- 1Department of Thoracic Surgery, The Affiliated Cancer Hospital of Zhengzhou University & Henan Cancer Hospital, Zhengzhou, Henan, China
- 2Department of Physical Medicine and Rehabilitation, Xiangya Hospital Central South University, Changsha, Hunan, China
Introduction: This study aimed to assess the knowledge, attitudes, and practices (KAP) of esophageal cancer patients concerning pulmonary rehabilitation training.
Methods: A cross-sectional study was conducted at the Henan Cancer Hospital from July 1, 2024, to August 31, 2024. Data were collected through questionnaires that gathered demographic information and KAP scores.
Results: A total of 530 esophageal cancer patients participated, including 197 (37.17%) regular smokers and 145 (27.36%) regular alcohol consumers. The mean ± SD scores were 7.78 ± 4.56 for knowledge (range: 0–20), 40.42 ± 4.66 for attitudes (range: 10–50), and 21.13 ± 3.08 for practices (range: 5–25). Correlation analyses showed positive relationships between knowledge and attitude scores (r = 0.335, p < 0.001), knowledge and practice scores (r = 0.323, p < 0.001), and attitude and practice scores (r = 0.567, p < 0.001). Structural Equation Modeling (SEM) indicated significant effects of knowledge on attitude (β = 0.420, p < 0.001) and attitude on practice (β = 0.711, p < 0.001).
Conclusion: Esophageal cancer patients showed inadequate knowledge but positive attitudes and proactive practices regarding pulmonary rehabilitation. These findings highlight the need for targeted educational interventions to improve patient knowledge, enhancing overall engagement in rehabilitation practices.
Introduction
Esophageal cancer ranks seventh in incidence and sixth in mortality among all malignancies globally, with a higher prevalence in men, particularly those aged 60 to 70 years (1). In 2020, there were approximately 604,000 new cases and 544,000 deaths worldwide, with significant regional variations in incidence and mortality. The highest incidence rates were observed in Eastern Asia and Southern and Eastern Africa, driven by specific risk factors such as tobacco use, alcohol consumption, hot beverage intake, and indoor air pollution. Projections indicate that the global burden of esophageal cancer will increase by over 50% from 2020 to 2040, reaching nearly 1 million new cases annually (2).
Esophagectomy is the cornerstone of treatment for resectable esophageal cancer; however, it carries higher morbidity and mortality rates compared to other gastrointestinal surgeries (3, 4). Although esophagectomy is crucial for treating esophageal cancer, the surgical procedure may compress the lungs and damage thoracic muscles, leading to postoperative pulmonary complications such as respiratory dysfunction, atelectasis, and even respiratory failure. These complications can severely impair patients’ quality of life and hinder recovery, further complicating postoperative treatments (5, 6). Pulmonary morbidity is a common complication following esophagectomy, with recent studies reporting that it still occurs in 16 to 23% of cases despite improvements (4, 7–9). Pulmonary complications are also a major cause of hospital mortality and may independently predict poorer long-term survival (10, 11). Pulmonary rehabilitation plays a vital role in mitigating these postoperative complications. Through interventions such as respiratory function training and guided physical exercises, pulmonary rehabilitation can effectively improve lung function, alleviate breathing difficulties, and enhance exercise tolerance after surgery. Long-term, systematic respiratory training has been widely recognized for its ability to improve lung function and reduce the incidence of complications following thoracic surgeries, including esophagectomy, ultimately improving patients’ overall survival and quality of life. From this perspective, incorporating pulmonary rehabilitation into postoperative care is increasingly being emphasized in clinical practice (5, 12).
KAP (Knowledge, Attitude, and Practice) theory emphasizes that knowledge is the foundation for behavior change, while attitudes and beliefs serve as the driving force behind such changes (13). According to KAP theory, behavior change progresses through three stages: acquiring knowledge, forming attitudes and beliefs, and finally, adopting practices and behaviors (14). However, knowledge alone does not automatically lead to behavior change; it must first alter perceptions, which in turn drive behavioral adjustments (15).
China is among the top five countries with the highest incidence of esophageal cancer, with Linxian in Henan Province and Cixian and Shexian in Hebei Province reporting the highest incidence rates globally (1, 16). While esophagectomy remains a critical treatment for resectable esophageal cancer, the high rates of postoperative pulmonary complications greatly affect patient recovery and long-term survival (17, 18). Therefore, understanding the KAP of esophageal cancer patients regarding pulmonary rehabilitation training is essential for developing targeted educational and intervention strategies. Effective strategies could improve rehabilitation outcomes by enhancing lung function, reducing pulmonary complications, and improving the patients’ quality of life following surgery. Given the importance of this issue, research focusing on this population is crucial for informing clinical practice and optimizing rehabilitation approaches.
Currently, there is a lack of KAP studies specifically addressing pulmonary rehabilitation in this patient population. Unlike previous KAP studies in oncology, this research specifically targets pulmonary rehabilitation among esophageal cancer patients and employs both conventional statistical analyses and structural equation modeling (SEM) to elucidate the interrelationships among knowledge, attitudes, and practices. This design provides new insights into behavioral factors influencing rehabilitation engagement and offers an evidence base for developing targeted educational strategies in this high-risk surgical population. This study aimed to assess the KAP of esophageal cancer patients concerning pulmonary rehabilitation training.
Materials and methods
Study design and participants
This cross-sectional study was conducted at the Henan Cancer Hospital from July 1, 2024, to August 31, 2024, involving esophageal cancer patients. This study was approved by the Ethic Committee of Henan Cancer Hospital (2024–282), and all participants provided written informed consent.
Inclusion Criteria: Patients diagnosed with esophageal cancer through clinical and auxiliary examinations, those eligible for radical esophageal cancer surgery, and those without a history of mental illness or communication barriers.
Exclusion Criteria: Patients who were uncooperative or demonstrated poor treatment adherence, pregnant or breastfeeding patients, those with congenital deformities or congenital diseases, patients with severe diseases of major organs or acute/chronic infections, and those with severe liver or kidney dysfunction or acute/chronic diseases.
Questionnaires were distributed to participants in both electronic and paper formats.
Questionnaire introduction
The questionnaire was developed based on relevant guidelines and literature (19–21). Following its initial design, the questionnaire was revised according to feedback from three experts, including two rehabilitation specialists, and a pilot test was conducted with 30 participants. The questionnaire demonstrated a reliability coefficient of 0.911.
The final questionnaire, written in Chinese, comprised four dimensions with a total of 37 items: Basic Information (11 items), Knowledge Dimension (11 items, including a trap question as the 8th item to identify invalid responses), Attitude Dimension (10 items), and Practice Dimension (5 items). For statistical analysis, scores were assigned according to the number of response options. In the Knowledge Dimension, responses of “very familiar” were scored 2 points, “heard of” 1 point, and “not clear” 0 points, with a total possible score ranging from 0 to 20 points. In the Attitude Dimension, items A1-A5 (positive attitude) were scored from 5 points (“strongly agree”) to 1 point (“strongly disagree”), while items A6-A10 (negative attitude) were reverse-scored from 1 point (“strongly agree”) to 5 points (“strongly disagree”), resulting in a total possible score ranging from 10 to 50 points. In the Practice Dimension, responses ranged from 5 points (“always”) to 1 point (“never”), with a total possible score ranging from 5 to 25 points (Supplementary Questionnaire). A scoring threshold of greater than 70% was established for each dimension to define adequate knowledge, positive attitudes, and proactive practices (22).
This study was conducted at a single center. The questionnaires were distributed in both electronic format via the Wenjuanxing platform and paper format with QR codes in outpatient and inpatient settings. A total of 578 questionnaires were collected from willing participants. Of these, 35 were incomplete or involved mid-study withdrawals, and 10 were discarded due to careless or random responses. After excluding 1 questionnaire from a participant under 18 years old and 2 questionnaires with logical errors in the trap question, 530 valid questionnaires were included in the final analysis.
Sample size calculation
The sample size was calculated using the formula for determining the minimum sample size in cross-sectional studies:
Where α = 0.05.
.
δ = 0.05.
p = 0.5.
.
This calculation resulted in a minimum required sample size of 384. Considering an anticipated effective questionnaire return rate of 80%, a minimum of 480 questionnaires were planned to be collected.
Statistical methods
Descriptive statistics will be utilized for demographic data and KAP scores, with continuous data presented as means and standard deviations (SD), and categorical responses reported as n (%). Differences in knowledge (K), attitudes (A), and practices (P) scores across different demographic groups will be compared using t-tests for two-group comparisons and ANOVA for comparisons among three or more groups. Multivariate regression analysis will be performed with practice scores as the dependent variable to examine the relationships among demographic characteristics, knowledge, attitudes, and practices. Practice scores will be dichotomized based on 70% of the maximum score, and all relevant variables will be included in the regression model. p-values will be reported to three decimal places, with p < 0.05 considered statistically significant. Statistical analyses will be conducted using SPSS 26.0 and AMOS 26.0 (IBM, Armonk, NY, United States).
Results
Basic information on the population
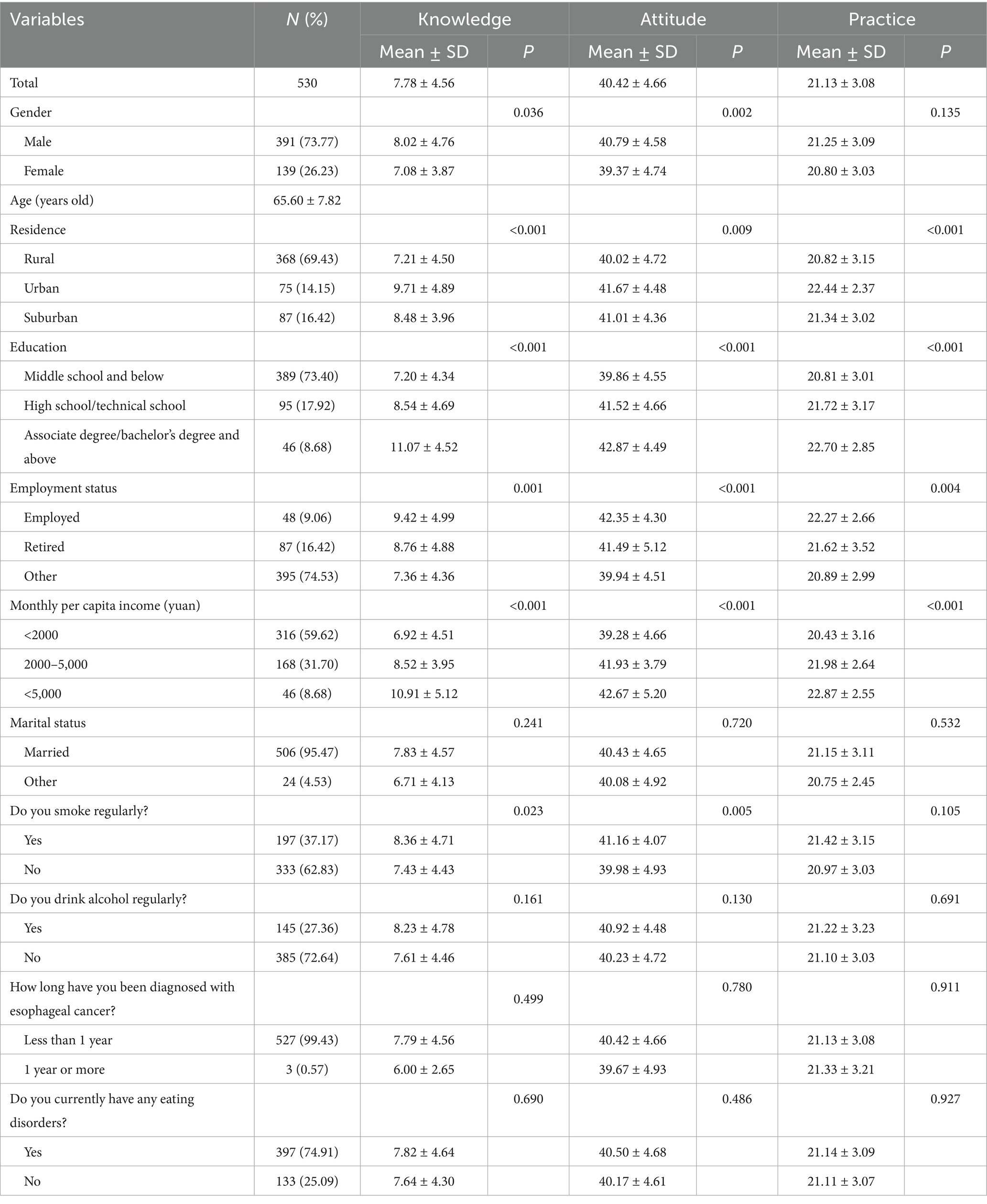
Among the 530 esophageal cancer patients included in this study, 391 (73.77%) were male, with a mean age of 65.60 ± 7.82 years. A total of 389 participants (73.40%) had an educational level of middle school or below, 316 (59.62%) had a monthly per capita income of less than 2,000 yuan, 197 (37.17%) were regular smokers, 145 (27.36%) regularly consumed alcohol, and 397 (74.91%) currently had eating disorders. The mean ± SD scores for knowledge, attitude, and practice were 7.78 ± 4.56, 40.42 ± 4.66, and 21.13 ± 3.08, respectively. Analysis of demographic characteristics revealed that knowledge, attitude, and practice scores varied significantly by residence (p < 0.001, p = 0.009, p < 0.001), education level (p < 0.001, p < 0.001, p < 0.001), employment status (p = 0.001, p < 0.001, p = 0.004), and monthly per capita income (p < 0.001, p < 0.001, p < 0.001). Additionally, knowledge and attitude scores differed significantly by gender (p = 0.036, p = 0.002) and smoking status (p = 0.023, p = 0.005) (Table 1).
Knowledge attitude practice
In the knowledge dimension, the three questions with the highest proportion of participants selecting “Not clear” were: “Do you know that during pulmonary rehabilitation training, the intensity should be moderate to high (where the patient feels slightly breathless and fatigued but can continue) to achieve optimal benefits?” (K6) with 43.77%, “Do you know that pulmonary rehabilitation training is a personalized comprehensive intervention conducted after a thorough assessment of the patient’s condition?” (K3) with 43.40%, and “Do you know that if symptoms such as cough, sputum production, or worsening of breathing difficulties occur due to a cold or other reasons, pulmonary rehabilitation training should only be resumed after at least 2 weeks of symptom relief?” (K7) with 42.26% (Supplementary Table S1).
Regarding attitude, 11.13% agreed that “pulmonary rehabilitation training is less important than other preoperative preparations because it takes too long to show effects” (A6), 7.36% agreed that “even if the pulmonary rehabilitation program is strictly followed, it might not be effective, so there is no need for strict adherence” (A7), and 6.04% agreed that “their family might not cooperate with or support them in carrying out pulmonary rehabilitation training” (A9) (Supplementary Table S2).
For the practice dimension, 16.79% sometimes and 3.40% seldom shared knowledge about esophageal cancer and the preoperative pulmonary rehabilitation program with friends and relatives to gain their support (P4), 13.40% sometimes and 5.09% seldom sought to learn relevant knowledge (P1), and 11.70% sometimes and 1.32% seldom maintained a positive attitude toward esophageal cancer treatment and pulmonary rehabilitation training, believing that this attitude would ultimately benefit them (P5) (Supplementary Table S3).
Correlations between KAP
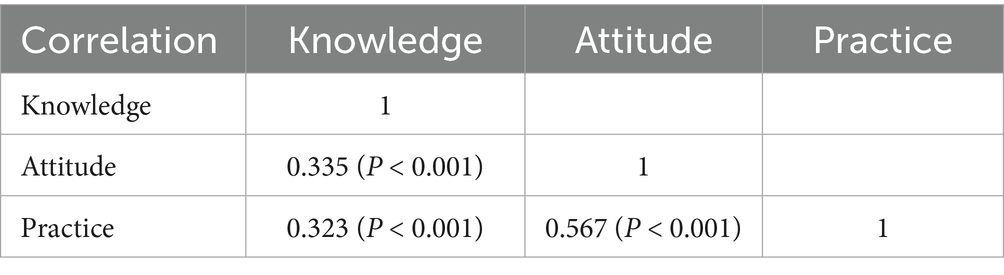
Further correlation analysis revealed positive correlations between knowledge scores and attitude scores (r = 0.335, p < 0.001), between knowledge scores and practice scores (r = 0.323, p < 0.001), and between attitude scores and practice scores (r = 0.567, p < 0.001) (Table 2).
Factors associated with KAP
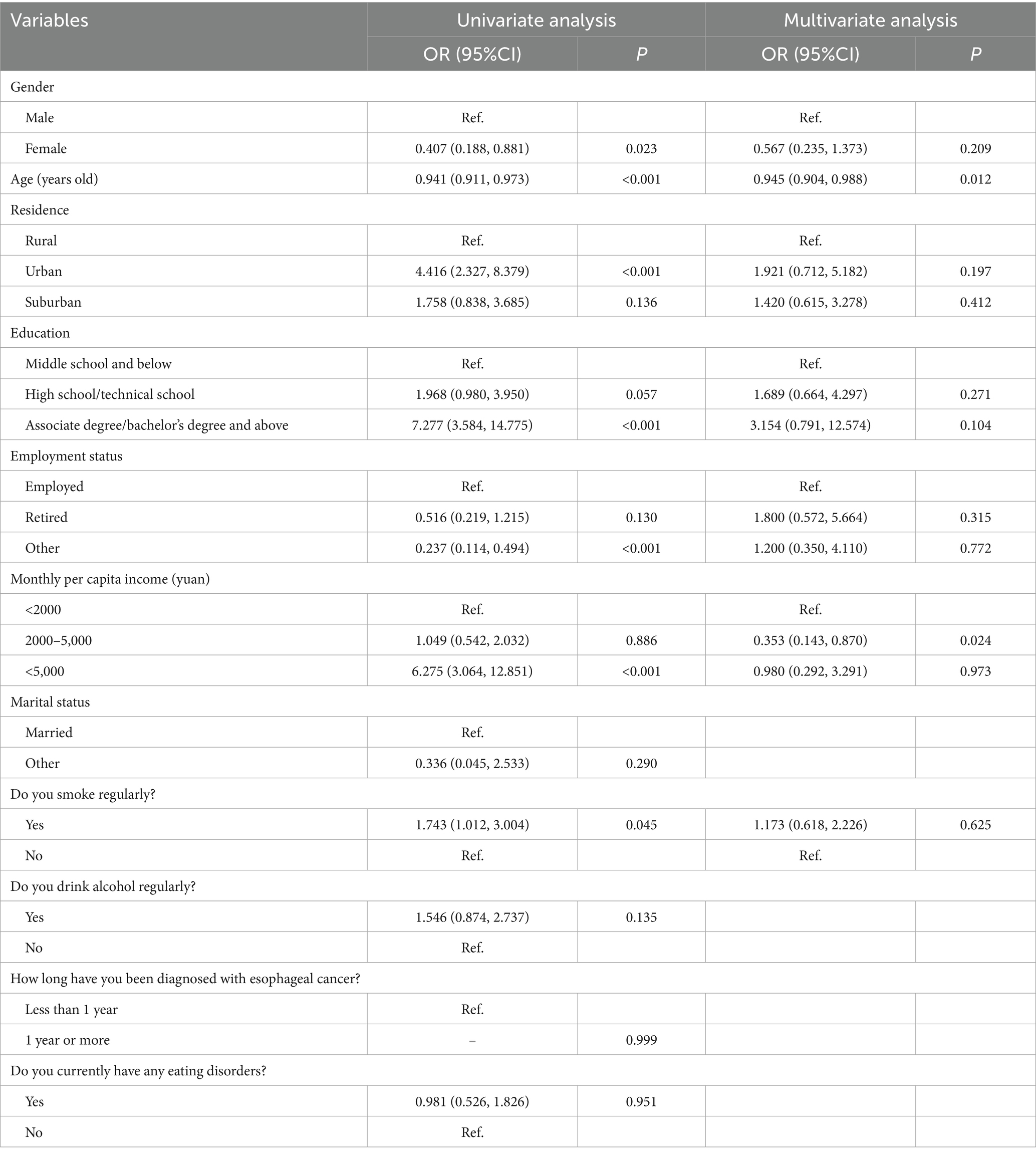
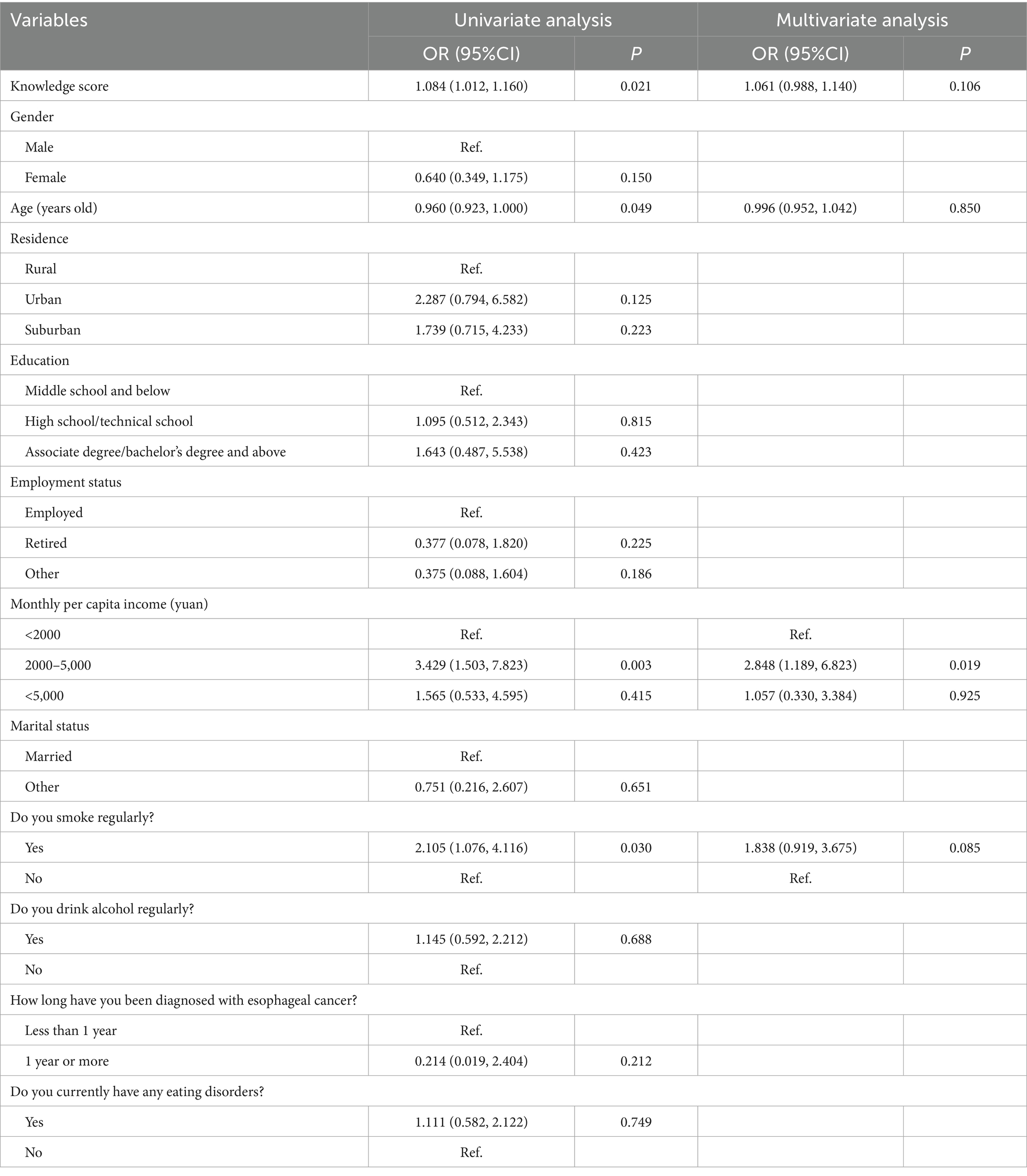
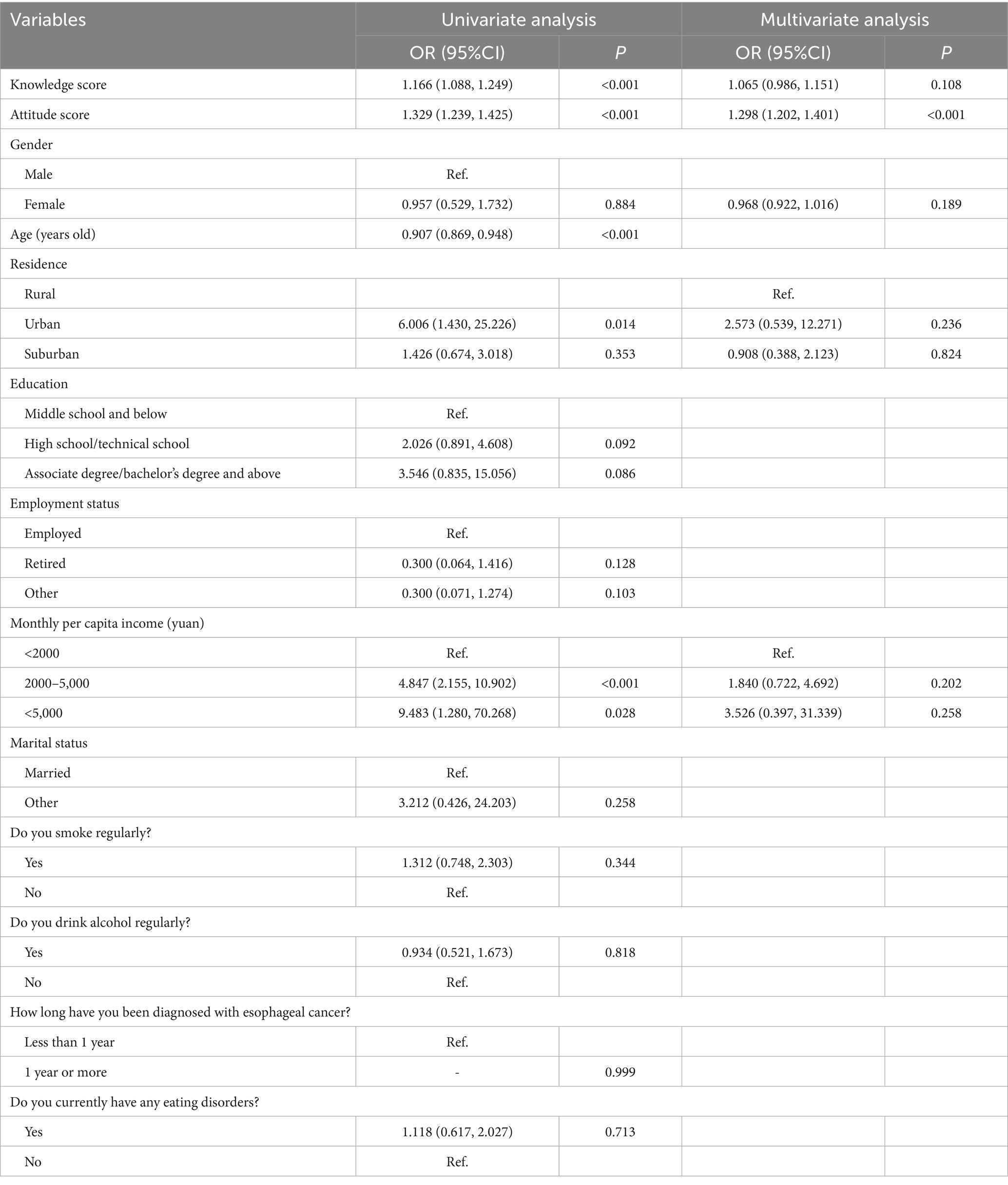
Multivariate logistic regression analysis showed that age (OR = 0.945, 95% CI: [0.904, 0.988], p = 0.012) and a monthly per capita income of 2,000–5,000 yuan (OR = 0.353, 95% CI: [0.143, 0.870], p = 0.024) were independently associated with knowledge (Table 3). Additionally, a monthly per capita income of 2,000–5,000 yuan (OR = 2.848, 95% CI: [1.189, 6.823], p = 0.019) was independently associated with a positive attitude (Table 4). Moreover, the attitude score (OR = 1.298, 95% CI: [1.202, 1.401], p < 0.001) was independently associated with proactive practice (Table 5).
Interactions between KAP
The Structural Equation Modeling (SEM) analysis demonstrated good model fit with the following indices: RMSEA = 0.060, IFI = 0.924, TLI = 0.913, and CFI = 0.924 (Supplementary Table S1). The results indicated a significant direct effect of knowledge on attitude (β = 0.420, p < 0.001) and of attitude on practice (β = 0.711, p < 0.001), while the direct effect of attitudes on practice was not significant (β = 0.092, p = 0.073) (Supplementary Table S2 and Figure 1).
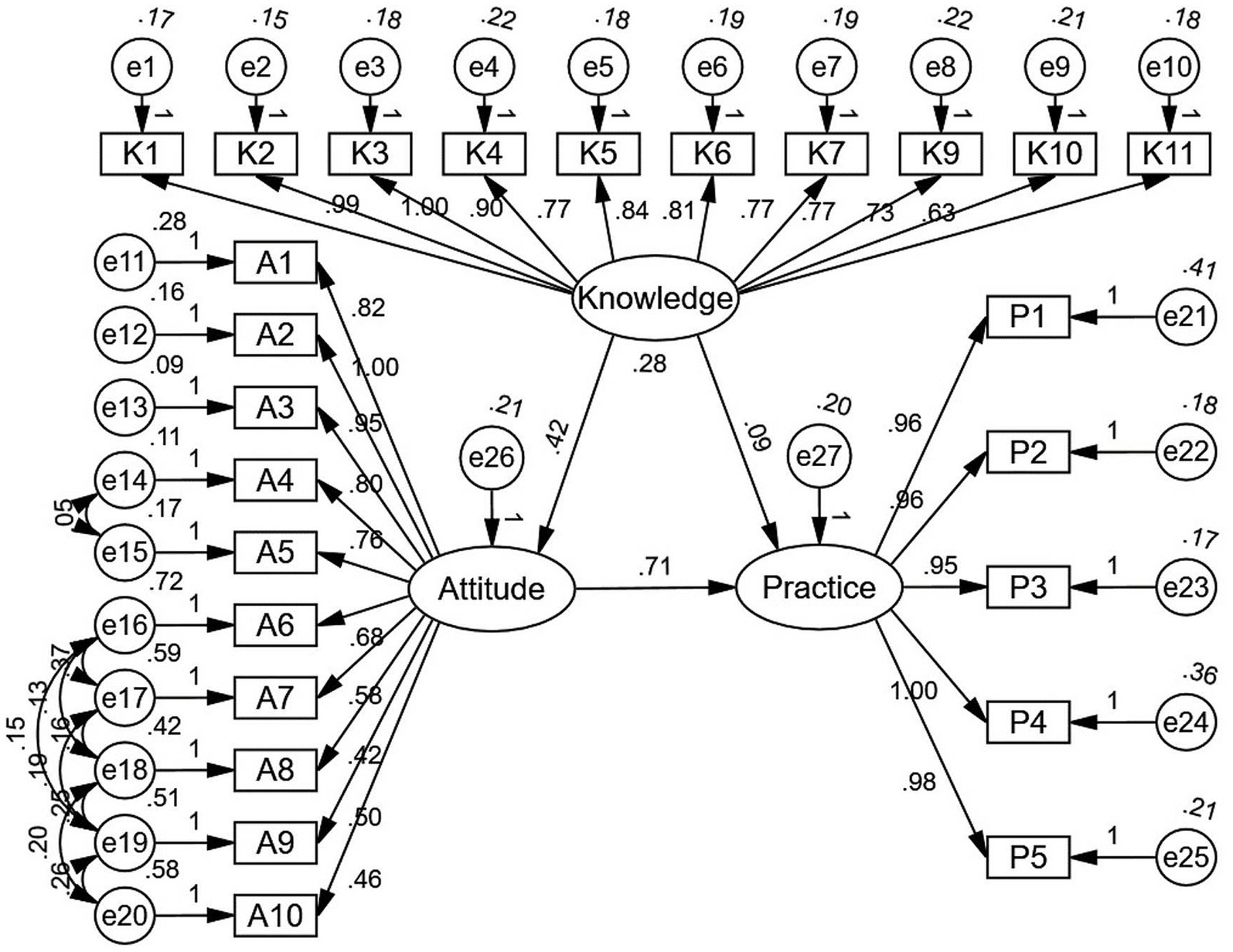
Figure 1. SEM analysis result. This figure presents the path model for Knowledge, Attitude, and Practice (KAP) variables, displaying the relationships among various indicators. The standardized path coefficients are shown along each arrow, indicating the strength of the relationship between constructs. Circles labeled e1–e27 represent error terms associated with each observed variable, while the elliptical shapes represent the latent variables of Knowledge, Attitude, and Practice. Direct effects are denoted by arrows, with significant pathways indicating strong relationships between Knowledge and Attitude (0.42), Attitude and Practice (0.71), and Knowledge and Practice (0.28). Indicator variables (K1-K11 for Knowledge, A1-A10 for Attitude, and P1-P5 for Practice) show their respective factor loadings, demonstrating their contribution to the latent constructs.
Discussion
Esophageal cancer patients demonstrated inadequate knowledge but maintained positive attitudes and proactive practices concerning pulmonary rehabilitation training. These findings suggest the need for targeted educational interventions to enhance patients’ knowledge, which may further strengthen their attitudes and practices in clinical settings.
The results of this study show that while esophageal cancer patients demonstrated positive attitudes and proactive practices toward pulmonary rehabilitation training, their knowledge was notably inadequate. This finding is consistent with other studies, which have similarly reported low awareness, skepticism about the necessity, and limited acceptance of pulmonary rehabilitation among COPD patients in China (23). Additionally, there remains a significant gap in understanding and referral practices for pulmonary rehabilitation among Chinese respiratory physicians, further limiting access for patients with chronic respiratory diseases (24). The positive attitudes and proactive behaviors observed in this study suggest that patients are generally willing to engage in rehabilitation. However, the lack of knowledge may hinder them from fully benefiting from these programs. This gap between attitude and knowledge highlights the critical need for targeted educational interventions to ensure that patients are adequately informed and able to effectively participate in pulmonary rehabilitation. In addition to individual knowledge and socioeconomic disparities, difficulties in follow-up and limited accessibility to medical personnel may also hinder effective pulmonary rehabilitation among cancer patients. In real-world clinical settings, many patients have limited opportunities to communicate with their physicians due to short consultation times and heavy workloads in oncology departments. Consequently, important issues such as medication side effects, symptom management, and the rationale behind rehabilitation training are often insufficiently discussed. Establishing regular follow-up systems and enhancing doctor–patient communication could therefore be crucial to improving patients’ understanding, adherence, and overall participation in pulmonary rehabilitation programs. Furthermore, the rise of artificial intelligence–based medical platforms and telemedicine systems has greatly improved patients’ ability to follow up and understand their treatment processes. These technologies facilitate continuous communication between patients and healthcare providers, enhance access to educational resources, and enable personalized rehabilitation guidance even outside hospital settings. Such innovations have shown promising applications in esophageal surgery and postoperative care, providing new opportunities for improving patient outcomes (25–27).
The findings from correlation analysis, multivariate logistic regression, and SEM all indicate significant interconnections. These results were supported by the SEM analysis, which demonstrated that knowledge had a significant direct effect on attitude (β = 0.420, p < 0.001) and attitude on practice (β = 0.711, p < 0.001). However, the direct effect of knowledge on practice was not significant (β = 0.092, p = 0.073), suggesting that attitudes may act as a mediator between knowledge and practice. This highlights the importance of not only improving patients’ knowledge but also ensuring that their attitudes are aligned with evidence-based practices to encourage positive behavioral outcomes (28, 29). In this model, knowledge appears to influence practice primarily through its effect on attitudes rather than through a direct pathway. This finding suggests that simply increasing patients’ knowledge about pulmonary rehabilitation may not be sufficient unless it is accompanied by changes in their beliefs and motivation toward participation. Educational efforts that connect factual understanding with perceived personal benefit may therefore play a key role in strengthening this indirect pathway.
When examining the individual variables, several significant associations were identified. For gender, male patients exhibited significantly higher knowledge (p = 0.036) and attitude scores (p = 0.002) compared to female patients. However, no significant difference was found in practice scores (p = 0.135). This could indicate that while men may be more informed and maintain a positive outlook toward pulmonary rehabilitation, both genders face similar barriers when it comes to implementing these practices. Residence was another important factor, with urban and suburban patients scoring higher in knowledge (p < 0.001), attitude (p = 0.009), and practice (p < 0.001) compared to rural patients. This may be attributed to better access to healthcare resources and educational materials in urban and suburban areas. Rural patients often face challenges such as limited access to healthcare services and lower health literacy, which could explain their lower scores across all three dimensions (30, 31).
Educational level was strongly associated with KAP scores, where patients with higher education levels demonstrated significantly better knowledge (p < 0.001), attitudes (p < 0.001), and practices (p < 0.001). This is consistent with existing literature indicating that education is a key determinant of health literacy and health-related behaviors (32, 33). The multivariate logistic regression analysis supported this, showing that higher education was independently associated with better knowledge and attitudes, which subsequently influenced practice scores. Employment status also showed significant differences in all KAP dimensions. Employed and retired patients scored higher in knowledge (p = 0.001), attitude (p < 0.001), and practice (p = 0.004) compared to those in other employment categories. This could be due to greater social support and access to information among employed and retired individuals. Interestingly, multivariate analysis indicated that employment status was not an independent predictor of KAP outcomes, suggesting that other factors, such as income and education, might mediate these relationships (34, 35).
Monthly per capita income was another significant variable, with higher income being associated with better knowledge (p < 0.001), attitudes (p < 0.001), and practices (p < 0.001). This association was further confirmed by multivariate logistic regression, which showed that a monthly income of 2,000–5,000 yuan was independently associated with better knowledge (OR = 0.353, 95% CI: [0.143, 0.870], p = 0.024) and attitudes (OR = 2.848, 95% CI: [1.189, 6.823], p = 0.019). Higher income likely provides better access to healthcare resources, educational materials, and a supportive environment, facilitating better health outcomes (36).
Interestingly, significant differences in KAP were not observed across marital status, smoking, or alcohol consumption for practice scores, despite differences in knowledge and attitudes. For example, regular smokers had higher knowledge (p = 0.023) and attitude (p = 0.005) scores compared to non-smokers, yet no significant difference was observed in practice scores (p = 0.105). This lack of difference in practice might be attributed to external factors such as limited access to resources or support for behavioral changes, suggesting that improving knowledge alone may not be sufficient to translate into better practices without addressing these underlying barriers (37).
The distribution of responses across the knowledge, attitude, and practice dimensions indicates several areas where esophageal cancer patients exhibit inadequate understanding, particularly regarding the principles and importance of pulmonary rehabilitation. A significant portion of the patients were unclear about key aspects of pulmonary rehabilitation, such as its components, intensity, and the necessity for personalization based on specific health conditions. For instance, nearly half of the patients were unfamiliar with the importance of moderate to high-intensity training during pulmonary rehabilitation, and many did not recognize that rehabilitation could continue effectively outside of a hospital setting. These findings are consistent with similar studies in which patients often show limited understanding of complex medical regimens, leading to suboptimal engagement and outcomes (38). On the other hand, the attitude and practice dimensions revealed generally positive responses, with the majority of patients expressing interest and willingness to participate in rehabilitation, although a small subset harbored misconceptions or doubts about its effectiveness.
Given these knowledge gaps, targeted educational interventions are essential. First, tailored educational materials should be developed to clearly explain the specific benefits of pulmonary rehabilitation, emphasizing the role of high-intensity training and the flexibility of performing these exercises outside the hospital. These materials could include visual aids, simplified language, and practical examples that resonate with patients’ everyday experiences. In addition, hands-on workshops or interactive sessions led by healthcare professionals could enhance patient understanding and retention of this information (39–41).
Considering the significant disparities observed in knowledge across different demographic groups, specific strategies should be implemented to address these gaps. For example, rural patients and those with lower educational levels demonstrated notably poorer knowledge scores. For these groups, community-based programs that leverage local healthcare workers could be particularly effective. Such programs might include home visits or small group sessions that offer personalized education and support, thereby overcoming barriers related to health literacy and access. Moreover, employing digital platforms like mobile apps tailored to deliver bite-sized, easy-to-understand information on pulmonary rehabilitation could reach a broader audience, particularly among younger or tech-savvy patients (42, 43).
To improve the more challenging aspects, such as the misunderstanding about the necessity of strict adherence to rehabilitation plans, motivational interviewing techniques could be integrated into routine care. This approach has been shown to effectively change health behaviors by aligning the intervention with patients’ personal values and goals (44, 45). Additionally, addressing concerns related to the potential for harm or the perceived burden of rehabilitation on family dynamics should be a priority. Structured family counseling sessions, where both patients and their families receive clear guidance on the benefits and practical aspects of rehabilitation, could alleviate these concerns and foster a supportive environment.
This study has several limitations. First, as a cross-sectional study, it captures only a snapshot of the participants’ KAP at a single point in time, limiting the ability to assess changes over time or causality. Future research may include longitudinal or interventional designs to explore how knowledge, attitudes, and practices evolve over time and to examine whether targeted educational measures can lead to measurable behavioral improvements. Second, the data were collected using self-reported questionnaires, which may introduce response bias, particularly in sensitive areas such as smoking and alcohol consumption. Because the responses were self-reported, some participants might have provided socially desirable answers or understated certain behaviors. Although the questionnaire included a control item to identify inconsistent responses, self-reporting bias cannot be completely ruled out. Third, the study was conducted at a single cancer hospital, which may limit the generalizability of the findings to other populations or settings. Because the participants were all recruited from one institution, the findings should be interpreted with some caution. Differences in healthcare resources, patient education, and rehabilitation practices in other regions may lead to somewhat different outcomes. Future studies involving several centers could help verify whether these patterns hold in broader contexts.
In conclusion, esophageal cancer patients demonstrated inadequate knowledge, positive attitudes, and proactive practices concerning pulmonary rehabilitation training. These findings highlight the need for targeted educational interventions to enhance patients’ knowledge, which may further strengthen their attitudes and practices toward pulmonary rehabilitation, ultimately improving their overall treatment outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Henan Cancer Hospital (2024–282). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WW: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. WX: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. PC: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. HS: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. ZW: Conceptualization, Writing – original draft, Writing – review & editing. YZ: Data curation, Writing – original draft, Writing – review & editing. YY: Formal analysis, Writing – original draft, Writing – review & editing. DZ: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Henan provincial Medical Science and Technology Research Project (LHGJ20220195).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1647650/full#supplementary-material
References
1. Bray, F, Ferlay, J, Soerjomataram, I, Siegel, RL, Torre, LA, and Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
2. Morgan, E, Soerjomataram, I, Rumgay, H, Coleman, HG, Thrift, AP, Vignat, J, et al. The global landscape of Esophageal squamous cell carcinoma and Esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: new estimates from GLOBOCAN 2020. Gastroenterology. (2022) 163:649–58.e2. doi: 10.1053/j.gastro.2022.05.054
3. Takeuchi, H, Miyata, H, Gotoh, M, Kitagawa, Y, Baba, H, Kimura, W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. (2014) 260:259–66. doi: 10.1097/sla.0000000000000644
4. Yoshida, N, Yamamoto, H, Baba, H, Miyata, H, Watanabe, M, Toh, Y, et al. Can minimally invasive esophagectomy replace open esophagectomy for Esophageal Cancer? Latest analysis of 24,233 esophagectomies from the Japanese National Clinical Database. Ann Surg. (2020) 272:118–24. doi: 10.1097/sla.0000000000003222
5. Kubo, Y, Tanaka, K, Yamasaki, M, Yamashita, K, Makino, T, Saito, T, et al. The impact of perioperative fluid balance on postoperative complications after esophagectomy for Esophageal Cancer. J Clin Med. (2022) 11:11. doi: 10.3390/jcm11113219
6. Wang, W, Yu, Y, Sun, H, Wang, Z, Zheng, Y, Liang, G, et al. Predictive model of postoperative pneumonia after neoadjuvant immunochemotherapy for esophageal cancer. J Gastrointest Oncol. (2022) 13:488–98. doi: 10.21037/jgo-22-149
7. Molena, D, Mungo, B, Stem, M, and Lidor, AO. Incidence and risk factors for respiratory complications in patients undergoing esophagectomy for malignancy: a NSQIP analysis. Semin Thorac Cardiovasc Surg. (2014) 26:287–94. doi: 10.1053/j.semtcvs.2014.12.002
8. Yang, CK, Teng, A, Lee, DY, and Rose, K. Pulmonary complications after major abdominal surgery: National Surgical Quality Improvement Program analysis. J Surg Res. (2015) 198:441–9. doi: 10.1016/j.jss.2015.03.028
9. Yoshida, N, Morito, A, Nagai, Y, Baba, Y, Miyamoto, Y, Iwagami, S, et al. Clinical importance of sputum in the respiratory tract as a predictive marker of postoperative morbidity after esophagectomy for Esophageal Cancer. Ann Surg Oncol. (2019) 26:2580–6. doi: 10.1245/s10434-019-07477-7
10. Baba, Y, Yoshida, N, Shigaki, H, Iwatsuki, M, Miyamoto, Y, Sakamoto, Y, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. (2016) 264:305–11. doi: 10.1097/sla.0000000000001510
11. Saeki, H, Tsutsumi, S, Tajiri, H, Yukaya, T, Tsutsumi, R, Nishimura, S, et al. Prognostic significance of postoperative complications after curative resection for patients with Esophageal squamous cell carcinoma. Ann Surg. (2017) 265:527–33. doi: 10.1097/sla.0000000000001692
12. Su, J, Li, S, Sui, Q, and Wang, G. The influence of minimally invasive esophagectomy versus open esophagectomy on postoperative pulmonary function in esophageal cancer patients: a meta-analysis. J Cardiothorac Surg. (2022) 17:139. doi: 10.1186/s13019-022-01824-8
13. Gao, L, Su, S, Du, N, Han, Y, Wei, J, Cao, M, et al. Medical and non-medical students' knowledge, attitude and willingness towards the COVID-19 vaccine in China: a cross-sectional online survey. Hum Vaccin Immunother. (2022) 18:2073757. doi: 10.1080/21645515.2022.2073757
14. Twinamasiko, N, Olum, R, Gwokyalya, AM, Nakityo, I, Wasswa, E, and Sserunjogi, E. Assessing knowledge, attitudes and practices towards COVID-19 public health preventive measures among patients at Mulago National Referral Hospital. Risk Manag Healthc Policy. (2021) 14:221–30. doi: 10.2147/rmhp.S287379
15. Wang, J, Chen, L, Yu, M, and He, J. Impact of knowledge, attitude, and practice (KAP)-based rehabilitation education on the KAP of patients with intervertebral disc herniation. Ann Palliat Med. (2020) 9:388–93. doi: 10.21037/apm.2020.03.01
16. Lin, Y, Totsuka, Y, Shan, B, Wang, C, Wei, W, Qiao, Y, et al. Esophageal cancer in high-risk areas of China: research progress and challenges. Ann Epidemiol. (2017) 27:215–21. doi: 10.1016/j.annepidem.2016.11.004
17. Kröll, D, Borbély, YM, Dislich, B, Haltmeier, T, Malinka, T, Biebl, M, et al. Favourable long-term survival of patients with esophageal cancer treated with extended transhiatal esophagectomy combined with en bloc lymphadenectomy: results from a retrospective observational cohort study. BMC Surg. (2020) 20:197. doi: 10.1186/s12893-020-00855-z
18. Lorenzo, A, Goltsman, D, Apostolou, C, Das, A, and Merrett, N. Diabetes adversely influences postoperative outcomes after oesophagectomy: an analysis of the National Surgical Quality Improvement Program Database. Cureus. (2022) 14:e21559. doi: 10.7759/cureus.21559
19. Ajani, JA, D'Amico, TA, Bentrem, DJ, Chao, J, Corvera, C, Das, P, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2019) 17:855–83. doi: 10.6004/jnccn.2019.0033
20. Ajani, JA, D'Amico, TA, Bentrem, DJ, Cooke, D, Corvera, C, Das, P, et al. Esophageal and esophagogastric junction cancers, version 2.2023, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2023) 21:393–422. doi: 10.6004/jnccn.2023.0019
21. Ge, F, Huo, Z, Cai, X, Hu, Q, Chen, W, Lin, G, et al. Evaluation of clinical and safety outcomes of neoadjuvant immunotherapy combined with chemotherapy for patients with resectable esophageal cancer: a systematic review and meta-analysis. JAMA Netw Open. (2022) 5:e2239778. doi: 10.1001/jamanetworkopen.2022.39778
22. Salman, M, Mustafa, ZU, Rao, AZ, Khan, QU, Asif, N, Hussain, K, et al. Serious inadequacies in high alert medication-related knowledge among Pakistani nurses: findings of a large, multicenter, cross-sectional survey. Front Pharmacol. (2020) 11:1026. doi: 10.3389/fphar.2020.01026
23. Xie, L, Liu, Z, Hao, S, Wu, Q, Sun, L, Luo, H, et al. Assessment of knowledge, attitude, and practice towards pulmonary rehabilitation among COPD patients: a multicenter and cross-sectional survey in China. Respir Med. (2020) 174:106198. doi: 10.1016/j.rmed.2020.106198
24. Hao, S, Xie, L, Wang, H, Wu, Q, Jiang, P, Guo, C, et al. Respiratory physicians' awareness and referral of pulmonary rehabilitation in China: a cross-sectional study. J Thorac Dis. (2021) 13:4753–61. doi: 10.21037/jtd-20-2587
25. Gaddi, AV, and Lugaresi, M. Telemedicine: a unique, univocal, and shared definition for everyone. Artif Intell Surg. (2024) 4:37–43. doi: 10.20517/ais.2024.03
26. Peek, G, and Ross, SB. The future implementation of artificial intelligence technology in esophageal surgery. Artif Intell Surg. (2023) 3:249–54. doi: 10.20517/ais.2023.56
27. Talwar, A, Talwar, AA, Broach, RB, Ungar, LH, Hashimoto, DA, and Fischer, JP. Artificial intelligence unlocks the healthcare data lake. Artif Intell Surg. (2025) 5:239–46. doi: 10.20517/ais.2024.109
28. Jung, ME, Locke, SR, Bourne, JE, Beauchamp, MR, Lee, T, Singer, J, et al. Cardiorespiratory fitness and accelerometer-determined physical activity following one year of free-living high-intensity interval training and moderate-intensity continuous training: a randomized trial. Int J Behav Nutr Phys Act. (2020) 17:25. doi: 10.1186/s12966-020-00933-8
29. Pokhrel, P, Bennett, BL, and Boushey, CJ. Body esteem, weight-control outcome expectancies, and e-cigarette use among young adults. Nicotine Tob Res. (2021) 23:454–61. doi: 10.1093/ntr/ntaa009
30. He, T, Pu, YY, Zhang, YQ, Qian, ZB, Guo, LH, Sun, LP, et al. 5G-based telerobotic ultrasound system improves access to breast examination in rural and remote areas: a prospective and two-scenario study. Diagnostics. (2023) 13:362. doi: 10.3390/diagnostics13030362
31. Peng, MM, Ma, Z, and Ran, MS. Family caregiving and chronic illness management in schizophrenia: positive and negative aspects of caregiving. BMC Psychol. (2022) 10:83. doi: 10.1186/s40359-022-00794-9
32. Hajialibeigloo, R, Moradi, Y, Habibzadeh, H, Baghaei, R, Alinejad, V, and Namazi Nia, M. The COVID-19 patients' educational needs assessment questionnaire (COPENAQ): development and psychometrics. Health Qual Life Outcomes. (2022) 20:16. doi: 10.1186/s12955-022-01922-0
33. Lee, W, Park, JO, Hong, SO, and Kim, Y. Bicycle injury prevention education using 360° virtual reality experiences of accidents and computer-based activity. Children. (2022) 9:9. doi: 10.3390/children9111623
34. Gezimu, W, Bekele, F, and Habte, G. Pregnant mothers' knowledge, attitude, practice and its predictors towards nutrition in public hospitals of southern Ethiopia: a multicenter cross-sectional study. SAGE Open Med. (2022) 10:20503121221085843. doi: 10.1177/20503121221085843
35. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about Cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:21501319211063051. doi: 10.1177/21501319211063051
36. Torres, JM, Yang, Y, Rudolph, KE, and Courtin, E. Increased adult child schooling and older parents' health behaviors in Europe: a quasi-experimental study. SSM Popul Health. (2022) 19:101162. doi: 10.1016/j.ssmph.2022.101162
37. Dall'Oglio, I, Mascolo, R, Portanova, A, Ragni, A, Amadio, P, Fiori, M, et al. Staff perceptions of family-centered care in Italian neonatal intensive care units: a multicenter cross-sectional study. Children. (2022) 9:1401. doi: 10.3390/children9091401
38. Lyu, Y, Xu, Q, Yang, Z, and Liu, J. Prediction of patient choice tendency in medical decision-making based on machine learning algorithm. Front Public Health. (2023) 11:1087358. doi: 10.3389/fpubh.2023.1087358
39. Gressier, A, Gourier, G, Metges, JP, Dewitte, JD, Loddé, B, and Lucas, D. Occupational exposures and Esophageal Cancer: prog study. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19169782
40. Obermannová, R, Alsina, M, Cervantes, A, Leong, T, Lordick, F, Nilsson, M, et al. Oesophageal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. (2022) 33:992–1004. doi: 10.1016/j.annonc.2022.07.003
41. Zhang, X, Yang, X, Zhang, T, Yin, X, Man, J, and Lu, M. Association of educational attainment with esophageal cancer, Barrett's esophagus, and gastroesophageal reflux disease, and the mediating role of modifiable risk factors: a mendelian randomization study. Front Public Health. (2023) 11:1022367. doi: 10.3389/fpubh.2023.1022367
42. Lee, M, Kang, D, Kang, E, Kim, S, Kim, Y, Ahn, JS, et al. Efficacy of the PRO-CTCAE mobile application for improving patient participation in symptom management during cancer treatment: a randomized controlled trial. Support Care Cancer. (2023) 31:321. doi: 10.1007/s00520-023-07779-3
43. Yang, K, Oh, D, Noh, JM, Yoon, HG, Sun, JM, Kim, HK, et al. Feasibility of an interactive health coaching Mobile app to prevent malnutrition and muscle loss in Esophageal Cancer patients receiving neoadjuvant concurrent chemoradiotherapy: prospective pilot study. J Med Internet Res. (2021) 23:e28695. doi: 10.2196/28695
44. DiSiena, M, Perelman, A, Birk, J, and Rezaizadeh, H. Esophageal Cancer: an updated review. South Med J. (2021) 114:161–8. doi: 10.14423/smj.0000000000001226
Keywords: knowledge, attitude, practice, esophageal cancer, pulmonary rehabilitation, cross-sectional study
Citation: Wang W, Xing W, Chen P, Sun H, Wang Z, Zheng Y, Yu Y and Zeng D (2025) Knowledge, attitudes, and practices of esophageal cancer patients regarding pulmonary rehabilitation training. Front. Public Health. 13:1647650. doi: 10.3389/fpubh.2025.1647650
Edited by:
Hong Xiao, Fred Hutchinson Cancer Center, United StatesReviewed by:
Heba Taher, Cairo University, EgyptKulbhushan Thakur, University of Delhi, India
Yuxi Zhang, Nanjing Medical University, China
Copyright © 2025 Wang, Xing, Chen, Sun, Wang, Zheng, Yu and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenqun Xing, eHdxOTI2MzI3ODhAMTYzLmNvbQ==
 Wei Wang1
Wei Wang1 Wenqun Xing
Wenqun Xing Peinan Chen
Peinan Chen Haibo Sun
Haibo Sun Yan Zheng
Yan Zheng