- 1Department of Emergency Medicine and West China School of Nursing, West China Hospital, Sichuan University, Chengdu, China
- 2Disaster Medical Center, Sichuan University, Chengdu, China
- 3Nursing Key Laboratory of Sichuan Province, Chengdu, China
Background: Somatic symptom disorder is influenced by various factors, with increasing evidence highlighting its close association with burnout. This study aimed to investigate the correlation between somatization symptoms and burnout levels among emergency nurses, focusing on the impact of burnout on somatization.
Methods: A cross-sectional study was conducted involving 1,540 emergency nurses working in tertiary hospitals in China. Data collection occurred between December 26, 2023, and January 18, 2024, using the Chinese versions of the Maslach burnout inventory–general survey (MBI-GS) and the somatic symptom disorder self-rating scale (SSD-CN). Statistical analyses were performed using SPSS version 25.0.
Results: The mean SSD score was 39.58 ± 13.61, with 53.4% of participants exhibiting moderate to severe somatization symptoms. The mean burnout score was 4.77 ± 6.16, with a burnout incidence of 57.3%. A positive correlation was identified between the composite burnout score and the total SSD score (Pearson correlation coefficient = 0.534, p < 0.01). Emotional exhaustion and depersonalization scores were also positively correlated with individual SSD domain scores and the total SSD score (p < 0.01), Multivariate linear regression analysis revealed significant factors influencing somatization symptoms, including 6–10 and 11–15 years of work experience, weekly working hours of 41–48 or 49–58, 5–8 or >9 night shifts per week, monthly incomes ≥10,000 RMB and the composite burnout score (p < 0.05).
Conclusion: Emergency nurses in this study exhibited severe somatization symptoms, with burnout identified as a significant contributing factor. To address this issue, healthcare management should consider implementing alternative shift patterns, optimizing workforce allocation, and revising compensation systems to ensure equitable labor distribution. These measures would support the healthy development of emergency nurses. Furthermore, nurses should prioritize self-care by engaging in activities such as psychological interventions, positive thinking training, and yoga to reduce burnout and enhance overall health.
1 Introduction
The occupational health of emergency nurses is significantly impacted by the urgency of their tasks, high workload, operational demands, and complex work environments. Somatic symptom disorder (SSD) is characterized by the presence of one or more somatic symptoms, often accompanied by mood disturbances, leading to severe anxiety, depression, and functional impairment in affected individuals (1). Among healthcare workers, the prevalence of SSD is reported to be 34.8% (2). A study conducted in the United States revealed that anxiety and depression are highly prevalent among healthcare workers, affecting over 80% of this population-substantially higher than in the general U.S. population (3). Nurses, in particular, experience elevated rates of anxiety and depression compared with other professions (4). The cooccurrence of increased somatic symptoms with heightened anxiety and depression intensifies the burden of illness among emergency nurses (5), underscoring the need for additional healthcare resources to support this workforce (6). As the largest professional group within the healthcare sector, nurses experiencing severe SSD are at risk of diminished care quality and heightened susceptibility to suicidal ideation (7). Despite the evident challenges, global studies on the health of emergency nurses remain limited. Therefore, comprehensive health surveys targeting emergency nurses are essential to establish a reliable foundation for improving clinical care management and promoting their health and wellbeing.
SSD is influenced by various factors, with increasing evidence highlighting its close association with burnout (8–11). Burnout is a syndrome characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment, typically resulting from prolonged work-related stress (12). This negative emotional state adversely affects healthcare workers, leading to reduced work quality and efficiency, as well as increased conflicts with patients (13, 14). In 2019, the World Health Organization officially recognized burnout as an occupational health syndrome for the first time (15). Studies from multiple countries report burnout prevalence rates among healthcare workers reaching as high as 75% (16–18), with emergency nurses being disproportionately affected (19, 20), particularly in terms of emotional exhaustion (21). The nature of emergency nursing marked by high-risk, heavy workloads, and time sensitive tasks places these professionals at an elevated risk of burnout (22, 23). Research has demonstrated that burnout significantly impacts the mental health of healthcare workers, contributing to conditions such as anxiety, depression, cardiovascular disease and chronic pain (9, 10, 24–26). However, global studies in emergency medicine have provided limited evidence on the relationship between burnout and the health of emergency nurses. Therefore, exploring burnout levels and their health impact on this population warrants attention.
To address this gap, this study conducted a multicenter, large-sample, cross-sectional survey of emergency nurses across various regions of China. The study aimed to examine the correlation between somatization symptoms and burnout and to explore the impact of burnout on emergency nurses' health. The findings are intended to inform clinical interventions targeting burnout and promote health management strategies for emergency nurses, providing meaningful insights into mitigating this critical issue.
2 Methods
2.1 Research design
This study employed a cross-sectional survey design.
2.2 Survey respondents and sampling method
A stratified cluster sampling method was used to select participants. China was divided into seven geographic regions (Southwest, Northwest, South China, North China, East China, Central China, and Northeast China). From each region, two to three provincial capitals were chosen, one to two tertiary hospitals in each selected city were included, and a total of 30 hospitals were surveyed. Emergency nurses meeting the inclusion and exclusion criteria were enrolled in the study from December 26, 2023, to January 18, 2024. Inclusion criteria include at least 1 year of experience working in emergency medicine, licensed nurses employed in the emergency department, and aged 18 years or older. Exclusion criteria include nurses undergoing further training, specialist nurses, or those in standardized training programs, nurses with a previous medical diagnosis of a related psychiatric disorder, and nurses on sick leave, maternity leave, or lactation leave for 1 month or longer.
2.3 Research instruments
This survey collected data on general sociodemographic characteristics, somatization symptoms and burnout.
2.4 General sociodemographic information
Data were collected on the following variables: sex, education level, age, weekly working hours, night shifts, years of service, job title, parity and income.
2.5 Self-rating scale for somatic symptom disorder, Chinese (SSD-CN)
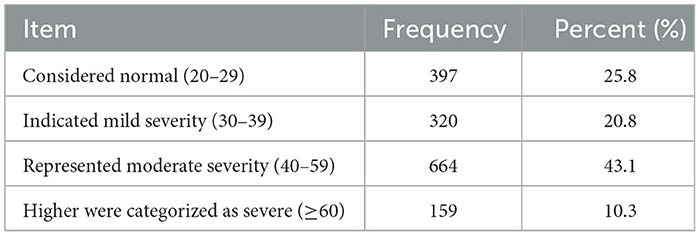
The Chinese version of the self-rating scale for somatic symptom disorder (SSD-CN) (27) was used. This scale consists of 20 items categorized into four domains: somatization symptoms, anxiety, depression, and combined anxiety-depression. The scale comprises 10 items assessing physical discomfort, four items evaluating anxiety, four items measuring depression, and two items addressing combined anxiety and depression. The scoring methodology assessed the occurrence and severity of each symptom on a scale from 1 to 4. A score of 1 indicated that the symptom was not present, 2 signified that it was present for a few days or tolerable, three indicated that it occurred for approximately half the days or was intermittently relieved, and four reflected symptoms that were present almost daily or difficult to endure. The total score ranged from 20 to 80. The severity of SSD was classified as follows: 20–29 was considered normal, 30–39 indicated mild severity, 40–59 represented moderate severity, and scores of 60 or higher were categorized as severe. Correlation coefficients for the SSD scale ranged from 0.76 to 0.88 between the domains and the total score and from 0.56 to 0.70 within each domain, demonstrating strong internal consistency. The test–retest reliability of the scale was 0.9. A cutoff score of 36 was established for diagnostic purposes, with a sensitivity of 0.97 and a specificity of 0.96.
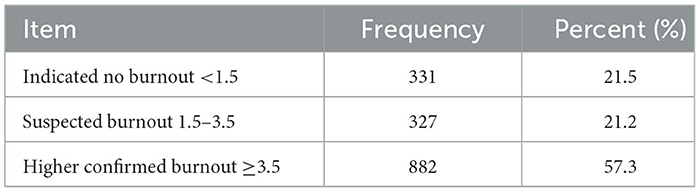
2.6 Burnout survey
Burnout was evaluated using the Chinese version of the Maslach burnout inventory-general survey, adapted by Wei et al. (28). It is used to assess burnout levels among emergency nurses. The scale, validated by Chinese scholars Yueping et al. (29) demonstrated good reliability and validity. The MBI-GS comprises 16 items scored on a seven-point Likert scale ranging from 0 to 6. These items are divided into three domains: emotional exhaustion, depersonalization, and work achievement. Emotional exhaustion and depersonalization scores were interpreted positively, with higher scores indicating greater burnout. Conversely, the work achievement domain was scored negatively, with lower scores signifying greater burnout. A burnout score of <1.5 indicated no burnout, a score between 1.5 and 3.5 suggested suspected burnout, and a score of 3.5 or higher confirmed burnout. Cronbach's α coefficients for the overall scale and its three domains were 0.860, 0.914, 0.814, and 0.899, respectively, demonstrating good internal consistency.
2.7 Data collection
Data were collected using an electronic version of the questionnaire. To ensure completeness and prevent duplication, all questions were set as mandatory and could only be answered once by each participant. One investigator at each hospital provided training on completing the questionnaire before the survey. The survey link was distributed via the WeChat platform, and the study's purpose was explained to participants. Participation was anonymous, and respondents were required to read and provide consent via an informed consent form before accessing the questionnaire. Once completed, respondents submitted their responses.
2.8 Methods of statistical analysis
Data were imported into SPSS 25.0 for statistical analysis frequency and percentage were used to describe categorical data, while the mean and standard deviation were used for continuous data. Analysis of variance was employed to compare SSD scores and overall burnout scores across demographic characteristics. Pearson's was used to analyse studies on the correlational relationship between somatisation symptoms and burnout, and multivariate linear regression was applied to assess the effects of somatization symptoms and burnout on each other.
3 Results
3.1 Basic information
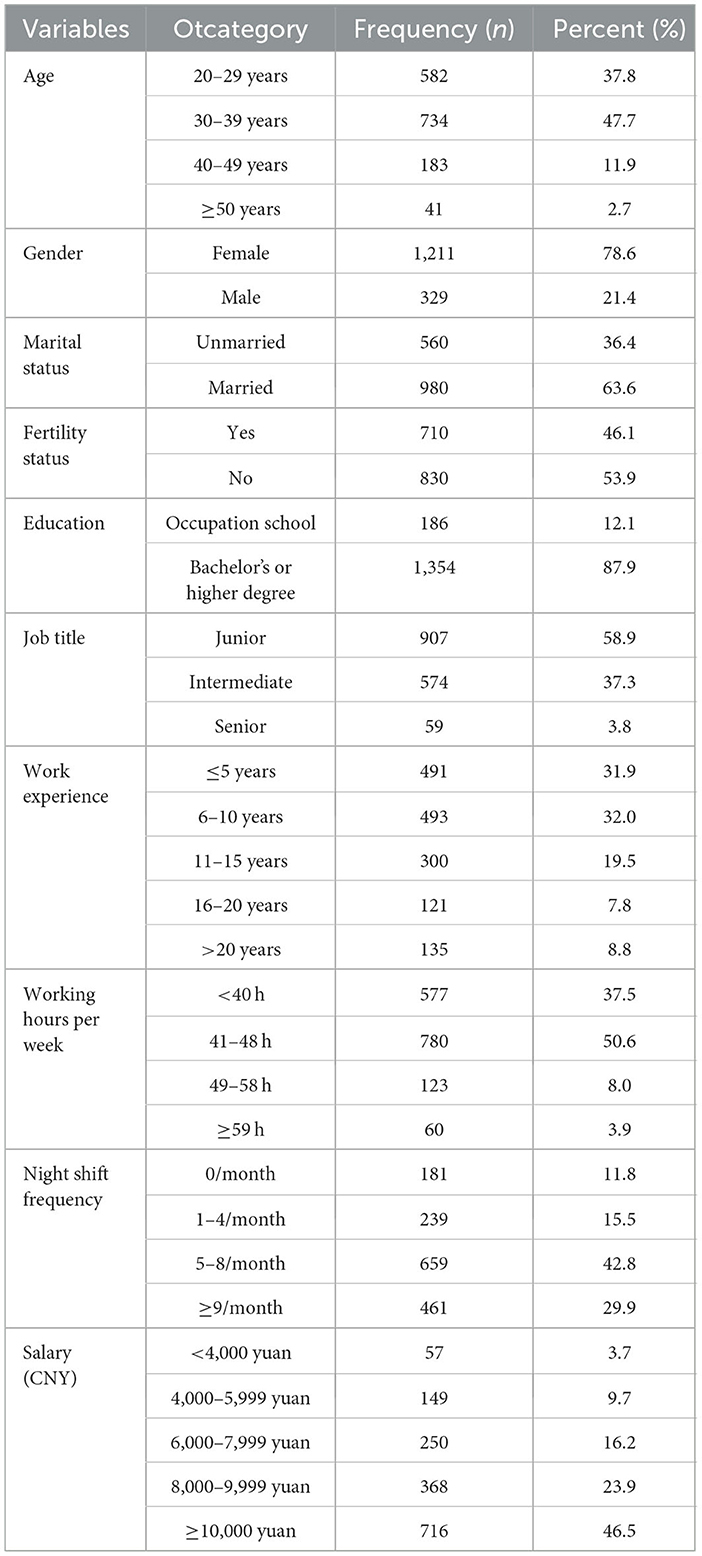
A total of 1,550 questionnaires were collected, of which 1,540 were valid after excluding 10 with identical responses. Among the participants, 1,211 (78.6%) were female, and 329 (21.4%) were male. The majority of participants (734, or 47.7%) were aged 30–39 years. Regarding educational background, 1,354 participants (87.9%) held a bachelor's degree or higher. Half of the respondents (780, or 50.6%) worked 41–48 h per week, and 1,359 participants (88.2%) reported working night shifts, as shown in Table 1.
3.2 SSD score and overall burnout score analysis
The total SSD score was 39.58 ± 13.61, with 53.4% of participants experiencing moderate to severe somatic symptoms. Only 25.8% reported no somatic symptoms, as shown in Table 2. The overall burnout score was 4.77 ± 6.16, with burnout affecting 57.3% of participants and suspected burnout observed in 21.2%, as shown in Table 3.
3.3 Two-way correlation analysis of burnout and SSD scores by domain
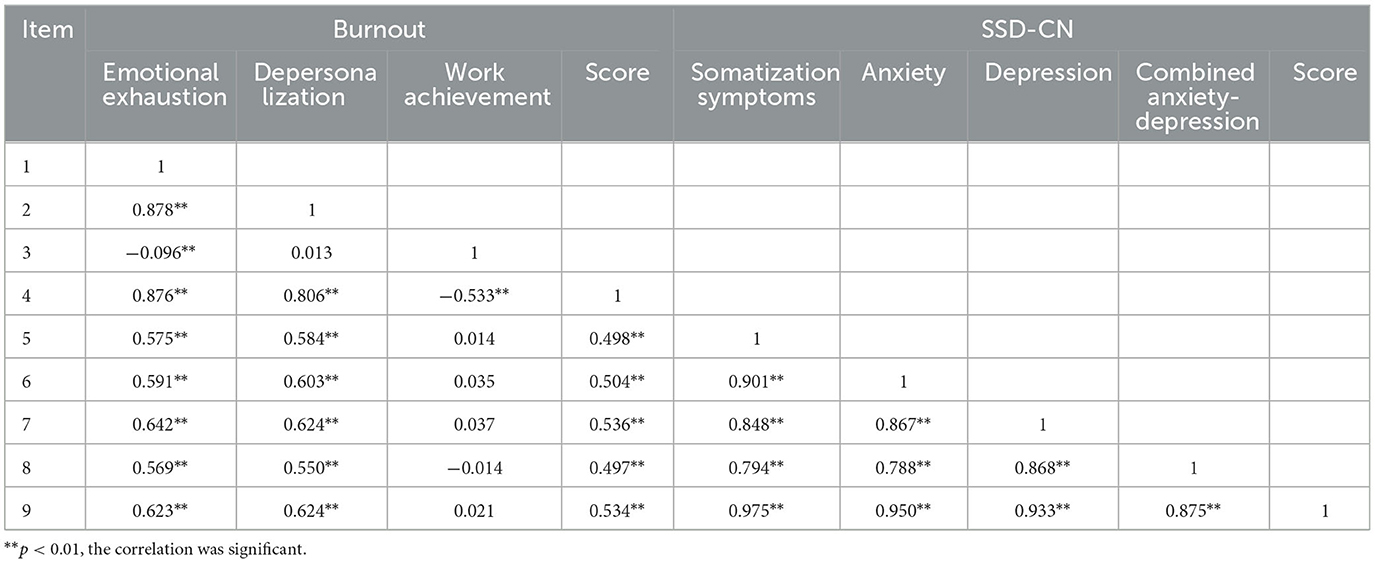
The overall burnout score showed a significant positive correlation with the total SSD score (Pearson's correlation coefficient: 0.534, p < 0.01). The emotional exhaustion scores were both significantly positively correlated with each SSD domain and the total SSD score (Pearson's correlation coefficient:0.575, 0.591, 0.642, 0.569, 0.623, p < 0.01), depersonalization domain scores were both significantly positively correlated with each SSD domain and the total SSD score (Pearson's correlation coefficient: 0.584, 0.603, 0.624, 0.550, 0.624, p < 0.01). However, the work achievement domain was not correlated with any SSD domain, as shown in Table 4.
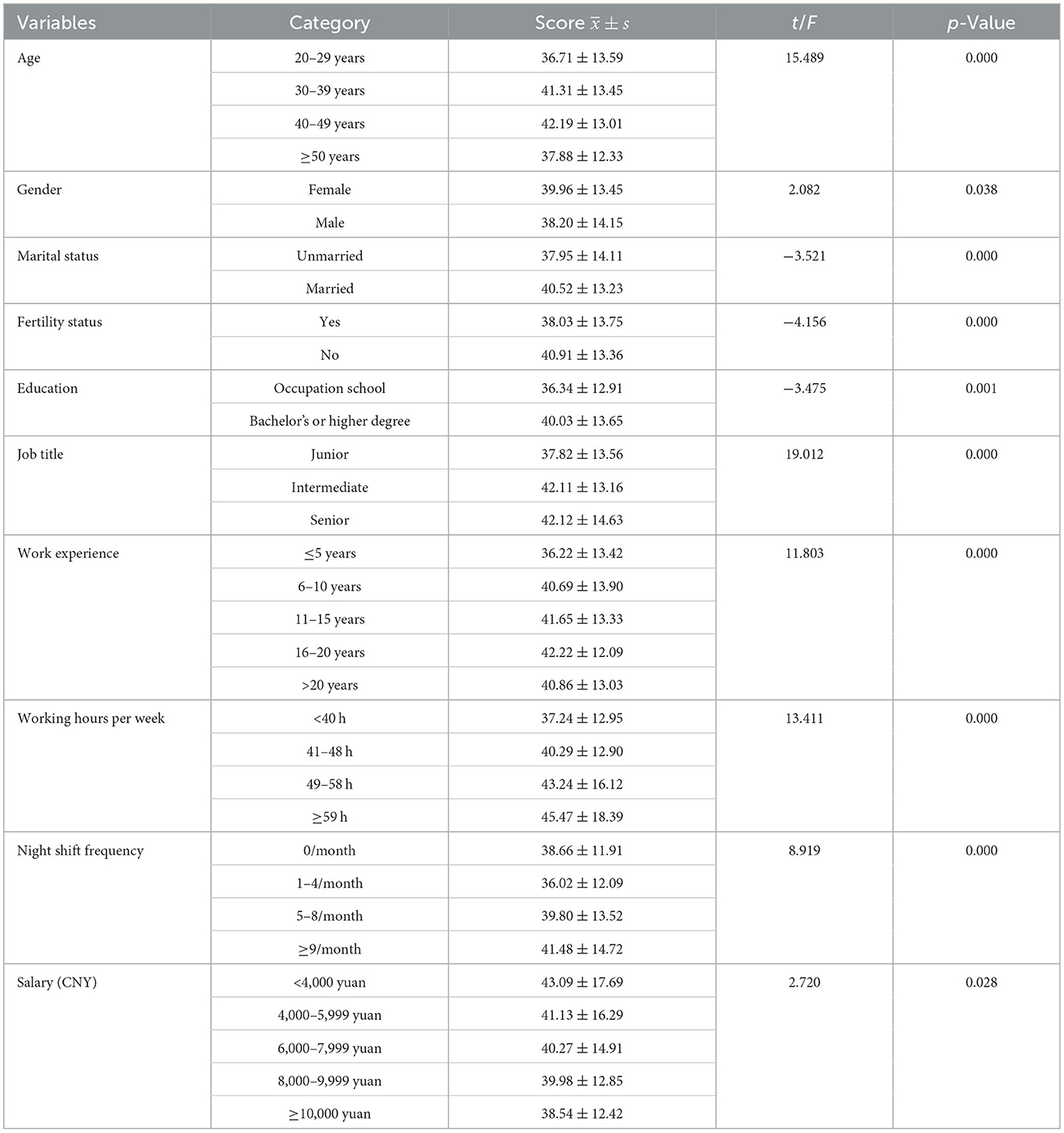
3.4 Factors influencing somatization symptoms univariate analysis
The univariate analysis revealed that gender, age, marital status, reproductive status, weekly working hours, frequency of night shifts, job title, monthly income, years of service, and education were all statistically significant factors influencing somatization symptoms (p < 0.05), as shown in Table 5.
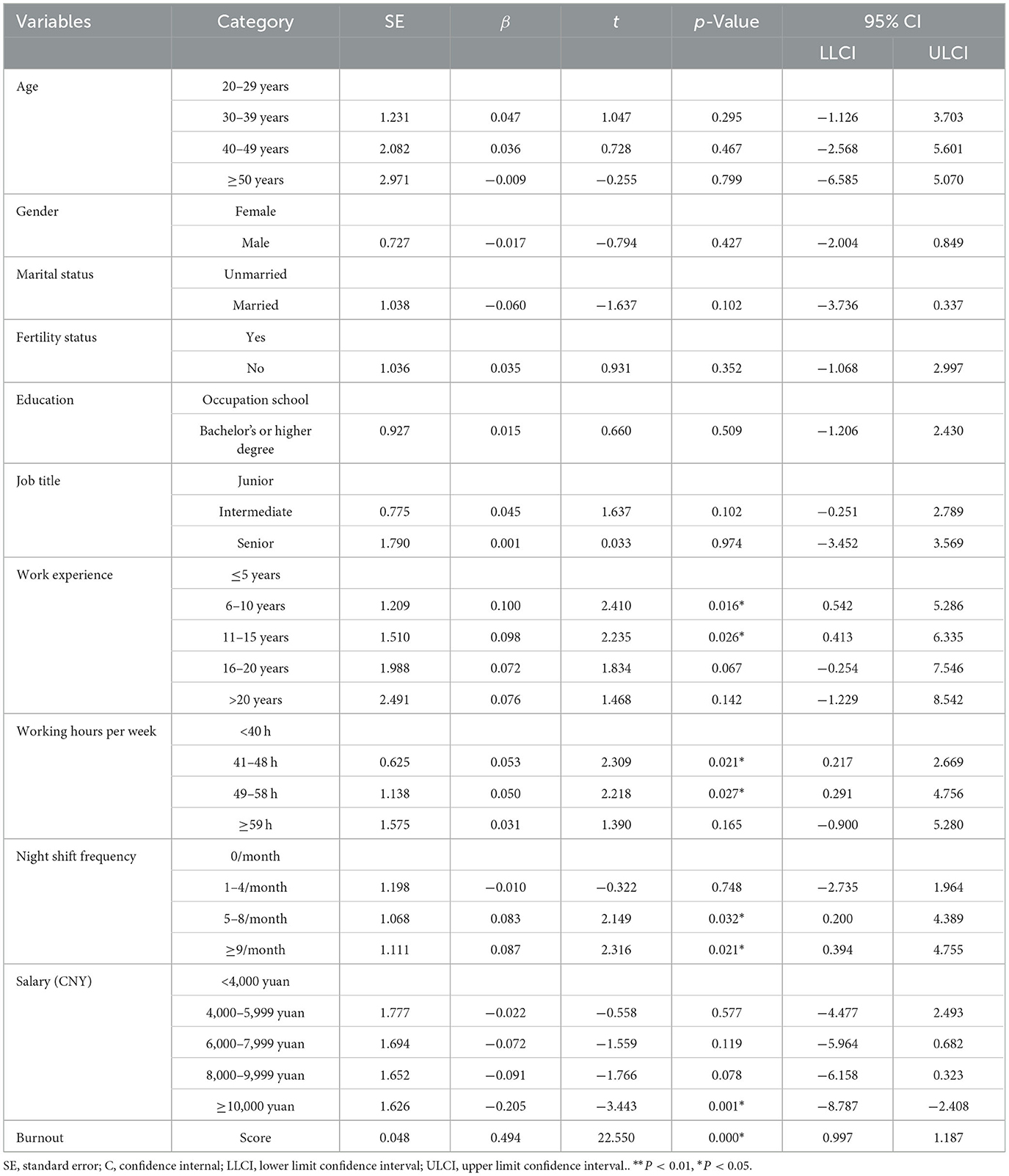
3.5 Multivariate analysis
Multivariate linear regression analysis identified several factors influencing somatization symptoms. These included 6–10 years of service (B = 2.914; 95% CI, 0.542–5.286) and 11–15 years of service (B = 3.374; 95% CI, 0.413–6.335), weekly working hours of 41–48 h (B = 1.443; 95% CI, 0.217–2.669) and 49–58 h (B = 2.524; 95% CI, 0.291–4.756), 5–8 night shifts per week (B = 2.294; 95% CI, 0.200–4.389) and ≥9 night shifts per week (B = 2.575; 95% CI, 0.394–4.755), a monthly income ≥10,000 RMB (B = −5.598; 95% CI, −8.787 to −2.408), and burnout (B = 1.092; 95% CI, 0.997–1.187), all of which were statistically significant (p < 0.05), as shown in Table 6.
4 Discussion
The study found that severe somatization symptoms affected 53.4% of emergency nurses, underscoring the urgent need to improve their health. These findings align with other studies indicating high levels of anxiety, depression, and severe somatization symptoms among healthcare workers (2, 30, 31). The continuous development of the medical industry has resulted in an increasingly heavy workload for emergency nurses, who are expected to possess advanced professional skills and scientific research capabilities. Emergency nurses are frequently exposed to a range of traumatic situations and accidents, often confronting death, which can lead to posttraumatic stress disorder and increase the risk of mental health issues and somatization symptoms. To address these challenges, management can introduce online information management methods aimed at reducing depression and anxiety (4), such as text message reminders, mobile mental health assessments, and online continuity of care programs. Furthermore, emotional awareness and expressive arts therapy have been shown to significantly reduce somatic symptoms (32). Our survey indicates a high prevalence of burnout among emergency nurses in China, with an incidence rate of 57.3%. This finding aligns with previous studies (33–36), which also highlighted a high level of burnout among emergency nurses. However, this result contrasts with a study by Adriaenssens et al. It could be that the career is too stressful and while excessive effort increased the risk of burnout (37, 38) which reported a burnout prevalence of 26% among emergency nurses in Western countries. This discrepancy may stem from differences in healthcare systems and medical environments. Western countries generally have more robust healthcare resources and more equitable access to care, while Chinese tertiary hospitals face challenges such as uneven medical resources, overcrowded facilities, high patient expectations, which contribute to significant pressure and burnout among emergency nurses (36). Improve working conditions, such as developing flexible workload management, increasing salaries, adjusting promotion mechanisms, and supporting policies to alleviate burnout (37). Personalized music interventions have been recommended as an adjunctive method to alleviate emotional exhaustion among emergency nurses, thus enhancing their overall health (33).
The correlation analysis in this study demonstrated that the overall burnout score was positively correlated with the total SSD score, meaning that higher burnout scores were associated with more severe somatization symptoms. This finding is consistent with other studies, which have shown that burnout syndrome is significantly linked to higher rates of depression and somatic disorders (39, 40). The results of the multivariate hierarchical regression analysis indicated that burnout was a significant factor influencing somatization symptoms. This finding is consistent with several studies that have concluded burnout negatively impacts health (14, 26), serving as a risk factor for musculoskeletal pain, cardiovascular disease, and depression (9, 11). Gulen et al. (42) suggested that both depression and burnout syndromes are influenced by S100B protein levels. Similarly, Pilger et al. (43) found that salivary cortisol levels influenced anxiety and depressive symptoms, which could be treated to alleviate the health status of nurses. Long-term exposure to noisy environments in Chinese emergency departments activates the sympathetic nervous system, inducing a stress response (34). Emergency nurses face common occupational health problems, and experiences of workplace violence can have a serious impact on their physical and mental health (44). In addition to their ability to manage emergencies and apply their nursing skills, emergency nurses must also cope with pressure from patients and their families. Working in such a complex environment can lead to burnout, anxiety, depression, and somatic discomfort. Flexible work schedules, telecommuting options, and family support policies should be introduced that may help increase job satisfaction and reduce burnout (45, 46). Haghighinejad et al. (47) concluded that positive thinking training could be an effective strategy to reduce burnout and improve health. The researchers (41, 48) found that yoga training led to significant improvements in both burnout and overall health, recommending that nurses engage in such practices during their spare time. Medisauskaite et al. (49) highlighted that education in psychological knowledge significantly reduced anxiety. The harm of workplace violence to the health of emergency nurses can be mitigated by improving sleep quality (44). Effective nurse management can further alleviate burnout by rationally allocating human resources, providing diverse promotional opportunities, and optimizing the work environment to enhance motivation. This would not only improve the overall health of emergency nurses but also reduce burnout levels.
The results of the multivariate hierarchical regression analysis revealed that several factors such as having 6–15 years of work experience, working 41–58 h per week, working more than five night shifts per week, and earning a monthly income of ≥10,000 RMB significantly influenced somatization symptoms. Emergency nurses with 6–15 years of experience make up 51.5% of the workforce, serving as the backbone of emergency clinical care. However, they are often burdened with family caregiving responsibilities, which, when combined with the demands of their profession, can lead to work-family role behavioral conflicts, negatively impacting both their physical and mental health (50, 51). Therefore, it is crucial for mid-career and senior emergency nurses to engage in research and innovation, contribute new knowledge and technologies to clinical practice, and find ways to balance work with family obligations, thereby enhancing their professional value and sense of accomplishment. Extended working hours and frequent night shifts can cause fatigue, disrupt circadian rhythms, and impair sleep. making it difficult for their bodily functions to adapt to the shift system, leading to sleep deprivation, which in turn affects the clearance of β-amyloid from the brain, and then causes sleep disorders. Sleep disturbances can have a serious negative impact on nurse health, patient safety, and social productivity (52, 53). Improved staffing levels and the ability to take uninterrupted breaks have been shown to positively affect the health status of emergency nurses (54). Management should explore alternative shift patterns (44), reduce the frequency of night shifts, and ensure sufficient rest periods to mitigate burnout and improve the nurses' occupational health. Finally, monthly income ≥10,000 RMB was found to be a protective factor against somatization symptoms. Management should consider ensuring that labor compensation is distributed fairly and reasonably, as this can play a key role in promoting the health and wellbeing of emergency nurses (37).
5 Limitations
This study only examined the correlation between burnout and somatization symptoms, without establishing a causal relationship. Future longitudinal studies may explore this relationship in greater depth. Additionally, the study population, environment, and job characteristics are specific to emergency nurses and may not be representative of other occupational groups. Further research is needed to determine the generalizability of these findings to other fields. Finally, the use of self-reported measures, which may introduce response or recall bias.
6 Conclusions
This study found that emergency nurses experience significant somatization symptoms, with their overall burnout score being positively correlated with the total SSD score. Somatization symptoms were influenced by multiple factors, with burnout identified as a key determinant. This was determined through a multicenter, large-sample survey. Management should prioritize exploring alternative shift patterns, optimizing human resource allocation, and refining the compensation system. At the individual level, strategies such as positive thinking training, yoga, and personalized music interventions can help reduce burnout and improve the health of emergency nurses.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NL: Investigation, Writing – original draft, Data curation, Formal analysis. NX: Writing – review & editing. XC: Formal analysis, Data curation, Writing – review & editing. HZ: Writing – review & editing, Data curation, Formal analysis. LZho: Formal analysis, Data curation, Writing – review & editing. DD: Data curation, Writing – review & editing. LZhu: Writing – review & editing, Data curation. YZ: Supervision, Methodology, Software, Writing – review & editing, Conceptualization, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank all the participants of this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association D, American Psychiatric Association DS. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association. (2013). doi: 10.1176/appi.books.9780890425596
2. Haller H, Cramer H, Lauche R, Dobos G. Somatoform disorders and medically unexplained symptoms in primary care. Dtsch Arztebl Int. (2015) 112:279–87. doi: 10.3238/arztebl.2015.0279
3. Agarwal AK, Southwick L, Gonzales RE, Bellini LM, Asch DA, Shea JA, et al. Digital engagement strategy and health care worker mental health: a randomized clinical trial. JAMA Netw Open. (2024) 7:e2410994. doi: 10.1001/jamanetworkopen.2024.10994
4. O'Brien WH, Singh RS, Horan K, Moeller MT, Wasson R, Jex SM. Group-based acceptance and commitment therapy for nurses and nurse aides working in long-term care residential settings. J Altern Complement Med. (2019) 25:753–61. doi: 10.1089/acm.2019.0087
5. Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. (2018) 20:23–31. doi: 10.31887/DCNS.2018.20.1/phenningsen
6. Tomenson B, McBeth J, Chew-Graham CA, MacFarlane G, Davies I, Jackson J, et al. Somatization and health anxiety as predictors of healthcare use. Psychosom Med. (2012) 74:656–64. doi: 10.1097/PSY.0b013e31825cb140
7. Melnyk BM, Davidson JE, Mayfield C, Zisook S, Tucker S, Hsieh AP, et al. A study protocol for the modified interactive screening program plus MINDBODYSTRONG© RCT: a mental health resiliency intervention for nurses. PLoS ONE. (2024) 19:e0303425. doi: 10.1371/journal.pone.0303425
8. Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, et al. The association between burnout and physical illness in the general population–results from the Finnish health 2000 study. J Psychosom Res. (2006) 61:59–66. doi: 10.1016/j.jpsychores.2005.10.002
9. Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. (2017) 12:e0185781. doi: 10.1371/journal.pone.0185781
10. Traunmüller C, Stefitz R, Gaisbachgrabner K, Hofmann P, Roessler A, Schwerdtfeger AR. Psychophysiological concomitants of burnout: evidence for different subtypes. J Psychosom Res. (2019) 118:41–8. doi: 10.1016/j.jpsychores.2019.01.009
11. Armon G, Melamed S, Shirom A, Shapira I. Elevated burnout predicts the onset of musculoskeletal pain among apparently healthy employees. J Occup Health Psychol. (2010) 15:399–408. doi: 10.1037/a0020726
12. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
13. Gardner RL, Cooper E, Haskell J, Harris DA, Poplau S, Kroth PJ, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc. (2019) 26:106–14. doi: 10.1093/jamia/ocy145
14. Wang K, Wang X, Han Y, Ye C, Pan L, Zhu C. The risk factors for burnout among nurses: an investigation study. Medicine. (2024) 103:e39320. doi: 10.1097/MD.0000000000039320
15. World Health Organization. Burn-Out An “Occupational Phenomenon”: International Classification of Diseases. (2019). Available online at: http://www.WHO.int/mental_health/evidence/burn-out/en/
16. Bruce CT, Thomas PS, Yates DH. Burnout and psychiatric morbidity in new medical graduates. Med J Aust. (2005) 182:599. doi: 10.5694/j.1326-5377.2005.tb06833.x
17. Shanafelt TD. Burnout and self-reported patient care in an internal medicine residency program. Ann Int Med. (2002) 136:358. doi: 10.7326/0003-4819-136-5-200203050-00008
18. Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. (2014) 89:443–51. doi: 10.1097/ACM.0000000000000134
19. Torre M, Santos Popper MC, Bergesio A. Burnout 91prevalence in intensive care nurses in Argentina. Enferm Intensiva. (2019) 30:108–15. doi: 10.1016/j.enfie.2018.04.005
20. Yazici MU, Teksam O, Agin H, Erkek N, Arslankoylu AE, Akca H, et al. The burden of burnout syndrome in pediatric intensive care unit and pediatric emergency department: a multicenter evaluation. Pediatr Emerg Care. (2021) 37:e955–61. doi: 10.1097/PEC.0000000000001839
21. Yuguero O, Rius N, Soler-González J, Esquerda M. Increase of burnout among emergency department professionals due to emotional exhaustion during the SARSCov2 pandemic: evolution from 2016 to 2021. Medicine. (2022) 101:e31887. doi: 10.1097/MD.0000000000031887
22. Liu Y, Zhang J, Hennessy DA, Zhao S, Ji H. Psychological strains, depressive symptoms, and suicidal ideation among medical and non-healthcare professionals in urban China. J Affect Disord. (2019) 245:22–7. doi: 10.1016/j.jad.2018.10.111
23. Rivaz M, Asadi F, Mansouri P. Assessment of the relationship between nurses' perception of ethical climate and job burnout in intensive care units. Invest Educ Enferm. (2020) 38:e12. doi: 10.17533/udea.iee.v38n3e12
24. Ahola K. Occupational Burnout and Health. Finland: Tampereen Yliopistopaino Oy-Juvenes Print (2007). p. 23–35.
25. La Torre G, Sestili C, Imeshtari V, Masciullo C, Rizzo F, Guida G, et al. Association of health status, sociodemographic factors and burnout in healthcare professionals: results from a multicentre observational study in Italy. Public Health. (2021) 195:15–7. doi: 10.1016/j.puhe.2021.04.004
26. Arrogante O, Aparicio-Zaldivar EG. Burnout syndrome in intensive care professionals: relationships with health status and wellbeing. Enfermería Intensiva. (2020) 31:60–70. doi: 10.1016/j.enfie.2019.03.004
27. Jiang M, Zhang W, Su X, Gao C, Chen B, Feng Z, et al. Identifying and measuring the severity of somatic symptom disorder using the self-reported somatic symptom scale-China (SSS-CN): a research protocol for a diagnostic study. BMJ Open. (2019) 9:e024290. doi: 10.1136/bmjopen-2018-024290
28. Wei Z, Xiaoping L, Zhiming W. The study of construct validity and reliability of the Maslach burnout inventory-general survey (MBI-GS) for nurses. Chin J Behav Med Sci. (2007) 16:849–51. doi: 10.3760/cma.j.issn.1674-6554.2007.09.031
29. Yueping G, Mingzhi X. Job burnout scale-general survey: development, reliability, and validity. Chin Gen Pract. (2017) 20:4167–73. doi: 10.3969/j.issn.1007-9572.2017.00.121
30. Commander SJ, Ellis D, Williamson H, Grabski D, Sallah AY, Derbew M, et al. Predictors of burnout and depression in surgeons practicing in east, central, and southern Africa. J Surg Res. (2020) 255:536–48. doi: 10.1016/j.jss.2020.04.038
31. Malaquin S, Mahjoub Y, Musi A, Zogheib E, Salomon A, Guilbart M, et al. Burnout syndrome in critical care team members: a monocentric cross sectional survey. Anaesth Crit Care Pain Med. (2017) 36:223–8. doi: 10.1016/j.accpm.2016.06.011
32. Maroti D, Lumley MA, Schubiner H, Lilliengren P, Bileviciute-Ljungar I, Ljótsson B, et al. Internet-based emotional awareness and expression therapy for somatic symptom disorder: a randomized controlled trial. J Psychosom Res. (2022) 163:111068. doi: 10.1016/j.jpsychores.2022.111068
33. Matthew J, Mike L, Huang HC, Wang CH, Shih CY, Chen YC, et al. Effects of personalized music intervention on nurse burnout: a feasibility randomized controlled trial. Nurs Health Sci. (2022) 24:836–44. doi: 10.1111/nhs.12984
34. Wei R, Ji H, Li J, Zhang L. Active intervention can decrease burnout in Ed nurses. J Emerg Nurs. (2017) 43:145–9. doi: 10.1016/j.jen.2016.07.011
35. Luo L, Li J, Wu F, Peng X, Zhou F. Investigation of occupational burnout status and influencing factors among emergency department healthcare workers using the MBI-GS scale. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2024) 49:981–8. doi: 10.11817/j.issn.1672-7347.2024.230415
36. Lupo R, Lezzi A, Conte L, Santoro P, Carvello M, Artioli G, et al. Work environment and related burnout levels: survey among healthcare workers in two hospitals of southern Italy. Acta Biomed. (2021) 92:e2021009. doi: 10.23750/abm.v92iS2.11307
37. Tong L, Zhu L, Zhang H, Zhong L, Diao D, Chen X, et al. Effort-reward imbalance and health outcomes in emergency nurses: the mediating role of work-family conflict and intrinsic effort. Front Public Health. (2025) 12:1515593. doi: 10.3389/fpubh.2024.1515593
38. Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. (2015) 52:649–61. doi: 10.1016/j.ijnurstu.2014.11.004
39. Serrano FT, Calderón Nossa LT, Gualdrón Frías CA, Mogollón GJD, Mejía CR. Burnout syndrome and depression in students of a Colombian medical school, 2018. Rev Colomb Psiquiatr. (2023) 52:345–51. doi: 10.1016/j.rcpeng.2021.09.001
40. von Känel R, Princip M, Holzgang SA, Fuchs WJ, van Nuffel M, Pazhenkottil AP, et al. Relationship between job burnout and somatic diseases: a network analysis. Sci Rep. (2020) 10:18438. doi: 10.1038/s41598-020-75611-7
41. Alexander GK, Rollins K, Walker D, Wong L, Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf . (2015) 63:462–70. doi: 10.1177/2165079915596102
42. Gulen B, Serinken M, Eken C, Karcioglu Ö, Kucukdagli OT, Kilic E, et al. Serum S100B as a surrogate biomarker in the diagnoses of burnout and depression in emergency medicine residents. Acad Emerg Med. (2016) 23:786–9. doi: 10.1111/acem.12973
43. Pilger A, Haslacher H, Meyer BM, Lackner A, Nassan-Agha S, Nistler S, et al. Midday and nadir salivary cortisol appear superior to cortisol awakening response in burnout assessment and monitoring. Sci Rep. (2018) 8:9151. doi: 10.1038/s41598-018-27386-1
44. Zhang H, Zhou J, Zhong L, Zhu L, Chen X. Relationship between workplace violence and occupational health in emergency nurses: the mediating role of dyssomnia. Nurs Crit Care. (2025) 30:e70008. doi: 10.1111/nicc.70008
45. Borgmann LS, Kroll LE, Müters S, Rattay P, Lampert T. Work-family conflict, self-reported general health and work-family reconciliation policies in Europe: results from the European working conditions survey 2015. SSM Popul Health. (2019) 9:100465. doi: 10.1016/j.ssmph.2019.100465
46. Borgmann LS, Rattay P, Lampert T. Health-related consequences of work-family conflict from a European perspective: results of a scoping review. Front Public Health. (2019) 7:189. doi: 10.3389/fpubh.2019.00189
47. Haghighinejad H, Ghazipoor H, Jafari P, Taghipour K, Rezaie M, Liaghat L, et al. Investigating the impact of modified mindfulness-based stress reduction (MBSR) program on occupational burnout and other mental health status among nonmedical staff in a hospital: a randomized controlled trial. Int Arch Occup Environ Health. (2022) 95:2005–16. doi: 10.1007/s00420-022-01902-3
48. Hilcove K, Marceau C, Thekdi P, Larkey L, Brewer MA, Jones K. Holistic nursing in practice: mindfulness-based yoga as an intervention to manage stress and burnout. J Holist Nurs. (2021) 39:29–42. doi: 10.1177/0898010120921587
49. Medisauskaite A, Kamau C. Reducing burnout and anxiety among doctors: randomized controlled trial. Psychiatry Res. (2019) 274:383–90. doi: 10.1016/j.psychres.2019.02.075
50. Kaplow R, Willis P, Steele D, Swann J, Feistritzer NR. Clinician wellbeing and mental health assessment across two acute care hospitals during the COVID-19 pandemic. Nurs Adm Q. (2024) 48:325–35. doi: 10.1097/NAQ.0000000000000645
51. Diao D, Chen X, Zhong L, Zhang H, Zhang J. Sex differences in burnout and work-family conflict among Chinese emergency nurses: a cross-sectional study. Front Public Health. (2024) 12:1492662. doi: 10.3389/fpubh.2024.1492662
52. Shokri-Kojori E, Wang GJ, Wiers CE, Demiral SB, Guo M, Kim SW, et al. β-amyloid accumulation in the human brain after one night of sleep deprivation. Proc Natl Acad Sci USA. (2018) 115:4483–8. doi: 10.1073/pnas.1721694115
53. Morgenthaler TI, Lee-Chiong T, Alessi C, Friedman L, Aurora RN, Boehlecke B, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm dyssomnia. An American academy of sleep medicine report. Sleep. (2007) 30:1445–59. doi: 10.1093/sleep/30.11.1445
54. Turnbach E, Coates L, Vanek FD, Cotter E, Pogue CA, Clark RRS, United States Clinician Well-being Study Consortium, Philadelphia, PA, et al. Emergency nurses' well-being in magnet hospitals and recommendations for improvements in work environments: a multicenter cross-sectional observational study. J Emerg Nurs. (2024) 50:153–60. doi: 10.1016/j.jen.2023.06.012
Keywords: somatization symptoms, burnout, emergency nurse, mental health, sleep disturbances
Citation: Li N, Xie N, Chen X, Zhang H, Zhong L, Diao D, Zhu L and Zhou Y (2025) Somatization symptoms and burnout: a correlational study among emergency nurses. Front. Public Health 13:1647123. doi: 10.3389/fpubh.2025.1647123
Received: 14 June 2025; Accepted: 29 July 2025;
Published: 19 August 2025.
Edited by:
Petros Galanis, National and Kapodistrian University of Athens, GreeceReviewed by:
Amel Moustafa, Damanhour University, EgyptFrancisco Palencia-Sánchez, Pontifical Javeriana University, Colombia
Copyright © 2025 Li, Xie, Chen, Zhang, Zhong, Diao, Zhu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Zhou, MjU4MzA0NDYwNUBxcS5jb20=
 Ningxiang Li
Ningxiang Li Nan Xie1,2,3
Nan Xie1,2,3 Xiaoli Chen
Xiaoli Chen Hao Zhang
Hao Zhang Dongmei Diao
Dongmei Diao Ling Zhu
Ling Zhu