provision, including target populations, session content and structure, implementation challenges, and best practices in dog selection, training, and welfare monitoring.
Results: Of 72 invitations sent to DAI organizations and therapists, 31 participants completed the survey (response rate: 41.3%). DAIs were primarily used to support individuals with mental health and neurodevelopmental conditions (e.g., anxiety, depression, autism) across the National Health Service (80.6%), private healthcare (61.3%), and educational settings (41.9%). Respondents estimated delivering DAIs across 7,679 institutions. Interventions included structured therapeutic sessions (61.3%) and spontaneous activities (51.6%), mostly delivered individually (90.5%) rather than to groups. Over half reported delivering dog-assisted therapy, but 38.7% were unsure whether sessions had individualized goals. Session frequency and duration varied; most lasted 31–60 min (54.8%) and occurred weekly (45.2%). Key challenges included limited access to delivery spaces (35.5%), infection control concerns (32.3%), and difficulties “matching” dogs to service users (22.6%). Dog selection relied on temperament assessments (100%). While 54.8% of handlers received formal training, content varied. Some were trained in dog body language and risk assessment; others were not. Welfare monitoring primarily depended on handler observation (90.3%) and access to basic resources such as water.
Discussion: DAIs are now implemented in thousands of health, care and educational settings across England, serving diverse clinical populations of all ages, especially those with mental health and neurodevelopmental conditions. Interventions range from structured, goal-oriented sessions (e.g., supporting mental, emotional, or physical health) to spontaneous interactions (e.g., community programmes, social events, recreational activities). Participant responses highlight substantial variation in DAI characteristics and delivery. These findings underscore the clear need for standardized good practice guidelines encompassing aspects related to outcome reporting, dog selection and welfare monitoring, and provider training.
Introduction
In England and many other countries worldwide, demand, provision and research of animal-assisted interventions (AAIs) to improve human health and wellbeing has been rapidly growing (1–7). Although a variety of species (e.g., dogs, horses, small mammals, farm animals) are involved in AAI research and practice, dog-assisted interventions (DAIs) are currently the most commonly provided and researched type of AAI (8). DAIs can include dog-assisted therapy (DAT), which is goal-orientated, structured and delivered by certified therapists (7, 9, 10), whereas dog-assisted activities (DAAs) are typically based on spontaneous interaction and do not have documented, defined outcomes (7, 10).
Despite the expanding interest and research activity surrounding DAIs, there remains a limited understanding of the prevalence, nature, and characteristics of DAI provision within England. While health and safety guidelines for implementing DAIs have been developed across multiple sectors (e.g., healthcare, education, voluntary organizations) (11, 12), the overall provision of DAIs remain largely unregulated (13). Moreover, there is an absence of uniformly accepted standards, procedures, or policies to govern the delivery of these interventions, leading to considerable variability in practice (14, 15). While surveys reporting on real-life practices of AAIs have been conducted in the United States (14, 15), no comparable studies, except one focusing on AAIs in intensive care units (16), have been undertaken in England.
Understanding current practices and standards of DAI provision is critical not only for effective implementation and the safe and ethical delivery of these interventions, but also for enhancing the quality and transparency of research in this field. While a growing body of literature demonstrates the potential benefits of DAIs across diverse clinical populations and age groups (17–23), the extent to which these findings reflect real-world practice remains unclear. Little is known about how DAIs are implemented in a real-world context, including session content and structure, how dog-handler teams are selected and trained, and adherence to existing guidelines (7). This disconnect may suggest that a discrepancy exists between the controlled environments of research and the realities of service provision, highlighting the need for data on real-world practices.
Understanding more about the landscape of DAI provision in England will also facilitate international comparisons and the exchange of best practices, ensuring a more cohesive and informed approach to intervention development and evaluation. Therefore, the aim of the reported study was to undertake a survey of DAI service provision and practice in England.
Methods
Study design
A cross-sectional online survey was distributed to DAI providers in England.
Recruitment and procedures
The survey was released in Qualtrics survey software (Qualtrics, Provo, UT, USA). Organizations specializing in the provision of DAIs in England (e.g., Dogs for Good, Pets as Therapy) were identified based on the researchers' multi-sector networks and extensive internet searches. These searches were conducted using Google with combinations of key terms such as “dog-assisted therapy,” “dog-assisted activity,” and “animal-assisted interventions” and restricted to results in England. We also manually reviewed directories and public listings of third-sector and healthcare organizations known to deliver or promote DAIs. Additionally, the British Association for Counseling and Psychotherapy Therapist Directory was searched to identify therapists with registered expertise in delivering DAIs. Personalized email invitations were sent to organizations and therapists, with up to two follow-up reminders. For organizations, only one participant was permitted to complete the survey on behalf of each organization to avoid duplication. Participants were asked to self-nominate or be nominated by their organization as the most appropriate person to complete the survey based on their familiarity with DAI delivery practices. To be eligible to participate, participants were required to be affiliated with an organization delivering DAIs in England, rather than those involved in the placement of assistance dogs.
Prospective participants were invited to follow a link to the survey where they were presented with a Participant Information Sheet (PIS) and consent form. Consent to participate was indicated by ticking an online check box. The PIS described a survey incentive being offered (opportunity to enter a prize draw with three participants randomly selected to win shopping vouchers). Screening questions required participants to confirm their involvement in DAI delivery and residence in England. All data were stored on the Qualtrics server of the University of York.
The survey opened for recruitment on September 2nd, 2024, and closed on January 13th, 2025. Approval for this research was granted by the Health Sciences Research Ethics Committee at the University of York, UK, on 29th September 2023 (Ref: HSRGC/2023/586/E).
Measures
A bespoke survey was developed to enable collection of data most relevant to understanding the types and characteristics of DAI service provision in England. It was piloted by an expert group comprising a multi-disciplinary team of academics (n = 7), third sector animal welfare organizations (n = 3), and DAI providers (n = 3). Based on comprehensive feedback, a number of reinfements were made to the survey, including the addition of pre-determined response options, revisions to the definitions of dog-assisted therapy and activities to improve clarity, and adjustments to the survey logic to enhance flow and usability. The revised version was subsequently reviewed and piloted again to ensure that changes had been implemented as intended. Questionnaire items are summarized below; the full instrument is presented in Supplementary material 1.
Demographic data
Demographic information was gathered about participants' age (in ranges), gender (male/female/non-binary), their primary role/position within their organization (e.g., professional/paid animal handler, director, volunteer, occupational therapist, clinician, teacher, social worker), and number of years' experience of providing DAIs.
Organizational information
Information was gathered about the respondent's affiliated DAI organization. If the participant worked at more than one organization, they were asked to answer questions with their primary DAI-providing organization in mind. Information was collected on organization type (e.g., third sector/charity organization, local authority/council, NHS organization, private hospital, residential care and nursing home, hospice, school, nursery or pre-school); the number of paid and volunteer dog handlers registered at the organization, and not-for-profit status (yes/no).
DAI settings and target populations
Information was collected regarding the settings in which organizations currently delivered DAIs. Options included NHS mental health settings (e.g., adult mental health services, older people's mental health services, child and adolescent mental health services); NHS physical health settings (e.g., GP practices, outpatient clinics, inpatient wards, intensive care units); non-NHS health and care settings (e.g., hospices, care/nursing homes), and educational settings (e.g., nurseries, pre-schools, schools, universities). Participants were asked to provide the approximate number of settings or institutions in which their organization currently provided DAIs, and, if known, to provide this number.
Participants were also asked to identify the target populations to whom DAIs were delivered. Response options included adults and/or children and young people with physical health conditions; adults with mental health and neurodevelopmental conditions [e.g., anxiety, depression, schizophrenia, post-traumatic stress disorder, autism, eating disorders, attention-deficit/hyperactivity disorder (ADHD), intellectual disabilities]; children with mental health and neurodevelopmental conditions (e.g., anxiety, depression, emerging behavioral problems, autism, ADHD, eating disorders, trauma, attachment-related difficulties, intellectual disabilities); and adults with neurodegenerative conditions (e.g., dementia).
DAI types, frequency, duration, and session structure
Based on a brief list of definitions provided within the survey, participants were asked to identify what kind of DAIs their organization provided: dog-assisted therapy (i.e., goal-directed, documented, therapeutic intervention as part of a treatment plan, delivered by specialist-trained dog-handler teams), dog-assisted activities (i.e., activities focused on spontaneous interactions that can be delivered by volunteers and untrained dogs), both, or other. Dog-assisted therapy was defined as goal-directed interactions with dogs, led by trained professionals, and dog-assisted activities were defined as spontaneous interactions with dogs, often led by volunteers. If participants indicated their organization delivered dog-assisted therapy, they were asked to specify whether these sessions had clear individualized goals for the service user. We do acknowledge the recent suggestion of the new terminology [animal-assisted services; AASs (24)] within the survey (see Supplementary material 1). However, items were developed in collaboration with our expert group, who advised the new terminology may not yet be nationally recognized in the UK and so may confuse respondents. Therefore, we opted to use the original terminology in the context of this survey.
Participants were also asked to indicate whether DAIs are typically delivered on an individual basis or in group settings (e.g., with peers and/or family members). Additional information was collected regarding the frequency of DAI delivery (e.g., multiple times per week, once per week, more than once every 2 weeks but less than weekly, every 2 weeks, or varying by service user); the typical duration over which DAIs were provided (in weeks), and the usual length of individual sessions (e.g., 30 min or less, 31 min to 1 hour, more than 1 h but < 2, 2 h or more).
Dog-handler team training
Handler training
Participants were asked whether handlers within their organization received formal training (yes/no), and if so, to indicate the training received among nine pre-specified options, or to specify it themselves. The pre-specified training options included: “service user wellbeing/safety”; “dog wellbeing/safety”; “dog obedience/skill training”; “risk assessment and awareness”; “human-dog bond” (e.g., exercises to build mutual trust and responsiveness between the dog and handler, such as eye contact games or joint play activities); “dog body language”; “general mental health”; “condition/diagnosis-specific training,” and “safeguarding.”
Handler confidence
Participants were then asked to indicate their confidence level within their role, using a ten-point Likert scale (1 = not at all confident; 10 = very confident). An option was included for participants to leave an open-ended, free-text comment to share further information on their confidence level within their role.
Dog training
Participants were asked to indicate what training a dog receives prior to working, selecting from six pre-specified options, or to specify themselves. The pre-specified options included: “obedience training (e.g., leadwork, sit, down)”; “handling training (e.g., to be stroked/touched by strangers); greeting training (e.g., to greet people calmly)”; “human-dog bond”; “trick training,” or “socialization training in environments likely to work in.”
Dog characteristics, selection and welfare
Dog characteristics
Participants were asked to indicate what type of dogs are typically involved in the DAIs using Kennel Club groups (25), the youngest age a dog may start working, and the oldest age a dog will normally work until.
Dog selection
Participants were asked to specify how a dog is selected for work, selecting from the following options: “temperament/behavior assessment”; “pass obedience test [e.g., Kennel Club test (26)]”; “health status (pass veterinary assessment)”; “specific characteristics (e.g., size, color, breed, age),” or for the participant to specify their own reason.
Information was collected about whether the dogs needed to have any health checks passed prior to their involvement in DAIs (yes/no), and if so, to indicate the health checks among six pre-specified options, or to specify it themselves. The pre-specified health check options included: “annual vaccinations”; “regular worming programme”; “not currently receiving any veterinary-prescribed medication”; “no current health issues that have prohibited the issuing of veterinary sign off”; “regular grooming schedule,” and “not on a raw food diet.”
Dog welfare
Information was gathered regarding how many handlers, on average, the dogs work with; how frequently a dog is involved in the DAI (daily, a few days a week, weekly, less than once a week), and whether there is a maximum number of hours a dog can work per week (yes/no). Participants were also asked to indicate whether strategies are in place to ensure the dog's welfare is monitored, and if so, to indicate the strategies among five pre-specified options, or to specify it themselves. The pre-specified options included: “handler observation”; “veterinary observation”; “using checklists or other written materials”; “access to water,” and “access to a place the dog can choose to go by themselves.”
Participants were also asked whether a formal process was in place for reporting incidents of inappropriate dog behavior or injuries to either human participants or the dog (yes/no).
Barriers and facilitators to DAI provision
Participants were asked whether they experienced barriers when delivering DAIs, and if so, to indicate the reason among seven pre-specified options, or to specify it themselves. The pre-specified barriers included: “controlling potential risk factors and infection prevention control”; “access to appropriate space for delivery”; “challenges related to monitoring dog welfare”; “challenges related to matching dogs to service users”; “working with other professions”; “lack of appropriate skills/training for dog,” and “challenges related to access to appropriate training for handler.” A free-text, open-ended box was provided for participants to identify the most important facilitators for successful implementation.
Data analysis
Data were analyzed in SPSS v29.0 (IBM SPSS Inc., Chicago, USA) (27) and descriptive summary statistics are presented for demographic variables and data relating to the nature and characteristics of DAI provision, settings and target populations, session structure, dog-handler team training, dog characteristics, selection and welfare, and implementation barriers and facilitators. Categorical variables were analyzed using frequencies and percentages, while continuous variables were analyzed using means, standard deviations, and ranges. Free-text response content was analyzed descriptively to identify common themes and frequently mentioned issues across participants.
Results
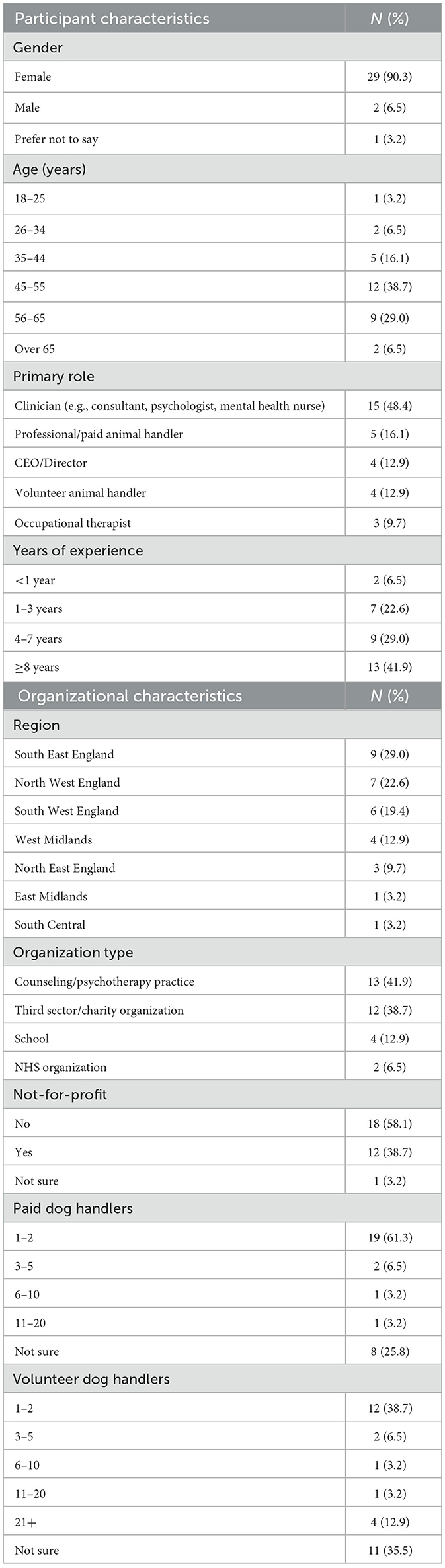
Of the 72 invitations sent to DAI organizations (n = 44) and therapists (n = 28), 40 individuals accessed the survey link. Two respondents were excluded due to ineligibility, as they were based outside of England, resulting in 38 eligible participants who consented to participate in the survey. Of these, six were excluded from analysis for not completing the survey beyond the initial screening questions. Additionally, one response was identified as a duplicate, as two members of the same organization completed the survey. Therefore, the final sample comprised 31 participants, all of whom completed the questionnaire in full, with no missing data (response rate = 43.1%). A summary of participant and organizational characteristics is presented in Table 1.
DAI settings and target populations
Most participants reported that their organizations delivered DAIs in non-NHS health and care settings (n = 25; 80.6%), followed by educational settings (n = 13; 41.9%), NHS mental health services (n = 10; 32.3%), and NHS physical health services (n = 9; 29.0%). NHS settings refer to services provided within the publicly funded National Health Service, whereas non-NHS settings operate outside this system, often under private or third-sector provision.
With non-NHS settings, DAIs were most commonly reported to be provided in mental health settings (n = 14), care or nursing homes (n = 9), physical healthcare settings (n = 8), assisted living facilities (n = 6), and hospices (n = 5). Educational settings included schools (n = 12), universities (n = 7), pre-schools (n = 5), and nurseries (n = 4). Among NHS mental health settings, DAIs were delivered in adult and older adult mental health services (each n = 7), child and adolescent mental health services (n = 5), and forensic services (i.e., secure wards; n = 5). In NHS physical healthcare settings, delivery occurred primarily in inpatient wards (n = 9), followed by intensive care units (n = 6), outpatient clinics (n = 5), and general practice (GP) clinics (n = 2).
Twenty-one participants (67.7%) reported they were aware of the approximate number of institutions (e.g., hospitals, health services, community centers) where their organization provided DAIs. Estimates ranged from 1 to 6,000 institutions, with a cumulative total of 7,679 institutions across all participants. This wide range reflects the diversity in organizational size and reach among respondents, including both smaller local providers and some of the largest DAI organizations operating nationally within the UK.
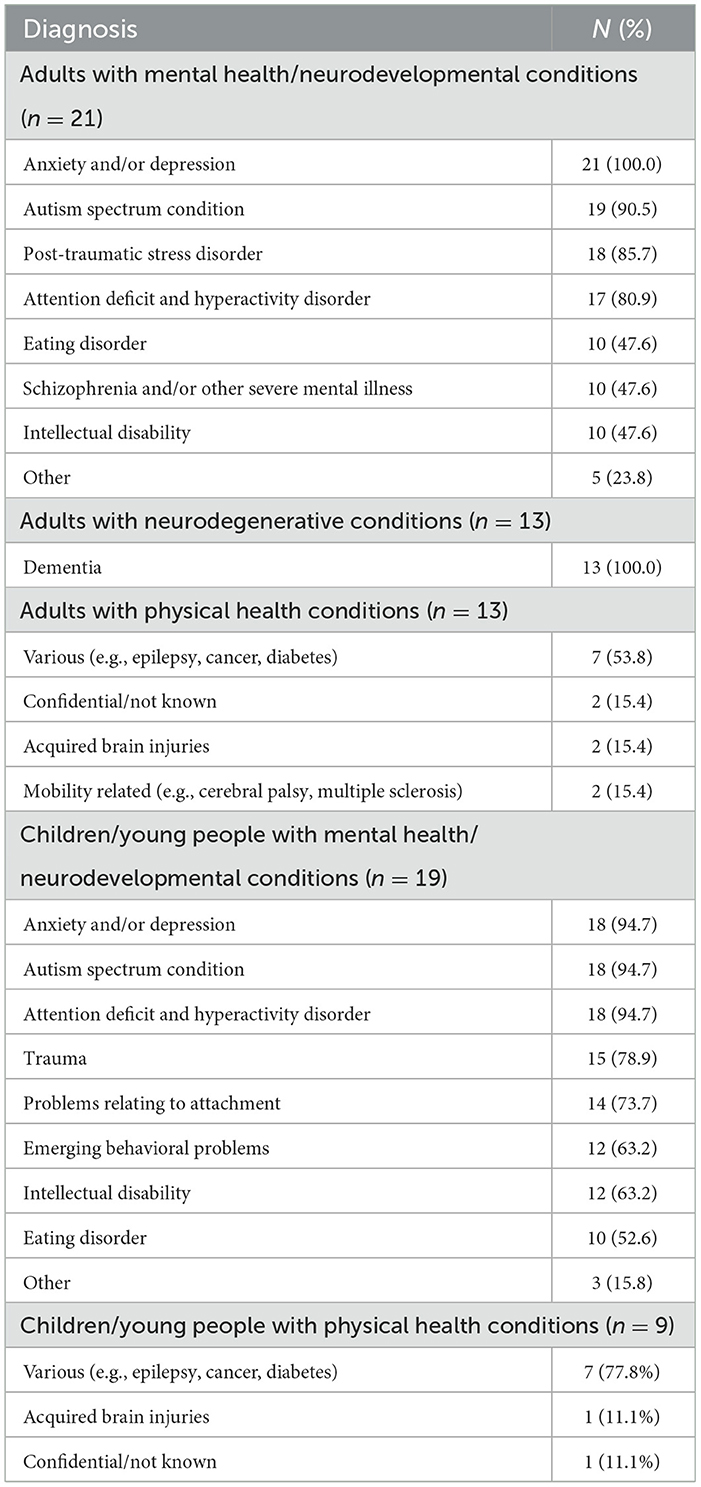
Populations served varied substantially across organizations, as DAIs were delivered to adults with a mental health or neurodevelopmental condition (n = 21; 67.7%), a physical health condition (n = 13; 41.9%), and/or a neurodegenerative condition (n = 13; 41.9%). Organizations also delivered DAIs to children and young people with a mental health or neurodevelopmental condition (n = 19; 61.3%) or a physical health condition (n = 9; 29.0%). Table 2 provides an overview of service user diagnoses.
DAI types, frequency, duration and session structure
The majority of participants reported their organization delivered dog-assisted therapy (i.e., goal-oriented interactions with dogs, led by trained animal-handler professionals and/or certified therapists; n = 19; 61.3%), whereas just over half reported delivering dog-assisted activities (i.e., spontaneous interactions with dogs, often led by volunteers; n = 16; 51.6%). When asked how often the DAI session had clear goals for the user, seven participants (22.6%) indicated “always,” six participants (19.4%) reported “most of the time,” six participants (19.4%) reported “sometimes,” and 12 (38.7%) reported they were unsure/did not know.
Regardless of intervention type or population served, DAIs were most frequently delivered on an individual basis (n = 28; 90.3%), followed by group-based delivery with peers (n = 16; 61.6%), and group-based delivery with relatives (n = 6; 19.4%). While 18 participants (58.1%) reported that the duration of DAIs “varied considerably” depending on the population group and their specific needs, seven participants (22.6%) typically delivered DAIs for a duration of 6–10 weeks. Other reported durations included 1–5 weeks (n = 3; 9.7%) and 11–15 weeks (n = 3; 9.7%). Likewise, nine participants (29.0%) indicated that the frequency of DAI sessions per service user “varied considerably.” However, for those reporting a consistent frequency, the most common was once a week (n = 14; 45.2%), followed by multiple times per week (n = 7; 22.6%). Only one participant (3.2%) stated that their organization delivered sessions once every 2 weeks. The average length of a DAI session was frequently reported as 31 min – 1 h (n = 17, 54.8%). However, nine participants (29.0%) reported sessions could last anywhere from >1 to < 2 h, and five participants (16.1%) reported their sessions were 30 min or less.
Dog-handler team training
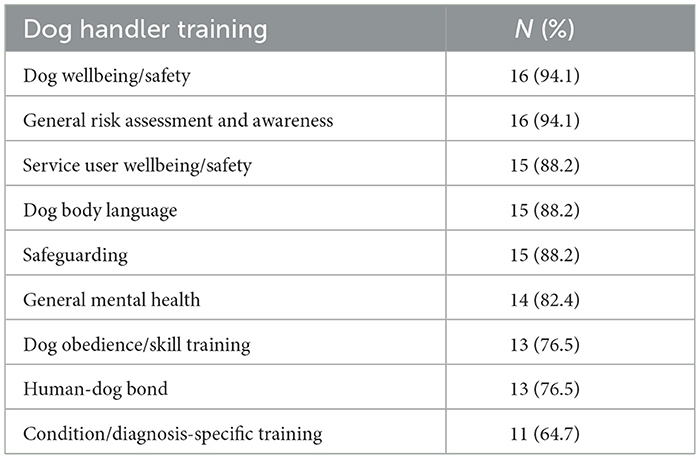
Just over half of the participants (n = 17; 54.8%) reported the dog handlers received formal training. Among those, the most frequently reported training included dog wellbeing and safety (94.1%), general risk assessment and awareness (94.1%), service user wellbeing and safety (88.2%), and recognizing dog body language (88.2%). A full overview of the training reported is presented in Table 3.
When participants were asked to rate their confidence within their role on a 10-point Likert scale (1 = not at all confident; 10 = very confident), the mean score was 8.7 (range = 5–10, standard deviation = 1.26).
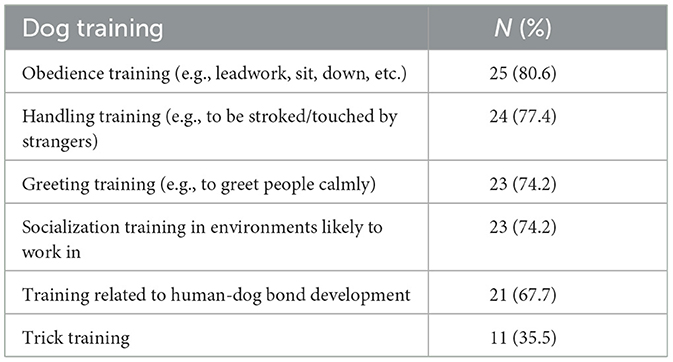
In addition to handler training, participants also reported a range of training activities undertaken by dogs prior to their involvement in DAIs. The most frequently reported training activities included basic obedience (e.g., leadwork, sit, down; 80.6%), handling training (77.4%), and greeting training (74.2%). Socialization in environments similar to those in which the dogs would work (74.2%) and training to support the development of the human-dog bond (67.7%) were also commonly reported. A full summary of reported training types is provided in Table 4.
Dog characteristics, selection, and welfare
Participants reported that dogs involved in DAI sessions were most commonly from the following UK Kennel Club classifications: Gundog group (e.g., Labradors, Golden Retrievers, Spaniels; n = 15; 48.4%) and crossbreeds (n = 15; 48.4%). Other represented classifications included the Working group dogs (e.g., Boxers, Dobermans, Rottweilers; n = 9; 29.0%), and Toy group dogs (e.g., Cavalier King Charles Spaniels, Chihuahuas; n = 8; 25.8%). Those less commonly reported included Terrier group dogs (e.g., Border Terriers; n = 7; 22.6%), Hound group dogs (e.g., Beagles, Greyhounds; n = 6, 19.4%), Pastoral group dogs (e.g., Border Collies, German Shepherds; n = 6; 19.4%), and Utility group dogs (e.g., Bulldogs, Dalmatians; n = 5; 16.1%).
Regardless of dog type, the youngest age at which the dog would start DAI work differed across organizations. Thirteen participants (41.9%) reported the youngest age a dog would commence work was 7–12 months, whereas others reported >2 years (n = 5; 16.1%); ≤ 6 months (n = 5; 16.1%); 13–18 months (n = 4; 12.9%), or 19–24 months (n = 4; 12.9%). Eight participants (25.8%) reported that there was no maximum age limit for dogs to continue working, while 10 participants (32.3%) indicated that the maximum age for a working dog would be 10 years. Five participants (16.1%) stated that the maximum age would be < 10 years, and four participants (12.9%) reported it would be over 10 years. Additionally, four participants (12.9%) were unsure whether there was a maximum age limit for the dogs involved.
When selecting dogs for DAIs, all participants (100%) reported temperament/behavior assessment as a selection criterion. Additional selection criteria were identified, including health status (passing veterinary assessment; n = 14; 45.2%); passing obedience test (e.g., Kennel Club test; n = 10; 32.3%), and selecting dogs based on specific characteristics (e.g., size, color, breed, age; n = 6; 19.4%).
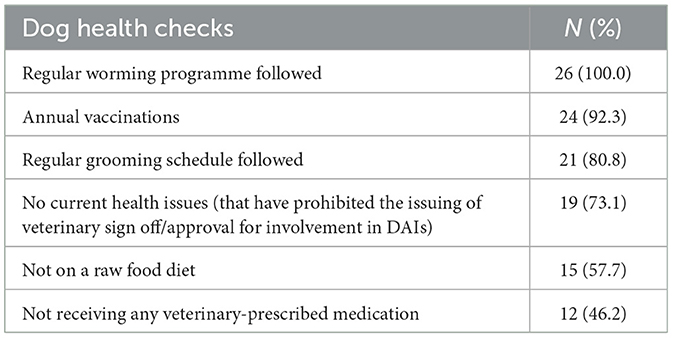
In addition to these selection criteria, 26 participants (83.9%) reported the type of health checks in place for dogs prior to or during their involvement (Table 5). In addition to the pre-determined options, one participant reported in a free-text box that “the dog must have been neutered/spayed,” and another indicated “there must be proof of immunity as per the World Small Animal Veterinary Association (28).”
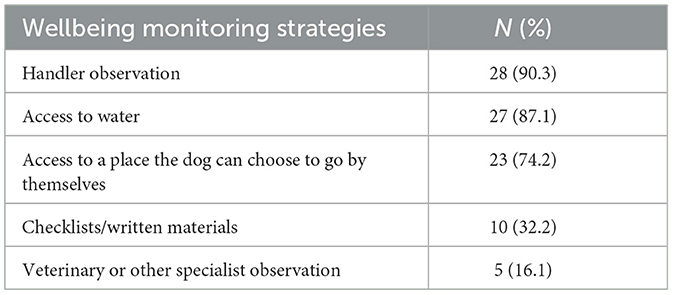
To monitor the wellbeing of dogs involved in DAIs, the most commonly reported strategies included handler observation (90.3%), ensuring access to water (87.1%), and providing a space the dog could choose to retreat independently (74.2%). Fewer organizations reported using tools such as checklists or written materials (32.2%) or veterinary or specialist observation (16.1%). The full set of reported wellbeing monitoring strategies are summarized in Table 6. Where participants indicated veterinary or other specialist observations were conducted (n = 5), the frequency ranged from every 3 months (n = 2) to every 6 months (n = 2), to twice a year (n = 1).
Lastly, the majority of participants (n = 25; 80.7%) reported their organization had a process to report undesirable dog behavior/participant injury, whereas three participants (9.7%) indicated no processes were in place, and three participants (9.7%) were unsure. Participants who reported the presence of a formalized process in free-text responses frequently described procedures including dog assessments, incident reporting through accident books, session recording forms, and the reporting of incidents or concerns to a designated point of contact, in accordance with established safeguarding protocols.
Barriers and facilitators to DAI provision
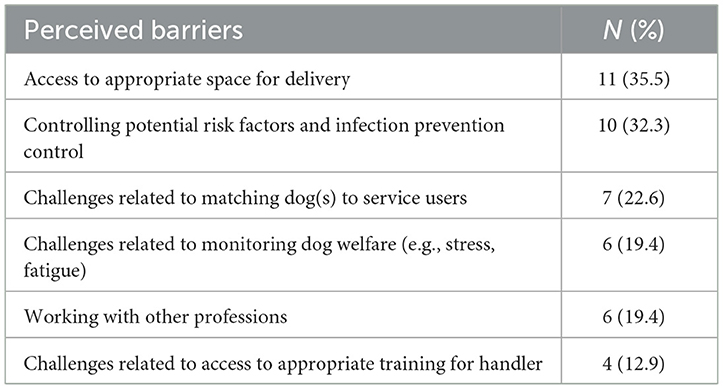
While six participants (19.4%) reported no perceived barriers to DAI implementation, others reported several challenges. The most frequently cited barriers included limited access to appropriate delivery spaces (35.5%), infection prevention and control concerns (32.3%), and challenges in appropriately matching dogs to service users (22.6%). Additional issues included difficulties in monitoring dog welfare and interprofessional collaboration. A full overview of the reported barriers are presented in Table 7.
Facilitators reported by free text included: a highly trained dog and handler adhering to animal welfare practices, an appropriate matching process to ensure a suitable dog-service user “fit,” allowing service users sufficient time to develop a relationship with the dog, and regular evaluation throughout implementation.
Discussion
To our knowledge, this survey provides the first attempt to report on the types and characteristics of current DAI practice in England. Results indicate that DAIs have been implemented in thousands of health, care and educational settings, including NHS and non-NHS health and care settings, as well as schools, and are delivered across a range of mental and physical health conditions for both children and adults. Our findings reveal substantial variation in the delivery of DAIs, particularly in the service settings, training of handlers and dogs, and approaches to monitoring both human and animal welfare. These insights contribute to the ongoing discourse on best practice and the need for standardized guidelines in the field.
The majority of participants reported implementing dog-assisted therapy (goal-orientated, structured involving clinical professionals and trained dog handlers) just over half the sample also reported using dog-assisted activities (spontaneous interaction, often no defined outcomes). This suggests that while therapeutic interventions involving dogs are prevalent, there is also a considerable focus on non-therapeutic activities aimed at enhancing general wellbeing. However, it could also be a reflection of the lack of uniformity in defining and categorizing AAIs, as highlighted in previous research (24). In response to criticisms in the field regarding inconsistent taxonomy and definitions (29, 30), there have been recent efforts to propose uniform terminology that accurately reflect the key features of different AAI approaches within this field to ensure the appropriate preparation, training, and support of all parties involved and improve clarity for those involved in the delivery and receipt of AAIs (24). This approach proposes that animal-assisted services (AASs) should be used as an over-arching term, which is further categorized into three main areas: treatment, education, and support programs (24).
We found that most participating providers served individuals with mental health and neurodevelopmental conditions, particularly autism, ADHD, anxiety/depression, and PTSD. This aligns with existing evidence that suggests DAIs may be particularly beneficial for these populations (3, 17, 31, 32). It was not possible to conduct a meaningful comparison of survey responses across population groups due to the small sample size. Additionally, our expert group that details of the intervention are likely to be determined based on individual needs rather than the needs associated with a specific condition. Across target population groups, DAIs were primarily delivered on an individual basis, with fewer organizations providing group-based interventions. This suggests that a personalized approach is favored, potentially to better address individual needs and facilitate stronger human-animal bonds. Notably, session goals varied in consistency, with only a quarter of respondents indicating that sessions “always” had clear goals, and a substantial proportion (38.7%) reporting they did not know or were unsure. This inconsistency may reflect differences in organizational structures, training levels, or philosophical approaches to DAI implementation.
The reported frequency and duration of DAIs also varied considerably. While 45.2% of organizations provided sessions once per week, others offered multiple sessions per week or had variable schedules based on user needs. Similarly, while most sessions lasted between 31 min and 1 h (54.8%), others extended beyond 1 h or were shorter than 30 min. The findings on frequency and duration variability are congruent with a recent survey conducted in intensive care unit settings in the UK (16), indicating this may be common practice across a range of settings. These variations highlight the importance of flexibility in DAI programming, allowing for adaptations based on service user requirements and organizational capacity. However, they also highlight the importance of clear definitions and frameworks to ensure consistency in practice and research, depending upon the needs of the service users, service capacity and the needs, behavior and welfare of the dog.
Comparable to previous research in the field, our findings identified Gundogs (e.g., Labradors, Golden Retrievers, and Spaniels) as the most commonly involved dog type followed by crossbreeds (33). Our findings also highlight the methods used for dog selection (e.g., temperament/behavior assessment, health status, obedience tests), which is an important observation given recent research indicates selection methods are seldom specified (33). This considerable variability in selection protocols reflects the absence of standardized criteria or validated tests for identifying dogs or dog-related characteristics which make them most suitable for specific types of DAIs, and aligns with variability reported in multiple studies (34–37).
Another key issue highlighted by this study is the variability in handler and dog training. Only 54.8% of handlers received formal training. There was a lack of consistency in the breadth of essential training provided, and notable gaps in important areas such as risk assessment and understanding of dog body language. This lack of consistent and comprehensive training raises concerns about the safe and ethical delivery of DAI implementation. Given the increasing recognition of the importance of handler competency in ensuring safe and effective DAI delivery (15), future efforts should focus on establishing educational training standards in terms of both content and quality assured qualifications. Dog welfare was also a critical consideration in DAI implementation, with organizations claiming to employ a range of wellbeing strategies, including handler observation, access to water, and designated rest areas. However, only a small proportion of providers reported formal veterinary assessments or structured welfare checklists. This variability raises concerns about the potential for undetected distress or fatigue in working dogs, which has been noted as a limitation in previous studies (38). The development of standardized welfare assessment tools could enhance the consistency of monitoring practices across organizations. Several challenges to DAI implementation were identified, and these are important to consider when designing a research study or when considering implementing DAIs in practice. Around a third of participants (35.5%) cited limited access to appropriate space as a barrier, while concerns regarding infection control and the complexities of matching dogs to service users were also noted. These findings align with existing literature emphasizing issues relating to welfare and infection control in AAIs (15, 16). Furthermore, ensuring dog welfare and securing appropriate training for handlers were identified as additional challenges, highlighting the need for robust training protocols and ethical oversight. In contrast, key facilitators of successful DAI implementation included the use of highly trained dogs and handlers, adherence to strict animal welfare practices, and a well-structured matching process between dogs and service users; although it should be noted that the scientific quality of the latter process remains unknown. Additionally, allowing sufficient time for relationship-building between the dog and service user, as well as regular evaluation throughout implementation, were identified as beneficial strategies. These findings reinforce the need for a comprehensive framework grounded in robust scientific evidence that integrates best practices in DAI delivery and focused on ensuring both service user benefit and animal welfare.
Implications
We established that DAIs are now implemented in many thousands of health, care and educational settings across the UK. There is clear potential for the further development and refinement of DAIs. The variability in session structure, duration, and goal-setting suggests a need for standardized guidelines to enhance consistency, ethical provision, safety, and efficacy, while allowing for individualized adaptations. Additionally, addressing reported key barriers, such as access to appropriate operational spaces, could facilitate wider implementation of DAIs. Future research should explore the long-term outcomes of DAIs for service users, as well as the impact of intervention structure and frequency on therapeutic effectiveness. Moreover, further investigation into best practices for dog assessment, welfare monitoring and handler training would contribute to the robustness, ethical and sustainable development of DAIs.
Limitations
This study represents one of the first surveys focused on DAI provision in England, offering valuable insights into current practices and standards. However, several limitations should be acknowledged. Firstly, the study relied on self-reported data, which will be subject to bias or inaccuracies. Additionally, only one individual per organization was invited to complete the survey, which may have introduced variability in response quality depending on the respondent's role (e.g., director vs. volunteer). Secondly, the small sample size (n = 31) and relatively low response rate (43.1%) may not fully capture the full spectrum of DAI practices across England. Indeed, it is likely that DAIs are currently being provided in many thousands more settings than we captured, and with even greater variability in the reported aspects. Future research should aim to expand the sample and incorporate qualitative methodologies to gain a deeper understanding of implementation challenges. Furthermore, despite free-text boxes available in the survey, there was an absence of in-depth free-text data, which would have allowed for a more comprehensive exploration of participants' responses. However, this decision was made intentionally to avoid the survey from becoming overly time-consuming and burdensome, particularly given the substantial number of specific items included. It should also be recognized that this survey was limited to those practicing DAIs in England. The results reported here may support future comparisons across countries, and across varying socioeconomic demographics.
Conclusion
This study demonstrates an encouraging breadth and versatility of DAIs across health and care settings in England, reflecting their integration into services that support individuals of all ages and clinical backgrounds and a clear indication of high demand and acceptability. From structured therapeutic programmes to informal community-based activities, DAIs appear to be valued for their potential to enhance mental, emotional, and physical wellbeing. At the same time, our findings underscore the pressing need for more standardized and validated procedures, particularly in areas such as practitioner training and animal welfare monitoring, to ensure the safe, ethical, and effective delivery of these interventions. While previous research points to the promise of DAIs, especially for individuals with mental health and neurodevelopmental conditions, inconsistency in practice and reporting continues to present barriers to achieving reliable outcomes and scaling services. Moving forward, greater collaboration between researchers, practitioners, and policymakers will be critical to address these challenges and establish a cohesive framework for best practice. By doing so, we can ensure that the full potential of DAIs is realized, delivering meaningful and lasting impact for service users and the wider field.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Health Sciences Research Ethics Committee at the University of York, UK. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ES: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Writing – original draft, Writing – review & editing. SH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ERi: Data curation, Formal analysis, Investigation, Project administration, Resources, Software, Writing – review & editing. DSM: Investigation, Methodology, Supervision, Writing – review & editing. SG: Investigation, Methodology, Supervision, Writing – review & editing. DM: Writing – review & editing. QW: Writing – review & editing. CC: Writing – review & editing. ERa: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Institute for Health and Care Research (NIHR) Programme Development Grant (PDG) (Award number 205656). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. ES, ERi, DM, QW, and ERa were supported by the NIHR Yorkshire and Humber Applied Research Collaboration (https://www.arc-yh.nihr.ac.uk).
Acknowledgments
We would also like to thank all participants who completed the survey.
Conflict of interest
SG is affiliated with an organization that participated in the survey. However, SG did not complete the survey on behalf of the organization and was not involved in the data analysis or interpretation of the data.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1645811/full#supplementary-material
References
1. Ratschen E, Sheldon TA. Elephant in the room: animal-asissted interventions in healthcare. BMJ. (2019) 367:l6260. doi: 10.1136/bmj.l6260
2. Jones MG, Rice SM, Cotton SM. Incorporating animal-assisted therapy in mental health treatments for adolescents: a systematic review of canine assisted psychotherapy. PLoS ONE. (2019) 14:e0210761. doi: 10.1371/journal.pone.0210761
3. Hediger K, Wagner J, Künzi P, Haefeli A, Theis F, Grob C, et al. Effectiveness of animal-assisted interventions for children and adults with post-traumatic stress disorder symptoms: a systematic review and meta-analysis. Eur J Psychotraumatol. (2021) 12:1879713. doi: 10.1080/20008198.2021.1879713
4. Hüsgen CJ, Peters-Scheffer NC, Didden R. A systematic review of dog-assisted therapy in children with behavioural and developmental disorders. Adv Neurodev Disord. (2022) 6:1–10. doi: 10.1007/s41252-022-00239-9
5. Nieforth LO, Schwichtenberg A, O'Haire ME. Animal-assisted interventions for autism spectrum disorder: a systematic review of the literature from 2016 to 2020. Rev J Autism Dev Disord. (2023) 10:255–80. doi: 10.1007/s40489-021-00291-6
6. O'Haire ME, Guerin NA, Kirkham AC. Animal-assisted intervention for trauma: a systematic literature review. Front Psychol. (2015) 6:1121. doi: 10.3389/fpsyg.2015.01121
7. Shoesmith E, Hall S, Sowden A, Stevens H, Pervin J, Riga J, et al. Dog-assisted interventions for children and adults with mental health or neurodevelopmental conditions: systematic review. Br J Psychiatry. (2025) 1–14. doi: 10.1192/bjp.2025.8
8. Nimer J, Lundahl B. Animal-assisted therapy: a meta-analysis. Anthrozoos. (2007) 20:225–38. doi: 10.2752/089279307X224773
9. Grové C, Henderson L, Lee F, Wardlaw P. Therapy dogs in educational settings: guidelines and recommendations for implementation. Front Vet Sci. (2021) 8:655104. doi: 10.3389/fvets.2021.655104
10. Lundqvist M, Carlsson P, Sjodahl R, Theodorsson E, Levin LÅ. Patient benefit of dog-assisted interventions in health care: a systematic review. BMC Complement Altern Med. (2017) 17:358. doi: 10.1186/s12906-017-1844-7
11. Lefebvre SL, Golab GC, Christensen E, Castrodale L, Aureden K, Bialachowski A, et al. Guidelines for animal-assisted interventions in health care facilities. Am J Infect Control. (2008) 36:78–85. doi: 10.1016/j.ajic.2007.09.005
12. Murthy R, Bearman G, Brown S, Bryant K, Chinn R, Hewlett A, et al. Animals in healthcare facilities: recommendations to minimize potential risks. Infect Control Hosp Epidemiol. (2015) 36:495–516. doi: 10.1017/ice.2015.15
13. Freeman L, Linder D, Mueller M, Gibbs D. Animal-assisted interventions: How-to Guide for Facilities. North Grafton, MA: Tufts Institute for Human-Animal Interaction (2016).
14. Linder DE, Siebens HC, Mueller MK, Gibbs DM, Freeman LM. Animal-assisted interventions: a national survey of health and safety policies in hospitals, eldercare facilities, and therapy animal organizations. Am J Infect Control. (2017) 45:883–7. doi: 10.1016/j.ajic.2017.04.287
15. Serpell JA, Kruger KA, Freeman LM, Griffin JA, Ng ZY. Current standards and practices within the therapy dog industry: results of a representative survey of United States therapy dog organizations. Front Vet Sci. (2020) 7:35. doi: 10.3389/fvets.2020.00035
16. Wright S, McAree H, Hosey M, Tantam K, Connolly B. Animal-assisted intervention services across UK intensive care units: a national service evaluation. J Intensive Care Soc. (2024) 26:68–79. doi: 10.1177/17511437241301000
17. Nieforth LO, Guerin NA, Stehli A, Schuck SEB, Yi K, O'Haire ME. Observation of human-animal interaction for research (OHAIRE) behavior coding in a randomized control trial of children with attention-deficit hyperactivity disorder (ADHD) and a canine-assisted intervention. Front Psychiatry. (2024) 15:1327380. doi: 10.3389/fpsyt.2024.1327380
18. Allen B, Shenk CE, Dreschel NE, Wang M, Bucher AM, Desir MP, et al. Integrating animal-assisted therapy into TF-CBT for abused youth with PTSD: a randomized controlled feasibility trial. Child Maltreat. (2021) 27:466–77. doi: 10.1177/1077559520988790
19. Calvo P, Fortuny JR, Guzmán S, Macías C, Bowen J, García ML, et al. Animal assisted therapy (AAT) program as a useful adjunct to conventional psychosocial rehabilitation for patients with schizophrenia: results of a small-scale randomized controlled trial. Front Psychol. (2016) 7:631. doi: 10.3389/fpsyg.2016.00631
20. Stefanini MC, Martino A, Bacci B, Tani F. The effect of animal-assisted therapy on emotional and behavioral symptoms in children and adolescents hospitalized for acute mental disorders. Eur J Integr Med. (2016) 8:81–8. doi: 10.1016/j.eujim.2016.03.001
21. Wijker C, Kupper N, Leontjevas R, Spek A, Enders-Slegers MJ. The effects of Animal Assisted Therapy on autonomic and endocrine activity in adults with autism spectrum disorder: a randomized controlled trial. Gen Hosp Psychiatry. (2021) 72:36–44. doi: 10.1016/j.genhosppsych.2021.05.003
22. Hill J, Ziviani J, Driscoll C, Teoh AL, Chua JM, Cawdell-Smith J. Canine assisted occupational therapy for children on the autism spectrum: a pilot randomised control trial. J Autism Dev Disord. (2020) 50:4106–20. doi: 10.1007/s10803-020-04483-7
23. Parra E, Manuel Hernández Garre J, Echevarría Pérez P. Impact of dog-assisted therapy for institutionalized patients with dementia: a controlled clinical trial. Altern Ther Health Med. (2022) 28:26–31.
24. Binder AJ, Parish-Plass N, Kirby M, Winkle M, Skwerer DP, Ackerman L, et al. Recommendations for uniform terminology in animal-assisted services (AAS). Hum Anim Interact. (2024) 12:1. doi: 10.1079/hai.2024.0003
25. The Kennel Club. The Kennel Club. (2025). Available online at: www.thekennelclub.org.uk
26. The Kennel Club. Canine Good Citizen. (2025). Available online at: www.thekennelclub.org.uk/dog-training/good-citizen-dog-training-scheme/
28. World Small Animal Veterinary Association. World Small Animal Veterinary Association: Transforming Care Together. (2025). Available online at: https://wsava.org
29. Rodriguez KE, Green FLL, Binfet J-T, Townsend L, Gee NR. Complexities and considerations in conducting animal-assisted intervention research: a discussion of randomized controlled trials. Hum-Anim Interact. (2023). doi: 10.1079/hai.2023.0004
30. Rodriguez KE, Herzog H, Gee NR. Variability in human-animal interaction research. Front Vet Sci. (2021) 7:619600. doi: 10.3389/fvets.2020.619600
31. O'Haire ME. Research on animal-assisted intervention and autism spectrum disorder, 2012–2015. Appl Dev Sci. (2017) 21:200–16. doi: 10.1080/10888691.2016.1243988
32. Schuck SEB, Johnson HL, Abdullah MM, Stehli A, Fine AH, Lakes KD. The role of animal assisted intervention on improving self-esteem in children with attention deficit/hyperactivity disorder. Front Pediatr. (2018) 6:300. doi: 10.3389/fped.2018.00300
33. Santaniello A, Garzillo S, Cristiano S, Fioretti A, Menna LF. The research of standardized protocols for dog involvement in animal-assisted therapy: a systematic review. Animals. (2021) 11:2576. doi: 10.3390/ani11092576
34. Rodrigo-Claverol M, Malla-Clua B, Marquilles-Bonet C, Sol J, Jove-Naval J, Sole-Pujol M, et al. Animal-assisted therapy improves communication and mobility among institutionalized people with cognitive impairment. Int J Environ Res Public Health. (2020) 17:5899. doi: 10.3390/ijerph17165899
35. Dell C, Chalmers D, Stobbe M, Rohr B, Husband A. Animal-assisted therapy in a Canadian psychiatric prison. Int J Prison Health. (2019) 15:209–31. doi: 10.1108/IJPH-04-2018-0020
36. Mueller MK, Anderson EC, King EK, Urry HL. Null effects of therapy dog interaction on adolescent anxiety during a laboratory-based social evaluative stressor. Anxiety Stress Coping. (2021) 34:365–80. doi: 10.1080/10615806.2021.1892084
37. Binfet J-T, Green FLL, Draper ZA. The importance of client–canine contact in canine-assisted interventions: a randomized controlled trial. Anthrozoos. (2022) 35:1–22. doi: 10.1080/08927936.2021.1944558
Keywords: dog-assisted intervention, England, national survey, dog training, dog welfare, barriers, facilitators
Citation: Shoesmith E, Hall SS, Riga E, Mills DS, Gibsone S, McMillan D, Wu Q, Clarke C and Ratschen E (2025) Dog-assisted interventions to support health and wellbeing: a national survey of current practice in England. Front. Public Health 13:1645811. doi: 10.3389/fpubh.2025.1645811
Received: 12 June 2025; Accepted: 22 July 2025;
Published: 05 August 2025.
Edited by:
Ricardo Gusmão, University of Porto, PortugalReviewed by:
Emma Kathryn Grigg, University of California, Davis, United StatesTemple Grandin, Colorado State University, United States
Copyright © 2025 Shoesmith, Hall, Riga, Mills, Gibsone, McMillan, Wu, Clarke and Ratschen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emily Shoesmith, ZW1pbHkuc2hvZXNtaXRoQHlvcmsuYWMudWs=
†These authors have contributed equally to this work and share first authorship
 Emily Shoesmith
Emily Shoesmith Sophie S. Hall
Sophie S. Hall Evgenia Riga1
Evgenia Riga1 Daniel S. Mills
Daniel S. Mills Elena Ratschen
Elena Ratschen