- 1University Hospital Medical Information Network (UMIN) Center, The University of Tokyo Hospital, Tokyo, Japan
- 2Department of Health Communication, School of Public Health, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
- 3Teikyo University Graduate School of Public Health, Tokyo, Japan
Background: Health literacy has gained importance as a factor related to health behaviors and the risk of developing metabolic syndrome (MetS). Although the health literacy of family members may affect lifestyle habits among individuals with MetS, few studies have examined these relationships. We examined the associations between lifestyle habits (dietary habits, exercise, drinking, and smoking) among individuals with MetS and their family members’ health literacy.
Methods: We conducted a cross-sectional observational study at a Japanese machine manufacturing company using a self-administered questionnaire. Participants were recruited by the health insurance society based on the criterion of specific health guidance; and participants’ family members were also included in this study. Participants’ lifestyle habits were assessed on the basis of specific health checkup questionnaires. Health literacy was assessed using the Communicative and Critical Health Literacy scale. We used two binary logistic regression models to examine the associations of participants’ lifestyle habits with the health literacy of participants and their family members.
Results: We analyzed data for 125 participants with MetS and 125 family members. After adjusting for variables related to sociodemographic factors and occupation and workplace factors, participants’ exercise habits (moderate exercise, walking/equivalent physical activity) were significantly associated with participants’ health literacy (OR = 4.654, p < 0.001 and OR = 2.689, p = 0.001, respectively). After adjusting for variables related to sociodemographic factors, occupation and workplace factors, and participants’ health literacy, participants’ dietary habits (time dinner is eaten) and exercise habits (moderate exercise) were independently associated with family members’ health literacy (OR = 2.485, p = 0.006 and OR = 2.819, p = 0.034, respectively).
Conclusion: The findings suggested that health education for individuals with MetS as well as for their family members may be effective in improving dietary and exercise habits among individuals with MetS themselves. Additional intervention studies are needed to examine which educational model focusing on family is most effective in improving lifestyle habits among individuals with MetS.
1 Introduction
Metabolic syndrome (MetS) refers to a cluster of conditions (e.g., abdominal obesity, hypertension, hyperglycemia, elevated triglyceride levels, and reduced high-density lipoprotein cholesterol) that together substantially increase the risk of cardiovascular disease and type 2 diabetes (1). According to the International Diabetes Federation, the global prevalence of MetS among the general adult population is estimated to be between 20 and 25% (2). The World Health Organization also states that non-communicable conditions, including cardiovascular disease, type 2 diabetes and obesity, now account for roughly two-thirds of deaths worldwide (3). Thus, MetS represents an important public health concern.
In recent years, growing attention has been paid to the importance of health literacy in the prevention and management of MetS. Although definitions of health literacy are still evolving, one definition is “the personal skills that enable individuals to obtain, understand, and use information to make decisions and take actions that will impact their health” (4). Previous studies have consistently indicated that individuals with limited health literacy tend to have unhealthy lifestyles, poorer health self-management, and poorer health status (5–8). Thus, health literacy is closely associated with the adoption of lifestyle habits that help to prevent MetS (9).
Individuals with MetS tend to have lower levels of health literacy. Previous studies have suggested that low health literacy is associated with poor disease awareness, insufficient engagement in preventive behaviors such as engaging in physical activity and consuming a healthy diet, and deterioration of physical health status (10, 11). To address this issue, educational interventions (e.g., the distribution of informational pamphlets and verbal counseling) targeting individuals with MetS have been implemented. Previous reports have indicated improvements in clinical indicators such as body weight, waist circumference, and body mass index following lifestyle guidance (12, 13). However, such interventions targeting individuals with MetS are often influenced by individual factors such as receptiveness, motivation, and environmental conditions. Thus, the effectiveness of interventions in sustaining long-term behavioral change and disease management remains limited.
Individuals with MetS are influenced by their family members. Previous research has shown that emotional and practical support from family members—particularly spouses—can contribute to improved dietary and drinking habits, as well as to better clinical outcomes such as improved blood pressure, blood glucose, and lipid levels. (14–16). A previous report also suggested that family members’ knowledge about nutrition and physical activity may promote improvement in the patient’s own lifestyle (17).
Given these findings, family members’ health literacy may influence preventive behaviors and disease management in individuals with MetS. However, no studies to date have assessed health literacy among family members of individuals with MetS. Thus, it is unknown whether lifestyle habits in patients with MetS are associated with the health literacy of their family members. In this study, we aimed to examine the associations between lifestyle habits (dietary habits, exercise, alcohol consumption, and smoking) among individuals with MetS and the health literacy of their family members. The findings are expected to highlight the need for comprehensive support systems that include family involvement, as well as the importance of providing health education targeting family members. This study may contribute to the development of more effective and sustainable support models for the improvement of lifestyles among individuals with MetS.
2 Materials and methods
2.1 Study design
We conducted a cross-sectional observational study to examine the associations between lifestyle habits (dietary habits, exercise, alcohol consumption, and smoking) among middle-aged Japanese adults with MetS and the health literacy of their family members.
2.2 Study participants
Study participants were individuals with MetS who worked at a machine manufacturing company. Since 2008, specific health checkups are conducted by all health insurance societies in Japan for individuals aged 40 years or older with MetS to reduce the risk of cardiovascular disease (18, 19). On the basis of this criterion in the related guidance, our participants were recruited by the health insurance society. Because medical treatments and lifestyle guidance provided by medical practitioners can influence an individual’s lifestyle habits, we excluded individuals who had received medical treatment for blood glucose, blood pressure, and lipids. We finally included 275 individuals with MetS in this study.
2.3 Research methods
We conducted a survey using a self-administered questionnaire among the 275 included participants between September 9, 2024 and December 28, 2024. Self-administered questionnaires, instructions and information about participation in this study, and return-mail envelopes were sent to the home of these 275 participants on September 9, 2024 by the health insurance society. The questionnaire was sent again on October 10, 2024 to participants who had not returned a completed questionnaire to their employer. Participants and their family members (members of the participants’ family who were living in the same household and most supportive of participants’ health care) provided written informed consent via the self-administered questionnaires. Through December 28, 2024, a total of 165 out of 275 participants returned a completed questionnaire to the health insurance society (response rate, 59.9%). Among these 165 participants, 134 lived with family members; 125 family members of participants completed the questionnaire (response rate, 93.3%). Thus, 125 participants and 125 family members were included in the analysis.
2.4 Measures
2.4.1 Outcomes
We investigated participants’ lifestyle habits (dietary habits, exercise, alcohol consumption, and smoking status) using information provided by the health insurance society based on specific health checkup questionnaires (19). To assess dietary habits, participants were asked, “Do you skip breakfast more than 3 times a week?” and “Do you eat dinner at least 2 h before bedtime at least 3 times a week?” Similarly, to assess exercise habits, participants were asked, “Do you engage in moderate exercise—enough to work up a sweat—for at least 30 min at a time, at least 2 days a week for at least 1 year?” and “Do you perform walking or equivalent physical activity, daily for at least 1 h per day?” Additionally, to measure drinking habits, participants were asked, “How often do you drink alcohol (sake, shochu, beer, other liquor)?” and the amount of alcohol consumed per day, if consumed. Using the Ministry of Health, Labour and Welfare Healthy Japan 21 standards (20), we assessed whether participants’ daily alcohol intake was less than 20 g using their responses. If intake was less than 20 g per day, the participant was defined as drinking an appropriate amount of alcohol. Finally, to measure smoking status, participants were asked, “Do you currently smoke cigarettes?”
2.4.2 Covariates
2.4.2.1 Health literacy
We measured health literacy among participants and their family members using a scale developed and validated in Japan to assess communicative and critical health literacy (21). The scale includes three items on communicative health literacy and two on critical health literacy. Participants were asked whether they could do the following: (i) obtain health-related information from various sources; (ii) extract the required information; (iii) understand and communicate the information obtained; (iv) assess the reliability of the information; (v) make decisions based on the information, specifically in the context of health-related issues. We rated each item on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Scores for the five items were summed and divided by 5 to yield a scale score (theoretical range: 1–5). The internal consistency of the scale was adequate (Cronbach’s α = 0.86).
2.4.2.2 Personal factors
To investigate participants’ personal factors, we assessed sex (male or female), age (40–49 years, 50–59 years, ≥60 years), education level (junior or senior high school, higher professional school/vocational school/junior college, college or graduate school), marital status (single, married, divorced or widowed), parenting and caregiving responsibilities (parenting responsibilities, caregiving responsibilities, parenting and caregiving responsibilities, no parenting or caregiving responsibilities), relationships with family members (spouse, mother, father, child, other), and household income (<4.0 million JPY, 4.0–8.0 million JPY, >8.0 million JPY) to determine participants’ socioeconomic status.
2.4.2.3 Occupation and workplace factors
To investigate factors related to participants’ occupation and workplace, we assessed their employment status (permanent employee, contracted employee/non-permanent employee), work format (shift work, no shift work), overtime (<1.0 h per day, 1.0–1.9 h per day, 2.0–2.9 h per day, ≥3.0 h per day), and type of work (production line work, clerical position, junior position, managerial position, other).
2.5 Statistical analysis
Bivariate association between participants’ and family members’ health literacy was examined using Pearson correlation analysis. We used the independent samples t-test to examine univariate associations among participants’ lifestyle habits and participants’ and family members’ health literacy. We then used two binary logistic regression models to examine the associations between participants’ lifestyle habits and the health literacy of participants and their family members. We set each participant’s lifestyle habits as the dependent variable in these logistic regression models. In Model 1, we examined the associations between participants’ lifestyle habits and participants’ health literacy, controlling for seven variables related to sociodemographic factors as well as variables related to occupation and workplace; these variables have been shown in previous studies to be significantly associated with lifestyle factors. In Model 2, we examined the associations between participants’ lifestyle habits and their family members’ health literacy, controlling for the same variables as in Model 1 and participants’ health literacy. We analyzed the data using IBM SPSS version 21.0 (IBM Corp., Armonk, NY, United States).
2.6 Ethical considerations
The study was approved by the ethical review committee of the Graduate School of Medicine, The University of Tokyo (examination number 2024174NI).
3 Results
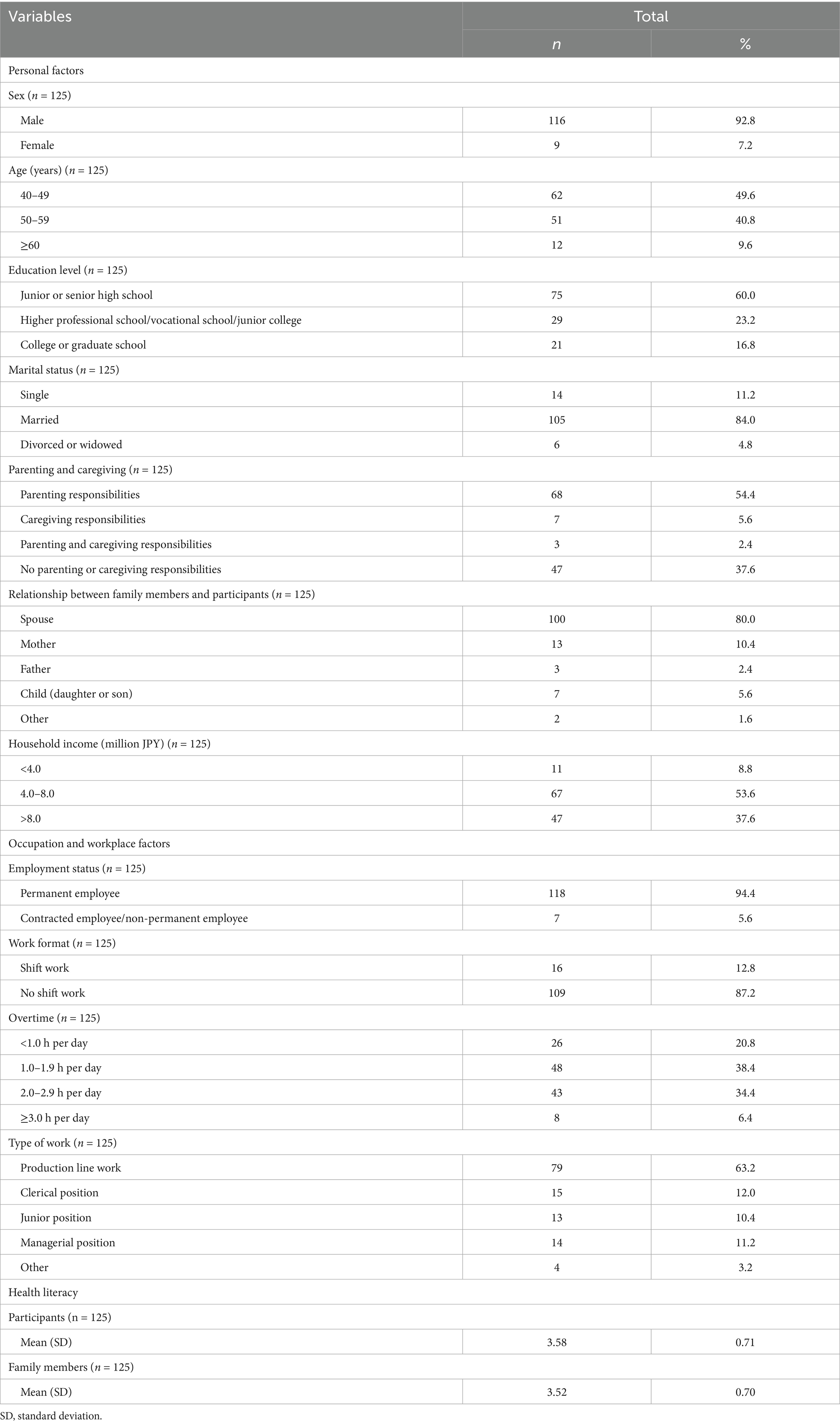
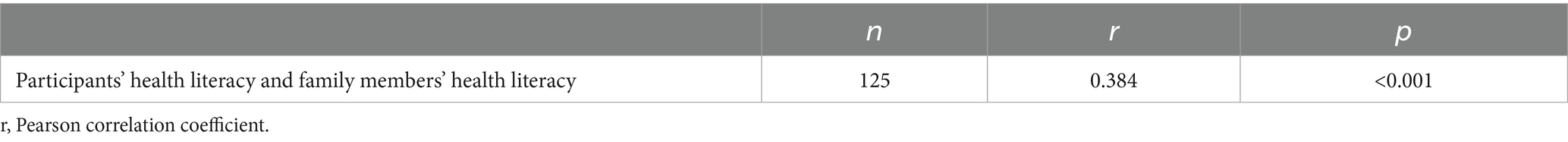
Table 1 shows the characteristics and health literacy scores for participants and their family members. A total of 116 (92.8%) participants were men, 62 (49.6%) were in their 40s, 105 (84.0%) were married, and 109 (87.2%) were not shift workers. In 100 participants (80.0%), the family member who completed the survey was the participant’s spouse. The mean participant and family member health literacy scores were 3.58 (standard deviation [SD] 0.71) and 3.52 (SD 0.70). Table 2 shows the bivariate association between participants’ and family members’ health literacy. The health literacy score for family members was positively correlated with the health literacy score of participants (r = 0.384, p < 0.001). Table 3 shows the univariate associations between participants’ lifestyle habits and participants’ and family members’ health literacy. Among participants, 46 (37.1%) ate dinner at least 2 h before bedtime at least 3 times a week, 38 (30.6%) performed walking or equivalent physical activity each day for at least 1 h daily, and 43 (34.4%) were smokers. We found univariate associations between participants’ health literacy and participants’ exercise habits (moderate exercise and walking or equivalent physical activity). We also found univariate associations between family members’ health literacy and participants’ dietary habits (time dinner is eaten), exercise habits (moderate exercise, walking or equivalent physical activity), and smoking status. Table 4 shows the results of binary logistic regression analysis. After adjusting for seven variables related to sociodemographic factors and occupation and workplace factors, we found that participants’ exercise habits (moderate exercise, walking or equivalent physical activity) were significantly associated with participants’ health literacy (OR = 4.654, p < 0.001 and OR = 2.689, p = 0.001, respectively) (Model 1). Additionally, we found that participants’ dietary habits (dinner time) and exercise habits (moderate exercise) were independently associated with family members’ health literacy (OR = 2.485, p = 0.006 and OR = 2.819, p = 0.034, respectively) (Model 2).
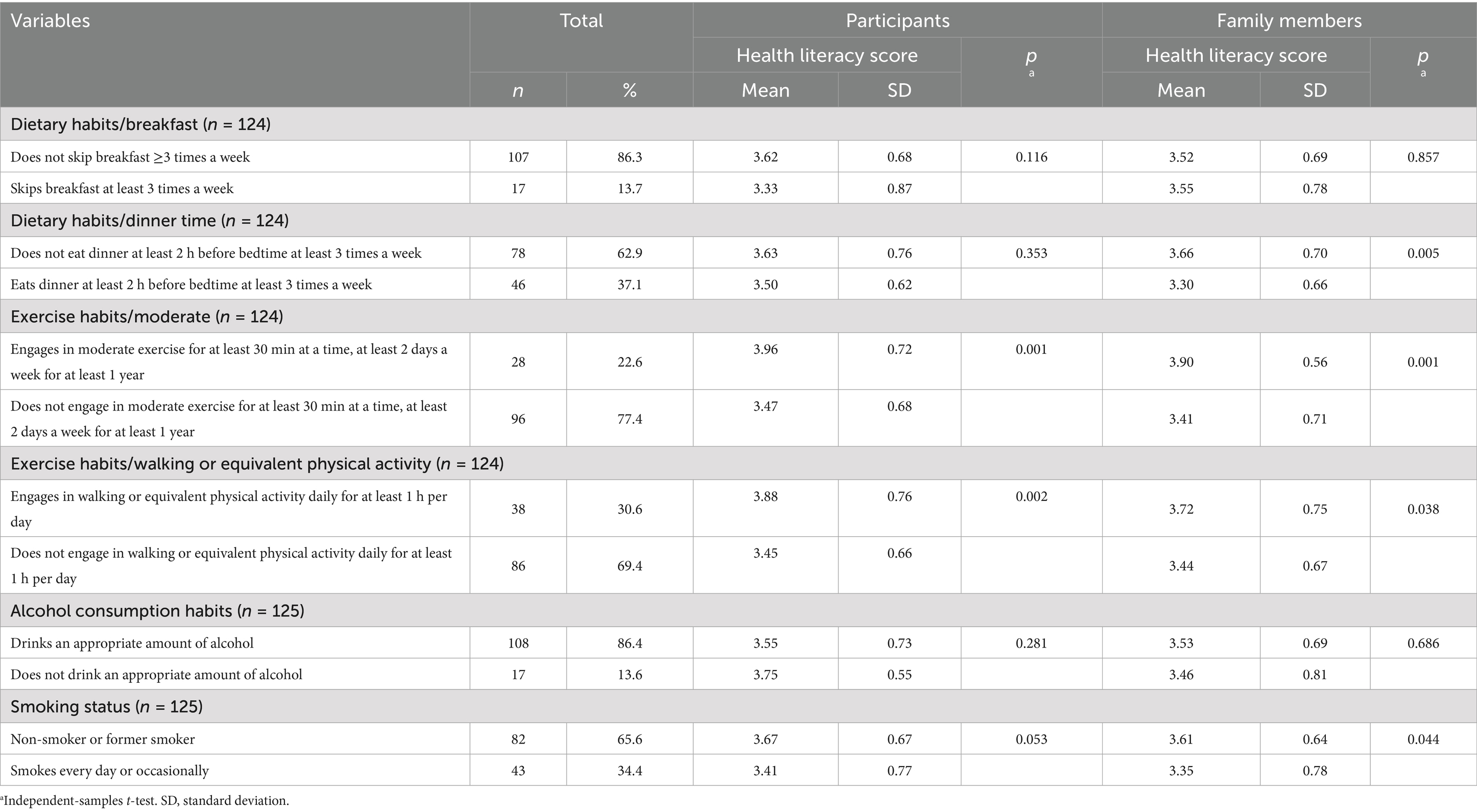
Table 3. Univariate associations of participants’ lifestyle habits with health literacy of participants and their family members (n = 125).
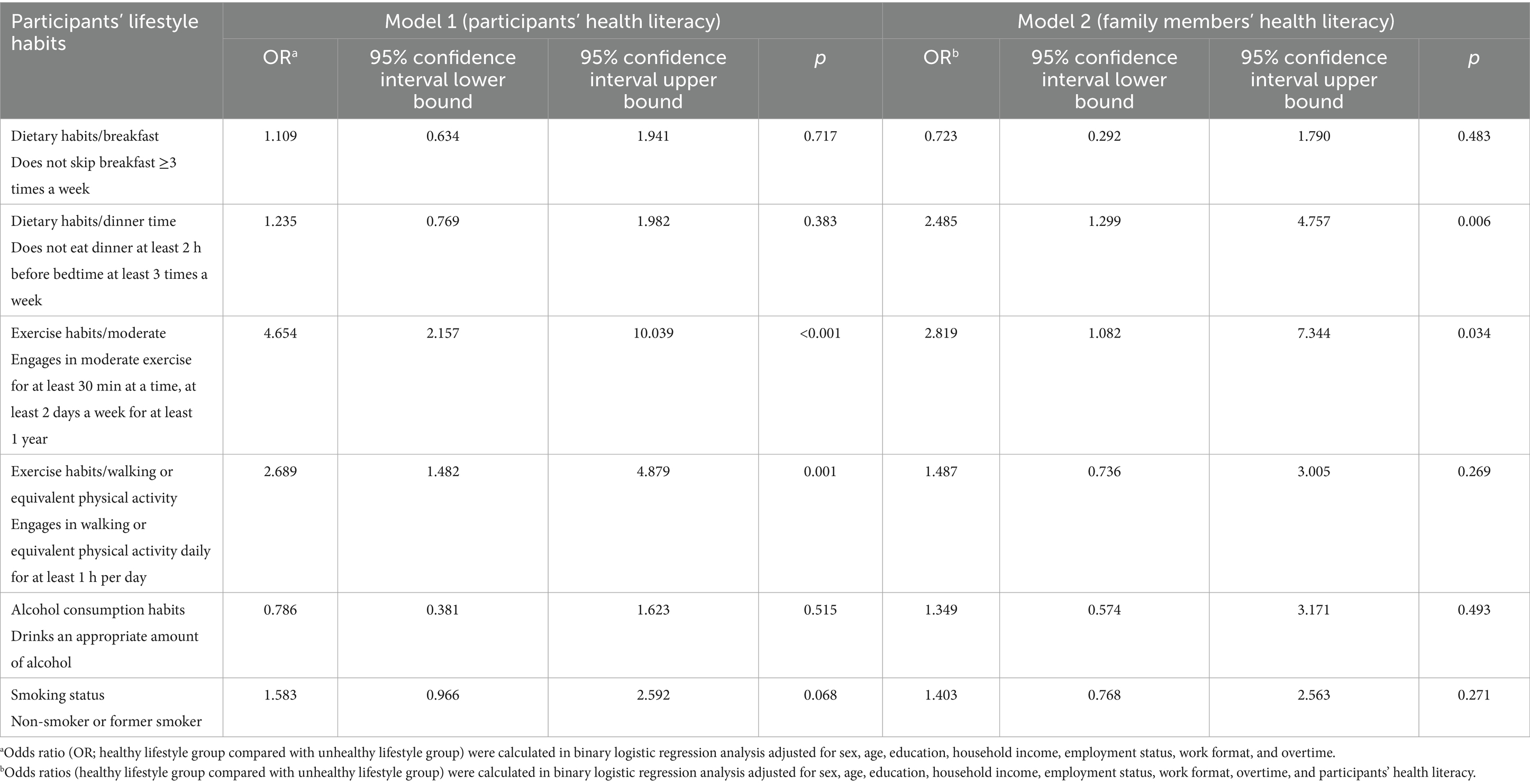
Table 4. Associations between participants’ lifestyle habits and health literacy of participants and their family members (n = 125).
4 Discussion
In this study, we examined the associations of lifestyle habits among MetS in middle-aged adults and their family members’ health literacy. Compared with the results of specific health checkups conducted for all Japanese citizens aged 40 years and older, the participants in this study had lower rates of skipping breakfast 3 or more times a week, eating dinner at least 2 h before bedtime at least 3 times a week, engaging in moderate exercise, and engaging in walking or equivalent activity each day for at least 1 h daily (22). The mean health literacy scores among participants’ family members were 3.52 (SD 0.70). This score is comparable to the findings of a previous study conducted among 501 pairs of Japanese residents aged 30–79 years and family members with whom participants most often consulted for help with health issues (mean ± SD 3.50 ± 0.77) (23). The health literacy score of family members was positively correlated with participants’ health literacy score. This finding is consistent with those of a previous study that identified a close correlation of family members’ health literacy with participants’ health literacy (23). In the present study, family members’ health literacy was independently associated with participants’ dietary habits (time dinner is eaten) and exercise habits (moderate exercise).
Our study participants who lived in the same household as family members who had better health literacy tended to eat dinner at least 2 h before bedtime, at least 3 times a week, as compared with those whose family members had poorer health literacy. According to a survey conducted by the Statistics Bureau of the Ministry of Internal Affairs and Communications, married Japanese women spend 14.6 times more time managing meals than husbands (24), and it has been reported that many employed women in Japan are responsible for meal management (25). In our study, 80.0% of participants reported that their cohabiting spouse was the person most concerned about their health, and 92.8% of the participants were men. Thus, it is possible that many of our participants were married men living with their wives and that they typically consumed dinners prepared by their spouse. Thus, participants who lived with family members—particularly wives—who had high health literacy may have had dinner served and consumed at appropriate times, regardless of their own level of health literacy. In general, eating dinner close to bedtime is associated with lifestyle-related diseases, including MetS (26). Enhancing the health literacy of family members may reduce the risk of worsening metabolic syndrome and associated cardiovascular diseases among individuals with MetS through optimization of their mealtimes.
Our study participants who lived in the same household as family members with better health literacy tended to engage in moderate physical activity, as compared with those whose family members had poorer health literacy. Previous studies have suggested that family support is a predictive factor of exercise adherence (27) and is associated with persistent or increasing physical activity (28). Previous studies have revealed that individuals benefit from the “distributed nature” of health literacy through shared knowledge, supported skills and practices, supported behaviors, and supported decision-making provided by health literacy mediators belonging to their social networks (23, 29). Thus, participants who lived with family members who had high health literacy may have been more likely to engage in physical activity, as they were more likely to receive support for decision-making and adherence related to exercise from their family members.
This study has several limitations. First, because this was a cross-sectional observational study, we were unable to determine causal relationships among the determinants of participants’ lifestyle habits. Second, participants were recruited from only one company. Additionally, our study population was limited to those over 40 years of age. The generalizability of our findings should be approached with caution based on these sample characteristics. Third, contrary to previous reports measuring functional health literacy, we assessed interactive and critical health literacy. The mean participant health literacy score was 3.58 (SD 0.71), which is lower than that found in a study of Japanese office workers (N = 190; mean ± SD 3.72 ± 0.68) (21). The scores obtained in this study were also lower than those in a nationwide online survey of the general Japanese population, which included older adults (N = 712; mean ± SD 3.59 ± 0.62) (30). Fewer participants in the present study may have had sufficient health literacy to engage in behaviors to protect their health; thus, participants’ lifestyle may have been more easily influenced by their family members’ health literacy. Fourth, most participants in this study were men. Thus, the findings may have differed if the study population included more female participants. Future research should include women to evaluate potential sex-based differences.
5 Conclusion
Despite the above limitations, we explored the associations between lifestyle habits among middle-aged adults with MetS and their family members’ health literacy. In our study, participants’ dietary habits (time dinner was eaten) and exercise habits (moderate exercise) were independently associated with their family members’ health literacy. Our results indicate that health education for individuals with MetS as well as their family members may be effective in improving dietary and exercise habits among individuals with MetS themselves. To address the development of sustainable support models for individuals with MetS, further research is needed to examine the effects of family health education on individuals’ improvement in lifestyles habits.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the ethical review committee of the Graduate School of Medicine, The University of Tokyo (examination number 2024174NI). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants.
Author contributions
EG: Methodology, Writing – original draft, Formal analysis, Investigation, Visualization, Data curation, Resources, Validation, Software, Supervision, Writing – review & editing, Conceptualization, Project administration, Funding acquisition. HO: Project administration, Validation, Data curation, Visualization, Methodology, Formal analysis, Software, Conceptualization, Resources, Investigation, Supervision, Writing – review & editing, Funding acquisition, Writing – original draft. HI: Funding acquisition, Supervision, Writing – review & editing, Validation, Formal analysis, Software, Methodology, Data curation, Writing – original draft, Project administration, Conceptualization, Investigation, Visualization, Resources.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Japan Society for the Promotion of Science KAKENHI (no. 23K12892).
Acknowledgments
We would like to thank all study participants. We thank Analisa Avila, MPH, ELS, of Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mottillo, S, Filion, KB, Genest, J, Joseph, L, Pilote, L, Poirier, P, et al. The metabolic syndrome and cardiovascular risk. A systematic review and meta-analysis. J Am Coll Cardiol. (2010) 56:1113–32. doi: 10.1016/j.jacc.2010.05.034
2. Alberti, KG, Zimmet, P, and Shaw, J. Metabolic syndrome--a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. (2006) 23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x
3. Riley, L, Guthold, R, Cowan, M, Savin, S, Bhatti, L, Armstrong, T, et al. The World Health Organization STEPwise approach to noncommunicable disease risk-factor surveillance: methods, challenges, and opportunities. Am J Public Health. (2016) 106:74–8. doi: 10.2105/AJPH.2015.302962
4. Nutbeam, D, Levin-Zamir, D, and Rowlands, G. Health literacy in context. Int J Environ Res Public Health. (2018) 15:2657. doi: 10.3390/ijerph15122657
5. Papadakos, JK, Hasan, SM, Barnsley, J, Berta, W, Fazelzad, R, Papadakos, CJ, et al. Health literacy and cancer self-management behaviors: a scoping review. Cancer. (2018) 124:4202–10. doi: 10.1002/cncr.31733
6. Sørensen, K, Van den Broucke, S, Fullam, J, Doyle, G, Pelikan, J, Slonska, Z, et al. (HLS-EU) consortium health literacy project European. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80
7. Rasu, RS, Bawa, WA, Suminski, R, Snella, K, and Warady, B. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. (2015) 4:747–55. doi: 10.15171/ijhpm.2015.151
8. Kim, K, and Han, HR. Potential links between health literacy and cervical cancer screening behaviors: a systematic review. Psychooncology. (2016) 25:122–30. doi: 10.1002/pon.3883
9. Yokokawa, H, Fukuda, H, Yuasa, M, Sanada, H, Hisaoka, T, and Naito, T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetol Metab Syndr. (2016) 8:30. doi: 10.1186/s13098-016-0142-8
10. Peiris, C, Harding, K, Porter, J, Shields, N, Gilfillan, C, and Taylor, N. Understanding the hidden epidemic of metabolic syndrome in people accessing community rehabilitation: a cross-sectional study of physical activity, dietary intake, and health literacy. Disabil Rehabil. (2023) 45:1471–9. doi: 10.1080/09638288.2022.2065540
11. Peltzer, S, Hellstern, M, Genske, A, Jünger, S, Woopen, C, and Albus, C. Health literacy in persons at risk of and patients with coronary heart disease: a systematic review. Soc Sci Med. (2020) 245:112711. doi: 10.1016/j.socscimed.2019.112711
12. Shackelford, S. Lifestyle intervention in primary care patients with metabolic syndrome. J Clin Lipidol. (2023) 17:e49. doi: 10.1016/j.jacl.2023.05.073
13. Tejera, C, Porca, C, Rodriguez-Carnero, G, Andújar, P, Casanueva, FF, Bellido, D, et al. Reducing metabolic syndrome through a group educational intervention program in adults with obesity: IGOBE program. Nutrients. (2022) 14:1066. doi: 10.3390/nu14051066
14. Umberson, D. Family status and health behaviors: social control as a dimension of social integration. J Health Soc Behav. (1987) 28:306–19. doi: 10.2307/2136848
15. Lewis, MA, and Rook, KS. Social control in personal relationships: impact on health behaviors and psychological distress. Health Psychol. (1999) 18:63–71. doi: 10.1037/0278-6133.18.1.63
16. Nam, HK, Chang, SJ, Kim, CB, Jeong, KS, Kim, SK, Kang, DR, et al. The association between social support, metabolic syndrome, and incidence of cardio-cerebrovascular diseases in older adults: the ARIRANG study. Yonsei Med J. (2024) 65:363–70. doi: 10.3349/ymj.2023.0455
17. Ho, YL, Mahirah, D, Ho, CZ, and Thumboo, J. The role of the family in health promotion: a scoping review of models and mechanisms. Health Promot Int. (2022) 37:daac119. doi: 10.1093/heapro/daac119
18. Tsushita, K, Hosler, SA, Miura, K, Ito, Y, Fukuda, T, Kitamura, A, et al. Rationale and descriptive analysis of specific health guidance: the Nationwide lifestyle intervention program targeting metabolic syndrome in Japan. J Atheroscler Thromb. (2018) 25:308–22. doi: 10.5551/jat.42010
19. Japanese Ministry of Health, Labour and Welfare. Guidance for smooth implementation of specific health examination and specific health guidance (version 4.1). Available online at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/handbook_31132.html (accessed May 13, 2025)
20. Ministry of Health, Labour and Welfare. Healthy Japan 21 standards. Available online at: https://www.mhlw.go.jp/www1/topics/kenko21_11/b5.html#A52 (accessed May 13, 2025)
21. Ishikawa, H, Nomura, K, Sato, M, and Yano, E. Developing a measure of communicative and critical health literacy: a pilot study of Japanese office workers. Health Promot Int. (2008) 23:269–74. doi: 10.1093/heapro/dan017
22. Survey analysis of the medical insurance group, production department, Federation of Health Insurance Associations. Survey on the questionnaire responses for the specific health examination in fiscal year (2008). Available online at: https://www.kenporen.com/toukei_data/pdf/chosa_r02_11_04-3.pdf (accessed May 13, 2025)
23. Ishikawa, H, and Kiuchi, T. Association of health literacy levels between family members. Front Public Health. (2019) 7:169. doi: 10.3389/fpubh.2019.00169
24. Statistics Bureau of Japan. (2017). 2016 survey on time use and leisure activities. Ministry of Internal Affairs and Communications. Available online at: https://www.stat.go.jp/data/shakai/2016/kekka.html (accessed May 13, 2025)
25. Statistics Bureau of Japan. (2022). 2021 survey on time use and leisure activities. Ministry of Internal Affairs and Communications. Available online at: https://www.stat.go.jp/data/shakai/2021/kekka.html (accessed May 13, 2025)
26. Yoshida, J, Eguchi, E, Nagaoka, K, Ito, T, and Ogino, K. Association of night eating habits with metabolic syndrome and its components: a longitudinal study. BMC Public Health. (2018) 18:1366. doi: 10.1186/s12889-018-6262-3
27. Ormel, HL, van der Schoot, GGF, Sluiter, WJ, Jalving, M, Gietema, JA, and Walenkamp, AME. Predictors of adherence to exercise interventions during and after cancer treatment: a systematic review. Psychooncology. (2018) 27:713–24. doi: 10.1002/pon.4612
28. Lounassalo, I, Salin, K, Kankaanpää, A, Hirvensalo, M, Palomäki, S, Tolvanen, A, et al. Distinct trajectories of physical activity and related factors during the life course in the general population: a systematic review. BMC Public Health. (2019) 19:271. doi: 10.1186/s12889-019-6513-y
29. Edwards, M, Wood, F, Davies, M, and Edwards, A. 'Distributed health literacy': longitudinal qualitative analysis of the roles of health literacy mediators and social networks of people living with a long-term health condition. Health Expect. (2015) 18:1180–93. doi: 10.1111/hex.12093
Keywords: metabolic syndrome, lifestyle factors, family, health literacy, family health education
Citation: Goto E, Okada H and Ishikawa H (2025) Associations between lifestyle habits and family members’ health literacy in middle-aged adults with metabolic syndrome: a cross-sectional study in Japan. Front. Public Health. 13:1648414. doi: 10.3389/fpubh.2025.1648414
Edited by:
Uday Venkat Mateti, NGSM Institute of Pharmaceutical Sciences, Nitte (Deemed to be University), IndiaReviewed by:
Dana Teodora Anton Paduraru, Grigore T. Popa University of Medicine and Pharmacy, RomaniaPiotr Toczyski, The Maria Grzegorzewska University, Poland
Copyright © 2025 Goto, Okada and Ishikawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eiko Goto, Z290b3VlLXRreUB1bWluLmFjLmpw
 Eiko Goto
Eiko Goto Hiroko Okada
Hiroko Okada Hirono Ishikawa
Hirono Ishikawa